Decoding the Ubiquitin Code in Cancer: Mechanisms, Therapeutic Targeting, and Clinical Frontiers
The ubiquitin code, a complex system of post-translational modifications, is fundamentally altered in cancer, driving tumorigenesis through dysregulated protein stability, signaling, and cellular homeostasis.
Decoding the Ubiquitin Code in Cancer: Mechanisms, Therapeutic Targeting, and Clinical Frontiers
Abstract
The ubiquitin code, a complex system of post-translational modifications, is fundamentally altered in cancer, driving tumorigenesis through dysregulated protein stability, signaling, and cellular homeostasis. This article synthesizes current research for a scientific audience, exploring how specific alterations in ubiquitin ligases, deubiquitinases, and chain topology contribute to hallmarks of cancer such as metabolic reprogramming, immune evasion, and therapy resistance. We examine foundational concepts of the ubiquitin code, methodological advances in its study, challenges in therapeutic targeting, and emerging preclinical and clinical strategies, including PROTACs and molecular glues, that aim to exploit ubiquitin system vulnerabilities for precision oncology.
The Ubiquitin Code: Foundational Principles and Its Dysregulation in Oncogenesis
The Core Enzymatic Cascade of the UPS
The Ubiquitin-Proteasome System (UPS) is a crucial selective proteolytic system that maintains cellular protein homeostasis by degrading short-lived, misfolded, damaged, and regulatory proteins [1] [2]. This degradation is essential for controlling countless cellular processes, including immune response, apoptosis, cell cycle, differentiation, and signaling [1]. The process involves a hierarchical enzymatic cascade that conjugates the small, highly conserved protein ubiquitin onto substrate proteins, marking them for degradation by the proteasome [1] [3].
The Ubiquitin-Conjugation Cascade The conjugation of ubiquitin to substrate proteins is a three-step enzymatic process [4] [2] [5]:
- Activation (E1): A ubiquitin-activating enzyme (E1) activates ubiquitin in an ATP-dependent manner. The E1 forms a high-energy thioester bond between the C-terminal glycine (Gly76) of ubiquitin and a cysteine residue in its active site [4] [3].
- Conjugation (E2): The activated ubiquitin is transferred from the E1 to the active site cysteine of a ubiquitin-conjugating enzyme (E2), forming an E2-ubiquitin thioester intermediate [4] [3].
- Ligation (E3): A ubiquitin ligase (E3) binds both the E2-ubiquitin complex and the protein substrate, facilitating the final transfer of ubiquitin to a lysine residue on the substrate, forming an isopeptide bond [4]. The E3 ligase provides specificity to the system by recognizing and recruiting target substrates [1].
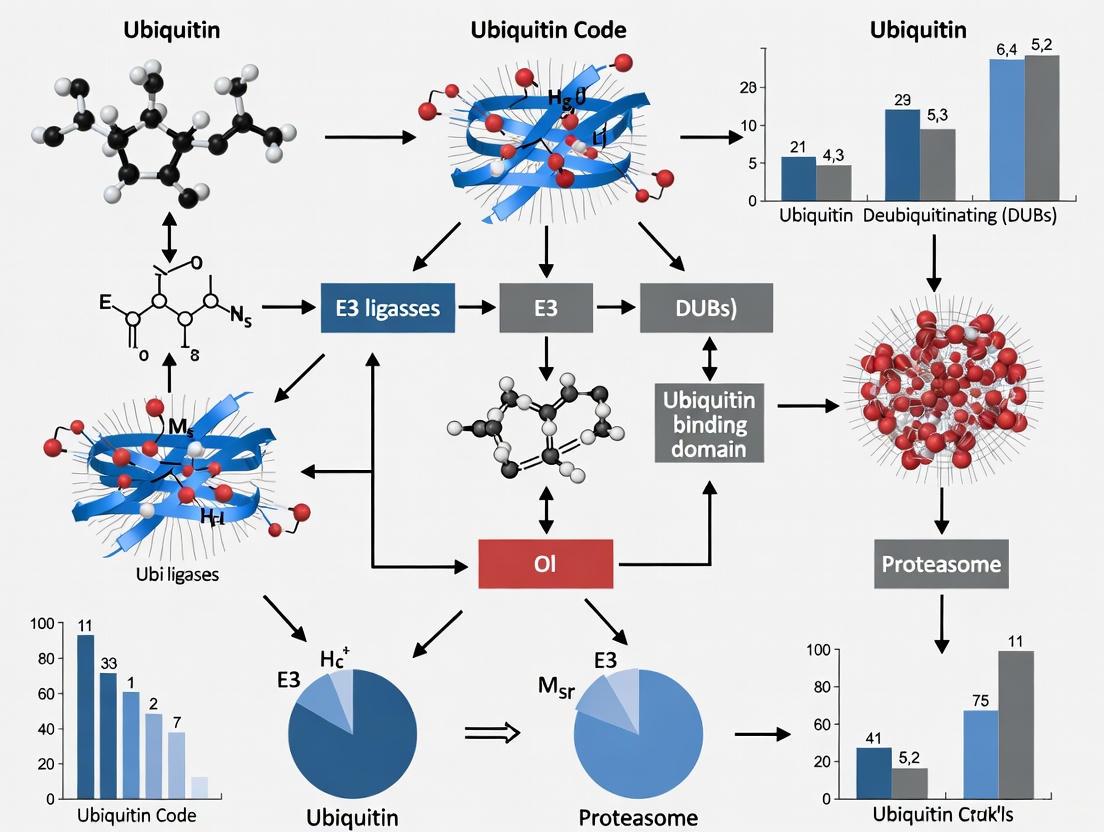
This cascade is visually summarized in the diagram below.
The Complexity of the Ubiquitin Code
Ubiquitination is not a single signal but a diverse post-translational modification that forms a complex "ubiquitin code" [2]. The functional consequences of ubiquitination depend on the type of ubiquitin modification attached to the substrate [4].
Types of Ubiquitin Modifications
- Monoubiquitination: Attachment of a single ubiquitin molecule to a substrate lysine. This modification is typically non-degradative and can regulate protein-protein interactions, protein activity, and subcellular localization [4] [6].
- Multi-Monoubiquitination: Attachment of single ubiquitin molecules to multiple different lysine residues on the same substrate protein [6].
- Polyubiquitination: Formation of a chain of ubiquitin molecules by conjugating additional ubiquitins to one of the seven internal lysine residues (K6, K11, K27, K29, K33, K48, K63) or the N-terminal methionine (M1) of the previously attached ubiquitin [1] [4] [2]. Polyubiquitin chains can be homogenous (composed of a single linkage type), heterogeneous (mixed linkages), or branched (multiple chains on a single ubiquitin) [4] [6]. The topology of the chain determines the fate of the modified protein.
Table 1: Major Ubiquitin Linkage Types and Their Primary Functions
| Linkage Type | Primary Known Function(s) | Proteasomal Degradation |
|---|---|---|
| K48-linked | Major signal for proteasomal degradation [1] | Yes [1] |
| K11-linked | Proteasomal degradation, particularly in ERAD and cell cycle regulation [1] [4] | Yes [1] |
| K29/K48-branched | Potent signal for proteasomal degradation, can overcome DUB protection [7] | Yes [7] |
| K63-linked | DNA damage response, endocytosis, inflammatory signaling; generally non-degradative [1] [4] | No [1] |
| M1-linked (Linear) | NF-κB activation, inflammatory signaling [2] [6] | No |
| K27-linked & K33-linked | Context-dependent roles in immune signaling, autophagy [1] | Context-dependent |
Deubiquitinases (DUBs): Editors of the Ubiquitin Code
The ubiquitin system is dynamic and reversible. Deubiquitinases (DUBs) are proteases that cleave ubiquitin from substrates or disassemble ubiquitin chains, providing an essential editing and regulatory layer to the ubiquitin code [2] [6]. DUBs can counteract E3 ligase activity, rescue proteins from degradation, refine the ubiquitin signal by trimming chains, and recycle ubiquitin to maintain the cellular pool [1]. They are classified into seven families based on their catalytic domains: USP, OTU, MJD, UCH, JAMM, MINDY, and ZUFSP [7] [6]. Some DUBs, like OTULIN, show high specificity for particular linkage types such as M1-linear chains, while others have broader activity [2].
Experimental Analysis of the UPS
Studying the UPS requires specific methodologies to identify substrates, elucidate enzymatic functions, and characterize ubiquitin chain topology.
Key Experimental Workflows
A powerful approach for discovering novel E3 ligase substrates involves combining genetic perturbation (e.g., siRNA knockdown) with quantitative proteomics, as demonstrated in a 2025 study identifying the DUB OTUD5 as a substrate of the E3 ligase TRIP12 [7]. The general workflow for such a discovery pipeline is illustrated below.
The Scientist's Toolkit: Key Research Reagents
Table 2: Essential Reagents for UPS Research
| Reagent / Tool | Function / Application | Key Feature |
|---|---|---|
| Single-Lysine Ubiquitin Mutants (e.g., Ub-K48Only, Ub-K63Only) | Determine the linkage specificity of E3 ligases and DUBs in in vitro assays [7]. | Allows for the formation of homogenous ubiquitin chains of a defined topology. |
| TUBE (Tandem Ubiquitin Binding Entity) | Affinity purification of polyubiquitinated proteins from cell lysates; protects chains from DUBs [7]. | High-affinity, pan-specific ubiquitin chain binder composed of multiple UBA domains. |
| Linkage-Specific Ubiquitin Binders (e.g., GST-TRABID-NZF1 for K29/K33) | Enrich and detect specific ubiquitin chain types from cell lysates or in vitro reactions [7]. | Uses naturally occurring ubiquitin-binding domains (UBDs) with defined linkage preferences. |
| Proteasome Inhibitors (e.g., MG132, Bortezomib) | Block degradation of ubiquitinated proteins, allowing for their accumulation and detection. | Essential for studying endogenous protein ubiquitination levels in cells. |
| PROTACs (PROteolysis TArgeting Chimeras) | Bifunctional molecules that recruit E3 ligases to neosubstrates, inducing their ubiquitination and degradation [1] [4]. | Tool for targeted protein degradation and a promising therapeutic modality. |
UPS Alterations in Cancer and Therapeutic Targeting
Dysregulation of the UPS is a hallmark of cancer, contributing to uncontrolled proliferation, evasion of growth suppressors, and resistance to therapy [4] [6]. E3 ligases and DUBs can function as oncogenes or tumor suppressors, and their mutations or aberrant expression are common in tumors [4].
- Oncoprotein Stabilization & Tumor Suppressor Degradation: Aberrant UPS activity can lead to the hyper-stabilization of oncoproteins (e.g., RAS isoforms via altered ubiquitination [8]) or the accelerated degradation of tumor suppressors like p53 [4].
- Immune Evasion: The UPS regulates immune checkpoint proteins like PD-1/PD-L1. For instance, the DUB USP2 stabilizes PD-1, promoting tumor immune escape, while the E3 ligase AIP4 promotes PD-L1 internalization and degradation, inhibiting immune escape [6].
- Therapeutic Strategies:
- Proteasome Inhibitors: Drugs like Bortezomib inhibit the proteasome broadly, used in hematologic malignancies but with broad effects [1].
- Targeted Protein Degradation (PROTACs): Bifunctional molecules like ARV-110 and ARV-471 re-purpose E3 ligases to selectively degrade disease-driving proteins, offering a more precise therapeutic approach [1] [4] [6].
- E1/E2/E3/DUB Inhibitors: Developing specific inhibitors for individual components of the UPS cascade is an active area of cancer drug discovery [4] [9] [6].
The ubiquitin code represents a sophisticated post-translational signaling system that regulates virtually all aspects of cellular physiology in eukaryotes. This complex language, composed of monoubiquitination and diverse polyubiquitin chain topologies, dictates fundamental processes including protein degradation, DNA repair, immune signaling, and cell cycle progression. When dysregulated, alterations in ubiquitin signaling contribute significantly to oncogenesis, making the ubiquitin system an attractive therapeutic target. This technical review comprehensively examines the mechanisms of ubiquitin chain formation, the structural characteristics of distinct chain topologies, and their functional consequences, with particular emphasis on cancer development. We integrate current experimental methodologies and research tools essential for investigating ubiquitin signaling, providing a foundation for developing novel cancer therapeutics that exploit the ubiquitin code.
Ubiquitination is a crucial post-translational modification involving the covalent attachment of the 76-amino acid protein ubiquitin to substrate proteins. This process regulates nearly all aspects of eukaryotic cell biology, from protein degradation to signal transduction and DNA repair [10]. The modification occurs through a sequential enzymatic cascade involving E1 (activating), E2 (conjugating), and E3 (ligating) enzymes, with E3 ligases providing substrate specificity [11] [12].
The term "ubiquitin code" describes the complex language generated through diverse ubiquitin modifications. This coding capacity arises from several variables: (1) the number of ubiquitin molecules attached (mono- versus polyubiquitination); (2) the specific lysine residues used to connect ubiquitin molecules in chains; (3) chain architecture (homotypic, heterotypic, or branched); and (4) additional modifications to ubiquitin itself, such as phosphorylation or acetylation [10]. This sophisticated system generates an extensive repertoire of biological signals that determine cellular outcomes, with particular relevance to cancer development where ubiquitin signaling pathways are frequently dysregulated [11] [13].
Monoubiquitination: Mechanisms and Functional Outcomes
Definition and Molecular Mechanisms
Monoubiquitination refers to the attachment of a single ubiquitin molecule to a substrate protein, typically occurring on lysine residues but also possible on serine, threonine, or cysteine residues [11] [14]. This modification differs fundamentally from polyubiquitination in both structure and function. While historically overshadowed by the more extensively studied degradative polyubiquitination, monoubiquitination has emerged as a critical regulator of non-proteolytic cellular processes.
The mechanism of monoubiquitination involves the same E1-E2-E3 enzymatic cascade but is often determined by specific E2/E3 combinations that favor single ubiquitin transfer. Research on the SCF(^{Cdc4})/Cdc34 complex in yeast demonstrated that point mutations in the catalytic core of the Cdc34 E2 enzyme can convert it from a polyubiquitinating enzyme into a monoubiquitinating enzyme, highlighting how subtle structural determinants direct the mode of ubiquitination [15]. This specificity arises from amino acid determinants in the E2 catalytic region and their compatibility with residues surrounding acceptor lysines in substrates [15].
Biological Functions and Cancer Relevance
Monoubiquitination regulates diverse cellular processes through non-proteolytic mechanisms:
Membrane Trafficking and Endocytosis: Monoubiquitination of cell surface receptors targets them for internalization and subsequent lysosomal degradation, providing a mechanism for signal termination [14]. This process is hijacked in cancer to downregulate tumor suppressor receptors or enhance oncogenic signaling.
DNA Damage Repair: Histone monoubiquitination, particularly of H2A and H2B, alters chromatin structure to facilitate access of DNA repair machinery [14] [16]. This function is crucial for maintaining genomic integrity, and its disruption promotes cancer progression.
Transcriptional Regulation: Monoubiquitination of transcription factors can either activate or inhibit their function, representing a rapid mechanism for adjusting gene expression programs in response to cellular signals [13]. In cancer, oncogenic transcription factors may be stabilized through altered monoubiquitination patterns.
Protein Activation and Localization: Monoubiquitination can serve as a switch that modulates protein activity or subcellular localization, influencing signaling pathway output [14].
The functional significance of monoubiquitination is amplified through multi-monoubiquitination, where multiple lysine residues on a single substrate are modified with individual ubiquitin molecules, creating a robust signal for processes such as endocytosis [14].
Polyubiquitin Chain Topologies: Structural and Functional Diversity
Classification of Ubiquitin Linkages
Polyubiquitin chains are classified based on the specific lysine residue used to connect ubiquitin molecules, with eight distinct linkage types identified: Met1 (linear), Lys6, Lys11, Lys27, Lys29, Lys33, Lys48, and Lys63. Each linkage type generates structurally distinct chains with unique functional properties [11] [10]. The table below summarizes the key characteristics and functions of major ubiquitin linkage types.
Table 1: Ubiquitin Chain Linkage Types and Their Functional Roles
| Linkage Type | Structural Features | Primary Functions | Key E2/E3 Enzymes | Cancer Relevance |
|---|---|---|---|---|
| Lys48 | Compact conformations | Proteasomal degradation [11] | CDC34/SCF complexes [15] | Tumor suppressor degradation [11] |
| Lys63 | Extended "open" conformations [17] | DNA repair, signaling, endocytosis [15] | Ubc13-MMS2 complex [15] | NF-κB activation, survival signaling |
| Met1 (Linear) | Extended and compact conformations [17] | NF-κB activation, inflammation [11] | LUBAC complex (HOIP, HOIL-1) [11] | Inflammatory signaling in tumor microenvironment |
| Lys11 | Mixed compact/extended | Cell cycle regulation, ERAD [11] | UBE2S/APC/C [12] | Cell cycle dysregulation |
| Lys27 | Not well characterized | Mitochondrial quality control, innate immunity [11] | Parkin, RNF185, AMFR [11] | Mitophagy dysregulation |
| Lys29 | Not well characterized | Proteasomal degradation, innate immunity [11] | HECT-type E3s [11] | Unfolded protein response |
| Lys6 | Not well characterized | DNA damage response [11] | Unknown | Genomic instability |
| Lys33 | Not well characterized | Intracellular trafficking [11] | Unknown | Metabolic reprogramming |
Chain Conformations and Functional Implications
The three-dimensional architecture of polyubiquitin chains plays a crucial role in determining their functional specificity. Single-molecule FRET studies have revealed that differently linked diubiquitin (diUb) chains exist in multiple conformational states in solution, and these dynamics provide an additional layer of regulation in the ubiquitin system [17].
Lys48-linked diUb: Adopts predominantly compact conformations (~90% high-FRET, ~10% low-FRET) with limited exposure of hydrophobic patches, facilitating proteasomal recognition [17].
Lys63-linked diUb: Exists in an equilibrium between extended (~25-30% non-FRET) and compact conformations (~70-75% low-FRET), enabling diverse interactions with signaling proteins [17].
Met1-linked diUb: Displays both extended and compact conformations, with the UBAN domain of NEMO selecting pre-existing compact conformations to activate NF-κB signaling [17].
These conformational equilibria enable ubiquitin chains to be recognized by different ubiquitin-binding proteins, with domains such as UBDs and DUBs selecting pre-existing conformations rather than inducing structural changes [17]. This conformational selection mechanism has profound implications for how ubiquitin signals are decoded in cellular pathways relevant to cancer.
Diagram 1: Ubiquitin Code Decoding Pathway. This diagram illustrates how different ubiquitin chain types adopt specific conformations that determine cellular outcomes.
Atypical Ubiquitin Linkages and Their Functions
Beyond the well-characterized Lys48 and Lys63 linkages, "atypical" ubiquitin chains (Lys6, Lys11, Lys27, Lys29, Lys33, and Met1) have emerged as important regulators of specialized cellular processes:
Lys11-linked chains: Play crucial roles in cell cycle regulation and ER-associated degradation (ERAD), with the anaphase-promoting complex/cyclosome (APC/C) and E2 enzyme UBE2S specifically generating Lys11-linked chains to control mitotic progression [11] [12].
Lys27-linked chains: Regulate mitochondrial quality control through Parkin-mediated mitophagy and modulate innate immune response via RNF185-targeting of cGAS and AMFR-targeting of STING [11].
Lys29-linked chains: Involved in proteasomal degradation, innate immune response, and regulation of AMPK-related protein kinases [11].
Lys6 and Lys33 linkages: Participate in DNA damage response and intracellular trafficking, respectively, though their mechanisms remain less characterized [11].
The expanding understanding of atypical ubiquitin linkages reveals an unexpected sophistication in ubiquitin signaling, with chain topology serving as a critical determinant of functional specificity in pathways frequently altered in cancer.
E3 Ubiquitin Ligases: Writers of the Ubiquitin Code
Classification and Mechanisms of E3 Ligases
E3 ubiquitin ligases constitute a diverse family of enzymes that determine substrate specificity in the ubiquitination cascade. Humans possess over 600 E3 ligases, classified into four major types based on their structural and mechanistic features [11]:
Table 2: Major Classes of E3 Ubiquitin Ligases
| E3 Class | Representative Members | Catalytic Mechanism | Structural Features | Cancer Associations |
|---|---|---|---|---|
| RING-finger | MDM2, CBL, COP1 | Direct ubiquitin transfer from E2 to substrate [11] | Zinc-binding RING domain [11] | MDM2-p53 axis dysregulation |
| HECT | NEDD4, HERC, HUWE1 | E3-Ub intermediate via catalytic cysteine [11] | HECT C-terminal domain [11] | HERC6 overexpression in cancers |
| RBR | Parkin, HOIP | RING-HECT hybrid mechanism [11] | RING1-IBR-RING2 domains [11] | Parkin mutations in Parkinson's |
| U-box | CHIP, UFD2 | Similar to RING but without zinc [11] | U-box domain stabilized by hydrogen bonds [11] | CHIP in protein quality control |
Regulatory Mechanisms of E3 Ligases
E3 ligase activity is tightly controlled through multiple regulatory mechanisms that ensure precise spatiotemporal control of ubiquitination:
Non-covalent ubiquitin interactions: Many E2 and E3 enzymes contain secondary ubiquitin-binding sites that regulate their activity. For example, the Arkadia RING E3 ligase binds regulatory ubiquitin molecules that enhance processive ubiquitin chain formation [12].
Post-translational modifications: Phosphorylation, acetylation, and other modifications directly regulate E3 ligase activity, localization, and substrate specificity.
Multi-subunit complexes: Many RING E3 ligases, particularly cullin-RING ligases (CRLs), assemble into multi-protein complexes that integrate regulatory inputs and enhance catalytic versatility [11].
Allosteric activation: Some E3 ligases, such as Parkin, are maintained in autoinhibited states until activated by specific signals, preventing spurious ubiquitination [10].
The dysregulation of E3 ligase activity represents a common mechanism in oncogenesis, with both tumor-suppressive and oncogenic E3s being frequently altered in human cancers through mutations, amplifications, or deletions [11] [13].
Experimental Methods for Studying Ubiquitin Signaling
Biochemical and Biophysical Approaches
Several sophisticated methodologies have been developed to investigate the structure and function of ubiquitin modifications:
Single-molecule FRET (smFRET): Enables real-time observation of ubiquitin chain conformational dynamics by measuring energy transfer between fluorophores attached to different ubiquitin molecules [17]. This approach revealed the conformational equilibria of Lys48-, Lys63-, and Met1-linked diUb.
Linkage-specific antibodies: Monoclonal antibodies that recognize specific ubiquitin linkages (Met1, Lys11, Lys48, Lys63) allow immunological detection and quantification of chain types in cells and tissues [10].
Mass spectrometry-based proteomics: Advanced MS techniques, including AQUA and TMT labeling, enable comprehensive identification and quantification of ubiquitination sites and chain topologies [10].
X-ray crystallography and NMR spectroscopy: Provide high-resolution structural information about ubiquitin chains and their complexes with binding proteins [17].
In Vitro Ubiquitination Assays
Reconstituted biochemical systems allow detailed mechanistic studies of ubiquitination:
Protocol: SCF/Cdc34 Ubiquitination Assay [15]
Reagent Preparation:
- Purify SCF E3 complex (Skp1, Cul1, Rbx1, and F-box protein Cdc4)
- Prepare E1 (Uba1) and E2 (Cdc34) enzymes
- Obtain substrate (Sic1) and ubiquitin
Reaction Setup:
- Assemble 50 μL reaction containing: 50 mM Tris-HCl (pH 7.5), 5 mM MgCl₂, 2 mM ATP, 0.2 mM DTT, 2 mM creatine phosphate, 0.1 U creatine phosphokinase
- Add 100 nM E1, 1-5 μM E2, 100-500 nM SCF complex, 5-20 μM ubiquitin, and 1-5 μM substrate
Reaction Conditions:
- Incubate at 30°C for 0-120 minutes
- Terminate by adding SDS-PAGE sample buffer
Analysis:
- Resolve products by SDS-PAGE and immunoblot with substrate-specific antibodies
- Assess mono- versus polyubiquitination patterns
This assay enabled the discovery that amino acids surrounding acceptor lysines and key residues in the Cdc34 catalytic core determine the efficiency of ubiquitination and choice between mono- versus polyubiquitination [15].
Research Reagent Solutions for Ubiquitin Studies
Table 3: Essential Research Reagents for Ubiquitin Code Investigation
| Reagent Category | Specific Examples | Applications | Key Features |
|---|---|---|---|
| Linkage-specific Antibodies | Anti-K48, Anti-K63, Anti-M1 [10] | Immunoblotting, immunofluorescence | Selective recognition of specific ubiquitin linkages |
| Activity-based Probes | Ubiquitin vinyl sulfones, HA-Ub-VS [10] | DUB profiling, mechanism studies | Covalent trapping of active DUBs |
| E2/E3 Expression Systems | Baculovirus (E1/E2/E3), Bacterial (Ub) [15] | In vitro ubiquitination assays | Recombinant enzyme production |
| Mass Spectrometry Standards | AQUA ubiquitin peptides, SILAC labeling [10] | Ubiquitin proteomics | Absolute quantification of ubiquitin modifications |
| Chain-specific DUBs | OTUB1 (K48-specific), AMSH-LP (K63-specific) [17] | Chain linkage validation, cleavage | Enzymatic confirmation of chain topology |
| Ubiquitin Mutants | K48R, K63R, K0 (all lysines mutated) [15] | Mechanism studies | Block specific chain formation |
Ubiquitin Code Alterations in Cancer Development
Dysregulation of the ubiquitin system contributes fundamentally to oncogenesis through multiple mechanisms:
Tumor suppressor degradation: Oncogenic E3 ligases, such as MDM2, inappropriately target tumor suppressors like p53 for proteasomal degradation, enabling uncontrolled cell proliferation [13].
Oncoprotein stabilization: Loss of tumor-suppressive E3 ligases or gain of deubiquitinases (DUBs) can stabilize oncoproteins, enhancing their half-life and signaling output [13].
DNA repair defects: Alterations in ubiquitin-mediated DNA damage response, particularly involving Lys63-linked and Lys6-linked chains, promote genomic instability [11] [16].
Signaling pathway dysregulation: Ubiquitination regulates key cancer-relevant pathways including NF-κB, Wnt, and TGF-β, with chain-type specific alterations driving pathway hyperactivation or suppression [11].
Transcription factor modulation: Ubiquitination directly regulates transcription factors such as NF-κB, c-Myc, and p53, with cancer-associated mutations frequently affecting their ubiquitin-mediated control [13].
Therapeutic targeting of ubiquitin code alterations represents a promising anticancer strategy, with approaches including PROTACs (Proteolysis Targeting Chimeras) that hijack the ubiquitin system to degrade specific oncoproteins, and small molecule inhibitors targeting specific E3 ligases or DUBs [11] [16] [13].
The ubiquitin code represents a sophisticated language that governs cellular physiology through diverse modifications including monoubiquitination and polyubiquitin chains of distinct topologies. The structural characteristics of different ubiquitin linkages, their conformational dynamics, and specific recognition by effector proteins create a complex signaling network that determines protein fate and function. In cancer development, alterations in writing, reading, and erasing the ubiquitin code contribute fundamentally to hallmark capabilities including sustained proliferation, evasion of growth suppression, and genomic instability. Continued elucidation of ubiquitin code mechanisms, coupled with advanced experimental approaches to decipher this complexity, will accelerate the development of novel cancer therapeutics that target specific aspects of ubiquitin signaling.
The ubiquitin code, a complex system of post-translational modifications, fundamentally governs cellular homeostasis by precisely regulating protein stability, localization, and interaction networks. In oncogenesis, this code undergoes profound alterations, directly enabling the hyperactivation of oncogenic pathways and the inactivation of tumor suppressive networks. This whitepaper provides a technical analysis of ubiquitin code alterations within five core cancer pathways—RAS, mTOR, PTEN, p53, and c-Myc. We synthesize the molecular mechanisms of pathogenic ubiquitination and deubiquitination, summarize key experimental methodologies for their investigation, and visualize the disrupted signaling networks. Furthermore, we catalog essential research tools and emerging therapeutic strategies, including proteolysis-targeting chimeras (PROTACs), that aim to correct the dysregulated ubiquitin signaling in human malignancies. The insights presented herein frame ubiquitin code alterations as a central thesis in cancer biology, offering a roadmap for future research and drug discovery.
The ubiquitin-proteasome system (UPS) is a critical enzymatic cascade responsible for the controlled degradation of intracellular proteins, thereby regulating fundamental processes such as the cell cycle, DNA repair, and signal transduction [18] [19]. Ubiquitination involves a sequential reaction catalyzed by ubiquitin-activating (E1), ubiquitin-conjugating (E2), and ubiquitin-ligating (E3) enzymes, which conjugate the 76-amino-acid ubiquitin protein to specific substrate lysine residues [20]. The specificity of this process is largely determined by the E3 ligases, of which there are over 600 in the human genome [19]. Deubiquitinating enzymes (DUBs) counteract this process by removing ubiquitin chains, adding a dynamic layer of regulation [6] [21]. The functional consequence of ubiquitination is dictated by the topology of the ubiquitin chain. Whereas K48-linked polyubiquitination primarily targets substrates for proteasomal degradation, K63-linked chains often serve non-proteolytic roles in signaling activation, and monoubiquitination can regulate protein activity and trafficking [22] [18]. Cancer cells hijack this sophisticated system to destabilize tumor suppressors, stabilize oncoproteins, and rewire core signaling pathways, making the UPS a compelling area for therapeutic intervention [23] [18].
Ubiquitin Code Alterations in Core Signaling Pathways
The following sections detail the specific alterations to the ubiquitin code within five critical cancer pathways.
RAS Ubiquitination
RAS proteins are the most frequently mutated oncoproteins in human cancers, driving tumor proliferation, metastasis, and therapeutic resistance [8] [24]. Recent research has revealed that ubiquitination is a key mechanism for the dynamic post-translational regulation of RAS stability, membrane localization, and signal transduction.
- Regulatory Enzymes and Sites: A series of E3 ligases, DUBs, and regulatory proteins orchestrate the ubiquitination of RAS. Studies have identified specific ubiquitination sites and demonstrated heterogeneity in ubiquitination patterns across different RAS isoforms (KRAS4A, KRAS4B, NRAS, and HRAS), which contribute to their functional disparities in cancer [8] [24].
- Therapeutic Targeting: Targeting the RAS ubiquitination pathway presents novel therapeutic opportunities. Future research directions include integrating protein structure analysis with high-throughput screening to develop specific ubiquitination modulators. Combination strategies that pair RAS ubiquitination-targeting agents with direct RAS inhibitors or immunotherapy hold promise for overcoming RAS-driven malignancies [8].
mTOR Ubiquitination
The mechanistic target of rapamycin (mTOR) is a central kinase that integrates environmental and intracellular signals to control cell growth and metabolism, and its ubiquitination represents a critical regulatory node.
- K63-Linked Ubiquitination for Activation: The E3 ligase TRAF6 mediates K63-linked polyubiquitination of mTOR in an amino acid-dependent manner. This modification, facilitated by the adapter protein p62, promotes the translocation of the mTORC1 complex to the lysosomal surface, a prerequisite for its full activation [21]. This mechanism is frequently upregulated in cancer cells.
- Regulation of Stability: Conversely, the E3 ligases FBX8 and FBXW7 have been implicated in the K48-linked ubiquitination of mTOR, which can lead to its proteasomal degradation. The decreased activity of these ligases in some cancers results in mTOR stabilization and pathway hyperactivation [21].
PTEN Ubiquitination
The tumor suppressor PTEN (Phosphatase and Tensin Homolog) antagonizes the oncogenic PI3K-AKT pathway, and its activity is tightly controlled by ubiquitination.
- Regulation of Stability and Localization: PTEN can undergo both monoubiquitination and polyubiquitination. Monoubiquitination has been shown to regulate PTEN's nuclear-cytoplasmic trafficking, which is important for its tumor-suppressive functions in different cellular compartments [18].
- Oncogenic Degradation: Several E3 ligases promote the polyubiquitination and degradation of PTEN, effectively inactivating its phosphatase activity and leading to constitutive AKT signaling. The identity of specific E3 ligases involved and their counteracting DUBs that stabilize PTEN are active areas of investigation with significant therapeutic implications [18].
p53 Ubiquitination
The p53 tumor suppressor is a master regulator of the cellular stress response, and its stability is predominantly controlled by ubiquitination.
- Major Regulator MDM2: The primary E3 ligase for p53 is MDM2 (Mouse Double Minute 2). MDM2 mediates the K48-linked polyubiquitination of p53, targeting it for proteasomal degradation and maintaining low basal levels in normal cells [18]. In many cancers, MDM2 is overamplified, leading to excessive degradation of p53.
- Non-Proteolytic Ubiquitination: In addition to degradation, p53 can be modified by K63-linked and monoubiquitination. For instance, TRAF6 can modify p53 with K63 linkages, which can convert it into a mitochondrial pro-survival factor under certain conditions, illustrating the context-dependent nature of the ubiquitin code [22].
- Deubiquitinating Enzymes (DUBs): Several DUBs, including USP7 (HAUSP), USP10, and USP29, can deubiquitinate and stabilize p53, forming a complex regulatory network that determines p53's fate in response to genotoxic stress [6] [18].
c-Myc Ubiquitination
The c-Myc oncoprotein is a transcription factor that drives cell proliferation and metabolism, and its rapid turnover is essential to prevent tumorigenesis.
- Degradation by SCF Complexes: The stability of c-Myc is primarily regulated by the SCF (SKP1-CUL1-F-box protein) family of E3 ubiquitin ligases. Specifically, the F-box protein FBXW7 (also known as CDC4) recognizes phosphorylated degrons on c-Myc and mediates its K48-linked polyubiquitination and degradation [18].
- Stabilization in Cancer: Mutations in FBXW7 or the phosphorylation sites on c-Myc are common in cancers, leading to c-Myc stabilization and enhanced oncogenic activity. Additionally, the DUB USP28 has been shown to antagonize FBXW7, deubiquitinating and stabilizing c-Myc in certain contexts [6] [18].
Table 1: Summary of Ubiquitin Code Alterations in Core Cancer Pathways
| Pathway | Key E3 Ligases | Key DUBs | Ubiquitin Linkage | Functional Outcome |
|---|---|---|---|---|
| RAS | Various, isoform-specific | Various, isoform-specific | Not Specified | Alters stability, membrane localization, signaling [8] [24] |
| mTOR | TRAF6, FBXW7, FBX8 | Not Well Characterized | K63, K48 | K63: Activates via lysosomal recruitment; K48: Targets for degradation [21] |
| PTEN | Multiple | Not Well Characterized | Mono, K48 | Mono: Regulates localization; K48: Targets for degradation [18] |
| p53 | MDM2, TRAF6 | USP7, USP10, USP29 | K48, K63, Mono | K48: Degradation; K63/Mono: Alters activity/localization [22] [18] |
| c-Myc | FBXW7 | USP28 | K48 | FBXW7 mediates degradation; USP28 stabilizes [6] [18] |
Experimental Protocols for Investigating the Ubiquitin Code
A robust methodological framework is essential for dissecting the complexities of ubiquitination. Below are detailed protocols for key experimental approaches.
Ubiquitination Assays
Objective: To confirm a specific protein is ubiquitinated and identify the type of ubiquitin linkage formed. Workflow:
- Cell Lysis and Immunoprecipitation (IP): Lyse cells under denaturing conditions (e.g., using RIPA buffer with 1% SDS followed by dilution) to preserve transient ubiquitination and disrupt non-covalent interactions. Immunoprecipitate the protein of interest using a specific antibody.
- Immunoblotting (Western Blot): Resolve the immunoprecipitated proteins by SDS-PAGE and transfer to a membrane.
- Detection: Probe the membrane with anti-ubiquitin antibodies. To determine chain topology, use linkage-specific ubiquitin antibodies (e.g., anti-K48-Ub, anti-K63-Ub). A characteristic upward smear on the blot indicates polyubiquitination. Critical Notes: Always include controls with proteasome inhibitors (e.g., MG132) to enhance the detection of K48-linked ubiquitinated species, and co-transfect epitope-tagged ubiquitin (e.g., HA-Ub, MYC-Ub) to facilitate detection [22] [18].
Identification of E3 Ligases and DUBs
Objective: To discover the specific E3 ligase or DUB that regulates a target protein. Workflow:
- Functional Screening: Perform siRNA or CRISPR-based screens targeting libraries of E3 ligases or DUBs. Monitor changes in the abundance or ubiquitination status of the target protein via immunoblotting.
- Co-Immunoprecipitation (Co-IP): To validate physical interaction, lyse cells under non-denaturing conditions and immunoprecipitate the target protein. Probe for co-precipitating E3s or DUBs by western blot.
- In Vitro Ubiquitination/Deubiquitination Assay: Purify the candidate E3 ligase (or DUB), the target protein, and the necessary E1/E2 enzymes (and ubiquitin). Incubate the components with ATP. Analyze the reaction products by western blot to detect ubiquitination (smear) or deubiquitination (loss of smear) of the target protein [6] [20].
Proteomics for Ubiquitin Signatures
Objective: To profile global ubiquitination changes in response to a stimulus (e.g., drug treatment, pathway activation) or in a disease state. Workflow:
- Sample Preparation: Lyse cells or tissues.
- Enrichment of Ubiquitinated Peptides: Digest the protein lysate with trypsin and use antibodies specific for di-glycine (diGly) remnants—a signature left on ubiquitinated lysines after trypsin digestion—to enrich for ubiquitinated peptides.
- Mass Spectrometry (MS) Analysis: Analyze the enriched peptides by liquid chromatography-tandem mass spectrometry (LC-MS/MS).
- Data Analysis: Use bioinformatic tools to identify the sites of ubiquitination and quantify changes in ubiquitination levels across different conditions [22].
Diagram 1: Experimetal workflow for ubiquitination analysis.
