From Biochemical Curiosity to Clinical Breakthrough: The Discovery and Evolution of the Ubiquitin-Proteasome System
This article chronicles the seminal discovery of the ubiquitin-proteasome system (UPS), a fundamental pathway for regulated intracellular protein degradation.
From Biochemical Curiosity to Clinical Breakthrough: The Discovery and Evolution of the Ubiquitin-Proteasome System
Abstract
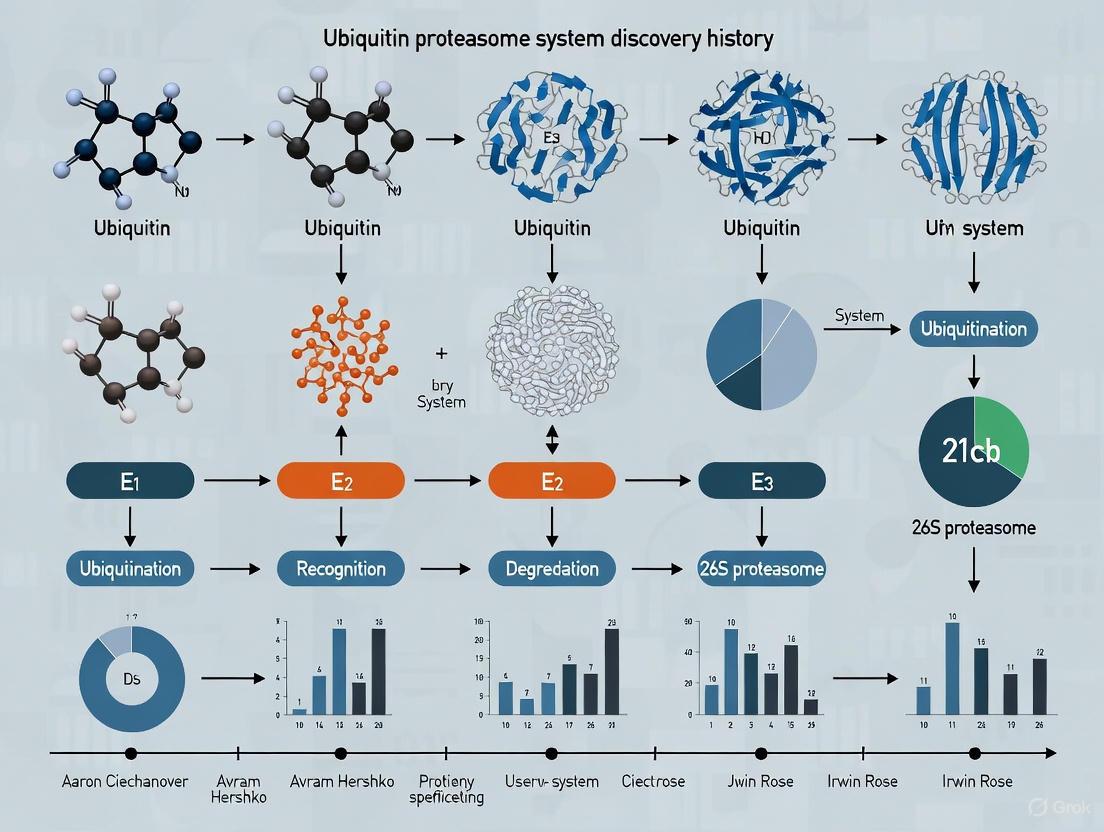
This article chronicles the seminal discovery of the ubiquitin-proteasome system (UPS), a fundamental pathway for regulated intracellular protein degradation. It details the foundational biochemical work in the 1980s by Hershko, Ciechanover, and Rose that identified the E1-E2-E3 enzymatic cascade, followed by the pivotal biological validation of its roles in cell cycle, DNA repair, and stress responses. The review further explores the translation of this basic science into clinical applications, including the development of proteasome inhibitors for multiple myeloma and the revolutionary emergence of targeted protein degradation technologies like PROTACs and molecular glues. Finally, it addresses current challenges and future directions in troubleshooting UPS-targeting therapies and validating their efficacy against a broadening range of diseases, providing a comprehensive resource for researchers and drug development professionals.
The Pioneering Experiments: Unraveling the Ubiquitin-Proteasome Pathway
For much of the scientific history preceding the discovery of the ubiquitin system, intracellular protein degradation was considered a non-specific, largely constitutive process that occurred without energy expenditure. This perception was rooted in the understanding of digestive proteases like trypsin and the function of lysosomes, which degrade extracellular proteins without requiring adenosine triphosphate (ATP) [1]. However, this model failed to explain a critical paradox observed as early as the 1950s: the breakdown of the cell's own proteins clearly required metabolic energy [1]. This energy requirement was chemically perplexing; while dietary proteins provide energy upon degradation, the cell apparently needed to invest energy to break down its own proteins to amino acids. Resolving this paradox became the fundamental challenge that would lead to the discovery of a sophisticated regulatory system rivaling transcription and translation in biological importance [2] [3].
The Experimental System: Reticulocyte Lysate as a Model
Rationale for System Selection
Avram Hershko's decision to employ a reticulocyte lysate system proved instrumental to the discovery. The reticulocyte, an immature red blood cell, presented unique experimental advantages. As it matures into a fully differentiated erythrocyte, the reticulocyte extensively degrades its intracellular machineries and organelles, including lysosomes [4] [5]. This elimination of lysosomal activity created a clean background to identify and characterize non-lysosomal, energy-dependent proteolytic pathways. Researchers hypothesized that the same mechanism responsible for the maturation-related degradation also handled the removal of abnormal proteins in pathological conditions like thalassemia and sickle cell anemia [4].
Key Technical Challenges
The primary technical obstacle was the overwhelming presence of hemoglobin, which constituted approximately 85% of the total cellular protein in reticulocytes [5]. This abundance interfered with biochemical fractionation and analysis. Initial attempts to separate the proteolytic activity from hemoglobin using standard chromatography methods were unsuccessful, as the activity co-eluted with the hemoglobin fraction [5]. This impediment necessitated the development of innovative separation techniques.
The Critical Experiments: Fractionation and Identification
The Seminal Fractionation Experiment
The breakthrough came when Aaron Ciechanover and Michael Fry, while Hershko was on sabbatical, attempted a radical approach: heat treatment of the reticulocyte extract [5]. They boiled the hemoglobin-rich fraction, which resulted in the precipitation of hemoglobin "like mud," leaving a heat-stable, yellowish supernatant that retained full activity [5]. This simple yet decisive experiment demonstrated that the active component was a heat-stable polypeptide, which they designated APF-1 (ATP-dependent Proteolysis Factor 1) [1] [5].
The subsequent reconstitution experiments revealed that the reticulocyte lysate could be separated into two complementary fractions (Table 1):
- Fraction I: Contained the heat-stable APF-1.
- Fraction II: Contained the remaining essential components.
Individually, these fractions were proteolytically inactive. However, when recombined in the presence of ATP, they restored ATP-dependent protein degradation [1]. This critical finding indicated that the system involved multiple cooperating factors.
Table 1: Key Experimental Findings from Reticulocyte Lysate Fractionation
| Experimental Observation | Interpretation | Significance |
|---|---|---|
| ATP required for proteolysis in lysates [1] | Energy-dependent process | Contradicted prevailing models of passive degradation |
| System separable into two fractions (I and II) [1] | Multiple components involved | Suggested a complex, multi-step mechanism |
| APF-1 is heat-stable [5] | APF-1 is a robust, small protein | Enabled its purification and characterization |
| Activity restored upon fraction recombination [1] | Components are complementary | Confirmed a defined biochemical pathway |
The Discovery of Covalent Conjugation
Collaboration with Irwin Rose at the Fox Chase Cancer Center was pivotal for the next conceptual leap. In 1980, Ciechanover, Hershko, and Rose demonstrated that APF-1 was not merely a cofactor but was covalently conjugated to target protein substrates via a stable peptide bond [1] [4]. Furthermore, they observed that multiple molecules of APF-1 could be attached to a single target protein, a phenomenon they termed polyubiquitination [1]. This conjugation was identified as the energy-requiring step, solving the long-standing paradox: ATP was consumed not for proteolysis itself, but for the precise labeling of specific proteins for destruction [1] [5].
The Identity of APF-1 Revealed
The connection was made through a parallel line of research. In 1975, ubiquitin had been isolated and named for its ubiquitous presence in tissues and organisms [1]. Independently, a chromatin-associated protein, Ub-H2A (a ubiquitin-histone H2A conjugate), had been discovered in 1977 [2]. In 1980, Wilkinson, Urban, and Haas in Rose's laboratory established the critical link by proving that APF-1 was identical to ubiquitin [2] [5]. This unification of the protein degradation and chromatin biology fields revealed that ubiquitin's role extended far beyond histone modification, positioning it as a central player in a general regulatory mechanism.
Diagram 1: The experimental pathway from the initial paradox to the discovery of the ubiquitin system.
Elucidating the Enzymatic Machinery: E1, E2, and E3
Between 1981 and 1983, the collaborative efforts of Ciechanover, Hershko, and Rose led to the formulation of the "multistep ubiquitin-tagging hypothesis" and the identification of a cascade of three enzymes (Table 2) [1]:
- E1 (Ubiquitin-Activating Enzyme): This enzyme activates ubiquitin in an ATP-dependent reaction, forming a high-energy thioester bond.
- E2 (Ubiquitin-Conjugating Enzyme): Activated ubiquitin is transferred to a cysteine residue on an E2 enzyme.
- E3 (Ubiquitin Ligase): This enzyme confers specificity by recognizing target proteins and facilitating the transfer of ubiquitin from E2 to a lysine residue on the substrate, forming an isopeptide bond [2] [1].
The successive action of these enzymes results in the attachment of a polyubiquitin chain to the target protein, which serves as the recognition signal for degradation by the proteasome [1].
Table 2: The Enzymatic Cascade of the Ubiquitin System
| Enzyme | Key Function | Characteristic |
|---|---|---|
| E1 (Ubiquitin-Activating) | Activates ubiquitin using ATP | A single type or few types per cell [1] |
| E2 (Ubiquitin-Conjugating) | Carries activated ubiquitin | Several tens of types per cell [1] |
| E3 (Ubiquitin Ligase) | Recognizes specific protein substrates | Several hundred types, determines specificity [1] [3] |
Diagram 2: The ubiquitin conjugation cascade involving the sequential action of E1, E2, and E3 enzymes.
The Scientist's Toolkit: Key Research Reagents and Methods
Table 3: Essential Research Reagents and Methodologies for Studying the Ubiquitin System
| Reagent / Method | Function in Research | Role in Discovery |
|---|---|---|
| Reticulocyte Lysate | Cell-free system for biochemical analysis | Provided the source for initial fractionation and identification of APF-1/Ubiquitin [4] [5] |
| ATP (Adenosine Triphosphate) | Energy source for enzymatic reactions | Used to demonstrate energy dependence of conjugation and proteolysis [1] |
| Heat Inactivation | Method to isolate heat-stable proteins | Critical for separating APF-1 (heat-stable) from hemoglobin (heat-labile) [5] |
| Chromatography | Protein separation and purification technique | Used to fractionate the lysate into complementary active fractions (I and II) [1] |
| Immunochemical Methods | Isolate and detect ubiquitin-protein conjugates | Developed later to confirm the system's activity in living cells [1] |
| Fluorogenic Ub/UBL Probes | Assess activity of deubiquitinases (DUBs) | Modern tool (e.g., Ub-ACA) for studying enzyme activities in the pathway [6] |
From Biochemical Mechanism to Biological Principle
The initial characterization of the ubiquitin system in a cell-free extract was a biochemical triumph, but its true physiological significance was cemented by subsequent genetic and cellular studies. The identification of a temperature-sensitive mouse cell mutant (ts85) with a defective cell cycle was a key link [2] [1]. Researchers, including Alexander Varshavsky's group, demonstrated that the heat-sensitive protein in these cells was the E1 ubiquitin-activating enzyme [1] [5]. This proved that the ubiquitin system was not only essential for cell viability but was also a master regulator of critical processes like the cell cycle, DNA repair, and transcriptional regulation [2] [3]. The discovery of degradation signals, such as the N-end rule, further revealed how the system achieves its exquisite specificity [3].
The journey from an obscure heat-stable polypeptide (APF-1) in a reticulocyte extract to the identification of the ubiquitous protein regulator, ubiquitin, represents a cornerstone of modern molecular biology. The elegant biochemical work of Ciechanover, Hershko, and Rose, which elucidated the E1-E2-E3 enzymatic cascade, solved the fundamental energy paradox of intracellular proteolysis and established a new biological paradigm: that regulated protein degradation is a selective, dynamic, and essential regulatory process [2] [3]. This discovery laid the foundation for understanding the mechanistic basis of numerous cellular pathways and has provided critical insights into the pathogenesis of many diseases, including cancer and neurodegenerative disorders, opening avenues for targeted therapeutic interventions [7] [8].
The discovery of the E1-E2-E3 enzymatic cascade marked a pivotal advancement in our understanding of the ubiquitin-proteasome system (UPS). This hierarchical enzymatic pathway, culminating in the precise ligation of ubiquitin to target proteins, governs essential cellular processes ranging from protein degradation to cell signaling. This whitepaper provides an in-depth technical guide to the core biochemical principles of this cascade. It details the historical discovery of the ubiquitin thioester relay, summarizes key quantitative data on enzyme specificity, outlines modern experimental protocols for probing cascade activity, and visualizes critical workflows. Framed within the context of UPS research history, this review equips researchers and drug development professionals with the foundational knowledge and contemporary methodologies to study and therapeutically target this complex system.
The elucidation of the ubiquitin-proteasome system represents a cornerstone of modern cell biology. The initial discovery of ubiquitin as a tag for protein degradation was followed by a formidable challenge: unraveling the enzymatic mechanism of its conjugation. For years, it was postulated that ubiquitination required a three-enzyme cascade, but the precise biochemical steps remained enigmatic. The prevailing model suggested that E3 ubiquitin ligases functioned merely as passive "docking proteins," binding a substrate and an E2 enzyme to facilitate the direct transfer of ubiquitin from the E2 to the substrate [9].
A critical breakthrough in this field was published in Nature in 1995, which provided the first biochemical evidence for a more complex "ubiquitin thioester cascade." The Scheffner et al. study demonstrated that for the E3 ligase E6-AP, ubiquitin is transferred from the E2 enzyme to an active-site cysteine on the E3 itself, forming a distinct E3-ubiquitin thioester intermediate before the final ligation to the substrate [9]. This finding fundamentally redefined the enzymatic role of HECT-family E3 ligases, establishing that they are not simple docking adaptors but active catalysts that form a critical transient intermediate in the ubiquitin transfer pathway. This mechanistic insight opened the door for the biochemical dissection of the entire cascade, a process essential for understanding cellular regulation and developing novel therapeutics for diseases like cancer and neurodegeneration where the UPS is often dysregulated [10] [11].
The Core E1-E2-E3 Enzymatic Mechanism
The ubiquitination cascade is an ATP-dependent process involving three distinct classes of enzymes that work in sequence to activate and conjugate ubiquitin to substrate proteins. The following diagram illustrates this conserved mechanism, highlighting the key thioester intermediates at each step.
Figure 1: The Ubiquitin Transfer Cascade. The pathway involves sequential thioester transfers from E1 to E2 and, for HECT E3s, to E3, before final isopeptide linkage to a substrate lysine. RING E3s facilitate direct transfer from E2 to substrate.
The Three-Step Enzymatic Cascade
- E1: Ubiquitin Activation. The cascade initiates with a single E1 ubiquitin-activating enzyme. E1 consumes ATP to catalyze the adenylation of the C-terminus of ubiquitin, forming a high-energy ubiquitin-AMP intermediate. This activated ubiquitin is then transferred to the catalytic cysteine residue of the E1 itself, forming an E1~ubiquitin thioester bond. This step is the "alarm clock" of the UPS, committing ubiquitin to the degradation pathway [12].
- E2: Ubiquitin Conjugation. The second step involves a family of E2 ubiquitin-conjugating enzymes (also called UBCs). The E1~ubiquitin thioester complex interacts with an E2 enzyme, and through a transthiolation reaction, the ubiquitin is transferred from the E1's catalytic cysteine to the catalytic cysteine of the E2, forming an E2~ubiquitin thioester intermediate. The E2 thus acts as the "baton passer" in the relay [12].
- E3: Ubiquitin Ligation. The final step is mediated by a large family of E3 ubiquitin ligases, which provide substrate specificity. E3s are broadly categorized based on their mechanism:
- HECT E3 Ligases: As definitively shown for E6-AP, HECT E3s form a mandatory thioester intermediate with ubiquitin. The ubiquitin is transferred from the E2~ubiquitin complex to a catalytic cysteine on the HECT domain of the E3, before the E3 directly ligates it to a lysine residue on the substrate protein [9].
- RING E3 Ligases: RING E3s function as scaffolds and do not form a covalent bond with ubiquitin. Instead, they simultaneously bind both the E2~ubiquitin complex and the substrate, facilitating the direct transfer of ubiquitin from the E2 to the substrate [10].
This cascade can be repeated to form polyubiquitin chains of different linkages (e.g., K48 for proteasomal degradation, K63 for signaling), with the specific topology determining the fate of the modified protein [10] [11].
Quantitative Biochemical Profiling of the Cascade
A thorough biochemical dissection requires quantitative data on enzyme kinetics, specificities, and interactions. The following tables summarize key quantitative findings from foundational and modern studies.
Table 1: Key Enzyme Classes and Specificity Determinants in Human Ubiquitin/NEDD8 Cascades
| Enzyme Class | Representative Members | Key Specificity Determinant | Functional Outcome |
|---|---|---|---|
| E1 (Ubiquitin) | UBA1 | Specific for Ubiquitin-Arg72 | Recognizes and activates ubiquitin, not NEDD8 [13] |
| E1 (NEDD8) | APPBP1-UBA3 heterodimer | Specific for NEDD8-Ala72; UBA3-Arg190 as negative gate | Prevents spurious activation of ubiquitin-Arg72 [13] |
| E2 (Ubiquitin) | ~50 different E2s (e.g., UBE2D2) | Interaction surfaces for specific E1 and E3 partners | Determines possible E3 partnerships and chain topology [12] [14] |
| E3 (HECT) | E6-AP, NEDD4L | Catalytic Cysteine residue | Forms E3~Ub thioester intermediate essential for transfer [9] |
| E3 (RING) | Mdm2, MuRF1 | No catalytic cysteine; mediates E2-substrate interaction | Facilitates direct Ub transfer from E2 to substrate [10] |
Table 2: Experimentally Determined Kinetic and Functional Parameters
| Parameter Studied | Experimental System | Key Quantitative Finding | Reference |
|---|---|---|---|
| E1-E2 Ubiquitin Transfer | Orthogonal UB Transfer (OUT) | Engineered xUB-xE1-xE2 pairs showed zero cross-reactivity with native enzymes | [14] |
| E3 Substrate Scope | Quantitative Ubiquitin Profiling (Yeast) | 27% of identified UPS substrates required Rpn10 for turnover; UIM domain responsible for only 1/5 of these | [15] |
| E1 Heterodimer Function | FRET-based NEDD8 Activation | UBA3 alone activated NEDD8; APPBP1 acted as a scaffold to accelerate reaction rate | [16] |
| Proteasome Inhibition | GFPu Reporter Assay | Inhibition by Bortezomib or MG-132 causes accumulation of GFPu, measurable by increased fluorescence | [10] |
Key Experimental Protocols for Dissecting the Cascade
Protocol 1: Identification of E3-Ubiquitin Thioester Intermediates
This protocol is based on the seminal study that first demonstrated the E3-ubiquitin thioester intermediate for E6-AP [9].
- Objective: To provide biochemical evidence that an E3 ligase forms a covalent thioester bond with ubiquitin.
- Principle: Thioester bonds are labile and susceptible to cleavage by reducing agents like β-mercaptoethanol or DTT, whereas isopeptide bonds (the final substrate-ubiquitin linkage) are stable. This property allows for differential analysis.
- Methodology:
- Reconstituted System: Set up a complete in vitro ubiquitination reaction containing E1 enzyme, E2 enzyme, E3 ligase (e.g., E6-AP), ubiquitin, ATP, and an energy-regenerating system. Omit the protein substrate.
- Control Reactions: Include control reactions missing individual components (e.g., -E1, -E2, -ATP).
- Electrophoresis: Split the reaction products and subject them to non-reducing SDS-PAGE (without β-mercaptoethanol/DTT) and reducing SDS-PAGE (with β-mercaptoethanol/DTT).
- Detection: Perform western blotting using an anti-ubiquitin antibody.
- Expected Results: In the non-reducing gel, a higher molecular weight band corresponding to the E3-ubiquitin thioester complex will be observed. This band will disappear in the reducing gel, confirming its thioester nature. Control reactions will show no such band.
- Significance: This experiment is definitive proof of a catalytic E3-ubiquitin intermediate and distinguishes HECT E3 mechanisms from RING E3 mechanisms.
Protocol 2: Measuring UPS Activity with GFPu Reporter
This protocol details a widely used cellular assay to monitor global UPS functionality [10].
- Objective: To measure proteasome activity in living cells in a quantitative manner.
- Principle: A reporter protein (e.g., GFP) is fused to a potent degron sequence (e.g., CL1). This constitutively targets the reporter (GFPu) for ubiquitination and rapid degradation by the proteasome, resulting in low basal fluorescence. Upon proteasome inhibition, GFPu accumulates, leading to a measurable increase in fluorescence.
- Methodology:
- Cell Line Generation: Stably transfect cells with a plasmid encoding the GFPu construct.
- Treatment: Treat cells with a proteasome inhibitor (e.g., Bortezomib, MG-132) or vehicle control (DMSO) for a defined period.
- Quantification: Measure cellular fluorescence using flow cytometry, fluorescence microscopy, or a plate reader.
- Data Analysis: Fluorescence intensity in treated samples is normalized to control samples. A fold-increase in fluorescence is directly correlated with the degree of proteasome inhibition.
- Applications: This reporter is ideal for high-throughput screening of novel proteasome inhibitors, studying UPS dysfunction in disease models (e.g., neurodegeneration), and investigating the role of the UPS in cellular processes like differentiation [10].
The workflow for this and other proximity-labeling assays is complex, as visualized below.
Figure 2: ProteasomeID Workflow for Mapping E3/Proteasome Interactions. This proximity-labeling approach uses a biotin ligase (BirA) fused to a proteasome subunit to tag and identify interacting proteins and endogenous substrates in vivo [17].*
Protocol 3: Mapping Proteasome Interactomes and Substrates with ProteasomeID
For a systems-level view, ProteasomeID uses proximity labeling to capture the dynamic environment of the proteasome, including E3 ligases [17].
- Objective: To comprehensively identify proteins that interact with the proteasome in vivo, including transient E3 contacts and endogenous substrates.
- Principle: A promiscuous biotin ligase (BirA*) is genetically fused to a subunit of the core (20S) or regulatory (19S) proteasome particle. Upon expression in cells or a transgenic mouse model and addition of biotin, the ligase biotinylates all proteins within a ~10 nm radius.
- Methodology:
- Tagging: Generate stable cell lines or mice expressing BirA* fused to a proteasome subunit (e.g., PSMA4-BirA*).
- In Vivo Biotinylation: Administer biotin to the system to allow labeling of proximal proteins.
- Affinity Purification: Lyse cells/tissues and capture biotinylated proteins using streptavidin beads under stringent conditions.
- Mass Spectrometry: After on-bead digestion, identify and quantify the captured peptides using Liquid Chromatography with Tandem Mass Spectrometry (LC-MS/MS), ideally in Data-Independent Acquisition (DIA) mode for depth and reproducibility.
- Applications: This method allows for the unbiased discovery of novel proteasome-interacting proteins (E3s, shuttling factors), characterization of proteasome composition across different tissues, and identification of endogenous proteasome substrates by comparing samples with and without proteasome inhibition [17].
The Scientist's Toolkit: Key Research Reagents
The following table catalogues essential reagents for studying the ubiquitin-proteasome system, as featured in the cited research.
Table 3: Key Research Reagent Solutions for UPS Investigation
| Reagent / Technology | Core Function | Example Application |
|---|---|---|
| Orthogonal UB Transfer (OUT) Cascades | Engineered xUB, xE1, xE2 enzymes that function orthogonally to native machinery. | Mapping substrates of a specific E3 ligase without background from native cascades [14]. |
| Tandem Ubiquitin-Binding Entities (TUBEs) | Engineered high-affinity reagents with multiple UBA domains to bind polyUb chains. | Isolation of polyubiquitinated proteins from cell lysates; protection from DUBs [12]. |
| GFPu Reporter | A degron (CL1)-tagged Green Fluorescent Protein. | Real-time, live-cell measurement of global proteasome activity [10]. |
| Ub^G76V^-GFP Reporter | GFP fused to a non-cleavable ubiquitin mutant. | Monitoring proteasome-dependent degradation independent of DUB activity [10]. |
| ProteasomeID (e.g., PSMA4-BirA*) | Proximity-dependent biotinylation system targeted to the proteasome. | Unbiased mapping of proteasome interactomes and substrates in vivo [17]. |
| Natural Product Inhibitors | Small molecules from natural sources that target specific UPS components. | Probing UPS function and serving as leads for drug development (e.g., Bortezomib) [18]. |
The biochemical dissection of the E1-E2-E3 cascade has evolved from initial mechanistic discoveries to the current era of systems-level quantitative analysis. The journey began with critical experiments demonstrating covalent E3-ubiquitin intermediates [9] and has advanced to sophisticated technologies like ProteasomeID that provide holistic views of proteasome networks in living animals [17]. This deep mechanistic understanding has firmly established the UPS as a premier therapeutic target.
The future of targeting this cascade lies in increasing specificity. The clinical success of proteasome inhibitors like Bortezomib for multiple myeloma validated the UPS as a drug target but also highlighted the need for more precise strategies [10] [11]. Current research is focused on moving downstream from the proteasome to target specific E3 ligases or even developing molecules like PROTACs (PROteolysis TArgeting Chimeras) that hijack the E3 machinery to degrade disease-causing proteins [12]. The continued development of quantitative tools, such as engineered orthogonal cascades [14] and sensitive in vivo reporters [10] [17], will be essential for deciphering the complex biology of the UPS and for translating this knowledge into the next generation of targeted therapeutics for cancer, neurodegenerative disorders, and immune diseases.
The discovery that ubiquitin, initially identified as a chromatin-associated protein, serves as a central regulator of intracellular protein degradation represents a fundamental paradigm shift in cell biology. This whitepaper traces the critical historical pathway through which researchers connected ubiquitin's role in chromatin modification to its function in the ubiquitin-proteasome system (UPS). We examine the key experimental evidence that bridged these seemingly disparate fields, the methodological approaches that enabled this connection, and the profound implications this synthesis has had for understanding cellular regulation and therapeutic development. The convergence of chromatin biology and protein degradation research exemplifies how interdisciplinary investigation can revolutionize our understanding of fundamental biological processes.
The ubiquitin field emerged from two distinct research pathways that converged to establish a new understanding of cellular regulation. For decades, intracellular proteins were largely believed to be long-lived, with regulated protein degradation not considered a major control mechanism for cellular processes [2]. The discovery of the ubiquitin system fundamentally overturned this conception, revealing that controlled proteolysis rivals transcriptional and translational regulation in significance [2].
Ubiquitin was independently discovered through separate investigative streams:
- Immunological research: Gideon Goldstein and colleagues identified a universally present polypeptide they termed "ubiquitin" (originally UBIP for "ubiquitous immunopoietic polypeptide") during studies of thymic hormones influencing lymphocyte differentiation [19].
- Chromatin research: A separate track identified a protein conjugate between histone H2A and a non-histone moiety, initially termed protein A24, which was subsequently shown to contain ubiquitin [2] [19].
The connection between these disparate research domains—chromatin biology and protein degradation—represented one of the most significant conceptual breakthroughs in modern cell biology, fundamentally altering our understanding of how cells regulate protein stability and function.
Historical Timeline of Key Discoveries
Table 1: Chronological Development of the Ubiquitin Field
| Year | Discovery | Key Researchers | Significance |
|---|---|---|---|
| 1975 | Identification of ubiquitin as a universal protein | Goldstein et al. [19] | Initial characterization of ubiquitin as a distinct molecular entity |
| 1977 | Identification of A24 (ubiquitin-H2A conjugate) in chromatin | Goldknopf & Busch [2] | First evidence of ubiquitin modification of histones |
| 1978-1980 | APF-1 (later identified as ubiquitin) conjugated to proteins before degradation | Hershko, Ciechanover, Rose [2] [19] | Establishment of ubiquitin's role in protein degradation |
| 1980 | APF-1 identified as ubiquitin | Wilkinson et al. [2] | Critical connection between chromatin and degradation research |
| 1980-1982 | Ubiquitin-containing nucleosomes localized to transcribed genes | Levinger & Varshavsky [2] | Functional connection between ubiquitin and gene regulation |
| 1982-1983 | E1, E2, E3 enzymatic cascade characterized | Hershko, Ciechanover, Rose [2] | Mechanistic understanding of ubiquitin conjugation |
| 1984-1990 | Biological functions of ubiquitin system identified in cell cycle, DNA repair | Varshavsky group [2] | Expansion of ubiquitin functions beyond degradation |
Methodological Approaches and Experimental Evidence
Critical Experimental Workflows
The paradigm shift connecting chromatin ubiquitin to protein degradation relied on several key experimental approaches that enabled researchers to bridge these domains.
