Mapping the Ubiquitinome: Advanced Strategies for Identifying Ubiquitination Substrates in Tumor Samples
The identification of ubiquitination substrates in tumor samples is a critical frontier in cancer research, holding immense potential for understanding tumor biology, developing prognostic biomarkers, and discovering new therapeutic targets.
Mapping the Ubiquitinome: Advanced Strategies for Identifying Ubiquitination Substrates in Tumor Samples
Abstract
The identification of ubiquitination substrates in tumor samples is a critical frontier in cancer research, holding immense potential for understanding tumor biology, developing prognostic biomarkers, and discovering new therapeutic targets. This article provides a comprehensive guide for researchers and drug development professionals, covering the foundational role of ubiquitination in cancer, from established pancancer networks like the OTUB1-TRIM28-MYC axis to novel non-proteinaceous substrates. It details cutting-edge methodological toolkits, including BioE3 for specific E3 ligase substrate mapping, TUBEs for stabilizing labile ubiquitination events, and mass spectrometry-based proteomics. The content further addresses critical troubleshooting and optimization challenges inherent in working with clinical samples and offers a framework for validating and comparatively analyzing substrate specificity across different tumor contexts. The synthesis of these areas provides a actionable roadmap for advancing cancer diagnostics and drug discovery through the ubiquitin-proteasome system.
The Ubiquitin Landscape in Cancer: From Core Biology to Clinical Relevance
Ubiquitination as a Pivotal Post-Translational Modification in Cellular Homeostasis and Oncogenesis
Ubiquitination is a crucial post-translational modification that regulates the "quantity" and "quality" of diverse proteins, serving to ensure cellular homeostasis and proper life activities [1]. This process involves the covalent attachment of ubiquitin, a highly conserved 76-amino acid protein, to substrate proteins via a sequential enzymatic cascade involving E1 (activating), E2 (conjugating), and E3 (ligating) enzymes [1]. The human genome encodes two E1 enzymes, approximately 40 E2 enzymes, and over 600 E3 ligases, which provide remarkable specificity in substrate recognition [2] [1]. This modification is reversible through the action of deubiquitinating enzymes (DUBs), of which approximately 100 exist in humans, creating a dynamic regulatory system [2] [1].
The complexity of ubiquitin signaling arises from the diversity of ubiquitin chain topologies. Ubiquitin can modify substrates as a single moiety (monoubiquitination), as multiple single units (multi-monoubiquitination), or as polymers (polyubiquitination) formed through linkage to any of seven lysine residues (K6, K11, K27, K29, K33, K48, K63) or the N-terminal methionine (M1) of ubiquitin itself [2] [1]. Each linkage type can encode distinct functional consequences for the modified substrate. K48-linked chains primarily target substrates for proteasomal degradation, while K63-linked chains typically regulate non-proteolytic processes such as kinase activation, DNA repair, and endocytosis [2] [1]. The maintenance of ubiquitination homeostasis through the orchestrated interplay of conjugating and deconjugating enzymes is essential for normal cellular function, and its dysregulation represents a hallmark of numerous pathologies, particularly cancer [2] [1].
Ubiquitination in Oncogenesis: Mechanisms and Pathways
Dysregulation of the ubiquitin system contributes profoundly to tumorigenesis through multiple mechanisms, including altered tumor metabolism, modulation of the immunological tumor microenvironment, and maintenance of cancer stem cell (CSC) stemness [1]. In tumor metabolism, ubiquitination regulates key signaling nodes in critical pathways. For instance, ubiquitination of components in the mTORC1, AMPK, and PTEN-AKT signaling pathways significantly influences cancer cell metabolism and growth [1]. Prominent oncoproteins and tumor suppressors such as c-Myc, p53, RagA, mTOR, PTEN, and AKT are all subject to regulatory ubiquitination, highlighting the central role of this modification in cancer-relevant signaling networks [1].
The immunological tumor microenvironment is similarly regulated by ubiquitin-dependent mechanisms. Ubiquitination events in Toll-like receptor (TLR), RIG-I-like receptor (RLR), and STING-dependent signaling pathways modulate immune responses within the tumor microenvironment, influencing cancer progression and therapeutic responses [1]. Additionally, the maintenance of CSC stemness—a property linked to tumor initiation, metastasis, and therapy resistance—is governed by ubiquitination of core stem cell regulators. The pluripotency factors Nanog, Oct4, and Sox2, as well as components of the Wnt and Hippo-YAP signaling pathways, are regulated by ubiquitination, providing a mechanistic link between the ubiquitin system and cancer stemness [1].
Table 1: Key Ubiquitination-Regulated Processes in Oncogenesis
| Process in Oncogenesis | Key Ubiquitination Targets | Biological Consequences |
|---|---|---|
| Tumor Metabolism | RagA, mTOR, PTEN, AKT, c-Myc, p53 | Altered activity of mTORC1, AMPK, and PTEN-AKT signaling pathways |
| Immunological Tumor Microenvironment | Components of TLR, RLR, and STING pathways | Modulation of immune responses within the tumor microenvironment |
| Cancer Stem Cell Stemness | Nanog, Oct4, Sox2, Wnt and Hippo-YAP pathway components | Maintenance of stemness properties supporting tumor initiation and metastasis |
Recent multi-omics approaches have further elucidated the prognostic value of ubiquitination signatures in cancer. In lung adenocarcinoma (LUAD), ubiquitin-related genes have been used to construct robust risk models that predict patient survival, immune profiles, and drug sensitivity [3]. These models have identified specific ubiquitination-related genes (B4GALT4, DNAJB4, GORAB, HEATR1, LPGAT1, FAT1, GAB2, MTMR4, and TCP11L2) as independent prognostic markers, with high-risk patients showing significantly poorer overall survival [3]. Functional validation has confirmed that knockdown of HEATR1 significantly reduces LUAD cell viability, migration, and invasion, establishing its role as a driver of oncogenic phenotypes [3].
Experimental Approaches for Identifying Ubiquitination Substrates in Tumor Samples
The identification of ubiquitination substrates in tumor tissues presents significant technical challenges due to the low stoichiometry of ubiquitination, the diversity of ubiquitin chain architectures, and the dynamic nature of this modification [2]. Several enrichment strategies have been developed to overcome these challenges, each with distinct advantages and limitations for tumor sample analysis.
Antibody-Based Enrichment Methods
Anti-ubiquitin remnant antibody-based enrichment represents one of the most powerful approaches for mapping ubiquitination sites in clinical samples. This method utilizes antibodies specifically recognizing the di-glycine (K-ε-GG) remnant left on trypsinized peptides derived from ubiquitinated proteins [4] [5]. The workflow involves tissue protein extraction, tryptic digestion, enrichment of ubiquitinated peptides using anti-K-ε-GG antibodies, and subsequent liquid chromatography-tandem mass spectrometry (LC-MS/MS) analysis [4]. This approach has been successfully applied to human pituitary adenoma tissues, identifying 158 ubiquitination sites on 108 proteins and revealing altered ubiquitination in signaling pathways including PI3K-AKT and Hippo [4]. A key advantage of this method is its applicability to clinical samples without genetic manipulation, making it ideal for studying human tumor tissues [2] [4].
Ubiquitin-Binding Domain Based Approaches
Ubiquitin-binding domains (UBDs) from various proteins can be leveraged to enrich ubiquitinated substrates. Recently, a high-affinity UBD from Orientia tsutsugamushi (OtUBD) has been developed that exhibits nanomolar affinity for ubiquitin [6]. The OtUBD resin can enrich both mono- and poly-ubiquitinated proteins from complex lysates and can be used under both native and denaturing conditions [6]. Under denaturing conditions, OtUBD specifically enriches covalently ubiquitinated proteins, while under native conditions it also co-purifies proteins that interact with ubiquitin or ubiquitinated proteins [6]. This method does not require genetic manipulation and works effectively with mammalian cell lysates, making it suitable for tumor tissue analysis.
Ubiquitin Tagging Strategies
The expression of epitope-tagged ubiquitin (e.g., His-, FLAG-, or HA-tagged) enables purification of ubiquitinated proteins using affinity resins directed against the tag [7]. This approach typically involves generating cell lines or animal models stably expressing tagged ubiquitin, followed by affinity purification under denaturing conditions to minimize non-specific interactions [2] [7]. While this method allows stringent purification and has been successfully applied to identify hundreds to thousands of ubiquitination sites in model systems, its application to human tumor tissues is limited by the inability to genetically tag endogenous ubiquitin in clinical samples [2] [7].
Table 2: Comparison of Ubiquitinated Protein Enrichment Methods
| Method | Principle | Advantages | Disadvantages | Suitable for Tumor Tissues |
|---|---|---|---|---|
| Antibody-Based (K-ε-GG) | Antibodies recognize GG-remnant on tryptic peptides | High specificity; works directly with clinical samples; identifies modification sites | Cannot detect non-lysine ubiquitination; expensive antibodies | Yes |
| UBD-Based (OtUBD) | High-affinity ubiquitin-binding domain enriches ubiquitinated proteins | Works with native and denatured conditions; captures all ubiquitin conjugates | May co-purify ubiquitin-interacting proteins under native conditions | Yes |
| Tagged Ubiquitin | Epitope-tagged ubiquitin expressed in cells | High purity and yield; well-established protocols | Requires genetic manipulation; not applicable to human tissues | Limited to engineered models |
Protocol: Ubiquitinome Analysis of Tumor Tissues Using Anti-K-ε-GG Antibody Enrichment
This protocol describes a comprehensive approach for identifying and quantifying ubiquitination sites in human tumor tissues using anti-K-ε-GG antibody-based enrichment and LC-MS/MS analysis, adapted from methodologies successfully applied to lung adenocarcinoma and pituitary adenoma tissues [4] [5].
Sample Preparation and Protein Extraction
Tissue Homogenization: Freshly frozen tumor and matched control tissues (50-100 mg) are cryogenically pulverized using a mortar and pestle cooled with liquid nitrogen. Alternatively, tissue samples can be cut into small pieces on dry ice.
Protein Extraction: Transfer powdered tissue to a pre-chilled tube containing four volumes of lysis buffer (1% Triton X-100, 1% protease inhibitor cocktail, 50 μM PR-619 deubiquitinase inhibitor, 50 mM Tris-HCl, pH 8.0) [5]. Homogenize using a pre-cooled Dounce homogenizer or by sonication on ice (3 × 10-second pulses at 20% amplitude with 30-second intervals on ice).
Clarification: Centrifuge lysates at 12,000 × g for 10 minutes at 4°C. Transfer supernatant to a new tube and determine protein concentration using a bicinchoninic acid (BCA) assay.
