Comparative Analysis of Ubiquitination Pathways in Cancer: From Molecular Mechanisms to Precision Therapeutics
Ubiquitination, a crucial post-translational modification, is profoundly dysregulated across cancer types, influencing tumorigenesis, progression, and therapeutic response.
Comparative Analysis of Ubiquitination Pathways in Cancer: From Molecular Mechanisms to Precision Therapeutics
Abstract
Ubiquitination, a crucial post-translational modification, is profoundly dysregulated across cancer types, influencing tumorigenesis, progression, and therapeutic response. This review provides a comprehensive comparative analysis of ubiquitination pathway alterations in diverse cancers. We explore the foundational biology of the ubiquitin-proteasome system and examine advanced methodological approaches for profiling the cancer ubiquitinome. The article addresses key challenges in the field and discusses innovative strategies for targeting ubiquitination pathways therapeutically. Through a cross-cancer lens, we validate prognostic ubiquitination signatures and synthesize insights that bridge fundamental research with emerging clinical applications, including proteolysis-targeting chimeras (PROTACs) and immunotherapy combination strategies. This synthesis aims to equip researchers and drug developers with a holistic understanding of ubiquitination as a central regulatory node in cancer biology.
The Ubiquitin-Proteasome System: Core Machinery and Cancer-Specific Alterations
The ubiquitin-proteasome system (UPS) stands as one of the most crucial regulatory mechanisms in eukaryotic cells, governing the precise degradation of intracellular proteins to maintain cellular homeostasis [1]. At the heart of this system operates a finely tuned enzymatic cascade comprising three core enzyme classes: E1 (ubiquitin-activating), E2 (ubiquitin-conjugating), and E3 (ubiquitin-ligating) enzymes [2] [3]. This sequential pathway conjugates the small protein modifier ubiquitin to specific substrate proteins, thereby dictating their stability, activity, or localization [4]. The specificity of this system, particularly conferred by the extensive E3 ligase family, allows for the selective regulation of virtually every cellular process, from cell cycle progression and DNA repair to signal transduction and immune responses [3] [5]. In cancer biology, this pathway becomes critically dysregulated, with aberrant ubiquitination patterns contributing directly to sustained proliferation, evasion of apoptosis, and other hallmark capabilities of cancer cells [3] [5]. A comparative analysis across malignancies reveals both common themes and cancer-specific adaptations in how the ubiquitination cascade is co-opted during oncogenesis, presenting compelling opportunities for therapeutic intervention.
The Core Enzymatic Machinery: E1, E2, and E3
The ubiquitination cascade is a three-step enzymatic process that culminates in the covalent attachment of ubiquitin to substrate proteins.
The Sequential Catalytic Steps
The process initiates with the E1 ubiquitin-activating enzyme, which activates ubiquitin in an ATP-dependent reaction to form an E1~ubiquitin thioester intermediate [6]. In humans, only two E1 enzymes, UBA1 and UBA6, initiate the majority of ubiquitination cascades, highlighting a key regulatory bottleneck [7]. The activated ubiquitin is then transferred to the catalytic cysteine residue of an E2 ubiquitin-conjugating enzyme (UBC) via a transthioesterification reaction [6]. Structural analyses reveal that this transfer is facilitated by specific residues in the E1 enzyme, such as Thr601 and Arg603, which help stabilize the reactive transition state and modify the pKa of the incoming E2 nucleophile [6]. The human genome encodes approximately 40 E2s, which begin to impart some specificity to the pathway [8].
The final and most specific step involves the E3 ubiquitin ligase, which mediates the transfer of ubiquitin from the E2 to a lysine residue on the target protein. With over 600 members identified, E3 ligases are responsible for substrate recognition and confer the remarkable specificity of the ubiquitin system [3]. They accomplish this through specialized domains that recognize specific peptide motifs, or degrons, within their target substrates [3]. These degrons include phospho-degrons, proline-rich motifs, and other structural features that ensure precise substrate selection.
Table 1: Core Components of the Ubiquitination Enzymatic Cascade
| Component | Number in Humans | Core Function | Catalytic Mechanism |
|---|---|---|---|
| E1 (Activating) | 2 (UBA1, UBA6) | Ubiquitin activation via ATP hydrolysis | Forms E1~Ub thioester via adenylation |
| E2 (Conjugating) | ~40 | Ubiquitin carrier and E3 cooperation | E2~Ub thioester intermediate |
| E3 (Ligating) | >600 | Substrate recognition and specificity | Direct or indirect ubiquitin transfer to substrate |
Structural and Mechanistic Diversity of E3 Ligases
E3 ubiquitin ligases are categorized into three major families based on their structural features and catalytic mechanisms [3]. The RING (Really Interesting New Gene) finger family represents the largest group and functions by directly catalyzing the transfer of ubiquitin from the E2~Ub complex to the substrate without forming a covalent intermediate [3]. Notable subtypes include the multisubunit Cullin-RING ligases (CRLs) and the Anaphase Promoting Complex/Cyclosome (APC/C) [3]. In contrast, HECT (Homologous to the E6AP C Terminus) family E3s form a catalytic thioester intermediate with ubiquitin before transferring it to the substrate [3]. The RING-between-RING (RBR) family employs a hybrid mechanism, utilizing RING domains for E2 binding and a catalytic cysteine similar to HECT ligases for ubiquitin transfer [3]. This mechanistic diversity enables precise temporal and spatial control over protein ubiquitination, allowing the system to regulate a vast array of cellular processes.
Comparative Analysis of Ubiquitination Pathways Across Cancers
Dysregulation of the ubiquitination cascade is a hallmark of numerous malignancies, though the specific components affected and functional consequences vary significantly across cancer types.
Glioblastoma: E3 Ligases in Pro-Survival Signaling and Therapeutic Resistance
In glioblastoma (GB), E3 ubiquitin ligases play multifaceted roles in promoting tumor survival and resistance to standard therapies. Receptor tyrosine kinase (RTK) signaling, particularly through EGFR, is aberrantly regulated by several E3 ligases in GB [5]. Casitas B-lineage lymphoma (Cbl), a well-characterized E3, normally targets activated EGFR for degradation via ubiquitination; however, in GB, the constitutively active EGFRvIII mutant displays hypophosphorylation at the Cbl docking site (Y1045), attenuating Cbl-dependent internalization and degradation and leading to sustained oncogenic signaling [5]. Furthermore, the E3 ligase PARK2, frequently lost or mutated in GB, normally suppresses EGFR expression through direct ubiquitination and degradation, with its loss contributing to enhanced EGFR signaling [5]. The β-TrCP E3 ligase complex regulates Akt signaling by targeting the phosphatase PHLPP1 for degradation, thereby enhancing pro-survival signaling pathways in GB cells [5]. These alterations collectively promote tumor progression and represent potential therapeutic vulnerabilities.
Cervical Cancer: HPV Oncoprotein Subversion of the Ubiquitin Cascade
HPV-driven cervical cancer provides a striking example of viral subversion of the host ubiquitination machinery. The viral oncoproteins E6 and E7 directly interact with and manipulate cellular E3 ligases to promote viral persistence and cellular transformation [8]. Specifically, HPV E6 recruits the cellular E3 ligase E6AP to form a complex that targets the tumor suppressor p53 for ubiquitination and proteasomal degradation, effectively disabling a critical checkpoint against uncontrolled proliferation [8]. Meanwhile, HPV E7 promotes the degradation of the retinoblastoma protein (pRb) through another E3 ligase complex, driving aberrant cell cycle progression [8]. Recent bioinformatic studies have identified specific ubiquitination-related genes, including MMP1, RNF2, TFRC, SPP1, and CXCL8, that are significantly associated with cervical cancer outcomes and can stratify patient risk [1]. The risk score model developed from these biomarkers demonstrates strong predictive value for patient survival (AUC >0.6 for 1/3/5 years), highlighting the clinical relevance of ubiquitination pathways in this malignancy [1].
Pan-Cancer Commonalities and Distinctions
Across cancer types, several common themes emerge in the dysregulation of the ubiquitination cascade. First, E3 ligases frequently function as tumor suppressors when their normal role is to degrade oncoproteins, with their loss or inactivation leading to stabilization of drivers such as c-Myc, β-catenin, and cyclins [3]. Second, certain E3 ligases can act as oncoproteins when overexpressed or hyperactive, leading to excessive degradation of tumor suppressors like p53, p27, and PTEN [3]. Third, the specificity of E3 ligases makes them attractive therapeutic targets, with both small-molecule inhibitors and proteolysis-targeting chimeras (PROTACs) being actively explored across multiple cancer types [5]. However, tissue-specific expression patterns of E2 and E3 enzymes, differential substrate availability, and distinct mutational backgrounds create cancer-type specific vulnerabilities that necessitate comparative analyses for effective therapeutic development.
Table 2: Comparative Analysis of Ubiquitination Cascade Alterations Across Cancer Types
| Cancer Type | Key Altered Components | Functional Consequences | Clinical/Prognostic Relevance |
|---|---|---|---|
| Glioblastoma | Cbl, PARK2, β-TrCP, CHIP | Dysregulated RTK signaling, enhanced PI3K/Akt pathway, resistance to therapy | Associated with stemness and therapeutic resistance; potential for PROTAC-based therapies |
| Cervical Cancer | E6AP, UBE2 enzymes, MMP1, RNF2, TFRC | p53 and pRb degradation, sustained proliferation, immune evasion | 5-gene signature predicts survival (AUC>0.6); associated with immune cell infiltration |
| Multiple Cancers | CRL complexes, APC/C, MDM2 | Cell cycle dysregulation, genomic instability, evasion of growth suppression | Common therapeutic target across malignancies; small-molecule inhibitors in development |
Experimental Approaches for Profiling Ubiquitination Cascades
Proximity Labeling for Mapping Localized Ubiquitination Networks
Recent advances in proximity labeling technologies have revolutionized our ability to profile ubiquitination cascades in specific cellular compartments. The iAPEX (in situ APEX activation) system represents a significant innovation that combines APEX2 with a D-amino acid oxidase (DAAO) to locally generate hydrogen peroxide, thereby minimizing toxicity and reducing non-specific background labeling associated with traditional APEX approaches [9]. This enzyme cascade enables sensitive and specific proteomic mapping in challenging biological systems, including primary cilia, mitochondria, and lipid droplets [9]. The experimental workflow involves: (1) fusing DAAO to a specific organelle or protein complex of interest; (2) co-expressing or fusing APEX2 to the same location; (3) providing D-amino acids (e.g., D-Ala) to drive local H2O2 production; (4) adding biotin-tyramide to enable APEX2-mediated biotinylation of proximal proteins; and (5) streptavidin-based purification and mass spectrometric identification of labeled proteins [9]. This approach has been successfully applied to profile the proteomes of primary cilia in cell lines previously inaccessible to conventional APEX labeling, identifying novel ciliary proteins and revealing heterogeneity in primary cilia composition across cell types [9].
Bioinformatics Approaches for Ubiquitination Signature Identification
Computational methods have been developed to identify ubiquitination-related gene signatures with prognostic significance in cancer. As demonstrated in cervical cancer research, the typical workflow involves: (1) identifying differentially expressed genes (DEGs) between tumor and normal samples across multiple datasets; (2) intersecting these DEGs with known ubiquitination-related genes (UbLGs) to identify key crossover genes; (3) applying univariate Cox regression and LASSO algorithms to identify prognostic biomarkers; (4) constructing a risk score model based on biomarker expression; and (5) validating the model using independent datasets and functional assays such as RT-qPCR [1]. This approach successfully identified a five-gene ubiquitination-related signature (MMP1, RNF2, TFRC, SPP1, and CXCL8) that effectively stratifies cervical cancer patients into high- and low-risk groups with significant differences in survival outcomes [1]. Furthermore, immune infiltration analyses revealed that this ubiquitination-related signature correlates with distinct immune microenvironments, including differences in memory B cells, M0 macrophages, and immune checkpoint expression [1].
The Scientist's Toolkit: Essential Research Reagents and Methodologies
Table 3: Essential Research Reagents for Studying the Ubiquitination Cascade
| Reagent/Method | Primary Function | Key Applications | Technical Considerations |
|---|---|---|---|
| iAPEX Proximity Labeling | Spatial proteomic mapping of ubiquitination microenvironments | Identification of ubiquitination complexes in specific organelles | Superior to traditional APEX with reduced background; requires DAAO expression and D-amino acid substrates |
| Ubiquitin Remodeling Assays | Profiling ubiquitin chain linkage and topology | Determining K48 vs K63 linkages in specific pathways | Requires linkage-specific antibodies or UBD probes; mass spectrometry for detailed characterization |
| PROTAC Molecules | Targeted protein degradation via E3 ligase recruitment | Therapeutic validation of E3 ligase functionality | Blood-brain barrier permeability crucial for CNS malignancies like glioblastoma |
| Bioinformatic Ubiquitin Signatures | Prognostic stratification based on ubiquitination-related genes | Patient risk assessment and therapeutic targeting | Multigene models (e.g., 5-gene cervical cancer signature) show clinical relevance |
The enzymatic cascade of ubiquitination represents a master regulatory system whose dysregulation features prominently across cancer types. While common principles govern its operation, comparative analyses reveal cancer-specific alterations that inform both biological understanding and therapeutic development. The E1-E2-E3 axis offers multiple nodes for therapeutic intervention, with E3 ligases presenting particularly attractive targets due to their substrate specificity. Emerging technologies such as iAPEX proximity labeling and sophisticated bioinformatic approaches are deepening our understanding of ubiquitination networks in spatial and disease contexts. Future research directions will likely focus on developing tissue-specific E3 ligase modulators, understanding the functional significance of atypical ubiquitin chain topologies in cancer, and exploiting synthetic lethal interactions based on ubiquitination pathway alterations. As our toolkit for studying and manipulating this system expands, so too does our potential to develop innovative therapies that restore normal ubiquitination homeostasis in cancer cells.
Ubiquitination is a fundamental post-translational modification that involves the covalent attachment of ubiquitin, a 76-amino acid protein, to substrate proteins. This process regulates virtually all aspects of eukaryotic cell biology, including protein degradation, DNA repair, cell signaling, and immune response [10]. The ubiquitination cascade involves three key enzymes: E1 (ubiquitin-activating enzyme), E2 (ubiquitin-conjugating enzyme), and E3 (ubiquitin ligase), which work in concert to attach ubiquitin to specific substrate proteins [11] [12]. The human genome encodes approximately 8 E1 enzymes, 41 E2 enzymes, and over 600 E3 ligases, providing tremendous specificity in substrate selection and regulatory control [13].
The versatility of ubiquitin signaling stems from the ability of ubiquitin itself to be modified in different ways. Monoubiquitination involves attachment of a single ubiquitin molecule to a substrate lysine, while polyubiquitination forms chains through linkage between ubiquitin molecules. Ubiquitin contains seven lysine residues (K6, K11, K27, K29, K33, K48, K63) and an N-terminal methionine (M1) that can form polyubiquitin chains, each creating structurally distinct signals with different functional consequences [10]. This diversity of ubiquitin modifications constitutes a complex "ubiquitin code" that determines specific functional outcomes for modified substrates, ranging from proteasomal degradation to non-proteolytic signaling functions [14] [10].
Comparative Analysis of Ubiquitination Types
Structural and Functional Diversity
The type of ubiquitin modification determines the functional outcome for the modified substrate protein. Monoubiquitination typically serves regulatory roles in membrane trafficking, endocytosis, histone function, and DNA repair [11] [15]. In contrast, polyubiquitin chains generate diverse three-dimensional structures that are recognized by specific ubiquitin-binding domains, leading to different cellular outcomes depending on the chain linkage type [10].
Table 1: Comparative Functions of Ubiquitin Chain Linkages
| Chain Type | Primary Functions | Cellular Processes | Outcome for Substrate |
|---|---|---|---|
| K48-linked | Proteasomal targeting [11] | Cell cycle control, protein turnover [14] | Degradation [12] |
| K63-linked | Signaling scaffold assembly [14] | DNA repair, kinase activation, inflammation [11] [14] | Altered activity/localization [12] |
| K11-linked | Proteasomal degradation [12] | Cell cycle regulation [10] | Degradation [10] |
| K27-linked | DNA damage response [10] | Kinase activation [11] | Signaling adaptation [14] |
| K29-linked | Proteasomal targeting (minor) [16] | Stress response [10] | Degradation or signaling [10] |
| K33-linked | Kinase regulation [10] | Signal transduction [10] | Altered activity [10] |
| M1-linked | NF-κB signaling [10] | Immune and inflammatory responses [10] | Signaling complex assembly [10] |
The mechanisms controlling lysine selection during ubiquitin chain formation involve both structural features of E2/E3 complexes and sequence determinants surrounding acceptor lysines. For the E2 enzyme Cdc34, specific residues in its catalytic core (such as S139 and Y89) can determine whether substrates undergo monoubiquitination or polyubiquitination [11]. Single point mutations in these residues can convert Cdc34 from a polyubiquitinating enzyme into a monoubiquitinating enzyme, demonstrating the precise control mechanisms governing ubiquitin signaling outcomes [11].
Cancer-Specific Ubiquitin Signaling Pathways
In cancer biology, ubiquitination pathways demonstrate remarkable context-dependent functionality across different tumor types. The following table summarizes key ubiquitin system components with dual roles in cancer radioresistance, illustrating how the same enzyme can exert opposite effects depending on cellular context.
Table 2: Context-Dependent Roles of Ubiquitin System Components in Cancer Radioresistance
| Enzyme | Tumor Type | Pro-tumor Role | Anti-tumor Role | Therapeutic Vulnerability |
|---|---|---|---|---|
| FBXW7 | Colorectal cancer | Degrades p53 to promote radioresistance [14] | - | MDM2/FBXW7 co-inhibition [14] |
| NSCLC | - | Degrades SOX9 to enhance radiosensitivity [14] | SOX9 targeting [14] | |
| USP14 | Glioma | Stabilizes ALKBH5 to maintain stemness [14] | - | USP14 inhibitors [14] |
| HNSCC | Degrades IκBα to activate NF-κB [14] | - | Catalytic inhibition [14] | |
| TRIM21 | Nasopharyngeal carcinoma | Degrades VDAC2 to suppress cGAS-STING immunity [14] | - | Combined immunotherapy [14] |
| β-TrCP | Lung cancer | K48-linked degradation of radioprotective LZTS3 [14] | - | EGFR-directed PROTACs [14] |
The functional duality of ubiquitin enzymes in cancer is exemplified by FBXW7, which promotes radioresistance in p53-wildtype colorectal tumors by degrading p53, yet enhances radiosensitivity in non-small cell lung cancer (NSCLC) with SOX9 overexpression by destabilizing SOX9 and alleviating p21 repression [14]. This contextual duality extends to metabolic adaptation, where SMURF2-mediated HIF1α degradation compromises hypoxic survival, while SOCS2/Elongin B/C-driven SLC7A11 destruction increases ferroptosis sensitivity in liver cancer [14].
Experimental Methodologies for Ubiquitin Research
Advanced Techniques for Ubiquitinome Analysis
The comprehensive analysis of ubiquitin modifications requires specialized methodologies that can capture the diversity and dynamics of the ubiquitin code. Several advanced platforms have been developed to address the challenges in studying ubiquitin-like protein modifications:
BioUbL System: This comprehensive platform utilizes in vivo biotinylation with the E. coli biotin protein ligase BirA to study ubiquitin-like modifications. The system employs multicistronic expression vectors that enable rapid validation of UbL conjugation for both exogenous and endogenous proteins. A key advantage is the ability to purify under denaturing conditions, which inactivates deconjugating enzymes and preserves ubiquitination states, while stringent washes remove UbL interactors and non-specific background [17].
Tandem Ubiquitin-Binding Entities (TUBEs): These molecular traps consisting of tandem ubiquitin-binding domains enable enrichment of ubiquitinated proteins from complex mixtures. TUBEs protect ubiquitin chains from deubiquitinating enzymes and allow purification under native conditions, making them particularly valuable for studying endogenous ubiquitination dynamics [17].
Di-Gly Residual Peptide Antibodies: Monoclonal antibodies specifically recognizing the di-glycine remnant left on trypsinized peptides after ubiquitination enable proteome-wide identification of ubiquitination sites by mass spectrometry. This approach has identified tens of thousands of ubiquitination sites, revealing that most cellular proteins undergo ubiquitination at some point [17] [10].
Linkage-Specific Ubiquitin Tools: The development of linkage-specific antibodies and ubiquitin-binding domains has enabled researchers to specifically detect and purify particular polyubiquitin chain types. These tools are essential for deciphering the functional consequences of specific ubiquitin linkages in cellular pathways [10].
Diagram 1: Experimental Workflow for Ubiquitin Modification Analysis. This diagram outlines key methodological approaches for studying ubiquitin modifications, highlighting both denaturing and native purification strategies.
Targeted Protein Degradation Technologies
The understanding of ubiquitin signaling mechanisms has enabled the development of revolutionary therapeutic platforms, particularly in targeted protein degradation:
PROTACs (Proteolysis-Targeting Chimeras): These heterobifunctional molecules consist of two ligands connected by a linker - one that binds to an E3 ubiquitin ligase and another that binds to a target protein of interest. This proximity-induced ubiquitination leads to target degradation by the proteasome. PROTACs have matured from a chemical biology concept to a promising drug discovery paradigm, currently exploiting E3 ligases including VHL, CRBN, MDM2, IAPs, and DCAF15 [13] [14].
Molecular Glues: These small molecules induce or stabilize interactions between E3 ubiquitin ligases and target proteins, leading to ubiquitination and degradation. Unlike PROTACs, molecular glues are not necessarily bifunctional but work by altering the surface topography of protein complexes to enable new interactions [14].
Radiotherapy-Activated PROTACs: Innovative platforms such as radiotherapy-triggered PROTAC (RT-PROTAC) prodrugs are activated by tumor-localized X-rays to degrade specific targets like BRD4/2, synergizing with radiotherapy in cancer models. Similarly, X-ray-responsive nanomicelles selectively release PROTACs within irradiated tumors, enabling spatially-controlled protein degradation [14].
Ubiquitin Signaling Networks in Cancer Biology
DNA Damage Response and Repair Pathways
Ubiquitin signaling plays critical roles in the cellular response to DNA damage, with distinct chain types orchestrating specific repair pathways. K63-linked ubiquitin chains serve as platforms to assemble DNA repair complexes at damage sites, while K48-linked chains target inhibitory proteins for degradation to facilitate repair progression [14]. The E3 ligase RNF126 promotes ATR-CHK1 activation through K63-linked ubiquitination in triple-negative breast cancer, creating synthetic lethality with ATM inhibition [14]. Meanwhile, the deubiquitinase OTUB1 stabilizes CHK1 to enhance repair fidelity in lung cancer, making OTUB1 inhibition a promising strategy for radiosensitization [14].
Diagram 2: Ubiquitin Signaling in DNA Damage Response and Repair. This diagram illustrates how different ubiquitin chain types coordinate DNA repair processes through distinct mechanisms, with K63-linked chains facilitating signaling complex assembly and K48-linked chains mediating proteolytic events.
Epigenetic Regulation Through Ubiquitin Signaling
Recent research has revealed sophisticated mechanisms by which ubiquitin signaling regulates chromatin dynamics and epigenetic states. The ASB7 E3 ligase serves as a key negative regulator of heterochromatin maintenance by targeting the H3K9me3 methyltransferase SUV39H1 for degradation [18]. ASB7 localizes to heterochromatin through interaction with HP1 proteins via a conserved PxVxL motif, restricting the spread of repressive H3K9me3 marks beyond heterochromatin boundaries [18].
This ubiquitin-mediated epigenetic regulation is dynamically controlled through the cell cycle. During mitosis, CDK1-Cyclin B1 phosphorylates ASB7 at multiple residues, disrupting its ability to bind and degrade SUV39H1. This mitotic inactivation permits transient SUV39H1 accumulation and H3K9me3 re-establishment post-replication, while ASB7 reactivation in G1 phase restricts further heterochromatin propagation [18]. The identification of truncating ASB7 mutations in cancers, particularly in its SOCS domain, highlights the therapeutic relevance of this ubiquitin-epigenetics crosstalk [18].
Research Reagent Solutions for Ubiquitin Studies
Table 3: Essential Research Tools for Ubiquitin Signaling Studies
| Reagent Category | Specific Examples | Research Applications | Key Features |
|---|---|---|---|
| Ubiquitin Activation Inhibitors | PYR-41, TAK-243 | E1 enzyme inhibition | Blocks ubiquitination initiation [12] |
| Proteasome Inhibitors | MG132, Bortezomib, Carfilzomib | Proteasome function studies | Stabilizes ubiquitinated proteins [12] |
| DUB Inhibitors | PR-619 (pan-DUB inhibitor), USP14 inhibitors, OTUB1 inhibitors | Deubiquitinase functional analysis | Linkage-specific or general DUB blockade [14] |
| Linkage-Specific Antibodies | K48-linkage specific, K63-linkage specific, M1-linkage specific | Ubiquitin chain typing | Selective detection of chain architectures [10] |
| Activity-Based Probes | Ubiquitin-based fluorogenic substrates, HA-Ub-VS | DUB activity profiling | Mechanism-based DUB capture and identification [17] |
| Recombinant E2/E3 Enzymes | Cdc34 mutants (S139D, Y89N), SCF complexes | In vitro ubiquitination assays | Study of enzyme mechanisms and specificity [11] |
| Biotinylated Ubiquitin Tools | BioUbL system, AviTag-ubiquitin conjugates | Affinity purification of ubiquitinated proteins | High-affinity streptavidin-based capture [17] |
The UbiHub database represents a valuable online resource that integrates biological, structural, and chemical data on phylogenetic trees of human protein families involved in ubiquitination signaling, including E3 ligases and deubiquitinases. This platform enables researchers to visualize diverse data types and informs target prioritization and drug design efforts [13].
The complexity of ubiquitin signaling pathways presents both challenges and opportunities for therapeutic intervention, particularly in oncology. The development of PROTACs has demonstrated the feasibility of harnessing the ubiquitin-proteasome system for targeted protein degradation, with several candidates advancing through clinical development [13] [14]. The functional redundancy within the ubiquitin system and the contextual duality of many E3 ligases and DUBs necessitate careful patient stratification and biomarker-guided approaches for successful clinical translation [14].
Emerging strategies focus on exploiting tumor-specific vulnerabilities created by ubiquitin pathway alterations, such as synthetic lethality between E3 ligases and DNA repair pathways, or targeting the ubiquitin-mediated control of epigenetic states [14] [18]. The integration of advanced ubiquitin profiling technologies with functional genomics approaches will continue to uncover novel therapeutic opportunities within this complex regulatory system, ultimately enabling more precise manipulation of ubiquitin signaling for cancer therapy.
The ubiquitin-proteasome system (UPS) is a critical regulator of cellular homeostasis, governing approximately 80-90% of intracellular protein degradation in eukaryotic cells. This comprehensive pan-cancer analysis examines the genetic and expression alterations of ubiquitination enzymes across multiple cancer types, revealing consistent dysregulation patterns that correlate with prognosis, immune infiltration, and therapeutic response. By integrating multi-omics data from large-scale cancer cohorts, we demonstrate that ubiquitination enzymes including E1 activators, E2 conjugators, E3 ligases, and deubiquitinases exhibit cancer-specific mutation signatures and expression profiles that significantly influence tumor progression and patient outcomes. Our findings establish the UPS as a rich source of prognostic biomarkers and therapeutic targets across the cancer spectrum.
Ubiquitination represents the second most prevalent post-translational modification following phosphorylation, enacting a sophisticated enzymatic cascade mediated by ubiquitin-activating enzymes (E1), ubiquitin-conjugating enzymes (E2), and ubiquitin ligases (E3). This system facilitates the covalent attachment of ubiquitin molecules to substrate proteins, regulating diverse cellular processes including proteolysis, signal transduction, cell cycle progression, and DNA repair. The reverse reaction, deubiquitination, is catalyzed by deubiquitinating enzymes (DUBs). Mounting evidence indicates that dysregulation of ubiquitination enzymes constitutes a hallmark across multiple cancer types, driving oncogenic transformation, metabolic reprogramming, and therapeutic resistance.
Despite the established role of individual ubiquitination enzymes in specific cancer contexts, a systematic pan-cancer analysis of the entire ubiquitination apparatus has been lacking. This study fills this critical knowledge gap by providing a comprehensive characterization of genetic alterations and expression dysregulation across the complete ubiquitination enzyme spectrum. By employing integrated bioinformatics approaches on multi-omics data from The Cancer Genome Atlas (TCGA) and complementary datasets, we reveal consistent patterns of ubiquitination enzyme dysregulation that transcend individual cancer types, offering novel insights for prognostic stratification and therapeutic development.
Results
Expression Dysregulation of Ubiquitination Enzymes Across Cancers
Ubiquitination enzymes demonstrate consistent overexpression patterns across diverse cancer types compared to normal tissues. Pan-cancer analyses reveal significant elevation of key enzymes including UBE2T, UBA1, UBA6, and USP37 in multiple malignancies, with distinct patterns according to cancer and histological subtypes.
Table 1: Ubiquitination Enzyme Dysregulation Across Cancer Types
| Enzyme | Enzyme Class | Cancer Types with Overexpression | Associated Clinical Outcomes |
|---|---|---|---|
| UBE2T | E2 conjugating enzyme | Pancreatic cancer, breast cancer, renal cell carcinoma, ovarian cancer, cervical cancer, retinoblastoma | Reduced overall and progression-free survival [19] [20] |
| UBA1 | E1 activating enzyme | Lung cancer, liver cancer, colorectal cancer | Poor prognosis, associated with advanced tumor stage [21] |
| UBA6 | E1 activating enzyme | Multiple cancer types | Correlation with tumor grade and stage [21] |
| USP37 | Deubiquitinating enzyme | Colorectal cancer, renal cancer, breast cancer, gastric cancer, pancreatic cancer | Poor prognosis, associated with immune infiltration [22] |
| CDC20 | E3 ligase | Lung adenocarcinoma | Poor patient prognosis, associated with immune cell infiltration [23] |
The ubiquitination-related prognostic signature (URPS), derived from ubiquitination enzyme expression patterns, effectively stratifies patients into distinct risk categories across multiple cancers including lung cancer, esophageal cancer, cervical cancer, urothelial cancer, and melanoma. High-risk URPS patients demonstrate significantly worse overall survival (HR = 0.54, 95% CI: 0.39–0.73, p < 0.001) in lung adenocarcinoma, with validation across six external cohorts confirming its prognostic value (HR = 0.58, 95% CI: 0.36–0.93, p<0.023) [24] [25].
Genetic Alterations in Ubiquitination Enzymes
Genomic analyses reveal distinctive mutation patterns across different classes of ubiquitination enzymes. The UBE2T gene displays "amplification" as its predominant genetic alteration, followed by mutations, with copy number variations occurring more frequently than single nucleotide variants across pan-cancer cohorts [19]. In lung adenocarcinoma, comprehensive analysis of E3 ubiquitin ligases identified 19 key genes with significant dysregulation, including CDC20, AURKA, CCNF, POC1A, and UHRF1, which are specifically overexpressed in tumor tissues and associated with poor prognosis [23].
ActiveDriver analysis of acetylation and ubiquitination sites demonstrates significant enrichment of cancer mutations in these functionally important regions, with stronger evolutionary conservation and accumulation in protein domains. Mutations in post-translational modification sites occur in known oncoproteins including TP53, AKT1, and IDH1, and accumulate in cancer-related processes such as cell cycle regulation, apoptosis, chromatin organization, and metabolism [26].
Table 2: Genetic Alteration Patterns in Ubiquitination Enzymes
| Genetic Alteration Type | Affected Enzymes | Functional Consequences | Analysis Method |
|---|---|---|---|
| Copy number variations | UBE2T, UBA1, UBA6 | Increased enzyme expression, enhanced oncogenic activity | GSCALite database analysis [19] [21] |
| Single nucleotide variants | Multiple E3 ligases, DUBs | Altered substrate specificity, enzyme activity modulation | ActiveDriver, cBioPortal analysis [22] [26] |
| Mutation hotspots in PTM sites | TP53, AKT1, IDH1, histone proteins | Disrupted regulatory switches, pathway dysregulation | ActiveDriver method [26] |
| Amplifications | CDC20, AURKA, UHRF1 | Enhanced proliferation, cell cycle disruption | TCGA pan-cancer analysis [23] |
Ubiquitination Enzymes in Cancer Signaling and Immune Regulation
Ubiquitination enzymes regulate crucial cancer-associated signaling pathways across different cancer types. The OTUB1-TRIM28 ubiquitination axis modulates MYC pathway activity and influences oxidative stress responses, contributing to immunotherapy resistance and poor patient prognosis [24]. USP37 regulates lung cancer cell proliferation and the Warburg effect by deubiquitinating and stabilizing c-Myc expression [22]. In lung adenocarcinoma, CDC20 enrichment correlates with activation of G2/M checkpoint, mTORC1 signaling, oxidative phosphorylation, and glycolysis pathways [23].
The tumor immune microenvironment is significantly influenced by ubiquitination enzyme activity. Ubiquitination scores positively correlate with squamous or neuroendocrine transdifferentiation in adenocarcinoma and associate with macrophage infiltration patterns [24]. UBE2T expression shows significant associations with tumor immune markers, checkpoint genes, and immune cell infiltration, while USP37 expression correlates strongly with immune regulators, tumor mutational burden (TMB), and microsatellite instability (MSI) [19] [22]. E3 ubiquitin ligases in lung adenocarcinoma demonstrate negative correlations with B cells and dendritic cells, but positive associations with neutrophil infiltration [23].
Diagram 1: Ubiquitination Enzyme Regulation of Cancer Signaling and Immune Pathways. Ubiquitination enzymes modulate critical cancer-associated pathways including MYC signaling, mTORC1 activity, immune checkpoint expression, and tumor microenvironment (TME) infiltration, contributing to therapy resistance and metabolic reprogramming.
Prognostic and Predictive Value of Ubiquitination Signatures
Ubiquitination-based biomarkers demonstrate significant prognostic value across multiple cancer types. The ubiquitination-related risk score (URRS) developed for lung adenocarcinoma, incorporating DTL, UBE2S, CISH, and STC1 expression, effectively stratifies patients into high-risk and low-risk categories with distinct clinical outcomes [25]. High URRS patients exhibit worse prognosis, elevated PD-1/PD-L1 expression, increased tumor mutation burden (TMB), higher tumor neoantigen load (TNB), and distinctive tumor microenvironment scores (p < 0.001) [25].
The URPS signature shows predictive value for immunotherapy response, potentially identifying patients more likely to benefit from immune checkpoint inhibition across multiple solid tumors including lung cancer, esophageal cancer, cervical cancer, urothelial cancer, and melanoma [24]. Ubiquitination scores also associate with histological fate decisions in cancer cells, particularly squamous or neuroendocrine transdifferentiation in adenocarcinoma contexts [24].
Discussion
This pan-cancer analysis establishes ubiquitination enzymes as central players in cancer pathogenesis, with consistent patterns of genetic and expression dysregulation across diverse malignancies. The frequent overexpression of E1, E2, E3, and deubiquitinating enzymes, coupled with specific mutation signatures in functional domains, underscores the fundamental role of ubiquitination deregulation in oncogenic processes.
The prognostic significance of ubiquitination-related signatures across multiple independent cohorts highlights their potential clinical utility for risk stratification. Notably, the consistency of these signatures across cancer types suggests common mechanisms of ubiquitination-mediated oncogenesis that transcend tissue-of-origin specificities. The association between ubiquitination signatures and immune microenvironment composition further reinforces the interconnected nature of protein homeostasis and anti-tumor immunity.
From a therapeutic perspective, the ubiquitin-proteasome system presents attractive targeting opportunities. The success of proteasome inhibitors in hematological malignancies has established proof-of-concept for targeting protein degradation pathways in cancer. Our findings suggest that specific ubiquitination enzymes, particularly those with recurrent genetic alterations or consistent overexpression patterns, may represent promising targets for drug development. The predictive value of ubiquitination signatures for immunotherapy response merits particular attention, as this may enable better patient selection for immune checkpoint inhibitors.
