Deubiquitinating Enzymes (DUBs) in Cancer: Mechanisms, Therapeutic Targeting, and Future Directions
This comprehensive review elucidates the critical functions of deubiquitinating enzymes (DUBs) in oncogenesis and cancer progression.
Deubiquitinating Enzymes (DUBs) in Cancer: Mechanisms, Therapeutic Targeting, and Future Directions
Abstract
This comprehensive review elucidates the critical functions of deubiquitinating enzymes (DUBs) in oncogenesis and cancer progression. Covering foundational biology to clinical applications, it details how DUBs regulate key cancer hallmarks—including cell proliferation, metabolic reprogramming, and immune evasion—by controlling protein stability and signaling pathways. The article systematically analyzes recent advances in DUB inhibitor development, current challenges in therapeutic targeting, and emerging strategies like PROTACs and DUBTACs. Through validation of specific DUBs as biomarkers and therapeutic targets across cancer types, this resource provides researchers and drug development professionals with an integrated perspective on targeting the ubiquitin system for novel cancer therapeutics.
The Biology of DUBs: Unraveling Their Roles in Cancer Pathogenesis
The Ubiquitin-Proteasome System (UPS) is a highly selective, ATP-dependent mechanism that serves as the primary pathway for intracellular protein degradation in eukaryotic cells, playing a critical role in maintaining cellular protein homeostasis [1] [2]. This system regulates a vast array of cellular processes, including cell cycle progression, apoptosis, signal transduction, DNA repair, and immune responses [1] [2]. Dysregulation of the UPS is implicated in numerous human diseases, most notably cancer, neurodegenerative disorders, and autoimmune conditions, making it a focal point for therapeutic development [3] [4] [5].
The core function of the UPS is to target specific proteins for degradation by covalently tagging them with ubiquitin polymers. Ubiquitin is a small, 76-amino acid polypeptide that is highly conserved across species [2] [6]. The process of ubiquitin conjugation, known as ubiquitination, involves a sequential enzymatic cascade [1] [6]:
- E1 (Ubiquitin-Activating Enzyme): Activates ubiquitin in an ATP-dependent reaction
- E2 (Ubiquitin-Conjugating Enzyme): Accepts the activated ubiquitin from E1
- E3 (Ubiquitin Ligase): Recognizes specific protein substrates and facilitates the transfer of ubiquitin from E2 to the target protein
The fate of the ubiquitinated protein is determined by the topology of the ubiquitin chain. Proteins tagged with K48-linked or K11-linked polyubiquitin chains are typically directed to the 26S proteasome for degradation [1]. In contrast, monoubiquitination or K63-linked polyubiquitination often serves non-proteolytic functions, regulating processes such as endocytosis, DNA repair, and kinase activation [1] [2].
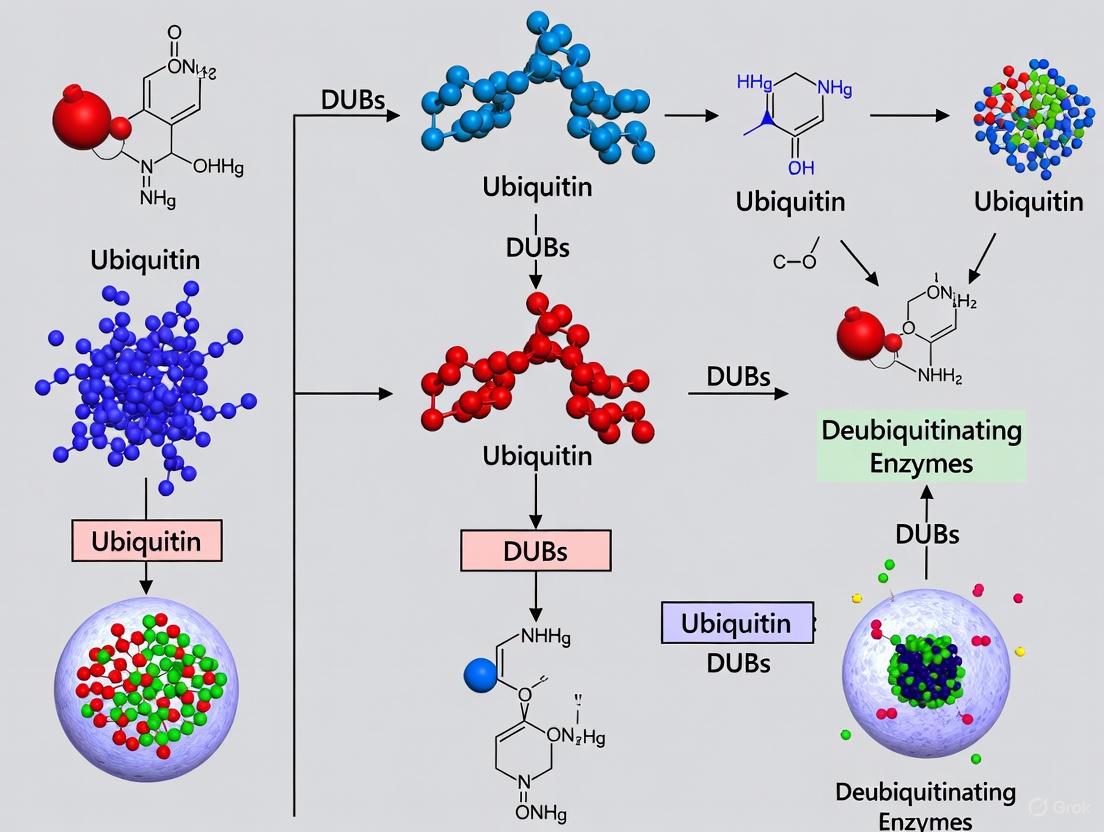
Figure 1: The Ubiquitin-Proteasome System Pathway. This diagram illustrates the sequential enzymatic cascade of ubiquitination, culminating in proteasomal degradation of the target protein.
Deubiquitinating Enzymes (DUBs): Classification and Functions
Deubiquitinating enzymes (DUBs) constitute a diverse family of proteases that catalyze the reverse reaction of ubiquitination, removing ubiquitin moieties from modified proteins [3] [4]. This activity allows DUBs to exert precise control over ubiquitin-dependent signaling pathways by: rescuing proteins from degradation, editing ubiquitin chain topology, recycling ubiquitin, and processing ubiquitin precursors [3]. The human genome encodes approximately 100 DUBs, which are categorized into seven families based on their catalytic domain structure and mechanism of action [3] [4].
Table 1: Major Deubiquitinating Enzyme (DUB) Families
| Family | Representative Members | Catalytic Mechanism | Key Functions in Cancer |
|---|---|---|---|
| USP (Ubiquitin-Specific Proteases) | USP1, USP7, USP9X, USP14, USP22, USP28, USP33, USP34 | Cysteine Protease | DNA damage repair, oncoprotein stabilization, stemness regulation, chemoresistance [3] [4] [7] |
| OTU (Ovarian Tumor Proteases) | OTUB1, OTUD1, OTUD3, A20 | Cysteine Protease | Immune signaling regulation, suppression of metastasis [3] [4] |
| UCH (Ubiquitin C-Terminal Hydrolases) | UCH-L1, UCH-L3, UCH-L5, BAP1 | Cysteine Protease | Neurodegeneration, tumor suppression, histone modification [3] [4] [5] |
| MJD (Machado-Josephin Domain Proteases) | Ataxin-3, MJD1, MJD2 | Cysteine Protease | Protein aggregation diseases, transcriptional regulation |
| JAMM/MPN (Zinc Metalloproteases) | PSMD14, BRCC36, AMSH | Zinc Metalloprotease | Proteasomal subunit, DNA damage response, endosomal sorting [3] |
| MINDY | MINDY-1, MINDY-2 | Cysteine Protease | Preferential cleavage of K48-linked ubiquitin chains |
| ZUP1 | ZUP1 | Cysteine Protease | RNA regulation, ribosome-associated quality control |
Except for the JAMM/MPN family, which are zinc metalloproteases, all DUB families utilize a cysteine protease mechanism [3]. The catalytic triad for cysteine protease DUBs typically consists of three conserved amino acids: histidine, cysteine, and asparagine/aspartate [3]. Metalloprotease DUBs rely on the coordination of histidine, aspartic acid, and serine residues with zinc ions for their catalytic activity [3].
DUBs demonstrate remarkable specificity for different ubiquitin chain linkages. For instance, certain DUBs preferentially cleave K48-linked chains (typically associated with proteasomal degradation), while others target K63-linked chains (often involved in signaling) or other atypical linkages [1] [3]. This specificity allows for precise regulation of diverse ubiquitin-dependent processes.
DUBs in Cancer Biology and Therapeutic Resistance
Dysregulation of DUB activity is a hallmark of numerous cancers, with specific DUBs functioning as either oncogenes or tumor suppressors depending on cellular context [4] [7]. DUBs contribute to tumorigenesis through multiple mechanisms, including stabilization of oncoproteins, inactivation of tumor suppressors, regulation of DNA damage response, and modulation of cancer stemness [4] [7].
In pancreatic ductal adenocarcinoma (PDAC), several DUBs have been identified as key drivers of disease progression. USP28 promotes cell cycle progression and inhibits apoptosis by stabilizing the transcription factor FOXM1, thereby activating the Wnt/β-catenin pathway [4]. USP21 maintains cancer stemness by stabilizing TCF7 and promotes tumor growth through mTOR signaling activation and micropinocytosis induction, supporting amino acid sustainability [4]. Interestingly, USP9X demonstrates context-dependent functions, acting as a tumor suppressor in some PDAC models while promoting tumor cell survival in others [4].
DUBs also play critical roles in developing chemoresistance across various cancer types [7]. They can confer resistance by stabilizing drug targets, enhancing DNA repair capacity, inhibiting apoptosis, and promoting survival pathways. For instance, USP1 regulates DNA damage repair and is associated with resistance to platinum-based chemotherapy [3] [7]. USP7 stabilizes MDM2, leading to p53 degradation and reduced apoptosis in response to genotoxic stress [3] [7]. USP9X inhibits apoptosis by stabilizing anti-apoptotic proteins like MCL1, contributing to resistance in various blood cancers and solid tumors [7].
Table 2: DUBs in Cancer Chemoresistance and Their Mechanisms
| DUB | Cancer Type | Resistance Mechanism | Therapeutic Implication |
|---|---|---|---|
| USP1 | Non-small cell lung cancer, ovarian cancer | DNA damage repair regulation, replication stress response | USP1 inhibitors reverse cisplatin resistance [3] [7] |
| USP7 (HAUSP) | Multiple cancers | Stabilizes MDM2, promotes p53 degradation, enhances DNA repair | USP7 inhibition restores p53 function and chemosensitivity [3] [7] |
| USP9X | Blood cancers, pancreatic cancer | Stabilizes MCL1, BCL2 family proteins, inhibits apoptosis | USP9X inhibition promotes apoptosis in combination with chemotherapy [7] |
| USP22 | Triple-negative breast cancer | Regulates Warburg effect via c-Myc deubiquitination | Promotes stemness, EMT, and chemoresistance [7] |
| USP14 | Multiple cancers | Proteasome-associated, regulates protein turnover | Inhibition enhances sensitivity to proteasome inhibitors [3] |
| UCH-L1 | Breast cancer, lymphoma | Regulates oxidative stress response, stabilizes oncoproteins | Elevated in chemoresistant cancers, potential biomarker [7] [5] |
| USP8 | Pancreatic cancer | Stabilizes Nrf2, enhances antioxidant response | Promotes gemcitabine resistance [7] |
Experimental Approaches for DUB Research
Screening and Profiling DUB Inhibitors
The development of selective DUB inhibitors requires robust screening methods and careful assessment of compound properties. Key approaches include:
High-Throughput Screening (HTS): Utilizes fluorogenic substrates such as Ubiquitin-Rhodamine (Ub-Rho) to identify initial hit compounds [8]. This assay measures DUB activity by the increase in fluorescence upon cleavage of ubiquitin from the rhodamine tag.
Competitive Activity-Based Protein Profiling (ABPP): Employs electrophilic probe compounds that covalently modify the active site cysteine of DUBs, enabling assessment of target engagement and selectivity across the DUB family [8]. This approach helps characterize inhibitor selectivity and identify potential off-target effects.
On-Chip Preconcentration Microchip Capillary Electrophoresis: An advanced method for high-throughput selectivity profiling of DUB inhibitors, providing improved sensitivity and resolution for assessing compound binding [8].
Open-Source Electrophilic Fragment Screening: Identifies chemical starting points for covalent inhibitor development, particularly useful for challenging targets like UCHL1 [8].
Table 3: Key Research Reagents and Tools for DUB Studies
| Research Tool | Composition/Type | Application in DUB Research |
|---|---|---|
| Ubiquitin-Rhodamine (Ub-Rho) | Fluorogenic ubiquitin substrate | High-throughput screening of DUB inhibitors [8] |
| Activity-Based Probes (ABPs) | Covalent probes with reporter tags | Profiling DUB activity and inhibitor selectivity [8] |
| Tandem Ubiquitin-Binding Entities (TUBEs) | Engineered ubiquitin-binding domains | Protection of polyubiquitin chains from DUBs, isolation of ubiquitinated proteins [6] |
| PROTACs (Proteolysis-Targeting Chimeras) | Bifunctional molecules (E3 ligase binder + target binder) | Targeted protein degradation by recruiting E3 ubiquitin ligases [1] [6] |
| DUBTACs (Deubiquitinase-Targeting Chimeras) | Bifunctional molecules (DUB binder + target binder) | Selective stabilization of target proteins by recruiting DUBs [3] |
Target Validation and Functional Assessment
Once potential DUB inhibitors are identified, comprehensive validation is essential:
Cellular Target Engagement: Confirm compound interaction with the intended DUB in live cells using cellular thermal shift assays (CETSA) or competitive ABPP [8].
Pathway Modulation: Assess effects on known DUB substrates and downstream signaling pathways through immunoblotting, quantitative PCR, or proteomic analyses [4] [7].
Phenotypic Screening: Evaluate impact on cancer cell viability, apoptosis, cell cycle progression, migration, and invasion [4] [7].
Combination Studies: Test synergy with standard chemotherapy agents to assess potential for overcoming chemoresistance [7].
Figure 2: Experimental Workflow for DUB Inhibitor Discovery. This diagram outlines the key stages in identifying and validating potential therapeutic DUB inhibitors.
Therapeutic Targeting of DUBs in Cancer
The strategic inhibition of specific DUBs represents a promising approach for cancer therapy, particularly for overcoming chemoresistance [3] [7]. Several DUB inhibitors have shown promising results in preclinical studies and are advancing through clinical development.
USP1 inhibitors have demonstrated potential for treating cancers with DNA repair deficiencies, particularly in combination with DNA-damaging agents [3]. In non-small cell lung cancer models, USP1 inhibition has been shown to reverse cisplatin resistance [3] [7]. USP7 inhibitors can reactivate p53 signaling by disrupting the USP7-MDM2 interaction, leading to p53 stabilization and restoration of apoptosis in response to chemotherapy [3] [7]. USP9X inhibitors have shown efficacy in blood cancers and solid tumors by promoting the degradation of anti-apoptotic proteins like MCL1 [7].
Beyond monotherapies, DUB inhibitors show significant promise in combination regimens with conventional chemotherapy or targeted agents [7]. For example, USP9X inhibition enhances the efficacy of gemcitabine in pancreatic cancer by inhibiting autophagy and promoting apoptosis [7]. Similarly, USP8 inhibition sensitizes gastric cancer cells to chemotherapy by suppressing RhoA and Ras-mediated signaling pathways [7].
Emerging technologies are expanding the therapeutic potential of DUB targeting. PROTACs (Proteolysis-Targeting Chimeras) repurpose E3 ligases for targeted degradation of disease-causing proteins [1] [6]. Conversely, DUBTACs (Deubiquitinase-Targeting Chimeras) represent a novel approach to stabilize beneficial proteins by recruiting DUBs to prevent their degradation [3]. These bifunctional molecules offer new avenues for precisely manipulating the ubiquitin-proteasome system for therapeutic benefit.
The continued development of selective DUB inhibitors, combined with a deeper understanding of DUB biology in specific cancer contexts, holds significant promise for advancing cancer therapy, particularly for overcoming the persistent challenge of chemoresistance.
Deubiquitinating enzymes (DUBs) represent a critical regulatory node in the ubiquitin-proteasome system (UPS), functioning as proteases that cleave ubiquitin from protein substrates to reverse ubiquitin signaling [9] [10]. The human genome encodes approximately 100 DUBs that regulate diverse cellular processes including protein degradation, localization, activity, and protein-protein interactions [11] [9]. By antagonizing the function of E3 ubiquitin ligases, DUBs create a dynamic, reversible signaling system that responds to environmental cues and maintains cellular homeostasis [11] [10]. Dysregulation of DUB activity disrupts this delicate balance, leading to aberrant stabilization of oncoproteins or destabilization of tumor suppressors, which contributes fundamentally to cancer pathogenesis across multiple malignancies [11] [4] [12]. The classification of DUBs into distinct families based on sequence and structural similarity provides a critical framework for understanding their mechanistic roles in cancer biology and developing targeted therapeutic interventions.
Comprehensive DUB Family Classification
Deubiquitinating enzymes are classified into two fundamental classes based on their catalytic mechanisms: cysteine proteases and metalloproteases [9]. The cysteine protease class encompasses five major families (USP, UCH, OTU, MJD, MINDY), while the metalloprotease class contains only the JAMM family [9] [13]. This classification reflects evolutionary relationships and provides insights into structural characteristics and catalytic mechanisms that inform drug discovery efforts.
Table 1: Major Deubiquitinating Enzyme Families in Humans
| Family | Class | Catalytic Mechanism | Human Members | Representative DUBs | Structural Features |
|---|---|---|---|---|---|
| USP | Cysteine protease | Catalytic triad (Cys, His, Asp/Asn) | ~58 [9] | USP28, USP9X, USP22, USP7 | Large, diverse domains; insertions in catalytic domain [9] |
| UCH | Cysteine protease | Catalytic triad (Cys, His, Asp/Asn) | 4 [9] | UCH-L1, UCH-L5, BAP1 | Compact structure; restricted substrate access [11] |
| OTU | Cysteine protease | Catalytic triad (Cys, His, Asp/Asn) | 16 [9] [4] | OTUD5, A20, OTUB1 | Variant of USP-like fold; linkage specificity [4] |
| MJD | Cysteine protease | Catalytic triad (Cys, His, Asn) | 4 [9] | Ataxin-3, MJD1, MJD2 | Josephin domain; ubiquitin-interacting motifs [12] |
| MINDY | Cysteine protease | Catalytic triad (Cys, His, Asn) | 5 [4] | MINDY1-3 | Prefers K48-linked polyubiquitin chains [4] |
| JAMM | Metalloprotease | Zinc-dependent metalloprotease | 12 [13] | Rpn11, BRCC36, CSN5, AMSH | JAMM motif (ExnHxHx7Sx2D); MPN domain [13] |
Table 2: Key Characteristics of DUB Families
| Family | Ubiquitin Linkage Preference | Cellular Functions | Regulatory Mechanisms | Cancer Associations |
|---|---|---|---|---|
| USP | Broad specificity | DNA repair, cell cycle, signaling pathways, chromatin remodeling [11] | Protein-protein interactions, post-translational modifications, subcellular localization [10] | USP28 (overexpressed in colon/lung cancer) [9]; USP9X (context-dependent in PDAC) [4] |
| UCH | Monoubiquitin, small adducts | Ubiquitin recycling, processing precursors [9] | Dimerization, substrate access control [11] | UCH-L1 (elevated in malignancies) [9]; BAP1 (tumor suppressor mutated in multiple cancers) [11] [4] |
| OTU | Linkage-specific | NF-κB signaling, immune regulation, DNA damage response [11] [14] | Oxidation sensitivity, interaction partners [10] | OTUD5 (stabilizes YAP1 in TNBC) [14] |
| MJD | K48, K63-linked chains [10] | Protein homeostasis, endoplasmic reticulum-associated degradation, transcription regulation, DNA repair [10] [12] | Ubiquitin-interacting motifs, polyglutamine expansions [12] | Ataxin-3 (overexpressed in gastric, lung, breast cancers) [12] |
| MINDY | Prefers K48-linked chains [4] | Proteasomal degradation regulation | Unknown | Under investigation in cancer |
| JAMM | Linkage-specific (varies by member) | Proteasome function (Rpn11), DNA repair (BRCC36), endocytosis (AMSH) [13] | Complex assembly, subcellular localization, Ins-1 loop conformation [13] | BRCC36 (DNA damage control); CSN5 (PD-L1 stabilization) [13] [14] |
DUB Family Classification
Structural Features and Catalytic Mechanisms
Cysteine Protease DUBs
The cysteine protease DUBs constitute approximately 90% of all deubiquitinating enzymes and share a common catalytic mechanism centered on a nucleophilic cysteine residue [9] [10]. These enzymes employ catalytic dyads or triads (typically cysteine, histidine, and aspartate or asparagine) to facilitate hydrolysis of the isopeptide bond between ubiquitin and substrate proteins [9]. The histidine residue acts as a base to polarize the cysteine residue, lowering its pKa and enhancing its nucleophilicity for attack on the carbonyl carbon of the scissile bond [9]. This mechanism renders cysteine protease DUBs particularly sensitive to oxidative inactivation, as reactive oxygen species can directly modify the catalytic cysteine, providing a regulatory link between cellular redox state and ubiquitin signaling [10].
JAMM Metalloprotease DUBs
The JAMM family represents the only metalloprotease DUBs, characterized by a catalytic JAMM motif (ExnHxHx7Sx2D) that coordinates a Zn²⁺ ion to activate a water molecule for nucleophilic attack on the isopeptide bond [9] [13]. Unlike cysteine proteases, JAMM metalloproteases are not susceptible to oxidative inactivation of their catalytic site, making them attractive therapeutic targets with distinct pharmacological properties [13]. Structural studies reveal that most JAMM proteins contain two unique insertions (Ins-1 and Ins-2) that facilitate substrate recognition and binding [13]. The Ins-1 segment undergoes conformational transitions between inactive and active states, functioning as a regulatory gate that controls access to the catalytic site [13].
DUB Catalytic Mechanisms
DUB Functions in Cancer Biology and Signaling Pathways
Dysregulation of DUB activity contributes to oncogenesis through multiple mechanisms, including stabilization of oncoproteins, inactivation of tumor suppressors, and modulation of cancer-relevant signaling pathways. The tables below highlight specific DUBs with established roles in cancer progression.
Table 3: Oncogenic DUBs and Their Mechanisms in Cancer
| DUB | Family | Cancer Type | Substrate/Mechanism | Biological Outcome |
|---|---|---|---|---|
| USP28 | USP | Colon, lung, PDAC | Stabilizes c-Myc, Notch1, ΔNp63, FOXM1 [9] [4] | Promotes proliferation, chemoresistance, cell cycle progression |
| USP9X | USP | Pancreatic cancer | Context-dependent: regulates Hippo pathway, LATS kinase, YAP/TAZ [4] | Tumor promoter or suppressor depending on context |
| USP22 | USP | Pancreatic cancer | Modulates PTEN-MDM2-p53 axis; stabilizes DYRK1A [4] | Cancer stem cell marker; promotes proliferation |
| USP10 | USP | PDAC | Deubiquitinates YAP1; upregulates PD-L1 and galectin-9 [14] | Immune evasion; desensitizes to NK cell killing |
| Ataxin-3 | MJD | Gastric, lung, breast | Regulates PI3K/Akt, Hippo/YAP pathways; modulates p53 [12] | Promotes proliferation, metastasis, poor prognosis |
| BAP1 | UCH | Mesothelioma, melanoma, renal carcinoma | Deubiquitinates H2A; frequently mutated in cancers [4] | Tumor suppressor; "BAP1 cancer syndrome" |
| OTUD5 | OTU | Triple-negative breast cancer | Stabilizes YAP1; upregulates M2-related cytokines [14] | Promotes M2 macrophage polarization and metastasis |
| CSN5 | JAMM | Multiple | Deubiquitinates PD-L1 [14] | Immune evasion; inhibits NK cell function |
Table 4: Tumor Suppressor DUBs and Their Mechanisms
| DUB | Family | Cancer Type | Substrate/Mechanism | Biological Outcome |
|---|---|---|---|---|
| CYLD | USP | Cylindromatosis, hepatocellular carcinoma | Deubiquitinates TRAF2/6, NEMO; inhibits NF-κB pathway [11] | Familial tumor suppressor; NF-κB pathway negative regulation |
| BAP1 | UCH | Renal tumorigenesis, various cancers | Deubiquitinates H2A; chromatin remodeling [11] | Tumor suppressor; frequently mutated in cancers |
| USP9X | USP | Pancreatic cancer | Regulates Hippo pathway; cooperates with LATS kinase [4] | Suppresses tumor growth in specific contexts |
DUB Dysregulation in Cancer Pathways
Experimental Approaches for DUB Research
Activity-Based Protein Profiling (ABPP)
Activity-based protein profiling represents a powerful chemoproteomic approach for identifying active DUBs in complex biological systems and assessing inhibitor engagement [15]. This methodology utilizes reactive covalent probes that target the catalytic cysteine of cysteine protease DUBs, enabling quantitative assessment of DUB activity states and inhibition profiles in cell lysates and live cells [15].
Protocol Summary:
- Design and synthesis of a bespoke covalent library targeting the catalytic cysteine
- Primary screening in cell lysates using activity-based protein profiling with mass spectrometry readout
- Hit validation through biochemistry assays, intact protein mass spectrometry, and cysteine profiling
- Target engagement assessment in live cells to confirm cellular activity [15]
DUB Inhibitor Development Strategies
The development of selective DUB inhibitors has evolved significantly, moving from non-selective compounds to highly specific chemical probes. Current approaches emphasize structure-guided diversification combined with high-content chemoproteomic screening to simultaneously identify hits and drive structure-activity relationship (SAR) analysis against challenging DUB targets [15].
Key Methodological Considerations:
- Covalent vs. non-covalent strategies: Covalent libraries target the catalytic cysteine, while non-covalent approaches may offer alternative selectivity profiles
- Selectivity profiling: Comprehensive assessment against multiple DUB families to minimize off-target effects
- Cellular target engagement: Validation of inhibitor binding and functional effects in physiologically relevant systems
Research Reagent Solutions for DUB Studies
Table 5: Essential Research Tools for DUB Investigation
| Reagent Category | Specific Examples | Key Applications | Technical Considerations |
|---|---|---|---|
| Activity-Based Probes | Ubiquitin-based covalent probes; HA-Ub-VS | DUB activity profiling; identification of active DUBs [15] | Target catalytic cysteine; require mass spectrometry detection |
| Selective Inhibitors | b-AP15 (USP14/UCHL5); HBX41108 (USP7); WP1130 (USP9X) [12] | Functional validation; therapeutic potential assessment | Varying selectivity profiles; require careful control experiments |
| Genetic Tools | CRISPR/Cas9 knockout libraries; siRNA/shRNA collections | Target identification; functional screening | Context-dependent effects; potential compensation mechanisms |
| Ubiquitin Linkage-Specific Reagents | K48- vs K63-linked ubiquitin chains; linkage-specific antibodies | DUB specificity profiling; substrate characterization | Define linkage preference; inform biological function |
| Mass Spectrometry Platforms | Quantitative proteomics; ubiquitin remnant profiling | Global ubiquitome analysis; substrate identification | Complex data analysis; specialized computational tools |
| Cellular Assay Systems | Reporter cell lines; patient-derived organoids | Physiological relevance; translational potential | Model system limitations; microenvironment considerations |
Therapeutic Targeting of DUBs in Cancer
The strategic targeting of dysregulated DUBs represents an emerging frontier in cancer therapeutics, with several approaches showing promising preclinical results. The development of DUB inhibitors has gained significant momentum, with compounds targeting specific DUB families advancing toward clinical evaluation.
JAMM Family Targeting
The JAMM metalloproteases present particularly attractive drug targets due to their distinct catalytic mechanism and smaller family size compared to cysteine protease DUBs [13]. Several JAMM inhibitors have demonstrated promising therapeutic efficacy in preclinical models:
- BRCC36 inhibitors: Target DNA damage repair pathways in cancer cells
- CSN5 inhibitors: Modulate PD-L1 stability and immune checkpoint regulation
- Rpn11 inhibitors: Disrupt proteasome function and protein homeostasis [13]
Cysteine Protease DUB Inhibitors
The cysteine protease DUBs represent the majority of therapeutic targets, with several advanced compounds:
- USP7 inhibitors (HBX41108, P22077): Under investigation for neuroblastoma, acute leukemia
- USP14/UCHL5 inhibitors (b-AP15, VLX1570): Evaluated in multiple myeloma models
- USP9X inhibitors (WP1130): Tested in colorectal, lung, and prostate cancers [12]
The future clinical application of DUB inhibitors will likely involve combination strategies with existing modalities, particularly immune checkpoint blockade, where DUB inhibition can modulate the tumor microenvironment and enhance antitumor immunity [14].
The systematic classification of deubiquitinating enzymes into distinct families provides an essential framework for understanding their diverse functions in cellular homeostasis and cancer pathogenesis. The structural and mechanistic differences between cysteine protease and metalloprotease DUB families present unique opportunities for targeted therapeutic intervention. As research continues to elucidate the complex roles of specific DUBs in oncogenic signaling, immune evasion, and therapeutic resistance, the strategic targeting of these enzymes holds significant promise for advancing cancer treatment. The ongoing development of selective chemical probes and inhibitors, coupled with sophisticated screening methodologies, continues to accelerate this rapidly evolving field, positioning DUBs as compelling targets for next-generation cancer therapeutics.
The ubiquitin-proteasome system (UPS) serves as a critical regulatory mechanism for protein homeostasis in eukaryotic cells, governing the degradation of proteins and influencing virtually every cellular process [16] [17]. Ubiquitination involves the covalent attachment of a small 76-amino acid protein, ubiquitin, to target proteins via a sequential enzymatic cascade involving E1 (activating), E2 (conjugating), and E3 (ligating) enzymes [18] [19]. This process can mark proteins for degradation by the 26S proteasome or alter their function, activity, and localization through non-proteolytic mechanisms [19]. The reversibility of this modification is equally crucial, achieved through a specialized group of proteases known as deubiquitinating enzymes (DUBs) [18] [16].
DUBs counterbalance the action of E3 ubiquitin ligases by cleaving the isopeptide bond between ubiquitin and substrate proteins or between ubiquitin molecules within a polyubiquitin chain [17]. In humans, approximately 100 DUBs have been identified, categorized into seven subfamilies based on sequence and domain conservation [14] [16]. These enzymes are pivotal regulators in numerous biological processes, and their dysregulation is frequently associated with pathological conditions, most notably cancer [16] [20]. This review provides an in-depth technical analysis of the biochemical mechanisms by which DUBs reverse ubiquitination and dictate protein fate, with a specific focus on their implications in oncogenesis and cancer therapy.
DUB Classification and Biochemical Mechanisms
Major DUB Families and Their Characteristics
Deubiquitinating enzymes are classified into two major classes based on their catalytic mechanism: cysteine proteases and metalloproteases. The vast majority of DUBs are cysteine proteases, which include six subfamilies. The JAMM/MPN domain-associated metallopeptidases (JAMMs) constitute the only metalloprotease family [14].
Table 1: Major Deubiquitinating Enzyme (DUB) Families and Characteristics
| DUB Family | Catalytic Type | Number of Members | Representative Members | Key Characteristics |
|---|---|---|---|---|
| USPs (Ubiquitin-Specific Proteases) | Cysteine Protease | ~54 | USP28, USP21, USP34, USP9X, USP22 | Largest DUB family; diverse substrate recognition; involved in multiple cancer-associated processes [18] [16] |
| OTUs (Ovarian Tumor Proteases) | Cysteine Protease | ~16 | OTUD5, OTUB2 | Often exhibit linkage specificity for particular ubiquitin chain types [21] [16] |
| UCHs (Ubiquitin C-Terminal Hydrolases) | Cysteine Protease | ~4 | BAP1, UCHL1 | Primarily involved in processing ubiquitin precursors and cleaving small adducts [16] |
| MJDs (Machado-Josephin Domain-containing Proteases) | Cysteine Protease | ~4 | ATXN3, MJD | Josephin domain-containing proteases [18] [16] |
| MINDYs (Motif-Interacting with Ubiquitin-containing Novel DUB Family) | Cysteine Protease | ~4 | MINDY1, MINDY2 | Preferentially cleave K48-linked polyubiquitin chains [18] [16] |
| JAMMs (JAB1/MPN/MOV34 Metalloenzymes) | Metalloprotease | ~5 | POH1, BRCC36 | Zinc-dependent metalloproteases; often part of multi-protein complexes [18] [14] [16] |
Core Biochemical Functions of DUBs
DUBs execute four primary biochemical functions that maintain ubiquitin homeostasis and regulate protein fate [17]:
- Processing of Ubiquitin Precursors: Ubiquitin is transcribed as linear fusion polymers (e.g., polyubiquitin or fused to ribosomal proteins). DUBs hydrolyze these precursors to generate mature, biologically active free ubiquitin monomers, which are essential for initiating the ubiquitination cascade [21] [17].
- Reversal of Protein Ubiquitination: This is the most recognized function, wherein DUBs completely remove ubiquitin chains from modified protein substrates. This activity can rescue proteins from proteasomal degradation, thereby stabilizing them and altering their abundance within the cell [16] [17]. For instance, USP28 stabilizes the transcription factor FOXM1 by deubiquitinating it, promoting cell cycle progression in pancreatic ductal adenocarcinoma (PDAC) [18].
- Chain Editing and Trimming: DUBs can selectively cleave polyubiquitin chains at specific positions or linkages, thereby editing the topology of the ubiquitin signal. This can alter the fate of the substrate—for example, converting a K48-linked chain (typically degradative) into a K63-linked chain (typically signaling) [21] [16].
- Ubiquitin Recycling: During proteasomal degradation, DUBs associated with the 19S regulatory particle (e.g., USP14, UCHL5, and POH1) disassemble polyubiquitin chains from substrates being degraded, ensuring the recycling of ubiquitin to maintain a sufficient cellular pool of free ubiquitin [21] [17].
The following diagram illustrates the central role of DUBs in maintaining the ubiquitin cycle and regulating protein fate.
Diagram Title: The Ubiquitin Cycle and DUB Intervention Points.
Regulation of Protein Fate by DUBs in Cancer
DUBs govern critical aspects of cellular function by determining the stability, activity, and localization of key regulatory proteins. In cancer, the dysregulation of these processes drives tumorigenesis and disease progression.
Stabilization of Oncoproteins and Transcription Factors
A primary oncogenic mechanism of DUBs is the stabilization of proteins that promote cell growth and survival. This is achieved by removing degradative ubiquitin chains, thereby increasing the half-life of these oncogenic factors.
- Proliferation and Cell Cycle Regulation: In pancreatic ductal adenocarcinoma (PDAC), USP28 stabilizes the transcription factor FOXM1, which activates the Wnt/β-catenin pathway to drive cell cycle progression and inhibit apoptosis [18]. Similarly, USP5 stabilizes FOXM1 to accelerate PDAC tumor growth and also regulates DNA damage response and apoptosis [18].
- Transcription Factor Stability: The regulation of transcription factors (TFs) by DUBs is a key mechanism in drug resistance. As directly targeting TFs with small molecules is challenging, inhibiting their stabilizing DUBs presents an attractive therapeutic strategy [20]. For example, USP15 negatively regulates the Nrf2-mediated antioxidant response by deubiquitinating its inhibitor, Keap1 [20].
Table 2: Selected DUBs and Their Key Substrates in Cancer
| DUB | Cancer Type | Key Substrate(s) | Biological Outcome | Reference |
|---|---|---|---|---|
| USP28 | Pancreatic Ductal Adenocarcinoma | FOXM1 | Promotes cell cycle progression, inhibits apoptosis | [18] |
| USP21 | Pancreatic Ductal Adenocarcinoma | TCF7, MAPK3 | Maintains stemness, activates mTOR signaling | [18] |
| USP10 | Pancreatic Ductal Adenocarcinoma | YAP1 | Upregulates PD-L1 and Gal-9, desensitizes to NK cells | [14] |
| OTUB2 | Colorectal Cancer | PKM2 | Enhances glycolysis, accelerates cancer progression | [19] |
| USP7 | Glioblastoma | p53, PLK1 | Regulates cell cycle, DNA damage response, and apoptosis | [20] |
| USP22 | Various Cancers | PTEN, DYRK1A, Histones | Promotes proliferation, regulates epigenetics | [18] [21] |
| BAP1 | Mesothelioma, Melanoma | Histones (H2A) | Tumor suppressor; frequently mutated | [18] |
Modulation of the Tumor Microenvironment and Immune Evasion
Emerging research highlights the critical role of DUBs in shaping the tumor microenvironment (TME) to foster immune evasion, a key hallmark of cancer. DUBs expressed in either tumor cells or infiltrating immune cells can suppress anti-tumor immunity [14].
- Regulation of Immune Checkpoints: DUBs directly regulate the stability of immune checkpoint proteins. USP10 in PDAC cells deubiquitinates and stabilizes YAP1, which transcriptionally upregulates PD-L1 and Galectin-9, leading to impaired Natural Killer (NK) cell function and immune tolerance [14]. Furthermore, USP2 can stabilize PD-1 on T cells, promoting T-cell exhaustion and tumor immune escape [19].
- Control of Immune Cell Infiltration and Polarization: DUBs influence the recruitment and function of immune cells within the TME. For instance, macrophage-intrinsic OTUD5 deubiquitinates and stabilizes YAP1, driving M2 polarization (an immunosuppressive phenotype) of tumor-associated macrophages (TAMs) and promoting metastasis in triple-negative breast cancer (TNBC) [14]. Similarly, USP22 has been shown to suppress NK cell infiltration in pancreatic cancer by altering the tumor cell transcriptome [14].
The diagram below summarizes how DUBs in different cellular compartments of the tumor microenvironment contribute to immune evasion.
Diagram Title: DUB-Mediated Mechanisms of Immune Evasion in the TME.
Experimental Approaches for Studying DUB Function
Investigating the specific functions and substrates of DUBs requires a combination of molecular, cellular, and biochemical techniques. Below is a detailed protocol for a foundational experiment to identify and validate DUB-substrate relationships.
Detailed Protocol: Identifying and Validating a DUB-Substrate Interaction
Objective: To determine whether a candidate DUB (e.g., USP10) directly binds to and deubiquitinates a protein of interest (POI, e.g., YAP1), thereby regulating its stability.
Key Reagents and Materials:
- Plasmids: Expression vectors for wild-type (WT) and catalytically inactive (C/S) mutant of the DUB, the POI, and epitope-tagged ubiquitin (e.g., HA-Ub, Myc-Ub).
- Cell Lines: Relevant cancer cell lines (e.g., PANC-1 or AsPC-1 for PDAC studies).
- Transfection Reagent: Lipofectamine 3000 or polyethylenimine (PEI).
- Lysis Buffer: RIPA buffer supplemented with protease inhibitors (e.g., PMSF, aprotinin) and deubiquitinase inhibitors (e.g., N-Ethylmaleimide (NEM) or PR-619) to preserve ubiquitination states.
- Antibodies: Antibodies against the DUB, the POI, the ubiquitin tag (e.g., anti-HA), and relevant control antibodies for immunoprecipitation (IP) and western blotting (WB).
- Proteasome Inhibitor: MG-132 to block protein degradation and accumulate ubiquitinated species.
Methodology:
Step 1: Co-Immunoprecipitation (Co-IP) to Assess Binding
- Transfection: Co-transfect cells with plasmids expressing the DUB (WT or C/S) and the POI.
- Cell Lysis: Harvest cells after 24-48 hours using a mild lysis buffer (without SDS) to preserve protein-protein interactions.
- Immunoprecipitation: Incubate the cell lysate with an antibody against the POI (or the DUB) and Protein A/G beads. Use a non-specific IgG as a negative control.
- Washing and Elution: Wash beads extensively with lysis buffer to remove non-specifically bound proteins. Elute bound proteins with SDS sample buffer.
- Western Blot Analysis: Resolve eluted proteins by SDS-PAGE and perform western blotting. Probe the membrane with an antibody against the DUB to confirm interaction. Expected Outcome: The DUB should be detected in the POI immunoprecipitate, indicating a physical interaction.
Step 2: Deubiquitination Assay to Assess Functional Outcome
- Induce Ubiquitination: Co-transfect cells with plasmids for the POI, HA-tagged ubiquitin, and either the DUB (WT or C/S) or an empty vector control.
- Inhibit Degradation: Treat cells with MG-132 (e.g., 10 µM) for 4-6 hours before harvesting to enrich for ubiquitinated forms of the POI.
- Immunoprecipitation: Lyse cells in RIPA buffer with NEM. Immunoprecipitate the POI.
- Detection of Ubiquitination: Analyze the immunoprecipitates by western blotting using an anti-HA antibody to detect ubiquitinated POI species, which appear as high-molecular-weight smears or ladders. Expected Outcome: Co-expression of the wild-type DUB, but not the catalytically inactive mutant, should reduce the intensity of the ubiquitin smear, indicating deubiquitination of the POI.
Step 3: Validation of Protein Stabilization
- DUB Modulation: Generate stable cell lines with DUB knockdown (shRNA) or overexpression.
- Cycloheximide Chase Assay: Treat cells with cycloheximide (CHX, e.g., 100 µg/mL) to inhibit new protein synthesis. Harvest cells at different time points (e.g., 0, 2, 4, 8 hours).
- Western Blotting: Analyze the levels of the POI and the DUB at each time point. Expected Outcome: DUB overexpression should slow the degradation of the POI (longer half-life), while DUB knockdown should accelerate it (shorter half-life).
The Scientist's Toolkit: Essential Reagents for DUB Research
Table 3: Key Research Reagents for Investigating DUB Function
| Reagent Category | Specific Examples | Function and Application |
|---|---|---|
| Chemical Inhibitors | PR-619 (pan-DUB inhibitor), P5091 (USP7 inhibitor), ML323 (USP1-UAF1 inhibitor), VLX1570 (USP14/UCHL5 inhibitor) | Tool compounds to acutely inhibit DUB activity in cells; used for target validation and functional studies [20] [17]. |
| Activated Ubiquitin Probes | HA-Ub-VS, TAMRA-Ub-PA | Cell-active, mechanism-based probes that covalently label the active site of a subset of DUBs; used for profiling DUB activity and engagement by inhibitors [17]. |
| Expression Plasmids | Plasmids for WT and Catalytic Mutant (C>S) DUBs, Epitope-tagged Ubiquitin (HA-Ub, Myc-Ub, FLAG-Ub) | Essential for overexpression, interaction, and deubiquitination assays. Catalytic mutants serve as critical negative controls. |
| siRNA/shRNA | ON-TARGETplus siRNA SMARTpools, Lentiviral shRNA constructs | For targeted knockdown of DUB gene expression to study loss-of-function phenotypes and substrate stabilization. |
| DUB Inhibitor Cocktails | N-Ethylmaleimide (NEM), Iodoacetamide | Added to cell lysis buffers to inhibit endogenous DUB activity during protein extraction, thereby preserving the native ubiquitination state of proteins. |
| Proteasome Inhibitors | MG-132, Bortezomib, Carfilzomib | Used in deubiquitination assays to block the degradation of ubiquitinated proteins, allowing for their accumulation and detection. |
Therapeutic Targeting of DUBs in Cancer
The critical roles of DUBs in oncogenesis and drug resistance make them attractive targets for cancer therapy. The development of DUB inhibitors (DUBi) is a rapidly advancing field with several compounds in preclinical and clinical development [20] [17].
Strategies for DUB Inhibition
- Small Molecule Inhibitors: These compounds are designed to bind the catalytic pocket of DUBs, competitively inhibiting their activity. For example, VLX1570, an inhibitor of USP14 and UCHL5, advanced to clinical trials for multiple myeloma but was halted due to toxicity concerns [17]. KSQ-4279 is a USP1 inhibitor currently in clinical trials [20].
- Combination Therapies: A promising approach is combining DUBi with existing therapies to overcome drug resistance. For instance, inhibiting USP9X can enhance the efficacy of EGFR tyrosine kinase inhibitors in non-small cell lung cancer (NSCLC) by preventing the stabilization of anti-apoptotic proteins like MCL-1 [20].
Challenges and Future Perspectives
Despite the promise, developing specific DUB inhibitors faces challenges. The catalytic sites of many DUBs, particularly USPs, are shallow and highly conserved, making it difficult to design highly selective inhibitors. Future efforts will focus on developing allosteric inhibitors or proteolysis-targeting chimeras (PROTACs) that degrade DUBs rather than just inhibit their enzymatic activity. Furthermore, understanding the complex biology and context-dependent roles of DUBs, such as the dual function of USP9X as both an oncogene and tumor suppressor in different cancers, is crucial for designing effective and safe therapeutic strategies [18] [20].