Protein Precipitation and Denaturation: Add trichloroacetic acid (TCA) to a final concentration of 20% to precipitate proteins. Incubate for 2 hours at 4°C, then centrifuge at 4,500 × g for 5 minutes. Wash pellet twice with ice-cold acetone and air-dry.
Protein Digestion and Peptide Cleanup
Reduction and Alkylation: Dissolve protein pellet in 200 mM tetraethylammonium bromide (TEAB) buffer. Add dithiothreitol (DTT) to a final concentration of 5 mM and incubate at 56°C for 30 minutes. Then add iodoacetamide to a final concentration of 11 mM and incubate for 15 minutes at room temperature in the dark.
Trypsin Digestion: Add sequencing-grade trypsin at a 1:50 (enzyme:protein) ratio and digest overnight at 37°C with gentle agitation.
Peptide Desalting: Desalt peptides using C18 solid-phase extraction columns according to manufacturer's instructions. Lyophilize desalted peptides and store at -80°C until enrichment.
Enrichment of Ubiquitinated Peptides
Peptide Reconstitution: Dissolve dried peptides in IP buffer (100 mM NaCl, 1 mM EDTA, 50 mM Tris-HCl, 0.5% NP-40, pH 8.0).
Antibody Enrichment: Incubate peptides with anti-K-ε-GG antibody-conjugated beads (commercially available) overnight at 4°C with gentle rotation. Typically, 2-5 mg of antibody-conjugated resin is used per 10-20 mg of starting peptide material.
Washing: Wash resin four times with IP buffer and twice with deionized water to remove non-specifically bound peptides.
Elution: Elute bound peptides with 0.1% trifluoroacetic acid (TFA). Collect eluate and lyophilize.
LC-MS/MS Analysis and Data Processing
Liquid Chromatography: Reconstitute peptides in 0.1% formic acid and separate using a nanoflow UHPLC system with a C18 reversed-phase column (75 μm × 25 cm) with a 120-minute gradient from 2% to 30% acetonitrile in 0.1% formic acid.
Mass Spectrometry Analysis: Analyze eluting peptides using a timsTOF Pro or similar mass spectrometer operating in data-dependent acquisition mode. MS1 spectra should be acquired at 60,000 resolution, with MS2 spectra triggered for the top 20 most intense precursors.
Database Searching: Process raw files using MaxQuant (version 1.6.6.0 or later) against the appropriate UniProt database. Search parameters should include: trypsin/P as protease with up to 4 missed cleavages; carbamidomethylation of cysteine as fixed modification; oxidation of methionine and N-terminal acetylation as variable modifications; and GlyGly (K) as a fixed modification for ubiquitination sites.
False Discovery Rate (FDR) Control: Set FDR thresholds to 1% at both peptide and protein levels using a target-decoy approach.
The Scientist's Toolkit: Essential Reagents and Materials
Table 3: Essential Research Reagents for Ubiquitination Studies in Tumor Samples
| Reagent/Material | Function/Purpose | Examples/Details |
|---|---|---|
| Deubiquitinase Inhibitors | Prevent loss of ubiquitination during sample processing | PR-619 (broad-spectrum DUB inhibitor), N-ethylmaleimide (NEM) |
| Protease Inhibitor Cocktails | Prevent protein degradation during extraction | EDTA-free cocktails for metal-free MS compatibility |
| Anti-K-ε-GG Antibodies | Specific enrichment of ubiquitinated peptides | Commercial kits (PTMScan); recognize diglycine remnant after trypsinization |
| Ubiquitin-Binding Domains | Enrichment of intact ubiquitinated proteins | OtUBD resin; TUBEs (Tandem Ubiquitin Binding Entities) |
| Tag-Specific Resins | Purification of tagged ubiquitin conjugates | Ni-NTA for His-tags; Anti-FLAG/HA affinity gels |
| Trypsin/Lys-C Mix | Protein digestion for MS analysis | Sequencing grade, MS-compatible |
| C18 Desalting Columns | Peptide cleanup prior to enrichment | StageTips; commercial spin columns |
| UHPLC-MS Systems | High-sensitivity peptide separation and detection | nanoElute systems coupled to timsTOF Pro or Orbitrap instruments |
Data Analysis and Bioinformatics Approaches
The analysis of ubiquitinome data requires specialized bioinformatics approaches to extract biological insights from complex mass spectrometry datasets. Following database searching, several analytical steps are essential:
Ubiquitination Site Localization: Use software such as MaxQuant to calculate localization probabilities for ubiquitination sites. Only sites with localization probability >0.75 should be considered for further analysis.
Differential Ubiquitination Analysis: Apply statistical tests (e.g., Student's t-test with Benjamini-Hochberg correction) to identify ubiquitination sites significantly altered between tumor and control tissues. A fold-change threshold of >1.5 or <-1.5 with an adjusted p-value <0.05 is commonly used.
Motif Analysis: Use motif-x or similar algorithms to identify conserved amino acid sequences surrounding ubiquitination sites, which may reveal sequence preferences for specific E3 ligases.
Pathway and Network Analysis: Input significantly altered ubiquitinated proteins into pathway analysis tools such as DAVID or KEGG to identify enriched biological pathways. As demonstrated in pituitary adenoma studies, ubiquitination frequently affects signaling pathways including PI3K-AKT, Hippo, ribosome, and nucleotide excision repair [4].
Integration with Transcriptomic and Proteomic Data: Combine ubiquitinome data with matching transcriptome and proteome datasets to determine whether changes in ubiquitination occur independently of or correlate with changes in protein abundance or mRNA expression.
Therapeutic Targeting of the Ubiquitin System in Oncology
The central role of ubiquitination in oncogenesis has made components of the ubiquitin system attractive therapeutic targets. Several classes of targeted agents have been developed:
Proteasome Inhibitors: Bortezomib, carfilzomib, oprozomib, and ixazomib target the 20S proteasome catalytic core, preventing degradation of ubiquitinated proteins and inducing endoplasmic reticulum stress in cancer cells. These agents have achieved tangible success in multiple myeloma and mantle cell lymphoma [1].
E1 Enzyme Inhibitors: MLN7243 and MLN4924 (pevonedistat) inhibit the NEDD8-activating enzyme, which regulates the activity of cullin-RING E3 ubiquitin ligases. MLN4924 has shown promising anti-tumor activity in preclinical models and clinical trials [1].
E2 Enzyme Inhibitors: Compounds such as Leucettamol A and CC0651 target specific E2 enzymes, disrupting the transfer of ubiquitin to substrates [1].
E3 Ligase-Targeting Agents: Nutlin and MI-219 inhibit the MDM2 E3 ligase, activating p53 tumor suppressor function. Additionally, proteolysis-targeting chimeras (PROTACs) represent a novel approach that hijacks E3 ligases to selectively degrade target proteins [1].
Deubiquitinase Inhibitors: Compounds G5 and F6 target specific DUBs, preventing removal of ubiquitin from substrates and altering their stability or function [1].
The integration of ubiquitinome analysis with drug sensitivity profiling has revealed promising correlations that could guide therapeutic decisions. In LUAD, drug sensitivity studies have identified that medications including TAE684, Cisplatin, and Midostaurin exhibit significant negative correlations with ubiquitination-based risk scores, suggesting potential efficacy in high-risk patients [3]. These findings highlight the potential of ubiquitination signatures as biomarkers for treatment selection and drug development.
Ubiquitination represents a fundamental regulatory mechanism that maintains cellular homeostasis while serving as a critical driver of oncogenesis when dysregulated. The development of sophisticated proteomic methodologies, particularly anti-K-ε-GG antibody-based enrichment coupled with high-resolution mass spectrometry, has enabled comprehensive mapping of the ubiquitinome in human tumor tissues. These approaches have revealed ubiquitination-mediated regulation of key oncogenic processes including tumor metabolism, immune microenvironment modulation, and cancer stem cell maintenance. The continued refinement of ubiquitinome analysis protocols and the development of targeted therapies against specific components of the ubiquitin system hold significant promise for advancing cancer diagnostics and therapeutics. Integration of ubiquitinome data with other omics datasets and clinical outcomes will further enhance our understanding of the prognostic and predictive value of ubiquitination signatures across cancer types.
Application Note & Protocol
Ubiquitination is a crucial post-translational modification that orchestrates cellular homeostasis and oncogenic pathways, yet it remains underexplored as a pancancer regulatory hub [8]. This application note details comprehensive methodologies and insights from a large-scale study that integrated data from 4,709 patients across 26 cohorts spanning five solid tumor types: lung cancer, esophageal cancer, cervical cancer, urothelial cancer, and melanoma [8]. The constructed pancancer ubiquitination regulatory network reveals important pathways and offers insights into predicting patient prognosis and understanding biological mechanisms, with particular focus on identifying ubiquitination substrates in tumor samples.
Key Quantitative Findings
Table 1: Patient Cohort Distribution Across Cancer Types
| Cancer Type | Number of Patients | Data Source | Notable Histological Subtypes |
|---|---|---|---|
| Lung Cancer | 650 (ADC), 840 (SQC) | TCGA | ADC, SQC, NEC |
| Esophageal Cancer | 179 (SQC), 37 (ADC) | GSE53625, GSE183924 | ADC, SQC |
| Cervical Cancer | 64 (ADC), 221 (SQC) | GSE44001, GSE56303 | ADC, SQC |
| Urothelial Carcinoma | 404 | TCGA | NMIBC, MIBC |
| Melanoma | 57 | GSE91061 | - |
| Total | 4,709 | 26 cohorts |
Table 2: Ubiquitination-Related Prognostic Signature (URPS) Performance
| Assessment Metric | Finding | Clinical Implication |
|---|---|---|
| Risk Stratification | Effectively stratified patients into high-risk and low-risk groups | Distinct survival outcomes across all analyzed cancers |
| Immunotherapy Prediction | Novel biomarker for predicting immunotherapy response | Identifies patients more likely to benefit from immunotherapy |
| Key Molecular Axis | OTUB1-TRIM28 ubiquitination modulates MYC pathway | Influences patient prognosis and histological fate |
| Single-cell Resolution | Enables precise classification of distinct cell types | Associated with macrophage infiltration in TME |
Experimental Protocols
Ubiquitination Regulatory Network Construction
Protocol Title: Construction of Pancancer Ubiquitination Regulatory Network
Principle: This protocol outlines the integration of multi-cohort transcriptomic data to map molecular profiles to ubiquitination interaction networks, enabling identification of key regulatory nodes and pathways across cancer types.