Future research directions should focus on elucidating the substrate specificities of dysregulated ubiquitination enzymes, developing isoform-selective inhibitors, and exploring combination therapies targeting ubiquitination pathways alongside conventional treatments. The integration of ubiquitination signatures into clinical trial designs may facilitate personalized treatment approaches based on individual tumor ubiquitination profiles.
Methods
Data Collection and Processing
We extracted RNA sequencing data and clinical information from The Cancer Genome Atlas (TCGA) pan-cancer cohort, encompassing 33 cancer types and normal tissue data from the Genotype-Tissue Expression (GTEx) database [22]. A total of 966 ubiquitination-related genes (URGs), including ubiquitin-activating enzymes (E1s), ubiquitin-conjugating enzymes (E2s), and ubiquitin-protein ligases (E3s), were collected from the iUUCD 2.0 database [25]. Additional validation datasets were obtained from the Gene Expression Omnibus (GEO), including GSE30219, GSE135222, GSE126044, GSE183924, GSE53625, GSE44001, and GSE56303 [24].
Ubiquitination Enzyme Expression Analysis
Differential expression analysis of ubiquitination enzymes between tumor and normal tissues was performed using the TIMER 2.0 database, with statistical significance assessed via Wilcoxon test [19]. Protein expression patterns were validated using the Human Protein Atlas (HPA) database [21] [22]. Consensus clustering analysis employing the "KM" method with Euclidean distance was applied to identify distinct molecular subtypes based on URG expression patterns, implemented through the "ConsensusClusterPlus" R package with maxK=5, reps=1000, pItem=0.8, pFeature=1 [25].
Genetic Alteration Analysis
Genomic alterations in ubiquitination enzymes were analyzed using cBioPortal for Cancer Genomics, examining mutation frequencies, copy number variations, and structural rearrangements across cancer types [22]. The GSCA database facilitated analysis of single nucleotide variants (SNVs) and copy number variations (CNVs) [19] [21]. Site-specific mutation enrichment in post-translational modification sites was assessed using ActiveDriver, which employs a Poisson regression model accounting for protein disorder, direct and flanking PTM residues, and site density [26].
Survival and Prognostic Analysis
Survival analysis was conducted using univariate Cox regression and Kaplan-Meier methods, with patients stratified into high and low expression groups based on median expression values of target ubiquitination enzymes [24] [22]. The ubiquitination-related risk score (URRS) was developed through integration of univariate Cox regression, Random Survival Forest algorithm (variable importance >0.25), and LASSO Cox regression analysis [25]. Time-dependent ROC curves evaluated the predictive accuracy of URRS for one-, three-, and five-year survival endpoints.
Immune Infiltration Analysis
Correlations between ubiquitination enzyme expression and immune cell infiltration were assessed using the CIBERSORT algorithm to estimate the relative proportions of 22 immune cell types [21]. The TISIDB database facilitated analysis of associations with immune subtypes and checkpoint expression [21]. ESTIMATE algorithm was employed to calculate immune scores, stromal scores, and estimate scores in the tumor microenvironment [25].
Gene Set Enrichment Analysis
Gene Set Enrichment Analysis (GSEA) was performed using the "clusterProfiler" R package with the hallmark gene set file (h.all.v7.4.symbols.gmt) from the Molecular Signatures Database (MSigDB) [22]. Significance thresholds were set at nominal p-value <0.05 and false discovery rate (FDR) <0.05 [23]. Gene Ontology and Kyoto Encyclopedia of Genes and Genomes analyses identified biological processes and pathways enriched in ubiquitination enzyme-high tumors.
Diagram 2: Computational Analysis Workflow. The integrated bioinformatics pipeline encompasses data acquisition from TCGA and GEO databases, ubiquitination enzyme annotation, multi-dimensional analysis of molecular features, and validation in independent cohorts.
Experimental Validation
For key ubiquitination enzymes, experimental validation was performed using pancreatic cancer cell lines (PANC1, ASPC, BXPC3, MIA2, SW1990, CAPAN1) and normal pancreatic epithelial cells (HPDE) [19]. Western blotting was conducted using established protocols with primary antibodies specific to target proteins (e.g., UBE2T at 1:2,000 dilution) and HRP-conjugated secondary antibodies (1:5,000) [19]. Reverse transcription-quantitative PCR (RT-qPCR) was performed using SYBR Premix Ex Taq kits with β-actin as internal control, calculating relative expression via the 2−ΔΔCq method [19] [25].
The Scientist's Toolkit
Table 3: Essential Research Reagents for Ubiquitination Enzyme Studies
| Reagent/Resource | Function | Example Application | Source |
|---|---|---|---|
| iUUCD 2.0 Database | Comprehensive repository of ubiquitination enzymes | Identification of E1, E2, E3 enzymes and DUBs for analysis | http://iuucd.biocuckoo.org/ [25] |
| TCGA Pan-Cancer Data | Multi-omics data across 33 cancer types | Differential expression, survival analysis, genomic alteration studies | https://www.cancer.gov/ccg/research/genome-sequencing/tcga [22] |
| UALCAN Database | TCGA data analysis portal | Protein and mRNA expression analysis in cancer vs. normal tissues | http://ualcan.path.uab.edu/ [19] [21] |
| cBioPortal | Visualization and analysis of cancer genomics data | Genetic alteration frequency and patterns across cancer types | http://cbioportal.org [22] |
| Human Protein Atlas | Tissue immunohistochemistry database | Protein expression validation in normal and cancer tissues | https://www.proteinatlas.org/ [21] [22] |
| TISIDB Database | Tumor-immune system interaction database | Analysis of associations with immune subtypes and infiltration | http://cis.hku.hk/TISIDB/ [21] |
| ConsensusClusterPlus | Unsupervised clustering package | Identification of molecular subtypes based on expression patterns | R Bioconductor package [25] |
| CIBERSORT Algorithm | Deconvolution of immune cell fractions | Estimation of immune cell infiltration from expression data | https://cibersort.stanford.edu/ [21] |
Ubiquitination, a fundamental post-translational modification, regulates protein stability, localization, and function through a coordinated enzymatic cascade involving E1 activating enzymes, E2 conjugating enzymes, E3 ligases, and deubiquitinating enzymes (DUBs) [27]. The ubiquitin-proteasome system (UPS) degrades approximately 80-90% of intracellular proteins, maintaining cellular homeostasis and genomic integrity [1] [20]. Dysregulation of ubiquitination pathways represents a hallmark of cancer pathogenesis, influencing critical processes including cell cycle progression, DNA damage repair, immune evasion, and therapeutic resistance [27] [28].
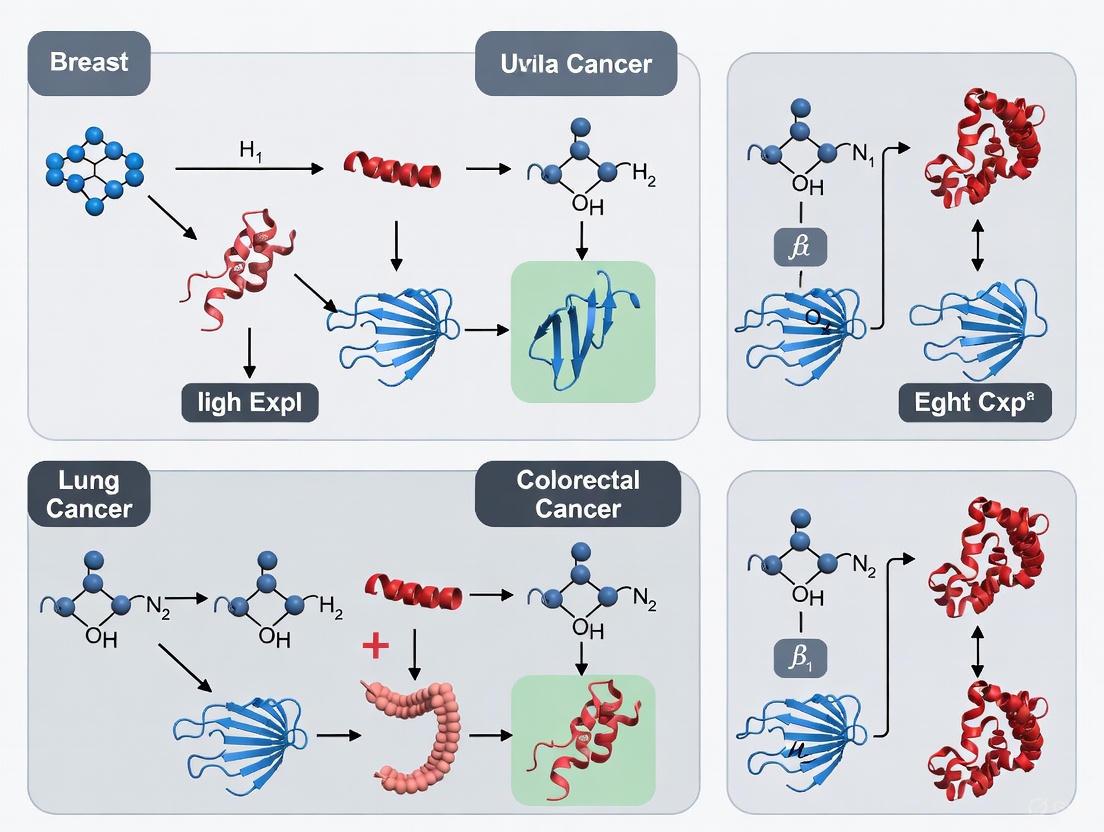
While core ubiquitination machinery is conserved across tissues, emerging evidence reveals remarkable tissue-specificity in how ubiquitination pathways are altered in different cancers. This comparative analysis examines ubiquitination pathway alterations across major cancer types—including cervical, lung, breast, colorectal, and prostate cancers—to identify both shared and tissue-specific molecular patterns. By integrating recent transcriptomic studies, risk model analyses, and mechanistic investigations, this review aims to elucidate the tissue-specific ubiquitination signatures that drive cancer progression and influence therapeutic outcomes, providing a foundation for developing targeted interventions that exploit these pathway-specific vulnerabilities.
Comparative Analysis of Ubiquitination-Related Gene Signatures Across Cancers
Table 1: Ubiquitination-Related Biomarkers and Their Prognostic Value Across Cancer Types
| Cancer Type | Key Ubiquitination-Related Biomarkers | Risk Model Performance (AUC) | Biological Functions Affected | Clinical Associations |
|---|---|---|---|---|
| Cervical Cancer | MMP1, RNF2, TFRC, SPP1, CXCL8 [1] | 1/3/5-year AUC >0.6 [1] | Immune infiltration, Angiogenesis, Extracellular matrix organization [1] | Survival prediction, Immune checkpoint expression [1] |
| Lung Adenocarcinoma | DTL, UBE2S, CISH, STC1 [29] | Validated in 6 external cohorts (HR=0.58) [29] | Cell proliferation, Epithelial-mesenchymal transition, Immune evasion [29] | Tumor mutation burden, PD-1/L1 expression, Chemotherapy response [29] |
| Breast Cancer | FBXL6, PDZRN3, RNF126 [30] [27] | Multiple validation cohorts [30] | DNA damage repair, ATR-CHK1 pathway, Cell cycle regulation [30] | Therapeutic resistance, Immune microenvironment, Patient survival [30] |
| Colorectal Cancer | HSPA1A, USP21, USP44, USP51 [31] [28] | Strong prognostic value [31] | Wnt/β-catenin signaling, HIF1A stabilization, Chemoresistance [31] [28] | Lymph node metastasis, Recurrence, Post-chemotherapy survival [31] |
| Prostate Cancer | USP21, UBE2T, EZH2, FOXD1 [32] [20] | Independent validation [32] | Androgen receptor signaling, HIF1-α transcription, DNA repair [32] [20] | Castration resistance, Metastatic progression, Therapeutic vulnerability [32] |
The development of ubiquitination-related gene signatures has revealed both common and cancer-specific prognostic biomarkers across malignancies. In cervical cancer, a 5-gene signature (MMP1, RNF2, TFRC, SPP1, and CXCL8) demonstrates significant predictive value for patient survival, with particular strength in forecasting 1-, 3-, and 5-year outcomes [1]. These biomarkers predominantly influence immune modulation and extracellular matrix remodeling, with upregulated expression of MMP1, TFRC, and CXCL8 confirmed in tumor tissues [1].
Lung adenocarcinoma exhibits a distinct 4-gene ubiquitination signature (DTL, UBE2S, CISH, STC1) that effectively stratifies patients into high- and low-risk groups [29]. Notably, this signature shows robust performance across six independent validation cohorts, with high-risk patients demonstrating elevated tumor mutation burden, increased PD-1/L1 expression, and differential sensitivity to conventional chemotherapeutics [29].
Breast cancer ubiquitination patterns reveal substantial heterogeneity, with research focusing particularly on triple-negative breast cancer (TNBC) and its associated immunological and metabolic aspects [27]. An 8-gene prognostic signature has been developed, with FBXL6 and PDZRN3 experimentally validated as critical regulators of breast cancer development through in vitro and in vivo models [30].
Colorectal cancer investigations have identified HSPA1A as a central regulator among ubiquitination-related genes, with knockdown experiments demonstrating significant inhibition of cancer cell proliferation, migration, and invasion both in vitro and in vivo [31]. Multiple ubiquitin-specific proteases (USPs), including USP21, USP44, and USP51, contribute to colorectal cancer progression through regulation of key signaling pathways including Wnt/β-catenin and HIF1A [28].
Prostate cancer studies highlight USP21 as a key oncogenic driver that correlates with poor prognosis [32]. USP21 mediates deubiquitination and stabilization of YBX1, which in turn transactivates HIF1A expression, creating a pro-tumorigenic signaling axis that promotes disease progression [32].
Tissue-Specific Ubiquitination Pathway Alterations
Cervical and Breast Cancer: Immune and Angiogenic Regulation
In cervical cancer, ubiquitination pathways predominantly influence tumor immunity and angiogenesis. The identified ubiquitination-related biomarkers (MMP1, RNF2, TFRC, SPP1, and CXCL8) significantly impact immune cell infiltration patterns, with notable differences observed in memory B cells, M0 macrophages, and multiple T-cell populations between high- and low-risk patient groups [1]. Additionally, immune checkpoint expression varies significantly according to ubiquitination risk profiles, suggesting potential implications for immunotherapy responsiveness [1].
Breast cancer ubiquitination pathways demonstrate strong associations with hormone receptor status and therapeutic resistance mechanisms. The ubiquitin-related gene signature effectively stratifies patients based on estrogen receptor status, AJCC stages, and nodal involvement [30]. Furthermore, risk groups show differential sensitivity to endocrine therapies (tamoxifen, fulvestrant), chemotherapeutic agents (cyclophosphamide, cisplatin, paclitaxel, epirubicin), and targeted therapies (gefitinib, lapatinib), highlighting the clinical utility of ubiquitination-based classification [30].
Lung Cancer: KCTD10/β-catenin/PD-L1 Axis
In lung cancer, the KCTD10 protein exemplifies tissue-specific ubiquitination regulation by functioning as a novel E3 ligase adaptor that promotes β-catenin degradation through K48-linked ubiquitin chains [33]. This mechanism has profound implications for both tumor progression and immunotherapy response. Reduced KCTD10 expression in lung cancer tissues leads to β-catenin accumulation, resulting in enhanced PD-L1 transcription and immune evasion [33]. This establishes a direct molecular connection between ubiquitination pathways and immune checkpoint regulation.
The therapeutic potential of targeting this axis was demonstrated through combination experiments where KCTD10 overexpression synergized with anti-PD-1 antibodies to suppress lung cancer progression and brain metastatic colonization in murine models [33]. Additionally, vascular endothelial cell-specific knockout of Kctd10 promoted lung cancer metastasis and tumor angiogenesis through β-catenin signaling, highlighting the importance of ubiquitination regulation within the tumor microenvironment [33].
Gastrointestinal Cancers: Wnt/β-catenin and HIF1A Signaling
Colorectal and prostate cancers share common ubiquitination-mediated regulation of central signaling pathways, albeit through distinct molecular mechanisms. In colorectal cancer, multiple ubiquitin-specific proteases including USP44 and USP38 regulate the Wnt/β-catenin pathway through deubiquitination and stabilization of Axin1 and HMX3, respectively [28]. Additionally, USP51 stabilizes HIF1A through deubiquitination, creating a positive feed-forward loop that maintains cancer stemness and chemoresistance [28].
Prostate cancer employs a different mechanism wherein USP21 deubiquitinates and stabilizes YBX1, which subsequently enhances HIF1A transcription [32]. This USP21/YBX1/HIF1-α axis promotes prostate cancer malignancy and represents a promising therapeutic target, with pharmacological inhibition of USP21 using Bay-805 demonstrating significant antitumor efficacy in experimental models [32].
Table 2: Tissue-Specific Ubiquitination Pathway Alterations and Functional Consequences
| Cancer Type | Key Ubiquitination Pathways | Primary Molecular Mechanisms | Downstream Effects | Therapeutic Implications |
|---|---|---|---|---|
| Cervical Cancer | Immune checkpoint regulation [1] | Ubiquitination-related biomarker expression (MMP1, RNF2, TFRC, SPP1, CXCL8) [1] | Altered immune cell infiltration, Angiogenesis promotion [1] | Immunotherapy response prediction [1] |
| Lung Cancer | KCTD10/β-catenin/PD-L1 axis [33] | KCTD10-mediated β-catenin ubiquitination and degradation [33] | PD-L1 downregulation, Enhanced immune surveillance [33] | Synergy with anti-PD-1 therapy [33] |
| Breast Cancer | DNA damage response, Cell cycle regulation [30] | RNF126-mediated ATR-CHK1 pathway regulation [30] | Radiation sensitivity, Proliferation control [30] | Radiation sensitization, Targeted therapy [30] |
| Colorectal Cancer | Wnt/β-catenin, HIF1A stabilization [31] [28] | USP-mediated deubiquitination of pathway components [28] | Cancer stemness maintenance, Chemoresistance [28] | USP inhibitor development [28] |
| Prostate Cancer | USP21/YBX1/HIF1-α axis [32] | USP21-mediated YBX1 deubiquitination and stabilization [32] | HIF1-α transactivation, Metabolic reprogramming [32] | Bay-805 (USP21 inhibitor) application [32] |
Methodologies for Ubiquitination Pathway Analysis
Bioinformatics Approaches for Ubiquitination Signature Development
The identification of ubiquitination-related gene signatures across cancer types employs standardized bioinformatics workflows. Typically, ubiquitination-related genes are compiled from specialized databases such as iUUCD 2.0 or Molecular Signatures Database (MSigDB), yielding approximately 763-1,006 genes encompassing E1 activating enzymes, E2 conjugating enzymes, E3 ligases, and deubiquitinating enzymes [29] [30].
Differentially expressed ubiquitination-related genes between tumor and normal tissues are identified using packages such as DESeq2 or limma, with standard thresholds of |log2FoldChange| > 0.5-0.585 and p-value < 0.05 [1] [31]. Prognostic gene selection typically employs univariate Cox regression analysis followed by feature refinement using Least Absolute Shrinkage and Selection Operator (LASSO) Cox regression and Random Survival Forests algorithms [29] [31]. Risk scores are calculated using the formula: Risk score = Σ(coefficient of genei × expression of genei), with patients stratified into high- and low-risk groups based on median risk score thresholds [29].
Validation procedures include internal validation through cross-validation approaches and external validation using independent cohorts from databases such as GEO and TCGA [29] [30]. Model performance is assessed through Kaplan-Meier survival analysis, receiver operating characteristic (ROC) curves, and calculation of concordance indices (C-index) [1] [29].
Experimental Validation Techniques
Functional validation of ubiquitination-related biomarkers employs standardized experimental approaches both in vitro and in vivo. Gene expression validation typically utilizes Reverse Transcription-Quantitative Polymerase Chain Reaction (RT-qPCR) and western blotting on paired tumor and normal tissues [1] [20]. For functional characterization, gene manipulation through small interfering RNA (siRNA) or short hairpin RNA (shRNA)-mediated knockdown and cDNA overexpression are performed in relevant cancer cell lines [30] [32].
Phenotypic assays assess proliferation (Cell Counting Kit-8), migration (wound healing), and invasion (Transwell chambers with Matrigel coating) [31] [30]. In vivo validation employs subcutaneous xenograft models for tumor growth assessment and tail vein injection models for metastatic potential evaluation [32] [30]. Zebrafish xenograft models provide additional platforms for assessing tumor growth and metastatic behavior [31].
Mechanistic studies utilize co-immunoprecipitation (Co-IP) combined with mass spectrometry to identify protein-protein interactions, while ubiquitination assays determine specific ubiquitin linkage types (K48, K63, etc.) [33] [32]. Chromatin immunoprecipitation (ChIP) and dual-luciferase reporter assays elucidate transcriptional regulation mechanisms [32].
Table 3: Essential Research Reagents for Ubiquitination Pathway Studies
| Reagent/Resource Category | Specific Examples | Primary Applications | Key Considerations |
|---|---|---|---|
| Bioinformatics Tools | DESeq2, limma, ConsensusClusterPlus, CIBERSORT, ESTIMATE [1] [29] [30] | Differential expression analysis, Clustering, Immune infiltration estimation | Parameter optimization, Multiple testing correction, Batch effect adjustment |
| Databases | TCGA, GEO, iUUCD 2.0, MSigDB, UALCAN, GEPIA2 [1] [29] [30] | Data retrieval, Ubiquitination gene compilation, Pan-cancer analysis | Data normalization, Platform compatibility, Clinical annotation quality |
| Molecular Biology Reagents | Lipofectamine 3000, Specific antibodies (KCTD10, β-catenin, PD-L1, USP21), HA-tagged ubiquitin plasmids [33] [32] | Gene manipulation, Protein detection, Ubiquitination assays | Transfection efficiency, Antibody specificity, Ubiquitin chain linkage types |
| Cell Culture Models | Cancer cell lines (A549, HCT-116, DU145, MCF7), Patient-derived organoids [33] [31] [32] | In vitro validation, Drug screening, Mechanistic studies | Authentication, Mycoplasma testing, Physiological relevance |
| In Vivo Models | Mouse xenograft models, Zebrafish xenografts, Conditional knockout mice (Kctd10flox/floxCDH5CreERT2/+) [33] [31] [30] | Tumor growth assessment, Metastasis studies, Microenvironment analysis | Immunocompetent vs. deficient models, Orthotopic vs. subcutaneous implantation |
| Specialized Assays | Co-immunoprecipitation, Ubiquitination assays, Chromatin immunoprecipitation, Dual-luciferase reporter [33] [32] | Protein interaction mapping, Ubiquitination detection, Transcriptional regulation | Appropriate controls, Quantitative normalization, Specificity validation |
Ubiquitination Pathway Visualization and Signaling Networks
The ubiquitination signaling network illustrates the coordinated enzymatic cascade that regulates protein fate in cancer cells. The core machinery comprises E1 activating enzymes, E2 conjugating enzymes (including UBE2T and UBE2S), E3 ligases (such as RNF2, KCTD10, and FBXL6), and deubiquitinating enzymes (including USP21, USP44, and USP51) [20] [29] [33]. These enzymes collectively determine the ubiquitination status of key cancer-relevant substrates including β-catenin, YBX1, HIF1-α, and p53 [33] [32] [29].
Tissue-specific ubiquitination patterns emerge through selective expression and regulation of specific enzyme-substrate pairs. In lung cancer, KCTD10 acts as an E3 ligase adaptor that promotes β-catenin degradation, subsequently reducing PD-L1 transcription and enhancing immune surveillance [33]. Conversely, in prostate cancer, USP21 stabilizes YBX1 through deubiquitination, leading to transactivation of HIF1-α and promotion of malignant progression [32]. These tissue-specific mechanisms highlight how the core ubiquitination machinery is co-opted in distinct ways across cancer types to drive pathogenesis.
This comparative analysis reveals that while the core ubiquitination machinery is universally present across tissues, its deregulation in cancer follows distinct tissue-specific patterns. Cervical cancer ubiquitination signatures predominantly influence immune modulation, while lung cancer exhibits prominent KCTD10/β-catenin/PD-L1 regulatory axis alterations. Breast cancer ubiquitination pathways demonstrate strong associations with hormone responsiveness and DNA damage repair, whereas gastrointestinal and prostate cancers share common themes in Wnt/β-catenin and HIF1A pathway regulation through distinct molecular mechanisms.
The development of ubiquitination-related gene signatures provides robust prognostic tools across cancer types, with consistent demonstration of predictive value for patient survival, therapeutic response, and tumor microenvironment characteristics. These signatures offer clinical utility in risk stratification, treatment selection, and patient prognosis.
Future research directions should focus on elucidating the precise molecular mechanisms through which identified ubiquitination-related biomarkers influence cancer progression, particularly in the context of therapy resistance. The development of targeted therapies exploiting specific ubiquitination pathway vulnerabilities, such as USP21 inhibition in prostate cancer or KCTD10 modulation in lung cancer, represents a promising frontier. Additionally, integrating ubiquitination signatures with other molecular profiling data may enable more comprehensive classification systems that reflect the complex interplay between ubiquitination pathways and other cancer hallmarks.
As our understanding of tissue-specific ubiquitination patterns deepens, the translation of these insights into clinical practice promises to enhance personalized cancer therapy through improved patient stratification and targeted intervention strategies.
Ubiquitination represents a crucial post-translational modification process that governs virtually all cellular functions through its ability to regulate protein stability, localization, and activity. This sophisticated enzymatic cascade involves the coordinated action of ubiquitin-activating enzymes (E1), ubiquitin-conjugating enzymes (E2), and ubiquitin ligases (E3), which collectively tag target proteins with ubiquitin molecules [34] [35]. The reverse process, deubiquitination, is mediated by deubiquitinases (DUBs) that remove ubiquitin chains, providing dynamic control over protein fate [34]. The ubiquitin-proteasome system (UPS) is responsible for degrading 80-90% of intracellular proteins, establishing it as a master regulator of cellular homeostasis [24] [1].
In cancer biology, ubiquitination has emerged as a pivotal mechanism governing hallmark capabilities including uncontrolled proliferation, evasion of apoptosis, and metabolic reprogramming. Dysregulation of ubiquitination pathways drives tumorigenesis through multiple mechanisms: stabilization of oncoproteins, degradation of tumor suppressors, and rewiring of signaling networks [35] [36]. The development of therapies targeting ubiquitination components, particularly proteolysis-targeting chimeras (PROTACs), has created unprecedented opportunities for cancer intervention [37] [35]. This comparative analysis examines how ubiquitination machinery orchestrates key cancer hallmarks across different tumor types, providing a foundation for developing novel therapeutic strategies.
Molecular Machinery of Ubiquitination: Components and Mechanisms
The ubiquitination cascade initiates with E1 activation using ATP, followed by ubiquitin transfer to E2 enzymes, and culminates in substrate-specific modification by E3 ligases [34]. The human genome encodes approximately 8 E1 enzymes, 39 E2 enzymes, and over 600 E3 ligases, creating tremendous specificity in substrate recognition [37]. Deubiquitinases (approximately 100 in humans) provide counter-regulation by removing ubiquitin chains [34]. This sophisticated system generates diverse ubiquitin chain topologies through different linkage types (K48, K63, K11, K27, K29, M1), each encoding distinct functional outcomes [35].
Table 1: Major Ubiquitination Linkage Types and Their Functional Consequences in Cancer
| Linkage Type | Primary Function | Cancer-Relevant Examples |
|---|---|---|
| K48-linked chains | Proteasomal degradation | Degradation of tumor suppressors like p53 [35] |
| K63-linked chains | Signal transduction, DNA repair | NF-κB pathway activation; FBXO22 inhibits LKB1 via K63 ubiquitination in NSCLC [35] |
| K11-linked chains | Cell cycle regulation | UBE2S stabilizes β-catenin via K11 ubiquitination in colorectal cancer [35] |
| K27-linked chains | Immune regulation, mitophagy | MARCH5 degrades γC through K27 ubiquitination to inhibit immune function [35] |
| K29-linked chains | Tumor progression | HECTD3 mediates K29 ubiquitination of c-Myc in gastric cancer [35] |
| M1-linear chains | Innate immune signaling | STAT3 self-regulation in glioblastoma [35] |
The following diagram illustrates the core ubiquitination machinery and its regulatory complexity in cancer cells:
Ubiquitination in Apoptosis Regulation: Balancing Cell Survival and Death
Ubiquitination exerts precise control over apoptotic pathways by regulating the stability and function of key pro-apoptotic and anti-apoptotic factors. The Bcl-2 family proteins, central regulators of mitochondrial apoptosis, are prominent ubiquitination substrates. Pro-apoptotic Bax undergoes ubiquitination at K21, which modulates its activity and sensitivity to TRAIL-induced apoptosis in human colon cancer HCT116 cells [35]. The deubiquitinase inhibitor Aumdubicin induces Bax-dependent apoptosis in lung cancer cells A549 and H1299 by stabilizing Bax protein levels [35].
Anti-apoptotic Bcl-2 members are similarly regulated by ubiquitination. The E3 ligase SCF^FBXO10 promotes Bcl-2 degradation, while USP9X stabilizes Mcl-1 through deubiquitination [35]. The interplay between ubiquitinating and deubiquitinating enzymes creates a dynamic equilibrium that determines cellular fate. Dysregulation of this balance enables cancer cells to evade programmed cell death, contributing to tumor progression and therapy resistance. USP7 and USP1 overexpression, frequently observed in cancers, stabilizes anti-apoptotic proteins and promotes defective DNA repair, respectively, fostering tumorigenesis [35].
Table 2: Ubiquitination Regulation of Apoptotic Factors in Cancer
| Apoptotic Regulator | Ubiquitination Enzyme | Effect | Cancer Context |
|---|---|---|---|
| Bax | Unknown E3 ligase | K21 ubiquitination modulates activity | Colon cancer HCT116 cells [35] |
| Bcl-2 | SCF^FBXO10 E3 ligase | Promotes degradation | Hematological malignancies [35] |
| Mcl-1 | USP9X deubiquitinase | Stabilizes protein | Multiple cancers [35] |
| FLIP | Cullin-3 E3 ligase | Promotes degradation | Influences TRAIL sensitivity [35] |
| Caspase-8 | Cullin-3 E3 ligase | Regulates activity | Modulates apoptosis initiation [35] |
The complexity of apoptotic regulation through ubiquitination is visualized in the following pathway:
Metabolic Reprogramming Through Ubiquitination: The Lipid Metabolism Nexus
Cancer cells extensively rewire their metabolic pathways to support rapid proliferation, and ubiquitination serves as a key regulatory mechanism in this reprogramming. Lipid metabolism represents a particularly crucial target, with ubiquitination governing the stability and activity of multiple enzymes involved in lipid synthesis, storage, and utilization [34]. Adenosine triphosphate citrate lyase (ACLY), which links glycolysis to lipid metabolism by converting citrate to acetyl-CoA, undergoes sophisticated ubiquitination regulation in lung cancer. ARHGEF3 enhances ACLY stability by reducing acetylation at Lys17 and Lys86, leading to dissociation from the E3 ligase NEDD4 [34]. Conversely, Cullin 3 interacts with ACLY through adaptor protein KLHL25, promoting ubiquitination and degradation to inhibit lipid synthesis and tumor growth [34].
Fatty acid synthase (FASN), a pivotal enzyme in de novo lipogenesis, is similarly regulated by ubiquitination. In mouse livers, phosphorylated COP1 accumulates in the cytoplasm and binds FASN through Shp2, forming a FASN-Shp2-COP1 complex that mediates FASN ubiquitination and degradation [34]. Additionally, deacetylation by HDAC3 enhances FASN binding to E3 ligase TRIM21, reducing lipogenesis and inhibiting cancer cell growth [34]. The tumor suppressor SPOP, an E3 ubiquitin ligase mutated in several cancers, regulates lipid metabolism by reducing FASN expression and fatty acid synthesis in prostate cancer [34] [35].
The regulation of lipid metabolism enzymes through ubiquitination is summarized in the following table:
Table 3: Ubiquitination Regulation of Lipid Metabolism Enzymes in Cancer
| Metabolic Enzyme | Regulatory Mechanism | Biological Outcome | Cancer Type |
|---|---|---|---|
| ACLY | ARHGEF3 reduces acetylation, dissociating from E3 ligase NEDD4 | Enhanced stability, increased lipogenesis | Lung cancer [34] |
| ACLY | Cullin3-KLHL25 complex mediates ubiquitination | Degradation, inhibited lipid synthesis | Lung cancer [34] |
| ACLY | PCAF acetylates K540/K546/K554, reducing UBR4 binding | Enhanced stability, increased acetyl-CoA production | Lung cancer [34] |
| FASN | COP1-Shp2 complex mediates ubiquitination | Degradation, reduced lipogenesis | Liver cancer models [34] |
| FASN | HDAC3 deacetylation enhances TRIM21 binding | Degradation, reduced cancer growth | Multiple cancers [34] |
| FASN | SPOP E3 ligase mediates ubiquitination | Degradation, tumor suppression | Prostate cancer [34] |
The interconnected regulation of metabolic enzymes through ubiquitination is depicted below:
Proliferation and Cell Cycle Control: Ubiquitination as the Conductor
The ubiquitin-proteasome system exerts masterful control over cell cycle progression through targeted degradation of cyclins, CDK inhibitors, and other regulatory proteins. The anaphase-promoting complex/cyclosome (APC/C) and SCF (Skp1-Cullin-F-box) complexes represent two major E3 ligase families that coordinate the precise timing of phase transitions [35]. Dysregulation of these systems drives uncontrolled proliferation, a fundamental cancer hallmark.
Ubiquitin-conjugating enzymes have emerged as critical players in oncogenic proliferation across cancer types. UBE2T demonstrates elevated expression in multiple tumors including breast cancer, renal cell carcinoma, ovarian cancer, and retinoblastoma, where it correlates with reduced overall and progression-free survival [38]. Functional studies connect UBE2T to key cellular processes including proliferation, invasion, and epithelial-mesenchymal transition through pathways such as cell cycle regulation, ubiquitin-mediated proteolysis, p53 signaling, and mismatch repair [38].
Similarly, UBE2S promotes tumor progression in skin cutaneous melanoma (SKCM) and other malignancies. Single-cell analysis reveals UBE2S involvement in 14 functional states including tumor cell stemness, invasion, metastasis, proliferation, and epithelial-mesenchymal transition [39]. The correlation between UBE2S expression and immune cell infiltration further highlights its multifaceted role in shaping the tumor microenvironment to favor cancer growth [39].
Comprehensive pan-cancer analyses have identified conserved ubiquitination-related prognostic signatures (URPS) that effectively stratify patients into distinct risk categories across multiple cancer types [24]. These signatures reveal that ubiquitination score positively correlates with squamous or neuroendocrine transdifferentiation in adenocarcinoma, influencing both tumor histology and therapeutic response [24]. The OTUB1-TRIM28 ubiquitination axis specifically modulates MYC pathway activity and oxidative stress response, ultimately driving immunotherapy resistance and poor patient prognosis [24].
Experimental Approaches and Research Reagent Solutions
The investigation of ubiquitination in cancer relies on sophisticated methodological approaches and specialized research tools. The following section details key experimental protocols and reagent solutions essential for advancing this field.