Deubiquitinating enzymes are master regulators of cellular signaling, exerting precise control over protein fate by reversing ubiquitination. Through their ability to stabilize oncoproteins, modulate transcription factors, and reshape the tumor immune microenvironment, DUBs play indispensable roles in cancer initiation, progression, and therapeutic resistance. A deep and mechanistic understanding of how DUBs recognize their specific substrates and execute their deubiquitinating functions provides the foundational knowledge required to translate these insights into novel cancer therapeutics. The continued development of sophisticated experimental tools and highly specific inhibitors will be paramount in targeting the DUB family for next-generation anti-cancer strategies.
Deubiquitinating enzymes (DUBs) represent a critical component of the ubiquitin-proteasome system, comprising approximately 100 proteases that specifically cleave ubiquitin from modified substrate proteins [22] [23]. This deubiquitination process functions as a dynamic reversal mechanism that regulates protein stability, localization, and activity, thereby influencing virtually all cellular processes [24] [25]. The dysregulation of DUB activity emerges as a fundamental characteristic in numerous cancers, where these enzymes modulate core hallmarks of tumorigenesis through stabilization of oncoproteins, disruption of tumor suppressor pathways, and alteration of DNA repair fidelity [22] [19]. DUBs are classified into seven distinct families based on their ubiquitin-protease domains: ubiquitin-specific proteases (USPs), ovarian tumor proteases (OTUs), ubiquitin C-terminal hydrolases (UCHs), Machado-Joseph disease proteases (MJDs), JAB1/MPN/MOV34 metalloenzymes (JAMMs), motif interacting with ubiquitin-containing novel DUB family (MINDY), and zinc-finger and UFSP domain protein (ZUFSP) [22] [24]. Understanding the mechanistic roles of specific DUBs in proliferation, apoptosis evasion, and DNA damage response provides not only crucial insights into cancer biology but also reveals promising therapeutic targets for innovative cancer treatment strategies.
DUBs and Uncontrolled Proliferation
Regulation of Cell Cycle and Growth Signaling
DUBs control tumor cell proliferation primarily through direct regulation of cell cycle components and central growth signaling pathways. They ensure the precise stability of cyclins, cyclin-dependent kinases (CDKs), and transcription factors that drive cell division, often overriding checkpoint controls [22] [24].
USP17 demonstrates high expression in colon, esophageal, and cervical cancers, where it facilitates the G1-S transition by deubiquitinating and destabilizing the CDK inhibitor p21, thereby removing a critical barrier to cell cycle progression [22]. Simultaneously, USP17 stabilizes the transcription factor ELK-1, further promoting proliferation [22]. OTUD6B-2, operating downstream of mTORC1 signaling in non-small cell lung cancer (NSCLC), stabilizes both cyclin D1 and c-Myc, two fundamental drivers of G1 phase progression [22]. USP22, identified as a cancer stem cell marker, enhances breast cancer growth by stabilizing c-Myc and cyclin D1, thereby accelerating the G1-S transition [26]. USP14, frequently elevated in breast cancer tissues, controls cell cycle progression by deubiquitinating CyclinB1, regulating G2-M phase transition, with its knockdown inducing G2/M arrest [26].
Table 1: DUBs Regulating Cell Cycle Progression
| DUB | Phase Regulated | Key Substrate(s) | Cancer Context | Functional Outcome |
|---|---|---|---|---|
| USP17 | G1-S transition | p21, ELK-1 | Colon, esophageal, cervical cancers | Depletes p21, stabilizes ELK-1 |
| OTUD6B-2 | G1 phase | Cyclin D1, c-Myc | Non-small cell lung cancer | Promotes G1 progression |
| USP22 | G1-S transition | c-Myc, Cyclin D1 | Breast cancer | Enhances cyclin stability |
| USP14 | G2-M transition | CyclinB1 | Breast cancer | Regulates mitotic entry |
| DUB3 | S/G2 transition | Cyclin A | Various cancers | Controls S/G2 progression |
| USP7 | Mitotic phase | PHF8 | Various cancers | Regulates mitotic progression |
Stabilization of Oncogenic Signaling Pathways
Beyond direct cell cycle regulation, DUBs stabilize core oncogenic signaling pathways. The p53 tumor suppressor pathway represents a frequent target, with multiple DUBs acting either directly on p53 or through its primary negative regulator MDM2 [22] [24]. USP7 exemplifies this strategy across multiple cancers, where it deubiquitinates and stabilizes both MDM2 (the E3 ligase responsible for p53 degradation) and p53 itself, creating a complex regulatory circuit [22] [26]. In pancreatic ductal adenocarcinoma (PDAC), USP10 stabilizes p53, while USP28 promotes cell cycle progression and inhibits apoptosis by stabilizing FOXM1, subsequently activating the Wnt/β-catenin pathway [4]. USP21 further supports PDAC growth by interacting with and stabilizing TCF7 to maintain cancer stemness and activating mTOR signaling through binding to MAPK3 [4]. USP34 facilitates PANC-1 cell survival through AKT and PKC pathways, with its suppression markedly inhibiting tumor growth in mouse xenograft models [4].
The diagram below illustrates how DUBs coordinate proliferation signaling through multiple interconnected pathways:
DUBs in Apoptosis Evasion
Direct Regulation of Apoptotic Machinery
Cancer cells evade programmed cell death through multiple mechanisms orchestrated by DUBs, which directly target both core apoptotic components and regulatory pathways. The balance between pro-apoptotic and anti-apoptotic factors is frequently disrupted by DUB activity, providing survival advantages to tumor cells [22] [24].
JOSD1 promotes apoptosis resistance by specifically deubiquitinating and stabilizing the anti-apoptotic protein MCL1, a critical member of the BCL-2 family that prevents mitochondrial apoptosis [22]. USP9X enhances breast cancer cell survival through stabilization of the anti-apoptotic protein BCL2, while in pancreatic cancer contexts, it demonstrates both pro-survival and tumor-suppressive functions depending on specific cellular environments [4]. USP15 supports breast tumor-initiating cells by deubiquitinating and stabilizing BMI1, a cell cycle regulator and tumor growth promoter, downstream of IL1R2 signaling [26]. Conversely, OTUD3 exhibits tumor-suppressing activity in breast cancer by rescuing p53 from MDM2-mediated degradation, thereby activating cancer cell apoptosis, and also stabilizes PTEN by removing ubiquitin chains [26].
Table 2: DUBs in Apoptosis Evasion
| DUB | Apoptotic Role | Key Substrate(s) | Molecular Mechanism | Cancer Context |
|---|---|---|---|---|
| JOSD1 | Anti-apoptotic | MCL1 | Stabilizes anti-apoptotic BCL-2 family member | Various cancers |
| USP9X | Anti-apoptotic | BCL2 | Prevents mitochondrial apoptosis | Breast cancer, PDAC |
| USP15 | Anti-apoptotic | BMI1 | Stabilizes cell cycle regulator | Breast cancer |
| OTUD3 | Pro-apoptotic | p53, PTEN | Stabilizes tumor suppressors | Breast cancer |
| ATXN3 | Anti-apoptotic | p53 | Attenuates p53-mediated apoptosis | Various cancers |
| USP5 | Context-dependent | p53, MAF bZIP | Regulates apoptosis via p53 pathway | Various cancers |
Indirect Apoptosis Regulation Through Signaling Pathways
DUBs additionally modulate apoptotic thresholds through indirect mechanisms involving key cellular signaling pathways. CYLD, typically functioning as a tumor suppressor, is downregulated in hepatocellular carcinoma (HCC) tissues and cell lines [24]. Mouse models with liver-specific CYLD deletion demonstrate increased biliary injury, liver fibrosis, and susceptibility to diethylnitrosamine phenobarbital (DEN/PB)-induced liver tumor development [24]. The anti-apoptotic effects of CYLD loss involve increased infiltration of T cells and macrophages, along with elevated mRNA expression of inflammation-related genes via nuclear factor κB (NF-κB) signaling [24]. USP7 further contributes to apoptosis evasion in breast cancer through deubiquitination and stabilization of ERα, subsequently inhibiting cell cycle arrest and apoptosis in ERα+ breast cancer [26].
The coordinated regulation of apoptotic pathways by DUBs creates a formidable barrier to cell death, enabling cancer cell survival under diverse stress conditions. This mechanistic understanding reveals potential therapeutic vulnerabilities that could be exploited to re-sensitize tumor cells to apoptotic stimuli.
DUBs in DNA Damage Response
DUBs in DNA Repair Pathway Choice and Execution
The DNA damage response (DDR) represents a complex network of pathways that detect and repair DNA lesions, with DUBs emerging as critical regulators at multiple levels of this process [23] [27]. DUB activity ensures appropriate pathway choice, regulates repair protein stability and localization, and contributes to pathway termination once repair is complete.
In the Fanconi anemia (FA) pathway, which repairs DNA interstrand crosslinks, USP1 forms a complex with UAF1 to deubiquitinate the FANCD2-FANCI heterodimer [23]. This deubiquitination is required for proper FA pathway function, as USP1 depletion results in complete monoubiquitination of the cellular FANCD2 pool and deregulated recruitment to damage sites [23]. USP7 prevents degradation of RAD18 and Pol η, thereby supporting UV-induced PCNA monoubiquitination and subsequent recruitment of TLS polymerases to stalled replication forks [23]. For double-strand break repair, USP3 modulates histone H2A and γH2AX to influence DNA end resection, while USP11 regulates BRCA2 stability in homologous recombination [22] [23]. USP1 also regulates translesion synthesis by deubiquitinating monoubiquitinated PCNA, preventing excessive recruitment of TLS polymerases that could reduce replication fidelity [23].
Table 3: DUB Roles in DNA Damage Response Pathways
| DNA Repair Pathway | Key DUBs | DUB Substrates | Functional Impact |
|---|---|---|---|
| Fanconi Anemia (ICL Repair) | USP1 | FANCD2-FANCI complex | Maintains FANCD2 ubiquitination equilibrium |
| Translesion Synthesis | USP1, USP7 | PCNA, RAD18, Pol η | Regulates TLS polymerase recruitment |
| Homologous Recombination | USP11, USP3, USP7 | BRCA2, H2A/γH2AX, BRCA1 | Promotes error-free DSB repair |
| Non-Homologous End Joining | USP14, USP3 | H2A/γH2AX | Influences DSB repair pathway choice |
| Nucleotide Excision Repair | USP7, USP3 | RNA Polymerase II, H2A/γH2AX | Facilitates bulky lesion repair |
| Base Excision Repair | USP47, USP3 | DNA Polymerase β, H2A/γH2AX | Supports oxidative damage repair |
Methodologies for Studying DUB Roles in DNA Repair
Investigating DUB functions in DNA damage response requires specialized experimental approaches that capture the dynamic nature of repair processes. Standard methodologies include:
Co-immunoprecipitation (Co-IP) and Ubiquitination Assays: Cells are transfected with plasmids expressing the DUB of interest, along with ubiquitin. After treatment with DNA damaging agents (e.g., UV radiation, cisplatin, or ionizing radiation), proteins are immunoprecipitated with specific antibodies against potential substrates. Western blotting with anti-ubiquitin antibodies reveals changes in substrate ubiquitination status upon DUB expression or knockdown [23] [26].
Immunofluorescence and Foci Formation Analysis: Cells are treated with DNA damaging agents, fixed at various timepoints, and stained with antibodies against DNA repair proteins (e.g., γH2AX, RAD51, FANCD2) and the DUB of interest. High-resolution microscopy quantifies recruitment kinetics and co-localization at DNA damage sites, with USP1-UAF1 complex regulation of FANCD2 foci serving as a well-established example [23].
DNA Fiber Assay and Replication Dynamics: Cells are sequentially labeled with nucleotide analogs (e.g., CldU and IdU), followed by DNA damage induction. Spreading of DNA fibers on glass slides and immunostaining allows visualization of replication fork progression, stalling, and restart. This approach effectively demonstrates how USP1-mediated PCNA deubiquitination influences replication fork dynamics and translesion synthesis [23].
Clonogenic Survival Assays Post-DNA Damage: Cells with DUB knockdown or overexpression are treated with increasing doses of DNA damaging agents, then allowed to form colonies for 10-14 days. Survival curves quantify cellular sensitivity, establishing functional significance of DUB activity in DNA repair proficiency, as demonstrated in studies of USP11-deficient cells showing hypersensitivity to PARP inhibitors [23].
The diagram below illustrates the experimental workflow for characterizing DUB functions in DNA damage response:
The Scientist's Toolkit: Research Reagent Solutions
Table 4: Essential Research Reagents for DUB Investigation
| Reagent Category | Specific Examples | Research Application | Key Considerations |
|---|---|---|---|
| DUB Modulators | siRNAs, shRNAs, CRISPR-Cas9 constructs, DUB inhibitors (e.g., P5091 for USP7) | Functional studies of DUB knockdown/knockout or pharmacological inhibition | Select validated targeting sequences; verify specificity of inhibitors |
| Ubiquitin Probes | HA-Ub, FLAG-Ub, Tandem Ubiquitin Binding Entities (TUBEs) | Detection of protein ubiquitination status; pull-down of ubiquitinated proteins | TUBEs protect labile ubiquitin chains during purification |
| DNA Damage Inducers | Ionizing radiation, UV-C, Cisplatin, Mitomycin C, PARP inhibitors | Induce specific DNA lesions to study DUB roles in DDR | Optimize dose and timing for specific damage pathways |
| Repair Protein Antibodies | γH2AX (Ser139), RAD51, FANCD2, BRCA1, p53, PCNA | Immunofluorescence, Western blot, IP to monitor repair progression | Validate antibodies for specific applications (IF vs WB vs IP) |
| Live-Cell Imaging Reporters | GFP-tagged repair factors (e.g., 53BP1-GFP, RPA-GFP), FUCCI cell cycle indicators | Real-time tracking of repair protein recruitment and cell cycle progression | Optimize expression levels to avoid artifacts |
| Proteasome Inhibitors | MG132, Bortezomib, Carfilzomib | Stabilize ubiquitinated proteins for detection | Use appropriate controls to distinguish proteasomal effects |
DUBs occupy strategic positions in the regulation of core cancer hallmarks, functioning as crucial determinants of proliferation, apoptosis evasion, and DNA repair fidelity. Their ability to selectively stabilize key regulatory proteins places them as master regulators of tumorigenic processes, with different DUB families demonstrating both overlapping and unique substrate specificities. The mechanistic insights into DUB functions, as detailed in this review, highlight their potential as therapeutic targets, particularly through the development of selective small-molecule inhibitors. Future research directions should focus on elucidating the context-dependent functions of paradoxical DUBs like USP9X, understanding DUB cooperation in regulatory networks, and developing isoform-specific inhibitors to minimize therapeutic toxicity. As our knowledge of DUB biology expands, so too does the promise of targeting these enzymes for innovative cancer therapeutics that potentially overcome conventional resistance mechanisms.
The ubiquitin-proteasome system (UPS) represents a crucial regulatory mechanism for protein homeostasis, controlling the stability, localization, and activity of numerous cellular proteins [19]. As a reversible post-translational modification, ubiquitination is counterbalanced by deubiquitinating enzymes (DUBs), which remove ubiquitin chains from substrate proteins [11] [16]. The human genome encodes approximately 100 DUBs, categorized into six major families based on their catalytic domains: ubiquitin-specific proteases (USPs), ubiquitin C-terminal hydrolases (UCHs), ovarian tumor proteases (OTUs), Machado-Josephin domain-containing proteases (MJDs), motif-interacting with ubiquitin-containing novel DUB family (MINDYs), and JAB1/MPN/MOV34 metalloenzymes (JAMMs) [4] [11]. DUBs regulate diverse cellular processes including cell cycle progression, DNA damage repair, signal transduction, and metabolic reprogramming through four primary mechanisms: processing ubiquitin precursors, rescuing substrate proteins from degradation, cleaving polyubiquitin chains for ubiquitin recycling, and editing ubiquitin chains to alter signaling outcomes [16].
In cancer biology, DUBs demonstrate remarkable functional diversity, acting as either oncogenes or tumor suppressors in a context-dependent manner [28] [16]. This duality presents both challenges and opportunities for therapeutic targeting. The opposing functions of DUBs stem from their regulation of key cancer-associated pathways, with their impact varying based on cellular context, cancer type, genetic background, and tumor microenvironment [4] [28]. This review comprehensively examines the molecular mechanisms underlying the context-dependent functions of DUBs in cancer, providing experimental frameworks for their investigation, and discussing emerging therapeutic strategies targeting DUB activities.
Molecular Mechanisms of Context-Dependent DUB Functions
Tissue and Cellular Context Determinants
The specific function of a DUB—whether oncogenic or tumor-suppressive—is heavily influenced by tissue type, cellular compartmentalization, and expression patterns. For instance, USP9X demonstrates contrasting roles in different cancers. In pancreatic ductal adenocarcinoma (PDAC), USP9X can function as a tumor suppressor, as demonstrated by Sleeping Beauty transposon-mediated insertional mutagenesis screens that revealed high mutation frequencies in PDAC tumors [4]. This tumor-suppressive function involves regulation of the Hippo pathway through cooperation with LATS kinase and YAP/TAZ to impede PDAC growth [4]. Conversely, in other malignancies, USP9X promotes tumor cell survival and malignant phenotypes, highlighting its context-dependent functionality [4] [28].
The subcellular localization of DUBs, controlled by post-translational modifications such as phosphorylation and ubiquitination, significantly influences their substrate specificity and functional outcomes [16]. For example, phosphorylation of OTUB1 by casein kinase 2 facilitates its nuclear import, potentially altering its access to nuclear substrates, while AKT-mediated phosphorylation promotes nuclear export of USP4 [16]. Similarly, ubiquitination of BAP1 by UBE2O inhibits its nuclear translocation, a process reversible through auto-deubiquitination activity [16].
Genetic and Signaling Background
The genetic landscape of tumor cells profoundly influences DUB function, particularly in cancers driven by specific oncogenic mutations. In KRAS-driven pancreatic cancer (present in ~90% of PDAC cases), several DUBs interact with downstream signaling pathways to modulate tumor progression [4]. USP28 promotes cell cycle progression and inhibits apoptosis in PDAC cells by stabilizing FOXM1 to activate the Wnt/β-catenin pathway [4]. Similarly, USP21 interacts with and stabilizes TCF7 to maintain PDAC cell stemness, with orthotopic pancreatic transplantation models showing that USP21-expressing cells undergo pathological progression from PanIN to PDAC [4].
The regulation of RAS proteins by ubiquitination provides another compelling example of how DUB functions are integrated with oncogenic signaling. Recent research has revealed that ubiquitination dynamically regulates RAS protein stability, membrane localization, and signaling transduction, with distinct patterns across different RAS isoforms (KRAS4A, KRAS4B, NRAS, and HRAS) [29]. This heterogeneity suggests that DUBs targeting specific RAS isoforms may demonstrate context-dependent functions based on the predominant RAS mutation profile in different cancers.
Table 1: Context-Dependent Functions of Selected DUBs in Cancer
| DUB | Cancer Type | Oncogenic Function | Tumor-Suppressive Function | Molecular Mechanisms |
|---|---|---|---|---|
| USP9X | Pancreatic Cancer | Promotes tumor cell survival in human pancreatic tumor cells [4] | Suppresses tumor growth in KPC mouse models [4] | Regulates Hippo pathway via LATS kinase and YAP/TAZ [4] |
| BAP1 | Multiple Cancers | - | Frequently mutated in mesothelioma, melanoma, breast cancer [4] | Deubiquitinates H2A; mutations lead to "BAP1 cancer syndrome" [4] [11] |
| USP28 | Pancreatic Cancer | Promotes cell cycle progression, inhibits apoptosis [4] | - | Stabilizes FOXM1 to activate Wnt/β-catenin pathway [4] |
| CYLD | Various Cancers | - | Suppresses NF-κB and JNK pathways [11] | Deubiquitinates TRAF2/6, NEMO; familial tumor suppressor in cylindromatosis [11] |
| USP22 | Multiple Cancers | Promotes proliferation in PDAC; cancer stem cell marker [4] | - | Upregulates p21 via PTEN-MDM2-p53; increases DYRK1A levels [4] |
Substrate Specificity and Signaling Pathway Integration
The dual functions of DUBs frequently stem from their interactions with multiple substrates within competing signaling pathways. A single DUB may regulate both proliferative and suppressive pathways, with the net outcome determined by the relative dominance of these pathways in specific cellular contexts. USP7 exemplifies this principle through its regulation of both the oncogenic MDM2 and tumor-suppressive p53 [28]. By deubiquitinating and affecting the stability of both proteins, USP7 can either promote or suppress tumorigenesis depending on cellular context and interacting partners [28].
DUBs also demonstrate remarkable plasticity in response to therapeutic interventions. For example, USP1 undergoes self-processing and degradation upon UV radiation, representing an adaptive mechanism to DNA damage [16]. Similarly, the DUB OTUD5 exhibits phosphorylation-dependent catalytic activity enhancement through structural stabilization of its catalytic domain [16]. These regulatory mechanisms enable dynamic cellular responses to environmental stresses and contribute to the context-dependent functionality of DUBs in cancer progression and therapeutic resistance.
Experimental Approaches for DUB Functional Characterization
Genetic Screening and Validation Methods
Comprehensive genetic screening approaches have been instrumental in identifying context-dependent DUB functions. The Sleeping Beauty (SB) transposon-mediated insertional mutagenesis system has proven particularly valuable for uncovering DUBs that cooperate with specific oncogenic drivers. In one notable screen investigating KRASG12D-driven pancreatic cancer, USP9X emerged with the highest mutation frequency, observed in at least 50% of PDAC tumors, leading to its identification as a major tumor suppressor with high prognostic value in this context [4].
Protocol 1: Sleeping Beauty Transposon-Mediated Mutagenesis Screen for DUB Identification
- Transposon Construction: Generate a bidirectional transposon construct containing gene trap and polyA termination elements flanked by SB transposon inverted repeats.
- Mouse Model Generation: Cross SB transposon transgenic mice with appropriate Cre-driver lines (e.g., Pdx1-Cre for pancreatic cancer) and oncogene-bearing mice (e.g., KrasLSL-G12D).
- Tumor Monitoring: Monitor mice for tumor development over time, with typical PDAC formation requiring 6-12 months.
- DNA Extraction and Sequencing: Isolate genomic DNA from tumors and perform linker-mediated PCR amplification of transposon-genome junctions.
- Insertion Site Mapping: Map insertion sites to the reference genome and identify common insertion sites (CIS) using statistical algorithms (e.g., Gaussian Kernel Convolution).
- Validation: Validate candidate DUBs through immunohistochemistry of tumor tissues and functional assays in cell lines.
Mechanistic Investigation Techniques
Elucidating the molecular mechanisms underlying context-dependent DUB functions requires integrated experimental approaches encompassing biochemical, cellular, and in vivo methods. The following protocol outlines a comprehensive strategy for mechanistic DUB characterization:
Protocol 2: Comprehensive DUB Functional Characterization
- Substrate Identification:
- Perform co-immunoprecipitation followed by mass spectrometry (CoIP-MS) to identify DUB-interacting proteins.
- Conduct ubiquitin remnant profiling (UbiSite) to map specific deubiquitination sites on substrates.
- Implement phage display or protein microarrays for high-throughput substrate screening.
Functional Validation:
- Establish isogenic cell lines with DUB knockout (CRISPR-Cas9) or overexpression (lentiviral transduction).
- Assess phenotypic impacts using proliferation assays (MTT, CellTiter-Glo), colony formation, and invasion assays (Boyden chamber).
- Evaluate pathway modulation through Western blotting of key signaling components and qRT-PCR of target genes.
In Vivo Validation:
- Utilize xenograft models with DUB-modified cancer cells in immunocompromised mice.
- Employ genetically engineered mouse models (GEMMs) with tissue-specific DUB deletion or mutation.
- Monitor tumor growth, metastasis, and therapeutic responses using bioluminescent imaging and histopathological analysis.
Research Reagent Solutions for DUB Investigation
Table 2: Essential Research Reagents for DUB Functional Analysis
| Reagent Category | Specific Examples | Applications and Functions |
|---|---|---|
| Genetic Tools | Sleeping Beauty Transposon System [4] | Genome-wide mutagenesis screening for DUB identification |
| CRISPR-Cas9 Knockout Libraries | High-throughput functional screening of DUB families | |
| Tetracycline-inducible Expression Systems | Controlled DUB overexpression for functional studies | |
| Chemical Inhibitors | Auranofin (UCHL5/USP14 inhibitor) [11] | Proteasome-associated DUB inhibition; induces cytotoxicity |
| SIM0501 (USP1 inhibitor) [30] | FDA-approved for clinical trials in advanced solid tumors | |
| P5091 (USP7 inhibitor) | Targets MDM2-p53 pathway; induces apoptosis in cancer cells | |
| Analytical Tools | Tandem Ubiquitin Binding Entities (TUBEs) | Isolation of polyubiquitinated proteins for proteomics |
| Linkage-Specific Ubiquitin Antibodies (K48, K63, etc.) | Discrimination of ubiquitin chain topology in substrates | |
| Activity-Based Probes (HA-Ub-VS, HA-Ub-AMC) | Direct monitoring of DUB catalytic activity in cell lysates | |
| Model Systems | Patient-Derived Organoids (PDOs) | Physiological 3D culture models for DUB function studies |
| Genetically Engineered Mouse Models (GEMMs) [4] | In vivo validation of DUB roles in specific cancer contexts | |
| Orthotopic Transplantation Models [4] | Site-specific tumor growth and metastasis analysis |
Therapeutic Implications and Future Directions
Targeting Context-Dependent DUB Functions
The dual nature of DUBs as both oncogenes and tumor suppressors presents unique challenges for therapeutic development. Successful targeting strategies must consider the cellular context, including tissue type, genetic background, and tumor microenvironment. Several DUB-targeted agents have shown promise in preclinical models and early clinical trials. Auranofin, initially developed for rheumatoid arthritis, inhibits proteasome-associated DUBs UCHL5 and USP14, demonstrating selective tumor growth inhibition in vivo and inducing cytotoxicity in cancer cells from patients with acute myeloid leukemia [11]. Similarly, the small molecule inhibitor SIM0501, which targets USP1, has received FDA approval for clinical trials in advanced solid tumors [30].
Emerging research focuses on developing isoform-selective DUB inhibitors that minimize off-target effects. The structural characterization of DUB catalytic domains has enabled structure-based drug design approaches, yielding compounds with improved specificity and potency. Additionally, PROTAC (Proteolysis Targeting Chimera) technology offers an alternative strategy for targeting DUB functions by directing their ubiquitination and degradation, rather than merely inhibiting catalytic activity [19]. ARV-110 and ARV-471 represent pioneering PROTAC candidates that have progressed to phase II clinical trials for prostate and breast cancers, respectively [19].
Biomarker-Driven Patient Stratification
Given the context-dependent functions of DUBs, identifying robust biomarkers for patient stratification represents a critical component of therapeutic development. Comprehensive molecular profiling—including genomic, transcriptomic, and proteomic analyses—can help identify cancers most likely to respond to specific DUB-targeted therapies. For instance, tumors with specific KRAS mutations might exhibit heightened sensitivity to DUBs regulating RAS ubiquitination and membrane localization [29]. Similarly, cancers with dysregulated Wnt/β-catenin signaling may demonstrate increased dependence on DUBs such as USP28 and USP21 [4].
Functional imaging approaches, including positron emission tomography (PET) with novel DUB-targeted radiotracers, offer potential for non-invasive assessment of DUB expression and activity in tumors. Such techniques could enable real-time monitoring of therapeutic responses and guide treatment adaptation in clinical settings.
Future Research Directions
Several key questions remain unresolved in the field of context-dependent DUB functions. First, the precise molecular determinants that dictate whether a DUB acts as an oncogene or tumor suppressor in specific contexts require further elucidation. Second, the regulation of DUB activity by post-translational modifications and interacting partners needs comprehensive characterization across different cancer types. Third, the potential compensatory mechanisms among DUB family members upon targeted inhibition warrants systematic investigation.
Future research should prioritize the development of more sophisticated experimental models, including patient-derived organoids and humanized mouse models, that better recapitulate the tumor microenvironment and immune context. Additionally, advanced technologies such as single-cell sequencing, spatial transcriptomics, and live-cell imaging of DUB activities will provide unprecedented insights into the dynamic regulation of DUB functions in cancer progression and treatment response.
The integration of artificial intelligence and machine learning approaches for analyzing multi-omics datasets holds particular promise for predicting context-dependent DUB functions and identifying optimal therapeutic combinations. As these technologies mature, they will accelerate the development of personalized cancer therapies targeting the ubiquitin system.
Deubiquitinating enzymes represent master regulators of cellular signaling pathways with profound implications for cancer development and treatment. Their context-dependent functions as either oncogenes or tumor suppressors are dictated by a complex interplay of tissue specificity, genetic background, substrate availability, and microenvironmental influences. Understanding these nuanced relationships requires sophisticated experimental approaches that integrate genetic screening, mechanistic biochemistry, and validated disease models.
The continued elucidation of context-dependent DUB functions will undoubtedly yield novel therapeutic opportunities and biomarker strategies for precision oncology. As DUB-targeted agents progress through clinical development, careful attention to patient selection and combination therapies will be essential for maximizing therapeutic efficacy while minimizing unintended consequences. With rapid advances in structural biology, chemical proteomics, and functional genomics, the field is poised to translate fundamental discoveries about DUB biology into meaningful clinical benefits for cancer patients.
Deubiquitinating enzymes (DUBs) are critical regulators of cellular signaling pathways through their ability to cleave ubiquitin chains from substrate proteins. This technical review examines the mechanistic roles of DUBs in regulating three pivotal signaling pathways—p53, NF-κB, and Wnt/β-catenin—within the context of cancer research. We synthesize current understanding of how specific DUBs control the stability, localization, and activity of key components in these pathways, thereby influencing tumorigenesis, metastasis, and therapeutic resistance. The review also presents experimental frameworks for investigating DUB functions and discusses emerging therapeutic strategies targeting DUBs in cancer, providing researchers with both theoretical foundations and practical methodologies for advancing drug discovery in this field.
The ubiquitin-proteasome system (UPS) represents a crucial regulatory mechanism for protein degradation and functionality in eukaryotic cells. Within this system, deubiquitinating enzymes (DUBs) perform the reverse reaction of ubiquitination by specifically cleaving ubiquitin chains from substrate proteins, thereby modulating protein stability, activity, and interaction networks [31]. Approximately 100 DUBs have been identified in humans, classified into seven major families based on their catalytic domains: ubiquitin-specific proteases (USPs), ubiquitin carboxyl-terminal hydrolases (UCHs), ovarian tumor proteases (OTUs), Machado-Joseph disease proteases (MJDs), motif interacting with ubiquitin-containing novel DUB family (MINDY), JAMM/MPN domain-associated metallopeptidases (JAMMs), and zinc-finger containing ubiquitin peptidase 1 (ZUP1) [3].
Dysregulation of DUB activity is increasingly recognized as a contributing factor in cancer pathogenesis. DUBs govern fundamental cellular processes including cell cycle progression, apoptosis, DNA damage repair, and metabolic reprogramming by controlling the turnover of key regulatory proteins [4]. Through their substrate specificity, DUBs can function as either oncoproteins or tumor suppressors in a context-dependent manner. The balanced regulation of ubiquitination and deubiquitination is essential for maintaining cellular homeostasis, and disruption of this equilibrium can drive malignant transformation and tumor progression [30]. Consequently, DUBs have emerged as attractive therapeutic targets in cancer drug development, with several small-molecule inhibitors currently in preclinical and clinical evaluation [3].
The Wnt/β-Catenin Signaling Pathway
Pathway Mechanism and Biological Significance
The Wnt/β-catenin signaling pathway, also known as the canonical Wnt pathway, is an evolutionarily conserved signaling axis that regulates embryonic development, tissue homeostasis, cell proliferation, differentiation, and stem cell renewal [32]. In the absence of Wnt ligands, cytoplasmic β-catenin is recruited to a destruction complex comprising adenomatous polyposis coli (APC), Axin, casein kinase 1α (CK1α), and glycogen synthase kinase 3β (GSK3β). Within this complex, β-catenin undergoes sequential phosphorylation by CK1α and GSK3β, leading to its ubiquitination by β-TrCP E3 ligase and subsequent proteasomal degradation [33] [32].
Upon binding of Wnt ligands to Frizzled (FZD) receptors and LRP5/6 co-receptors, the destruction complex is disrupted through recruitment of Disheveled (DVL). This stabilization allows β-catenin to accumulate in the cytoplasm and translocate to the nucleus, where it partners with T-cell factor/lymphoid enhancer factor (TCF/LEF) transcription factors to activate expression of target genes including c-MYC, cyclin D1, and CDKN1A, which collectively promote cell proliferation and survival [33] [32].
Dysregulation of Wnt/β-catenin signaling is frequently observed in various cancers and contributes to tumor initiation, progression, metastasis, and therapy resistance [32]. Aberrant activation of this pathway can result from mutations in pathway components (e.g., APC, AXIN, or CTNNB1) or from altered expression of regulatory proteins, including DUBs that stabilize β-catenin and other core components.
Key Regulatory DUBs and Their Mechanisms
Table 1: DUBs Regulating the Wnt/β-Catenin Signaling Pathway
| DUB | Family | Molecular Target | Effect on Pathway | Cancer Context |
|---|---|---|---|---|
| USP4 | USP | β-catenin | Stabilizes β-catenin through deubiquitination | Colorectal cancer [34] |
| USP5 | USP | β-catenin | Removes ubiquitin chains from β-catenin | Breast cancer, Pancreatic cancer [4] [35] |
| USP9X | USP | Multiple components | Context-dependent regulation | Pancreatic cancer [4] |
| USP15 | USP | APC, DVL | Stabilizes destruction complex components | Various cancers [33] |
| USP21 | USP | TCF7 | Stabilizes TCF7 to maintain stemness | Pancreatic cancer [4] |
| USP28 | USP | FOXM1 | Stabilizes FOXM1 to activate Wnt pathway | Pancreatic cancer [4] |
| OTUD1 | OTU | Multiple substrates | Suppresses Wnt signaling | Breast cancer [31] |
Multiple DUBs regulate Wnt/β-catenin signaling through distinct mechanisms. USP4 directly binds to and deubiquitinates β-catenin, enhancing its stability and promoting nuclear translocation. Clinical evidence shows a positive correlation between USP4 and β-catenin expression levels in colorectal cancer tissues [34]. Similarly, USP5 mediates β-catenin deubiquitination in a DEPDC1B-dependent manner in breast cancer, facilitating metastasis through pathway activation [35]. In pancreatic ductal adenocarcinoma (PDAC), USP28 promotes cell cycle progression by stabilizing FOXM1, which subsequently activates the Wnt/β-catenin pathway [4].
The regulatory functions of DUBs can be context-dependent. USP9X demonstrates dual roles in pancreatic cancer, acting as either an oncogene or tumor suppressor depending on cellular context [4]. While USP9X promotes tumor cell survival in human pancreatic tumor cells, it functions as a tumor suppressor in KPC (KrasLSL-G12D/+; Trp53LSL-R172H/+; Pdx1-Cre) mouse-derived tumors, highlighting the complexity of DUB functions in different biological settings [4].
Experimental Approaches for Investigating DUB Regulation
Co-immunoprecipitation (Co-IP) and Ubiquitin Assays: To determine whether a DUB directly interacts with and deubiquitinates β-catenin, researchers can employ co-immunoprecipitation followed by ubiquitination assays. Cells are transfected with plasmids expressing the DUB of interest, β-catenin, and ubiquitin. After treatment with a proteasome inhibitor (e.g., MG132) to preserve ubiquitinated proteins, cell lysates are immunoprecipitated with β-catenin antibody. The interaction between DUB and β-catenin is confirmed by Western blotting, while deubiquitination activity is assessed by measuring ubiquitin signal intensity on β-catenin [34] [35].
Functional Assays for Pathway Activity: The transcriptional activity of Wnt/β-catenin signaling can be measured using TCF/LEF luciferase reporter assays (e.g., TOPFlash). Cells are co-transfected with the reporter construct and DUB expression vector or siRNA. Changes in luciferase activity indicate pathway modulation by the DUB. Additionally, subcellular localization of β-catenin can be visualized by immunofluorescence staining following DUB manipulation [35].
In Vivo Validation: Xenograft mouse models provide physiological relevance for DUB functions. Cancer cells with stable DUB knockdown or overexpression are implanted into immunodeficient mice. Tumor growth, metastasis, and molecular changes (e.g., β-catenin levels, target gene expression) are monitored to confirm the pathological significance of DUB-mediated pathway regulation [4] [35].
Figure 1: Wnt/β-catenin Signaling Pathway and DUB Regulation. Schematic representation of the canonical Wnt pathway in inactive (Wnt OFF) and active (Wnt ON) states, highlighting points of regulation by DUBs. In the absence of Wnt, β-catenin is targeted for proteasomal degradation. Wnt activation stabilizes β-catenin, allowing nuclear translocation and target gene transcription. DUBs regulate this pathway at multiple levels, primarily by stabilizing key components.
The p53 Tumor Suppressor Pathway
Pathway Mechanism and Biological Significance
The p53 tumor suppressor protein serves as a critical guardian of the genome, integrating diverse cellular stress signals to orchestrate appropriate responses including cell cycle arrest, DNA repair, senescence, and apoptosis. Under normal conditions, p53 is maintained at low levels primarily through MDM2-mediated ubiquitination and proteasomal degradation. Various stress signals, including DNA damage, oncogene activation, and oxidative stress, trigger p53 stabilization through post-translational modifications that disrupt its interaction with MDM2.
Once stabilized and activated, p53 functions as a sequence-specific transcription factor that regulates numerous target genes, including p21 (cell cycle arrest), PUMA and BAX (apoptosis), and GADD45 (DNA repair). The critical role of p53 in tumor prevention is evidenced by the high frequency of TP53 mutations in human cancers, which exceed 50% across all cancer types.
Key Regulatory DUBs and Their Mechanisms
Table 2: DUBs Regulating the p53 Signaling Pathway
| DUB | Family | Molecular Target | Effect on Pathway | Cancer Context |
|---|---|---|---|---|
| USP7 (HAUSP) | USP | p53, MDM2 | Dual role: stabilizes both p53 and MDM2 | Multiple cancers [3] |
| USP10 | USP | p53 | Deubiquitinates and stabilizes p53 | Various cancers [3] |
| OTUD1 | OTU | p53 | Cleaves K48-linked ubiquitin chains on p53 | Multiple cancers [31] |
| USP2a | USP | MDM2 | Stabilizes MDM2 to promote p53 degradation | Prostate cancer [3] |
| USP4 | USP | ARF | Stabilizes ARF to inhibit MDM2 | Various cancers [3] |
| USP11 | USP | p53 | Regulates p53-dependent apoptosis | Breast cancer [3] |
| USP24 | USP | p53 | Negatively regulates p53 stability | Lung cancer [3] |
DUBs regulate p53 signaling through diverse mechanisms, primarily by controlling the stability of p53 itself or its key regulators. USP7 (HAUSP) exemplifies the complexity of DUB functions, as it can deubiquitinate both p53 and its negative regulator MDM2. The net effect of USP7 inhibition depends on cellular context, with cancer cells often exhibiting dependence on USP7-mediated MDM2 stabilization, making USP7 an attractive therapeutic target [3].
USP10 stabilizes p53 by removing ubiquitin chains, particularly in the cytoplasm, and plays a role in DNA damage response. OTUD1 preferentially cleaves K48-linked ubiquitin chains from p53, thereby enhancing p53 stability and promoting apoptosis in response to cellular stress [31]. In contrast, USP2a functions as an oncogene by stabilizing MDM2 and promoting p53 degradation in prostate cancer [3].
The regulatory network connecting DUBs to p53 signaling continues to expand with the identification of novel DUB-p53 interactions, highlighting the importance of this regulatory layer in fine-tuning p53 activity in response to diverse cellular stimuli.
Experimental Approaches for Investigating DUB Regulation
p53 Stability and Half-life Studies: To assess DUB-mediated regulation of p53 stability, researchers can monitor p53 protein half-life using cycloheximide chase assays. Cells expressing or deficient in the DUB of interest are treated with cycloheximide to inhibit new protein synthesis, and p53 protein levels are measured by Western blotting at various time points. Extended half-life indicates stabilization by the DUB [31].
Apoptosis and Cell Cycle Analysis: The functional consequences of DUB-mediated p53 regulation can be evaluated by flow cytometry-based analysis of apoptosis (Annexin V staining) and cell cycle distribution (propidium iodide staining). Following DUB modulation and appropriate stress induction (e.g., DNA damage), changes in apoptotic populations and cell cycle profiles provide insights into p53 functional output [31].
Gene Expression Profiling: Transcriptional activity of p53 can be assessed by quantifying mRNA levels of canonical p53 target genes (e.g., p21, PUMA, BAX) using quantitative RT-PCR. Chromatin immunoprecipitation (ChIP) assays can further determine whether DUB expression affects p53 binding to specific target gene promoters [3].
Figure 2: p53 Signaling Pathway and DUB Regulation. The p53 pathway responds to cellular stress by stabilizing p53, which functions as a transcription factor for target genes governing cell fate decisions. DUBs regulate this pathway by directly deubiquitinating p53 or modulating its negative regulator MDM2, with different DUBs exerting stabilizing or destabilizing effects on p53.
The NF-κB Signaling Pathway
Pathway Mechanism and Biological Significance
The NF-κB (Nuclear Factor kappa-light-chain-enhancer of activated B cells) signaling pathway represents a critical mediator of immune and inflammatory responses, cell survival, and proliferation. In resting cells, NF-κB dimers (typically p50/p65) are sequestered in the cytoplasm through interaction with inhibitory IκB proteins. Two major NF-κB activation pathways have been characterized: the canonical and non-canonical pathways.
The canonical pathway is triggered by diverse stimuli including pro-inflammatory cytokines (e.g., TNF-α, IL-1), pathogen-associated molecular patterns, and antigen receptor engagement. These signals activate the IκB kinase (IKK) complex, leading to IκB phosphorylation, ubiquitination, and proteasomal degradation. This process releases NF-κB dimers to translocate to the nucleus and activate target genes involved in inflammation (e.g., cytokines, chemokines), anti-apoptosis (e.g., BCL-2, c-FLIP), and proliferation (e.g., cyclin D1).
Constitutive or aberrant NF-κB activation is a hallmark of many inflammatory diseases and cancers, where it promotes cell survival, proliferation, angiogenesis, and therapy resistance. Consequently, precise regulation of NF-κB signaling, including through DUB-mediated mechanisms, is crucial for maintaining immune homeostasis and preventing malignant transformation.
Key Regulatory DUBs and Their Mechanisms
While the search results provided limited specific details about NF-κB regulation by DUBs compared to the Wnt and p53 pathways, several DUB families have established roles in modulating NF-κB signaling based on general knowledge:
CYLD: A member of the USP family that negatively regulates NF-κB signaling by deubiquitinating key signaling molecules including TRAF2, TRAF6, and NEMO. CYLD removal of K63-linked ubiquitin chains from these proteins dampens NF-κB activation. CYLD mutations are associated with cylindromatosis, a condition characterized by multiple tumors of skin appendages.
A20 (TNFAIP3): An OTU family DUB that serves as a critical negative feedback regulator of NF-κB signaling. A20 deubiquitinates multiple NF-κB signaling components including RIP1, TRAF6, and NEMO, employing a unique dual mechanism that involves both deubiquitination (OTU domain) and E3 ubiquitin ligase activity (Zinc finger domains). Genetic studies have linked A20 polymorphisms to various autoimmune and inflammatory diseases.
USP11: Regulates NF-κB activity through deubiquitination of IκBα, preventing its degradation and thereby maintaining NF-κB in an inactive state. USP11 overexpression has been associated with impaired NF-κB activation in response to pro-inflammatory stimuli.
The development of selective DUB inhibitors targeting NF-κB regulators represents an active area of investigation for inflammatory diseases and cancers characterized by aberrant NF-κB activation.
Experimental Approaches for Investigating DUB Regulation
NF-κB Reporter Assays: The most direct method for assessing NF-κB transcriptional activity involves luciferase reporter constructs under the control of NF-κB response elements. Cells are co-transfected with the reporter and DUB expression vectors or siRNAs, followed by appropriate stimulation (e.g., TNF-α). Changes in luciferase activity indicate the DUB's effect on pathway activation.
Electrophoretic Mobility Shift Assay (EMSA): This technique assesses NF-κB DNA binding activity directly. Nuclear extracts from cells with DUB modulation are incubated with labeled oligonucleotides containing NF-κB binding sites. Protein-DNA complexes are resolved by non-denaturing gel electrophoresis, with supershift assays using specific antibodies confirming the identity of NF-κB subunits.
Subcellular Localization Studies: Immunofluorescence staining and cellular fractionation followed by Western blotting can visualize NF-κB translocation in response to stimulation. DUB effects on the kinetics and extent of NF-κB nuclear accumulation provide insights into their regulatory roles in the activation process.