Biochemical Fractionation and Enzymology
The Hershko laboratory employed systematic biochemical fractionation of reticulocyte extracts to identify the components of the protein degradation machinery:
Figure 1: Biochemical Workflow for UPS Discovery
This approach identified APF-1 (ATP-dependent proteolytic factor 1) as a key component that became covalently conjugated to proteins before their degradation in cell extracts [2]. The critical breakthrough came when APF-1 was recognized as identical to ubiquitin, creating the conceptual link between the chromatin and degradation fields [2] [19].
Genetic and Cell Biological Approaches
Parallel genetic approaches in yeast and mammalian cells established the biological relevance of the ubiquitin system:
Figure 2: Genetic Approaches to Ubiquitin Biology
The identification of a temperature-sensitive mouse cell line (ts85) that lost ubiquitin-histone conjugates at restrictive temperatures provided crucial genetic evidence connecting the ubiquitin system to cellular viability [2].
The Ubiquitin-Proteasome System: Core Mechanisms
The core ubiquitin-proteasome system comprises a coordinated enzymatic cascade:
Figure 3: Ubiquitin-Proteasome System Cascade
The system features a single E1 activating enzyme, multiple E2 conjugating enzymes, and numerous E3 ligases that provide substrate specificity [20] [21]. Polyubiquitinated substrates are recognized and degraded by the 26S proteasome, a massive 2.5 MDa protease complex [2].
The Scientist's Toolkit: Key Research Reagents and Methods
Table 2: Essential Research Tools in Ubiquitin Research
| Category | Specific Reagents/Methods | Function/Application | Key References |
|---|---|---|---|
| Model Systems | Rabbit reticulocyte lysate | In vitro reconstitution of ubiquitination and degradation | Hershko et al. [2] |
| ts85 mouse cell line | Temperature-sensitive mutant for functional studies | Varshavsky [2] | |
| Saccharomyces cerevisiae (yeast) | Genetic dissection of ubiquitin pathway | Varshavsky, Hochstrasser [2] | |
| Biochemical Tools | ATPγS (non-hydrolyzable ATP analog) | Study of ATP dependence in ubiquitin activation | Hershko et al. [2] |
| Proteasome inhibitors (MG132, lactacystin) | Investigation of proteasome function | Goldberg [22] | |
| Ubiquitin conjugation enzymes (E1, E2, E3) | In vitro reconstitution of ubiquitination | Ciechanover et al. [2] | |
| Molecular Biology Reagents | Ubiquitin mutants (K48R, K63R, etc.) | Study of chain linkage specificity | Pickart et al. [21] |
| N-end rule substrates | Identification of degradation signals | Varshavsky [2] | |
| siRNA/shRNA libraries | Functional screening of ubiquitin system components | Multiple groups |
Quantitative Analysis of Ubiquitin System Components
Table 3: Quantitative Aspects of the Ubiquitin System
| Parameter | Value/Magnitude | Biological Significance | Experimental Basis |
|---|---|---|---|
| Enzyme Diversity | ~1 E1, 14 E2s, >1000 E3s | Extraordinary substrate specificity potential | Genomic analysis [20] |
| Polyubiquitin Chain Linkages | 8 types (K6, K11, K27, K29, K33, K48, K63, M1) | Differential functional consequences | Mass spectrometry [21] |
| Proteasome Size | 2.5 MDa | Massive degradation machinery | Structural studies [2] |
| Ubiquitin-H2A Conjugate Stability | Cell cycle-dependent | Regulation of chromatin structure | Cell biological studies [19] |
| Histone Modification Sites | H2A: 13 sites, H2B: 12 sites, H3: 21 sites, H4: 14 sites | Complex regulatory potential | Mass spectrometry [20] |
Implications and Future Directions
Therapeutic Applications
The understanding of ubiquitin biology has spawned entirely new therapeutic approaches, most notably in the field of targeted protein degradation [21]. Proteolysis-Targeting Chimeras (PROTACs) represent a groundbreaking application that harnesses the ubiquitin system to selectively degrade disease-causing proteins [21]. These bifunctional molecules simultaneously bind to a target protein and an E3 ubiquitin ligase, inducing target ubiquitination and degradation [21]. The first PROTAC molecule was developed in 2001, and by 2022, several candidates had entered clinical trials [21].
Expanding Paradigms: Beyond Proteasomal Degradation
Subsequent research has revealed that ubiquitin's roles extend far beyond proteasomal targeting, including:
- Histone regulation: Ubiquitination of histones H2A and H2B regulates chromatin structure and gene expression through both proteasome-independent and dependent mechanisms [20] [23].
- DNA repair: Specific ubiquitin modifications on histones recruit DNA repair proteins like 53BP1 to sites of damage [24].
- Lysosomal targeting: Certain ubiquitin chain types (particularly K63-linked) target proteins to lysosomal degradation pathways [25] [26].
- Selective autophagy: Ubiquitin serves as a signal for selective autophagy of protein aggregates, organelles, and pathogens [26].
The connection between ubiquitin in chromatin and protein degradation represents one of the most fruitful syntheses in modern cell biology. What began as separate investigations into lymphocyte biology and chromatin structure converged to reveal a universal regulatory system of profound importance. This paradigm shift transformed our understanding of cellular regulation, demonstrating that controlled protein degradation rivals transcriptional control in significance. The continued exploration of ubiquitin biology promises further insights into cellular regulation and new therapeutic opportunities for human disease.
The Ubiquitin-Proteasome System (UPS) represents one of the most sophisticated and selective mechanisms for intracellular protein degradation in eukaryotic cells. Since its groundbreaking discovery, which earned Avram Hershko, Aaron Ciechanover, and Irwin Rose the 2004 Nobel Prize in Chemistry, the UPS has been recognized as a central regulator of cell viability and function [22]. This complex system operates through a sequential enzymatic cascade— involving E1 (activating), E2 (conjugating), and E3 (ligating) enzymes—that tags target proteins with ubiquitin chains, marking them for destruction by the proteasome [7] [22]. This targeted degradation is not merely a disposal mechanism but a crucial regulatory process controlling fundamental cellular processes including cell cycle progression, apoptosis, DNA repair, and stress response [22]. The indispensability of the UPS is underscored by its involvement in eliminating damaged or misfolded proteins and precisely regulating the concentrations of key regulatory proteins, thereby maintaining cellular homeostasis. This whitepaper examines the experimental evidence validating the UPS as essential for cell viability and explores the technical approaches used to demonstrate its critical functions.
Historical Context and Fundamental Principles
The Discovery of a Revolutionary Cellular System
The elucidation of the UPS began with pioneering work in the late 1970s and early 1980s, when Hershko, Ciechanover, and Rose discovered the ATP-dependent proteolytic system that would revolutionize our understanding of cellular regulation. Their initial experiments, conducted with limited resources but extraordinary intellectual rigor, unveiled an unprecedented concept: a 2.5 million Dalton protease complex, three tagging enzymes, and a small protein tag (ubiquitin) working in concert to selectively target proteins for degradation [22]. This discovery was particularly remarkable because it revealed that protein degradation was not a passive process but a highly specific, regulated mechanism central to cellular control. The historical significance of this discovery was celebrated two decades later in a 2025 symposium titled "The Ubiquitin Revolution: Celebrating 20 Years of Avram Hershko's Nobel Legacy," highlighting how this fundamental biological insight continues to fuel major biomedical advances [27].
The Ubiquitin-Proteasome System Cascade
The UPS operates through a carefully orchestrated enzymatic cascade:
- Activation: The E1 ubiquitin-activating enzyme activates ubiquitin in an ATP-dependent reaction
- Conjugation: Activated ubiquitin is transferred to an E2 ubiquitin-conjugating enzyme
- Ligation: E3 ubiquitin ligases facilitate the transfer of ubiquitin from E2 to specific substrate proteins
- Polyubiquitination: Repeated cycles lead to polyubiquitin chain formation on substrate proteins
- Degradation: The 26S proteasome recognizes and degrades polyubiquitinated proteins, recycling ubiquitin
This system provides the structural basis for targeted protein degradation that is essential for cellular health, and its dysfunction is implicated in numerous pathological conditions including cancer, neurodegenerative disorders, and infectious diseases [7] [22].
Table 1: Key Components of the Ubiquitin-Proteasome System
| Component | Function | Significance |
|---|---|---|
| E1 Enzyme | Activates ubiquitin using ATP | Initiates the entire ubiquitination cascade |
| E2 Enzyme | Carries activated ubiquitin | Determines ubiquitin chain topology |
| E3 Ligase | Binds specific substrates and facilitates ubiquitin transfer | Provides substrate specificity (>600 identified) |
| Proteasome | Degrades ubiquitinated proteins | Recycles amino acids and regulates protein turnover |
| Deubiquitinases (DUBs) | Remove ubiquitin from proteins | Provide counter-regulation and ubiquitin recycling |
Methodological Framework: Assessing Cell Viability in UPS Research
Cell Viability Assays: Principles and Applications
Validating the essential nature of the UPS for cell viability requires robust methodological approaches that can accurately distinguish between live and dead cells. According to the Organisation for Economic Co-operation and Development (OECD) classification, cell viability methods can be categorized into four groups: non-invasive cell structure damage, invasive cell structure damage, cell growth, and cellular metabolism [28]. The careful selection of appropriate viability assays is crucial for researchers, as each method operates on different principles with distinct advantages and disadvantages [28].
Cell viability is fundamentally defined as the proportion of living, healthy cells within a population, with viable cells capable of performing essential metabolic functions [28] [29]. A cell is considered dead when it irreversibly loses plasma membrane barrier function, forms apoptotic bodies, or is engulfed by phagocytes [28]. This distinction is critical when studying UPS function because UPS inhibition can trigger various cell death pathways, including apoptosis and necrosis.
OECD-Classified Viability Assessment Methods
Table 2: Cell Viability Assays Classified by OECD Guidelines with Relevance to UPS Research
| Assay Category | Examples | Principle | Applications in UPS Research |
|---|---|---|---|
| Non-invasive Structural Damage | LDH release, AK release | Measures cytoplasmic enzymes released upon membrane damage | Detects necrosis secondary to UPS inhibition |
| Invasive Structural Damage | Trypan blue, Propidium iodide, Hoechst stains | Dyes penetrate compromised membranes of dead cells | Distinguishes viable/non-viable cells after UPS disruption |
| Cell Growth Assays | Cell counting, BrdU incorporation | Measures proliferation capacity | Assesses long-term consequences of UPS impairment |
| Cellular Metabolism Assays | MTT, XTT, ATP assays | Measures metabolic activity via mitochondrial function | Evaluates metabolic consequences of UPS inhibition |
Specialized Viability Assessment in UPS Studies
For research specifically focused on validating UPS function, several specialized approaches provide critical insights:
Apoptosis Detection Assays: Since UPS inhibition frequently induces programmed cell death, apoptosis-specific assays are particularly valuable. These include:
- Caspase activity assays measuring activation of executioner caspases
- Annexin V staining detecting phosphatidylserine externalization
- DNA fragmentation analysis identifying endonuclease activation [28] [29]
Cell Proliferation Monitoring: As proliferating cells are always viable, proliferation assays serve as excellent indicators of cell health in UPS studies. These include:
- DNA content analysis using propidium iodide to identify cells in different cell cycle phases
- BrdU incorporation measuring DNA synthesis during S phase
- Proliferation protein detection (PCNA, Ki67, Phospho-histone H3) [29]
Metabolic Activity Assays: The MTT and XTT assays quantify the reduction of tetrazolium dyes by mitochondrial enzymes in viable cells, providing a colorimetric readout of cell health [29]. Similarly, ATP measurement assays quantify ATP content using luminescent, fluorometric, or colorimetric readouts, with signal generation proportional to the number of healthy, metabolically active cells [29].
Experimental Validation: Key Protocols and Techniques
Pharmacological Inhibition of the UPS
The most direct approach to validate the essential nature of the UPS involves targeted inhibition followed by comprehensive viability assessment:
Protocol: Proteasome Inhibitor Treatment and Viability Analysis
- Cell Preparation: Plate cells at appropriate density (e.g., 5,000-10,000 cells/well in 96-well plates) and allow attachment for 24 hours
- Inhibitor Treatment: Apply proteasome inhibitors (e.g., MG132, Bortezomib/PS-341, Lactacystin) across a concentration gradient (typically 1 nM-10 μM) and multiple time points (6-72 hours)
- Viability Assessment:
- Metabolic Activity: Add MTT (0.5 mg/mL) for 2-4 hours, solubilize formazan crystals with DMSO or isopropanol, measure absorbance at 570 nm [29]
- Membrane Integrity: Collect culture supernatant, measure LDH activity colorimetrically (absorbance at 490-500 nm) [28]
- Direct Counting: Trypan blue exclusion with automated cell counters (e.g., Bio-Rad TC20, ThermoFisher Countess II) [30]
Expected Results: Proteasome inhibition typically produces a dose-dependent reduction in viability evidenced by decreased metabolic activity, increased LDH release, and rising trypan blue-positive cells. Research demonstrates that proliferating malignant cells show particular sensitivity to proteasome blockade, providing the therapeutic rationale for drugs like Bortezomib in multiple myeloma [22].
Genetic Manipulation of UPS Components
Genetic approaches provide targeted validation of specific UPS components:
RNA Interference Protocol for E3 Ligase Validation
- Design and Transfection: Design siRNA sequences targeting specific E3 ligases or other UPS components; transfert using appropriate reagents (e.g., lipofectamine)
- Efficiency Validation: Confirm knockdown efficiency via Western blotting or qRT-PCR 48-72 hours post-transfection
- Phenotypic Assessment:
CRISPR-Cas9 Knockout Approaches
- Generate knockout cell lines for essential E3 ligases or proteasome subunits
- Assess compensatory mechanisms and potential adaptations
- Evaluate cell viability under various stress conditions
Monitoring UPS-Specific Cell Death Pathways
UPS disruption typically activates specific cell death programs that require specialized detection methods:
Apoptosis Pathway Analysis Protocol
- Caspase Activation: Use fluorogenic caspase substrates (e.g., DEVD-afc for caspase-3) or antibody-based detection of cleaved caspases
- Mitochondrial Assessment: Measure mitochondrial membrane potential using JC-1 or TMRM dyes
- Morphological Analysis: Assess nuclear condensation and fragmentation with Hoechst 33342 or DAPI staining [28] [29]
Research has demonstrated that UPS inhibitors potentiate cisplatin-induced apoptosis and can reverse drug resistance by inhibiting nucleotide excision repair pathways, highlighting the interconnectedness of UPS function with other cellular processes [22].
Technical Visualization: Experimental Workflows and Pathway Diagrams
UPS Mechanism and Experimental Validation Pathway
Cell Viability Assessment Workflow
The Scientist's Toolkit: Essential Research Reagents
Table 3: Essential Research Reagents for UPS and Cell Viability Studies
| Reagent Category | Specific Examples | Function/Application | Key Considerations |
|---|---|---|---|
| Proteasome Inhibitors | MG132, Bortezomib (PS-341), Lactacystin, Carfilzomib | Specifically inhibit proteasomal activity | Varying specificity, different chemical classes (peptide aldehydes, boronic acids, β-lactones) |
| E1/E2/E3 Inhibitors | PYR-41 (E1 inhibitor), CC0651 (E2 inhibitor), Nutlin (MDM2 inhibitor) | Target specific components of ubiquitination cascade | Varying selectivity, potential off-target effects |
| Viability/Cytotoxicity Assay Kits | MTT/XTT kits, LDH release kits, ATP measurement kits, Live/Dead staining kits | Quantify viable cells through different mechanisms | Differ in sensitivity, dynamic range, and compatibility with high-throughput screening |
| Apoptosis Detection Reagents | Annexin V kits, Caspase activity assays, TUNEL assay kits | Detect and quantify apoptotic cells | Multiple parameters needed for definitive apoptosis confirmation |
| Cell Permeable Dyes | Propidium iodide, 7-AAD, Hoechst 33342, Acridine Orange | Distinguish viable/non-viable cells based on membrane integrity | Varying spectral properties, potential cytotoxicity with prolonged exposure |
| Automated Cell Counters | Bio-Rad TC10/TC20, ThermoFisher Countess II, Nexcelom Cellometer | Automated viability assessment using trypan blue or fluorescent dyes | Improve reproducibility and throughput for large-scale studies |
Discussion and Future Perspectives
The experimental validation of the UPS as essential for cell viability has transformed our understanding of cellular regulation and created new therapeutic paradigms. The fundamental discovery of the ubiquitin system has evolved into a sophisticated research field with profound clinical implications, particularly in oncology where proteasome inhibitors have become standard care for multiple myeloma [22]. The continuing revolution in ubiquitin research, highlighted by recent symposiums honoring the legacy of the original discovery, points toward an expanding frontier of therapeutic opportunities [27].
Future research directions include:
- Advanced Targeted Protein Degradation: Developing novel therapeutic strategies like molecular glues and PROTACs that harness the UPS to target previously "undruggable" proteins [27]
- Tissue-Specific UPS Function: Understanding how UPS components perform specialized functions in different tissues and cellular contexts
- System-Wide UPS Monitoring: Developing comprehensive approaches to monitor ubiquitination events and proteasome activity in real-time within living cells
- Combination Therapies: Optimizing UPS-targeted therapies in combination with other treatment modalities to overcome resistance mechanisms
The critical role of the UPS in maintaining cell viability through regulated protein degradation represents one of the most significant conceptual advances in modern cell biology. As noted by Dr. Lan Huang, "Prof. Hershko's Nobel-recognized discovery of the ubiquitin-proteasome system has been one of the most profound scientific advances in modern biology" [27]. The continued validation of this system's essential functions ensures that UPS research will remain at the forefront of biomedical science, driving both fundamental discoveries and transformative therapies for decades to come.
From Mechanism to Medicine: Therapeutic Targeting of the UPS
The ubiquitin-proteasome system (UPS) represents a primary conduit for selective intracellular protein degradation in eukaryotic cells, regulating a vast array of cellular processes including cell cycle progression, apoptosis, and stress response [2] [22]. This highly conserved system involves a cascade of enzymes (E1, E2, E3) that tag target proteins with ubiquitin chains, marking them for recognition and degradation by the 26S proteasome—a large, multi-subunit complex comprising a 20S catalytic core and 19S regulatory particles [31] [2]. The critical discovery that proliferating malignant cells exhibit heightened sensitivity to proteasome inhibition fundamentally transformed oncology therapeutics, establishing the UPS as a validated target for anticancer drug development [32] [22]. This review traces the scientific trajectory from fundamental discoveries of the UPS to the clinical implementation of proteasome inhibitors, focusing on the research tool MG132 and the first-in-class therapeutic bortezomib.
Historical Foundations of Ubiquitin-Proteasome Research
The conceptual foundation for proteasome inhibition was established through pioneering work on the UPS in the late 1970s and 1980s. Avram Hershko, Aaron Ciechanover, and Irwin Rose discovered the ATP-dependent proteolytic system in reticulocyte extracts, identifying ubiquitin (initially termed APF-1) as the central tag in this degradation pathway [2] [22]. Their elucidation of the enzymatic cascade (E1, E2, E3) responsible for ubiquitin conjugation, coupled with the identification of the 26S proteasome as the degradation machinery, earned them the 2004 Nobel Prize in Chemistry [22]. Concurrently, Alexander Varshavsky's laboratory uncovered the biological functions of the UPS, demonstrating its essential roles in cell cycle regulation, DNA repair, and transcriptional control [2]. These complementary discoveries revealed that regulated protein degradation rivals transcriptional regulation in significance for cellular circuit control, fundamentally reshaping understanding of intracellular physiology and pathology [2].
Table 1: Key Historical Discoveries in the Ubiquitin-Proteasome System
| Year Range | Key Discovery | Principal Investigators | Significance |
|---|---|---|---|
| 1978-1980 | ATP-dependent protein degradation & APF-1 (ubiquitin) conjugation | Hershko, Ciechanover, Rose | Established enzymatic pathway for targeted protein degradation |
| 1980-1983 | Identification of E1, E2, E3 enzymes | Hershko and colleagues | Elucidated the ubiquitin conjugation machinery |
| 1984-1990 | Biological functions in cell cycle, DNA repair, and degradation signals | Varshavsky and colleagues | Revealed physiological roles of UPS in living cells |
| 1990s | Proteasome as target for apoptosis induction | Goldberg and others | Validated proteasome inhibition as anticancer strategy |
| 2003 | FDA approval of bortezomib | Millennium Pharmaceuticals | First proteasome inhibitor approved for human therapy |
The Research Tool: MG132 and Laboratory Applications
MG132 (carbobenzoxyl-L-leucyl-L-leucyl-leucinal) represents a potent, reversible peptide aldehyde inhibitor that primarily targets the chymotrypsin-like activity of the 20S proteasome's β-subunits [33] [22]. As a laboratory reagent, MG132 has been instrumental in elucidating proteasome functions and mechanisms of apoptosis, serving as a fundamental tool for basic research long before clinical applications were realized.
Experimental Protocols for MG132 Applications
Standardized experimental methodologies have been established for investigating MG132 effects in cellular models:
Cytotoxicity Assessment (CCK-8 Assay): Cells are inoculated into 96-well plates and treated with MG132 concentration gradients (typically 0.5-10 μM) for 8-48 hours. After treatment, CCK-8 solution is added and optical density (OD450) measured to determine cell viability and calculate IC50 values [33].
Apoptosis Quantification: Following 24-hour MG132 treatment (0.5-2 μM), cells are collected, stained with Annexin V-FITC/PI, and analyzed by flow cytometry to distinguish early apoptotic (Annexin V+/PI-), late apoptotic (Annexin V+/PI+), and necrotic (Annexin V-/PI+) populations [33].
Wound Healing/Migration Assay: Cells are cultured to confluence in 6-well plates, a scratch created with a pipette tip, and MG132 (0.125-0.5 μM) added in serum-free medium. Migration is quantified at 0, 12, and 24-hour intervals using microscopy and ImageJ software analysis [33].
Western Blot Analysis: After 24-hour MG132 treatment (0.5-2 μM), cellular proteins are extracted, separated by SDS-PAGE, transferred to PVDF membranes, and probed with primary antibodies against targets of interest (e.g., p53, p21, caspase-3, Bcl-2, CDK2), followed by HRP-conjugated secondary antibodies and ECL detection [33].
Mechanism of Action: MG132 as a Multi-Target Agent
Research in A375 melanoma cells has elucidated MG132's dual regulatory capacity, demonstrating potent anti-tumor activity with an IC50 of 1.258 ± 0.06 μM [33]. Mechanistic studies reveal that MG132 simultaneously activates the p53/p21/caspase-3 axis while suppressing CDK2/Bcl-2 signaling, triggering cell cycle arrest and DNA damage cascades [33]. Additionally, MAPK pathway activation emerges as a critical apoptosis driver, with western blot analyses confirming dose-responsive modulation of these molecular targets [33]. The compound induces concentration-dependent apoptosis, with 2 μM treatment producing early apoptosis in 46.5% and total apoptotic response in 85.5% of cells within 24 hours, while significantly suppressing cellular migration at therapeutic concentrations [33].
Diagram 1: MG132 mechanism of action in cancer cells
From Bench to Bedside: Bortezomib as First-Line Therapy
The transition from research tool to clinical therapeutic culminated with the development of bortezomib (PS-341, Velcade), a first-in-class, reversible dipeptidyl boronic acid proteasome inhibitor. Bortezomib's journey from concept to clinic radically overturned initial skepticism about UPS inhibition as a feasible therapeutic approach, ultimately establishing proteasome inhibition as a validated strategy for cancer treatment [32].
Pharmacology and Mechanism of Action
Bortezomib exhibits high specificity for the 26S proteasome, forming reversible covalent bonds with the threonine residues in the active sites of the 20S subunit's β-rings, preferentially inhibiting the chymotrypsin-like activity [34]. Its pleiotropic mechanisms of action include:
NF-κB Pathway Inhibition: By stabilizing Iκ-B, bortezomib prevents nuclear translocation of NF-κB, thereby inhibiting transcription of anti-apoptotic factors (Bcl-2, XIAP), growth factors (IL-6, VEGF), and adhesion molecules (VCAM-1, ICAM-1) [34].
Apoptosis Induction: Bortezomib activates both intrinsic and extrinsic apoptotic pathways through JNK activation, mitochondrial membrane potential disruption, ROS generation, and caspase activation [34].
Cell Cycle Disruption: The drug induces cell cycle arrest by accumulating cyclin-dependent kinase inhibitors and disrupting cyclin regulation [35].
Bortezomib is typically administered intravenously or subcutaneously at 1.3 mg/m² on a twice-weekly schedule for two weeks followed by a treatment-free week in a 21-day cycle [34]. It demonstrates approximately 80% plasma protein binding, rapid tissue redistribution with preferential accumulation in gastrointestinal tissues, and hepatic metabolism via CYP-450 isoenzymes with oxidative deboronation forming inactive metabolites [34].
Table 2: Pharmacological Properties of Clinical Proteasome Inhibitors
| Parameter | Bortezomib | Carfilzomib | Ixazomib |
|---|---|---|---|
| Inhibitor Class | Reversible boronic acid | Irreversible epoxyketone | Reversible boronic acid |
| Administration | IV, subcutaneous | IV | Oral |
| Half-life | 9-15 hours (first dose) | ≤1 hour | 3.4-9.5 days |
| Major Toxicities | Peripheral neuropathy, cytopenias | Cardiotoxicity, cytopenias | Gastrointestinal, rash |
| FDA Approval | 2003 (multiple myeloma) | 2012 (multiple myeloma) | 2015 (multiple myeloma) |
Clinical Efficacy and Real-World Evidence
The phase 3 VISTA trial established bortezomib plus melphalan and prednisone (VMP) as a standard regimen for elderly patients with newly diagnosed multiple myeloma ineligible for transplantation [35]. Real-world studies have corroborated this efficacy; a retrospective analysis of 164 elderly patients (median age 75 years) demonstrated an overall response rate of 81.7% with complete response rate of 10.36% [35]. After median follow-up of 38.51 months, median overall survival was 34.33 months and event-free survival after VMP was 18.51 months [35]. Importantly, VMP efficacy extended to high-risk cytogenetic profiles, with no significant differences in response rates or survival parameters between patients with t(4;14), t(14;16), or del17p and those with normal cytogenetics [35].
Diagram 2: Bortezomib's multifaceted mechanism in multiple myeloma
The Scientist's Toolkit: Essential Research Reagents and Methods
Contemporary proteasome inhibitor research employs a sophisticated array of reagents and methodologies to elucidate mechanisms and therapeutic potential:
Table 3: Essential Research Reagents for Proteasome Inhibition Studies
| Reagent/Cell Line | Application | Key Features | Experimental Use |
|---|---|---|---|
| MG132 | Reversible proteasome inhibition | Peptide aldehyde, primarily inhibits chymotrypsin-like activity | Mechanism studies, apoptosis induction (0.5-10 μM) |
| Bortezomib | Clinical compound testing | Dipeptidyl boronic acid, reversible inhibition | Preclinical models, combination therapy studies |
| A375 Melanoma Cells | Melanoma research | Human malignant melanoma cell line | Migration, apoptosis, mechanism studies (in vitro) |
| H1299 Non-Small Cell Lung | Reporter cell assays | p53-null lung carcinoma | Proteasome Inhibition Reporter (PIR) development |
| PIR-YFP Reporter | High-throughput screening | YFP-tagged p53 mutant with defective NLS | Cytoplasm-to-nucleus translocation upon proteasome inhibition |
| Fluorogenic Proteasome Substrates | Enzymatic activity assays | Suc-LLVY-AMC (chymotrypsin-like) | Direct proteasome activity measurement in cell lysates |
| Ubi(G76V)-GFP Reporter | UPS functionality | Ubiquitin fusion degradation substrate | Continuous monitoring of UPS activity in live cells |
High-Throughput Screening Methodologies
Innovative screening approaches have accelerated proteasome inhibitor discovery. The image-based screening assay utilizing H1299 cells stably expressing a fluorescent Proteasome Inhibition Reporter (PIR) protein enables high-throughput compound evaluation [31]. This system exploits the cytoplasm-to-nucleus translocation of PIR upon proteasome inhibition, with automated microscopy (e.g., WiScan Cell Imaging System) and image processing facilitating rapid screening of chemical libraries [31]. Using this approach, researchers screened the NCI Diversity Set (1,992 compounds) and identified four proteasome inhibitors, three with novel structures [31].
Clinical Landscape and Future Directions
The proteasome inhibitors market continues to expand, valued at approximately $2.7 billion in 2024 with projected growth to $6.1 billion by 2034, driven by increasing hematologic cancer incidence and therapeutic advancements [36]. Bortezomib's patent expiry in 2022 has accelerated development of next-generation inhibitors and generic formulations, while clinical applications continue to broaden beyond multiple myeloma to include mantle cell lymphoma and investigation in solid tumors [37] [36].
Current research focuses on overcoming limitations of first-generation inhibitors, particularly peripheral neuropathy associated with bortezomib and cardiotoxicity with carfilzomib [34] [35]. Subcutaneous administration and once-weekly dosing regimens have demonstrated reduced neurotoxicity while maintaining efficacy [34]. Additionally, combination strategies with other targeted therapies, immunomodulatory agents, and CAR-T cell therapies represent promising approaches to enhance efficacy and overcome resistance [37] [36]. The recent FDA approval of Abecma (idecabtagene vicleucel), a CAR-T cell therapy for relapsed/refractory multiple myeloma, highlights the ongoing integration of proteasome inhibitors with emerging immunotherapeutic modalities [37].