Key Experimental Protocols
Ubiquitination-Regulated Pathway Analysis: The identification of OTUB1-TRIM28 regulation of MYC pathway exemplifies rigorous ubiquitination research [24]. This discovery involved integrated analysis of 23 datasets across six cancer types from TCGA and GEO databases, followed by experimental validation. The methodological workflow included:
- Construction of ubiquitination regulatory networks using correlation coefficient matrices with significance screening (p<0.05)
- Prognostic analysis via Cox regression and Kaplan-Meier survival methods
- Functional enrichment analysis using Gene Set Enrichment Analysis (GSEA)
- Protein-protein interaction analysis using Retrieval of Interacting Genes/Proteins database
- Validation through in vivo and in vitro models confirming the functional role of identified ubiquitination pairs
Prognostic Signature Development: The creation of ubiquitination-related prognostic signatures (URPS) employs standardized bioinformatics pipelines [24] [37] [1]:
- Differential expression analysis of ubiquitination-related genes between tumor and normal tissues using DESeq2 with thresholds (p<0.05 and |log2Fold Change|>0.5)
- Univariate Cox regression to identify survival-associated ubiquitination genes
- LASSO Cox regression for feature selection and overfitting prevention
- Risk score calculation using the formula: Risk score = Σ(Coefi × Expressioni)
- Stratification of patients into high-risk and low-risk groups based on optimal risk score threshold
- Validation using independent cohorts (e.g., GSE165808 and GSE26712 for ovarian cancer) [37]
Research Reagent Solutions
Table 4: Essential Research Reagents for Ubiquitination Studies in Cancer
| Reagent Category | Specific Examples | Research Applications | Experimental Context |
|---|---|---|---|
| Proteasome Inhibitors | Bortezomib, Carfilzomib | Block degradation of ubiquitinated proteins; induce apoptosis through protein accumulation | Clinical use in multiple myeloma; research tool for UPS inhibition [35] |
| E3 Ligase Inhibitors | MDM2 inhibitors, SCF complex inhibitors | Interfere with specific substrate ubiquitination; modulate signaling pathways | Research tools for validating E3-substrate relationships [35] |
| Deubiquitinase Inhibitors | Aumdubicin, USP7 inhibitors | Promote substrate degradation or alter regulatory functions; induce Bax-dependent apoptosis | Aumdubicin induces apoptosis in lung cancer cells [35] |
| PROTACs | Various targeted degraders | Facilitate degradation of traditionally "undruggable" targets; overcome drug resistance | Target 50+ ubiquitination-related genes; clinical development [37] [35] |
| Ubiquitination-Related Antibodies | Anti-UBE2T, Anti-UBE2S, Anti-K48/K63 ubiquitin | Detect expression, localization, and ubiquitination status of targets | Validation of UBE2T protein expression in pancreatic cancer lines [38] |
| Cell Line Models | A549, HCT116, H1299, cancer-specific panels | Functional validation of ubiquitination mechanisms | Bax ubiquitination studies in HCT116; apoptosis assays in A549/H1299 [35] |
Therapeutic Implications and Future Perspectives
The targeting of ubiquitination pathways has yielded clinically effective cancer therapies, most notably proteasome inhibitors for hematological malignancies. However, the emerging repertoire of ubiquitination-targeted therapeutics continues to expand with several promising approaches:
PROTACs (Proteolysis-Targeting Chimeras): These bifunctional molecules represent a breakthrough therapeutic modality, simultaneously engaging E3 ubiquitin ligases and target proteins of interest to induce selective degradation [37] [35]. Their advantages include reduced drug dosage requirements, prolonged therapeutic effects, minimized toxicity, and ability to overcome drug resistance [37]. Currently, PROTACs target more than 50 ubiquitination-related genes, with several candidates in clinical development [37].
Combination Therapies: The interconnected nature of metabolic and signaling pathways in cancer suggests combination therapies will be essential for effective treatment [40] [35]. Simultaneous targeting of multiple ubiquitination-regulated pathways may prevent compensatory resistance mechanisms that limit single-agent efficacy.
Immunotherapy Integration: Ubiquitination significantly influences immune checkpoint regulation, particularly PD-1/PD-L1 stability [35]. Tumor cells frequently upregulate deubiquitinases to remove ubiquitin from PD-L1, enhancing its surface expression and immune suppressive function [35]. Combining ubiquitination modulators with immunotherapy represents a promising strategy to enhance antitumor immune responses.
The future ubiquitination research landscape will focus on developing more selective inhibitors, elucidating the dynamics of ubiquitination networks, and advancing precision medicine approaches based on individual tumor ubiquitination profiles [35]. As our understanding of ubiquitination in cancer hallmarks deepens, so too will our ability to therapeutically manipulate this sophisticated regulatory system for patient benefit.
Advanced Methodologies for Profiling the Cancer Ubiquitinome
Protein ubiquitination is a pivotal post-translational modification that regulates diverse fundamental features of protein substrates, including stability, activity, and localization [41]. This highly conserved pathway involves the covalent attachment of ubiquitin to target proteins through a sequential enzymatic cascade involving E1 activating enzymes, E2 conjugating enzymes, and E3 ligases [42] [43]. The reverse reaction is catalyzed by deubiquitinating enzymes (DUBs), making ubiquitination a dynamic and reversible process [42]. The complexity of ubiquitin signaling arises from the ability to form various ubiquitin polymer chains with different lengths and linkage types, which function as distinct molecular signals within cells [41].
In cancer research, understanding ubiquitination pathways has become increasingly important due to their pervasive role in tumorigenesis. Genomic analyses of 9,125 tumor samples across 33 cancer types from The Cancer Genome Atlas revealed that ubiquitin pathway genes are frequently altered in cancer, with specific driver candidates like FBXW7 and MDM2 showing cancer-type-specific mutation patterns [42]. The ubiquitin-proteasome system regulates all hallmarks of cancer, including cell cycle progression, metabolic reprogramming, immune evasion, and DNA damage response [43]. Consequently, comprehensive mapping of ubiquitination sites across different cancer types provides critical insights for developing targeted therapies and biomarkers.
Enrichment Strategies for Ubiquitinated Proteins
The low stoichiometry of ubiquitinated proteins necessitates efficient enrichment strategies prior to mass spectrometry analysis. Several approaches have been developed, each with distinct advantages and limitations for specific research contexts.
Affinity Tag-Based Enrichment
Tag-based ubiquitination enrichment involves genetically engineering cells to express ubiquitin fused to an affinity tag, enabling purification of ubiquitinated proteins under controlled conditions.
- His-Tag Purification: The 6xHis-tagged ubiquitin system allows purification under denaturing conditions using nickel chromatography, significantly reducing non-specific protein interactions [44] [41]. Peng et al. pioneered this approach in yeast, identifying 1,075 potential ubiquitinated proteins and 110 ubiquitination sites on 72 proteins [44]. A modified tandem tag system (His-biotin) implemented by Tagwerker et al. employed two-step purification under denaturing conditions, identifying 258 ubiquitinated proteins with reduced background [44].
- Strep-Tag Purification: Danielsen et al. utilized Strep-tagged ubiquitin with Strep-Tactin resins, identifying 753 ubiquitination sites on 471 proteins in human cell lines [41]. This approach offers an alternative to His-tag purification with different specificity profiles.
The table below summarizes key studies utilizing affinity tag-based enrichment:
Table 1: Affinity Tag-Based Enrichment Studies
| Study | Tag System | Biological System | Proteins Identified | Ubiquitination Sites |
|---|---|---|---|---|
| Peng et al. [44] | (His)6-Ub | Yeast | 1,075 | 110 sites on 72 proteins |
| Hitchcock et al. [44] | (His)6-Ub | Yeast (ERAD pathway) | 211 | 34 sites on 29 proteins |
| Tagwerker et al. [44] | (His)6-biotin-Ub | Yeast | 258 | 21 sites on 15 proteins |
| Danielsen et al. [41] | Strep-tag-Ub | Human cells (U2OS, HEK293T) | 471 proteins | 753 sites |
While tag-based approaches are powerful for discovery, they require genetic manipulation and may not completely mimic endogenous ubiquitination due to potential structural alterations of tagged ubiquitin [41].
Antibody-Based Enrichment
Antibody-based methods enable the study of endogenous ubiquitination without genetic engineering, making them suitable for clinical samples and tissues.
- Pan-Specific Ubiquitin Antibodies: Antibodies like P4D1 and FK1/FK2 recognize all ubiquitin linkages. Denis et al. used FK2 affinity chromatography to enrich ubiquitinated proteins from MCF-7 breast cancer cells, identifying 96 ubiquitination sites [41]. Matsumoto et al. compared native and denaturing conditions for antibody affinity capture, identifying 670 and 345 proteins respectively [44].
- Linkage-Specific Antibodies: Antibodies have been developed that specifically recognize particular ubiquitin chain linkages (M1, K11, K27, K48, K63) [41]. For example, Nakayama et al. generated a K48-linkage specific antibody and demonstrated abnormal accumulation of K48-linked polyubiquitinated tau proteins in Alzheimer's disease [41].
- Diglycine Remnant Antibodies: A popular approach involves tryptic digestion of samples followed by enrichment of peptides containing the diglycine remnant (K-ε-GG) left on modified lysine residues, using specific antibodies [41] [45] [46]. However, this method shows some bias toward certain sequences and cannot distinguish ubiquitination from modifications by other ubiquitin-like proteins [47].
- UbiSite Antibody: Akimov et al. developed the UbiSite antibody that recognizes a 13-amino-acid remnant specific to ubiquitin after LysC digestion, overcoming limitations of diglycine-based approaches [47]. This method identified over 63,000 ubiquitination sites on more than 9,000 proteins in human cell lines, demonstrating the widespread nature of ubiquitination across all cellular processes [47].
Ubiquitin-Binding Domain (UBD) Based Enrichment
Proteins containing ubiquitin-binding domains (UBDs) can be utilized to capture ubiquitinated proteins. While single UBDs typically have low affinity, engineered tandem-repeated UBDs (TUBEs) exhibit significantly improved binding capacity and protect ubiquitin chains from deubiquitinase activity [41]. Mayor et al. employed an affinity column with the Rpn10 UBD under native conditions, identifying 127 ubiquitinated proteins [44].
Comparative Analysis of Enrichment Methodologies
Each enrichment strategy offers distinct advantages and limitations, making them suitable for different research applications. The table below provides a systematic comparison of these approaches:
Table 2: Comparison of Ubiquitin Enrichment Strategies
| Method | Key Advantage | Principal Limitation | Throughput | Suitable for Tissue Samples | Linkage Specificity |
|---|---|---|---|---|---|
| His-Tag | Effective under denaturing conditions; low non-specific binding | Requires genetic manipulation; potential artifacts from tagged Ub | High | No | No |
| Strep-Tag | Strong binding affinity; different specificity profile | Requires genetic manipulation; co-purification of biotinylated proteins | High | No | No |
| Pan-Ub Antibody | Works with endogenous ubiquitination; no genetic manipulation needed | Non-specific binding; high antibody cost | Medium | Yes | No |
| K-ε-GG Antibody | Enriches modified peptides directly; avoids protein-level contaminants | Sequence bias; cannot distinguish from Ubl modifications | High | Yes | No |
| UbiSite Antibody | Ubiquitin-specific; avoids sequence bias of K-ε-GG | Requires LysC digestion; relatively new method | High | Yes | No |
| Linkage-Specific Antibody | Provides linkage information directly | Limited to specific chain types; availability/cost | Medium | Yes | Yes |
| UBD/TUBE | Works with endogenous ubiquitination; protects chains from DUBs | Potential preference for certain chain types | Medium | Yes | Variable |
Ubiquitination Site Mapping by Mass Spectrometry
Mass Spectrometry Platforms and Detection Principles
Mass spectrometry has emerged as the primary technology for high-sensitivity mapping of ubiquitination sites. Two common proteomics platforms are widely used:
- GeLC-MS/MS: Protein mixtures are separated by SDS-PAGE, followed by in-gel digestion and LC-MS/MS analysis of resulting peptides [44].
- LC/LC-MS/MS: Digested peptide mixtures are resolved using two-dimensional chromatography prior to tandem mass spectrometry analysis [44].
After trypsin digestion, ubiquitinated peptides carry a characteristic di-glycine remnant (-GG) with a monoisotopic mass shift of 114.043 Da on the modified lysine residue [44] [41]. Miscleavages can generate a longer tag (-LRGG) [44]. Database-searching algorithms detect these characteristic mass shifts to identify ubiquitination sites from MS/MS spectra.
Advanced MS Applications in Ubiquitinomics
Recent technological advances have significantly expanded ubiquitinomics capabilities:
- Quantitative Ubiquitinomics: Integration of label-free quantification (LFQ) and data-independent acquisition (DIA) enables precise quantification of ubiquitination changes under different conditions [48] [45]. A 2025 study by Hao et al. combined 4D-LFQ technology with K-ε-GG-based enrichment to profile ubiquitome changes in maize during viral infection, demonstrating how ubiquitination regulates metabolic pathways during stress responses [45].
- Tissue-Specific Ubiquitinome Mapping: Becher et al. employed single-step immunoenrichment of di-glycine modified peptides to map over 20,000 unique ubiquitination sites across murine tissues, revealing both core signaling pathways common to all tissues and tissue-specific ubiquitination networks, with particular complexity in brain tissue [46].
- Pan-Cancer Ubiquitinome Analysis: Integrated genomic analysis of ubiquitination pathways across cancer types has identified significant therapeutic targets. For instance, FBXW7, a component of the SCF ubiquitin ligase complex, shows distinct mutation patterns across uterine cancers, melanoma, and gastrointestinal cancers [42].
Cancer-Relevant Ubiquitination Pathways and Therapeutic Targeting
Ubiquitination regulates numerous cancer-relevant pathways, making its comprehensive mapping critical for therapeutic development. The diagram below illustrates key ubiquitination-regulated pathways in cancer:
Key cancer-relevant ubiquitination pathways include:
- Cell Cycle Regulation: FBXW7 mediates degradation of cell cycle promoters including cyclin E, c-Myc, and mTOR [42]. Dysregulation of this ubiquitination pathway promotes uncontrolled proliferation.
- Tumor Suppressor Control: MDM2, frequently amplified in cancers, targets p53 for ubiquitin-mediated degradation [42].
- Immune Checkpoint Regulation: The ubiquitin-proteasome system regulates PD-1/PD-L1 protein levels in the tumor microenvironment [43]. USP2 deubiquitinase stabilizes PD-1 and promotes tumor immune escape [43].
- Metabolic Reprogramming: Parkin E3 ligase ubiquitinates pyruvate kinase M2 (PKM2), while OTUB2 deubiquitinase inhibits this modification, enhancing glycolysis and accelerating colorectal cancer progression [43].
Therapeutic strategies targeting ubiquitination include:
- PROTACs (Proteolysis Targeting Chimeras): Bifunctional molecules that recruit E3 ligases to target specific proteins for degradation. ARV-110 and ARV-471 have progressed to phase II clinical trials [43].
- Molecular Glues: Small molecules that induce proximity between E3 ligases and target proteins. CC-90009 promotes GSPT1 degradation and is in phase II trials for leukemia [43].
- DUB Inhibitors: Compounds targeting deubiquitinating enzymes to modulate protein stability.
The Scientist's Toolkit: Essential Research Reagents
Table 3: Essential Research Reagents for Ubiquitin Proteomics
| Reagent Category | Specific Examples | Research Application |
|---|---|---|
| Affinity Tags | 6xHis-tag, Strep-tag, HA-tag, FLAG-tag | Purification of ubiquitinated proteins from engineered systems |
| Ubiquitin Antibodies | P4D1, FK1/FK2, K-ε-GG, UbiSite, linkage-specific antibodies | Enrichment of endogenous ubiquitinated proteins or peptides |
| UBD Reagents | TUBEs (tandem ubiquitin-binding entities) | Protection and purification of ubiquitin chains |
| Mass Spectrometry Platforms | GeLC-MS/MS, LC/LC-MS/MS, 4D-LFQ systems | Identification and quantification of ubiquitination sites |
| Protease Inhibitors | MG132, bortezomib | Inhibition of proteasomal degradation to stabilize ubiquitinated proteins |
| Bioinformatic Tools | Database search algorithms, ubiquitinome analysis software | Identification and interpretation of ubiquitination sites from MS data |
Experimental Workflow for Ubiquitinomics
A comprehensive ubiquitinomics experiment follows a structured workflow from sample preparation to data analysis, as illustrated below:
Key methodological considerations for each step include:
- Sample Preparation: Use of proteasome inhibitors (e.g., MG132) to preserve ubiquitinated proteins; application of denaturing conditions to minimize deubiquitination and protein-protein interactions [44] [45].
- Enrichment Strategy Selection: Choice between tag-based, antibody-based, or UBD-based methods depending on research questions, sample availability, and need for genetic manipulation.
- Proteolytic Digestion: Trypsin digestion for K-ε-GG remnant generation or LysC digestion for UbiSite approach; consideration of enzyme specificity and efficiency [47].
- Mass Spectrometry Analysis: Method selection based on quantification needs (label-free vs. labeled approaches); data-independent acquisition for comprehensive peptide detection [48].
- Data Analysis and Validation: Implementation of appropriate false discovery rate controls; orthogonal validation using Western blotting, mutagenesis, or functional assays [44].
Mass spectrometry-based proteomics has revolutionized our ability to comprehensively map ubiquitination sites and understand their functional implications in cancer biology. The continuous improvement of enrichment strategies, from early tag-based approaches to sophisticated antibody-based methods, has dramatically expanded the depth and precision of ubiquitinome analyses. The integration of quantitative proteomics with genomic and transcriptomic data enables researchers to place ubiquitination events within the broader context of cellular signaling networks dysregulated in cancer.
Future directions in the field include developing more robust methods for characterizing ubiquitin chain architecture, improving the sensitivity of detection for low-abundance ubiquitination events, and implementing spatial proteomics approaches to map ubiquitination within subcellular compartments. As large-scale ubiquitinome mapping becomes increasingly accessible, these datasets will provide invaluable resources for identifying novel therapeutic targets and biomarkers across cancer types, ultimately advancing toward more personalized cancer therapeutics.
The identification of ubiquitinated substrates is a cornerstone for understanding the role of ubiquitination in cellular regulation and cancer pathogenesis. Affinity tagging of ubiquitin provides a powerful methodological framework for capturing and characterizing these transient modifications. This guide objectively compares the performance of three principal tagging systems—HIS, Strep, and epitope tags (such as FLAG)—in the context of ubiquitin substrate identification. We evaluate these tags based on purity, yield, specificity, and compatibility with mass spectrometric analysis, supported by experimental data. The strategic selection of an affinity tag is paramount for researchers and drug development professionals aiming to decipher ubiquitination pathways dysregulated across cancer types, ultimately informing the development of targeted therapies.
Ubiquitination is a dynamic post-translational modification that regulates fundamental cellular processes, including protein degradation, signal transduction, and DNA repair [49]. The versatility of ubiquitin signaling arises from the complexity of ubiquitin conjugates, which can vary in length, linkage type, and architecture [49]. In cancer, the dysregulation of ubiquitination pathways—governed by the orchestrated interplay of E3 ubiquitin ligases and deubiquitinases (DUBs)—can drive tumorigenesis, metastasis, and therapeutic resistance [36]. For instance, recent studies have revealed that the ubiquitination of RAS proteins profoundly impacts their stability, membrane localization, and oncogenic functions [50].
To crack the molecular mechanisms of specific ubiquitin ligase-substrate pairs, researchers require robust methods to isolate and identify ubiquitinated proteins from complex cellular milieus. A key strategy involves the exogenous expression of ubiquitin fused to an affinity tag. This approach covalently labels cellular ubiquitination substrates, enabling their subsequent enrichment and analysis [49]. The choice of affinity tag directly impacts the success of these investigations by influencing the efficiency, purity, and functional integrity of the isolated substrates. This guide provides a comparative analysis of the most prevalent tagging systems to inform experimental design in cancer and basic research.
Comparison of Ubiquitin Tagging Systems
We focus on three widely used affinity tags for ubiquitin substrate identification: the HIS-tag, the Strep-tag, and epitope tags like the FLAG-tag. The table below summarizes their core characteristics and performance metrics based on published literature and commercial data.
Table 1: Performance Comparison of Key Affinity Tags for Protein Purification
| Tag Type | Typical Sequence | Binding Partner / Matrix | Elution Method | Typical Purity | Typical Yield | Relative Cost |
|---|---|---|---|---|---|---|
| HIS-tag | H6-10 | Ni2+ or Co2+-NTA | Imidazole (0.25 - 1 M) | Moderate to Low [51] [52] | High [51] | Low [51] |
| Strep-tag II | WSHPQFEK | Strep-Tactin | Biotin or Desthiobiotin | High / Excellent [51] [52] | Good [51] | Moderate [51] |
| FLAG-tag | DYKDDDK | Anti-FLAG Antibody (e.g., M2) | Low pH or FLAG Peptide [53] [54] | High [51] | Moderate [51] | High [51] |
HIS-Tag
The HIS-tag, a stretch of six to ten histidine residues, is one of the most commonly used affinity tags [54]. It binds with high capacity to nickel- or cobalt-charged nitrilotriacetic acid (NTA) resins, and elution is achieved with imidazole, which competes with the histidine residues for coordination sites on the immobilized metal ions [54].
- Strengths: The key advantages of the HIS-tag are its small size, which minimizes the risk of interfering with the structure or function of the fused ubiquitin or the conjugated substrate, and its high yield from inexpensive, high-capacity resins [51]. This makes it a cost-effective option for initial protein isolation.
- Limitations for Ubiquitination Studies: The primary drawback is its moderate to low purity, as host proteins with surface-exposed histidine clusters can bind non-specifically to the resin [51] [52]. Furthermore, the binding is sensitive to strong metal-chelating agents like EDTA or EGTA, which are often present in protease inhibitor cocktails, and can be incompatible with proteins that possess essential metal cofactors [54]. A comparative study found that the HIS-tag provided relatively poor purification efficiency from complex extracts like those derived from HeLa cells [51].
Strep-Tag
The Strep-tag II (WSHPQFEK) is a short peptide that binds with high affinity and specificity to a streptavidin derivative called Strep-Tactin [54] [52]. Elution is accomplished under gentle, native conditions using biotin or its derivative desthiobiotin [54].
- Strengths: The standout feature of the Strep-tag system is its ability to provide excellent purification with high specificity, resulting in very little background contamination [54] [52]. It functions well in the presence of detergents and reducing agents, offering broad compatibility with various buffer conditions. Studies have shown it to be an acceptable compromise, offering excellent purification with good yields at a moderate cost [51]. The system is particularly useful when a single-step purification is required.
- Limitations for Ubiquitination Studies: While the affinity is high, the binding capacity of Strep-Tactin resin is generally lower than that of Ni-NTA, which can be a consideration for preparative-scale purifications. The cost, though moderate, is higher than that of HIS-tag purification.
Epitope Tags (FLAG-tag)
Epitope tags are short peptide sequences for which highly specific antibodies are available. The FLAG-tag (DYKDDDK) is a prime example, rationally designed to be small, hydrophilic, and well-tolerated by most proteins, potentially even increasing their solubility [54]. FLAG-tagged proteins are typically purified using an anti-FLAG antibody resin and eluted with a low pH buffer or, more gently, by competition with an excess of the FLAG peptide [53] [54].
- Strengths: The primary strength of the FLAG-tag and similar epitope tags is the high purity of the isolated protein from diverse extract sources, including mammalian cell lines [51]. The availability of different antibodies (e.g., M1, M2) allows for flexibility; the M2 antibody, for instance, can bind tags at either the N- or C-terminus [54]. The gentle elution with the FLAG peptide helps maintain the native structure and activity of the purified ubiquitin conjugates.
- Limitations for Ubiquitination Studies: The main limitation is the high cost associated with the antibody-based resins, which also have a lower binding capacity compared to Ni-NTA resins [51]. Low pH elution, an alternative to peptide competition, carries a risk of denaturing the protein of interest [53].
Experimental Protocols for Ubiquitin Substrate Identification
The following section outlines key methodologies that leverage affinity tags to identify and validate ubiquitinated substrates, incorporating recent technological advances.
Ubiquitin Tagging-Based Proteomics
This is a foundational approach for high-throughput profiling of the ubiquitinome.
- Plasmid Construction: Clone the gene for ubiquitin, N-terminally tagged with your chosen affinity tag (e.g., 6xHis, Strep-tag II, or FLAG), into a mammalian expression vector.
- Cell Culture and Transfection: Culture relevant cells (e.g., HEK293T, U2OS) and transfect them with the tagged-ubiquitin construct. For studies targeting a specific E3 ligase, co-transfect with a plasmid expressing the ligase of interest.
- Cell Lysis: Harvest cells and lyse them in a suitable non-denaturing lysis buffer (e.g., RIPA buffer). For HIS-tag purifications, ensure the buffer contains no EDTA or EGTA, and consider including a low concentration (5-50 mM) of imidazole in the load and wash buffers to reduce non-specific binding [54].
- Affinity Enrichment: Incubate the clarified cell lysate with the appropriate resin:
- HIS-tag: Ni-NTA agarose beads.
- Strep-tag: Strep-Tactin beads.
- FLAG-tag: Anti-FLAG M2-agarose beads.
- Incubate for 1-2 hours at 4°C with gentle agitation.
- Washing: Wash the beads extensively with lysis buffer to remove non-specifically bound proteins.
- Elution:
- HIS-tag: Elute with lysis buffer supplemented with 250 mM - 1 M imidazole [54].
- Strep-tag: Elute with buffer containing biotin or desthiobiotin (e.g., 2.5 mM) [54].
- FLAG-tag: Elute with lysis buffer containing 100-200 µg/mL of 3x FLAG peptide, or alternatively, with a low pH buffer (e.g., 0.1 M glycine-HCl, pH 3.5) [53] [54].
- Analysis: The eluted proteins can be analyzed by immunoblotting to confirm ubiquitination or prepared for mass spectrometry (MS) to identify specific substrates and ubiquitination sites.
The TR-TUBE Method for Stabilizing Ubiquitinated Substrates
A significant challenge in identifying ubiquitin ligase substrates is the transient nature of ubiquitination, as substrates are rapidly deubiquitinated or degraded by the proteasome. A powerful solution to this problem is the use of Tandem Ubiquitin-Binding Entities (TUBEs). The following workflow, which can be combined with affinity tags, stabilizes polyubiquitin chains in cells.
Diagram 1: TR-TUBE method for substrate stabilization.
- Principle: TR-TUBE is a recombinant protein composed of multiple ubiquitin-associated domains (UBDs) with trypsin-resistant linkers. When expressed in cells, it binds with high affinity to polyubiquitin chains on substrates, physically shielding them from deubiquitinating enzymes (DUBs) and the proteasome, thereby leading to their accumulation [55].
- Methodology:
- Co-express a FLAG-tagged TR-TUBE along with your E3 ubiquitin ligase of interest in cells.
- The TR-TUBE will stabilize substrates ubiquitinated by both the exogenous and endogenous ligases.
- Lyse cells and perform immunoprecipitation using anti-FLAG beads to isolate the TR-TUBE/substrate complexes [55].
- Elute and analyze the co-precipitated ubiquitinated substrates by immunoblotting or MS.
- Advantages: This method allows for the direct detection of a specific ligase's activity and the isolation of its native substrates without the need for global proteasome inhibition, which can create high background [55].
DiGly Antibody-Based Site Mapping
After enriching ubiquitinated proteins via affinity tags, identifying the exact site of ubiquitination is crucial. This is achieved using an antibody that recognizes the diglycine (diGly) remnant left on the modified lysine residue after tryptic digestion.
- Sample Preparation: The enriched ubiquitinated protein sample is denatured, reduced, alkylated, and digested with trypsin.
- diGly Enrichment: The resulting peptides are incubated with an anti-diGly (Lys-ε-Gly-Gly) antibody to specifically immunoprecipitate peptides derived from ubiquitinated proteins [55] [49].
- Mass Spectrometry: The enriched diGly-modified peptides are analyzed by LC-MS/MS. The identification of a lysine residue with a 114.04 Da mass shift (the diGly signature) localizes the ubiquitination site [49].
This method can be combined with the TR-TUBE approach. While the diGly antibody alone is effective, co-expression of TR-TUBE with an E3 ligase has been shown to significantly elevate the levels of substrate-derived diGly peptides specific to that ligase, enhancing their detection against the background [55].
The Scientist's Toolkit: Key Research Reagents
Table 2: Essential Reagents for Ubiquitin Substrate Identification
| Reagent / Tool | Function in Ubiquitination Studies | Example Use Case |
|---|---|---|
| Tagged-Ubiquitin Plasmids | Serves as the donor for affinity-based purification of ubiquitinated substrates. | 6xHis-Ub, Strep-Ub, or FLAG-Ub vectors for global ubiquitinome profiling [49]. |
| TR-TUBE Plasmids | Stabilizes polyubiquitinated substrates in cells by blocking deubiquitination and degradation. | FLAG-TR-TUBE for identifying substrates of a specific co-expressed E3 ligase [55]. |
| Anti-diGly Antibody | Enriches for tryptic peptides containing the ubiquitination signature; critical for site identification by MS. | Immunoprecipitation of diGly-modified peptides from digested protein samples for proteomics [55] [49]. |
| Linkage-Specific Ub Antibodies | Detects or enriches for polyubiquitin chains with a specific linkage type (e.g., K48, K63). | Determining the chain topology on a substrate of interest via Western blot or enrichment [49]. |
| Proteasome Inhibitor (MG132) | Blocks degradation of ubiquitinated proteins, leading to their accumulation. | Used in conjunction with other methods to enhance the recovery of proteasome-targeted substrates [55]. |
The selection of an affinity tag for ubiquitin substrate identification involves a careful trade-off between purity, yield, cost, and experimental goals. The HIS-tag offers a high-yield, low-cost entry point but often at the expense of purity. The Strep-tag system strikes an excellent balance, delivering high purity and good yield under mild conditions for a moderate cost. Epitope tags like FLAG provide superior purity, particularly from mammalian systems, but require a higher budget.
For the challenging task of identifying specific E3 ubiquitin ligase substrates, the integration of TR-TUBE technology with these affinity tags represents a cutting-edge methodology. By stabilizing the ubiquitinated proteome, it overcomes the inherent lability of these modifications. Ultimately, combining a robust enrichment strategy (using HIS, Strep, or FLAG tags) with stabilization tools (TUBEs) and precise analytical methods (diGly proteomics) provides a comprehensive and powerful pipeline for decoding the ubiquitin code in cancer and beyond, paving the way for novel therapeutic interventions.
Linkage-Specific Antibodies and Ubiquitin-Binding Domains for Enrichment of Modified Proteins
The ubiquitin code, a complex post-translational modification system, regulates virtually all aspects of eukaryotic cell biology, with particular significance in cancer signaling pathways [56]. Ubiquitin can be conjugated to substrates as a single molecule or as polyubiquitin chains with distinct linkages between ubiquitin moieties, each encoding specific cellular outcomes [57]. The diversity of ubiquitin signals—including eight distinct chain linkage types (M1, K6, K11, K27, K29, K33, K48, K63) and additional non-canonical modifications—creates a challenging analytical landscape for researchers [57] [56]. To decipher this complexity, scientists have developed two principal classes of enrichment tools: linkage-specific antibodies and ubiquitin-binding domains (UBDs). These reagents enable the selective isolation and study of specific ubiquitin modifications, providing crucial insights into their roles in cancer biology, protein homeostasis, and cellular signaling networks. This guide provides a comparative analysis of these methodologies, supporting informed reagent selection for ubiquitin proteomics research in oncological contexts.
Table 1: Core Characteristics of Enrichment Tools
| Feature | Linkage-Specific Antibodies | Ubiquitin-Binding Domains (UBDs) |
|---|---|---|
| Molecular Basis | Immunoglobulin-based recognition of specific ubiquitin chain epitopes | Protein domains with natural affinity for ubiquitin surfaces |
| Primary Applications | Immunoblotting, immunofluorescence, immunoprecipitation, peptide enrichment | Affinity purification, structural studies, in vitro reconstitution |
| Key Advantage | High specificity for intended linkage; well-established protocols | Preservation of native interactions; modular engineering potential |
| Common Linkages Targeted | K48, K63, K11, M1 [58] [56] | K63, M1, K29, K33 (varies by specific UBD) [59] |
| Typical Affinity Range | High (nM-pM) [58] | Weaker (μM-mM) [59] |
| Structural Information | Epitope mapping required [58] | Often determined by X-ray crystallography/NMR [59] |
Linkage-Specific Antibodies
Linkage-specific antibodies represent immunoreagents engineered to recognize unique structural epitopes presented by specific ubiquitin linkage types. The development of these reagents marked a significant advancement in the ubiquitin field, with landmark studies producing antibodies against K63 and K48 linkages through sophisticated immunization strategies [58]. The molecular basis for their specificity was elucidated through structural approaches such as cocrystal structures of antibody-antigen complexes, revealing how complementarity-determining regions engage with linkage-specific surfaces on diubiquitin [58]. These reagents have since expanded to target multiple linkage types, including K11 and M1-linked chains, providing researchers with a versatile immunological toolkit for probing the ubiquitin code [56].
Ubiquitin-Binding Domains
Ubiquitin-binding domains (UBDs) are compact protein modules (typically 20-150 amino acids) that naturally interact with ubiquitin and are repurposed as affinity tools. Over 20 distinct UBD families have been identified, including zinc finger (NZF), ubiquitin-associated (UBA), and coupling of ubiquitin to ER degradation (CUE) domains [59] [56]. These domains typically recognize common ubiquitin surfaces such as the hydrophobic patch centered around Ile44, though with varying linkage preferences and affinities [59]. Their natural function involves transducing ubiquitin signals into cellular outcomes by recruiting ubiquitinated proteins to specific complexes or organelles, making them ideal reagents for studying physiological ubiquitin interactions [59] [56].
Comparative Performance Analysis
Specificity and Affinity Profiles
The utility of enrichment tools depends critically on their specificity and affinity for target ubiquitin linkages. Quantitative assessments reveal distinct performance characteristics across reagent classes.
Table 2: Specificity and Affinity Profiles of Major Enrichment Tools
| Tool Category | Specific Example | Preferred Linkage(s) | Affinity (KD) | Specificity Fold-Change |
|---|---|---|---|---|
| Antibodies | Anti-K63 [58] | K63-linked chains | Not quantified | Highly specific vs K48 chains |
| Anti-K48 [58] | K48-linked chains | Not quantified | Highly specific vs K63 chains | |
| Anti-M1 [56] | M1-linked chains | Not quantified | Specific vs other linkages | |
| NZF UBDs | HOIL-1L NZF [59] | M1-linked chains | 4 μM | 50-fold vs other linkages |
| TRABID NZF1 [59] | K29/K33-linked chains | Not specified | 50-fold vs other linkages | |
| TAB2 NZF [59] | K63-linked, phosphorylated K6 | Not specified | Strong preference | |
| HOIP NZF1 [59] | Monoubiquitinated substrates | 110-190 μM | No linkage preference | |
| RYBP NZF [59] | Various linkages | 255-348 μM | No linkage preference |
Applications in Experimental Workflows
Both antibody and UBD-based tools have been integrated into standardized proteomics workflows, though with distinct implementations and outcomes.
diGLY Antibody Workflow: The diGLY remnant profiling approach utilizes antibodies recognizing the Gly-Gly tag left on modified lysines after tryptic digestion [60]. This method enables identification of thousands of ubiquitination sites in single experiments, with recent technical improvements achieving greater depth from reduced starting material (down from 35mg) through optimized antibody-to-lysate ratios and cross-linking strategies [60]. A significant consideration is that this approach cannot distinguish between ubiquitin, NEDD8, and ISG15 modifications, as all generate identical diGLY signatures after trypsin digestion [60].
UBD Affinity Purification: UBD-based enrichments typically occur at the protein level under native conditions, preserving protein complexes and structural information lost in digest-based approaches [60]. However, this presents challenges with co-purifying contaminants, requiring careful optimization of washing conditions [60]. Tandem UBD configurations can significantly enhance affinity and linkage selectivity through avidity effects, making them particularly valuable for studying specific ubiquitin-dependent processes [59].
Diagram 1: Comparative Workflows for Ubiquitin Enrichment. The antibody-based path (red) utilizes denaturing conditions and peptide-level enrichment, while UBD-based approaches (blue) maintain native interactions for protein-level analysis.
Experimental Protocols
Linkage-Specific Immunoprecipitation
Purpose: To isolate and characterize proteins modified with specific ubiquitin linkages from cell lysates.
Materials:
- Linkage-specific ubiquitin antibodies (K48, K63, etc.)
- Protein A/G agarose beads
- Lysis buffer (e.g., RIPA with protease/phosphatase inhibitors)
- Wash buffer (compatible with antibody affinity)
- Elution buffer (low pH or competitive elution)
Procedure:
- Prepare cell lysates under denaturing (for antibody-based) or native (for UBD-based) conditions
- Pre-clear lysate with control beads (30-60 minutes, 4°C)
- Incubate lysate with linkage-specific antibody (2-4 hours, 4°C)
- Add Protein A/G beads and incubate (overnight, 4°C)
- Wash beads 3-5 times with appropriate wash buffer
- Elute bound proteins with SDS sample buffer or competitive elution
- Analyze by immunoblotting or mass spectrometry
Technical Notes: Denaturing conditions prevent co-purification of interacting proteins but may disrupt some epitopes. Native conditions preserve complexes but require stringent washes to reduce non-specific binding [60].
diGLY Remnant Peptide Enrichment
Purpose: To comprehensively identify ubiquitination sites by enriching tryptic peptides containing the diGLY modification.