Cross-Pathway Integration and Therapeutic Targeting
Network-Level Integration of DUB Functions
DUBs do not operate in isolation but rather function within interconnected signaling networks that enable cells to integrate diverse inputs and mount appropriate responses. Several DUBs demonstrate cross-pathway regulatory capabilities, simultaneously influencing multiple signaling axes. For instance, USP7 regulates both p53 and Wnt pathways through its effects on MDM2 and β-catenin, respectively, creating potential signaling nodes that could be exploited therapeutically [3].
The functional outcome of DUB activity is further modulated by post-translational modifications of the DUBs themselves. Recent evidence indicates that reactive oxygen species (ROS) can oxidize the catalytic cysteine residue in cysteine-dependent DUBs, leading to reversible inactivation. This redox regulation of DUB activity creates a feedback loop that links cellular metabolic status to signaling pathway output, particularly in the tumor microenvironment where oxidative stress is prevalent [36].
Therapeutic Targeting of DUBs in Cancer
The critical regulatory functions of DUBs in cancer-relevant signaling pathways have motivated extensive drug discovery efforts targeting DUB activities. Several strategic approaches have emerged:
Small-Molecule DUB Inhibitors: Targeted inhibition of specific DUBs represents the most direct therapeutic strategy. USP1 inhibitors show promise in preclinical models for overcoming cisplatin resistance in non-small cell lung cancer [3]. USP7 inhibitors have demonstrated efficacy in multiple myeloma models by inducing apoptosis and overcoming bortezomib resistance [3]. USP14 inhibitors promote degradation of oncoproteins and enhance proteasome activity, showing potential in various cancer models [3].
PROTAC and DUBTAC Technologies: Proteolysis-targeting chimeras (PROTACs) and deubiquitinase-targeting chimeras (DUBTACs) represent innovative approaches for targeted protein degradation or stabilization, respectively. These bifunctional molecules recruit either E3 ubiquitin ligases (PROTACs) or DUBs (DUBTACs) to specific target proteins, enabling precise manipulation of protein stability [3].
Combination Therapies: DUB inhibitors frequently exhibit synergistic effects when combined with conventional chemotherapeutics or targeted agents. For example, USP9X inhibition enhances the efficacy of FLT3 inhibitors in acute myeloid leukemia, while USP1 inhibition sensitizes cancer cells to DNA-damaging agents [3].
Table 3: Selected DUB Inhibitors in Preclinical and Clinical Development
| DUB Target | Inhibitor | Development Stage | Cancer Type | Primary Mechanism |
|---|---|---|---|---|
| USP1 | SIM0501 | FDA clinical approval (planned) | Advanced solid tumors | Overcomes chemoresistance [30] |
| USP7 | Multiple compounds | Preclinical/Clinical | Multiple myeloma, other cancers | Induces apoptosis, overcomes resistance [3] |
| USP14 | b-AP15 | Preclinical | Various cancers | Enhances proteasome activity [3] |
| USP2a | ML364 | Preclinical | Colorectal cancer | Accelerates cyclin D1 degradation [3] |
| USP5 | Multiple compounds | Preclinical | Breast cancer, pancreatic cancer | Inhibits β-catenin stabilization [3] |
The Scientist's Toolkit: Essential Research Reagents and Methodologies
Table 4: Essential Research Reagents for DUB and Signaling Pathway Studies
| Reagent Category | Specific Examples | Research Application | Key Considerations |
|---|---|---|---|
| Activity-Based Probes | Ubiquitin-rhodamine, HA-Ub-VS | DUB activity profiling, inhibitor screening | Covalently label active site cysteine; enable high-throughput screening [8] |
| DUB Modulators | siRNA/shRNA libraries, CRISPR-Cas9 systems, Expression vectors | Functional studies of specific DUBs | Both genetic and pharmacological tools needed for validation |
| Pathway Reporters | TOPFlash (Wnt), p53-responsive luciferase, NF-κB-responsive luciferase | Pathway activity measurement | Critical for functional assessment of DUB effects |
| Ubiquitination Assay Components | MG132 (proteasome inhibitor), HA-Ub or FLAG-Ub plasmids, NEM (DUB inhibitor) | Detection of protein ubiquitination status | Essential for confirming direct DUB substrates |
| Protein Interaction Tools | Co-immunoprecipitation antibodies, Proximity ligation assay reagents | Protein-protein interaction studies | Validate physical DUB-substrate relationships |
| Clinical Specimens | Tumor tissue microarrays, Patient-derived xenografts | Translational validation | Assess clinical relevance of findings |
Experimental Workflow for DUB-Pathway Research
Figure 3: Experimental Workflow for DUB-Pathway Research. A systematic approach for investigating DUB functions in signaling pathways, from initial target identification through preclinical validation.
DUBs have emerged as critical regulators of key signaling pathways implicated in cancer, including Wnt/β-catenin, p53, and NF-κB. Through their ability to modulate the stability, activity, and localization of core pathway components, DUBs fine-tune signaling outputs that govern cell fate decisions in both physiological and pathological contexts. The development of selective DUB inhibitors represents a promising therapeutic strategy, with several candidates advancing through preclinical and clinical evaluation.
Future research directions should focus on elucidating the context-dependent functions of DUBs, understanding their regulation by post-translational modifications, and developing more selective pharmacological tools. Additionally, exploring the potential of DUB-targeting agents in combination therapies and patient stratification approaches will be essential for realizing their full clinical potential. As our understanding of DUB biology continues to expand, so too will opportunities for innovative therapeutic interventions in cancer and other diseases characterized by signaling pathway dysregulation.
Targeting DUBs: From Research Tools to Therapeutic Development
Experimental Approaches for Studying DUB Function and Substrate Identification
Deubiquitinating enzymes (DUBs) represent a family of approximately 100 proteases that catalyze the removal of ubiquitin from target proteins, thereby reversing the process of ubiquitination [4] [37]. As essential components of the ubiquitin-proteasome system (UPS), DUBs regulate diverse cellular processes including protein stability, localization, activity, and complex formation [37]. The balance between ubiquitination and deubiquitination is crucial for maintaining cellular homeostasis, and disruption of this balance contributes significantly to human diseases, particularly cancer [4] [3].
In cancer biology, DUBs have emerged as promising therapeutic targets due to their role in regulating oncogenic and tumor-suppressive pathways [4] [3]. They modulate the stability of key proteins involved in cell proliferation, apoptosis, DNA damage repair, metabolic reprogramming, and chemotherapy resistance [4]. For instance, in pancreatic ductal adenocarcinoma (PDAC), multiple DUBs including USP28, USP21, and USP9x have been documented to drive tumor progression through stabilization of oncoproteins like FOXM1 and c-Myc, or through regulation of critical pathways such as Wnt/β-catenin and mTOR signaling [4]. The development of precise methodologies to identify DUB substrates and characterize DUB function is therefore paramount for advancing both basic cancer biology and therapeutic development.
Core Methodological Frameworks for DUB Investigation
Researchers employ multiple complementary methodologies to decipher DUB-substrate interactions and functional roles. Each approach offers unique advantages and addresses specific aspects of DUB biology, from substrate identification to functional validation in physiological contexts. The selection of appropriate methods depends on the specific research questions, available resources, and desired throughput.
Table 1: Core Methodologies for Studying DUB Function and Substrate Identification
| Method Category | Key Techniques | Primary Applications | Key Strengths | Inherent Limitations |
|---|---|---|---|---|
| Biochemical & In Vitro Assays | In vitro deubiquitination assays; Protein degradation rate analysis; Isotopic pulse-chase; Ubiquitin chain linkage specificity assays [37] | Validation of direct DUB-substrate relationships; Characterization of enzymatic kinetics and specificity [37] | Direct mechanistic insights; Controlled experimental conditions; Quantitative readouts | May lack physiological context; Limited representation of cellular complexity |
| Live-Cell & Fluorescence-Based Monitoring | Photoconvertible reporters; Fluorescent protein timers; FRET (Förster Resonance Energy Transfer) [37] | Real-time monitoring of substrate turnover and DUB activity in live cells; Spatial-temporal dynamics [37] | Preservation of cellular context; Dynamic measurements; Subcellular localization | Technical challenges in implementation; Potential phototoxicity; Probe accessibility issues |
| Genetic & Genomic Screening | Systematic DUB overexpression; CRISPR/Cas9 knockout screens; RNAi screens; Transposon mutagenesis (e.g., Sleeping Beauty) [4] [38] | Unbiased identification of DUB substrates; Discovery of DUB functions in specific pathways; Validation of genetic interactions [38] | Comprehensive, genome-wide scope; Functional context; Identification of redundancy | Overexpression may cause artifacts; Indirect effects; Compensation mechanisms |
| Chemical Biology & Proteomics | Activity-based protein profiling (ABPP); Ubiquitin/ISG15-based probes; Chemoproteomic screens; Competitive ABPP with DUB inhibitors [39] [40] | Profiling DUB activity states in complex proteomes; Inhibitor screening and validation; Detection of active DUB pools [39] | Activity-based readouts (not just abundance); High specificity; Suitable for inhibitor studies | Requires specialized probe design; May not capture all cellular DUBs equally |
Detailed Experimental Protocols
In Vitro Deubiquitination Assay
This foundational protocol determines whether a DUB can directly remove ubiquitin chains from a putative substrate in a purified system [37].
Materials:
- Purified recombinant DUB protein
- Purified ubiquitinated substrate (can be generated using E1, E2, and E3 enzymes in vitro)
- Reaction buffer (e.g., 50 mM Tris-HCl, pH 7.5, 50 mM NaCl, 1 mM DTT)
- Positive control (e.g., known DUB-substrate pair)
- Negative control (e.g., catalytically inactive DUB mutant)
Procedure:
- Prepare Reaction Mixtures: Combine 100-500 ng of ubiquitinated substrate with 50-200 ng of active DUB enzyme in reaction buffer. Adjust final volume to 20-50 μL.
- Set Up Controls: Include reactions with (a) substrate only (no DUB), (b) DUB only (no substrate), and (c) catalytically inactive DUB (e.g., Cys to Ala mutant) with substrate.
- Incubate: Conduct reactions at 30°C or 37°C for 30-120 minutes.
- Terminate Reaction: Add SDS-PAGE loading buffer containing DTT or β-mercaptoethanol to stop the reaction.
- Analyze Results: Resolve proteins by SDS-PAGE and perform immunoblotting using antibodies against the substrate, ubiquitin, and/or specific ubiquitin chain linkages (e.g., K48, K63) to detect decreased ubiquitin signal.
Protein Degradation Rate Analysis via Isotopic Pulse-Chase
This method measures the half-life of a putative DUB substrate upon modulation of DUB activity to establish functional relevance [37].
Materials:
- Cells with DUB modulation (overexpression, knockout, or knockdown)
- Radiolabeled amino acids (e.g., ^35^S-methionine/cysteine) or stable isotope-labeled amino acids
- Culture medium with excess unlabeled ("chase") amino acids
- Lysis buffer and immunoprecipitation reagents
Procedure:
- Metabolic Labeling (Pulse): Grow DUB-modulated and control cells in medium lacking methionine/cysteine for 30-60 minutes. Incubate cells with radiolabeled or isotope-labeled amino acids for a short period (typically 15-60 minutes) to label newly synthesized proteins.
- Chase Phase: Replace the labeling medium with complete medium containing excess unlabeled methionine/cysteine. This prevents further incorporation of labeled amino acids.
- Time-Point Collection: Harvest cells at multiple time points after chase initiation (e.g., 0, 15, 30, 60, 120 minutes).
- Immunoprecipitation: At each time point, lyse cells and immunoprecipitate the protein of interest using a specific antibody.
- Quantification: Resolve immunoprecipitated proteins by SDS-PAGE. For radiolabels, visualize and quantify bands using a phosphorimager. For stable isotopes, use mass spectrometry analysis. Plot the remaining protein quantity over time to determine half-life. A stabilized substrate in DUB-overexpressing cells (or destabilized substrate in DUB-deficient cells) suggests a functional DUB-substrate relationship.
Activity-Based Protein Profiling (ABPP) for DUB Activity
This chemoproteomic approach uses engineered probes to monitor functional DUB activity in complex biological samples [39].
Materials:
- Ubiquitin or Ubl (e.g., ISG15)-based ABP with C-terminal electrophilic warhead (e.g., vinyl sulfone, propargylamide) and reporter tag (fluorophore or biotin)
- Cell lysates from relevant experimental conditions
- Control recombinant DUBs
- Streptavidin beads (for pull-down) if using biotinylated probes
Procedure:
- Sample Preparation: Prepare lysates from control and treated cells (e.g., inhibitor treatment, pathway stimulation) under native conditions.
- Probe Labeling: Incubate lysates with ABP (0.1-5 μM final concentration) for 30-60 minutes at room temperature or 37°C.
- Detection/Analysis:
- For Fluorescent Probes: Resolve proteins by SDS-PAGE and visualize labeled DUBs via in-gel fluorescence scanning.
- For Affinity-Tagged Probes: Perform streptavidin pull-down, then identify captured DUBs by immunoblotting with specific DUB antibodies or by mass spectrometry for unbiased profiling.
- Validation: Use recombinant DUBs and DUB inhibitors as positive and negative controls to confirm specificity.
Figure 1: Experimental Workflow for DUB-Substrate Identification and Validation. This diagram outlines a logical progression from initial discovery to therapeutic application, integrating multiple methodological approaches.
DUB Signaling Pathways in Cancer and Research Applications
Understanding how DUBs regulate oncogenic and tumor suppressive pathways provides critical context for experimental design and interpretation. Several key DUB-modulated pathways have been extensively studied in cancer models.
Table 2: Key Cancer-Relevant Pathways Regulated by DUBs and Research Approaches
| Signaling Pathway | Regulating DUB(s) | Cancer Context | Substrate(s) | Research Methods Employed |
|---|---|---|---|---|
| p53 Signaling | USP28, USP7, USP10 [4] [40] | Multiple cancers (e.g., pancreatic, lung) [40] | p53, 53BP1, MDM2 [4] [40] | Co-IP, CRISPR screens, inhibitor studies (e.g., CAS-010) [40] |
| Wnt/β-catenin | USP28, USP21 [4] | Pancreatic ductal adenocarcinoma [4] | FOXM1, TCF7 [4] | In vitro deubiquitination, xenograft models, protein stability assays [4] |
| mTOR Signaling | USP21, OTUD5 [4] [31] | PDAC, Bladder Cancer [4] [31] | MAPK3, mTOR pathway components [4] [31] | Metabolic labeling, immunoblotting for phosphorylation, growth assays [4] |
| TGF-β/SMAD | OTUD1 [31] | Breast Cancer [31] | SMAD7 [31] | Knockdown/rescue experiments, migration/invasion assays, ubiquitin linkage mapping [31] |
| c-Myc Stability | USP28, USP36 [4] [40] | Various solid tumors and hematologic cancers [40] | c-Myc [40] | Cycloheximide chase, gene expression analysis, chemical inhibitors [40] |
Figure 2: Generalized Framework of DUB Function in Cancer Signaling. This diagram illustrates the central role of DUBs in regulating cancer-relevant pathways by controlling substrate ubiquitination status, and highlights the methodological approaches used to investigate these relationships.
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Research Reagent Solutions for DUB Studies
| Reagent Category | Specific Examples | Research Application | Key Features & Considerations |
|---|---|---|---|
| Commercial DUB Assay Kits | Fluorogenic Ubiquitin-based kits (e.g., for BAP1, USP7, UCHL1) [41] | High-throughput screening of DUB activity/inhibition; Kinetic or endpoint analysis [41] | 96-well format; No substrate preparation needed; Excitation/emission ~485/535 nm [41] |
| Activity-Based Probes (ABPs) | Ubiquitin-VS, ISG15-VS, Selective USP18 ABPs [39] | Profiling active DUB populations in lysates/live cells; Inhibitor screening [39] | Covalent active-site labeling; Can be tailored for selectivity (e.g., via HyCoSuL screening) [39] |
| Chemical Probes & Inhibitors | CAS-010 (USP28 inhibitor); WP1130 derivatives; USP7 inhibitors [40] [3] | Acute pharmacological DUB inhibition; Target validation; Pathway analysis [40] | Best practice: use with matched negative control compound (e.g., WPT-086 for CAS-010) [40] |
| Expression Systems | Yeast (S. cerevisiae) overexpression libraries; Lentiviral DUB constructs [38] | Genetic screening; Substrate identification; Functional complementation [38] | Yeast offers simplified genetics; Lentiviral systems enable stable expression in mammalian cells [38] |
The multifaceted experimental approaches outlined in this technical guide—spanning biochemical, genetic, cellular, and chemical biology methods—provide researchers with a powerful toolkit to dissect DUB functions and identify their physiological substrates. The integration of these complementary methodologies is crucial for establishing robust DUB-substrate relationships and understanding their roles in cancer biology. As the field advances, the development of more selective chemical probes, improved activity-based profiling methods, and sophisticated genetic models will further accelerate the translation of basic DUB research into novel therapeutic strategies for cancer treatment.
Metabolic reprogramming, a established hallmark of cancer, enables rapidly proliferating tumor cells to rewire their metabolic pathways to meet the substantial energy and biosynthetic demands of growth and survival [42]. This reprogramming encompasses profound alterations in glucose and lipid metabolism, including the well-characterized Warburg effect (aerobic glycolysis) and enhanced de novo lipogenesis [43] [42]. Recent research has illuminated that the intricate regulation of these metabolic pathways extends to the level of post-translational modifications, with ubiquitination and its reversal by deubiquitinating enzymes (DUBs) emerging as critical regulatory mechanisms.
DUBs constitute a family of approximately 100 proteases that specifically cleave ubiquitin chains from substrate proteins, thereby counterbalancing the activity of ubiquitin ligases [18] [43]. This dynamic process regulates protein stability, localization, and function, maintaining cellular homeostasis. DUBs are categorized into seven subfamilies based on their catalytic domains: ubiquitin-specific proteases (USPs), ovarian tumor proteases (OTUs), ubiquitin C-terminal hydrolases (UCHs), Machado-Josephin domain-containing proteases (MJDs), JAMM/MPN domain-associated metalloproteases, and motif-interacting with ubiquitin-containing novel DUB family (MINDYs) [18] [43]. Dysregulation of DUB expression and activity is frequently observed in human cancers, where they stabilize oncoproteins, enhance tumor cell survival, and drive malignant progression [18] [43]. This review comprehensively examines the mechanistic roles of specific DUBs in regulating glycolytic and lipid metabolic pathways in cancer, explores their therapeutic potential, and provides essential methodological resources for researchers investigating this rapidly evolving field.
DUBs in Glycolytic Regulation
Direct Stabilization of Glycolytic Enzymes
Cancer cells exhibit markedly increased glucose uptake and lactate production even under normoxic conditions, a phenomenon known as the Warburg effect or aerobic glycolysis. Several DUBs have been identified as direct regulators of key glycolytic enzymes through deubiquitination and stabilization, facilitating this metabolic shift (Table 1).
Table 1: DUBs Regulating Glycolytic Enzymes in Cancer
| DUB | Cancer Type | Glycolytic Target | Mechanism | Functional Outcome |
|---|---|---|---|---|
| JOSD2 | Non-small cell lung cancer | ALDOA, PFK1 | Deubiquitinates and stabilizes ALDOA and PFK1 | Enhances glycolytic rate and cancer cell proliferation [43] |
| CSN5 | Hepatocellular carcinoma | HK2 | Deubiquitinates and stabilizes HK2 | Increases glucose uptake and glycolytic flux [43] |
| USP7/USP20 | HeLa cells | PKM2 | Deubiquitinates and stabilizes PKM2 | Promotes glucose catabolism [43] |
| UCHL3 | Pancreatic cancer | FOXM1 | Stabilizes FOXM1, activating LDHA transcription | Promotes aerobic glycolysis via UCHL3-FOXM1-LDHA axis [43] |
Hexokinase 2 (HK2), which catalyzes the first committed step of glycolysis, is stabilized by CSN5 (COP9 signalosome subunit 5) in hepatocellular carcinoma (HCC). CSN5 attenuates ubiquitin-proteasome system-mediated degradation of HK2 through its deubiquitinase function, and there exists a positive correlation between CSN5 and HK2 levels in HCC samples [43]. Similarly, Josephin Domain-containing protein 2 (JOSD2) exerts comprehensive effects on glucose catabolism in non-small cell lung cancer (NSCLC) by simultaneously stabilizing two critical glycolytic enzymes—aldolase A (ALDOA) and phosphofructokinase-1 (PFK1)—through deubiquitination, thereby enhancing their activities and the overall glycolytic rate [43]. Further down the glycolytic pathway, pyruvate kinase isoenzyme M2 (PKM2), which regulates the final step of glycolysis, is stabilized by both USP7 and USP20 in HeLa cells, though the precise mechanistic details require further elucidation [43].
Regulation of Transcriptional Drivers of Glycolysis
Beyond direct enzyme stabilization, DUBs regulate glycolysis through key transcription factors that orchestrate the expression of multiple glycolytic genes. The hypoxia-inducible factor 1α (HIF-1α) and oncogenic MYC family proteins are two master regulators of cancer metabolism, both subject to DUB-mediated stabilization (Table 2).
Table 2: DUBs Regulating Transcriptional Drivers of Glycolysis
| DUB | Cancer Type | Transcription Factor | Mechanism | Functional Outcome |
|---|---|---|---|---|
| USP29 | Multiple cancers | HIF-1α, MYC | Direct interaction and deubiquitination | Stabilizes HIF-1α and MYC, promoting glucose consumption and lactate secretion [43] |
| USP25 | Pancreatic ductal adenocarcinoma | HIF-1α | Deubiquitinates and stabilizes HIF-1α | Promotes HIF-1α-driven glycolysis and tumor survival in hypoxic core [44] |
| OTUB2 | Non-small cell lung cancer | U2AF2 | Stabilizes U2AF2 | Promotes Warburg effect via AKT/mTOR signaling [43] |
| USP10 | Colorectal cancer | AMPK | Removes ubiquitination on AMPK | Forms positive feedforward loop with AMPK under energy stress [43] |
In pancreatic ductal adenocarcinoma (PDAC), USP25 has been identified as a master regulator of HIF-1α-driven metabolic reprogramming. PDAC is characterized by a severely hypoxic microenvironment, and USP25 deubiquitinates and stabilizes HIF-1α, enabling sustained transcriptional activation of glycolytic genes. Genetic or pharmacological inhibition of USP25 impairs glycolysis and induces PDAC cell death, particularly in the hypoxic tumor core [44]. USP29 demonstrates remarkable versatility by stabilizing both HIF-1α and MYC under normoxic and hypoxic conditions across multiple cancer types. Systematic knockout of Usp29 in MYC-driven animal models significantly decreases intratumoral MYC, HIF-1α, and their key downstream metabolic targets, underscoring its central role in glycolytic regulation [43].
The regulatory network extends to additional signaling pathways. OTUB2, significantly upregulated in NSCLC primary tissues, stabilizes U2 small nuclear RNA auxiliary factor 2 (U2AF2) to promote the Warburg effect and tumorigenesis via the AKT/mTOR signaling pathway [43]. Furthermore, the USP10-AMPK axis forms a positive feedforward loop that facilitates AMPK activation under energy stress, although the precise mechanistic details of this regulation in glycolytic control remain under investigation [43].
Diagram: DUB Regulation of Cancer Glycolysis. DUBs (blue) stabilize key glycolytic enzymes (green) directly or through transcription factors (red) to enhance glycolytic flux from glucose to lactate.
DUBs in Lipid Metabolism Reprogramming
Regulation of Fatty Acid Synthesis Enzymes
Lipid metabolic reprogramming in cancer involves enhanced de novo fatty acid synthesis, increased lipid uptake, and altered cholesterol metabolism to support membrane biosynthesis, energy storage, and signaling processes. DUBs play pivotal roles in regulating the stability and activity of key lipogenic enzymes, particularly adenosine triphosphate citrate lyase (ACLY) and fatty acid synthase (FASN).
ACLY catalyzes the conversion of citrate and coenzyme A into oxaloacetate and acetyl-CoA, representing a critical link between glycolysis and lipid metabolism. In lung cancer, the deacetylation of ACLY and subsequent ubiquitination of lysine residues are important processes regulating its protein activity and stability. ARHGEF3, a member of the Rho-GEFs family, enhances ACLY protein stability by reducing its acetylation at Lys17 and Lys86, leading to dissociation of ACLY from its E3 ligase NEDD4 [30]. Additionally, under high glucose conditions, ACLY's K540, K546, and K554 sites are acetylated by histone acetyltransferase PCAF, reducing interaction with the RING-type E3 ubiquitin ligase UBR4 and thereby maintaining ACLY-mediated protein homeostasis. Sirtuin 2 (SIRT2), a NAD+-dependent class III histone deacetylase, reverses this process by regulating ACLY deacetylation and destabilization [30]. Cullin 3 interacts with ACLY through its adaptor protein Kelch-like family member 25 (KLHL25), ubiquitinating and degrading ACLY in cells. By negatively regulating ACLY, CUL3 inhibits lipid synthesis, cell proliferation, and xenograft tumor growth in lung cancer cells [30].
FASN, the multi-enzyme complex responsible for de novo fatty acid synthesis, is similarly regulated by ubiquitination. In prostate cancer, the tumor suppressor gene speckle-type POZ protein (SPOP), which functions as an E3 ubiquitin ligase, regulates lipid metabolism by reducing FASN expression and fatty acid synthesis, thereby exerting tumor suppressive effects [30]. Furthermore, FASN undergoes deacetylation by HDAC3, which enhances its binding with the E3 ubiquitin ligase TRIM21. This deacetylation stabilizes FASN, allowing more effective interaction with TRIM21, thereby reducing lipogenesis and inhibiting cancer cell growth [30].
Cholesterol Metabolism and Lipid Storage
Cholesterol metabolism represents another crucial aspect of lipid reprogramming influenced by DUB activity. Transcription factors such as Sterol Regulatory Element-Binding Protein-1 (SREBP-1) and Peroxisome Proliferator-Activated Receptors (PPARs) promote the expression of key genes like FASN and stearoyl-CoA desaturase 1 (SCD1), resulting in elevated lipid synthesis and enhanced cancer cell proliferation [30]. 3-Hydroxy-3-methylglutaryl-coenzyme A reductase (HMGCR), a crucial enzyme in cholesterol synthesis, is frequently upregulated in cancers such as gastric, brain, and prostate cancer, promoting cancer cell growth and migration [30].
While the direct involvement of specific DUBs in cholesterol metabolism requires further investigation, the broader ubiquitination system undoubtedly contributes to its regulation. The emerging role of DUBs in lipid droplet dynamics and fatty acid oxidation presents an exciting frontier for future research, particularly given the importance of lipid storage and mobilization in cancer cell survival under metabolic stress.
Experimental Approaches for Studying DUBs in Cancer Metabolism
Activity-Based Proteomics and Genetic Screening
A comprehensive understanding of DUB functions in cancer metabolism requires sophisticated experimental approaches that capture both enzymatic activity and biological relevance. An innovative pipeline combining activity-based proteomics with loss-of-function genetic screening in patient-derived organoids (PDOs) has proven particularly powerful for identifying therapeutically relevant DUBs (Table 3).
Table 3: Key Experimental Approaches for DUB Research
| Methodology | Key Components | Application Example | Outcome |
|---|---|---|---|
| Activity-Based Proteomics | Ubiquitin-ABPs with different electrophilic warheads (PA, VME, VS); Mass spectrometry | Identification of active DUBs in PDAC organoids and murine models | Identified 28 significantly active DUBs in KPCY organoids and 23 in PDOs [44] |
| Loss-of-Function Genetic Screening | shRNA library in lentiviral pLKO.1 vector; High-content imaging of organoid growth | Functional screening of active DUBs in PDAC organoids | Identified USP25 as essential DUB for PDAC growth and viability [44] |
| Organoid Models | Patient-derived organoids (PDOs); Genetically defined murine organoids (KPCY) | Modeling PDAC heterogeneity and therapeutic responses | Retained original tumor heterogeneity; correlated with patient therapeutic responses [44] |
| Metabolic Flux Analysis | Glucose consumption, lactate production, isotopic tracer studies | Assessment of glycolytic function after DUB manipulation | Confirmed impaired glycolysis upon USP25 depletion [44] |
This integrated approach begins with activity-based protein profiling using ubiquitin-conjugated activity-based probes (ABPs) with different electrophilic warheads (propargylamide [PA], vinylmethylester [VME], or vinylsulfone [VS]) that covalently interact with the nucleophilic cysteine residue in DUB active sites. These ABPs enable identification of enzymatically active DUBs rather than simply measuring protein abundance. Following labeling with biotin-conjugated ABPs and mass spectrometry analysis, researchers can identify significantly active DUBs in specific cancer models [44]. In PDAC, this approach identified 28 significantly active DUBs in KPCY organoids and 23 in PDOs, with 18 overlapping DUBs conserved across both models [44].
Subsequent functional validation through loss-of-function genetic screening using lentiviral shRNA libraries in organoid models enables identification of DUBs essential for cancer cell growth and viability. High-content imaging monitors organoid growth and viability post-knockdown, revealing DUBs with critical functional roles. In PDAC, this approach identified USP25 as the most significantly essential DUB, with all three targeting shRNAs dramatically impairing organoid growth [44].
Diagram: Experimental Workflow for DUB Discovery. Integrated approach combining patient-derived organoids, activity-based proteomics, functional screening, and mechanistic studies to identify therapeutically relevant DUBs.
The Scientist's Toolkit: Essential Research Reagents
Investigating DUB functions in cancer metabolism requires specialized reagents and tools. The following table summarizes key resources for studying DUB activity, function, and therapeutic potential:
Table 4: Essential Research Reagents for DUB Studies
| Reagent/Tool | Category | Function/Application | Examples/Notes |
|---|---|---|---|
| Ubiquitin-ABPs | Chemical probes | Covalently bind active DUBs for identification and enrichment | Probes with PA, VME, VS warheads; Cy5 or biotin conjugates [44] |
| PR-619 | Small molecule inhibitor | Pan-DUB inhibitor for specificity controls | Attenuates DUB binding to ABPs; validates target engagement [44] |
| shRNA Libraries | Genetic tools | Loss-of-function screening | pLKO.1 vector system; 3 shRNAs per gene recommended [44] |
| Patient-Derived Organoids | Biological models | Maintain tumor heterogeneity and patient-specific responses | Grown in 3D matrices; retain original tumor characteristics [44] |
| Metabolic Assay Kits | Functional assays | Quantify glycolytic and lipogenic activity | Glucose consumption, lactate production, lipid accumulation assays [43] |
| Cycloheximide | Protein synthesis inhibitor | Measure protein half-life in stability assays | Combined with DUB manipulation to assess substrate stabilization [18] |
| MG132/ Bortezomib | Proteasome inhibitors | Confirm proteasomal degradation pathway | Blocks degradation of ubiquitinated proteins [42] |
This toolkit enables researchers to comprehensively investigate DUB functions from initial identification to mechanistic validation. The combination of activity-based probes, specialized inhibitors, advanced organoid models, and metabolic assays provides a robust platform for delineating DUB roles in cancer metabolic reprogramming.
Therapeutic Targeting of DUBs in Cancer Metabolism
Development of DUB-Targeted Therapies
The critical roles of DUBs in regulating cancer metabolism, combined with their enzymatic nature and druggability, make them attractive therapeutic targets. Several strategies have emerged for targeting DUB functions in cancer, with small-molecule inhibitors representing the most advanced approach.
The development of specific DUB inhibitors has gained significant momentum, with some candidates already advancing to clinical evaluation. For instance, SIM0501, a small molecule inhibitor targeting USP1, has received FDA clinical approval and is planned for trials in advanced solid tumors [30]. Similarly, LCL161, an inhibitor of apoptosis protein (IAP) inhibitor that modulates the ubiquitin system, induces TNF-dependent apoptosis in multiple myeloma cells and enhances anti-tumor immune responses [30]. While these examples target DUBs involved in various cancer processes, they establish important precedents for targeting the ubiquitin system therapeutically.
In PDAC, where USP25 has been identified as a master regulator of HIF-1α-driven glycolysis, pharmacological inhibition of USP25 causes dramatic regression of patient-derived xenografts, while normal pancreatic organoids remain relatively insensitive, suggesting a potential therapeutic window [44]. This cancer cell specificity is particularly important for therapeutic development, as global DUB inhibition might be expected to cause significant toxicity in normal tissues.
Biomarker Potential and Clinical Translation
Beyond direct therapeutic targeting, DUBs show promise as biomarkers for cancer diagnosis, prognosis, and treatment response monitoring. Comprehensive analysis of human cancers by in situ hybridization has revealed that DUBs are frequently dysregulated in tumor samples, with many showing significant overexpression compared to normal tissues [43]. For example, USP22 is recognized as a marker of cancer stem cells and was reported to promote stemness in hepatocellular carcinoma cells [18]. In thyroid cancer, OTUD1 (also known as DUBA7) is differentially expressed and can serve as a biomarker for early detection [31].
The biomarker potential of DUBs extends to metabolic pathways specifically. In PDAC, elevated USP25 expression correlates with poorer patient survival, suggesting its utility as a prognostic marker [44]. Similarly, in NSCLC, OTUB2 is significantly upregulated in primary tissues and associated with tumor malignancy [43]. The development of non-invasive detection methods for DUB activity or expression, potentially through liquid biopsy-based approaches, could significantly enhance their clinical utility as biomarkers.
DUBs have emerged as critical regulators of cancer metabolic reprogramming, fine-tuning glycolytic and lipogenic pathways through direct stabilization of metabolic enzymes and master transcriptional regulators. The integrated experimental approaches discussed, particularly activity-based proteomics combined with functional screening in patient-derived organoids, provide powerful platforms for identifying therapeutically relevant DUBs in specific cancer contexts.
Several important questions and challenges remain for the field. The context-dependent functions of certain DUBs, exemplified by USP9X which can act as either an oncogene or tumor suppressor in different PDAC models, complicate therapeutic targeting strategies [18]. Additionally, the extensive crosstalk between different metabolic pathways and the potential redundancy among DUB family members may necessitate combination approaches rather than single-DUB targeting. Future research should also explore the role of less-characterized DUB families in metabolic regulation and investigate the potential of targeting DUBs in combination with existing metabolic inhibitors or immunotherapies.
As our understanding of DUB functions in cancer metabolism continues to expand, so too will opportunities for therapeutic intervention. The continued development of specific DUB inhibitors, combined with patient stratification strategies based on DUB expression patterns, holds significant promise for advancing precision medicine approaches in oncology. By targeting the very enzymes that drive metabolic adaptations in cancer cells, we may ultimately overcome the limitations of current therapies and develop more effective treatments for aggressive malignancies, particularly those like pancreatic cancer where metabolic reprogramming plays such a central role in pathogenesis and therapy resistance.
Deubiquitinating enzymes (DUBs) have emerged as pivotal regulators in cancer biology, controlling the stability and function of key proteins involved in tumor progression. Among them, PSMD14 (Proteasome 26S Subunit, Non-ATPase 14), a JAMM metalloprotease family DUB, demonstrates significant overexpression across multiple malignancies including gastric adenocarcinoma (GAC) and correlates with poor patient prognosis [45] [46]. This case study examines the mechanistic role of PSMD14 in driving gastric carcinogenesis through its regulation of PFKFB2, a critical glycolytic regulator, thereby establishing a novel connection between deubiquitination and metabolic reprogramming in cancer.
Molecular Mechanism: Linking Deubiquitination to Metabolic Reprogramming
The PSMD14-PFKFB2 Signaling Axis
Research by Zhao et al. (2024) elucidates a precise molecular pathway through which PSMD14 activates glycolytic flux in gastric adenocarcinoma. PSMD14 directly interacts with and deubiquitinates PFKFB2 at lysine 355, thereby stabilizing this key glycolytic regulator [47]. This deubiquitination event facilitates subsequent phosphorylation of PFKFB2 at serine residues 466 and 483 by the kinase SCYL2. The activated, phosphorylated PFKFB2 then enhances production of fructose-2,6-bisphosphate (F2,6BP), the most potent allosteric activator of phosphofructokinase-1 (PFK-1) [47] [48]. This final step crucially activates PFK-1, the primary rate-limiting enzyme of glycolysis, resulting in accelerated glycolytic flux and lactate production—a hallmark of cancer metabolism known as the Warburg effect [47].
Transcriptional Reinforcement via Histone Lactylation
The metabolic consequences of PSMD14 activity extend beyond immediate glycolytic activation. Increased lactate generation from enhanced glycolysis serves as a substrate for histone lactylation, particularly at the H3K27la mark [47]. This novel epigenetic modification creates a positive feedback loop by enhancing the transcription of both PSMD14 and the stemness factor SOX9, thereby amplifying tumor stemness properties and driving malignant progression in gastric adenocarcinoma [47].
Table 1: Key Molecular Events in PSMD14-PFKFB2 Signaling
| Molecular Event | Functional Consequence | Biological Outcome |
|---|---|---|
| PSMD14-mediated deubiquitination of PFKFB2 at K355 | Stabilization of PFKFB2 protein | Increased F2,6BP production |
| SCYL2-mediated phosphorylation of PFKFB2 at S466/S483 | Enhanced PFKFB2 kinase activity | PFK-1 activation and glycolytic acceleration |
| Lactate accumulation from glycolysis | H3K27 histone lactylation | Transcriptional activation of PSMD14 and SOX9 |
| Formation of H3K27la/PSMD14/SCYL2/p-PFKFB2 axis | Sustained metabolic activation | Enhanced cancer stemness and tumor progression |
Experimental Evidence and Validation
Key Experimental Findings
Multiple experimental approaches have validated the functional significance of the PSMD14-PFKFB2 axis in gastric cancer models:
Genetic Knockdown Studies: PSMD14 depletion in GAC cell lines significantly impaired cancer cell proliferation, migration, and invasion capabilities [45] [46]. These findings were corroborated by in vivo experiments demonstrating that PSMD14 knockdown suppressed tumor growth in xenograft models [45].
Metabolic Measurements: Direct assessment of glycolytic parameters revealed that PSMD14 strengthens tumor stemness and drives progression by increasing glycolysis and lactate accumulation [47].
Clinical Correlation: Analysis of patient specimens showed that the H3K27la/PSMD14/SCYL2/p-PFKFB2 axis correlates with increased glucose metabolic activity and poor prognosis in GAC patients [47].
Drug Screening: High-throughput screening of FDA-approved compounds identified Daclatasvir (DCV) as possessing high binding affinity for PSMD14, disrupting the PSMD14-PFKFB2 interaction and reducing both PFKFB2 activity and tumor burden [47].
Essential Research Reagents and Tools
Table 2: Key Research Reagents for Studying PSMD14-PFKFB2 Biology
| Reagent/Resource | Specific Application | Experimental Function |
|---|---|---|
| PSMD14-specific shRNAs | Genetic knockdown | Deplete PSMD14 to assess functional consequences |
| Anti-PSMD14 antibodies | Immunohistochemistry/Immunoblotting | Detect protein expression and localization |
| Anti-p-PFKFB2 (S466/S483) | Phospho-specific immunoblotting | Monitor PFKFB2 activation status |
| Daclatasvir (DCV) | Pharmacological inhibition | Disrupt PSMD14-PFKFB2 interaction |
| Recombinant PSMD14 protein | In vitro assays | Study enzymatic activity and binding |
| Lactate measurement kits | Metabolic phenotyping | Quantify glycolytic output |
| H3K27la-specific antibodies | Chromatin immunoprecipitation | Assess epigenetic modifications |
Detailed Experimental Protocols
Protocol 1: Assessing PSMD14-PFKFB2 Interaction
Co-immunoprecipitation Methodology:
- Lyse gastric cancer cells (e.g., AGS, HGC-27) in RIPA buffer supplemented with protease and deubiquitinase inhibitors.
- Incubate cell lysates with anti-PSMD14 antibody or species-matched IgG control overnight at 4°C with gentle rotation.
- Add protein A/G beads and incubate for 2-4 hours at 4°C.
- Wash beads extensively with lysis buffer and elute bound proteins with SDS-PAGE sample buffer.
- Analyze eluates by immunoblotting using anti-PFKFB2 and anti-PSMD14 antibodies to confirm interaction.
Deubiquitination Assay:
- Transfect cells with HA-ubiquitin plasmid and treat with MG132 (10 μM) for 6 hours before harvesting to accumulate ubiquitinated proteins.
- Immunoprecipitate PFKFB2 using specific antibodies under denaturing conditions to preserve ubiquitination status.
- Detect ubiquitinated PFKFB2 levels via immunoblotting with anti-HA antibody.
- Compare ubiquitination levels in PSMD14-knockdown versus control cells to assess PSMD14-mediated deubiquitination.
Protocol 2: Metabolic Functional Assays
Glycolytic Rate Measurement:
- Seed gastric cancer cells in XF96 cell culture microplates at appropriate density (20,000-30,000 cells/well).
- Following PSMD14 modulation, measure extracellular acidification rate (ECAR) using Seahorse XF Glycolysis Stress Test kit.
- Sequentially inject glucose, oligomycin, and 2-deoxy-glucose according to manufacturer's protocol.
- Calculate key glycolytic parameters: basal glycolysis, glycolytic capacity, and glycolytic reserve.
PFKFB2 Kinase Activity Assay:
- Immunoprecipitate PFKFB2 from cell lysates.
- Incubate immunoprecipitates with reaction buffer containing fructose-6-phosphate, ATP, and MgCl2.
- Stop reaction at various time points and quantify fructose-2,6-bisphosphate production using enzymatic assays.
- Normalize activity to immunoprecipitated PFKFB2 amount.
PSMD14 in Broader Cancer Context
PSMD14 Functions Across Malignancies
The oncogenic role of PSMD14 extends beyond gastric adenocarcinoma, with consistent findings across diverse cancer types:
Breast Cancer: PSMD14 stabilizes ERα signaling through deubiquitination, contributing to endocrine resistance. A positive feedback loop exists where ERα transcriptionally activates PSMD14 expression while PSMD14 stabilizes ERα protein [49].
Ovarian Cancer: PSMD14 decreases K63-linked ubiquitination on PKM2, altering pyruvate kinase isoform stoichiometry to favor the dimeric form, which exhibits reduced kinase activity but enhanced nuclear transcriptional function [50].
Pancreatic Cancer: PSMD14 represents one of numerous DUBs implicated in PDAC progression, highlighting the broader significance of DUB dysregulation in gastrointestinal malignancies [4].
Table 3: PSMD14 Substrates and Functional Consequences Across Cancers
| Cancer Type | Key PSMD14 Substrate(s) | Primary Oncogenic Function |
|---|---|---|
| Gastric Adenocarcinoma | PFKFB2, PTBP1 | Metabolic reprogramming, enhanced proliferation |
| Breast Cancer | ERα | Endocrine resistance, transcriptional activation |
| Ovarian Cancer | PKM2 | Glycolytic reprogramming, gene transcription |
| Hepatocellular Carcinoma | TGF-β receptors, Caveolin-1 | Enhanced metastasis, growth factor signaling |
| Esophageal Cancer | SNAIL | EMT induction, stabilization of transcription factor |
Therapeutic Targeting and Clinical Implications
Intervention Strategies
The PSMD14-PFKFB2 axis presents multiple therapeutic targeting opportunities:
Direct PSMD14 Inhibition: Daclatasvir (DCV), identified through high-throughput screening, exhibits promising binding affinity for PSMD14 and disrupts its interaction with PFKFB2 [47]. In experimental models, DCV treatment significantly reduced PFKFB2 activity and tumor burden.
Small Molecule Inhibitors: O-phenanthroline (OPA) has demonstrated efficacy in inhibiting PSMD14 function in ovarian cancer models, suppressing malignant behaviors in vitro and reducing tumor growth in vivo [50].
Combination Approaches: For cancers with established feedback loops, such as breast cancer, simultaneous targeting of PSMD14 and endocrine signaling pathways may yield synergistic effects [49].
Clinical Translation Considerations
The prognostic significance of PSMD14 overexpression across multiple cancers suggests potential applications as:
- Biomarker for aggressive disease and metabolic dysregulation
- Predictive indicator for therapeutic response to metabolic-targeting agents
- Candidate for pharmacodynamic monitoring during DUB-targeted therapies
Visualizing the PSMD14-PFKFB2 Signaling Pathway
Visualizing Experimental Workflow for Mechanism Validation
The PSMD14-PFKFB2 signaling axis represents a paradigm-shifting connection between deubiquitination and metabolic reprogramming in gastric adenocarcinoma. This mechanistic link demonstrates how DUBs can orchestrate profound metabolic alterations that drive cancer stemness and progression through both direct enzymatic regulation and epigenetic modifications. The discovery that lactate-derived histone lactylation completes a positive feedback loop reinforces the self-sustaining nature of this oncogenic pathway.
Future research should focus on developing more specific PSMD14 inhibitors with improved pharmacological properties, identifying patient selection biomarkers for DUB-targeted therapies, and exploring potential synergies between PSMD14 inhibition and existing metabolic-targeting agents. As the broader field of DUB biology continues to evolve, the PSMD14-PFKFB2 axis in gastric adenocarcinoma serves as an instructive model for understanding how deubiquitination networks integrate with cancer metabolism to drive malignant progression.