The trajectory from MG132 as a fundamental research tool to bortezomib as first-line therapy exemplifies the successful translation of basic biological discoveries into transformative cancer therapeutics. The initial characterization of the ubiquitin-proteasome system, once considered a fundamental but therapeutically inaccessible pathway, has yielded an entirely new class of anticancer agents that have fundamentally improved outcomes for patients with multiple myeloma and other hematologic malignancies. Ongoing research continues to refine proteasome inhibitor chemistry, administration strategies, and combination approaches, while basic investigations using tools like MG132 continue to reveal novel biological insights and potential therapeutic applications beyond oncology. The continued evolution of proteasome-targeted therapeutics underscores the enduring impact of fundamental biochemical research on clinical medicine.
Targeted protein degradation (TPD) represents a transformative approach in drug discovery, moving beyond the occupancy-driven model of traditional small-molecule inhibitors toward a paradigm of event-driven pharmacology [38] [39]. While conventional drugs transiently block protein activity by binding to active sites, TPD strategies harness the cell's intrinsic protein quality control machinery to achieve irreversible removal of disease-causing proteins [21] [39]. This approach has unlocked therapeutic possibilities for previously "undruggable" targets, including transcription factors, scaffolding proteins, and mutant oncoproteins that lack conventional binding pockets [38]. Among TPD strategies, PROteolysis TArgeting Chimeras (PROTACs) and molecular glue degraders have emerged as the most prominent technologies, both exploiting the ubiquitin-proteasome system (UPS) but differing fundamentally in their design principles and mechanisms of action [21] [39].
The Ubiquitin-Proteasome System: Cellular Foundation for Targeted Degradation
The ubiquitin-proteasome system (UPS) is the primary intracellular pathway for maintaining protein homeostasis in eukaryotic cells, responsible for degrading damaged, misfolded, and regulatory proteins [21] [40]. This highly regulated process involves a sequential enzymatic cascade:
- Ubiquitin Activation: A ubiquitin-activating enzyme (E1) activates ubiquitin in an ATP-dependent manner [21] [40].
- Ubiquitin Conjugation: The activated ubiquitin is transferred to a ubiquitin-conjugating enzyme (E2) [21] [40].
- Ubiquitin Ligation: A ubiquitin ligase (E3) recognizes specific substrate proteins and catalyzes the transfer of ubiquitin from E2 to the target protein [21] [40].
Repeated cycles of ubiquitination result in polyubiquitin chains attached to substrate proteins. While several ubiquitin linkage types exist, K48-linked chains serve as the primary signal for proteasomal recognition and degradation [21]. The 26S proteasome then recognizes these polyubiquitinated proteins, degrades them into small peptides, and recycles ubiquitin molecules [21]. With approximately 600 E3 ligases in the human genome that confer substrate specificity, the UPS provides an ideal framework for developing targeted degradation strategies [21].
Figure 1: The Ubiquitin-Proteasome System Pathway. This diagram illustrates the sequential enzymatic cascade involving E1, E2, and E3 enzymes that leads to protein ubiquitination and subsequent proteasomal degradation.
PROTACs: Heterobifunctional Inducers of Targeted Degradation
Design Principles and Mechanism of Action
PROTACs are heterobifunctional molecules consisting of three covalently linked components: a ligand that binds the protein of interest (POI), a ligand that recruits an E3 ubiquitin ligase, and a chemical linker that connects these two moieties [21] [38]. The molecular weight of PROTACs typically exceeds 700 Da, often placing them outside the conventional "rule of five" for drug-like compounds [41]. The mechanism of action involves:
- Simultaneous Binding: The PROTAC molecule simultaneously engages both the target protein and an E3 ubiquitin ligase [21] [38].
- Ternary Complex Formation: This binding induces the formation of a POI-PROTAC-E3 ternary complex [38].
- Ubiquitin Transfer: The E3 ligase catalyzes the transfer of ubiquitin chains from its associated E2 enzyme to lysine residues on the target protein [21] [38].
- Proteasomal Degradation: Polyubiquitinated proteins are recognized and degraded by the 26S proteasome [21] [38].
- Catalytic Recycling: The PROTAC molecule is released unchanged and can participate in additional degradation cycles [38].
A key advantage of PROTACs is their sub-stoichiometric, catalytic mode of action, enabling potent degradation at low concentrations [38]. The degradation efficiency depends critically on the formation of a productive ternary complex with appropriate spatial geometry, which is influenced by linker length, flexibility, and composition [38].
Historical Development and Clinical Progress
The conceptual foundation for PROTACs was established in 2001 with the development of PROTAC-1, a peptide-based molecule that recruited methionine aminopeptidase-2 (MetAP-2) to the Skp1-Cullin-F-box (SCF) ubiquitin ligase complex [21]. A significant advancement occurred in 2008 with the first small-molecule PROTAC, which utilized nonsteroidal androgen receptor and MDM2 ligands to degrade the androgen receptor (AR) [21]. The field accelerated with the identification of small-molecule ligands for E3 ligases, particularly cereblon (CRBN) in 2010 and Von Hippel-Lindau (VHL) in 2012, which now represent the most commonly utilized E3 ligases in PROTAC design [21] [41].
The clinical translation of PROTAC technology has progressed rapidly, with multiple candidates reaching advanced clinical stages:
Table 1: Clinical-Stage PROTAC Candidates
| Molecule | Target Protein | E3 Ligase | Clinical Phase | Indication |
|---|---|---|---|---|
| ARV-471 | Estrogen Receptor (ER) | CRBN | NDA/BLA | ER+/HER2− Breast Cancer |
| ARV-110 | Androgen Receptor (AR) | CRBN | Phase II | Prostate Cancer |
| ARV-766 | Androgen Receptor (AR) | CRBN | Phase II | Prostate Cancer |
| DT-2216 | Bcl-XL | VHL | Phase I/II | Hematologic Malignancies |
| NX-2127 | Bruton's Tyrosine Kinase (BTK) | CRBN | Phase I | B-cell Malignancies |
| KT-474 | IRAK4 | CRBN | Phase II | Auto-inflammatory Disorders |
Advantages and Challenges
PROTACs offer several advantages over traditional inhibitors:
- Expanded Target Range: Capable of degrading proteins without deep binding pockets [21] [38]
- Complete Function Ablation: Eliminate all protein functions rather than just inhibiting specific activities [21]
- Catalytic Efficiency: Function sub-stoichiometrically, enabling efficacy at low doses [21] [38]
- Potential Resistance Mitigation: May overcome resistance mutations that impair inhibitor binding [21]
However, PROTAC development faces significant challenges:
- Molecular Size: Large molecular weights can compromise cellular permeability and oral bioavailability [38] [41]
- Hook Effect: High concentrations can paradoxically reduce degradation efficiency by forming inactive binary complexes [38]
- Linker Optimization: Requires extensive empirical optimization of linker length and composition [38]
- Limited E3 Ligase Toolkit: Current approaches predominantly utilize CRBN and VHL, limiting tissue-specific targeting [38]
Molecular Glue Degraders: Monovalent Inducers of Protein-Protein Interactions
Design Principles and Mechanism of Action
Molecular glue degraders are small, monovalent molecules that induce novel protein-protein interactions (PPIs) between an E3 ubiquitin ligase and a target protein [39] [42]. Unlike PROTACs, molecular glues typically function by binding to a single protein (usually the E3 ligase) and subtly remodeling its surface to create a novel interface that can recognize and engage target proteins that would not normally interact with the ligase [42]. The mechanism involves:
- Surface Remodeling: The molecular glue binds to an E3 ubiquitin ligase and induces conformational changes or creates new molecular interaction surfaces [42] [40].
- Neo-Substrate Recruitment: The modified E3 ligase surface recognizes and engages target proteins (neo-substrates) that it does not normally interact with [42] [40].
- Ubiquitination and Degradation: The induced proximity leads to ubiquitination of the neo-substrate and its subsequent degradation by the proteasome [42] [40].
Molecular glues typically have lower molecular weights than PROTACs and exhibit better compliance with Lipinski's rule of five, resulting in improved cellular permeability and more favorable drug-like properties [42] [43].
Historical Development and Clinical Examples
The concept of "molecular glues" first emerged in the early 1990s with the characterization of immunosuppressants cyclosporine A (CsA) and FK506, which were found to function by forming ternary complexes between immunophilins and calcineurin [21] [43]. However, the discovery of their protein degradation capabilities came later. Key historical milestones include:
- Thalidomide and Analogs: Originally marketed for morning sickness in the 1950s, thalidomide was later discovered to act as a molecular glue that binds to cereblon (CRBN) and induces degradation of transcription factors IKZF1 and IKZF3 [21] [42]. This mechanism explains both its therapeutic effects in multiple myeloma and its teratogenicity [42].
- Auxin: The plant hormone auxin functions as a natural molecular glue that promotes the interaction between TIR1 and SCF E3 ubiquitin ligase, leading to degradation of Aux/IAA transcriptional repressors [40].
- Indisulam: This anticancer compound was discovered to induce interaction between RBM39 and DCAF15 E3 ligase, resulting in RBM39 degradation [40].
Table 2: Clinically Approved Molecular Glue Degraders
| Molecule | E3 Ligase | Target Protein(s) | Clinical Indication |
|---|---|---|---|
| Thalidomide | CRBN | IKZF1, IKZF3, others | Multiple Myeloma, Erythema Nodosum |
| Lenalidomide | CRBN | IKZF1, IKZF3, CK1α | Multiple Myeloma, Myelodysplastic Syndromes |
| Pomalidomide | CRBN | IKZF1, IKZF3 | Multiple Myeloma |
Advantages and Challenges
Molecular glue degraders offer distinct advantages:
- Favorable Drug Properties: Lower molecular weight improves cellular permeability and oral bioavailability [42] [43]
- Blood-Brain Barrier Penetration: Potential for treating CNS disorders [42]
- Targeting Undruggable Proteins: Can degrade proteins without conventional binding pockets [42] [43]
- Synthetic Tractability: Simpler structure-activity relationships compared to PROTACs [42]
However, significant challenges remain:
- Serendipitous Discovery: Most molecular glues have been discovered accidentally rather than through rational design [42] [43]
- Limited Predictive Frameworks: Difficulty in anticipating which compounds will induce productive PPIs [42]
- Specificity Concerns: Potential for off-target effects due to promiscuous degradation [42]
Comparative Analysis: PROTACs vs. Molecular Glues
Figure 2: Comparative Analysis of PROTACs and Molecular Glues. This diagram highlights the fundamental differences in structure, mechanism, and discovery approaches between these two targeted protein degradation technologies.
Table 3: Direct Comparison of Key Characteristics
| Characteristic | PROTACs | Molecular Glues |
|---|---|---|
| Molecular Structure | Heterobifunctional (three components) | Monovalent (single molecule) |
| Molecular Weight | Typically >700 Da | Typically <500 Da |
| Rule of Five Compliance | Often non-compliant | Generally compliant |
| Mechanism of Action | Simultaneous binding to POI and E3 | Primarily binds E3, induces surface remodeling |
| Design Strategy | Rational, modular design | Primarily serendipitous discovery |
| Linker Requirement | Essential component requiring optimization | No linker required |
| Cell Permeability | Challenging due to size and polarity | Favorable due to smaller size |
| Oral Bioavailability | Limited | Generally favorable |
| Discovery Approach | Structure-based design, library screening | Phenotypic screening, repurposing |
The Scientist's Toolkit: Essential Research Reagents and Methodologies
The development and characterization of targeted protein degraders require specialized reagents and experimental approaches. Key research tools include:
Table 4: Essential Research Reagents for TPD Investigations
| Reagent Category | Specific Examples | Research Application |
|---|---|---|
| Recombinant E3 Ligases | CRBN, VHL, BIRC3, BIRC7, HERC4, MGRN1, RanBP2, RNF34, TRIM37, WWP2, CBL | Screening for ternary complex formation, binding assays, structural studies |
| Target Proteins | Kinases, nuclear hormone receptors, transcription factors, epigenetic regulators | PROTAC warhead validation, degradation efficiency assessment |
| Ubiquitination System Components | E1 activating enzymes, E2 conjugating enzymes, ubiquitin | In vitro ubiquitination assays, mechanism studies |
| Functional Assay Reagents | Multi-omics profiling tools, proteasome activity assays, cellular viability assays | High-throughput screening, mechanistic validation, off-target assessment |
| Cellular Model Systems | Cancer cell lines, primary cells, engineered lines with specific mutations | Functional assessment of degradation, resistance mechanism studies |
Key Experimental Protocols
Ternary Complex Formation Assay
Purpose: To evaluate the ability of PROTACs or molecular glues to induce productive interactions between the target protein and E3 ligase.
Methodology:
- Incubate purified POI, E3 ligase, and degrader molecule under physiological conditions
- Employ techniques such as surface plasmon resonance (SPR), analytical ultracentrifugation, or HTRF (Homogeneous Time-Resolved Fluorescence) to detect complex formation
- Quantify binding affinity (Kd) and cooperativity factors to assess complex stability [42]
Cellular Degradation Efficiency Assessment
Purpose: To evaluate target protein degradation potency and kinetics in relevant cellular models.
Methodology:
- Treat cells with varying concentrations of degrader molecule for different time periods
- Lyse cells and quantify target protein levels using Western blotting or targeted proteomics
- Determine DC50 (half-maximal degradation concentration) and Dmax (maximal degradation) values
- Assess protein recovery kinetics after degrader removal [38] [41]
Ubiquitination Detection Assay
Purpose: To confirm that observed degradation occurs through the ubiquitin-proteasome pathway.
Methodology:
- Treat cells with degrader molecule in presence of proteasome inhibitor (e.g., MG132)
- Immunoprecipitate target protein under denaturing conditions
- Detect ubiquitin conjugation via anti-ubiquitin Western blotting or mass spectrometry [38]
Future Directions and Concluding Perspectives
The TPD field continues to evolve rapidly, with several promising directions emerging:
- Expanding the E3 Ligase Toolkit: Moving beyond CRBN and VHL to leverage tissue-specific and conditionally active E3 ligases for improved therapeutic windows [38]
- Lysosomal-Targeting Degraders: Developing technologies such as LYTACs, AbTACs, and AUTACs that harness lysosomal degradation pathways for extracellular proteins and organelles [21] [40]
- Rational Molecular Glue Design: Applying structural biology, computational modeling, and machine learning to transition from serendipitous discovery to predictive design [39] [43]
- Tissue-Specific Targeting: Engineering degraders with improved pharmacokinetic properties for specific tissue applications, including central nervous system disorders [38] [42]
The rise of targeted protein degradation technologies represents a fundamental paradigm shift in therapeutic intervention, moving beyond occupancy-driven pharmacology to event-driven elimination of disease-causing proteins. Both PROTACs and molecular glues have demonstrated compelling proof-of-concept in clinical settings, validating the UPS as a viable framework for therapeutic development. As these technologies continue to mature, they promise to significantly expand the druggable proteome and provide new treatment options for diseases previously considered intractable to conventional therapeutic approaches [38] [39].
Historical Perspective: The Foundation of the Ubiquitin-Proteasome System
The development of proteasome inhibitors for multiple myeloma is a premier example of how fundamental biological discovery can revolutionize clinical practice. This journey began with the elucidation of the ubiquitin-proteasome system (UPS), the primary pathway for selective intracellular protein degradation in eukaryotic cells. For much of the 20th century, intracellular proteins were believed to be largely long-lived. This paradigm was fundamentally overturned in the 1980s through complementary discoveries by the laboratories of Avram Hershko (Technion, Haifa, Israel) and Alexander Varshavsky (then at MIT, Cambridge, USA) [2].
The Hershko laboratory, using biochemical fractionation and enzymology in reticulocyte extracts, made the seminal discovery that a small protein, initially termed APF-1 (ATP-dependent proteolytic factor 1), was covalently conjugated to target proteins prior to their degradation [2]. APF-1 was soon identified as ubiquitin [2]. Hershko and his colleagues, including student Aaron Ciechanover and collaborator Irwin Rose, subsequently identified and characterized the enzymatic cascade—comprising E1 (ubiquitin-activating enzyme), E2 (ubiquitin-carrier protein), and E3 (ubiquitin-protein ligase) enzymes—responsible for ubiquitin conjugation [2]. Their work described the core biochemical mechanism: E1 activates ubiquitin in an ATP-dependent manner, E2 enzymes carry the activated ubiquitin, and E3 ligases confer substrate specificity, facilitating the transfer of ubiquitin to target proteins [2]. This multi-ubiquitin chain then serves as a recognition signal for degradation by a large, ATP-dependent protease, later characterized as the 26S proteasome [2].
Concurrently, Varshavsky's laboratory discovered the profound biological functions of this system. Through genetic, biochemical, and cell biological studies, they demonstrated that the UPS was not merely a cellular "garbage disposal" but was essential for cell viability and played critical roles in regulating the cell cycle, DNA repair, transcriptional regulation, and stress responses [2]. They deciphered the source of the system's specificity by identifying degradation signals (degrons) in short-lived proteins and discovered key mechanistic attributes like the polyubiquitin chain [2]. These foundational discoveries, which earned Hershko, Ciechanover, and Rose the 2004 Nobel Prize in Chemistry, revealed that "the control through regulated protein degradation rivals, and often surpasses in significance, the classical regulation through transcription and translation" [2]. This radical new understanding of intracellular logic provided the essential scientific basis for targeting the proteasome as a therapeutic strategy in cancer.
Proteasome Inhibitors in Multiple Myeloma: Clinical Applications and Workflows
The translation of this basic science into therapy was driven by the observation that multiple myeloma (MM) cells are exquisitely sensitive to proteasome inhibition [44]. This sensitivity is attributed to their high rate of protein production, particularly immunoglobulins, which creates immense stress on the endoplasmic reticulum. Proteasome inhibition disrupts protein homeostasis, leading to the accumulation of misfolded proteins, endoplasmic reticulum stress, and ultimately, apoptosis of the malignant plasma cells [44].
Key Clinical Use Cases and Therapeutic Regimens
Proteasome inhibitors (PIs) have become a cornerstone of multiple myeloma treatment, with applications across the entire disease continuum [45] [44]. The following table summarizes the primary clinical use cases for these agents as of 2025.
Table 1: Key Clinical Use Cases for Proteasome Inhibitors in Multiple Myeloma
| Use Case | Description | Example Regimens & Clinical Impact |
|---|---|---|
| First-Line Treatment | Used as initial therapy for newly diagnosed MM (NDMM) to rapidly reduce tumor burden [45]. | Often combined with immunomodulatory drugs (IMiDs) and corticosteroids. Bortezomib-based regimens improve progression-free survival (PFS) by ~30% vs. chemotherapy alone [45]. |
| Maintenance Therapy | Administered post-remission to prolong response and prevent relapse [45]. | Ongoing use of bortezomib demonstrated a 20% increase in PFS over observation alone. Key metric is extended time to progression [45]. |
| Relapsed/Refractory Disease | Treatment for patients who have relapsed or become resistant to initial therapy [45] [46]. | Carfilzomib or ixazomib show efficacy in overcoming resistance, with response rates of 40-50% in refractory cases [45] [46]. |
| Combination Therapies | PIs combined with other drug classes to enhance efficacy [45] [44]. | Bortezomib + daratumumab (anti-CD38 mAb) leads to response rates >70% [45]. Combinations with IMiDs, histone deacetylase inhibitors are also standard [44]. |
| Palliative Care | Used in advanced stages for symptom control and quality of life improvement [45]. | Alleviates bone pain, anemia, and renal impairment associated with MM, providing meaningful symptom control [45]. |
The clinical workflow for integrating these agents into patient care involves careful monitoring and management. The diagram below outlines a generalized treatment pathway for a newly diagnosed multiple myeloma patient, incorporating the key use cases from above.
Generalized MM Treatment Pathway
Currently Approved Proteasome Inhibitors and Their Profiles
Three proteasome inhibitors have received widespread approval for the treatment of multiple myeloma, each with distinct characteristics [44] [46]. The following table provides a detailed comparison of these agents, including their mechanisms, administration routes, and key efficacy data.
Table 2: Approved Proteasome Inhibitors for Multiple Myeloma: A Comparative Profile
| Agent (Brand Name) | Key Characteristics & Generation | Mechanistic Profile | Approved Indications Context | Notable Clinical Trial Efficacy Data |
|---|---|---|---|---|
| Bortezomib (Velcade) | First-in-class, reversible PI [46]. | Boronate-based inhibitor; primarily inhibits chymotrypsin-like activity of proteasome [44]. | NDMM and RRMM [46]. Backbone of many first-line regimens [45]. | In transplant-eligible NDMM: VD → PFS: 36 months; VTD → CR: 35% pre-transplant [46]. |
| Carfilzomib (Kyprolis) | Second-generation, irreversible PI [46]. | Epoxyketone-based inhibitor; binds irreversibly to chymotrypsin-like site [44]. | RRMM (monotherapy and combination) [46]. | ASPIRE Trial (KRd vs Rd): Median OS: 48.3 vs 40.4 mos; ORR: 87.1% vs 66.7% [46]. |
| Ixazomib (Ninlaro) | First oral, reversible PI [47] [46]. | Boronate-based, reversible inhibitor [44]. | RRMM in combination [46]. Offers patient convenience [45]. | TOURMALINE-MM1: PFS improvement vs placebo (20.6 vs 14.7 mos) in RRMM [46]. |
Detailed Experimental and Clinical Methodology
This section outlines the core experimental approaches used to investigate proteasome inhibitors, from basic mechanistic studies to the clinical trials that establish their therapeutic value.
Core Experimental Protocol: Assessing PI Mechanism and EfficacyIn Vitro
The following workflow details a standard methodology for evaluating the biological effects of proteasome inhibitors on multiple myeloma cell lines in a research setting.
In Vitro PI Testing Workflow
Step-by-Step Protocol:
- Cell Culture and Preparation: Human multiple myeloma cell lines (e.g., RPMI8226, U266) are maintained in appropriate media (e.g., RPMI-1640 with 10% FBS) under standard conditions (37°C, 5% CO₂). Cells are seeded at a standardized density (e.g., 1-5 x 10⁴ cells/well) in multi-well plates for assays [44].
- Compound Treatment: Proteasome inhibitor stocks are prepared in suitable vehicles (e.g., DMSO for bortezomib) and diluted to a range of final concentrations (e.g., 1 nM to 100 μM) in culture media. Vehicle controls are essential. Treatment is typically performed in triplicate or quadruplicate.
- Incubation: Cells are incubated with the compounds for a predetermined period, usually 24 to 72 hours, to capture both short-term (e.g., proteasome inhibition, initial protein accumulation) and long-term effects (e.g., apoptosis, reduced viability).
- Downstream Analysis:
- Cell Viability Assay: Viability is quantified using colorimetric assays like MTT or WST-1, which measure metabolic activity. Results are used to generate dose-response curves and calculate IC₅₀ values (concentration that inhibits 50% of viability) [44].
- Apoptosis Assay: Apoptosis is detected by staining cells with Annexin V-FITC and Propidium Iodide (PI) followed by analysis via flow cytometry. This distinguishes early apoptotic (Annexin V+/PI-), late apoptotic/necrotic (Annexin V+/PI+), and viable cells (Annexin V-/PI-) [44].
- Protein Accumulation Analysis: Western blotting is performed to detect the accumulation of proteasome substrates, such as the tumor suppressor p53 or the NF-κB inhibitor IκBα, providing direct evidence of proteasome inhibition [44].
- Proteasome Activity Assay: Cell lysates are incubated with fluorogenic peptides specific for different proteasome catalytic activities (e.g., chymotrypsin-like, trypsin-like). Cleavage releases a fluorescent group, the intensity of which is proportional to proteasome activity [44].
- Data Analysis: IC₅₀ values are calculated from dose-response curves using non-linear regression. Statistical significance between treatment groups and controls is determined using tests like Student's t-test or ANOVA.
Clinical Trial Framework: Evaluating PIs in Patients
The efficacy and safety of proteasome inhibitors in humans are established through phased clinical trials. Key trial designs that have shaped the MM treatment landscape include:
- PERSEUS Trial (NCT03710603): A phase III study for transplant-eligible NDMM patients comparing D-VRd (daratumumab, bortezomib, lenalidomide, dexamethasone) followed by daratumumab/lenalidomide maintenance versus VRd followed by lenalidomide maintenance. This trial established D-VRd as a superior frontline option, showing improved PFS and higher rates of minimal residual disease (MRD) negativity across all risk groups [47].
- IMROZ Trial: A phase III study leading to the 2025 approval of isatuximab (SARCLISA) in combination with VRd for transplant-ineligible NDMM. The regimen demonstrated a 40% reduction in the risk of disease progression or death compared to VRd alone [47].
- ASPIRE Trial: A phase III study in relapsed/refractory MM comparing KRd (carfilzomib, lenalidomide, dexamethasone) to Rd (lenalidomide, dexamethasone). KRd significantly improved overall survival (median OS: 48.3 vs. 40.4 months) and overall response rate (87.1% vs. 66.7%) [46].
- CARTITUDE-4 Trial (NCT04181827): While evaluating a CAR-T therapy (cilta-cel), this phase III trial in lenalidomide-refractory MM provides context for PIs, showing that 69% of evaluable patients achieved MRD negativity by day 56, highlighting the deep response benchmarks in modern therapy [47].
The Scientist's Toolkit: Key Research Reagents and Materials
Research into the ubiquitin-proteasome system and the development of proteasome inhibitors relies on a standardized set of reagents and tools. The following table catalogs essential items for researchers in this field.
Table 3: Essential Research Reagents for Ubiquitin-Proteasome System and PI Studies
| Reagent/Material | Function/Description | Primary Research Application |
|---|---|---|
| Fluorogenic Proteasome Substrates (e.g., Suc-LLVY-AMC) | Peptide substrates whose fluorescence is unmasked upon proteasomal cleavage. AMC (7-amino-4-methylcoumarin) is a common fluorophore. | Direct measurement of chymotrypsin-like (and other) proteasome activities in cell lysates or purified proteasomes [44]. |
| Anti-Ubiquitin Antibodies (Monoclonal/Polyclonal) | Immunoreagents for detecting ubiquitin and ubiquitinated proteins. | Western blotting to visualize accumulation of polyubiquitinated proteins; immunofluorescence; immunohistochemistry [2] [44]. |
| Anti-Specific Protein Antibodies (e.g., anti-IκBα, anti-p53) | Antibodies against known short-lived proteasome substrates. | Western blotting to provide indirect, but specific, evidence of proteasome inhibition in cells [44]. |
| E1, E2, E3 Enzymes (Purified, Recombinant) | Core components of the ubiquitination cascade for biochemical reconstitution. | In vitro ubiquitination assays to study the enzymatic cascade or to screen for inhibitors of specific E3 ligases [2] [7]. |
| Human Multiple Myeloma Cell Lines (e.g., RPMI8226, U266, MM.1S) | Immortalized cell lines derived from human multiple myeloma patients. | In vitro models for screening PI efficacy, studying mechanisms of action and resistance, and testing combination therapies [44]. |
| Annexin V / Propidium Iodide (PI) Kit | Standard kit for detecting phosphatidylserine externalization (Annexin V) and membrane integrity (PI). | Flow cytometry-based quantification of apoptosis and necrosis induced by PIs in MM cell lines [44]. |
| Bortezomib, Carfilzomib, MG132 | Tool compounds: first-generation and commonly used experimental PIs. | Used as positive controls in experiments and to benchmark the activity of novel investigational inhibitors [44] [46]. |
The field of proteasome inhibition in multiple myeloma continues to evolve rapidly. Key future directions focus on overcoming resistance, improving patient convenience, and developing more targeted therapeutic strategies.
- Next-Generation Inhibitors and Novel Targets: Research is ongoing to develop next-generation PIs with improved safety profiles, particularly reduced neurotoxicity [45]. Beyond the proteasome itself, the drug discovery pipeline is targeting other components of the ubiquitin system. Orphan Drug Designation was granted in 2025 for OPN-6602, an oral small molecule inhibitor of EP300 and CBP, for relapsed/refractory MM, highlighting this trend [47].
- Personalized and Biomarker-Driven Therapy: By 2025, the use of PIs is expected to become more personalized, with biomarker-driven approaches guiding therapy choices to maximize efficacy for individual patients [45].
- Expansion of Combination and Immunotherapy Regimens: The success of combining PIs with other drug classes continues to expand. The integration of PIs with monoclonal antibodies (e.g., daratumumab, isatuximab) has become standard, and combinations with emerging immunotherapies like CAR-T cells (e.g., cilta-cel) and bispecific antibodies are being actively explored to deepen and prolong responses [45] [47].
- Formulation Advances: The development of oral proteasome inhibitors like ixazomib aims to improve patient convenience and adherence, a significant shift from intravenous/subcutaneous administration [45] [46].
In conclusion, the journey of proteasome inhibitors from a fundamental discovery in the ubiquitin-proteasome system to a backbone of multiple myeloma therapy is a landmark achievement in translational medicine. The continued refinement of these agents, their intelligent integration into combination regimens, and the exploration of novel targets within the UPS promise to further expand this essential arsenal, ultimately improving outcomes for patients with this challenging hematologic malignancy.