Materials:
- diGLY remnant motif antibody (commercially available)
- Cross-linked antibody beads
- Strong cation exchange (SCX) StageTips
- Sera-Mag beads for clean-up
- LC-MS/MS system
Procedure:
- Digest cellular proteins to peptides using trypsin
- Desalt peptides using C18 StageTips
- Incubate peptides with diGLY antibody beads (overnight, 4°C)
- Wash beads to remove non-specifically bound peptides
- Elute enriched diGLY-modified peptides
- Clean up eluate using Sera-Mag beads
- Analyze by LC-MS/MS
Technical Notes: Proteasome inhibitors (e.g., MG132) can be used to increase ubiquitylation levels and enhance detection of low-abundance substrates. Approximately 6% of identified diGLY peptides may result from NEDDylation rather than ubiquitylation [60].
Signaling Pathways and Biological Applications
Ubiquitin Editing in NF-κB Signaling
Linkage-specific tools have been instrumental in elucidating dynamic ubiquitination events in innate immune signaling. Research using K63 and K48 linkage-specific antibodies revealed the "ubiquitin editing" phenomenon in NF-κB activation, where signaling components initially acquire K63-linked chains for activation, followed by replacement with K48-linked chains for proteasomal degradation [58]. This mechanism ensures appropriate signal duration and prevents excessive inflammatory responses.
Diagram 2: Ubiquitin Editing in NF-κB Signaling. Linkage-specific tools reveal the temporal transition from K63-linked signaling chains to K48-linked degradative chains, ensuring appropriate signal duration.
Substrate Recognition by UBDs
UBDs achieve specificity through multivalent interactions that extend beyond simple ubiquitin binding. The NZF1 domain of HOIP exemplifies this principle, recognizing not only ubiquitin but also the ubiquitinated substrate itself. This domain preferentially binds NEMO ubiquitinated at K285 and optineurin ubiquitinated at K448, demonstrating how UBDs can read both the ubiquitin modification and the substrate context [59]. This dual recognition mechanism explains how low-affinity UBDs achieve specific biological outcomes despite the high cellular concentration of free ubiquitin.
Research Reagent Solutions
Table 3: Essential Research Tools for Ubiquitin Enrichment Studies
| Reagent Category | Specific Examples | Key Applications | Considerations |
|---|---|---|---|
| Linkage-Specific Antibodies | Anti-K48, Anti-K63, Anti-M1, Anti-K11 [58] [56] | Immunoblotting, immunofluorescence, immunoprecipitation | Validate for intended application; check cross-reactivity |
| diGLY Remnant Antibodies | Commercial monoclonal antibodies [60] | Ubiquitin site mapping by mass spectrometry | Recognizes NEDD8/ISG15 modifications; sequence bias reported |
| Engineered UBD Reagents | TAB2 NZF, HOIL-1L NZF, TRABID NZFs [59] | Affinity purification, linkage-specific enrichment | Weaker affinity requires optimized conditions; can be engineered |
| UBD Expression Constructs | Plasmids encoding various UBDs [59] | Recombinant protein production, pulldown assays | Can be tagged for detection (GST, His, FLAG) |
| DUB Inhibitors | Broad-spectrum DUB inhibitors [60] | Stabilize ubiquitylated substrates | Acute inhibition effects differ from genetic knockdown |
| Proteasome Inhibitors | MG132, bortezomib [60] | Enhance ubiquitylated protein detection | Increases global ubiquitylation but may alter biology |
Linkage-specific antibodies and ubiquitin-binding domains provide complementary approaches for dissecting the complexity of the ubiquitin code. Antibodies offer high specificity and sensitivity for well-characterized linkages, making them ideal for diagnostic applications and targeted studies. UBDs provide insights into native interactions and can be engineered for novel specificities, advancing our understanding of physiological ubiquitin signaling. The continued development and refinement of these tools will be essential for unraveling the roles of specific ubiquitin modifications in cancer pathways and developing targeted therapeutic strategies. Selection between these approaches should be guided by experimental objectives, with antibodies favoring sensitivity and standardization, and UBDs offering physiological relevance and engineering potential.
Protein ubiquitination has emerged as a critical regulatory mechanism in cancer pathogenesis, representing a promising frontier for therapeutic intervention. This post-translational modification, orchestrated by the sequential action of E1 activating, E2 conjugating, and E3 ligase enzymes—and reversed by deubiquitinating enzymes (DUBs)—controls protein stability, localization, and function [61]. The intricate nature of ubiquitination pathways, coupled with their pervasive role in oncogenic and tumor suppressive processes, necessitates sophisticated computational approaches to unravel their complexity. Multi-omics integration provides a powerful framework to reconstruct ubiquitination regulatory networks, bridging molecular layers from genomic alterations to proteolytic outcomes. For drug development professionals, these networks offer unprecedented opportunities to identify novel targets, particularly for proteins traditionally considered "undruggable" through conventional approaches [61]. This guide compares computational methods for building ubiquitination networks, evaluates their performance, and provides practical protocols for implementation in cancer research settings.
Computational Methodologies for Network Inference
Network-Based Multi-Omics Integration Approaches
Table 1: Categories of Network-Based Multi-Omics Integration Methods
| Method Category | Key Algorithms | Ubiquitination Applications | Strengths | Limitations |
|---|---|---|---|---|
| Network Inference | MINIE, Bayesian networks, Differential-algebraic equations | Inference of ubiquitination enzyme-substrate relationships from time-series data [62] | Captures causal, directional relationships; models timescale separation between molecular layers [62] | Computationally intensive; requires temporal data |
| Network Propagation/Diffusion | Random walk with restart, Heat diffusion, Diffusion kernel networks | Prioritizing ubiquitin-related disease genes; identifying functional modules [63] | Robust to noise; leverages network topology for signal amplification | May infer indirect associations; dependent on prior network quality |
| Graph Neural Networks | Graph convolutional networks, Graph attention networks, Multi-view learning | Predicting novel ubiquitination interactions; integrating structural and sequence data [64] | Captures non-linear, high-order relationships; powerful for prediction tasks | "Black box" nature challenges interpretation; data hungry |
| Similarity-Based Integration | Matrix factorization, Multi-omics clustering | Ubiquitination subtype identification; patient stratification [63] | Intuitive; works with static data; identifies co-regulated modules | Limited causal inference; primarily identifies correlations |
Method-Specific Performance Comparisons
MINIE (Multi-omIc Network Inference from timE-series data) represents a specialized approach for dynamic network inference that explicitly addresses the timescale separation between molecular layers—a critical consideration when modeling ubiquitination, which occurs rapidly compared to transcriptional changes [62]. The method employs a Bayesian regression framework to integrate single-cell transcriptomics with bulk metabolomics or proteomics data, formulating the network inference problem through differential-algebraic equations (DAEs). This architecture enables MINIE to accurately capture the rapid dynamics of ubiquitination events relative to slower transcriptional responses. Benchmarking studies demonstrate MINIE's superior performance against single-omic methods, particularly in identifying cross-layer regulatory relationships [62].
Graph Neural Networks (GNNs) have shown remarkable performance in predicting novel ubiquitination sites and enzyme-substrate relationships by integrating structural information with multi-omic profiles [64]. These methods operate on graph-structured data where nodes represent biological entities (proteins, genes, metabolites) and edges represent their interactions. Through message-passing mechanisms, GNNs aggregate information from local neighborhoods to generate node embeddings that capture both node features and network topology. In comprehensive benchmarks for link prediction (identifying missing ubiquitination interactions), GNNs consistently rank among top performers, particularly when trained on heterogeneous networks combining protein-protein interaction, genetic interaction, and gene expression data [63].
Network Propagation Methods excel at prioritizing ubiquitination-related genes and identifying functional modules dysregulated in cancer. These approaches simulate the flow of information through molecular networks, starting from seed nodes (e.g., known ubiquitination enzymes) and diffusing signal along edges to identify regions of the network enriched for relevant functions [63]. Validation studies demonstrate that network propagation significantly outperforms methods that do not incorporate network information, with random walk with restart showing particular strength in identifying novel cancer-associated ubiquitination enzymes when seeded with known candidates [63].
Experimental Protocols for Network Validation
Integrative Multi-Omics Analysis of Ubiquitination in Pancreatic Cancer
Objective: To identify and validate key ubiquitination regulators in pancreatic cancer through multi-omics integration.
Experimental Workflow:
Protocol Details:
Single-Cell RNA Sequencing Data Processing
- Download pancreatic cancer scRNA-seq data (GSE155698) from GEO database [65] [66].
- Perform quality control using Seurat package (v4.4.0): exclude genes expressed in <3 cells, remove cells with <200 or >7000 genes, exclude cells with >15% mitochondrial gene expression [65] [66].
- Normalize data using
NormalizeDatafunction and select highly variable genes (3000 genes) using "vst" method. - Integrate samples using CCA method, perform dimensionality reduction (PCA, tSNE, UMAP with dims=20), and cluster cells using KNN (resolution=0.6) [65] [66].
Spatial Transcriptomics Validation
Ubiquitination Regulator Identification
- Obtain ubiquitination-related genes (405 genes) from GeneCard database (relevance score >10) [65] [66].
- Calculate ubiquitination scores using
irGSEA,AUCell, andUCellpackages. - Identify high-ubiquitination cell populations (High_ubiquitin-Endo) and their interactions with fibroblasts/macrophages via WNT, NOTCH, and integrin pathways using
CellChatpackage [65] [66].
Genetic Prioritization with Mendelian Randomization
- Perform Summary-data-based Mendelian Randomization (SMR) analysis using
TwoSampleMRR package (v0.6.6) with pancreatic cancer GWAS datasets (bbj-a-140, ebi-a-GCST90018673) from IEU database [65] [66]. - Apply thresholds: pSMR < 0.05 and PHEIDI > 0.05 to prioritize TRIM9 as a PC-protective gene [65] [66].
- Perform Summary-data-based Mendelian Randomization (SMR) analysis using
Co-expression Network Analysis
- Conduct Weighted Gene Co-expression Network Analysis (WGCNA) to identify TRIM9-co-expressed modules using
pickSoftThresholdfunction to determine optimal soft-thresholding power [65] [66]. - Set minimum module size to 200 genes, deepSplit=2, and correlate modules with TRIM9 expression and survival data.
- Conduct Weighted Gene Co-expression Network Analysis (WGCNA) to identify TRIM9-co-expressed modules using
Functional Validation
- In vitro: TRIM9 overexpression and knockdown assays in pancreatic cancer cells to assess proliferation and migration effects [65] [66].
- Mechanistic: Co-immunoprecipitation and ubiquitination assays to validate TRIM9-mediated K11-linked ubiquitination and proteasomal degradation of HNRNPU, testing RING domain dependency [65] [66].
- In vivo: Xenograft models with TRIM9 overexpression ± HNRNPU co-expression to assess tumor growth [65] [66].
Multi-Omics Deubiquitinating Enzyme (DUB) Profiling
Objective: To systematically characterize DUB functions and identify therapeutic targets using integrated multi-omics.
Experimental Workflow:
Protocol Details:
CRISPR-Cas9 DUB Knockout Screening
- Utilize arrayed CRISPR-Cas9 library targeting 81 DUBs with four pooled guides per target [61].
- Transfert cells and validate knockout efficiency via Western blotting for selected DUBs.
- Perform RNA sequencing to measure transcriptome-wide changes following DUB knockout.
Small Molecule DUB Inhibition
- Treat cells with seven selective DUB inhibitors, including clinical candidates targeting USP1 and USP30 [61].
- Conduct RNA sequencing to generate perturbation signatures for each inhibited DUB.
Multi-Omics Data Mining
- Extract DUB dependency scores from DepMap (CRISPR screens across 700+ cancer cell lines) [61].
- Query Connectivity Map (CMap) for genes with similar transcriptional effects as DUB knockouts.
- Integrate Cancer Cell Line Encyclopedia (CCLE) proteomics data (12,000 proteins across 375 lines) [61].
- Mine protein-protein interaction databases (BioGRID, IntAct, Pathway Commons) for DUB interactors [61].
Target Validation
- Test predicted DUB-substrate relationships using focused knockout and functional assays.
- Validate USP7-MDM2-TP53 and USP28-c-Myc axes as therapeutic paradigms [61].
The Scientist's Toolkit: Essential Research Reagents
Table 2: Key Research Reagents for Ubiquitination Network Studies
| Reagent/Resource | Specifications | Application | Source/Reference |
|---|---|---|---|
| DUB CRISPR Library | Arrayed library targeting 81 DUBs, 4 guides/target | Systematic DUB functional characterization | [61] |
| Selective DUB Inhibitors | USP1 inhibitor (KSQ Therapeutics), USP30 inhibitor (Mission Therapeutics) | Chemical perturbation of specific DUB activities | [61] |
| scRNA-seq Dataset | GSE155698, 17 pancreatic tumor samples, 16 after QC | Cell-type specific ubiquitination analysis | [65] [66] |
| Spatial Transcriptomics | GSE235315, 3 pancreatic cancer samples | Spatial validation of ubiquitination patterns | [65] [66] |
| Ubiquitination Gene Set | 405 genes with GeneCard relevance score >10 | Ubiquitination activity scoring | [65] [66] |
| DUB Portal | Integrated knowledgebase of DUB activities, co-dependent genes, and substrates | Resource for DUB target prioritization | [61] |
| DepMap Database | CRISPR dependency scores for 700+ cancer cell lines | Identification of essential DUBs across cancer types | [61] |
| CCLE Proteomics | Shotgun proteomics data for 375 cell lines, ~12,000 proteins | Protein-level correlation with DUB dependencies | [61] |
Comparative Performance Across Cancer Types
Table 3: Method Performance in Ubiquitination Network Construction
| Cancer Type | Best-Performing Method | Key Findings | Validation Approach | Therapeutic Implications |
|---|---|---|---|---|
| Pancreatic Cancer | WGCNA + SMR analysis | TRIM9 as tumor suppressor via HNRNPU ubiquitination (K11-linked) [65] [66] | In vitro proliferation/migration assays; in vivo xenografts | TRIM9 as prognostic biomarker; HNRNPU degradation strategy |
| Colorectal Cancer | Integrated proteomics/ubiquitinomics | PF-3758309 promotes POLR2A/B/E degradation via DDB2 E3 ligase [67] | MLN4924 reversal assays; ubiquitination profiling | PAK4-independent anti-tumor mechanism revealed |
| Multiple Cancers | DepMap mining + network propagation | USP7 and USP28 as priority targets for TP53 and c-Myc modulation [61] | Selective inhibitor studies; substrate stabilization assays | Indirect targeting of "undruggable" oncoproteins |
| Liver Cancer | Patient-specific GRN integration | JUND identified as transcriptional regulator of fatty acid metabolism [68] | Independent cohort validation; metabolic pathway analysis | Novel regulatory mechanisms of cancer progression |
The integration of multi-omics data through computational network inference methods has dramatically advanced our understanding of ubiquitination pathways in cancer. The comparative analysis presented herein demonstrates that method selection must be guided by specific research objectives: network inference approaches like MINIE excel for dynamic, cross-layer regulatory mapping [62]; graph neural networks offer superior performance for interaction prediction [64] [63]; and propagation methods effectively prioritize candidate genes within known networks [63]. The consistent identification of novel ubiquitination regulators across cancer types—including TRIM9 in pancreatic cancer [65] [66], DDB2-mediated POLR2 degradation in colorectal cancer [67], and USP7/USP28 across multiple malignancies [61]—validates the power of these integrative approaches. As multi-omics technologies evolve toward single-cell and spatial resolutions, computational methods must similarly advance to leverage these rich datasets. Future developments should focus on incorporating structural information, improving interpretability of complex models, and establishing standardized benchmarks for performance evaluation across diverse cancer contexts.
The ubiquitin-proteasome system (UPS) represents a crucial regulatory pathway in eukaryotic cells, with protein ubiquitination serving as one of the most abundant post-translational modifications in cellular signaling [69]. Within this hierarchical cascade, E3 ubiquitin ligases perform the essential function of determining substrate specificity, facilitating the transfer of ubiquitin to target proteins and thereby regulating their stability, localization, and activity [69] [70]. With over 600 putative E3 ligases encoded in the human genome, these enzymes collectively regulate a diverse array of cellular processes including protein degradation, cell cycle progression, DNA repair, transcription, and immune function [69]. The deregulation of this tightly controlled system has been definitively implicated in various human diseases, with particular significance in cancer pathogenesis [69] [70].
The critical importance of E3 ligases in oncology stems from their ability to control the turnover of oncoproteins and tumor suppressors. As determining factors in substrate recognition, E3 ligases represent promising therapeutic targets for cancer intervention [69] [71]. However, the development of targeted therapies has been hindered by incomplete understanding of ligase-substrate relationships and biological functions [69]. This knowledge gap has driven the development of sophisticated functional screening methods to systematically identify and validate E3 ligase substrates, underpinning rapid advances in our understanding of UPS biochemistry and biology while supporting drug development efforts targeting various aspects of UPS function [69].
Comparative Analysis of Major Screening Methodologies
BioE3: Proximity-Dependent Biotinylation Strategy
The BioE3 system represents an innovative approach for matching substrates to ubiquitin E3 ligases of interest through proximity-dependent biotinylation. This method employs BirA-E3 ligase fusions combined with bioUb (a biotinylatable ubiquitin variant) to achieve site-specific biotinylation of ubiquitin-modified substrates of particular E3 ligases, facilitating their proteomic identification [72].
Experimental Protocol Optimization: Key to the BioE3 methodology is the engineering of specificity through use of an AviTag variant with lower affinity for BirA (bioGEF) fused to ubiquitin. Compared to the wild-type AviTag (bioWHE), which demonstrates general and unspecific biotinylation independently of BirA localization, the bioGEF variant enables precise spatial-specific labeling when combined with controlled biotin availability and timing [72]. The experimental workflow involves: (1) generation of stable cell lines (e.g., HEK293FT, U2OS) with doxycycline-inducible bioGEFUb expression; (2) introduction of BirA-E3 fusion constructs into these cells under biotin-depleted conditions; (3) timed induction of bioGEFUb expression and BirA-E3 fusion production; (4) limited biotin labeling enabling proximity-dependent biotinylation of bioGEFUb as it is incorporated by the BirA-E3 fusion onto specific substrates; and (5) streptavidin capture and LC-MS/MS identification of tagged substrates [72].
Validation and Applications: Researchers have successfully applied BioE3 to identify both known and novel targets of RING-type E3 ligases including RNF4 (involved in DNA damage response and PML bodies) and MIB1 (regulating endocytosis, autophagy, and centrosome dynamics). The methodology has been extended to organelle-specific E3s (MARCH5) and poorly characterized E3s (RNF214), and has demonstrated compatibility with HECT-type E3 ligases such as NEDD4, identifying new targets linked to vesicular trafficking [72]. Furthermore, BioE3 can detect altered specificity in response to chemical treatments, opening avenues for targeted protein degradation research [72].
CRISPR-Cas9 Loss-of-Function Screening
CRISPR-Cas9 screening offers a powerful genetic approach for identifying E3 ligases involved in specific cancer-relevant pathways. This method enables systematic functional assessment of ubiquitination-related genes on a genome-wide scale [73].
Experimental Protocol: A representative CRISPR screening protocol for identifying autophagy regulators involved: (1) generation of a pancreatic cancer reporter cell line (AsPC-1) stably expressing mCherry-GFP-LC3 autophagy flux reporter; (2) transduction with a pooled CRISPR library containing 11,108 sgRNAs targeting 660 ubiquitin-related proteins (E1, E2, E3 ligases, and deubiquitinating enzymes) plus 1000 non-targeting control sgRNAs; (3) induction of autophagy with Torin1 treatment; (4) fluorescence-activated cell sorting (FACS) to isolate cells with impaired autophagy (high GFP:mCherry ratio); (5) sequential expansion and sorting through multiple rounds to enrich for autophagy-defective populations; and (6) genomic DNA extraction and next-generation sequencing followed by MAGeCK-VISPR analysis to identify significantly enriched sgRNAs [73].
Key Findings: This approach successfully identified known autophagy regulators including ATG7, FBXO2, TBC1D25, UCHL1, and USP18, validating the screening methodology. Notably, it revealed G2E3, a G2/M-phase-specific E3 ubiquitin ligase not previously associated with autophagy, as a novel autophagy regulator. Functional validation confirmed that G2E3 knockout impaired autophagosome-lysosome fusion through interactions with GABARAP and GABARAPL1, establishing its role in late-stage autophagy and cancer cell progression [73].
Proteolysis-Targeting Chimera (PROTAC) Screening
PROTAC technology represents a chemical biology approach that leverages the ubiquitin-proteasome system for targeted protein degradation, simultaneously providing insights into E3 ligase substrate preferences and functional relationships [74].
Experimental Framework: PROTAC molecules are heterobifunctional compounds consisting of one ligand that binds to an E3 ubiquitin ligase, another ligand that binds to a protein of interest (POI), and a linker connecting them. The PROTAC induces formation of a ternary complex (E3-degrader-POI) that results in POI ubiquitination and subsequent degradation by the proteasome. Systematic characterization of E3 ligases for PROTAC development involves assessment of multiple parameters: (1) chemical ligandability (availability of binders); (2) expression patterns in tumor versus normal tissues; (3) protein-protein interaction networks; (4) structure availability; (5) functional essentiality; (6) cellular localization; and (7) protein-protein interaction interfaces [74].
Current Landscape and Opportunities: Analysis reveals that while over 600 E3 ligases exist in the human genome, less than 2% have been utilized in PROTAC development, with clinical-phase PROTACs predominantly recruiting only VHL or CRBN [74]. Systematic characterization has identified 76 E3 ligases as promising candidates for future PROTAC development, including RNF4, HUWE1, and FBXO7, which have high confidence scores similar to currently employed E3s [74]. Expansion of the PROTACtable E3 ligase universe addresses several limitations of current approaches: reducing on-target toxicities through tissue-selective E3 expression, circumventing acquired resistance due to E3 ligase mutations, and targeting challenging proteins through diverse E3-substrate relationships [74].
Pancancer Ubiquitination Network Analysis
Advanced bioinformatics approaches integrating multi-omics data enable systematic construction of ubiquitination regulatory networks across cancer types, providing insights into E3 ligase functions and substrate relationships in tumor biology [24].
Methodological Framework: This methodology involves: (1) integration of transcriptomic, genomic, and clinical data from large patient cohorts across multiple cancer types; (2) identification of key nodes and prognostic pathways within ubiquitination networks; (3) development of ubiquitination-related prognostic signatures (URPS) through Cox regression and LASSO analysis; (4) validation of prognostic models using independent patient cohorts; (5) functional enrichment analysis to identify downstream pathways; and (6) experimental validation of key interactions through in vitro and in vivo models [24].
Key Insights: A pan-cancer analysis integrating data from 4,709 patients across 26 cohorts and five solid tumor types identified OTUB1-TRIM28 ubiquitination as a crucial regulator of the MYC pathway, influencing patient prognosis and immunotherapy response [24]. The resulting ubiquitination score positively correlated with squamous or neuroendocrine transdifferentiation in adenocarcinoma and effectively stratified patients into distinct risk categories with differential survival outcomes and treatment responses [24].
Table 1: Comparative Analysis of E3 Ligase-Substrate Screening Methodologies
| Method | Key Principle | Throughput | Key Applications | Technical Considerations |
|---|---|---|---|---|
| BioE3 | Proximity-dependent biotinylation with BirA-E3 fusions and bioUb | Medium | Identification of direct substrates for specific E3s; works with RING and HECT E3s | Requires optimization of biotin labeling timing; bioGEF tag essential for specificity |
| CRISPR-Cas9 Screening | Genetic knockout of ubiquitin-related genes with phenotypic readout | High | Functional discovery of E3s in specific pathways (e.g., autophagy) | Identifies pathway involvement but not direct substrates; requires robust phenotypic assay |
| PROTAC Screening | Chemical induction of ternary complexes for targeted degradation | Medium | Assessing E3 ligase engagement capacity; therapeutic development | Limited to E3s with known ligands; reveals functional relationships rather than natural substrates |
| Network Analysis | Bioinformatics integration of multi-omics data across cancer types | Very High | Identification of prognostic ubiquitination signatures; pancancer patterns | Computational predictions require experimental validation; reveals correlations rather than direct interactions |
Experimental Design and Technical Considerations
Protocol for BioE3 Implementation
Cell Line Engineering:
- Generate stable cell lines (HEK293FT or U2OS) with doxycycline-inducible bioGEFUbnc (non-cleavable ubiquitin with GEF tag) using lentiviral transduction
- Establish biotin-depletion protocol using dialyzed serum for 24 hours prior to experiments
- Transfer BirA-E3 fusion constructs into bioGEFUbnc cells using appropriate transfection methods
Biotin Labeling and Substrate Capture:
- Induce bioGEFUbnc expression and BirA-E3 production with doxycycline (24 hours)
- Add exogenous biotin for time-limited labeling (2 hours optimal for many E3s)
- Lyse cells under denaturing conditions to preserve ubiquitination status
- Perform streptavidin capture with stringent washing (e.g., 1% SDS, high salt buffers)
- Process captured proteins for LC-MS/MS analysis using tryptic digestion
Validation Approaches:
- Confirm BirA-E3 localization and functionality through immunofluorescence
- Verify substrate ubiquitination through complementary methods (e.g., immunoprecipitation, ubiquitination assays)
- Assess functional consequences of identified E3-substrate relationships through knockdown/rescue experiments [72]
CRISPR Screening Optimization Strategies
Library Design Considerations:
- Include multiple sgRNAs per target (typically 5-10) to account for variability in knockout efficiency
- Incorporate non-targeting and essential gene controls for normalization
- Use focused libraries targeting ubiquitin-related genes or genome-wide approaches depending on research question
Reporter System Selection:
- For autophagy studies: mCherry-GFP-LC3 reporter system that exploits pH sensitivity
- For protein stability assessments: fluorescent protein fusion reporters or luciferase-based degradation reporters
- For pathway-specific screening: transcriptional reporters responsive to pathway activation
Hit Validation Framework:
- Employ orthogonal validation using multiple sgRNAs targeting the same gene
- Confirm phenotype in multiple cell line models where feasible
- Assess direct versus indirect effects through mechanistic studies
- Establish physiological relevance through rescue experiments with wild-type and catalytically inactive E3 variants [73]
Table 2: Essential Research Reagents and Experimental Tools
| Reagent/Tool | Function/Application | Key Features | Example Uses |
|---|---|---|---|
| bioGEFUb | Biotinylatable ubiquitin variant for proximity labeling | Lower affinity for BirA reduces background; enables specific biotinylation | BioE3 screening; identification of E3-specific substrates |
| BirA-E3 Fusion Constructs | Targeted biotinylation at E3 ligase localization sites | Enables spatial-specific labeling of ubiquitination events | BioE3 screening; mapping subcellular sites of E3 activity |
| mCherry-GFP-LC3 Reporter | Autophagic flux measurement | pH-sensitive GFP quenches in lysosomes; mCherry stable | CRISPR screens for autophagy regulators; monitoring autophagic flux |
| PROTAC Molecules | Induced protein degradation via ternary complex formation | Heterobifunctional degraders; bridge E3 ligases to targets | Assessing E3 engagement capacity; therapeutic development |
| Ubiquitin Variants (UbVs) | Specific inhibition or activation of UPS components | Engineered ubiquitin with optimized binding properties | Functional dissection of specific E3 ligases; mechanistic studies |
Data Interpretation and Integration
Validation of Screening Hits
Robust validation of E3 ligase-substrate interactions identified through functional screening requires a multi-faceted approach. Secondary validation should include co-immunoprecipitation experiments to confirm physical interactions under physiological conditions, in vitro ubiquitination assays to demonstrate direct E3 activity toward candidate substrates, and functional assessment of substrate stability and turnover upon E3 manipulation [69] [72]. For CRISPR screening hits, rescue experiments with wild-type E3s are essential to confirm phenotype specificity, while mechanistic studies should delineate whether effects are direct or indirect [73].
The dynamic nature of protein ubiquitylation presents particular challenges for validation, as E3 ligase-substrate interactions may be transient and regulated by post-translational modifications, subcellular localization, and competing protein interactions [69]. Furthermore, significant redundancy and multiplicity within the UPS means individual protein substrates may be targeted by multiple E3s, and single E3s may have multiple protein substrates, complicating functional attribution [69].
Integration with Cancer Biology
Functional screening data gains maximum impact when integrated with cancer genomic and clinical datasets. Correlation of E3 ligase expression with patient outcomes across cancer types can prioritize candidates for therapeutic development [24] [25] [1]. For example, pancancer analyses reveal that ubiquitination-related prognostic signatures (URPS) effectively stratify patients into distinct risk categories with differential survival outcomes and treatment responses [24].
The clinical relevance of E3 ligase-substrate relationships is further supported by their association with specific oncogenic pathways. For instance, the OTUB1-TRIM28 ubiquitination axis regulates MYC pathway activity, influencing cancer cell fate decisions and therapy resistance [24]. Similarly, DTX3L emerges as a promising oncology target through its regulation of substrates including p53, androgen receptor, GSK-3β, and EGFR across multiple cancer types [75].
Functional screening methods have dramatically accelerated the identification and validation of critical E3 ligase-substrate interactions in cancer biology. The complementary approaches reviewed here—BioE3 proximity labeling, CRISPR-Cas9 genetic screening, PROTAC-based chemical screening, and computational network analysis—provide researchers with a versatile toolkit for dissecting the complex landscape of ubiquitination regulation in cancer.
The integration of these methods is driving significant advances in understanding E3 ligase biology while creating opportunities for therapeutic intervention. As systematic characterization of E3 ligases expands the "PROTACtable" genome, future research will likely focus on developing ligands for underutilized E3s, optimizing screening methodologies for in vivo applications, and integrating multi-omics data to build comprehensive maps of ubiquitination networks across cancer types [74]. These efforts will further illuminate the complex biochemistry of the ubiquitin-proteasome system while supporting the development of novel therapeutics targeting E3 ligases in cancer and other diseases.
E3 Ligase Screening Methodology Integration: This diagram illustrates how different functional screening methods generate complementary outputs that advance cancer research applications through both primary pathways (solid arrows) and secondary contributions (dashed arrows).
Ubiquitination Cascade and Functional Outcomes: This diagram illustrates the hierarchical ubiquitination cascade with E3 ligases determining substrate specificity, and the diverse cellular outcomes determined by ubiquitin chain topology.
Overcoming Challenges in Ubiquitination Research and Therapeutic Targeting
Ubiquitination, a crucial post-translational modification, regulates virtually all cellular processes in eukaryotic cells, with particular significance in cancer biology. This enzymatic process involves the covalent attachment of ubiquitin molecules to target proteins, ultimately directing them for proteasomal degradation or altering their function, localization, and activity [44] [76]. The ubiquitin-proteasome system (UPS) employs a cascade of enzymes: ubiquitin-activating (E1), ubiquitin-conjugating (E2), and ubiquitin-ligating (E3) enzymes, which work in concert to tag substrate proteins with ubiquitin [77] [78]. The human genome encodes approximately 600 E3 ligases that provide substrate specificity, while deubiquitinating enzymes (DUBs) reverse this process by removing ubiquitin moieties [76] [78].
Despite its fundamental importance, the comprehensive analysis of ubiquitination faces two major technical challenges: its characteristically low stoichiometry, where only a small fraction of any given substrate is ubiquitinated at any time, and its highly dynamic nature, with rapid conjugation and removal cycles [44] [79]. These characteristics make capturing and quantifying ubiquitination events particularly challenging for researchers studying cancer pathways, where precise understanding of ubiquitination dynamics could reveal novel therapeutic targets. This guide objectively compares current methodologies addressing these limitations, providing experimental frameworks for advancing ubiquitination research in cancer biology.
Technical Challenges in Ubiquitination Research
The Stoichiometry Problem
The low stoichiometry of ubiquitinated proteins presents a significant detection challenge in research settings. In most cases, only a minimal percentage of a specific substrate protein undergoes ubiquitination simultaneously, creating a signal-to-noise ratio problem where the modified species is dwarfed by its unmodified counterpart [44]. This stoichiometric limitation stems from several biological realities, including the transient nature of signaling ubiquitination, efficient deubiquitination by DUBs, and rapid proteasomal degradation of tagged proteins [79].
Protein-level dosage compensation mechanisms further complicate stoichiometric analysis, particularly for subunits of multiprotein complexes. Cells maintain precise subunit ratios through accelerated degradation of unassembled proteins, with approximately 10-25% of the yeast genome and 57% of human genes encoding complex subunits subject to this compensation mechanism [79]. This regulated degradation ensures proper complex assembly but results in inherently low detection levels for researchers studying these pathways.
The Dynamic Regulation Challenge
Ubiquitination represents a rapidly reversible modification, with constant equilibrium between conjugation by E1-E2-E3 enzyme cascades and removal by DUBs [77] [80]. This dynamic balance creates a transient modification window that researchers must capture to obtain accurate snapshots of cellular ubiquitination states.
The dynamic nature of ubiquitination is exemplified by regulatory mechanisms such as the DA2-UBP12/UBP13 axis in plants, where an E3 ligase (DA2) undergoes continuous auto-ubiquitination that is counteracted by deubiquitinating enzymes (UBP12 and UBP13) [80]. This constant cycling regulates DA2's enzymatic activity toward its substrate DA1 without affecting DA2 stability, demonstrating a non-proteolytic function for K48-linked polyubiquitination [80]. While this example comes from plant studies, similar regulatory mechanisms exist in mammalian systems, creating challenges for consistent experimental detection.
Comparative Analysis of Methodologies for Overcoming Technical Limitations
Table 1: Comparison of Enrichment Strategies for Low-Stoichiometry Ubiquitinated Proteins
| Methodology | Principle | Advantages | Limitations | Typical Yield |
|---|---|---|---|---|
| His-Tag Purification (denaturing conditions) | Polyhistidine-tagged ubiquitin expression; purification under denaturing conditions | Minimal protein-protein interactions; reduced background [44] | Requires genetic manipulation; challenging in mammalian cells with native His-rich proteins [44] | 1,075 proteins identified in yeast [44] |
| Tandem Affinity Purification | Sequential purification using His-biotin or other dual tags | Enhanced specificity; reduced contaminants [44] | More complex procedure; potential yield loss [44] | 258 proteins identified in yeast [44] |
| Antibody-based Affinity (native) | Immunoprecipitation using ubiquitin antibodies under native conditions | Applicable to unengineered systems; preserves complexes [44] | High background from associated proteins; may not directly bind ubiquitin [44] | 670 proteins identified [44] |
| Antibody-based Affinity (denaturing) | Immunoprecipitation with ubiquitin antibodies under denaturing conditions | Reduces non-specific binding; more specific for ubiquitinated proteins [44] | May disrupt some ubiquitin-protein interactions [44] | 345 proteins identified [44] |
| Ubiquitin-Binding Domains | Utilization of natural UBDs (e.g., Rpn10) for affinity capture | High affinity for ubiquitin; native recognition [44] | Limited availability; may prefer specific chain types [44] | 127 proteins identified [44] |
Table 2: Approaches for Capturing Dynamic Ubiquitination Events
| Methodology | Application | Mechanism of Action | Considerations |
|---|---|---|---|
| Proteasomal Inhibition (MG132) | Accumulation of polyubiquitinated proteins | Blocks proteasomal degradation, allowing ubiquitinated protein buildup [79] [77] | May disrupt cellular homeostasis; non-specific effects [79] |
| DUB Inhibition | Stabilization of ubiquitin signals | Prevents deubiquitination, extending modification half-life [76] | Limited specificity; can affect multiple pathways [76] |
| Crosslinking Strategies | Snapshots of transient interactions | Covalently stabilizes enzyme-substrate relationships [44] | May introduce artifacts; optimization required [44] |
| Kinetic Pulse-Chase Analysis | Monitoring ubiquitination dynamics | Temporal tracking of ubiquitination and degradation rates [77] | Technically challenging; requires specialized labeling [77] |
Experimental Protocols for Key Methodologies
Protocol 1: Tandem Affinity Purification of Ubiquitinated Proteins
This protocol adapts methodologies from Tagwerker et al. [44] for comprehensive isolation of ubiquitinated proteins with minimal contamination.