The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential Research Reagents for Ubiquitination Studies
| Reagent / Tool | Category | Primary Function in Research | Example Application |
|---|---|---|---|
| Linkage-Specific Ub Antibodies | Antibody | Detect specific ubiquitin chain topologies (K48, K63, etc.) by Western Blot/IF | Determining if a protein is degraded (K48) or signal-activated (K63) [22] |
| Epitope-Tagged Ubiquitin (HA-, MYC-, FLAG-Ub) | DNA Construct | Express ubiquitin in cells; tag allows specific pulldown and detection | Overexpression to enhance detection of ubiquitinated proteins in IP assays [18] |
| Proteasome Inhibitors (MG132, Bortezomib) | Small Molecule Inhibitor | Block proteasomal degradation, causing accumulation of ubiquitinated proteins | Essential for visualizing K48-polyubiquitinated substrates in assays [18] |
| E1 Inhibitor (MLN7243) | Small Molecule Inhibitor | Blocks the ubiquitination cascade at its initiation step | Positive control to confirm ubiquitin-dependent processes [18] |
| siRNA/shRNA E3/DUB Libraries | Functional Genomics Tool | For high-throughput screens to identify regulators of a target protein | Identifying novel E3 ligases or DUBs for a protein of interest [6] |
| Tandem Ubiquitin Binding Entities (TUBEs) | Affinity Reagent | Bind polyubiquitin chains with high affinity, enriching ubiquitinated proteins from lysates | Proteomics studies; stabilizing labile ubiquitination events [22] |
| PROTACs (e.g., ARV-110, ARV-471) | Bifunctional Degrader | Recruit E3 ligases to neo-substrates, inducing their ubiquitination and degradation | Targeted protein degradation as a therapeutic strategy and research tool [23] [6] |
Visualization of Pathway Alterations and Crosstalk
The following diagram synthesizes the ubiquitin-mediated regulatory network connecting the five core cancer pathways, highlighting key ubiquitination events and their functional consequences.
Diagram 2: Ubiquitin-mediated regulation in core cancer pathways.
Concluding Remarks and Therapeutic Perspectives
The intricate alteration of the ubiquitin code is a non-genetic hallmark of cancer that empowers the rewiring of core pathways like RAS, mTOR, PTEN, p53, and c-Myc. A deep mechanistic understanding of these processes, facilitated by the experimental and reagent tools outlined herein, is paving the way for a new class of therapeutics. The clinical success of proteasome inhibitors has already validated the UPS as a target. The future lies in developing more precise agents, such as specific E3 ligase inhibitors, DUB inhibitors, and most notably, PROTACs, which leverage the cell's own ubiquitination machinery to degrade previously "undruggable" oncoproteins [23] [6] [18]. As research continues to decode the complexities of ubiquitin chain diversity and crosstalk with other post-translational modifications, the development of biomarker-guided combination therapies that target the ubiquitin code will be crucial for achieving durable responses in cancer patients.
The RAS family of GTPases (KRAS4A, KRAS4B, HRAS, and NRAS) represents one of the most frequently mutated oncoprotein families in human cancers, with mutations occurring in approximately 19% of all malignancies [25]. These mutations drive constitutive activation of downstream signaling pathways such as MAPK and PI3K-AKT, leading to uncontrolled cell proliferation, metastasis, and therapeutic resistance [25]. While oncogenic mutations have long been the focus of RAS biology, recent research has illuminated that post-translational modifications (PTMs), particularly ubiquitination, play a pivotal role in regulating RAS protein stability, membrane localization, and signaling transduction [8] [25].
Ubiquitination exerts bidirectional control over RAS activity: it can promote degradation to suppress oncogenic signaling or activate RAS via non-degradative mechanisms that alter GTP binding, effector interaction, and subcellular localization [25]. This review synthesizes current understanding of the heterogeneous ubiquitination patterns across RAS isoforms, their functional consequences in cancer progression, and the experimental approaches driving these discoveries. Understanding these isoform-specific regulatory mechanisms provides crucial insights for developing novel therapeutic strategies against RAS-driven cancers [8].
Molecular Mechanisms of RAS Ubiquitination
The Ubiquitination Machinery
Ubiquitination involves a sequential enzymatic cascade comprising E1 ubiquitin-activating enzymes, E2 ubiquitin-conjugating enzymes, and E3 ubiquitin ligases [26]. The E3 ligase, as the most heterogeneous component, provides substrate specificity by recognizing specific "degron" motifs on target proteins [25] [26]. The process concludes with the covalent attachment of one or more ubiquitin molecules to lysine residues on the target protein [26]. This modification is reversible through the action of deubiquitinases (DUBs), which remove ubiquitin chains, thereby stabilizing substrates [25] [26].
The fate of ubiquitinated RAS proteins is predominantly determined by the topology of ubiquitin chains. Canonical K48-linked polyubiquitination predominantly marks substrates for proteasomal degradation, whereas K63-linked chains often act as signals for alternative degradation routes, including the autophagy-lysosomal pathway, or for non-degradative signaling functions [25]. The dynamic balance between ubiquitinating and deubiquitinating enzymes precisely controls RAS protein homeostasis and function [25].
Structural Determinants of RAS Ubiquitination
Mammalian RAS comprises four isoforms—KRAS4A, KRAS4B, HRAS, and NRAS—encoded by three genes, all sharing a conserved G domain but diverging in their hypervariable regions (HVRs) [25]. The G domain contains conserved motifs critical for RAS function: GTP binding sites, the phosphate binding loop (P loop), and two switch regions (Switch I/II). The C-terminal HVR, through PTMs including prenylation and palmitoylation, directs RAS trafficking between the plasma membrane and endomembranes [25].
Both the G-domain and the HVR contain sites of ubiquitination, directly linking structural features to proteostatic regulation. The table below summarizes key ubiquitination sites identified in RAS proteins and their functional consequences:
Table 1: Key Ubiquitination Sites in RAS Proteins and Their Functional Impacts
| Ubiquitination Site | RAS Isoform | Functional Consequence | Molecular Mechanism |
|---|---|---|---|
| Lys117 | Pan-RAS | Enhanced activation | Facilitates nucleotide exchange [25] |
| Lys147 | Pan-RAS | Enhanced activation | Hinders GAP-mediated GTP hydrolysis [25] |
| Lys104 | KRAS | Enhanced activation | Promotes binding with GEF [25] |
| Lys128 | Pan-RAS | Attenuated activation | Facilitates RAS binding to GAP [25] |
| Lys170 | HRAS | Altered localization | Impairs membrane association [25] |
Isoform-Specific Ubiquitination Landscapes
Regulatory Enzymes with Isoform Specificity
The ubiquitination landscape of RAS isoforms is shaped by distinct profiles of E3 ligases and DUBs that confer isoform-specific regulation. This intricate regulatory network enables precise control over individual RAS family members despite their structural similarities.
Table 2: E3 Ubiquitin Ligases in RAS Regulation
| E3 Ligase | Type | Substrate | RAS Regulation | Role in Cancer | Cancer Context |
|---|---|---|---|---|---|
| NEDD4-1 | HECT E3 | Pan-RAS | Degradation | Bifunctional | Cervical cancer, colorectal cancer, glioblastoma [25] |
| Rabex5 | RING E3 | HRAS, NRAS | Location, GTP-binding | Bifunctional | Colorectal, breast, prostate cancer [25] |
| β-TrCP | RING E3 | Pan-RAS | Degradation | Bifunctional | Colorectal cancer, pancreatic cancer, melanoma [25] |
| SMURF2 | HECT E3 | KRAS | Degradation | Bifunctional | Lung cancer, colorectal cancer [25] |
| LZTR1 | RING E3 | Pan-RAS | Location, degradation | Tumor suppressor | Lung adenocarcinoma, liver cancer, glioblastoma [25] |
| WDR76 | RING E3 | Pan-RAS | Degradation | Tumor suppressor | Colorectal cancer, hepatocellular carcinoma [25] |
| FBXL6 | RING E3 | KRAS | Effector binding | Tumor promoter | Hepatocellular carcinoma, lung cancer [25] |
The HECT-family E3 ligase NEDD4-1 exemplifies this regulatory complexity, targeting multiple RAS isoforms for degradation while exhibiting context-dependent functions in various cancer types [25]. In contrast, RABEX5 demonstrates more restricted substrate specificity, primarily regulating HRAS and NRAS through mechanisms that influence subcellular localization and GTP-binding capacity rather than degradation [25]. The CRL family adapter LZTR1 represents another critical regulator, assembling with CUL3 to facilitate the degradation of RAS proteins through ubiquitination, with particular significance in Noonan syndrome and cancer contexts [25].
Mutation-Specific Effects on Ubiquitination
Oncogenic mutations in RAS genes not only confer constitutive activation but also potentially alter the ubiquitination landscape. Most RAS oncogenic mutations drive constitutive activation through three distinct mechanistic categories: (1) impairing GTP hydrolysis (e.g., G12D, Q61L) by inducing steric hindrance or disrupting catalytic networks; (2) accelerating nucleotide exchange (e.g., G13D, A59G) via enhanced GEF interaction or destabilized GDP binding; and (3) rewiring conformational states (e.g., A146T) to modulate effector selectivity [25].
The influence of distinct site-specific ubiquitination on these various RAS mutants remains an active area of investigation. Certain mutations may potentially create or obscure degron motifs recognized by specific E3 ligases, thereby altering the ubiquitination efficiency and subsequent degradation of mutant RAS proteins. This mutation-specific regulation may contribute to the varying degradation rates observed among different RAS mutants and their corresponding sensitivities to ubiquitination-targeting therapies [25].
Experimental Approaches for Studying RAS Ubiquitination
Methodological Framework
Deciphering the ubiquitination landscape of RAS proteins requires a multidisciplinary approach combining biochemical, cellular, and computational methods. The following workflow outlines key experimental strategies for identifying and validating RAS ubiquitination events:
The Scientist's Toolkit: Essential Research Reagents
Table 3: Essential Research Reagents for Studying RAS Ubiquitination
| Reagent/Category | Specific Examples | Function/Application |
|---|---|---|
| Ubiquitin Expression Plasmids | HA-Ub, FLAG-Ub, Myc-Ub | Detection of ubiquitinated proteins via immunoprecipitation and Western blot [25] |
| E3 Ligase Expression Constructs | NEDD4-1, RABEX5, SMURF2, LZTR1 | Functional studies of specific E3 ligases in RAS regulation [25] |
| RAS Isoform Constructs | Wild-type and mutant KRAS4A/B, HRAS, NRAS | Isoform-specific ubiquitination studies and functional assays [25] |
| Site-Directed Mutants | K117R, K147R, K104R, K128R | Identification of specific ubiquitination sites and functional consequences [25] |
| Proteasome Inhibitors | MG132, Bortezomib | Assessment of proteasomal degradation dependence of ubiquitinated RAS [25] |
| Deubiquitinase Inhibitors | PR-619 (broad-spectrum DUB inhibitor) | Investigation of DUB function in RAS stability and signaling [25] |
| Computational Prediction Tools | Ubibrowser 2.0 | Prediction of E3 ligase-substrate interactions for RAS proteins [25] |
Functional Consequences and Therapeutic Implications
Biological Outcomes of RAS Ubiquitination
The functional consequences of RAS ubiquitination extend across multiple cellular compartments and signaling pathways, as illustrated in the following pathway map:
The spatiotemporal control of RAS signaling through ubiquitination directly impacts critical cancer hallmarks. By regulating RAS protein abundance through degradative ubiquitination, the ubiquitin system can suppress oncogenic signaling [25]. Conversely, non-degradative ubiquitination events at specific lysine residues can enhance RAS activation by facilitating nucleotide exchange or impeding GTP hydrolysis, thereby amplifying downstream effector pathways that drive proliferation, metastasis, and therapy resistance [25]. The balance between these opposing functions depends on the specific E3 ligases and DUBs engaged, the cellular context, and the genetic background of the tumor.
Therapeutic Exploitation of RAS Ubiquitination
Targeting the ubiquitination pathway offers novel strategies to overcome RAS-driven cancers. Several therapeutic approaches are emerging:
- E3 ligase enhancers: Small molecules that promote the interaction between specific E3 ligases and mutant RAS proteins could selectively degrade oncogenic RAS [25].
- DUB inhibitors: Compounds targeting RAS-stabilizing DUBs could reactivate endogenous degradation mechanisms against oncogenic RAS [25].
- Combination therapies: Ubiquitination-targeting agents combined with RAS inhibitors or immunotherapy may help overcome resistance mechanisms [25].
- PROTAC technology: Proteolysis-Targeting Chimeras (PROTACs) that recruit E3 ligases to RAS proteins represent a promising avenue for targeted degradation [6].
Future research should integrate protein structure analysis and high-throughput screening to develop specific ubiquitination modulators and explore combination strategies with direct RAS inhibitors or immunotherapy, aiming to overcome RAS-driven malignant phenotypes [8] [25].
The heterogeneous ubiquitination of RAS isoforms represents a critical layer of regulation in cancer development and progression. The distinct ubiquitination patterns, E3 ligase associations, and functional outcomes across KRAS, NRAS, and HRAS underscore the complexity of the ubiquitin code in RAS biology. Understanding these isoform-specific mechanisms provides not only fundamental insights into RAS pathophysiology but also exciting opportunities for therapeutic intervention. As our knowledge of the RAS ubiquitin code expands, so does the potential for developing innovative strategies to target this once "undruggable" oncoprotein family in precision oncology.
The ubiquitin code—a complex system of post-translational modifications (PTMs) that controls protein stability, localization, and function—is frequently dysregulated in cancer development. Ubiquitination does not function in isolation; rather, it engages in extensive crosstalk with other PTMs, including phosphorylation, acetylation, and SUMOylation, to orchestrate sophisticated signaling networks that drive tumorigenesis. This dynamic interplay creates regulatory circuits that allow cancer cells to adapt to therapeutic pressures, evade immune surveillance, and maintain proliferative advantages. The integration of these modification systems generates a complex signaling language that researchers are only beginning to decipher. Understanding this crosstalk is critical for developing novel cancer therapeutics that target the ubiquitin-proteasome system and its interconnected networks, particularly in the context of overcoming treatment resistance [16] [22].
The following diagram illustrates the core conceptual framework of PTM crosstalk with ubiquitination in cancer biology:
Ubiquitin-Phosphorylation Crosstalk: Reciprocal Regulation in Signaling Networks
The interplay between ubiquitination and phosphorylation represents one of the most prevalent and biologically significant forms of PTM crosstalk in cancer. These modifications engage in reciprocal regulation, where phosphorylation often creates recognition motifs for E3 ubiquitin ligases, while ubiquitination can conversely modulate kinase activity and stability. This bidirectional relationship forms sophisticated regulatory circuits that control key oncogenic and tumor suppressive pathways.
Phosphorylation-Dependent Ubiquitination
The phosphodegron motif—a specific phosphorylated sequence recognized by E3 ubiquitin ligases—serves as a critical interface in ubiquitin-phosphorylation crosstalk. The F-box protein FBXW7 exemplifies this mechanism by specifically recognizing phosphorylated degrons on substrates such as p53. When p53 is phosphorylated at residues S33 and S37, it creates a phosphodegron that facilitates FBXW7-mediated ubiquitination and subsequent degradation, promoting radioresistance in colorectal cancer [22]. This phosphorylation-dependent recognition system enables precise temporal control over protein stability, directly linking kinase activity to proteasomal degradation.
The contextual nature of this crosstalk is demonstrated by FBXW7's opposing roles in different cancer types. While it promotes radioresistance in p53-wildtype colorectal tumors, FBXW7 enhances radiosensitivity in non-small cell lung cancer (NSCLC) with SOX9 overexpression by destabilizing SOX9 and alleviating p21 repression. This functional switch highlights how tumor-specific genetic backgrounds influence the outcome of ubiquitin-phosphorylation crosstalk [22].
Ubiquitination-Mediated Kinase Regulation
Ubiquitination reciprocally regulates kinase activity through both proteolytic and non-proteolytic mechanisms. K63-linked ubiquitin chains play particularly important roles in organizing kinase signaling complexes. For instance, TRAF4 utilizes K63 modifications to activate the JNK/c-Jun pathway, driving overexpression of anti-apoptotic Bcl-xL in colorectal cancer and MCL-1 in oral cancers [22]. This non-degradative ubiquitination creates signaling platforms that enhance kinase activity and promote survival pathways in cancer cells.
The functional consequences of ubiquitin-phosphorylation crosstalk are illustrated in the following experimental findings from cancer research:
Table 1: Experimental Evidence of Ubiquitin-Phosphorylation Crosstalk in Cancer
| E3 Ligase/ Enzyme | Kinase/ Phosphorylation Site | Substrate | Functional Outcome | Cancer Type |
|---|---|---|---|---|
| FBXW7 | p53-S33/S37 phosphorylation | p53 | Degradation → Radioresistance | Colorectal Cancer |
| FBXW7 | SOX9 phosphorylation | SOX9 | Degradation → Radiosensitivity | NSCLC |
| TRAF4 | JNK/c-Jun pathway activation | Bcl-xL, MCL-1 | Stabilization → Anti-apoptotic signaling | Colorectal & Oral Cancers |
| ATM | RNF168 phosphorylation | H2A/H2AX | Altered conformation enhances ubiquitination | Multiple Cancers |
| RNF126 | MRE11 phosphorylation | MRE11 | Activates ATM-CHK1 axis → Error-prone repair | Triple-Negative Breast Cancer |
Experimental Approaches for Studying Ubiquitin-Phosphorylation Crosstalk
Deciphering the complex relationship between ubiquitination and phosphorylation requires integrated methodological approaches:
Phosphomimetic and Phosphodeficient Mutagenesis: Replace phosphorylatable serine/threonine residues with glutamic acid (phosphomimetic) or alanine (phosphodeficient) to assess the impact on ubiquitination efficiency and substrate stability. For example, mutating S33/S37 of p53 to alanine prevents FBXW7 recognition and degradation [22].
Co-immunoprecipitation with Phosphospecific Antibodies: Validate phosphorylation-dependent protein interactions by immunoprecipitating with antibodies specific to phosphorylated epitopes, followed by detection of associated E3 ligases.
Kinase Inhibitor Screens Combined with Ubiquitination Assays: Treat cancer cells with targeted kinase inhibitors while monitoring changes in substrate ubiquitination status to identify regulatory kinases.
Mass Spectrometry with Phospho- and Ubiquitin-Enrichment: Combine phosphopeptide enrichment (using TiO2 or IMAC) with diGly remnant enrichment (K-ε-GG antibody) to comprehensively map phosphorylation and ubiquitination sites on the same protein.
Ubiquitin-SUMOylation Crosstalk: Balancing Act in Genome Integrity and Immune Signaling
The interplay between ubiquitination and SUMOylation represents a sophisticated regulatory axis in cancer biology, with these ubiquitin-like modifiers engaging in both antagonistic and cooperative relationships. SUMOylation—the covalent attachment of small ubiquitin-like modifier (SUMO) proteins to target lysines—shares structural and mechanistic similarities with ubiquitination but typically serves distinct cellular functions, primarily modulating protein-protein interactions, subcellular localization, and activity rather than promoting degradation.
SUMO-Directed Ubiquitination
A key mechanism of ubiquitin-SUMOylation crosstalk involves SUMO-targeted ubiquitin ligases (STUbLs) that recognize SUMO-modified proteins and catalyze their ubiquitination. RNF4, a prominent STUbL, binds to poly-SUMO chains through its SUMO-interaction motifs (SIMs) and mediates ubiquitination of the SUMOylated substrate, targeting it for proteasomal degradation. This sequential modification creates a SUMO-to-ubiquitin switch that regulates protein stability in response to specific cellular cues [27].
This crosstalk plays a particularly important role in maintaining genome integrity. Radiation-induced RNF168 activation is amplified by ZNF451-dependent SUMOylation, which subsequently promotes ubiquitination of H2A/H2AX to open chromatin and recruit BRCA1-A complexes, enhancing DNA repair fidelity but potentially promoting radioresistance in cancer cells [22]. This coordinated modification system ensures precise control over DNA damage response pathways.
Competitive Modification and Functional Interplay
SUMOylation and ubiquitination often compete for modification of the same lysine residues on substrate proteins, creating a modification switch that toggles protein function between different states. This competitive relationship is evident in the regulation of transcription factors and chromatin modifiers, where the balance between SUMOylation and ubiquitination determines transcriptional output and chromatin dynamics.
The functional integration between these pathways is further facilitated by shared enzymes. Certain deubiquitinases (DUBs), including USP7 and USP11, also function as SUMO-targeted ubiquitin-specific proteases (STUbPs), cleaving ubiquitin chains from SUMOylated substrates and adding another layer of regulatory complexity [27]. This enzymatic promiscuity enables fine-tuned control of the SUMO-ubiquitin equilibrium in cancer cells.
Table 2: Experimental Evidence of Ubiquitin-SUMOylation Crosstalk in Cancer
| Modification Type | Key Enzymes | Substrate | Functional Outcome | Cancer Context |
|---|---|---|---|---|
| SUMO-directed Ubiquitination | RNF4 (STUbL) | Poly-SUMOylated proteins | Ubiquitination → Degradation | Multiple Cancers |
| SUMO-enhanced Ubiquitination | ZNF451 (E4), RNF168 | H2A/H2AX | Chromatin opening → Enhanced DNA repair | Radioresistant Cancers |
| Competitive Modification | Shared lysine residues | Transcription factors | Functional switching | Altered transcriptional programs |
| SUMOylation-induced Stability | UBC9, PIAS | NSUN2, MDM2 | Prevents ubiquitination → Oncogene stabilization | Colon, Prostate Cancer |
| DeSUMOylation-induced Degradation | SENPs | β-catenin | Enables ubiquitination → Tumor suppressor | Myeloma |
SUMOylation in Tumor Immunity and Therapeutic Targeting
Recent research has illuminated the significance of ubiquitin-SUMOylation crosstalk in regulating anti-tumor immunity. SUMO hyperexpression drives covalent SUMO conjugation to STAT1 at K703, impairing IFN-I/II-triggered STAT1 activation dynamics in several cancers, including human glioblastoma astrocytoma, cervical cancer, and hepatocellular carcinoma [27]. This SUMOylation creates an immune-evasive environment by dampening interferon signaling.
Therapeutic targeting of this crosstalk shows promising preclinical results. Combination of SUMOylation inhibitors such as TAK-981 or 2-D08 with immune checkpoint inhibitors (ICIs) significantly improves tumor prognosis by reactivating anti-tumor immunity [27]. These approaches leverage the ubiquitin-SUMO interplay to overcome resistance to cancer immunotherapy.
Experimental Strategies for Analyzing Ubiquitin-SUMOylation Crosstalk
SIM/UIM Mapping: Identify SUMO-interaction motifs (SIMs) in ubiquitin system components and ubiquitin-interaction motifs (UIMs) in SUMO pathway enzymes through peptide array screens and co-immunoprecipitation.
Tandem Affinity Purification with SUMO/Ubiquitin Traps: Utilize sequential purification with SUMO-binding entities (SUBEs) followed by ubiquitin-binding domains to isolate proteins dually modified or engaged in cross-regulatory complexes.
SUMO Protease Sensitivity Assays: Treat cell lysates with SENP proteases to remove SUMO conjugates while monitoring changes in ubiquitination patterns to identify SUMO-dependent ubiquitination events.
STUbL Activity Assays: Measure ubiquitin ligase activity of candidate STUbLs toward SUMOylated substrates in vitro using recombinant proteins.
The relationship between SUMOylation and ubiquitination pathways can be visualized as follows:
Ubiquitin-Acetylation Crosstalk: Metabolic Regulation and Transcriptional Control
The intersection between ubiquitination and acetylation represents a crucial regulatory nexus in cancer, particularly in the contexts of metabolic reprogramming and epigenetic regulation. These modifications engage in both competitive and cooperative relationships on shared lysine residues, creating a dynamic interplay that influences protein stability, activity, and complex formation.
Competitive Lysine Modifications
Acetylation and ubiquitination directly compete for modification of the same lysine residues, creating a modification switch that determines protein fate. Acetylation neutralizes the positive charge on lysine residues, which can sterically hinder ubiquitination and thereby stabilize proteins by blocking degradation signals. This competition is particularly relevant for metabolic enzymes and transcription factors that require rapid regulation in response to cellular signals.
The reciprocal regulation also occurs, where ubiquitination can influence acetylation dynamics. For instance, acetylation of ubiquitin itself at K6 and K48 inhibits the formation and elongation of ubiquitin chains, adding another layer of complexity to this crosstalk [18]. This chemical modification of ubiquitin represents an emerging area of investigation in cancer biology.
Metabolic Regulation Through Dual Modification
The ubiquitin-acetylation crosstalk plays a significant role in cancer metabolic reprogramming, a hallmark of tumorigenesis. The E3 ligase Parkin facilitates the ubiquitination of pyruvate kinase M2 (PKM2), a key glycolytic enzyme, while the deubiquitinase OTUB2 interacts with PKM2 to inhibit its Parkin-mediated ubiquitination, thereby enhancing glycolysis and accelerating colorectal cancer progression [6]. This balance between ubiquitination and deubiquitination directly controls metabolic flux in cancer cells.
Similarly, ubiquitination critically regulates cancer metabolism by reprogramming processes such as ferroptosis susceptibility, hypoxia adaptation, and nutrient flux. SMURF2-mediated HIF1α degradation compromises hypoxic survival [22], while SOCS2/Elongin B/C-driven SLC7A11 destruction increases ferroptosis sensitivity in liver cancer [22]. These ubiquitination events are potentially modulated by acetylation status, though the precise mechanisms remain under investigation.
Experimental Approaches for Ubiquitin-Acetylation Crosstalk
Acetyl-lysine Mimetic Mutagenesis: Replace target lysines with glutamine (acetyl-mimetic) or arginine (acetylation-deficient) to assess impact on ubiquitination efficiency and protein half-life.
HDAC and HAT Inhibitor Treatments: Modulate cellular acetylation status using pharmacological inhibitors while monitoring changes in ubiquitination patterns via ubiquitin remnant profiling.
Combined Immunoprecipitation with Acetyl- and Ubiquitin-Specific Antibodies: Sequential IP with acetyl-lysine antibodies followed by ubiquitin detection to identify dually modified proteins.
Structural Biology Approaches: Utilize X-ray crystallography or cryo-EM to visualize competitive binding of ubiquitination and acetylation machinery to shared lysine residues.
Research Toolkit: Experimental Methods and Reagent Solutions
Investigating PTM crosstalk requires specialized methodological approaches and research tools. The following table summarizes key experimental methods and reagents essential for deciphering the complex relationships between ubiquitination and other PTMs:
Table 3: Research Reagent Solutions for Studying PTM Crosstalk
| Research Tool Category | Specific Reagents/Assays | Key Applications | Technical Considerations |
|---|---|---|---|
| Ubiquitination Detection | K-ε-GG antibody; TUBE (Tandem Ubiquitin Binding Entities); Ubiquitin remnant profiling | Enrichment and detection of ubiquitinated proteins; DiGly remnant mass spectrometry | Lysis conditions critical to preserve modifications; Proteasome inhibition often required |
| SUMOylation Tools | SUMO-traps (SUBEs); SENP proteases; SUMOylation consensus mutagenesis | Isolation of SUMOylated proteins; Validation of SUMO-dependent functions | Rapid denaturation needed to preserve SUMO conjugates; Multiple paralogs add complexity |
| Phosphorylation Resources | Phosphospecific antibodies; Phos-tag gels; Kinase inhibitor libraries | Mapping phosphodegrons; Assessing phosphorylation-dependent ubiquitination | Phosphatase inhibition essential; Context-dependent effects |
| Acetylation Reagents | Acetyl-lysine antibodies; HDAC/HAT inhibitors; Acetyl-mimetic mutants | Competitive modification studies; Metabolic regulation analysis | Short inhibitor treatments preferred to avoid compensatory mechanisms |
| Genetic Manipulation | CRISPR/Cas9 knockout; siRNA/shRNA knockdown; Dominant-negative constructs | Functional validation of specific enzymes; Pathway manipulation | Redundancy challenges; Off-target effects monitoring |
| Proteomic Approaches | Sequential IP; Tandem affinity purification; Cross-linking mass spectrometry | Identification of modification networks; Complex mapping | Bioinformatics expertise required; Validation essential |
| Structural Biology | X-ray crystallography; Cryo-EM; NMR spectroscopy | Molecular mechanism elucidation; Interface mapping | Technical complexity; May require truncated constructs |
Integrated Workflow for PTM Crosstalk Analysis
A comprehensive approach to studying PTM crosstalk involves multiple complementary techniques:
Initial Discovery Phase: Utilize quantitative proteomics (SILAC, TMT) with PTM-specific enrichment to identify coordinated changes in ubiquitination, phosphorylation, SUMOylation, and acetylation in response to specific cancer-relevant stimuli.
Validation Stage: Employ targeted methods such as Western blotting with modification-specific antibodies, co-immunoprecipitation, and proximity ligation assays (PLA) to confirm interactions and modifications.
Functional Characterization: Implement genetic approaches (CRISPR, RNAi) to modulate specific enzymes combined with phenotypic assays relevant to cancer biology (proliferation, invasion, therapy resistance).
Mechanistic Elucidation: Apply structural biology and biophysical techniques to understand molecular details of modification interfaces and enzymatic regulation.
The following diagram illustrates a recommended experimental workflow for investigating PTM crosstalk:
Therapeutic Implications and Future Perspectives
The intricate crosstalk between ubiquitination and other PTMs presents both challenges and opportunities for cancer therapy. Understanding these networks enables the development of innovative therapeutic strategies that exploit nodal points in PTM cross-regulation.
Targeting PTM Crosstalk in Precision Oncology
The contextual duality of many ubiquitin system components—exemplified by FBXW7's opposing roles in different cancer types—underscores the importance of biomarker-guided therapeutic approaches [22]. Successful targeting of PTM crosstalk requires careful patient stratification based on genetic background, PTM enzyme expression patterns, and metabolic dependencies.
PROTACs (Proteolysis Targeting Chimeras) represent a groundbreaking application of ubiquitin biology that leverages the cell's natural degradation machinery. These bifunctional molecules recruit E3 ubiquitin ligases to target proteins of interest, inducing their ubiquitination and degradation. EGFR-directed PROTACs selectively degrade β-TrCP substrates in EGFR-dependent tumors (e.g., lung and head/neck squamous cell carcinomas), suppressing DNA repair while minimizing impact on normal tissues [22]. The efficacy of PROTACs can be modulated by the phosphorylation status of their targets, creating opportunities to integrate PTM crosstalk understanding into drug design.
Combination Therapies and Resistance Management
Targeting single components of PTM networks often leads to adaptive resistance mechanisms, necessitating rational combination approaches. For instance, combining SUMOylation inhibitors with immune checkpoint blockers addresses multiple vulnerabilities simultaneously: TAK-981 or 2-D08 (SUMOylation inhibitors) combined with anti-PD-1/PD-L1 antibodies significantly improve tumor prognosis in preclinical models [27].
Radiation-responsive therapeutic platforms represent another innovative approach that leverages PTM crosstalk. Radiotherapy-triggered PROTAC (RT-PROTAC) prodrugs activated by tumor-localized X-rays degrade BRD4/2, synergizing with radiotherapy in breast cancer models [22]. Similarly, X-ray-responsive nanomicelles selectively release PROTACs within irradiated tumors, creating spatial control over ubiquitin-mediated protein degradation [22].
Future Research Directions
Several emerging areas warrant further investigation in the field of PTM crosstalk:
Branched Ubiquitin Chains: The functional significance of heterotypic ubiquitin chains and their intersection with other PTMs remains largely unexplored territory with potential therapeutic implications.
Single-Cell PTM Analysis: Developing methods to map PTM crosstalk at single-cell resolution will reveal tumor heterogeneity and microenvironment-specific regulation.
Chemical Biology Tools: Creating more selective inhibitors and activators for PTM-writing, -reading, and -erasing enzymes will enable precise manipulation of these networks.
Computational Modeling: Integrating multi-omics PTM data into predictive models will help identify key regulatory nodes and optimize combination therapy schedules.
The dynamic and reversible nature of ubiquitination and its crosstalk with other PTMs offers unique clinical advantages for therapeutic intervention. As our understanding of these complex networks deepens, so too will our ability to develop precisely targeted interventions that disrupt cancer-specific pathways while sparing normal tissue, ultimately advancing toward more effective and personalized cancer treatments.
Advanced Methodologies for Mapping and Targeting the Ubiquitin Code in Malignancies
Mass Spectrometry-Based Proteomics and Linkage-Specific Antibodies for Ubiquitin Code Analysis
The post-translational modification of proteins by ubiquitin is a master regulator of cellular function, controlling processes as critical as protein degradation, DNA damage repair, and signal transduction. The remarkable diversity of ubiquitin signaling—termed the "ubiquitin code"—arises from the ability of ubiquitin to form polymers (polyubiquitin chains) through eight distinct linkage sites (seven lysine residues and the N-terminal methionine). These chains vary in their topology, length, and function, creating a complex regulatory language that cells use to coordinate physiological processes [28] [6]. In cancer biology, deciphering this code is of paramount importance, as malignant cells often hijack or dysregulate ubiquitin signaling to drive tumor proliferation, metastasis, and therapeutic resistance [8] [29].
The functional consequences of ubiquitination are profoundly linkage-dependent. K48-linked ubiquitin chains primarily target substrate proteins for proteasomal degradation, while K63-linked chains typically serve as scaffolds for non-proteolytic signaling complexes, such as those activating the NF-κB pathway [29] [28]. The roles of less abundant "atypical" chains (K6, K11, K27, K29, K33) are increasingly being elucidated in cancer contexts. For instance, K29-linked chains have been implicated in proteotoxic stress response and the regulation of key chromatin modifiers like the histone methyltransferase SUV39H1, thereby influencing the cancer epigenome [30] [31]. Similarly, K27-linked chains have been shown to be critical for cell fitness and are associated with p97 activity in the nucleus [31].
For researchers investigating ubiquitin code alterations in cancer, two technological pillars have proven indispensable: mass spectrometry (MS)-based proteomics and linkage-specific antibodies. These methodologies enable the direct detection, quantification, and characterization of ubiquitin chain architectures on cellular substrate proteins, moving the field beyond indirect genetic approaches [32]. This whitepaper provides an in-depth technical guide to these core methodologies, detailing experimental protocols, analytical workflows, and their application in cancer research.
Methodological Pillars: Principles and Technologies
Mass Spectrometry-Based Proteomics for Ubiquitin Analysis
Mass spectrometry-based proteomics has become the cornerstone for system-wide investigations of protein ubiquitination. The primary strategy for identifying ubiquitination sites involves enriching ubiquitinated peptides from complex protein digests and analyzing them via high-resolution liquid chromatography-tandem mass spectrometry (LC-MS/MS) [33].
A critical innovation in this field is ubiquitin remnant profiling (also known as di-glycine proteomics). When ubiquitylated proteins are digested with the protease trypsin, a signature di-glycine (Gly-Gly) remnant (~114.04 Da mass shift) remains attached to the modified lysine residue [33]. This di-glycine modification serves as a mass tag that can be pinpointed by MS, allowing for the precise localization of the ubiquitination site within the protein sequence. To overcome the challenge of low stoichiometry, specific monoclonal antibodies (e.g., GX41) have been developed that selectively recognize the di-glycine adduct on lysine, enabling the highly specific enrichment of these modified peptides prior to LC-MS/MS analysis [33].
For quantitative analyses, ubiquitin remnant profiling is typically combined with isotopic or isobaric labeling techniques, such as:
- SILAC (Stable Isotope Labeling by Amino Acids in Cell Culture): Metabolic labeling that incorporates stable isotopes into cellular proteins.
- TMT (Tandem Mass Tagging): Chemical labeling of peptides with isobaric tags for multiplexed relative quantification.
These approaches allow researchers to compare the abundance of thousands of ubiquitination sites across different conditions—for example, between normal and cancerous tissues, or in response to therapeutic interventions [33].
Beyond site identification, advanced MS methods are being developed to characterize ubiquitin chain topology. These include techniques like Ub-clipping and the use of linkage-specific ubiquitin-binding entities (TUBEs) to enrich for proteins modified with specific chain types before MS analysis [30] [28]. A significant challenge, however, is that tryptic digestion also produces a di-glycine remnant from the ubiquitin-like modifiers NEDD8 and ISG15. Careful experimental design and data interpretation are required to distinguish these modifications from canonical ubiquitination [33].
Linkage-Specific Antibodies and Affinity Reagents
Linkage-specific antibodies represent a powerful complementary approach to MS, allowing for the direct detection and visualization of specific ubiquitin chain types in cells and tissues. These reagents are generated by immunizing animals with synthetically produced diubiquitin of defined linkage, resulting in antibodies that can distinguish, for instance, K48-linked from K63-linked chains with high specificity [32] [30].
The utility of these antibodies extends across multiple platforms:
- Western Blotting: For detecting the presence and relative abundance of specific chain linkages in whole-cell lysates.
- Immunofluorescence/Immunohistochemistry: For visualizing the subcellular localization of specific ubiquitin signals within fixed cells or tissue sections.
- Immunoprecipitation (IP): For enriching proteins modified with a specific chain type prior to downstream identification by MS [28].
Recent advances have expanded the toolkit beyond traditional antibodies to include engineered synthetic antigen-binding fragments (sABs) and affimers. For example, the sAB-K29 was specifically developed to recognize K29-linked diubiquitin and was instrumental in uncovering the role of K29 linkages in proteotoxic stress response and cell cycle regulation [30]. The crystal structure of sAB-K29 bound to K29-linked diubiquitin revealed the molecular basis for its exquisite linkage specificity [30].
Similarly, linkage-specific Ubiquitin Binding Entities (TUBEs) have been developed. These are tandem-repeated ubiquitin-binding domains (UBDs) engineered to exhibit high affinity for ubiquitin chains and, in some cases, linkage preference. TUBEs can be used to stabilize ubiquitin conjugates by protecting them from deubiquitinases (DUBs) during cell lysis and to enrich ubiquitinated proteins from complex mixtures for subsequent analysis [7] [28].
Experimental Protocols and Workflows
Workflow for Ubiquitin Remnant Profiling by Mass Spectrometry
The following workflow outlines the key steps for the proteome-wide identification of ubiquitination sites using the di-glycine remnant capture method. This process is foundational for quantifying changes in the ubiquitinome in response to cellular perturbations, such as DNA damage in cancer cells.
Diagram 1: Ubiquitin Remnant Profiling Workflow
Step-by-Step Protocol:
- Cell Culture and Treatment: Culture cells under experimental conditions (e.g., cancer cell lines treated with a chemotherapeutic agent or DUB inhibitor). For quantitative comparisons using SILAC, grow cells in "light" (L-lysine/ L-arginine), "medium" (D4-lysine/ (^{13})C6-arginine), or "heavy" ( (^{13})C6-(^{15})N2-lysine/ (^{13})C6-(^{15})N4-arginine) media [33].