The ubiquitin-proteasome system (UPS), a fundamental physiological process for controlled protein degradation, has been transformed from a basic biological concept into a pivotal therapeutic platform. This transformation is epitomized by the strategic hijacking of E3 ubiquitin ligases—the substrate-recognition components of the UPS—for targeted protein destruction. Among over 600 human E3 ligases, Cereblon (CRBN), Von Hippel-Lindau (VHL), and Inhibitor of Apoptosis Proteins (IAPs) have emerged as the most extensively utilized ligases in novel therapeutic modalities. The advent of proteolysis-targeting chimeras (PROTACs) and related molecular glue degraders represents a paradigm shift in drug discovery, enabling the direct degradation of disease-causing proteins previously considered "undruggable." This whitepaper provides a comprehensive technical analysis of CRBN, VHL, and IAPs—detailing their physiological functions, mechanistic roles in targeted protein degradation, experimental methodologies for their investigation, and their growing impact on therapeutic development. As the field advances beyond the limitations of traditional occupancy-based inhibitors, harnessing the diverse E3 ligase family promises to unlock unprecedented opportunities for precision medicine across oncology, inflammatory disorders, and beyond.
The ubiquitin-proteasome system represents a sophisticated hierarchical enzymatic cascade that governs controlled protein degradation in eukaryotic cells. This process involves three key enzyme classes: E1 (activating), E2 (conjugating), and E3 (ligating) enzymes. E3 ubiquitin ligases serve as the critical substrate-recognition components that confer specificity to the system by facilitating the transfer of ubiquitin from E2 enzymes to specific target proteins. The human genome encodes approximately 600 E3 ligases, which are categorized into distinct families based on their structural features and mechanisms, with RING (Really Interesting New Gene) and HECT (Homologous to E6AP C-Terminus) domains representing the primary classes.
The journey from the initial discovery of the UPS to its therapeutic application has spanned decades of fundamental research. The 2004 Nobel Prize in Chemistry awarded for the discovery of ubiquitin-mediated protein degradation underscored the system's fundamental biological importance. More recently, the field has witnessed the intentional hijacking of this natural cellular machinery for therapeutic purposes, primarily through bifunctional PROTAC molecules and monovalent molecular glues. These technologies create a synthetic ternary complex between an E3 ligase and a protein of interest (POI), leading to polyubiquitination and subsequent proteasomal degradation of the POI. This represents a revolutionary shift from traditional inhibition to complete protein removal, offering potential advantages in potency, duration of effect, and ability to target proteins without conventional binding pockets.
E3 Ligase Deep Dive: CRBN, VHL, and IAPs
Cereblon (CRBN)
Physiological Function and Discovery Timeline: Cereblon (CRBN) functions as a substrate receptor within the CRL4^CRBN E3 ubiquitin ligase complex, which consists of CUL4, RBX1, DDB1, and CRBN. Initially identified for its role in ion channel regulation and mental retardation when mutated, CRBN gained profound therapeutic significance when identified as the primary target of thalidomide and its analogs (immunomodulatory imide drugs [IMiDs]) [48]. The discovery that IMiDs reprogram CRBN to target novel neo-substrates for degradation explained both the efficacy (degradation of Ikaros, Aiolos, CK1α) and teratogenicity of these agents. Beyond IMiD-induced degradation, recent research has revealed that CRBN also participates in physiological protein homeostasis, including Wnt signaling pathway regulation where it mediates the degradation of Casein kinase 1α (CK1α) in response to Wnt stimulation [49].
Structural Characteristics and Ligand Binding: CRBN contains a three-dimensional pocket that accommodates the glutarimide moiety of IMiDs through critical hydrogen bonds with His380 and Trp382 and van der Waals interactions with a hydrophobic pocket composed of Phe404, Trp388, and Trp380 [50]. The phthalimide ring of IMiDs projects outward from this binding pocket, enabling solvent exposure that facilitates linker attachment for PROTAC design without significant affinity loss. This structural feature has been extensively exploited in PROTAC development, making CRBN the most commonly hijacked E3 ligase currently.
Table 1: Key Small Molecule Ligands for CRBN
| Ligand Name | Binding Affinity (KD) | Key Structural Features | Applications |
|---|---|---|---|
| Thalidomide | Not specified | Phthalimide + glutarimide rings; chiral center | First-generation IMiD; MM and ENL |
| Lenalidomide | Not specified | Amino group at position 4 of phthaloyl ring; carbonyl removal | Multiple myeloma; MDS |
| Pomalidomide | Not specified | 3-aminothalidomide analog | Multiple myeloma |
| Analog 4 | 55 nM | Modified phthalimide region | PROTAC development |
| Analog 5 | 549 nM | Modified phthalimide region | PROTAC development |
| Analog 6 | 111 nM | Modified phthalimide region | PROTAC development |
| Compound 7 | <10 μM | Piperidine-2,6-dione derivative | Degronimer development |
| TD-106 | Not specified | Aminobenzotriazino glutarimide | Enhanced IKZF1/3 degradation |
Therapeutic Applications and Notable Degraders: CRBN-based degraders have demonstrated remarkable success in hematological malignancies. ARV-825 and dBET1, which conjugate thalidomide analogs to the BET inhibitor JQ1, achieved nanomolar-range degradation of BRD4 and showed potent anti-leukemic activity [50]. The degradation efficiency of CRBN-based PROTACs depends heavily on the specific IMiD analog employed, linker composition, and attachment chemistry. Beyond oncology, CRBN recruiters are being explored for viral protein degradation (e.g., DGY-08-097 for HCV NS3/4A protease) and neurological disorders, highlighting the versatility of this E3 ligase platform.
Von Hippel-Lindau (VHL)
Physiological Function and Disease Association: The VHL tumor suppressor protein serves as the substrate recognition component of the CUL2-RBX1-ELOB-ELOC E3 ubiquitin ligase complex (CRL2^VHL). Its best-characterized physiological function involves oxygen-sensing regulation through ubiquitination and degradation of hypoxia-inducible factors (HIF-1α and HIF-2α). Under normoxic conditions, VHL recognizes hydroxylated HIF-α, targeting it for proteasomal degradation. In VHL disease, an autosomal dominant cancer predisposition syndrome, germline mutations disrupt this function, leading to HIF-α accumulation and driving tumorigenesis in multiple organs [51]. Additionally, biallelic VHL mutations cause familial erythrocytosis type 2 (ECYT2), characterized by elevated red blood cell production due to dysregulated hypoxia response [52].
Structural Characteristics and Ligand Binding: VHL forms a stable complex with elongin B, elongin C, and cullin-2. Small-molecule VHL ligands, such as VH298 and related compounds, mimic the hydroxyproline residue of HIF-1α, engaging key residues in the VHL binding pocket. These interactions primarily involve hydrogen bonding with His115, Asn78, and His110 of VHL. The co-crystal structure of VHL complexed with HIF-1α peptide revealed that the 4-hydroxyproline inserts into a deep binding pocket, while the surrounding peptide sequence provides additional interaction points that enhance binding affinity. Structure-based drug design has yielded potent, drug-like VHL ligands with favorable pharmacokinetic properties suitable for PROTAC development.
Therapeutic Applications and Notable Degraders: VHL recruiters have been successfully employed in PROTACs targeting various oncoproteins, nuclear receptors, and transcription factors. A prominent example, MZ1, achieves selective degradation of BRD4 over other BET family members, demonstrating that E3 ligase choice can influence isoform selectivity [53]. VHL-based PROTACs have also shown efficacy against validated targets such as the androgen receptor (AR), estrogen receptor (ER), and receptor tyrosine kinases. Compared to CRBN-based degraders, VHL recruiters may offer advantages in certain cellular contexts due to differential E3 ligase expression patterns and ternary complex formation kinetics.
Inhibitors of Apoptosis Proteins (IAPs)
Physiological Function and Family Diversity: IAPs comprise a family of eight anti-apoptotic proteins (NAIP, c-IAP1, c-IAP2, XIAP, survivin, BRUCE, ML-IAP, and ILP2) characterized by the presence of baculoviral IAP repeat (BIR) domains [54]. While initially studied for caspase inhibition and apoptosis regulation, several IAPs (particularly cIAP1, XIAP, and cIAP2) function as RING-domain containing E3 ubiquitin ligases. Beyond apoptosis, IAPs regulate inflammatory signaling, innate immunity, and cell migration. For instance, cIAP1/2 modulate canonical and non-canonical NF-κB pathways by controlling RIPK1 and NIK stability, respectively [54].
Novel Roles in Protein Degradation: Recent research has revealed non-apoptotic substrates for IAP-mediated ubiquitination. Specifically, cIAP1 and XIAP directly ubiquitinate the RhoGTPase Rac1 at lysine 147, targeting it for proteasomal degradation and thereby influencing cell migration and invasion [55]. This degradation occurs in a nucleotide-independent manner and regulates Rac1 stability under various conditions, including CNF1 toxin treatment and RhoGDI1 depletion. Unlike HACE1 (another Rac1 E3 ligase that prefers GTP-bound Rac1), IAPs interact with Rac1 irrespective of its activation status, suggesting distinct regulatory mechanisms [55].
Therapeutic Targeting Approaches: IAPs are exploited in PROTAC design primarily through SMAC (Second Mitochondria-derived Activator of Caspases) mimetics, which mimic the endogenous IAP antagonist SMAC/DIABLO. These small molecules bind to the BIR domains of IAPs, potentially enabling PROTAC-mediated recruitment. Additionally, IAP antagonists induce rapid auto-ubiquitination and degradation of cIAP1/2, leading to non-canonical NF-κB activation and TNF-α-mediated apoptosis in certain cancer contexts. The dual functionality of IAPs—as both E3 ligases for degradation and apoptosis regulators—creates unique opportunities and challenges for therapeutic development.
Table 2: Comparative Analysis of Key E3 Ligases in TPD
| Parameter | CRBN | VHL | IAPs |
|---|---|---|---|
| E3 Complex | CRL4^CRBN | CRL2^VHL | Multiple independent members |
| Native Substrates | IKZF1/3, CK1α, others | HIF-1α, HIF-2α | Caspases, RIPK1, NIK, Rac1 |
| Common Ligands | IMiDs (thalidomide, lenalidomide, pomalidomide) | VH032 derivatives, VH298 | SMAC mimetics (e.g., LCL161) |
| Binding Domain | Glutarimide binding pocket | β-domain hydroxyproline pocket | BIR domains |
| Key Interactions | His380, Trp382 (H-bonds); hydrophobic pocket | His115, Asn78 (H-bonds) | AVPI binding groove |
| Tissue Expression | Ubiquitous | Ubiquitous | Variable (often elevated in cancers) |
| Clinical Stage | Phase III (multiple PROTACs) | Phase I/II | Preclinical/early clinical |
| Key Advantages | Extensive ligand optimization, oral bioavailability | Well-characterized ligands, selectivity potential | Apoptosis sensitization |
| Key Limitations | Teratogenicity risk, resistance emergence | Limited ligand diversity | Complex biology with multiple family members |
Experimental Protocols and Methodologies
Assessing E3 Ligase-Substrate Interactions
Co-immunoprecipitation (Co-IP) Assays: To validate physiological E3 ligase-substrate relationships, Co-IP remains a foundational technique. For investigating Wnt-induced CRBN-CK1α interaction [49]: (1) Culture HEK293T cells and treat with recombinant Wnt3a ligand (100 ng/mL) for specified durations; (2) Lyse cells in NP-40 buffer supplemented with protease and phosphatase inhibitors; (3) Pre-clear lysates with protein A/G beads; (4) Incubate with anti-CRBN antibody or species-matched IgG control overnight at 4°C; (5) Capture immune complexes with protein A/G beads; (6) Wash beads extensively and elute with Laemmli buffer; (7) Analyze by SDS-PAGE and immunoblotting for CRBN, CK1α, and destruction complex components (APC, Axin1).
In Vitro Ubiquitination Assays: These reconstituted systems establish direct E3 ligase activity toward substrates [49]: (1) Purify CRBN complex from Wnt-treated and control cells via immunoprecipitation; (2) Combine recombinant substrate (CK1α), E1 enzyme (100 nM), E2 enzyme (UbcH5a, 200 nM), ubiquitin (50 μM), and ATP regeneration system in reaction buffer; (3) Initiate reaction by adding purified CRBN complex; (4) Incubate at 30°C for 60-90 minutes; (5) Terminate reaction with SDS sample buffer; (6) Detect ubiquitinated species by immunoblotting with anti-ubiquitin antibody or substrate-specific antibody.
Evaluating Protein Degradation Kinetics
Cycloheximide Chase Assays: To measure protein half-life and degradation kinetics [49]: (1) Culture cells and pre-treat with Wnt3a or vehicle control; (2) Add cycloheximide (100 μg/mL) to inhibit new protein synthesis; (3) Harvest cells at multiple time points (0, 1, 2, 4, 8 hours) post-cycloheximide treatment; (4) Prepare lysates and quantify target protein levels by immunoblotting; (5) Normalize to loading controls (α-Tubulin, GAPDH); (6) Calculate half-life using nonlinear regression of protein abundance versus time.
PROTAC Degradation Efficiency Assessment: To characterize novel PROTAC molecules [50] [53]: (1) Seed appropriate cell line expressing target protein; (2) Treat with serial dilutions of PROTAC (typically 1 nM-10 μM) for 16-24 hours; (3) Prepare whole-cell lysates; (4) Analyze target protein levels by quantitative immunoblotting or cellular thermal shift assays; (5) Determine DC50 (half-maximal degradation concentration) and Dmax (maximal degradation) using nonlinear curve fitting; (6) Assess specificity through proteomics analysis or immunoblotting for related proteins.
Ternary Complex Analysis
Surface Plasmon Resonance (SPR): SPR measures real-time binding kinetics for ternary complex formation [50]: (1) Immobilize E3 ligase or target protein on CMS sensor chip; (2) Pre-incubate soluble binding partner with varying PROTAC concentrations; (3) Inject pre-formed complexes over immobilized ligand; (4) Monitor association and dissociation phases; (5) Analyze sensorgrams to calculate cooperative binding factors.
Cellular Thermal Shift Assay (CETSA): CETSA validates target engagement in cellular contexts [53]: (1) Treat cells with PROTAC or vehicle control; (2) Heat aliquots of cell suspension to different temperatures (37-65°C); (3) Separate soluble protein from aggregates; (4) Detect remaining soluble target protein by immunoblotting; (5) Calculate thermal stabilization (ΔTm) induced by PROTAC binding.
Visualization of E3 Ligase Mechanisms and Experimental Workflows
Diagram 1: E3 ligase mechanisms in targeted protein degradation
Diagram 2: Experimental workflow for E3 ligase validation
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Research Reagent Solutions for E3 Ligase Studies
| Reagent Category | Specific Examples | Function/Application | Key Considerations |
|---|---|---|---|
| E3 Ligase Ligands | Lenalidomide, Pomalidomide (CRBN); VH032, VH298 (VHL); SMAC mimetics (IAPs) | PROTAC development; molecular glue degraders; competition studies | Binding affinity, cell permeability, solubility, off-target effects |
| Proteasome Inhibitors | MG132, Bortezomib, Carfilzomib | Validate proteasome-dependent degradation; distinguish from autophagy | Cytotoxicity at prolonged exposures; potential effects on ubiquitination |
| Lysosome Inhibitors | Bafilomycin A1, Chloroquine | Rule out lysosomal degradation pathways | Specificity for lysosomal vs. proteasomal inhibition |
| Protein Synthesis Inhibitors | Cycloheximide, Anisomycin | Measure protein half-life in chase assays | Concentration optimization to balance complete inhibition and cytotoxicity |
| Recombinant Ligands | Wnt3a (CRBN pathway activation); EGF (signaling modulation) | Pathway-specific regulation of E3 ligase activity | Bioactivity validation; appropriate controls (e.g., FZD8-CRD for Wnt) |
| E3 Ligase Modulators | MLN4924 (NEDD8 activation inhibitor) | Pan-E3 ligase inhibition; validate E3 dependence | Broad-spectrum effects require careful interpretation |
| CRISPR/siRNA Tools | CRBN, VHL, XIAP, cIAP1/2 knockdown/knockout | Genetic validation of E3 ligase requirements | Off-target effects; compensatory mechanisms; complete vs. partial knockdown |
| Ubiquitination Assay Components | Recombinant E1, E2s, ubiquitin, ATP regeneration system | In vitro ubiquitination validation | E2 specificity; reaction optimization; positive controls |
| Detection Antibodies | Anti-ubiquitin, anti-HA-ubiquitin, E3-specific antibodies, substrate antibodies | Immunoblotting, immunofluorescence, Co-IP | Specificity validation; species compatibility; application suitability |
| Cellular Models | HEK293T (ubiquitination assays); HCT116, MIA PaCa-2 (cancer models) | Context-specific E3 ligase function | Endogenous E3 ligase expression; pathway activity; genetic background |
The strategic hijacking of E3 ubiquitin ligases—particularly CRBN, VHL, and IAPs—represents a transformative approach in therapeutic development that builds upon decades of fundamental research into the ubiquitin-proteasome system. The current landscape is dominated by CRBN and VHL recruiters, with multiple PROTACs advancing through clinical trials and demonstrating compelling proof-of-concept in challenging disease contexts. However, the field is rapidly evolving to address key limitations, including on-target off-tissue toxicity, resistance mechanisms, and the restricted repertoire of hijackable E3 ligases.
Future directions will likely focus on several critical areas: First, expanding the E3 ligase toolbox beyond CRBN and VHL to include cell-type and tissue-specific ligases that could enable precise spatial control of protein degradation. Second, developing advanced delivery technologies to overcome pharmacological challenges associated with large bifunctional molecules. Third, elucidating and engineering the structural principles governing ternary complex formation to optimize degradation efficiency and selectivity. Finally, integrating targeted protein degradation with other therapeutic modalities to address complex disease pathologies through multi-target approaches.
As our fundamental understanding of E3 ligase biology deepens and technological innovations continue to emerge, hijacking the ubiquitin-proteasome system promises to unlock new dimensions in therapeutic intervention across diverse disease areas. The journey from basic mechanistic discoveries to clinical applications exemplifies the power of fundamental biological research to fuel therapeutic breakthroughs, establishing targeted protein degradation as a cornerstone of next-generation precision medicines.
Overcoming Hurdles: Challenges in UPS-Targeted Drug Development
Addressing Drug Resistance to Proteasome Inhibitors in Cancer Therapy
The discovery of the ubiquitin-proteasome system (UPS) marked a paradigm shift in our understanding of cellular protein homeostasis. The groundbreaking work of Aaron Ciechanover, Avram Hershko, and Irwin Rose, recognized with the 2004 Nobel Prize in Chemistry, unveiled the intricate enzymatic cascade that tags proteins for degradation with ubiquitin, designating them for destruction by the proteasome [22]. This system is the central hub of non-lysosomal cellular proteolysis, mediating essential processes such as cell cycle control, immune response, and apoptosis [56]. The 26S proteasome, a 2.5 megadalton complex, consists of a 20S core particle capped by one or two 19S regulatory particles. The core particle's proteolytic activity is housed within three specific β-subunits: β5 (chymotrypsin-like, CT-L), β2 (trypsin-like, T-L), and β1 (caspase-like, C-L) [56] [57]. The realization that malignant cells are more reliant on proteasome function for their survival and proliferation provided the rationale for targeting the UPS in cancer therapy [56] [58]. This led to the development of proteasome inhibitors (PIs), which have transformed the treatment landscape for hematological malignancies like multiple myeloma (MM) and mantle cell lymphoma (MCL) [56] [59]. However, the emergence of drug resistance has limited their efficacy, prompting intensive research into the underlying mechanisms and strategies to overcome them.
The Problem of Resistance to Proteasome Inhibitors
Despite the success of PIs, a significant number of patients exhibit intrinsic resistance or develop acquired resistance during treatment, leading to disease relapse [56] [59]. Resistance is a multifaceted phenomenon driven by a complex interplay of cellular adaptations.
Table 1: Clinically Approved Proteasome Inhibitors and Their Profiles
| Inhibitor | Electrophile | Reversibility | Primary Subunit Target | Key Clinical Indications |
|---|---|---|---|---|
| Bortezomib (Velcade) | Boronate | Reversible | β5 / CT-L | Multiple Myeloma, Mantle Cell Lymphoma |
| Carfilzomib (Kyprolis) | Epoxyketone | Irreversible | β5 / CT-L | Multiple Myeloma |
| Ixazomib (Ninlaro) | Boronate | Reversible | β5 / CT-L | Multiple Myeloma |
Molecular Mechanisms of Proteasome Inhibitor Resistance
Resistance to PIs arises through several distinct, and often co-occurring, molecular mechanisms:
- Target Alteration: Cancer cells can acquire mutations in the gene encoding the PSMB5 subunit, which is the primary target of bortezomib and carfilzomib [56] [60]. These mutations can reduce the binding affinity of the drug. Furthermore, cells can upregulate the expression of proteasome subunits, increasing the total proteasome capacity and overwhelming the inhibitory capacity of the drug [56] [58].
- Proteasome Subunit Switching: Normal cells express constitutive proteasome subunits (β1, β2, β5). Upon exposure to cytokines like interferon-gamma, cells can express immunoproteasome subunits (β1i, β2i, β5i). The upregulation of immunoproteasomes has been implicated in resistance, as these subunits can have different catalytic properties and inhibitor sensitivities [57] [59].
- Activation of Compensatory Protein Clearance Pathways: When the proteasome is inhibited, cells activate alternative pathways to manage protein overload. Autophagy is a key compensatory mechanism that can be upregulated to sustain cell survival, and its inhibition can re-sensitize resistant cells to PIs [59].
- Adaptations in the Unfolded Protein Response (UPR) and ER Stress: PIs cause an accumulation of misfolded proteins, triggering ER stress and the UPR—a pro-survival signaling cascade. Resistant cells can develop adaptations that enhance their ability to manage this stress, for instance, by upregulating molecular chaperones, thereby avoiding the transition from a pro-survival to a pro-apoptotic UPR [58].
- The Role of the Bone Marrow Microenvironment (BMME): The bone marrow niche provides a protective sanctuary for cancer cells. Stromal cells in the BMME secrete survival factors and cytokines that activate pro-survival signaling pathways in tumor cells, such as NF-κB and PI3K/Akt, conferring direct resistance to PIs [60] [59].
Table 2: Key Mechanisms of Resistance and Associated Evidence
| Resistance Mechanism | Molecular Alteration / Process | Experimental / Clinical Evidence |
|---|---|---|
| Target Mutation & Overexpression | PSMB5 gene mutations; Overexpression of β5 subunit | Acquired in bortezomib-resistant cell lines [56] [58]. |
| Proteasome Overload | Upregulation of proteasome content and activity | Observed in patients with advanced, drug-resistant metastatic breast or colon cancers [61]. |
| Activation of Bypass Pathways | Induction of Autophagy; Aggresome formation | Inhibition of autophagy restores PI sensitivity in vitro [59]. |
| Microenvironment Protection | Stroma-mediated activation of NF-κB, IL-6, and other survival signals | Co-culture with stromal cells protects myeloma cells from bortezomib-induced apoptosis [60] [59]. |
| Enhanced Drug Efflux | Upregulation of P-glycoprotein (ABCB1) | Contributes to multidrug resistance phenotypes, though its role in PI-specific resistance is less clear [60] [59]. |
Diagram 1: Key cellular adaptations driving proteasome inhibitor resistance.
Experimental Approaches for Investigating Resistance
Understanding and overcoming PI resistance requires a multifaceted experimental approach, ranging from high-throughput screening to detailed molecular biology techniques.
Detecting Protein Damage and the Cellular Response
A recent study revealed that a broad spectrum of anticancer drugs induces widespread protein damage, triggering a coordinated Protein Damage Response (PDR) [61]. The following workflow can be used to investigate this phenomenon in the context of PI resistance:
Diagram 2: Experimental workflow for profiling protein damage and PDR activation.
Detailed Protocol: Assessing the Protein Damage Response (PDR) [61]
- Cell Line and Culture: Use relevant cancer cell lines (e.g., MDA-MB-231 for breast cancer, multiple myeloma cell lines). Generate resistant sub-lines via prolonged exposure to increasing concentrations of a PI like bortezomib.
- Drug Treatment: Treat cells with the PI at its IC50 concentration or a clinically relevant dose. Include a vehicle (e.g., DMSO) control.
- Protein Misfolding/Aggregation Assay (PROTEOSTAT):
- At 1 hour post-treatment, harvest cells and stain with the PROTEOSTAT dye according to the manufacturer's protocol.
- This dye exhibits enhanced fluorescence upon binding to aggregated proteins, which expose hydrophobic regions.
- Quantify fluorescence intensity via flow cytometry or fluorescence microscopy.
- Protein Oxidative Damage Assay (Protein Carbonyls):
- At 8 hours post-treatment, lyse cells.
- Derivatize protein carbonyl groups to 2,4-dinitrophenylhydrazone (DNP-hydrazone) using a commercial kit.
- Detect the DNP-labeled proteins by immunoblotting with an anti-DNP antibody and quantify the signal.
- Limited Proteolysis-Coupled Mass Spectrometry (LiP-MS):
- Treat cells with the PI or vehicle for 1 hour.
- Lyse cells and subject the lysate to limited, non-specific proteolysis with proteinase K.
- Process the digested samples for standard LC-MS/MS analysis.
- Data Analysis: Identify peptides with significantly altered abundance in the treated sample vs. control. Increased proteolysis indicates structural unfolding/alteration, while decreased proteolysis suggests drug binding and protection.
- PDR Activation Readouts:
- Protein Ubiquitination: Perform immunoblotting on cell lysates with antibodies against K48-linked polyubiquitin chains to visualize the accumulation of proteins tagged for degradation.
- Proteasome Activity: Use fluorogenic substrates specific for the CT-L (Suc-LLVY-AMC), T-L (Bz-VGR-AMC), and C-L (Z-LLE-AMC) activities in cell lysates to measure functional proteasome capacity.
The Scientist's Toolkit: Key Research Reagents
Table 3: Essential Reagents for Studying PI Resistance
| Research Reagent / Assay | Function / Application | Key Details / Interpretation |
|---|---|---|
| Fluorogenic Proteasome Substrates | Quantifying chymotrypsin-like (CT-L), trypsin-like (T-L), and caspase-like (C-L) proteasome activities. | Suc-LLVY-AMC (for CT-L). A decrease in activity confirms on-target PI engagement. Elevated baseline activity in resistant cells suggests proteasome overload [61] [57]. |
| PROTEOSTAT Aggresome Detection Kit | Detecting and quantifying protein aggregates and misfolded proteins in cells. | Fluorescence signal indicates protein aggregation due to proteasome inhibition. Resistant cells may clear aggregates faster via autophagy [61]. |
| Anti-K48-linkage Specific Ubiquitin Antibody | Immunoblotting to detect proteins tagged for proteasomal degradation. | Accumulation of K48-polyUb proteins confirms UPS disruption. Resistant cells may show altered ubiquitination dynamics [61] [59]. |
| OxyBlot Protein Oxidation Detection Kit | Detecting protein carbonyls formed by oxidative damage. | Increased carbonyl levels indicate drug-induced oxidative protein damage, a key cytotoxic mechanism [61]. |
| CRISPR/Cas9 Knockout Libraries | Genome-wide screening to identify genes whose loss confers sensitivity or resistance to PIs. | Identifies synthetic lethal interactions and novel resistance mechanisms, such as genes in the autophagy or UPR pathways [59]. |
| Biotinylated Drug Conjugates (e.g., CIS-biotin) | Pull-down assays to identify direct protein binding partners of anticancer drugs. | Mass spectrometry analysis of pulled-down proteins reveals which cellular proteins are directly damaged by the drug, providing mechanistic insight [61]. |
Strategies to Overcome Clinical Resistance
The knowledge gained from mechanistic studies has been translated into several promising clinical strategies to overcome PI resistance.
Next-Generation and Combination Therapies
- Next-Generation Proteasome Inhibitors: New PIs with distinct properties are under investigation. For example, ixazomib is the first oral PI, offering convenience, while marizomib (NPI-0052) is a potent, irreversible inhibitor that also targets the immunoproteasome, potentially overcoming resistance conferred by β5 subunit mutations [58].
- Targeting the Ubiquitin System Upstream: Inhibition of upstream components of the UPS is a validated strategy. MLN4924 (Pevonedistat) inhibits the NEDD8-activating enzyme (NAE), blocking the activity of cullin-RING ligases (CRLs), a major class of E3 ubiquitin ligases. This disrupts the turnover of a specific subset of proteins and can synergize with PIs [62].
- Inhibition of Compensatory Pathways: Combining PIs with autophagy inhibitors like chloroquine is a rational approach to block a key resistance pathway. Similarly, targeting the aggresome pathway with histone deacetylase 6 (HDAC6) inhibitors prevents the clearance of aggregated proteins and synergistically induces apoptosis with bortezomib [59].
- Nuclear Export Inhibition: The exportin-1 inhibitor selinexor forces the nuclear retention and activation of tumor suppressor proteins, leading to cell death. It has shown clinical efficacy in combination with PIs for the treatment of PI-resistant multiple myeloma [59].
- Immunotherapy Combinations: The combination of PIs with modern immunotherapies represents a paradigm shift. Monoclonal antibodies (e.g., daratumumab targeting CD38), bispecific T-cell engagers, and CAR-T therapies have shown remarkable success. PIs can enhance the efficacy of these immunotherapies by potentiating antigen presentation and modulating the tumor microenvironment [63] [64].
Clinical Evidence and Future Directions
Recent clinical trials underscore the success of combination therapies. The CASSIOPEIA trial demonstrated that adding daratumumab to the bortezomib-based regimen (Dara-VTd) significantly improved depth of response and survival in transplant-eligible newly diagnosed MM patients [64]. Furthermore, a 2025 study reported that proteasome inhibition with bortezomib overcame resistance to targeted therapies (PI3K and Bcl-2 inhibitors) in models of B-cell malignancy and in a multi-refractory CLL patient, leading to initial clinical improvement [63]. The future of overcoming PI resistance lies in personalized, biomarker-driven therapy. Efforts are focused on using minimal residual disease (MRD) monitoring to guide treatment duration and intensity, and on developing sensitive kits to detect elevated proteasome activity as a predictive biomarker for resistance, allowing for pre-emptive intervention [61] [64].