Cell Preparation and Lysis:
- Express His₆-biotin-tagged ubiquitin in your target system
- Harvest cells and lyse in denaturing buffer (6 M guanidine-HCl, 100 mM Na₂HPO₄/NaH₂PO₄, 10 mM Tris-HCl, pH 8.0)
- Include protease inhibitors (e.g., 10 μM MG132) and DUB inhibitors (e.g., 1 mM N-ethylmaleimide) to preserve ubiquitin conjugates
- Sonicate to reduce viscosity and clarify by centrifugation at 16,000 × g for 15 minutes
Two-Step Purification:
- Nickel Affinity Chromatography:
- Incubate lysate with Ni²⁺-NTA agarose for 2-4 hours at room temperature
- Wash sequentially with:
- Buffer A: 8 M urea, 100 mM Na₂HPO₄/NaH₂PO₄, 10 mM Tris-HCl, pH 8.0
- Buffer B: 8 M urea, 100 mM Na₂HPO₄/NaH₂PO₄, 10 mM Tris-HCl, pH 6.3
- Elute with buffer containing 250 mM imidazole
- Streptavidin Affinity Capture:
- Dilute eluate to reduce imidazole concentration
- Incubate with streptavidin-coated beads for 2 hours
- Wash with PBS containing 0.1% Triton X-100
- Elute with SDS-PAGE sample buffer or biotin-containing solutions
Validation:
- Analyze by Western blotting with anti-ubiquitin antibodies
- Confirm specificity using negative controls (wild-type ubiquitin expression)
- Identify ubiquitination sites by mass spectrometry
Protocol 2: Ubiquitination Site Mapping by Mass Spectrometry
Based on Peng et al. [44], this protocol enables identification of specific lysine residues modified by ubiquitin.
Sample Preparation:
- Enrich ubiquitinated proteins using preferred method
- Separate proteins by SDS-PAGE and excise gel bands
- Reduce with dithiothreitol (10 mM, 30 minutes, 56°C) and alkylate with iodoacetamide (55 mM, 20 minutes, room temperature in darkness)
- Digest with trypsin (1:20-1:50 enzyme-to-substrate ratio, 37°C, 12-16 hours)
Mass Spectrometry Analysis:
- Desalt and concentrate peptides using C18 StageTips
- Separate peptides by reverse-phase nano-LC (e.g., 2-40% acetonitrile gradient over 120 minutes)
- Analyze with tandem mass spectrometry (LC-MS/MS)
- For quantitative studies, use isobaric tags (TMT) following Thermo Fisher's protocols [77]
Data Processing:
- Search data against appropriate database using search engines (e.g., MaxQuant, SEQUEST)
- Include the following variable modifications:
- GlyGly remnant on lysine (+114.0429 Da) [44]
- Methionine oxidation (+15.9949 Da)
- Carbamidomethylation on cysteine (+57.0215 Da, fixed)
- Set mass tolerance at 10-20 ppm for precursor ions and 0.02-0.05 Da for fragment ions
- Validate identifications using target-decoy approach with FDR <1%
Research Reagent Solutions for Ubiquitination Studies
Table 3: Essential Research Tools for Ubiquitination Analysis
| Reagent Category | Specific Examples | Applications | Key Features |
|---|---|---|---|
| Proteasome Inhibitors | MG132, Bortezomib, Carfilzomib [79] [76] | Accumulation of polyubiquitinated proteins | Enhances detection of low-abundance ubiquitinated species [79] |
| Ubiquitin Antibodies | Anti-ubiquitin, Anti-K48-linkage, Anti-K63-linkage [77] | Western blot, Immunoprecipitation, Immunofluorescence | Specific recognition of ubiquitin or chain types [77] |
| Ubiquitin Enrichment Kits | Ubiquitin Enrichment Kit (Thermo Fisher) [77] | Isolation of polyubiquitinated proteins from lysates | High-binding affinity resin for efficient pull-down [77] |
| Activity Assays | LanthaScreen Conjugation Assay [77] | HTS of ubiquitination kinetics | Real-time monitoring of ubiquitin transfer [77] |
| DUB Inhibitors | PR-619, P22077, G5, F6 [76] | Stabilization of ubiquitination events | Various specificities for different DUB classes [76] |
| Click Chemistry Tools | Click-iT Plus Technology [77] | Pulse-chase degradation studies | Temporal analysis of protein synthesis and degradation [77] |
Visualization of Experimental Workflows
Diagram 1: Ubiquitin Enrichment and Identification Workflow
Diagram 2: Ubiquitin-Proteasome Pathway and Regulation
The methodological advancements in ubiquitination research have substantially improved our capacity to address the challenges of low stoichiometry and dynamic regulation. Current affinity enrichment strategies, particularly tandem purification under denaturing conditions, have demonstrated significant success in identifying hundreds to thousands of ubiquitination events [44]. When coupled with highly sensitive mass spectrometry techniques that detect characteristic GlyGly remnants on modified lysines, researchers can now map ubiquitination sites with increasing precision [44].
For cancer researchers, these technical advances are particularly relevant given the central role of ubiquitination in oncogenesis and tumor suppression. The development of targeted protein degradation technologies (PROTACs) exemplifies how understanding ubiquitination mechanisms can yield novel therapeutic strategies [76] [81]. Furthermore, the ability to profile ubiquitination alterations across cancer types provides opportunities for identifying biomarkers and drug targets, as demonstrated by the association between UBE2C overexpression and hepatocellular carcinoma progression [82].
Future methodological developments will likely focus on enhancing temporal resolution to better capture ubiquitination dynamics, improving linkage-specific analysis to decipher the ubiquitin code, and developing more sophisticated tools for spatial analysis of ubiquitination within cellular compartments. As these technologies mature, they will undoubtedly accelerate our understanding of ubiquitination pathways in cancer biology and facilitate the development of targeted interventions exploiting the ubiquitin-proteasome system.
Ubiquitination is a critical, reversible post-translational modification that orchestrates diverse cellular functions including proteolysis, signal transduction, and cell cycle regulation [24]. As the second most common PTM after phosphorylation, ubiquitination involves a enzymatic cascade that attaches ubiquitin molecules to target proteins, ultimately determining their stability, activity, and localization [24] [83]. The ubiquitin-proteasome system is responsible for 80-90% of cellular proteolysis, making it a fundamental regulatory mechanism [24]. In cancer research, ubiquitination has emerged as a pivotal process influencing tumor progression, metabolic reprogramming, and response to immunotherapy [24] [50]. Recent pancancer analyses reveal that ubiquitination regulatory networks effectively stratify patients into distinct risk groups with divergent survival outcomes, highlighting its clinical relevance [24]. The dynamic nature of ubiquitination poses significant technical challenges for its study, particularly regarding the efficient isolation of ubiquitinated proteins with high specificity and minimal background interference—a prerequisite for accurate mechanistic discovery and therapeutic targeting.
Comparative Analysis of Ubiquitin Enrichment Methodologies
Antibody-Based DiGly Enrichment Approaches
The most widely adopted strategy for ubiquitinome analysis leverages antibodies specific to the diglycine (diGly) remnant left on trypsinized peptides following ubiquitination [84]. This approach has enabled large-scale ubiquitination studies, though traditional implementations using data-dependent acquisition (DDA) mass spectrometry have limitations in sensitivity and quantitative accuracy [84]. Recent optimization efforts have significantly enhanced this method through several key improvements. Data-independent acquisition (DIA) mass spectrometry has demonstrated superior performance compared to DDA, identifying approximately 35,000 diGly peptides in single measurements—nearly double the identification rate of DDA methods [84]. This approach also improves quantitative accuracy, with 45% of diGly peptides showing coefficients of variation (CVs) below 20% across replicates compared to only 15% with DDA [84]. Strategic fractionation management, particularly separating highly abundant K48-linked ubiquitin-chain derived diGly peptides, reduces competition during antibody enrichment and improves detection of co-eluting peptides [84]. Additionally, parameter optimization for diGly precursors, which often generate longer peptides with higher charge states, increases identification rates by 6-13% [84].
Table 1: Performance Comparison of DiGly Enrichment Methods
| Method Parameter | Traditional DDA Approach | Optimized DIA Approach | Improvement |
|---|---|---|---|
| DiGly Peptides Identified | ~20,000 | ~35,000 | +75% |
| Quantitative Precision (CV <20%) | 15% | 45% | 3-fold |
| Sample Input Requirement | High (multiple mg) | Moderate (1 mg) | Reduced |
| Antibody Consumption | Full vial | 1/8 vial (31.25 μg) | 8-fold reduction |
| Data Completeness | Moderate | High | Significant |
Combined Affinity Purification with Proximity Labeling
A innovative approach termed Affinity Purification coupled with Proximity Labeling-Mass Spectrometry (APPLE-MS) addresses fundamental limitations in traditional affinity purification methods [85]. This method integrates the high specificity of Twin-Strep tag enrichment with PafA-mediated proximity labeling to capture weak, transient, and membrane-associated interactions that often evade conventional techniques [85]. APPLE-MS demonstrates a 4.07-fold improvement in specificity over standard AP-MS, particularly enhancing the detection of membrane protein interactions in native contexts [85]. The methodology has proven valuable for mapping dynamic interactomes, such as the mitochondrial interactome of SARS-CoV-2 ORF9B during antiviral responses and endogenous PIN1 interactomes with minimal tag interference [85]. This approach enables in situ mapping of membrane receptor complexes like GLP-1R, demonstrating unique capabilities for studying membrane protein-protein interactions that are particularly challenging with conventional methods [85].
Table 2: Comparison of Ubiquitin Enrichment and Detection Strategies
| Enrichment Strategy | Mechanism | Advantages | Limitations | Best Applications |
|---|---|---|---|---|
| Anti-diGly Antibody (DDA) | Immunoaffinity enrichment of tryptic peptides with Gly-Gly remnant | Well-established; commercial kits available | Moderate sensitivity; limited dynamic range; high input requirements | Discovery studies with abundant sample |
| Anti-diGly Antibody (DIA) | Immunoaffinity with optimized DIA MS acquisition | High sensitivity (35,000 IDs); excellent reproducibility | Requires spectral libraries; method development needed | Large cohort studies; quantitative precision |
| APPLE-MS | Combines affinity purification with proximity labeling | Captures weak/transient interactions; excellent for membrane proteins | More complex workflow; requires genetic manipulation | Membrane interactomes; dynamic complexes |
| Label-free MS with Antibody Enrichment | Antibody enrichment without isotopic labeling | No labeling cost; high throughput; wide dynamic range | Limited to abundant ubiquitination events | Targeted studies; verification experiments |
Experimental Protocols for High-Specificity Ubiquitinome Analysis
Optimized DiGly Enrichment with DIA Mass Spectrometry
Sample Preparation:
- Extract proteins from cells or tissues of interest, with proteasome inhibitor treatment (e.g., 10 μM MG132 for 4 hours) recommended to enhance ubiquitinated protein detection [84].
- Digest proteins using trypsin or LysC to generate peptides with diGly remnants [83] [84].
- Quantify peptide concentration using BCA or similar assays [86].
diGly Peptide Enrichment:
- Use 1 mg of peptide material and 31.25 μg of anti-diGly antibody for enrichment [84].
- Employ optimized binding conditions with rotation for 1-2 hours at 4°C [84].
- Wash beads thoroughly to remove non-specifically bound peptides [84].
- Elute diGly peptides using acid elution (0.1-0.5% TFA) [84].
Liquid Chromatography and Mass Spectrometry:
- Analyze only 25% of the total enriched material to maintain sensitivity [84].
- Utilize micro-flow LC systems (≤50 μL/min) for improved robustness compared to nano-flow systems [87].
- Implement DIA method with 46 precursor isolation windows and MS2 resolution of 30,000 [84].
- Employ short chromatographic gradients coupled with high-sensitivity mass spectrometers for optimal throughput [87].
Data Analysis:
- Use comprehensive spectral libraries containing >90,000 diGly peptides for optimal identification [84].
- Process data with artificial intelligence and machine learning-based algorithms for enhanced analysis efficiency [87].
- Verify results using orthogonal methods such as Western blot or immunoprecipitation [83].
APPLE-MS for Membrane and Transient Interactions
Experimental Workflow:
- Express protein of interest with Twin-Strep tag in relevant cell system [85].
- Perform PafA-mediated proximity labeling to biotinylate nearby interacting proteins [85].
- Lyse cells and perform Twin-Strep tag affinity purification under native conditions [85].
- Capture biotinylated proteins using streptavidin beads [85].
- Digest enriched proteins and analyze by tandem mass spectrometry [85].
- Process data using specialized computational pipelines to distinguish specific interactions from background [85].
Visualization of Optimized Experimental Workflows
High-Specificity DiGly Enrichment Workflow
APPLE-MS Integrated Workflow
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Research Reagents for Optimized Ubiquitin Enrichment
| Reagent / Tool | Function | Specific Application Notes |
|---|---|---|
| Anti-diGly Antibody | Immunoaffinity enrichment of ubiquitinated peptides | Use 31.25 μg per 1 mg peptide input; commercial sources available [84] |
| Proteasome Inhibitors (MG132) | Enhances detection by blocking degradation | 10 μM for 4 hours pretreatment significantly increases ubiquitinated protein yield [84] |
| Twin-Strep Tag System | High-affinity purification tag | Provides superior specificity in APPLE-MS workflow [85] |
| PafA Enzyme | Proximity labeling | Biotinylates proteins in immediate vicinity of target in APPLE-MS [85] |
| Micro-flow LC Systems | Chromatographic separation | ≤50 μL/min flow rates improve robustness vs. nano-flow systems [87] |
| DIA-Optimized Mass Spectrometers | High-sensitivity detection | Instruments with fast scanning speeds (e.g., timsTOF Pro) enable short gradients [87] [84] |
| Spectral Libraries | DIA data interpretation | Comprehensive libraries (>90,000 diGly peptides) dramatically improve identification [84] |
Concluding Remarks
The field of ubiquitin enrichment has evolved significantly from basic antibody-based approaches to sophisticated integrated methodologies that dramatically reduce background and enhance specificity. The optimization of diGly antibody enrichment with DIA mass spectrometry represents a substantial advancement, delivering approximately 35,000 diGly peptide identifications in single measurements with excellent quantitative precision [84]. For challenging targets such as membrane proteins and transient interactions, the APPLE-MS method combining affinity purification with proximity labeling offers a powerful alternative with 4.07-fold improvement in specificity over conventional approaches [85]. These technical advances coincide with growing recognition of ubiquitination's crucial role in cancer biology, where ubiquitination signatures can stratify patient risk and predict immunotherapy response [24]. The continued refinement of these methodologies will undoubtedly accelerate our understanding of the ubiquitin code in cancer and beyond, potentially revealing novel therapeutic targets for intervention in ubiquitination-driven pathologies.
Ubiquitination is a critical post-translational modification that extends far beyond simple protein degradation, acting as a versatile cellular signaling mechanism that regulates virtually all cellular processes, including cell cycle progression, DNA repair, and immune responses [88] [89]. The complexity of ubiquitin signaling originates from the ability of ubiquitin molecules to form polymers (polyubiquitin chains) through eight distinct linkage types (Lys6, Lys11, Lys27, Lys29, Lys33, Lys48, Lys63, and Met1), creating a "ubiquitin code" that determines the fate of modified proteins [88] [90]. The higher-order architecture of these chains—including their specific linkage types, length, and branching patterns—forms a complex language that cells utilize to coordinate intricate biological processes [90].
In cancer research, decoding this ubiquitin code has become increasingly important, as dysregulated ubiquitination is strongly implicated in tumorigenesis across cancer types [24] [38]. Recent pancancer analyses have revealed that ubiquitination-related genes are significantly upregulated in tumor tissues and correlate with poor clinical outcomes [82] [38]. For instance, the ubiquitin-conjugating enzyme UBE2T demonstrates elevated expression across multiple tumor types and is associated with worsened prognosis, highlighting the clinical relevance of understanding ubiquitin signaling dynamics [38]. Similarly, the OTUB1-TRIM28 ubiquitination axis has been identified as a key modulator of the MYC pathway, influencing patient prognosis and immunotherapy response [24]. This article provides a comparative analysis of the experimental methodologies essential for deciphering the complex ubiquitin code, with particular emphasis on their applications in cancer research.
Methodological Comparison for Ubiquitin Chain Analysis
Table 1: Comparison of Key Ubiquitin Chain Analysis Methods
| Method | Key Applications | Linkage Coverage | Chain Architecture Insight | Throughput | Key Limitations | Typical Sample Input |
|---|---|---|---|---|---|---|
| UbiCRest [88] | Linkage type identification, basic architecture assessment | All 8 linkage types (with specific DUBs) | Qualitative (homotypic vs. heterotypic) | Medium (parallel reactions) | Qualitative only; may miss complex mixtures | Western blot quantities of endogenous protein |
| Ub-AQUA/PRM [90] | Absolute quantification of linkage stoichiometry | All 8 linkage types simultaneously | Limited (identifies branched chains) | High | Requires specialized MS expertise and equipment | Complex cell or tissue lysates |
| Linkage-Specific Antibodies [88] [90] | Detection of specific, common linkages (K48, K63, K11, M1) | Limited (typically 4 linkages) | No direct information | Medium-High | Limited linkage coverage; potential cross-reactivity | Various, depending on application |
| Ub-ProT [90] | Ubiquitin chain length measurement | Not primary purpose | Infers length distribution | Medium | Does not identify linkage types; requires substrate-specific isolation | Immunopurified substrate |
UbiCRest: Deubiquitinase-Based Linkage Mapping
The UbiCRest (Ubiquitin Chain Restriction) method employs a panel of linkage-specific deubiquitinating enzymes (DUBs) to qualitatively assess ubiquitin chain linkage types and architecture through parallel enzymatic reactions followed by gel-based analysis [88].
Experimental Protocol:
- Sample Preparation: Prepare ubiquitinated substrates, which can be immunopurified proteins, in vitro ubiquitination reactions, or purified ubiquitin chains. The method works with Western blotting quantities of endogenously ubiquitinated proteins [88].
- DUB Panel Setup: Set up parallel digestion reactions containing the substrate and individual, linkage-specific DUBs. A typical panel includes DUBs such as:
- OTUB1: Highly specific for Lys48-linked chains (working concentration: 1-20 µM) [88].
- OTUD1: Specific for Lys63-linked chains (0.1-2 µM) [88].
- Cezanne: Preferentially cleaves Lys11-linked chains (0.1-2 µM) [88].
- OTUD3: Cleaves Lys6 and Lys11 linkages (1-20 µM) [88].
- OTUD2: Cleaves Lys27 linkages (also cleaves Lys11, Lys29, Lys33; 1-20 µM) [88].
- TRABID: Cleaves Lys29 and Lys33 linkages (0.5-10 µM) [88].
- USP21 or USP2: Broad-specificity positive controls that cleave all linkages (1-5 µM for USP21) [88].
- Digestion and Analysis: Incubate reactions at 37°C for 1-2 hours. Stop reactions with SDS loading buffer, resolve proteins by SDS-PAGE, and analyze by Western blotting using ubiquitin- or substrate-specific antibodies [88].
- Data Interpretation: The cleavage pattern reveals linkage composition. Complete digestion by a linkage-specific DUB indicates the presence of that linkage type. Sequential digestion strategies can probe heterotypic chain architecture [88].
Cancer Research Application: UbiCRest is ideal for initial characterization of ubiquitin linkages on cancer-relevant proteins. For example, it could be used to identify the specific chain types attached to tumor suppressors like p53 or oncoproteins like MYC, providing mechanistic insight into their regulation [24] [89].
Ub-AQUA/PRM: Mass Spectrometry-Based Absolute Quantification
Ubiquitin-Absolute Quantification with Parallel Reaction Monitoring (Ub-AQUA/PRM) is a targeted mass spectrometry approach for direct and highly sensitive measurement of the stoichiometry of all eight ubiquitin linkage types simultaneously [90].
Experimental Protocol:
- Sample Preparation and Digestion: Lyse cells or tissues under denaturing conditions to preserve ubiquitin modifications and inactivate endogenous DUBs. Digest proteins with trypsin, which cleaves ubiquitin after arginine 74, generating signature di-glycine (Gly-Gly) remnant peptides for each ubiquitin linkage type [90].
- AQUA Peptide Spike-In: Add known quantities of synthetic, isotopically labeled AQUA peptides corresponding to the tryptic signature peptides for all eight ubiquitin linkages as internal standards [90].
- LC-MS/MS Analysis with PRM: Analyze the peptide mixture using liquid chromatography coupled to a high-resolution mass spectrometer (e.g., Q Exactive) operating in PRM mode. The PRM method is configured to specifically target the signature peptides and their AQUA counterparts [90].
- Data Analysis and Quantification: Extract the MS2 fragment ion chromatograms for both endogenous and AQUA peptides. The ratio of their peak areas allows for absolute quantification of the amount of each ubiquitin linkage type present in the original sample [90]. The method can also be adapted to quantify branched ubiquitin chains, such as K48/K63 branched chains [90].
Cancer Research Application: Ub-AQUA/PRM is powerful for pancancer studies comparing global ubiquitin chain linkage profiles between normal and tumor tissues, or between different cancer subtypes. This can reveal cancer-specific ubiquitination signatures, as suggested by studies showing upregulation of specific ubiquitination pathways in squamous cell carcinomas and adenocarcinomas [24].
Ub-ProT: Measuring Ubiquitin Chain Length
The Ubiquitin Chain Protection from Trypsinization (Ub-ProT) method determines the average length of ubiquitin chains attached to a specific substrate, which is critical as chain length can directly influence downstream outcomes like proteasomal targeting [90].
Experimental Protocol:
- Substrate Immunopurification: Isolate the ubiquitinated protein of interest from cell lysates or in vitro reactions using immunoprecipitation with a substrate-specific antibody under denaturing conditions [90].
- Chain Protector Incubation: Incubate the isolated ubiquitinated substrate with a "chain protector," such as a recombinant ubiquitin-associated (UBA) domain that binds tightly to ubiquitin chains and protects a defined region from subsequent protease digestion [90].
- Limited Trypsin Digestion: Treat the complex with a low concentration of trypsin for a limited time. Trypsin cleaves ubiquitin at arginine 74, but only in the unprotected regions of the chain [90].
- Western Blot Analysis: Resolve the digested products by SDS-PAGE and probe with an antibody that recognizes the N-terminal region of ubiquitin protected by the UBA domain. The resulting ladder of bands corresponds to ubiquitin chains of different lengths, allowing estimation of the average chain length on the substrate [90].
Cancer Research Application: Ub-ProT can be used to investigate how chain length on key regulatory proteins (e.g., cell cycle regulators) is altered in cancer, potentially revealing mechanisms of drug resistance or oncogenic activation.
Visualizing Ubiquitin Signaling and Analysis Workflows
UbiCRest Experimental Workflow
Diagram 1: UbiCRest workflow uses linkage-specific DUBs to analyze ubiquitin chains.
Ubiquitin Chain Signaling in Cancer Pathways
Diagram 2: The ubiquitination cascade is dysregulated in cancer, affecting key substrates.
The Scientist's Toolkit: Essential Research Reagents
Table 2: Key Reagents for Ubiquitination Analysis
| Reagent / Tool | Category | Primary Function | Example Application | Specific Example (from search results) |
|---|---|---|---|---|
| Linkage-Specific DUBs | Enzyme | Cleaves specific ubiquitin linkages to determine chain type. | UbiCRest assay [88] | OTUB1 (K48-specific), Cezanne (K11-specific) [88] |
| AQUA Peptides | Synthetic Standard | Isotopically labeled internal standards for absolute quantification by MS. | Ub-AQUA/PRM [90] | Synthetic peptides with Gly-Gly remnant for each linkage type [90] |
| Linkage-Specific Antibodies | Antibody | Detects and immunoprecipitates specific ubiquitin chain types. | Immunoblotting, Immunofluorescence [88] [90] | Antibodies for K48, K63, K11, M1 linkages [90] |
| Ubiquitin Mutants (K-to-R) | Genetic Tool | Identifies linkage requirements in vivo by blocking specific chain formation. | Cell-based functional assays [88] | Ubiquitin mutant where all lysines except one are mutated to arginine [88] |
| Chain Binders (UBA Domains) | Protein Domain | Binds and protects ubiquitin chains from proteolysis. | Ub-ProT chain length analysis [90] | Recombinant UBA domain used as a "chain protector" [90] |
| Proteasome Inhibitors | Small Molecule | Blocks proteasomal degradation, enriching for ubiquitinated proteins. | Sample preparation for ubiquitinomics. | MG132, Bortezomib (not explicitly in results, but standard practice) |
| DUB Inhibitors | Small Molecule | Inhibits deubiquitinating enzymes, preserves ubiquitin signals. | Stabilizing ubiquitination in cell assays. | PR-619, WP1130 (not explicitly in results, but standard practice) |
Deciphering the ubiquitin code requires a multifaceted methodological approach. While UbiCRest offers an accessible, qualitative entry point for linkage analysis, Ub-AQUA/PRM provides powerful quantitative depth, and Ub-ProT addresses the critical dimension of chain length. The choice of method depends on the specific research question, available resources, and required throughput. In cancer biology, integrating these techniques is proving essential for understanding how dysregulated ubiquitination drives tumor progression and influences immunotherapy response. For instance, correlating Ub-AQUA/PRM-derived linkage profiles with patient survival data can validate prognostic ubiquitination signatures, while UbiCRest can mechanistically dissect the regulation of specific oncoproteins and tumor suppressors [24] [38]. As these tools continue to evolve, they will undoubtedly uncover novel therapeutic vulnerabilities in the ubiquitin system, paving the way for new cancer treatments.
Overcoming Therapeutic Resistance to Proteasome Inhibitors in Hematological and Solid Tumors
The ubiquitin-proteasome system (UPS) serves as a critical regulatory hub for intracellular protein degradation, maintaining cellular homeostasis by eliminating damaged, misfolded, and short-lived regulatory proteins [91]. In eukaryotic cells, the UPS involves a sophisticated enzymatic cascade where target proteins are marked for degradation through ubiquitination—a process involving E1 (activating), E2 (conjugating), and E3 (ligase) enzymes that attach ubiquitin chains to substrate proteins [91]. These ubiquitinated proteins are then recognized and degraded by the 26S proteasome, a multi-subunit complex comprising a 20S catalytic core particle and 19S regulatory caps [91] [92]. The proteasome possesses three primary catalytic activities: chymotrypsin-like (β5 subunit), trypsin-like (β2 subunit), and caspase-like (β1 subunit), with the chymotrypsin-like activity being the primary pharmacological target [93] [92].
Given the heightened dependency of many cancer cells on proteasome function for survival, particularly in hematological malignancies characterized by excessive protein production, proteasome inhibitors (PIs) have emerged as transformative therapeutics [94]. Bortezomib, the first-in-class PI, demonstrated remarkable efficacy in multiple myeloma and mantle cell lymphoma, establishing the proteasome as a valid therapeutic target in oncology [95] [96]. Subsequent generations of PIs, including carfilzomib and ixazomib, have further expanded the treatment arsenal [94]. However, the emergence of intrinsic and acquired resistance to these agents represents a significant clinical challenge that limits their long-term efficacy [93] [92]. This review provides a comprehensive comparative analysis of resistance mechanisms to proteasome inhibitors across cancer types and outlines experimental approaches for investigating and overcoming these resistance pathways.
Proteasome Inhibitors: Mechanisms and Clinical Applications
Approved Proteasome Inhibitors
Table 1: Characteristics of FDA-Approved Proteasome Inhibitors
| Inhibitor | Chemical Class | Target Subunits | Binding Mechanism | Primary Indications | Key Resistance Factors |
|---|---|---|---|---|---|
| Bortezomib | Peptide boronate | β5 (primarily), β1 | Reversible | Multiple myeloma, Mantle cell lymphoma | PSMB5 mutations, upregulated subunits, efflux pumps |
| Carfilzomib | Epoxyketone | β5, β5i (LMP7) | Irreversible | Relapsed/refractory multiple myeloma | PSMB5 mutations, immunoproteasome upregulation |
| Ixazomib | Peptide boronate | β5 | Reversible (oral) | Relapsed/refractory multiple myeloma | Multidrug resistance mechanisms |
Bortezomib, a peptide boronate, reversibly inhibits the chymotrypsin-like activity of the β5 subunit with an IC50 of 7.9 nM, while also affecting the caspase-like activity of the β1 subunit (IC50 = 53 nM) [92]. Its mechanism of action involves accumulation of polyubiquitinated proteins, leading to endoplasmic reticulum (ER) stress, unfolded protein response (UPR) activation, and ultimately apoptosis through multiple pathways including NF-κB inhibition, JNK activation, and disruption of cell cycle regulators [95] [96].
Carfilzomib represents a second-generation epoxyketone inhibitor that irreversibly binds to the β5 subunit, demonstrating improved specificity for the chymotrypsin-like activity and a distinct toxicity profile compared to bortezomib [94]. Its irreversible binding mechanism enables sustained proteasome inhibition, potentially overcoming some resistance mechanisms associated with reversible inhibitors [92] [94].
Ixazomib, the first oral proteasome inhibitor, shares the boronate pharmacophore with bortezomib but offers improved administration convenience [94]. While all three agents primarily target the β5 subunit, their differential binding kinetics, specificity profiles, and administration routes contribute to distinct clinical efficacy and resistance patterns.
Mechanisms of Resistance to Proteasome Inhibitors
Proteasomal Subunit Alterations
Table 2: Proteasome-Specific Resistance Mechanisms
| Resistance Mechanism | Molecular Alterations | Experimental Evidence | Cancer Types Observed |
|---|---|---|---|
| PSMB5 point mutations | G322A (Ala49Thr), C323T (Ala50Val), G326T (Ala50Val) | Reduced bortezomib binding affinity; Jurkat, THP1, MM resistant cell lines | Hematological malignancies, NSCLC |
| Conjoined PSMB5 mutations | G322A + C326T | Stronger resistance than single mutations; JurkatB cells | Lymphoblastic lymphoma/leukemia |
| Regulatory subunit mutations | LMP7 (Phe50Ile) in immunoproteasome | Altered recovery of proteasome activity; HT-29 resistant clones | Colorectal adenocarcinoma |
| Proteasome subunit overexpression | Upregulation of β5, β1, β2 subunits | Increased proteasome content and activity; MM resistant cells | Multiple myeloma |
| Immunoproteasome upregulation | Increased β5i (LMP7), β1i (LMP2), β2i (MECL1) | Shift in proteasome composition; Hematopoietic cells | Hematological malignancies |
Mutations in the PSMB5 gene, which encodes the β5 proteasome subunit, represent a well-characterized resistance mechanism. The G322A mutation resulting in Ala49Thr substitution was initially identified in bortezomib-resistant Jurkat and THP1 cell lines [93]. Structural analyses reveal that Ala49 and Ala50 residues form critical contacts with bortezomib through hydrogen bonding networks, and substitutions at these positions induce conformational changes that disrupt inhibitor binding [93] [92]. Additional mutations including C323T (Ala50Val), C326T (Ala50Val), and conjoined mutations (G322A + C326T) confer progressively stronger resistance phenotypes [93].
Computational modeling of these mutant proteasomes demonstrates reduced affinity for bortezomib within the S1 specificity pocket, primarily due to altered hydrogen bonding patterns and steric hindrance [93]. The spatial localization of these mutations around the inhibitor binding pocket directly impacts drug-target interactions, with certain mutations (Thr21Ala, Ala49Thr, Ala50Val) directly involved in bortezomib binding, while others (Cys52Phe, Met45Ile) exert indirect effects through allosteric mechanisms [93].
Upregulation of proteasome subunits represents an alternative adaptation to chronic proteasome inhibition. Cancer cells can increase proteasome abundance and activity through elevated expression of standard proteasome subunits or induction of immunoproteasome subunits, effectively augmenting proteolytic capacity and restoring protein homeostasis despite inhibitor presence [92] [96]. This compensatory mechanism is particularly relevant in hematological malignancies where immunoproteasome expression is naturally higher [93] [94].
Cellular Adaptive Responses
Beyond direct proteasomal modifications, cancer cells employ diverse cellular strategies to evade PI-induced cytotoxicity. Upregulation of efflux transporters, including P-glycoprotein, enhances drug extrusion and reduces intracellular accumulation [93]. Alterations in apoptotic signaling pathways, particularly increased expression of anti-apoptotic Bcl-2 family members, elevate the threshold for cell death initiation [96]. Additionally, activation of alternative protein clearance mechanisms, such as the aggresome-autophagy pathway, provides compensatory degradation routes when proteasomal function is compromised [96].
The tumor microenvironment further contributes to resistance through stromal cell interactions that activate pro-survival signaling cascades, including NF-κB and integrin-mediated pathways [96]. In multiple myeloma, bone marrow stromal cells secrete protective cytokines and establish adhesion-mediated resistance that diminishes PI efficacy [96].
Experimental Approaches for Investigating Resistance Mechanisms
Generation of Resistant Cell Models
Protocol 1: Development of Proteasome Inhibitor-Resistant Cell Lines
- Initial Culture Conditions: Begin with parent cancer cell lines (e.g., Jurkat, MM.1S, THP1) maintained in appropriate media with 10% FBS at 37°C in 5% CO₂.
- Stepwise Selection: Expose cells to progressively increasing concentrations of proteasome inhibitor (e.g., bortezomib starting at 2-5 nM).
- Dose Escalation: Increase inhibitor concentration by 10-25% once cells demonstrate stable proliferation for at least 3 passages.
- Clone Isolation: After reaching target resistance level (typically 10-50x IC50 of parent line), isolate single-cell clones by limiting dilution.
- Characterization: Validate resistance phenotype through:
- Cell viability assays (MTT, MTS, or WST-8)
- Proteasome activity profiling (fluorogenic substrates)
- Apoptosis assessment (Annexin V/PI staining)
- Western blotting for polyubiquitinated protein accumulation
This methodology has been successfully employed to establish various resistant models, including JurkatB (bortezomib-resistant Jurkat), THP1/BTZ, and 8226/BTZ cells [93]. The resulting cell lines typically exhibit 10- to 50-fold increased IC50 values compared to their parental counterparts and provide valuable tools for resistance mechanism investigation.
Molecular Characterization Techniques
Protocol 2: Comprehensive Analysis of Proteasome Alterations
PSMB5 Gene Sequencing:
- Isolate genomic DNA and total RNA from resistant and parent cells
- Amplify PSMB5 coding region by PCR (primers spanning exons 1-9)
- Perform Sanger sequencing or next-generation sequencing of amplicons
- Confirm mutations at cDNA level by RT-PCR and sequencing
Proteasome Activity Profiling:
- Prepare cell lysates in buffer (50 mM HEPES, 5 mM EDTA, 150 mM NaCl, 1% Triton X-100)
- Incubate with fluorogenic substrates:
- Suc-LLVY-AMC for chymotrypsin-like activity (β5)
- Z-ARR-AMC for trypsin-like activity (β2)
- Z-LLE-AMC for caspase-like activity (β1)
- Measure fluorescence (380 nm excitation/460 nm emission) over 60 minutes
- Calculate activity rates and determine inhibition IC50 values
Computational Modeling of Mutant Proteasomes:
- Retrieve wild-type proteasome structure (e.g., PDB 5LF3)
- Introduce point mutations using molecular modeling software (PyMOL, Chimera)
- Dock inhibitor molecules (bortezomib, carfilzomib) into active sites
- Analyze binding interactions and calculate binding free energies
Application of these techniques has revealed that PSMB5 mutations decrease inhibitor binding affinity through structural alterations in the S1 pocket, with the magnitude of resistance correlating with the specific mutation profile [93] [92].
Diagram 1: Experimental workflow for generating and characterizing proteasome inhibitor-resistant cell models, integrating genomic, biochemical, and computational approaches.
Strategies to Overcome Resistance
Next-Generation Proteasome Inhibitors
Second-generation PIs have been designed to circumvent common resistance mechanisms. Carfilzomib, an irreversible epoxyketone inhibitor, demonstrates efficacy in bortezomib-resistant models due to its distinct binding mechanism and increased specificity [94]. Marizomib (NPI-0052), a naturally-derived β-lactone inhibitor, broadly targets all three catalytic subunits and exhibits activity against bortezomib-resistant cells [96]. The differential inhibition profiles of these agents enable strategic sequencing or combination approaches to overcome resistance.