- Protein Extraction and Denaturation: Lyse cells in a denaturing buffer (e.g., containing SDS or urea) to inactivate endogenous DUBs and proteases, thereby preserving the native ubiquitination state. A common method is to use 8 M urea lysis buffer.
- Proteolytic Digestion: Digest the extracted proteins into peptides using a sequence-specific protease, typically trypsin. Trypsin cleaves the ubiquitin molecule after arginine 74, leaving the C-terminal Gly-Gly remnant of ubiquitin covalently attached via an isopeptide bond to the modified lysine on the substrate peptide [33].
- Peptide-Level Enrichment: Dilute the digested peptide mixture to reduce the concentration of denaturants. Incubate with anti-di-glycine (diGly) remnant antibody (e.g., covalently coupled to beads) to specifically immunoaffinity-capture peptides containing the Gly-Gly modification. After extensive washing, elute the enriched peptides [33].
- LC-MS/MS Analysis: Separate the enriched peptides using reverse-phase nano-liquid chromatography and analyze them with a high-resolution tandem mass spectrometer. The instrument is set to perform data-dependent acquisition, automatically selecting the most abundant precursor ions for fragmentation.
- Data Analysis and Site Mapping: Process the raw MS data using software tools like MaxQuant or Proteome Discoverer. The software identifies peptides by matching the observed MS/MS spectra to a protein sequence database. A key search parameter is the variable modification of lysine with the diGly remnant (+114.04293 Da), which allows for the confident localization of ubiquitination sites [33].
Protocol for Immunoprecipitation with Linkage-Specific Antibodies
This protocol describes the use of linkage-specific antibodies to enrich for proteins modified with a particular ubiquitin chain linkage, which can be followed by Western blotting or MS-based identification.
Detailed Protocol:
- Cell Lysis: Lyse cells in a non-denaturing (native) lysis buffer (e.g., RIPA buffer) supplemented with DUB inhibitors (e.g., N-ethylmaleimide or PR-619) and protease inhibitors. Native lysis preserves protein-protein interactions and the structure of ubiquitin chains but requires DUB inhibition to prevent chain disassembly during processing.
- Pre-clearing: Incubate the cell lysate with control beads (e.g., Protein A/G beads) for 30-60 minutes at 4°C. This step removes proteins that bind non-specifically to the beads, reducing background signal.
- Immunoprecipitation: Incubate the pre-cleared lysate with the linkage-specific antibody (e.g., anti-K48, anti-K63, anti-K29) conjugated to Protein A/G beads. Alternatively, incubate the lysate with the free antibody first, followed by the addition of beads. Perform this incubation for 2-4 hours to overnight at 4°C with gentle rotation.
- Washing: Pellet the beads by gentle centrifugation and wash them 3-5 times with ice-cold lysis buffer to remove unbound proteins.
- Elution and Analysis:
- For Western Blotting: Resuspend the beads in 2X SDS-PAGE loading buffer and boil for 5-10 minutes to elute the immunoprecipitated proteins. Separate the proteins by SDS-PAGE and transfer to a membrane. Probe the membrane with a pan-ubiquitin antibody (e.g., FK2) or an antibody against a protein of interest to confirm the presence and linkage type of ubiquitin conjugates [28].
- For Mass Spectrometry: After washing, the beads can be subjected to on-bead digestion. Add a denaturant, reduce disulfide bonds with DTT, alkylate with iodoacetamide, and digest with trypsin. The resulting peptides, derived from the ubiquitinated proteins and their interactors, are then analyzed by LC-MS/MS to identify the specific proteins enriched by the linkage-specific antibody [28].
The Scientist's Toolkit: Key Research Reagents
The following table summarizes essential reagents for studying the ubiquitin code, as featured in the cited literature.
Table 1: Key Research Reagent Solutions for Ubiquitin Code Analysis
| Reagent Category | Specific Example | Function and Application | Key Feature |
|---|---|---|---|
| Linkage-Specific Antibodies | Anti-K48, Anti-K63 [32] | Western Blot, IP, IHC: Detect or enrich proteins modified with specific chain linkages. | High specificity for a single ubiquitin linkage type. |
| Synthetic Antibody Fragments | sAB-K29 [30] | Specific recognition of K29-linked ubiquitin chains for imaging and enrichment. | Engineered for high specificity; crystal structure with antigen available. |
| Ubiquitin-Binding Domains | Tandem Ubiquitin Binding Entities (TUBEs) [28] | Pan-selective enrichment of ubiquitinated proteins; stabilizes ubiquitin conjugates during lysis. | Protects ubiquitin chains from deubiquitinases (DUBs). |
| Ubiquitin Remnant Antibodies | Anti-diGly (e.g., GX41) [33] | Enrichment of ubiquitinated peptides for mass spectrometry (ubiquitin remnant profiling). | Enables system-wide mapping of ubiquitination sites. |
| Activity-Based Probes | Ubiquitin-based probes [28] | Labeling and detection of active DUBs or E3 ligases in cell lysates or live cells. | Covalently binds active enzymes, reporting on their functional state. |
| Defined Ubiquitin Chains | Recombinant K29-, K48-, K63-linked diUb/TriUb [30] | Standards for antibody validation, in vitro assays, and structural studies. | Precisely defined linkage and structure. |
Quantitative Insights: Ubiquitin Linkages in Cellular Function and Cancer
The functional output of ubiquitination is critically determined by chain linkage type. Quantitative proteomic studies and linkage-specific tools have revealed the relative abundance and distinct roles of various ubiquitin chains in cellular homeostasis and disease.
Table 2: Functions and Quantitative Roles of Ubiquitin Chain Linkages
| Ubiquitin Linkage | Relative Abundance & Key Functions | Relevance in Cancer & Experimental Evidence |
|---|---|---|
| K48-linked | - Most abundant degradative signal [28].- Directs substrates to the 26S proteasome. | - Contextual duality in radioresistance: FBXW7 degrades p53 (radioresistance) in some contexts, but SOX9 (radiosensitization) in others [29]. |
| K63-linked | - Major non-detegradative signaling scaffold [29].- Regulates NF-κB activation, DNA repair, endocytosis. | - Promotes survival: TRAF4 uses K63 chains to activate JNK/c-Jun and upregulate anti-apoptotic Bcl-xL/MCL-1 [29].- DNA repair: RNF8/RNF168 build K63/K27 scaffolds at DNA double-strand breaks [31]. |
| K29-linked | - Low abundance; associated with proteotoxic stress and cell cycle [30].- Forms heterotypic branched chains with K48 for degradation. | - Epigenetic regulation: TRIP12-mediated K29 ubiquitination targets SUV39H1 for degradation, regulating H3K9me3 marks [31].- DUB resistance: K29 linkages overcome OTUD5 deubiquitination to facilitate degradation [7]. |
| K27-linked | - Low abundance (<0.5%) [31].- Critical for cell fitness, nuclear p97 activity [31]. | - DNA damage repair: RNF168 builds K27-linked chains at DNA damage sites for repair factor recruitment [31]. |
| K11-linked | - Contributes to proteasomal degradation, cell cycle regulation [7]. | - Branched chains: K11/K48 branched chains serve as priority signals for proteasomal degradation [7]. |
| K6-linked | - Very low abundance; role in DNA damage response, mitophagy [31]. | - Stress response: Upregulated during proteotoxic stress and implicated in resolving RNA-protein crosslinks [31]. |
Application in Cancer Research: Decoding Oncogenic Signaling
The methodologies detailed herein are powerfully applied to unravel specific mechanisms of cancer pathogenesis and therapy resistance. The following pathway diagram synthesizes findings from multiple studies to illustrate how ubiquitin linkages regulate a key oncogenic process: radiation resistance in tumors.
Diagram 2: Ubiquitin Linkages in Radiotherapy Resistance
This diagram illustrates how radiotherapy perturbs the ubiquitin code, leading to therapy resistance through linkage-specific mechanisms. For example, mass spectrometry and linkage-specific antibodies revealed that the E3 ligase TRIM26 stabilizes the antioxidant enzyme GPX4 via K63-linked ubiquitination, thereby protecting glioma cells from radiation-induced ferroptosis [29]. Conversely, K48-linked ubiquitination by FBXW7 can promote resistance by degrading tumor suppressors like p53 in certain cancers [29]. Meanwhile, K29-linked chains assembled by TRIP12 control the degradation of chromatin regulators like SUV39H1, linking this atypical chain to epigenetic dysregulation in cancer [31]. These findings, enabled by the tools described in this guide, highlight specific E3 ligases and DUBs as promising therapeutic targets to overcome treatment resistance.
The synergistic use of mass spectrometry-based proteomics and linkage-specific affinity reagents has fundamentally transformed our ability to decipher the complex language of the ubiquitin code. As these technologies continue to evolve—offering greater sensitivity, specificity, and throughput—they will undoubtedly uncover deeper layers of regulation in both normal physiology and cancer biology. The integration of these methodologies is already paving the way for novel therapeutic strategies, such as the development of PROTACs (Proteolysis-Targeting Chimeras) that exploit the ubiquitin-proteasome system to degrade oncogenic proteins, and the targeting of specific E3 ligases or DUBs that are dysregulated in cancer [29] [6]. For researchers in oncology and drug development, mastering these tools is no longer a niche specialty but an essential component of cracking the molecular code of cancer.
High-Throughput Screening for E3 Ligase and DUB Modulators in Drug Discovery
The ubiquitin system represents a master regulatory network controlling cellular protein homeostasis, with profound implications for cancer development and treatment. Ubiquitination—a reversible post-translational modification—orchestrates critical oncogenic pathways through a coordinated enzymatic cascade involving E1 activating, E2 conjugating, and E3 ligase enzymes, alongside deubiquitinating enzymes (DUBs) that reverse this process [34]. The specificity of this system is largely determined by E3 ligases, which recognize substrate proteins, and DUBs, which fine-tune ubiquitination dynamics. Dysregulation of the ubiquitin code is now recognized as a hallmark of cancer pathogenesis, driving tumor proliferation, metastasis, and therapeutic resistance [8] [35]. For instance, recent studies have revealed that ubiquitination dynamically regulates the stability, membrane localization, and signaling transduction of RAS proteins, the most frequently mutated oncoproteins in human cancers [8].
The therapeutic potential of targeting ubiquitination pathways remains largely untapped, with many E3 ligases and DUBs representing unexplored drug targets. This whitepaper provides a comprehensive technical guide for deploying high-throughput screening (HTS) methodologies to identify modulators of E3 ligases and DUBs, framed within the context of ubiquitin code alterations in cancer. We present detailed experimental protocols, data analysis frameworks, and visualization tools to accelerate drug discovery in this emerging frontier.
Biological Background: Ubiquitin Signaling in Cancer Pathways
The Ubiquitin-Proteasome System
The ubiquitin-proteasome system (UPS) comprises a sophisticated enzymatic cascade that regulates protein degradation and function:
- E1 activating enzymes (2 in humans): Initiate ubiquitination by activating ubiquitin in an ATP-dependent manner
- E2 conjugating enzymes (~40 in humans): Serve as intermediaries that carry activated ubiquitin
- E3 ligases (>600 in humans): Provide substrate specificity by recognizing target proteins and facilitating ubiquitin transfer
- Deubiquitinating enzymes (DUBs) (~100 in humans): Reverse ubiquitination by cleaving ubiquitin from modified substrates [34]
This system generates a complex ubiquitin code consisting of monoubiquitination or polyubiquitin chains of different linkages (e.g., Lys48-linked for proteasomal degradation, Lys63-linked for signaling activation) that determine diverse functional outcomes for modified proteins [34].
Ubiquitination Alterations in Oncogenesis
Ubiquitination dysregulation represents a fundamental mechanism in cancer development, with E3 ligases and DUBs operating as both oncogenes and tumor suppressors. A recent pan-cancer analysis of ubiquitination networks across 4,709 patients from 26 cohorts revealed that ubiquitination patterns effectively stratify patients into distinct prognostic groups and are associated with immunotherapy response [35]. Key oncogenic pathways regulated by ubiquitination include:
- MYC signaling: The OTUB1-TRIM28 ubiquitination axis modulates MYC pathway activity and influences patient prognosis across multiple cancer types [35]
- RAS dynamics: Ubiquitination controls the stability, membrane localization, and signaling output of mutant RAS proteins [8]
- Histological fate decisions: Ubiquitination scores correlate with squamous or neuroendocrine transdifferentiation in adenocarcinoma, contributing to therapy resistance [35]
- Immune checkpoint regulation: Ubiquitination influences PD-1/PD-L1 protein levels in the tumor microenvironment, thereby modulating immunotherapy efficacy [35]
Table 1: Key Ubiquitin System Components as Cancer Therapeutic Targets
| Component | Representative Targets | Cancer Relevance | Therapeutic Approach |
|---|---|---|---|
| E3 Ligases | CRBN, SCF complex, TRIM28 | RAS stabilization, MYC signaling, Histological fate | Molecular glue degraders, PROTACs [36] |
| DUBs | OTUB1, USP7 | Prognostic stratification, Immune regulation | Small molecule inhibitors [35] |
| Ligase Complex | Cullin-RING ligases | Substrate recognition for degradation | Cullin neddylation inhibitors |
High-Throughput Screening Methodologies
HTS Platform Fundamentals
High-throughput screening employs automated, large-scale experimental approaches to rapidly test thousands to millions of compounds for biological activity against therapeutic targets. The global HTS market, valued at USD 32.0 billion in 2025 and projected to reach USD 82.9 billion by 2035, reflects the critical role of these technologies in modern drug discovery [37]. HTS platforms for ubiquitin system targets leverage several core technological components:
- Robotic automation and liquid handling systems for assay assembly and compound dispensing
- Microplate readers for absorbance, luminescence, and fluorescence detection
- Assay miniaturization (384-well, 1536-well formats) to reduce reagent costs and increase throughput
- Advanced detection technologies including fluorescence resonance energy transfer (FRET), time-resolved FRET (TR-FRET), and AlphaScreen [38]
For E3 ligases and DUBs, both biochemical (cell-free) and cell-based screening approaches offer complementary advantages, as summarized in Table 2.
Table 2: Comparison of HTS Approaches for E3 Ligase and DUB Modulators
| Screening Type | Throughput | Key Assay Technologies | Advantages | Limitations |
|---|---|---|---|---|
| Biochemical HTS | Ultra-high (>100,000 compounds/day) | TR-FRET, Fluorescence polarization, AlphaScreen | Direct target engagement, Minimal cellular complexity | Lacks cellular context, Membrane impermeability issues |
| Cell-Based HTS | High (10,000-100,000 compounds/day) | Reporter gene assays, Protein complementation, High-content imaging | Physiological relevance, Accounts for cell permeability | More complex data interpretation, Higher variability |
| Phenotypic HTS | Medium-high (1,000-50,000 compounds/day) | High-content imaging, Gene expression profiling | Unbiased discovery, Functional outcomes | Target deconvolution required |
Experimental Protocols
TR-FRET Ubiquitination Assay Protocol
Time-resolved FRET (TR-FRET) assays represent a robust biochemical HTS approach for identifying E3 ligase modulators. This protocol outlines a standardized method for screening compound libraries against E3 ligase activity:
Reagents and Materials:
- Recombinant E1, E2, E3 enzymes (commercially available or purified in-house)
- Biotinylated-ubiquitin and FLAG-tagged substrate protein
- TR-FRET detection antibodies: Europium-labeled anti-FLAG and APC-labeled streptavidin
- Assay buffer: 50 mM Tris-HCl (pH 7.5), 50 mM NaCl, 5 mM MgCl₂, 1 mM DTT, 0.01% Tween-20
- ATP solution (10 mM stock)
- 384-well low-volume white plates
Procedure:
- Assay Assembly: Dispense 5 μL of compound (in DMSO, final concentration 10 μM) or DMSO control to appropriate wells using automated liquid handling
- Enzyme/Substrate Mixture Preparation: Combine E1 (50 nM), E2 (500 nM), E3 (50-100 nM), and FLAG-substrate (200 nM) in assay buffer
- Reaction Initiation: Add 5 μL of enzyme/substrate mixture to each well, followed by 5 μL of ubiquitination master mix containing biotin-ubiquitin (2 μM) and ATP (50 μM)
- Incubation: Incubate plates at 25°C for 60 minutes with gentle shaking
- Detection: Add 5 μL of detection mixture containing anti-FLAG-Eu³⁺ (2 nM) and streptavidin-APC (20 nM) in detection buffer (50 mM Tris-HCl pH 7.5, 100 mM KF, 0.1% BSA)
- Signal Measurement: Incubate 30 minutes at 25°C, then measure TR-FRET signal using compatible plate reader (excitation: 320 nm, emission: 615 nm and 665 nm)
- Data Acquisition: Calculate TR-FRET ratio (665 nm/615 nm) for each well
Quality Control Parameters:
- Z'-factor ≥0.5 for robust assay performance
- Signal-to-background ratio ≥3:1
- Coefficient of variation <10% for control wells
Cell-Based DUB Activity Reporter Assay
For identifying DUB inhibitors in a cellular context, this protocol utilizes a ubiquitin-PLA2 (phospholipase A2) reporter system:
Reagents and Materials:
- DUB-PLA2 reporter cell line (stable expression of ubiquitin-PLA2 fusion protein)
- Compound library (1,000-10,000 compounds in 384-well format)
- PLA2 substrate: Red/Green cPLA2 assay kit (commercially available)
- Cell culture medium appropriate for reporter cell line
- Lysis buffer: 20 mM Tris-HCl (pH 7.5), 150 mM NaCl, 1% Triton X-100, protease inhibitors
- 384-well tissue culture-treated plates
Procedure:
- Cell Seeding: Dispense 50 μL of reporter cells (20,000 cells/mL) into each well of 384-well plates
- Incubation: Culture cells for 24 hours at 37°C, 5% CO₂
- Compound Treatment: Add 100 nL of compound (in DMSO) or controls to appropriate wells (final concentration 10 μM)
- Incubation: Incubate plates for 6 hours at 37°C, 5% CO₂
- Lysis: Remove medium and add 20 μL of lysis buffer per well, incubate 15 minutes at room temperature
- PLA2 Activity Measurement: Add 20 μL of PLA2 substrate solution per well, incubate 30 minutes at 37°C
- Signal Detection: Measure fluorescence (excitation/emission: 535/585 nm) using plate reader
- Data Analysis: Normalize signals to DMSO controls (100% activity) and positive inhibition controls (0% activity)
Fragment-Based Screening for Ubiquitin System Targets
Fragment-based drug discovery (FBDD) represents a powerful complementary approach to traditional HTS, particularly for challenging ubiquitin system targets:
Library Design:
- Library Size: 500-2,000 compounds following "rule of 3" (MW <300 Da, ≤3 H-bond donors, ≤3 H-bond acceptors, logP ≤3) [34]
- Covalent Fragments: Include electrophilic warheads (acrylamides, chloroacetamides) for cysteine-targeting DUBs and E3 ligases
- Structural Diversity: Maximize coverage of chemical space with minimal library size
Screening Methodology:
- Primary Screening: Employ surface plasmon resonance (SPR) or differential scanning fluorimetry (DSF) for initial hit identification
- Hit Validation: Confirm binding using orthogonal methods (ITC, NMR)
- Structural Characterization: Determine fragment-bound structures using X-ray crystallography (e.g., XChem platform)
- Fragment Evolution: Grow, merge, or link validated fragments into lead compounds with increased affinity and specificity [34]
Data Analysis and Hit Validation
Primary Data Processing and Normalization
Robust data analysis pipelines are essential for distinguishing true hits from assay artifacts in HTS campaigns:
Normalization Methods:
- Plate-based normalization: Convert raw signals to percentage activity relative to plate controls
- B-score normalization: Remove systematic plate position effects using robust regression
- Z-score transformation: Standardize signals based on plate mean and standard deviation
Hit Selection Criteria:
- Activity Threshold: Typically >3 standard deviations from mean or >50% inhibition/activation
- Ligand Efficiency: For fragment screens, prioritize hits with high ligand efficiency (>0.3 kcal/mol/heavy atom)
- Dose-Response Confirmation: Retest hits in concentration-response format to determine IC₅₀/EC₅₀ values
Counter-Screening and Triaging
Artifact Identification:
- Aggregation Detection: Test hits in presence of non-ionic detergents (e.g., 0.01% Triton X-100)
- Redox Activity: Assess interference with redox-sensitive assay components
- Fluorescence/Quenching: Counter-screen in assay-independent fluorescence interference tests
Selectivity Profiling:
- Related Enzyme Families: Test hits against panels of related E3 ligases or DUBs
- Cellular Toxicity: Assess general cytotoxicity in relevant cell lines (e.g., MTT assay)
- Mechanistic Studies: Employ biochemical techniques (SPR, ITC) to characterize binding kinetics and mechanism of action
The Scientist's Toolkit: Essential Research Reagents and Platforms
Table 3: Key Research Reagent Solutions for HTS of E3 Ligase and DUB Modulators
| Reagent Category | Specific Examples | Function/Application | Commercial Sources |
|---|---|---|---|
| Recombinant Enzymes | E1 (UBA1), E2 (UbcH5a), E3 (CRBN, SCF complexes) | Biochemical ubiquitination assays | Boston Biochem, R&D Systems, Enzo Life Sciences |
| Activity Assay Kits | Ubiquitinylation, DUB activity, Proteasome activity | Standardized assay protocols | Cayman Chemical, LifeSensors, BPS Bioscience |
| Cellular Reporters | Ubiquitin-PLA2, Tethering assays, NanoBIT | Cell-based screening systems | Promega, DiscoverX |
| Detection Reagents | TR-FRET pairs, Luminescent substrates, Fluorescent antibodies | Signal generation and detection | Cisbio, PerkinElmer, Thermo Fisher |
| Fragment Libraries | DSi-Poised library, Covalent fragment collections | FBDD screening campaigns | Diamond-SGC Consortium, commercial vendors |
| Specialized Platforms | XChem crystallography, DNA-encoded libraries | Advanced screening technologies | Diamond Light Source, X-Chem |
Integration with Drug Discovery Pipelines
Hit-to-Lead Optimization
Validated HTS hits require systematic optimization to develop lead compounds with drug-like properties:
Structure-Activity Relationship (SAR) Studies:
- Analog Testing: Screen commercially available structural analogs to establish preliminary SAR
- Focused Library Design: Synthesize compound arrays exploring key structural modifications
- Property Optimization: Balance potency with physicochemical properties (lipophilicity, solubility, metabolic stability)
Structural Biology Support:
- Co-crystallization: Determine high-resolution structures of compound-target complexes
- Structure-Based Design: Utilize structural insights to guide compound optimization
- Molecular Modeling: Employ computational chemistry to predict binding modes and suggest modifications
Emerging Technologies and Future Directions
The HTS landscape for ubiquitin system targets is rapidly evolving with several emerging technologies:
DNA-Encoded Libraries (DEL):
- Enable screening of ultra-large compound collections (>1 billion members) through tag-mediated identification
- Particularly valuable for protein-protein interaction targets like E3 ligase-substrate interfaces [36]
Cryo-Electron Microscopy (cryo-EM):
- Facilitates structural characterization of large E3 ligase complexes in solution
- Provides insights into conformational dynamics and allosteric regulation
Artificial Intelligence (AI) and Machine Learning:
- Predict compound activity and selectivity from chemical structure
- Design novel chemotypes with optimized properties for ubiquitin system targets
- Analyze high-dimensional screening data to identify complex patterns and relationships [36]
Visualizing Screening Workflows and Ubiquitin Pathways
High-Throughput Screening Decision Pathway
Ubiquitin-Proteasome System in Cancer
High-throughput screening represents an indispensable approach for targeting the ubiquitin system in cancer therapeutics. By implementing robust biochemical and cell-based screening protocols, researchers can identify novel chemical starting points for modulating E3 ligases and DUBs—key regulators of oncogenic pathways. The integration of traditional HTS with emerging technologies like fragment-based screening, DNA-encoded libraries, and AI-driven design promises to accelerate the discovery of transformative therapies that manipulate the ubiquitin code against cancer. As our understanding of ubiquitination alterations in cancer deepens, HTS methodologies will continue to evolve, enabling more precise targeting of this complex regulatory system to address unmet needs in oncology.
Targeted protein degradation (TPD) represents a paradigm shift in drug discovery, moving beyond traditional occupancy-driven inhibition toward event-driven elimination of disease-causing proteins. This whitepaper examines how proteolysis-targeting chimeras (PROTACs) and molecular glues exploit the ubiquitin-proteasome system to degrade pathogenic proteins, with particular emphasis on their application in cancer research where ubiquitin code alterations drive oncogenesis. These technologies have unlocked therapeutic possibilities for previously "undruggable" targets, including transcription factors, scaffolding proteins, and mutant oncoproteins. With the first PROTAC molecules completing Phase III clinical trials and molecular glues already approved for hematological malignancies, TPD modalities are poised to transform cancer therapy. This technical guide provides comprehensive mechanistic insights, current clinical landscape analysis, experimental methodologies, and essential research tools for investigating and applying these innovative therapeutic strategies.
The ubiquitin-proteasome system (UPS) maintains cellular proteostasis through precisely orchestrated ubiquitin codes—specific patterns of ubiquitin chain linkage that determine protein fate. In cancer development, alterations in this ubiquitin code contribute significantly to oncogenic transformation, tumor progression, and therapeutic resistance. Oncoproteins may escape normal degradation pathways while tumor suppressors may be prematurely targeted for destruction, creating imbalanced signaling networks that drive malignant phenotypes [8].
Targeted protein degradation represents a strategic approach to correct these ubiquitin code alterations by reprogramming E3 ubiquitin ligase activity against specific pathological proteins. Unlike traditional inhibitors that merely block protein function temporarily, TPD modalities achieve complete protein removal through the catalytic redirection of ubiquitin machinery [39]. This fundamental shift from occupancy-driven to event-driven pharmacology addresses critical limitations of conventional therapeutics, particularly for proteins lacking defined binding pockets or those that have developed resistance mutations [40].
The integration of TPD strategies into cancer research provides unprecedented opportunities to dissect ubiquitin code functions while developing transformative therapeutics. This technical guide examines the two primary TPD modalities—PROTACs and molecular glues—within the context of ubiquitin code manipulation for cancer therapy, providing researchers with comprehensive frameworks for their application in both basic and translational research settings.
Molecular Mechanisms and Design Principles
PROTACs: Heterobifunctional Degraders
Proteolysis-Targeting Chimeras (PROTACs) are heterobifunctional molecules consisting of three covalently linked components: a target protein-binding ligand, an E3 ubiquitin ligase-recruiting ligand, and a chemical linker that spatially optimizes the ternary complex formation [39]. The molecular weight of PROTACs typically ranges from 700-1200 Da, creating design challenges for cellular permeability and oral bioavailability [41].
The degradation mechanism occurs through a sequential process: (1) simultaneous binding of the PROTAC to both the protein of interest (POI) and E3 ubiquitin ligase, (2) formation of a productive POI-PROTAC-E3 ternary complex with proper spatial orientation, (3) transfer of ubiquitin molecules from the E2 conjugating enzyme to lysine residues on the POI, (4) polyubiquitination with specific chain linkages (typically K48 or K11), and (5) recognition by the 26S proteasome and subsequent degradation [39]. The catalytic nature of PROTACs enables sub-stoichiometric activity, as each molecule can facilitate multiple degradation cycles [40].
Ternary Complex Formation Dynamics The efficiency of PROTAC-induced degradation depends critically on ternary complex stability and cooperativity rather than solely on binding affinity of individual components. Even weak-affinity ligands can drive potent degradation if the linker supports favorable ternary complex geometry [39]. Linker properties—including length, flexibility, polarity, and spatial orientation—directly influence the protein-protein interface and determine whether the complex adopts a ubiquitination-competent conformation [39]. Structural biology approaches have revealed that optimal linkers position the POI and E3 ligase approximately 30-40 Å apart to enable efficient ubiquitin transfer.
E3 Ligase Recruitment Landscape While CRBN- and VHL-based recruiters dominate current PROTAC designs, expanding the E3 ligase repertoire enhances tissue selectivity and reduces potential resistance. Alternative E3 recruiters including IAPs, MDM2, DCAF family members, and TRIM21 are being explored to broaden the therapeutic scope [39]. Recent work has demonstrated that TRIM21-based PROTACs show particular promise for selective degradation of multimeric proteins and those within biomolecular condensates, important for addressing protein aggregation pathologies [42].
Molecular Glues: Monovalent Inducers
Molecular glue degraders are monovalent small molecules that induce or stabilize novel protein-protein interactions between an E3 ubiquitin ligase and a target protein, leading to ubiquitination and degradation [40]. Unlike PROTACs, molecular glues typically have lower molecular weight (<500 Da) and do not contain a linker, often resulting in improved pharmacokinetic properties and blood-brain barrier penetration [41].
The mechanism of molecular glue action involves surface remodeling of protein interfaces. Most molecular glues bind primarily to one protein (often the E3 ligase) and induce conformational changes or create neosurfaces that become complementary to specific regions on the target protein [40]. This "surface matching" enables interactions between proteins that would not normally bind, effectively reprogramming E3 ligase specificity. The resulting ternary complex facilitates ubiquitin transfer to the target protein, marking it for proteasomal degradation.
Naturally Occurring vs. Engineered Molecular Glues The first molecular glues were discovered serendipitously through natural products and approved drugs. Immunosuppressants like cyclosporine A, FK506, and rapamycin function as molecular glues by stabilizing complexes between immunophilins and calcineurin or mTOR [43]. Similarly, immunomodulatory imide drugs (IMiDs) such as thalidomide, lenalidomide, and pomalidomide were later found to act as molecular glues that promote interaction between CRBN and transcription factors IKZF1/IKZF3, leading to their degradation [40]. More recently, rational design approaches and high-throughput screening have enabled systematic discovery of novel molecular glues with enhanced specificity and potency [40].
Structural Determinants of Glue Efficiency The efficiency of molecular glue-induced degradation depends on the precise geometry of the induced interface and the cooperativity of ternary complex formation. Structural studies have revealed that effective molecular glues typically bind at the interface between the E3 ligase and target protein, with key functional groups making contact with both proteins simultaneously. Recent advances in computational modeling, including AlphaFold Multimer and MaSIF, are enabling more predictive design of molecular glues by simulating protein-protein interactions and interface compatibility [40].
Comparative Analysis: PROTACs vs. Molecular Glues
Table 1: Comparative Analysis of PROTACs and Molecular Glues
| Feature | PROTACs | Molecular Glues |
|---|---|---|
| Molecular Structure | Heterobifunctional | Monovalent |
| Molecular Weight | High (700-1200 Da) | Low (<500 Da) |
| Linker Requirement | Required | Linker-less |
| Discovery Approach | Rational design | Historically serendipitous, increasingly rational/AI-driven |
| Oral Bioavailability | Challenging | Generally favorable |
| BBB Penetration | Limited | Enhanced potential |
| Design Predictability | Higher due to modular nature | Lower due to complex interface requirements |
| E3 Ligase Scope | Broad range exploitable | Limited to adaptable E3s |
| Catalytic Mechanism | Yes, sub-stoichiometric | Yes, sub-stoichiometric |
Current Clinical Landscape in Cancer Therapy
The clinical translation of TPD technologies has advanced rapidly, with numerous PROTAC candidates entering clinical trials and several molecular glues already approved for hematological malignancies. The therapeutic focus has predominantly been in oncology, where these modalities address significant unmet needs in resistant and refractory cancers.
PROTAC Clinical Candidates
Table 2: Selected PROTACs in Advanced Clinical Development for Cancer
| Drug Candidate | Company | Target | Indication | Development Phase |
|---|---|---|---|---|
| Vepdegestrant (ARV-471) | Arvinas/Pfizer | ER | ER+/HER2- breast cancer | Phase III |
| BMS-986365 (CC-94676) | Bristol Myers Squibb | AR | mCRPC | Phase III |
| BGB-16673 | BeiGene | BTK | R/R B-cell malignancies | Phase III |
| ARV-110 | Arvinas | AR | mCRPC | Phase II |
| ARV-766 | Arvinas/Novartis | AR | mCRPC | Phase II |
| KT-333 | Kymera | STAT3 | Liquid and solid tumors | Phase I |
| ASP-3082 | Astellas | KRAS G12D | Solid tumors | Phase I |
As of 2025, over 40 PROTAC drug candidates are undergoing clinical evaluation, targeting diverse proteins including nuclear hormone receptors, kinases, transcription factors, and challenging oncoproteins like KRAS mutants [44]. Notably, vepdegestrant (ARV-471) has demonstrated clinically meaningful improvement in progression-free survival in patients with ESR1 mutations in the Phase III VERITAC-2 trial, positioning it as a potential first-in-class oral PROTAC degrader [44]. Similarly, BMS-986365 has shown promising activity in metastatic castration-resistant prostate cancer, with 55% of patients receiving the 900 mg twice-daily dose achieving a ≥30% decline in PSA levels [44].
Clinically Approved Molecular Glues
The immunomodulatory imide drugs (IMiDs) represent the most successful class of molecular glues in clinical use. Thalidomide, lenalidomide, and pomalidomide are FDA-approved for multiple myeloma and other hematological malignancies and function by redirecting CRBN E3 ligase activity toward transcription factors IKZF1 and IKZF3 [40]. These drugs have revolutionized treatment paradigms for multiple myeloma and demonstrate the profound therapeutic potential of molecular glue degraders.
Beyond IMiDs, additional molecular glues are advancing through clinical development. For example, (S)-ACE-OH, a metabolite of the antipsychotic drug acepromazine, functions as a molecular glue that induces interaction between TRIM21 and nucleoporin NUP98, leading to degradation of nuclear pore proteins [42]. This discovery highlights the potential for drug repurposing approaches in molecular glue development.
Experimental Methodologies for TPD Research
Assessing Degradation Efficiency and Kinetics
HiBiT-Based Degradation Assays The HiBiT tagging system enables precise quantification of protein degradation kinetics in live cells. This approach involves:
- Cell Line Engineering: Knock-in of the HiBiT tag at the N-terminus of the endogenous target gene locus using CRISPR-Cas9 technology [45].
- Compound Treatment: Application of PROTACs or molecular glues at varying concentrations and timepoints.
- Signal Detection: Measurement of luminescence after addition of the LgBiT complementation partner and substrate.
- Data Analysis: Calculation of DC50 (half-maximal degradation concentration) and Dmax (maximal degradation) values from dose-response curves, and determination of degradation rate constants from time-course experiments [45].
This methodology was successfully employed to identify cellular signaling pathways that modulate BRD4 degradation, revealing enhancement by PARG, PERK, and HSP90 inhibitors [45].
Western Blot Analysis of Endogenous Proteins While HiBiT provides excellent kinetic data, western blotting remains essential for confirming degradation of endogenous proteins:
- Cell Treatment: Exposure of relevant cell lines to degraders for predetermined timepoints.
- Protein Extraction: Lysis of cells in denaturing or non-denaturing buffers according to target protein properties.
- Immunoblotting: Separation by SDS-PAGE, transfer to membranes, and probing with target-specific antibodies.
- Normalization: Use of housekeeping proteins (e.g., GAPDH, actin) for quantification of degradation efficiency.
This approach validated that PARG inhibition enhances degradation of BRD2, BRD3, and BRD4 but not MEK1/2 or ERα, demonstrating substrate-specific effects of degradation enhancers [45].
Evaluating Ternary Complex Formation
Cellular Thermal Shift Assay (CETSA) CETSA assesses target engagement by measuring thermal stabilization of proteins upon ligand binding:
- Compound Treatment: Incubation of cells with degraders or vehicle control.
- Heat Denaturation: Subjecting aliquots of cell lysate or intact cells to a range of temperatures.
- Protein Quantification: Analysis of soluble protein remaining after heat treatment by western blot or MSD immunoassay.
- Data Interpretation: Shift in melting temperature (ΔTm) indicates direct binding or stabilization through complex formation.
Surface Plasmon Resonance (SPR) SPR provides quantitative analysis of ternary complex kinetics:
- Immobilization: Capture of E3 ligase complex onto sensor chip.
- Binding Analysis: Sequential or simultaneous injection of PROTAC and target protein.
- Kinetic Modeling: Determination of binding affinities (KD), association rates (ka), and dissociation rates (kd) for ternary complex formation.
Proteome-Wide Specificity Assessment
Mass Spectrometry-Based Proteomics Comprehensive profiling of degrader specificity employs quantitative mass spectrometry:
- Sample Preparation: SILAC, TMT, or label-free quantification of proteomes from treated vs. control cells.
- LC-MS/MS Analysis: High-resolution mass spectrometry with data-independent acquisition (DIA) for comprehensive protein quantification.
- Data Processing: Identification of significantly altered proteins beyond the intended target.
- Validation: Orthogonal confirmation of off-target hits by western blotting.
This approach is crucial for identifying selective degraders and eliminating candidates with undesirable off-target effects [41].
Signaling Pathways Modulating TPD Efficiency
Recent research has revealed that intrinsic cellular signaling pathways significantly influence the efficiency of targeted protein degradation. Understanding these modulatory pathways provides opportunities to enhance degrader efficacy and overcome potential resistance mechanisms.
Diagram 1: Signaling pathways modulating PROTAC efficiency. Inhibitors of PARG, HSP90, and PERK enhance degradation at distinct steps.
The diagram illustrates how specific pathway inhibitors enhance PROTAC-mediated degradation at multiple regulatory steps. PARG inhibition promotes chromatin dissociation of BRD4 and facilitates ternary complex formation, while HSP90 inhibition acts after the ubiquitylation step to enhance proteasomal targeting [45]. These findings demonstrate that targeted inhibition of intrinsic signaling pathways can sensitize cells to PROTAC-induced degradation, potentially lowering therapeutic doses and overcoming resistance.
Ubiquitin Chain Architecture in TPD
The ubiquitin chain linkage type significantly influences degradation efficiency. While K48-linked chains represent the canonical proteasomal degradation signal, recent research has revealed the importance of branched ubiquitin chains in TPD. TRIP12 cooperates with CRL2VHL or CRL4CRBN to assemble K29/K48-linked branched ubiquitin chains that promote efficient degradation of neosubstrates like BRD4 [45]. Understanding these ubiquitin code specifications provides opportunities to engineer degraders that promote optimal chain architectures for enhanced efficiency.