The journey from the fundamental discovery of the ubiquitin-proteasome system to the clinical application of its inhibitors exemplifies successful translational medicine. However, the emergence of drug resistance remains a formidable challenge. Overcoming this requires a deep understanding of the diverse resistance mechanisms, including proteasome subunit alterations, activation of the Protein Damage Response, and protection from the tumor microenvironment. The experimental strategies outlined provide a roadmap for ongoing research, while combination therapies leveraging immunotherapy, novel small molecules, and biomarker-guided treatment offer a powerful multi-pronged attack to reclaim the efficacy of proteasome inhibition and improve outcomes for cancer patients.
The discovery of the ubiquitin-proteasome system (UPS) laid the essential groundwork for developing targeted protein degradation therapies. The pioneering work of Aaron Ciechanover, Avram Hershko, and Irwin Rose, recognized with the 2004 Nobel Prize in Chemistry, revealed the intricate enzymatic cascade whereby proteins are tagged with ubiquitin for degradation by the proteasome [22] [2]. This process involves a coordinated sequence: an E1 ubiquitin-activating enzyme activates ubiquitin, which is then transferred to an E2 ubiquitin-conjugating enzyme, and finally, an E3 ubiquitin ligase facilitates the transfer of ubiquitin to specific protein substrates [65]. The realization that this system provides intracellular protein degradation as a fundamental regulatory mechanism—rivaling transcription and translation in significance—opened the door for therapeutic exploitation [2]. Proteolysis-Targeting Chimeras (PROTACs) represent a revolutionary application of this knowledge, hijacking the native protein destruction machinery to target disease-causing proteins for degradation [66] [65].
PROTAC Mechanism of Action and the Critical Role of the Ternary Complex
PROTACs are heterobifunctional molecules comprising three key elements: a warhead that binds to a protein of interest (POI), an E3 ligase-binding ligand (anchor), and a chemical linker connecting these two moieties [66] [65]. Unlike traditional small-molecule inhibitors that merely occupy a binding site, PROTACs operate via an event-driven mechanism [66] [65]. The PROTAC molecule simultaneously engages both the POI and an E3 ubiquitin ligase, inducing the formation of a ternary complex [66]. This chemically-induced proximity brings the POI into close contact with the ubiquitination machinery, leading to its polyubiquitination and subsequent recognition and degradation by the 26S proteasome [65]. A key advantage of this catalytic mechanism is that a single PROTAC molecule can mediate the degradation of multiple POI copies, enabling efficacy at low concentrations and the potential targeting of proteins previously considered "undruggable" [66] [65].
Table 1: Key Advantages of PROTAC Technology over Traditional Inhibition
| Feature | Traditional Small-Molecule Inhibitors | PROTAC Degraders |
|---|---|---|
| Mechanism of Action | Occupancy-driven | Event-driven, catalytic [66] |
| Pharmacology | High systemic exposure often required | Sub-stoichiometric, lower dosing possible [65] |
| Target Scope | Limited to proteins with functional pockets | Potential to target non-enzymatic functions & "undruggable" proteins [66] [65] |
| Selectivity | Primarily from binary complex formation | Additional layer from ternary complex interactions [66] |
The stability and spatial configuration of the ternary complex are paramount for efficient degradation. The linker is not merely a passive tether; its properties directly influence the geometry and stability of the ternary complex, thereby governing the overall degradative efficacy of the PROTAC [67].
Linker Design Principles: Chemistry, Structure, and Optimization Strategies
The linker is a pivotal component that governs the biodegradation efficiency of PROTACs. Its design impacts cell permeability, physicochemical properties, and, most critically, the ability to form a productive ternary complex [66] [67].
Linker Classification and Characteristics
Linkers are broadly categorized based on their flexibility and composition:
- Flexible Linkers: These include alkyl chains (e.g., simple carbon chains) and polyethylene glycol (PEG) chains. PEG-based linkers are widely used due to their hydrophilicity, which can improve solubility, and their inherent flexibility [66] [68]. For instance, early DCAF1-based WDR5 PROTACs required PEG-based linkers of sufficient length (e.g., PROTAC 1 (OICR-40333) and PROTAC 2 (OICR-40407)) to successfully form a ternary complex and induce degradation [68].
- Rigid Linkers: These incorporate cyclic or unsaturated structures (e.g., piperazine, triazole rings) that reduce conformational freedom. They can help pre-organize the PROTAC into a bioactive conformation, potentially enhancing selectivity and potency [66].
- Cleavable Linkers: Some strategies incorporate linkers sensitive to specific environmental cues, such as acidic pH or intracellular enzymes, though this is less common in standard PROTAC design [66].
Influence of Linker Parameters on PROTAC Efficacy
The rational design of linkers involves optimizing several key parameters, as summarized in the table below.
Table 2: Impact of Linker Characteristics on PROTAC Efficacy
| Linker Parameter | Impact on PROTAC Properties | Experimental Findings |
|---|---|---|
| Length | Determines optimal distance for E3 ligase and POI interaction [67]. | A study on DCAF1-based WDR5 PROTACs found that only molecules with longer PEG linkers (e.g., ~14-18 atoms) formed productive ternary complexes, while shorter linkers failed despite good binary binding [68]. |
| Flexibility | Balances entropy loss upon binding with the ability to explore conformational space for productive complex formation [66] [67]. | Flexible alkyl/PEG linkers are common but can lead to suboptimal entropy. Rigid or semi-rigid linkers can pre-organize the molecule for better binding [66]. |
| Composition | Affects physicochemical properties like solubility, metabolic stability, and cell permeability [66] [67]. | PEG linkers enhance hydrophilicity. Incorporating rigid aromatic rings can improve metabolic stability. The attachment point (vector) on both warhead and E3 ligand is critical [66] [68]. |
Recent trends indicate a shift from traditional alkyl and PEG linkers to more sophisticated, functionally enriched linkers that can positively influence the ternary complex's properties and overall drug-likeness [66].
The Emergence of Linker-Free PROTACs
Challenging the conventional wisdom that a linker is an absolute requirement, a groundbreaking study published in 2025 introduced linker-free PROTACs [69]. This design paradigm directly conjugates an N-degron (e.g., the amino acid Proline) to a target protein ligand (e.g., a Brigatinib analog, BA) without any spacer. The resulting molecule, Pro-BA, demonstrated superior efficacy in degrading the EML4-ALK oncoprotein compared to its linker-bearing counterpart, Pro-PEG3-BA [69]. Pro-BA exhibited a lower DC50 (74 nM vs. 416 nM) and greater maximal degradation, likely by inducing a stronger interaction between the target and the E3 ubiquitin ligase [69]. This strategy, which yields smaller, more drug-like degraders, represents a significant simplification and potential advancement in PROTAC design.
Experimental and Computational Approaches for Analyzing Ternary Complexes
Biochemical and Biophysical Assays
Evaluating ternary complex formation and stability is crucial for rational PROTAC optimization. Key experimental methods include:
- Differential Scanning Fluorimetry (DSF): This assay measures the thermal stabilization (change in melting temperature, ΔTm) of proteins upon ligand binding. It can confirm the formation of a ternary complex by demonstrating a cooperative stabilization effect when both the E3 ligase and POI are present with the PROTAC. For example, this method was used to validate the binding of DCAF1-WDR5 PROTACs to both proteins and their ternary complex formation [68].
- Cellular Thermal Shift Assay (CETSA): This method assesses target engagement in a cellular context, confirming that the PROTAC binds to its intended proteins within cells [68].
- X-ray Crystallography: High-resolution crystal structures of ternary complexes provide atomic-level insights into the protein-protein interactions facilitated by the PROTAC and the specific role of the linker. For instance, crystal structures of DCAF1-PROTAC-WDR5 complexes revealed how DCAF1 loops provide surface plasticity for substrate recognition [68].
Computational Modeling and Molecular Dynamics
Computational approaches are indispensable for rational PROTAC design, especially in the absence of crystal structures.
- Ternary Complex Modeling: A robust approach combines protein-protein docking (e.g., using HADDOCK) with induced fit docking of the PROTAC. This method has been validated on known crystal structures and is particularly effective for modeling cereblon (CRBN)-based ternary complexes, helping to predict key interactions that govern complex stability [70].
- Molecular Dynamics (MD) Simulations: MD simulations (e.g., 500 ns trajectories) are used to analyze the stability of the modeled ternary complexes over time. Metrics such as buried surface area (BSA) and the radius of gyration provide quantitative insights into the compactness and dynamic behavior of the complex, which correlate with degradation efficacy [70].
The diagram below illustrates the experimental workflow for developing and optimizing PROTACs.
The Scientist's Toolkit: Essential Reagents and Methods
Table 3: Key Research Reagent Solutions for PROTAC Development
| Reagent / Method | Function in PROTAC R&D | Specific Example / Application |
|---|---|---|
| E3 Ligase Ligands | Recruit specific E3 ubiquitin ligases to form the ternary complex. | VH032 (for VHL), Thalidomide analogs (for CRBN), OICR-8268 (for DCAF1) [66] [65] [68]. |
| PROTAC Linker Libraries | Enable empirical screening of linker length, composition, and attachment points. | Alkyl (e.g., -(CH₂)ₙ-) and PEG (e.g., - (OCH₂CH₂)ₙ-) chains of varying lengths [66] [68]. |
| Computational Tools | Model ternary complexes and predict stability to guide rational design. | HADDOCK for protein-protein docking; Molecular Dynamics (MD) simulations for stability analysis [70]. |
| Biophysical Assay Kits | Characterize binding and ternary complex formation in vitro. | Differential Scanning Fluorimetry (DSF) to measure ΔTm [68]. |
| Cell-Based Degradation Assays | Quantify PROTAC efficacy and potency in a cellular context. | Western Blotting to measure DC50 (half-maximal degradation concentration) and T1/2 (degradation half-life) [69]. |
The optimization of PROTAC design has evolved into a sophisticated discipline where linker chemistry is recognized as a critical determinant of success, directly influencing the stability and geometry of the ternary complex. The field is rapidly advancing from initial trial-and-error approaches toward more rational design strategies [66] [67]. Future directions will likely focus on expanding the repertoire of E3 ligases beyond the commonly used CRBN and VHL to overcome potential resistance and enable tissue-specific targeting [68] [71]. Furthermore, the integration of advanced computational modeling and structural biology, complemented by innovative concepts like linker-free PROTACs, promises to accelerate the development of this transformative therapeutic modality and unlock its full potential for treating a wide array of human diseases [66] [70] [69].
Managing Off-Target Effects and Specificity in Ubiquitin Pathway Modulation
The ubiquitin-proteasome system (UPS) represents a crucial regulatory pathway for intracellular protein degradation, maintaining cellular homeostasis through the precise tagging and destruction of target proteins. Since the initial discovery of ubiquitin-mediated protein degradation by Aaron Ciechanover, Avram Hershko, and Irwin Rose (recognized with the 2004 Nobel Prize in Chemistry), research has revealed the astounding complexity of this system [72] [73]. The UPS encompasses an enzymatic cascade involving ubiquitin-activating (E1), ubiquitin-conjugating (E2), and ubiquitin-ligating (E3) enzymes that collectively mediate the covalent attachment of ubiquitin to substrate proteins, typically targeting them for proteasomal degradation [74] [72].
A fundamental challenge in therapeutic targeting of the UPS lies in achieving sufficient specificity to minimize off-target effects. With approximately 2 E1 enzymes, 40 E2 enzymes, and over 600 E3 ligases in human cells, the system exhibits remarkable inherent specificity [74] [72]. However, this complexity also creates substantial challenges for therapeutic intervention, as off-target effects can disrupt vital cellular processes and cause unacceptable toxicity. This technical guide examines the current strategies and methodologies for managing specificity in ubiquitin pathway modulation, providing researchers with frameworks for developing more precise therapeutic interventions.
Historical Evolution of Ubiquitin Research and Specificity Challenges
Table 1: Historical Milestones in Ubiquitin Proteasome System Research
| Year | Discovery Milestone | Impact on Specificity Understanding |
|---|---|---|
| 1975 | Identification of ubiquitin by Gideon Goldstein et al. | Initial recognition of ubiquitin as a widely distributed protein [72] |
| 1977 | Discovery of ubiquitination as a PTM by Goldknopf et al. | Recognition of ubiquitination as a novel protein modification mechanism [72] |
| 1980s | ATP-dependent ubiquitination linked to 26S proteasome degradation | Established the fundamental connection between ubiquitination and protein degradation [74] |
| 2001 | First PROTAC molecule developed | Proof-of-concept for targeted protein degradation using bifunctional molecules [21] |
| 2003 | FDA approval of bortezomib for multiple myeloma | Validation of UPS as therapeutic target; revealed specificity limitations of proteasome inhibition [74] |
| 2008 | First small molecule-based PROTAC | Advancement toward more drug-like targeted degradation platforms [21] |
| 2010s | Molecular glue degraders mechanism elucidation | Understanding of serendipitous targeted degradation with improved specificity profiles [21] |
| 2020s | Expansion to lysosomal degradation strategies (LYTAC, AbTAC) | Broaden target scope beyond intracellular proteins to membrane and extracellular targets [21] |
The historical progression of UPS research demonstrates a continual refinement of specificity understanding. Initial research focused on fundamental mechanisms of protein degradation, while contemporary investigations prioritize precise targeting strategies to minimize off-pathway effects [74] [72]. The emergence of resistance to first-generation proteasome inhibitors like bortezomib highlighted the consequences of inadequate specificity, driving development of next-generation approaches with improved target engagement profiles [74].
Quantitative Assessment of Ubiquitin Pathway Modulation
Table 2: Quantitative Analysis of Ubiquitinome Profiling Methodologies
| Methodological Approach | Identification Depth (diGly Sites) | Quantitative Accuracy (CV) | Key Advantages | Limitations |
|---|---|---|---|---|
| Data-Dependent Acquisition (DDA) | ~20,000 sites per run | 15% of sites with CV <20% | Established methodology; well-characterized workflows | Lower identification depth; higher missing values [75] |
| Data-Independent Acquisition (DIA) | ~35,000 sites per run | 45% of sites with CV <20% | Superior reproducibility; enhanced quantitative accuracy | Requires comprehensive spectral libraries [75] |
| Anti-diGly Antibody Enrichment | 89,650 sites with fractionation | Dependent on MS method | High specificity for ubiquitinated peptides; compatible with multiple MS platforms | Limited to tryptic peptides with diGly remnant; antibody variability [75] |
| FACET-IP for Acetylation | 16,740 acetylation sites | Not specified | Improved acetylation site detection; enables PTM crosstalk analysis | Specialized methodology requiring optimization [76] |
Advanced mass spectrometry techniques have revolutionized our ability to quantify ubiquitination events comprehensively. The development of anti-diGly antibody-based enrichment, which specifically isolates peptides containing the diglycine remnant left after tryptic digestion of ubiquitinated proteins, has enabled systems-wide ubiquitinome analyses [77] [75]. Recent methodological improvements, particularly the implementation of data-independent acquisition (DIA) mass spectrometry, have dramatically enhanced the depth and quantitative accuracy of ubiquitination site identification, nearly doubling the number of sites detectable in single measurements compared to traditional data-dependent acquisition (DDA) approaches [75].
Figure 1: Experimental Workflow for Comprehensive Ubiquitinome Analysis Using DIA-MS
Current Therapeutic Strategies and Specificity Profiles
Table 3: Targeted Protein Degradation Platforms and Specificity Considerations
| Therapeutic Platform | Molecular Mechanism | Specificity Advantages | Specificity Challenges |
|---|---|---|---|
| Proteasome Inhibitors (Bortezomib, Carfilzomib) | Reversible/inreversible inhibition of 20S proteasome catalytic activity | Broad efficacy in hematologic malignancies | Pan-proteasome inhibition affects multiple pathways; drug resistance [74] [72] |
| PROTACs | Bifunctional molecules recruiting E3 ligases to target proteins | Catalytic mechanism; event-driven pharmacology; targets "undruggable" proteins | Molecular size affecting permeability; hook effect at high concentrations [21] |
| Molecular Glues | Induced proximity between E3 ligase and target protein | Small molecule properties; favorable pharmacokinetics | Serendipitous discovery; rational design challenges [21] |
| E1 Inhibitors (MLN7243) | Inhibition of ubiquitin activation | Upstream pathway control | Broad effects on entire ubiquitination system; toxicity concerns [72] [73] |
| E2 Inhibitors (CC0651) | Block ubiquitin conjugation | Intermediate specificity between E1 and E3 | Limited to specific E2-enzyme pairs; potential compensatory mechanisms [72] |
| E3 Ligase Inhibitors (Nutlin, MI-219) | Block substrate recognition by specific E3 ligases | High theoretical specificity through substrate recognition | Complex regulation; potential functional redundancy [72] |
| DUB Inhibitors | Inhibit deubiquitinating enzyme activity | Precise modulation of specific ubiquitination events | Substrate scope often broad for individual DUBs [72] |
The therapeutic landscape for UPS modulation has evolved significantly from broad-spectrum proteasome inhibition toward increasingly targeted approaches. First-generation proteasome inhibitors like bortezomib demonstrated clinical efficacy but revealed the limitations of targeting the downstream degradation machinery, affecting multiple cellular pathways and leading to drug resistance [74]. Subsequent strategies have focused on upstream components of the ubiquitination cascade, with E3 ligases representing particularly attractive targets due to their substrate specificity [72] [73].
The emergence of bifunctional degradation platforms like PROTACs (PROteolysis TArgeting Chimeras) represents a paradigm shift in UPS targeting. Unlike traditional inhibitors that merely block protein function, PROTACs catalyze the destruction of target proteins by recruiting them to E3 ubiquitin ligases, initiating ubiquitination and subsequent proteasomal degradation [21]. This event-driven pharmacology offers several specificity advantages, including the ability to target proteins previously considered "undruggable" and sustained effects even after drug clearance due to the catalytic mechanism of action [21].
Experimental Approaches for Specificity Validation
Comprehensive Ubiquitinome Profiling
Global analysis of ubiquitination changes in response to therapeutic intervention provides critical assessment of off-target effects. The optimized DIA-based ubiquitinome workflow enables quantification of over 35,000 distinct diGly peptides in single measurements, dramatically improving the ability to detect off-target ubiquitination events [75]. This approach combines diGly antibody-based enrichment with optimized Orbitrap-based DIA methods and comprehensive spectral libraries, offering superior quantitative accuracy compared to traditional DDA methods [75].
Specificity Validation for Targeted Degradation
Rigorous validation of degradation specificity requires multi-faceted experimental approaches:
Ternary Complex Formation Analysis: Assessment of target protein-E3 ligase interaction using techniques such as surface plasmon resonance (SPR) and bioluminescence resonance energy transfer (BRET) provides crucial mechanistic validation for PROTAC-mediated degradation [21].
Time-Resolved Degradation Kinetics: Monitoring the temporal sequence of protein degradation helps distinguish primary targets from secondary effects, with true targets typically showing earlier degradation onset [21].
CRISPR-Based Validation: Genetic knockout of candidate E3 ligases establishes necessity for observed degradation, while rescue experiments confirm specificity [21].
Global Proteomics Analysis: Quantitative mass spectrometry-based proteomics enables system-wide assessment of protein abundance changes, identifying off-target degradation events with high confidence [75].
Figure 2: Targeted Protein Degradation Platforms and Their Cellular Pathways
The Scientist's Toolkit: Essential Research Reagents
Table 4: Key Research Reagent Solutions for Ubiquitin Pathway Studies
| Research Reagent | Specific Function | Application Context | Specificity Considerations |
|---|---|---|---|
| Anti-K-ε-GG Antibody | Immunoaffinity enrichment of ubiquitinated peptides containing diglycine remnant | Ubiquitinome profiling by MS; identification of ubiquitination sites | Cross-reactivity with other ubiquitin-like modifications (<6%) [77] [75] |
| Proteasome Inhibitors (MG132) | Reversible inhibition of 26S proteasome function | Accumulation of polyubiquitinated proteins; ubiquitinome expansion for MS analysis | Broad inhibition affects multiple protein degradation pathways [75] |
| NEDD8-Activating Enzyme Inhibitors (MLN4924) | Inhibition of cullin neddylation and CRL activity | Investigation of cullin-RING ligase-specific substrates | Affects multiple CRL complexes simultaneously [72] [73] |
| E1 Inhibitors (PYR-41) | Inhibition of ubiquitin activation | Assessment of ubiquitin-dependent processes; control experiments | Pan-inhibition of ubiquitination system [73] |
| Activity-Based DUB Probes | Chemical tools profiling deubiquitinase activity | Identification of DUBs involved in specific pathways | Varying selectivity across DUB families [72] |
| TR-TARGET System | Temperature-responsive control of protein degradation | Kinetics studies of protein turnover; validation of degradation dependencies | Limited to engineered cell systems [21] |
Emerging Technologies and Future Perspectives
Novel approaches continue to advance the specificity of ubiquitin pathway modulation:
Dual-PROTAC Systems: These innovative molecules simultaneously target two E3 ligases to a single protein of interest, potentially enhancing degradation specificity and efficiency while reducing off-target effects through cooperative recognition [21].
Lysosome-Targeting Chimeras (LYTACs): Expanding the degradation landscape beyond the proteasome, LYTACs recruit cell surface proteins to lysosomal trafficking pathways, enabling degradation of extracellular and membrane proteins that traditional UPS-based approaches cannot target [21].
Antibody-Based PROTACs (AbTACs): These bispecific antibodies bind cell surface E3 ligases and target proteins, combining the specificity of antibody-based recognition with targeted protein degradation principles [21].
PHICS Technology: The Proteasome-Hijacking Antibody technology represents another innovative approach, utilizing anti-protein of interest antibodies conjugated to proteasome-associating ligands to direct target proteins to the proteasome [21].
Advanced screening methodologies including DNA-encoded library screening and covalent ligand discovery are expanding the arsenal of E3 ligase recruiters, enabling targeting of previously inaccessible E3 ligases and enhancing the specificity landscape of targeted protein degradation [21].
The strategic evolution from broad UPS inhibition to precision targeted degradation represents a fundamental shift in therapeutic targeting of the ubiquitin pathway. While challenges remain in achieving absolute specificity, current methodologies provide robust frameworks for characterizing and validating target engagement while minimizing off-pathway effects. The continued development of advanced screening technologies, structural insights into E3 ligase mechanisms, and innovative degradation platforms promises to further enhance the specificity and therapeutic potential of ubiquitin pathway modulation. As these technologies mature, they offer unprecedented opportunities for targeting previously intractable disease drivers across diverse therapeutic areas.
The ubiquitin-proteasome system (UPS) represents the primary pathway for targeted protein degradation in eukaryotic cells, an essential process for maintaining cellular homeostasis. This sophisticated system controls the precise regulation of countless proteins involved in cell cycle progression, stress responses, DNA repair, and signal transduction. The UPS operates through a coordinated enzymatic cascade that tags target proteins with ubiquitin chains, marking them for destruction by the proteasome—a large multi-subunit proteolytic complex. The critical importance of the UPS is perhaps most strikingly revealed when this system falters; accumulating evidence firmly implicates UPS dysfunction in the pathogenesis of multiple neurodegenerative disorders, including Alzheimer's disease (AD), Parkinson's disease (PD), and Huntington's disease (HD). These conditions share a common pathological feature: the accumulation of misfolded, aggregation-prone proteins that form toxic intracellular inclusions, ultimately leading to neuronal dysfunction and cell death. This whitepaper examines the intricate relationship between UPS dysregulation and neurodegenerative diseases, exploring historical discoveries, underlying mechanisms, research methodologies, and emerging therapeutic strategies targeting this vital proteolytic pathway.
Historical Foundations of Ubiquitin-Proteasome Research
The conceptual foundation for understanding protein degradation was laid in the 1930s by Schoenheimer and Rittenberg, who first demonstrated that cellular proteins exist in a dynamic state of synthesis and degradation [78]. However, the specific molecular machinery responsible for regulated intracellular proteolysis remained elusive for decades. The field of ubiquitin research emerged in the 1980s through complementary discoveries by the laboratories of Avram Hershko (Technion, Haifa, Israel) and Alexander Varshavsky (then at MIT, Cambridge, USA) [2].
Hershko and colleagues, using biochemical fractionation of reticulocyte extracts, discovered that protein degradation required ATP and involved a small protein they initially termed APF-1 (ATP-dependent proteolytic factor 1) [2]. In a pivotal convergence of research lines, APF-1 was subsequently identified as ubiquitin by Wilkinson, Urban, and Haas in the laboratory of Irwin Rose [2]. Between 1978-1983, Hershko, his student Aaron Ciechanover, and collaborator Irwin Rose elucidated the fundamental enzymatic cascade of ubiquitin conjugation: E1 (ubiquitin-activating enzyme), E2 (ubiquitin-conjugating enzyme), and E3 (ubiquitin ligase) enzymes work sequentially to attach ubiquitin to protein substrates [2]. They further characterized the ATP-dependent protease that degrades ubiquitin-tagged proteins, later identified as the 26S proteasome [2].
Parallel work from Varshavsky's laboratory connected ubiquitin to chromatin biology, demonstrating that ubiquitin conjugated to histone H2A was enriched in transcribed regions of chromosomes [2]. Reading the 1980 papers from Hershko and Wilkinson, Varshavsky recognized the connection between protein degradation and chromatin-associated ubiquitin, predicting "a regulatory system of great complexity and broad, still-to-be-discovered biological functions" [2]. His group subsequently pioneered genetic approaches in yeast to uncover the first biological functions of the UPS, establishing its essential roles in cell cycle progression, DNA repair, protein synthesis, transcriptional regulation, and stress responses [2]. These complementary biochemical and genetic approaches in the 1980s fundamentally transformed our understanding of intracellular regulation, revealing that controlled protein degradation rivals transcription and translation in physiological significance.
Table 1: Key Historical Discoveries in UPS Research
| Year | Discovery | Key Researchers |
|---|---|---|
| 1978-1980 | Identification of ATP-dependent protein degradation and APF-1/ubiquitin conjugation | Hershko, Ciechanover, Rose |
| 1980-1983 | Elucidation of E1, E2, E3 enzymatic cascade | Hershko, Ciechanover, Rose |
| 1984-1990 | Identification of biological functions (cell cycle, DNA repair) and degradation signals | Varshavsky laboratory |
| 1990s | Characterization of the 26S proteasome | Multiple laboratories |
| 2000s | Link between UPS dysfunction and neurodegenerative diseases | Multiple laboratories |
Molecular Architecture of the Ubiquitin-Proteasome System
The Ubiquitination Cascade
The UPS employs a highly coordinated three-enzyme cascade to tag proteins for degradation. The process initiates with E1 ubiquitin-activating enzyme, which activates ubiquitin in an ATP-dependent reaction, forming a thioester bond between its active-site cysteine and the C-terminal glycine of ubiquitin [79] [80]. The activated ubiquitin is then transferred to a cysteine residue of an E2 ubiquitin-conjugating enzyme. Finally, an E3 ubiquitin ligase simultaneously binds both the E2~ubiquitin complex and the target protein substrate, facilitating the transfer of ubiquitin to a lysine residue on the substrate [81] [79].
E3 ubiquitin ligases constitute the most diverse and specialized component of this cascade, determining substrate specificity. Humans possess approximately 35 E2 enzymes but over 600 E3 ligases, enabling precise recognition of a vast array of substrates [79]. E3 ligases are categorized into three major families based on their structural domains and mechanisms: Really Interesting New Gene (RING) domain-containing E3s, Homologous to E6AP C-Terminus (HECT) domain-containing E3s, and RING-between-RING (RBR) domain-containing E3s [81]. RING E3s catalyze direct ubiquitin transfer from E2 to the substrate, while HECT and RBR E3s form an obligate thioester intermediate with ubiquitin before transferring it to the substrate [81].
The fate of the ubiquitinated protein is determined by the topology of the polyubiquitin chain. Ubiquitin itself contains seven lysine residues (K6, K11, K27, K29, K33, K48, K63), each capable of forming polyubiquitin chains with distinct biological meanings [81] [80]. K48-linked chains predominantly target substrates for proteasomal degradation, while K63-linked chains typically mediate non-proteolytic processes including DNA repair, endocytosis, and inflammatory signaling [81]. Other chain types (K11, K29, K33) have mixed or context-dependent functions.
Diagram 1: Ubiquitin-Proteasome System Pathway
The Proteasome Complex
The 26S proteasome is the executive component of the UPS, responsible for the actual degradation of ubiquitinated proteins. This massive (~2.5 MDa) multi-subunit complex consists of two primary assemblies: the 20S core particle (CP) and one or two 19S regulatory particles (RP) [79]. The 20S CP is a barrel-shaped structure composed of four stacked heptameric rings: two identical outer α-rings and two identical inner β-rings. The α-rings control substrate access to the proteolytic chamber, while the β-rings contain the proteolytic active sites facing the interior cavity [79]. Three different β-subunits confer distinct proteolytic activities: caspase-like (cleaving after acidic residues), trypsin-like (cleaving after basic residues), and chymotrypsin-like (cleaving after hydrophobic residues) [79].
The 19S RP recognizes polyubiquitinated substrates, removes the ubiquitin chains, unfolds the target protein, and translocates it into the 20S catalytic chamber. This process is ATP-dependent and involves six homologous ATPases (Rpt1-6) that form a ring in the base subcomplex of the 19S RP [79]. Additional proteasome activators include the 11S regulator (PA28) and PA200/Blm10, which can replace the 19S RP under certain conditions and facilitate ubiquitin-independent degradation of unstructured proteins [79].