Materials:
- RNA-seq data from TCGA and GEO databases
- Clinical data from 26 patient cohorts
- Computational resources for large-scale bioinformatic analysis
- R statistical environment with appropriate packages
Procedure:
- Data Collection and Integration
- Obtain RNA-seq data and clinicopathological features from TCGA for lung cancer, esophageal cancer, cervical cancer, urothelial carcinoma, and melanoma
- Include datasets with at least five patients classified as classic pathological subtypes (SQC or ADC)
- Standardize correlation coefficient matrix through significance screening (p-value < 0.05)
Ubiquitination Score Calculation
- Analyze ubiquitination scores for prognostic significance
- Screen downstream genes using LASSO algorithm to identify key prognosis-associated genes
- Perform functional enrichment and protein-protein interaction analyses
Validation Framework
- Validate findings using independent patient cohorts, cell line models, and in vivo experiments
- Utilize transcriptomic data from non-small cell lung cancer, small cell lung cancer, and non-tumoral lung tissues from GEO dataset GSE30219
- Incorporate transcriptomic profiles of lung cancer patients undergoing immunotherapy from GSE135222 and GSE126044 datasets
Troubleshooting:
- Ensure consistent normalization across datasets from different sources
- Address batch effects through appropriate statistical methods
- Verify histological classification consistency across different grading systems
Ubiquitinomics Profiling in Tumor Tissues
Protocol Title: Label-Free Quantitative Identification of Abnormally Ubiquitinated Proteins in Tumor Tissues
Principle: This mass spectrometry-based protocol enables comprehensive identification of differentially ubiquitinated proteins (DUPs) and ubiquitination sites in clinical tumor samples, providing insights into ubiquitination-involved molecular network alterations.
Materials:
- Fresh frozen tumor tissues and matched controls
- Anti-ubiquitin antibody (specific anti-K-ε-GG group)
- Urea lysis buffer (7 M urea, 2 M thiourea, 100 mM DTT, 1 mM PMSF)
- C18 Cartridges (Empore SPE Cartridges C18) for desalting
- LC-MS/MS system
Procedure:
- Tissue Processing and Protein Extraction
- Mix multiple patient tissue samples (150 mg per patient, n=5) to create pooled LSCC and control samples
- Wash tissues in 0.9% NaCl solution to remove blood contamination
- Homogenize in urea lysis buffer and sonicate (80 W, 10 sec, interval 15 sec, 10×)
- Centrifuge at 15,000×g for 20 minutes at 4°C and collect supernatant
Trypsin Digestion and Peptide Preparation
- Treat samples with DTT (final concentration 10 mM) at 600 rpm, 37°C for 1.5 hours
- Alkylate with iodoacetamide (final concentration 50 mM) in dark for 30 minutes
- Digest with trypsin (trypsin:protein = 1:50 wt:wt) at 37°C for 15-18 hours
- Acidify with TFA (final TFA = 0.1%), adjust to pH ≤ 3
- Desalt tryptic peptides using C18 Cartridges and lyophilize
Ubiquitinated Peptide Enrichment and LC-MS/MS Analysis
- Enrich ubiquitinated peptides using anti-K-ε-GG antibody-based enrichment
- Perform LC-MS/MS analysis to identify DUPs and ubiquitination sites
- Identify ubiquitination motifs through sequence analysis
Data Integration and Validation
- Integrate ubiquitinomics data with transcriptomics data from TCGA
- Perform protein-protein interaction network analysis to identify hub molecules
- Conduct survival analysis to identify prognosis-related mRNAs
- Validate key findings through proteasome inhibition experiments
Troubleshooting:
- Optimize antibody enrichment efficiency through positive controls
- Verify ubiquitination site identification through synthetic peptide validation
- Address sample heterogeneity through adequate sample pooling and replication
Signaling Pathways and Molecular Mechanisms
Research Reagent Solutions
Table 3: Essential Research Reagents for Ubiquitination Network Studies
| Reagent/Category | Specific Examples | Function/Application |
|---|---|---|
| Enrichment Tools | Anti-K-ε-GG antibody | Immunoaffinity enrichment of ubiquitinated peptides for MS analysis |
| Mass Spectrometry | LC-MS/MS systems | Identification and quantification of ubiquitination sites |
| Computational Tools | UbiBrowser | Prediction of E3/DUB-substrate interactions |
| Database Resources | TCGA, GEO | Access to multi-omics cancer data |
| E3 Ligase Targets | TRIM28, NEDD4L, TRIM2 | Key regulators of ubiquitination in cancer pathways |
| Validation Reagents | siRNA/shRNA for OTUB1, TRIM28 | Functional validation of ubiquitination regulators |
Discussion and Clinical Implications
This comprehensive analysis demonstrates that the OTUB1-TRIM28 ubiquitination regulatory enzyme influences the histological fate of cancer cells by modulating MYC and its downstream pathways and altering oxidative stress, ultimately leading to immunotherapy resistance and poor prognosis in patients [8]. The established ubiquitination-related prognostic signature (URPS) provides a novel strategy for predicting overall survival in pancancer patients receiving surgery or immunotherapy, with significant implications for personalized treatment approaches.
The study further reveals that ubiquitination score positively correlates with squamous or neuroendocrine transdifferentiation in adenocarcinoma, providing mechanistic insights into cancer plasticity and progression [8]. These findings unveil a novel strategy for drug development targeting traditionally "undruggable" targets like MYC, whereby ubiquitination regulatory modifiers for such targets can be screened through the constructed pancancer ubiquitination regulatory network, providing new therapeutic alternatives for improving immunotherapy efficacy and patient prognosis.
The integration of multi-cohort analyses across 4,709 patients has enabled the construction of a comprehensive pancancer ubiquitination regulatory network that offers significant insights into prognostic prediction, biological mechanisms, and therapeutic targeting. The detailed protocols provided herein facilitate the replication and extension of these findings, supporting ongoing efforts to decipher the complex role of ubiquitination networks in cancer biology and treatment response.
Ubiquitination is a critical post-translational modification that orchestrates cellular homeostasis and oncogenic pathways, serving as a pivotal regulatory hub in cancer biology [8] [9]. The reversible and enzymatically regulated process of ubiquitination plays a complex role in cancer development, progression, metabolic reprogramming, and immunotherapy efficacy [8]. Among the intricate network of ubiquitination regulators, the OTUB1-TRIM28-MYC axis has emerged as a crucial pathway influencing tumor progression and patient outcomes across multiple cancer types. This application note details the mechanisms, experimental evidence, and methodological protocols for investigating this pathway within the broader context of identifying ubiquitination substrates in tumor samples.
The OTUB1-TRIM28 ubiquitination regulatory enzyme significantly influences the histological fate of cancer cells by modulating MYC and its downstream pathways, altering oxidative stress, ultimately leading to immunotherapy resistance and poor prognosis in patients [8]. Understanding this axis provides not only prognostic insights but also unveils a novel strategy for drug development targeting traditionally "undruggable" targets like MYC through screening ubiquitination regulatory modifiers [8].
Mechanistic Insights into the OTUB1-TRIM28-MYC Axis
Molecular Regulation
The OTUB1-TRIM28-MYC axis represents a sophisticated regulatory circuit where ubiquitination dynamics control oncogenic signaling:
OTUB1 Functional Mechanisms: OTUB1, an OTU-family deubiquitinase, antagonizes ubiquitination through two distinct mechanisms: (1) direct deubiquitination via its catalytic activity, and (2) non-canonical inhibition of ubiquitin transfer by binding to and blocking ubiquitin-conjugated E2 enzymes [10]. OTUB1 exhibits strong preference for Lys48-linked polyubiquitin chains, which are primarily associated with proteasomal degradation [10].
TRIM28 Multifunctionality: TRIM28 (also known as TIF1β and KAP1) contains an N-terminal TRIM structure and a C-terminal PHD-Bromo dual epigenetic reader domain, functioning as both a canonical RING-type E3 ubiquitin ligase and an E3 SUMO ligase under certain conditions [11]. The B-box2 domain of TRIM28 is necessary for its interaction with PD-L1 [11].
MYC Pathway Modulation: The OTUB1-TRIM28 ubiquitination regulatory enzyme influences the MYC pathway, altering oxidative stress and contributing to immunotherapy resistance [8]. Ubiquitination score positively correlates with squamous or neuroendocrine transdifferentiation in adenocarcinoma, with MYC serving as a central downstream effector [8].
Role in Tumor Immune Regulation
The axis significantly impacts tumor immune evasion through multiple mechanisms:
PD-L1 Stabilization: TRIM28 directly binds to and stabilizes PD-L1 by inhibiting PD-L1 ubiquitination while promoting PD-L1 SUMOylation [11]. TRIM28 depletion significantly shortens the half-life of PD-L1, indicating its crucial role in PD-L1 protein stabilization in cancer cells [11].
Immune Pathway Activation: TRIM28 facilitates K63 polyubiquitination of TBK1, activating TBK1-IRF1 and TBK1-mTOR pathways, resulting in enhanced PD-L1 transcription [11]. This creates a dual mechanism of PD-L1 regulation at both protein stability and transcriptional levels.
Table 1: Functional Roles of Key Components in the OTUB1-TRIM28-MYC Axis
| Component | Molecular Function | Role in Cancer | Regulatory Mechanism |
|---|---|---|---|
| OTUB1 | Deubiquitinase | Oncogenic | Inhibits substrate ubiquitination via catalytic activity and E2 blockade [10] |
| TRIM28 | E3 ubiquitin/SUMO ligase | Oncogenic | Stabilizes PD-L1, activates TBK1 pathways [11] |
| MYC | Transcription factor | Oncogenic | Downstream effector of OTUB1-TRIM28 regulation [8] |
| PD-L1 | Immune checkpoint | Immunosuppression | Stabilized by TRIM28-mediated inhibition of ubiquitination [11] |
Quantitative Analysis of Pathway Significance
Prognostic Implications
Comprehensive studies across multiple cancer types have established the clinical significance of the OTUB1-TRIM28-MYC axis:
Pancancer Ubiquitination Signature: Analysis of 4,709 patients from 26 cohorts across five solid tumor types (lung cancer, esophageal cancer, cervical cancer, urothelial cancer, and melanoma) identified a conserved ubiquitination-related prognostic signature (URPS) that effectively stratified patients into high-risk and low-risk groups with distinct survival outcomes [8].
Gastric Cancer Validation: In a cohort of 466 gastric cancer patients, high TRIM28 expression correlated with poor survival, consistent with observations in publicly available databases [11]. Ectopic TRIM28 expression facilitated tumor growth, increased PD-L1 expression, and suppressed T cell activation in mouse models [11].