The ubiquitin-proteasome system (UPS) is a crucial post-translational modification mechanism that governs virtually all cellular processes, including immune regulation. Within this system, deubiquitinating enzymes (DUBs) represent a family of approximately 100 proteases that counterbalance the action of E3 ubiquitin ligases by removing ubiquitin chains from substrate proteins [51] [52]. This dynamic equilibrium between ubiquitination and deubiquitination precisely controls the stability, localization, and activity of key immune checkpoint proteins, most notably the programmed cell death protein 1 (PD-1) and its ligand (PD-L1) [53] [54]. The PD-1/PD-L1 axis constitutes a critical immunosuppressive pathway exploited by cancer cells to evade immune surveillance. When PD-L1 on tumor cells engages PD-1 on T cells, it initiates a signaling cascade that suppresses T-cell receptor (TCR) signaling through dephosphorylation events mediated by phosphatases like SHP2, ultimately leading to T-cell exhaustion and immune tolerance [55]. As research has progressed, it has become increasingly evident that DUBs play a pivotal role in modulating the stability and abundance of these immune checkpoints, thereby offering promising new avenues for therapeutic intervention in cancer immunotherapy [53] [12].
Regulatory Mechanisms: DUBs in PD-1/PD-L1 Homeostasis
Direct Regulation of PD-L1 by DUBs
Multiple DUBs have been identified as direct regulators of PD-L1 stability through deubiquitination, protecting it from proteasomal degradation and thereby enhancing tumor immune evasion. The following table summarizes key DUBs known to regulate PD-L1 and their specific mechanisms of action.
Table 1: DUBs Directly Regulating PD-L1 Stability
| DUB | Cancer Context | Mechanism of Action | Functional Outcome |
|---|---|---|---|
| USP8 | Pancreatic Cancer | Binds and deubiquitinates PD-L1, reducing its degradation [56] | Enhances PD-L1 stability, suppresses T-cell activity [56] |
| USP9X | Multiple Cancers | Removes ubiquitin chains from PD-L1 [53] | Increases PD-L1 levels and promotes immune evasion [53] |
| USP22 | Under Investigation | Potential PD-L1 regulator through deubiquitination [53] | May stabilize PD-L1; requires further validation [53] |
| Ataxin-3 (ATXN3) | Multiple Cancers | Identified in CRISPR screens as a PD-L1 activator; stabilizes PD-L1 [12] | Promotes immune escape; correlates with poor prognosis [12] |
Direct Regulation of PD-1 by DUBs
While research has predominantly focused on PD-L1 regulation, emerging evidence indicates that DUBs also influence PD-1 expression on immune cells, thereby modulating the immunosuppressive signals received by T cells in the tumor microenvironment.
Table 2: DUBs Directly Regulating PD-1 Expression
| DUB | Cellular Context | Mechanism of Action | Functional Outcome |
|---|---|---|---|
| OTUB1 | T Cells | Catalytically inhibits PD-1 ubiquitination [53] | Enhances PD-1 stability, exacerbating T-cell exhaustion [53] |
| USP7 | Under Investigation | Potential regulator of PD-1 [53] | May influence T-cell function; under active research [53] |
Indirect Regulation of Immune Checkpoints
Beyond direct stabilization, DUBs indirectly modulate immune checkpoint expression and activity through various signaling pathways. For instance, USP39, while lacking direct deubiquitination activity toward PD-L1, influences cancer immunity through its critical role in RNA splicing, potentially affecting the expression of immune-related genes [56]. Additionally, USP21 promotes pancreatic ductal adenocarcinoma (PDAC) growth by activating mTOR signaling and inducing micropinocytosis to support amino acid sustainability, thereby creating an immunosuppressive tumor microenvironment [4]. The PI3K/Akt/mTOR, NF-κB, and MAPK pathways—all known to be regulated by various DUBs—converge to control the expression of PD-L1 and other immune checkpoints, establishing a complex network of indirect regulation [51].
The following diagram illustrates the complex regulatory network of DUBs controlling PD-1/PD-L1 stability and function:
Experimental Approaches for Studying DUB-Immune Checkpoint Interactions
Methodologies for Identifying DUB-Substrate Relationships
Establishing direct functional relationships between DUBs and immune checkpoints requires integrated experimental approaches. CRISPR-based genetic screening has emerged as a powerful discovery tool, as demonstrated by the identification of Ataxin-3 (ATXN3) as a novel regulator of PD-L1 expression through genome-wide screens [12]. Following initial identification, co-immunoprecipitation (Co-IP) assays are essential for validating physical interactions between DUBs and their putative substrate proteins. For example, the interaction between USP8 and PD-L1 was confirmed through Co-IP experiments in pancreatic cancer models [56]. To quantify the effects of DUB manipulation on substrate stability, cycloheximide chase assays are employed to measure protein half-life by inhibiting new protein synthesis and monitoring degradation rates over time. This approach can demonstrate how DUB overexpression extends PD-L1 half-life by reducing its turnover [53]. Additionally, in vitro deubiquitination assays using purified components provide direct evidence of DUB enzymatic activity toward specific substrates. These assays typically involve incubating ubiquitinated immune checkpoint proteins with the candidate DUB and detecting reduced ubiquitination through immunoblotting [12].
Functional Validation in Immune Contexts
Once molecular interactions are established, functional validation is crucial to confirm the immunological relevance of DUB-mediated checkpoint regulation. T-cell activation and cytotoxicity assays measure the functional consequences of DUB modulation by co-culturing tumor cells with primary T cells and assessing T-cell activation markers (e.g., CD69, CD25), cytokine production (IFN-γ, IL-2), and tumor cell killing capacity [56]. For in vivo validation, syngeneic mouse models with appropriate immune-intact hosts provide a physiologically relevant context to evaluate how DUB targeting affects tumor growth and immune cell infiltration. These models can demonstrate whether DUB inhibition enhances the efficacy of existing checkpoint inhibitors [12]. Advanced multi-color flow cytometry enables comprehensive immune profiling of tumor microenvironments, allowing researchers to quantify changes in immune cell populations (T cells, NK cells, macrophages), activation states, and checkpoint expression following DUB manipulation [55].
The following diagram illustrates a comprehensive experimental workflow for identifying and validating DUB-immune checkpoint interactions:
Table 3: Key Research Reagents for Investigating DUB-Checkpoint Biology
| Reagent Category | Specific Examples | Research Application |
|---|---|---|
| DUB Inhibitors | HBX41108, P22077 (USP7 inhibitors); b-AP15 (USP14/UCHL5 inhibitor); WP1130 (USP9X inhibitor) [12] | Pharmacological inhibition to validate DUB function and assess therapeutic potential |
| Genetic Tools | CRISPR/Cas9 systems for DUB knockout; siRNA/shRNA for DUB knockdown; DUB overexpression plasmids [12] | Genetic manipulation to establish causal relationships between DUBs and checkpoint regulation |
| Antibodies for Detection | Anti-PD-1, anti-PD-L1, anti-ubiquitin, anti-K48/K63 ubiquitin linkage, DUB-specific antibodies [53] [54] | Protein detection, quantification, and localization in Western blot, flow cytometry, and immunohistochemistry |
| Cell-based Assays | Reporter systems with PD-L1 promoter; T-cell activation assays; co-culture systems [56] [12] | Functional assessment of DUB manipulation on immune cell activity and tumor-immune interactions |
| Animal Models | Syngeneic mouse models; humanized mouse models with human immune system [12] | In vivo validation of DUB targeting in physiologically relevant tumor microenvironments |
Therapeutic Implications and Clinical Translation
The strategic inhibition of specific DUBs represents a promising approach to enhance cancer immunotherapy by modulating immune checkpoint levels in the tumor microenvironment. Preclinical studies have demonstrated that targeting DUBs such as USP7, USP8, and USP9X can reduce PD-L1 expression on tumor cells and potentially ameliorate T-cell exhaustion by modulating PD-1 levels [56] [53] [12]. The Dana-Farber Cancer Institute has pioneered a comprehensive DUB drug discovery platform that employs activity-based proteomics, high-throughput screening, and specialized data analytics to identify selective small-molecule modulators of DUB activity [52]. This systematic approach has already yielded selective inhibitors for 23 DUBs across four subfamilies, including lead compounds targeting USP7 that stabilize the p53 tumor suppressor and show promise for treating various cancers [52].
Given the complexity of tumor immune evasion mechanisms, combination therapies represent a particularly promising strategy. Simultaneous targeting of specific DUBs alongside existing PD-1/PD-L1 axis inhibitors may yield synergistic effects by addressing multiple resistance mechanisms simultaneously [56] [12]. For instance, combining USP7 inhibition with PD-1 blockade could potentially enhance T-cell-mediated tumor killing through both checkpoint blockade and stabilization of p53 in tumor cells [52]. The development of DUB-focused small molecules is accelerating, with several candidates advancing toward clinical trials. However, challenges remain in achieving sufficient selectivity among the approximately 100 human DUBs and understanding the complex, context-dependent functions of individual DUBs across different cancer types [51] [52].
The investigation of DUBs in tumor immunity represents a rapidly evolving frontier with significant implications for cancer therapy. Future research directions should prioritize the comprehensive mapping of DUB-immune checkpoint interactions across different cancer types, as current knowledge likely represents only a fraction of the regulatory landscape. The development of highly selective DUB inhibitors with improved pharmacological properties remains a critical challenge that requires continued investment in structural biology and medicinal chemistry. Additionally, greater emphasis on understanding the cell-type-specific functions of DUBs within the tumor microenvironment—distinguishing between their roles in tumor cells versus various immune cell populations—will be essential for developing targeted therapies with minimized off-target effects.
The integration of DUB targeting into cancer immunotherapy represents a paradigm shift in our approach to modulating immune checkpoint pathways. Rather than merely blocking receptor-ligand interactions, DUB inhibition offers the potential to dynamically regulate the protein stability of key immune checkpoints, potentially leading to more durable and effective anti-tumor immunity. As research in this field advances, DUB-based therapies are poised to become important components of the precision oncology toolkit, potentially overcoming limitations of current immunotherapies and benefiting broader patient populations.
Deubiquitinating enzymes (DUBs) constitute a family of approximately 100 proteases that catalyze the removal of ubiquitin molecules from substrate proteins, thereby reversing ubiquitination signals and regulating protein stability, localization, and function [3] [57]. This dynamic process positions DUBs as critical regulators of cellular homeostasis, influencing diverse processes including cell cycle progression, DNA damage repair, and signal transduction [3]. In cancer, DUB dysregulation is frequently observed, leading to the aberrant stabilization of oncoproteins or destabilization of tumor suppressors [57] [12]. Consequently, the targeted inhibition of specific DUBs has emerged as a promising therapeutic strategy to disrupt key survival pathways in cancer cells [3] [57].
The development of small-molecule DUB inhibitors represents a rapidly advancing frontier in oncology drug discovery. These compounds aim to achieve high potency and selectivity for specific DUB family members, with several candidates now progressing through clinical and preclinical development [58] [59]. This technical guide provides a comprehensive overview of the current landscape of small-molecule DUB inhibitors, detailing screening methodologies, candidate compounds, and the underlying signaling pathways they modulate in the context of cancer research.
Current Landscape of DUB Inhibitors in Oncology
The DUB inhibitor pipeline features a diverse array of compounds targeting various DUB families, with most candidates in early-stage development. The following table summarizes key candidate compounds currently under investigation.
Table 1: Selected Small-Molecule DUB Inhibitors in Development
| Compound/Program | Target | Developed By | Development Stage | Key Indications/Cancer Types |
|---|---|---|---|---|
| KSQ-4279 | USP1 | KSQ Therapeutics/Roche | Phase I | Solid Tumors [58] [59] |
| MTX325 | USP30 | Mission Therapeutics | Phase I | Parkinson's Disease; Oncology [58] |
| MTX652 | USP30 | Mission Therapeutics | Phase I | Oncology [58] [60] |
| TNG348 | USP1 | Tango Therapeutics | Phase I | BRCA-mutant cancers [58] [59] |
| OAT-4828 | USP7 | Molecure | Preclinical | Oncology [58] |
| ARN12502 | USP14 | Academic Research | Preclinical (Hit Compound) | Ovarian Carcinoma, Cisplatin Resistance [61] |
| VLX1570 | USP14/UCHL5 | Vivolux | Clinical Trial Terminated | Multiple Myeloma [58] [57] |
Most advanced DUB inhibitors, such as KSQ-4279 and TNG348, target USP1, a DUB that plays a critical role in the DNA damage response by regulating the stability of key proteins like ID1 and PCNA [58] [59]. This makes USP1 inhibition a promising strategy for targeting cancers with deficiencies in DNA repair pathways, such as those harboring BRCA mutations [3]. Another prominent target is USP30, a mitochondrial DUB that regulates mitophagy. Mission Therapeutics is developing MTX325 and MTX652 as first-in-class inhibitors of USP30 [58] [60]. Furthermore, DUBs like USP7, USP14, and UCHL5 are also active targets, with inhibitors in various stages of development aiming to modulate the stability of oncogenic clients like p53, AKT, and HIF-1α [3] [61] [57].
Despite growing interest, the clinical advancement of DUB inhibitors has faced challenges. VLX1570, an inhibitor of USP14 and UCHL5, progressed to Phase I/II trials for multiple myeloma but was subsequently terminated due to toxicity concerns, highlighting the critical need for improved selectivity in this drug class [57]. As of the most recent data in 2025, no DUB inhibitors have yet received market approval [3] [57].
Screening and Discovery Methods for DUB Inhibitors
The identification of potent and selective DUB inhibitors requires robust, DUB-specific screening cascades designed to eliminate false positives and focus on genuine drug candidates from the outset.
Biochemical and Cell-Based Screening Cascades
Mission Therapeutics's proprietary platform exemplifies a rigorous screening cascade. Key steps include [60]:
- Primary Screening: Screening compound libraries against full-length DUBs purified from mammalian cells to ensure proper folding, post-translational modifications, and the presence of necessary co-factors.
- Physiologically Relevant Assays: Employing substrates that closely mimic natural conditions, such as ubiquitin chains incorporating isopeptide linkages or peptides derived from the DUB's cellular target.
- Orthogonal Confirmatory Assays: Using multiple secondary assays to eliminate false positives early in the process.
- Cellular Target Engagement: Performing proprietary cellular assays as early as possible to confirm specific DUB inhibition within the complex cellular environment.
This iterative "design-make-test" cycle, driven by medicinal chemistry and guided by molecular modeling and structural biology, accelerates the discovery of optimized lead compounds [60].
Specific Screening Protocols: A Case Study of USP14 Inhibitor Discovery
A recent study aimed at identifying USP14 inhibitors for overcoming cisplatin resistance in ovarian carcinoma provides a detailed example of an experimental screening workflow [61]:
- Assay Principle: An optimized hydrolysis assay measuring USP14's deubiquitinating activity was used for primary screening.
- Library: A library of 1,056 small molecules was screened.
- Hit Identification: Compounds were screened at a final concentration of 20 µM. From this, five candidate molecules were identified, with ARN12502 showing the strongest inhibitory activity.
- Potency Determination: The half-maximal inhibitory concentration (IC50) of ARN12502 was determined to be 18.4 µM.
- Binding Mode Validation: Docking and molecular dynamics simulations were employed to predict and confirm stable binding modes of ARN12502 within the USP14 catalytic domain.
- Functional Cellular Assay: In proteasome sensor-expressing cells, ARN12502 demonstrated functional proteasome-inhibitory activity, validating its on-target effect [61].
This workflow, from biochemical screening to cellular validation and computational analysis, represents a standard approach for triaging and validating initial hits in the DUB inhibitor discovery pipeline.
The Scientist's Toolkit: Key Research Reagent Solutions
The following table outlines essential reagents and tools utilized in DUB inhibitor discovery and validation, as evidenced by recent protocols.
Table 2: Key Research Reagents for DUB Inhibitor Screening and Validation
| Reagent / Tool | Function / Application | Example in Use |
|---|---|---|
| Full-Length DUB Proteins | Biochemically relevant enzymes for primary screening; purified from mammalian systems to ensure native conformation and co-factors. | Mission Therapeutics purifies full-length DUBs for its screening cascade [60]. |
| Ubiquitin-Based Probes | Tool compounds for profiling DUB activity and selectivity; e.g., Ubiquitin Vinyl Sulfone (UbVS) for irreversible inhibition and mechanistic studies. | UbVS is used as a non-selective pan-DUB inhibitor tool compound [57]. |
| Cellular Target Engagement Assays | Proprietary or published cell-based assays to confirm that a compound engages its intended DUB target in a live-cell context. | Mission Therapeutics uses these assays early in the discovery process [60]. |
| Specialized Compound Libraries | Libraries containing proprietary chemotypes optimized for DUB targets; e.g., covalent inhibitors with low-reactivity functional groups. | Mission Therapeutics's library of >17,000 molecules with exclusive chemotypes [60]. |
| siRNA/shRNA Knockdown Tools | Functional genomics tools for target validation; used to mimic pharmacological inhibition and assess DUB's role in disease phenotypes. | Used in ovarian carcinoma study to validate USP14's role in cisplatin resistance [61]. |
Key Signaling Pathways and Therapeutic Applications
DUB inhibitors exert their antitumor effects by modulating critical cancer-related signaling pathways. The following diagram illustrates two key pathways targeted by DUB inhibitors in cancer therapy, highlighting the points of intervention.
Diagram 1: Key Cancer-Relevant Signaling Pathways Targeted by DUB Inhibitors. USP1 inhibition disrupts the DNA damage response, while USP30 inhibition promotes the clearance of damaged mitochondria.
Targeting the DNA Damage Response (DDR)
The USP1-UAF1 complex is a key regulator of the DNA damage response. USP1 deubiquitinates and stabilizes proteins like ID1 and PCNA, which are crucial for DNA replication and repair in the face of genomic insult [3]. In cancers with inherent DNA repair deficiencies (e.g., BRCA-mutant cancers), the inhibition of USP1 creates a state of "synthetic lethality." Inhibitors such as KSQ-4279 and TNG348 block USP1 activity, leading to the degradation of its substrate proteins, collapse of DNA replication forks, and ultimately, cancer cell death [58] [59]. This mechanism offers a promising therapeutic strategy for a defined patient population.
Modulating Mitochondrial Homeostasis and Mitophagy
USP30 is a mitochondrial outer membrane protein that acts as a negative regulator of PINK1-Parkin-mediated mitophagy. By removing ubiquitin chains from mitochondrial proteins, USP30 counteracts Parkin's labeling of damaged mitochondria for clearance [60] [62]. Inhibitors like MTX652 and MTX325 inhibit USP30, thereby promoting the ubiquitination of mitochondrial substrates, enhancing mitophagy, and eliminating dysfunctional mitochondria [58] [60]. This is particularly relevant in cancer, as many tumors rely on functional mitochondria for energy and biosynthesis. Furthermore, this pathway is also being explored in neurodegenerative diseases like Parkinson's disease, where impaired mitophagy is a key pathological feature [62].
Challenges and Future Perspectives in DUB Inhibitor Development
The development of selective small-molecule DUB inhibitors faces several significant challenges. The high structural conservation among DUB active sites makes achieving selectivity for a single DUB member a primary hurdle, as off-target inhibition could lead to adverse effects [3] [57]. Furthermore, a lack of in-depth studies on the natural regulatory mechanisms of many DUBs complicates predicting the full biological consequences of their inhibition [58] [59]. The previous clinical termination of VLX1570 due to safety concerns underscores the critical importance of addressing these selectivity and toxicity issues [57].
Future directions in the field are evolving to overcome these challenges. Novel screening technologies and the use of more physiologically relevant assays are being employed to improve the quality of lead compounds [3] [60]. Targeted protein degradation approaches, such as Proteolysis-Targeting Chimeras (PROTACs), are being explored to target DUBs themselves. This modality offers potential advantages over traditional inhibition, including catalytic efficacy and the ability to target non-enzymatic scaffolding functions [3] [57]. Finally, the development of Deubiquitinase-Targeting Chimeras (DUBTACs) aims to stabilize specific proteins by recruiting them to a DUB, opening up a new therapeutic modality for diseases caused by haploinsufficiency [3].
Continued research into DUB biology, coupled with advanced screening and drug design technologies, is poised to overcome current limitations and unlock the full therapeutic potential of DUB-targeted agents in oncology and beyond.
The ubiquitin-proteasome system (UPS) represents a crucial regulatory pathway for maintaining protein homeostasis in eukaryotic cells, with its dysregulation implicated in numerous diseases, particularly cancer. Within this landscape, two transformative technologies have emerged: Proteolysis-Targeting Chimeras (PROTACs) for targeted protein degradation and Deubiquitinase-Targeting Chimeras (DUBTACs) for targeted protein stabilization. These heterobifunctional molecules represent a paradigm shift from traditional occupancy-based inhibitors to event-driven therapeutic modalities [63] [64].
While PROTACs harness the ubiquitin-proteasome system to eliminate disease-causing proteins, DUBTACs leverage deubiquitinating enzymes (DUBs) to rescue protective proteins from aberrant degradation. For cancer research, where loss of tumor suppressor function is a hallmark of disease pathogenesis, DUBTAC technology offers a novel approach to restore protective protein function that remains largely unaddressed by conventional therapeutic strategies [63] [65]. This technical guide comprehensively examines both platforms, with particular emphasis on their mechanistic basis, research applications, and integration within cancer research frameworks focused on DUB biology.
Deubiquitinating Enzymes (DUBs): Critical Regulators in Cancer Biology
Deubiquitinating enzymes (DUBs) constitute a family of approximately 100 proteases that cleave ubiquitin conjugates from protein substrates, thereby counterregulating the activity of E3 ubiquitin ligases [11] [66]. DUBs are categorized into six major families based on sequence and structural similarity: ubiquitin-specific proteases (USPs), ovarian tumor proteases (OTUs), ubiquitin carboxy-terminal hydrolases (UCHs), Machado-Josephin domain-containing proteases (MJDs), motif-interacting with ubiquitin-containing novel DUB family (MINDYs), and JAB1, MPN, MOV34 family (JAMMs) [4].
In cancer biology, DUBs function as critical regulators of tumor suppression and oncogenesis through their influence on key cellular processes including cell cycle progression, apoptosis, DNA damage repair, and metabolic reprogramming [11]. The table below summarizes several DUBs with established roles in cancer pathogenesis:
Table 1: Cancer-Relevant Deubiquitinating Enzymes and Their Functions
| DUB | Substrate(s) | Role in Cancer | Associated Cancers |
|---|---|---|---|
| BAP1 | H2A | Tumor suppressor | Mesothelioma, melanoma, renal carcinoma [4] |
| CYLD | TRAF2/6, NEMO | Tumor suppressor | Cylindromatosis, trichoepithelioma [11] |
| USP7 | MDM2, p53 | Oncogenic | Multiple (stabilizes MDM2 to downregulate p53) [66] |
| USP9X | Multiple | Context-dependent | Pancreatic cancer (suppressor or promoter) [4] |
| USP28 | c-Myc, FOXM1 | Oncogenic | Pancreatic ductal adenocarcinoma [4] [66] |
| OTUB1 | Multiple | Stabilizer for DUBTACs | Multiple cancer types [65] |
DUBs manifest both tumor-promoting and tumor-suppressive functions in a context-dependent manner. For instance, USP9X demonstrates this duality particularly well in pancreatic ductal adenocarcinoma (PDAC), where it functions as a tumor suppressor in KPC (KrasLSL-G12D/+; Trp53LSL-R172H/+; Pdx1-Cre) mouse models but promotes tumor cell survival in human pancreatic cancer cell lines [4]. This functional complexity underscores the importance of understanding specific DUB biological contexts when developing targeted therapies.
PROTACs: Targeted Protein Degradation Technology
Mechanistic Basis of PROTACs
PROTACs are heterobifunctional molecules consisting of three key components: a ligand that binds the protein of interest (POI), a ligand that recruits an E3 ubiquitin ligase, and a linker connecting these two moieties [64]. The molecular mechanism involves the simultaneous binding of both target protein and E3 ligase, forming a productive POI-PROTAC-E3 ligase ternary complex. This complex enables the transfer of ubiquitin chains from the E2 ubiquitin-conjugating enzyme to the target protein, marking it for recognition and degradation by the 26S proteasome [63] [64].
Unlike traditional small-molecule inhibitors that require occupancy of active sites and often face limitations due to compensatory overexpression or mutations, PROTACs operate catalytically through an "event-driven" mechanism. A single PROTAC molecule can theoretically mediate multiple rounds of degradation, offering potential advantages in potency, duration of effect, and the ability to target proteins without traditional druggable binding pockets [64].
Research and Clinical Applications
PROTAC technology has demonstrated remarkable success in targeting previously "undruggable" proteins, including transcription factors and scaffolding proteins. The technology has advanced rapidly toward clinical application, with approximately 20 PROTAC candidates currently in clinical trials [63].
Notable examples include:
- ARV-471 (Vepdegestrant): An estrogen receptor (ER) degrader in Phase III clinical trials for ER+/HER2− breast cancer (NCT05909397, NCT05654623) [63]
- ASP3082: A first-in-class KRAS G12D protein degrader showing promising results in Phase I trials for non-small cell lung cancer (NSCLC) with 37.5% objective response rate and 78% average degradation of KRAS G12D at the 600 mg dose [67]
- ARV-806: A preclinical PROTAC KRAS G12D degrader that engages both GTP-bound active and GDP-bound inactive forms of KRAS G12D, demonstrating subnanomolar potency across multiple cancer cell lines and tumor regressions in xenograft models [67]
Table 2: E3 Ligases Commonly Exploited in PROTAC Design
| E3 Ligase | Ligand | Key Features | Example Applications |
|---|---|---|---|
| Von Hippel-Lindau (VHL) | VH032 | First small-molecule ligand developed in 2012; binds HIF-1α site | ERα degraders; RTK degradation [64] |
| Cereblon (CRBN) | Thalidomide derivatives | Extensive clinical validation; immunomodulatory imide drugs | BET degraders (e.g., MZ1) [64] |
| MDM2 | Nutlin | Key regulator of p53 tumor suppressor | First small-molecule PROTAC (2008) targeting AR [64] |
| cIAP1 | Methyl bestatin (MeBS) | Can induce autoubiquitination and degradation of itself | SNIPERs for BCR-ABL and AR degradation [64] |
Figure 1: PROTAC Mechanism of Action. PROTAC molecules simultaneously bind to the target protein and recruit E3 ubiquitin ligases, facilitating ubiquitination and subsequent proteasomal degradation of the protein of interest.
DUBTACs: Targeted Protein Stabilization Technology
Conceptual Foundation and Mechanism
While PROTACs promote protein degradation, many disease states are characterized by loss-of-function mutations or reduced expression of protective proteins, necessitating stabilization rather than elimination. DUBTAC technology addresses this therapeutic need by leveraging the native deubiquitination system to rescue proteins from aberrant degradation [63] [65].
DUBTACs similarly consist of three components: a ligand for the protein of interest, a ligand for a specific deubiquitinating enzyme, and a connecting linker. The mechanism involves formation of a POI-DUBTAC-DUB ternary complex that brings the DUB into proximity with the target protein, enabling removal of ubiquitin chains and preventing proteasomal recognition [63]. This approach is particularly relevant for stabilizing tumor suppressor proteins—such as p53, VHL, and KEAP1—whose functional loss drives cancer pathogenesis [65].
Proof-of-Concept Studies and Research Applications
The DUBTAC platform, though more recently developed than PROTAC technology, has demonstrated significant potential in preclinical studies. Notable advances include:
Stabilization of Tumor-Suppressive E3 Ligases: A groundbreaking study published in the Journal of the American Chemical Society (2025) established a PRO-DUBTAC platform for stabilizing tumor-suppressive E3 ubiquitin ligases [65]. Researchers developed two series of PRO-DUBTACs—VHL-DUBTAC and KEAP1-DUBTAC—that effectively stabilized VHL and KEAP1 proteins in cells in an OTUB1-dependent manner. These molecules conjugated E3 ligase ligands (VH032 for VHL) with a covalent OTUB1 ligand (MS5105) via optimized linkers.
Key Findings:
- Compounds V6 (MS4170) and V8 (MS4172) demonstrated concentration- and time-dependent VHL stabilization with concomitant reduction of HIF-1α levels
- Stabilization effects were abolished by cotreatment with either VHL ligand VH032 or OTUB1 ligand MS5105, confirming target specificity
- OTUB1 depletion blocked VHL stabilization, establishing DUB dependency
- Negative control compounds with modified ligands showed no stabilization effect
Therapeutic Potential: This approach opens new avenues for cancer therapy by harnessing the tumor-suppressive potential of E3 ligases themselves. For example, VHL stabilization reactivates its function in degrading HIF-1α, subsequently reducing expression of downstream targets like VEGF, GLUT1/3, and PKM2—critical drivers of tumor angiogenesis and metabolism [65].
Figure 2: DUBTAC Mechanism of Action. DUBTAC molecules recruit deubiquitinating enzymes to target proteins, removing ubiquitin chains and preventing degradation, thereby stabilizing proteins with protective functions.
Experimental Protocols and Methodologies
PRO-DUBTAC Development Protocol (Based on VHL-DUBTAC Study)
The following protocol outlines the key methodological steps for developing and validating PRO-DUBTACs, based on the recently published stabilization of tumor-suppressive E3 ligases [65]:
Step 1: Ligand Selection and Characterization
- Select appropriate target protein ligands with confirmed binding specificity (e.g., VH032 for VHL with Kd values in nanomolar range)
- Choose DUB ligands with established potency and selectivity (e.g., MS5105 for OTUB1)
- Confirm binding through pulldown assays: incubate biotinylated ligands (e.g., Biotin-VHL-ligand) with cell lysates or recombinant protein; capture with streptavidin beads; detect binding via Western blot
- Validate ligand specificity using wild-type versus mutant proteins (e.g., VHL L158S mutant)
Step 2: Linker Optimization and Compound Synthesis
- Design linkers of varying composition, length, and flexibility
- Conjugate POI ligand and DUB ligand via synthetic chemistry approaches
- Generate compound series with systematic linker variations (e.g., V1-V12 for VHL-DUBTAC)
- Include negative controls with inactive ligand enantiomers or binding-deficient analogs
Step 3: Functional Screening and Validation
- Treat relevant cell lines (e.g., HeLa cells for VHL-DUBTAC) with compound series (typical concentration range: 0.1-10 μM, time course: 0-48 hours)
- Assess target protein stabilization via Western blot (e.g., VHL antibody)
- Measure downstream functional effects (e.g., HIF-1α reduction for VHL-DUBTAC)
- Confirm mRNA levels unchanged via qRT-PCR to rule out transcriptional effects
Step 4: Mechanism of Action Studies
- Demonstrate ternary complex formation through co-immunoprecipitation (e.g., enhanced VHL-OTUB1 interaction with MS4170 treatment)
- Perform competition experiments with free ligands (VH032 or MS5105) to abolish stabilization
- Validate DUB dependency using CRISPR/Cas9 knockout or siRNA knockdown of the recruited DUB
- Test negative control compounds to confirm specificity
Step 5: Functional Consequences Assessment
- Evaluate effects on downstream pathways (e.g., HIF-1α targets VEGF, GLUT1, PKM2 via qRT-PCR)
- Assess phenotypic outcomes (e.g., tumor cell growth retardation in viability assays)
- Conduct proteomic analysis to identify global protein changes (e.g., mass spectrometry for HIF-1α targets NDRG1 and TFRC)
DUBTAC Specificity and Validation Protocols
Rigorous validation of DUBTAC specificity requires multiple orthogonal approaches:
Genetic Dependency Tests:
- Utilize CRISPR-Cas9 knockout libraries targeting DUB families (e.g., 81-member DUB CRISPR-Cas9 library)
- Measure dependency scores across cancer cell lines using resources like Dependency Map (DepMap)
- Confirm DUBTAC resistance in DUB-knockout cells
Transcriptomic Profiling:
- Employ Connectivity Map (CMap) database analysis to compare transcriptional signatures
- Identify genes with similar knockout or inhibition profiles
- Validate pathway-specific effects through RNA sequencing
Selectivity Screening:
- Profile against panels of recombinant DUBs to assess off-target engagement
- Utilize activity-based protein profiling (ABPP) with broad-spectrum DUB probes
- Confirm selective stabilization of intended POI without effects on related proteins
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Essential Research Reagents for DUBTAC and PROTAC Development
| Reagent/Category | Specific Examples | Function/Application | Key Characteristics |
|---|---|---|---|
| E3 Ligase Ligands | VH032 (VHL), Thalidomide derivatives (CRBN), Nutlin (MDM2) | Recruit E3 ubiquitin machinery in PROTACs | Well-characterized binding, nanomolar affinity [64] |
| DUB Ligands | MS5105 (OTUB1), FT671 (USP7), HBX 41,108 (USP7) | Recruit deubiquitinases in DUBTACs | Covalent or high-affinity non-covalent binders [65] [66] |
| Linker Chemistry | PEG chains, alkyl chains, piperazine-based | Connect warhead ligands | Optimized length and composition for ternary complex formation [65] |
| Validation Tools | Biotinylated ligands, CRISPR DUB libraries, DUB inhibitors | Mechanism of action studies | Confirm target engagement and functional specificity [65] [66] |
| Cell Line Models | Cancer cell lines with specific mutations (e.g., KRAS G12D, VHL loss) | Functional testing | Context-dependent response assessment [67] [65] |
| Analytical Methods | Western blot, co-IP, mass spectrometry, qRT-PCR | Efficacy and mechanism assessment | Quantify protein levels, complex formation, pathway effects [65] |
Quantitative Comparison of PROTAC and DUBTAC Platforms
Table 4: Comparative Analysis of PROTAC and DUBTAC Technologies
| Parameter | PROTACs | DUBTACs |
|---|---|---|
| Primary Mechanism | Induce ubiquitination and degradation | Remove ubiquitin and prevent degradation |
| Therapeutic Application | Reduce oncoproteins, mutated proteins | Stabilize tumor suppressors, protective proteins |
| Key Components | POI ligand + E3 ligase ligand + linker | POI ligand + DUB ligand + linker |
| Catalytic Nature | Event-driven, sub-stoichiometric activity | Event-driven, sub-stoichiometric activity |
| Clinical Status | Advanced (20+ in clinical trials) | Preclinical development |
| Validated Targets | KRAS G12D, AR, ER, BRD4 [67] | VHL, KEAP1, CFTR, cGAS [65] |
| E3/DUB Engaged | VHL, CRBN, MDM2, cIAP1 [64] | OTUB1, other DUBs under investigation |
| Key Challenges | Selectivity, pharmacokinetics, resistance | Limited DUB ligands, stabilization control |
PROTAC and DUBTAC technologies represent complementary approaches in the targeted protein regulation landscape, with particular relevance for cancer research focused on DUB biology. While PROTACs have demonstrated clinical validation for degrading disease-driving proteins, DUBTACs offer a novel strategy for addressing pathological protein insufficiency—a particularly valuable approach for restoring tumor suppressor function.
The convergence of these technologies with multi-omics approaches—including functional genomics screens (DepMap), transcriptomic profiling (CMap), and proteomic analyses—will accelerate the identification of context-specific DUB dependencies and optimal therapeutic applications [66]. Furthermore, the emerging integration of nanotechnology with TPD systems promises to address current challenges in bioavailability, tissue specificity, and therapeutic efficacy [68].
For cancer researchers, these technologies provide powerful chemical biology tools to probe DUB function and manipulate specific nodes in the ubiquitin-proteasome system. As DUBTAC technology matures and additional DUB-chemical ligands are developed, the platform holds exceptional promise for addressing the significant portion of human cancers driven by loss of tumor suppressor function through targeted stabilization of protective proteins.
Overcoming Challenges in DUB-Targeted Cancer Therapy
Deubiquitinating enzymes (DUBs), a family of approximately 100 proteases in humans, are critical regulators of the ubiquitin-proteasome system that cleave ubiquitin moieties from protein substrates, thereby reversing ubiquitination signals [51] [66]. This reversible modification governs protein stability, localization, and interaction networks, positioning DUBs as key regulators in fundamental cellular processes and disease pathways, particularly in oncology [69] [70]. The therapeutic potential of DUB inhibition is substantial, offering strategies to indirectly target proteins traditionally considered "undruggable," such as transcription factors and scaffolding proteins [66]. However, the development of selective DUB inhibitors faces significant specificity hurdles stemming from structural conservation across DUB families, the complexity of ubiquitin chain recognition, and the intricate regulation of DUB activity within cellular contexts. Overcoming these challenges requires a multidisciplinary approach combining advanced structural biology, innovative screening methodologies, and sophisticated chemical biology.
The Structural and Functional Landscape of DUB Families
Classification and Catalytic Mechanisms
DUBs are classified into seven structurally distinct families based on their catalytic domains and mechanisms: ubiquitin-specific proteases (USP), ubiquitin C-terminal hydrolases (UCH), ovarian tumor proteases (OTU), Machado-Josephin domain proteases (MJD), motif interacting with ubiquitin-containing novel DUB family (MINDY), JAB1/MPN/Mov34 metalloenzymes (JAMM), and zinc finger-containing ubiquitin peptidases (ZUFSP) [51]. The majority of DUB families (USP, UCH, OTU, MJD, MINDY) function as cysteine proteases featuring a canonical catalytic triad composed of cysteine, histidine, and aspartic acid or glutamic acid residues. In contrast, the JAMM family represents the only metal-dependent DUBs, utilizing a zinc-dependent metalloprotease mechanism for isopeptide bond hydrolysis [51]. This fundamental mechanistic division informs inhibitor design strategies, with cysteine-targeting electrophiles applicable to most DUB families but ineffective against JAMM proteases.
DUB Classification and Catalytic Mechanisms
Structural Determinants of Specificity
Beyond the catalytic core, DUBs contain specialized domains that govern substrate recognition, cellular localization, and regulation. These include zinc-finger (ZnF) motifs, ubiquitin-binding domains (UBD), ubiquitin-like domains (UBL), coiled-coil domains, and ubiquitin interaction motifs (UIM) that work cooperatively with catalytic domains to achieve precise hydrolysis control [51]. The USP family, comprising over 50 members, exemplifies this structural complexity with conserved USP domains containing the catalytic triad flanked by variable insertion sequences and accessory domains that confer functional diversity [51]. For instance, USP7 features an N-terminal TRAF-like domain and five C-terminal UBL domains that contribute to substrate recognition and specificity determination [51]. This modular architecture presents both challenges and opportunities for inhibitor development—while the conserved catalytic sites complicate selective targeting, the diverse auxiliary domains offer potential for allosteric modulation and selective interaction interfaces.
Table 1: Human DUB Families and Characteristic Features
| DUB Family | Catalytic Type | Representative Members | Characteristic Domains | Linkage Preference |
|---|---|---|---|---|
| USP | Cysteine protease | USP7, USP14, USP22 | USP domain, UBL, ZnF | Broad specificity |
| OTU | Cysteine protease | OTUB1, OTUD1, A20 | OTU domain | Variable (K11, K48, K63) |
| UCH | Cysteine protease | UCHL1, UCHL3 | UCH domain | Monoubiquitin, small adducts |
| MJD | Cysteine protease | Ataxin-3, JOSD1, JOSD2 | MJD domain | K63-linked chains |
| MINDY | Cysteine protease | MINDY1, MINDY2 | MINDY domain | K48-linked chains |
| JAMM | Zinc metalloprotease | BRCC3, AMSH, MPND | JAMM/MPN domain | K63-linked chains |
| ZUFSP | Cysteine protease | ZUFSP | ZUFSP domain | K63-linked chains |
The Specificity Challenge: Structural and Functional Perspectives
Conservation of Active Sites
The high degree of structural conservation across DUB active sites represents the most significant hurdle in developing selective inhibitors. Cysteine-based DUBs share a common catalytic triad geometry, while JAMM family metalloproteases conserve the zinc-coordinating residues essential for their mechanism [51]. This conservation is particularly pronounced within DUB subfamilies; for example, USP family members exhibit substantial homology in their catalytic USP domains, making the development of selective inhibitors that distinguish between closely related USPs exceptionally challenging. Early-generation DUB inhibitors frequently exhibited pan-family activity due to this structural conservation, limiting their therapeutic utility and increasing the potential for off-target effects. The problem is compounded by the fact that conventional substrate-competitive inhibitors target these conserved active sites, creating an inherent selectivity barrier that demands innovative approaches beyond active-site targeting.
Diversity of Ubiquitin Chain Recognition
Despite active site conservation, DUBs demonstrate remarkable specificity in biological contexts through differential recognition of ubiquitin chain types and substrates. Systematic profiling of 42 human DUBs against all possible diubiquitin linkages revealed striking differences in specificity patterns across families [71]. While certain DUBs like OTULIN (M1/linear-specific), OTUB1 (K48-specific), and AMSH (K63-specific) exhibit exquisite linkage selectivity, most USP family members display broad specificity across multiple linkage types [71]. This diversity stems from specialized ubiquitin-binding domains and surface epitopes that determine chain-type recognition. For drug discovery, this creates a paradoxical situation—targeting the catalytic site often yields broad inhibition across multiple DUBs, while targeting chain-recognition domains may preserve catalytic activity but block specific cellular functions. Successful inhibitor strategies must therefore account for both catalytic inhibition and context-specific functional blockade.
Table 2: DUB Specificity Profiling Against Ubiquitin Linkages
| Specificity Group | Representative DUBs | Linkage Preference | Inhibitor Development Implications |
|---|---|---|---|
| Highly specific | OTULIN, OTUB1, AMSH, AMSH-LP, BRCC3 | Single linkage (M1, K48, or K63) | Favorable for therapeutic targeting; clear functional outcomes |
| Context-dependent specific | Cezanne, OTUD1, A20, TRABID | Preferred linkages (K11, K48, K63, K29/K33) | Cellular context crucial for inhibitor efficacy prediction |
| Broad specificity | Most USP family members | Multiple linkages | High risk of off-target effects; challenging therapeutic development |
Complex Cellular Regulation and Compensation Mechanisms
DUB function is precisely regulated through multiple mechanisms including protein-protein interactions, post-translational modifications, subcellular localization, and tissue-specific expression patterns. For example, USP1 requires complex formation with UAF1 for full enzymatic activity, while CDK-mediated phosphorylation regulates its stability and function [72]. This multi-layered regulation means that DUB inhibition consequences are highly context-dependent, varying by cell type, physiological state, and disease status. Additionally, functional redundancy within the DUB family enables compensatory mechanisms where inhibition of one DUB may be offset by increased activity of related enzymes, potentially diminishing therapeutic efficacy. These regulatory complexities necessitate thorough target validation across relevant disease models and careful consideration of potential resistance mechanisms during inhibitor development.
Advanced Methodologies for Selective Inhibitor Development
High-Throughput Screening Platforms
Innovative screening technologies have emerged to address DUB inhibitor specificity challenges. The MALDI-TOF mass spectrometry-based DUB assay represents a significant advancement, enabling sensitive quantification of DUB activity and specificity using unmodified diubiquitin substrates [71]. This method utilizes 15N-labeled ubiquitin as an internal standard to precisely measure ubiquitin generation from specific diubiquitin topoisomers, achieving a lower quantification limit of 10 nM (2 fmol on target) with high linearity (r² ≥ 0.99) over a 500-fold concentration range [71]. The assay's miniaturized format reduces enzyme and substrate requirements dramatically compared to traditional methods, facilitating comprehensive profiling of inhibitor specificity across multiple DUBs and linkage types. This platform has been successfully deployed to characterize the linkage specificity of 42 human DUBs and profile 11 inhibitory compounds against 32 DUBs, providing an extensive resource for selectivity assessment [71].
MALDI-TOF MS DUB Screening Workflow
Targeted Library Design and Synthesis
Structure-guided library design focused on privileged chemotypes for DUBs has emerged as a powerful strategy to enhance selectivity. Recent advances include high-throughput synthesis-to-screening approaches for constructing DUB-focused compound libraries featuring cyanimide warheads, which demonstrated success in identifying selective inhibitors for mUSP18 with 35 nM potency [73]. This integrated method utilizes acoustic liquid handling for nanoliter-scale compound synthesis directly in 1536-well plates, enabling rapid generation and screening of 7,536 cyanimide compounds against twelve ubiquitin(-like) proteases [73]. The approach addresses key limitations of conventional library screening by minimizing compound requirements and directly coupling synthesis with biological assessment. The resulting first-in-class mUSP18 inhibitor (BB07CA902) exhibited exceptional specificity, inhibiting only mUSP18 across a panel of 41 DUBs and effectively modulating cellular ISGylation [73]. This demonstrates the potential of targeted library strategies coupled with innovative screening methodologies to overcome selectivity hurdles.