Table 2: Major Proteasome Components and Functions
| Component | Structure | Function |
|---|---|---|
| 20S Core Particle | 28 subunits (α7β7β7α7) | Catalytic core with multiple proteolytic activities |
| 19S Regulatory Particle | 19 subunits (lid + base) | Recognizes ubiquitinated proteins, deubiquitination, unfolding, translocation |
| 11S Regulator (PA28) | Heptameric ring (α/β/γ) | ATP-independent activator; enhances peptide hydrolysis |
| PA200/Blm10 | Monomeric | Nuclear regulator; involved in DNA repair, spermatogenesis |
UPS Dysregulation in Neurodegenerative Diseases
Alzheimer's Disease
Alzheimer's disease is characterized by two hallmark pathological lesions: extracellular amyloid plaques composed primarily of β-amyloid (Aβ) peptides, and intracellular neurofibrillary tangles consisting of hyperphosphorylated tau protein [81]. The UPS is intimately involved in the clearance of both these pathogenic proteins. Multiple E3 ubiquitin ligases, including CHIP (C-terminus of Hsc70-interacting protein), parkin, and UBE3A, mediate the ubiquitination of tau and target it for proteasomal degradation [78]. UPS dysfunction in AD is evidenced by the accumulation of ubiquitin-conjugated proteins within neurofibrillary tangles and the documented impairment of proteasomal activity [81] [78].
Notably, a vicious cycle appears to operate in AD: pathological protein aggregates impair proteasome function, which in turn leads to further accumulation of misfolded proteins. Aβ oligomers have been shown to directly inhibit the proteasome's chymotrypsin-like activity, while hyperphosphorylated tau aggregates may physically obstruct proteasomal access [82] [78]. This proteolytic stress creates a cellular environment permissive to additional protein aggregation, accelerating disease progression.
Parkinson's Disease
The connection between UPS dysfunction and PD is particularly strong, with multiple familial forms of PD directly linked to mutations in UPS components. Autosomal recessive forms of PD can result from mutations in the genes encoding parkin (an E3 ubiquitin ligase) and UCH-L1 (a deubiquitinating enzyme) [81] [80]. The primary pathological feature of PD is the presence of Lewy bodies—intracellular inclusions whose major component is aggregated α-synuclein—alongside selective loss of dopaminergic neurons in the substantia nigra [81] [80].
Under normal conditions, α-synuclein is degraded by both UPS and autophagy pathways. However, elevated levels or mutant forms of α-synuclein can directly inhibit proteasome function [80]. Parkin normally works in concert with PINK1 to regulate mitochondrial quality control via mitophagy, and parkin mutations result in accumulation of damaged mitochondria, increased oxidative stress, and ultimately neuronal vulnerability [80]. Additionally, oxidative modifications to UPS components themselves further compromise proteolytic capacity in PD, creating a feed-forward cycle of proteostatic collapse.
Polyglutamine Disorders
Huntington's disease and other polyglutamine expansion diseases (such as spinocerebellar ataxias) are caused by CAG trinucleotide repeat expansions in the coding regions of respective genes, resulting in proteins with elongated polyglutamine tracts that are highly prone to misfolding and aggregation [81]. The UPS plays a crucial role in clearing these mutant proteins, and UPS impairment is a consistent feature in cellular and animal models of polyglutamine diseases.
Notably, expanded polyglutamine tracts themselves can inhibit the proteasome by physically clogging the proteolytic channel, potentially through incomplete degradation attempts [78]. This direct inhibition has profound consequences for overall protein homeostasis, as the accumulating mutant proteins sequester essential UPS components, including ubiquitin and certain E3 ligases, thereby impairing the degradation of other cellular substrates and disrupting normal cellular functions.
Experimental Methods for Studying UPS Function
High-Content Screening for UPS Activators
Recent methodological advances have enabled systematic screening for compounds that enhance UPS activity. Wang et al. (2022) established a robust high-content fluorescence imaging system using stable YFP-CL1 HT22 cells for high-throughput screening of UPS activators [82]. The CL1 degron is a well-characterized ubiquitin-proteasome degradation signal, and its fusion to yellow fluorescent protein (YFP) creates a reporter whose fluorescence intensity inversely correlates with UPS activity [82].
Experimental Protocol:
- Cell Line Generation: HT22 hippocampal neurons are stably transfected with YFP-CL1 plasmid and selected with G418 to create a homogeneous reporter cell line.
- Compound Screening: Test compounds from library (e.g., traditional Chinese medicine library) are applied to cells in multi-well plates.
- Fluorescence Quantification: After incubation, YFP fluorescence intensity is measured using high-content fluorescence imaging systems and confirmed by flow cytometry.
- Validation: Hit compounds are further validated in disease-relevant models, such as HT22 cells transiently transfected with APP, Tau, or mutant Tau P301L, where clearance of these pathogenic proteins is assessed by Western blot and immunofluorescence [82].
Using this approach, researchers identified salvianolic acid A, salvianolic acid B, and ellagic acid as potent UPS activators that effectively reduced levels of Alzheimer's-related proteins [82].
Diagram 2: UPS Activator Screening Workflow
The Scientist's Toolkit: Key Research Reagents
Table 3: Essential Research Reagents for UPS Studies
| Reagent/Tool | Application | Function/Principle |
|---|---|---|
| YFP-CL1 Reporter | UPS activity measurement | CL1 degron targets YFP for UPS degradation; fluorescence inversely correlates with UPS activity [82] |
| Proteasome Inhibitors (MG132, Bortezomib) | UPS inhibition studies | Reversibly inhibit proteasomal chymotrypsin-like activity, inducing UPS impairment |
| Ubiquitin Mutants (K48R, K63R, etc.) | Chain linkage specificity | Identify specific polyubiquitin chain linkages involved in degradation signals |
| E3 Ligase Inhibitors/Activators | Pathway modulation | Investigate specific E3 ligase functions in protein degradation pathways |
| Tandem Ubiquitin Binding Entities (TUBEs) | Isolation of ubiquitinated proteins | Affinity matrices for purification of polyubiquitinated proteins from cell lysates |
Therapeutic Strategies Targeting the UPS
PROTAC Technology
Proteolysis Targeting Chimeras (PROTACs) represent a revolutionary therapeutic approach that hijacks the UPS to selectively degrade disease-causing proteins [83]. These bifunctional molecules consist of three elements: a ligand that binds the target protein of interest (POI), a ligand that recruits an E3 ubiquitin ligase, and a linker connecting these two moieties [83]. PROTACs bring the E3 ligase into proximity with the POI, leading to its ubiquitination and subsequent proteasomal degradation.
The catalytic nature of PROTACs represents a significant advantage over traditional inhibitors, as a single PROTAC molecule can theoretically mediate the degradation of multiple POI copies [83]. Furthermore, PROTACs can target proteins traditionally considered "undruggable," such as transcription factors and scaffold proteins, by exploiting their structural features for recognition rather than functional active sites.
As of 2025, over 40 PROTAC drug candidates are in clinical development, with three advanced to Phase III trials: vepdegestran (ARV-471, targeting ER for breast cancer), BMS-986365 (targeting AR for prostate cancer), and BGB-16673 (targeting BTK for B-cell malignancies) [84]. While most current applications focus on oncology, PROTAC technology holds tremendous promise for neurodegenerative diseases by targeting the clearance of pathological proteins like tau, α-synuclein, and huntingtin.
Emerging Modulation Strategies
Beyond PROTACs, several innovative strategies are being explored to rectify UPS dysfunction in neurodegeneration. These include:
- UPS Activators: Small molecules like the identified salvianolic acids and ellagic acid that enhance proteasome activity or reduce proteasome inhibition by aggregates [82].
- E3 Ligase Modulators: Compounds that enhance the activity of specific neuroprotective E3 ligases (e.g., parkin, CHIP) to promote clearance of pathological proteins.
- Deubiquitinating Enzyme Inhibitors: Targeting DUBs that are overactive in disease states, potentially rebalancing ubiquitination dynamics toward degradation.
- Proteasome Activators: Molecules that directly bind and enhance the proteolytic capacity of the proteasome, potentially counteracting age-related declines in proteasome function.
Table 4: Selected PROTACs in Clinical Development
| PROTAC Name | Target | E3 Ligase | Indication | Development Phase |
|---|---|---|---|---|
| Vepdegestran (ARV-471) | Estrogen Receptor | CRBN | ER+/HER2- Breast Cancer | Phase III [84] |
| BMS-986365 | Androgen Receptor | CRBN | Metastatic Castration-Resistant Prostate Cancer | Phase III [84] |
| BGB-16673 | BTK | CRBN | B-cell Malignancies | Phase III [84] |
| ARV-110 | Androgen Receptor | CRBN | Prostate Cancer | Phase II [84] |
| KT-474 | IRAK4 | IAP | Hidradenitis Suppurativa, Atopic Dermatitis | Phase II [84] |
The ubiquitin-proteasome system represents both a vulnerability and therapeutic opportunity in neurodegenerative diseases. The historical elucidation of this sophisticated proteolytic machinery, from the initial biochemical characterization to the genetic dissection of its physiological functions, has provided the essential foundation for understanding its role in neurodegeneration. The intricate interplay between UPS dysfunction and pathological protein accumulation creates self-reinforcing cycles of proteostatic collapse that drive disease progression. However, emerging technologies—from high-throughput screening for UPS enhancers to the revolutionary PROTAC platform—offer unprecedented opportunities to intervene in these destructive processes. As our understanding of UPS biology continues to deepen, and as innovative therapeutic modalities advance through clinical development, targeting the UPS represents a promising strategy for developing disease-modifying treatments for Alzheimer's disease, Parkinson's disease, and other neurodegenerative disorders.
Efficacy and Impact: Validating UPS Strategies in Research and Clinic
The history of drug discovery has been profoundly shaped by our understanding of cellular machinery, particularly the ubiquitin-proteasome system (UPS). Discovered and characterized through pioneering research spanning the late 20th century, the UPS is the primary pathway for regulated intracellular protein degradation in eukaryotic cells [85] [86]. This system maintains cellular homeostasis by tagging proteins with ubiquitin chains for recognition and degradation by the 26S proteasome, a complex multi-subunit protease [85]. The foundational research into this system, which earned the Nobel Prize in Chemistry in 2004, unveiled a new universe of pharmacological intervention beyond traditional occupancy-driven inhibition.
The UPS functions through a sequential enzymatic cascade: an E1 activating enzyme activates ubiquitin in an ATP-dependent process and transfers it to an E2 conjugating enzyme, which then works in concert with an E3 ubiquitin ligase to attach ubiquitin to specific substrate proteins [85] [86]. Polyubiquitinated substrates are subsequently degraded by the 26S proteasome, and ubiquitin molecules are recycled [85]. This intricate cellular process forms the mechanistic foundation for Proteolysis-Targeting Chimeras (PROTACs), a revolutionary technology that hijacks this natural protein-quality-control system for therapeutic purposes [87].
PROTACs represent a fundamental departure from traditional small-molecule inhibitors (SMIs), moving beyond simple inhibition to direct targeted protein removal [87]. This shift has expanded the druggable proteome, challenged established drug design principles, and opened new therapeutic avenues for previously intractable targets. This review provides a comprehensive technical comparison between these two therapeutic modalities, contextualized within the historical framework of UPS research.
Mechanisms of Action: Occupancy-Driven Inhibition vs. Event-Driven Degradation
Traditional Small-Molecule Inhibitors
Traditional SMIs operate on an occupancy-driven mechanism. They function by binding directly to the active site or an allosteric site on a target protein, physically obstructing its enzymatic activity or functional interactions [88] [87]. Their efficacy is contingent upon maintaining sufficient systemic concentration to sustain high target occupancy, as their pharmacological effect is proportional to the number of inhibited targets at any given moment [88] [85]. This requirement for continuous high occupancy often necessitates higher and more frequent dosing to achieve clinical benefit, which can increase the risk of off-target effects [89].
PROTACs: Catalytic Protein Degraders
In contrast, PROTACs employ an event-driven mechanism that subverts the traditional occupancy model. These heterobifunctional molecules consist of three covalently linked components: a ligand that binds the protein of interest (POI), a ligand that recruits an E3 ubiquitin ligase, and a chemical linker connecting the two moieties [89] [90] [87]. The PROTAC does not inhibit the target protein but instead acts as a molecular bridge, bringing the POI into close proximity with an E3 ubiquitin ligase. This forced interaction facilitates the formation of a productive ternary complex (POI-PROTAC-E3 ligase), leading to the transfer of ubiquitin chains onto the POI [89] [85]. The polyubiquitinated protein is then recognized and degraded by the proteasome [85]. Crucially, the PROTAC molecule is released unchanged after each degradation cycle, allowing it to catalyze the destruction of multiple target proteins [85] [87]. This catalytic nature means that substoichiometric amounts of PROTAC can achieve profound and sustained pharmacological effects.
Diagram Title: PROTAC Mechanism of Action
Comparative Advantages and Limitations
Quantitative Comparison of Key Characteristics
The table below summarizes the fundamental differences between PROTACs and traditional small-molecule inhibitors across multiple parameters.
Table 1: Direct Comparison of PROTACs and Traditional Small-Molecule Inhibitors
| Characteristic | PROTACs | Traditional Small-Molecule Inhibitors |
|---|---|---|
| Mechanism of Action | Event-driven, catalytic degradation [85] [87] | Occupancy-driven, stoichiometric inhibition [88] |
| Molecular Weight | High (700–1,100 Da) [89] [90] | Low (typically <500 Da) |
| Pharmacology | Sustained effect after clearance; catalytic & substoichiometric [89] [85] | Effect requires sustained exposure; stoichiometric [88] |
| Target Scope | Can target proteins without functional pockets (e.g., scaffolds, transcription factors) [88] [87] | Limited to proteins with accessible, functional binding pockets [88] |
| Dosing | Lower doses and/or less frequent dosing possible [85] | Often requires high doses/frequent administration for target saturation [89] |
| Resistance | Can overcome mutations that reduce inhibitor binding and protein overexpression [88] [85] | Susceptible to resistance via point mutations and protein overexpression [88] |
| PK/PD Relationship | Complex, non-linear (hook effect); efficacy tied to degradation kinetics [88] [90] | Generally linear; efficacy tied to plasma concentration [90] |
| Oral Bioavailability | Challenging due to large molecular size and polarity [89] [90] | Typically more favorable (often follow Lipinski's Rule of Five) [90] |
| Selectivity | Can achieve high selectivity via ternary complex formation [89] | Selectivity depends solely on binary binding to the target |
Key Advantages of PROTACs
- Targeting the "Undruggable" Proteome: PROTACs can theoretically degrade any protein that contains a surface lysine residue accessible for ubiquitination, provided a binding ligand is available. This dramatically expands the druggable proteome to include transcription factors, scaffolding proteins, and non-enzymatic regulators previously considered "undruggable" by traditional SMIs [88] [87]. For example, PROTACs have been developed to target KRAS, STAT3, and MYC, which are high-value cancer targets that have largely evaded conventional inhibition [88] [84].
- Catalytic Efficiency and Sustained Effects: The catalytic mechanism allows a single PROTAC molecule to degrade multiple copies of the target protein, leading to potent effects at low concentrations [85] [87]. Furthermore, because the target protein must be resynthesized to restore function, the pharmacological effect persists even after the PROTAC has been cleared from the system, potentially enabling lower dosing frequencies [87].
- Overcoming Drug Resistance: Resistance to targeted therapies often arises from mutations in the drug-binding pocket or target overexpression. Since PROTACs require only binding (not necessarily inhibition) to recruit the target to the E3 ligase, they can remain effective against mutants with reduced affinity for the original inhibitor [89] [85]. Degrading the entire protein also circumvents resistance caused by target overexpression, a common mechanism of adaptive resistance to SMIs [88].
Key Challenges and Limitations of PROTACs
- Suboptimal Drug-Like Properties: PROTACs typically have high molecular weights (700–1,100 Da), excessive hydrogen bond donors/acceptors, and large polar surface areas. These properties often lead to poor membrane permeability, low oral bioavailability, and challenging pharmacokinetics, violating the traditional "Rule of Five" for drug-likeness [89] [90].
- The "Hook Effect": At high concentrations, PROTACs can form unproductive binary complexes (PROTAC-POI or PROTAC-E3), saturating the binding sites without forming the necessary ternary complex. This leads to a characteristic bell-shaped dose-response curve where degradation efficiency decreases at high concentrations, complicating dose optimization [88] [90].
- Limited E3 Ligase Toolkit: Despite over 600 E3 ligases in the human genome, the vast majority of current PROTACs recruit only a handful, primarily Cereblon (CRBN) and Von Hippel-Lindau (VHL) [89] [87]. The ubiquitous expression of these E3 ligases limits opportunities for tissue-selective targeting and may contribute to on-target toxicities in healthy tissues [90].
- Analytical and Developmental Complexity: The large molecular size and complex structure of PROTACs present significant challenges for bioanalysis, including issues with ion suppression, peak splitting in LC-MS/MS, and non-specific binding to labware [90]. Their metabolic stability is also a concern, with over 70% of PROTACs undergoing rapid biotransformation at the aliphatic linker region, primarily via CYP3A-mediated oxidation [90].
Experimental Methodologies for PROTAC Development and Evaluation
Key Experimental Workflow
The development and evaluation of PROTACs require a series of specialized experimental protocols that differ significantly from those used for traditional SMIs. The workflow integrates medicinal chemistry, structural biology, and cellular and molecular biology techniques.
Diagram Title: PROTAC Development Workflow
Detailed Experimental Protocols
1. Ternary Complex Formation Analysis
- Objective: Confirm and characterize the formation of the POI-PROTAC-E3 ligase ternary complex.
- Methodologies:
- Surface Plasmon Resonance (SPR): A biotinylated E3 ligase is immobilized on a streptavidin chip. The PROTAC is injected, followed by the POI. Binding responses are measured in real-time to determine cooperative binding and complex stability [90].
- Isothermal Titration Calorimetry (ITC): Measures the heat change during binding events. Titrating the PROTAC into a solution containing both the POI and E3 ligase can reveal positive or negative cooperativity based on binding thermodynamics [90].
- Cryo-Electron Microscopy (cryo-EM): Used to obtain high-resolution structures of the ternary complex, informing on spatial orientation and guiding linker optimization [87].
2. Cellular Degradation and Potency Assessment
- Objective: Quantify the efficiency and potency of target degradation in a cellular context.
- Methodology:
- Treat cells with a concentration gradient of the PROTAC molecule for a predetermined time (typically 4-24 hours).
- Lyse cells and analyze target protein levels by Western blotting or quantitative immunofluorescence.
- Normalize protein levels to loading controls and plot percentage degradation versus PROTAC concentration to determine the DC~50~ (concentration that degrades 50% of the target protein) and D~max~ (maximum degradation achieved) [90].
- Compare degradation kinetics and efficiency across different cell lines, including those resistant to traditional SMIs.
3. Global Proteomic Profiling for Selectivity
- Objective: Identify on-target and off-target degradation events across the entire proteome.
- Methodology (Tandem Mass Tag Mass Spectrometry - TMT-MS):
- Treat cells with the PROTAC or vehicle control.
- Harvest cells, digest proteins with trypsin, and label peptides with isobaric TMT reagents.
- Pool samples and analyze by liquid chromatography-tandem mass spectrometry (LC-MS/MS).
- Quantify protein levels across thousands of proteins simultaneously.
- Statistically analyze data to identify proteins significantly downregulated by PROTAC treatment, excluding those affected by vehicle controls or related DMSO treatments [90].
4. In Vivo Pharmacokinetic/Pharmacodynamic (PK/PD) Modeling
- Objective: Establish the relationship between PROTAC exposure and target degradation in vivo.
- Methodology:
- Administer the PROTAC to animal models (e.g., mouse xenografts) via the intended route (e.g., oral gavage, IV).
- Collect plasma and tissue samples (e.g., tumor) at multiple time points.
- PK Analysis: Use LC-MS/MS with optimized low-binding protocols to quantify PROTAC concentrations in plasma and tissues over time [90].
- PD Analysis: Measure target protein levels in tissues (e.g., by Western blot or immunohistochemistry) from the same time points.
- Modeling: Develop a mechanistic PK/PD model that integrates systemic exposure, tumor penetration, and degradation kinetics (EC~50~, maximum degradation, degradation half-life) to inform dosing regimen selection [90].
The Scientist's Toolkit: Essential Research Reagents and Materials
The table below outlines key reagents and materials essential for the design, synthesis, and evaluation of PROTAC molecules.
Table 2: Essential Research Reagents for PROTAC Development
| Reagent / Material | Function / Application | Specific Examples & Notes |
|---|---|---|
| E3 Ligase Ligands | Recruits the ubiquitin ligase machinery to the ternary complex. | CRBN Ligands: Thalidomide, Lenalidomide, Pomalidomide derivatives [89] [83]. VHL Ligands: VH-032, VH-101 based on hydroxyproline [89]. IAP and MDM2 ligands are also used [89]. |
| Target Protein Binders | Binds the Protein of Interest (POI) with high affinity. | Can be known inhibitors/agonists (e.g., JQ1 for BRD4, Bicalutamide for AR) [89] [88]. Novel binders from phage display or DNA-encoded libraries are also used [88]. |
| PROTAC Linkers | Covalently connects the E3 ligand and the POI ligand; critical for optimal ternary complex geometry. | PEG Linkers: NH2-PEG4-OH, Boc-NH-PEG3-Tosylate [89]. Alkyl Chain Linkers: Vary in length and rigidity. Linker optimization is crucial for degradation efficiency and physicochemical properties [89] [90]. |
| Cell Lines with Endogenous E3 Ligases | For in vitro degradation assays in a physiologically relevant context. | Wild-type cell lines expressing CRBN or VHL. Isogenic lines with CRISPR-mediated E3 ligase knockouts are essential for mechanistic validation and ruling out non-specific effects [90]. |
| Affinity Purification Resins | For isolating ternary complexes and identifying binding partners. | Streptavidin beads for biotinylated PROTACs, antibody-conjugated beads for immunoprecipitation of specific complex components. |
| Mass Spectrometry Reagents | For global proteomic analysis to assess selectivity and off-target effects. | Tandem Mass Tag (TMT) reagents for multiplexed relative protein quantification. Trypsin for protein digestion. Stable isotope-labeled internal standards for absolute quantification [90]. |
| Low-Binding Labware | To minimize non-specific adsorption of PROTACs during bioanalytical and in vitro assays. | Low-binding microcentrifuge tubes, multi-well plates, and pipette tips are critical for achieving accurate quantitation and reproducible results due to the "sticky" nature of many PROTACs [90]. |
The advent of PROTAC technology, built upon decades of fundamental research into the ubiquitin-proteasome system, represents a true paradigm shift in therapeutic development. By transitioning from an occupancy-driven to an event-driven pharmacological model, PROTACs have not only provided a novel strategy to overcome the limitations of traditional small-molecule inhibitors but have also dramatically expanded the universe of druggable targets. While significant challenges remain—particularly in optimizing drug-like properties, expanding the E3 ligase toolbox, and managing complex PK/PD relationships—the clinical progress of candidates like vepdegestrant (ARV-471) and BMS-986365 underscores the transformative potential of this modality [84]. As the field matures, integrating advanced technologies like AI-driven design and novel delivery systems will be crucial to fully realizing the promise of targeted protein degradation, ultimately propelling small-molecule drug discovery into its next golden age [83] [90] [87].
The ubiquitin-proteasome system (UPS) represents a sophisticated regulatory mechanism for controlled protein degradation in eukaryotic cells, orchestrating numerous cellular processes including cell cycle progression, DNA repair, and stress response. The foundational discoveries of the UPS by Avram Hershko, Aaron Ciechanover, and Alexander Varshavsky in the 1980s revealed a complex enzymatic cascade wherein proteins are tagged for degradation through ubiquitination. This process involves sequential action of E1 (ubiquitin-activating), E2 (ubiquitin-conjugating), and E3 (ubiquitin-ligase) enzymes that attach ubiquitin chains to substrate proteins, targeting them for destruction by the 26S proteasome—a multicatalytic protease complex. The recognition that cancer cells exhibit heightened dependence on proteasome function for eliminating misfolded proteins and regulating cell-cycle controllers provided the fundamental rationale for developing proteasome inhibitors as antineoplastic agents, establishing an entirely new paradigm in oncology therapeutics.
Historical Foundations: From Basic Research to Clinical Application
The journey from basic mechanistic discoveries to clinical implementation of proteasome inhibitors represents a triumph of translational medicine. Early work in Hershko's laboratory using biochemical fractionation of reticulocyte extracts identified the ATP-dependent proteolytic system and the crucial role of ubiquitin conjugation in protein degradation. Parallel investigations by Varshavsky's group revealed the profound biological significance of the UPS through genetic and cell biological studies, establishing its essential roles in cell cycle regulation, DNA repair, and transcriptional control. These complementary approaches converged to demonstrate that regulated intracellular proteolysis rivals transcriptional and translational control in significance for cellular circuit regulation.
The transformation of this basic biological knowledge into therapeutic strategy emerged from the recognition that malignant cells, particularly those with high protein turnover like multiple myeloma plasma cells, exhibit exceptional vulnerability to proteasome disruption. The first clinical validation of this approach came with the 2003 FDA approval of bortezomib for relapsed and refractory multiple myeloma, which demonstrated that targeting protein degradation machinery could yield significant clinical benefits even in advanced disease states. This breakthrough initiated ongoing efforts to develop increasingly sophisticated UPS-targeted therapies with improved efficacy and safety profiles.
Currently Approved Proteasome Inhibitors: Mechanisms and Clinical Applications
Since the initial approval of bortezomib, the therapeutic arsenal of proteasome inhibitors has expanded significantly, with multiple agents now available for clinical use. These compounds share the common mechanism of inhibiting the proteolytic activity of the 20S proteasome core particle but differ in their chemical structures, pharmacological properties, and specific clinical indications.
Table 1: FDA-Approved Proteasome Inhibitors in Oncology
| Name (Brand) | Kinetics | Active Moiety | Primary Indications | Administration | Common Toxicities |
|---|---|---|---|---|---|
| Bortezomib (Velcade) | Slowly reversible inhibitor β5>β1>β2 | Boronate | First-line, relapsed/refractory MM and MCL | IV/SC | Peripheral neuropathy, nausea, vomiting, diarrhea, cytopenias, infection |
| Carfilzomib (Kyprolis) | Irreversible inhibitor β5>β2/β1 | Epoxyketone | Relapsed or refractory MM | IV | Dyspnea, cytopenias, nausea, vomiting, diarrhea, fatigue, headache, peripheral edema |
| Ixazomib (Ninlaro) | Reversible inhibitor β5>β1 | Boronate | MM after one prior therapy | Oral | Diarrhea, constipation, cytopenias, peripheral neuropathy, nausea, vomiting, peripheral edema, back pain |
These agents primarily target the chymotrypsin-like (β5) subunit of the proteasome, with varying effects on the trypsin-like (β2) and caspase-like (β1) subunits at higher concentrations. Their clinical efficacy stems from multiple interconnected mechanisms that disrupt cellular homeostasis in malignant cells.
Molecular Mechanisms of Proteasome Inhibitor Action
Proteasome inhibitors exert their antineoplastic effects through several interconnected pathways that collectively induce apoptosis in malignant cells:
NF-κB Pathway Inhibition: The transcription factor NF-κB promotes cell survival, proliferation, and angiogenesis in many hematologic malignancies. Under normal conditions, the endogenous inhibitor IκBα undergoes proteasomal degradation upon cellular activation, allowing NF-κB nuclear translocation. Proteasome inhibition prevents IκBα degradation, maintaining NF-κB in an inactive cytoplasmic complex and suppressing its pro-survival transcriptional program.
Unfolded Protein Response (UPR) and Endoplasmic Reticulum (ER) Stress: Plasma cells, including multiple myeloma cells, produce substantial immunoglobulins, creating exceptional ER protein-folding demands. The ER quality control system identifies misfolded proteins and targets them for proteasomal degradation. Proteasome inhibition causes accumulation of misfolded proteins within the ER, resulting in severe ER stress that initiates the UPR, ultimately triggering apoptosis when adaptive responses are overwhelmed.
Cell Cycle Arrest and Apoptosis Induction: Proteasome inhibitors disrupt the degradation of key cell cycle regulators such as cyclins and cyclin-dependent kinase inhibitors, causing cell cycle arrest. Additionally, they stabilize pro-apoptotic proteins including NOXA, BIM, and p53, while concurrently inhibiting anti-apoptotic factors, shifting the cellular balance toward programmed cell death.
c-Jun NH2-terminal Kinase (JNK) Activation: Proteasome inhibition leads to JNK pathway activation, resulting in caspase-8 and caspase-3 mediated apoptosis. This pathway can be further amplified through p53-MDM2 interactions that enhance JNK signaling.
The following diagram illustrates the key mechanistic pathways through which proteasome inhibitors induce apoptosis in cancer cells:
Experimental Approaches for Evaluating Proteasome Inhibitors
In Vitro Assessment of Proteasome Activity
Methodology for Proteasome Inhibition Profiling
The evaluation of proteasome inhibitor activity requires multifaceted experimental approaches that assess both enzymatic inhibition and functional cellular consequences. Standardized in vitro assays measure direct inhibition of proteasome catalytic subunits using fluorogenic substrates specific for each active site:
- Chymotrypsin-like (β5) Activity: Assessed using the substrate Suc-LLVY-AMC (N-succinyl-Leu-Leu-Val-Tyr-7-amido-4-methylcoumarin). Cleavage releases the fluorescent AMC group, with fluorescence intensity proportional to activity.