Table 3: Strategies to Overcome PI Resistance
| Therapeutic Strategy | Mechanistic Basis | Experimental Support | Clinical Status |
|---|---|---|---|
| Irreversible inhibitors (Carfilzomib) | Covalent binding circumvents mutations | Activity in bortezomib-resistant MM models | FDA-approved |
| Pan-proteasome inhibitors (Marizomib) | Multi-subunit targeting prevents compensation | Synergy with bortezomib in resistant cells | Clinical trials |
| Immunoproteasome inhibitors (KZR-616) | Specific targeting of i20S subunits | Efficacy in hematological models | Clinical development |
| HDAC inhibitors (Panobinostat) | Dual aggresome/proteasome inhibition | Synergy in bortezomib-resistant MM | FDA-approved combination |
| HSP90 inhibitors (Tanespimycin) | Disruption of client protein stability | Enhanced ER stress in resistant cells | Clinical trials |
Rational Combination Therapies
Combination approaches targeting complementary pathways represent a promising strategy to overcome resistance. HDAC inhibitors, particularly those targeting HDAC6, disrupt aggresome formation and synergize with PIs by simultaneously blocking both major protein degradation pathways [97] [98]. Preclinical studies demonstrate that HDAC inhibitors like vorinostat and panobinostat enhance PI-induced apoptosis in resistant models through multiple mechanisms, including Hsp90 hyperacetylation, client protein destabilization, and augmented ER stress [97] [98].
Heat shock protein 90 (Hsp90) inhibitors provide another rational combination partner by disrupting the stability of oncogenic clients and enhancing proteotoxic stress [97]. The molecular chaperone Hsp90 stabilizes numerous signaling proteins essential for tumor survival, and its inhibition leads to simultaneous disruption of multiple oncogenic pathways while augmenting PI efficacy [97].
Diagram 2: Synergistic mechanisms of combination therapies targeting complementary protein degradation pathways to overcome proteasome inhibitor resistance.
The Scientist's Toolkit: Essential Research Reagents
Table 4: Key Reagents for Investigating PI Resistance Mechanisms
| Reagent Category | Specific Examples | Research Applications | Key Features |
|---|---|---|---|
| Proteasome inhibitors | Bortezomib, Carfilzomib, MG-132, Lactacystin | Resistance induction, mechanism studies | Varied specificity, reversibility |
| Fluorogenic substrates | Suc-LLVY-AMC, Z-ARR-AMC, Z-LLE-AMC | Proteasome activity profiling | Subunit-specific cleavage sites |
| Cell viability assays | MTT, MTS, WST-8, Alamar Blue | Cytotoxicity assessment | Colorimetric/fluorometric readouts |
| Apoptosis detection | Annexin V/PI, caspase activity assays | Cell death mechanism analysis | Flow cytometry compatible |
| Protein degradation markers | Anti-polyubiquitin, anti-K48/K63 ubiquitin | Proteostasis disruption assessment | Modification-specific antibodies |
| Proteasome subunits antibodies | Anti-PSMB5, anti-β5, anti-LMP7 | Expression and mutation analysis | Wild-type vs mutant specific |
| HDAC inhibitors | Vorinostat, Panobinostat, Trichostatin A | Combination therapy studies | Class-specific inhibition |
| HSP90 inhibitors | Tanespimycin, Ganetespib | Chaperone function disruption | Client protein degradation |
These research tools enable comprehensive investigation of PI resistance mechanisms, from initial phenotypic characterization to molecular pathway analysis. The selection of appropriate reagents should be guided by specific research questions, whether focused on proteasomal adaptations, alternative degradation pathways, or cell survival mechanisms.
The landscape of proteasome inhibitor resistance reveals remarkable complexity, encompassing proteasomal mutations, compensatory cellular adaptations, and microenvironmental factors. Comparative analysis across cancer types demonstrates both shared and unique resistance mechanisms, with hematological malignancies predominantly exhibiting proteasomal subunit alterations while solid tumors more frequently employ alternative survival pathway activation.
Future directions should focus on personalized resistance profiling to guide therapeutic sequencing, development of mutant-selective next-generation inhibitors, and rational polytherapy approaches targeting complementary vulnerabilities. The integration of proteasome inhibition with emerging modalities including immunotherapies and targeted protein degraders (PROTACs) represents a promising frontier for overcoming resistance. Furthermore, advanced biomarker development for early resistance detection and mechanism identification will be essential for optimizing PI utilization across the cancer spectrum.
As our understanding of the intricate feedback networks governing proteostasis in cancer deepens, so too will our capacity to devise innovative strategies that restore sensitivity and extend the clinical benefit of proteasome-directed therapeutics. The continued elucidation of resistance mechanisms through integrated genomic, structural, and functional approaches will provide the foundation for next-generation therapeutic paradigms in oncology.
Strategic Development of E3 Ligase-Targeted Therapies and PROTAC Platforms
The ubiquitin-proteasome system (UPS) represents a sophisticated regulatory mechanism for intracellular protein homeostasis, with E3 ubiquitin ligases serving as the pivotal determinants of substrate specificity. These enzymes facilitate the transfer of ubiquitin from E2 conjugating enzymes to specific target proteins, marking them for proteasomal degradation [3] [99]. With over 600 E3 ligases encoded in the human genome, this protein family offers a vast yet underexplored therapeutic landscape [100] [74]. The strategic importance of E3 ligases in cancer therapeutics stems from their regulatory roles across all recognized cancer hallmarks, including sustained proliferation, evasion of apoptosis, and immune evasion [3]. As the key arbiters of protein stability for critical regulators of cell division, DNA repair, and apoptotic pathways, E3 ligases can function as either tumor promoters or suppressors depending on their specific substrates and cellular context [3] [101].
The emergence of targeted protein degradation (TPD) technologies, particularly proteolysis-targeting chimeras (PROTACs), has transformed drug discovery by leveraging endogenous E3 ligases to eliminate disease-causing proteins [102] [99]. This approach represents a paradigm shift from traditional inhibition to complete protein removal, offering potential solutions for targeting previously "undruggable" proteins and addressing drug resistance mechanisms [99] [103]. The therapeutic application of E3 ligases is now rapidly advancing, with multiple PROTAC candidates entering clinical trials and showcasing the immense potential of harnessing the ubiquitin-proteasome system for cancer therapy [104] [100].
E3 Ligase Classification and Mechanistic Diversity
E3 ubiquitin ligases are categorized into three major families based on their structural features and catalytic mechanisms: RING finger family, HECT family, and RBR family [3]. Understanding these classifications provides the foundation for rational degrader design.
The RING finger family constitutes the largest E3 group, characterized by cysteine-rich domains that coordinate zinc ions and mediate direct ubiquitin transfer from E2 enzymes to substrates [3]. This family includes both single-subunit E3s (such as MDM2 and cIAP) and multi-subunit complexes. The Cullin-RING ligases (CRLs) represent particularly important multi-subunit complexes, with the Cullin protein serving as a scaffold that bridges substrate recognition modules and RING-box proteins [3]. The Anaphase Promoting Complex/Cyclosome (APC/C), another critical multi-subunit RING E3, plays essential roles in cell cycle progression by targeting key regulators for degradation [3].
The HECT family employs a distinct catalytic mechanism involving a conserved cysteine residue that forms a thioester intermediate with ubiquitin before transferring it to substrates [3]. This two-step transfer mechanism differentiates HECT ligases from RING types and may influence the processivity and chain topology of ubiquitination.
The RBR family represents a hybrid category that combines features of both RING and HECT mechanisms, utilizing a RING1 domain to bind E2~Ub and a RING2 domain with catalytic cysteine for ubiquitin transfer [101].
Table 1: Major E3 Ubiquitin Ligase Families and Characteristics
| E3 Family | Catalytic Mechanism | Representative Members | Key Structural Features |
|---|---|---|---|
| RING Finger | Direct transfer from E2 to substrate | MDM2, cIAP, CRBN, VHL, SCF complex | Zinc-binding RING domain, often functions as multi-subunit complexes |
| HECT Family | Two-step transfer via thioester intermediate | NEDD4, HACE1, HECTD1 | Conserved C-terminal HECT domain with catalytic cysteine |
| RBR Family | Hybrid RING-HECT mechanism | HOIP, HOIL-1, TRIAD1 | RING1 domain for E2 binding, RING2 domain with catalytic cysteine |
PROTAC Technology: Mechanism and Clinical Advancement
PROTACs represent a groundbreaking class of heterobifunctional molecules that co-opt the ubiquitin-proteasome system to achieve targeted protein degradation. These molecules consist of three essential components: a target protein-binding ligand, an E3 ligase-recruiting ligand, and a chemical linker connecting these two moieties [100] [105] [99]. The molecular mechanism involves the simultaneous engagement of both target protein and E3 ligase, forming a productive ternary complex that enables ubiquitin transfer to the target protein, marking it for proteasomal degradation [102] [99].
A defining advantage of the PROTAC platform is its catalytic mode of action, wherein a single degrader molecule can facilitate the destruction of multiple target protein molecules, enabling sustained pharmacological effects at sub-stoichiometric concentrations [99]. This technology has demonstrated particular utility against recalcitrant targets including transcription factors, scaffolding proteins, and non-enzymatic regulators that have eluded conventional inhibition strategies [102] [103].
The clinical translation of PROTAC technology has progressed rapidly, with over 40 PROTAC candidates currently in clinical trials as of 2025 [104] [105]. These investigational degraders target diverse proteins implicated in oncology, including androgen receptor (AR), estrogen receptor (ER), Bruton's tyrosine kinase (BTK), and interleukin-1 receptor-associated kinase 4 (IRAK4) [104].
Table 2: Selected PROTAC Degraders in Advanced Clinical Development
| Drug Candidate | Target | E3 Ligase | Indication | Development Status |
|---|---|---|---|---|
| Vepdegestran (ARV-471) | Estrogen Receptor (ER) | CRBN | ER+/HER2- Breast Cancer | Phase III |
| BMS-986365 (CC-94676) | Androgen Receptor (AR) | CRBN | Metastatic Castration-Resistant Prostate Cancer | Phase III |
| BGB-16673 | BTK | CRBN | R/R B-cell Malignancies | Phase III |
| ARV-110 | Androgen Receptor (AR) | CRBN | Metastatic Castration-Resistant Prostate Cancer | Phase II |
| KT-474 (SAR444656) | IRAK4 | CRBN | Hidradenitis Suppurativa and Atopic Dermatitis | Phase II |
Recent clinical readouts have demonstrated both promise and challenges for PROTAC therapeutics. Vepdegestran (ARV-471) met its primary endpoint in patients with ESR1 mutations in the Phase III VERITAC-2 trial, showing statistically significant improvement in progression-free survival compared to fulvestrant, though it did not reach significance in the overall intent-to-treat population [104]. This mixed outcome underscores the importance of patient stratification strategies in degrader development.
Comparative Analysis of E3 Ligase Platforms in TPD
Established E3 Ligase Platforms
Current PROTAC development heavily relies on a narrow set of E3 ligases, with CRBN and VHL dominating clinical-stage candidates [100] [74]. Each platform offers distinct advantages and limitations:
The CRBN platform utilizes immunomodulatory imide drug (IMiD) derivatives such as thalidomide, lenalidomide, and pomalidomide as E3-recruiting ligands [100] [99]. These compounds demonstrate favorable pharmacological properties and have well-characterized safety profiles from their clinical use in hematological malignancies. CRBN-based PROTACs benefit from extensive precedent and optimization knowledge, though resistance mechanisms via CRBN mutations present clinical concerns [74].
The VHL platform employs hydroxyproline-based ligands that mimic the natural VHL substrate HIF-1α [100]. These recruiters typically offer high specificity and well-defined binding modes, though their physicochemical properties can present challenges for oral bioavailability. VHL expression patterns can be leveraged for tissue-selective targeting, as demonstrated by DT2216, which minimizes platelet toxicity due to low VHL expression in platelets [74].
Emerging E3 Ligase Platforms
The heavy reliance on CRBN and VHL has prompted systematic efforts to identify and characterize novel E3 ligases for TPD applications. Several promising candidates have emerged:
MDM2 leverages natural regulation of p53 and offers opportunities for dual-targeting strategies in cancers with wild-type p53 [100]. cIAP1 recruiters based on SMAC mimetics can potentially synergize with apoptotic induction in cancer cells [100]. KEAP1 functions as a substrate receptor for Cullin3-RING ligase and possesses a well-defined binding pocket for natural inhibitor NRF2, facilitating ligand development [100].
A comprehensive analysis of E3 ligase ligandability identified 76 E3s as promising candidates for PROTAC development based on confidence score, ligandability, expression pattern, and protein-protein interaction potential [74]. This expansion addresses critical limitations of current platforms, including tissue-specific expression patterns for reduced toxicity, diverse subcellular localizations for targeting compartment-specific proteins, and redundancy to circumvent resistance mechanisms [74].
Table 3: Comparative Analysis of Major E3 Ligase Platforms for PROTAC Development
| E3 Ligase | Recruiting Ligand | Advantages | Limitations | Clinical Stage |
|---|---|---|---|---|
| CRBN | Thalidomide derivatives (IMiDs) | Favorable drug-like properties, extensive precedent | Resistance via CRBN mutations | Phase III (Multiple candidates) |
| VHL | Hydroxyproline derivatives | High specificity, tissue-selective expression | Challenges with oral bioavailability | Phase III |
| MDM2 | Nutlin analogs | Potential for p53 synergy, well-characterized | On-target hematological toxicity | Phase I |
| cIAP1 | SMAC mimetics | Apoptosis potentiation, covalent recruiters | Potential inflammatory effects | Preclinical |
| KEAP1 | NRF2-derived peptides | Reactive oxygen species modulation, natural ligand available | Competition with endogenous NRF2 | Preclinical |
Experimental Approaches in E3 Ligase and PROTAC Research
Ternary Complex Analysis
The efficacy of PROTAC molecules hinges on productive ternary complex formation between target protein, degrader, and E3 ligase. Several methodological approaches enable detailed characterization of these complexes:
X-ray Crystallography provides high-resolution structural information for rational degrader optimization. Researchers have resolved over 36 ternary complex structures, enabling structure-activity relationship studies [106]. Experimental protocols involve co-crystallization of the target protein-PROTAC-E3 ligase complex, followed by data collection using synchrotron radiation and structure determination through molecular replacement.
Computational Modeling platforms including PRosettaC and AlphaFold3 enable predictive modeling of ternary complex geometry [106]. Benchmarking studies demonstrate that PRosettaC outperforms AlphaFold3 in predicting biologically relevant ternary complex configurations, with superior DockQ scores reflecting more accurate interface predictions [106]. The standard protocol involves input of target and E3 structures, PROTAC linker specification in SMILES format, and generation of 200-1000 models followed by clustering and interface analysis.
Biophysical Characterization through surface plasmon resonance (SPR) and isothermal titration calorimetry (ITC) provides quantitative assessment of binding affinities and cooperative effects in ternary complex formation.
Degradation Efficiency Assessment
Functional validation of PROTAC activity employs multiple complementary approaches:
Cell-Based Degradation Assays treat appropriate cell lines with PROTAC compounds across a concentration range (typically 0.001-10 μM) for 4-24 hours, followed by quantification of target protein levels via western blotting or cellular thermal shift assays [100]. Key parameters include DC50 (concentration achieving 50% degradation) and Dmax (maximum degradation achieved).
Kinetic Profiling evaluates the temporal dynamics of protein degradation and resynthesis through time-course experiments, providing insights into degradation efficiency and pharmacological persistence.
Proteome-Wide Specificity Assessment utilizes techniques like thermal proteome profiling or multiplexed quantitative proteomics to identify off-target degradation effects, a critical consideration for therapeutic development.
Diagram 1: PROTAC Mechanism of Action - This diagram illustrates the catalytic cycle of PROTAC-mediated protein degradation, highlighting the ternary complex formation and ubiquitin transfer process.
Emerging Technologies and Future Directions
Advanced TPD Modalities
Beyond conventional PROTACs, several innovative TPD platforms have emerged to address limitations and expand the degradable proteome:
Molecular Glues represent a distinct class of monovalent degraders that induce novel protein-protein interactions between E3 ligases and target proteins without requiring a pre-existing binding pocket [102] [99]. These compounds typically exhibit superior pharmacological properties compared to bifunctional PROTACs, though their discovery remains largely serendipitous. Established examples include immunomodulatory imide drugs (thalidomide, lenalidomide) that redirect CRBN to degrade transcription factors IKZF1 and IKZF3 [102].
Lysosome-Targeting Chimeras expand degradation capability to extracellular and membrane proteins by recruiting cell surface lysosome-targeting receptors instead of E3 ligases [105] [99]. This approach utilizes the endolysosomal pathway rather than the ubiquitin-proteasome system, significantly broadening the scope of addressable targets.
Antibody-Based PROTACs combine the target specificity of antibodies with the degradation mechanism of PROTACs, enabling improved tissue selectivity and pharmacokinetic profiles [74].
Pro-PROTAC and Conditional Activation Strategies
The development of PROTAC prodrugs represents an innovative approach to enhance specificity and reduce off-target effects:
Opto-PROTACs incorporate photolabile caging groups (e.g., DMNB, DEACM) that prevent E3 ligase engagement until uncaged by specific light wavelengths [105]. This enables precise spatiotemporal control of protein degradation, particularly valuable for research applications and potential precision therapeutics. Standard implementation involves installation of photolabile groups on critical hydrogen bond donors of E3 ligands, with activation typically at 365 nm UV light [105].
Bio-orthogonal PROTACs utilize bio-labile moieties that are cleaved by disease-specific enzymes (e.g., matrix metalloproteinases in tumor microenvironments), enabling context-dependent activation [105].
Computational and AI-Driven Design
Artificial intelligence is revolutionizing PROTAC development through multiple applications:
Predictive Modeling platforms like DeepPROTAC and AIMLinker employ graph neural networks to extract structural features from target and E3 binding pockets, generating optimized linker designs [105] [106].
Ternary Complex Prediction tools including PRosettaC and PROflow implement constraint-based sampling and iterative refinement to model degrader-induced interfaces more accurately than conventional docking approaches [106].
High-Throughput Screening algorithms can virtually screen thousands of potential warhead-linker combinations, prioritizing synthetically feasible candidates with favorable physicochemical properties.
Diagram 2: PROTAC Development Workflow - This diagram outlines the iterative process of rational PROTAC design, from target identification to experimental validation.
Research Toolkit: Essential Reagents and Methodologies
Table 4: Key Research Reagent Solutions for E3 Ligase and PROTAC Studies
| Research Tool | Function/Application | Example Products/Sources |
|---|---|---|
| E3 Ligase Recruitment Ligands | PROTAC construction for specific E3 ligases | VHL Ligands (VH-032, VH-101), CRBN Ligands (Pomalidomide, Lenalidomide), MDM2 Ligands (Nutlin-3) |
| Ubiquitination Assay Kits | In vitro assessment of E3 ligase activity | Ubiquitin Ligase Assay Kits (containing E1, E2, ubiquitin, ATP), Tandem Ubiquitin Binding Entities (TUBEs) |
| Proteasome Inhibitors | Validation of ubiquitin-proteasome system dependence | MG-132, Bortezomib, Carfilzomib |
| Ternary Complex Analysis Tools | Structural and biophysical characterization | PRosettaC Software, AlphaFold3, Surface Plasmon Resonance (SPR) platforms |
| Degradation Reporter Systems | High-throughput screening of degraders | NanoLuc-tagged protein constructs, HaloTag fusion systems, GFP-deGron reporters |
| E3 Ligase Expression Plasmids | Functional studies of E3 ligases | cDNA clones for CRBN, VHL, MDM2, and other E3s in mammalian expression vectors |
| Selective E3 Inhibitors | Validation of E3-specific degradation mechanisms | MLN4924 (NEDD8 activation inhibitor), CC-90009 (CDK9 inhibitor) |
The strategic development of E3 ligase-targeted therapies represents a transformative approach in cancer therapeutics, with PROTAC technology leading this paradigm shift. The current landscape is characterized by rapid clinical advancement alongside expanding fundamental knowledge of E3 ligase biology and degradation mechanisms. Future progress will necessitate diversification of utilized E3 ligases, enhanced understanding of resistance mechanisms, and continued innovation in degrader technologies to fully exploit the therapeutic potential of the ubiquitin-proteasome system. As these technologies mature, they promise to significantly expand the druggable proteome and address critical unmet needs in oncology and beyond.
Validating Ubiquitination Signatures and Cross-Cancer Comparative Analysis
Prognostic Ubiquitination-Related Gene Signatures Across Multiple Cancer Types
The ubiquitin-proteasome system (UPS) represents a crucial post-translational regulatory mechanism that controls nearly all cellular processes through targeted protein degradation and modulation of protein function [1] [107]. This system employs a sequential enzymatic cascade involving E1 activating enzymes, E2 conjugating enzymes, and E3 ligases to attach ubiquitin molecules to substrate proteins, while deubiquitinases (DUBs) reverse this process [108] [107]. The specificity of ubiquitination is largely determined by the combinatorial action of E2/E3 enzymes, with humans encoding approximately 40 E2s and 600 E3s [107] [109]. Dysregulation of ubiquitination pathways is now recognized as a hallmark of cancer, driving uncontrolled cell proliferation, evasion of apoptosis, and metastasis [110]. Recent advances in transcriptomic technologies have enabled the identification of ubiquitination-related gene (URG) signatures that demonstrate significant prognostic value across multiple cancer types, offering new opportunities for risk stratification and personalized treatment approaches [1] [111] [112].
Comparative Analysis of Ubiquitination-Related Prognostic Signatures
Pan-Cancer URG Signatures
Comprehensive pan-cancer analyses have identified several ubiquitination-related enzymes with broad prognostic significance across multiple malignancies. Table 1 summarizes key URG signatures with validated prognostic value across different cancer types.
Table 1: Ubiquitination-Related Gene Signatures with Prognostic Value Across Cancers
| Cancer Type | Signature Genes | Performance (AUC) | Clinical Utility | Reference |
|---|---|---|---|---|
| Cervical Cancer | MMP1, RNF2, TFRC, SPP1, CXCL8 | 1/3/5-year AUC >0.6 | Survival prediction, immune microenvironment characterization | [1] |
| Cervical Cancer | KLHL22, UBXN11, FBXO25, ANKRD13A, WSB1, WDTC1, ASB1, INPPL1, USP21, MIB2, USP30, TRIM32, SOCS1 | Robust prognostic separation | Risk stratification, TME assessment | [112] |
| Breast Cancer | TCN1, DIRAS3, IZUMO4 | Significant prognostic value | Immunotherapy response prediction, drug sensitivity | [111] |
| Gastric Cancer | OTULIN, UBE2C, USP1, USP2, MAPT | Validated in multiple cohorts | Prognostic classification, immunotherapy guidance | [113] |
| Pan-Cancer | UBE2T | Consistently prognostic | Therapeutic target, immune infiltration marker | [20] |
The ubiquitin-conjugating enzyme UBE2T has emerged as a particularly promising pan-cancer biomarker, with comprehensive analyses revealing elevated expression across multiple tumor types where its upregulation correlates strongly with poor clinical outcomes [20]. Functional studies demonstrate that UBE2T promotes key oncogenic processes including proliferation, invasion, and epithelial-mesenchymal transition through pathways such as cell cycle regulation, ubiquitin-mediated proteolysis, p53 signaling, and mismatch repair [20]. Beyond UBE2T, various cancer types exhibit distinct yet overlapping URG signatures that reflect both tissue-specific and shared oncogenic mechanisms.
Cancer-Type Specific Signatures
In cervical cancer, two independent studies have identified distinct but partially overlapping URG signatures. One research team developed a 5-gene signature (MMP1, RNF2, TFRC, SPP1, and CXCL8) that effectively stratifies patients into high-risk and low-risk groups with significant differences in overall survival [1]. The risk score model demonstrated consistent predictive value across training, testing, and validation cohorts, with area under the curve (AUC) values exceeding 0.6 for 1-, 3-, and 5-year survival predictions [1]. A separate investigation identified a more extensive 13-gene signature that similarly enabled robust prognostic stratification [112]. Both signatures were associated with distinct tumor immune microenvironments, suggesting potential utility in guiding immunotherapy approaches.
For breast cancer, a 3-gene ubiquitination-related signature (TCN1, DIRAS3, and IZUMO4) has shown significant prognostic value, with the high-risk group demonstrating markedly poorer survival outcomes [111]. This signature functioned as an independent prognostic factor in both univariate and multivariate Cox regression analyses, and exhibited significant correlations with tumor microenvironment composition and immunotherapy response [111]. The risk score showed positive association with immunosuppressive elements in the tumor microenvironment and negative correlation with immunotherapy response, providing potential mechanistic insights into the observed survival differences.
In gastric cancer, researchers established a 5-gene ubiquitination-associated signature (OTULIN, UBE2C, USP1, USP2, and MAPT) that effectively categorizes patients into distinct risk groups with significant survival differences [113]. Functional validation through in vitro experiments demonstrated that OTULIN knockdown suppressed cell viability and metastatic capacity in gastric cancer cell lines, supporting its direct role in cancer progression [113]. This signature also correlated with immune landscape features and showed predictive value for immunotherapy response, highlighting the interconnection between ubiquitination pathways and anti-tumor immunity.
Methodological Framework for URG Signature Development
Core Analytical Pipeline
The development of prognostic URG signatures follows a relatively standardized bioinformatics pipeline, as illustrated in Figure 1 below.
The analytical workflow begins with comprehensive data acquisition from public repositories such as The Cancer Genome Atlas (TCGA), Gene Expression Omnibus (GEO), and Genotype-Tissue Expression (GTEx) projects [1] [111] [112]. Following quality control and normalization, differential expression analysis identifies genes with significant expression differences between tumor and normal tissues using tools such as DESeq2 or the limma package [1] [111]. These differentially expressed genes are then filtered against curated ubiquitination-related gene sets from databases like GeneCards or the Integrated Annotations for Ubiquitin and Ubiquitin-Like Conjugation Database (IUUCD) to identify ubiquitination-related candidates [1] [112] [113].
Consensus clustering utilizing the ConsensusClusterPlus package often follows to identify molecular subtypes based on URG expression patterns, revealing intrinsic tumor classifications with prognostic significance [111] [112]. The core feature selection process typically employs univariate Cox regression to identify prognosis-associated URGs, followed by least absolute shrinkage and selection operator (LASSO) Cox regression to prevent overfitting and select the most robust prognostic genes [1] [111] [112]. The final risk model is constructed using a linear combination of selected gene expression levels weighted by their regression coefficients: Risk Score = Σ(Coefi * Expressioni) [111] [112]. Patients are stratified into high-risk and low-risk groups based on the median risk score or optimal cutoff determined through survival analysis.
Validation and Functional Characterization
Robust validation represents a critical step in URG signature development. This typically involves internal validation through bootstrap resampling or split-sample approaches, and external validation using independent datasets from repositories like GEO [1] [112]. Validation metrics include Kaplan-Meier survival analysis with log-rank tests, time-dependent receiver operating characteristic (ROC) curves assessing sensitivity and specificity at 1, 3, and 5 years, and calculation of the concordance index (C-index) to evaluate model discrimination [1] [111]. Multivariate Cox regression establishes whether the URG signature provides prognostic information independent of standard clinical parameters such as age, stage, and grade [111] [112].
Functional characterization explores the biological underpinnings of prognostic signatures through Gene Ontology (GO) and Kyoto Encyclopedia of Genes and Genomes (KEGG) enrichment analyses using the clusterProfiler package [1] [112]. Gene Set Enrichment Analysis (GSEA) identifies pathways differentially activated between risk groups, with common ubiquitination-related pathways including cell cycle regulation, ubiquitin-mediated proteolysis, p53 signaling, and DNA repair mechanisms [20] [112]. Immune correlation analysis has become an integral component, with algorithms such as CIBERSORT, ESTIMATE, and MCPcounter quantifying immune cell infiltration, and tools like TIDE predicting immunotherapy response [1] [111] [112].
The Ubiquitin Code in Cancer Signaling Pathways
The ubiquitination process creates a complex "ubiquitin code" that determines substrate fate, with different chain linkages triggering distinct cellular outcomes as depicted in Figure 2.
The specificity of ubiquitin signaling arises from several mechanisms. First, monoubiquitination typically alters protein activity, localization, or interactions without triggering degradation [110]. For example, monoubiquitination of histones represents a key DNA damage response mechanism [110]. Second, different polyubiquitin chain linkages create distinct structural motifs recognized by specific receptor proteins: K48-linked chains primarily target substrates for proteasomal degradation; K63-linked chains facilitate non-proteolytic signaling in pathways such as NF-κB activation and DNA damage repair; while K11-linked chains play specialized roles in cell cycle regulation [107] [110]. Third, mixed or branched chains create combinatorial complexity that expands the functional repertoire of ubiquitin signaling [110].
In cancer cells, disruption of the ubiquitin code can occur at multiple levels. Oncogenic mutations may alter E3 ligase substrate recognition, as seen with PARKIN mutations in Parkinson's disease and certain cancers [107]. Overexpression of specific E2 enzymes like UBE2T can drive hyper-proliferation by accelerating the degradation of tumor suppressors [20]. Dysregulated DUB activity can stabilize oncoproteins that would normally be targeted for destruction, creating a permissive environment for tumor growth and survival [114]. The prognostic URG signatures identified through bioinformatics approaches likely reflect these fundamental disruptions in ubiquitin signaling homeostasis, explaining their strong association with clinical outcomes.
Experimental Validation and Translational Applications
Functional Validation Approaches
While bioinformatics discoveries provide valuable insights, experimental validation remains essential to establish causal relationships between URGs and cancer phenotypes. Common validation approaches include:
In vitro functional assays typically begin with gene manipulation using siRNA, shRNA, or CRISPR-Cas9 systems to knock down or knock out target URGs in cancer cell lines [113]. Subsequent phenotypic assessments evaluate changes in proliferation (CCK-8, MTT assays), apoptosis (Annexin V staining), cell cycle distribution (flow cytometry), migration (wound healing assays), and invasion (Transwell assays) [112] [113]. For example, OTULIN knockdown in gastric cancer cell lines significantly suppressed both cell viability and metastatic capacity, providing mechanistic support for its inclusion in prognostic signatures [113].
Molecular techniques help elucidate the mechanisms underlying URG functions. Reverse Transcription-Quantitative PCR (RT-qPCR) and western blotting confirm gene expression changes at mRNA and protein levels, respectively [1] [20]. Ubiquitination assays evaluate changes in substrate ubiquitination status following URG manipulation. Immunoprecipitation and mass spectrometry identify specific protein substrates and interaction partners, helping to place URGs within specific cellular pathways [107] [114].
In vivo models provide important physiological context through xenograft experiments where URG-manipulated cancer cells are implanted into immunodeficient mice to assess effects on tumor growth, metastasis, and treatment response [114]. More complex genetically engineered mouse models can further validate URG functions in authentic tumor microenvironments with intact immune systems.
Clinical Translation and Therapeutic Implications
The translational potential of URG signatures extends beyond prognosis to include treatment selection and therapeutic development. Several applications show particular promise:
Immunotherapy guidance represents a major clinical application, as URG signatures consistently correlate with immune cell infiltration patterns and checkpoint inhibitor expression [1] [111] [113]. For example, in breast cancer, the URG-based risk score showed significant correlation with tumor microenvironment composition and predicted response to immunotherapy, with the high-risk group exhibiting stronger immunosuppressive characteristics [111]. Similarly, in cervical cancer, immune microenvironment analysis revealed significant differences in 12 immune cell types between high-risk and low-risk groups, including memory B cells and M0 macrophages, along with differential expression of four immune checkpoints [1].
Drug sensitivity prediction enables more personalized therapeutic approaches. Several studies have demonstrated that URG signatures can predict sensitivity to both conventional chemotherapeutic agents and targeted therapies [111] [20]. For instance, UBE2T expression showed positive correlation with trametinib and selumetinib sensitivity, and negative correlation with CD-437 and mitomycin in pan-cancer analyses [20]. In breast cancer, distinct IC50 values for various targeted agents were observed between URG-based risk groups, with rapamycin showing higher efficacy in low-risk patients, while axitinib, AZD6244, erlotinib, and several other agents demonstrated greater potency in high-risk patients [111].
Therapeutic development directly targets dysregulated ubiquitination pathways. Several strategies have emerged, including small molecule inhibitors targeting specific E1, E2, E3, or DUB enzymes [108] [107] [114]; proteolysis-targeting chimeras (PROTACs) that hijack E3 ligases to degrade specific oncoproteins [108] [110]; and fragment-based drug discovery (FBDD) approaches to develop selective ubiquitin system modulators [109]. While clinical success has been limited thus far, with only a handful of FDA-approved drugs targeting the ubiquitin system, the growing recognition of ubiquitination dysregulation in cancer continues to drive therapeutic innovation in this space [107] [114].
Table 2: Key Research Reagents and Computational Tools for URG Signature Development
| Resource Category | Specific Tools/Reagents | Primary Application | Key Features |
|---|---|---|---|
| Bioinformatics Databases | TCGA, GEO, GTEx, cBioPortal | Data acquisition | Multi-omics cancer data, normal tissue reference |
| URG Curation Sources | GeneCards, IUUCD, MSigDB | Ubiquitin-related gene filtering | Curated gene sets with relevance scores |
| Differential Expression Analysis | DESeq2, limma R package | Identifying DEGs | Statistical rigor, handling of RNA-seq/microarray data |
| Consensus Clustering | ConsensusClusterPlus R package | Molecular subtype identification | Determines optimal cluster number with stability assessment |
| Survival Analysis | survival, survminer R packages | Prognostic model validation | Kaplan-Meier curves, Cox regression, log-rank tests |
| Immune Infiltration Analysis | CIBERSORT, TIMER, MCPcounter, TIDE | Tumor microenvironment characterization | Deconvolution of immune cell fractions, immunotherapy response prediction |
| Functional Enrichment | clusterProfiler, GSEA software | Biological pathway analysis | GO, KEGG, Hallmark gene set enrichment |
| Experimental Validation | siRNA/shRNA, RT-qPCR, Western blot, Transwell assays | Functional confirmation | Gene manipulation, expression confirmation, migration/invasion assessment |
The experimental and computational tools summarized in Table 2 represent essential resources for researchers working to develop and validate URG prognostic signatures. These resources enable the complete workflow from initial data mining through functional validation, facilitating robust and reproducible research in this emerging field.
Ubiquitination-related gene signatures represent powerful tools for prognostic stratification across multiple cancer types, with demonstrated clinical utility in cervical, breast, gastric, and various other malignancies. The consistent observation that these signatures provide independent prognostic information beyond standard clinical parameters highlights the fundamental role of ubiquitination dysregulation in cancer progression. Furthermore, the strong associations between URG signatures and tumor immune microenvironments offer exciting opportunities for guiding immunotherapy approaches and understanding treatment resistance mechanisms. While significant progress has been made in signature development through bioinformatics approaches, future research should prioritize functional validation of individual signature components, standardization of analytical pipelines across institutions, and prospective validation in clinical trial cohorts. As our understanding of the ubiquitin code continues to expand, along with developments in targeted protein degradation technologies, URG signatures are poised to play an increasingly important role in personalized cancer management, ultimately improving patient outcomes through more precise risk assessment and treatment selection.
Single-Cell Resolution of Ubiquitination Patterns in the Tumor Microenvironment
The tumor microenvironment (TME) represents a complex ecosystem where tumor cells interact with immune cells, stromal components, and extracellular matrix in a dynamic interplay that dictates disease progression and therapeutic response [115] [116]. Within this multifaceted environment, ubiquitination has emerged as a crucial post-translational modification that regulates virtually all cellular processes, including those governing tumor-immune interactions [36]. This reversible process, mediated by ubiquitin-activating enzymes (E1), ubiquitin-conjugating enzymes (E2), and ubiquitin ligases (E3), controls protein stability, localization, and activity, thereby influencing key oncogenic signaling pathways and immune cell functions [21] [36].