The Scientist's Toolkit: Essential Research Reagents
Table 3: Essential Research Reagents for TPD Investigations
| Reagent/Category | Specific Examples | Research Application | Key Function |
|---|---|---|---|
| E3 Ligase Ligands | VHL ligands, CRBN ligands, IAP antagonists, MDM2 binders | PROTAC design and optimization | Recruit specific E3 ubiquitin ligases to enable target ubiquitination |
| Target Protein Binders | JQ1 (BRD4), ARV-110 (AR), osimertinib (EGFR) | Warhead selection for PROTAC development | Provide binding specificity for the protein targeted for degradation |
| Linker Chemistry | PEG linkers, alkyl chains, alkyl/ether chains | PROTAC structure-activity relationship studies | Spatially optimize ternary complex formation; influence pharmacokinetics |
| Pathway Modulators | PDD00017273 (PARGi), luminespib (HSP90i), GSK2606414 (PERKi) | Enhancement of degradation efficiency | Inhibit intrinsic pathways that counteract targeted degradation |
| Proteasome Inhibitors | Carfilzomib, bortezomib, b-AP15 (DUB inhibitor) | Mechanism validation experiments | Block degradation to confirm UPS dependence; study ubiquitin dynamics |
| Ubiquitin System Reagents | E1/UBA1 inhibitors, specific E2 enzymes, DUB substrates | Ubiquitination pathway analysis | Dissect specific steps in the ubiquitin-proteasome cascade |
| Detection Tools | HiBiT tagging system, ubiquitin remnant motifs, ternary complex assays | Degradation kinetics and mechanism | Quantify degradation efficiency and ternary complex formation |
The selection of appropriate research reagents is critical for rigorous TPD investigations. Linker chemistry deserves particular attention, as PEG-based linkers of varying lengths help optimize the distance and flexibility between target and E3 ligase binding domains [43]. Similarly, pathway modulators like PARG inhibitors have emerged as valuable tools for enhancing degradation of recalcitrant targets like BRD2 and BRD3 [45].
Advanced detection systems including the HiBiT tagging platform enable precise quantification of degradation kinetics in endogenous settings, providing superior data to overexpression systems [45]. Mass spectrometry-based proteomics platforms employing data-independent acquisition (DIA) technology offer comprehensive assessment of degradation selectivity and off-target effects across the entire proteome [41].
Future Directions and Research Opportunities
Several emerging areas present compelling opportunities for advancing TPD research and clinical application:
Expanding the E3 Ligase Toolbox While CRBN and VHL dominate current TPD approaches, expanding the repertoire of exploitable E3 ligases will enhance tissue specificity, reduce adaptation resistance, and address targets refractory to conventional degraders. TRIM21-based approaches show particular promise for degrading multimeric proteins and biomolecular condensates [42]. Similarly, DCAF15-recruiting molecular glues like indisulam demonstrate the potential of less characterized E3 ligases [43].
Tissue-Specific Targeting Strategies Advances in delivery technologies including antibody-PROTAC conjugates, nanoparticle formulations, and tissue-restricted E3 ligase expression may overcome current limitations in bioavailability and tissue penetration. Blood-brain barrier penetration remains a particular challenge for PROTACs that might be addressed through molecular glue approaches or specialized carrier systems.
Overcoming Resistance Mechanisms As with all targeted therapies, resistance to TPD agents eventually emerges through various mechanisms including E3 ligase downregulation, point mutations in binding interfaces, and UPS component alterations. Combination approaches with pathway inhibitors that enhance degradation sensitivity, such as PARG or HSP90 inhibitors, may delay or prevent resistance development [45].
Integration with Ubiquitin Code Mapping Advanced techniques for mapping ubiquitin chain architecture and dynamics will elucidate the precise ubiquitin codes required for efficient degradation of different target classes. This knowledge will enable rational design of degraders that promote optimal ubiquitin chain patterns for enhanced efficiency and selectivity.
Targeted protein degradation with PROTACs and molecular glues represents a transformative approach to therapeutic intervention, particularly for cancer driven by alterations in the ubiquitin code. These technologies have progressed from concept to clinical validation at an remarkable pace, demonstrating their potential to address previously undruggable targets and overcome resistance to conventional therapies. As research continues to elucidate the intricate mechanisms governing degradation efficiency, ternary complex formation, and ubiquitin code specification, the rational design of increasingly sophisticated degraders will become feasible. The integration of TPD strategies into cancer research provides not only powerful therapeutic modalities but also valuable tools for probing ubiquitin biology and protein function in malignant transformation.
CRISPR Screens to Identify Ubiquitin System Vulnerabilities in Cancer Cells
The ubiquitin-proteasome system (UPS) is a critical post-translational regulatory mechanism that governs nearly every cellular process through targeted protein degradation and signaling. In cancer development, the "ubiquitin code"—defined by diverse ubiquitin chain topologies and modifications—becomes profoundly rewired, driving tumor progression, therapeutic resistance, and metabolic reprogramming [29] [22]. With approximately 600 E3 ubiquitin ligases recognizing specific substrates, the UPS presents extensive but underexplored therapeutic opportunities [46]. CRISPR-Cas9 functional genomics has emerged as a powerful discovery engine for systematically identifying vulnerabilities within this complex network, revealing novel ubiquitin-linked dependencies across cancer types [47] [48] [49]. This whitepaper synthesizes current methodologies, key findings, and experimental frameworks for leveraging CRISPR screens to decode ubiquitin system vulnerabilities in cancer biology and drug discovery.
Key Concepts and Rationale
Ubiquitin System Architecture and Cancer Relevance
The ubiquitination cascade involves E1 (activating), E2 (conjugating), and E3 (ligating) enzymes that collectively coordinate substrate specificity and polyubiquitin chain formation. Different chain topologies determine functional outcomes: K48-linked chains typically target proteins for proteasomal degradation; K63-linked chains facilitate non-proteolytic signaling in DNA repair and immune pathways; while monoubiquitination regulates chromatin dynamics and membrane trafficking [29] [22]. Cancer cells exploit this system through multiple mechanisms:
- Premature degradation of tumor suppressors (e.g., p53 ubiquitination by MDM2)
- Stabilization of oncoproteins through altered E3 ligase or deubiquitinase (DUB) activity
- Rewiring of DNA damage response via K63-linked ubiquitination of repair complexes
- Metabolic reprogramming through ubiquitin-mediated regulation of metabolic enzymes and transporters
- Immune evasion via ubiquitination of immune signaling components [29] [22] [13]
CRISPR Screening Platforms for Ubiquitin Vulnerability Discovery
CRISPR loss-of-function screens provide an unbiased approach to identify essential ubiquitin system components across genomic scales. Two primary screening modalities have proven particularly effective:
- In vitro pooled screens utilizing cancer cell lines expressing Cas9 and sgRNA libraries targeting ubiquitin-related genes
- In vivo functional screens employing immunocompetent mouse models to uncover ubiquitin regulators of tumor-immune interactions [47] [49]
These approaches have revealed context-specific dependencies across cancer lineages, highlighting the therapeutic potential of targeting ubiquitin ligases, DUBs, and associated factors [48].
Key Experimental Findings from Recent CRISPR Screens
Recent CRISPR screens have identified numerous ubiquitin system vulnerabilities across cancer types. The table below summarizes quantitative findings from key studies.
Table 1: Key Ubiquitin System Vulnerabilities Identified through CRISPR Screening
| Target Identified | Cancer Type | Screen Approach | Biological Function | Therapeutic Implication |
|---|---|---|---|---|
| G2E3 [50] | Pancreatic ductal adenocarcinoma (PDAC) | In vitro CRISPR screen of 660 ubiquitin-related genes with mCherry-GFP-LC3 reporter | Regulates autophagosome-lysosome fusion via GABARAP interaction; knockout impairs autophagic flux | Potential target for autophagy-dependent cancers; knockout reduces cancer cell migration/invasion |
| Cop1 (RFWD2) [47] | Triple-negative breast cancer (TNBC) | In vivo CRISPR screen in syngeneic models (4,500-gene library) | Degrades C/ebpδ protein; regulates macrophage chemokine secretion | Cop1 deletion enhances anti-tumor immunity and anti-PD-1 response; reduces macrophage infiltration |
| OTUB1-TRIM28 [35] | Pan-cancer (lung, esophageal, cervical, urothelial, melanoma) | Ubiquitination regulatory network analysis across 4,709 patients | Stabilizes MYC pathway; influences oxidative stress and histological fate | Defines immunotherapy-resistant subset; prognostic biomarker across multiple cancers |
| FBXW7 [29] [22] | Colorectal cancer (p53-wt) vs. NSCLC (p53-null) | Context-specific dependency | K48-linked degradation of p53 (colorectal) vs. SOX9 (NSCLC) | Context-dependent therapeutic target: radioresistance (colorectal) vs. radiosensitization (NSCLC) |
| USP14 [29] [22] | Glioma vs. Head/neck squamous cell carcinoma | Functional validation of screen hits | Stabilizes ALKBH5 (glioma) vs. degrades IκBα (HNSCC) | Tissue-specific effects necessitate precision targeting approaches |
Detailed Experimental Protocols
Pooled CRISPR Screen for Autophagy Regulators in Pancreatic Cancer
This protocol outlines the methodology for identifying ubiquitin-related autophagy regulators, as demonstrated in recent research [50].
Cell Line Engineering and Validation
- Step 1: Generate reporter cell line. Stably transduce AsPC-1 human pancreatic cancer cells with lentiviral mCherry-GFP-LC3 construct. The dual-fluorescent reporter exploits GFP's pH sensitivity (quenched in acidic lysosomes) and mCherry's pH stability.
- Step 2: Validate reporter functionality. Treat cells with 250 nM Torin1 (autophagy inducer) and 20 μM chloroquine (CQ, lysosomal acidification inhibitor). Confirm that Torin1 increases mCherry-only puncta (autolysosomes) while CQ increases dual-labeled puncta (autophagosomes) via confocal microscopy.
- Step 3: Establish sorting gates. Using FACS, identify cells with low GFP:mCherry ratio (intact autophagy) versus high GFP:mCherry ratio (defective autophagy) after Torin1 treatment.
Library Design and Screening
- Step 4: Select sgRNA library. Utilize a pooled library containing 11,108 sgRNAs targeting 660 ubiquitin-related genes (E1, E2, E3 ligases, and DUBs) plus 1,000 non-targeting control sgRNAs.
- Step 5: Transduce and select. Transduce AsPC-1-mCherry-GFP-LC3 reporter cells at low MOI (0.3-0.4) to ensure single sgRNA integration. Select with puromycin (1-2 μg/mL) for 7 days.
- Step 6: Induce autophagy and sort. Treat cells with 250 nM Torin1 for 4-6 hours. Use FACS to isolate the top 3% of cells with highest GFP:mCherry ratios (autophagy-defective population). Expand sorted cells and repeat sorting for 4 additional rounds to enrich true hits.
- Step 7: Sequence and analyze. Extract genomic DNA from enriched population. Amplify sgRNA regions via PCR and sequence on Illumina platform. Analyze sgRNA enrichment using MAGeCK-VISPR algorithm.
Validation Experiments
- Step 8: Generate knockout clones. Design CRISPR-Cas9 constructs targeting top candidates (e.g., G2E3). Isolate monoclonal knockout populations and validate via DNA sequencing and Western blotting.
- Step 9: Functional validation. Assess autophagic flux by monitoring LC3B-II and GABARAP protein levels via immunoblotting in knockout versus wild-type cells under basal and Torin1-induced conditions.
- Step 10: Mechanistic studies. Perform co-immunoprecipitation to confirm protein-protein interactions (e.g., G2E3 with GABARAP/GABARAPL1). Use confocal microscopy to quantify autophagosome-lysosome colocalization via LAMP1 and LC3B staining.
In Vivo CRISPR Screen for Immunomodulatory Ubiquitin Ligases
This protocol describes the approach for identifying ubiquitin regulators of tumor-immune interactions, as demonstrated in TNBC models [47].
Library Design and Validation
- Step 1: Construct focused library. Design a murine CRISPR knockout (MusCK) library with 5 sgRNAs per gene targeting ~4,500 genes implicated in tumor progression and immune modulation, including comprehensive coverage of ubiquitin system components.
- Step 2: Validate library quality. Transduce library into 4T1 mouse TNBC cells at coverage >200x. Culture for 10 passages and compare sgRNA abundance distributions to initial timepoint. Confirm depletion of essential gene sgRNAs and enrichment of tumor suppressor targeting sgRNAs.
In Vivo Screening
- Step 3: Engineer immune-responsive cells. Stably express membrane-bound ovalbumin (mOva) in 4T1 cells to enhance antigen-specific T cell responses.
- Step 4: Transduce and implant. Transduce mOva-4T1 cells with MusCK library and implant into three host conditions: (1) BALB/c Foxn1nu/nu (T cell-deficient), (2) immunocompetent BALB/c, and (3) Ova-vaccinated BALB/c (n=12/group). Maintain >200x library coverage throughout.
- Step 5: Harvest and analyze. Harvest tumors at 16 days post-implantation. Extract genomic DNA and sequence sgRNA regions. Compare sgRNA abundance distributions across host conditions using MAGeCK or similar algorithms to identify immune-dependent vulnerabilities.
Multi-Omic Target Validation
- Step 6: Transcriptomic profiling. Perform RNA-seq on control and candidate knockout cells (e.g., Cop1) to identify differentially expressed genes, particularly chemokines and immune regulators.
- Step 7: Proteomic analysis. Conduct quantitative proteomics (e.g., TMT-MS) to identify stabilized/degraded proteins upon target knockout.
- Step 8: Epigenomic assessment. Perform ATAC-seq to assess chromatin accessibility changes in regulatory regions of differentially expressed genes.
- Step 9: Mechanistic studies. Employ co-immunoprecipitation and ubiquitination assays to identify direct substrates (e.g., C/ebpδ for Cop1) and scaffolding proteins (e.g., Trib2 for Cop1-C/ebpδ interaction).
Diagram Title: CRISPR Screen Workflow for Ubiquitin Vulnerabilities
The Scientist's Toolkit: Essential Research Reagents
Table 2: Key Research Reagents for CRISPR Screens of Ubiquitin System
| Reagent/Category | Specific Examples | Function/Application | Considerations |
|---|---|---|---|
| CRISPR Libraries | Custom ubiquitin-focused (e.g., 660 genes, 11,108 sgRNAs) [50]; MusCK (4,500 genes) [47] | Target specific gene families with optimized sgRNA coverage | Ensure >200x library coverage; include non-targeting controls |
| Reporter Systems | mCherry-GFP-LC3 [50]; Membrane-bound ovalbumin (mOva) [47] | Monitor autophagic flux (pH-sensitive GFP); enhance anti-tumor immunity for in vivo screens | Validate reporter functionality pre-screen; optimize sorting gates |
| Cell Lines | AsPC-1 (PDAC) [50]; 4T1 (TNBC) [47]; A549, HEK293TN [50] | Model-specific biological contexts; syngeneic models for immuno-oncology | Authenticate lines; check mycoplasma contamination |
| Autophagy Modulators | Torin1 (250 nM) [50]; Chloroquine (20 μM) [50] | Induce autophagy (Torin1) or block lysosomal degradation (CQ) | Titrate concentrations for specific cell lines; include both induction and inhibition controls |
| In Vivo Models | BALB/c (immunocompetent); BALB/c Foxn1nu/nu (T cell-deficient) [47] | Assess immune-dependent gene essentiality; study tumor microenvironment | Use age-matched animals; power studies appropriately (n=12/group) |
| Analytical Tools | MAGeCK-VISPR [50]; RNA-seq, ATAC-seq, Proteomics [47] | Identify enriched/depleted sgRNAs; multi-omics mechanistic validation | Plan for sufficient sequencing depth; include biological replicates |
Therapeutic Implications and Translational Potential
CRISPR screens have revealed numerous therapeutically actionable ubiquitin system vulnerabilities with promising translational potential:
- G2E3 Inhibition: Targeting this autophagy regulator may combat pancreatic cancers dependent on autophagic flux for survival [50].
- Cop1 Targeting: Small molecule inhibitors of Cop1 could stabilize C/ebpδ, suppress macrophage recruitment, and enhance anti-PD-1 efficacy in TNBC [47].
- OTUB1-TRIM28 Disruption: This ubiquitin axis represents a promising target for overcoming immunotherapy resistance across multiple cancer types [35].
- Context-Specific FBXW7 Modulation: Therapeutic strategies must account for opposing functions in different tumor contexts [29] [22].
The expanding repertoire of ubiquitin-targeting modalities—including molecular glues, PROTACs, and DUB inhibitors—provides diverse avenues for translating these CRISPR-derived insights into clinical candidates [29] [22] [13].
CRISPR screening technologies have fundamentally accelerated the discovery of ubiquitin system vulnerabilities in cancer, revealing novel therapeutic targets and biological mechanisms. The integrated experimental frameworks presented here provide a roadmap for researchers to systematically identify and validate ubiquitin-related dependencies across cancer types. As screening methodologies evolve toward more physiologically relevant models—including organoid systems, in vivo microenvironments, and single-cell readouts—they will undoubtedly uncover additional layers of complexity in the ubiquitin code and its therapeutic exploitation. These advances promise to expand the repertoire of targeted interventions for manipulating ubiquitin signaling in cancer, ultimately enabling more precise and effective treatments for oncogene-driven malignancies.
Ubiquitin signatures—defined by specific patterns of protein ubiquitination—are emerging as a powerful new class of molecular biomarkers for cancer patient stratification. These signatures capture the dynamic state of cellular signaling networks, offering unprecedented insights into tumor behavior, therapeutic resistance, and patient prognosis. This technical guide examines the fundamental principles, methodological frameworks, and clinical applications of ubiquitin-based biomarkers, positioning them within the broader context of ubiquitin code alterations in cancer development. For researchers and drug development professionals, mastering ubiquitin signature analysis represents a critical advancement toward predictive, preventive, and personalized medicine (PPPM) in oncology.
The ubiquitin-proteasome system (UPS) represents the second most abundant post-translational modification system in eukaryotic cells, regulating virtually all cellular processes through targeted protein degradation and signaling modulation [51]. The "ubiquitin code" comprises diverse ubiquitin chain topologies—including K48-linked (proteolytic), K63-linked (signaling), and monoubiquitination—that collectively govern protein fate and function [22] [51]. Cancer cells systematically reprogram this ubiquitin code to drive proliferation, evade cell death, and develop therapeutic resistance [22].
Ubiquitin signatures refer to comprehensive profiles of ubiquitination events within a biological sample, capturing disease-specific alterations in the ubiquitin landscape. Unlike genetic markers that indicate static predisposition, ubiquitin signatures provide dynamic, functional readouts of cellular state, reflecting real-time adaptations to therapeutic pressures and microenvironmental cues [52]. This positions them as ideal biomarkers for patient stratification across multiple dimensions: prognosis prediction, therapy selection, and resistance monitoring.
Methodological Framework for Ubiquitin Signature Analysis
Core Proteomic Technologies
Modern ubiquitinomics relies on advanced mass spectrometry (MS) platforms that enable comprehensive identification and quantification of ubiquitination sites:
4D Label-Free Quantitative Ubiquitination Proteomics: This cutting-edge approach combines four-dimensional separation (including ion mobility) with high-resolution mass spectrometry to significantly enhance the depth and accuracy of ubiquitinome profiling. A recent study on oral adenoid cystic carcinoma (OACC) identified 4,152 ubiquitination sites across 1,993 proteins using this technology, with 1,648 sites on 859 proteins yielding reliable quantitative information [53].
Ubiquitin Remnant Motif (K-ε-GG) Enrichment: The PTMScan Ubiquitin Remnant Motif Kit employs specific antibodies to enrich for peptides containing the diglycine (K-ε-GG) remnant left after tryptic digestion of ubiquitinated proteins. This enrichment is crucial for detecting low-abundance ubiquitination events amidst complex cellular proteomes [52].
Liquid Chromatography-Tandem Mass Spectrometry (LC-MS/MS): Following enrichment, ubiquitinated peptides are separated by ultra-performance liquid chromatography and analyzed by tandem mass spectrometry. The NanoElute UPLC system coupled with Tims-TOF Pro MS provides exceptional sensitivity, enabling detection of ubiquitination sites at unprecedented depths [53].
Table 1: Core Proteomic Technologies for Ubiquitin Signature Profiling
| Technology | Key Features | Applications | Performance Metrics |
|---|---|---|---|
| 4D Label-Free Quantitative Proteomics | Ion mobility separation + high-resolution MS; no isotopic labeling | Deep ubiquitinome profiling; biomarker discovery | 4,152 ubiquitination sites identified from OACC tissue [53] |
| K-ε-GG Immunoaffinity Enrichment | Anti-K-ε-GG antibody-based peptide enrichment | Detection of low-abundance ubiquitination events | Essential for comprehensive ubiquitinome coverage [52] |
| LC-MS/MS with PASEF | Parallel Accumulation-Serial Fragmentation; high sequencing speed | High-throughput ubiquitination site mapping | 10x increase in sequencing speed compared to conventional MS [53] |
Bioinformatics and Computational Analysis
The computational pipeline for ubiquitin signature analysis involves multiple specialized steps:
Database Searching and FDR Control: MaxQuant or similar platforms are used to search MS/MS spectra against protein databases. Stringent false discovery rate (FDR) thresholds (<1%) are applied at the peptide spectrum match level to ensure data quality [53].
Differentially Ubiquitinated Protein (DUP) Identification: Statistical analysis (typically with limma package in R) identifies DUPs with significant abundance changes between sample groups. Thresholds commonly used include fold-change ≥1.5 and p-value <0.05 [53] [52].
Functional Enrichment Analysis: Gene Ontology (GO) and KEGG pathway analyses reveal biological processes, molecular functions, and signaling pathways enriched in DUPs. In sigmoid colon cancer, this approach identified 35 significantly altered pathways, including salmonella infection, glycolysis/gluconeogenesis, and ferroptosis [52].
Consensus Clustering: Unsupervised clustering algorithms (e.g., ConsensusClusterPlus in R) stratify patients into molecular subtypes based on ubiquitination patterns. Resampling 1,000 times with a subsample ratio of 0.8 ensures robust cluster stability [54] [55].
The following diagram illustrates the comprehensive experimental workflow for ubiquitin signature analysis:
Ubiquitin Signature Analysis in Cancer Typing and Stratification
Molecular Subtyping Through Consensus Clustering
Ubiquitination-based molecular subtyping has demonstrated remarkable utility across diverse malignancies:
In acute lymphoblastic leukemia (ALL), consensus clustering of 1,121 ubiquitination-related genes (URGs) identified four distinct molecular subtypes with significantly different survival outcomes. Cluster D emerged as a high-risk subgroup characterized by aggressive disease and poor prognosis, enabling stratification of patients who might benefit from more intensive therapeutic regimens [54].
Similarly, in lung adenocarcinoma (LUAD), unsupervised clustering of 966 URGs revealed distinct ubiquitination subtypes with differential mutation frequencies and tumor mutation burden (TMB). This classification provided insights into the underlying biological drivers of disease heterogeneity [55].
Prognostic Model Development
Ubiquitination-based prognostic models leverage machine learning approaches to generate quantitative risk scores:
Ubiquitination-Related Risk Score (URRS) in LUAD: Integration of univariate Cox regression, Random Survival Forests, and LASSO Cox regression identified four key prognostic genes (DTL, UBE2S, CISH, and STC1) for constructing a URRS. Patients with high URRS showed significantly worse prognosis (HR=0.54, 95% CI: 0.39-0.73, p<0.001), validated across six external datasets [55].
Nine-Gene Predictive Model in ALL: LASSO and Cox regression analyses developed a nine-gene prognostic signature that effectively stratified ALL patients into high- and low-risk groups. The model demonstrated significant predictive power for overall survival and revealed distinct immune microenvironment characteristics between risk groups [54].
Table 2: Clinically Validated Ubiquitin-Based Biomarkers Across Cancer Types
| Cancer Type | Biomarker | Function | Clinical Utility | Reference |
|---|---|---|---|---|
| Colorectal Cancer | UBR5 | E3 ubiquitin ligase; oncogenic role | Independent prognostic predictor; high expression correlates with poor survival | [56] |
| Acute Lymphoblastic Leukemia | FBXO8 | E3 ubiquitin ligase; tumor suppressor | Protective factor; knockdown enhances proliferation and suppresses apoptosis | [54] |
| Lung Adenocarcinoma | UBE2S | E2 ubiquitin-conjugating enzyme | Component of URRS; high expression associated with worse prognosis | [55] |
| Ovarian Cancer | TOP2A, MYLIP | Ubiquitin pathway genes | Survival risk model; stratifies patients into prognostic categories | [57] |
| Sigmoid Colon Cancer | 46 DUPs | Various ubiquitinated proteins | Overall survival-related biomarkers; potential for patient stratification | [52] |
The Scientist's Toolkit: Essential Research Reagents
Successful implementation of ubiquitin signature analysis requires specialized reagents and tools:
Table 3: Essential Research Reagents for Ubiquitin Signature Analysis
| Reagent/Tool | Function | Application Notes |
|---|---|---|
| Anti-K-ε-GG Antibody (PTMScan) | Immunoaffinity enrichment of ubiquitinated peptides | Critical for comprehensive ubiquitinome coverage; validates with ΔGG ubiquitin mutant [53] [51] |
| Protease Inhibitor Cocktail | Prevents protein degradation during extraction | Must include PR-619 (DUB inhibitor), TSA, and NAM to preserve ubiquitination states [53] |
| BCA Protein Assay Kit | Quantifies protein concentration | Essential for normalizing input material across samples [53] |
| Trypsin | Proteolytic digestion for MS sample prep | Specific for trypsin/P with ≤4 missed cleavages allowed [53] |
| ConsensusClusterPlus R Package | Unsupervised molecular subtyping | Parameters: maxK=5, reps=1000, pItem=0.8, clusterAlg="km", distance="euclidean" [54] [55] |
| Glmnet R Package | LASSO regression for feature selection | Implements Cox regression for prognostic model development [54] [55] |
Functional Validation of Ubiquitin Biomarkers
In Vitro and In Vivo Assessment
The transition from biomarker discovery to clinical application requires rigorous functional validation:
For the FBXO8 biomarker in ALL, researchers conducted comprehensive functional assays demonstrating that FBXO8 knockdown enhanced cell proliferation and suppressed apoptosis in ALL cells. In vivo validation using FBXO8-knockdown mouse models confirmed increased tumor growth, reduced apoptosis, and diminished survival rates, establishing FBXO8 as a genuine functional regulator rather than a passive correlative marker [54].
Similarly, for UBR5 in colorectal cancer, both in vitro (proliferation, colony formation, migration, and invasion assays) and in vivo (xenograft models) studies confirmed its oncogenic function. UBR5 knockdown significantly suppressed CRC tumor growth in animal models, providing mechanistic insights to support its biomarker utility [56].
Integration with Immune Profiling
Ubiquitin signatures provide unique insights into tumor-immune interactions:
In ALL, the high-risk ubiquitination subtype exhibited an immunosuppressive microenvironment characterized by increased regulatory T cells and M2 macrophage infiltration. This immune contexture, linked to FBXO8 expression patterns, may explain the aggressive clinical behavior observed in these patients [54].
In lung adenocarcinoma, the high URRS group showed significantly higher PD-1/PD-L1 expression levels (p<0.05), tumor mutation burden (p<0.001), and tumor neoantigen load (p<0.001), suggesting enhanced immunogenicity and potential responsiveness to immunotherapy [55].
The following diagram illustrates how ubiquitination regulates key cancer-relevant pathways that can be exploited for patient stratification:
Clinical Translation and Therapeutic Implications
Predictive Biomarkers for Therapy Selection
Ubiquitin signatures show exceptional promise for guiding targeted therapies:
In radiotherapy-resistant cancers, ubiquitination signatures involving K48-linked degradation of SOX9 (via FBXW7) or K63-linked stabilization of DNA repair proteins (via TRAF4) identify tumors likely to respond to radiosensitization strategies. These signatures can guide the use of PROTACs (Proteolysis Targeting Chimeras) that specifically target radioresistance networks [22].
For immunotherapy selection, ubiquitin signatures related to immune evasion mechanisms—such as TRIM21-mediated degradation of VDAC2 (suppressing cGAS/STING activation) or USP14-mediated stabilization of IRF3—can stratify patients into "hot" and "cold" tumor categories, informing combination approaches with immune checkpoint inhibitors [22] [54].
Integration with PPPM Framework
The application of ubiquitin signatures aligns perfectly with the Predictive, Preventive, and Personalized Medicine (PPPM) paradigm:
- Prediction: Ubiquitin signatures identify high-risk individuals before clinical manifestation of aggressive disease.
- Prevention: Stratification enables targeted interventions for prevention of progression or recurrence.
- Personalization: Signature-guided therapy selection tailors treatment to individual molecular profiles.
In sigmoid colon cancer, the identification of 46 overall survival-related DUPs and their drug sensitivity profiles enables truly personalized therapeutic approaches based on the individual's ubiquitinome [52].
Ubiquitin signature analysis represents a paradigm shift in cancer biomarker development, moving beyond static genetic alterations to dynamic, functional readouts of cellular state. The methodologies outlined in this technical guide—from advanced proteomic platforms to sophisticated computational pipelines—provide researchers and clinicians with powerful tools for patient stratification across multiple cancer types.
Future developments in this field will likely focus on single-cell ubiquitinomics to resolve intratumoral heterogeneity, spatial ubiquitinomics to map ubiquitination patterns within tissue architecture, and liquid biopsy applications to enable non-invasive monitoring of treatment response. Additionally, the integration of ubiquitin signatures with other omics layers (genomics, transcriptomics, proteomics) will generate comprehensive molecular portraits that further refine patient stratification.
As these technologies mature and become more accessible, ubiquitin signature-based stratification promises to become a standard component of oncology practice, ultimately fulfilling the vision of predictive, preventive, and personalized cancer medicine.
Overcoming Challenges in Targeting the Ubiquitin Code for Cancer Therapy
Addressing Functional Redundancy and Adaptive Responses in the Ubiquitin Network
The ubiquitin system, a crucial post-translational modification pathway, has emerged as a master regulator of cancer development and therapy resistance. This enzymatic cascade, involving E1 activating, E2 conjugating, and E3 ligating enzymes that tag proteins with ubiquitin, alongside deubiquitinases (DUBs) that remove these tags, governs virtually every cellular process. In cancer, tumors strategically exploit this system to drive proliferation, evade cell death, and develop resistance to treatments. However, two fundamental biological properties—functional redundancy and robust adaptive responses—have consistently impeded successful therapeutic targeting of ubiquitin networks. Functional redundancy arises from the staggering complexity of the ubiquitin system, with hundreds of enzymes often capable of regulating common substrates through overlapping mechanisms. Simultaneously, cancer cells activate compensatory survival pathways when ubiquitin function is compromised, creating adaptive responses that maintain cellular viability despite targeted intervention. Understanding and addressing these challenges is paramount for developing effective ubiquitin-targeted therapies that can overcome treatment resistance in cancer.
The Ubiquitin System: Complexity Breeds Redundancy
Architectural Foundations of Ubiquitin Signaling
The ubiquitin system's architecture inherently possesses redundant and adaptive capabilities. The human genome encodes approximately 2 E1 enzymes, ~35 E2 enzymes, over 600 E3 ligases, and around 100 DUBs that maintain ubiquitination homeostasis [58] [28]. This substantial enzymatic repertoire far exceeds the number of dedicated enzymes for other major post-translational modifications, immediately suggesting built-in redundancy. Ubiquitination complexity extends beyond enzyme diversity to the ubiquitin code itself—a single ubiquitin molecule contains seven lysine residues (K6, K11, K27, K29, K33, K48, K63) and an N-terminal methionine (M1) that can each form polyubiquitin chains with distinct structures and functions [59]. These chains can be homotypic (same linkage), heterotypic (mixed linkages), or even branched, creating a sophisticated language that controls diverse substrate fates including proteasomal degradation, altered subcellular localization, modified activity, and changed interaction partners.
Table 1: Major Ubiquitin Chain Linkages and Their Primary Functions in Cancer
| Linkage Type | Primary Functions | Role in Cancer Therapy Resistance |
|---|---|---|
| K48-linked | Proteasomal degradation [16] | Contextual duality in radiation response [22] |
| K63-linked | Signaling scaffolds, DNA repair, endocytosis [58] | Promotes accurate NHEJ repair via FBXW7/XRCC4 [16] |
| K11-linked | Proteasomal degradation, cell cycle regulation | Less characterized in therapy resistance |
| K27/K29-linked | DNA damage response | Activates ATM-CHK1 axis via MRE11 modification [22] |
| M1-linear | NF-κB activation, inflammation | Regulation of immune responses [58] |
| Monoubiquitination | Chromatin dynamics, DNA repair, endocytosis | Maintains genome integrity during radiation [22] |
Mechanisms of Functional Redundancy
Functional redundancy in the ubiquitin system manifests through several distinct mechanisms:
- Enzyme multiplicity: Critical substrate proteins are frequently regulated by multiple E3 ligases or DUBs with overlapping functions. For example, the stability of the DNA repair protein BRCA1 is controlled by several E3 ligases, creating a buffering system wherein inhibition of one enzyme can be compensated by another [22].
- Linkage plasticity: Many E2/E3 enzyme pairs demonstrate remarkable flexibility in synthesizing different ubiquitin chain types, enabling tumors to rewire ubiquitin signaling in response to therapeutic pressure. Radiation exposure dynamically reprograms ubiquitin chain hierarchies, with cancer cells strategically manipulating K63-linked chains to stabilize DNA repair factors while concurrently inhibiting K48-mediated degradation of survival proteins like GPX4 [22].
- Cross-regulation within the network: Ubiquitin system components extensively regulate each other, creating complex feedback and feedforward loops that maintain network stability. For instance, many E3 ligases themselves are ubiquitinated and degraded, while certain DUBs can stabilize E3 ligases, creating homeostatic control mechanisms [60].
Experimental Characterization of Redundancy and Adaptation
Quantitative Proteomic Approaches
Cutting-edge proteomic technologies have enabled researchers to systematically map ubiquitin network redundancy and identify adaptive responses to ubiquitin perturbation. Stable Isotope Labeling with Amino acids in Cell culture (SILAC) and Tandem Mass Tagging (TMT) represent two powerful mass spectrometry-based approaches that allow multiplexed, quantitative analysis of proteomic changes following targeted disruption of ubiquitin system components [61] [60]. These methodologies can quantify thousands of proteins and their post-translational modifications across multiple experimental conditions, providing systems-level insights into compensatory mechanisms.
Table 2: Key Methodologies for Characterizing Ubiquitin Network Adaptations
| Methodology | Key Features | Applications in Redundancy Research |
|---|---|---|
| SILAC (Stable Isotope Labeling) | Metabolic labeling; precise quantification [61] | Identification of proteins with stable levels despite E2 knockdown [60] |
| TMT (Tandem Mass Tagging) | Isobaric tags; multiplexing capability (up to 10-plex) [61] | Global proteome changes upon UBA1/E2 combinatorial knockdown [60] |
| Ubiquitin Tagging (StUbEx) | His/Strep-tagged ubiquitin expression [28] | Mapping ubiquitination sites under normal and stress conditions |
| Linkage-Specific Antibodies | Immunoenrichment of specific chain types [28] | Detecting chain-type rewiring after enzyme inhibition |
| TUBEs (Tandem Ubiquitin Binding Entities) | High-affinity enrichment of ubiquitinated proteins [28] | Monitoring global ubiquitination changes during adaptation |
A landmark study by the Harper laboratory utilized deep-coverage TMT mass spectrometry to define the "UBA1/E2-sensitive proteome" in human cells, systematically quantifying how individual E2 enzyme knockdowns remodel the proteome [60]. Surprisingly, partial reduction of UBA1 (the major E1 enzyme) was well-tolerated, with only specific proteome subsets showing sensitivity to ubiquitination capacity reduction. This approach identified precise adaptive responses, including compensatory upregulation of peroxisomal import machinery (PEX proteins) that sustained cellular function despite global ubiquitination impairment [60].
Figure 1: Experimental workflow for quantifying ubiquitin network adaptations using TMT proteomics. This approach enables multiplexed comparison of proteomic changes following targeted perturbation of ubiquitin system components.
CRISPR-Based Functional Screening
CRISPR-Cas9 loss-of-function screens have emerged as powerful tools for systematically mapping functional redundancies and synthetic lethal relationships within the ubiquitin network. By measuring how simultaneous knockout of multiple ubiquitin system components affects cell viability or therapy response, researchers can identify non-redundant enzyme pairs and compensatory pathways. For example, CRISPR screens have identified TRIM21 as a radiosensitization target whose inhibition synergizes effectively with radiotherapy, suggesting limited redundancy in its function [22]. These approaches are particularly valuable for identifying therapeutic windows where tumor-specific vulnerabilities can be exploited while sparing normal tissues.
Adaptive Resilience Mechanisms in the Ubiquitin Network
Organelle-Specific Adaptive Responses
Research has revealed that cells possess remarkable organelle-specific adaptive mechanisms to maintain function despite ubiquitination defects. When global ubiquitination capacity is compromised through UBA1 or combinatorial E2 knockdown, cells activate a compensatory program that specifically upregulates peroxisomal protein import machinery [60]. This adaptation occurs despite the fact that peroxisomal import normally relies on ubiquitin-dependent cycling of the cargo receptor PEX5. Rather than impairing peroxisomal function, reduced ubiquitination triggers counterbalancing upregulation of other PEX proteins necessary for PEX5 docking to the peroxisomal membrane, thereby maintaining organelle function through redundant pathways. This organelle-specific adaptation demonstrates the sophisticated layer of regulation that cells employ to sustain essential functions when ubiquitination capacity is compromised.
Metabolic Rewiring Under Ubiquitin Stress
Cancer cells exhibit profound metabolic plasticity when ubiquitin function is impaired, activating alternative pathways to maintain energy production and redox homeostasis. Ubiquitination critically regulates cancer metabolism, reprogramming processes including ferroptosis susceptibility, hypoxia adaptation, and nutrient flux [16] [22]. Under conditions of ubiquitin stress, tumors can shift toward metabolic states that are less dependent on ubiquitin-regulated pathways, or they may upregulate specific E2/E3 pairs that remain functional to maintain critical metabolic enzymes. For instance, TRIM26 stabilizes GPX4 via K63 ubiquitination to prevent ferroptosis in gliomas, creating a dependency that can be therapeutically exploited when other redox control systems are compromised [22].