Multi-Omics Integration for Functional Annotation
Systematic integration of diverse functional genomics datasets provides critical context for predicting inhibitor efficacy and potential toxicity. A comprehensive multi-omics analysis combined CRISPR-Cas9 knockout screens, transcriptomic profiling, proteomic data from the Cancer Cell Line Encyclopedia (CCLE), and protein-protein interaction networks to elucidate DUB functions and co-dependencies [66]. This integrative approach enabled the identification of context-specific DUB essentiality, substrate relationships, and potential biomarkers for predicting inhibitor response. The resulting DUB Portal resource facilitates hypothesis generation about DUB functions and prioritization of therapeutic targets, addressing the significant knowledge gap that has hampered DUB drug development [66]. By contextualizing DUB inhibition within broader cellular networks, these functional maps guide the development of selective inhibitors with predictable physiological effects and inform combination strategies to overcome compensatory mechanisms.
Current Clinical Pipeline and Therapeutic Applications
Emerging DUB Inhibitors in Development
The DUB inhibitor clinical pipeline is rapidly expanding, with several candidates entering early-phase trials for oncology indications. Key companies actively developing DUB inhibitors include Mission Therapeutics, KSQ Therapeutics, Tango Therapeutics, Molecure, and Cothera Bioscience, among others [59]. Notable candidates in development include KSQ-4279 (USP1 inhibitor) being advanced by KSQ Therapeutics in partnership with Roche, MTX325 and MTX652 (USP30 inhibitors) from Mission Therapeutics, TNG348 (USP1 inhibitor) from Tango Therapeutics, and OAT-4828 from Molecure [59]. The clinical progression of these candidates demonstrates growing confidence in targeting DUBs therapeutically, though selectivity remains a critical differentiator in their development prospects. Most candidates are in early development phases (preclinical or Phase I), reflecting the nascent state of the field and the technical challenges in achieving therapeutic windows through selective DUB inhibition.
Table 3: Selected DUB Inhibitors in Clinical Development
| Compound | Target | Developer | Development Stage | Indication Focus |
|---|---|---|---|---|
| KSQ-4279 | USP1 | KSQ Therapeutics/Roche | Phase I | Advanced solid tumors |
| MTX325 | USP30 | Mission Therapeutics | Preclinical/Phase I | Parkinson's disease, cancer |
| MTX652 | USP30 | Mission Therapeutics | Preclinical | Kidney disease, cancer |
| TNG348 | USP1 | Tango Therapeutics | Phase I | BRCA-deficient tumors |
| OAT-4828 | Undisclosed | Molecure | Discovery/Preclinical | Not specified |
| Sepantronium (YM155) | USP1? | Cothera Bioscience | Clinical (repurposing) | Cancer |
Therapeutic Applications in Oncology
DUB inhibitors offer novel approaches to target key oncogenic drivers and therapy resistance mechanisms in cancer. USP1 inhibition has emerged as a promising strategy in BRCA1-deficient cancers, where it is required for replication fork protection, and USP1 inhibitors can overcome PARP inhibitor resistance in preclinical models [72]. Additionally, USP7 inhibition represents an indirect strategy to activate p53 tumor suppressor function by destabilizing its negative regulator MDM2, offering an approach to target the frequently dysregulated p53 pathway in cancer [66]. USP28 inhibition has been proposed to target c-Myc stability, potentially addressing this challenging oncogene [66]. Beyond direct anti-tumor effects, DUB inhibitors are being explored for immunomodulatory applications, as evidenced by the role of USP18 in regulating interferon signaling and immune responses [73]. The expanding understanding of DUB functions in tumorigenesis, metastasis, and therapy resistance continues to reveal new therapeutic applications for selective DUB inhibitors in oncology.
The Scientist's Toolkit: Essential Research Reagents and Methodologies
Table 4: Essential Research Tools for DUB Inhibitor Development
| Reagent/Method | Function/Application | Key Features | References |
|---|---|---|---|
| MALDI-TOF MS DUB assay | Quantitative DUB activity and specificity screening | Uses unmodified diubiquitin substrates; 15N-ubiquitin internal standard; high sensitivity (LLOQ: 10 nM) | [71] |
| Diubiquitin topoisomers | Substrates for specificity profiling | All 8 linkage types (M1, K6, K11, K27, K29, K33, K48, K63); native isopeptide bonds | [71] |
| Cyanimide-focused libraries | Targeted compound collections for DUB screening | DUB-privileged chemotype; enables rapid SAR exploration | [73] |
| DUB-focused CRISPR libraries | Functional genomics and target validation | Arrayed or pooled formats; enables essentiality screening | [66] |
| Activity-based probes (ABPs) | Profiling DUB activity and engagement | Covalent modifiers (Ub-VME, Ub-VS); assess target engagement | [71] |
| DepMap/CCLE datasets | Context-specific essentiality and biomarker discovery | CRISPR screens across 700+ cancer cell lines; proteomic data | [66] |
| DUB Portal | Integrated multi-omics resource | Functional annotations; co-dependencies; substrate predictions | [66] |
The development of selective DUB inhibitors represents a frontier in targeted therapy, particularly for oncology applications where DUBs regulate key oncogenic and tumor suppressive pathways. While substantial challenges remain due to structural conservation and functional complexity, innovative approaches in screening technology, library design, and target validation are progressively overcoming these hurdles. The emerging clinical pipeline demonstrates the therapeutic viability of DUB inhibition and provides valuable learning opportunities for the field. Future progress will likely depend on continued advances in structural biology to identify allosteric sites, improved understanding of context-specific DUB functions, and the development of bifunctional molecules that recruit DUBs to specific substrates. As these scientific and technical advances mature, selective DUB inhibitors may ultimately fulfill their potential as transformative therapeutics for cancer and other diseases.
Mechanisms of Drug Resistance Involving DUB Upregulation and Adaptation
Deubiquitinating enzymes (DUBs) have emerged as critical regulators of oncogenic signaling pathways and key mediators of therapeutic resistance in cancer. This whitepaper examines the molecular mechanisms through which DUB upregulation enables cancer cells to evade the cytotoxic effects of chemotherapeutic agents, targeted therapies, and immunotherapies. We systematically analyze how specific DUB families, particularly ubiquitin-specific proteases (USPs) and ovarian tumor proteases (OTUs), confer resistance by stabilizing oncoproteins, enhancing DNA damage repair, preventing apoptosis, maintaining cancer stem cell properties, and regulating immune checkpoint molecules. The clinical implications of these findings are substantial, as DUB inhibition represents a promising strategy to overcome treatment resistance and improve patient outcomes across multiple cancer types. This review also provides experimental frameworks for investigating DUB function and discusses the current landscape of DUB-targeted therapeutic development.
The ubiquitin-proteasome system (UPS) represents a crucial regulatory mechanism for protein degradation and function in eukaryotic cells, with deubiquitinating enzymes (DUBs) serving as key counter-regulatory elements to ubiquitination. Approximately 100 DUBs have been identified in humans, categorized into seven major families based on sequence and structural conservation: ubiquitin-specific proteases (USPs), ovarian tumor proteases (OTUs), ubiquitin C-terminal hydrolases (UCHs), Machado-Josephin domain-containing proteases (MJDs), JAMM/MPN domain-associated metallopeptidases (JAMMs), MINDYs, and ZUFSP [74] [3]. These enzymes cleave ubiquitin chains from substrate proteins, thereby reversing their ubiquitin-mediated fate—whether degradation, altered localization, or modified function [74].
DUBs maintain protein homeostasis by regulating the stability, activity, and interaction networks of numerous cellular proteins. The balanced interplay between ubiquitination and deubiquitination ensures proper control of critical processes including cell cycle progression, DNA damage repair, apoptosis, and signal transduction [74] [20]. However, in cancer, this balance is frequently disrupted. The upregulation or hyperactivation of specific DUBs can lead to the stabilization of oncoproteins, enhancement of DNA repair mechanisms in tumor cells, inhibition of cell death pathways, and promotion of stem-like properties—all contributing to tumor progression and therapeutic resistance [75] [20]. Understanding these mechanisms provides the foundation for targeting DUBs to overcome drug resistance in cancer treatment.
Molecular Mechanisms of DUB-Mediated Drug Resistance
Enhancement of DNA Damage Repair
Cancer therapies such as cisplatin and radiation exert their cytotoxic effects primarily by inducing DNA damage. DUBs contribute to resistance by enhancing the cancer cell's ability to repair this therapy-induced DNA damage.
USP1 forms a complex with UAF1 and promotes resistance to cisplatin in non-small cell lung cancer (NSCLC) by deubiquitinating and stabilizing inhibitor of DNA binding 1 (ID1), thereby facilitating DNA repair and cell survival [75] [3]. USP7 (HAUSP) plays multiple roles in DNA damage response through interactions with key repair proteins. It stabilizes checkpoint kinase 2 (CHK2) by removing its ubiquitin tags, enhancing DNA repair capability and promoting radio-resistance [20]. Additionally, USP7 deubiquitinates and stabilizes DNA damage response mediators such as MDC1 and 53BP1, further enhancing repair efficiency [20].
Table 1: DUBs Involved in DNA Damage Repair-Mediated Drug Resistance
| DUB | Cancer Type | Substrate | Resistance Mechanism | Therapeutic Agent |
|---|---|---|---|---|
| USP1 | Non-small cell lung cancer | ID1 | Enhanced DNA repair | Cisplatin |
| USP7 | Multiple cancers | CHK2, MDC1, 53BP1 | DNA damage response signaling | Radiotherapy, Cisplatin |
| USP51 | Lung cancer | γH2AX | Reduced DNA damage marker formation | Cisplatin |
| USP22 | Lung adenocarcinoma | PALB2, BRCA2 complex | Facilitates homologous recombination | DNA-damaging agents |
| USP39 | Multiple cancers | CHK2 | Stabilizes checkpoint kinase | Chemotherapy |
USP51 is upregulated in cisplatin-resistant lung cancer cells, where it diminishes the formation of γH2AX (a marker of DNA double-strand breaks) and increases CHK1 phosphorylation, enabling effective cell cycle progression despite genotoxic stress [75]. USP22 contributes to robust DNA damage response in lung adenocarcinoma by interacting with PALB2 and facilitating the recruitment of the PALB2-BRCA2-Rad51 complex, thereby enhancing homologous recombination-mediated repair of double-strand breaks [75].
Inhibition of Apoptotic Pathways
Many anticancer agents eliminate cancer cells by inducing apoptotic cell death. DUBs can confer resistance by stabilizing anti-apoptotic proteins or destabilizing pro-apoptotic factors.
USP9X plays a context-dependent role in cancer cell survival. In pancreatic cancer and other malignancies, USP9X deubiquitinates and stabilizes anti-apoptotic proteins such as MCL1, thereby inhibiting apoptosis and promoting resistance to targeted therapies and chemotherapeutic agents [4] [20]. USP24 regulates the stability of cellular FLICE-inhibitory protein (c-FLIP), an anti-apoptotic protein that suppresses death receptor-mediated apoptosis. Elevated USP24 expression leads to c-FLIP accumulation and resistance to death ligand-based therapies [20].
The OTUD1 protein demonstrates the complex regulatory roles DUBs can play in cell death pathways. In esophageal squamous cell carcinoma (ESCC), OTUD1 promotes cell death by cleaving K27-type and K63-type polyubiquitin chains from apoptosis-inducing factor (AIF) on K244, leading to mitochondrial structural disruption and impairment of oxidative phosphorylation [31]. Low OTUD1 expression is associated with chemoresistance and poor prognosis in ESCC patients, highlighting its tumor-suppressive role in this context [31].
Regulation of Cancer Stem Cells (CSCs) and Signaling Pathways
Cancer stem cells represent a subpopulation of tumor cells with self-renewal capacity and enhanced resistance to conventional therapies. DUBs contribute to drug resistance by maintaining the CSC phenotype through regulation of key developmental signaling pathways.
USP22 is recognized as a marker of cancer stem cells and promotes stemness in hepatocellular carcinoma and pancreatic cancer cells [4]. It upregulates p21 expression through PTEN-MDM2-p53 signaling and increases DYRK1A levels, both contributing to enhanced proliferation and stem-like properties in pancreatic ductal adenocarcinoma (PDAC) [4]. USP21 maintains the stemness of PDAC cells by interacting with and stabilizing TCF7, a key transcription factor in the Wnt/β-catenin pathway. In orthotopic pancreatic transplantation models, USP21 expression drives pathological progression from pancreatic intraepithelial neoplasia (PanIN) to PDAC [4].
The Wnt/β-catenin pathway is particularly important in CSC maintenance, and multiple DUBs regulate this pathway. USP28 promotes cell cycle progression and inhibits apoptosis in PDAC cells by stabilizing FOXM1, thereby activating Wnt/β-catenin signaling [4]. Similarly, USP5 extends the half-life of FOXM1 to accelerate PDAC tumor growth and also regulates DNA damage response, cell cycle arrest, and apoptosis to promote tumor formation [4].
Table 2: DUBs Regulating Cancer Stem Cell and Developmental Signaling Pathways
| DUB | Pathway Regulated | Substrate | Biological Outcome | Therapeutic Resistance |
|---|---|---|---|---|
| USP22 | PTEN-MDM2-p53 | PTEN, DYRK1A | Enhanced stemness, proliferation | Chemotherapy, Targeted therapy |
| USP21 | Wnt/β-catenin | TCF7 | Maintenance of stem cell properties | Multiple agents |
| USP28 | Wnt/β-catenin | FOXM1 | Cell cycle progression, anti-apoptosis | DNA-damaging agents |
| USP5 | Wnt/β-catenin, DNA damage | FOXM1 | Enhanced tumor growth | Platinum-based drugs |
| OTUD1 | TGF-β/SMAD | SMAD7 | Inhibition of EMT (context-dependent) | Chemotherapy |
Immune Evasion and Immunotherapy Resistance
The emergence of immunotherapy has revolutionized cancer treatment, but resistance remains a significant challenge. DUBs contribute to immune evasion through multiple mechanisms, including regulation of immune checkpoint molecules.
Ataxin-3 (ATXN3), a member of the MJD family, has been identified as a key regulator of programmed death-ligand 1 (PD-L1) expression. CRISPR-based screening identified ATXN3 as a leading PD-L1 activator, whose depletion significantly reduces PD-L1 abundance on cancer cells. ATXN3 deubiquitinates and stabilizes PD-L1 by removing K48-linked ubiquitin chains, thereby preventing its proteasomal degradation and enhancing tumor immune evasion [12]. This mechanism represents a promising target for overcoming resistance to immune checkpoint inhibitors.
USP7 inhibition has been shown to enhance the antitumor immune response by stabilizing the transcription factor T-bet in CD8+ T cells, thereby promoting their effector function and improving tumor control [20]. Additionally, USP15 negatively regulates the transcription factor Nrf2 through deubiquitination of Keap1, indirectly influencing the tumor immune microenvironment [20].
Drug Target Alteration and Inactivation
DUBs can directly stabilize drug targets or associated signaling molecules, leading to reduced drug efficacy and acquired resistance.
In EGFR-mutant lung adenocarcinoma, USP22 promotes resistance to EGFR tyrosine kinase inhibitors (TKIs) by preventing ubiquitination-mediated EGFR degradation. USP22 depletion enhances EGFR degradation and restores sensitivity to osimertinib, a third-generation EGFR TKI [20]. Similarly, USP8 regulates the stability of EGFR and other receptor tyrosine kinases, with inhibition leading to increased ubiquitination and degradation of these oncogenic drivers [3].
The OTUD3 deubiquitinase stabilizes phosphatase and tensin homolog (PTEN), a critical tumor suppressor. In breast cancer, OTUD3 downregulation leads to decreased PTEN stability and enhanced activation of the PI3K/AKT pathway, contributing to resistance to PI3K inhibitors and other targeted agents [31].
Experimental Approaches for Studying DUB Function in Drug Resistance
Genetic Manipulation of DUB Expression
RNA Interference and CRISPR-Cas9 Screening Systematic loss-of-function screening using siRNA, shRNA, or CRISPR-Cas9 technology represents a powerful approach for identifying DUBs involved in drug resistance. CRISPR-based screening has been instrumental in identifying novel regulators such as ATXN3 as key modulators of PD-L1 expression [12]. These screens typically involve introducing a library of guide RNAs targeting multiple DUB genes into cancer cells, followed by treatment with therapeutic agents and sequencing to identify guides that become enriched or depleted.
Protocol: CRISPR-Cas9 Screening for DUBs in Drug Resistance
- Transduce target cancer cells with a lentiviral CRISPR-Cas9 library containing 3-5 guides per DUB gene
- Select transduced cells with puromycin for 72 hours
- Split cells into treatment groups (drug-treated vs. vehicle control)
- Culture cells for 14-21 days under selective pressure
- Harvest genomic DNA and amplify integrated guide sequences
- Sequence amplified products and analyze guide enrichment/depletion using specialized algorithms (MAGeCK, DESeq2)
- Validate hits using individual guides in secondary assays
Overexpression Studies Gain-of-function experiments involve introducing cDNA constructs encoding wild-type or catalytically inactive mutant DUBs into drug-sensitive cells to assess their ability to confer resistance. For example, overexpression of USP21 in HPNE cells promotes pathological progression to PDAC in orthotopic transplantation models [4].
Activity-Based Protein Profiling (ABPP)
Activity-based profiling utilizes reactive chemical probes that covalently bind to the active sites of DUBs, enabling assessment of their catalytic activity and engagement by small-molecule inhibitors [3] [8]. This approach is particularly valuable for:
- Profiling DUB activity across different cellular states
- Assessing inhibitor selectivity and potency
- Identifying active DUBs in complex proteomes
Protocol: ABPP for DUB Inhibitor Screening
- Prepare cell lysates from drug-resistant and sensitive cancer cells
- Incubate lysates with HA-ubiquitin-vinyl sulfone or ubiquitin-propargylamide probes
- Allow covalent modification of active DUBs (30-60 minutes, 37°C)
- Conjugate with reporter tags (biotin, fluorophores) via click chemistry if using propargylamide probes
- Separate proteins by SDS-PAGE and visualize by streptavidin-HRP or fluorescent scanning
- For identification, capture probe-labeled proteins with streptavidin beads and analyze by mass spectrometry
Biochemical and Cellular Assays
Deubiquitination Assays In vitro deubiquitination assays determine DUB specificity and activity toward different ubiquitin chain types. These assays typically involve incubating purified DUBs with di-ubiquitin or polyubiquitin chains of specific linkages (K48, K63, K11, etc.), followed by analysis using gel electrophoresis or mass spectrometry to measure cleavage [74].
Cell Viability and Apoptosis Assays Standard cell viability assays (MTT, CellTiter-Glo) and apoptosis detection methods (annexin V staining, caspase activation) are used to assess the functional consequences of DUB manipulation on drug sensitivity. For example, OTUD1 restoration sensitizes esophageal squamous cell carcinoma cells to chemotherapy-induced death [31].
Protein Stability and Turnover Measurements Cycloheximide chase experiments determine the effect of DUBs on substrate half-life. Cells are treated with cycloheximide to inhibit new protein synthesis, and substrate levels are monitored over time by immunoblotting. Complementary experiments involve monitoring protein degradation rates after proteasomal (MG132) or lysosomal (chloroquine) inhibition.
Research Reagent Solutions for DUB Studies
Table 3: Essential Research Reagents for DUB Investigation
| Reagent Category | Specific Examples | Application | Key Features |
|---|---|---|---|
| Activity-Based Probes | HA-ubiquitin-vinyl sulfone, Ubiquitin-propargylamide | DUB activity profiling, inhibitor screening | Covalently modifies active DUBs, compatible with fluorescence or biotin detection |
| DUB Inhibitors | P5091 (USP7 inhibitor), ML323 (USP1-UAF1 inhibitor), VLX1570 (USP14/UCHL5 inhibitor) | Functional validation, combination therapy studies | Varying selectivity, tool compounds for multiple DUB families |
| Ubiquitin Chain Linkage Reagents | K48-linked di-ubiquitin, K63-linked tetra-ubiquitin, M1-linked linear chains | Biochemical characterization of DUB specificity | Defined linkage types, available from commercial suppliers |
| CRISPR Libraries | Custom DUB-focused sgRNA libraries, Whole-genome libraries | Genetic screening for DUBs in drug resistance | Targeted coverage of DUB family, validation with multiple guides per gene |
| Antibody Resources | Phospho-specific antibodies (γH2AX, pCHK1), Cleaved caspase antibodies, Ubiquitin remnant motifs | Detection of signaling and cell death pathways | Critical for monitoring DNA damage, apoptosis, and ubiquitination |
| Proteasome Inhibitors | MG132, Bortezomib, Carfilzomib | Block protein degradation to assess ubiquitination | Enable accumulation of ubiquitinated substrates |
| Expression Constructs | Wild-type and catalytic mutant DUBs, Ubiquitin mutants (K48R, K63R) | Overexpression and mechanistic studies | Structure-function analysis, identification of essential residues |
Signaling Pathways in DUB-Mediated Drug Resistance
The following diagrams illustrate key signaling pathways through which DUBs mediate drug resistance in cancer cells, highlighting potential intervention points for therapeutic development.
DUB Regulation of DNA Damage Response
DUB Regulation of Apoptosis Pathways
DUB Regulation of Immune Checkpoints
Therapeutic Targeting of DUBs to Overcome Drug Resistance
DUB Inhibitor Development
The development of selective DUB inhibitors represents a promising approach for reversing therapeutic resistance. Several DUB inhibitors have shown promise in preclinical studies and clinical trials:
USP1 inhibitors have demonstrated efficacy in reversing cisplatin resistance in non-small cell lung cancer models [3]. These inhibitors target the USP1-UAF1 complex, leading to increased ubiquitination and degradation of key DNA repair proteins.
USP7 inhibitors (e.g., HBX41108, P22077) show antitumor activity in neuroblastoma, acute leukemia, and colorectal cancer models [12]. USP7 inhibition destabilizes multiple oncogenic substrates and enhances p53-mediated apoptosis, particularly in cancers with wild-type TP53.
USP14/UCHL5 inhibitors (e.g., b-AP15, VLX1570) have progressed to clinical trials. VLX1570 was evaluated in a phase I/II study for multiple myeloma, though development was challenged by toxicity issues [3] [20]. These compounds induce accumulation of polyubiquitinated proteins and endoplasmic reticulum stress, leading to apoptosis.
OTUD family targeting remains in early development, with no specific inhibitors currently in clinical trials. However, the elucidation of OTUD1's role in chemosensitivity and OTUD3's regulation of PTEN highlights the potential therapeutic value of targeting this DUB subfamily [31].
Combination Therapy Strategies
Combining DUB inhibitors with conventional therapies represents a rational approach to overcome resistance:
DUB inhibitors with DNA-damaging agents: USP1 inhibition synergizes with cisplatin in lung cancer models by preventing efficient DNA damage repair [75] [3]. Similarly, USP7 inhibitors enhance the efficacy of radiotherapy across multiple cancer types.
DUB inhibitors with targeted therapies: USP9X inhibition potentiates the activity of BCL-2 family inhibitors in hematological malignancies by reducing MCL1 stability [20]. USP22 depletion restores sensitivity to EGFR inhibitors in lung adenocarcinoma.
DUB inhibitors with immunotherapy: ATXN3 inhibition represents a promising strategy to enhance response to anti-PD-1/PD-L1 therapy by reducing PD-L1 stability on tumor cells [12]. Conversely, USP7 inhibition in T cells may enhance antitumor immunity by stabilizing T-bet and promoting effector function.
Challenges in DUB-Targeted Therapy
Despite the promising outlook, several challenges remain in developing DUB-targeted therapies:
Selectivity: The high structural conservation among DUB active sites makes achieving selectivity challenging. Off-target effects may lead to unacceptable toxicity, as seen with some pan-DUB inhibitors.
Context-dependent functions: Many DUBs exhibit tissue-specific or cancer-type-specific roles, necessitating careful patient selection strategies. For example, USP9X functions as an oncogene in some contexts but as a tumor suppressor in others [4].
Compensation and adaptive resistance: Inhibition of specific DUBs may lead to upregulation of compensatory DUBs or alternative resistance mechanisms, requiring rational combination approaches.
Biomarker development: Identifying predictive biomarkers for DUB inhibitor response remains crucial for successful clinical translation. Potential biomarkers include substrate expression levels, specific genetic alterations, or DUB expression patterns.
DUB upregulation represents a significant mechanism of adaptive resistance to cancer therapeutics, occurring through diverse molecular pathways including enhanced DNA repair, inhibition of apoptosis, maintenance of stem cell properties, and immune evasion. The intricate involvement of DUBs across these resistance mechanisms highlights their potential as therapeutic targets to reverse or prevent treatment failure.
Future research directions should focus on: (1) Developing more selective DUB inhibitors with improved pharmacological properties; (2) Identifying predictive biomarkers for DUB inhibitor response; (3) Elucidating context-dependent functions of DUBs to guide appropriate patient selection; (4) Exploring novel therapeutic modalities such as PROTACs (proteolysis-targeting chimeras) that target DUBs for degradation; and (5) Investigating the role of less-characterized DUB family members in therapy resistance.
As the field advances, DUB inhibitors used in rational combination strategies hold significant promise for overcoming therapeutic resistance and improving outcomes for cancer patients. The integration of DUB targeting into current treatment paradigms represents an emerging frontier in precision oncology that warrants continued investigation.
DUBs in Cancer Stem Cell Maintenance and Therapeutic Resistance
Cancer stem cells (CSCs) represent a subpopulation of tumor cells with capabilities for self-renewal, differentiation, and therapeutic resistance, contributing significantly to tumor recurrence and metastasis. The ubiquitin-proteasome system, particularly deubiquitinating enzymes (DUBs), plays a crucial role in maintaining CSC properties by regulating protein stability and function. This comprehensive review examines the mechanistic roles of specific DUBs in CSC maintenance, signaling pathway regulation, and resistance to conventional therapies. We synthesize current knowledge on DUB-mediated stabilization of core stemness factors and explore the therapeutic potential of DUB inhibition for targeting CSCs. The findings presented herein establish DUBs as critical regulators of CSC pathophysiology and promising targets for innovative cancer therapeutics.
Deubiquitinating enzymes (DUBs) constitute a family of approximately 100 proteases that remove ubiquitin chains from target proteins, thereby counteracting the activity of E3 ubiquitin ligases and regulating protein stability, localization, and function [10]. DUBs are classified into seven major families based on their catalytic domains and mechanisms: ubiquitin-specific proteases (USPs), ubiquitin carboxy-terminal hydrolases (UCHs), ovarian tumor proteases (OTUs), Machado-Joseph disease protein domain proteases (MJDs), JAB1/MPN/MOV34 metalloenzymes (JAMMs), motif interacting with Ub-containing novel DUB family (MINDY), and Zn-finger and UFSP domain proteins (ZUFSP) [76] [10]. The balanced regulation of ubiquitination and deubiquitination is essential for cellular homeostasis, and dysregulation of DUB activity is increasingly recognized as a hallmark of cancer pathogenesis.
Cancer stem cells (CSCs), also known as tumor-initiating cells, constitute a minor subpopulation within tumors that possess self-renewal capacity and the ability to differentiate into heterogeneous tumor cell lineages [76] [77]. CSCs contribute to multiple aspects of tumor progression, including metastasis, heterogeneity, multidrug resistance, and radiation resistance [76]. The functional properties of CSCs are regulated by well-balanced processes of ubiquitination and deubiquitination of proteins related to cellular stemness, which execute various stem cell fate decisions [76]. Key developmental signaling pathways, including Notch, Wnt, and Sonic hedgehog (Shh), play essential roles in normal stem cell development and CSC regulation, with their dysregulation contributing to carcinogenesis [76]. Understanding how DUBs regulate these pathways and core stemness factors provides critical insights for developing novel therapeutic strategies to eliminate CSCs and prevent tumor recurrence.
DUB Regulation of Core CSC Signaling Pathways
Wnt/β-Catenin Signaling
The Wnt/β-catenin pathway is a crucial regulator of stem cell maintenance and differentiation, with several DUBs identified as key modulators of this pathway in CSCs. USP34 has been demonstrated to facilitate pancreatic cancer cell survival through AKT and PKC pathways, promoting CSC properties [4]. Similarly, USP21 interacts with and stabilizes TCF7 to maintain the stemness of pancreatic ductal adenocarcinoma (PDAC) cells [4]. In vivo studies using orthotopic pancreatic transplantation models revealed that USP21-overexpressing cells undergo pathological progression from pancreatic intraepithelial neoplasia (PanIN) to PDAC, highlighting its role in tumor initiation [4]. USP28 represents another significant regulator of Wnt signaling, promoting cell cycle progression and inhibiting apoptosis in PDAC cells by stabilizing FOXM1, a key proliferation-associated transcription factor that activates the Wnt/β-catenin pathway [4].
Hippo Signaling Pathway
The Hippo pathway, particularly its effectors YAP/TAZ, plays a fundamental role in regulating organ size and stem cell function. USP9X has been identified as a crucial regulator of the Hippo pathway in pancreatic cancer, where it cooperates with LATS kinase and YAP/TAZ to impede tumor growth [4]. This tumor-suppressive function contrasts with its oncogenic role in other contexts, highlighting the tissue-specific functions of DUBs in CSC regulation. The Hippo pathway's involvement in contact inhibition and mechanical signaling makes it particularly relevant to CSC maintenance in dense tumor microenvironments.
Cell Cycle and Apoptosis Regulation
DUBs directly regulate core cell cycle components and apoptotic machinery in CSCs. USP22 promotes breast cancer cell proliferation by deubiquitinating and stabilizing G1 cyclin D1 (CCND1), protecting it from proteasome-mediated degradation and facilitating G1-S progression [26]. USP14 controls cell cycle progression in breast CSCs through deubiquitination of Cyclin B1, with knockdown of USP14 inducing cell cycle arrest at G2/M phase and apoptosis [26]. In pancreatic cancer, USP5 promotes tumor growth by prolonging the half-life of FOXM1, thereby accelerating cell cycle progression and inhibiting apoptotic pathways [4].
Table 1: Key DUBs Regulating CSC Signaling Pathways
| DUB | Cancer Type | Substrate/Pathway | Biological Effect in CSCs |
|---|---|---|---|
| USP21 | Pancreatic | TCF7/Wnt | Maintains stemness, promotes tumor initiation |
| USP22 | Breast, Pancreatic | Cyclin D1, Histone H2B | Promotes proliferation, regulates transcription |
| USP28 | Pancreatic | FOXM1/Wnt | Promotes cell cycle progression, inhibits apoptosis |
| USP34 | Pancreatic | AKT/PKC | Facilitates cancer cell survival |
| USP9X | Pancreatic | LATS/YAP/TAZ Hippo | Suppresses tumor growth (context-dependent) |
| USP5 | Pancreatic | FOXM1 | Promotes tumor growth, regulates DNA damage response |
| USP14 | Breast | Cyclin B1 | Controls cell cycle progression, prevents apoptosis |
DUB-Mediated Stabilization of Stemness Factors
Core Stem Cell Transcription Factors
DUBs regulate the stability and function of core transcription factors that govern stem cell identity and plasticity. USP22 stabilizes c-Myc by removing polyubiquitin chains and antagonizing the ubiquitination activity of its E3 ligase FBW7, thereby promoting breast cancer cell growth [26]. Similarly, USP36 increases breast cancer cell proliferation by deubiquitinating c-Myc in the nucleolus and inhibiting its proteasomal degradation mediated by SCFFbw7 [26]. A positive feedback loop exists between USP36 and c-Myc, wherein c-Myc transcriptionally activates USP36 expression, creating an auto-amplifying circuit that enhances stemness properties [26].
The pluripotency factor NANOG, critical for maintaining embryonic stem cell identity, is regulated by USP21 through removal of K48-linked polyubiquitination, thereby stabilizing NANOG and promoting stemness in CSCs [77]. This regulatory mechanism represents a potential vulnerability for targeting CSCs across multiple cancer types.
KLF5 Stabilization in Triple-Negative Breast Cancer
Krüppel-like factor 5 (KLF5) performs protumorigenic activity in breast cancer, particularly in triple-negative breast cancer (TNBC), where it is regarded as a poor prognosis factor [26]. Multiple DUBs regulate KLF5 stability, including ATXN3L, BAP1, and USP3, all of which promote breast cancer development through KLF5 stabilization [26]. The identification of these regulatory axes provides novel therapeutic opportunities for TNBC, a breast cancer subtype with limited treatment options and poor clinical outcomes.
Histone Modification and Epigenetic Regulation
DUBs play significant roles in epigenetic regulation of CSCs through histone modifications. The human SAGA complex (hSAGA), containing USP22 as a catalytic subunit, deubiquitinates histone H2B with the assistance of regulatory components ATXN7L3 and ENY2 [26]. USP27X and USP51, while structurally independent of hSAGA, also deubiquitinate histone H2B by competing with USP22 for interaction with regulatory components [26]. Depletion of any of these DUBs inhibits breast cancer growth partly through downregulation of H2Bub1 levels [26]. USP44 represents another histone-modifying DUB that exhibits context-dependent functions by removing ubiquitin from H2Bub1, with opposing effects in different breast cancer subtypes [26].
Figure 1: DUB-Mediated Stabilization of Stemness Factors in CSCs. Multiple DUBs regulate core transcription factors and histone modifications that maintain cancer stem cell properties and promote therapeutic resistance.
DUBs in Therapeutic Resistance Mechanisms
Chemotherapy Resistance
Cisplatin resistance represents a significant clinical challenge across multiple cancer types, and DUBs have emerged as key mediators of this resistance mechanism [78]. The development of cisplatin resistance involves pre-target, on-target, post-target, and off-target mechanisms, with DUBs operating at multiple levels within this framework [78]. Pre-target resistance involves reduced drug accumulation through altered transport mechanisms, while on-target resistance includes enhanced DNA damage repair. Post-target resistance encompasses dysregulation of cell death signaling pathways, and off-target resistance involves activation of alternative survival pathways [78]. Several USP family members have been specifically implicated in mediating cisplatin resistance, highlighting their potential as therapeutic targets for overcoming treatment failure.
Immunotherapy Resistance and Immune Evasion
The tumor immune microenvironment represents another critical area of DUB activity in therapeutic resistance. USP22 has been identified as a key regulator of immune evasion through multiple mechanisms [79]. In pancreatic ductal adenocarcinoma (PDAC), knockdown of USP22 improved response to immunotherapy, accompanied by increased infiltration of natural killer (NK) cells and CD8+ T cells into tumors [79]. Similar findings were reported in liver cancer models, where ablation of USP22 enhanced tumor immunogenicity and promoted T-cell infiltration [79]. USP22 stabilizes programmed death ligand 1 (PD-L1) through deubiquitination, thereby enabling cancer cells to evade immune surveillance [79]. Additionally, USP22 serves as a positive regulator of forkhead box protein 3 (FOXP3) expression in regulatory T cells (Tregs), with Treg-specific ablation of USP22 resulting in reduced tumor volume across multiple cancer models [79].
Table 2: DUBs in Therapeutic Resistance Mechanisms
| Resistance Mechanism | Key DUBs | Molecular Substrates/Pathways | Therapeutic Implications |
|---|---|---|---|
| Chemotherapy Resistance | Multiple USPs | Drug transporters, DNA repair proteins, apoptosis regulators | DUB inhibition sensitizes to conventional chemotherapy |
| Immunotherapy Resistance | USP22 | PD-L1 stability, FOXP3 expression in Tregs | Combined DUB and immune checkpoint inhibition enhances response |
| Radiation Resistance | USP22, others | DNA damage response, antioxidant systems | DUB inhibitors overcome radioresistance of CSCs |
| Multidrug Resistance | USP1, USP7, USP14 | ABC transporters, survival pathways | Targeted DUB inhibition reverses broad-spectrum resistance |
Experimental Methodologies for Studying DUBs in CSCs
DUB Activity and Substrate Identification
The systematic identification of DUB substrates in CSCs employs multiple complementary approaches. Co-immunoprecipitation coupled with mass spectrometry (Co-IP/MS) enables comprehensive mapping of DUB interaction networks [26] [4]. For investigating specific DUB-substrate relationships, tandem ubiquitin binding entities (TUBEs) are utilized to capture and analyze endogenous ubiquitinated proteins, allowing researchers to monitor changes in substrate ubiquitination status following DUB modulation [78]. Additionally, activity-based probes (ABPs) containing ubiquitin variants with C-terminal electrophilic traps covalently label active DUBs, facilitating profiling of DUB activity in CSC populations under various conditions [3].
Functional Validation in CSC Models
Robust functional validation of DUB roles in CSCs requires specialized experimental systems. In vitro sphere formation assays under low-attachment conditions measure self-renewal capacity following DUB manipulation [76] [77]. For in vivo assessment, limiting dilution transplantation experiments using immunocompromised mice (e.g., NOD/SCID/IL2Rγnull strains) quantitatively evaluate tumor-initiating cell frequency upon DUB inhibition [76]. To model therapy resistance, CSCs are exposed to sublethal doses of chemotherapeutic agents or radiation, followed by assessment of survival and sphere-forming efficiency with and without DUB targeting [77] [78]. Genetic approaches for DUB modulation include CRISPR/Cas9-mediated knockout for complete ablation, RNA interference for partial knockdown, and overexpression constructs to assess gain-of-function effects [26] [4].
Figure 2: Experimental Workflow for Investigating DUB Functions in CSCs. A systematic approach from target identification through therapeutic development for studying DUB roles in cancer stem cell biology and therapeutic resistance.
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Research Reagents for DUB and CSC Investigations
| Reagent Category | Specific Examples | Research Applications | Key Considerations |
|---|---|---|---|
| DUB Activity Probes | HA-Ub-VS, HA-Ub-Br2 | Profiling active DUB populations, competition studies | Requires controlled labeling conditions, validation of specificity |
| CSC Markers | CD44, CD133, ALDH | Identification and isolation of CSC populations | Marker combinations improve purity, context-dependent expression |
| DUB Inhibitors | P5091 (USP7), ML323 (USP1-UAF1) | Functional studies, therapeutic potential assessment | Selectivity profiling essential, potential off-target effects |
| In Vivo Models | Patient-derived xenografts (PDX), genetically engineered mouse models (GEMMs) | Preclinical validation of DUB targets | PDX models maintain tumor heterogeneity, GEMMs enable tissue-specific manipulation |
| Ubiquitin Assays | TUBE reagents, diGly antibody | Monitoring substrate ubiquitination status | TUBEs protect chains from DUBs during processing, diGly MS enables global profiling |
Concluding Perspectives and Future Directions
The investigation of DUBs in CSC maintenance and therapeutic resistance represents a rapidly advancing field with significant translational potential. The multifaceted roles of DUBs in regulating core stemness pathways, stabilizing transcription factors, and mediating treatment resistance establish them as promising therapeutic targets for eliminating CSCs. Future research directions should focus on developing more selective DUB inhibitors with improved pharmacological properties, understanding compensatory mechanisms among DUB family members, and identifying predictive biomarkers for patient stratification. Additionally, the integration of DUB inhibitors with conventional therapies and immunotherapeutic approaches may provide synergistic benefits for overcoming therapeutic resistance. As our understanding of the complex regulatory networks governed by DUBs in CSCs continues to expand, so too will opportunities for developing innovative strategies to target these critical mediators of tumor persistence and recurrence.
Deubiquitinating enzymes (DUBs) have emerged as critical regulators of cancer cell survival, orchestrating metabolic reprogramming that enables tumors to evade conventional therapies. This whitepaper delineates the molecular mechanisms by which specific DUB families stabilize key metabolic enzymes, transcription factors, and signaling intermediates to sustain energy production and biomass synthesis under therapeutic stress. We present a comprehensive analysis of DUB-mediated pathways in glucose metabolism, lipid biosynthesis, and hypoxia response, supported by experimental data and pathway visualizations. Furthermore, we detail methodologies for investigating DUB functions and catalog essential research reagents for targeting DUB-driven metabolic adaptation. Understanding these mechanisms provides a rational foundation for developing novel combinatorial strategies to overcome treatment resistance in oncology.
Deubiquitinating enzymes (DUBs) comprise approximately 100 proteases that catalyze the removal of ubiquitin chains from target proteins, thereby counteracting ubiquitin-mediated degradation and altering protein function, localization, and interaction networks [4] [20]. The dynamic balance between ubiquitination and deubiquitination constitutes a crucial regulatory mechanism for cellular homeostasis, with dysregulation of this system being a hallmark of cancer pathogenesis [80] [19]. DUBs are categorized into seven subfamilies based on their catalytic domains: ubiquitin-specific proteases (USPs), ovarian tumor proteases (OTUs), ubiquitin C-terminal hydrolases (UCHs), Machado-Josephin domain-containing proteases (MJDs), JAB1/MPN/MOV34 metalloenzymes (JAMMs), motif-interacting with ubiquitin-containing novel DUB family (MINDY), and monocyte chemotactic protein-induced protein (MCPIP) [20] [7].
Cancer cells exhibit profound metabolic reprogramming to support rapid proliferation, survival under nutrient deprivation, and resistance to therapeutic agents [80]. This reprogramming encompasses enhanced glucose uptake, glycolytic flux, lipid synthesis, and adaptive responses to hypoxia. DUBs have been identified as master regulators of these processes, stabilizing rate-limiting metabolic enzymes and transcription factors to maintain energy production and biosynthetic pathways [80] [30]. For instance, the stabilization of c-MYC and HIF1α by specific DUBs enhances glycolytic metabolism and promotes chemoresistance across various cancer types [81] [7]. This review systematically examines the evidence for DUB-mediated metabolic adaptation and its contribution to treatment evasion, providing a framework for therapeutic targeting of these enzymes.
Molecular Mechanisms of DUB-Mediated Metabolic Regulation
Regulation of Glucose Metabolism and Hypoxia Response
DUBs intricately control glycolytic flux and cellular adaptation to hypoxia by stabilizing key transcription factors and metabolic enzymes. The hypoxia-inducible factor 1 alpha (HIF1α), a master regulator of oxygen homeostasis, is normally degraded under normoxic conditions following prolyl hydroxylation and VHL-mediated ubiquitination. However, increased DUB activity can stabilize HIF1α even under normoxic conditions, a phenomenon known as pseudohypoxia [81]. This stabilization leads to transcriptional activation of genes encoding glucose transporters (GLUT1, GLUT3) and glycolytic enzymes (HK2, PGK1), redirecting glucose metabolism toward lactate production and supporting cell survival under metabolic stress [81].
The Warburg effect, wherein cancer cells preferentially utilize glycolysis over oxidative phosphorylation for energy generation, is reinforced by DUB activity. For example, USP22 has been demonstrated to deubiquitinate and stabilize c-MYC, enhancing the transcription of glycolytic genes and contributing to chemoresistance in triple-negative breast cancer [7]. Similarly, OTUB2 interacts with pyruvate kinase M2 (PKM2), inhibiting its Parkin-mediated ubiquitination and thereby enhancing glycolytic flux in colorectal cancer [19]. The table below summarizes key DUBs involved in regulating glucose metabolism and the hypoxia response.
Table 1: DUBs Regulating Glucose Metabolism and Hypoxia Response
| DUB | Cancer Type | Substrate | Metabolic Effect | Impact on Treatment |
|---|---|---|---|---|
| USP22 | Triple-negative Breast Cancer | c-MYC | Promotes Warburg effect, enhances glycolysis | Induces chemoresistance [7] |
| OTUB2 | Colorectal Cancer | PKM2 | Inhibits PKM2 ubiquitination, enhances glycolysis | Accelerates cancer progression [19] |
| USP14 | Gastric Cancer | KPNA2 (indirectly c-MYC) | Promotes c-MYC nuclear translocation | Enhances proliferation, migration, invasion [82] |
| Multiple DUBs | Various Cancers | HIF1α | Stabilizes HIF1α, induces pseudohypoxia | Promotes survival under hypoxia, chemoresistance [81] |
Control of Lipid Metabolism
Lipid metabolism is frequently dysregulated in cancer to provide membranes for rapidly dividing cells, signaling molecules, and energy storage. DUBs play a pivotal role in stabilizing key lipogenic enzymes, thereby promoting lipid biosynthesis and tumor growth. Adenosine triphosphate citrate lyase (ACLY), which converts citrate to acetyl-CoA in the cytoplasm, is a critical node linking glucose metabolism to lipid synthesis. The stability of ACLY is regulated by opposing acetylation and ubiquitination events, with SIRT2 deacetylating ACLY and promoting its interaction with the E3 ligase UBR4, leading to ACLY degradation [30]. Conversely, ACLY acetylation reduces UBR4 binding, stabilizing the enzyme and enhancing lipogenesis.
Fatty acid synthase (FASN), the primary enzyme responsible for de novo fatty acid synthesis, is another key target of DUB regulation. The E3 ubiquitin ligase SPOP negatively regulates FASN, and its mutation in prostate cancer leads to FASN stabilization and increased fatty acid synthesis [30]. Furthermore, HDAC3-mediated deacetylation of FASN enhances its binding to the E3 ligase TRIM21, promoting FASN degradation and suppressing cancer cell growth [30]. These findings highlight the complex interplay between post-translational modifications in controlling lipid metabolism.