The advent of single-cell technologies has revolutionized our understanding of cancer biology by enabling researchers to dissect the cellular heterogeneity that characterizes human malignancies [117]. While bulk sequencing approaches average signals across diverse cell populations, single-cell RNA sequencing (scRNA-seq), mass cytometry (CyTOF), and imaging flow cytometry (IFC) provide unprecedented resolution to examine molecular processes at the individual cell level [118] [117] [119]. The integration of these advanced analytical platforms with ubiquitination research now allows scientists to map the ubiquitin modification landscape across distinct cellular compartments within the TME, revealing previously unappreciated complexity in cancer-immune crosstalk [120].
Single-Cell Technologies for Ubiquitination Analysis
Technological Platforms and Workflows
Multiple high-resolution platforms have been adapted for studying ubiquitination patterns within the TME. Each technology offers unique advantages for capturing different dimensions of ubiquitin-mediated regulation:
Single-cell RNA sequencing enables comprehensive profiling of the ubiquitination machinery by quantifying expression of E1, E2, E3, and deubiquitination enzymes (DUBs) across individual cells [120]. The standard workflow begins with tissue dissociation and single-cell suspension preparation, followed by cell partitioning using microfluidic devices (e.g., 10x Genomics Chromium) [121] [117]. After reverse transcription and cDNA amplification, libraries are sequenced to generate digital gene expression matrices that can be analyzed to identify cell subtypes based on their ubiquitin-related enzyme expression patterns [117] [120]. Computational tools like AUCell then allow quantification of "ubiquitination activity" in individual cells based on enrichment of ubiquitination-related gene sets [120].
Mass cytometry (CyTOF) combines flow cytometry with mass spectrometry, using metal-tagged antibodies to simultaneously quantify over 40 parameters at single-cell resolution [122]. This technology is particularly valuable for tracking ubiquitination-mediated protein degradation and signaling pathway activity in complex cell mixtures. A key application is the assessment of Treg suppression capacity within PBMC populations, where a 52-marker CyTOF panel can quantify cell division and phenotypic responses across multiple immune subsets while monitoring ubiquitination-related proteins [122]. Unlike conventional fluorescence-based flow cytometry, CyTOF eliminates spectral overlap issues, providing more precise quantification of low-abundance signaling proteins regulated by ubiquitination [122].
Imaging flow cytometry merges the high-throughput capabilities of conventional flow cytometry with high-resolution morphological imaging [119]. This technology captures multichannel images of individual cells as they flow through the detection system, enabling simultaneous quantification of ubiquitination markers and their subcellular localization. The system employs a fluidics system to hydrodynamically focus cells into a single-file stream, illumination sources (typically lasers) to excite fluorophores, and a high-speed camera to capture brightfield, darkfield, and fluorescent images of each cell [119]. This approach is particularly powerful for studying ubiquitination-dependent protein aggregation, nuclear-cytoplasmic shuttling, and organelle-specific degradation events within heterogeneous tumor samples [119].
Comparative Analysis of Single-Cell Platforms
Table 1: Comparison of Single-Cell Technologies for Ubiquitination Studies
| Technology | Key Applications in Ubiquitination Research | Throughput | Multiplexing Capacity | Spatial Information | Key Limitations |
|---|---|---|---|---|---|
| scRNA-seq | Expression profiling of E1/E2/E3/DUB enzymes; inference of ubiquitination states from transcriptional signatures | 10,000-100,000 cells | Whole transcriptome (>10,000 genes) | No native spatial context (requires integration with spatial transcriptomics) | Indirect measurement of ubiquitination; does not directly quantify protein degradation |
| Mass Cytometry (CyTOF) | High-dimensional protein quantification; phospho-signaling analysis; monitoring ubiquitination-mediated protein turnover | 1,000-10,000 cells | 40-50 protein markers simultaneously | Limited to coarse spatial patterns | Requires specific metal-conjugated antibodies; destructive to cells |
| Imaging Flow Cytometry | Subcellular localization of ubiquitinated proteins; morphological analysis of protein aggregates; quantification of ubiquitin foci | 5,000-20,000 cells | 6-10 fluorescent channels | High-resolution subcellular images | Lower multiplexing compared to CyTOF; potential spectral overlap issues |
Ubiquitination Patterns Across Cancer Types
Pan-Cancer Analysis of Ubiquitination Machinery
Comprehensive pan-cancer analyses have revealed that components of the ubiquitin-proteasome system (UPS) are frequently dysregulated across multiple cancer types [21]. Studies integrating data from The Cancer Genome Atlas (TCGA) with single-cell datasets have demonstrated that UBA1 and UBA6, the two primary ubiquitin-activating E1 enzymes, show elevated expression in numerous malignancies including breast cancer (BRCA), colorectal cancer (COAD), renal cancer (KIRC), and lung adenocarcinoma (LUAD) [21]. This elevated expression often correlates with advanced disease stage and poorer patient survival, suggesting a fundamental role in cancer progression [21]. Importantly, single-cell resolution has revealed that these expression patterns are not uniform across all cells within tumors but show cell-type-specific regulation that is masked in bulk analyses.
In lung adenocarcinoma, integrated analysis of scRNA-seq datasets (GSE117570, GSE131907, GSE149655, GSE123902) with bulk transcriptomic data has identified PSMD14, a critical deubiquitination enzyme, as a promising therapeutic target [120]. PSMD14 stabilizes the AGR2 protein, promoting LUAD progression through enhanced tumor cell survival and proliferation pathways [120]. The single-cell approach enabled researchers to pinpoint this enzyme's specific overexpression in malignant epithelial cells rather than the stromal or immune compartments, highlighting the precision afforded by single-cell technologies in identifying cell-type-specific therapeutic targets.
Cancer-Type-Specific Ubiquitination Signatures
Uterine Leiomyosarcoma (ULSA) exhibits a profoundly immunosuppressive TME characterized by exhausted CD8+ T cells, M2-polarized macrophages, and N2 neutrophils [121]. Single-cell profiling of metastatic lesions from treatment-naïve ULSA patients has revealed that T cell exhaustion markers (LAG3, HAVCR2, TIGIT) are enriched over time, replacing initial T cell markers (CCR7, MAL) [121]. This exhausted phenotype is maintained through ubiquitination-mediated degradation of key T cell signaling proteins, creating a barrier to effective immune checkpoint blockade. Additionally, the MIF-(CD74+CD44) and CXCL8 signaling axes identified through cell-cell communication analysis represent potential ubiquitination regulatory nodes that could be therapeutically targeted [121].
Colorectal Cancer (CRC) showcases how specific tumor cell subpopulations manipulate ubiquitination pathways to influence immune responses. The MKI67+ tumor cell subpopulation dynamically interacts with macrophages through the MIF-(CD74+CD44) axis to promote pro-tumorigenic signaling [116]. HMGA1, a transcription factor enriched in this subpopulation, emerges as a critical regulator subject to ubiquitination-mediated control [116]. Experimental validation using siRNA knockdown demonstrated that HMGA1 suppression impedes CRC cell proliferation, motility, and invasion, suggesting that targeting its stability through ubiquitination pathways could represent a viable therapeutic strategy. Furthermore, chronic inflammation in the CRC TME creates a feed-forward loop where inflammatory signaling enhances ubiquitination of tumor suppressors while stabilizing oncoproteins, contributing to both cancer progression and associated cardiac dysfunction [116].
Table 2: Key Ubiquitination-Related Enzymes and Their Cancer-Type-Specific Roles
| Enzyme | Class | Cancer Types | Biological Function in TME | Therapeutic Implications |
|---|---|---|---|---|
| UBA1 | E1 ubiquitin-activating enzyme | Pan-cancer (especially BRCA, COAD, KIRC, LUAD) | Global protein ubiquitination; elevated in most cancers; correlates with poor prognosis | Essential for tumor cell survival; potential target for small molecule inhibitors |
| UBA6 | E1 ubiquitin-activating enzyme | Pan-cancer (especially BRCA, COAD, KIRC, LUAD) | Activates both ubiquitin and FAT10; regulates p53 stability | Tumor-specific expression patterns may enable selective targeting |
| PSMD14 | Deubiquitinase (DUB) | Lung adenocarcinoma | Stabilizes AGR2 oncoprotein; promotes tumor progression | Small molecule inhibitors show preclinical efficacy |
| EDARADD | Ubiquitination adapter | Uterine leiomyosarcoma | Associated with metastasis-susceptible cell subset (U11-EDARADD) | Potential biomarker for aggressive disease |
Experimental Protocols for Single-Cell Ubiquitination Analysis
Mass Cytometry Protocol for Treg Suppression Profiling
The single-cell suppression profiling of human Tregs (scSPOT) protocol exemplifies how high-dimensional single-cell analysis can elucidate functional immune regulation relevant to ubiquitination pathways [122]. This methodology enables quantification of Treg-mediated suppression within autologous peripheral blood mononuclear cells (PBMCs) while simultaneously assessing proliferation and phenotypic responses across multiple immune subsets.
Day 1: Cell Preparation and Staining
- Thaw frozen PBMCs and assess viability (>90% required)
- Stain with CFSE cell proliferation dye (1:1000 dilution) to track cell division
- Isolate Tregs using magnetic-activated cell sorting (MACS) with CD4 Positive Selection Kit, followed by fluorescence-activated cell sorting (FACS) for CD4+CD25+CD127lo population
- Recombine Tregs with autologous PBMCs at defined ratios (typically 1:1 to 1:16 Treg:PBMC ratios)
- Stimulate cultures with anti-CD3 antibody (0.5 μg/mL) and IL-2 (100 U/mL)
Days 2-5: Culture and Perturbation
- Maintain cultures in complete RPMI-1640 medium with 10% FBS
- Add experimental perturbations (e.g., ubiquitination inhibitors, immune checkpoint blockers)
- Include controls: untreated, isotype controls, single cultures of Tregs and responder cells
Day 5: Mass Cytometry Staining
- Harvest cells and stain with viability marker (Cell-ID Cisplatin-198Pt, 1:2000 dilution)
- Perform barcoding with DCED Palladium (1:500 dilution) to enable sample multiplexing
- Pre-stain with antibodies against surface markers that require 37°C staining (CD45RA-153Eu, CXCR3-154Sm, CCR7-155Gd)
- Fix and permeabilize cells using Foxp3 Transcription Factor Staining Buffer Set
- Stain intracellular targets with metal-tagged antibodies (52-parameter panel recommended)
- Acquire data on CyTOF instrument following standard operation procedures
Days 6-14: Data Analysis
- Normalize data using EQ Four Element Calibration Beads
- Debarcode samples based on palladium staining patterns
- Apply dimensionality reduction (t-SNE, UMAP) and clustering (PhenoGraph) algorithms
- Quantify suppression metrics by comparing proliferation (CFSE dilution) and activation markers in cultures with versus without Tregs
- Analyze differential expression of ubiquitination-related proteins across cell types and conditions
Single-Cell RNA Sequencing Workflow for Ubiquitination Enzyme Expression
The following protocol outlines the standard approach for processing scRNA-seq data to investigate ubiquitination patterns, as applied in studies of lung adenocarcinoma and colorectal cancer [116] [120]:
Quality Control and Preprocessing
- Import single-cell data into R using Seurat package (v4.3.0 or higher)
- Filter cells based on quality metrics:
- Retain cells with 500 < nFeature_RNA < 6000
- Exclude cells with mitochondrial gene content >25%
- Remove doublets using DoubletFinder algorithm (v2.0.3)
- Normalize data using SCTransform function with glmGamPoi method
- Identify highly variable features using the 'vst' method (3000 genes recommended)
Dimensionality Reduction and Clustering
- Perform principal component analysis (PCA) on scaled data
- Select significant principal components based on elbow plot (typically 10-20 PCs)
- Apply graph-based clustering using Louvain algorithm (resolution 0.4-1.2)
- Generate 2D visualizations with UMAP or t-SNE
Ubiquitination-Specific Analysis
- Extract ubiquitination-related genes from the Integrated Ubiquitin and Ubiquitin-like Conjugation Database (iUUCD)
- Calculate ubiquitination activity scores using AUCell to identify cells with active ubiquitination pathways
- Identify differentially expressed ubiquitination enzymes across cell subtypes using Wilcoxon rank-sum test
- Infer copy number variations in malignant cells using InferCNV with immune cells as reference
- Reconstruct cellular trajectories using Monocle3 to understand ubiquitination dynamics in cell state transitions
Visualization of Ubiquitination Signaling Networks
Ubiquitination-Mediated Immune Regulation in the TME
The following diagram illustrates the key ubiquitination pathways that regulate immune cell function within the tumor microenvironment, integrating findings from multiple cancer types:
Diagram 1: Ubiquitination Pathways in Immune Regulation. This diagram illustrates how the ubiquitin-proteasome system regulates key immune processes in the TME, including T cell exhaustion, macrophage polarization, and Treg suppression through protein degradation and signal activation pathways.
Single-Cell Analysis Workflow for Ubiquitination Studies
The following workflow outlines the integrated experimental and computational pipeline for analyzing ubiquitination patterns at single-cell resolution:
Diagram 2: Single-Cell Analysis Workflow. This diagram outlines the integrated pipeline for processing tumor samples through multiple single-cell technologies to characterize ubiquitination patterns, from tissue processing through computational analysis to biological insights.
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Research Reagent Solutions for Single-Cell Ubiquitination Studies
| Reagent Category | Specific Examples | Application in Ubiquitination Research | Considerations for Experimental Design |
|---|---|---|---|
| Cell Isolation Kits | EasySep Human CD4 Positive Selection Kit; MACS Tumor Dissociation Kits | Isolation of specific immune populations; preparation of single-cell suspensions from tumor tissue | Maintain cell viability >90%; minimize activation during processing; include viability controls |
| Metal-Labeled Antibodies | Self-conjugated antibodies for CyTOF (0.5 mg/mL stock); Standard BioTools pre-conjugated antibodies | High-dimensional protein quantification; monitoring ubiquitination-related signaling | Validate specificity using knockdown/knockout controls; titrate carefully to optimize signal-to-noise |
| Viability Stains | Cell-ID Cisplatin-198Pt; DCED Palladium for barcoding | Exclusion of dead cells; sample multiplexing in mass cytometry | Titrate for optimal separation of live/dead cells; use fresh preparations for consistent results |
| Cell Tracing Dyes | CellTrace CFSE; Cell Proliferation Dyes | Tracking cell division in functional assays | Optimize concentration to avoid toxicity; include proliferation controls without inhibitors |
| Ubiquitination Modulators | Tazemetostat (EZH2 inhibitor); Ipilimumab biosimilar; Proteasome inhibitors (MG132, Bortezomib) | Perturbation experiments to test ubiquitination dependencies | Include dose-response curves; use combination treatments to identify synthetic lethality |
| Single-Cell Reagents | 10x Genomics Chromium Chip Kits; BD Rhapsody Cartridges | Partitioning cells for single-cell RNA sequencing | Quality control input cells; optimize cell concentration to maximize cell recovery |
| Data Analysis Tools | Seurat R package; InferCNV; AUCell; CellChat | Computational analysis of ubiquitination patterns | Implement rigorous quality control pipelines; use appropriate statistical corrections for multiple testing |
The integration of single-cell technologies with ubiquitination research has unveiled remarkable complexity in how protein degradation pathways shape the tumor microenvironment. The comparative analyses across cancer types presented herein reveal both conserved mechanisms and tumor-specific adaptations in ubiquitination regulation. As these technologies continue to evolve, several promising directions emerge for both basic research and therapeutic development.
First, the spatial dimension of ubiquitination regulation remains underexplored. While current single-cell technologies excel at characterizing cellular heterogeneity, they largely discard native spatial context. Emerging spatial transcriptomics and proteomics platforms, when combined with ubiquitination-specific probes, could map the geographic distribution of ubiquitination activity within tumor sections, revealing how positional relationships influence protein stability signaling.
Second, dynamic tracking of ubiquitination events in live cells represents a formidable technical challenge. Novel biosensors that couple ubiquitination-dependent degradation with fluorescent reporters could enable real-time monitoring of pathway activity in living tumor ecosystems, potentially revealing rapid adaptations to therapy that are missed in endpoint analyses.
Finally, the therapeutic targeting of ubiquitination pathways requires greater specificity to avoid detrimental effects on normal cellular processes. The cell-type-specific expression patterns of E3 ligases and DUBs revealed by single-cell analyses suggest opportunities for more selective interventions. As our resolution of the ubiquitin-modified TME continues to sharpen, so too will our ability to manipulate this system for therapeutic benefit in cancer treatment.
The ubiquitin-proteasome system (UPS) represents a crucial regulatory mechanism in cellular homeostasis, governing protein degradation, DNA repair, cell cycle progression, and signal transduction [123]. This enzymatic cascade involves E1 (activating), E2 (conjugating), and E3 (ligating) enzymes that collectively mediate the attachment of ubiquitin chains to target proteins, determining their stability, localization, and function [124] [123]. The intricate role of ubiquitination has gained prominence in oncology, with emerging evidence highlighting its pathogenetic significance across various malignancies. In gynecological cancers, particularly ovarian and cervical carcinomas, ubiquitination pathways demonstrate both shared and distinct mechanistic contributions to tumor initiation, progression, and therapeutic resistance.
The clinical burden of gynecological cancers remains substantial, with ovarian cancer representing the leading cause of gynecological cancer-related mortality and cervical cancer constituting the fourth most common cancer in women worldwide [125] [123]. Understanding the molecular underpinnings of these diseases, especially the nuanced role of post-translational modifications like ubiquitination, provides critical insights for developing targeted therapeutic strategies. This comparative analysis systematically examines the ubiquitination-related mechanisms in ovarian and cervical cancers, highlighting disease-specific pathways, prognostic implications, and emerging therapeutic opportunities tailored to each malignancy's unique ubiquitination landscape.
Comparative Pathogenic Mechanisms
Ubiquitination in Cervical Cancer Pathogenesis
Cervical carcinogenesis is intimately linked to persistent infection with high-risk human papillomavirus (HPV) types, primarily HPV16 and HPV18, which account for approximately 70% of cases [126] [123]. The viral oncoproteins E6 and E7 strategically hijack the host ubiquitination machinery to enable viral persistence and drive malignant transformation. The most characterized mechanism involves E6-mediated recruitment of the cellular E3 ubiquitin ligase E6AP (E6-associated protein), which subsequently targets the tumor suppressor p53 for proteasomal degradation [123]. This deliberate sabotage of p53 function abrogates its pro-apoptotic and cell-cycle checkpoint activities, permitting uncontrolled proliferation and genomic instability.
Concurrently, the HPV E7 oncoprotein facilitates the ubiquitin-mediated degradation of another critical tumor suppressor, the retinoblastoma protein (pRb), through the SKP2-containing SCF (Skp1-Cullin-F-box) E3 ubiquitin ligase complex [123]. The resultant pRb loss leads to aberrant E2F transcription factor activation and unchecked cell cycle progression from G1 to S phase. Beyond these canonical pathways, emerging evidence indicates that HPV oncoproteins manipulate ubiquitin-like proteins (ULPs), including SUMO and NEDD8, to further modify the cellular environment toward malignant transformation [123]. The cumulative effect of these ubiquitination-related disruptions creates a permissive landscape for cervical cancer development and progression.
Ubiquitination in Ovarian Cancer Pathogenesis
Ovarian cancer pathogenesis involves a more diverse array of ubiquitination-related alterations, often centered on hereditary predisposition factors and therapy resistance mechanisms. Hereditary syndromes driven by mutations in BRCA1 and BRCA2 genes significantly elevate ovarian cancer risk, with pathogenic mutations in the BRCA1 ubiquitin ligase increasing risk by 75-fold [125]. These mutations impair DNA damage repair through homologous recombination, creating reliance on alternative repair pathways that can be therapeutically targeted.
Recent prognostic models based on ubiquitination-related genes have identified 17-gene signatures that effectively stratify ovarian cancer patients into distinct risk categories [125] [37]. Among these, FBXO45—an E3 ubiquitin ligase—has been experimentally validated as a key driver of ovarian cancer progression through activation of the Wnt/β-catenin signaling pathway [125] [37]. This ubiquitin ligase promotes the growth, spread, and migration of ovarian cancer cells, establishing it as a critical pathogenetic factor. Additionally, recurrent repression of the polyubiquitin gene UBB has been observed in approximately 30% of high-grade serous ovarian cancers (HGSOCs), creating a unique ubiquitin dependency that can be exploited therapeutically [127].
Table 1: Key Ubiquitination-Related Alterations in Gynecological Cancers
| Characteristic | Cervical Cancer | Ovarian Cancer |
|---|---|---|
| Primary Ubiquitination Trigger | HPV oncoproteins E6 and E7 | Genetic mutations (BRCA1/2), ubiquitin gene repression |
| Key E3 Ligases Involved | E6AP, SKP2 | FBXO45, BRCA1, RNF168, UBR5, WWP2 |
| Main Substrates Targeted | p53, pRb | p53, DNA repair proteins, β-catenin |
| Characteristic Pathway | p53 and pRb degradation | Wnt/β-catenin signaling, DNA damage response |
| Ubiquitin Gene Alterations | Not prominent | UBB repression (30% of HGSOC) |
Therapeutic Targeting and Clinical Implications
Cervical Cancer Therapeutic Strategies
The well-defined role of HPV oncoproteins in subverting ubiquitination pathways has unveiled promising therapeutic avenues for cervical cancer. Proteolysis-targeting chimeras (PROTACs) represent an innovative class of therapeutics that harness the ubiquitin-proteasome system to selectively degrade target proteins [124]. These bifunctional molecules simultaneously bind to E3 ubiquitin ligases and protein targets of interest, facilitating polyubiquitination and subsequent degradation of oncogenic drivers. For cervical cancer, PROTACs could potentially target viral oncoproteins or their interacting partners, thereby eliminating the fundamental drivers of carcinogenesis.
Additional investigative approaches focus on developing small-molecule inhibitors that disrupt the critical interaction between HPV E6 and E6AP, thereby restoring p53 tumor suppressor function [123]. Similarly, targeting the E7-SKP2-pRb axis offers complementary opportunities for therapeutic intervention. The strategic application of these ubiquitination-focused modalities may overcome the limitations of conventional therapies, particularly in advanced or recurrent disease settings where current treatments often yield suboptimal outcomes.
Ovarian Cancer Therapeutic Strategies
Ovarian cancer treatment has been revolutionized by the introduction of PARP inhibitors, which exemplify the clinical translation of ubiquitination-related knowledge into effective therapeutics. These agents selectively target tumors with homologous recombination deficiencies, particularly those harboring BRCA1/2 mutations, through synthetic lethality [128]. The expanding repertoire of ubiquitination-focused interventions for ovarian cancer includes PROTACs targeting ubiquitin enzymes, with at least 50 ubiquitination-related genes currently being investigated as PROTAC targets [125] [124].
Notably, the recurrent repression of UBB in a substantial subset of HGSOCs creates a therapeutic vulnerability characterized by exquisite dependence on the remaining polyubiquitin gene, UBC [127]. Preclinical studies demonstrate that inducible knockdown of UBC in UBB-repressed ovarian cancer models triggers dramatic tumor regression and confers long-term survival benefits, revealing a promising synthetic lethal approach [127]. Additionally, combining ubiquitinase/deubiquitinase inhibitors with immunotherapeutic strategies shows potential for overcoming the drug resistance that frequently complicates ovarian cancer management [129].
Table 2: Therapeutic Approaches Targeting Ubiquitination in Gynecological Cancers
| Therapeutic Approach | Molecular Target | Mechanism of Action | Development Status |
|---|---|---|---|
| Cervical Cancer | |||
| PROTACs | HPV E6/E7 or host factors | Targeted protein degradation | Preclinical investigation |
| E6-E6AP interaction inhibitors | E6-E6AP interface | p53 stabilization | Early development |
| Ovarian Cancer | |||
| PARP inhibitors | PARP enzymes | Synthetic lethality in BRCA-deficient cells | FDA-approved |
| UBC-targeting therapies | UBC polyubiquitin gene | Exploiting UBB repression synthetic lethality | Preclinical validation |
| PROTACs | Various E3 ligases | Targeted protein degradation | Clinical trials for various cancers |
| Ubiquitinase/DUB inhibitors + Immunotherapy | Ubiquitinases/DUBs + Immune checkpoints | Restoring drug sensitivity, enhancing immune response | Investigational |
Experimental Models and Methodologies
Prognostic Model Development for Ovarian Cancer
The development of ubiquitination-based prognostic models for ovarian cancer exemplifies the translational potential of ubiquitination-related research. A standardized methodology has emerged from recent investigations [125] [37]:
Data Acquisition and Processing: Transcriptomic data and clinical profiles are obtained from public repositories such as The Cancer Genome Atlas (TCGA) and Genotype-Tissue Expression (GTEx) databases. For ovarian cancer, this typically involves 376 tumor and 88 normal ovarian tissue samples. Differential gene expression analysis between cancerous and normal tissues identifies significantly dysregulated genes using criteria of |logFC| ≥ 1 and adjusted p-value < 0.01.
Candidate Gene Selection: Ubiquitination-related genes are compiled from specialized databases like the Ubiquitin and Ubiquitin-like Conjugation Database (UUCD), yielding approximately 929 genes categorized into E1 (8 genes), E2 (39 genes), and E3 (882 genes) enzymes. Intersection with differentially expressed genes typically identifies around 162 co-expressed ubiquitination-related genes.
Predictive Model Construction: COX univariate analysis selects ubiquitination-related genes significantly associated with survival (p < 0.05). LASSO regression and deviance tests further refine the gene set, typically yielding a prognostic signature of approximately 17 genes. Risk scores are calculated using the formula: Risk score = Σ(Coefi × Ai), where Coefi represents the regression coefficient and Ai represents the gene expression level. Patients are stratified into high-risk and low-risk groups based on the median risk score.
Validation and Immune Analysis: The model's predictive performance is assessed using Kaplan-Meier survival curves, receiver operating characteristic (ROC) curves, and nomograms. External validation employs independent datasets such as GSE165808 and GSE26712. Subsequent immune landscape analysis evaluates 22 immune cell types, while mutation profiling identifies differentially mutated genes between risk groups.
Experimental Validation of Key Targets
Functional validation of prognostic model components employs comprehensive in vitro methodologies [125] [37]:
Cell Culture and Transfection: Human ovarian cancer cell lines (e.g., A2780, HEY) are maintained under standard conditions with mycoplasma testing and short tandem repeat (STR) authentication. Gene manipulation is achieved through transfection with reagents such as Lipo2000 or Lipo8000.
Molecular Techniques: Quantitative real-time PCR analyzes gene expression using specific primers and RNAiso Reagent for extraction. Western blotting assesses protein expression and pathway activation using antibodies against targets of interest (e.g., FBXO45, WNT1, β-catenin, c-myc). Functional assays including proliferation, migration, and invasion tests evaluate the phenotypic consequences of gene manipulation.
Pathway Analysis: Investigation of signaling pathways (e.g., Wnt/β-catenin) involves measuring expression changes in key pathway components following experimental manipulation of ubiquitination-related genes.
Signaling Pathway Diagrams
HPV Manipulation of Ubiquitination in Cervical Cancer
FBXO45-Mediated Wnt Pathway Activation in Ovarian Cancer
Research Reagent Solutions Toolkit
Table 3: Essential Research Reagents for Ubiquitination Studies in Gynecological Cancers
| Reagent/Category | Specific Examples | Research Application | Experimental Context |
|---|---|---|---|
| Cell Lines | A2780, HEY, OVCAR-3 | In vitro functional studies | Ovarian cancer models [125] [124] |
| Antibodies | FBXO45, WNT1, β-catenin, c-Myc, GAPDH | Protein detection, pathway analysis | Western blot, immunohistochemistry [125] |
| Molecular Biology Kits | RNAiso Reagent, Real-time qPCR kits, RNA Reverse Transcription Kits | Gene expression analysis | Quantifying ubiquitination-related genes [125] |
| Transfection Reagents | Lipo2000, Lipo8000 | Gene manipulation | Overexpression/knockdown studies [125] |
| Proteasome Inhibitors | Bortezomib, MG132 | UPS functional studies | Validating ubiquitin-mediated degradation [124] |
| Database Resources | TCGA, GTEx, UUCD | Bioinformatic analyses | Prognostic model development [125] [37] |
The comparative analysis of ubiquitination pathways in ovarian and cervical cancers reveals both shared and distinct mechanisms that drive pathogenesis and therapeutic responses. Cervical cancer demonstrates viral hijacking of ubiquitination machinery through HPV E6/E7 oncoproteins, predominantly targeting p53 and pRb tumor suppressors. In contrast, ovarian cancer exhibits more heterogeneous ubiquitination alterations, including hereditary mutations in BRCA1, recurrent repression of UBB, and oncogenic activation through ligases like FBXO45.
These molecular differences translate to divergent therapeutic opportunities. Cervical cancer management may benefit from strategies that disrupt HPV E6/E6AP interactions or employ PROTACs against viral oncoproteins. Ovarian cancer treatment continues to advance through PARP inhibitors, UBC-targeting approaches in UBB-repressed tumors, and combinations of ubiquitinase/DUB inhibitors with immunotherapy.
Future research directions should prioritize comprehensive mapping of ubiquitination networks in both cancer types, development of more selective E3 ligase modulators, and clinical validation of synthetic lethal approaches. Additionally, investigating the interplay between ubiquitination and other post-translational modifications may reveal novel regulatory nodes. As our understanding of ubiquitination pathways in gynecological cancers deepens, so too will opportunities for precision medicine approaches that transform patient outcomes through targeting of these fundamental regulatory mechanisms.
The ubiquitin-proteasome system (UPS) is a crucial post-translational modification pathway that regulates protein stability and function in eukaryotic cells [130] [43]. This sophisticated system involves a sequential enzymatic cascade comprising ubiquitin-activating enzymes (E1), ubiquitin-conjugating enzymes (E2), and ubiquitin ligases (E3), which work in concert to attach ubiquitin molecules to target proteins [130] [131]. The human genome encodes approximately 600-700 E3 ligases and 100 deubiquitinating enzymes (DUBs), which confer substrate specificity and determine the functional outcomes of ubiquitination [130] [132] [133]. Depending on the linkage type and ubiquitin chain topology, ubiquitination can target proteins for proteasomal degradation, alter their subcellular localization, modulate enzymatic activity, or affect protein-protein interactions [43]. The dysregulation of ubiquitinating and deubiquitinating enzymes is a hallmark of various cancers, underscoring the imperative to investigate ubiquitin ligases and deubiquitinases for insights into oncogenic processes and the development of therapeutic interventions [43].
This review provides a comparative analysis of ubiquitination pathways across three distinct solid tumors: lung cancer, esophageal squamous cell carcinoma (ESCC), and melanoma. By examining the unique and shared characteristics of ubiquitination dysregulation in these malignancies, we aim to identify cancer-type-specific vulnerabilities and therapeutic opportunities that could inform drug development strategies.
Ubiquitination Mechanisms and Functional Diversity
The ubiquitination process represents a sophisticated protein modification system that regulates virtually all cellular processes. The enzymatic cascade begins with E1 activating ubiquitin in an ATP-dependent manner, followed by transfer to E2, and finally E3 mediates the attachment of ubiquitin to specific substrate proteins [130] [131]. The remarkable diversity of E3 ligases (approximately 600-700 in humans) ensures precise substrate recognition, while DUBs provide the counterbalancing activity to remove ubiquitin modifications [130] [133].
Ubiquitination manifests in various forms, each with distinct functional consequences. Monoubiquitination involves attachment of a single ubiquitin molecule and typically regulates protein trafficking, histone modification, and DNA repair [43]. Multi-monoubiquitination occurs when multiple single ubiquitin molecules attach to different lysine residues on the same substrate. Polyubiquitination involves chains of ubiquitin molecules linked through specific lysine residues, with K48-linked chains primarily targeting proteins for proteasomal degradation, and K63-linked chains facilitating non-proteolytic functions including signal transduction, DNA repair, and inflammation [130] [43]. More recently, linear ubiquitination (M1-linked) has been recognized as a crucial regulator of NF-κB signaling and immune responses [43].
The following diagram illustrates the core ubiquitination machinery and its functional diversity in cancer contexts:
Figure 1: The ubiquitination machinery and its functional diversity in cancer. The E1-E2-E3 enzymatic cascade conjugates ubiquitin to target proteins, with different ubiquitin chain linkages determining functional outcomes. DUBs reverse these modifications. In cancer, dysregulation of this system can lead to oncoprotein stabilization or tumor suppressor degradation.
Comparative Analysis of Ubiquitination Across Cancer Types
Lung Cancer
Lung cancer represents the leading cause of cancer-related mortality worldwide, with non-small cell lung cancer (NSCLC) accounting for approximately 85% of cases and small cell lung cancer (SCLC) comprising the remaining 15% [130]. The ubiquitin system contributes significantly to lung cancer pathogenesis through regulation of critical signaling pathways including EGFR/Ras/PI3K, Rb/p53, and apoptotic pathways [130]. In NSCLC, mutations in KRAS disrupt ubiquitination pathways that normally regulate KRAS protein stability, leading to prolonged oncogenic signaling [25]. Additionally, the MDM2/MDMX complex functions as the primary E3 ubiquitin ligase for p53, and dysregulation of this pathway in NSCLC results in decreased p53 levels, enhanced cell proliferation, and survival [25].
Recent studies have identified specific ubiquitination-related genes with prognostic significance in lung adenocarcinoma (LUAD). A ubiquitination-related risk score (URRS) developed from TCGA-LUAD data incorporates four genes: DTL, UBE2S, CISH, and STC1 [25]. Patients with high URRS demonstrate worse prognosis (HR=0.54, 95% CI: 0.39-0.73, p<0.001), higher PD-1/PD-L1 expression, increased tumor mutation burden, and enhanced tumor microenvironment scores [25]. These findings highlight the potential of ubiquitination-based signatures as biomarkers for prognosis and treatment response prediction in lung cancer.
Esophageal Squamous Cell Carcinoma
ESCC accounts for approximately 90% of esophageal cancer cases worldwide, with a particularly high prevalence in the "esophageal cancer belt" extending from northern China to the Middle East [134]. Despite advances in diagnosis and treatment, the 5-year survival rate for ESCC patients remains below 20%, necessitating the identification of novel biomarkers and therapeutic targets [134].
A comprehensive analysis of ubiquitination-related differentially expressed genes (URDEGs) in ESCC identified 85 URDEGs, with five key genes (BUB1B, CHEK1, DNMT1, IRAK1, and PRKDC) demonstrating significant prognostic value [134]. These genes play crucial roles in essential cellular processes including cell cycle regulation and immune response. Functional enrichment analysis revealed that these URDEGs are involved in critical pathways such as the cell cycle, DNA replication, and p53 signaling pathway [134].
The GPR37-ATP1A1 axis represents a particularly promising therapeutic target in ESCC. GPR37 interacts with ATP1A1 protein to promote its ubiquitination-induced degradation, thereby limiting activation of the AKT/mTOR signaling pathway [135]. GPR37 is frequently downregulated in ESCC, especially in radioresistant tumors, and its insufficiency correlates with malignant characteristics and unfavorable prognosis [135]. These findings position the ubiquitination system as a valuable source of biomarkers and therapeutic targets in ESCC.
Melanoma
Melanoma ranks among the most aggressive skin cancers, with fiercely increasing incidence and mortality rates worldwide [132]. Despite remarkable advances in targeted therapy and immunotherapy, the prognosis for melanoma patients, particularly those with distant metastasis, remains poor with a 5-year survival rate of approximately 27% for advanced disease [136].
The ubiquitination system contributes significantly to melanoma pathogenesis through regulation of key driver mutations and signaling pathways. BRAF mutations, particularly the V600E substitution, occur in approximately 50% of melanomas, leading to constitutive activation of the MAPK pathway [132] [136]. NRAS mutations are found in about 25% of melanoma cases and represent another crucial oncogenic driver [136]. Ubiquitination regulates the stability and activity of these and other critical factors in melanoma progression.
Several DUBs have been implicated in melanoma pathogenesis. USP4 is significantly elevated in melanoma and plays an oncogenic role by simultaneously inhibiting stress-induced cell apoptosis and promoting tumor metastasis [133]. Additionally, the E3 ligase Parkin can facilitate the ubiquitination of pyruvate kinase M2 (PKM2), while the DUB OTUB2 interacts with PKM2 to inhibit its ubiquitination, thereby enhancing glycolysis and accelerating cancer progression [43]. These findings highlight the complex interplay between ubiquitinating and deubiquitinating enzymes in melanoma metabolism and progression.