- Trypsin-like (β2) Activity: Measured using Bz-VGR-AMC (benzoyl-Val-Gly-Arg-7-amido-4-methylcoumarin).
- Caspase-like (β1) Activity: Evaluated using Z-LLE-AMC (N-carbobenzoxy-Leu-Leu-Glu-7-amido-4-methylcoumarin).
Enzyme kinetics are determined by incubating purified 20S proteasomes with varying inhibitor concentrations and monitoring time-dependent changes in fluorescence. IC50 values are calculated for each catalytic subunit to determine inhibitor specificity and potency.
Cell-Based Efficacy Assessment
Cellular models provide critical information on membrane permeability, intracellular stability, and functional consequences of proteasome inhibition:
- Cell Viability Assays: Multiple myeloma cell lines (e.g., RPMI-8226, U266, MM.1S) are treated with serial dilutions of proteasome inhibitors for 48-72 hours, with viability assessed via MTT, XTT, or ATP-based luminescence assays.
- Apoptosis Detection: Flow cytometric analysis of Annexin V/propidium iodide staining quantifies apoptotic populations following 24-48 hours of inhibitor treatment.
- Ubiquitinated Protein Accumulation: Western blot analysis of whole-cell lysates using anti-ubiquitin antibodies demonstrates target engagement through accumulation of high-molecular-weight ubiquitin conjugates.
- Biomarker Stabilization: Immunoblotting for specific proteasome substrates (e.g., p27, IκBα, NOXA) confirms functional inhibition at the molecular level.
In Vivo Evaluation and Translation to Clinical Trials
Animal Models for Efficacy Assessment
The transition from in vitro assessment to in vivo models typically employs human tumor xenografts in immunocompromised mice:
- Subcutaneous Xenograft Models: Multiple myeloma cell lines are implanted subcutaneously in NOD/SCID or athymic nude mice. Treatment begins after established tumor formation (100-200 mm³), with proteasome inhibitors administered intravenously or orally according to proposed clinical routes.
- Systemic Disseminated Models: For hematologic malignancies, more clinically relevant models involve intravenous injection of luciferase-expressing tumor cells, enabling bioluminescent monitoring of tumor burden and response to therapy.
- Patient-Derived Xenografts (PDX): Tumors obtained directly from patients are implanted and propagated in mice, potentially offering superior predictive value for clinical response.
Key Pharmacodynamic and Pharmacokinetic Parameters
In vivo studies focus on establishing relationships between drug exposure, proteasome inhibition, and antitumor efficacy:
- Proteasome Inhibition Pharmacodynamics: Blood and tissue samples are collected at various timepoints post-dose to measure proteasome activity levels, establishing the magnitude and duration of target inhibition.
- Drug Exposure Monitoring: Plasma pharmacokinetic profiling defines Cmax, Tmax, AUC, and elimination half-life, correlating drug exposure with both proteasome inhibition and antitumor activity.
- Therapeutic Index Determination: Dose-ranging studies identify minimally effective doses, optimal biological doses, and maximally tolerated doses based on body weight loss, hematologic parameters, and organ toxicity.
Table 2: Key Clinical Trial Endpoints for Proteasome Inhibitor Development
| Evaluation Category | Specific Endpoints | Clinical Significance |
|---|---|---|
| Efficacy Endpoints | Overall Response Rate (ORR), Complete Response (CR) Rate, Duration of Response (DoR), Progression-Free Survival (PFS), Overall Survival (OS) | Direct measures of clinical benefit and disease control |
| Safety Endpoints | Incidence and severity of adverse events (AEs), Serious AEs, laboratory abnormalities, dose reductions/discontinuations | Defines therapeutic window and manageability of toxicities |
| Pharmacodynamic Endpoints | Proteasome inhibition in blood and tissues, biomarker modulation (e.g., ubiquitinated proteins) | Confirmation of target engagement and biological activity |
| Pharmacokinetic Endpoints | C~max~, T~max~, AUC, half-life, clearance, volume of distribution | Characterization of drug exposure and disposition |
The Scientist's Toolkit: Essential Research Reagents and Methodologies
Advancing proteasome inhibitor research requires specialized reagents and methodologies that enable comprehensive evaluation of compound activity, mechanism of action, and therapeutic potential.
Table 3: Essential Research Reagents for Proteasome Inhibitor Evaluation
| Reagent Category | Specific Examples | Research Application |
|---|---|---|
| Proteasome Activity Probes | Fluorogenic substrates (Suc-LLVY-AMC, Bz-VGR-AMC, Z-LLE-AMC), Active-site directed probes | Quantification of proteasome inhibition potency and specificity |
| Cell Line Models | Multiple myeloma (RPMI-8226, U266, MM.1S), Mantle cell lymphoma (Jeko-1, Mino), Solid tumor panels | Assessment of cellular sensitivity, mechanism of action, and resistance |
| Antibodies for Biomarker Analysis | Anti-ubiquitin, anti-p27, anti-IκBα, anti-cleaved caspase-3, anti-NOXA, anti-p53 | Verification of target engagement and downstream pharmacological effects |
| Animal Models | Subcutaneous xenografts, Systemic disseminated models, Patient-derived xenografts (PDX) | In vivo efficacy assessment and pharmacokinetic/pharmacodynamic modeling |
| Analytical Standards | Reference compounds (bortezomib, carfilzomib), Metabolite standards, Isotopically labeled internal standards | Bioanalytical method development and validation for pharmacokinetic studies |
Emerging Directions and Next-Generation Agents
The clinical success of first-generation proteasome inhibitors has stimulated development of novel agents with improved properties and expanded applications. Several promising directions are currently being explored:
Novel Proteasome Inhibitors and Combination Strategies
Recent clinical advances include the approval of new combination regimens that enhance the efficacy of established proteasome inhibitors. The October 2025 FDA approval of belantamab mafodotin (Blenrep) combined with bortezomib and dexamethasone for relapsed multiple myeloma demonstrated a 51% reduction in risk of death and tripled median progression-free survival to 31.3 months compared to daratumumab-based regimens in the phase 3 DREAMM 7 trial. This combination strategy exemplifies the potential of targeted therapy combinations to significantly improve patient outcomes.
The clinical development of marizomib represents an effort to overcome limitations of existing proteasome inhibitors. Unlike bortezomib and carfilzomib, marizomib is an irreversible natural product inhibitor that crosses the blood-brain barrier and exhibits broad-spectrum inhibition across all three catalytic subunits, showing potential application in glioblastoma and other solid tumors.
Radioactive Ligand Therapies and Targeted Degradation Approaches
The convergence of proteasome inhibition principles with radiopharmaceutical development has created innovative therapeutic modalities. Radioligand therapies such as lutetium Lu 177 vipivotide tetraxetan (Pluvicto) represent a novel targeting approach for prostate cancer, delivering radiation directly to PSMA-positive cells. Recent phase 3 PSMAddition trial data presented in 2025 demonstrated that this agent combined with standard care reduced radiographic progression or death risk by 28% in PSMA-positive metastatic hormone-sensitive prostate cancer, with a favorable safety profile consistent with previous studies.
The following diagram illustrates the rapid evolution of targeted protein degradation therapies beyond traditional proteasome inhibition:
Addressing Resistance Mechanisms and Therapeutic Limitations
Despite significant clinical benefits, proteasome inhibitor resistance remains a substantial challenge. Research efforts focus on understanding and overcoming resistance through multiple strategies:
- Mutation-Driven Resistance: Mutations in the PSMB5 gene encoding the proteasome β5 subunit can decrease drug binding affinity. Next-generation inhibitors with distinct chemical structures maintain activity against some bortezomib-resistant mutants.
- Adaptive Cellular Responses: Upregulation of alternative protein degradation pathways, including aggressome formation and autophagy, represents a compensatory mechanism. Rational combination therapies targeting these parallel pathways show synergistic activity.
- Microenvironment-Mediated Resistance: Interactions with bone marrow stromal cells and other tumor microenvironment components can confer protective effects. Novel treatment approaches aim to disrupt these supportive interactions.
Additionally, efforts to mitigate characteristic toxicities of proteasome inhibitors, particularly peripheral neuropathy associated with bortezomib, include alternative dosing schedules, subcutaneous administration, and neuroprotective agents that maintain efficacy while improving tolerability.
The clinical validation of proteasome inhibitors represents a landmark achievement in translational cancer research, demonstrating the therapeutic potential of targeting protein homeostasis networks in malignant cells. From the foundational discoveries of the ubiquitin-proteasome system to the current development of sophisticated degradation technologies, this field continues to evolve through iterative cycles of basic scientific discovery and clinical innovation. The ongoing refinement of proteasome-directed therapies, expansion into novel indications, and development of combination strategies ensure that manipulation of the ubiquitin-proteasome pathway will remain a cornerstone of oncologic therapeutics. Future advances will likely focus on enhancing therapeutic index through improved targeting, overcoming resistance mechanisms, and personalizing treatment approaches based on molecular profiling of individual tumors.
The discovery of the Ubiquitin Proteasome System (UPS) unveiled a fundamental paradigm for regulated intracellular protein degradation. The pioneering work of Hershko, Ciechanover, and Rose in the 1980s, recognized with the 2004 Nobel Prize in Chemistry, identified the core enzymatic cascade—E1 (activating), E2 (conjugating), and E3 (ligating) enzymes—that tags proteins with ubiquitin for proteasomal destruction [2] [22]. This initial biochemical characterization was followed by foundational biological insights from Varshavsky's laboratory, which revealed the UPS's critical roles in cell cycle progression, DNA repair, and transcriptional regulation, establishing that controlled protein degradation rivals transcription and translation in physiological importance [2]. Over recent decades, research has progressively linked UPS dysregulation to cancer pathogenesis, creating a new frontier in oncology: the development of UPS-related gene expression signatures as powerful prognostic tools for predicting patient survival and therapeutic response [91] [92] [93].
UPS in Oncogenesis: Molecular Mechanisms and Pathways
The UPS exerts multifaceted influence on tumor development and progression through precise regulation of key oncoproteins and tumor suppressors. The stability of critical regulators such as p53, NF-κB, and various cyclins is directly controlled by ubiquitin-mediated degradation, creating a system that, when dysregulated, drives malignant transformation [22]. Notably, the UPS also governs the IAP (Inhibitor of Apoptosis) family of proteins, which contain RING domains functioning as E3 ubiquitin ligases to modulate caspase activity and cell survival pathways [22]. Tumor cells often exploit the Unfolded Protein Response (UPR), an interconnected stress-response pathway, to manage endoplasmic reticulum stress resulting from accelerated protein synthesis, further integrating UPS pathways with cancer cell survival mechanisms [91] [92].
Methodologies for Developing UPS-Based Prognostic Signatures
Data Acquisition and Gene Selection
The construction of UPS-related prognostic models relies on standardized computational workflows that leverage large-scale molecular datasets. Researchers typically obtain transcriptome profiles and corresponding clinical data from public repositories such as The Cancer Genome Atlas (TCGA) and Gene Expression Omnibus (GEO) [91] [92] [93]. UPS-related genes are curated from databases like MSigDB or GeneCards using relevant keyword searches ("unfolded protein response," "ubiquitin-mediated proteolysis") [91] [93]. Differential expression analysis between tumor and normal tissues identifies UPS genes with significant expression alterations in malignancy [93]. Univariate Cox regression then screens these genes for individual association with overall survival, retaining those with statistical significance (typically p < 0.01) for further model construction [91].
Signature Construction and Validation
Table 1: Statistical Methods for UPS Signature Development
| Method | Purpose | Key Parameters |
|---|---|---|
| LASSO-Cox Regression | Prevents overfitting by penalizing coefficients of non-informative genes; selects most predictive features | Lambda value determined via cross-validation |
| Multivariate Cox Regression | Calculates weighted coefficients for each gene in final signature; adjusts for confounding variables | Hazard ratios, 95% confidence intervals for each gene |
| Risk Score Formula | Calculates individual patient risk: Risk Score = Σ(Exprᵢ × Coefᵢ) | Expression value (Exprᵢ) and regression coefficient (Coefᵢ) for each gene |
| ROC Analysis | Evaluates predictive accuracy of signature over time | Area Under Curve (AUC) for 1, 3, 5-year survival |
| Kaplan-Meier Analysis | Compares survival between risk groups stratified by median risk score | Log-rank test p-value |
The core analytical process employs Least Absolute Shrinkage and Selection Operator (LASSO) Cox regression to identify the most informative gene subset while preventing model overfitting [91] [93]. Subsequently, multivariate Cox regression calculates weighted coefficients for each selected gene, generating a risk score formula: Risk Score = Σ(Expression of Geneᵢ × Coefficient of Geneᵢ) [91]. Patients are stratified into high-risk and low-risk groups based on the median risk score. The model's predictive performance is evaluated using time-dependent Receiver Operating Characteristic (ROC) curves and Kaplan-Meier survival analysis with log-rank testing [91] [93]. Validation in independent patient cohorts from GEO or other databases confirms the signature's robustness and generalizability [93].
Diagram 1: Workflow for developing and validating UPS prognostic signatures, showing key steps from data collection to clinical application.
Current UPS-Derived Prognostic Signatures Across Cancers
Hematologic Malignancies
In Acute Myeloid Leukemia (AML), a recent study established a 6-gene UPR-related signature that effectively stratifies patients into distinct risk categories with significantly different survival outcomes (5-year overall survival AUC = 0.912) [91]. The high-risk group demonstrated distinct tumor microenvironment characteristics, including enhanced immunosuppressive cell infiltration and potential resistance to conventional chemotherapy, but potentially greater sensitivity to immunotherapy [91]. This signature was integrated with clinical variables into a prognostic nomogram to enhance individualized survival prediction [91].
Solid Tumors
Table 2: UPS-Derived Prognostic Signatures in Solid Cancers
| Cancer Type | Signature Components | Prognostic Value | Clinical Implications |
|---|---|---|---|
| Glioblastoma | HSPA5, P4HB, PDIA4 (risk); MAPK8/JNK1 (protective) [92] | High-risk genes associated with poor survival [92] | Correlates with immunosuppressive microenvironment; potential therapeutic target |
| Breast Cancer | 8-gene UPR signature [93] | Stratifies patients into molecular subtypes with distinct outcomes [93] | Predicts immunotherapy response and chemotherapy sensitivity |
| Prostate Cancer | CCP score (Prolaris test) [94] | Predicts biochemical recurrence [94] | Guides treatment intensification or de-escalation decisions |
In Glioblastoma, a comprehensive transcriptional analysis identified HSPA5, P4HB, and PDIA4 as UPR-related risk genes, while MAPK8 (JNK1) emerged as a protective factor [92]. This signature not only predicts survival but also correlates with an immunosuppressive tumor microenvironment, particularly through IRE1α-XBP1 signaling axis activity [92]. For Breast Cancer, researchers developed molecular subtypes based on 10 differentially expressed UPR genes, subsequently constructing an 8-gene prognostic signature that correlates with immune infiltration patterns and predicted responses to both immunotherapy and chemotherapy [93].
Table 3: Key Research Reagents and Databases for UPS Prognostic Studies
| Resource | Type | Application in Prognostic Studies |
|---|---|---|
| TCGA Database | Molecular & clinical database | Primary source of tumor transcriptomes and patient outcomes [91] [92] |
| GEO Database | Molecular data repository | Independent validation cohorts [91] [93] |
| CIBERSORT | Computational algorithm | Deconvolution of immune cell infiltration from bulk RNA-seq [91] |
| ESTIMATE | Computational tool | Tumor microenvironment analysis (stromal/immune scores) [91] |
| pRRophetic | R package | Chemotherapy sensitivity prediction from gene expression [91] |
| GDSC | Drug sensitivity database | Reference data for therapy response prediction [91] |
| ConsensusClusterPlus | R package | Molecular subtype identification [91] |
| GeneCards | Gene database | UPR-related gene compilation [91] |
Experimental Protocols for UPS Signature Validation
Bioinformatics Validation Workflow
For differential expression analysis, researchers apply the R package "DESeq2" with thresholds typically set at |log2FC| ≥ 1 and adjusted p-value < 0.05 [91]. Functional enrichment analysis of the resulting gene sets is performed using "clusterProfiler" for Gene Ontology (GO) and Kyoto Encyclopedia of Genes and Genomes (KEGG) pathway analysis [91]. Gene Set Enrichment Analysis (GSEA) further elucidates biological pathways differentially activated between risk groups [91]. To evaluate tumor microenvironment differences, the CIBERSORT algorithm estimates immune cell fractions, while ESTIMATE calculates stromal, immune, and combined scores [91].
Laboratory Validation Approaches
While bioinformatics predictions provide powerful insights, experimental validation remains crucial for confirming the biological and clinical relevance of UPS signatures. Core genes identified in prognostic models require expression validation in clinical samples using quantitative RT-PCR and immunohistochemistry on independent patient cohorts [91]. For functional characterization, RNA interference (siRNA/shRNA)-mediated gene knockdown or CRISPR-Cas9 gene editing determines the effect of signature genes on cancer cell proliferation, apoptosis, and drug sensitivity in vitro [92]. To assess translational potential, patient-derived xenograft (PDX) models treated with UPS-targeting compounds (e.g., proteasome inhibitors) or standard chemotherapies can evaluate whether the signature predicts in vivo treatment response [22].
Diagram 2: UPS and UPR signaling pathway in cancer progression, showing how pathway activation leads to clinical outcomes through molecular and cellular changes.
The integration of UPS-related gene expression signatures into cancer prognosis represents a significant advancement in molecular oncology, transforming fundamental discoveries about protein degradation into clinically applicable tools. Current evidence demonstrates that these signatures provide robust prognostic stratification across diverse malignancies including AML, glioblastoma, and breast cancer, often surpassing conventional clinicopathological criteria [91] [92] [93]. Furthermore, UPS signatures offer insights into tumor microenvironment composition and potential therapy response, positioning them as valuable companions for personalized treatment selection [91] [93].
Future research directions should focus on standardizing analytical protocols across institutions, validating signatures in prospective clinical trials, and developing targeted therapeutics against high-risk UPS features [7]. The clinical translation of bortezomib for multiple myeloma and other hematologic malignancies established the precedent for targeting the UPS in cancer therapy [22] [7]. Next-generation approaches may involve combining UPS signatures with other molecular markers to create integrated prognostic models, potentially leveraging artificial intelligence for enhanced pattern recognition [95] [96]. As these tools mature, they promise to fulfill the vision of precise, biologically-informed cancer management initially inspired by the pioneering discoveries of the ubiquitin-proteasome system.
The ubiquitin-proteasome system (UPS) represents a fundamental regulatory mechanism governing intracellular protein turnover, with its discovery constituting a landmark achievement in biochemical research. Initially characterized as a primary conduit for selective intracellular protein degradation, the UPS is now recognized as a master regulator of virtually all cellular processes, extending far beyond its original conception as a mere disposal pathway [7] [97]. The system's core mechanism involves the covalent attachment of ubiquitin molecules to target proteins, which are subsequently recognized and degraded by the proteasome, a multi-subunit proteolytic complex [97]. This hierarchical organization enables precise control over protein half-lives, thereby influencing critical processes including cell cycle progression, gene expression, and stress responses [2] [97].
The historical trajectory of UPS research began with seminal discoveries in the late 1970s and early 1980s by Avram Hershko, Aaron Ciechanover, and Irwin Rose, who elucidated the enzymatic cascade—comprising E1 (activating), E2 (conjugating), and E3 (ligating) enzymes—responsible for ubiquitin conjugation [2]. This foundational work, recognized by the 2004 Nobel Prize in Chemistry, revealed the biochemical principles governing ATP-dependent protein degradation. Subsequent biological investigations, particularly from Alexander Varshavsky's laboratory, uncovered the profound physiological significance of ubiquitin-mediated proteolysis, demonstrating its essential roles in cell cycle regulation, DNA repair, and transcriptional control [2]. These discoveries catalyzed a paradigm shift in understanding cellular regulation, establishing that controlled protein degradation rivals transcriptional and translational mechanisms in significance for circuit control within cells [2].
In recent decades, research has progressively illuminated the indispensable functions of the UPS in immunological processes, positioning it as a crucial mediator of immune homeostasis and inflammation. The UPS governs both innate and adaptive immune responses by regulating key signaling molecules, transcription factors, and inflammatory mediators [98] [99]. This review will explore the validation of specific UPS components as therapeutic targets for immune and inflammatory disorders, emphasizing experimental approaches, methodological considerations, and translational applications within a historical framework of UPS research.
The Ubiquitin-Proteasome System: Molecular Architecture and Historical Foundations
Core Components and Enzymatic Cascade
The UPS operates through a coordinated enzymatic cascade that tags proteins for degradation with high specificity:
- E1 Ubiquitin-Activating Enzymes: Initiate ubiquitination by activating ubiquitin in an ATP-dependent manner, forming a thioester bond with ubiquitin's C-terminal glycine residue. This represents the committing step in the ubiquitination pathway [98] [99].
- E2 Ubiquitin-Conjugating Enzymes: Receive activated ubiquitin from E1 and collaborate with E3 ligases to facilitate ubiquitin transfer to target substrates. Humans possess approximately 40 E2 enzymes that help determine the type of ubiquitin chain topology [98].
- E3 Ubiquitin Ligases: Provide substrate specificity by recognizing target proteins and facilitating or directly catalyzing ubiquitin transfer from E2 to substrate. With over 600 members in humans, E3 ligases constitute the most diverse component of the system and include RING, HECT, and RBR domain families [98] [99].
- Deubiquitinases (DUBs): Counteract ubiquitination by removing ubiquitin from modified proteins, providing an additional layer of regulation. DUBs help maintain free ubiquitin pools and can rescue proteins from degradation [98] [99].
- Proteasome: A multi-subunit proteolytic complex that recognizes and degrades polyubiquitinated proteins. The 26S proteasome consists of a 20S core particle (containing proteolytic active sites) and 19S regulatory particles that recognize ubiquitinated substrates, remove ubiquitin chains, unfold target proteins, and translocate them into the catalytic core [97].
The specificity of ubiquitin signaling is further enhanced by the diversity of ubiquitin chain linkages. Ubiquitin contains eight potential acceptor sites (Met1, Lys6, Lys11, Lys27, Lys29, Lys33, Lys48, and Lys63), with different chain topologies encoding distinct functional consequences [98] [99]. While K48-linked chains predominantly target substrates for proteasomal degradation, K63-linked chains typically mediate non-proteolytic signaling events in immune and inflammatory pathways [99]. Other atypical linkages (K6, K11, K27, K29, K33) continue to have their specialized functions elucidated.
Table 1: Major Ubiquitin Chain Linkages and Their Functional Roles in Immunity
| Linkage Type | Primary Function | Role in Immune Signaling | Key E3 Ligases |
|---|---|---|---|
| K48-linked | Proteasomal degradation | Controls stability of transcription factors (NF-κB, IRFs), signaling adapters | Various E3s |
| K63-linked | Non-proteolytic signaling | Regulates kinase activation, protein-protein interactions in TLR, TNF-R pathways | TRAF6, TRAF3 |
| Linear (M1-linked) | NF-κB pathway regulation | NEMO modification, NF-κB activation | LUBAC complex |
| K11-linked | Proteasomal degradation | Cell cycle regulation, immune cell development | UBE2S, APC/C |
| K29-linked | Proteasomal degradation | Wnt signaling, potential immune functions | UBE3C, HUL5 |
Historical Perspective: Key Discoveries Elucidating the UPS
The elucidation of the UPS represents a compelling narrative of scientific discovery, beginning with unexpected observations and culminating in a fundamental biological paradigm:
1977-1980: Initial Discoveries
- Goldberg and Etlinger identified ATP-dependent protein degradation in reticulocyte extracts, challenging the prevailing view that lysosomes were the primary site of intracellular proteolysis [97].
- Hershko, Ciechanover, and Rose discovered ATP-dependent proteolysis factor 1 (APF-1), later identified as ubiquitin, which became covalently conjugated to protein substrates prior to degradation [2] [97].
- Wilkinson, Urban, and Haas established the identity between APF-1 and ubiquitin, previously known as a chromatin-associated protein of unknown function, thereby unifying two previously separate research avenues [2].
1980-1983: Enzymatic Machinery Elucidation
- Hershko and colleagues systematically identified and characterized the three-enzyme cascade (E1, E2, E3) responsible for ubiquitin conjugation, establishing the biochemical framework for substrate specificity [2].
- Simultaneously, Varshavsky's laboratory discovered that ubiquitin-histone conjugates were enriched in transcriptionally active chromatin regions, hinting at regulatory functions beyond bulk protein degradation [2].
1984-1990: Biological Significance Uncovered
- Varshavsky's group made seminal contributions to understanding the biological roles of ubiquitination, including identification of the N-end rule pathway, discovery of polyubiquitin chains, and demonstration of the UPS's essential functions in cell cycle progression and stress responses [2].
- The development of genetic approaches in yeast established the UPS as an essential system with specific physiological functions, moving beyond biochemical observations to physiological relevance [2].
1990s-Present: Mechanistic Refinement and Therapeutic Exploration
- The 26S proteasome was characterized as the downstream effector of ubiquitin signaling [2].
- Baumeister's group utilized cryo-electron microscopy to resolve proteasome architecture, providing structural insights into substrate recognition, unfolding, and degradation mechanisms [97].
- The immunoproteasome was identified as a specialized form induced by inflammatory cytokines, optimizing antigen processing for MHC class I presentation [97].
- Dysregulated UPS components were increasingly linked to autoimmune, inflammatory, and other pathological conditions, opening new therapeutic avenues [98] [99].
Diagram 1: UPS Mechanism and Historical Discovery Timeline
Methodological Framework: Experimental Approaches for Validating UPS Targets
Target Identification and Genetic Validation
The initial validation of UPS components as therapeutic targets in immune disorders employs multifaceted experimental approaches:
Genetic Manipulation Techniques:
- RNA Interference (RNAi): Systematic knockdown of E3 ligases, DUBs, or proteasome subunits in immune cells (macrophages, dendritic cells, T cells) followed by functional assessment of inflammatory responses. For example, siRNA-mediated silencing of TRAF6 impairs TLR4-mediated NF-κB activation and proinflammatory cytokine production [98] [99].
- CRISPR-Cas9 Gene Editing: Generation of knockout immune cell lines or primary cells to evaluate the consequences of specific UPS component ablation. CRISPR-edited macrophages lacking A20 (TNFAIP3) exhibit amplified NF-κB signaling and heightened production of IL-6, IL-1β, and TNF-α upon stimulation [99].
- Transgenic Animal Models: Tissue-specific conditional knockout mice (e.g., myeloid-specific A20 deletion, T cell-specific Cbl-b deficiency) to assess UPS functions in physiological immune contexts. These models demonstrate cell-type-specific effects and have revealed that A20 deficiency in dendritic cells lowers activation thresholds and promotes autoimmune phenotypes [99].
Functional Readouts:
- Signaling Pathway Activation: Western blot analysis of phosphorylated kinases (IKK, p38, JNK) and NF-κB translocation in response to pathogen-associated molecular patterns (PAMPs) or cytokines.
- Cytokine/Chemokine Production: Multiplex ELISA or cytometric bead array quantification of secreted mediators (IL-1β, IL-6, TNF-α, IL-8, IFN-β) following stimulation.
- Immune Cell Differentiation: Flow cytometric analysis of T helper cell subsets (Th1, Th2, Th17, Treg) following E3 ligase perturbation, assessing master transcription factors (T-bet, GATA3, RORγt, FoxP3) and signature cytokines.
Table 2: Key Experimental Models for UPS Target Validation in Immune Disorders
| Experimental System | Key Applications | Advantages | Limitations |
|---|---|---|---|
| Immortalized macrophage/monocyte cell lines (RAW264.7, THP-1) | High-throughput screening of UPS inhibitors; siRNA screening | Reproducible, scalable, genetically tractable | May not fully recapitulate primary cell physiology |
| Primary human peripheral blood mononuclear cells (PBMCs) | Translationally relevant mechanistic studies | Human-derived, multiple cell types, donor variability | Limited expansion capacity, donor-to-donor variability |
| Mouse models of autoimmunity (collagen-induced arthritis, EAE) | In vivo validation of target relevance | Complex pathophysiology, therapeutic assessment | Species differences in immune regulation |
| Conditional knockout mice | Cell-type-specific functions of UPS components | Physiological context, temporal control | Potential developmental compensation |
| Human patient-derived samples (synovial fluid, PBMCs) | Confirmation of clinical relevance | Direct human disease relevance, biomarker identification | Limited availability, confounding factors |
Biochemical and Molecular Validation
Protein-Protein Interaction Mapping:
- Co-immunoprecipitation (Co-IP) and Pull-Down Assays: Identify physical interactions between E3 ligases and putative substrates in immune signaling pathways. For instance, TRAF6 interacts with IRAK1 following IL-1R/TLR stimulation, facilitating K63-linked ubiquitination that enables TAK1 and IKK complex recruitment [98].
- Mass Spectrometry-Based Interactomics: Comprehensive profiling of E3 ligase complexes and ubiquitinated substrates under resting and activated conditions in immune cells.
Ubiquitination Status Assessment:
- In Vivo and In Vitro Ubiquitination Assays: Direct examination of substrate ubiquitination using epitope-tagged ubiquitin (HA-, FLAG-, Myc-Ub) in combination with mutation of specific lysine residues (K48R, K63R) to determine chain topology.