Epigenetic and Transcriptional Reprogramming
Long-term adaptation to ubiquitin network perturbations frequently involves epigenetic and transcriptional reprogramming that fundamentally alters cellular identity and dependency patterns. Radiation treatment dynamically alters the ubiquitin landscape by modifying chain formation and recruitment of chromatin regulators [22]. For example, RNF40-mediated H2Bub1 recruits the FACT complex to relax nucleosome packing, facilitating DNA repair while simultaneously suppressing immunogenic cell death [22]. These chromatin modifications can create stable adaptive states that promote therapy resistance through both ubiquitin-dependent and ubiquitin-independent mechanisms, effectively bypassing the need for specific ubiquitin enzymes that have been therapeutically targeted.
Therapeutic Strategies to Overcome Redundancy and Adaptation
Targeting Non-Redundant Network Nodes
The most straightforward approach to addressing functional redundancy involves identifying and targeting network nodes with minimal backup. Enzymes that regulate critical, non-redundant substrates represent promising therapeutic targets. For example, PROTACs (Proteolysis-Targeting Chimeras) that simultaneously engage E3 ligases and target proteins have shown remarkable efficacy in degrading oncogenic drivers despite the overall redundancy of the ubiquitin system [22]. The specificity of these agents is exemplified by EGFR-directed PROTACs that selectively degrade β-TrCP substrates in EGFR-dependent tumors, suppressing DNA repair while minimizing impact on normal tissues [22]. These approaches leverage the ubiquitin system itself to achieve target specificity, effectively hijacking natural degradation mechanisms for therapeutic purposes.
Combinatorial Targeting Strategies
Given the extensive redundancy within the ubiquitin network, combinatorial approaches that simultaneously target multiple components or parallel pathways often yield superior outcomes compared to single-agent therapies. Several strategic combinations show particular promise:
- E3 ligase/DUB combinations: Simultaneously inhibiting an E3 ligase and a counteracting DUB that regulates the same pathway can create synthetic lethality. For instance, blocking USP14 stabilizes K63-ubiquitinated IRF3, triggering STING-dependent type I interferon responses that synergize with radiotherapy to overcome immune evasion [22].
- Ubiquitin pathway + conventional therapy: Combining ubiquitin-targeted agents with DNA-damaging chemotherapy or radiation leverages non-overlapping mechanisms of action. Radiation-responsive PROTAC platforms are emerging to overcome radioresistance, including radiotherapy-triggered PROTAC prodrugs activated by tumor-localized X-rays to degrade BRD4/2 [22].
- Vertical pathway inhibition: Targeting multiple components within the same linear pathway can prevent adaptive bypass mechanisms. For example, simultaneously targeting an upstream E2 enzyme and downstream E3 ligase involved in the same degradation pathway may yield more complete pathway suppression.
Biomarker-Guided Patient Stratification
Precision targeting of the ubiquitin network requires sophisticated biomarker strategies to identify tumors dependent on specific ubiquitin pathways. Contextual duality—where the same ubiquitin enzyme exerts opposite effects in different genetic backgrounds—necessitates careful patient selection [22]. FBXW7 exemplifies this challenge: in p53-wild type colorectal tumors, it promotes radioresistance by degrading p53, while in non-small cell lung cancer with SOX9 overexpression, FBXW7 enhances radiosensitivity by destabilizing SOX9 [22]. Comprehensive molecular profiling including mutation status, ubiquitin enzyme expression patterns, and ubiquitin chain linkage analysis can help identify patients most likely to respond to specific ubiquitin-targeted therapies.
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Research Reagents for Studying Ubiquitin Network Redundancy
| Reagent Category | Specific Examples | Research Applications |
|---|---|---|
| Tagged Ubiquitin Constructs | His-Ub, Strep-Ub, HA-Ub [28] | Affinity purification of ubiquitinated proteins; ubiquitination site mapping |
| Linkage-Specific Antibodies | K48-linkage specific, K63-linkage specific, M1-linear specific [28] | Detection and enrichment of specific ubiquitin chain types |
| TUBEs (Tandem Ubiquitin-Binding Entities) | Recombinant proteins with multiple UBDs [28] | High-affinity enrichment of polyubiquitinated proteins; protection from DUBs |
| Activity-Based Probes | Ub-VS, Ub-PA, linkage-specific DUB probes [28] | Profiling DUB activity and specificity in complex mixtures |
| E1/E2/E3 Inhibitors | TAK-243 (E1 inhibitor), CC-90009 (E2 inhibitor), MLN4924 (NAE inhibitor) | Specific perturbation of ubiquitination cascade components |
| DUB Inhibitors | b-AP15, PR-619, P5091, VLX1570 | Pan-DUB inhibition; identification of DUB-specific substrates |
| CRISPR Libraries | E3 ligase knockout library, DUB knockout library | Systematic identification of functional redundancies and synthetic lethal interactions |
Future Directions and Concluding Perspectives
The intricate redundancy and adaptive capacity of the ubiquitin network represent both a formidable challenge and a potential opportunity for cancer therapy. Future progress will require development of more sophisticated experimental approaches that capture the dynamic, multi-scale nature of ubiquitin signaling. Advanced proteomic methods that simultaneously quantify protein abundance, ubiquitination status, and phosphorylation events across multiple time points will be essential for mapping the systems-level adaptations that occur following ubiquitin network perturbation [61]. Similarly, single-cell analysis technologies applied to ubiquitin signaling may reveal cell-to-cell heterogeneity in adaptive responses that are masked in bulk analyses.
From a therapeutic perspective, the field is increasingly moving toward context-specific targeting strategies that account for the genetic background, tissue origin, and evolutionary state of individual tumors. Innovative therapeutic platforms such as radiation-activated PROTACs [22] and ubiquitin variant technologies that selectively disrupt specific protein-protein interactions within the ubiquitin network [59] offer promising approaches for achieving sufficient specificity to overcome redundant networks. Additionally, targeting the adaptive responses themselves—for instance, by inhibiting the transcriptional programs that are activated when ubiquitination is impaired—may create synergistic effects that prevent resistance development.
In conclusion, addressing functional redundancy and adaptive responses in the ubiquitin network requires a multifaceted strategy combining sophisticated diagnostic approaches, rational combination therapies, and innovative therapeutic modalities. As our understanding of ubiquitin network dynamics continues to deepen, particularly through systematic quantitative proteomics and functional genomics approaches, we can anticipate increasingly effective strategies for manipulating this crucial regulatory system in cancer therapy.
The ubiquitin-proteasome system (UPS) has been validated as a therapeutic target in oncology, most notably by the clinical success of the proteasome inhibitor bortezomib for treating hematologic malignancies [62] [63]. However, the therapeutic targeting of upstream components of the UPS, particularly E3 ubiquitin ligases and deubiquitinases (DUBs), offers the potential for greater specificity by modulating discrete subsets of cellular proteins rather than causing global proteostasis disruption [62]. This strategic shift promises to reduce the offtarget toxicity associated with broader proteasome inhibition while potentially overcoming the resistance mechanisms that have limited earlier therapies.
The central challenge in therapeutic targeting of E3 ligases and DUBs lies in achieving sufficient specificity to minimize on-target toxicities while maintaining therapeutic efficacy. Although the human genome encodes approximately 600 E3 ligases and nearly 100 DUBs, these enzyme families exhibit remarkable structural conservation in their catalytic cores, presenting significant hurdles for selective small-molecule inhibition [63] [64]. This technical guide examines the molecular basis for specificity in E3 ligase and DUB function, outlines experimental approaches for developing selective inhibitors, and provides methodologies for profiling inhibitor selectivity and on-target toxicity within the context of cancer research.
Molecular Foundations of Specificity in the Ubiquitin System
E3 Ligase Architecture and Substrate Recognition
E3 ubiquitin ligases confer specificity to the ubiquitination system by recognizing substrate proteins and facilitating ubiquitin transfer. They are broadly categorized into two major classes based on their catalytic mechanisms: RING-type E3s that function as scaffolds to directly transfer ubiquitin from E2 enzymes to substrates, and HECT-type E3s that form an obligate thioester intermediate with ubiquitin before transferring it to substrates [62]. This structural distinction creates different opportunities for therapeutic intervention, with HECT domains offering a defined catalytic pocket that may be more amenable to small-molecule targeting.
The specificity of E3 ligases is determined by multiple molecular interactions beyond the catalytic core. Many E3s contain substrate-recognition domains that bind to specific degron motifs in target proteins, while others require assembly into multi-protein complexes (such as SCF complexes) that modulate their substrate specificity [62]. Additionally, allosteric regulatory mechanisms control the activity of many E3 ligases, providing yet another avenue for selective modulation. For instance, the HECT E3 ligase family members are frequently maintained in autoinhibited states that require specific activating signals, suggesting that molecules mimicking these regulatory interactions could achieve greater specificity than active-site-directed inhibitors [62].
DUB Enzyme Families and Linkage Selectivity
Deubiquitinases counterbalance E3 ligase activity by removing ubiquitin modifications from protein substrates. The approximately 100 human DUBs are classified into two major mechanistic classes: cysteine proteases (including USP, UCH, OTU, MJD, and MCP families) and zinc metalloproteases (JAMM family) [65] [63]. This classification has important implications for inhibitor development, as the distinct catalytic mechanisms require different chemotypes for effective inhibition.
DUBs exhibit varying degrees of specificity for different ubiquitin chain linkages. Comprehensive specificity profiling of 42 human DUBs against all possible diubiquitin topoisomers has revealed distinct patterns of linkage preference [65]. As shown in Table 1, DUBs can be categorized based on their linkage specificity, which informs both their biological functions and their potential for selective targeting.
Table 1: Categorization of DUB Specificity Based on Linkage Preference
| Specificity Group | Representative DUBs | Linkage Preference | Characteristics |
|---|---|---|---|
| High Specificity | OTULIN, OTUB1, AMSH, BRCC3 | M1/linear, K48, or K63 | Cleave only one diubiquitin substrate even at high enzyme concentrations |
| Moderate Selectivity | Cezanne, OTUD1, A20, TRABID | K11, K48, K63, or K29/K33 | Highly specific to one linkage at low concentrations but less selective at high concentrations |
| Low Selectivity | Most USP family members | Multiple linkages | Display little linkage selectivity across concentration ranges |
Beyond linkage specificity, DUBs employ multiple mechanisms to achieve substrate selectivity. Many DUBs contain ubiquitin-binding domains (UBDs) that facilitate recognition of specific ubiquitin chain topologies, while others are recruited to specific cellular compartments or protein complexes where they encounter particular substrates [63]. The proteasome-associated DUBs (USP14, UCHL5, and RPN11) exemplify this compartmentalization, as their activity is regulated by proteasome binding, creating a unique therapeutic opportunity for targeting localized DUB functions without affecting the same enzymes in other cellular contexts [66].
Strategic Approaches for Achieving Specific Inhibition
Allosteric Targeting and Molecular Glues
The high degree of conservation in catalytic sites across E3 and DUB families has prompted exploration of allosteric inhibition strategies. Structural studies have revealed that many DUBs exist in autoinhibited conformations that are activated through specific protein interactions or post-translational modifications. For example, USP7 and USP4 employ different allosteric regulatory mechanisms despite their structural similarity, suggesting that family-specific allosteric sites may be targeted for selective inhibition [66]. Similarly, the deubiquitinase UCHL5 can be switched on and off by structurally related regulators in the context of the proteasome and the INO80 chromatin remodeler, respectively [66].
Molecular glues represent another emerging strategy for achieving specificity. These compounds induce or stabilize protein-protein interactions between E3 ligases and target proteins, effectively hijacking the ubiquitin system for targeted protein degradation. While not direct inhibitors of E3 catalytic activity, molecular glues like the immunomodulatory drugs (IMiDs) that target the CRL4CRBN E3 complex demonstrate how small molecules can achieve remarkable specificity by modulating substrate receptor interactions rather than directly blocking catalytic function [64].
Exploiting Structural Variations and Family-Wide Screening
The strategic selection of E3 ligase and DUB targets with unique structural features can facilitate the development of specific inhibitors. For instance, the HECT family E3s possess a catalytic domain that is structurally distinct from the more prevalent RING-type E3s, potentially offering better opportunities for selective inhibitor development [62]. Similarly, the JAMM family DUBs employ a zinc metalloprotease mechanism that is fundamentally different from the cysteine protease mechanism used by most other DUB families, enabling the development of chemotypes that selectively target this enzyme class [65] [63].
Family-wide screening approaches have emerged as powerful tools for identifying selective starting points for inhibitor development. Parallel screening of multiple DUBs against the same compound library enables the rapid identification of selectivity patterns and helps prioritize chemical series with inherent specificity. As illustrated in Figure 1, this approach facilitates the direct comparison of inhibitor potency across multiple DUBs, enabling the selection of compounds with the desired selectivity profile early in the discovery process [64].
Figure 1: High-Throughput Screening Workflow for Selective DUB Inhibitor Identification. This multi-DUB parallel screening approach enables rapid identification of compounds with inherent selectivity profiles [64].
Experimental Methodologies for Specificity Profiling
Advanced Biochemical Assays for DUB Specificity Assessment
MALDI-TOF Mass Spectrometry-Based DUB Assay
The MALDI-TOF DUB assay represents a significant advancement in specificity profiling by enabling direct quantification of DUB activity against physiological ubiquitin chain linkages. This method uses unmodified diubiquitin substrates with defined linkage topologies, preserving the native isopeptide bonds that are critical for assessing true linkage specificity [65].
Protocol:
- Reaction Setup: Prepare 5 μL reactions containing recombinant DUB (0.1-1000 ng), specific diubiquitin topoisomer (125 ng, 7,300 fmol) in 40 mM Tris-HCl pH 7.5, 5 mM DTT, and 0.25 μg BSA carrier.
- Incubation: Conduct reactions for 1 hour at 30°C.
- Termination: Stop reactions by adding 1 μL of 10% trifluoroacetic acid.
- Internal Standard Addition: Spike 2 μL of each sample with 2 μL (1,000 fmol) of 15N-labeled ubiquitin for quantitative normalization.
- Matrix Preparation: Add 2 μL of 15.2 mg/mL 2,5-dihydroxyacetophenone (DHAP) matrix and 2 μL of 2% trifluoroacetic acid.
- Spotting and Analysis: Spot 0.5 μL onto a 1,536 microtiter plate MALDI anchor target and analyze by high mass accuracy MALDI-TOF MS in reflector positive ion mode.
This assay achieves a lower limit of quantification of 10 nM ubiquitin (2 fmol on target), significantly reducing enzyme and substrate requirements compared to traditional gel-based methods [65]. The methodology has been applied to profile the linkage specificity of 42 human DUBs, generating an extensive resource for DUB activity and specificity.
AlphaLISA-Based Tetraubiquitin Cleavage Assay
For higher throughput screening applications, AlphaLISA technology combined with Tandem Ubiquitin Binding Entities (TUBEs) and tetraubiquitin substrates provides a sensitive, homogeneous assay format that maintains biological relevance through the use of longer ubiquitin chains with specific linkages [66]. This approach bridges the gap between the physiological relevance of diubiquitin cleavage assays and the throughput requirements of drug discovery programs.
Cellular Target Engagement and Selectivity Assessment
Endpoint and Phenotypic Cellular Assays
Cellular validation of E3 ligase and DUB inhibitors requires demonstration of target engagement and expected phenotypic consequences. For E3 ligase inhibitors targeting specific substrates, immunoblotting for substrate accumulation provides direct evidence of target engagement. Similarly, for DUB inhibitors, monitoring the stabilization of known substrates or changes in global ubiquitination patterns can confirm cellular activity [64] [67].
For inhibitors targeting the ubiquitin system in specific pathological contexts, synthetic lethality screens in isogenic cell lines can demonstrate the therapeutic window and mechanistic specificity. For example, USP11 inhibition was shown to selectively kill platinum-resistant ovarian cancer cells while sparing platinum-sensitive counterparts, establishing a therapeutic window rooted in genetic vulnerability [66].
Activity-Based Protein Profiling (ABPP)
Activity-based probes that covalently label the active sites of DUBs enable direct assessment of target engagement in cellular lysates and live cells. These probes, such as ubiquitin-vinyl sulfones or ubiquitin-ABPs, can be used to measure the occupancy of DUB active sites by inhibitors, providing a direct readout of cellular target engagement [66]. When combined with quantitative mass spectrometry, ABPP enables comprehensive selectivity profiling across the entire DUB family in cellular contexts.
The Scientist's Toolkit: Essential Research Reagents and Solutions
Table 2: Key Research Reagents for E3 Ligase and DUB Inhibitor Development
| Reagent/Solution | Function and Application | Key Features |
|---|---|---|
| Diubiquitin Topoisomers | Substrates for linkage specificity profiling | All eight native linkage types (M1, K6, K11, K27, K29, K33, K48, K63); preserve physiological isopeptide bonds |
| Ubiquitin-Rhodamine 110 (Ub-Rho) | Fluorogenic substrate for high-throughput screening | Continuous, sensitive readout; adaptable to most DUBs; compatible with HTS automation |
| Activity-Based DUB Probes | Target engagement and occupancy studies | Covalently label active DUBs; enable cellular target engagement assessment |
| 15N-Labeled Ubiquitin | Internal standard for MALDI-TOF quantification | Enables precise quantification of ubiquitin generation; normalizes experimental variability |
| Tandem Ubiquitin Binding Entities (TUBEs) | Isolation of polyubiquitinated proteins | High affinity for polyubiquitin chains; protect against DUB-mediated deubiquitination |
| Recombinant DUB Panels | Selectivity profiling | Comprehensive coverage of DUB families; standardized activity for cross-comparison |
Case Studies in Specific Inhibitor Development
USP7 Inhibitor Development: From Screening to Clinical Candidates
USP7 represents one of the most extensively studied DUB targets, with multiple chemical series advancing to preclinical development. The development of USP7 inhibitors illustrates several key principles for achieving specificity:
Exploiting Unique Structural Features: Selective USP7 inhibitors often target allosteric sites or unique conformational states rather than the conserved catalytic triad [66].
Cellular Validation through Substrate Stabilization: Successful USP7 inhibitors demonstrate dose-dependent stabilization of known substrates such as p53, providing functional evidence of target engagement [64].
Dual Mechanisms of Action: Interestingly, USP7 inhibitors have demonstrated both direct antitumor activity through p53 stabilization and immune-mediated effects through Treg impairment, highlighting how understanding the full biological context of target inhibition can reveal additional therapeutic benefits [66].
Proteasome-Associated DUB Inhibitors: b-AP15 and VLX1570
The proteasome-associated DUB inhibitors b-AP15 and its optimized derivative VLX1570 target both USP14 and UCHL5, demonstrating that selective inhibition of specific DUB subclasses can achieve therapeutic effects distinct from broad proteasome inhibition [66]. These compounds:
- Act as competitive inhibitors of proteasome DUB activity without affecting the catalytic activities of the 20S proteasome core particle
- Generate a robust proteotoxic stress response characterized by chaperone upregulation, ER stress, and oxidative stress
- Show in vivo efficacy in models of multiple myeloma with a potential therapeutic window
The development of VLX1570 highlights how targeting specific DUB complexes (in this case, the proteasome-associated DUBs) can achieve a desired therapeutic effect while potentially minimizing offtarget toxicity relative to broader proteasome inhibition.
Future Directions and Concluding Perspectives
The field of E3 ligase and DUB inhibitor development is rapidly evolving, with several promising strategies emerging to enhance specificity and minimize on-target toxicity. PROTAC (Proteolysis Targeting Chimera) technology represents a complementary approach that hijacks E3 ligases for targeted protein degradation rather than inhibiting their catalytic activity, potentially bypassing some of the specificity challenges associated with direct inhibition [16]. Similarly, the development of bifunctional DUB inhibitors that simultaneously target DUB enzymes and their specific substrate recognition interfaces may enable more precise modulation of DUB activity toward specific pathogenic substrates.
Tissue-specific delivery approaches, including antibody-drug conjugates and nanoparticle-based delivery systems, offer potential solutions to on-target toxicity by restricting inhibitor activity to diseased tissues [68]. Additionally, the integration of structural biology and machine learning approaches is enabling more rational design of specific inhibitors by identifying subtle structural differences among closely related E3 ligases and DUBs that can be exploited for selective targeting.
As our understanding of the complexity of the ubiquitin code deepens, the therapeutic targeting of E3 ligases and DUBs will continue to evolve toward greater specificity and sophistication. The experimental frameworks and methodologies outlined in this technical guide provide a foundation for developing the next generation of ubiquitin system therapeutics that achieve the requisite specificity to minimize on-target toxicity while effectively modulating disease-relevant pathways in cancer and other pathologies.
Strategies to Overcome Therapy Resistance in Ubiquitin-Targeted Treatments
The ubiquitin-proteasome system (UPS) represents a sophisticated post-translational regulatory network that governs virtually all cellular processes through targeted protein degradation and signal transduction. In cancer biology, alterations to the ubiquitin code—the specific patterns and chain topologies by which ubiquitin molecules are attached to substrate proteins—drive tumor development, progression, and therapeutic resistance [16] [69]. The ubiquitin system employs a hierarchical enzymatic cascade consisting of E1 activating enzymes, E2 conjugating enzymes, and E3 ligases to conjugate ubiquitin to specific protein substrates, while deubiquitinating enzymes (DUBs) reverse this process through ubiquitin removal [69] [70]. While ubiquitin-targeted therapies have emerged as promising anti-cancer strategies, their efficacy is frequently limited by the development of resistance mechanisms that allow cancer cells to adapt and survive [71] [72]. Understanding and overcoming these resistance pathways is paramount for advancing the next generation of ubiquitin-focused cancer therapeutics.
The clinical burden of therapy resistance is substantial across oncology, affecting approximately 90% of chemotherapy failures and more than 50% of targeted therapy or immunotherapy failures [73]. In the specific context of ubiquitin-targeted treatments, resistance manifests through diverse adaptive mechanisms including functional redundancy within ubiquitin network components, alteration of substrate recognition sites, upregulation of compensatory survival pathways, and metabolic rewiring [16] [69]. This comprehensive review synthesizes current strategies to overcome resistance in ubiquitin-targeted cancer treatments, with a specific focus on mechanistic insights, experimental approaches, and emerging therapeutic modalities that target the UPS.
Molecular Mechanisms of Resistance in Ubiquitin-Targeted Therapies
Alterations in E2 Conjugating Enzymes and E3 Ligases
The specificity of ubiquitin signaling is largely determined by the coordinated action of E2 conjugating enzymes and E3 ligases, which collectively recognize and ubiquitinate specific protein substrates. Dysregulation of these components represents a fundamental resistance mechanism in ubiquitin-targeted therapies. In prostate cancer, resistance to antiandrogen therapies frequently develops through loss of the ubiquitin-conjugating enzyme E2 J1 (UBE2J1), which occurs in 5-15% of patients [71]. UBE2J1 normally promotes the ubiquitination and degradation of the androgen receptor (AR), and its loss leads to AR accumulation, enhanced AR signaling, and therapy resistance [71]. Beyond hormonal cancers, UBE2J1 also demonstrates tumor-suppressive functions in colorectal cancer by promoting degradation of RPS3 and inhibiting NF-κB signaling, suggesting its loss may confer resistance across multiple cancer types [71].
E3 ligases represent the largest family of UPS components, with over 600 members in the human genome, yet only a handful are currently targeted therapeutically [74]. This limited repertoire creates vulnerability to resistance through mutational escape and functional compensation. Tumors frequently develop resistance to E3-targeting therapies through point mutations in substrate recognition domains, overexpression of alternative E3 ligases with overlapping functions, or epigenetic rewiring that bypasses the targeted E3 dependency [16] [72]. The spatiotemporal control of E3 ligase expression and activity further complicates therapeutic targeting, as dynamic adaptation following treatment pressure enables resistant clones to emerge [16].
Overexpression and Dysregulation of Deubiquitinating Enzymes (DUBs)
Deubiquitinating enzymes (DUBs), particularly ubiquitin-specific proteases (USPs), counterbalance ubiquitin signaling by removing ubiquitin modifications from substrate proteins. Overexpression of specific USPs represents a major resistance mechanism across multiple cancer therapy modalities, including chemotherapy, targeted therapy, immunotherapy, and radiotherapy [69]. USP family members promote resistance by stabilizing key oncoproteins, enhancing DNA damage repair capacity, maintaining cancer stem cell properties, and facilitating immune evasion [69] [70].
In lung cancer, USP51 overexpression contributes to cisplatin resistance by diminishing γH2AX formation (a marker of DNA double-strand breaks) and increasing checkpoint kinase 1 (CHK1) phosphorylation, thereby ensuring effective cell cycle progression despite genotoxic stress [69]. Similarly, USP22 enhances DNA damage repair in lung adenocarcinoma by interacting with PALB2 and facilitating recruitment of the PALB2-BRCA2-Rad51 complex to damage sites [69]. Beyond DNA damage response, USPs stabilize numerous oncoproteins across cancer types; in biliary tract cancer, multiple USP family members (including USP1, USP3, USP7, USP8, USP9X, USP21, and USP22) demonstrate differential expression that correlates with stabilization of key oncoproteins like PARP1, DNM1L, and OGT [70].
Table 1: Deubiquitinating Enzymes Implicated in Therapy Resistance
| DUB Family | Specific Member | Cancer Type | Resistance Mechanism |
|---|---|---|---|
| USP | USP51 | Lung Cancer | Diminishes γH2AX formation, increases CHK1 phosphorylation |
| USP | USP22 | Lung Adenocarcinoma | Enhances DNA repair via PALB2-BRCA2-Rad51 complex recruitment |
| USP | USP1 | Prostate Cancer | Blocks K48-linked polyubiquitination of SIX1 |
| USP | USP7 | Colorectal Cancer | Upregulates Wnt/β-catenin signaling |
| USP | USP48 | Hepatocellular Cancer | Alters SIRT6 stabilization |
| USP | Multiple | Biliary Tract Cancer | Stabilizes oncoproteins (PARP1, DNM1L, OGT) |
Ubiquitin Chain Topology Alterations and Signaling Rewiring
The ubiquitin code encompasses diverse chain topologies that determine functional outcomes for modified substrates. Cancer cells exploit this complexity to develop resistance through alterations in chain assembly and recognition [16]. The specific linkage types—including K48-linked proteolysis versus K63-mediated signaling—create a sophisticated regulatory network that tumors dynamically rewire under therapeutic pressure [16]. For instance, monoubiquitination of both histone and non-histone proteins collaboratively modulates chromatin dynamics and DNA damage responses to maintain genome integrity during radiation treatment, contributing to radiotherapy resistance [16].
Beyond chain topology, ubiquitin signaling exhibits extensive crosstalk with other post-translational modifications including phosphorylation, SUMOylation, and acetylation [16]. This PTM crosstalk creates multidimensional regulatory networks that enable robust adaptive responses to ubiquitin-targeted therapies. Tumors frequently develop resistance through upregulation of compensatory modification pathways that bypass inhibited ubiquitin signaling nodes, creating complex dependencies that evolve during treatment [16] [69]. The dynamic reversibility of ubiquitin modifications further enables rapid adaptive responses that protect essential oncoproteins from targeted degradation [16].
Advanced Therapeutic Strategies to Overcome Resistance
Next-Generation Targeted Protein Degradation Approaches
Targeted protein degradation (TPD) represents a revolutionary therapeutic strategy that leverages the cell's intrinsic proteolytic systems to eliminate disease-causing proteins. Two primary technologies dominate this field: proteolysis-targeting chimeras (PROTACs) and molecular glues [74]. PROTACs are bifunctional molecules that consist of a target protein-binding ligand connected via a linker to an E3 ligase-recruiting ligand, thereby bringing the E3 ligase into proximity with the target protein to facilitate its ubiquitination and degradation [71] [74]. This approach offers several advantages over traditional inhibition, including the ability to target "undruggable" proteins, achieve higher specificity, and overcome resistance mutations that affect drug binding but not degradation [74].
PROTACs have demonstrated remarkable efficacy in overcoming resistance to conventional therapies. In prostate cancer resistant to antiandrogens due to UBE2J1 deficiency, ubiquitination-based AR degraders (such as AC0176) effectively restored AR degradation and suppressed tumor growth [71]. Similarly, PROTAC-type degraders like ARD-61 and ARD-266 have shown promising results in both enzalutamide-sensitive and resistant prostate cancer models, significantly reducing AR-regulated gene expression and inhibiting tumor growth [71]. Beyond prostate cancer, PROTACs have shown efficacy in breast cancer and T-cell acute lymphoblastic leukemia (T-ALL), where they disrupt critical pathways and reduce tumor progression effectively [71].
Table 2: Comparison of Targeted Protein Degradation Platforms
| Platform | Mechanism | Advantages | Limitations | Clinical Status |
|---|---|---|---|---|
| PROTAC | Bifunctional molecule connecting target protein to E3 ligase | Targets "undruggable" proteins; catalytic activity; broad target range | Large molecular size; potential hook effect; limited E3 ligase toolbox | Multiple candidates in clinical trials (e.g., KT-253) |
| Molecular Glues | Monovalent molecules enhancing natural protein-protein interactions | Smaller size; favorable pharmacokinetics; oral bioavailability | Serendipitous discovery; limited rational design capability | Several in clinical use (e.g., immunomodulatory drugs) |
| SNIPER | IAP-based PROTAC variants | Dual degradation of target and IAPs; strong anti-proliferative activity | Complex selectivity patterns | Preclinical development |
Molecular glues represent an alternative TPD strategy that operates through monovalent molecules that enhance natural protein-protein interactions between E3 ligases and target proteins [74]. Unlike PROTACs, molecular glues are typically smaller molecules with favorable pharmacokinetic properties and potential for oral administration. However, their discovery has been largely serendipitous due to the unpredictable nature of protein-protein interactions, making rational design challenging [74]. Both PROTACs and molecular glues complement each other in advancing the TPD landscape, offering diverse approaches to overcome resistance in ubiquitin-targeted therapies.
Inhibition of Deubiquitinating Enzymes
Strategic inhibition of specific DUBs, particularly USPs, presents a promising approach to reverse therapy resistance across multiple cancer types. USP inhibitors can resensitize resistant tumors by preventing the stabilization of oncoproteins, impairing DNA damage repair, and restoring apoptotic sensitivity [69]. The integration of USP inhibitors with existing anti-cancer therapies offers a rational combination strategy to circumvent drug resistance [69].
Several USP inhibitors have demonstrated preclinical efficacy in overcoming resistance. For instance, targeting USP1 in prostate cancer restores K48-linked polyubiquitination of SIX1, while USP7 inhibition in colorectal cancer downregulates Wnt/β-catenin signaling [75]. In breast cancer, USP1 inhibition reduces metastasis and cell migration in vitro [75]. The therapeutic potential of USP inhibition extends beyond monotherapy, as combining USP inhibitors with conventional chemotherapy, targeted therapy, or immunotherapy can synergistically enhance anti-tumor efficacy and prevent resistance development [69].
Despite promising preclinical results, clinical translation of USP inhibitors faces challenges including functional redundancy among USP family members, unintended on-target toxicity, and adaptive tumor responses [16] [69]. Overcoming these limitations will require improved isoform selectivity, biomarker-guided patient selection, and optimized combination regimens that maximize therapeutic index while minimizing toxicity.
Biomarker-Driven Patient Stratification and Combination Therapies
Precision medicine approaches that incorporate biomarker-guided therapeutic strategies are emerging as fundamental components of next-generation ubiquitin-targeted treatments [16] [75]. The identification of predictive biomarkers enables patient stratification to identify those most likely to benefit from specific ubiquitin-targeted therapies, thereby maximizing efficacy while minimizing unnecessary toxicity.
In lung adenocarcinoma (LUAD), ubiquitin-related gene signatures have been developed to predict prognosis and therapeutic response [75]. A risk model incorporating nine ubiquitin-related genes (B4GALT4, DNAJB4, GORAB, HEATR1, LPGAT1, FAT1, GAB2, MTMR4, and TCP11L2) effectively stratified LUAD patients into low- and high-risk groups, with significant differences in overall survival and immune cell infiltration patterns [75]. Similarly, in colon adenocarcinoma (COAD), a prognostic signature based on six ubiquitin-related gene pairs (URGPs) successfully classified patients according to risk, with the low-risk group demonstrating higher levels of immune cell infiltration and improved response to immunotherapy [76].
Rational combination therapies that simultaneously target multiple nodes within the ubiquitin network or combine ubiquitin-targeted agents with conventional therapies represent a promising strategy to overcome resistance. For example, combining PROTACs with USP inhibitors may prevent stabilization of the target protein, thereby enhancing degradation efficacy [69] [74]. Similarly, integrating ubiquitin-targeting agents with standard chemotherapy, radiotherapy, or immunotherapy can leverage synthetic lethal interactions and prevent compensatory adaptation [16] [72].
Experimental Approaches and Research Methodologies
Computational and Machine Learning Approaches
Advanced computational methods have revolutionized the identification of ubiquitin-related biomarkers and resistance mechanisms. Machine learning algorithms integrated with multi-omics data enable robust prediction of therapeutic response and resistance patterns [77] [76]. For colon cancer, the ABF-CatBoost integration model achieves exceptional accuracy (98.6%), specificity (0.984), sensitivity (0.979), and F1-score (0.978) in classifying patients based on molecular profiles and predicting drug responses [77]. This approach facilitates multi-targeted therapeutic strategies by analyzing mutation patterns, adaptive resistance mechanisms, and conserved binding sites.
Weighted Gene Co-expression Network Analysis (WGCNA) represents another powerful bioinformatics method to identify ubiquitin-related gene modules associated with cancer progression and therapy resistance [75] [76]. By constructing co-expression networks from transcriptomic data, researchers can identify clusters of highly correlated genes (modules) that may represent functional networks within the ubiquitin system. These modules can then be correlated with clinical traits, including therapy response and resistance development, to prioritize candidate genes for functional validation [75].
The following diagram illustrates a typical computational workflow for identifying ubiquitin-related resistance signatures:
Functional Validation Experiments
Robust functional validation is essential for confirming the role of candidate ubiquitin system components in therapy resistance. A comprehensive experimental approach typically includes in vitro cell-based assays, in vivo animal models, and mechanistic studies to elucidate molecular pathways [75].
Key functional assays include:
- CCK-8 proliferation assays to assess cell viability following targeted inhibition or genetic perturbation of ubiquitin system components [75]
- Wound healing assays to evaluate migratory capacity in the context of ubiquitin pathway modulation [75]
- Transwell invasion assays to measure invasive potential following manipulation of specific E3 ligases or DUBs [75]
- Colony formation assays to determine long-term clonogenic survival following treatment with ubiquitin-targeted agents [72]
- Apoptosis assays to quantify cell death induction following targeted protein degradation or DUB inhibition [72]
For in vivo validation, xenograft mouse models represent the gold standard for evaluating the therapeutic efficacy of ubiquitin-targeted agents and assessing resistance development. Patient-derived xenograft (PDX) models that maintain the tumor microenvironment and heterogeneity of human cancers offer particularly relevant platforms for studying resistance mechanisms and testing combination strategies [71] [74].
The following diagram illustrates the key signaling pathways regulated by ubiquitination that contribute to therapy resistance:
The Scientist's Toolkit: Essential Research Reagents and Platforms
Table 3: Key Research Reagent Solutions for Studying Ubiquitin-Mediated Resistance
| Reagent Category | Specific Examples | Research Applications | Commercial Sources |
|---|---|---|---|
| E3 Ligase Ligands | VHL ligands, CRBN ligands (lenalidomide), MDM2 ligands (Nutlin-3), IAP ligands (LCL-161) | PROTAC development, E3 ligase function studies | MedChemExpress, Selleckchem, Cayman Chemical |
| DUB Inhibitors | USP1, USP7, USP9X, USP14 inhibitors | DUB target validation, combination therapy studies | Sigma-Aldrich, Tocris, APExBIO |
| PROTAC Molecules | AR degraders (ARD-61, ARD-266), BET degraders (ARV-825) | Targeted protein degradation studies, resistance modeling | MedChemExpress, Tocris, Cayman Chemical |
| Ubiquitin Activity Probes | HA-Ub-VS, TAMRA-Ub-PA, Ub-AMC | DUB activity profiling, ubiquitin chain linkage specificity | Boston Biochem, R&D Systems, LifeSensors |
| Computational Tools | iUUCD 2.0 database, WGCNA R package, CatBoost algorithm | Ubiquitin gene signature development, resistance prediction | Public databases, open-source platforms |
| Cell Line Models | UBE2J1-deficient prostate cancer lines, USP-overexpressing models | Resistance mechanism validation, drug screening | ATCC, DSMZ, commercial providers |
The ubiquitin system represents a sophisticated regulatory network that cancer cells exploit to develop resistance to targeted therapies. Overcoming this resistance requires multi-faceted strategies that target specific vulnerabilities within the ubiquitin code. Next-generation targeted protein degradation platforms like PROTACs and molecular glues offer promising approaches to eliminate traditionally "undruggable" oncoproteins and overcome resistance mutations [74]. Complementary strategies focusing on inhibition of specific DUBs, particularly USPs, can reverse stabilization of key resistance drivers and restore therapeutic sensitivity [69].
Future advances in overcoming resistance will depend on improved biomarker development for patient stratification, rational combination therapies that prevent compensatory adaptation, and enhanced understanding of ubiquitin chain topology in resistance mechanisms [16] [75]. Computational approaches integrating multi-omics data with machine learning algorithms will play an increasingly important role in predicting resistance patterns and guiding therapeutic selection [77] [76]. Additionally, the development of novel E3 ligase ligands beyond the current limited repertoire will expand the therapeutic landscape of ubiquitin-targeted therapies and reduce vulnerability to resistance through functional redundancy [74].
As the field advances, the dynamic reversibility of ubiquitin modifications, chain topology diversity, and recent breakthroughs in targeted degradation technologies position the ubiquitin system as a central focus for next-generation cancer therapeutics [16]. By integrating mechanistic insights with biomarker-guided therapeutic strategies, ubiquitin-targeting agents are poised to become fundamental components of precision oncology approaches designed to overcome therapy resistance and improve patient outcomes.