Therapeutic Response Prediction: The URPS serves as a novel biomarker for predicting immunotherapy response, with potential to identify patients more likely to benefit from immunotherapy in clinical settings [8].
Table 2: Clinical Correlations of OTUB1-TRIM28-MYC Axis Components Across Cancer Types
| Cancer Type | Sample Size | Key Finding | Statistical Significance |
|---|---|---|---|
| Pancancer Cohort | 4,709 patients | URPS stratification of high/low risk groups | Distinct survival outcomes (p<0.05) [8] |
| Gastric Cancer | 466 patients | High TRIM28 = poor survival | Consistent across databases [11] |
| Multiple Solid Tumors | 26 cohorts | URPS predicts immunotherapy response | Potential for clinical application [8] |
Experimental Protocols
Protocol 1: Identifying Ubiquitination Substrates in Tumor Samples
Objective: To identify and validate ubiquitination substrates within the OTUB1-TRIM28-MYC axis using patient-derived tumor samples.
Materials:
- Fresh or snap-frozen tumor tissues and matched normal adjacent tissues
- Lysis buffer: 50 mM Tris-HCl (pH 7.5), 150 mM NaCl, 1 mM EDTA, 1% NP-40, supplemented with protease inhibitors (complete Mini, Roche) and deubiquitinase inhibitors (N-ethylmaleimide, 10 mM)
- Protein A/G agarose beads (Pierce)
- Anti-TRIM28 antibody (Abcam, ab22553), Anti-OTUB1 antibody (Cell Signaling, 3744S), Anti-c-MYC antibody (Santa Cruz, sc-40)
- Ubiquitin enrichment matrix: TUBE2 (Tandem Ubiquitin Binding Entities, LifeSensors)
- MG132 proteasome inhibitor (10 µM, Selleckchem)
Procedure:
- Tissue Processing: Homogenize 50-100 mg tumor tissue in 1 mL lysis buffer using a Dounce homogenizer. Centrifuge at 15,000 × g for 15 minutes at 4°C and collect supernatant.
- Protein Concentration Determination: Quantify protein concentration using BCA assay. Use 2 mg total protein for each immunoprecipitation.
- Ubiquitinated Protein Enrichment: Incubate lysate with TUBE2 agarose (25 µL bead volume) for 4 hours at 4°C with gentle rotation.
- Immunoprecipitation: For specific protein interactions, pre-clear lysate with protein A/G beads for 30 minutes. Incubate with primary antibody (1-2 µg) overnight at 4°C, then with protein A/G beads for 2 hours.
- Washing and Elution: Wash beads 3 times with lysis buffer. Elute proteins with 2× Laemmli buffer at 95°C for 10 minutes.
- Western Blot Analysis: Resolve proteins by SDS-PAGE, transfer to PVDF membrane, and probe with antibodies against target proteins and ubiquitin.
Validation:
- Confirm ubiquitination by probing with anti-ubiquitin antibody (P4D1, Santa Cruz)
- Use deubiquitinase treatment as negative control: incubate samples with USP2 catalytic domain (200 nM) for 1 hour at 37°C before analysis
Protocol 2: Functional Validation of OTUB1-TRIM28 Interaction
Objective: To characterize the functional consequences of OTUB1-TRIM28 interaction on MYC pathway activity.
Materials:
- Cancer cell lines (MGC-803, SGC-7901 gastric cancer cells recommended)
- Plasmid constructs: WT OTUB1, catalytic mutant OTUB1 (C91S), WT TRIM28, TRIM28 deletion mutants
- siRNA targeting OTUB1, TRIM28, and non-targeting control
- Dual-luciferase reporter system (Promega)
- MYC activity reporter plasmid
- Chromatin immunoprecipitation (ChIP) kit (Millipore)
Procedure:
- Genetic Manipulation:
- Transfect cells with siRNA (50 nM) using Lipofectamine RNAiMAX or plasmids (2 µg) using Lipofectamine 3000 according to manufacturer's protocol
- Allow 48-72 hours for protein knockdown or 24 hours for overexpression before analysis
Co-immunoprecipitation Assay:
- Lyse transfected cells in IP lysis buffer
- Incubate 1 mg protein with anti-TRIM28 antibody overnight at 4°C
- Capture immune complexes with protein A/G beads
- Analyze by Western blot with anti-OTUB1 and anti-TRIM28 antibodies
MYC Pathway Activity Assessment:
- Co-transfect MYC reporter plasmid with Renilla control
- Measure luciferase activity 24 hours post-transfection using dual-luciferase system
- Perform ChIP assay using anti-MYC antibody to assess MYC binding to target promoters
Functional Phenotyping:
- Assess cell proliferation using MTT assay at 24, 48, and 72 hours
- Evaluate apoptosis by Annexin V/propidium iodide staining after 48 hours of treatment
- Analyze cell cycle distribution by propidium iodide staining and flow cytometry
Pathway Visualization
Diagram 1: OTUB1-TRIM28-MYC Axis in Tumorigenesis. This pathway visualization illustrates the molecular mechanisms through which OTUB1 and TRIM28 coordinately regulate MYC stability and PD-L1 expression to promote tumor progression and immune evasion.
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Research Reagents for Investigating the OTUB1-TRIM28-MYC Axis
| Reagent Category | Specific Products | Application | Key Features |
|---|---|---|---|
| Antibodies | Anti-TRIM28 (Abcam ab22553), Anti-OTUB1 (CST 3744S), Anti-c-MYC (Santa Cruz sc-40) | Western blot, IP, IHC | Validated for multiple applications including ubiquitination studies |
| Ubiquitination Tools | TUBE2 Agarose (LifeSensors), HA-Ubiquitin plasmid, MG132 proteasome inhibitor | Ubiquitin enrichment, assays | TUBE2 preserves labile ubiquitinated species during extraction |
| Genetic Tools | OTUB1 siRNA (Santa Cruz sc-76310), TRIM28 CRISPR/Cas9 KO plasmid (Origene) | Functional studies | Enable loss-of-function and gain-of-function experiments |
| Cell Lines | MGC-803, SGC-7901 gastric cancer lines; YCCEL1 EBVaGC line | Mechanistic studies | Endogenous expression of pathway components |
| Activity Reporters | MYC luciferase reporter, PD-L1 promoter construct | Pathway activity measurement | Quantify functional output of the axis |
The OTUB1-TRIM28-MYC axis represents a clinically significant ubiquitination pathway with broad implications for tumor progression and patient prognosis. The experimental protocols detailed herein provide a standardized methodology for investigating this pathway in tumor samples, enabling researchers to validate ubiquitination substrates and their functional consequences. The conserved nature of this regulatory module across multiple cancer types highlights its fundamental importance in oncogenesis and positions it as a promising target for therapeutic intervention.
Future research directions should focus on developing small molecule inhibitors targeting OTUB1's non-canonical E2 inhibition function and TRIM28's substrate recognition domains. Additionally, combining OTUB1/TRIM28 targeting with immune checkpoint blockade may yield synergistic therapeutic effects, particularly in tumors with MYC pathway activation. The methodologies and reagents outlined in this application note provide a foundation for these advanced investigations into ubiquitination-mediated oncogenesis.
The ubiquitin system is a central regulator of eukaryotic homeostasis, historically known for modifying protein substrates to govern virtually all aspects of protein-mediated cellular functions [12]. However, the substrate realm of ubiquitination has recently expanded beyond proteins to include non-proteinaceous matter, opening a new chapter in ubiquitin biology [12]. This paradigm shift reveals that ubiquitin can be transferred to diverse biomolecules including lipids, carbohydrates, nucleic acids, and metabolites [12]. Most remarkably, recent research demonstrates that certain ubiquitin ligases can even modify exogenous, drug-like small molecules [12]. This article explores these expanding substrate boundaries within the specific context of identifying ubiquitination substrates in tumor samples, providing application notes and experimental protocols to advance research in cancer metabolism and therapeutic development.
Lipid Substrates in Tumor Metabolism
Lipid metabolic reprogramming is a fundamental hallmark of cancer, driving tumor progression, therapeutic resistance, and immune evasion [13]. In pediatric solid tumors, which account for approximately 60% of new childhood cancer diagnoses, lipid metabolic reprogramming occurs through enhanced fatty acid uptake, increased de novo lipid synthesis, and activated fatty acid β-oxidation (FAO) [13]. The ubiquitin-proteasome system (UPS) plays a crucial role in regulating this lipid metabolism by modulating the stability and activity of key metabolic enzymes and transporters involved in cholesterol and fatty acid pathways [13].
Table 1: Key Lipid Metabolism Proteins Regulated by Ubiquitination in Cancer
| Target Protein | Role in Lipid Metabolism | Ubiquitination Effect | Cancer Relevance |
|---|---|---|---|
| CD36 | Fatty acid translocase facilitating cellular uptake of long-chain fatty acids | Phosphorylation, ubiquitination, glycosylation, and palmitoylation regulate function | Highly expressed in HCC, breast cancer, oral squamous cell carcinoma, AML, and CRC [14] |
| SREBPs (SREBP-1, SREBP-2) | Master transcription factors controlling fatty acid and cholesterol synthesis | HSP90β facilitates ubiquitination and proteasomal degradation of mature SREBPs [14] | Key regulators of lipogenesis in multiple cancer types |
| ACLY | Converts citrate to acetyl-CoA for de novo lipogenesis | Protein stability controlled through acetylation and deubiquitination [14] | Regulates de novo lipogenesis and tumor growth |
| FASN | Produces palmitic acid from acetyl-CoA and malonyl-CoA | Protein stability controlled through dynamic acetylation and deacetylation [14] | Critical for synthesis of basic 16-carbon saturated fatty acids |
| HMGCR | Rate-limiting enzyme in cholesterol synthesis | Regulated by SREBP-2 and subject to ubiquitination [14] | Key enzyme in cholesterol biosynthesis pathway |
The ubiquitination primarily determines protein fate through proteasomal or lysosomal degradation, with most ubiquitinated proteins being processed by the 26S proteasome [13]. The complexity of ubiquitination is reflected in the diverse enzymatic machinery comprising two E1 enzymes, approximately 40 E2 enzymes, and over 600 E3 ligases in mammals, with E3 ligases conferring substrate specificity [13]. This sophisticated system allows for precise regulation of lipid metabolic pathways in cancer cells.
Diagram 1: Ubiquitination Regulation of Lipid Metabolism in Cancer. Key enzymes and transporters in lipid uptake, de novo synthesis, cholesterol metabolism, and fatty acid oxidation are regulated by ubiquitination (dashed lines).