Table 2: DUBs and Associated Enzymes Regulating Lipid Metabolism
| Regulatory Enzyme | Type | Target | Effect on Lipid Metabolism | Cancer Context |
|---|---|---|---|---|
| SIRT2 | Deacetylase | ACLY | Promotes ACLY degradation, inhibits lipogenesis | Lung Cancer [30] |
| KLHL25-CUL3 | E3 Ligase Complex | ACLY | Ubiquitinates and degrades ACLY | Suppresses tumor growth in lung cancer [30] |
| SPOP | E3 Ligase | FASN | Reduces FASN expression and fatty acid synthesis | Prostate Cancer [30] |
| HDAC3 | Deacetylase | FASN | Enhances FASN binding to TRIM21, promoting degradation | Inhibits cancer cell growth [30] |
DUBs in Drug Resistance Pathways
Chemoresistance remains a major obstacle in oncology, and DUBs contribute significantly to this phenomenon through multiple mechanisms. They can stabilize anti-apoptotic proteins, enhance DNA damage repair, and maintain the stemness of cancer stem cells (CSCs), which are often refractory to conventional therapies [83] [20] [7]. For instance, USP9x stabilizes the anti-apoptotic protein MCL-1 in breast cancer, conferring resistance to chemotherapeutic agents [7]. In pancreatic ductal adenocarcinoma (PDAC), USP22 upregulation enhances stemness properties and contributes to chemoresistance [4].
The Wnt/β-catenin and PI3K-AKT pathways, which are aberrantly activated in CSCs, are frequently regulated by DUBs. USP28 promotes cell cycle progression and inhibits apoptosis in PDAC by stabilizing the transcription factor FOXM1, which activates the Wnt/β-catenin pathway [4]. Similarly, USP14 deubiquitinates and stabilizes KPNA2, facilitating the nuclear translocation of c-MYC and driving proliferation and invasion in gastric cancer [82]. Targeting these DUBs presents a promising strategy for overcoming chemoresistance.
Detailed Signaling Pathways
The following diagrams illustrate key signaling pathways through which DUBs regulate metabolic adaptation and treatment evasion.
USP14-KPNA2-c-MYC Signaling Axis in Gastric Cancer
Diagram 1: USP14-KPNA2-c-MYC Axis. USP14 deubiquitinates and stabilizes KPNA2, which facilitates c-MYC nuclear translocation, leading to enhanced proliferation, invasion, and chemoresistance in gastric cancer [82].
DUB-Mediated Metabolic Regulation Network
Diagram 2: DUB Metabolic Regulation. Multiple DUBs and associated enzymes converge on key metabolic regulators (HIF1α, c-MYC, PKM2, ACLY, FASN) to enhance glycolysis and lipogenesis, ultimately fostering a chemoresistant phenotype [81] [30] [7].
Experimental Protocols for Investigating DUB Functions
Protocol 1: Validating DUB-Substrate Interactions and Stabilization
Objective: To confirm a physical interaction between a DUB and its putative substrate and assess the impact on substrate stability.
Co-Immunoprecipitation (Co-IP) and Mass Spectrometry (MS):
- Cell Lysis: Lyse cultured cancer cells (e.g., gastric cancer lines HGC-27 or SGC-7901) in RIPA buffer supplemented with protease and phosphatase inhibitors.
- Immunoprecipitation: Incubate cell lysates with an antibody against the DUB of interest (e.g., anti-USP14) or control IgG. Capture the immune complexes using Protein A/G beads.
- Mass Spectrometry: Separate the co-precipitated proteins by SDS-PAGE, followed by in-gel tryptic digestion. Analyze the resulting peptides by liquid chromatography-tandem mass spectrometry (LC-MS/MS) to identify interacting partners, as performed to identify KPNA2 as a USP14 interactor [82].
Cycloheximide Chase Assay:
- Treatment: Treat cells in which the DUB has been knocked down (via shRNA) or inhibited (via small molecules) with cycloheximide (e.g., 100 µg/mL) to block new protein synthesis.
- Time-Course Analysis: Harvest cells at various time points (e.g., 0, 2, 4, 8 hours) post-cycloheximide treatment.
- Western Blot: Analyze lysates by Western blotting to detect the protein levels of the substrate (e.g., KPNA2). A prolonged half-life of the substrate in control cells compared to DUB-deficient cells indicates that the DUB stabilizes the substrate [82].
In Vivo Ubiquitination Assay:
- Transfection: Co-transfect cells with plasmids expressing the substrate, HA- or Myc-tagged ubiquitin, and the DUB or a catalytically inactive mutant.
- Immunoprecipitation: Lyse cells and immunoprecipitate the substrate under denaturing conditions (e.g., using 1% SDS) to disrupt non-covalent interactions.
- Detection: Detect polyubiquitinated forms of the substrate by Western blotting using an anti-HA or anti-Myc antibody. A reduction in ubiquitinated species in the presence of the wild-type DUB confirms its deubiquitinating activity toward the substrate [82].
Protocol 2: Functional Assessment of DUB in Metabolic Phenotypes
Objective: To determine the functional consequence of DUB inhibition on cancer cell metabolism and chemosensitivity.
Metabolic Flux Analysis:
- Extracellular Acidification Rate (ECAR): Using a Seahorse XF Analyzer, measure the ECAR of live cells treated with a DUB inhibitor (e.g., IU1 for USP14) versus control. Inject glucose, oligomycin, and 2-DG sequentially to assess glycolytic function. A decreased ECAR upon DUB inhibition indicates reduced glycolytic flux [81] [82].
- Oxygen Consumption Rate (OCR): Using the same system, measure OCR by injecting oligomycin, FCCP, and rotenone/antimycin A. This assesses mitochondrial respiration.
Cell Viability and Chemosensitivity Assay (MTT):
- Plating: Seed cells in 96-well plates and treat with a concentration gradient of a chemotherapeutic agent (e.g., cisplatin, gemcitabine) with or without a DUB inhibitor.
- Incubation and Measurement: After 72 hours, add MTT reagent (3-(4,5-dimethylthiazol-2-yl)-2,5-diphenyltetrazolium bromide) to each well. The metabolically active cells reduce MTT to purple formazan crystals. Dissolve the crystals and measure the absorbance at 570 nm.
- Analysis: Calculate the half-maximal inhibitory concentration (IC50) for the chemotherapeutic agent in the presence and absence of the DUB inhibitor. A leftward shift in the dose-response curve (lower IC50) with DUB inhibition indicates sensitization to chemotherapy [82] [7].
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Reagents for Studying DUBs in Metabolic Adaptation
| Reagent / Tool | Function / Application | Example Use Case |
|---|---|---|
| shRNA/siRNA Lentiviral Particles | Stable or transient knockdown of specific DUBs to study loss-of-function phenotypes. | Knockdown of USP14 in gastric cancer cells to assess impact on KPNA2 stability and cell invasion [82]. |
| Specific Small-Molecule Inhibitors | Pharmacological inhibition of DUB catalytic activity for functional and therapeutic studies. | IU1 used to inhibit USP14, leading to reduced gastric cancer cell migration and invasion [82]. |
| Plasmids for Wild-Type and Catalytic Mutant DUBs | For overexpression and rescue experiments; catalytic mutants confirm enzyme activity dependence. | Expressing full-length USP14 to rescue phenotypes in shUSP14-treated cells [82]. |
| Co-Immunoprecipitation Kits | To investigate protein-protein interactions and identify novel DUB substrates. | Identifying KPNA2 as a novel interacting partner and substrate of USP14 [82]. |
| Seahorse XF Analyzer & Kits | Real-time measurement of metabolic fluxes (glycolysis and mitochondrial respiration) in live cells. | Measuring extracellular acidification rate (ECAR) to quantify glycolytic flux after DUB inhibition [81]. |
| Antibodies for Key Proteins | Detection of protein expression, localization, and stability via Western Blot, IHC, and IF. | Antibodies against USP14, KPNA2, c-MYC, and ubiquitin for mechanistic studies [82]. |
DUBs sit at the nexus of cellular signaling and metabolic regulation, functioning as critical enablers of the adaptive processes that allow cancer cells to evade treatment. The mechanistic insights detailed herein—from the stabilization of HIF1α and c-MYC to the control of rate-limiting enzymes in lipid synthesis—provide a compelling rationale for targeting DUBs in combination therapy. The ongoing development of specific small-molecule DUB inhibitors, such as VLX1570 and KSQ-4279 which have entered clinical trials, underscores the translational potential of this research area [20] [7].
Future research should focus on elucidating the full spectrum of DUB substrates within metabolic pathways, understanding the context-dependent roles of DUBs in different cancer types, and developing more potent and selective inhibitors. Combining DUB inhibitors with conventional chemotherapy or other targeted agents represents a promising strategy to disrupt the metabolic adaptability of tumors, potentially overcoming one of the most significant challenges in modern oncology. The experimental tools and conceptual frameworks presented in this whitepaper are intended to facilitate these crucial advancements.
The development of targeted therapies against deubiquitinating enzymes (DUBs) represents a promising frontier in cancer treatment, yet achieving optimal therapeutic windows remains a significant challenge. DUBs constitute a superfamily of more than 100 proteases that regulate protein stability and function by removing ubiquitin chains from substrate proteins, thereby influencing virtually all cellular processes relevant to oncogenesis [84] [85]. Their dysregulation is a common feature across numerous malignancies, making them attractive therapeutic targets. This whitepaper examines the core principles and strategies for balancing the antitumor efficacy of DUB-targeted agents against their potential toxicities. We explore innovative screening methodologies, the application of novel therapeutic modalities like deubiquitinase-targeting chimeras (DUBTACs), and the critical importance of understanding DUB functions within the tumor microenvironment to expand the therapeutic window for next-generation cancer therapeutics.
Deubiquitinating enzymes function as critical regulators of cellular homeostasis, with their activities finely tuned in normal physiological states. The therapeutic window—the dosage range between the minimally effective dose and the maximally tolerated dose—is particularly narrow for agents targeting fundamental cellular machinery like the ubiquitin-proteasome system (UPS) [3]. The challenge is twofold: first, many DUBs regulate essential physiological processes in healthy tissues, and their inhibition can lead to on-target toxicity; second, the high degree of structural conservation among DUB families, particularly their catalytic domains, complicates the development of highly selective inhibitors [3] [86].
The UPS is responsible for 80-90% of cellular proteolysis, and DUBs represent a key node in regulating this system [19]. As such, non-selective inhibition of DUB activity can disrupt protein homeostasis broadly, leading to significant cellular stress and toxicity. Furthermore, many DUBs, such as BAP1, play critical tumor-suppressive roles in specific tissue contexts, creating a complex landscape where therapeutic strategies must account for both oncogenic and tumor-suppressive functions [4] [87]. This nuanced biological context necessitates sophisticated approaches to drug development that maximize tumor cell-specific killing while sparing normal tissues.
DUB Families and Their Roles in Oncogenesis
DUBs are classified into seven primary families based on the structure and mechanism of their catalytic domains: ubiquitin-specific proteases (USPs), ubiquitin C-terminal hydrolases (UCHs), ovarian tumor proteases (OTUs), Machado-Josephin domain-containing proteases (MJDs), motif-interacting with ubiquitin-containing novel DUB family (MINDYs), JAB1/MPN/MOV34 family (JAMMs), and zinc finger-containing ubiquitin peptidase 1 (ZUFSP) [3] [85]. With the exception of the JAMM family, which are metalloproteases, all DUBs are cysteine proteases that rely on a catalytic triad of conserved amino acids (His, Cys, and Asn/Asp) for activity [3].
Table 1: Major DUB Families and Their Cancer-Relevant Functions
| DUB Family | Representative Members | Key Cancer-Related Functions | Therapeutic Considerations |
|---|---|---|---|
| USP | USP1, USP7, USP9X, USP10, USP22 | DNA damage repair, immune checkpoint regulation, stemness maintenance | Largest family with diverse functions; selectivity is a key challenge |
| OTU | OTUD1, OTUD5, A20 | Regulation of NF-κB signaling, metabolic reprogramming, metastasis | Several members regulate key immune signaling pathways |
| JAMM | BRCC36, MYSM1 | Proteasomal degradation, histone deubiquitination | Only metalloprotease family; distinct catalytic mechanism |
| UCH | BAP1, UCHL1 | Transcriptional regulation, neuronal development | BAP1 mutations define a cancer syndrome with tissue-specific tumor suppression |
The USP family, with its extensive membership and structural diversity, has received the most attention in drug discovery efforts. For example, USP9X demonstrates context-dependent roles in pancreatic ductal adenocarcinoma (PDAC), functioning as either an oncogene or tumor suppressor depending on the cellular context [4]. This duality highlights the importance of patient stratification and biomarker identification for successful therapeutic development. Similarly, BAP1, a UCH family member, exhibits tumor-suppressive functions, and its loss promotes the development of multiple malignancies, creating a "BAP1 cancer syndrome" [4] [87]. In such cases, therapeutic strategies must focus on synthetic lethal approaches or reversing the downstream consequences of tumor suppressor loss rather than direct inhibition.
Quantitative Profiling of DUB Inhibitors: Efficacy and Toxicity Metrics
The development of DUB inhibitors has progressed significantly, with several compounds now in preclinical and early clinical development. The following table summarizes key candidates and their therapeutic indices based on current literature.
Table 2: DUB Inhibitors in Development and Their Therapeutic Window Profiles
| Target DUB | Inhibitor/Compound | Reported Efficacy (IC₅₀ or EC₅₀) | Toxicity Concerns | Therapeutic Index (Preclinical) | Development Stage |
|---|---|---|---|---|---|
| USP1 | Multiple compounds | Low nM range in DNA repair assays | Hematological toxicity | Moderate | Preclinical to early clinical |
| USP7 | HBX 19,828, P5091 | 5-100 nM in cellular assays | Neurotoxicity, p53 pathway disruption | Narrow | Preclinical |
| USP14 | b-AP15, IU1 | 1.2-2.4 μM (b-AP15) | Limited data | Not fully established | Preclinical |
| HDACs (indirect) | Quisinostat | Sub-nM to nM | Cardiac toxicity, embryo toxicity | Narrow (but acceptable with screening) | Validated in mouse models |
The quantitative profiling of DUB inhibitors reveals a consistent pattern: high potency often comes with narrow therapeutic windows due to the fundamental biological processes regulated by these enzymes. For instance, USP7 inhibitors demonstrate potent antitumor effects at low nanomolar concentrations but risk disrupting the p53 pathway, a critical tumor suppressor mechanism, potentially leading to genomic instability or other toxicities [3]. Similarly, HDAC inhibitors like quisinostat, identified through a novel screening approach for BAP1-deficient cancers, show high potency but historically carry toxicity concerns, particularly cardiotoxicity [87].
Innovative Screening Methodologies for Enhanced Therapeutic Indices
Two-Phase Screening for Efficacy and Toxicity
A groundbreaking approach to address the therapeutic window challenge involves implementing parallel screening strategies that simultaneously assess efficacy and toxicity. A representative study developed a two-phase screening protocol that identified quisinostat as a therapeutic candidate for BAP1-mutant cancers while minimizing toxicity concerns [87].
Experimental Protocol: Two-Phase Screening
Phase I: Cell-Based Transcription Rescue Screen
- Objective: Identify compounds that reverse transcriptional repression caused by BAP1 loss.
- Cell Model: 92.1-Tet-shBAP1 cells (uveal melanoma with inducible BAP1 knockdown).
- Procedure:
- Plate cells in 384-well plates at 250 cells/well.
- Induce BAP1 knockdown with doxycycline (1 μg/mL) for 48 hours.
- Treat with compound libraries (LOPAC1280 and custom epigenetic libraries) for 72 hours.
- Measure rescue of glyoxalase 1 (GLO1) expression via RT-qPCR.
- Identify hits showing ≥70% rescue compared to positive controls.
Phase II: In Vivo Phenotype Rescue and Toxicity Screen
- Objective: Evaluate efficacy and toxicity of lead compounds in a whole-organism context.
- Model System: Xenopus laevis embryos.
- Procedure:
- Inject 1-cell stage embryos with control or Bap1-directed morpholino (15 ng).
- At stage 6, transfer embryos to buffer containing varying compound concentrations.
- Incubate for 48 hours at 21°C.
- Score for morphological abnormalities at early neurula and tailbud stages.
- Identify compounds that rescue Bap1-deficient phenotype without toxicity.
This innovative approach enabled researchers to identify quisinostat from a library of 1280 compounds as the only candidate that effectively rescued the BAP1-deficiency phenotype without causing significant toxicity in the Xenopus model [87]. The study highlights how conventional viability-based screens often miss compounds with desirable therapeutic windows, as they may eliminate candidates that reverse disease phenotypes without directly killing cells.
Diagram 1: Two-phase screening workflow for therapeutic window optimization.
Leveraging the Tumor Microenvironment for Selective Targeting
An alternative strategy for optimizing therapeutic windows involves exploiting differences between tumor and normal cells within the context of the tumor microenvironment (TME). Several DUBs have been identified as key regulators of immune cell function and infiltration within the TME, creating opportunities for selective immunomodulatory approaches [85] [14].
Key Findings on DUBs in the TME:
- USP10 desensitizes PDAC cells to natural killer (NK) cell-mediated cytotoxicity by deubiquitinating YAP1, leading to upregulated PD-L1 and galectin-9 expression [85] [14].
- USP22 suppresses NK cell infiltration by altering the transcriptome of pancreatic cancer cells [85].
- OTUD5 and USP14 promote M2 macrophage polarization, establishing an immunosuppressive microenvironment that facilitates metastasis [85].
- USP1 in macrophages inhibits CD8+ T cell recruitment while promoting cancer stemness and metastasis in colorectal cancer [14].
Targeting these DUBs offers a potential therapeutic window advantage because their inhibition may preferentially impact the immunosuppressive TME rather than directly affecting fundamental cellular processes in healthy tissues. This approach aligns with the broader shift in oncology toward immune-modulating strategies that leverage differences between tumor and normal microenvironments.
Emerging Technologies: DUBTACs and PROTACs
Nover therapeutic modalities that leverage the ubiquitin-proteasome system itself offer promising approaches to enhance therapeutic windows. Deubiquitinase-targeting chimeras (DUBTACs) and proteolysis-targeting chimeras (PROTACs) represent particularly innovative strategies [3] [88].
DUBTACs are heterobifunctional molecules that consist of a ligand for a target protein of interest linked to a recruiter for a specific DUB. This configuration brings the DUB into proximity with the target protein, promoting its deubiquitination and stabilization [3]. This approach is particularly valuable for targeting diseases caused by haploinsufficiency or loss-of-function mutations in tumor suppressors.
PROTACs operate on the opposite principle, recruiting E3 ubiquitin ligases to target proteins to induce their degradation. Several PROTACs have advanced to clinical trials, including ARV-110 and ARV-471 for prostate and breast cancer, respectively [19].
Table 3: Comparison of Targeted Protein Modulation Platforms
| Platform | Mechanism | Advantages for Therapeutic Window | Challenges |
|---|---|---|---|
| DUBTACs | Stabilization of target proteins | Potential to treat diseases caused by protein deficiency | Limited preclinical validation to date |
| PROTACs | Degradation of target proteins | Catalytic mode of action allows lower dosing | Tissue distribution and bioavailability |
| Traditional Inhibitors | Inhibition of enzymatic activity | Well-established development pathways | Target compensatory mechanisms often limit efficacy |
The catalytic nature of both DUBTACs and PROTACs may provide therapeutic window advantages by allowing lower drug exposures to achieve the desired pharmacological effect, potentially reducing off-target toxicities [3]. Additionally, these approaches can target proteins traditionally considered "undruggable" by small molecule inhibitors, greatly expanding the therapeutic landscape in oncology.
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 4: Key Research Reagents for DUB Therapeutic Window Investigations
| Reagent/Material | Function/Application | Example in Context |
|---|---|---|
| Tet-pLKO-puro vector | Inducible shRNA expression for conditional gene knockdown | Knockdown of BAP1 in uveal melanoma cell lines [87] |
| LOPAC1280 library | Library of Pharmacologically Active Compounds for screening | Identification of transcriptional rescue compounds [87] |
| Custom epigenetic libraries | Targeted compound collections focusing on epigenetic regulators | Screening for BAP1-related therapeutics [87] |
| Xenopus laevis embryos | In vivo model for simultaneous efficacy and toxicity assessment | Phenotype rescue and toxicity screening for lead compounds [87] |
| PDX-derived cell lines | Patient-derived xenograft cells maintaining tumor characteristics | BAP1-mutant uveal melanoma models (MM28, MP46) [87] |
| Activity-based probes (ABPs) | Chemical tools for profiling DUB activity and engagement | Assessing target occupancy and selectivity of DUB inhibitors [3] |
Optimizing the therapeutic window for DUB-targeted therapies requires a multifaceted approach that integrates innovative screening methodologies, tissue-specific delivery strategies, and patient stratification based on molecular biomarkers. The traditional drug development paradigm focused primarily on potency often fails to deliver clinically viable compounds for DUB targets due to their fundamental roles in cellular homeostasis. Future success will depend on:
- Advanced screening platforms that simultaneously evaluate efficacy and toxicity, such as the two-phase approach that identified quisinostat [87].
- Tissue-specific targeting strategies that leverage differences between tumor and normal tissue microenvironments, particularly through immunomodulatory mechanisms [85] [14].
- Patient stratification biomarkers to identify individuals most likely to respond to specific DUB-targeted therapies based on tumor genetics and DUB expression profiles.
- Novel therapeutic modalities like DUBTACs and PROTACs that offer catalytic activity and potentially wider therapeutic windows [3] [88].
As our understanding of DUB biology in both normal physiology and disease states continues to evolve, so too will our ability to design therapeutics that selectively target pathological processes while sparing essential physiological functions. The integration of mechanistic studies with sophisticated screening approaches represents the most promising path forward for unlocking the full potential of DUB-targeted cancer therapies with optimal therapeutic windows.
Deubiquitinating enzymes (DUBs) represent a family of approximately 100 proteases that catalyze the removal of ubiquitin chains from substrate proteins, thereby reversing the process of ubiquitination and regulating protein stability, localization, and activity [11] [19]. The dynamic balance between ubiquitination by E1, E2, and E3 enzymes and deubiquitination by DUBs constitutes a critical regulatory mechanism for cellular homeostasis [19]. In cancer, this balance is frequently disrupted, with many DUBs demonstrating overexpression or heightened activity that promotes tumorigenesis through stabilization of oncoproteins, protection from apoptosis, and enhancement of DNA repair mechanisms [4] [89]. The strategic inhibition of specific DUBs has consequently emerged as a promising therapeutic approach, particularly when integrated with established treatment modalities to overcome chemoresistance and enhance antitumor efficacy [7].
The molecular rationale for combining DUB inhibitors with conventional and targeted therapies stems from the multifaceted roles DUBs play in cancer cell survival pathways. DUBs regulate all core cancer hallmarks, including "evading growth suppressors," "reprogramming energy metabolism," "unlocking phenotypic plasticity," and maintaining "senescent cells" [19]. By disrupting these processes through DUB inhibition, cancer cells become more vulnerable to traditional chemotherapeutic agents and molecularly targeted drugs. Furthermore, emerging research reveals that DUB inhibition can modulate the tumor immune microenvironment, potentially enhancing response to immunotherapies [90]. This in-depth technical review examines the current landscape of DUB inhibitor-based combination strategies, detailing mechanistic insights, experimental evidence, and translational potential for researchers and drug development professionals working in oncology.
Molecular Mechanisms of DUBs in Cancer Therapy Resistance
Regulation of Oncoprotein Stability and DNA Damage Repair
DUBs confer resistance to conventional therapies through multiple interconnected mechanisms, chief among them being the stabilization of key oncoproteins and enhancement of DNA damage repair. USP7 exemplifies this dual function by deubiquitinating and stabilizing both MDM2 and p53, creating a complex regulatory circuit that influences tumor cell survival [90]. In the context of chemotherapy, USP7-mediated stabilization of MDM2 leads to enhanced degradation of p53, blunting the apoptotic response to genotoxic stress. Simultaneously, USP7 directly stabilizes p53 in certain cellular contexts, illustrating the context-dependent functions of DUBs that must be considered for therapeutic targeting [90]. This dual substrate specificity enables cancer cells to fine-tune their response to therapeutic insults.
The regulation of DNA damage repair represents another critical resistance mechanism orchestrated by DUBs. Numerous DUBs are recruited to sites of DNA damage where they modulate the stability and function of repair proteins [11]. For instance, USP1 regulates the Fanconi anemia pathway by deubiquitinating FANCD2, while USP10 deubiquitinates and stabilizes MutS homolog 2 (MSH2), a key mismatch repair protein [7]. By enhancing DNA repair capacity, these DUBs enable cancer cells to survive chemotherapy-induced DNA damage, particularly from platinum-based agents and radiation. Inhibition of these DUBs consequently sensitizes tumors to DNA-damaging therapies by preventing efficient repair of lethal lesions.
Metabolic Reprogramming and Immune Evasion
Cancer cells undergo metabolic reprogramming to support rapid proliferation and survival under stress conditions, and DUBs are integral to this process. Several DUBs regulate key metabolic enzymes and transcription factors that drive the Warburg effect (aerobic glycolysis) in cancer cells [43]. USP29 stabilizes both MYC and HIF1α, two master regulators of cancer metabolism, while UCHL3 promotes glycolysis in pancreatic cancer through the FOXM1-LDHA axis [43]. OTUB2 enhances glycolytic flux in colorectal cancer by stabilizing PKM2, and CSN5 (COPS5) stabilizes hexokinase 2 (HK2) in hepatocellular carcinoma [43]. These metabolic adaptations not only support biomass production but also confer resistance to therapies by maintaining energy homeostasis and redox balance under treatment stress.
Beyond cell-intrinsic mechanisms, DUBs also shape the tumor immune microenvironment to foster resistance. USP7 inhibition has been demonstrated to remodel the tumor microenvironment by enhancing T-cell cytotoxicity, reducing PD-L1 expression on myeloid cells, and diminishing immunosuppressive macrophage populations [90]. Similarly, USP2 can deubiquitinate and stabilize PD-1 on T cells, promoting T-cell exhaustion and immune escape [19]. These findings establish DUBs as crucial regulators of antitumor immunity and suggest that their inhibition may reverse immunosuppression and enhance response to immune checkpoint inhibitors, particularly in immunologically "cold" tumors.
Table 1: DUBs Implicated in Therapy Resistance and Their Key Substrates
| DUB | Cancer Type | Key Substrates | Resistance Mechanism |
|---|---|---|---|
| USP7 | Multiple (Melanoma, Colorectal, Hematological) | MDM2, p53, DNMT1 | Oncoprotein stabilization, DNA repair, Immune evasion |
| USP9X | Pancreatic | LATS kinase, YAP/TAZ | Regulation of Hippo pathway, Apoptosis avoidance |
| USP34 | Pancreatic | AKT, PKC pathways | Cell survival signaling |
| USP22 | Pancreatic | PTEN, DYRK1A | Stemness maintenance, Metabolic reprogramming |
| OTUB2 | Colorectal | PKM2, U2AF2 | Metabolic reprogramming, AKT/mTOR signaling |
| UCHL3 | Pancreatic | FOXM1 | Enhancement of aerobic glycolysis |
| USP10 | Multiple | AMPK, MSH2 | Energy stress response, DNA mismatch repair |
Strategic Combination Approaches with DUB Inhibitors
DUB Inhibitors with Conventional Chemotherapy
The combination of DUB inhibitors with conventional chemotherapy represents a promising strategy to overcome de novo and acquired chemoresistance. Preclinical studies across multiple cancer types have demonstrated that pharmacological inhibition of specific DUBs can resensitize resistant tumors to standard chemotherapeutic agents. In pancreatic ductal adenocarcinoma (PDAC), a malignancy notorious for chemoresistance, USP9X inhibition improves gemcitabine sensitivity by inhibiting autophagy [7]. Similarly, USP8 promotes gemcitabine resistance in pancreatic cancer by stabilizing Nrf2, and its inhibition restores therapeutic response [7]. These findings highlight how targeting DUB-mediated resistance pathways can expand the efficacy of cornerstone chemotherapies.
The molecular mechanisms underlying chemo-sensitization by DUB inhibitors are diverse and context-dependent. In gastric cancer, inhibition of USP11 sensitizes tumors to oxaliplatin by suppressing RhoA and Ras-mediated signaling pathways [7]. In non-small cell lung cancer (NSCLC), USP35 mediates cisplatin resistance by stabilizing BIRC3, an inhibitor of apoptosis protein, and its depletion enhances cisplatin-induced cell death [7]. The table below summarizes key DUB inhibitor-chemotherapy combinations with demonstrated preclinical efficacy, providing a roadmap for translational development.
Table 2: DUB Inhibitor Combinations with Conventional Chemotherapy
| DUB Target | Chemotherapy Agent | Cancer Type | Molecular Mechanism | Experimental Model |
|---|---|---|---|---|
| USP9X | Gemcitabine | Pancreatic | Inhibition of autophagy | In vitro, In vivo [7] |
| USP8 | Gemcitabine | Pancreatic | Stabilization of Nrf2 | In vitro [7] |
| USP11 | Oxaliplatin | Gastric | Suppression of RhoA/Ras signaling | In vitro [7] |
| USP35 | Cisplatin | Non-small cell lung | Stabilization of BIRC3 | In vitro [7] |
| USP22 | Cisplatin | Pancreatic | Modulation of stemness via Wnt/β-catenin | In vitro [7] |
| USP10 | 5-FU/Oxaliplatin | Colorectal | Regulation of AMPK energy sensing | In vitro [43] |
| USP1 | Cisplatin | Ovarian | Regulation of FANCD2 in DNA repair | In vitro [11] |
DUB Inhibitors with Targeted Therapies
The integration of DUB inhibitors with molecularly targeted agents offers opportunities for enhanced precision and reduced toxicity through synergistic pathway inhibition. This approach is particularly relevant for tumors driven by oncogenes that are stabilized by specific DUBs. For instance, in pancreatic cancer, KRAS mutations are present in approximately 90% of cases, and DUBs such as USP21 and USP34 facilitate downstream signaling through multiple pathways, including mTOR and MAPK signaling [4]. Co-targeting these DUBs with direct KRAS inhibitors or downstream pathway inhibitors may prevent compensatory stabilization of oncogenic signaling nodes and delay resistance emergence.
Emerging research highlights novel synthetic lethal interactions between DUB inhibitors and targeted agents. In acute myeloid leukemia (AML), combining MCL-1 inhibitors with SRC kinase inhibitors demonstrates synergistic lethality by preventing compensatory MCL-1 accumulation [91]. As many DUBs regulate protein stability in a context-dependent manner, systematic screening approaches are needed to identify optimal DUB inhibitor-targeted therapy combinations. The development of PROTACs (Proteolysis Targeting Chimeras) that leverage the ubiquitin-proteasome system for targeted protein degradation further expands combinatorial possibilities with DUB inhibitors [19]. These bifunctional molecules recruit E3 ligases to target proteins, and their efficacy may be enhanced by inhibiting DUBs that would otherwise protect the target protein from degradation.
Figure 1: Synergistic Interaction Between DUB Inhibitors and Targeted Therapies. DUB inhibitors prevent stabilization of oncoproteins, enhancing their degradation and increasing cancer cell dependence on targeted pathway inhibition.
DUB Inhibitors with Immunotherapy
The intersection between DUB function and immune regulation presents compelling opportunities for combination with immunotherapies. USP7 inhibition exemplifies this approach, with studies demonstrating that USP7 inhibitors remodel the tumor immune microenvironment by enhancing T-cell activation, reducing immunosuppressive populations, and decreasing PD-L1 expression on antigen-presenting cells [90]. The lead compound OAT-4828, a selective USP7 inhibitor, demonstrated significant antitumor activity in melanoma and colon cancer models that was critically dependent on T-cell function, as determined by depletion experiments [90]. This immunomodulatory effect provides strong rationale for combining USP7 inhibitors with immune checkpoint blockers.
Beyond USP7, multiple DUBs have been implicated in regulating immune checkpoint expression and function. USP2 can deubiquitinate and stabilize PD-1 on T cells, while USP22 promotes the Warburg effect in triple-negative breast cancer, potentially creating an immunosuppressive metabolic microenvironment [19] [7]. Additionally, the DUB CYLD regulates linear ubiquitination and NF-κB signaling, which plays important roles in immune cell activation [19]. Targeting these DUBs may reverse multiple resistance mechanisms to immunotherapy, including T-cell exhaustion, immunosuppressive metabolite production, and inadequate T-cell priming. The diagram below illustrates how DUB inhibition can reprogram the tumor immune microenvironment to enhance response to immunotherapies.
Figure 2: DUB Inhibition Reprograms the Tumor Immune Microenvironment. DUB inhibitors reduce immune checkpoint expression and diminish immunosuppressive cell populations, thereby enhancing T-cell function and response to immunotherapy.
Experimental Approaches and Methodological Considerations
Assessing Combination Efficacy: In Vitro and In Vivo Models
Robust preclinical evaluation of DUB inhibitor combinations requires integrated experimental approaches spanning molecular, cellular, and organismal levels. In vitro assessment typically begins with cell viability assays (e.g., MTT, CellTiter-Glo) to determine combination indices and identify synergistic, additive, or antagonistic interactions. For DUB inhibitors specifically, it is critical to concurrently monitor substrate protein stability via immunoblotting to verify target engagement and confirm mechanistic hypotheses. For instance, when combining USP7 inhibitors with DNA-damaging agents, researchers should demonstrate increased MDM2 degradation and p53 stabilization alongside enhanced apoptotic markers [90].
Advanced in vitro models provide deeper insights into combination mechanisms. Co-culture systems incorporating immune cells enable evaluation of DUB inhibitors' immunomodulatory effects. In such systems, OAT-4828 (a USP7 inhibitor) enhanced T-cell-mediated killing of cancer cells, demonstrating its potential to improve immunotherapy outcomes [90]. Similarly, 3D organoid cultures better recapitulate tumor architecture and microenvironmental interactions, offering more physiologically relevant platforms for assessing treatment efficacy and mechanisms of resistance.
In vivo validation remains essential for translational development. Patient-derived xenograft (PDX) models preserve tumor heterogeneity and microenvironmental interactions, providing clinically predictive assessment of combination efficacy. In PDAC models, USP34 suppression markedly inhibited tumor growth of PANC-1 cell xenografts in nude mice [4]. For immunocompetent models, syngeneic grafts enable evaluation of DUB inhibitors' effects on antitumor immunity. In B16F10 melanoma and CT26 colon carcinoma models, USP7 inhibition altered immune cell populations in the tumor microenvironment, enhancing T-cell activity and decreasing immunosuppressive proteins [90]. These comprehensive experimental approaches collectively build the mechanistic foundation for clinical translation of DUB inhibitor combinations.
The Scientist's Toolkit: Key Research Reagents and Assays
Table 3: Essential Research Reagents and Assays for DUB Inhibitor Studies
| Reagent/Assay | Specific Examples | Application and Function | Technical Considerations |
|---|---|---|---|
| Selective DUB Inhibitors | OAT-4828 (USP7 inhibitor) | Target validation, Combination studies | Verify selectivity across DUB families; assess on-target effects via substrate stabilization |
| Activity Assays | Ub-rhodamine 110 assay, Ub-CHOP2 assay | Measure DUB enzymatic activity and inhibition | Use recombinant DUBs; include catalytically inactive mutants as controls |
| Proteasome Inhibitors | Bortezomib, Carfilzomib | Distinguish proteasomal vs. non-proteasomal DUB functions | Can mask DUB inhibitor effects due to general proteostasis disruption |
| CRISPR/Cas9 Systems | DUB knockout cell pools | Genetic validation of pharmacological inhibition | Monitor for compensatory DUB upregulation |
| Ubiquitin Probes | HA-Ub, FLAG-Ub, Tandem Ubiquitin Binding Entities (TUBEs) | Assess ubiquitination status of substrates | Multiple linkage types (K48, K63, M1) to assess chain specificity |
| Apoptosis Assays | Annexin V staining, Caspase-3/7 activation | Quantify cell death in combination treatments | Distinguish apoptotic from non-apoptotic cell death mechanisms |
| Immune Monitoring Tools | Multiplex cytokine arrays, Flow cytometry panels | Evaluate immune microenvironment changes | Include exhaustive marker panels for immune cell subsets |
Clinical Translation and Future Perspectives
The transition of DUB inhibitor combinations from preclinical models to clinical application presents both challenges and opportunities. While no DUB inhibitors have yet received FDA approval, several candidates have entered early-phase clinical trials, predominantly in hematological malignancies [7]. The clinical development roadmap for these agents will likely mirror that of proteasome inhibitors, which initially demonstrated efficacy in multiple myeloma and later expanded to other indications [11]. Strategic trial design incorporating biomarker-driven patient selection and mechanistic combination strategies will be essential for maximizing clinical success.
Biomarker development represents a critical frontier for DUB inhibitor therapeutics. Potential predictive biomarkers include expression levels of the target DUB, genetic alterations in substrate proteins, and specific molecular subtypes. For instance, USP9X expression and mutation status may predict response to its inhibition in pancreatic cancer, where it demonstrates context-dependent oncogenic or tumor suppressive functions [4]. Similarly, p53 status likely influences response to USP7 inhibitors, given the intricate regulation of the MDM2-p53 axis [90]. Pharmacodynamic biomarkers demonstrating target engagement, such as reduced substrate protein levels in tumor tissue or surrogate compartments, will also be crucial for dose optimization and confirming mechanistic activity in early-phase trials.
Future directions in DUB inhibitor combination strategies will likely exploit emerging technologies and novel therapeutic modalities. The integration of artificial intelligence and machine learning approaches promises to accelerate the identification of synergistic drug combinations and predictive biomarkers [92]. Additionally, the growing understanding of ubiquitin chain diversity and specificity may enable development of linkage-selective DUB inhibitors with refined therapeutic windows. Finally, the convergence of DUB inhibitors with novel degradation technologies such as PROTACs and molecular glues presents exciting opportunities for multi-tiered regulation of the ubiquitin-proteasome system [19]. As our understanding of DUB biology continues to mature, so too will our ability to strategically deploy their inhibitors in rational combinations that maximize therapeutic efficacy and overcome treatment resistance in oncology.
Clinical Translation and Comparative Analysis of DUB Targets
The ubiquitin-proteasome system (UPS) represents a crucial regulatory pathway for protein degradation and homeostasis within eukaryotic cells. Deubiquitinating enzymes (DUBs) constitute a diverse family of proteases that counterbalance ubiquitination by removing ubiquitin chains from substrate proteins, thereby regulating protein stability, localization, and function [4] [30]. With over 100 identified members categorized into seven primary families—ubiquitin-specific proteases (USPs), ovarian tumor proteases (OTUs), ubiquitin carboxyl-terminal hydrolases (UCHs), Machado-Joseph disease proteases (MJDs), JAMM/MPN domain-associated metallopeptidases (JAMMs), motif interacting with ubiquitin-containing novel DUB family (MINDY), and zinc finger containing ubiquitin peptidase 1 (ZUP1)—DUBs fine-tune critical cellular processes including cell cycle progression, DNA damage repair, apoptosis, and immune responses [4] [3] [30]. The dysregulation of DUB expression and activity has been intimately linked to cancer pathogenesis, positioning them as promising therapeutic targets in oncology. This review focuses on the validation of specific DUB targets—particularly USP7, USP1, and USP14—across various cancer contexts, summarizing current preclinical and clinical evidence while providing technical guidance for ongoing research and drug development efforts.
Validated Oncogenic DUBs: Mechanisms and Preclinical Evidence
USP7: A Multifunctional Regulator in Cancer and Immunity
Ubiquitin-specific peptidase 7 (USP7), also known as herpesvirus-associated ubiquitin-specific protease (HAUSP), has emerged as a prominent oncogenic DUB with validated roles across multiple cancer types. USP7 exhibits its cancer-promoting effects primarily through stabilization of key oncoproteins and regulation of the tumor microenvironment.
Mechanistic Insights: USP7 demonstrates highest binding affinity for MDM2, the primary E3 ubiquitin ligase targeting p53 for degradation. Inhibition of USP7 triggers MDM2 destabilization, resulting in p53 stabilization and reactivation of its tumor-suppressive functions [90]. Beyond the MDM2-p53 axis, USP7 regulates additional cancer-relevant substrates. In acute myeloid leukemia (AML), USP7 directly binds to and deubiquitinates leucine-rich repeat kinase 2 (LRRK2), preventing its proteasomal degradation through removal of K48-linked polyubiquitin chains. This stabilization promotes AML cell growth and oncogenic potential, with USP7 inhibition suppressing these effects in a LRRK2-dependent manner [93]. USP7 also exhibits immunomodulatory functions within the tumor microenvironment, influencing T-cell activity, macrophage polarization, and dendritic cell function [90].
Therapeutic Development: The novel USP7 inhibitor OAT-4828 demonstrates potent antitumor activity in melanoma and colon cancer models. This orally available compound operates at nanomolar concentrations and significantly influences immune cell populations, enhancing T-cell cytotoxicity and reducing immunosuppressive protein expression [90].
Figure 1: USP7 Oncogenic Signaling Network. USP7 stabilizes multiple oncogenic substrates including MDM2 and LRRK2 while modulating immune cell function in the tumor microenvironment.
USP1: DNA Damage Response and Therapeutic Applications
USP1 functions as a key regulator of DNA damage response pathways, particularly through its association with the cofactor UAF1, which markedly enhances its catalytic activity. USP1/UAF1 complex has emerged as a promising target in specific cancer contexts.
Mechanistic Insights: USP1/UAF1 primarily targets proliferating cell nuclear antigen (PCNA) and Fanconi anemia proteins FANCI/FANCD2, playing crucial roles in DNA damage tolerance (DDT) and interstrand crosslink repair [94]. During replication stress, PCNA monoubiquitination at K164 (PCNA-Ub) recruits translesion synthesis polymerases to bypass DNA lesions. Recent research reveals that USP1/UAF1 processes polyubiquitinated PCNA through an exo-cleavage mechanism, preferentially cleaving ubiquitin-ubiquitin bonds over ubiquitin-PCNA bonds. This enzymatic preference can temporarily enrich monoubiquitinated PCNA during polyubiquitination, potentially influencing the balance between error-prone translesion synthesis and error-free template switching pathways [94].
Therapeutic Applications: USP1 inhibition demonstrates particular efficacy in BRCA1/2-deficient tumors, where it exhibits synthetic lethality with PARP inhibition. This combination approach may also help prevent PARP resistance development. In the absence of functional USP1, K48-linked ubiquitin chains accumulate on PCNA through UBE2K and RNF138 activity, ultimately leading to PCNA degradation by the proteasome [94].
USP14: Proteasomal Regulation and Drug Resistance
USP14 associates with the 19S regulatory particle of the proteasome and has been validated as a contributor to aggressive tumor behavior and drug resistance in various malignancies.
Functional Validation in Ovarian Carcinoma: USP14 mRNA expression correlates with tumor grade in clinical specimens from 134 ovarian carcinoma patients. Functional studies demonstrate that exogenous USP14 overexpression enhances survival of cisplatin-resistant IGROV-1/Pt1 cells upon cisplatin exposure. Conversely, USP14 knockdown in resistant cells reduces aggressive features and restores cisplatin sensitivity, establishing USP14 as a mediator of the cisplatin-resistant phenotype [95]. Screening of 1,056 small molecules identified ARN12502 as a promising USP14 inhibitor with an IC50 of 18.4 µM. Molecular dynamics simulations confirmed stable binding in two distinct modes, while cellular assays demonstrated proteasome-inhibitory activity in sensor-expressing cells [95].
Broader Oncogenic Roles: Beyond ovarian cancer, USP14 promotes tumor progression through multiple mechanisms. In hepatocellular carcinoma, USP14 enhances cancer cell growth by deubiquitinating HK2, AKT, and p62, thereby regulating glycolysis and autophagy. In oral squamous cell carcinoma, USP14 deubiquitinates SOX2, promoting stem-like properties and tumor aggressiveness [95].
Methodological Approaches for DUB Research
Biochemical and Cellular Assays for DUB Activity Assessment
Ubiquitin-Rhodamine 110 Hydrolysis Assay: This fluorescence-based assay employs Ub-Rho110Gly substrate (500 nM final concentration) in buffer containing 50 mM HEPES pH 7.5, 150 mM sodium chloride, 2 mM DTT, 0.05% Tween 20, and 1 mg/mL BSA. The DUB enzyme (e.g., USP7 at 0.4 nM) is incubated with candidate inhibitors, and fluorescence is measured at excitation 485 nm/emission 535 nm following 30-minute incubation at 25°C [90].
Ub-CHOP2 Reporter Assay: This catalytic reporter system utilizes USP7 enzyme (0.75 nM) with substrates Ub-CHOP2-Reporter and CHOP2-Substrate (100 nM each) in 20 mM Tris pH 8, 2 mM CaCl₂, 0.05% Tween, 2 mM DTT. Fluorescence is measured after 60-minute incubation at 25°C [90].