The ubiquitin-proteasome system (UPS) represents a master regulatory network in cellular homeostasis, with its dysfunction being a hallmark of cancer. This whitepaper examines the context-dependent functionalities of the E3 ligase FBXW7 and the deubiquitinase USP14 within the cancer ubiquitin landscape. Through detailed analysis of molecular mechanisms, signaling pathways, and experimental approaches, we demonstrate how these enzymes exhibit paradoxical roles as both tumor suppressors and promoters depending on cellular context, genetic background, and tumor microenvironment. Our findings underscore the critical importance of understanding contextual ubiquitin code alterations for developing precision oncology therapeutics that target the UPS.
The ubiquitin code constitutes a sophisticated post-translational regulatory language that governs virtually all cellular processes through targeted protein degradation and signaling modulation. The ubiquitination process involves a sequential enzymatic cascade comprising ubiquitin-activating (E1), conjugating (E2), and ligase (E3) enzymes, while deubiquitinases (DUBs) provide the counterbalancing editing function [78] [6]. With over 600 E3 ligases and approximately 100 DUBs encoded in the human genome, this system exhibits tremendous specificity and regulatory complexity [79]. FBXW7 (F-box and WD repeat domain-containing 7) represents one of the most well-characterized tumor suppressor E3 ligases, functioning as the substrate recognition component of the SKP1-CUL1-F-box (SCF) ubiquitin ligase complex [78] [79]. Conversely, USP14 exemplifies a context-dependent DUB that dynamically regulates protein stability in cancer pathways. The emerging paradigm shift in ubiquitin research reveals that these enzymes do not operate with fixed functionalities but rather exhibit context-dependent roles influenced by cellular environment, genetic background, and tissue-specific factors [29] [22]. This whitepaper synthesizes current understanding of FBXW7 and USP14 as exemplars of ubiquitin code plasticity in cancer development and therapeutic resistance.
FBXW7: Structural Basis and Canonical Tumor Suppressor Functions
Molecular Architecture and Mechanism
FBXW7 serves as a critical substrate receptor within the SCF E3 ubiquitin ligase complex, characterized by a conserved structural organization that enables precise target recognition [78] [79]. The gene encodes three primary isoforms through alternative splicing—FBXW7α (nuclear), FBXW7β (cytoplasmic), and FBXW7γ (nucleolar)—each with distinct subcellular localizations and potential functional specializations [78] [80]. The protein contains three essential domains: an N-terminal dimerization domain that facilitates oligomerization and regulatory complexity; a central F-box domain that mediates binding to the SKP1 adapter protein, connecting FBXW7 to the core SCF complex; and C-terminal WD40 repeats that fold into a β-propeller structure responsible for recognizing phosphorylated degron motifs in substrate proteins [78] [79]. This structural configuration enables FBXW7 to specifically bind phosphorylated substrates containing conserved CPD (Cdc4 phosphodegron) sequences, typically (L)-X-pT/pS-P-(P)-X-pS/pT, leading to their polyubiquitination and subsequent proteasomal degradation [80].
Oncogenic Substrate Network and Tumor Suppressive Mechanisms
FBXW7 functions as a master negative regulator of oncogenic signaling by targeting numerous proto-oncoproteins for destruction [78] [79]. The table below summarizes key FBXW7 substrates and their roles in cancer pathways:
Table 1: Principal FBXW7 Substrates and Their Cancer-Related Functions
| Substrate | Role in Oncogenesis | Cancer Pathways Affected |
|---|---|---|
| c-MYC | Transcriptional activator of proliferative genes | Cell growth, metabolism, apoptosis evasion |
| Cyclin E | Cell cycle regulator | G1/S transition, genomic instability |
| NOTCH1 | Signaling transducer | Differentiation, cell fate decisions |
| mTOR | Kinase signaling node | Nutrient sensing, growth control |
| c-JUN | Transcription factor | AP-1 complex, stress response |
| MCL-1 | Anti-apoptotic protein | Mitochondrial apoptosis evasion |
| SNAIL | Transcription factor | Epithelial-mesenchymal transition |
The tumor-suppressive function of FBXW7 is evidenced by its frequent inactivation in human cancers, with mutation rates approaching 16% in colorectal carcinoma and significant prevalence in other gastrointestinal malignancies [78] [79]. FBXW7 mutations typically occur as missense mutations within the WD40 domain substrate-binding pocket, with hotspot residues R465, R479, and R505 accounting for approximately 43% of all mutations, effectively disrupting substrate recognition and degradation [80]. Functional loss of FBXW7 leads to stabilization of its oncogenic substrates, driving uncontrolled proliferation, metabolic reprogramming, and therapeutic resistance across cancer types [78] [79] [80].
The Contextual Duality of FBXW7 in Cancer Biology
Tissue and Genetic Background Determinants
Emerging evidence reveals that FBXW7 exhibits context-dependent functionalities that extend beyond its canonical tumor suppressor role, particularly in response to DNA damage and therapeutic interventions [29] [22]. The p53 status of tumors represents a critical determinant of FBXW7 function in radiation response. In p53-wild type colorectal tumors, FBXW7 surprisingly promotes radioresistance by facilitating p53 degradation, thereby inhibiting apoptosis [29] [22]. Conversely, in non-small cell lung cancer (NSCLC) models with SOX9 overexpression, FBXW7 enhances radiosensitivity by destabilizing SOX9 and relieving p21 repression, independently of p53 status [29] [22]. This functional switch underscores how genetic background and signaling microenvironment dictate FBXW7's role in therapeutic responses.
Ubiquitin Chain Topology and Functional Diversity
The functional outcome of FBXW7 activity is further complicated by its ability to utilize different ubiquitin chain topologies for distinct purposes. While FBXW7 primarily generates K48-linked polyubiquitin chains that target substrates for proteasomal degradation, it also catalyzes K63-linked ubiquitination in specific contexts [29] [22]. For instance, FBXW7 facilitates non-homologous end joining (NHEJ) DNA repair through K63-linked polyubiquitylation of XRCC4, enhancing DNA repair fidelity [29] [22]. This chain topology plasticity enables FBXW7 to participate in both destructive and signaling functions, expanding its regulatory potential beyond simple protein degradation.
The following diagram illustrates the contextual regulation and functional outputs of FBXW7:
Diagram 1: Contextual regulation of FBXW7 function. Multiple factors including genetic background, cellular environment, and ubiquitin chain type determine functional outcomes.
USP14: A Contextual Deubiquitinase in Cancer Signaling
Molecular Characteristics and Regulatory Functions
USP14 represents a proteasome-associated deubiquitinating enzyme that dynamically regulates protein stability by removing ubiquitin chains from substrate proteins, thereby counteracting the activity of E3 ubiquitin ligases [29] [81]. As a member of the ubiquitin-specific protease (USP) family, USP14 exhibits a conserved catalytic domain that hydrolyzes ubiquitin conjugates, functioning as a critical editor of the ubiquitin code [29]. Unlike FBXW7, USP14 does not function in isolation but rather as an integral component of the 19S proteasomal regulatory particle, where it trims ubiquitin chains and facilitates substrate processing [81]. This subcellular localization positions USP14 as a gatekeeper of proteasomal degradation, enabling context-dependent stabilization of its target proteins.
Tissue-Specific and Substrate-Determined Roles in Cancer
USP14 demonstrates remarkable functional plasticity across cancer types, exhibiting both tumor-promoting and tumor-suppressive activities depending on cellular context [29]. In glioblastoma, USP14 stabilizes the RNA demethylase ALKBH5, maintaining cancer stemness properties and contributing to therapeutic resistance [29] [22]. Conversely, in head and neck squamous cell carcinomas (HNSCC), USP14 promotes the degradation of IκBα, resulting in constitutive activation of NF-κB signaling and driving inflammatory tumor progression [29]. This paradoxical ability to either stabilize or destabilize different substrates underscores the context-dependent nature of USP14 function and complicates its therapeutic targeting.
A particularly significant role for USP14 has been elucidated in immune checkpoint regulation within the tumor microenvironment. In non-small cell lung cancer (NSCLC), USP14 is recruited by PSMD11 to deubiquitinate and stabilize PD-L1, the critical ligand for immune checkpoint receptor PD-1 [81]. This mechanism facilitates tumor immune escape by enhancing PD-L1-mediated suppression of cytotoxic T cells, highlighting USP14's role in modulating tumor-immune interactions [81]. Inhibition of USP14 in this context promotes PD-L1 degradation and enhances anti-tumor immunity, suggesting strategic therapeutic opportunities for combination with immune checkpoint blockade [81].
Experimental Approaches for Studying Contextual Ubiquitin Enzymes
Methodological Framework for Ubiquitin Enzyme Characterization
Deciphering the context-dependent functions of ubiquitin enzymes requires a multidisciplinary experimental approach that integrates biochemical, genetic, and cell biological techniques. The following diagram outlines a comprehensive workflow for characterizing the functional networks of FBXW7 and USP14:
Diagram 2: Experimental workflow for characterizing context-dependent ubiquitin enzyme functions.
Key Research Reagent Solutions
The following table provides essential research tools for investigating FBXW7 and USP14 functions in cancer models:
Table 2: Essential Research Reagents for Ubiquitin Enzyme Studies
| Reagent Category | Specific Examples | Research Application | Experimental Context |
|---|---|---|---|
| Genetic Modulators | FBXW7 isoform-specific expression vectors | Functional reconstitution | Rescue experiments in knockout models |
| USP14 catalytic mutant (C114A) | Enzyme mechanism studies | Distinguishing catalytic vs. scaffolding functions | |
| DYRK2 kinase expression constructs | Regulatory kinase studies | FBXW7 phosphorylation and stability assays | |
| Chemical Inhibitors | IU1 (USP14 inhibitor) | DUB activity blockade | PD-L1 stabilization studies; immune function assays |
| DYRK2 kinase inhibitors | Regulatory axis disruption | Chemosensitivity modulation experiments | |
| Antibody Reagents | Phospho-specific FBXW7 substrate antibodies | Degron phosphorylation detection | Substrate engagement validation |
| K48- and K63-linkage specific ubiquitin antibodies | Chain topology determination | Ubiquitin chain type functional assignment | |
| PD-L1 ubiquitination state antibodies | Immune checkpoint regulation | Tumor-immune interaction studies | |
| Cell Models | FBXW7-/- HCT116 cells | Substrate accumulation studies | Functional consequences of FBXW7 loss |
| DYRK2-/- HEK-293T cells | Kinase regulatory studies | FBXW7 stability and degradation mechanisms | |
| PSMD11 knockdown NSCLC lines | Proteasome complex function | USP14 recruitment and PD-L1 regulation |
Detailed Experimental Protocol: USP14-PD-L1 Regulation in NSCLC
Based on recent investigations of USP14 in immune checkpoint regulation [81], the following detailed protocol can be applied to study USP14-PD-L1 functional interactions:
Objective: To evaluate USP14-mediated deubiquitination and stabilization of PD-L1 in non-small cell lung cancer models.
Methodology:
- Cell Culture and Transfection: Maintain A549 and H1299 NSCLC cell lines in DMEM supplemented with 10% FBS at 37°C with 5% CO₂. Transfect cells at 50-60% confluence using lipofectamine 2000 with the following constructs: siPSMD11, siUSP14, pcDNA3.1-PD-L1, and pcDNA3.1-USP14 according to manufacturer specifications.
Co-immunoprecipitation (Co-IP):
- Lyse cells in NP-40 buffer (50 mM Tris-HCl pH 7.5, 150 mM NaCl, 1% NP-40) supplemented with protease and phosphatase inhibitors.
- Pre-clear lysates with protein A/G sepharose beads for 30 minutes at 4°C.
- Incubate with anti-PD-L1 antibody (1:100) or anti-USP14 antibody (1:100) overnight at 4°C with rotation.
- Add protein A/G beads and incubate for 2 hours at 4°C.
- Wash beads 5 times with IP buffer, elute with 1.5× SDS sample buffer, and analyze by Western blotting.
Ubiquitination Assay:
- Transfect cells with PD-L1 expression vector and HA-ubiquitin.
- Treat cells with MG132 (10 μM) for 6 hours before harvesting to prevent proteasomal degradation.
- Perform IP with anti-PD-L1 antibody under denaturing conditions (1% SDS in lysis buffer).
- Detect ubiquitinated PD-L1 by Western blot using anti-HA antibody.
T Cell Co-culture Assay:
- Isolate T cells from human peripheral blood using Ficoll extraction and Dynabeads Untouched human T cell isolation kit.
- Co-culture NSCLC cells with T cells at 10:1 ratio (T cell:cancer cell) in Transwell chambers for 72 hours.
- Analyze cancer cell apoptosis by annexin V-FITC/PI staining and flow cytometry.
- Assess T cell activation markers (CD69, CD25) by flow cytometry.
Expected Outcomes: PSMD11 or USP14 knockdown should enhance PD-L1 ubiquitination and degradation, leading to increased T cell-mediated killing of NSCLC cells. Conversely, USP14 overexpression should stabilize PD-L1 and promote immune evasion.
Therapeutic Implications and Future Perspectives
The contextual behaviors of FBXW7 and USP14 present both challenges and opportunities for therapeutic development. For FBXW7-deficient cancers, strategic vulnerabilities emerge through the concept of non-oncogene addiction, where tumors become dependent on stabilized FBXW7 substrates for survival [78] [79]. Therapeutic inhibition of these accumulated oncoproteins (e.g., c-MYC, mTOR, MCL-1) represents a promising precision medicine approach. Additionally, the DYRK2-FBXW7 regulatory axis offers a novel therapeutic opportunity, where DYRK2 inhibition could stabilize FBXW7 and enhance degradation of oncogenic substrates [80]. Preclinical studies demonstrate that targeting this axis sensitizes cancer cells to conventional chemotherapeutics like doxorubicin and paclitaxel, as well as to BET inhibitors in hematological malignancies [80].
For USP14, context-specific inhibition strategies show considerable promise, particularly in immunotherapy-resistant NSCLC where USP14-mediated PD-L1 stabilization drives immune evasion [81]. The development of selective USP14 inhibitors such as IU1 provides a foundation for therapeutic combinations with immune checkpoint blockade. However, the tissue-specific functions of USP14 necessitate careful patient stratification and biomarker development to identify tumors dependent on USP14 activity while minimizing potential toxicities.
The expanding repertoire of ubiquitin-targeting therapeutic modalities, including PROTACs (proteolysis-targeting chimeras) and molecular glues, offers innovative approaches to exploit contextual ubiquitin enzyme functions [29] [6]. These technologies enable targeted degradation of oncoproteins that have eluded conventional inhibition strategies, potentially overcoming resistance mechanisms inherent in cancer cell signaling networks. Future research directions should focus on comprehensive mapping of ubiquitin enzyme contextual dependencies across cancer types, development of isoform-specific targeting strategies, and integration of ubiquitin-focused therapeutics with conventional and immunotherapeutic approaches.
FBXW7 and USP14 exemplify the sophisticated contextual regulation within the ubiquitin-proteasome system, demonstrating that ubiquitin enzymes function not as binary switches but as nuanced integrators of cellular signals. Their roles oscillate between tumor suppressive and promotional activities based on genetic background, tissue context, signaling environment, and therapeutic pressures. Understanding these contextual dependencies is paramount for developing effective therapeutic strategies that target the ubiquitin system. Future research must prioritize comprehensive contextual mapping of ubiquitin enzyme functions across cancer types and states, enabling precision targeting of these critical regulatory nodes in oncology. The continued deciphering of the ubiquitin code promises to reveal novel therapeutic vulnerabilities and advance personalized cancer medicine.
The ubiquitin-proteasome system (UPS) has emerged as a master regulator of tumor progression, therapy resistance, and antitumor immunity. This technical review delineates the molecular mechanisms by which ubiquitin code alterations—including specific chain topologies and spatiotemporal enzyme activities—orchestrate cancer cell survival following radiotherapy and enable immune evasion. We synthesize emerging preclinical and clinical evidence demonstrating that targeted disruption of ubiquitin signaling, via inhibition of E3 ligases or deubiquitinases (DUBs), can profoundly sensitize tumors to conventional radiotherapy and immune checkpoint blockade. The development of novel modalities such as proteolysis-targeting chimeras (PROTACs) and deubiquitinase-targeting chimeras (DUBTACs) provides innovative strategies to exploit ubiquitin network vulnerabilities. This review offers a comprehensive framework for integrating ubiquitin-targeting agents with established cancer therapies, detailing mechanistic insights, experimental methodologies, and translational applications to guide future drug development and combination trial design.
Ubiquitination, a pivotal post-translational modification, regulates virtually all cellular processes through a sophisticated coding system involving diverse polyubiquitin chain architectures. The ubiquitin code is written via the sequential action of E1 (activating), E2 (conjugating), and E3 (ligating) enzymes and erased by deubiquitinases (DUBs), creating a dynamic, reversible signaling network [6]. In cancer, this system undergoes extensive reprogramming, enabling tumors to develop resistance to radiotherapy and immunotherapy through multiple mechanisms: enhancing DNA damage repair fidelity, promoting metabolic reprogramming, and establishing immunosuppressive tumor microenvironments (TME) [29] [22].
Radiation resistance remains a significant clinical challenge, largely driven by tumors' ability to dynamically adapt through complex molecular networks that are critically regulated by the ubiquitin system [29]. Similarly, cancer immunotherapy, particularly immune checkpoint blockade, has revolutionized oncology but achieves durable responses only in a subset of patients, with resistance frequently mediated by UPS-dependent stabilization of immunosuppressive proteins like PD-L1 [82] [83]. Understanding how ubiquitin code alterations drive these resistance mechanisms provides the foundational rationale for developing combination therapies that target the UPS to overcome therapeutic resistance.
Molecular Mechanisms of Ubiquitin-Mediated Therapy Resistance
Ubiquitin Chain Topologies in Radiation Response
The specific architecture of polyubiquitin chains determines their functional consequences in cellular responses to radiation, creating a hierarchical regulatory system.
Table 1: Ubiquitin Chain Topologies in Radiation Response
| Chain Type | Primary Function | Role in Radioresistance | Key Regulators |
|---|---|---|---|
| K48-linked | Proteasomal degradation | Contextual duality: promotes resistance (p53 degradation) or sensitivity (SOX9 degradation) | FBXW7, TRIM21, SMURF2 |
| K63-linked | Signaling complexes, endocytosis | Enhances DNA repair fidelity, activates pro-survival pathways, suppresses ferroptosis | FBXW7, TRAF4, TRAF6, TRIM26 |
| Monoubiquitination | Histone modification, protein trafficking | Regulates chromatin dynamics, DNA damage recognition, genome stability | RNF8, RNF40, UBE2T |
| Linear (M1-linked) | NF-κB activation, inflammation | Modulates immune cell activation in TME | LUBAC complex |
K48-linked chains typically target proteins for proteasomal degradation, but their impact on radiation response demonstrates remarkable contextual duality. For instance, FBXW7-mediated K48-linked ubiquitination of p53 promotes radioresistance in colorectal cancer by inhibiting apoptosis, whereas in non-small cell lung cancer (NSCLC), FBXW7 enhances radiosensitivity by destabilizing SOX9 and alleviating p21 repression [29] [22]. This functional switch depends on tumor-specific genetic backgrounds, emphasizing the need for precision medicine approaches.
K63-linked ubiquitination serves as a critical architect of adaptive survival mechanisms beyond its structural roles. FBXW7 employs K63 chains to modify XRCC4, enhancing the accuracy of non-homologous end joining (NHEJ) repair [22]. Similarly, TRAF4 utilizes K63 modifications to activate the JNK/c-Jun pathway, driving overexpression of anti-apoptotic Bcl-xL in colorectal cancer and MCL-1 in oral cancers [29]. K63 chains also integrate metabolic and immune regulation, as demonstrated by TRIM26 stabilization of GPX4 via K63 ubiquitination to prevent ferroptosis in gliomas [29] [22].
Monoubiquitination of both histones and non-histone proteins serves as a guardian of chromatin and genome stability. UBE2T/RNF8-mediated H2AX monoubiquitylation accelerates damage detection in hepatocellular carcinoma, while RNF40-generated H2Bub1 recruits the FACT complex to relax nucleosomes, facilitating DNA repair [22]. For non-histone targets, FANCD2 monoubiquitylation specifically resolves carbon ion-induced DNA crosslinks, positioning monoubiquitylation as a key coordinator of DNA repair and genomic integrity [22].
Ubiquitin-Mediated Regulation of Tumor Immune Microenvironment
The UPS plays a multifaceted role in shaping antitumor immunity by regulating immune checkpoint expression, antigen presentation, and immune cell function.
Table 2: Ubiquitin-Mediated Regulation of Immune Checkpoints and Antigen Presentation
| Regulatory Mechanism | Key Enzymes | Effect on Immune Function | Therapeutic Implications |
|---|---|---|---|
| PD-L1 Stability | SPOP, TRIM21, ARIH1, CDK5 | Regulates PD-L1 degradation; cancer cells often exploit stabilization | Small molecule inhibitors of stabilizing enzymes |
| PD-1 Expression | USP2, USP7, FBXW7 | DUBs stabilize PD-1; E3s promote degradation | DUB inhibitors enhance T-cell function |
| Antigen Presentation | HRD1, RNF5, MARCH family | Controls MHC I/II stability and peptide loading | Enhances tumor antigen visibility to T cells |
| cGAS-STING Pathway | TRIM21, RNF5, USP14 | Suppresses or activates innate immune sensing | Overcoming immune evasion in "cold" tumors |
PD-L1 stability is precisely controlled by competing E3 ligases and DUBs. The E3 ligase SPOP promotes PD-L1 ubiquitination and degradation in colorectal cancer, but this process is often inhibited in cancers by competitive binding of proteins like ALDH2 or BCLAF1 [82]. In NSCLC, TRIM21 ubiquitinates PD-L1 and promotes its degradation, but the long non-coding RNA LINC02418 can form a ternary complex with TRIM21 and PD-L1 to enhance this degradation, suggesting potential therapeutic strategies to overcome immunotherapy resistance [82]. Additionally, CDK5 promotes TRIM21-mediated PD-L1 ubiquitination, while EGFR signaling inhibits this process through suppression of GSK3α activity [82].
Antigen presentation machinery is extensively regulated by ubiquitination. The E3 ligase HRD1 promotes transcriptional expression of MHC II genes via ubiquitin-dependent degradation of BLIMP1, a transcriptional suppressor of the MHC class II transactivator (CIITA) [84]. HRD1 also participates in ER-associated degradation (ERAD), which processes extracellular proteins for cross-presentation on MHC I—a crucial process for CD8+ T cell responses against tumors [84]. Additionally, members of the MARCH family of E3 ubiquitin ligases mediate endosomal trafficking and degradation of MHC molecules, directly influencing antigen presentation capacity [84].
The cGAS-STING pathway, which mediates DC activation in the TME, is negatively regulated by ubiquitination. RNF5 mediates ubiquitin-dependent degradation of STING, negatively regulating antiviral innate immune responses [84]. Similarly, TRIM21 utilizes K48 ubiquitination to degrade VDAC2 in nasopharyngeal carcinoma, suppressing mitochondrial DNA release and subsequent cGAS/STING-mediated immune surveillance [29] [22]. Conversely, blocking USP14 leads to accumulation of K63-modified IRF3, triggering STING-dependent type I interferon responses and synergizing with radiotherapy to overcome immune evasion [22].
Ubiquitin-Targeting Strategies for Combination Therapies
Combining Ubiquitin-Targeting Agents with Immunotherapy
Several E3 ligases and DUBs have been identified as promising targets for enhancing immunotherapy efficacy by modulating immune checkpoint expression and immune cell function.
Table 3: Ubiquitin-Targeting Agents to Enhance Immunotherapy
| Target | Mechanism of Action | Combination Strategy | Experimental Evidence |
|---|---|---|---|
| SPOP activators | Promote PD-L1 degradation | Anti-PD-1/PD-L1 antibodies | Enhances T-cell mediated tumor killing in colorectal cancer models |
| TRIM21 stabilizers | Enhance PD-L1 ubiquitination | Anti-PD-L1 therapy | Overcomes resistance in NSCLC models |
| USP2/USP7 inhibitors | Prevent PD-1 deubiquitination | Anti-PD-1 therapy | Increases T-cell activation and tumor infiltration |
| USP14 inhibitors | Stabilize K63-IRF3, activate STING | Radiotherapy + immunotherapy | Triggers type I interferon responses in "cold" tumors |
The E3 ligase SPOP represents a particularly promising target. In hepatocellular carcinoma, the transcription factor BCLAF1 inhibits SPOP-mediated PD-L1 ubiquitination by binding to SPOP, thereby enhancing PD-L1 stability and promoting immune evasion [82]. Similarly, in various cancers, CDK4 promotes phosphorylation of SPOP at Ser6, enabling it to recognize and promote K48 ubiquitination of PD-L1, leading to its proteasomal degradation [82]. Small molecule SGLT2 inhibitors like canagliflozin can disrupt the SGLT2-PD-L1 interaction, prompting SPOP to recognize PD-L1 and promote its ubiquitination and degradation, thereby enhancing T-cell antitumor activity [82].
Targeting DUBs that stabilize immune checkpoints offers another strategic approach. USP2 can deubiquitinate and stabilize PD-1, promoting tumor immune escape [6]. Inhibition of USP2 or other PD-1-stabilizing DUBs like USP7 may therefore enhance the efficacy of anti-PD-1 therapy by reducing PD-1 levels on T cells, potentially reversing T-cell exhaustion and restoring antitumor immunity [6] [83].
The integration of ubiquitin modulation with immunotherapy extends beyond checkpoint regulation. A pancancer ubiquitination regulatory network analysis revealed that the OTUB1-TRIM28 ubiquitination axis modulates the MYC pathway and influences patient prognosis and immunotherapy response [35]. Ubiquitination scores derived from this network effectively stratified patients into high-risk and low-risk groups with distinct survival outcomes across multiple cancer types, suggesting potential for biomarker-driven therapy selection [35].
Combining Ubiquitin-Targeting Agents with Radiotherapy
Ubiquitin-targeting agents can overcome key radioresistance mechanisms by modulating DNA repair, cell death pathways, and metabolic adaptation.
DNA Damage Repair Manipulation: The ubiquitin system regulates all major DNA repair pathways, with specific E3 ligases and DUBs controlling key repair proteins. RNF126 mediates K63-linked ubiquitination that activates ATR-CHK1 in triple-negative breast cancer, promoting error-prone repair and radioresistance [29]. Combined RNF126 and ATM inhibition creates synthetic lethality in these tumors. Similarly, USP7 counteracts ubiquitination of DNA-PKcs to maintain repair competence in HPV+ tumors, suggesting that targeting p16 function or its ubiquitin cascade could impair DNA repair and radiosensitize [29].
Ferroptosis Sensitization: Ubiquitination critically regulates cancer metabolism and cell death pathways, particularly ferroptosis. TRIM26 stabilizes GPX4 via K63 ubiquitination to suppress ferroptosis in glioma [29]. Similarly, OTUB1 stabilizes GPX4 to suppress ferroptosis in gastric cancer [29]. Targeting the OTUB1-GPX4 interaction or inhibiting TRIM26 creates metabolic vulnerabilities that can be exploited with radiation, as radiation-induced lipid peroxidation synergizes with ferroptosis induction.
Metabolic Reprogramming: The ubiquitin system controls metabolic adaptation in hypoxic tumors. UCHL1 stabilizes HIF-1α to activate the pentose phosphate pathway, enhancing antioxidant defense in breast cancer [29]. UCHL1 inhibition specifically sensitizes hypoxic tumors to radiation by disrupting this adaptive response. Additionally, praja2, a RING E3 ubiquitin ligase highly expressed in IDH1 wild-type glioblastoma, ubiquitylates and degrades the kinase suppressor of Ras 2 (KSR2), restraining AMP-dependent protein kinase activity and attenuating oxidative metabolism [85]. Targeting praja2 with transferrin-targeted self-assembling nanoparticles (SANPs) delivering siRNA prevented KSR2 degradation and suppressed GBM growth in vivo [85].
Advanced Ubiquitin-Targeting Modalities
PROTACs (Proteolysis-Targeting Chimeras): These bifunctional molecules recruit E3 ligases to target proteins of interest, inducing their ubiquitination and degradation. EGFR-directed PROTACs selectively degrade β-TrCP substrates in EGFR-dependent tumors (e.g., lung and head/neck squamous cell carcinomas), suppressing DNA repair while minimizing impact on normal tissues [29] [22]. Innovative radiation-responsive PROTAC platforms include radiotherapy-triggered PROTAC (RT-PROTAC) prodrugs activated by tumor-localized X-rays to degrade BRD4/2, synergizing with radiotherapy in breast cancer models [29]. Additionally, X-ray-responsive nanomicelles (e.g., diselenide-bridged RCNprotac) selectively release PROTACs within irradiated tumors, enabling spatiotemporal control of protein degradation [22].
DUBTACs (Deubiquitinase-Targeting Chimeras): These novel agents recruit DUBs to specific target proteins to remove ubiquitin chains and stabilize proteins of interest [86]. While still in early development, DUBTACs provide a promising strategy for radiosensitizer development by harnessing the UPS to stabilize tumor suppressor proteins or immune-enhancing factors that are normally degraded in cancer cells.
Experimental Protocols and Research Methodologies
Assessing Ubiquitin-Dependent Radioresistance Mechanisms
Protocol 1: DNA Repair Fidelity Assay
- Objective: Quantify the impact of ubiquitin modulation on DNA repair efficiency post-irradiation.
- Methodology:
- Transfert cells with siRNA targeting E3 ligases (e.g., RNF126, FBXW7) or DUBs (e.g., USP14, OTUB1) or treat with small-molecule inhibitors.
- Irradiate cells at 2-8 Gy using clinical-grade irradiators.
- Fix cells at timepoints (0.5, 2, 8, 24h) post-irradiation and immunostain for γH2AX (double-strand breaks), 53BP1 (NHEJ), or RAD51 (homologous recombination).
- Quantify foci formation using high-content imaging and calculate repair kinetics.
- Correlate with clonogenic survival assays to determine functional significance.
- Validation: Western blotting for target protein knockdown and ubiquitination status using chain-specific ubiquitin antibodies (K48-, K63-linked).
Protocol 2: In Vivo Radiosensitization Studies
- Objective: Evaluate the efficacy of ubiquitin-targeting agents combined with radiotherapy.
- Methodology:
- Establish syngeneic or patient-derived xenograft models in immunocompetent or immunodeficient mice.
- Randomize animals to treatment groups: vehicle, radiation alone, drug alone, combination.
- Administer ubiquitin-targeting agents (e.g., PROTACs, DUB inhibitors) via optimal route (oral, intraperitoneal, or nanoparticle-mediated delivery).
- Deliver focal radiotherapy using small animal radiation research platforms (SARRP) with image guidance (2-5 Gy/fraction, total 10-20 Gy).
- Monitor tumor growth kinetics, survival, and perform immunohistochemistry for DNA damage (γH2AX), apoptosis (cleaved caspase-3), and immune cell infiltration (CD8+, CD4+ T cells).
- Advanced Analysis: Single-cell RNA sequencing of treated tumors to identify ubiquitin-dependent resistance subpopulations and immune microenvironment changes.
Evaluating Immune Synergy Mechanisms
Protocol 3: PD-L1 Turnover and Immune Cell Function Assay
- Objective: Determine how ubiquitin modulation affects PD-L1 dynamics and T-cell mediated killing.
- Methodology:
- Treat tumor cells with E3 ligase agonists (SPOP stabilizers) or DUB inhibitors (USP7, USP2 inhibitors) with/without IFNγ to simulate TME conditions.
- Perform cycloheximide chase assays to measure PD-L1 protein half-life.
- Co-culture treated tumor cells with activated human T-cells at varying effector:target ratios.
- Measure T-cell activation (CD69, CD25 surface staining), cytokine production (IFNγ ELISA), and tumor cell killing (real-time cell analysis, caspase activation).
- Validate findings in human tumor explant cultures whenever possible.
- Mechanistic Depth: Use ubiquitin mutants (K48R, K63R) to identify chain topology requirements for PD-L1 degradation.
Protocol 4: Antigen Presentation Modulation Studies
- Objective: Assess how ubiquitin manipulation enhances tumor antigen visibility.
- Methodology:
- Modulate E3 ligases (HRD1, MARCH family) or DUBs in dendritic cells (DCs) or tumor cells.
- Pulse cells with model antigens (ovalbumin) or tumor-derived neoantigens.
- Quantify MHC-I and MHC-II antigen presentation using antigen-specific T-cell hybridomas or mass spectrometry-based immunopeptidomics.
- Evaluate DC maturation markers (CD80, CD86, CD40) and migration capacity.
- In vivo, track antigen-specific T-cell priming using MHC tetramers and functional assays.
Visualization of Key Signaling Networks
Ubiquitin Network in Therapy Resistance
Combination Therapy Synergy Mechanism
Research Reagent Solutions
Table 4: Essential Research Tools for Ubiquitin-Combination Therapy Studies
| Reagent Category | Specific Examples | Research Application | Key Considerations |
|---|---|---|---|
| E3 Ligase Modulators | SPOP stabilizers, TRIM21 inhibitors, FBXW7 activators | Validate target engagement and PD-L1 degradation | Selectivity profiling across E3 family members essential |
| DUB Inhibitors | USP7, USP2, USP14, OTUB1 inhibitors | Assess immune checkpoint stabilization and DNA repair | Chain specificity and off-target effects must be characterized |
| PROTACs | EGFR-directed, BRD4-targeting, radiation-activated | Induce targeted protein degradation with spatiotemporal control | Pharmacokinetics and tissue penetration critical for efficacy |
| siRNA/mRNA Nanoparticles | Transferrin-targeted SANPs with praja2 siRNA | In vivo target validation with tissue-specific delivery | Optimization of loading efficiency and endosomal escape |
| Ubiquitin Chain-Specific Antibodies | K48-linkage, K63-linkage, monoubiquitin antibodies | Detect specific ubiquitin topology changes in treated samples | Validation using ubiquitin mutant constructs essential |
| Radiation Research Platforms | Small animal radiation research platform (SARRP) | Preclinical studies with clinical relevant radiation dosing | Image guidance enables precise tumor targeting |
| Immune Monitoring Tools | MHC tetramers, cytokine multiplex panels, scRNA-seq | Comprehensive immune profiling in combination studies | Longitudinal sampling captures dynamic immune changes |
The strategic targeting of ubiquitin signaling networks represents a paradigm shift in overcoming resistance to cancer radiotherapy and immunotherapy. The intricate involvement of specific E3 ligases and DUBs in DNA damage response, immune checkpoint regulation, and antigen presentation provides multiple actionable nodes for therapeutic intervention. Future research directions should focus on several key areas: (1) developing more selective ubiquitin modulators with reduced off-target effects; (2) optimizing biomarker strategies to identify patients most likely to benefit from ubiquitin-directed combination therapies; (3) advancing novel delivery systems such as radiation-activated PROTACs and tumor-targeted nanoparticles for enhanced therapeutic index; and (4) elucidating tissue-specific functions of ubiquitin enzymes to minimize toxicity. As our understanding of the ubiquitin code in cancer therapy resistance deepens, rationally designed combination regimens targeting ubiquitin pathways with conventional therapies hold significant promise for improving outcomes across multiple cancer types.
Validation and Comparative Analysis of Ubiquitin-Targeting Agents in Preclinical and Clinical Settings
The ubiquitin-proteasome system (UPS) stands as a critical regulatory network governing cellular protein homeostasis, with its dysfunction being a hallmark of cancer pathogenesis [87] [18]. This system orchestrates the precise degradation of proteins involved in cell cycle progression, apoptosis, and DNA repair through a coordinated enzymatic cascade comprising ubiquitin-activating enzymes (E1), ubiquitin-conjugating enzymes (E2), ubiquitin ligases (E3), and the proteolytic 26S proteasome complex [87]. The dynamic reversal of ubiquitination is mediated by deubiquitinases (DUBs), which remove ubiquitin from substrate proteins, thereby providing an additional layer of regulatory control [88] [6]. In cancer development, malignant cells exhibit heightened dependence on UPS function to maintain rapid proliferation and eliminate tumor suppressors, creating a therapeutic vulnerability that can be exploited pharmacologically [87] [18]. This whitepaper provides a comprehensive technical evaluation of clinical-stage agents targeting key nodes within the UPS, analyzing their mechanisms, efficacy, and application in contemporary oncology drug development.
Molecular Foundations of the Ubiquitin-Proteasome System
The Ubiquitination Cascade
The ubiquitination process initiates with E1 activating enzymes, which form a thioester bond with ubiquitin in an ATP-dependent manner. The human genome encodes only two E1 enzymes (UBA1 and UBA6), creating an attractive upstream target for intervention [87] [18]. Activated ubiquitin is subsequently transferred to approximately 50 E2 conjugating enzymes, which then collaborate with over 600 E3 ligases to confer substrate specificity during ubiquitin transfer to target proteins [87] [18]. Polyubiquitin chains linked through lysine 48 (K48) primarily target substrates for proteasomal degradation, while other linkage types (e.g., K63) regulate non-proteolytic functions including signal transduction and DNA repair [22] [18].
The Proteasome Complex
The 26S proteasome constitutes the proteolytic core of the UPS, comprising a 20S core particle (CP) capped by 19S regulatory particles (RP) [87]. The 20S CP contains three catalytically active subunits (β1 caspase-like, β2 trypsin-like, and β5 chymotrypsin-like activities) responsible for protein degradation, while the 19S RP recognizes ubiquitinated substrates, removes ubiquitin chains, and unfolds proteins for translocation into the catalytic chamber [87]. Immunoproteasomes, which incorporate alternative catalytic subunits (β1i, β2i, and β5i) during interferon stimulation, demonstrate enhanced efficiency in processing oxidized proteins and generating antigenic peptides, presenting a specialized target in hematological malignancies [87].
Deubiquitinating Enzymes (DUBs)
Approximately 100 DUBs encoded in the human genome counterbalance ubiquitination by cleaving ubiquitin from modified substrates [88]. These enzymes are categorized into six families based on catalytic domain structure: ubiquitin-specific proteases (USPs), ubiquitin C-terminal hydrolases (UCHs), ovarian tumor proteases (OTUs), Machado-Joseph disease domain proteases (MJDs), JAB1/MPN/MOV34 metalloenzymes (JAMMs), and the recently identified motif-interacting with Ub-containing novel DUB family (MINDYs) [88]. DUBs regulate protein stability, recycle ubiquitin to maintain free pools, and edit ubiquitin chain topology, positioning them as critical regulators of oncogenic signaling networks [88] [6].