Drug-like Small Molecules as Ubiquitination Substrates
HUWE1-Mediated Small Molecule Ubiquitination
A groundbreaking discovery has revealed that the human ubiquitin ligase HUWE1 can target drug-like small molecules, expanding the substrate realm of non-protein ubiquitination [12]. This finding originated from investigations into commercially available small-molecule inhibitors of HUWE1, specifically BI8622 and BI8626, which were initially identified as HUWE1 inhibitors but were subsequently found to be substrates of their target ligase [12].
The ubiquitination mechanism for these compounds follows the canonical catalytic cascade, linking ubiquitin to the compound's primary amino group via a covalent bond [12]. In vitro assays demonstrate that compound ubiquitination is selectively catalyzed by HUWE1, allowing the compounds to compete with protein substrates [12]. Cellular detection methods have confirmed that HUWE1 promotes - but does not exclusively drive - compound ubiquitination in cells [12].
Table 2: Characteristics of HUWE1-Targeted Small Molecule Substrates
| Parameter | BI8622 | BI8626 | Derivative 1 |
|---|---|---|---|
| Primary Amino Group Position | Meta position of benzyl ring | Meta position of benzyl ring | Para position of benzyl ring |
| Inhibition Potency | Low-micromolar IC50 | More potent than BI8622 | Retains HUWE1HECT inhibition |
| Ubiquitination Site | Primary amino group | Primary amino group | Primary amino group |
| Mass Addition to Ubiquitin | +408.21 Da | +422.23 Da | Not specified |
| Cellular Specificity | HUWE1-promoted but not exclusive | HUWE1-promoted but not exclusive | Not determined |
Structure-activity relationship studies demonstrate the critical importance of the primary amino group for the ubiquitination of these small molecules [12]. Shifting this group from the meta to the para position of the benzyl ring (derivative 1) retained HUWE1HECT inhibition, while removal of the amino group or substitution by a secondary or tertiary amine caused a complete loss of inhibition [12]. Mass spectrometry analyses confirmed the covalent attachment of ubiquitin to the inhibitor molecules, with Ub C-terminal peptides showing characteristic mass increases corresponding to the conjugated compounds [12].
Experimental Evidence and Validation
The substrate competitive nature of these inhibitors was demonstrated through comprehensive biochemical assays [12]. In multi-turnover ubiquitination reactions containing E1 (UBA1), E2 (UBE2L3), HUWE1HECT, Ub, and ATP, both BI8622 and BI8626 inhibited ubiquitination dose-dependently in the low-micromolar concentration range [12]. The inhibitors suppressed E3 autoubiquitination, E2 ubiquitination and free Ub chain formation, indicating broad inhibition of HUWE1HECT catalysis independent of the Ub-accepting protein [12].
Single-turnover assays revealed that the inhibitors do not obstruct Ub transfer from the E2 to HUWE1HECT, nor do they perturb the preceding Ub transfer from the E1 to the E2 [12]. This indicates that the compounds inhibit HUWE1HECT after the formation of a thioester-linked intermediate with Ub, specifically interfering with the second step of HECT E3 catalysis [12].
Application Notes: Ub-POD Protocol for Substrate Identification
The Ubiquitin-specific Proximity-Dependent Labeling (Ub-POD) technique represents a significant advancement in identifying E3 ubiquitin ligase substrates in human cells [15] [16]. This method enables the selective biotinylation of substrates of a given ubiquitin ligase, overcoming the challenge of capturing transient substrate-E3 ligase interactions that conventional methods often fail to address [15].
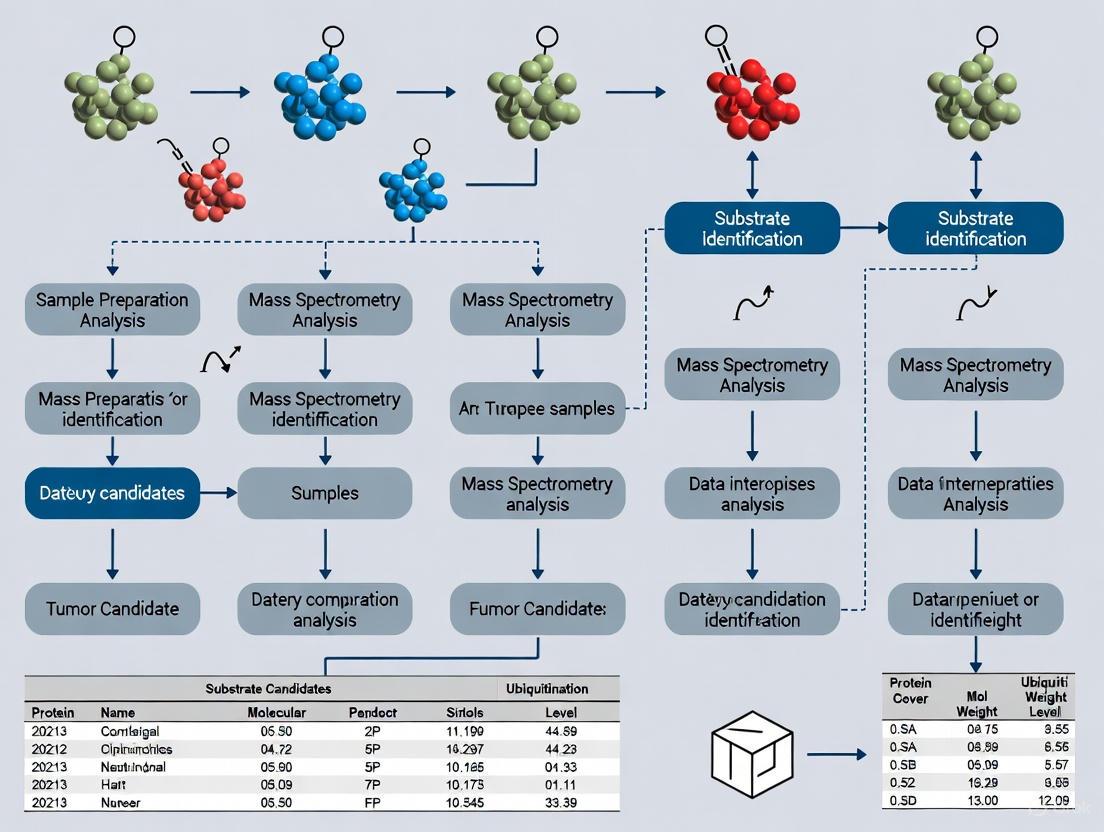
The core principle of Ub-POD involves fusing the candidate E3 ligase to the biotin ligase BirA and ubiquitin to a biotin acceptor peptide, an Avi-tag variant (-2) AP [15]. Cells are co-transfected with these fusion constructs and exposed to biotin, resulting in a BirA-E3 ligase-catalyzed biotinylation of (-2) AP-Ub when in complex with E2 [15]. The biotinylated (-2) AP-Ub is then transferred covalently to the substrate lysine, enabling enrichment via denaturing streptavidin pulldown [15]. Substrate candidates can subsequently be identified via mass spectrometry (MS) or validated through immunoblotting [15].
Diagram 2: Ub-POD Experimental Workflow. The protocol involves co-transfection of BirA-E3 and AP-Ub constructs, biotin exposure, biotinylation and ubiquitination reactions, denaturing lysis, streptavidin pulldown, and mass spectrometry analysis.
Key Advantages and Implementation
Ub-POD offers several distinct advantages over conventional approaches [15]:
- Specificity: Uses wild-type BirA instead of the highly reactive but promiscuous mutant BirA* (R118G mutation) to restrain activity to BirA's acceptor peptide substrate only
- Sensitivity: Incorporates a modified acceptor peptide (-2) AP of BirA attached to the N-terminus of ubiquitin, rendering it selectively biotinylated by BirA WT in a proximity-dependent manner
- Practicality: A simple and cost-effective method using common chemicals that can be implemented in any laboratory setting
The protocol is optimized for identification of novel substrates via mass spectrometry or as a validation tool in combination with immunoblotting or immunofluorescence [15]. Successful implementation benefits from prior knowledge of triggers and constraints of the E3 ligase activity under investigation [15].
Table 3: Research Reagent Solutions for Ub-POD Protocol
| Reagent/Material | Function/Role | Specifications/Notes |
|---|---|---|
| BirA Vectors | Fuses BirA to candidate E3 ligase | Available from Addgene: 232584 (Empty BirA), 232586 (N-terminal tagging), 232587 (C-terminal tagging), 232588 (C-terminal with GSGS linker) [15] |
| Avi-tagged Ub Constructs | Fuses biotin acceptor peptide to ubiquitin | Modified Avi-tagged Ub construct (-2)AP-Ub used in protocol (Addgene: 232577, 232582, 232583) [15] |
| Streptavidin Agarose | Enrichment of biotinylated substrates | Enables pulldown under denaturing conditions [15] |
| MG132 | Proteasome inhibitor | Preserves ubiquitinated substrates by blocking degradation [15] |
| Benzonase Nuclease | Digests nucleic acids | Reduces sample viscosity and non-specific interactions [15] |
| N-ethylmaleimide (NEM) | Deubiquitinase inhibitor | Alkylates cysteine residues to prevent deubiquitination [15] |
Critical Steps and Troubleshooting
Successful application of the Ub-POD protocol requires attention to several critical steps [15]:
- Transfection Efficiency: Optimal transfection reagent should be selected based on the specific cell line of interest
- Proteasome Inhibition: MG132 treatment preserves ubiquitinated substrates by preventing proteasomal degradation
- Denaturing Conditions: Streptavidin pulldown under denaturing conditions reduces non-specific interactions
- Comprehensive Controls: Include appropriate negative controls (e.g., catalytically dead E3 mutants) to distinguish specific substrates
The highly Ub-specific labeling makes Ub-POD more appropriate for identifying ubiquitination substrates compared to other conventional proximity labeling or immunoprecipitation approaches [15].
Implications for Cancer Research and Therapeutics
The expanding substrate realm of ubiquitination has profound implications for cancer research and drug development. In pediatric solid tumors, the complex interplay between ubiquitination and lipid metabolic reprogramming identifies potential UPS-mediated therapeutic targets [13]. Integrating ubiquitination-based strategies with existing treatments may disrupt tumor metabolism and improve treatment efficacy [13].
The discovery that drug-like small molecules can serve as ubiquitination substrates opens avenues for harnessing the ubiquitin system to transform exogenous small molecules into novel chemical modalities within cells [12]. However, converting existing compounds into specific HUWE1 substrates or inhibitors requires enhanced specificity, as BI8626 elicits widespread proteomic effects and broadly reduces ubiquitination at many protein sites [12].