Cellular Sensitivity Assays: Colony-forming assays evaluate drug sensitivity by seeding cells in 6-well plates (100 cells/cm²) followed by treatment with serial drug dilutions. After 2 weeks of continuous exposure, colonies are fixed, stained with crystal violet, and counted. IC50 values are defined as drug concentrations reducing cell survival by 50% [95].
Genetic Manipulation Techniques
Loss-of-Function Studies: siRNA-mediated knockdown utilizes specific siRNAs (e.g., Silencer Select s17358 and s17360 for USP14) transfected at 10 nM concentration using Lipofectamine RNAiMAX in Opti-MEM medium. Validation occurs 48-72 hours post-transfection [95].
Gain-of-Function Studies: Lentiviral infection introduces target genes (e.g., USP14-Myc-DDK tagged constructs) followed by selection with puromycin (5 μg/mL) initiated 72 hours post-infection. Transgene expression is verified by Western blotting [95].
Table 1: Experimental Approaches for DUB Target Validation
| Method Category | Specific Technique | Key Applications | Representative Parameters |
|---|---|---|---|
| Biochemical Assays | Ubiquitin-Rhodamine 110 assay | DUB inhibitor screening | 0.4 nM USP7, 500 nM Ub-Rho110, 30 min incubation |
| Cellular Assays | Colony formation assay | Drug sensitivity testing | 100 cells/cm², 2-week exposure, crystal violet staining |
| Genetic Manipulation | siRNA knockdown | Loss-of-function studies | 10 nM siRNA, Lipofectamine RNAiMAX, 48-72h validation |
| Genetic Manipulation | Lentiviral overexpression | Gain-of-function studies | USP14-Myc-DDK constructs, 5 μg/mL puromycin selection |
Research Reagent Solutions
Table 2: Essential Research Reagents for DUB Investigation
| Reagent Category | Specific Examples | Research Applications | Key Features |
|---|---|---|---|
| Cell Line Models | IGROV-1/Pt1 (cisplatin-resistant ovarian cancer) | Drug resistance studies | Derived from parental IGROV-1, maintained in RPMI-1640 + 10% FBS |
| Chemical Inhibitors | OAT-4828 (USP7 inhibitor) | Mechanism studies/therapeutic testing | Oral availability, nanomolar potency, immunomodulatory effects |
| Chemical Inhibitors | ARN12502 (USP14 inhibitor) | Target validation | IC50 18.4 µM, proteasome-inhibitory activity |
| Chemical Inhibitors | IU1 (USP14 inhibitor) | Proof-of-concept studies | Well-characterized reference compound |
| Activity Probes | Diubiquitin vinyl amide (UbVAUb) | Cleavage mechanism studies | K63-linkage mimic, conjugates to DUB during cleavage attempt |
| Screening Libraries | IIT compound library (1,056 molecules) | Inhibitor discovery | Initial screening at 20 µM concentration in DMSO |
Emerging DUB Targets and Clinical Perspectives
OTUD Family Members in Cancer Regulation
The OTUD subfamily represents a novel group within the OTU family with significant DUB activities. OTUD1 demonstrates tumor-suppressive functions by stabilizing p53 through preferential cleavage of K48-linked polyubiquitin chains, promoting apoptosis and inhibiting colony formation [31]. In breast cancer, OTUD1 prevents SMAD7 degradation by cleaving its K48-linked polyubiquitin chains, subsequently antagonizing TGF-β-mediated epithelial-mesenchymal transition and cancer stem cell properties [31]. OTUD5 (also known as DUBA) has been implicated in multiple cancer types, with ongoing investigations exploring its substrate profiles and therapeutic potential.
Ataxin-3: Context-Dependent Oncogenic Functions
Ataxin-3 (ATXN3), a member of the MJD family, exhibits context-dependent roles in cancer pathogenesis. Dysregulation or overexpression of ATXN3 occurs in gastric, breast, lung, renal, oral squamous cell carcinoma, and anaplastic thyroid cancer, often correlating with aggressive tumor phenotypes and poor prognosis [12]. ATXN3 modulates tumor progression through critical signaling cascades including PI3K/Akt, Hippo/YAP, and TGF-β pathways. Recent findings position ATXN3 as a regulator of immune checkpoints, particularly through enhancing PD-L1 expression, thereby facilitating immune evasion [12].
Figure 2: Emerging DUB Targets in Cancer. OTUD1 exhibits tumor-suppressive functions by stabilizing p53 and SMAD7, while ATXN3 displays context-dependent oncogenic roles through YAP1 stabilization and PD-L1 enhancement.
The systematic validation of DUB targets in specific cancer contexts has revealed compelling opportunities for therapeutic intervention. USP7, USP1, and USP14 represent the most extensively characterized targets with strong mechanistic links to oncogenesis, drug resistance, and immune evasion. The development of selective inhibitors for these DUBs continues to advance, with several candidates demonstrating promising preclinical efficacy.
Future research directions should prioritize the development of more selective DUB inhibitors with improved pharmacological properties, comprehensive exploration of DUB functions within the tumor microenvironment, identification of predictive biomarkers for patient stratification, and investigation of DUB inhibitors in rational combination therapies. As the DUB field matures, these targeted approaches hold significant potential for advancing precision oncology paradigms and addressing unmet needs in cancer therapy.
Deubiquitinating enzymes (DUBs) represent a growing class of therapeutic targets in oncology due to their central role in regulating protein stability and function within the ubiquitin-proteasome system (UPS). The UPS is a critical pathway for maintaining cellular homeostasis through controlled protein degradation, and its dysfunction is implicated in various human diseases, including cancer [3]. DUBs, comprising approximately 100 proteases, reverse the process of ubiquitination by removing ubiquitin chains from substrate proteins, thereby regulating protein fate and function [59] [4]. This regulatory capacity positions DUBs as pivotal modulators of key cellular processes often dysregulated in cancer, such as cell cycle progression, DNA damage repair, apoptosis, and immune response [4] [3].
The therapeutic rationale for targeting DUBs in cancer stems from the observation that specific DUBs are frequently overexpressed or dysregulated in various malignancies, where they often stabilize oncoproteins or destabilize tumor suppressors [4] [12]. For instance, USP7 stabilizes MDM2, leading to p53 degradation, while USP9X enhances Mcl-1 stability, promoting tumor cell survival [3]. Inhibiting these DUBs can therefore restore natural tumor suppressive mechanisms and trigger cancer cell death. The emergence of small molecule DUB inhibitors represents a promising frontier in targeted cancer therapy, with several candidates now advancing through preclinical and clinical development pipelines [59] [3].
Current DUB Inhibitor Pipeline: From Discovery to Clinical Evaluation
The DUB inhibitor landscape has expanded significantly, with multiple candidates progressing through various stages of development. The following table summarizes key DUB inhibitors currently in preclinical and clinical development:
Table 1: DUB Inhibitors in Development Pipelines
| Drug/Candidate | Target | Developers | Development Stage | Key Indications/Focus |
|---|---|---|---|---|
| MTX325 | USP30 | Mission Therapeutics | Phase I (Cleared for clinical trials) | Parkinson's disease, Cancer [59] [60] |
| MTX652 | USP30 | Mission Therapeutics | Clinical trials | Parkinson's disease, Cancer [59] [60] |
| TNG348 | USP1 | Tango Therapeutics | Phase I | BRCA-mutant cancers [59] |
| KSQ-4279 | USP1 | KSQ Therapeutics/Roche | Preclinical/Phase I | Advanced solid tumors [59] |
| OAT-4828 | Undisclosed | Molecure | Preclinical | Not specified [59] |
| ASN3186/AT012 | Undisclosed | Asieris Pharmaceuticals | Preclinical | Not specified [59] |
| Sepantronium (PC-002/YM155) | Undisclosed | Cothera Bioscience | Phase I | Various cancers [59] |
| VLX1570 | USP14/UCHL5 | Vivolux | Discontinued (Phase I/II) | Multiple myeloma [59] |
The pipeline demonstrates several notable trends. First, there is significant focus on specific DUB families, particularly ubiquitin-specific proteases (USPs), which constitute the largest DUB family with structural diversity [3]. Second, companies are pursuing both single-agent and combination therapy strategies, with some DUB inhibitors being explored alongside established modalities like PARP inhibitors for synergistic effects [59]. Third, the field is increasingly recognizing the potential of DUB inhibitors beyond oncology, with programs targeting neurodegenerative diseases, renal conditions, and fibrotic disorders [60] [96].
Mission Therapeutics has emerged as a key player with two USP30 inhibitors (MTX325 and MTX652) cleared for clinical trials. In July 2024, Mission Therapeutics received USD 5.2 million in funding from The Michael J. Fox Foundation for Parkinson's Research and Parkinson's UK to support MTX325 development, highlighting the growing interest and investment in DUB-targeted therapies [59]. Other notable companies advancing DUB inhibitors include KSQ Therapeutics (in collaboration with Roche), Tango Therapeutics, Carmot Therapeutics, and Almac Discovery [59] [97].
Mechanistic Insights: DUB Functions and Oncogenic Signaling Pathways
Molecular Classification and Functions of DUBs
Deubiquitinating enzymes are classified into seven primary families based on their catalytic domains and sequence conservation: ubiquitin-specific proteases (USPs), ubiquitin carboxyl-terminal hydrolases (UCHs), ovarian tumor proteases (OTUs), Machado-Joseph disease protein domain proteins (MJDs), JAMM/MPN domain-associated metallopeptidases (JAMMs), Zinc finger containing ubiquitin pepper 1 (ZUP1), and motif interacting with ubiquitin-containing novel DUB family proteins (MINDYs) [3]. The USP family is the largest and most structurally diverse, while JAMMs represent the only metallopeptidase family; the remaining six families are cysteine proteases [3].
DUBs regulate numerous cellular processes through several mechanisms: (1) processing ubiquitin precursors to generate mature ubiquitin; (2) removing ubiquitin chains from substrates to rescue them from degradation; (3) editing ubiquitin chains to alter signaling outcomes; and (4) maintaining free ubiquitin pools by recycling ubiquitin from substrates targeted to the proteasome [4] [3]. This functional versatility enables DUBs to fine-tune critical pathways dysregulated in cancer.
Key Oncogenic Pathways Regulated by DUBs
DUBs modulate multiple cancer-relevant signaling pathways. The following diagram illustrates several key DUB-regulated pathways in pancreatic ductal adenocarcinoma (PDAC), demonstrating their multifaceted roles in tumor biology:
Figure 1: DUB-Regulated Oncogenic Processes in PDAC. Multiple DUBs regulate key cancer hallmarks in pancreatic ductal adenocarcinoma through distinct mechanisms, highlighting their therapeutic potential. [4]
Specific examples of DUB-mediated pathway regulation include:
USP7 (HAUSP) and p53 Pathway: USP7 deubiquitinates and stabilizes MDM2, the primary E3 ubiquitin ligase for p53, leading to p53 degradation. USP7 inhibition consequently stabilizes p53, promoting cell cycle arrest and apoptosis [3]. USP7 also regulates PTEN stability and localization, further influencing oncogenic signaling [3] [12].
USP1 and DNA Damage Repair: USP1, in complex with UAF1, deubiquitinates PCNA and FANCD2, key regulators of DNA damage repair. USP1 inhibition persists DNA damage in cancer cells, creating synthetic lethality with DNA-damaging agents or PARP inhibitors, particularly in BRCA-deficient cancers [3].
USP30 and Mitophagy Regulation: USP30, a mitochondrial DUB, negatively regulates Parkin-mediated mitophagy by removing ubiquitin chains from mitochondrial proteins. USP30 inhibition enhances mitophagy, which may be beneficial in both neurodegenerative diseases and cancer [60] [96].
ATXN3 and Hippo/YAP Pathway: Ataxin-3 stabilizes Yes-associated protein 1 (YAP1), a transcriptional co-activator and central effector of the Hippo pathway, leading to enhanced proliferation and survival of cancer cells [12].
Experimental Approaches in DUB Inhibitor Development
Screening Cascades and Target Validation
Mission Therapeutics has developed a robust screening cascade designed to eliminate false positives early and focus on genuine drug candidates. Key elements of their approach include:
- Biochemical Assays: Using full-length DUBs purified from mammalian cells to ensure proper folding, post-translational modifications, and co-factors [60].
- Physiologically Relevant Substrates: Incorporating substrates with isopeptide linkages between ubiquitin and peptides derived from the DUB's cellular targets [60].
- Orthogonal Confirmatory Assays: Implementing multiple validation assays to eliminate false positives early in the discovery process [60].
- Cellular Target Engagement: Performing proprietary cellular target engagement assays as early as possible to confirm specific DUB inhibition in cells [60].
This comprehensive approach addresses historical challenges in DUB inhibitor development, particularly achieving specificity among the approximately 100 human DUBs with structurally similar active sites.
Chemistry Strategies for DUB Inhibition
Mission Therapeutics' chemistry platform has been optimized for therapeutically important DUB family members through several key strategies:
- Targeted Covalent Inhibitors: Developing compounds containing reversible, low-reactivity bond-forming functional groups that achieve >100-fold selectivity against large panels of DUBs and related enzymes [60].
- Proprietary Compound Library: Creating a DUB-specific library of over 17,000 molecules with exclusive and proprietary chemotypes that comply with 'rule of 5' criteria and lack toxicophores [60].
- Iterative Design-Make-Test Cycles: Accelerating drug discovery through in-house medicinal chemistry efforts guided by molecular modeling and structural biology [60].
These approaches have generated a high number of hits for particular DUB targets, enabling rapid progress in identifying optimized leads with candidate drug levels of potency, selectivity, pharmacokinetics, and in vivo efficacy.
Research Reagent Solutions for DUB Studies
Table 2: Essential Research Reagents for DUB Investigation
| Reagent Category | Specific Examples | Key Applications | Technical Considerations |
|---|---|---|---|
| Activity Assays | Ubiquitin-Rho-110 assay; Fluorescent polarization assays | High-throughput screening; Mechanistic studies | Substrate specificity; Signal-to-noise ratio [3] |
| Cellular Models | PDAC cell lines (PANC-1); KPC mouse models; Xenograft models | Target validation; Efficacy assessment | Physiological relevance; Species differences [4] [60] |
| Proteomic Tools | Activity-based probes; Ubiquitin chain linkage-specific antibodies | Target engagement; Mechanistic studies | Selectivity profiling; Endogenous detection [3] |
| Structural Biology | X-ray crystallography; Cryo-EM | Rational drug design; Selectivity optimization | Protein-cofactor complexes; Conformational states [3] [60] |
The experimental workflow for DUB inhibitor development typically follows a structured path from target identification through clinical candidate selection, as illustrated below:
Figure 2: DUB Inhibitor Development Workflow. The multi-stage process for developing DUB inhibitors incorporates rigorous screening and validation steps to address specificity challenges. [60]
Emerging Paradigms and Future Directions
Novel Therapeutic Applications
Beyond direct enzyme inhibition, DUB-targeting strategies are expanding to include several innovative approaches:
- PROTACs (Proteolysis-Targeting Chimeras): DUB inhibitors are being incorporated into PROTACs to selectively degrade target proteins. This approach leverages the UPS itself to eliminate disease-driving proteins [3].
- DUBTACs (Deubiquitinase-Targeting Chimeras): These bifunctional molecules recruit DUBs to specific target proteins to stabilize them, offering potential for treating diseases caused by protein deficiency [3].
- Immuno-oncology Applications: Emerging research reveals DUB involvement in immune checkpoint regulation. For example, ATXN3 was identified as a regulator of PD-L1, suggesting DUB inhibition may enhance anti-tumor immunity [12].
- Metabolic Reprogramming: DUBs are increasingly recognized as regulators of cancer metabolism. For instance, USP30 localizes to mitochondria and regulates metabolic pathways, positioning it as a target for metabolic diseases and cancer [30].
Clinical Development Considerations
Advancing DUB inhibitors to clinical application requires addressing several key challenges:
- Patient Selection Strategies: Incorporating biomarker strategies early in clinical development to enhance probability of demonstrating efficacy signals [60].
- Therapeutic Index Optimization: Balancing potent DUB inhibition with minimal off-target effects remains a critical hurdle, particularly for DUBs with widespread expression and multiple functions [3].
- Combination Therapy Rationale: Identifying synergistic partners, such as PARP inhibitors for USP1 inhibitors or DNA-damaging agents for USP7 inhibitors [3].
- Biomarker Development: Identifying predictive biomarkers for patient stratification and pharmacodynamic markers for target engagement monitoring [59] [60].
The DUB inhibitor field continues to evolve rapidly, with growing understanding of DUB biology and improving chemical tools for therapeutic intervention. While no DUB inhibitors have yet reached market approval, the compelling preclinical data and advancing clinical pipeline suggest these agents may soon emerge as valuable additions to the targeted therapy arsenal in oncology and beyond.
The ubiquitin-proteasome system (UPS) represents a critical therapeutic nexus in oncology, primarily targeted through two distinct strategies: proteasome inhibition and deubiquitinating enzyme (DUB) inhibition. While proteasome inhibitors like bortezomib and carfilzomib have established clinical utility in hematological malignancies, they face challenges including resistance development and systemic toxicity. Emerging DUB inhibitors offer a more targeted approach, modulating specific substrates and pathways with potentially refined therapeutic windows. This technical analysis comprehensively compares these complementary strategies, examining their molecular mechanisms, experimental methodologies, regulatory networks, and clinical translation potential within cancer therapeutics.
The ubiquitin-proteasome system represents the primary pathway for controlled intracellular protein degradation in eukaryotic cells, functioning through a coordinated enzymatic cascade [4] [98]. Ubiquitination initiates with ubiquitin activation by E1 enzymes, transfer to E2 conjugating enzymes, and final substrate specificity determination by E3 ligases, which covalently attach ubiquitin to target proteins [4]. The resulting ubiquitin code—comprising mono-ubiquitination, multi-ubiquitination, or poly-ubiquitination with various chain linkage types—dictates diverse cellular outcomes including proteasomal degradation, altered subcellular localization, modified activity, and regulated protein interactions [99] [57].
Deubiquitinating enzymes (DUBs) constitute approximately 100 proteases that reverse ubiquitination by cleaving ubiquitin from modified substrates, thereby functioning as crucial regulators of ubiquitin signaling dynamics [99] [4]. DUBs are categorized into seven families based on sequence and domain conservation: ubiquitin-specific proteases (USPs), ovarian tumor proteases (OTUs), ubiquitin carboxy-terminal hydrolases (UCHs), Machado-Josephin domain-containing proteases (MJDs), motif-interacting with ubiquitin-containing novel DUB family (MINDYs), JAB1/MPN/MOV34 family (JAMMs), and Zinc finger containing ubiquitin peptidase 1 (ZUP1) [4] [3]. With the exception of JAMMs (metalloproteases), all DUB families are cysteine proteases characterized by catalytic triads comprising conserved His, Cys, and Asn/Asp residues [3].
The balance between ubiquitination and deubiquitination regulates virtually all cellular processes, including cell cycle progression, apoptosis, DNA damage repair, transcriptional regulation, and immune signaling [100] [98]. Dysregulation of UPS components contributes significantly to oncogenesis, establishing both proteasomal complexes and DUBs as compelling therapeutic targets in cancer [4] [7].
Molecular Mechanisms and Regulatory Networks
Proteasome Inhibition: System-Level Disruption
Proteasome inhibitors function by blocking the 20S core particle of the proteasome, particularly its chymotrypsin-like activity, thereby inducing irreversible cell death through multiple interconnected mechanisms:
Protein Homeostasis Disruption: By preventing degradation of polyubiquitinated proteins, proteasome inhibitors cause accumulation of misfolded and deleterious proteins, triggering endoplasmic reticulum stress and unfolded protein response [101] [102].
Cell Cycle Arrest: Accumulation of cyclin-dependent kinase inhibitors (e.g., p21, p27) and modulation of cyclin levels disrupts cell cycle progression, particularly in rapidly dividing cancer cells [101].
Apoptosis Induction: Stabilization of pro-apoptotic factors (e.g., NOXA, BIM) and disruption of NF-κB signaling through inhibitor of κB (IκB) accumulation promotes programmed cell death [101].
Epigenetic Alterations: Recent evidence demonstrates that proteasome inhibition significantly alters DNA methylation patterns in colorectal cancer cells by suppressing DNA methyltransferase (DNMT1 and DNMT3B) synthesis via p300 accumulation and subsequent AKT-mTOR pathway inactivation [102].
Table 1: Clinically Utilized Proteasome Inhibitors
| Drug Name | Molecular Target | Approval Status | Primary Indications | Key Limitations |
|---|---|---|---|---|
| Bortezomib | 20S proteasome (chymotrypsin-like activity) | FDA-approved | Multiple myeloma, mantle cell lymphoma | Peripheral neuropathy, drug resistance |
| Carfilzomib | 20S proteasome (irreversible binding) | FDA-approved | Relapsed/refractory multiple myeloma | Cardiotoxicity, thrombotic microangiopathy [103] |
| Ixazomib | 20S proteasome (oral bioavailability) | FDA-approved | Relapsed multiple myeloma | Gastrointestinal toxicity, thrombocytopenia |
| MG132 | 20S proteasome (preclinical tool) | Research use only | Experimental models | Nonspecific effects |
DUB Inhibition: Precision Targeting of Ubiquitin Signaling
DUB inhibitors represent a more selective approach to modulating UPS by targeting specific components of the ubiquitin signaling network. The regulatory scope of DUBs is extensive, with recent studies identifying approximately 40,000 unique ubiquitination sites regulated by DUB activity, highlighting their profound influence on degradation-independent ubiquitin signaling [99]. Key mechanistic aspects include:
Substrate Stabilization Modulation: DUBs regulate stability of oncoproteins and tumor suppressors; inhibition promotes degradation of specific targets rather than global protein stabilization [4] [57].
Pathway-Specific Regulation: Individual DUBs frequently govern discrete signaling nodes, such as USP7's regulation of MDM2-p53 axis or USP9X's control of Hippo pathway effectors [4] [7].
DNA Damage Response Coordination: Multiple DUBs (USP1, USP10, USP11) regulate key DNA repair proteins, making their inhibition particularly relevant in BRCA-deficient cancers or in combination with genotoxic therapies [100].
Immune Microenvironment Modulation: DUBs shape antitumor immunity through regulation of PD-L1 stability (USP22), T-cell activation (USP7, CYLD, A20), and inflammatory signaling [98].
Table 2: Selected DUBs with Documented Roles in Cancer Pathways
| DUB | Family | Cancer Relevance | Key Substrates | Biological Processes Affected |
|---|---|---|---|---|
| USP1 | USP | DNA damage repair, chemotherapy resistance | ID proteins, PCNA | DNA damage tolerance, stemness maintenance [3] |
| USP7 | USP | Oncogene/tumor suppressor (context-dependent) | p53, MDM2, PTEN | Genome stability, cell cycle, apoptosis [3] [57] |
| USP9X | USP | Pancreatic cancer (dual roles) | FOXM1, MCL1, YAP/TAZ | Apoptosis resistance, Hippo signaling [4] [7] |
| USP22 | USP | Cancer stem cell marker | PD-L1, TRF2, RORγt | Immune evasion, telomere integrity [4] [98] |
| BAP1 | UCH | Tumor suppressor mutations | HCF1, ASXL1 | Chromatin remodeling, cell differentiation [4] |
| OTUD1 | OTU | Breast cancer metastasis | GSDMB, TRAF3 | Pyroptosis, innate immune signaling [4] |
Quantitative Comparison of Regulatory Scope
Global ubiquitinome analyses using advanced techniques like UbiSite technology have revealed distinct regulatory preferences within the UPS [99]:
Table 3: Ubiquitinome Regulation by DUB Inhibition vs. Proteasome Inhibition
| Parameter | DUB Inhibition (PR619) | Proteasome Inhibition (MG132) |
|---|---|---|
| Total regulated ubiquitination sites | >40,000 sites [99] | Preferentially regulates distinct substrate pool |
| Primary substrates affected | Degradation-independent signaling proteins | Proteasome-targeted degradation substrates |
| K48-linked ubiquitin chains | Accumulates | Strongly accumulates |
| K63-linked ubiquitin chains | Accumulates | Minimal effect |
| SUMO2/3 conjugates | Accumulates (mixed chains) | Accumulates (mixed chains) |
| Turnover kinetics | Rapid (hours) | Moderate |
| Cellular processes predominantly affected | Autophagy, apoptosis, genome integrity, telomere integrity, signal transduction, transcription, pre-mRNA splicing [99] | Cell cycle regulators, misfolded proteins, transcription factors |
These quantitative assessments demonstrate that DUBs and the proteasome regulate largely complementary aspects of the ubiquitinome, with DUBs exhibiting particularly strong influence on degradation-independent ubiquitin signaling networks.
Experimental Methodologies for Target Validation
Global Ubiquitinome Profiling
Comprehensive analysis of DUB and proteasome inhibitor effects requires integrated experimental approaches:
UbiSite Technology for Endogenous Ubiquitination Site Mapping
- Principle: Antibody recognizing Lys-C fragment of ubiquitin ensures specific enrichment of genuine ubiquitination sites without cross-reactivity with NEDD8 or ISG15 modifications [99].
- Cell Treatment: U2OS cells treated with DMSO (control), TAK243 (E1 inhibitor), MG132 (proteasome inhibitor), or PR619 (DUB inhibitor) for 3 hours.
- Ubiquitin Peptide Enrichment: UbiSite antibody-based immunoprecipitation of ubiquitinated peptides.
- Mass Spectrometry Analysis: LC-MS/MS with high-resolution Orbitrap instrumentation; database searching with false discovery rate correction.
- Data Processing: Intensity-based quantification; statistical analysis of ubiquitination site changes across conditions.
Tandem Ubiquitin Binding Entity (TUBE) Affinity Purification
- Application: Isolation of polyubiquitinated proteins while protecting against DUB activity during extraction.
- Lysis Conditions: Modified RIPA buffer supplemented with 20mM N-ethylmaleimide (DUB inhibitor), complete protease inhibitor cocktail, and 5mM EDTA.
- Purification: Incubation with agarose-conjugated TUBE1 for 2 hours at 4°C with rotation.
- Wash Steps: Three washes with lysis buffer containing 300mM NaCl, followed by two washes with 50mM ammonium bicarbonate.
- Analysis: On-bead tryptic digestion for MS analysis or elution for immunoblotting with linkage-specific ubiquitin antibodies.
Functional Validation of DUB Targets
Co-immunoprecipitation Assays for DUB-Substrate Identification
- Transfection: HEK293T cells co-transfected with FLAG-tagged DUB and MYC-tagged candidate substrate.
- Cell Lysis: NP-40 lysis buffer (50mM Tris-HCl pH 7.4, 150mM NaCl, 1% NP-40) with fresh 10mM N-ethylmaleimide.
- Immunoprecipitation: Anti-FLAG M2 affinity gel incubation for 4 hours at 4°C.
- Wash Conditions: Three washes with lysis buffer containing 500mM NaCl to reduce non-specific binding.
- Elution: 3X FLAG peptide competition or direct Laemmli buffer elution.
- Detection: Immunoblotting with anti-MYC for substrate association and anti-FLAG for DUB quantification.
Cycloheximide Chase Assays for Protein Half-Life Determination
- Pretreatment: Cells treated with DUB inhibitor or DMSO control for 4 hours.
- Translation Inhibition: 100μg/mL cycloheximide added to halt new protein synthesis.
- Time Course Collection: Cells harvested at 0, 1, 2, 4, 8, and 12 hours post-cycloheximide addition.
- Protein Quantification: Lysis with RIPA buffer, BCA protein assay normalization, and immunoblotting for protein of interest.
- Densitometry Analysis: ImageJ quantification with exponential decay modeling for half-life calculation.
Signaling Pathway Diagrams
Diagram Title: UPS Regulatory Network with Intervention Points
Diagram Title: Downstream Signaling Consequences
The Scientist's Toolkit: Essential Research Reagents
Table 4: Key Reagents for DUB and Proteasome Research
| Reagent/Category | Specific Examples | Research Application | Key Considerations |
|---|---|---|---|
| Proteasome Inhibitors | MG132, Bortezomib, Carfilzomib | Validation of proteasome-dependent degradation, induction of ER stress | Carfilzomib irreversible binding; MG132 broader specificity |
| DUB Inhibitors | PR619 (pan-DUB), P5091 (USP7), ML323 (USP1-UAF1) | Target validation, chemosensitization studies | PR619 inhibits cysteine DUBs; selectivity varies widely |
| Ubiquitin Enrichment Tools | UbiSite antibody, TUBE agarose, diGly remnant antibodies | Ubiquitinome profiling, substrate identification | UbiSite specific for ubiquitin (not NEDD8/ISG15) [99] |
| Activity-Based Probes | Ubiquitin-vinyl sulfone (UbVS), HA-Ub-VS | DUB activity profiling, catalytic site occupancy | Irreversible labeling of active DUBs; requires controlled labeling conditions |
| Linkage-Specific Antibodies | K48-Ub, K63-Ub, M1-Ub antibodies | Chain linkage analysis, pathway-specific ubiquitination | Validation with linkage-defined standards essential |
| Cell Line Models | HCT116 (colorectal), U2OS (osteosarcoma), MM.1S (multiple myeloma) | Mechanism studies, drug screening | Tissue-specific responses observed (e.g., DNMT downregulation) [102] |
Clinical Translation and Therapeutic Applications
Proteasome Inhibitors in Clinical Practice
Proteasome inhibitors have demonstrated significant clinical success, particularly in hematological malignancies:
Multiple Myeloma: Bortezomib-based regimens extended median survival from 2-3 years to 5-7 years; carfilzomib effective in bortezomib-resistant disease [101] [103].
Toxicity Management: Carfilzomib associated with thrombotic microangiopathy (8-day median onset); requires monitoring for anemia, thrombocytopenia, acute kidney injury [103].
Resistance Mechanisms: PSMB5 mutations, upregulated drug efflux pumps, and activation of alternative protein clearance pathways limit long-term efficacy [7].
Emerging DUB Inhibitors in Development
DUB inhibitor development has accelerated with several candidates entering clinical evaluation:
USP1 Inhibitors: KSQ-4279 in Phase I trials for BRCA-deficient cancers; demonstrates synthetic lethality in homologous recombination-deficient models [3].
USP7 Inhibitors: Multiple candidates (FT671, AL0024) in early-phase trials for solid tumors and hematologic malignancies; modulate p53-MDM2 axis [3] [57].
USP14/UCHL5 Inhibitors: VLX1570 advanced to Phase I/II trials for multiple myeloma but terminated due to toxicity concerns, highlighting delivery challenges [3].
Combination Therapy Strategies
Rational combination approaches leverage complementary mechanisms:
DUB Inhibitors with Chemotherapy: USP9X inhibition enhances gemcitabine efficacy in pancreatic cancer through autophagy inhibition [7].
DUB Inhibitors with Immunotherapy: USP7 and USP22 inhibition potentially reverse PD-L1-mediated T-cell exhaustion, enhancing checkpoint blockade efficacy [98].
Dual Pathway Targeting: Sequential or concurrent targeting of proteasome and specific DUBs may overcome resistance mechanisms while managing toxicity.
The comparative analysis of DUB targeting versus proteasome inhibition reveals two complementary therapeutic strategies with distinct mechanistic bases and clinical implications. Proteasome inhibitors achieve broad disruption of protein homeostasis with established efficacy but face limitations in solid tumors and toxicity management. DUB inhibitors offer precise targeting of specific oncogenic pathways with potential for enhanced therapeutic windows but require deeper target validation and optimized clinical development.
Future directions include advanced DUB inhibitor screening technologies, biomarker-driven patient stratification, and innovative therapeutic modalities such as DUB-targeting proteolysis-targeting chimeras (DUBTACs) that leverage specific DUBs to degrade pathogenic proteins. The integration of ubiquitinome profiling into clinical trial designs will further elucidate the complex regulatory networks governing treatment response and resistance mechanisms.
As the DUB inhibitor field advances from preclinical validation to clinical application, the strategic integration of both targeting approaches holds significant promise for overcoming current limitations in cancer therapy and expanding the therapeutic scope of ubiquitin-proteasome system modulation.
DUBs as Prognostic Markers and Biomarkers Across Cancer Types
Deubiquitinating enzymes (DUBs) represent a critical component of the ubiquitin-proteasome system, functioning as proteases that reverse protein ubiquitination by removing ubiquitin tags from target proteins. This process is fundamental to maintaining normal cellular homeostasis, influencing protein stability, localization, and activity [84]. The human genome encodes approximately 100 DUBs, which are classified into distinct families based on their catalytic domains, with the vast majority being cysteine proteases. The primary families include ubiquitin-specific proteases (USPs), ubiquitin C-terminal hydrolases (UCHs), ovarian tumor proteases (OTUs), Machado-Joseph disease proteases (MJDs), Jab1/Mov34/Mpr1 (JAMM) metalloproteases, and the motif-interacting with ubiquitin-containing novel DUB family (MINDY) [84] [24].
In cancer biology, DUBs have emerged as significant regulators of tumor progression, with their expression profiles often correlating with disease stage, patient prognosis, and therapeutic response [84]. They govern crucial cellular processes dysregulated in cancer, including cell cycle progression, apoptosis, DNA damage repair, and metastasis [24]. The balance between ubiquitination and deubiquitination determines the fate of key oncoproteins and tumor suppressors; consequently, aberrant DUB activity can disrupt this equilibrium, leading to uncontrolled cell growth and survival. Numerous studies have documented the elevated expression of specific DUB family members in various cancer cells and tissues, highlighting their potential not only as therapeutic targets but also as biomarkers for cancer diagnosis, staging, and prognosis prediction [84] [7]. This whitepaper synthesizes current evidence establishing DUBs as prognostic markers and biomarkers across diverse cancer types, providing a technical resource for researchers and drug development professionals.
DUBs as Prognostic Biomarkers in Specific Cancers
The expression levels of specific DUBs are frequently correlated with clinical outcomes in various cancers. Their role as prognostic biomarkers is often dependent on cancer type and cellular context. The table below summarizes key DUB biomarkers and their associated cancers and prognostic significance.
Table 1: DUBs as Prognostic Biomarkers Across Cancer Types
| DUB | Cancer Type | Expression in Cancer | Prognostic Significance | Molecular Substrates/Pathways |
|---|---|---|---|---|
| USP2 | Glioma | Increased | Correlates with malignant progression [84] | Mdm2, MdmX, Fatty Acid Synthase [84] |
| USP4 | Hepatocellular Carcinoma (HCC) | Increased | Novel marker for prognosis prediction [84] | CYPA, MAPK/CrkII signaling [84] |
| USP5 | Hepatocellular Carcinoma (HCC) | Increased | Potential therapeutic target; contributes to tumorigenesis [84] | p14–p53 signaling pathway [84] |
| USP7 | Hepatocellular Carcinoma (HCC) | Increased (mRNA & Protein) | Novel independent prognostic marker [84] | Ki-67, cell proliferation pathways [84] |
| USP8 | Cervical Squamous Cell Carcinoma (CSCC) | Upregulated | Independent prognostic marker; associated with tumor stage [84] | Smoothened, Frizzled, Receptor Tyrosine Kinases [84] |
| USP10 | Gastric Cancer | Decreased | Associated with invasion, metastasis, and poor survival [84] [89] | p53 [24] |
| USP22 | Hepatocellular Carcinoma (HCC) | Highly Elevated | Poor survival; independent prognostic marker [84] | Cancer stem cell marker [4] |
| USP32 | Primary Breast Cancer | Present in 22% of tumors | Implicated in oncogenesis [84] | Not specified in search results |
| CYLD | Hepatocellular Carcinoma (HCC) | Downregulated | Anti-inflammatory, anti-tumor role; deletion increases tumor susceptibility [24] | NF-κB signaling (via NEMO deubiquitination) [24] |
| OTUD3 | Breast Cancer | Decreased/Loss-of-function | Tumor-suppressing activity; stabilizes PTEN and p53 [26] | PTEN, p53 [26] |
Hepatocellular Carcinoma (HCC)
HCC demonstrates a strong association with the expression of several DUBs, making them valuable prognostic indicators. USP22 expression is extremely high in HCC tissues compared to normal liver, with elevated levels signifying poor patient survival, particularly in advanced tumor stages. Multivariate analyses establish USP22 as a self-regulating prognostic marker in HCC [84]. Similarly, USP7 mRNA and protein levels are significantly higher in HCC tissues, conferring cell proliferation, migration, and invasion capabilities, thus positioning it as a novel independent prognostic marker [84]. USP4 facilitates HCC progression by stabilizing CYPA and activating MAPK/CrkII signaling, acting as a novel marker to predict prognosis [84]. Conversely, CYLD often shows downregulation in HCC tissues and cell lines. Mouse model studies demonstrate that liver-specific deletion of CYLD increases susceptibility to chemically-induced liver tumor development, highlighting its anti-tumor and anti-inflammatory role, partly through the negative regulation of NF-κB signaling [24].
Breast Cancer
DUBs play complex, context-dependent roles in breast cancer pathogenesis and prognosis. USP32 is present in 22% of primary breast cancer tumors, suggesting a role in its development [84]. USP22, a member of a cancer stem cell signature, stabilizes the oncogenic protein c-Myc and promotes breast cancer cell growth. It also stabilizes estrogen receptor alpha (ERα), making it a biomarker in ER-positive breast cancer [26]. USP7 is overexpressed and indicates poor prognosis; it stabilizes ERα and the histone demethylase PHF8, forming positive feedback loops that drive tumor growth [26]. In contrast, OTUD3 exhibits tumor-suppressing activity by stabilizing both PTEN and p53, and its loss-of-function mutations or decreased expression are clinically significant in breast cancer [26].
Gastrointestinal and Gynecological Cancers
DUB dysregulation is also evident in other solid tumors. In gastric cancer (GC), clinical samples and cell lines show low-level expression of USP10, and its negative expression is associated with a marked propensity toward gastric wall invasion, lymph node metastasis, and poor survival, potentially serving as a new prognostic indicator [84] [89]. In cervical squamous cell carcinoma (CSCC), USP8 is upregulated compared to non-cancerous tissues, with high expression associated with tumor stage and identified as an independent prognostic marker [84]. For epithelial ovarian cancer (EOC), the combination of USP7 and MARCH7 protein expression may function as promising biomarkers for prognosis [84].
Quantitative Data on DUB Expression and Prognostic Value
The prognostic value of DUBs is often quantified through clinical studies correlating their expression levels with patient survival and other clinical parameters. The following table consolidates key quantitative findings from the literature.
Table 2: Quantitative Data on DUB Prognostic Value
| DUB | Cancer Type | Measurement / Finding | Clinical Correlation |
|---|---|---|---|
| USP22 | HCC | Expression frequency extremely high in HCC vs. normal liver [84] | Elevated levels represent poor patient survival; greater mortality in advanced stages [84] |
| USP32 | Breast Cancer | Present in 22% of primary breast cancer tumors [84] | Implicated in oncogenesis [84] |
| USP14 | Breast Cancer | Elevated in breast cancer tissues [26] | Inverse relevance to long-term survival [26] |
| USP10 | Gastric Cancer | Low-level expression in clinical samples and cell lines [84] | Negative expression associated with invasion, metastasis, and poor survival [84] |
| CYLD | HCC | Downregulated in tumor tissues and HCC cell lines [24] | Deletion increases biliary injury, liver fibrosis, and tumor susceptibility in models [24] |
Methodologies for Evaluating DUBs as Biomarkers
Establishing DUBs as reliable prognostic biomarkers requires a suite of standardized experimental protocols to assess their expression, functional roles, and interaction with substrates.
Expression Analysis
- Immunohistochemistry (IHC): A primary method for detecting and localizing DUB expression in formalin-fixed, paraffin-embedded (FFPE) tissue sections from patient cohorts. staining intensity and percentage of positive cells are scored and correlated with clinicopathological data (e.g., tumor stage, grade) and patient survival outcomes [84]. This technique was pivotal in associating high USP8 expression with tumor stage in CSCC [84].
- Quantitative Real-Time PCR (qRT-PCR): Used to quantify mRNA expression levels of DUBs in fresh-frozen or FFPE tissue samples. Studies frequently report upregulation of DUB mRNAs, such as USP7 in HCC, compared to matched non-cancerous tissues [84].
- Western Blotting: Employed to confirm the elevated protein expression of DUBs, such as USP7 in HCC, in cancer tissues versus normal controls, providing complementary data to mRNA analysis [84].
Functional Validation
- Gene Knockdown (siRNA/shRNA): Loss-of-function experiments are crucial for validating the oncogenic or tumor-suppressive roles of DUBs. For instance, knockdown of USP5 suppresses cell proliferation, migration, and drug resistance while inducing apoptosis [84]. Similarly, siRNA targeting USP7 increased ubiquitination of its substrate Ki-67 and led to delayed tumor growth in NSCLC models [84].
- Overexpression Studies: Ectopic expression of a DUB in cancer cell lines is used to investigate its tumor-promoting capabilities. Overexpression of USP5 has been shown to promote colony formation, migration, drug resistance, and tumorigenesis [84].
- In Vivo Models: Xenograft mouse models, where cancer cells with modulated DUB expression (knockdown or overexpression) are implanted into immunodeficient mice, are used to assess tumor growth and metastasis. Furthermore, genetically engineered mouse models (GEMMs), such as the liver-specific CYLD knockout mouse, demonstrate the impact of DUB loss on tumor development and susceptibility in vivo [24].
Mechanism Investigation
- Co-Immunoprecipitation (Co-IP) and Mass Spectrometry: Co-IP is used to identify protein-protein interactions and direct substrates of DUBs. When coupled with mass spectrometry, it allows for the unbiased discovery of novel DUB-binding partners and substrates [26].
- Ubiquitination Assays: In vivo and in vitro deubiquitination assays are essential for confirming a DUB's enzymatic activity toward a specific substrate. These assays can demonstrate whether a DUB removes ubiquitin chains from a protein, thereby stabilizing it, as seen with USP22 stabilizing c-Myc in breast cancer [26].
Signaling Pathways and DUB Interactions
DUBs exert their prognostic and biological effects by integrating into and regulating key oncogenic and tumor-suppressive signaling pathways. The diagram below illustrates the interplay between specific DUBs and critical cancer-related pathways.
Diagram Title: DUB Regulation of Key Cancer Pathways
This diagram visualizes how specific DUBs, identified as prognostic markers, interact with and stabilize components of critical signaling pathways in cancer, leading to enhanced tumor progression, survival, and proliferation.
The Scientist's Toolkit: Research Reagent Solutions
Research into DUBs as biomarkers and therapeutic targets relies on a specific toolkit of reagents and methodologies. The table below details essential materials and their applications in this field.
Table 3: Key Research Reagents for DUB Investigation
| Reagent / Tool | Function & Application | Specific Examples in Context |
|---|---|---|
| siRNA / shRNA | Loss-of-function studies to validate DUB role in oncogenesis. | USP5 knockdown suppressed proliferation & induced apoptosis [84]. |
| Activity-Based Probes | Chemical tools to monitor activity and specificity of DUBs in cell lysates. | Critical for profiling DUB activity in different cancer states [7]. |
| Small-Molecule Inhibitors | Pharmacological inhibition to assess therapeutic potential. | USP7 inhibitor P22077; USP14 inhibitor IU1 (preclinical) [104] [7]. |
| qPCR Assays | Quantify DUB mRNA expression in patient tissues. | Detect USP7 mRNA upregulation in HCC vs. normal liver [84]. |
| IHC Antibodies | Detect and localize DUB protein in patient tissue sections. | Correlate USP8 protein levels with CSCC tumor stage [84]. |
| Co-IP Reagents | Identify DUB-protein interactions and substrates. | Identify USP15 interaction with icd-IL1R2 in breast cancer [26]. |
| Xenograft Models | In vivo validation of DUB impact on tumor growth. | Study tumor growth delay after USP7 siRNA knockdown [84]. |
The burgeoning body of evidence unequivocally establishes deubiquitinating enzymes as potent prognostic markers and biomarkers across a wide spectrum of cancers. Their aberrant expression—whether upregulation like USP22 in HCC or downregulation like CYLD in the same cancer type—is intricately linked to critical oncogenic processes including proliferation, metastasis, and apoptosis evasion, ultimately impacting patient survival outcomes. The standardization of methodologies for their evaluation, from IHC and qRT-PCR to functional validation via gene knockdown and overexpression, provides a robust framework for their clinical assessment. As research progresses, the development of selective small-molecule inhibitors against specific DUBs not only holds promise for novel cancer therapeutics but also offers tools to further refine our understanding of their biomarker potential. Integrating DUB expression profiles into existing diagnostic and prognostic algorithms could significantly enhance cancer stratification, enable more personalized treatment approaches, and improve patient management. Future efforts should focus on validating these biomarkers in larger, prospective clinical cohorts and elucidating their complex interactions within the cellular network to fully unlock their clinical utility.