Table 1: Comparative Analysis of Ubiquitination Dysregulation in Solid Tumors
| Characteristic | Lung Cancer | Esophageal Squamous Cell Carcinoma | Melanoma |
|---|---|---|---|
| Key Ubiquitination-Related Genes | DTL, UBE2S, CISH, STC1 [25] | BUB1B, CHEK1, DNMT1, IRAK1, PRKDC [134] | USP4, Parkin, OTUB2 [133] [43] |
| Primary Affected Pathways | EGFR/Ras/PI3K, Rb/p53, Apoptosis [130] | Cell cycle, p53 signaling, AKT/mTOR [134] [135] | MAPK, Metabolism (PKM2), Apoptosis [132] [43] |
| Prognostic Biomarkers | URRS signature [25] | 5-gene URDEG signature [134] | USP4 expression [133] |
| Therapeutic Targets | MDM2/MDMX, KRAS ubiquitination [25] | GPR37-ATP1A1 axis [135] | USP4, OTUB2-PKM2 axis [133] [43] |
| Mutation Context | KRAS, p53 pathway [130] [25] | p53 pathway, cell cycle regulators [134] | BRAF (50%), NRAS (25%) [132] [136] |
Experimental Approaches and Methodologies
Proteomic Techniques for Ubiquitination Analysis
Mass spectrometry-based proteomic approaches have revolutionized the identification of ubiquitination sites and ubiquitination events under physiological conditions [132]. Due to the low abundance of ubiquitinated proteins in cells, enrichment strategies are essential for successful identification. The primary approaches include: (1) affinity tags (e.g., His6) engineered at the N-terminus of ubiquitin for purification of tagged ubiquitinated proteins; (2) high-affinity anti-ubiquitin antibodies (P4D1, FK2, FK1) for immunoprecipitation of ubiquitinated proteins, with linkage-specific monoclonal antibodies enabling isolation of chains with specific linkages (K11, K48, K63); and (3) ubiquitin-binding domains (UBDs) that exploit natural ubiquitin interactors for affinity purification [132].
A particularly powerful method involves ubiquitin remnant profiling, where proteins are extracted from cell lysates, digested with trypsin, and ubiquitin remnant-containing peptides are enriched by immunoprecipitation with anti-diglycyl lysine antibodies [132]. This approach leverages the diglycine remnant as an epitope for recognition of ubiquitinated proteins and has enabled the identification of over 20,000 ubiquitination sites in mammalian cell lines, greatly improving the efficiency of ubiquitination event identification at a proteome-wide level [132].
Bioinformatic Analysis of Ubiquitination-Related Genes
Bioinformatic approaches have been instrumental in identifying ubiquitination-related gene signatures with prognostic significance. A typical workflow includes: (1) collection of ubiquitination-related genes from databases such as iUUCD 2.0 and GeneCards; (2) identification of differentially expressed URGs using datasets from TCGA and GEO; (3) consensus clustering to identify molecular subtypes based on URG expression; (4) survival analysis to evaluate prognostic significance; and (5) functional enrichment analysis using GO and KEGG databases to understand biological implications [134] [25].
For prognostic model development, machine learning approaches such as Random Survival Forests and LASSO Cox regression are employed to identify the most predictive gene subsets [25]. These models are subsequently validated in external cohorts to ensure generalizability. The resulting risk scores can stratify patients into distinct prognostic groups and inform therapeutic decisions.
The following experimental workflow illustrates a typical pipeline for ubiquitination-focused cancer research:
Figure 2: Experimental workflow for ubiquitination-focused cancer research. The integrated approach combines mass spectrometry-based proteomics with genomic data mining to identify key ubiquitination-related targets, which are subsequently validated functionally for clinical application.
The Scientist's Toolkit: Essential Research Reagents
Table 2: Essential Research Reagents for Ubiquitination Studies in Cancer
| Reagent Category | Specific Examples | Research Applications |
|---|---|---|
| Ubiquitin Enrichment Tools | His6-tagged ubiquitin, Linkage-specific antibodies (K11, K48, K63), Anti-diglycine remnant antibodies [132] | Isolation and detection of ubiquitinated proteins; mapping ubiquitination sites |
| Proteomic Platforms | Mass spectrometry with ubiquitin remnant profiling, TMT labeling, SILAC [132] | Quantitative ubiquitinome analysis; identification of ubiquitination dynamics |
| Database Resources | iUUCD 2.0, GeneCards, TCGA, GEO [134] [25] | Collection of ubiquitination-related genes; analysis of differential expression |
| Bioinformatic Tools | Limma R package, ConsensusClusterPlus, Survival analysis, GSEA [134] [25] | Identification of URDEGs; molecular subtyping; prognostic modeling |
| Functional Validation Reagents | siRNA/shRNA libraries, E3 ligase/DUB expression constructs, Ubiquitin mutants (K48R, K63R) [135] | Target validation; mechanistic studies of ubiquitination pathways |
Therapeutic Implications and Future Directions
The ubiquitin system presents promising therapeutic opportunities across lung cancer, ESCC, and melanoma. Several strategic approaches have emerged:
PROTACs (Proteolysis-Targeting Chimeras) represent a revolutionary therapeutic modality that hijacks the ubiquitin system to selectively degrade target proteins [43] [131]. These bifunctional molecules simultaneously bind to an E3 ubiquitin ligase and a protein of interest, facilitating ubiquitination and degradation of the target. ARV-110 and ARV-471 are pioneering PROTACs that have progressed to phase II clinical trials, demonstrating the clinical viability of this approach [43].
Molecular Glues constitute another innovative strategy that induces or stabilizes interactions between E3 ligases and target proteins, leading to selective degradation [43]. Compared to PROTACs, molecular glues typically have smaller molecular dimensions, simplifying optimization of their pharmacological properties. CC-90009 represents a prominent example that facilitates GSPT1 degradation by recruiting the CRL4CRBN E3 ligase complex and is currently in phase II trials for leukemia [43].
Small Molecule Inhibitors targeting specific components of the ubiquitin system continue to show therapeutic promise. For instance, indomethacin has been found to diminish growth and recurrence of ESCC by enhancing SYVN1-mediated ubiquitination of ITGAV [43]. Similarly, honokiol directly interacts with KRT18 to induce its ubiquitination and degradation in melanoma models [43].
The comparative analysis presented in this review reveals both shared and cancer-type-specific vulnerabilities in the ubiquitin system. While certain pathways such as p53 regulation emerge as important across multiple cancers, tissue-specific contexts significantly influence the functional consequences of ubiquitination dysregulation. These insights highlight the necessity for precision medicine approaches that account for the unique ubiquitination landscape of each cancer type and individual tumor.
Future research directions should focus on expanding our understanding of the ubiquitin code in cancer contexts, developing more selective modulators of ubiquitin pathway components, and identifying predictive biomarkers that can guide patient selection for ubiquitin-targeted therapies. As our knowledge of ubiquitination in cancer continues to evolve, so too will the opportunities for therapeutic intervention across the spectrum of solid tumors.
The ubiquitin-proteasome system (UPS) represents a sophisticated enzymatic cascade that governs protein degradation and function, serving as a critical regulatory mechanism in cellular homeostasis. This system involves a sequential three-step process catalyzed by ubiquitin-activating enzymes (E1), ubiquitin-conjugating enzymes (E2), and ubiquitin ligases (E3), which collectively tag substrate proteins for proteasomal degradation or functional modification [137] [34]. The specificity of this process is primarily determined by E3 ligases, with approximately 500-1,000 human E3 ligases identified, providing remarkable substrate selectivity [137] [138]. Beyond its fundamental role in protein turnover, ubiquitination regulates diverse cellular processes including cell cycle progression, DNA repair, immune response, and metabolic pathways [137] [34]. Dysregulation of ubiquitination pathways is increasingly recognized as a hallmark of cancer pathogenesis, creating opportunities for therapeutic intervention across multiple cancer types [24] [38]. This comparative analysis examines current approaches for validating therapeutic targets within ubiquitination pathways, evaluating preclinical models, and translating these findings into clinical applications.
Comparative Analysis of Ubiquitination-Targeting Modalities
Table 1: Therapeutic Approaches Targeting Ubiquitination Pathways
| Therapeutic Class | Representative Agents | Molecular Target | Development Status | Cancer Types | Key Limitations |
|---|---|---|---|---|---|
| Proteasome Inhibitors | Bortezomib, Carfilzomib | 20S proteasome | FDA-approved | Multiple myeloma, Mantle cell lymphoma | Resistance development, Neuropathy [137] |
| E1 Enzyme Inhibitors | MLN7243 | UBA1 | Phase I/II trials | Solid tumors | Lack of specificity [137] |
| E2 Enzyme Inhibitors | CC0651, Leucettamol A | Cdc34, Ubc13-Uev1A | Preclinical | N/A | Limited clinical development [137] |
| E3 Ligase Modulators | Thalidomide derivatives, Nutlin-3a | CRBN, MDM2 | FDA-approved to Phase I | Multiple myeloma, Various cancers | Specificity concerns [137] |
| DUB Inhibitors | LCL161, SIM0501 | IAP, USP1 | FDA-approved to Clinical trials | Multiple myeloma, Advanced solid tumors | Early-stage development [34] |
| Ubiquitination Pathway Signatures | URPS | Multiple ubiquitination enzymes | Preclinical validation | Pancancer (lung, esophageal, cervical, urothelial, melanoma) | Prognostic not therapeutic [24] |
Table 2: Comparison of Target Validation Methodologies
| Validation Method | Key Features | Throughput | Clinical Predictive Value | Key Applications |
|---|---|---|---|---|
| Tensor Factorization (Rosalind) | Heterogeneous knowledge graph construction with relational inference | High | 75% recall for clinical trial successes at rank 200 [139] | Prioritizing therapeutic targets across diseases |
| TULIP2 Methodology | Direct identification of E3-specific ubiquitination substrates | Medium | Enables substrate discovery for E3 ligases [140] | Identifying novel E3 ligase substrates (e.g., BRCA1/BARD1-PCNA) |
| Patient-Derived in vitro Assays | Functional testing in disease-relevant cellular contexts | Low-medium | 5 promising RA targets identified in experimental screen [139] | Functional validation of computational predictions |
| Pancancer Ubiquitination Analysis | Integrated analysis of 4,709 patients across 26 cohorts | High | URPS predicts immunotherapy response [24] | Identifying conserved ubiquitination signatures across cancers |
| Immune Infiltration Correlation | Analysis of tumor microenvironment interactions | Medium | UBE2T correlates with immune cell infiltration and checkpoint expression [38] | Immunotherapy target identification |
Experimental Platforms for Target Validation
Computational Prediction Methods
Advanced computational approaches have revolutionized therapeutic target identification by integrating heterogeneous biological data. The Rosalind platform employs tensor factorization on knowledge graphs containing disease-gene-protein relationships, literature evidence, and clinical trial data to prioritize therapeutic targets [139]. This method demonstrates a 18-50% performance increase over comparable algorithms and achieves 75% recall for clinical trial successes at rank 200 [139]. When applied to rheumatoid arthritis, Rosalind identified 55 top-ranked targets for experimental validation, resulting in the discovery of several promising targets including MYLK, previously unexplored in this disease context [139]. The platform's time-slicing validation, training on data up to specific year thresholds and testing on subsequent discoveries, confirms its predictive capability for novel target identification.
Direct Substrate Identification Technologies
The TULIP2 (Targets of Ubiquitin Ligases Identified by Proteomics) methodology enables direct identification of E3-specific ubiquitination substrates through innovative experimental design [140]. This approach utilizes linear fusions between E3 ligases and ubiquitin, allowing the E3 to modify substrate proteins with its fused ubiquitin moiety. Following modification, substrates are co-purified with the E3-ubiquitin fusion and identified via mass spectrometry-based proteomics [140]. Control experiments with catalytically inactive E3 mutants (e.g., BRCA1-I26A) or ubiquitin lacking the C-terminal diGly motif (ΔGG) ensure specificity of substrate identification. Application of TULIP2 to BRCA1/BARD1 revealed PCNA as a novel ubiquitination substrate in unperturbed conditions, independently of RAD18, providing insights into BRCA1/BARD1's role in promoting continuous DNA synthesis and maintaining genome stability [140].
Functional Validation in Disease Models
Patient-derived in vitro assays provide crucial functional validation of computational predictions. In one representative study, Fibroblast-like synoviocytes (FLSs) from rheumatoid arthritis patients were used to test 55 top-ranked targets identified by computational prioritization [139]. This approach identified several promising targets capable of inactivating FLSs, including MYLK with no prior association to RA, demonstrating the value of combining computational prediction with disease-relevant functional assays. The success rate of this approach was comparable to similar assays testing established targets, confirming the predictive value of the computational prioritization [139].
Diagram 1: Computational Target Validation Workflow. The process integrates diverse data sources through knowledge graphs and tensor factorization to prioritize targets for experimental validation.
Key Ubiquitination Targets in Cancer Therapy
Pancancer Ubiquitination Signatures
Comprehensive analysis of ubiquitination pathways across multiple cancer types reveals conserved regulatory networks with prognostic and therapeutic implications. Integration of data from 4,709 patients across 26 cohorts spanning five solid tumors (lung cancer, esophageal cancer, cervical cancer, urothelial cancer, and melanoma) identified a conserved ubiquitination-related prognostic signature (URPS) that effectively stratifies patients into distinct risk categories [24]. The URPS signature demonstrates value in predicting immunotherapy response, with potential for identifying patients most likely to benefit from immune checkpoint inhibitors [24]. At the molecular level, the OTUB1-TRIM28 ubiquitination axis was found to modulate MYC pathway activity and influence patient prognosis, revealing a strategy for targeting traditionally "undruggable" oncogenes like MYC through their ubiquitination regulators [24].
UBE2T as a Pancancer Biomarker
Ubiquitin-conjugating enzyme 2T (UBE2T) emerges as a significant biomarker and potential therapeutic target across multiple cancer types. Comprehensive pancancer analysis reveals elevated UBE2T expression in various malignancies compared to adjacent normal tissues, with upregulation associated with poor clinical outcomes [38]. Genetic alteration analysis identifies amplification as the predominant UBE2T alteration across cancers, followed by mutations [38]. Functionally, UBE2T expression correlates with key oncogenic processes including proliferation, invasion, and epithelial-mesenchymal transition. Pathway enrichment analyses implicate cell cycle regulation, ubiquitin-mediated proteolysis, p53 signaling, and mismatch repair as mechanisms through which UBE2T exerts its oncogenic effects [38]. Additionally, UBE2T expression demonstrates significant association with tumor immune markers, checkpoint genes, and immune cell infiltration, suggesting potential relevance for immunotherapy approaches [38].
Diagram 2: UBE2T Oncogenic Signaling Network. UBE2T overexpression influences multiple cancer-relevant pathways culminating in disease progression.
BRCA1/BARD1 Ubiquitin E3 Ligase Activity
The BRCA1/BARD1 heterodimer represents a paradigmatic example of ubiquitin E3 ligase function in cancer pathogenesis and therapy. While initially controversial, recent research demonstrates that BRCA1/BARD1 ubiquitin E3 activity is dispensable for homologous recombination repair and resistance to PARP inhibitors like Olaparib [140]. Advanced substrate identification techniques reveal that BRCA1/BARD1 constitutively ubiquitinates PCNA independently of RAD18, facilitating continuous DNA synthesis and preventing ssDNA gap formation during replication [140]. This function provides insights into BRCA1's role in maintaining genome stability beyond its established functions in DNA repair. The evolving understanding of BRCA1/BARD1 substrates highlights the complexity of ubiquitin signaling in cancer and the importance of comprehensive substrate identification for therapeutic development.
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Research Reagents for Ubiquitination Studies
| Reagent Category | Specific Examples | Research Applications | Key Features |
|---|---|---|---|
| E3 Ligase Expression Constructs | BRCA1/BARD1-TULIP2 fusions, BRCA1-I26A mutant | Direct substrate identification | Catalytically active and inactive variants for control experiments [140] |
| Proteasome Inhibitors | Bortezomib, Carfilzomib, MG132 | UPS function studies | Reversible vs. irreversible inhibition; different binding specificities [137] |
| DUB Inhibitors | LCL161 (IAP inhibitor), SIM0501 (USP1 inhibitor) | Deubiquitination pathway analysis | Specificity for different DUB subfamilies [34] |
| Ubiquitin Binding Probes | Tandem Ubiquitin Binding Entities (TUBEs), DiGly antibody | Ubiquitinated protein enrichment | Affinity purification of ubiquitinated substrates [140] |
| Immune Checkpoint Antibodies | Anti-PD-1, Anti-PD-L1 | Immunotherapy interaction studies | Blockade of ubiquitination-mediated checkpoint regulation [138] |
| Pathway Reporter Systems | SMAD-responsive luciferase, MYC activity reporters | Signaling pathway validation | Readouts for ubiquitination pathway activity [24] [141] |
The validation of therapeutic targets within ubiquitination pathways presents both significant opportunities and challenges for cancer drug development. While numerous targets have been identified through computational and experimental approaches, translation to clinical success requires careful consideration of biological complexity, pathway redundancy, and therapeutic window. The integration of pancancer analyses revealing conserved ubiquitination signatures with advanced substrate identification methodologies provides a powerful framework for prioritizing the most promising therapeutic targets. Future directions will likely focus on developing more specific inhibitors targeting E3 ligases and deubiquitinating enzymes, combining ubiquitination-targeting agents with established therapies, and leveraging ubiquitination signatures for patient stratification in clinical trials. As our understanding of ubiquitination pathway complexity deepens, so too will our ability to strategically target these pathways for therapeutic benefit across diverse cancer types.
Conclusion
This comparative analysis underscores ubiquitination as a master regulatory system whose dysregulation presents common yet context-specific vulnerabilities across cancer types. The integration of advanced proteomic methodologies with computational network modeling has enabled the construction of comprehensive ubiquitination maps, revealing both pan-cancer mechanisms and tissue-specific alterations. Validated ubiquitination-related gene signatures demonstrate robust prognostic value across diverse malignancies, while emerging therapeutic strategies—including PROTACs, E3 ligase modulators, and combination therapies with immunotherapy—show immense potential for precision oncology. Future research must focus on elucidating the complex crosstalk between ubiquitination and other post-translational modifications, developing more specific ubiquitination pathway inhibitors, and advancing single-cell ubiquitinome technologies to fully exploit this critical regulatory axis for cancer diagnosis and treatment.
References
- 1. Frontiers | Identification and validation of ubiquitination -related genes... [https://www.frontiersin.org/journals/genetics/articles/10.3389/fgene.2025.1578075/full]
- 2. : Ubiquitin , Ligases , and Regulation Structure Function [https://pubmed.ncbi.nlm.nih.gov/28375744/]
- 3. The roles of E3 ubiquitin ligases in cancer progression and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9991012/]
- 4. Ubiquitin binding domains — from structures to functions - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC7359374/]
- 5. The role of E3 ubiquitin ligases in the development and ... [https://www.nature.com/articles/s41418-020-00696-6]
- 6. M-CSA - A database of enzyme mechanisms and catalytic sites [https://www.ebi.ac.uk/thornton-srv/m-csa/entry/939/]
- 7. Understanding specificity within the ubiquitin /UBL cascade | MRC PPU [https://www.ppu.mrc.ac.uk/lectures/paul-elliott-0]
- 8. and Ubiquitin -like proteins in HPV-driven carcinogenesis ubiquitin [https://www.nature.com/articles/s41388-025-03310-6?error=cookies_not_supported]
- 9. An enzymatic cascade enables sensitive and specific ... [https://www.nature.com/articles/s41467-025-65405-8]
- 10. The ubiquitin system: from cell signalling to disease ... [https://www.nature.com/articles/s41418-020-00703-w]
- 11. Mechanisms of mono- and poly - ubiquitination : Ubiquitination ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC2927562/]
- 12. Ubiquitin and Ubiquitin-Like Protein Resources [https://www.cellsignal.com/pathways/by-research-area/ubiquitin-protein-resources-pathways?srsltid=AfmBOoqfYMDRALfRqVqF1ulXGfTEgCAybCyUcae1XX5SQmvJplIPvzhE]
- 13. UbiHub: a data hub for the explorers of ubiquitination pathways [https://pmc.ncbi.nlm.nih.gov/articles/PMC6691330/]
- 14. Decoding the ubiquitin network: molecular mechanisms and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12492556/]
- 15. Function and Variety | News-Medical Ubiquitin [https://www.news-medical.net/life-sciences/Ubiquitin-Function-and-Variety.aspx]
- 16. The prokaryotic antecedents of the ubiquitin - signaling system and the... [https://genomebiology.biomedcentral.com/articles/10.1186/gb-2006-7-7-r60]
- 17. A comprehensive platform for the analysis of ubiquitin -like protein... [https://www.nature.com/articles/srep40756?error=cookies_not_supported]
- 18. ubiquitin signaling restricts heterochromatin spread [https://www.nature.com/articles/s41392-025-02349-x]
- 19. Comprehensive pan-cancer analysis reveals ubiquitin ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12402753/]
- 20. Comprehensive pan‑ cancer analysis reveals ubiquitin ‑conjugating... [https://www.spandidos-publications.com/10.3892/ol.2025.15237?text=fulltext]
- 21. Frontiers | Multi-omics analysis identifies UBA family as potential... [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2025.1510503/full]
- 22. An integrative pan-cancer analysis of USP37 and ... [https://www.frontiersin.org/journals/cell-and-developmental-biology/articles/10.3389/fcell.2025.1659747/full]
- 23. Multi-omics analysis of core E3 ubiquitin ligase identifies prognostic... [https://www.jcancer.org/v16p1363.htm]
- 24. Constructing a pancancer ubiquitination regulatory network to ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12382526/]
- 25. Construction of ubiquitination-related risk model for ... [https://www.nature.com/articles/s41598-025-92177-4]
- 26. Frequent mutations in acetylation and ubiquitination sites suggest... [https://genomemedicine.biomedcentral.com/articles/10.1186/s13073-016-0311-2]
- 27. Visualization analysis of breast cancer-related ubiquitination ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11958930/]
- 28. Ubiquitin-specific proteases as key regulators in the ... [https://link.springer.com/article/10.1007/s12672-025-04103-9]
- 29. Construction of ubiquitination -related risk model for predicting... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11973225/]
- 30. The Clinical Prediction Value of the Ubiquitination Model ... [https://www.jcancer.org/v16p0784.htm]
- 31. Integrative analysis of ubiquitination-related genes identifies ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11922989/]
- 32. USP21/YBX1/HIF1-α promotes the progression of prostate ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12548149/]
- 33. Frontiers | KCTD10 inhibits lung metastasis and angiogenesis... cancer [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2025.1630311/full]
- 34. The role of ubiquitination and deubiquitination in cancer ... [https://www.frontiersin.org/journals/oncology/articles/10.3389/fonc.2025.1464914/full]
- 35. The advancement of ubiquitination regulation in apoptosis ... [https://www.sciencedirect.com/science/article/abs/pii/S0003986125002103]
- 36. in Ubiquitination : mechanisms and therapeutic opportunities cancer [https://pubmed.ncbi.nlm.nih.gov/40537889/]
- 37. Frontiers | Prognostic model of ubiquitination -related genes in ovarian... [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2025.1654180/full]
- 38. Comprehensive pan‑cancer analysis reveals ubiquitin ... [https://www.spandidos-publications.com/10.3892/ol.2025.15237]
- 39. -conjugating enzyme E2S serves as a prognostic marker for... Ubiquitin [https://tcr.amegroups.org/article/view/108712/html]
- 40. Metabolic Reprogramming of Cancer Cells and Therapeutics ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12439291/]
- 41. Current methodologies in protein ubiquitination characterization [https://cellandbioscience.biomedcentral.com/articles/10.1186/s13578-022-00870-y]
- 42. Integrated Genomic Analysis of the Ubiquitin Pathway across ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5916807/]
- 43. Ubiquitination and deubiquitination in cancer [https://molecular-cancer.biomedcentral.com/articles/10.1186/s12943-024-02046-3]
- 44. Dissecting the ubiquitin pathway by mass spectrometry - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC1828906/]
- 45. Proteome and Ubiquitinome Analyses Reveal the ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12413316/]
- 46. Proteomic Analyses Reveal Divergent Ubiquitylation Site ... [https://www.sciencedirect.com/science/article/pii/S153594762033454X]
- 47. Comprehensive mapping of ubiquitination | Nature Methods [https://www.nature.com/articles/s41592-018-0122-z]
- 48. Systematic Comparison of Strategies for the Enrichment ... [https://pubmed.ncbi.nlm.nih.gov/31738065/]
- 49. Current methodologies in protein ubiquitination ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9373315/]
- 50. The ubiquitin code of RAS proteins: Decoding its role in ... [https://www.sciencedirect.com/science/article/pii/S2589004225012908]
- 51. Comparison of affinity tags for protein purification [https://www.sciencedirect.com/science/article/abs/pii/S1046592805000276]
- 52. Benefits of Strep-tag® vs His-tag purification [https://www.iba-lifesciences.com/strep-tag-vs-his-tag]
- 53. Overview of Affinity Tags for Protein Purification - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC4527311/]
- 54. 3 Small Peptide Tags for Affinity Protein Purification [https://www.goldbio.com/blogs/articles/3-small-peptide-tags-for-affinity-protein-purification?srsltid=AfmBOorQ6zw4piLQZWl5y5tIyEzp0CLQe_mNK6D3B0KEzxhXpryjo3Sg]
- 55. A comprehensive method for detecting ubiquitinated ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4403176/]
- 56. Ubiquitin modifications | Cell Research [https://www.nature.com/articles/cr201639]
- 57. The Molecular Toolbox for Linkage Type‐Specific Analysis ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12118340/]
- 58. Ubiquitin Chain Editing Revealed by Polyubiquitin Linkage ... [https://www.sciencedirect.com/science/article/pii/S0092867408009598]
- 59. Secondary interactions in ubiquitin-binding domains achieve ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11372445/]
- 60. Using the Ubiquitin-modified Proteome to Monitor Protein ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3861705/]
- 61. - Integrating data reveals function and therapeutic... multi omics [https://elifesciences.org/articles/72879]
- 62. Multi-omic network inference from time-series data [https://www.nature.com/articles/s41540-025-00591-1]
- 63. approaches for Computational -based network ... integrative [https://pmc.ncbi.nlm.nih.gov/articles/PMC9703081/]
- 64. -based Network - multi analysis omics in drug... integrative methods [https://biodatamining.biomedcentral.com/articles/10.1186/s13040-025-00442-z]
- 65. Single-cell and multi-omics analysis identifies TRIM9 as a ... [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2025.1631708/full]
- 66. Single-cell and multi-omics analysis identifies TRIM9 as a key ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12491318/]
- 67. Multi-omics analysis reveals RNA polymerase II ... [https://www.nature.com/articles/s41420-025-02677-5]
- 68. Gene regulatory network integration with multi-omics data ... [https://pubmed.ncbi.nlm.nih.gov/40619810/]
- 69. Systematic approaches to identify E3 ligase substrates - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC5103871/]
- 70. E3 Ubiquitin Ligases as Cancer Targets and Biomarkers - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC1601942/]
- 71. Screening for E3-Ubiquitin ligase inhibitors - PubMed Central [https://pmc.ncbi.nlm.nih.gov/articles/PMC4226663/]
- 72. BioE3 identifies specific substrates of ubiquitin E3 ligases [https://www.nature.com/articles/s41467-023-43326-8]
- 73. CRISPR-Cas9 screening reveals G2E3 as a novel ... [https://www.nature.com/articles/s41420-025-02717-0]
- 74. Expanding PROTACtable genome universe of E3 ligases [https://www.nature.com/articles/s41467-023-42233-2]
- 75. Review DTX3L E3 ligase: Molecular functions, regulatory ... [https://www.sciencedirect.com/science/article/abs/pii/S0141813025067510]
- 76. The role of ubiquitination in tumorigenesis and targeted ... [https://www.nature.com/articles/s41392-020-0107-0]
- 77. Degradation using the Protein -Proteasome Ubiquitin Pathway [https://www.thermofisher.com/us/en/home/life-science/cell-analysis/cell-analysis-learning-center/protein-degradation-resource-center/protein-degradation-using-ubiquitin-proteasome-pathway.html]
- 78. and Ubiquitin -Like Ubiquitin ... | Cell Signaling Technology Protein [https://www.cellsignal.com/pathways/by-research-area/ubiquitin-protein-resources-pathways]
- 79. Multilayered regulation of proteome stoichiometry - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC8592966/]
- 80. A dynamic ubiquitination balance of cell proliferation and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10936951/]
- 81. Enzymes in Ubiquitination , Cancer Immune Evasion, and... Cancer [https://pubmed.ncbi.nlm.nih.gov/39851497/]
- 82. Frontiers | Integrating multi-omics and experimental techniques to... [https://www.frontiersin.org/journals/pharmacology/articles/10.3389/fphar.2025.1545472/full]
- 83. Ubiquitin Labeling Free Mass Spectrometry Analysis [https://www.mtoz-biolabs.com/ubiquitin-labeling-free-mass-spectrometry-analysis.html]
- 84. Data-independent acquisition method for ubiquitinome ... [https://www.nature.com/articles/s41467-020-20509-1]
- 85. Sensitive and specific affinity purification-mass ... [https://www.sciencedirect.com/science/article/pii/S2667237525002024]
- 86. A Label-free Quantitative Proteomics Strategy to Identify E3 ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC2709196/]
- 87. [Advances in high - throughput analysis] proteomic [https://pubmed.ncbi.nlm.nih.gov/34227342/]
- 88. Deubiquitinase–based analysis of ubiquitin chain ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5011418/]
- 89. Decoding Ubiquitin for Mitosis - PMC - PubMed Central [https://pmc.ncbi.nlm.nih.gov/articles/PMC3636754/]
- 90. Methods to measure ubiquitin chain length and linkage [https://www.sciencedirect.com/science/article/abs/pii/S0076687918305159]
- 91. Targeting the Ubiquitin–Proteasome System for Cancer - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC12495026/]
- 92. The molecular mechanisms of acquired proteasome inhibitor ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3521846/]
- 93. The resistance mechanisms of proteasome inhibitor bortezomib [https://pmc.ncbi.nlm.nih.gov/articles/PMC4177604/]
- 94. Carfilzomib: A Promising Proteasome Inhibitor for the ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8631731/]
- 95. Bortezomib in cancer therapy: Mechanisms, side effects ... [https://www.sciencedirect.com/science/article/pii/S002432052400715X]
- 96. Mechanisms of proteasome inhibitor action and resistance ... [https://www.sciencedirect.com/science/article/abs/pii/S1368764608000472]
- 97. Inhibition of Histone Deacetylases Promotes Ubiquitin ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3361136/]
- 98. Overcoming inherent resistance to histone deacetylase ... [https://www.nature.com/articles/cddis201498]
- 99. Targeted protein degradation: mechanisms, strategies and ... [https://www.nature.com/articles/s41392-022-00966-4]
- 100. PROTACs: A novel strategy for cancer drug discovery and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10227178/]
- 101. E3 ubiquitin ligases in signaling, disease, and therapeutics [https://www.sciencedirect.com/science/article/pii/S0968000425001860]
- 102. Review Molecular glues and PROTACs in targeted protein ... [https://www.sciencedirect.com/science/article/abs/pii/S0006295225005623]
- 103. Design and development of PROTACs: A new paradigm in ... [https://www.sciencedirect.com/science/article/pii/S2590098625000181]
- 104. PROTAC Degraders in Clinical Trails: 2025 Update [https://www.biochempeg.com/article/434.html]
- 105. Recent Advances in the Development of Pro-PROTAC for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12473374/]
- 106. PRosettaC outperforms AlphaFold3 for modeling PROTAC ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12568945/]
- 107. exploring the ubiquitin system for drug development [https://www.nature.com/articles/cr201631]
- 108. Emerging drug development technologies targeting ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7112620/]
- 109. Targeting the ubiquitin system by fragment-based drug ... [https://www.frontiersin.org/journals/molecular-biosciences/articles/10.3389/fmolb.2022.1019636/full]
- 110. Enzymes in Ubiquitination , Cancer Immune Evasion, and... Cancer [https://pmc.ncbi.nlm.nih.gov/articles/PMC11763706/]
- 111. implication and immunotherapy response prediction of... Prognostic [https://pmc.ncbi.nlm.nih.gov/articles/PMC9845272/]
- 112. Identification and validation of a thirteen- gene based on... signature [https://link.springer.com/article/10.1007/s12672-025-02459-6]
- 113. Integrated Single-Cell and Transcriptome Sequencing Analyses... [https://www.imrpress.com/journal/FBL/28/11/10.31083/j.fbl2811304/htm]
- 114. Recent advances in the development of deubiquitinases ... [https://www.sciencedirect.com/science/article/abs/pii/S0223523424000412]
- 115. Involvement of the ubiquitin -proteasome system in the regulation of... [https://pubmed.ncbi.nlm.nih.gov/39759114/]
- 116. Single-cell technology reveals the crosstalk between tumor ... [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2025.1637144/full]
- 117. Single-cell multi-omics in cancer immunotherapy: from tumor ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12376342/]
- 118. Review Paper: Deciphering the Aging Process through Single - cell ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12147454/]
- 119. Frontiers | Imaging flow : from high - cytometry ... resolution [https://www.frontiersin.org/journals/bioengineering-and-biotechnology/articles/10.3389/fbioe.2025.1580749/full]
- 120. Bioinformatics analysis and single - cell RNA sequencing: elucidating... [https://jtd.amegroups.org/article/view/77282/html]
- 121. Frontiers | Single - cell delineates the profiling ... tumor [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2025.1653096/full]
- 122. Assessing Human Treg Suppression at Single - Cell Using... Resolution [https://bio-protocol.org/en/bpdetail?id=5424&type=0]
- 123. Ubiquitin and ubiquitin-like proteins in HPV-driven ... [https://www.nature.com/articles/s41388-025-03310-6]
- 124. Unraveling role of ubiquitination in drug resistance of gynecological... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11162667/]
- 125. Prognostic model of ubiquitination-related genes in ovarian ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12450667/]
- 126. : Key Differences | Acibadem... Cervical Cancer Vs Ovarian Cancer [https://www.acibademhealthpoint.com/cervical-cancer-vs-ovarian-cancer-key-differences/]
- 127. Ubiquitin levels: the next target against gynecological ... [https://www.jci.org/articles/view/98262]
- 128. . Cervical : A Comprehensive Cancer vs Ovarian Cancer Comparison [https://medicalrealities.com/cervical-cancer-vs-ovarian-cancer-a-comprehensive-comparison/]
- 129. Protein ubiquitination in ovarian cancer immunotherapy [https://www.sciencedirect.com/science/article/pii/S2352304223004415]
- 130. The Ubiquitin System: An Emerging Therapeutic Target for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8431782/]
- 131. The roles of protein ubiquitination in tumorigenesis and ... [https://www.frontiersin.org/journals/endocrinology/articles/10.3389/fendo.2023.1220108/full]
- 132. Ubiquitination in melanoma pathogenesis and treatment [https://pmc.ncbi.nlm.nih.gov/articles/PMC5463089/]
- 133. Deubiquitinating enzymes as cancer biomarkers [https://pmc.ncbi.nlm.nih.gov/articles/PMC6476481/]
- 134. Prognostic value of ubiquitination-related differentially ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11635202/]
- 135. GPR37-enhanced ubiquitination of ATP1A1 inhibits tumor ... [https://www.nature.com/articles/s41419-024-07240-1]
- 136. Signal pathways of melanoma and targeted therapy [https://www.nature.com/articles/s41392-021-00827-6]
- 137. Targeting ubiquitination for cancer therapies [https://pmc.ncbi.nlm.nih.gov/articles/PMC4976843/]
- 138. Emerging Role of Ubiquitination in the Regulation of PD-1/ ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7934629/]
- 139. Preclinical validation of therapeutic targets predicted by ... [https://www.nature.com/articles/s41598-020-74922-z]
- 140. BRCA1/BARD1 ubiquitinates PCNA in unperturbed ... [https://www.nature.com/articles/s41467-024-48427-6]
- 141. TGF-β Signaling in Cancer: Mechanisms of Progression and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12347881/]