For researchers investigating ubiquitination substrates in tumor samples, these findings highlight the importance of considering non-protein substrates in experimental designs and data interpretation. The Ub-POD protocol provides a robust methodology for identifying novel E3 ligase substrates, while the expanding understanding of lipid metabolism regulation offers new perspectives on cancer metabolic dependencies.
The continued exploration of non-protein ubiquitination substrates will likely yield additional surprises and opportunities for therapeutic intervention in cancer and other diseases. Researchers are encouraged to consider these expanded substrate categories when designing studies on ubiquitination in tumor samples, as they may reveal previously unrecognized regulatory mechanisms and therapeutic targets.
Linking Ubiquitination to Tumor Microenvironment, Immune Infiltration, and Immunotherapy Response
The ubiquitin-proteasome system (UPS) has emerged as a critical regulator of cancer immunity, extending far beyond its traditional role in protein degradation. Ubiquitination, a key post-translational modification, orchestrates the stability, function, and trafficking of numerous proteins within the tumor microenvironment (TIME) [17]. This process involves a sequential enzymatic cascade comprising ubiquitin-activating enzymes (E1), ubiquitin-conjugating enzymes (E2), and ubiquitin ligases (E3), which collectively tag target proteins with ubiquitin chains [17]. The reverse process, mediated by deubiquitinating enzymes (DUBs), removes these tags, providing a dynamic regulatory mechanism for protein homeostasis [18].
Research now demonstrates that the UPS profoundly influences tumor immune evasion and response to immunotherapy by modulating immune checkpoint expression, immune cell infiltration, and cytokine signaling [17] [19]. Understanding these mechanisms provides novel strategic approaches for enhancing cancer immunotherapy, particularly for patients exhibiting resistance to current immune checkpoint inhibitors (ICIs) [18]. This application note outlines experimental frameworks for investigating ubiquitination pathways within the TIME and their translational potential for biomarker discovery and therapeutic development.
Molecular Mechanisms of Ubiquitination in Immune Regulation
Regulation of PD-1/PD-L1 Stability by Ubiquitination
The PD-1/PD-L1 axis represents a pivotal immune checkpoint pathway subjected to extensive ubiquitination regulation. E3 ubiquitin ligases and DUBs dynamically control the protein levels of PD-L1 on tumor cells and PD-1 on T cells, thereby modulating the strength of immune suppression.
- E3 Ligases in PD-L1 Degradation: The E3 ubiquitin ligase SPOP (Speckle-type POZ protein) directly binds to PD-L1 and promotes its K48-linked ubiquitination and proteasomal degradation, particularly in colorectal cancer [17]. This process can be inhibited by competitive binding partners; for instance, ALDH2 and SGLT2 interact with PD-L1, shielding it from SPOP-mediated degradation [17].
- Deubiquitination in PD-L1 Stabilization: Several DUBs counteract E3 ligase activity to stabilize PD-L1. USP5 has been identified as a key DUB that specifically removes K48-linked polyubiquitin chains from PD-L1, preventing its degradation and promoting immune resistance in melanoma [18]. Other DUBs, including CSN5 and USP22, also participate in PD-L1 stabilization across various cancer types [18].
Table 1: Key Ubiquitination Regulators of PD-1/PD-L1 Axis
| Regulator | Type | Target | Effect | Cancer Context |
|---|---|---|---|---|
| SPOP | E3 Ligase | PD-L1 | K48-linked ubiquitination and degradation | Colorectal Cancer, Hepatocellular Carcinoma |
| β-TrCP | E3 Ligase | PD-L1 | Degradation via GSK3β-phosphorylated PD-L1 | Multiple Cancers |
| FBXO22 | E3 Ligase | PD-L1 | Degradation | Lung Cancer |
| USP5 | DUB | PD-L1 | Deubiquitination and stabilization | Melanoma |
| CSN5 | DUB | PD-L1 | Deubiquitination and stabilization | Multiple Cancers |
| USP22 | DUB | PD-L1 | Deubiquitination and stabilization | Multiple Cancers |
Ubiquitination in Immune Checkpoint Activation
Beyond simply regulating protein abundance, ubiquitination can directly modulate the functional activation of immune checkpoint receptors. Recent research on LAG3 (Lymphocyte Activation Gene 3) reveals a novel non-degradative ubiquitination mechanism essential for its immunosuppressive function [20].
Upon engagement with its ligands (MHC class II or membrane-bound FGL1), LAG3 undergoes robust non-K48-linked polyubiquitination mediated by the E3 ligases c-Cbl and Cbl-b [20]. This ubiquitination induces a conformational change by disrupting the membrane binding of the juxtamembrane basic residue-rich sequence, thereby stabilizing the LAG3 cytoplasmic tail in a membrane-dissociated conformation that enables signal transduction and inhibitory function [20]. Therapeutic LAG3 antibodies function at least partially by repressing this activation-associated ubiquitination event [20].
Signaling Pathway Diagram
The following diagram illustrates the core ubiquitination regulatory network of PD-L1 stability within the tumor microenvironment:
Quantitative Analysis of Ubiquitination in Tumor Immunology
Ubiquitination-Related Prognostic Signatures (URPS)
Comprehensive pancancer analyses have revealed that ubiquitination signatures serve as powerful predictors of clinical outcomes and immunotherapy response. A study integrating data from 4,709 patients across 26 cohorts and five solid tumor types (lung cancer, esophageal cancer, cervical cancer, urothelial cancer, and melanoma) established a conserved ubiquitination-related prognostic signature (URPS) that effectively stratifies patients into distinct risk categories [21].
The URPS high-risk group demonstrated significantly worse survival outcomes across all analyzed cancers and served as a novel biomarker for predicting immunotherapy response [21]. Single-cell resolution analysis confirmed that URPS enabled precise classification of distinct cell types and correlated strongly with macrophage infiltration within the TIME [21]. Experimental validation identified the OTUB1-TRIM28 ubiquitination axis as a crucial modulator of the MYC pathway and patient prognosis [21].
Table 2: Ubiquitination-Based Biomarkers in Cancer Immunotherapy
| Biomarker Type | Key Components | Predictive Value | Validation Context |
|---|---|---|---|
| Ubiquitination-Related Prognostic Signature (URPS) | Multi-gene ubiquitination network | Stratifies high-risk vs low-risk patients; predicts immunotherapy benefit | Pancancer analysis (4,709 patients, 26 cohorts) |
| LAG3/CBL Co-expression | LAG3 + E3 ligases c-Cbl/Cbl-b | Identifies patients likely to respond to LAG3 blockade | Preclinical models and patient cohort analyses |
| PPP2R1A Mutations | PP2A scaffolding subunit | Predicts improved survival after immunotherapy | Ovarian clear cell carcinoma clinical trials |
| F-box Protein Expression Patterns | FBXW1 (β-TrCP) and others | Correlates with immune score and CD8+ T-cell infiltration | Lung cancer (LUAD) and renal cancer (KIRC) analyses |
Tumor Microenvironment and Immune Infiltration Signatures
Advanced profiling of the TIME has identified distinct immune cell infiltration patterns that correlate with ubiquitination regulation and immunotherapy response. Gene expression-based classification of twenty tumor types (7,162 samples) revealed that a signature enriched in B-cell markers consistently associated with improved immunotherapy efficacy across multiple cohorts, including IMvigor210 for urothelial cancer [22].
Notably, these infiltrate population signatures demonstrated more consistent association with treatment outcome than single cell-type models, suggesting they capture complex immunological responses involving multilayered relationships between distinct immune effector cells [22]. The signatures were most highly expressed in tumors with prominent immune cell invasion but consistently identified infiltrate presence even in relatively immune-restricted cases [22].
Experimental Protocols
Protocol 1: Assessing PD-L1 Ubiquitination Status and Stability
Purpose: To evaluate the ubiquitination level and protein stability of PD-L1 in tumor cells under various experimental conditions.
Materials:
- Cycloheximide (CHX) - protein synthesis inhibitor
- MG132 - proteasome inhibitor
- Anti-PD-L1 antibody for immunoprecipitation
- Anti-ubiquitin antibody (specific for K48-linked chains if possible)
- Lysis buffer (RIPA buffer with protease and deubiquitinase inhibitors)
- Cell culture models (appropriate tumor cell lines)
Procedure:
- Treat Cells: Culture tumor cells and apply experimental conditions (e.g., small molecule inhibitors, cytokine stimulation).
- Inhibit Protein Synthesis: Add cycloheximide (100 µg/mL) to halt new protein synthesis for time-course stability analysis.
- Harvest Cells: Lyse cells in RIPA buffer containing protease inhibitors and N-ethylmaleimide (deubiquitinase inhibitor) at various time points (0, 1, 2, 4, 8 hours).
- Immunoprecipitation: Incubate cell lysates with anti-PD-L1 antibody overnight at 4°C, then pull down with protein A/G beads.
- Western Blot Analysis: Resolve immunoprecipitates by SDS-PAGE and immunoblot with anti-ubiquitin and anti-PD-L1 antibodies.
- Quantification: Measure band intensities to determine PD-L1 half-life and ubiquitination levels under different conditions.
Applications: This protocol enables researchers to identify regulators of PD-L1 stability, including E3 ligases and DUBs, and to test potential therapeutic compounds that modulate PD-L1 turnover [17] [18].
Protocol 2: Constructing Ubiquitination Regulatory Networks from Patient Data
Purpose: To develop pancancer ubiquitination regulatory networks for prognostic stratification and therapy response prediction.
Materials:
- RNA-seq data from tumor samples (TCGA, GEO databases)
- Clinical annotation data (survival, treatment response)
- R or Python programming environment with appropriate packages (limma, survival, ggplot2 for R)
- Single-cell RNA sequencing data (if available)
Procedure:
- Data Acquisition and Preprocessing: Obtain transcriptomic data from public databases (TCGA, GEO). Normalize to TPM format and apply batch effect correction using ComBat algorithm.
- Ubiquitination Gene Selection: Curate ubiquitination-related genes from Gene Ontology databases and published literature.
- Differential Expression Analysis: Identify differentially expressed ubiquitination-related genes using limma package (FDR < 0.05, |log2FC| > 1).
- Prognostic Model Construction: Perform univariate Cox regression to identify survival-associated genes. Apply machine learning algorithms (Stepwise Cox, Lasso, Random Survival Forest) with 10-fold cross-validation to build optimal prognostic signature.