Deubiquitinating enzymes (DUBs) represent a family of approximately 100 proteases that catalyze the removal of ubiquitin chains from target proteins, thereby reversing ubiquitination-mediated signaling, localization, and degradation processes [105] [106]. The delicate balance between ubiquitination and deubiquitination is crucial for maintaining cellular homeostasis, and its disruption contributes significantly to carcinogenesis across gastrointestinal malignancies [106] [18]. While DUB dysregulation is a common theme in cancer, specific DUB family members exhibit distinct, often cancer-type-specific functions that drive tumor progression through unique mechanisms. This technical analysis provides a comprehensive comparison of DUB functions across three lethal gastrointestinal cancers: pancreatic ductal adenocarcinoma (PDAC), hepatocellular carcinoma (HCC), and gastric cancer (GC). Understanding these differential roles is essential for developing targeted therapeutic strategies that account for tissue-specific molecular contexts.
Comparative Analysis of Key DUBs Across Gastrointestinal Cancers
Table 1: Differential Functions of Key DUBs in PDAC, HCC, and Gastric Cancer
| DUB | Cancer Type | Expression Pattern | Key Substrates | Functional Consequences | Therapeutic Implications |
|---|---|---|---|---|---|
| USP28 | PDAC | Upregulated [107] | FOXM1 [107] | Stabilizes FOXM1 → activates Wnt/β-catenin → promotes proliferation, cell cycle progression, inhibits apoptosis [107] | Potential diagnostic and therapeutic target; associated with shorter survival [107] |
| USP1 | HCC | Upregulated [106] | TAZ, CDK5 [106] | Stabilizes TAZ (Hippo pathway), enhances mitochondrial fission via CDK5-Drp1 axis → metabolic reprogramming [106] | USP1 inhibitor ML-323 inhibits HCC growth, induces G1 arrest and apoptosis [106] |
| USP2 | HCC | Isoform-specific: USP2a upregulated, USP2b downregulated [106] | RAB1A [106] | USP2a stabilizes RAB1A → promotes HCC progression; involved in lipid metabolism in NASH-related HCC [106] | USP2a expression positively correlates with poor prognosis [106] |
| PSMD14 | Gastric Cancer | Upregulated [45] | PTBP1 [45] | Stabilizes PTBP1 → promotes proliferation, migration, invasion, EMT (↓E-cadherin, ↑β-catenin, MMP2/9) [45] | Promotes GC development in vitro and in vivo; potential prognostic biomarker [45] |
| USP9X | PDAC | Context-dependent: promoter mutations common [18] | LATS kinase, YAP/TAZ (Hippo pathway) [18] | Dual roles: can act as tumor suppressor (via Hippo pathway) or promoter depending on context [18] | High prognostic value and therapeutic potential; complex context-dependent targeting [18] |
| OTUB1 | HCC | Upregulated [108] | Multiple (Lys48-linked chains) [108] | Promotes proliferation, migration, invasion; regulated by lncRNA GAS6-AS2 in HCC [108] | High expression associated with poor prognosis; shRNA inhibition suppresses malignant phenotype [108] |
Table 2: DUB Family Distribution and Characteristic Functions Across Cancers
| DUB Family | Representative Members | PDAC Role Examples | HCC Role Examples | Gastric Cancer Role Examples |
|---|---|---|---|---|
| USP | USP28, USP1, USP2, USP9X, USP21, USP22, USP34 | Proliferation (USP28, USP21), stemness (USP21), survival (USP34) [18] [107] | Cell cycle regulation (USP1), metabolic reprogramming (USP1), progression (USP2) [106] | General upregulation across multiple USPs; affects tumor size, classification, staging [109] |
| OTU | OTUB1, OTUD1, OTUD3 | Limited data in PDAC | Proliferation, migration, invasion (OTUB1) [108] | Members of OTU family affect 5-year survival rate [109] |
| JAMM/MPN | PSMD14, PSMD7 | PSMD7 stabilizes SOX2 → activates Notch1 pathway [110] | PSMD14 promotes metastasis via deubiquitinating TGF-β receptors [45] | PSMD14 promotes development via PTBP1 stabilization [45] |
| UCH | BAP1, UCHL1 | BAP1 mutations in "BAP1 cancer syndrome" [18] | Information limited in search results | UCH family members affect 5-year survival rate [109] |
| MJD | Ataxin-3, JOSD1 | Information limited in search results | Information limited in search results | MJD family members affect 5-year survival rate [109] |
Cancer-Specific DUB Functions and Mechanisms
Pancreatic Ductal Adenocarcinoma (PDAC)
PDAC demonstrates particular dependence on specific DUBs that drive its aggressive phenotype. USP28 emerges as a critical promoter of PDAC progression through its stabilization of FOXM1, which in turn activates the Wnt/β-catenin pathway [107]. This axis facilitates cell cycle progression and inhibits apoptosis, addressing core PDAC vulnerabilities. The USP9X gene illustrates the context-dependent complexity of DUB functions, exhibiting both tumor-promoting and suppressive activities in PDAC [18]. This duality may reflect the high mutational burden and heterogeneity characteristic of PDAC. Additionally, PSMD7 contributes to PDAC pathogenesis through stabilization of SOX2, leading to activation of the Notch1 signaling pathway [110]. The convergence of multiple DUBs on stemness pathways (SOX2, Notch1) underscores their importance in maintaining the progenitor-like properties that confer therapeutic resistance in PDAC.
Hepatocellular Carcinoma (HCC)
HCC exhibits distinct DUB regulation patterns, particularly within the USP family. USP1 drives HCC progression through parallel pathways—both by stabilizing TAZ in the Hippo pathway and promoting metabolic reprogramming through CDK5-mediated mitochondrial fission [106]. This dual functionality positions USP1 as a central coordinator of HCC pathogenesis. The USP2 gene demonstrates isoform-specific regulation in HCC, with USP2a acting as an oncogene through RAB1A stabilization while USP2b appears to have opposing functions [106]. This isoform-level complexity highlights the precision required for therapeutic targeting. Furthermore, OTUB1, a member of the OTU family, is significantly upregulated in HCC and promotes malignant phenotypes through interactions with long non-coding RNAs [108], illustrating the integration of DUBs with non-coding RNA networks in HCC.
Gastric Cancer
Gastric carcinogenesis is characterized by prominent involvement of JAMM/MPN family DUBs, particularly PSMD14, which is significantly upregulated in GC tissues and drives disease progression through stabilization of PTBP1 [45]. This stabilization activates oncogenic pathways including β-catenin, MMP2, MMP9, and uPA while suppressing E-cadherin, collectively promoting epithelial-mesenchymal transition and metastasis [45]. The broader DUB landscape in gastric cancer shows consistent upregulation across multiple DUB families (UCHs, USPs, OTUs, MJDs, JAMMs, MCPIPs) that collectively influence tumor size, classification, staging, and ultimately patient survival rates [109].
Key Signaling Pathways Visualized
Figure 1: Comparative DUB-Regulated Signaling Pathways in Gastrointestinal Cancers. Key DUBs in each cancer type stabilize specific substrates that activate distinct oncogenic pathways, resulting in cancer-type-specific phenotypic outcomes.
Experimental Methodologies for DUB Functional Characterization
Gain/Loss-of-Function Studies
Comprehensive DUB characterization requires well-designed gain/loss-of-function approaches. Stable gene knockdown is typically achieved using lentiviral delivery of short hairpin RNAs (shRNAs) with sequences specifically targeting DUB genes of interest [110]. Controls include non-targeting scrambled shRNA sequences. For overexpression studies, eukaryotic expression vectors encoding the target DUB are transfected into relevant cancer cell lines using Lipofectamine 3000 reagent [107] [110]. Selection of stable transfectants is performed using antibiotics such as G418, with validation of knockdown/overexpression efficiency achieved through quantitative RT-PCR and Western blot analysis [107].
Mechanistic Interaction Studies
Elucidating DUB-substrate relationships requires multiple complementary approaches. Co-immunoprecipitation (Co-IP) assays demonstrate physical interactions between DUBs and their substrate proteins [45]. Cells are lysed using NP-40 lysis buffer, and protein complexes are immunoprecipitated using antibodies specific to the DUB or substrate coupled to protein A/G agarose beads [110]. For deubiquitination assays, cells are co-transfected with DUB constructs and ubiquitin plasmids, followed by immunoprecipitation of the substrate and Western blot detection using ubiquitin-specific antibodies to visualize ubiquitination status [107] [45]. Protein half-life studies utilize cycloheximide chase assays to quantify substrate stabilization by measuring protein persistence over time when new protein synthesis is inhibited [107].
Phenotypic Characterization Assays
Functional consequences of DUB manipulation are assessed through standardized phenotypic assays. In vitro proliferation is quantified using Cell Counting Kit-8 (CCK-8) assays, where viable cells metabolize WST-8 to formazan dyes measurable at 450nm absorbance [107] [110]. Colony formation capacity evaluates long-term proliferative potential by staining fixed colonies with crystal violet after 2-3 weeks of culture [107]. Apoptosis is measured by flow cytometry using Annexin V-FITC/PI double staining to distinguish early and late apoptotic populations [107]. Cell cycle analysis employs propidium iodide staining followed by flow cytometry to determine phase distribution [107]. Migration and invasion capacities are assessed using Transwell assays with or without Matrigel coating, with quantified crystal violet staining of traversed cells [45].
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Research Reagents for DUB Functional Characterization
| Reagent Category | Specific Examples | Application | Technical Notes |
|---|---|---|---|
| Expression Vectors | USP28 eukaryotic expression vector [107], PSMD7 overexpression plasmid [110] | Gain-of-function studies | Typically include selection markers (e.g., G418 resistance) for stable line generation |
| Knockdown Systems | shRNA plasmids targeting USP28 [107], lentiviral shPSMD7 [110] | Loss-of-function studies | Scrambled shRNA controls essential; multiple target sequences recommended |
| Cell Line Models | PANC-1, AsPC-1 (PDAC) [107] [110]; HGC-27, MKN-45 (GC) [45]; various HCC lines [106] | In vitro studies | Authentication via STR profiling critical [110] |
| Inhibitors/Agonists | ML-323 (USP1 inhibitor) [106] | Pharmacological modulation | Limited availability for many DUBs; tool compounds emerging |
| Antibodies | Anti-USP28 [107], anti-PSMD7 [110], anti-FOXM1 [107], anti-PTBP1 [45] | Detection, IP, IHC | Validation for specific applications required |
| In Vivo Models | Mouse xenografts [107] [45], orthotopic models [18] | Preclinical validation | Monitoring via bioluminescence imaging [107] |
Figure 2: Comprehensive Workflow for DUB Functional Characterization in Cancer Research. This integrated experimental approach enables systematic investigation of DUB functions from initial identification through preclinical validation.
The comparative analysis of DUB functions across PDAC, HCC, and gastric cancer reveals both shared themes and distinct cancer-type-specific mechanisms. While DUB upregulation appears to be a common oncogenic strategy across gastrointestinal malignancies, each cancer type exhibits preference for specific DUB families and substrates that align with their unique pathogenic drivers. PDAC demonstrates particular dependence on USP family members that converge on stemness and proliferation pathways (Wnt/β-catenin, Notch1). HCC utilizes DUBs for metabolic reprogramming and Hippo pathway dysregulation. Gastric cancer prominently features JAMM/MPN family DUBs that drive EMT and metastasis.
Therapeutically, this comparative analysis suggests that both pan-DUB and cancer-type-specific targeting strategies may be viable. While common mechanisms like proteasome interaction (PSMD7, PSMD14) may allow for broader inhibitors, the distinct substrate specificities and functional roles suggest that precision approaches targeting individual DUBs in specific cancer contexts will be necessary. The development of DUB-targeted therapies remains challenging due to structural similarities across family members and the context-dependent functions exemplified by USP9X, but the expanding characterization of cancer-specific DUB functions provides a roadmap for rational therapeutic design. Future research should focus on elucidating the structural basis for substrate specificity, developing isoform-selective inhibitors, and exploring combination therapies that leverage DUB inhibition to enhance conventional and targeted cancer treatments.
Deubiquitinating enzymes (DUBs) have emerged as pivotal regulators in oncogenesis, controlling the stability and function of key proteins involved in cell proliferation, apoptosis, and immune evasion. As the understanding of DUB functions in cancer signaling pathways deepens, targeting these enzymes represents a promising therapeutic strategy. This whitepaper provides a comprehensive analysis of the current landscape of DUB-targeting in oncology, with a specific focus on drug repurposing opportunities. We evaluate the molecular mechanisms of DUB inhibition, detail experimental methodologies for validating DUB-targeting compounds, and visualize critical signaling pathways. While no DUB inhibitors have yet received FDA approval specifically for cancer indications, several investigational compounds show significant promise, and drug repurposing offers a accelerated path toward clinical application. This resource aims to equip researchers and drug development professionals with the technical frameworks and experimental tools necessary to advance this emerging drug class.
Deubiquitinating enzymes (DUBs) constitute a family of approximately 100 proteases that catalyze the removal of ubiquitin chains from target proteins, thereby reversing ubiquitination and regulating protein stability, localization, and activity [4]. DUBs are classified into six major families based on their catalytic domains: ubiquitin-specific proteases (USPs), ovarian tumor proteases (OTUs), ubiquitin carboxy-terminal hydrolases (UCHs), Machado-Josephin domain-containing proteases (MJDs), motif-interacting with ubiquitin-containing novel DUB family (MINDYs), and JAB1/MPN/MOV34 family metalloproteases (JAMMs) [4] [30]. As critical components of the ubiquitin-proteasome system, DUBs maintain protein homeostasis by counterbalancing the activity of E3 ubiquitin ligases.
In cancer biology, DUBs have been recognized as key modulators of tumorigenesis through their regulation of oncoproteins and tumor suppressors. Dysregulation of specific DUBs has been documented across multiple cancer types, where they influence critical cellular processes including cell cycle progression, apoptosis, DNA damage repair, metabolic reprogramming, and immune evasion [4] [12]. For instance, USP28 promotes cell cycle progression in pancreatic ductal adenocarcinoma (PDAC) by stabilizing the transcription factor FOXM1, thereby activating the Wnt/β-catenin pathway [4]. Similarly, Ataxin-3 (ATXN3), a member of the MJD family, exhibits context-dependent roles in cancer, stabilizing oncogenic proteins such as YAP1 in the Hippo pathway and modulating PD-L1 expression to facilitate immune evasion [12].
The therapeutic targeting of DUBs represents an innovative approach in precision oncology. By inhibiting specific DUBs that are overexpressed or hyperactive in cancers, it may be possible to restore the degradation of oncoproteins or stabilize tumor suppressors. However, the development of selective DUB inhibitors faces challenges, including the structural similarity of catalytic sites across DUB families and the context-dependent functions of individual DUBs, which can exhibit both oncogenic and tumor-suppressive roles in different cellular environments [12].
DUB Families as Therapeutic Targets in Human Cancers
Table 1: Major DUB Families and Their Documented Roles in Human Cancers
| DUB Family | Representative Members | Cancer Types Involved | Oncogenic/Tumor Suppressive Functions |
|---|---|---|---|
| USP | USP28, USP21, USP34, USP5, USP9X, USP22, USP33 | Pancreatic ductal adenocarcinoma, Breast cancer, Lung cancer, Renal carcinoma | Promotes proliferation, stemness, metabolic reprogramming, and chemoresistance; context-dependent roles (e.g., USP9X) |
| OTU | OTUD1 | Breast cancer | Suppresses metastasis via enzymatic activity |
| MJD | ATXN3, MJD | Gastric cancer, Breast cancer, Lung cancer, Renal cancer, Oral squamous cell carcinoma | Regulates PI3K/Akt, Hippo/YAP, and TGF-β pathways; promotes immune evasion via PD-L1 stabilization |
| UCH | BAP1 | Mesothelioma, Melanoma, Breast cancer, Renal carcinoma | "BAP1 cancer syndrome" from frequent mutations; primarily tumor-suppressive |
| JAMM/MPN | - | - | Metalloprotease activity; limited cancer association in reviewed literature |
| MINDY | - | - | Family less characterized in cancer contexts |
The ubiquitin-specific protease (USP) family represents the largest and most extensively studied group of DUBs in cancer. In pancreatic ductal adenocarcinoma (PDAC), multiple USPs including USP28, USP21, and USP34 drive tumor progression through distinct mechanisms. USP28 stabilizes FOXM1 to activate Wnt/β-catenin signaling and promote cell cycle progression [4]. USP21 maintains stemness in PDAC cells by stabilizing TCF7 and activates mTOR signaling to support metabolic adaptation [4]. USP9X demonstrates the context-dependent nature of DUB functions, acting as a tumor promoter in human pancreatic tumor cells while serving a suppressive role in KPC mouse models, where it regulates the Hippo pathway through LATS kinase and YAP/TAZ [4].
The Machado-Joseph disease (MJD) protease family, particularly Ataxin-3 (ATXN3), has gained attention for its multifaceted roles in cancer pathogenesis. ATXN3 is overexpressed in gastric, breast, lung, renal, and oral squamous cell carcinomas, where it often correlates with aggressive tumor phenotypes and poor prognosis [12]. Mechanistically, ATXN3 regulates critical signaling cascades including PI3K/Akt and Hippo/YAP pathways, contributing to proliferation, metastasis, resistance to apoptosis, and immune evasion. Recent discoveries highlight ATXN3's role in modulating PD-L1 expression, positioning it as a regulator of immune checkpoint dynamics [12].
Beyond these families, ovarian tumor proteases (OTUs) and ubiquitin carboxyl-terminal hydrolases (UCHs) also contribute to cancer progression. For example, BAP1, a UCH family member, is frequently mutated in mesothelioma, melanoma, and renal carcinoma, with these mutations defining a "BAP1 cancer syndrome" [4]. OTUD1 deficiency promotes breast cancer metastasis through its enzymatic activity, underscoring the tumor-suppressive potential of certain DUBs [4].
Experimentally Validated DUB-Targeting Compounds
Table 2: Experimentally Validated DUB-Targeting Compounds and Their Mechanisms
| Compound Name | Targeted DUB(s) | Developmental Stage | Proposed Mechanism of Action | Evidence Level |
|---|---|---|---|---|
| HBX41108, P22077 | USP7 | Preclinical | Inhibits USP7 deubiquitinase activity | In vitro and cell-based studies |
| b-AP15, VLX1570 | USP14, UCHL5 | Preclinical/Clinical (VLX1570 for multiple myeloma) | Dual inhibitor of proteasome-associated DUBs | In vivo models; clinical trials |
| WP1130 | USP9X, USP5, USP14 | Preclinical | Partially selective DUB inhibitor | In vitro and cell-based studies |
| Albendazole | Not a direct DUB inhibitor (targets RNF20 ubiquitin ligase) | FDA-approved (repurposing) | Modulates ubiquitination via RNF20 inhibition, promoting apoptosis | In vitro, in vivo (CRC models), patient-derived organoids |
| SIM0501 | USP1 | FDA clinical approval for trials | Targets USP1 for advanced solid tumors | Planned clinical trials |
While no highly specific DUB inhibitors have yet gained FDA approval for cancer therapy, several investigational compounds have provided proof-of-concept for DUB targeting in preclinical models. USP7 inhibitors including HBX41108 and P22077 demonstrate the feasibility of targeting USP family members, though selectivity remains a challenge [12]. The dual USP14/UCHL5 inhibitors b-AP15 and VLX1570 represent another class of DUB-targeting agents, with VLX1570 having advanced to clinical evaluation for multiple myeloma [12]. WP1130 exhibits a broader DUB inhibition profile, affecting USP9X, USP5, and USP14, highlighting the potential for multi-DUB targeting strategies [12].
Drug repurposing represents a promising avenue for identifying DUB-modulatory activities. Albendazole, an FDA-approved anti-helminth drug, has demonstrated potent anti-cancer effects in colon cancer models, though its primary mechanism involves targeting the ubiquitin ligase RNF20 rather than direct DUB inhibition [111]. This example illustrates how existing drugs with well-characterized safety profiles may be repositioned to target the ubiquitin system, offering accelerated paths to clinical application.
The development of selective DUB inhibitors faces significant challenges due to structural conservation of catalytic sites across DUB families and the complex, context-dependent biology of individual DUBs. Emerging strategies to enhance selectivity include targeting allosteric sites rather than catalytic domains, developing proteolysis-targeting chimeras (PROTACs) for specific DUB degradation, and employing molecular glues to modulate DUB-substrate interactions [92].
Experimental Protocols for Validating DUB Inhibitors
High-Throughput Screening for DUB-Modulatory Compounds
High-throughput screening (HTS) provides a systematic approach for identifying compounds with DUB-inhibitory activity from large chemical libraries. The following protocol outlines key steps for HTS implementation:
Library Selection: Utilize annotated libraries of FDA-approved drugs or diverse chemical compounds. For repurposing studies, focused libraries of clinically approved agents offer advantages in safety profiling and potential accelerated clinical translation [111].
Assay Development: Implement biochemical assays using recombinant DUB enzymes and ubiquitin-based substrates. Fluorescence-based (e.g., Ub-AMC) or luminescence-based readouts enable quantitative measurement of DUB activity. For cellular context, implement reporter systems sensitive to DUB inhibition.
Primary Screening: Conduct single-concentration screening against target DUBs. Include appropriate controls (e.g., reference inhibitors, vehicle controls) to establish assay robustness and calculate Z-factor values for quality assessment.
Hit Confirmation: Subject initial hits to dose-response analysis to determine potency (IC50 values). Counter-screen against related DUBs to assess selectivity within the DUB family.
Secondary Assays: Validate hits in cellular models using techniques such as:
- Immunoblotting: Monitor accumulation of ubiquitinated substrates of the target DUB.
- Cellular Thermal Shift Assay (CETSA): Confirm target engagement within cells.
- Proliferation/Viability Assays: Assess functional consequences of DUB inhibition.
This HTS framework successfully identified albendazole as a potent anti-colon cancer agent through its effects on the ubiquitin system, though notably through RNF20 ligase targeting rather than direct DUB inhibition [111].
Mechanistic Validation of DUB Inhibitors
Following initial identification, comprehensive mechanistic studies are essential to confirm target engagement and elucidate the functional consequences of DUB inhibition:
Target Engagement Assessment:
- Cellular Thermal Shift Assay (CETSA): Treat cells with candidate compounds, heat-shock cells at varying temperatures, and quantify remaining soluble target DUB by immunoblotting. Shift in thermal stability indicates direct binding.
- Drug Affinity Responsive Target Stability (DARTS): Incubate cell lysates with compounds, then subject to partial proteolysis. Reduced proteolytic degradation suggests compound binding and stabilization.
Functional Consequences Evaluation:
- Ubiquitinomics: Implement TUBE (Tandem Ubiquitin Binding Entity) pulldown coupled with mass spectrometry to comprehensively profile changes in the ubiquitinome following DUB inhibition.
- Pathway-Specific Analysis: Monitor stabilization or destabilization of known DUB substrates by immunoblotting (e.g., FOXM1 for USP28, YAP for ATXN3) [4] [12].
- Phenotypic Assays: Evaluate functional outcomes including:
- Cell Proliferation: MTT, PrestoBlue, or colony formation assays.
- Apoptosis: Annexin V staining and caspase activation assays.
- Cell Cycle Analysis: Flow cytometry with PI staining.
- Migration/Invasion: Transwell or wound healing assays.
In Vivo Validation:
- Utilize xenograft models, patient-derived xenografts (PDX), or genetically engineered mouse models (GEMM) relevant to the cancer type.
- Monitor tumor growth, metastasis, and perform immunohistochemical analysis of proliferation markers (Ki-67), apoptosis (cleaved caspase-3), and substrate stabilization.
This multi-tiered validation approach ensures comprehensive characterization of DUB inhibitors before advancing to clinical development.
Research Reagent Solutions for DUB Studies
Table 3: Essential Research Reagents for DUB-Targeting Studies
| Reagent Category | Specific Examples | Research Applications | Technical Notes |
|---|---|---|---|
| Recombinant DUB Enzymes | USP7, USP14, ATXN3, UCHL5 | Biochemical DUB activity assays, high-throughput screening | Available from commercial vendors; verify catalytic activity before use |
| Activity Probes | Ub-AMC, HA-Ub-VS, Cy5-labeled ubiquitin derivatives | Enzymatic activity measurements, inhibitor screening | Fluorescent and gel-based formats available; enable real-time kinetic measurements |
| Cell Line Models | PANC-1 (pancreatic), MCF-7 (breast), Patient-derived organoids (PDOs) | Cellular validation of DUB inhibitors, mechanistic studies | PDOs maintain tumor heterogeneity and drug response profiles |
| DUB-Specific Antibodies | Anti-USP28, Anti-USP21, Anti-ATXN3, Anti-BAP1 | Immunoblotting, immunohistochemistry, immunofluorescence | Validate specificity for intended applications; phospho-specific antibodies for regulation studies |
| Ubiquitin-Related Reagents | TUBE (Tandem Ubiquitin Binding Entities), K-ε-GG antibody | Ubiquitin pull-down assays, ubiquitinomics | TUBE reagents enrich polyubiquitinated proteins with minimal distortion |
| Animal Models | Xenograft models, Genetically engineered mouse models (GEMM), KPC (Kras/p53-driven) PDAC model | In vivo efficacy studies, toxicity assessment, biomarker identification | KPC model recapitulates human PDAC progression and therapeutic responses |
The research reagents outlined in Table 3 represent essential tools for investigating DUB biology and validating DUB-targeting compounds. Recombinant DUB enzymes and activity probes form the foundation for biochemical assays and high-throughput screening initiatives [111]. Cell line models, particularly patient-derived organoids (PDOs), offer physiologically relevant systems for evaluating compound efficacy and resistance mechanisms while maintaining tumor heterogeneity [111]. For in vivo studies, genetically engineered mouse models such as the KPC (Kras/p53-driven) PDAC model provide robust platforms for assessing therapeutic efficacy in immune-competent settings that recapitulate human disease progression [4].
Specialized reagents for ubiquitin research, including TUBE (Tandem Ubiquitin Binding Entities) and K-ε-GG antibodies, enable comprehensive analysis of the ubiquitinome and facilitate identification of DUB substrates under various treatment conditions. These tools are particularly valuable for elucidating the mechanisms of action of DUB-targeting compounds and understanding their effects on global protein stability networks.
DUB Signaling Pathways in Cancer: Mechanistic Insights
The intricate involvement of DUBs in oncogenic signaling pathways underscores their therapeutic relevance. The diagram below illustrates how specific DUBs regulate key cancer-associated signaling cascades:
Figure 1: DUB-Mediated Regulation of Oncogenic Signaling Pathways. This diagram illustrates how specific deubiquitinating enzymes (DUBs), highlighted in yellow, regulate key cancer-associated signaling pathways by stabilizing critical oncoproteins. USP28 stabilizes FOXM1 to activate Wnt/β-catenin signaling and promote proliferation [4]. ATXN3 stabilizes YAP1 in the Hippo pathway and PD-L1 in immune checkpoint regulation, contributing to tumor growth and immune evasion respectively [12]. ATXN3 also modulates the PI3K/Akt pathway, enhancing cell survival signals.
The visualization demonstrates how DUBs function as critical nodes in cancer signaling networks, with particular DUBs often regulating multiple pathways simultaneously. For example, ATXN3 modulates both the Hippo/YAP pathway through YAP1 stabilization and immune evasion through PD-L1 regulation, highlighting the potential for multi-faceted therapeutic effects from targeting a single DUB [12]. Similarly, USP family members including USP21, USP34, and USP5 converge on proliferation and survival pathways across different cancer types, suggesting both opportunities and challenges for achieving tumor-specific therapeutic effects.
The targeted inhibition of deubiquitinating enzymes represents a promising frontier in precision oncology, with potential to address unmet needs in treatment-resistant and metastatic cancers. While no DUB inhibitors have yet achieved FDA approval for cancer therapy, the compelling preclinical evidence summarized in this whitepaper supports continued investment in this drug class. The documented roles of DUBs in regulating key oncogenic pathways, coupled with their frequent dysregulation across cancer types, position them as attractive therapeutic targets.
Future directions in DUB-targeted therapy development should focus on several key areas: First, enhancing the selectivity of DUB inhibitors through structure-based drug design and allosteric targeting approaches will be critical for minimizing off-target effects. Second, understanding context-specific DUB functions will enable better patient stratification and identification of predictive biomarkers. Third, combination strategies pairing DUB inhibitors with established modalities such as immunotherapy, chemotherapy, or targeted agents may yield synergistic effects and overcome resistance mechanisms.
Drug repurposing represents a particularly promising avenue for accelerating the clinical translation of DUB-targeted therapies. As demonstrated by the anti-cancer effects of albendazole through modulation of the ubiquitin system, existing FDA-approved drugs may offer unexpected opportunities for targeting DUB-related pathways [111]. Systematic screening approaches combining multi-omics technologies with artificial intelligence are now enabling more efficient identification of such repurposing opportunities [112].
As the field advances, the integration of mechanistic insights regarding DUB functions in specific cancer contexts with innovative drug discovery approaches will be essential for realizing the full therapeutic potential of DUB modulation. The experimental frameworks and technical resources provided in this whitepaper aim to support researchers in these endeavors, ultimately contributing to the development of effective DUB-targeted therapies for cancer patients.
Conclusion
Deubiquitinating enzymes represent a promising yet complex therapeutic frontier in oncology, with growing evidence establishing their critical roles in virtually all cancer hallmarks. From foundational understanding of DUB biology to emerging clinical applications, this field has rapidly evolved to offer novel targeting strategies beyond conventional proteasome inhibition. The development of selective DUB inhibitors, coupled with advanced technologies like PROTACs, presents unprecedented opportunities for precision cancer therapy. Future directions must address key challenges including therapeutic resistance, tissue-specific toxicities, and biomarker identification for patient stratification. As research continues to unravel the intricate DUB networks governing cancer pathogenesis, targeting these enzymes will likely become an integral component of combinatorial treatment regimens, potentially overcoming limitations of current therapies and improving outcomes for cancer patients.
References
- 1. Ubiquitin proteasome system in immune regulation and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10163937/]
- 2. Ubiquitin/Proteasome System | Cell Metabolism [https://www.tocris.com/cell-biology/ubiquitin-and-proteasome-system]
- 3. Recent advances in small molecule inhibitors of ... [https://www.sciencedirect.com/science/article/abs/pii/S0223523425000893]
- 4. The multifaceted roles of deubiquitinating enzymes (DUBs ... [https://www.nature.com/articles/s41419-025-08052-7]
- 5. The Ubiquitin-Proteasome System: Potential Therapeutic ... [https://www.frontiersin.org/journals/molecular-neuroscience/articles/10.3389/fnmol.2016.00004/full]
- 6. Ubiquitin-Proteasome System [https://lifesensors.com/ubiquitinproteasomesystem/]
- 7. Emerging role of deubiquitinases in modulating cancer ... [https://www.sciencedirect.com/science/article/abs/pii/S1359644625000522]
- 8. Target Class Approach to Develop DUB Inhibitors [https://themarkfoundation.org/portfolio/target-class-approach-to-develop-dub-inhibitors/]
- 9. Deubiquitinating enzyme [https://en.wikipedia.org/wiki/Deubiquitinating_enzyme]
- 10. Deubiquitinating enzymes (DUBs): Regulation, homeostasis ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8424594/]
- 11. Deubiquitinases in cancer - PMC - PubMed Central - NIH [https://pmc.ncbi.nlm.nih.gov/articles/PMC4536986/]
- 12. Deciphering deubiquitinating enzyme Ataxin-3 as an ... [https://www.sciencedirect.com/science/article/abs/pii/S0141813025086702]
- 13. Structural and Functional Basis of JAMM Deubiquitinating ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9313428/]
- 14. Deubiquitinating enzymes: potential regulators of the ... [https://biosignaling.biomedcentral.com/articles/10.1186/s12964-024-01633-7]
- 15. Deubiquitinating Enzymes (DUBs) [https://themarkfoundation.org/blog/deubiquitinating-enzymes-dubs-revolutionizing-the-future-of-cancer-care-with-next-generation-inhibitors-for-targeted-protein-degradation/]
- 16. Functional analysis of deubiquitylating enzymes in ... [https://www.sciencedirect.com/science/article/abs/pii/S0304419X19301179]
- 17. Deubiquitinases (DUBs) and DUB inhibitors: a patent review [https://pmc.ncbi.nlm.nih.gov/articles/PMC4834700/]
- 18. The multifaceted roles of deubiquitinating enzymes (DUBs) ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12533248/]
- 19. Ubiquitination and deubiquitination in cancer [https://molecular-cancer.biomedcentral.com/articles/10.1186/s12943-024-02046-3]
- 20. Deubiquitinating enzymes: Promising targets for drug ... [https://www.sciencedirect.com/science/article/abs/pii/S1359644622002793]
- 21. DUBbing Cancer: Deubiquitylating Enzymes Involved in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4963401/]
- 22. Role of Deubiquitinases in Human Cancers: Potential Targeted Therapy - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC7177317/]
- 23. Role of Deubiquitinases in DNA Damage Response - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC6561784/]
- 24. Deubiquitinases in Cancers: Aspects of Proliferation ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9323628/]
- 25. The emerging role of deubiquitylating enzymes as therapeutic targets in cancer metabolism | Cancer Cell International | Full Text [https://cancerci.biomedcentral.com/articles/10.1186/s12935-022-02524-y]
- 26. Roles and Mechanisms of Deubiquitinases (DUBs) in Breast ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8467271/]
- 27. Role of deubiquitinases in DNA damage response [https://www.sciencedirect.com/science/article/abs/pii/S1568786418303082]
- 28. Emerging roles of deubiquitinases in cancer‐associated ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7165618/]
- 29. The ubiquitin code of RAS proteins: Decoding its role in ... [https://www.sciencedirect.com/science/article/pii/S2589004225012908]
- 30. Frontiers | The role of ubiquitination and deubiquitination ... in cancer [https://www.frontiersin.org/journals/oncology/articles/10.3389/fonc.2025.1464914/full]
- 31. Deubiquitinating Enzyme OTUDs: Focus on Cancers and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12493990/]
- 32. Targeting the Wnt/β-catenin signaling pathway in cancer [https://jhoonline.biomedcentral.com/articles/10.1186/s13045-020-00990-3]
- 33. Regulation of Wnt Signaling through Ubiquitination and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7311976/]
- 34. Ubiquitin specific protease 4 positively regulates the WNT/ ... [https://www.sciencedirect.com/science/article/pii/S1574789115001374]
- 35. DEPDC1B-mediated USP5 deubiquitination of β-catenin ... [https://pubmed.ncbi.nlm.nih.gov/37642235/]
- 36. Redox regulation of DUBs and its therapeutic implications ... [https://www.sciencedirect.com/science/article/pii/S2213231721003542]
- 37. Deubiquitinase dynamics: methodologies for understanding substrate ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12123204/]
- 38. of Deubiquitinase Identification in... | SpringerLink Substrates [https://link.springer.com/protocol/10.1007/978-1-0716-2803-4_14]
- 39. Chemical tools to define and manipulate interferon ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11754618/]
- 40. Pharmacologic interrogation of USP28 cellular function in ... [https://www.sciencedirect.com/science/article/abs/pii/S2451945625002326]
- 41. Sensitive and specific DUB enzyme assay kits - Engineering Update [https://engineering-update.co.uk/2025/04/24/sensitive-and-specific-dub-enzyme-assay-kits/]
- 42. The role of ubiquitination and deubiquitination in cancer ... [https://molecular-cancer.biomedcentral.com/articles/10.1186/s12943-020-01262-x]
- 43. The emerging role of deubiquitylating enzymes as ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8935717/]
- 44. USP25 promotes pathological HIF-1-driven metabolic ... [https://www.nature.com/articles/s41467-022-29684-9]
- 45. Deubiquitinating enzyme PSMD14 facilitates gastric ... [https://www.sciencedirect.com/science/article/abs/pii/S0014482722001410]
- 46. Deubiquitinating enzyme PSMD14 facilitates gastric ... [https://pubmed.ncbi.nlm.nih.gov/35405117/]
- 47. -mediated PSMD activates H3K27... 14 PFKFB 2 deubiquitination [https://pubmed.ncbi.nlm.nih.gov/41193870/]
- 48. Fructose 2,6-Bisphosphate in Cancer Cell Metabolism [https://www.frontiersin.org/journals/oncology/articles/10.3389/fonc.2018.00331/full]
- 49. PSMD14 stabilizes estrogen signaling and facilitates ... [https://www.nature.com/articles/s41388-023-02905-1]
- 50. Deubiquitinase PSMD14 promotes ovarian cancer ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8637564/]
- 51. Deubiquitinases as novel therapeutic targets for diseases - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC11645450/]
- 52. DUB Drug Discovery: A Platform for Creating ... [https://innovations.dana-farber.org/technology/dub-drug-discovery-a-platform-for-creating-dub-focused-small-molecules-to-regulate-protein-homeostasis-in-human-disease/]
- 53. Emerging role of ubiquitination/deubiquitination ... [https://www.sciencedirect.com/science/article/pii/S2352304222000320]
- 54. Post-translational modifications of immune checkpoints [https://ehoonline.biomedcentral.com/articles/10.1186/s40164-025-00627-6]
- 55. Regulatory mechanisms of PD-1/PD-L1 in cancers - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC11102195/]
- 56. Frontiers | USP39 at the crossroads of cancer immunity: regulating ... [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2025.1665775/full]
- 57. Recent advances in the development of deubiquitinases ... [https://www.sciencedirect.com/science/article/abs/pii/S0223523424000412]
- 58. Pipeline DUB : Comprehensive Clinical Trials And... Inhibitors 2025 [https://menafn.com/1109933804/DUB-Inhibitors-Pipeline-2025-Comprehensive-Clinical-Trials-And-Therapies-Analysis-With-Key-MOA-And-ROA-Insights-By-Delveinsight-Mission-Therapeutics-Ubiquigent-Almac-Discovery-KSQ-Therapeutics]
- 59. DUB Inhibitors Pipeline 2025: Comprehensive Clinical ... [https://www.barchart.com/story/news/34180960/dub-inhibitors-pipeline-2025-comprehensive-clinical-trials-and-therapies-analysis-with-key-moa-and-roa-insights-by-delveinsight-mission-therapeutics-ubiquigent-almac-discovery-ksq-therapeutics]
- 60. DUB Platform [https://missiontherapeutics.com/science/dub-platform/]
- 61. Molecular targeting of the deubiquitinase USP14 to circumvent cisplatin... [https://www.oaepublish.com/articles/cdr.2025.88]
- 62. Deubiquitinating enzymes in parkinson’s disease: molecular... [https://molmed.biomedcentral.com/articles/10.1186/s10020-025-01389-x]
- 63. Deubiquitinase-Targeting Chimeras (DUBTACs) as a ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12507175/]
- 64. Recent advances in targeted protein degraders as potential ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9930057/]
- 65. Deubiquitinase-Targeting Chimeras Mediated Stabilization of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12395470/]
- 66. Integrating multi-omics data reveals function and ... [https://elifesciences.org/articles/72879]
- 67. New Molecular Targets, Technologies, and Cancer ... [https://www.aacr.org/blog/2025/11/05/new-molecular-targets-technologies-and-cancer-treatments-take-center-stage-at-the-aacr-nci-eortc-conference/]
- 68. Targeted protein degradation technologies: Emerging ... [https://www.sciopen.com/article/10.26599/NR.2025.94907983]
- 69. Evolving role of deubiquitinating in oral enzymes (Review) cancer [https://www.spandidos-publications.com/10.3892/ol.2025.15100?text=fulltext]
- 70. Deubiquitylating Enzymes in Cancer and Immunity [https://pubmed.ncbi.nlm.nih.gov/37888853/]
- 71. Screening of DUB activity and specificity by MALDI-TOF ... [https://www.nature.com/articles/ncomms5763]
- 72. progress of Research in breast DUB | Clinical and... enzyme cancer [https://link.springer.com/article/10.1007/s10238-025-01878-7]
- 73. High-Throughput Synthesis and Screening of a Cyanimide ... [https://pubmed.ncbi.nlm.nih.gov/41058185/]
- 74. Molecular Mechanisms of DUBs Regulation in Signaling and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7863924/]
- 75. Drug resistance mechanisms and treatment strategies ... [https://molecular-cancer.biomedcentral.com/articles/10.1186/s12943-024-02005-y]
- 76. Deubiquitinating Enzyme-Mediated Signaling Networks in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7694198/]
- 77. Deubiquitylating enzymes as cancer stem cell therapeutics [https://www.sciencedirect.com/science/article/abs/pii/S0304419X17300987]
- 78. Unraveling the role of deubiquitinating enzymes on ... [https://www.sciencedirect.com/science/article/abs/pii/S0304419X25000393]
- 79. Immune Evasion and Drug Resistance Mediated by USP22 ... [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2022.918314/full]
- 80. The role of ubiquitination and deubiquitination in cancer ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7529510/]
- 81. Metabolic adaptation in hypoxia and cancer - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC8158653/]
- 82. The deubiquitination enzyme USP14 promotes ... [https://www.nature.com/articles/s41419-025-08065-2]
- 83. The role of deubiquitinating enzymes in cancer drug ... [https://pubmed.ncbi.nlm.nih.gov/32146496/]
- 84. Deubiquitinating enzymes as cancer biomarkers [https://pmc.ncbi.nlm.nih.gov/articles/PMC6476481/]
- 85. Deubiquitinating enzymes: potential regulators of the tumor ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11075295/]
- 86. Recent advances in small molecule inhibitors of ... [https://pubmed.ncbi.nlm.nih.gov/39908798/]
- 87. Dual screen for efficacy and toxicity identifies HDAC ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7864865/]
- 88. The Emerging Role of Deubiquitinases in Radiosensitivity [https://www.sciencedirect.com/science/article/pii/S0360301623082378]
- 89. Deubiquitinating enzymes as cancer biomarkers [https://www.bmbreports.org/journal/view.html?doi=10.5483/BMBRep.2019.52.3.048]
- 90. Therapeutic inhibition of USP7 promotes antitumor immune ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12481409/]
- 91. New combination treatment strategy dramatically... | ScienceDaily [https://www.sciencedaily.com/releases/2025/02/250227125112.htm]
- 92. Medicinal chemistry perspectives on anticancer drug design based on... [https://pubs.rsc.org/en/content/articlelanding/2025/ra/d5ra05472a]
- 93. Ubiquitin-specific protease 7 promotes the growth and ... [https://www.sciencedirect.com/science/article/pii/S002192582502527X]
- 94. USP1/UAF1 targets polyubiquitinated PCNA with an exo- ... [https://www.nature.com/articles/s41467-025-61768-0]
- 95. Molecular targeting of the deubiquitinase USP14 to ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12539213/]
- 96. Mission Therapeutics – Deubiquitylating enzymes: multiple ... [https://missiontherapeutics.com/]
- 97. DUB Inhibitors Competitive Landscape 2020: Market and ... [https://www.linkedin.com/pulse/dub-inhibitors-competitive-landscape-2020-market-pipeline-gaurav-bora-vfyje]
- 98. Uncovering global research frontiers in deubiquitinating ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11938311/]
- 99. Deubiquitinating enzymes and the proteasome regulate ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9117253/]
- 100. Deubiquitinases in DNA damage repair: Implication and ... [https://pubmed.ncbi.nlm.nih.gov/41197406/]
- 101. How Proteasome Drug Works — In One Simple Flow ( Inhibitor ) 2025 [https://www.linkedin.com/pulse/how-proteasome-inhibitor-drug-works-one-simple-flow-tt6kc]
- 102. Proteasome inhibition induces DNA methylation alteration ... [https://www.nature.com/articles/s41598-025-92390-1]
- 103. -associated thrombotic microangiopathy... Proteasome inhibitor [https://pubmed.ncbi.nlm.nih.gov/39939437/]
- 104. Deubiquitinating Enzymes in Osteoarthritis [https://orthopedicreviews.openmedicalpublishing.org/article/144733-deubiquitinating-enzymes-in-osteoarthritis-from-mechanisms-to-therapeutic]
- 105. The multifaceted roles of deubiquitinating ( enzymes ) in... DUBs [https://pubmed.ncbi.nlm.nih.gov/41102147/]
- 106. Deubiquitylating Enzymes in Hepatocellular Carcinoma - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC12210126/]
- 107. USP28 facilitates pancreatic progression through activation of... cancer [https://www.nature.com/articles/s41419-021-04163-z?error=cookies_not_supported]
- 108. Research Progress of DUB Enzyme in Hepatocellular ... [https://www.frontiersin.org/journals/oncology/articles/10.3389/fonc.2022.920287/full]
- 109. The role of deubiquitinating enzymes in gastric cancer [https://pubmed.ncbi.nlm.nih.gov/31897112/]
- 110. Deubiquitinase PSMD7 facilitates pancreatic progression... cancer [https://cellandbioscience.biomedcentral.com/articles/10.1186/s13578-024-01213-9]
- 111. Albendazole inhibits colon cancer progression and therapy resistance... [https://www.nature.com/articles/s41416-023-02570-x?error=cookies_not_supported&code=c9ef48b4-14f3-49a8-8c56-74fe988b07ca]
- 112. Multi-omics based and AI-driven drug repositioning for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12297790/]