Comparative Analysis of Clinical-Stage UPS-Targeting Agents
Table 1: Proteasome Inhibers in Clinical Development or Use
| Agent Name | Target Specificity | Development Stage | Key Clinical Applications | Mechanistic Notes |
|---|---|---|---|---|
| Bortezomib | 20S proteasome (chymotrypsin-like activity) | FDA-approved | Multiple myeloma, mantle cell lymphoma | Reversible inhibitor; boronate compound |
| Carfilzomib | 20S proteasome (chymotrypsin-like activity) | FDA-approved | Relapsed/refractory multiple myeloma | Irreversible epoxyketone inhibitor |
| Ixazomib | 20S proteasome (chymotrypsin-like activity) | FDA-approved | Multiple myeloma | Oral bioavailable; reversible boronate |
| Oprozomib | 20S proteasome | Phase II trials | Multiple myeloma, hematologic malignancies | Oral epoxyketone; structural analog of carfilzomib |
| Delanzomib | 20S proteasome | Phase II trials | Multiple myeloma, solid tumors | Reversible boronate; intravenous and oral formulations |
Table 2: E1 Inhibitors in Clinical Development
| Agent Name | Target Specificity | Development Stage | Key Clinical Applications | Mechanistic Notes |
|---|---|---|---|---|
| MLN4924 (Pevonedistat) | NEDD8-activating enzyme (NAE) | Phase III trials | Myelodysplastic syndromes, acute myeloid leukemia | Blocks cullin neddylation, disrupting CRL E3 ligase activity |
| MLN7243 (TAK-243) | Ubiquitin-activating enzyme (UBA1) | Phase I trials | Advanced solid tumors, hematologic malignancies | Directly targets E1; induces DNA damage and endoplasmic reticulum stress |
Table 3: DUB-Targeting Compounds in Development
| Agent Name | Target Specificity | Development Stage | Key Clinical Applications | Mechanistic Notes |
|---|---|---|---|---|
| VLX1570 | USP14/UCHL5 | Phase I/II (terminated) | Multiple myeloma | Showed efficacy but trial halted due to toxicity concerns |
| KSQ-4279 | USP1 | Phase I trials | Solid tumors, BRCA-mutant cancers | Synthetic lethal approach in homologous recombination-deficient contexts |
| AZ-1 | USP25/USP28 | Preclinical | Bacterial infection (host-directed therapy), potential in cancer | Dual inhibitor identified in high-throughput screening [89] |
| G5 | Undisclosed DUBs | Preclinical | Not specified | Early-stage inhibitor [18] |
| F6 | Undisclosed DUBs | Preclinical | Not specified | Early-stage inhibitor [18] |
Experimental Approaches for Evaluating UPS-Targeting Agents
High-Throughput Screening for DUB Inhibitors
Recent advances in DUB inhibitor discovery employ sophisticated high-throughput screening (HTS) platforms to identify compounds with therapeutic potential. The following methodology exemplifies contemporary approaches:
Primary Screening Protocol:
- Cell Model Preparation: Seed macrophages (e.g., RAW 264.7 or primary human macrophages) in 96-well plates at standardized densities (e.g., 10,000 cells/well).
- Fluorescent Pathogen Infection: Infect cells with GFP-expressing bacterial strains (e.g., Salmonella Typhimurium UK-1) at a predetermined multiplicity of infection (MOI) to model intracellular survival.
- Compound Library Application: Treat infected cells with UPS-targeted compound libraries (e.g., 257 small-molecule modulators) across a concentration range (typically 1 nM-10 μM).
- Cell Staining and Viability Assessment: Counterstain with Hoechst 33342 for nuclear visualization and HCS CellMask Red for cytoplasmic demarcation to enable normalization of bacterial counts to cell number.
- High-Content Imaging and Analysis: Utilize automated microscopy systems (e.g., ImageXpress Micro Confocal) to capture multi-channel images, followed by algorithmic quantification of intracellular GFP-positive bacteria per cell.
- Hit Selection Criteria: Identify primary hits as compounds demonstrating ≥1.5 log10 reduction in bacterial burden without compromising host cell viability (assessed via nucleus count) [89].
Secondary Validation Assays:
- Axenic Culture Testing: Exclude compounds with direct antibacterial activity by assessing impact on bacterial growth in cell-free culture systems.
- Transcriptomic Profiling: Employ RNA sequencing to evaluate infection-induced DUB expression patterns (e.g., USP25, USP46, OTUD7B upregulation) and compound-mediated pathway modulation.
- Genetic Validation: Conduct siRNA-mediated knockdown of candidate DUB targets (e.g., USP25) to confirm phenotypic recapitulation of inhibitor effects [89].
Figure 1: High-Throughput Screening Workflow for UPS-Targeting Compounds. This diagram illustrates the integrated experimental pipeline for identifying and validating DUB inhibitors, from primary screening through mechanistic validation.
Functional Assessment of PROTAC Platforms
Proteolysis-Targeting Chimeras (PROTACs) represent a transformative approach to targeted protein degradation, with several platforms entering clinical evaluation:
PROTAC Mechanism and Evaluation:
- Molecular Design: Construct heterobifunctional molecules comprising a target protein-binding ligand, E3 ligase-recruiting moiety, and synthetic linker optimizing spatial orientation.
- Cellular Potency Assessment: Treat cancer cell lines with escalating PROTAC concentrations (typically 1 nM-10 μM) and measure:
- Target protein degradation via immunoblotting at 2-24 hour timepoints
- Cellular viability using ATP-based assays (e.g., CellTiter-Glo) across 72-144 hours
- Apoptosis induction through annexin V/propidium iodide flow cytometry
- Mechanistic Validation:
- Employ E3 ligase CRISPR knockout lines to confirm degradation dependency
- Utilize proteasome inhibitors (e.g., MG132) to verify proteasomal requirement
- Conduct competitive binding assays with parent ligands to establish target engagement
- Therapeutic Efficacy Models: Evaluate antitumor activity in patient-derived xenografts measuring:
The Scientist's Toolkit: Essential Research Reagents
Table 4: Key Research Reagents for UPS-Targeting Studies
| Reagent/Category | Specific Examples | Research Application | Functional Role |
|---|---|---|---|
| Proteasome Inhibitors | MG132, Bortezomib, Carfilzomib | Mechanistic studies, control compounds | Block proteolytic activity of 20S proteasome; experimental benchmarks |
| E1 Inhibitors | MLN7243 (TAK-243), PYR-41 | Upstream UPS pathway inhibition | Block ubiquitin activation; induce unfolded protein response |
| DUB Inhibitors | AZ-1 (USP25/28), VLX1570 (USP14/UCHL5) | Target validation, pathway analysis | Modulate ubiquitin chain stability; probe DUB-specific functions |
| Activity-Based Probes | Ubiquitin vinyl sulfone (UbVS), HA-UbVS | DUB activity profiling | Covalently label active site cysteine residues in multiple DUB families |
| PROTAC Molecules | ARV-110, ARV-471 | Targeted protein degradation research | Induce ligand-dependent protein degradation via E3 ligase recruitment |
| siRNA/shRNA Libraries | USP family, OTU family members | Genetic target validation | Enable RNAi-mediated knockdown to assess DUB loss-of-function phenotypes |
| Ubiquitin Chain Linkage-Specific Antibodies | K48-Ub, K63-Ub, M1-Ub | Ubiquitin signaling analysis | Detect specific polyubiquitin chain types in immunoblotting/immunofluorescence |
Signaling Pathways and Therapeutic Applications
UPS Modulation in Oncogenic Signaling
Therapeutic targeting of UPS components intersects with multiple hallmark cancer pathways, creating diverse opportunities for intervention:
RAS-RAF-MAPK Pathway Regulation: Ubiquitination dynamically controls the stability, membrane localization, and signaling transduction of RAS proteins, the most frequently mutated oncoproteins in human cancers [8]. Distinct ubiquitination patterns across RAS isoforms (KRAS4A, KRAS4B, NRAS, HRAS) create isoform-specific vulnerabilities that can be exploited therapeutically [8]. E3 ligases and DUBs that regulate RAS stability represent promising targets for overcoming RAS-driven therapeutic resistance.
NF-κB Signaling Network: Multiple UPS components critically regulate NF-κB activation, a central pathway in inflammation and cancer survival. The E3 ligase LUBAC generates linear ubiquitin chains that activate NF-κB signaling through NEMO modification, promoting lymphoma progression [6]. Conversely, USP14 destabilizes IκBα to activate NF-κB in head and neck cancers, creating a context-dependent therapeutic target [22]. DUB inhibitors such as AZ-1 suppress NF-κB signaling, representing a mechanism contributing to their anticancer effects [89].
Immune Checkpoint Regulation: The UPS extensively modulates immune checkpoint protein stability, impacting tumor immune evasion. The DUB USP2 stabilizes PD-1, promoting tumor immune escape through deubiquitination [6]. Additionally, MTSS1 promotes AIP4-mediated monoubiquitination of PD-L1 at K263, driving its internalization and lysosomal degradation, thereby inhibiting immune escape in lung adenocarcinoma [6]. These mechanisms position DUB inhibitors as potential combinatory agents with immune checkpoint blockade.
Figure 2: UPS Integration in Oncogenic Signaling Pathways. This diagram illustrates how different UPS-targeting therapeutic approaches intersect with key cancer-relevant signaling networks.
The targeted disruption of ubiquitin signaling represents a rapidly advancing frontier in oncology therapeutics, with diverse agent classes demonstrating complementary mechanisms and application landscapes. Proteasome inhibitors have established the clinical validity of UPS targeting, particularly in hematological malignancies, while E1 inhibitors offer upstream pathway disruption with emerging efficacy in myeloid neoplasms. The DUB inhibitor landscape, though less clinically mature, presents compelling opportunities for precision intervention in defined molecular contexts, particularly through synthetic lethal approaches in DNA repair-deficient cancers. Emerging technologies, especially PROTAC platforms, transcend traditional occupancy-based inhibition by enabling event-driven protein degradation, potentially addressing historically intractable targets. Future progress will require enhanced target specificity within DUB inhibitor classes, biomarker-driven patient selection strategies, and innovative combination approaches that leverage the unique mechanistic attributes of each UPS-targeting modality. As understanding of ubiquitin code complexity deepens, the strategic integration of these distinct but interrelated therapeutic classes promises to expand the scope and efficacy of molecularly-targeted cancer therapy.
The ubiquitin-proteasome system (UPS) represents a cornerstone of cellular homeostasis, and its dysregulation is fundamentally implicated in oncogenesis. This whitepaper delineates a structured framework for the preclinical validation of two prominent enzyme families within the UPS: the TRIM (Tripartite Motif) family of E3 ubiquitin ligases and Ubiquitin-Specific Proteases (USPs). Within the context of altered ubiquitin signaling in cancer, we present integrated case studies, detailed experimental methodologies, and essential resource toolkits to guide researchers in systematically assessing the therapeutic potential of these targets. The content emphasizes the critical role of TRIM proteins and USPs in maintaining protein stability, regulating key oncogenic signaling pathways, and shaping the tumor immune microenvironment, thereby establishing their viability for targeted drug discovery.
Ubiquitination is a reversible post-translational modification that governs the stability, activity, and localization of thousands of proteins. This process is orchestrated by a cascade of E1 (activating), E2 (conjugating), and E3 (ligating) enzymes, with E3 ligases conferring substrate specificity. The human genome encodes over 600 E3 ligases, among which the TRIM family constitutes a major subclass [90]. Conversely, deubiquitinating enzymes (DUBs), such as Ubiquitin-Specific Proteases (USPs), reverse this process by cleaving ubiquitin moieties, providing a dynamic and finely-tuned regulatory layer [91] [92].
Dysregulation of this "ubiquitin code" is a hallmark of cancer. Alterations in the activity of E3 ligases and DUBs can lead to the aberrant stabilization of oncoproteins or degradation of tumor suppressors, driving tumor proliferation, metastasis, and therapeutic resistance [8] [35]. This whitepaper provides a technical guide for the preclinical validation of novel targets within the TRIM and USP families, framing the discussion within the broader thesis that targeting ubiquitin code alterations offers a powerful, albeit complex, strategy for cancer therapy.
TRIM Family E3 Ligases: Biological Significance and Preclinical Validation
Biological Significance in Cancer
The TRIM family comprises over 70 members in humans, characterized by a conserved N-terminal tripartite motif (RING, B-box, and coiled-coil domains) [93]. Many TRIM proteins function as E3 ubiquitin ligases, with their RING domain facilitating the transfer of ubiquitin to target substrates. A systematic analysis revealed that nearly half of all TRIM proteins positively regulate innate immune responses, underscoring their extensive dedication to fundamental cellular defense mechanisms [94]. In cancer, their roles are multifaceted, influencing proliferation, apoptosis, and DNA damage repair.
Table 1: Oncogenic Functions of Select TRIM Proteins
| TRIM Protein | Cancer Type | Molecular Function & Substrate | Pro-Tumorigenic Effect |
|---|---|---|---|
| TRIM29 | Pancreatic Cancer | Binds & stabilizes YAP1; reduces its ubiquitination [95] | Promotes tumor growth and progression |
| TRIM28 | Pan-cancer (e.g., Lung, Esophageal) | Forms regulatory axis with OTUB1; modulates MYC pathway [35] | Drives immunotherapy resistance & poor prognosis |
| TRIM24 | Multiple Cancers | E3 ubiquitin ligase activity; regulates oncogenic signaling [93] | Highly expressed in malignant tissues |
Case Study: Preclinical Validation of TRIM29 in Pancreatic Cancer
Hypothesis: TRIM29 promotes pancreatic cancer (PC) growth by stabilizing the Yes-associated protein 1 (YAP1) oncoprotein.
Experimental Workflow & Methodologies:
Expression Analysis:
- Methodology: Quantitative RT-PCR (qRT-PCR), Western Blot, and Immunohistochemistry (IHC) on matched human PC and adjacent normal tissues.
- Key Reagents: Anti-TRIM29 antibody (e.g., Abcam ab108627), anti-YAP1 antibody (e.g., Abcam ab205270), GAPDH loading control.
- Validation Criterion: Significant upregulation of TRIM29 and YAP1 at mRNA and protein levels in PC specimens correlates with malignant phenotype and poorer overall survival [95].
Functional Assays (In Vitro):
- Methodology:
- Proliferation: CCK-8 and EdU (5-ethynyl-2'-deoxyuridine) assays post-TRIM29 knockdown (siRNA/shRNA).
- Cell Cycle & Apoptosis: Flow cytometry for Propidium Iodide (PI) and Annexin-V staining.
- Validation Criterion: TRIM29 knockdown suppresses PC cell growth, arrests cell cycle progression, and promotes apoptosis [95].
- Methodology:
Mechanistic Investigation:
- Methodology:
- Protein-Protein Interaction: Co-immunoprecipitation (Co-IP) of endogenous TRIM29 and YAP1 from PC cell lysates.
- Ubiquitination Status: In vivo ubiquitination assay. Cells are treated with MG132 (proteasome inhibitor) before harvesting; YAP1 is immunoprecipitated, and its ubiquitination level is detected with an anti-Ub antibody.
- Validation Criterion: TRIM29 directly binds YAP1. TRIM29 overexpression decreases, while its knockdown increases, the polyubiquitination level of YAP1, confirming its role in stabilizing the YAP1 protein [95].
- Methodology:
Functional Rescue & In Vivo Validation:
- Methodology: Subcutaneous xenograft models in nude mice. PC cells with stable TRIM29 knockdown, with or without concurrent YAP1 overexpression, are injected.
- Key Reagents: TRIM29 shRNA lentivirus, YAP1 overexpression plasmid.
- Validation Criterion: Tumors with TRIM29 knockdown show reduced growth. Re-introduction of YAP1 restores tumor growth, confirming that TRIM29's oncogenic effect is YAP1-dependent [95].
Diagram 1: TRIM29-YAP1 Oncogenic Signaling
Ubiquitin-Specific Proteases (USPs): Biological Significance and Preclinical Validation
Biological Significance in Cancer
USPs represent the largest DUB family, characterized by significant structural diversity and a conserved catalytic core domain. They are critical regulators of immune cell function, DNA damage response, and the stability of key oncoproteins and tumor suppressors [92] [96]. Recent studies reveal a surprising variety in the catalytic mechanisms of different USPs, which may create opportunities for selective therapeutic targeting [97].
Table 2: Oncogenic Functions and Mechanisms of Select USPs
| USP | Cancer Relevance | Molecular Function & Substrate | Pathway & Effect |
|---|---|---|---|
| USP7 | Multiple Cancers, Immuno-oncology | Deubiquitinates and stabilizes Foxp3 in Tregs, Tip60 [92] | Modulates immunosuppressive TME; promotes cancer immune evasion |
| USP3 | Glioblastoma, Gastric Cancer | Deubiquitinates and stabilizes Claspin [96] | Enhances ATR-Chk1 signaling; confers radiation resistance |
| USP1 | e.g., Non-small Cell Lung Cancer | Stabilizes oncogenic proteins upon complexing with UAF1 [91] | Promotes DNA damage repair; confers chemotherapy resistance |
Case Study: Prevalidation of USP7 in Cancer Immunotherapy
Hypothesis: USP7 inhibition can reprogram the tumor immune microenvironment by targeting regulatory T cells (Tregs), thereby enhancing anti-tumor immunity.
Experimental Workflow & Methodologies:
Expression and Genetic Dependency:
- Methodology: Analysis of public transcriptomic datasets (e.g., TCGA) and in vitro CRISPR/Cas9 screening in immune cell co-culture systems.
- Validation Criterion: High USP7 expression correlates with Treg signatures; genetic knockout impairs Treg suppressive function and enhances cytotoxic T-cell activity [92].
Biochemical & Mechanistic Studies:
- Methodology:
- Catalytic Activity Assay: Fluorescence-based DUB assay using Ub-AMC or Ub-rhodamine substrates to test USP7 inhibitor potency.
- Substrate Validation: Co-IP and Western blot to assess Foxp3 and Tip60 protein stability in USP7-inhibited Tregs.
- Key Reagents: Recombinant USP7 catalytic domain, active-site directed inhibitors (e.g., HBX 41,108), anti-Foxp3 antibody.
- Validation Criterion: Pharmacologic inhibition of USP7 reduces Foxp3 protein levels and disrupts Foxp3 dimerization, leading to decreased expression of Treg functional markers like CTLA-4 [92].
- Methodology:
In Vitro Functional Immune Assays:
- Methodology: Teff suppression assay. CFSE-labeled effector T cells (Teffs) are co-cultured with Tregs (pre-treated with USP7 inhibitor). Teff proliferation is measured by flow cytometry.
- Validation Criterion: USP7-inhibited Tregs show a reduced capacity to suppress Teff proliferation, indicating a loss of immunosuppressive function [92].
In Vivo Efficacy & Combination Studies:
- Methodology: Syngeneic mouse tumor models. Mice are treated with a USP7 inhibitor alone or in combination with anti-PD-1 antibody.
- Key Reagents: USP7 small-molecule inhibitor, anti-PD-1 antibody.
- Validation Criterion: USP7 inhibitor monotherapy shows anti-tumor activity. Combination with anti-PD-1 demonstrates synergistic tumor growth inhibition, correlated with increased tumor-infiltrating cytotoxic T cells and reduced Treg suppression in the TME [92].
Diagram 2: USP7 Targeting in Immuno-oncology
The Scientist's Toolkit: Essential Research Reagents and Assays
Successful preclinical validation relies on a suite of well-characterized reagents and robust assays. The table below details key solutions for targeting TRIMs and USPs.
Table 3: Research Reagent Solutions for Preclinical Validation
| Reagent / Assay | Function & Utility | Example Application |
|---|---|---|
| siRNA/shRNA Lentivirus | Stable gene knockdown for in vitro and in vivo functional studies. | Validating the essential role of TRIM29 in pancreatic cancer growth [95]. |
| Co-IP Kit | Validates direct protein-protein interactions in a native cellular context. | Confirming the physical interaction between TRIM29 and YAP1 [95]. |
| In Vivo Ubiquitination Assay | Determines the effect of an E3 ligase or DUB on substrate ubiquitination status. | Measuring changes in YAP1 ubiquitination upon TRIM29 modulation [95]. |
| Active Recombinant USP Protein | Provides a validated enzymatic target for high-throughput screening (HTS) of inhibitors. | Screening compound libraries for USP7 catalytic inhibitors [97] [92]. |
| Fluorogenic DUB Substrate (Ub-AMC) | Measures DUB catalytic activity in real-time for inhibitor characterization. | Determining IC₅₀ values of novel USP7 inhibitors in biochemical assays [92]. |
| Syngeneic Mouse Model | Evaluates drug efficacy and immune modulation within an intact immune system. | Testing the effect of USP7 inhibition on Treg function and anti-tumor immunity [92]. |
The systematic preclinical validation of TRIM family ligases and USP deubiquitinases is a critical gateway to targeting the ubiquitin code in cancer. As demonstrated in the case studies, a multi-faceted approach encompassing expression analysis, genetic and pharmacologic perturbation, detailed mechanistic studies, and robust in vivo modeling is essential to establish a target's biological function and therapeutic rationale. The expanding toolkit of reagents and assays, combined with a deeper understanding of the unique catalytic mechanisms within these families [97], continues to accelerate the discovery of novel targets. The integration of these strategies will undoubtedly yield the next generation of therapeutics, particularly when combined with modalities like immunotherapy, to overcome the pervasive challenge of cancer drug resistance.
Radiotherapy remains a cornerstone for solid tumor treatment, yet its efficacy is frequently compromised by radioresistance. The ubiquitin system, comprising E3 ubiquitin ligases and deubiquitinases (DUBs), has emerged as a master regulator of radiation response, orchestrating DNA repair fidelity, metabolic reprogramming, and immune evasion. This whitepaper delineates the mechanistic roles of specific E3 ligases and DUBs in driving radioresistance and synthesizes the experimental and therapeutic strategies for targeting these enzymes to achieve radiosensitization. We provide a comprehensive analysis of the ubiquitin code's context-dependent functions, detailed protocols for validating key targets, and visualization of critical signaling pathways. Furthermore, we explore emerging therapeutic modalities, including proteolysis-targeting chimeras (PROTACs) and deubiquitinase-targeting chimeras (DUBTACs), which leverage the ubiquitin-proteasome system for targeted protein degradation. Integrating these targeted agents with radiotherapy presents a promising paradigm for precision oncotherapy, aiming to overcome resistance and improve patient survival.
Radiotherapy induces cancer cell death primarily through direct DNA damage and indirect immune activation [29] [22]. However, tumors exhibit a remarkable capacity to develop resistance through dynamic molecular adaptations, often mediated by post-translational modifications. Among these, ubiquitination—the covalent attachment of ubiquitin to target proteins—stands out as a critical regulator of radioresistance [98]. The ubiquitin system's complexity arises from its diverse chain topologies, including K48-linked chains that target proteins for proteasomal degradation and K63-linked chains that facilitate non-proteolytic signaling complexes [29] [22]. This "ubiquitin code" is dynamically written by E3 ligases and erased by DUBs, creating a reversible regulatory network that tumors exploit to survive radiation stress [99] [6]. Understanding and targeting this network offers unprecedented opportunities for radiosensitization within the broader context of ubiquitin code alterations in cancer development.
Mechanistic Insights: E3 Ligases and DUBs as Orchestrators of Radiosensitivity
Regulation of DNA Damage Repair Pathways
The cellular response to radiation-induced DNA damage is heavily governed by ubiquitin signaling. E3 ligases and DUBs regulate key proteins in DNA repair pathways, such as non-homologous end joining (NHEJ) and homologous recombination (HR).
- FBXW7: This E3 ligase enhances NHEJ accuracy via K63-linked ubiquitination of XRCC4, promoting error-free repair and radioresistance [29] [22]. Conversely, in non-small cell lung cancer (NSCLC), it can promote radiosensitivity by destabilizing SOX9 and alleviating p21 repression [29].
- RNF126: In triple-negative breast cancer (TNBC), RNF126 mediates K27/K29-linked polyubiquitination of MRE11, activating the ATR-CHK1 axis and promoting error-prone repair, contributing to radioresistance [22].
- USP14: This DUB disrupts NHEJ and promotes HR, and its inhibition sensitizes NSCLC cells to radiation by destabilizing the DNA damage response [29].
- USP7: It counteracts ubiquitination of DNA-PKcs, maintaining its repair competence, particularly in HPV+ tumors [29].
Control of Metabolic Reprogramming and Hypoxia Adaptation
Tumor metabolism and adaptation to hypoxia are critical determinants of radiation response. Ubiquitin enzymes directly regulate metabolic pathways and the hypoxia-inducible factor (HIF) system.
- TRIM26 and OTUB1: Both stabilize GPX4 via K63-linked ubiquitination (TRIM26) or direct interaction (OTUB1), suppressing radiation-induced ferroptosis, a form of iron-dependent cell death, in gliomas and gastric cancers [29].
- UCHL1: In breast cancer, this DUB stabilizes HIF-1α, activating the pentose phosphate pathway and enhancing antioxidant defense, thereby promoting radioresistance in hypoxic tumors [29].
- SMURF2: This E3 ligase targets HIF1α for degradation, compromising hypoxic survival and potentially sensitizing tumors to radiation [22].
Modulation of Tumor Immunity
Radiotherapy can stimulate anti-tumor immunity, but ubiquitin enzymes often help tumors evade this response.
- TRIM21: In nasopharyngeal carcinoma, TRIM21 mediates K48-linked degradation of VDAC2, inhibiting mitochondrial DNA release and subsequent cGAS/STING pathway activation. This suppresses type I interferon responses and promotes an immunosuppressive microenvironment [29] [22].
- USP14: Inhibition of USP14 leads to accumulation of K63-ubiquitinated IRF3, triggering STING-dependent antitumor immunity and synergizing with radiotherapy [22].
Table 1: Key E3 Ligases in Radioresistance and Targeted Intervention
| E3 Ligase | Tumor Type | Function in Radioresistance | Therapeutic Vulnerability |
|---|---|---|---|
| FBXW7 | Colorectal Cancer | Degrades p53, inhibiting apoptosis | MDM2/FBXW7 co-inhibition [29] |
| FBXW7 | NSCLC | Degrades SOX9, relieves p21 repression | Targeting SOX9 [29] |
| TRIM21 | Nasopharyngeal Carcinoma | Degrades VDAC2, inhibits cGAS-STING | Combine with immunotherapy [29] |
| RNF126 | TNBC | Activates ATR-CHK1 via MRE11 ubiquitination | RNF126 + ATM inhibition [29] |
| β-TrCP | Lung Cancer | Degrades radioprotective LZTS3 | EGFR-directed PROTACs [29] |
Table 2: Key Deubiquitinases (DUBs) in Radioresistance and Targeted Intervention
| DUB | Tumor Type | Function in Radioresistance | Therapeutic Vulnerability |
|---|---|---|---|
| USP14 | Glioma | Stabilizes ALKBH5 to maintain stemness | USP14 inhibitors [29] |
| USP14 | HNSCC | Degrades IκBα, activates NF-κB | Catalytic inhibition [29] [22] |
| USP7 | HPV+ Tumors | Stabilizes DNA-PKcs, maintains repair | Targeting p16 or its ubiquitin cascade [29] |
| OTUB1 | Lung Cancer | Stabilizes CHK1, enhances repair fidelity | Inhibiting OTUB1 to destabilize CHK1 [29] |
| UCHL1 | Breast Cancer | Stabilizes HIF-1α, enhances antioxidant defense | UCHL1 inhibition in hypoxic tumors [29] |
Experimental Validation: Methodologies for Target Identification and Functional Analysis
CRISPR-Based Functional Genomic Screens
Purpose: To identify novel E3 ligases and DUBs whose loss of function confers radiosensitization. Protocol:
- Library Transduction: Infect a representative panel of cancer cells (e.g., glioblastoma, NSCLC) with a genome-wide CRISPR knockout library targeting all E3 ligases and DUBs.
- Radiation Selection: Subject the transduced cells to fractionated radiation (e.g., 2 Gy daily for 5 days) while maintaining an unirradiated control arm.
- Genomic DNA Extraction and Sequencing: Isolate genomic DNA from surviving cells after radiation and the control arm at multiple time points. Amplify the integrated gRNA sequences by PCR and perform deep sequencing.
- Bioinformatic Analysis: Compare gRNA abundance between irradiated and control samples. E3 ligases/DUBs whose targeting gRNAs are significantly depleted in the irradiated sample represent candidate radiosensitizing targets. As demonstrated in studies, this approach has identified targets like TRIM21 [29] [22].
Profiling Ubiquitin Chain Dynamics Post-Irradiation
Purpose: To characterize the spatiotemporal dynamics of specific ubiquitin chain linkages (e.g., K48, K63) in response to ionizing radiation. Protocol:
- Cell Treatment and Lysis: Expose cancer cells to a clinically relevant radiation dose (e.g., 4-8 Gy). Harvest cells at various time points (e.g., 0.5, 2, 6, 24 hours) post-irradiation using a denaturing lysis buffer to preserve ubiquitination states.
- Ubiquitin Chain Enrichment: Utilize linkage-specific ubiquitin antibodies (e.g., anti-K48-Ub, anti-K63-Ub) for immunoprecipitation of ubiquitinated proteins from the whole-cell lysates.
- Mass Spectrometric Analysis: Digest the enriched proteins with trypsin and analyze the peptides by liquid chromatography-tandem mass spectrometry (LC-MS/MS).
- Data Integration: Identify proteins showing radiation-induced changes in specific ubiquitin linkages and integrate this data with functional genomic screens to prioritize targets regulating key processes like DNA repair (e.g., K63 on XRCC4) or metabolism (e.g., K63 on GPX4) [29] [22].
In Vitro Radiosensitization Assays
Purpose: To validate the functional role of a specific E3 ligase or DUB and evaluate the efficacy of targeted inhibitors. Protocol:
- Genetic and Pharmacological Modulation:
- Knockdown/Knockout: Use siRNA or CRISPR/Cas9 to deplete the target gene in cancer cell lines.
- Pharmacological Inhibition: Treat cells with a specific small-molecule inhibitor (e.g., USP14 inhibitor).
- Clonogenic Survival Assay: Seed cells at low density and treat with a range of radiation doses (e.g., 0, 2, 4, 6, 8 Gy). Allow colonies to form for 1-2 weeks, then fix, stain, and count colonies (>50 cells). Plot the survival fraction against radiation dose.
- Analysis of Mechanism:
Diagram 1: Ubiquitin network regulates radiation response. The diagram illustrates how radiation stress modulates E3 ligase and DUB activities, leading to K48- and K63-linked ubiquitination that drives radioresistance. Targeted inhibition of these enzymes can reverse these processes and induce radiosensitization.
Signaling Pathway Visualization and Logical Relationships
Diagram 2: Key ubiquitin pathways in radioresistance. This diagram maps specific E3 ligases and DUBs to their ubiquitin linkage types and downstream biological processes, highlighting their roles in promoting radiation resistance.
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Research Reagents for Ubiquitin and Radiosensitivity Studies
| Reagent/Category | Specific Example(s) | Function/Application in Research |
|---|---|---|
| CRISPR Knockout Libraries | Whole-genome or ubiquitin-family-focused libraries (e.g., Brunello) | Genome-wide or targeted loss-of-function screens to identify novel E3 ligase/DUB targets whose knockout induces radiosensitization [29]. |
| Linkage-Specific Ub Antibodies | Anti-K48-Ubiquitin, Anti-K63-Ubiquitin | Immunoprecipitation and western blot to detect and enrich for specific ubiquitin chain types and study their dynamics post-irradiation [99] [6]. |
| Small-Molecule Inhibitors | USP14 inhibitors, OTUB1 inhibitors | Pharmacological validation of target function in vitro and in vivo. Used to assess radiosensitization potential in clonogenic assays and animal models [29] [86]. |
| PROTACs | EGFR-directed PROTACs, RT-PROTAC (targeting BRD4/2) | Induce targeted degradation of oncoproteins or specific E3 ligases (e.g., β-TrCP substrates). Radiation-activated prodrugs allow for spatiotemporal control [29] [22]. |
| DUBTACs | Novel deubiquitinase-targeting chimeras | Stabilize specific tumor suppressor proteins by recruiting them to DUBs, thereby reversing their degradation and potentially sensitizing cells to radiation [86]. |
Therapeutic Translation and Emerging Platforms
Targeting the ubiquitin network for radiosensitization has moved from concept to clinical reality with several promising platforms.
Proteolysis-Targeting Chimeras (PROTACs): These bifunctional molecules recruit a target protein to an E3 ligase for ubiquitination and degradation. Their application in radio-sensitization is exemplified by EGFR-directed PROTACs that selectively degrade β-TrCP substrates in EGFR-dependent tumors, suppressing DNA repair capacity [29]. Innovative radiation-responsive PROTAC platforms, such as radiotherapy-triggered PROTAC (RT-PROTAC) prodrugs activated by tumor-localized X-rays, are being developed to degrade targets like BRD4/2, showing synergy with radiotherapy in breast cancer models [29] [22].
Deubiquitinase-Targeting Chimeras (DUBTACs): A complementary approach, DUBTACs are designed to stabilize specific proteins by recruiting them to a deubiquitinase, thereby removing ubiquitin chains and preventing degradation. This strategy holds promise for stabilizing tumor suppressors that are aberrantly degraded in radioresistant cancers [86].
Biomarker-Guided Strategies: The success of ubiquitin-targeting therapies is highly context-dependent. For instance, the radio-sensitizing effect of FBXW7 manipulation depends on p53 and SOX9 status [29] [22]. Therefore, patient stratification using biomarkers like p53 mutation status, SOX9 overexpression, or GPX4-K63 ubiquitination levels is critical for the effective clinical translation of these targeted agents [29].
The intricate network of E3 ligases and DUBs constitutes a pivotal regulatory layer controlling the cellular response to radiation. Through precise mechanisms involving DNA repair, metabolic adaptation, and immune modulation, these enzymes validate their roles as critical regulators of radiosensitivity. The experimental frameworks and therapeutic modalities outlined herein provide a roadmap for advancing ubiquitin network targeting from a research concept to a clinical strategy. The future of precision radio-oncology lies in leveraging the complexity of the ubiquitin code, using biomarker-guided combinations of radiotherapy with PROTACs, DUBTACs, and specific inhibitors to overcome resistance and achieve durable tumor control.
Proteolysis-Targeting Chimeras (PROTACs) represent a paradigm shift in targeted cancer therapy, catalytically degrading disease-causing proteins rather than merely inhibiting their activity. This whitepaper provides a comparative analysis of two pioneering PROTACs, ARV-110 and ARV-471, within the broader context of ubiquitin code alterations in cancer development. We examine their molecular design, clinical efficacy, and mechanisms of action, highlighting how these heterobifunctional molecules exploit the ubiquitin-proteasome system to achieve targeted protein degradation. The discussion encompasses detailed experimental protocols for assessing degradation efficacy, ternary complex formation, and anti-tumor activity, providing researchers with methodological frameworks for PROTAC characterization. Furthermore, we visualize critical signaling pathways and analyze the implications of clinical trial results for future drug development. This technical guide serves as a comprehensive resource for scientists and drug development professionals advancing targeted protein degradation therapeutics.
The ubiquitin-proteasome system (UPS) represents a crucial regulatory pathway for maintaining cellular proteostasis, with its dysregulation increasingly recognized as a hallmark of cancer pathogenesis. PROteolysis TArgeting Chimeras (PROTACs) are heterobifunctional molecules designed to exploit this system for therapeutic purposes [100] [101]. These compounds consist of three fundamental components: a ligand that binds to a protein of interest (POI), a ligand that recruits an E3 ubiquitin ligase, and a linker connecting these two moieties [102] [103]. The mechanistic action involves the formation of a ternary complex (POI-PROTAC-E3 ligase), which facilitates the transfer of ubiquitin chains to the target protein, marking it for degradation by the 26S proteasome [100] [104].
The concept of the "ubiquitin code" refers to the complex language of ubiquitin modifications that determine diverse cellular outcomes for modified proteins [8] [104]. In cancer development, alterations to this code can profoundly impact protein stability, localization, and function of critical regulators. PROTACs effectively rewrite this pathological ubiquitin code by redirecting E3 ligases to neo-substrates, thereby inducing their degradation [8]. This catalytic, event-driven mechanism enables sustained target suppression with reduced drug exposure compared to traditional inhibition approaches [101].
The clinical translation of PROTAC technology has gained substantial momentum, with over 40 PROTAC drug candidates currently in various stages of clinical development [44]. Among these, ARV-110 (targeting androgen receptor for prostate cancer) and ARV-471 (targeting estrogen receptor for breast cancer) represent the most advanced candidates, providing the first clinical proof-of-concept for this modality [105] [103]. Their progression to late-stage trials marks a critical milestone in targeted protein degradation therapeutics.
Comparative Analysis of ARV-110 and ARV-471
Molecular Design and Target Profiles
ARV-110 and ARV-471 share a common PROTAC architecture but diverge significantly in their target binding moieties, reflecting their distinct therapeutic indications.
ARV-110 utilizes an androgen receptor (AR) targeting ligand linked to a cereblon (CRBN) E3 ligase recruiter [103]. It is designed for treating metastatic castration-resistant prostate cancer (mCRPC) by degrading the AR, a primary driver of disease progression in this malignancy [105].
ARV-471 incorporates an estrogen receptor (ER) targeting ligand connected to the same CRBN E3 ligase ligand [103]. It is developed for ER-positive/HER2-negative breast cancer, aiming to degrade the estrogen receptor that fuels tumor growth [105].
Both PROTACs employ CRBN as their E3 ligase, leveraging the well-characterized molecular glue properties of immunomodulatory imide drugs (IMiDs) that redirect this ligase toward non-physiological substrates [104]. The linker compositions for both molecules have been optimized to facilitate productive ternary complex formation, though their exact chemical structures remain proprietary.