- Model Validation: Validate the prognostic model in independent immunotherapy cohorts. Assess predictive performance using ROC curves and C-index.
- Immune Correlations: Evaluate association between ubiquitination signature and immune cell infiltration using deconvolution algorithms (CIBERSORT) or single-cell data.
Applications: This computational approach identifies clinically relevant ubiquitination signatures, enables patient stratification, and reveals novel therapeutic targets [21] [18].
Experimental Workflow Diagram
The following diagram outlines the integrated experimental approach for studying ubiquitination in the tumor microenvironment:
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Research Reagents for Ubiquitination-Immunology Studies
| Reagent/Category | Specific Examples | Function/Application |
|---|---|---|
| Proteasome Inhibitors | MG132, Bortezomib, Carfilzomib | Blocks degradation of ubiquitinated proteins; stabilizes substrates for detection |
| DUB Inhibitors | PR-619 (broad-spectrum), P5091 (USP7), EOAI340214 (USP5) | Inhibits deubiquitinating enzymes; increases substrate ubiquitination and turnover |
| E3 Ligase Modulators | MLN4924 (NEDD8 activator), SCF complex inhibitors | Modulates E3 ligase activity; tests specificity of ubiquitination pathways |
| Ubiquitin Binding Reagents | K48- and K63-linkage specific antibodies, TUBE (Tandem Ubiquitin Binding Entity) reagents | Enrich and detect specific ubiquitin chain linkages; improve ubiquitinated protein recovery |
| Protein Synthesis Inhibitors | Cycloheximide (CHX) | Halts new protein synthesis; enables protein half-life determination in chase assays |
| Immunoprecipitation Antibodies | Anti-PD-L1, anti-PD-1, anti-LAG3, anti-ubiquitin | Target-specific immunoprecipitation for ubiquitination status analysis |
| Cell Line Models | Melanoma, NSCLC, colorectal cancer lines with defined ubiquitination profiles | Provide biological context for mechanistic studies and therapeutic testing |
The integration of ubiquitination regulation into our understanding of cancer immunity represents a paradigm shift in immunotherapy research. The experimental frameworks outlined herein provide systematic approaches for investigating how ubiquitination networks shape the tumor immune microenvironment and influence therapy response. The dynamic interplay between E3 ligases, DUBs, and immune checkpoints offers multiple therapeutic entry points for enhancing current immunotherapies.
Future directions should focus on developing selective small-molecule inhibitors targeting specific ubiquitination regulators in the TIME, validating ubiquitination-based biomarkers in prospective clinical trials, and exploring combination strategies that simultaneously target ubiquitination pathways and immune checkpoints. The convergence of ubiquitination research with artificial intelligence and multi-omics technologies promises to accelerate the discovery of novel therapeutic targets and personalized treatment approaches for cancer patients resistant to current immunotherapies [23] [24]. As our understanding of the ubiquitin code in cancer immunity deepens, targeting these pathways will undoubtedly become an integral component of precision immuno-oncology.
The Methodological Toolkit: From Proteomics to Proximity Labeling for Substrate Identification
Protein ubiquitination, a crucial post-translational modification, regulates diverse cellular functions including protein turnover, cell signaling, and trafficking. The dysregulation of ubiquitination pathways is implicated in various pathologies, most notably cancer. For researchers investigating tumor samples, comprehensively identifying ubiquitination substrates provides invaluable insights into disease mechanisms and potential therapeutic targets. This application note details three core high-throughput proteomic strategies—Ub tagging, antibody-based enrichment, and ubiquitin-binding domain (UBD)-based approaches—for the systematic mapping of ubiquitination events, with a specific focus on their application in tumor tissue research.
Ub Tagging-Based Approaches
Core Principle and Workflow
Ub tagging involves the genetic engineering of ubiquitin (Ub) with an affinity tag (e.g., His, Strep, or HA). When expressed in cells, this tagged Ub is incorporated into the ubiquitination machinery, allowing for the subsequent affinity-based purification of ubiquitinated substrates from complex lysates under denaturing conditions [2]. Following purification, the enriched proteins are digested with trypsin. A key feature of this process is the generation of a diagnostic di-glycine (Gly-Gly) remnant that remains attached to the modified lysine residue of the substrate peptide after tryptic digestion. This 114.04 Da mass shift is a definitive signature used for the mass spectrometry-based identification of ubiquitination sites [2].
Application in Tumor Research
This method is particularly powerful for cell line-based discovery studies. For instance, Danielsen et al. successfully identified 753 lysine ubiquitylation sites on 471 proteins in U2OS and HEK293T cells by constructing a cell line stably expressing Strep-tagged Ub [2]. The primary advantage is the ease of use and relatively low cost for initial, broad screening of ubiquitinated substrates in a controlled cellular environment.
Key Protocols
Protocol 1.1: Generation of Stable Cell Lines for Ub Tagging
- Construct Design: Clone the DNA sequence for the chosen affinity tag (e.g., 6xHis, Strep-tag II) in-frame at the N-terminus of ubiquitin in a mammalian expression vector.
- Cell Transfection: Introduce the construct into your chosen cancer cell line using a standard transfection method (e.g., lipofection, electroporation).
- Selection & Expansion: Select for stable integrants using the appropriate antibiotic (e.g., puromycin, G418) for 2-3 weeks.
- Validation: Confirm tag expression by western blotting of whole-cell lysates using an antibody against the tag or ubiquitin.
Protocol 1.2: Affinity Purification of Tagged Ubiquitinated Proteins
- Lysis: Harvest stable cells and lyse in a denaturing buffer (e.g., 8 M Urea, 100 mM NaH₂PO₄, 10 mM Tris-Cl, pH 8.0) supplemented with 5-10 mM imidazole and protease inhibitors (including deubiquitinase inhibitors like PR-619) [2] [25].
- Clarification: Centrifuge the lysate at 20,000 × g for 15 minutes to remove insoluble debris.
- Immobilized Metal Affinity Chromatography (IMAC): Incubate the clarified lysate with Ni-NTA agarose beads for 1-2 hours at room temperature with gentle rotation.
- Washing: Wash the beads sequentially with:
- Wash Buffer I: Lysis buffer.
- Wash Buffer II: Lysis buffer adjusted to pH 6.3.
- Elution: Elute the bound ubiquitinated proteins using an elution buffer containing 250 mM imidazole.
- Preparation for MS: Precipitate or buffer-exchange the eluate, then subject to tryptic digestion for LC-MS/MS analysis.
Advantages and Limitations
Table 1: Pros and Cons of Ub Tagging-Based Approaches
| Aspect | Advantages | Disadvantages |
|---|---|---|
| General Use | Easy, friendly, relatively low-cost [2] | Tagged Ub may not perfectly mimic endogenous Ub, potentially creating artifacts [2] |
| Sensitivity | Effective for broad substrate screening | Identification efficiency can be relatively low [2] |
| Specificity | Direct covalent labeling of substrates | Co-purification of histidine-rich or endogenously biotinylated proteins causes contamination [2] |
| Tumor Sample Application | Excellent for cell line models | Infeasible for direct use in animal or patient tissue samples [2] |
Antibody-Based Enrichment Strategies
Core Principle and Workflow
Antibody-based enrichment, often referred to as the PTMScan method, utilizes antibodies that are specific to the di-glycine (K-ε-GG) remnant left on ubiquitinated peptides after tryptic digestion. This allows for the direct immunoaffinity purification (IAP) of ubiquitinated peptides from a complex mixture of digested cellular proteins, which are then identified and quantified by LC-MS/MS [26]. This method is "target-agnostic" and does not require genetic manipulation, making it suitable for clinical samples.
High-Throughput Innovations and Applications
Recent advancements have significantly increased the throughput and reproducibility of antibody-based ubiquitinomics. The development of the automated UbiFast method is a key innovation. This approach uses magnetic bead-conjugated K-ε-GG antibodies (HS mag anti-K-ε-GG) and a magnetic particle processor to automate the enrichment and on-bead TMT labeling of Ub-peptides. This automated workflow can process up to 96 samples in a single day, identifies ~20,000 ubiquitylation sites from a TMT10-plex, and greatly improves reproducibility while reducing processing time [27]. This makes it ideal for large-scale patient cohort studies. Furthermore, platform like the one from NEOsphere Biotechnologies combines high-throughput global proteomics to identify protein downregulation with high-throughput interactomics to reveal ternary complex formation, providing a comprehensive view of degrader function in disease-relevant contexts, including primary cells and patient-derived tissues [28].
Key Protocols
Protocol 2.1: Automated UbiFast for Ubiquitinome Profiling (e.g., from Tumor Tissue)
- Sample Preparation: Homogenize patient-derived xenograft (PDX) or frozen tumor tissue. Perform in-solution digestion with trypsin to generate peptides [27].
- Peptide Clean-up: Desalt peptides using a solid-phase extraction cartridge (e.g., Sep-Pak tC18).
- Automated Enrichment: Use a magnetic particle processor with HS mag anti-K-ε-GG beads to enrich for K-ε-GG-containing peptides. The automation handles all washing steps.
- On-Bead TMT Labeling: While peptides are still bound to the magnetic beads, label them with Tandem Mass Tag (TMT) reagents. This step is performed on the automated platform [27].
- Pooling and Elution: Combine the TMT-labeled samples and elute the peptides from the beads.
- LC-MS/MS Analysis: Analyze the enriched, multiplexed peptide sample by liquid chromatography-tandem mass spectrometry.
Protocol 2.2: PTMScan Discovery for Ubiquitinated Peptides
- Digestion: Digest the protein sample from tumor lysates into peptides.
- Immunoaffinity Purification (IAP): Incubate the peptide mixture with a PTM-specific anti-K-ε-GG antibody immobilized on beads [26].
- Washing: Wash the beads extensively to remove non-specifically bound peptides.
- Elution: Elute the enriched ubiquitinated peptides using a low-pH buffer.
- LC-MS/MS Analysis: Identify and quantify the eluted peptides.
Advantages and Limitations
Table 2: Pros and Cons of Antibody-Based Enrichment
| Aspect | Advantages | Disadvantages |
|---|---|---|
| General Use | Does not require genetic manipulation; can use linkage-specific antibodies [2] | High cost of high-quality antibodies [2] |
| Sensitivity | High sensitivity for modified peptides; automated UbiFast identifies ~20,000 sites [27] | Non-specific binding can occur, requiring careful controls [2] |
| Specificity | Directly targets the definitive K-ε-GG signature | Underlying peptide sequence can influence antibody binding efficiency |
| Tumor Sample Application | Directly applicable to animal tissues and clinical samples [28] [27] [2] | Limited amount of starting material from biopsies can be a constraint |
UBD-Based Strategies
Core Principle and Workflow
This strategy leverages natural Ubiquitin-Binding Domains (UBDs), which are protein modules that recognize and bind to ubiquitin or specific ubiquitin chain linkages. These UBDs (e.g., from certain E3 ligases, DUBs, or Ub receptors) are used as affinity reagents to capture endogenously ubiquitinated proteins from native or denatured cell lysates [2] [25]. The use of tandem-repeated UBDs improves the affinity and specificity of the enrichment.