- Tandem Ubiquitin Binding Entity (TUBE) Pulldown: Enrichment and identification of endogenous ubiquitinated proteins to monitor changes in global ubiquitination or specific substrate modification in response to stimuli.
Structural Characterization:
- X-Ray Crystallography and Cryo-EM: Determination of atomic-level interactions between E3 ligases and their substrates, informing rational drug design. Structural analysis of the NEMO-ubiquitin complex revealed how linear ubiquitin binding activates IKK signaling [97].
- Hydrogen-Deuterium Exchange Mass Spectrometry (HDX-MS): Mapping conformational dynamics of UPS components upon binding to substrates or small-molecule inhibitors.
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Research Reagents for Investigating UPS in Immune Regulation
| Reagent Category | Specific Examples | Research Applications | Technical Considerations |
|---|---|---|---|
| E3 Ligase Inhibitors | LCL161 (IAP antagonist), Nutlin-3 (MDM2 inhibitor) | Functional validation of specific E3 ligases in immune signaling | Potential off-target effects; use multiple chemical scaffolds for confirmation |
| Proteasome Inhibitors | Bortezomib, MG132, Carfilzomib | Assess dependency on proteasomal degradation in immune responses | Distinguish immunoproteasome vs. constitutive proteasome inhibition |
| Activity-Based Probes | Ubiquitin-VS, HA-Ub-VME | Profiling deubiquitinase activities in immune cell lysates | Require specialized mass spectrometry analysis |
| Ubiquitin Binding Domains | UBA, UIM, UBZ, NZF domains | Detection and purification of specific ubiquitin chain types | Varying affinities for different chain linkages |
| K48/K63 Linkage-Specific Antibodies | Anti-K48-Ub, Anti-K63-Ub | Discrimination of degradative vs. signaling ubiquitination | Potential cross-reactivity; validate with linkage-specific DUBs |
| DUB Inhibitors | PR-619 (pan-DUB inhibitor), P5091 (USP7 inhibitor) | Investigate DUB functions in immune regulation | Broad vs. selective inhibition profiles |
| Ubiquitin Expression Plasmids | Wild-type and lysine-less ubiquitin mutants | Define chain topology requirements in signaling pathways | Transfection efficiency varies among primary immune cells |
| UPS Reporter Cell Lines | NF-κB, IRF, AP-1 luciferase reporters | High-throughput screening of UPS modulators | Reporter amplification may not reflect endogenous regulation |
Validated UPS Targets in Immune and Inflammatory Disorders
E3 Ubiquitin Ligases as Central Immune Regulators
E3 ubiquitin ligases confer substrate specificity within the UPS and have emerged as particularly promising therapeutic targets due to their selective functions in immune pathways:
TRAF6 (TNF Receptor-Associated Factor 6):
- Mechanism: RING-type E3 ligase that catalyzes K63-linked ubiquitination of key signaling molecules (IRAK1, TAK1 complex, NEMO) downstream of TLR/IL-1R signaling and antigen receptors, facilitating kinase activation and NF-κB/MAPK pathway induction [98] [99].
- Validation Evidence: Macrophage-specific TRAF6 deletion impairs proinflammatory cytokine production in response to multiple PAMPs. TRAF6 inhibition ameliorates disease severity in murine models of rheumatoid arthritis and lupus [99].
- Therapeutic Implications: Small-molecule TRAF6 inhibitors show efficacy in preclinical autoimmunity models but face challenges related to specificity and potential immunosuppression.
Cbl-b (Casitas B-Lymphoma Proto-Oncogene b):
- Mechanism: RING E3 ligase that ubiquitinates key signaling intermediates (PI3K, PKC-θ, PLC-γ1) downstream of TCR and CD28, establishing activation thresholds in T cells and maintaining peripheral tolerance [98] [100].
- Validation Evidence: Cbl-b-deficient T cells exhibit lowered activation thresholds and resistance to anergy induction. Cbl-b^-/- mice develop spontaneous autoimmunity and show enhanced antitumor immunity [98].
- Therapeutic Implications: Cbl-b inhibition represents a strategy to enhance CAR-T cell efficacy against solid tumors, though careful calibration is required to avoid autoimmune adverse effects.
A20 (TNFAIP3):
- Mechanism: Functions as both a DUB (removing K63 chains from signaling intermediates) and an E3 ligase (assembling K48 chains on the same targets), thereby terminating NF-κB activation downstream of multiple receptors (TNFR, TLR, NLR) [99].
- Validation Evidence: A20 polymorphisms associate with numerous autoimmune diseases (SLE, RA, psoriasis). Myeloid-specific A20 deletion causes systemic inflammation, while T cell-specific deletion enhances antitumor responses [99].
- Therapeutic Implications: A20 enhancement strategies may benefit autoimmune conditions, whereas partial inhibition could potentiate anticancer immunity.
TRIM Family Proteins:
- Mechanism: Numerous TRIM E3 ligases regulate innate immune signaling pathways. TRIM21 functions as an intracellular Fc receptor that ubiquitinates antibody-bound viral proteins, while TRIM27 negatively regulates TBK1/IRF3 signaling in antiviral responses [98].
- Validation Evidence: TRIM21 deficiency impairs antibody-dependent intracellular neutralization of viruses. TRIM27 silencing enhances type I IFN production and reduces viral replication [98].
- Therapeutic Implications: TRIM21 agonists might enhance intracellular pathogen clearance, while TRIM27 inhibitors could bolster antiviral responses.
UPS Regulation of Specific Immune Signaling Pathways
Diagram 2: UPS Regulation of Innate Immune Signaling (TLR/IL-1R Pathways)
NF-κB Signaling Pathway: The transcription factor NF-κB serves as a master regulator of inflammation, and its activation is extensively controlled by ubiquitination at multiple levels:
- Activation: K63-linked and linear ubiquitination events (mediated by TRAF6, LUBAC) facilitate IKK complex recruitment and activation [98] [99].
- Termination: Multiple E3 ligases (A20, ITCH) and DUBs (CYLD, OTULIN) provide negative feedback regulation by modifying signaling components [99].
- Experimental Validation: Co-immunoprecipitation assays demonstrate stimulus-dependent interactions between IKK components and E3 ligases/DUBs. Pharmacological proteasome inhibition blocks NF-κB activation by preventing IκBα degradation, confirming UPS dependence [99].
Inflammasome Regulation: The UPS governs inflammasome activation at multiple checkpoints:
- NLRP3 Stability: The E3 ligase TRIM31 promotes K48-linked ubiquitination and proteasomal degradation of NLRP3, while the DUB BRCC3 removes inhibitory ubiquitin chains to facilitate activation [99].
- Pro-IL-1β and Pro-IL-18 Processing: The immunoproteasome generates antigenic peptides but also cleaves pro-cytokines, linking adaptive and innate immunity [97].
- Experimental Approaches: Bone marrow-derived macrophages from immunoproteasome-deficient mice exhibit impaired IL-1β and IL-18 production following NLRP3 activation [97].
T Cell Activation and Differentiation:
- TCR Signaling: Multiple E3 ligases (Cbl-b, ITCH, GRAIL) establish activation thresholds by ubiquitinating TCR signaling components [98].
- Cytokine Signaling: The E3 ligase CUL5 targets phosphorylated JAK1 for degradation, influencing CD4+ T cell fate decisions toward Treg differentiation [98].
- Lineage Specification: SMURF1 ubiquitinates RORγt, limiting Th17 differentiation, while USP7 stabilizes FoxP3, enhancing Treg suppressive function [99].
- Experimental Validation: Intracellular cytokine staining and phospho-flow cytometry in T cells with genetically or pharmacologically perturbed UPS components reveal altered differentiation patterns and effector functions [98] [99].
UPS Dysregulation in Specific Autoimmune Diseases
Rheumatoid Arthritis (RA):
- E3 Ligases: ZNRF3 influences TNF-α, IL-1β, and IL-6 production in collagen-induced arthritis models. TRIM18 promotes synoviocyte proliferation and inflammatory cytokine secretion by targeting DPP4 for degradation [99].
- DUBs: USP5 promotes NF-κB activation and proinflammatory cytokine production in RA synovium [99].
- Therapeutic Implications: Proteasome inhibitors (bortezomib) show efficacy in refractory RA patients, particularly those with autoreactive plasma cell involvement.
Systemic Lupus Erythematosus (SLE):
- E2 Enzymes: UBE2L3 polymorphism associates with SLE risk, potentially by enhancing LUBAC-mediated NF-κB activation [99].
- E3 Ligases: TRIM21 suppresses NF-κB via monoubiquitination of phosphorylated IKKβ. FBXW7 promotes apoptosis by degrading the antiapoptotic protein MCL1 [99].
- DUBs: USP8 enhances the cGAS-STING pathway, while MYSM1 suppresses it, creating a regulatory balance in nucleic acid sensing [99].
Antiphospholipid Syndrome (APS):
- Pathogenic Mechanism: APS follows a "second hit" model where antiphospholipid antibodies (aPLs) require cofactors (infection, inflammation) to trigger thrombosis. The UPS regulates multiple steps in this process [99].
- E3 Ligases: TRAF6 participates in TLR4/tissue factor signaling pathways that promote thrombosis [99].
- DUBs: A20 determines activation thresholds in dendritic cells through modulation of canonical NF-κB signaling [99].
- Therapeutic Evidence: Low-dose proteasome inhibitors attenuate proinflammatory factor production and clinical manifestations in APS models [99].
Therapeutic Translation: Targeting the UPS in Immune Disorders
Established Modalities
Proteasome Inhibitors:
- First-Generation Agents: Bortezomib, a dipeptidyl boronic acid derivative, reversibly inhibits the chymotrypsin-like activity of the proteasome. Originally developed for multiple myeloma, bortezomib demonstrates efficacy in antibody-mediated autoimmune conditions (lupus nephritis, antiphospholipid syndrome) by targeting plasma cells for apoptosis [99].
- Second-Generation Agents: Carfilzomib, an epoxyketone irreversible inhibitor, shows improved specificity for the proteasome and reduced neurotoxicity. Carfilzomib effectively depletes autoreactive plasma cells in refractory SLE patients [99].
- Immunoproteasome-Selective Inhibitors: Compounds like KZR-616 preferentially target the immunoproteasome over constitutive proteasome, potentially offering improved therapeutic indices for autoimmune applications [97].
Emerging Targeted Protein Degradation Approaches:
PROTACs (Proteolysis-Targeting Chimeras):
- Molecular Architecture: Heterobifunctional molecules comprising a target-binding warhead, an E3 ligase recruiter, and a connecting linker. PROTACs induce proximity between the target protein and E3 ligase, leading to polyubiquitination and proteasomal degradation [100].
- Advantages Over Inhibitors: Event-driven rather than occupancy-driven pharmacology; ability to target non-enzymatic functions, scaffolding properties, and mutated proteins; potential to overcome resistance mechanisms [100].
- Immune Applications: IRAK4, BTK, and TYK2 PROTACs have shown promising results in preclinical models of autoimmune and inflammatory diseases [100].
Molecular Glues:
- Mechanism: Small molecules that induce or stabilize interactions between E3 ligases and target proteins, often by modifying the ligase's substrate-recognition surface [7].
- Therapeutic Examples: Clinically approved immunomodulatory drugs (thalidomide, lenalidomide, pomalidomide) function as molecular glues that redirect CRL4^CRBN E3 ligase activity toward transcription factors Ikaros and Aiolos in lymphocytes, leading to their degradation and immunomodulatory effects [7].
Table 4: UPS-Targeting Therapeutics in Development for Immune Disorders
| Therapeutic Class | Representative Agents | Molecular Target | Development Stage | Key Applications |
|---|---|---|---|---|
| Immunoproteasome Inhibitors | KZR-616 | Immunoproteasome β1i/β5i subunits | Phase II clinical trials | Lupus, inflammatory myositis |
| IRAK4 PROTACs | KT-474 | IRAK4 degradation via recruited E3 ligase | Phase I clinical trials | Hidradenitis suppurativa, atopic dermatitis |
| BTK PROTACs | DD-03-171 | BTK degradation | Preclinical development | Autoantibody-mediated diseases |
| TYK2 Molecular Glues | Deucravacitinib | TYK2 pseudokinase domain (allosteric inhibition) | FDA-approved | Psoriasis, psoriatic arthritis |
| LUBAC Inhibitors | HOIPIN-8 | Linear ubiquitin chain assembly | Preclinical development | Inflammation, immune activation |
| Cbl-b Inhibitors | Nx-1607 | Cbl-b E3 ligase activity | Phase I clinical trials | Oncology, potentially autoimmunity |
Experimental Protocols for Evaluating UPS-Targeting Therapeutics
PROTAC Validation Workflow:
- Cellular Target Engagement: Western blot analysis of target protein levels following PROTAC treatment across a concentration range (typically 1 nM-10 μM) and time course (2-48 hours) in relevant immune cell types.
- Specificity Assessment: Quantitative proteomics (TMT, SILAC) to evaluate global protein abundance changes, confirming on-target degradation while identifying potential off-target effects.
- Mechanistic Confirmation:
- Co-treatment with proteasome inhibitors (MG132, bortezomib) or neddylation inhibitors (MLN4924) to confirm proteasome-dependence.
- CRISPR-mediated knockout of the recruited E3 ligase to establish mechanism specificity.
- Use of target-binding competitive antagonists to confirm that degradation requires target engagement.
- Functional Immune Assays:
- Cytokine production (ELISA, multiplex arrays) following pathogen-associated molecular pattern (PAMP) or cytokine stimulation.
- Immune cell differentiation (Th1/Th2/Th17 polarization, Treg induction) assessed by flow cytometry.
- Phagocytosis, antigen presentation, or chemotaxis assays as relevant to target biology.
- In Vivo Efficacy: Assessment in relevant disease models (collagen-induced arthritis, experimental autoimmune encephalomyelitis, lupus-prone mice) with monitoring of disease severity, autoantibody production, and target engagement in tissues.
Pharmacodynamic Biomarker Assessment:
- Direct Target Modulation: Measurement of target protein levels in peripheral blood mononuclear cells (PBMCs) or specific immune cell subsets via flow cytometry, Western blot, or targeted mass spectrometry.
- Pathway Activity Readouts: Phospho-flow cytometry for key signaling intermediates (pSTAT, pIKB, p-p38) following ex vivo stimulation.
- Functional Immune Biomarkers: Antigen-specific T cell responses, serum cytokine levels, autoantibody titers, or acute phase reactants.
The ubiquitin-proteasome system has evolved from a fundamental protein degradation pathway to a recognized master regulator of immune homeostasis. The historical trajectory of UPS research—from initial biochemical characterization to current therapeutic targeting—exemplifies how fundamental biological discoveries can transform therapeutic landscapes. The validation of specific UPS components in immune and inflammatory disorders has created unprecedented opportunities for targeted therapeutic interventions that move beyond broad immunosuppression.
Future directions in this field will likely focus on several key areas:
- Cell-Type Specific Targeting: Developing approaches to selectively modulate UPS components in specific immune cell subsets while sparing others to maintain protective immunity.
- Temporal Precision: Designing therapeutic strategies that account for the dynamic, context-dependent functions of many UPS components in immune responses.
- Combination Approaches: Rational pairing of UPS-targeting agents with biologicals or small molecules to achieve synergistic efficacy while minimizing toxicity.
- Biomarker-Driven Patient Selection: Identifying predictive biomarkers to match specific UPS pathologies with corresponding targeted therapies.
The continued exploration of UPS functions in immunoregulation, coupled with advances in therapeutic modalities like PROTACs and molecular glues, promises to yield increasingly precise and effective treatments for autoimmune, inflammatory, and other immune-mediated disorders. As our understanding of ubiquitin signaling complexity deepens, so too will our ability to therapeutically harness this system to restore immune homeostasis in human disease.
Conclusion
The journey to elucidate the ubiquitin-proteasome system transformed our understanding of cellular regulation, revealing that controlled protein degradation is as critical as protein synthesis. The foundational discoveries of the 1980s, which initially explained a basic biochemical process, have now matured into a vibrant field with profound clinical implications. The successful translation of proteasome inhibitors into life-saving drugs for multiple myeloma, coupled with the revolutionary potential of PROTACs and molecular glues, validates the UPS as a premier target for therapeutic intervention. Future directions will focus on overcoming drug resistance, expanding the repertoire of druggable E3 ligases, and applying targeted degradation to previously 'undruggable' targets in oncology, neurodegenerative diseases, and beyond. The continued exploration of the UPS promises to yield a next generation of precision medicines, firmly establishing this pathway as a cornerstone of modern biomedical research and drug discovery.
References
- 1. The Nobel Prize in Chemistry 2004 - Popular information [https://www.nobelprize.org/prizes/chemistry/2004/popular-information/]
- 2. The early history of the ubiquitin field - PMC - PubMed Central [https://pmc.ncbi.nlm.nih.gov/articles/PMC2249785/]
- 3. Discovery of Cellular Regulation by Protein Degradation - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC3259866/]
- 4. Discovering the Ubiquitin Proteolytic System [https://rainmaker.uthsc.edu/discovering-the-ubiquitin-proteolytic-system/]
- 5. A conversation with Aaron Ciechanover [https://www.jci.org/articles/view/71859]
- 6. A Simple, Quick, and Scalable Route to Fluorogenic ... [https://pubmed.ncbi.nlm.nih.gov/40797270/]
- 7. From Discovery to Bedside: Targeting the Ubiquitin System [https://www.sciencedirect.com/science/article/pii/S2451945618303829]
- 8. Researchers discover new way to study protein, could lead ... [https://news.ohsu.edu/2025/03/31/researchers-discover-new-way-to-study-protein-could-lead-to-new-treatments-for-immune-system-diseases]
- 9. Protein ubiquitination involving an E1-E2-E3 enzyme ... [https://pubmed.ncbi.nlm.nih.gov/7800044/]
- 10. Measuring activity in the ubiquitin-proteasome system [https://pmc.ncbi.nlm.nih.gov/articles/PMC3758771/]
- 11. The ubiquitin system: from cell signalling to disease ... [https://www.nature.com/articles/s41418-020-00703-w]
- 12. Ubiquitin-Proteasome System [https://lifesensors.com/ubiquitinproteasomesystem/]
- 13. Structural Dissection of a Gating Mechanism Preventing ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC2587436/]
- 14. Orthogonal Ubiquitin Transfer through Engineered E1-E2 ... [https://www.sciencedirect.com/science/article/pii/S1074552112002888]
- 15. Quantitative Profiling of Ubiquitylated Proteins Reveals ... [https://www.sciencedirect.com/science/article/pii/S1535947620319228]
- 16. Dissecting Distinct Roles of NEDDylation E1 Ligase ... [https://www.nature.com/articles/s41598-018-28214-2]
- 17. Quantitative mapping of proteasome interactomes and ... [https://elifesciences.org/articles/93256]
- 18. chemical structures and their potential for drug discovery [https://pubs.rsc.org/en/content/articlelanding/2025/np/d5np00004a]
- 19. What history tells us XLI. Ubiquitin and proteolysis [https://link.springer.com/article/10.1007/s12038-016-9634-9]
- 20. Regulation of histone modifying enzymes by the ubiquitin ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3966433/]
- 21. Targeted protein degradation: mechanisms, strategies and ... [https://www.nature.com/articles/s41392-022-00966-4]
- 22. Discovery of the ubiquitin proteasome system and its ... [https://www.nature.com/articles/4401740]
- 23. Histone Ubiquitination - an overview [https://www.sciencedirect.com/topics/neuroscience/histone-ubiquitination]
- 24. Mechanisms of Ubiquitin-Nucleosome Recognition and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5523955/]
- 25. Ubiquitin: Same Molecule, Different Degradation Pathways [https://www.sciencedirect.com/science/article/pii/S0092867410012924]
- 26. Targeted Protein Degradation via Lysosomes - PubMed Central [https://pmc.ncbi.nlm.nih.gov/articles/PMC10245383/]
- 27. 20 Years of the Ubiquitin Revolution: Honoring Nobel ... [https://fox59.com/business/press-releases/globenewswire/9525585/20-years-of-the-ubiquitin-revolution-honoring-nobel-laureate-professor-avram-hershko-and-the-future-of-targeted-protein-degradation]
- 28. An Overview of the Current State of Cell Viability ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11719996/]
- 29. Overview of Cell Viability and Survival [https://www.cellsignal.com/science-resources/cell-viability-and-survival?srsltid=AfmBOoqOuOdH_S-vn9DzbQj3WsfnX87ZygqbphwzAcYEeCnUd5U2QEyM]
- 30. Assessment and comparison of viability assays for cellular ... [https://www.sciencedirect.com/science/article/pii/S1465324923011003]
- 31. Discovery of Novel Proteasome Inhibitors Using a High ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC2797363/]
- 32. An historic perspective of proteasome inhibition [https://pubmed.ncbi.nlm.nih.gov/22726542/]
- 33. Mechanistic insights into proteasome inhibitor MG132 ... [https://www.nature.com/articles/s41598-025-99151-0]
- 34. Efficacy of Bortezomib as First-Line Treatment for Patients with ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3588852/]
- 35. Real-Life Experience With First-Line Therapy Bortezomib ... [https://www.frontiersin.org/journals/medicine/articles/10.3389/fmed.2021.712070/full]
- 36. Proteasome Inhibitors Market Size & Share Report, 2025 [https://www.gminsights.com/industry-analysis/proteasome-inhibitors-market]
- 37. Proteasome Inhibitors Market Size 2025-2029 [https://www.technavio.com/report/proteasome-inhibitors-market-industry-size-analysis]
- 38. Proteolysis‐Targeting Chimera (PROTAC) - PubMed Central [https://pmc.ncbi.nlm.nih.gov/articles/PMC12495453/]
- 39. Review Molecular glues and PROTACs in targeted protein ... [https://www.sciencedirect.com/science/article/abs/pii/S0006295225005623]
- 40. Molecular glue-mediated targeted protein degradation [https://pmc.ncbi.nlm.nih.gov/articles/PMC11409024/]
- 41. PROTACs and MGDs role in drug discovery [https://www.news-medical.net/whitepaper/20250915/What-makes-PROTACs-and-MGDs-game-changers-in-drug-discovery.aspx]
- 42. Molecular Glues in Targeted Protein Degradation [https://www.sygnaturediscovery.com/news-and-events/blog/devil-in-a-glue-dress-molecular-glues-in-targeted-protein-degradation/]
- 43. Molecular Glues: A New Dawn After PROTAC [https://www.biochempeg.com/article/271.html]
- 44. The proteasome and proteasome in inhibitors multiple myeloma [https://pubmed.ncbi.nlm.nih.gov/29196868/]
- 45. For Proteasome in the Real World... Inhibitors Multiple Myeloma [https://www.linkedin.com/pulse/proteasome-inhibitors-multiple-myeloma-teswc]
- 46. Show Promise as Treatment for Proteasome ... Inhibitors Multiple [https://www.ajmc.com/view/proteasome-inhibitors-show-promise-as-treatment-for-multiple-myeloma]
- 47. Treatment: Breakthroughs & Future Innovations Multiple Myeloma [https://www.delveinsight.com/blog/latest-breakthroughs-multiple-myeloma-treatment]
- 48. Cereblon E3 ligase modulator [https://en.wikipedia.org/wiki/Cereblon_E3_ligase_modulator]
- 49. The E3 ubiquitin ligase component, Cereblon, is an ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8421366/]
- 50. Discovery of E3 Ligase Ligands for Target Protein Degradation [https://pmc.ncbi.nlm.nih.gov/articles/PMC9573645/]
- 51. VHL gene deletion+duplication and full mutation analysis ... [https://loinc.org/82533-1]
- 52. Familial erythrocytosis type 2 due to VHL germline mutations [https://pmc.ncbi.nlm.nih.gov/articles/PMC11886440/]
- 53. Hijacking the MDM2 E3 Ligase with Novel BRD4 ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12247027/]
- 54. Targeting the inhibitors of apoptosis proteins (IAPs) to ... [https://www.frontiersin.org/journals/pharmacology/articles/10.3389/fphar.2025.1562167/full]
- 55. IAPs as E3 ligases of Rac1: Shaping the move - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC3408978/]
- 56. The molecular mechanisms of acquired proteasome inhibitor ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3521846/]
- 57. Drug Development Targeting the Ubiquitin–Proteasome ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7226376/]
- 58. Mechanisms of proteasome inhibitor action and resistance ... [https://www.sciencedirect.com/science/article/abs/pii/S1368764608000472]
- 59. Different Strategies to Overcome Resistance ... [https://www.mdpi.com/1422-0067/25/16/8949]
- 60. A comprehensive bibliometric analysis - PMC - PubMed Central [https://pmc.ncbi.nlm.nih.gov/articles/PMC12419283/]
- 61. Suppressing protein damage response to overcome ... [https://www.nature.com/articles/s41421-025-00826-9]
- 62. exploring the ubiquitin system for drug development [https://www.nature.com/articles/cr201631]
- 63. Proteasome inhibition overcomes resistance to targeted ... [https://www.nature.com/articles/s41419-025-07884-7]
- 64. October - November 2025: What's New in Myeloma? [https://www.myeloma.org/blog/october-november-2025-whats-new-myeloma]
- 65. PROTACs: Past, Present and Future - PMC - PubMed Central [https://pmc.ncbi.nlm.nih.gov/articles/PMC10237031/]
- 66. Current strategies for the design of PROTAC linkers [https://pmc.ncbi.nlm.nih.gov/articles/PMC9400730/]
- 67. Characteristic roadmap of linker governs the rational ... [https://www.sciencedirect.com/science/article/pii/S2211383524001357]
- 68. Crystal structures of DCAF1-PROTAC-WDR5 ternary ... [https://www.nature.com/articles/s41467-024-54500-x]
- 69. Linker-free PROTACs efficiently induce the degradation of ... [https://www.nature.com/articles/s41467-025-60107-7]
- 70. HADDOCK-Guided modeling and molecular simulations of ... [https://www.sciencedirect.com/science/article/pii/S0010482525009217]
- 71. PROTAC targeted protein degraders: the past is prologue [https://www.nature.com/articles/s41573-021-00371-6]
- 72. The role of ubiquitination in tumorigenesis and targeted ... [https://www.nature.com/articles/s41392-020-0107-0]
- 73. Targeting the Ubiquitin Pathway for Cancer Treatment - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC4312704/]
- 74. Targeting the Ubiquitin–Proteasome System and Recent ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10778545/]
- 75. Data-independent acquisition method for ubiquitinome ... [https://www.nature.com/articles/s41467-020-20509-1]
- 76. Quantitative Proteomic Atlas of Ubiquitination and ... [https://www.sciencedirect.com/science/article/pii/S1097276515003421]
- 77. Quantitative Analysis of Ubiquitinated Proteins in Human ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6540463/]
- 78. The ubiquitin proteasome system in neurodegenerative ... [https://www.sciencedirect.com/science/article/abs/pii/S0301008212000044]
- 79. Ubiquitin-Proteasome System in Neurodegenerative Disorders [https://pmc.ncbi.nlm.nih.gov/articles/PMC6370320/]
- 80. Exploring the Role of Ubiquitin-Proteasome System in ... [https://www.mdpi.com/1424-8247/17/6/782]
- 81. Dysregulation of Ubiquitin-Proteasome System in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5156861/]
- 82. Screening of the ubiquitin-proteasome system activators for ... [https://www.sciencedirect.com/science/article/pii/S1875536422601523]
- 83. Recent Advances in the Development of Pro-PROTAC for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12473374/]
- 84. PROTAC Degraders in Clinical Trails: 2025 Update [https://www.biochempeg.com/article/434.html]
- 85. PROTAC: a revolutionary technology propelling small ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12597787/]
- 86. PROTAC: a revolutionary technology propelling small ... [https://www.frontiersin.org/journals/oncology/articles/10.3389/fonc.2025.1676414/full]
- 87. What are PROTACs? Mechanisms, advantages, and ... [https://www.drugdiscoverynews.com/what-are-protacs-mechanisms-advantages-and-challenges-16750]
- 88. Targeted protein degradation in oncology: novel ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12420340/]
- 89. PROTACs VS. Traditional Small Molecule Inhibitors [https://www.biochempeg.com/article/233.html]
- 90. Early-Stage PROTAC Development and the Road to IND [https://www.aapsnewsmagazine.org/cover-story-oct25]
- 91. Identification of a novel unfolded protein response related signature for predicting the prognosis of acute myeloid leukemia | Scientific Reports [https://www.nature.com/articles/s41598-025-91524-9]
- 92. Expression of key unfolded protein response genes predicts patient survival and an immunosuppressive microenvironment in glioblastoma | Translational Medicine Communications | Full Text [https://transmedcomms.biomedcentral.com/articles/10.1186/s41231-024-00164-0]
- 93. Unfolded protein response signature unveils novel insights into breast cancer prognosis and tumor microenvironment - ScienceDirect [https://www.sciencedirect.com/science/article/abs/pii/S2210776223000340]
- 94. Advance in prostate cancer biomarker discovery [https://pmc.ncbi.nlm.nih.gov/articles/PMC12125430/]
- 95. Current advances in prognostic and diagnostic biomarkers ... [https://www.sciencedirect.com/science/article/pii/S0753332221012749]
- 96. Emerging biomarkers for early cancer detection and diagnosis [https://eurjmedres.biomedcentral.com/articles/10.1186/s40001-025-03003-6]
- 97. Proteasome [https://en.wikipedia.org/wiki/Proteasome]
- 98. Ubiquitin proteasome system in immune regulation and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10163937/]
- 99. Ubiquitin-proteasome system: a potential participant and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11876059/]
- 100. The application of PROTACs in immune-inflammation ... [https://www.sciencedirect.com/science/article/abs/pii/S096808962400381X]