Table 1: Fundamental Characteristics of ARV-110 and ARV-471
| Parameter | ARV-110 | ARV-471 |
|---|---|---|
| Target Protein | Androgen Receptor (AR) | Estrogen Receptor (ER) |
| E3 Ligase | Cereblon (CRBN) | Cereblon (CRBN) |
| Indication | mCRPC | ER+/HER2- Breast Cancer |
| Administration | Oral, once-daily | Oral, once-daily |
| Developer | Arvinas | Arvinas/Pfizer |
| Highest Phase | Phase II | Phase III |
Clinical Efficacy and Degradation Profiles
Clinical data for both PROTACs demonstrate compelling proof-of-mechanism and preliminary efficacy, even in heavily pretreated patient populations.
ARV-110 has shown particular promise in molecularly defined subgroups. In patients with tumors harboring AR T878X or H875Y mutations, ARV-110 achieved a PSA50 (prostate-specific antigen reduction ≥50%) rate of 40-46% [105] [103]. One patient with a T878X mutation achieved a confirmed partial response with 80% tumor reduction [105]. In the broader patient population with wild-type AR, the PSA50 rate was 13% (2 of 15 patients), still notable given the advanced disease state and multiple prior therapies [105].
ARV-471 has demonstrated robust ER degradation and clinical activity in a patient population where 100% had prior CDK4/6 inhibitor treatment and 71% had received fulvestrant [105]. In paired tumor biopsies, ARV-471 achieved ER degradation up to 90%, with an average degradation of 62% at doses up to 120 mg [105]. This degradation efficiency significantly exceeds the 40-50% degradation rate typically observed with fulvestrant, the standard ER degrader [103]. Clinically, among evaluable patients, ARV-471 demonstrated a clinical benefit rate (CBR) of 42%, including one confirmed partial response with 51% reduction in target lesion size [105].
Table 2: Clinical Efficacy and Degradation Profiles from Early Trials
| Efficacy Parameter | ARV-110 | ARV-471 |
|---|---|---|
| Patient Prior Therapies (Median) | 5 prior lines [105] | 5 prior therapies [105] |
| Target Degradation | AR degradation confirmed [105] | Up to 90% ER degradation (avg. 62%) [105] |
| Biomarker Response | PSA50: 40% in T878X/H875Y mutants [105] | Not applicable |
| Objective Response | Confirmed PR in T878X mutant [105] | Confirmed PR (51% reduction) [105] |
| Clinical Benefit Rate | Not reported | 42% (5 of 12 patients) [105] |
Safety and Tolerability
ARV-110: The phase 1/2 trial established a favorable safety profile with no maximum tolerated dose identified in the initial escalation phase [105]. A dose of 420 mg daily was selected for phase 2 expansion based on pharmacokinetics, safety profile, and activity signals [105].
ARV-471: Similarly well-tolerated with no dose-limiting toxicities observed at once-daily oral doses up to 700 mg [103]. The most common treatment-related adverse events were Grade 1-2 nausea (24%), arthralgia (19%), fatigue (19%), and decreased appetite (14%), with none leading to treatment discontinuation or dose reduction [105].
The manageable safety profiles of both agents have enabled the initiation of combination therapy trials, including ARV-471 with palbociclib (CDK4/6 inhibitor) [105].
Experimental Protocols for PROTAC Characterization
Assessment of Target Degradation Efficiency
Objective: To quantify the efficiency and kinetics of target protein degradation following PROTAC treatment.
Methodology:
- Cell Culture and Treatment: Culture appropriate cell lines (e.g., prostate cancer lines for ARV-110, breast cancer lines for ARV-471) under standard conditions. Treat with serial dilutions of PROTAC (typically ranging from 1 nM to 10 µM) for predetermined time points (e.g., 4, 8, 24 hours) [100].
- Protein Extraction and Quantification: Lyse cells and quantify total protein concentration. Ensure equal loading across samples.
- Western Blot Analysis: Separate proteins by SDS-PAGE, transfer to membranes, and probe with target-specific antibodies (anti-AR for ARV-110, anti-ER for ARV-471) and loading control antibodies (e.g., GAPDH, β-actin) [100].
- Quantification and DC50 Calculation: Visualize bands using chemiluminescence and quantify band intensity using image analysis software. Plot concentration-response curves and calculate DC50 (degradation concentration 50) - the concentration that degrades 50% of the target protein [100].
Key Considerations:
- Include controls for PROTAC specificity (e.g., E3 ligase competition, proteasome inhibition with MG132) [104].
- Assess degradation kinetics through time-course experiments.
- Employ complementary methods such as immunofluorescence or cellular thermal shift assays to confirm target engagement [100].
Ternary Complex Formation and Cooperativity
Objective: To evaluate the formation and stability of the POI-PROTAC-E3 ligase ternary complex.
Methodology:
- Surface Plasmon Resonance (SPR): Immobilize the target protein or E3 ligase on a sensor chip. Measure binding kinetics by flowing the PROTAC alone, then assess ternary complex formation by introducing the third component [100].
- AlphaScreen/AlphaLISA: Use bead-based proximity assays where donor and acceptor beads are conjugated to antibodies against the target protein and E3 ligase, respectively. PROTAC-induced ternary complex formation brings beads into proximity, generating a luminescent signal [100].
- Biolayer Interferometry (BLI): Similar principle to SPR, using fiber-optic biosensors to measure binding kinetics and affinities [100].
Data Analysis:
- Calculate the cooperativity factor (α) defined as α = (KdbinaryPOI × KdbinaryE3) / (KdternaryPOI × KdternaryE3) [100].
- Interpret results: α > 1 indicates positive cooperativity (ternary complex more stable than binary complexes); α < 1 indicates negative cooperativity [100].
In Vivo Anti-tumor Efficacy
Objective: To evaluate the anti-tumor activity of PROTACs in animal models.
Methodology:
- Xenograft Models: Implant cancer cells expressing the target protein (e.g., AR-positive prostate cancer cells for ARV-110, ER-positive breast cancer cells for ARV-471) into immunocompromised mice [105].
- Dosing Regimen: Once tumors reach a predetermined volume (e.g., 150-200 mm³), randomize animals into treatment groups including vehicle control, PROTAC at various doses, and relevant standard-of-care controls (e.g., enzalutamide for ARV-110, fulvestrant for ARV-471) [105].
- Endpoint Measurements:
- Monitor tumor volume and body weight regularly (2-3 times weekly).
- Assess target degradation in harvested tumor tissues via Western blot or immunohistochemistry.
- Evaluate biomarker modulation (e.g., PSA levels for ARV-110, ER-dependent gene expression for ARV-471) [105].
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Research Reagents for PROTAC Development and Characterization
| Reagent/Category | Specific Examples | Function and Application |
|---|---|---|
| E3 Ligase Ligands | Thalidomide, Lenalidomide, Pomalidomide derivatives [102] | Recruit CRBN E3 ligase; fundamental components for PROTAC design. |
| Target Protein Ligands | AR antagonists (e.g., Enzalutamide derivatives), ER antagonists (e.g., Fulvestrant derivatives) [100] | Bind protein of interest; determine target specificity of PROTAC. |
| Linker Chemistries | PEG-based linkers, alkyl chains [100] [102] | Connect warhead to E3 ligand; optimize length and composition for ternary complex formation. |
| Ubiquitin-Proteasome Inhibitors | MG132, Bortezomib [104] | Validate ubiquitin-proteasome system dependence of degradation. |
| Ternary Complex Assays | AlphaScreen, Surface Plasmon Resonance, Biolayer Interferometry [100] | Measure cooperative interactions and binding kinetics between PROTAC, POI, and E3 ligase. |
| PROTAC Databases | Publicly available PROTAC databases [100] | Access structural and activity data for PROTAC design inspiration. |
Signaling Pathways and Experimental Workflows
PROTAC Mechanism of Action and Ternary Complex Formation
Experimental Workflow for PROTAC Characterization
Discussion: Clinical Implications and Future Directions
The clinical progression of ARV-110 and ARV-471 validates PROTAC technology as a viable therapeutic approach with distinct advantages over traditional small molecule inhibitors. Their ability to achieve catalytic degradation rather than sustained inhibition enables more durable pharmacodynamic responses with potentially lower systemic exposure [101]. Furthermore, their effectiveness in degrading clinically relevant mutant proteins (e.g., AR T878X in prostate cancer) demonstrates potential for overcoming resistance mutations that often limit targeted therapies [105] [103].
The differential activity of these agents in molecularly defined populations underscores the importance of patient stratification strategies in PROTAC development. For ARV-110, the enhanced efficacy in patients with AR T878X/H875Y mutations suggests a precision medicine approach may optimize therapeutic outcomes [105]. Similarly, ARV-471's robust degradation and clinical benefit in patients previously treated with fulvestrant highlights its potential to address resistance to current endocrine therapies [105].
Recent phase III results for ARV-471 (vepdegestrant) from the VERITAC-2 trial demonstrate a statistically significant improvement in progression-free survival compared to fulvestrant in patients with ESR1 mutations, though it did not reach significance in the overall intent-to-treat population [44]. This mixed outcome highlights both the promise and challenges of PROTAC therapeutics, emphasizing the need for continued optimization of patient selection criteria and combination strategies.
Future directions for PROTAC development include expanding the E3 ligase toolbox beyond CRBN and VHL to enhance tissue specificity and reduce potential resistance [100] [104]. Additionally, engineering controlled-degradation systems such as light-inducible PROTACs or phosphoPROTACs may enable spatiotemporal control over protein degradation [102]. Combination strategies with established targeted therapies also represent a promising avenue, as evidenced by the ongoing trials of ARV-471 with CDK4/6 inhibitors [105] [44].
ARV-110 and ARV-471 represent pioneering assets in the PROTAC landscape, providing compelling clinical validation for targeted protein degradation. Their distinct molecular designs against nuclear hormone receptors demonstrate the versatility of the PROTAC platform, while their clinical profiles highlight both the promises and challenges of this novel therapeutic modality. The continued development of these agents, alongside a growing pipeline of degraders targeting diverse proteins, positions PROTAC technology as a transformative approach in cancer therapeutics. As our understanding of the ubiquitin code in cancer deepens, these molecules offer powerful tools not only for treatment but also for probing biological pathways and resistance mechanisms, ultimately advancing the field of precision oncology.
The ubiquitin-proteasome system (UPS) has emerged as a pivotal therapeutic frontier in oncology, offering two distinct intervention paradigms: targeted protein degradation (TPD) and functional inhibition. This whitepaper provides a technical benchmark of these strategies, framing them within the broader context of ubiquitin code alterations in cancer. Through critical analysis of quantitative data, experimental protocols, and emerging technologies, we delineate the relative advantages, limitations, and appropriate applications of degradation versus inhibition for manipulating the ubiquitin network in therapeutic development.
The ubiquitin system constitutes a sophisticated post-translational regulatory network that controls virtually every cellular process through the covalent attachment of ubiquitin molecules to substrate proteins. This enzymatic cascade, involving E1 activating, E2 conjugating, and E3 ligase enzymes, creates a complex "ubiquitin code" that determines protein fate—not only directing substrates to proteasomal degradation via K48-linked chains but also regulating non-proteolytic functions including signal transduction, DNA repair, and metabolic reprogramming through alternative linkages such as K63 [16] [106]. In cancer development, this ubiquitin code undergoes profound alterations, driving tumor proliferation, metastasis, therapeutic resistance, and immune evasion [8] [16]. The ubiquitin system's dynamic reversibility, chain topology diversity, and central role in oncogenic pathways present unique clinical opportunities for therapeutic intervention [16].
Two principal strategies have emerged for therapeutically targeting the ubiquitin system: (1) Targeted Protein Degradation (TPD), which harnesses the endogenous ubiquitin machinery to eliminate disease-causing proteins, and (2) Functional Inhibition, which blocks the activity of specific ubiquitin system components or their substrates. This technical guide provides an in-depth benchmark of these approaches, equipping researchers with the experimental frameworks and analytical tools needed to develop next-generation ubiquitin-targeting therapeutics.
Comparative Analysis: Degradation vs. Inhibition
Strategic Mechanisms and Applications
Targeted Protein Degradation strategies, including proteolysis-targeting chimeras (PROTACs), molecular glues, and biological degraders (bioPROTACs), function by inducing proximity between target proteins and E3 ubiquitin ligases, leading to target ubiquitination and proteasomal degradation [107] [108]. This catalytic mode of action offers several advantages: it targets proteins traditionally considered "undruggable," achieves potent effects at sub-stoichiometric concentrations, and can overcome resistance mutations by eliminating the entire protein scaffold [107].
Functional Inhibition approaches employ small molecules or biologics to block the activity of specific components within the ubiquitin system, including E1/E2/E3 enzymes, deubiquitinases (DUBs), or ubiquitin-binding domains. Unlike degradation, inhibition is typically reversible and can precisely modulate specific ubiquitin-dependent signaling pathways without eliminating the target protein [109] [110].
Table 1: Strategic Comparison of Degradation vs. Inhibition Approaches
| Parameter | Targeted Degradation | Functional Inhibition |
|---|---|---|
| Mode of Action | Catalytic, event-driven | Stoichiometric, occupancy-driven |
| Target Scope | Expands to "undruggable" proteome (scaffolds, aggregates) | Limited to proteins with functional pockets |
| Specificity | High specificity potential but dependent on E3 ligase expression | Varies; can achieve high specificity with allosteric inhibitors |
| Resistance Potential | Lower (eliminates entire protein) | Higher (point mutations can confer resistance) |
| Dosing | Sub-stoichiometric, prolonged effect | Continuous exposure often required |
| Therapeutic Applications | Oncology, neurodegenerative diseases, targeted protein removal | Oncology (signaling inhibition), inflammation, precise pathway modulation |
Quantitative Performance Benchmarking
Recent studies have provided direct quantitative comparisons between degradation and inhibition strategies for specific targets. For the oncoprotein SHP2, E2-based bioPROTACs induced approximately 90% degradation of cellular SHP2, significantly outperforming both small molecule inhibitors and VHL-based degraders in suppression of downstream ERK signaling [108]. Similarly, PROTAC-mediated degradation of RIPK2 demonstrated complete ablation of protein levels, whereas inhibition only blocked enzymatic activity [106].
The functional consequences of ubiquitin system modulation extend beyond immediate target reduction. Global proteomic analyses reveal that E2-based degraders exhibit distinct off-target profiles compared to E3-based systems, potentially due to differential engagement with endogenous E3 ligase networks [108]. This highlights the importance of comprehensive proteomic assessment when benchmarking therapeutic strategies.
Table 2: Quantitative Benchmarking of Degradation vs. Inhibition for Specific Targets
| Target | Degradation Efficiency | Inhibition Efficacy | Functional Outcome |
|---|---|---|---|
| SHP2 | E2B bioPROTAC: ~90% reduction [108] | Small molecule: <50% signaling suppression | Degradation superior for pathway suppression |
| RIPK2 | PROTAC: Complete degradation [106] | Ponatinib: Blocks kinase activity only | Degradation ablates scaffolding functions |
| Oncogenic KRAS | E2 bioPROTAC: Demonstrated [108] | Direct inhibitors: Limited mutant specificity | Degradation addresses multiple mutants |
| F-box Proteins | Not typically degraded | Small molecules: Substrate-specific effects [109] | Inhibition allows precise pathway modulation |
Experimental Protocols for Strategy Evaluation
Assessing Ubiquitination Dynamics
Chain-Specific TUBE Assay for Monitoring Linkage-Specific Ubiquitination
Purpose: To quantitatively differentiate between K48-linked (degradative) and K63-linked (signaling) polyubiquitination events in response to degradation versus inhibition strategies [106].
Workflow:
- Cell Treatment & Lysis: Treat cells (e.g., THP-1 monocytes) with either:
- Degradation trigger: PROTAC/RIPK2-degrader (1µM, 4-6h) to induce K48 ubiquitination
- Inhibition control: L18-MDP (200ng/mL, 30min) to stimulate K63 ubiquitination
- Use ubiquitination-preserving lysis buffer (e.g., containing 50mM Tris-HCl pH7.5, 150mM NaCl, 1% NP-40, 1mM N-ethylmaleimide, protease/phosphatase inhibitors)
Chain-Specific Capture:
- Coat 96-well plates with either K48-TUBE, K63-TUBE, or Pan-TUBE (100µL, 5µg/mL, 4°C overnight)
- Block plates with 3% BSA in TBST (1h, RT)
- Incubate with cell lysates (200µg total protein, 2h, RT)
Target Detection:
- Wash 3x with TBST
- Incubate with target-specific primary antibody (e.g., anti-RIPK2, 1:1000, 2h, RT)
- Detect with HRP-conjugated secondary antibody (1:5000, 1h, RT)
- Develop with chemiluminescent substrate and quantify luminescence
Data Interpretation: K48-TUBE specifically captures degradative ubiquitination induced by PROTACs, while K63-TUBE captures signaling ubiquitination induced by inflammatory stimuli [106].
TUBE Assay Workflow for Linkage-Specific Ubiquitination Detection
Functional Degradation Assessment
bioPROTAC Delivery and Target Degradation Quantification
Purpose: To evaluate the efficacy of biological degraders (E2 or E3 fusions) against intracellular targets such as SHP2 and KRAS [108].
Workflow:
- bioPROTAC Design:
- E2 bioPROTAC: Fuse target-binding domain (e.g., aCS3 for SHP2) to human E2 enzyme (UBE2D1 or UBE2B) via (G4S)3 linker
- E3 bioPROTAC: Fuse same binding domain to E3 ligase domain (e.g., VHL)
- Include HA-tag for detection and appropriate controls (catalytic mutants, binding-deficient mutants)
Cell Transfection:
- Transfect U2OS cells with in vitro transcribed mRNA encoding bioPROTACs (100ng/well, 96-well format)
- Use lipid-based transfection reagents; incubate for 24h at 37°C
Target Quantification:
- Immunofluorescence: Fix cells, stain with anti-target (SHP2) and anti-HA antibodies, quantify fluorescence intensity normalized to untransfected cells
- Western Blotting: Resolve cell lysates by SDS-PAGE, transfer to PVDF, probe with anti-target and loading control antibodies, quantify band intensity
Mechanistic Validation:
- Proteasome dependence: Treat with MG132 (10µM, 6h) to block degradation
- E3 ligase dependence: Test E2 mutants with impaired E3 binding (e.g., E2D1F62A)
- Catalytic requirement: Test E2 catalytic cysteine mutants (e.g., E2D1C85A)
This protocol demonstrated that E2B_aCS3 bioPROTACs achieved ~90% SHP2 degradation, outperforming both E2D1-based degraders (~54% degradation) and VHL-based fusions (~62% degradation) [108].
Computational and Analytical Tools
Ubiquitin Ligase Activity Profiling
UbE3-APA (Ubiquitin E3 Ligase Activity Profiling Analysis) is a Python-based computational algorithm that identifies significantly activated or suppressed E3 ligases based on quantitative ubiquitylome datasets [111].
Methodology:
- Input Data: Site-specific ubiquitination ratios from quantitative proteomics (e.g., SILAC, TMT)
- Normalization: Options for computational normalization (median-based) or protein-normalized ratios (site ratio/protein ratio)
- Database Integration: Curated E3-substrate interactions from UbiBrowser, Ubinet, and multidimensional databases
- Statistical Analysis: Bootstrapping procedure with 10,000 iterations to compare target ratios against background distribution
- Output: Z-scores and p-values indicating significant E3 ligase activation or suppression
Application: UbE3-APA successfully validated SPOP enzyme activity modulation and revealed PARKIN activation during mitophagy, demonstrating utility for identifying E3 ligases amenable to degradation approaches [111].
Proteomics Data Analysis Considerations
Optimal differential expression analysis for ubiquitination proteomics requires careful workflow selection. Key considerations include:
- Normalization: For label-free DDA and TMT data, normalization and statistical methods for differential analysis exert greater influence than other preprocessing steps [112]
- Imputation: High-performing workflows for label-free data are enriched for SeqKNN, Impseq, or MinProb imputation while eschewing simple statistical tools [112]
- Ensemble Inference: Integrating results from top-performing workflows (e.g., combining top0 intensities, directLFQ, and MaxLFQ) can expand differential proteome coverage, improving pAUC(0.01) by up to 4.61% and G-mean scores by up to 11.14% [112]
Computational Analysis of E3 Ligase Activity
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Research Reagents for Ubiquitin-Targeting Therapeutic Development
| Reagent/Category | Specific Examples | Function/Application |
|---|---|---|
| Chain-Specific TUBEs | K48-TUBE, K63-TUBE, Pan-TUBE [106] | Selective capture and detection of linkage-specific polyubiquitin chains in high-throughput assays |
| E2 bioPROTAC Components | UBE2D1, UBE2B, target-binding domains (aCS3) [108] | Engineered biological degraders for targeted protein degradation |
| Computational Tools | UbE3-APA [111] | Python-based algorithm for E3 ligase activity profiling from ubiquitylome data |
| Proteasome Inhibitors | MG132, Bortezomib [108] | Validation of proteasome-dependent degradation mechanisms |
| Quantitative Proteomics Platforms | SILAC, TMT, DIA [113] [112] | Global quantification of ubiquitination dynamics and off-target effects |
| E3 Ligase Modulators | PROTACs, Molecular Glues [107] | Small molecules harnessing endogenous E3 ligases for targeted degradation |
| DUB Inhibitors/Activators | USP2 modulators [110] | Tools for investigating deubiquitination roles in cancer pathways |
Therapeutic Applications and Clinical Translation
Oncology Applications
In cancer therapy, the choice between degradation and inhibition strategies depends on target biology and therapeutic objectives. Degradation approaches show particular promise for:
- Oncoproteins with scaffolding functions (e.g., SHP2, RAS) where elimination disrupts multiple signaling nodes simultaneously [108]
- Therapy-resistant mutants where catalytic degradation can overcome acquired resistance [107]
- Undruggable targets lacking conventional binding pockets [107]
Inhibition strategies remain valuable for:
- Precise pathway modulation where complete elimination would cause toxicity
- DUB-targeting where restoring native substrate levels is therapeutic (e.g., USP2 inhibition in gastric cancer) [110]
- Combination therapies with targeted degraders to address compensatory mechanisms
Biomarker-Driven Strategy Selection
Emerging evidence supports biomarker-guided selection between degradation and inhibition. For instance, USP2 expression levels in gastric cancer correlate with patient prognosis and drug sensitivity, suggesting USP2 status could guide therapeutic decisions [110]. Similarly, E3 ligase expression patterns may predict responsiveness to degradation approaches [111] [109].
The integration of ubiquitin-focused biomarkers with proteomic profiling enables precision medicine approaches for ubiquitin-targeting therapies, potentially identifying patient subgroups most likely to benefit from degradation versus inhibition strategies.
The strategic choice between targeted degradation and functional inhibition within the ubiquitin system requires careful consideration of target biology, mechanism of action, and therapeutic context. Degradation approaches, particularly PROTACs and emerging bioPROTAC technologies, offer unprecedented ability to eliminate problematic proteins, especially those traditionally considered undruggable. Inhibition strategies provide precise temporal control over specific ubiquitin-dependent pathways without complete protein elimination. The experimental and computational frameworks presented herein provide researchers with robust methodologies for benchmarking these approaches in specific disease contexts, particularly cancer, where alterations to the ubiquitin code drive pathogenesis and treatment resistance. As both strategies advance toward clinical application, their intelligent deployment—and potential combination—will expand the therapeutic landscape for targeting the ubiquitin system in cancer and beyond.
Conclusion
The intricate ubiquitin code represents a master regulatory system in cell biology, and its deliberate subversion is a cornerstone of cancer development. Cracking this code has unveiled a rich landscape of therapeutic vulnerabilities, from specific E3 ligases and DUBs to the revolutionary paradigm of targeted protein degradation. Future research must focus on developing highly specific modulators, understanding context-dependent functions to minimize toxicity, and designing biomarker-driven combination therapies. Integrating ubiquitin-targeting strategies with existing modalities like immunotherapy and radiotherapy holds immense promise for overcoming resistance and achieving durable responses, ultimately establishing the ubiquitin system as a central pillar in the next generation of precision cancer medicines.
References
- 1. Ubiquitin proteasome system in immune regulation and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10163937/]
- 2. The ubiquitin system: from cell signalling to disease ... [https://www.nature.com/articles/s41418-020-00703-w]
- 3. Perilous journey: a tour of the ubiquitin–proteasome system [https://www.sciencedirect.com/science/article/abs/pii/S0962892413002274]
- 4. Ubiquitination Enzymes in Cancer, Cancer Immune Evasion ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11763706/]
- 5. Ubiquitin-Proteasome System [https://lifesensors.com/ubiquitinproteasomesystem/]
- 6. Ubiquitination and deubiquitination in cancer [https://molecular-cancer.biomedcentral.com/articles/10.1186/s12943-024-02046-3]
- 7. Combinatorial ubiquitin code degrades deubiquitylation- ... [https://www.nature.com/articles/s41467-025-57873-9]
- 8. The ubiquitin code of RAS proteins: Decoding its role in ... [https://www.sciencedirect.com/science/article/pii/S2589004225012908]
- 9. Expanding the ubiquitin code in pancreatic cancer [https://www.sciencedirect.com/science/article/pii/S0925443923002508]
- 10. Ubiquitin modifications | Cell Research [https://www.nature.com/articles/cr201639]
- 11. E3 ubiquitin ligases: styles, structures and functions - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC8607428/]
- 12. Noncovalent Ubiquitin Interactions Regulate the Catalytic ... [https://www.sciencedirect.com/science/article/abs/pii/S0968000416301037]
- 13. Ubiquitination of transcription factors in cancer: unveiling ... [https://pubmed.ncbi.nlm.nih.gov/40227962/]
- 14. Ubiquitin Function and Variety | News-Medical [https://www.news-medical.net/life-sciences/Ubiquitin-Function-and-Variety.aspx]
- 15. Mechanisms of mono- and poly - ubiquitination : Ubiquitination specificity... [https://pmc.ncbi.nlm.nih.gov/articles/PMC2927562/]
- 16. Decoding the ubiquitin network: molecular mechanisms ... [https://pubmed.ncbi.nlm.nih.gov/41039553/]
- 17. Ubiquitin chain conformation regulates recognition and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3605796/]
- 18. The role of ubiquitination in tumorigenesis and targeted ... [https://www.nature.com/articles/s41392-020-0107-0]
- 19. The Ubiquitin System: An Emerging Therapeutic Target for ... [https://www.mdpi.com/1422-0067/22/17/9629]
- 20. Emerging Role of Ubiquitin-Specific Protease 19 in ... [https://www.frontiersin.org/journals/cell-and-developmental-biology/articles/10.3389/fcell.2022.889166/full]
- 21. The role of ubiquitination and deubiquitination in cancer ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7529510/]
- 22. Decoding the ubiquitin network: molecular mechanisms and ... [https://molecular-cancer.biomedcentral.com/articles/10.1186/s12943-025-02433-4]
- 23. Ubiquitination in cancer: mechanisms and therapeutic ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12479132/]
- 24. The ubiquitin code of RAS proteins: Decoding its role in ... [https://pubmed.ncbi.nlm.nih.gov/40703447/]
- 25. The ubiquitin code of RAS proteins: Decoding its role in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12283562/]
- 26. The role of ubiquitination and deubiquitination in cancer ... [https://www.frontiersin.org/journals/oncology/articles/10.3389/fonc.2025.1464914/full]
- 27. Unraveling the critical role of SUMOylation in the governing ... [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2025.1654167/full]
- 28. Current methodologies in protein ubiquitination characterization: from... [https://cellandbioscience.biomedcentral.com/articles/10.1186/s13578-022-00870-y]
- 29. Decoding the ubiquitin network: molecular mechanisms and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12492556/]
- 30. K29-linked ubiquitin signaling regulates... | Nature Chemical Biology [https://www.nature.com/articles/s41589-021-00823-5?error=cookies_not_supported&code=f972e456-aec5-4927-a9ea-1559900eb1c5]
- 31. Functional landscape of ubiquitin linkages couples K29- ... [https://link.springer.com/article/10.1038/s44318-025-00599-7]
- 32. Interpreting the Language of Polyubiquitin with Linkage - Specific ... [https://pubmed.ncbi.nlm.nih.gov/30242722/]
- 33. Frontiers | Mass -Based Spectrometry for Investigating... Proteomics [https://www.frontiersin.org/journals/genetics/articles/10.3389/fgene.2016.00109/full]
- 34. Targeting the ubiquitin system by fragment-based drug ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9580268/]
- 35. Constructing a pancancer ubiquitination regulatory network to ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12382526/]
- 36. Rational discovery of molecular glue degraders based on ... [https://www.sciencedirect.com/science/article/abs/pii/S135964462500193X]
- 37. High Throughput Screening Market [https://www.futuremarketinsights.com/reports/high-throughput-screening-market]
- 38. High Throughput Screening (HTS) Market Size 2025-2029 [https://www.technavio.com/report/high-throughput-screening-market-industry-analysis]
- 39. Proteolysis‐Targeting Chimera (PROTAC) - PubMed Central [https://pmc.ncbi.nlm.nih.gov/articles/PMC12495453/]
- 40. Review Molecular glues and PROTACs in targeted protein ... [https://www.sciencedirect.com/science/article/abs/pii/S0006295225005623]
- 41. Targeted Protein Degradation with PROTACs and ... [https://blog.crownbio.com/targeted-protein-degradation-with-protacs-and-molecular-glues]
- 42. Selective degradation of multimeric proteins by TRIM21-based... [https://pubmed.ncbi.nlm.nih.gov/39488207/]
- 43. : A New Dawn After Molecular | Biopharma PEG Glues PROTAC [https://www.biochempeg.com/article/271.html]
- 44. PROTAC Degraders in Clinical Trails: 2025 Update [https://www.biochempeg.com/article/434.html]
- 45. Intrinsic signaling pathways modulate targeted protein degradation [https://www.nature.com/articles/s41467-024-49519-z?error=cookies_not_supported&code=a4a8faec-b9ed-4362-a567-54158ad718ec]
- 46. E3 Ubiquitin Ligases: Critical Roles in Cancer Progression ... [https://www.frontiersin.org/research-topics/70570/e3-ubiquitin-ligases-critical-roles-in-cancer-progression-and-therapeutic-implicationsundefined]
- 47. In Vivo CRISPR Screens Identify E3 Ligase Cop1 as a ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9136996/]
- 48. Comprehensive investigation of the molecular basis ... [https://www.cancerbiomed.org/content/early/2025/10/23/j.issn.2095-3941.2025.0290]
- 49. CRISPR screening redefines therapeutic target ... [https://www.sciencedirect.com/science/article/pii/S2095177925001741]
- 50. CRISPR-Cas9 screening reveals G2E3 as a novel ... [https://www.nature.com/articles/s41420-025-02717-0]
- 51. Ubiquitination Enzymes in Cancer, Cancer Immune ... [https://www.mdpi.com/2073-4409/14/2/69]
- 52. Ubiquitinomics revealed disease- and stage-specific patterns relevant... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10439878/]
- 53. Quantitative ubiquitylomics reveals the ubiquitination ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8385350/]
- 54. Frontiers | Ubiquitination and ALL: Identifying FBXO8 as a prognostic... [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2025.1554231/full]
- 55. Construction of ubiquitination-related risk model for ... [https://www.nature.com/articles/s41598-025-92177-4]
- 56. Significance of the E3 ubiquitin protein UBR5 as an... | Oncotarget [https://www.oncotarget.com/article/22531/text/]
- 57. Identification of ubiquitin markers for survival and ... [https://www.sciencedirect.com/science/article/pii/S2405844024133191]
- 58. Ubiquitin signaling in immune responses - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC4822134/]
- 59. Review Ubiquitin—A structural perspective [https://www.sciencedirect.com/science/article/abs/pii/S1097276524010104]
- 60. An adaptive stress response that confers cellular resilience ... [https://www.nature.com/articles/s41467-023-43262-7]
- 61. Quantifying Ubiquitin Signaling - PMC - PubMed Central [https://pmc.ncbi.nlm.nih.gov/articles/PMC4441763/]
- 62. Screening for E -Ubiquitin 3 : challenges and... ligase inhibitors [https://pmc.ncbi.nlm.nih.gov/articles/PMC4226663/]
- 63. Deubiquitinases (DUBs) and DUB inhibitors: a patent review [https://pmc.ncbi.nlm.nih.gov/articles/PMC4834700/]
- 64. Identification and validation of Selective Deubiquitinase ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9473745/]
- 65. Screening of DUB activity and specificity by MALDI-TOF ... [https://www.nature.com/articles/ncomms5763]
- 66. Targeting the Ubiquitin Proteasome System [https://www.discoveryontarget.com/ubiquitin-proteasome/15]
- 67. of ubiquitin Inhibitors as potential new antimalarial drug leads E 3 ligase [https://bmcpharmacoltoxicol.biomedcentral.com/articles/10.1186/s40360-017-0147-4]
- 68. Deubiquitinating enzymes as therapeutic targets in diabetic ... [https://www.sciencedirect.com/science/article/pii/S0165614725001580]
- 69. Drug resistance mechanisms and treatment strategies ... [https://molecular-cancer.biomedcentral.com/articles/10.1186/s12943-024-02005-y]
- 70. Molecular Mechanisms of the Ubiquitin-Specific Proteases ... [https://www.mdpi.com/2227-9059/13/11/2586]
- 71. Restoring our ubiquitination machinery to overcome ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11073315/]
- 72. Targeting the ubiquitin-proteasome pathway to overcome ... [https://www.sciencedirect.com/science/article/abs/pii/S1368764619300603]
- 73. Drug resistance in cancer: molecular mechanisms and ... [https://link.springer.com/article/10.1186/s43556-025-00352-w]
- 74. Targeted protein degradation: advances in drug discovery ... [https://www.nature.com/articles/s41392-024-02004-x]
- 75. Identification of biomarkers based on ubiquitin-correlated ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12394886/]
- 76. A novel machine learning model based on ubiquitin-related ... [https://eurjmedres.biomedcentral.com/articles/10.1186/s40001-023-00993-z]
- 77. Machine learning-driven multi-targeted drug discovery in ... [https://www.nature.com/articles/s41698-025-01058-6]
- 78. FBXW7 in gastrointestinal cancers: from molecular ... - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC11694028/]
- 79. Molecular insights and clinical implications for the tumor ... [https://www.sciencedirect.com/science/article/abs/pii/S0304419X24000714]
- 80. FBXW7 tumor suppressor regulation by dualspecificity ... [https://www.nature.com/articles/s41419-023-05724-0]
- 81. PSMD11 facilitates immune escape by recruiting USP14 to ... [https://jtd.amegroups.org/article/view/105980/html]
- 82. Molecular mechanisms and potential targeting strategies of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12511930/]
- 83. Ubiquitin modification in the regulation of tumor ... [https://ehoonline.biomedcentral.com/articles/10.1186/s40164-024-00552-0]
- 84. Targeting ubiquitin signaling for cancer immunotherapy - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC7804490/]
- 85. Targeted inhibition of ubiquitin signaling reverses ... [https://www.nature.com/articles/s42003-022-03639-8]
- 86. The Emerging Role of Deubiquitinases in Radiosensitivity [https://www.sciencedirect.com/science/article/pii/S0360301623082378]
- 87. Drug Development Targeting the Ubiquitin–Proteasome ... [https://www.mdpi.com/2072-6694/12/4/902]
- 88. Recent advances in the development of deubiquitinases ... [https://www.sciencedirect.com/science/article/abs/pii/S0223523424000412]
- 89. Targeting deubiquitinating enzymes and ubiquitin pathway ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12506015/]
- 90. The RING finger protein family in health and disease [https://www.nature.com/articles/s41392-022-01152-2]
- 91. Recent advances in small molecule inhibitors of ... [https://www.sciencedirect.com/science/article/abs/pii/S0223523425000893]
- 92. Targeting ubiquitin specific proteases (USPs) in cancer ... [https://jeccr.biomedcentral.com/articles/10.1186/s13046-023-02805-y]
- 93. The roles and targeting options of TRIM family proteins in ... [https://www.frontiersin.org/journals/pharmacology/articles/10.3389/fphar.2022.999380/full]
- 94. The E3-ligase TRIM family of proteins regulates signaling ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3584420/]
- 95. E3 ubiquitin ligase TRIM29 promotes pancreatic cancer ... [https://translational-medicine.biomedcentral.com/articles/10.1186/s12967-021-03007-w]
- 96. Ubiquitin specific peptidase 3: an emerging deubiquitinase ... [https://www.nature.com/articles/s41420-024-02010-6]
- 97. Variety in the USP deubiquitinase catalytic mechanism - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC10867860/]
- 98. The Mechanism of Ubiquitination or Deubiquitination ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10741492/]
- 99. Involvement of E3 Ligases and Deubiquitinases in the ... [https://www.mdpi.com/2073-4409/8/6/598]
- 100. Advancing Design Strategy of PROTACs for Cancer Therapy [https://pmc.ncbi.nlm.nih.gov/articles/PMC12188103/]
- 101. Proteolysis‐targeting chimeras in cancer therapy [https://pmc.ncbi.nlm.nih.gov/articles/PMC12535346/]
- 102. Targeting Oncoproteins for Degradation by Small Molecule ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8971670/]
- 103. Summary of PROTAC Degraders in Clinical Trials [https://www.biochempeg.com/article/282.html]
- 104. Cellular parameters shaping pathways of targeted protein ... [https://www.nature.com/articles/s42003-025-08104-w]
- 105. Press Release Details [https://ir.arvinas.com/news-releases/news-release-details/arvinas-releases-interim-clinical-data-further-demonstrating]
- 106. Unraveling chain specific ubiquitination in cells using tandem ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12217038/]
- 107. Opportunities in proximity modulation: Bridging academia ... [https://www.sciencedirect.com/science/article/pii/S1097276525006197]
- 108. Targeted protein degradation using chimeric human E2 ... [https://www.nature.com/articles/s42003-024-06803-4]
- 109. F-box proteins in cancer: from cancer cells to the tumor ... [https://biosignaling.biomedcentral.com/articles/10.1186/s12964-025-02445-z]
- 110. The downregulation of ubiquitin-specific peptidase 2 ... [https://www.nature.com/articles/s41598-025-08881-8]
- 111. UbE3-APA: a bioinformatic strategy to elucidate ubiquitin E3 ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9004656/]
- 112. Optimizing differential expression analysis for proteomics ... [https://www.nature.com/articles/s41467-024-47899-w]
- 113. Benchmarking SILAC Proteomics Workflows and Data ... [https://www.sciencedirect.com/science/article/pii/S1535947625000787]