Advanced Methodology: DRUSP for Enhanced Ubiquitinomics
A major challenge in UBD-based enrichment under native conditions is the interference from deubiquitinating enzymes (DUBs) and proteasomes, as well as inefficient protein extraction. The Denatured-Refolded Ubiquitinated Sample Preparation (DRUSP) method overcomes this. DRUSP involves lysing samples in a strongly denaturing buffer to inactivate enzymes and fully extract proteins, followed by a refolding step using filters to restore the native spatial structure of ubiquitin and ubiquitin chains. This allows for subsequent highly efficient recognition and enrichment by a tandem hybrid UBD (ThUBD) [25]. This method has been shown to yield a ubiquitin signal nearly three times stronger than control methods and improves overall ubiquitin signal enrichment by approximately 10-fold, significantly enhancing the stability and reproducibility of ubiquitinomics research [25]. It has been successfully applied to deep ubiquitinome profiling of early mouse liver fibrosis.
Key Protocols
Protocol 3.1: DRUSP with ThUBD Enrichment
- Denaturing Lysis: Lyse tumor tissue or cells in a strongly denatured buffer (e.g., containing SDS or Urea) to inactivate DUBs and proteasomes and ensure complete protein extraction [25].
- Refolding: Use a filter-based device to perform buffer exchange, replacing the denaturing buffer with a non-denaturing lysis buffer. This allows the ubiquitinated proteins to refold into their native conformations [25].
- UBD Enrichment: Incubate the refolded lysate with the immobilized ThUBD (or chain-specific UBDs) to capture ubiquitinated proteins.
- Washing: Wash the beads thoroughly with a non-denaturing buffer to remove non-specifically bound proteins.
- Elution and Digestion: Elute the bound ubiquitinated proteins, then proceed with standard tryptic digestion and LC-MS/MS preparation.
Advantages and Limitations
Table 3: Pros and Cons of UBD-Based Strategies
| Aspect | Advantages | Disadvantages |
|---|---|---|
| General Use | Can be engineered for linkage specificity; DRUSP offers superior versatility [25] | Low affinity of single UBDs can limit purification efficiency [2] |
| Sensitivity | DRUSP significantly enhances signal and positive identifications [25] | Tandem UBDs are more complex to produce |
| Specificity | High specificity for ubiquitin chains; can be tailored for chain-type | Potential for co-purification of UBD-binding partner proteins |
| Tumor Sample Application | DRUSP demonstrates enhanced quantitative accuracy and reproducibility for tissue samples [25] | The refolding step requires optimization for different sample types |
The Scientist's Toolkit: Research Reagent Solutions
Table 4: Essential Reagents for Ubiquitin Proteomics
| Reagent / Tool | Function | Example Use Cases |
|---|---|---|
| Tagged Ubiquitin | Affinity purification of ubiquitinated substrates | 6xHis-Ub, Strep-Ub for Ub tagging in cell lines [2] |
| Anti-K-ε-GG Antibody | Immunoaffinity enrichment of ubiquitinated peptides | PTMScan Discovery; Automated UbiFast [27] [26] |
| Linkage-Specific Ub Antibodies | Enrich proteins with specific Ub chain linkages (K48, K63, etc.) | Studying specific ubiquitination pathways in cancer [2] |
| Tandem Hybrid UBD (ThUBD) | High-affinity capture of diverse ubiquitinated proteins | DRUSP protocol for enhanced ubiquitinome coverage [25] |
| Deubiquitinase Inhibitors | Preserve ubiquitin signals during sample preparation | PR-619, added to lysis buffers [27] [25] |
| Tandem Mass Tags (TMT) | Multiplexed quantitative proteomics | Automated UbiFast for profiling 10+ samples simultaneously [27] |
Integrated Data Analysis Workflow
Following enrichment and LC-MS/MS, data processing is critical. Key steps include:
- Protein Identification: Using software to match spectra to peptides and proteins, focusing on the diagnostic 114.04 Da Gly-Gly modification [29].
- Quantification: Comparing protein/peptide abundance across samples (e.g., tumor vs. normal).
- Differential Expression Analysis: Identifying significantly altered ubiquitination sites using fold change (e.g., ≥1.5) and p-value (e.g., ≤0.05) thresholds [29].
- Functional Annotation: Using GO, KEGG, and other databases to understand the biological processes and pathways enriched for differentially ubiquitinated proteins [29].
- Network Analysis: Constructing protein-protein interaction (PPI) networks to identify key regulatory nodes [29].
Strategic Workflow Diagram
The following diagram illustrates the strategic decision-making process for selecting the appropriate high-throughput ubiquitin proteomics method based on research goals and sample type:
The choice of high-throughput proteomic approach for identifying ubiquitination substrates in tumor samples depends heavily on the specific research context. Ub tagging is ideal for foundational discovery in cell line models. Antibody-based enrichment, particularly automated platforms like UbiFast, offers a powerful, direct, and high-throughput solution for clinical tissues and complex sample sets. For the most challenging samples where maximizing signal and reproducibility is paramount, the UBD-based DRUSP method provides a significant advantage. By leveraging these complementary strategies, researchers can systematically decode the ubiquitinome to uncover novel disease mechanisms and therapeutic opportunities in cancer biology.
The ubiquitin-proteasome system (UPS) represents a crucial regulatory mechanism in eukaryotic cells, controlling approximately 80-90% of cellular proteolysis and governing virtually all cellular processes, from cell cycle progression to DNA repair and immune responses [8] [30]. In cancer research, dysregulation of the ubiquitin system is increasingly recognized as a hallmark of tumorigenesis, with alterations in ubiquitination pathways contributing to unchecked proliferation, evasion of apoptosis, and metabolic reprogramming [8]. For researchers investigating ubiquitination substrates in tumor samples, the fundamental challenge has been the transient nature of ubiquitination—polyubiquitin chains are rapidly removed by deubiquitinating enzymes (DUBs) or lead to instantaneous proteasomal degradation of the modified protein [31]. This instability is particularly problematic when working with precious clinical tumor specimens, where ubiquitination states may be captured at a single time point and sample quantity is limited.
Tandem Ubiquitin Binding Entities (TUBEs) have emerged as transformative tools that directly address these challenges. These engineered reagents comprise multiple ubiquitin-associated (UBA) domains fused in tandem, conferring nanomolar affinity for polyubiquitin chains and protecting them from deubiquitination and proteasomal degradation [32] [33]. This technology enables researchers to "freeze" the endogenous ubiquitination state of proteins in tumor samples, providing an unprecedented window into the dynamic ubiquitin code that regulates oncogenic and tumor suppressive pathways. The application of TUBEs in cancer research allows for the precise interrogation of ubiquitination-mediated events that dictate histological fate, therapeutic response, and patient prognosis [8].
TUBE Technology: Principles and Reagent Solutions
Fundamental Mechanism of Polyubiquitin Stabilization
TUBEs function through a multi-domain architecture that creates high-avidity interactions with polyubiquitin chains. Unlike single UBA domains with micromolar affinity, tandem UBA domains in TUBEs achieve nanomolar binding affinity (Kd) through avidity effects, significantly outperforming conventional ubiquitin antibodies [33]. This strong binding physically shields polyubiquitin chains from the activity of DUBs, thereby preserving the ubiquitination state of substrates during experimental procedures. Research demonstrates that TUBEs can protect polyubiquitinated proteins in cell lysates from proteasomal degradation and deubiquitination as efficiently as specific inhibitors of these processes [31]. This protective function is particularly critical for tumor samples, where endogenous DUB activity remains high even after cell lysis.
The development of trypsin-resistant TUBEs (TR-TUBEs) further advanced the utility of this technology for mass spectrometry-based proteomics. TR-TUBEs are engineered to resist tryptic digestion while maintaining their ability to interact with all eight types of polyubiquitin chain linkages (M1, K6, K11, K27, K29, K33, K48, and K63), enabling subsequent proteomic analysis without interference from TUBE-derived peptides [31]. This innovation allows researchers to directly identify ubiquitination sites on substrates isolated from complex tumor lysates.
Research Reagent Solutions for Tumor Substrate Identification
Table 1: Key TUBE Reagents for Ubiquitination Research in Tumor Samples
| Reagent Type | Specificity | Key Applications in Cancer Research | Technical Features |
|---|---|---|---|
| Pan-Selective TUBEs (TUBE1, TUBE2) | All ubiquitin chain linkages | Comprehensive ubiquitome analysis; Unknown substrate identification | Binds all linkage types; Ideal for initial discovery phases [33] |
| K48-Selective TUBE | K48-linked chains | Studying proteasomal degradation pathways; PROTAC mechanism validation | Enhanced selectivity for degradation signals [32] [33] |
| K63-Selective TUBE | K63-linked chains (1,000-10,000-fold preference) | Investigating signaling pathways, DNA repair mechanisms, inflammation | Critical for NF-κB, MAPK pathways in cancer [32] [33] |
| TR-TUBE (Trypsin-Resistant) | All ubiquitin chain linkages | Mass spectrometry-based substrate identification; Ubiquitin remnant profiling | Resists tryptic digestion; Compatible with MS workflows [31] |
| Phospho-TUBE (Emerging) | Ser65-phosphorylated ubiquitin | Monitoring mitochondrial quality control; Parkinson's disease research | Binds phospho-ubiquitin; Studies PINK1-parkin pathway [33] |
The selection of appropriate TUBE reagents depends on the specific research objectives. For discovery-phase projects aiming to identify novel ubiquitination substrates in tumor samples, pan-selective TUBEs provide the broadest coverage. When investigating specific pathways—such as degradation-mediated regulation of tumor suppressors or kinase signaling activation in cancer—chain-selective TUBEs offer precise interrogation tools. The integration of TR-TUBEs with anti-diglycine (diGly) remnant antibodies enables comprehensive mapping of ubiquitination sites, creating powerful workflows for substrate identification in tumor samples [31].
Quantitative Performance and Technical Specifications
Affinity and Sensitivity Comparisons
Recent technological advancements have yielded significant improvements in TUBE performance. The development of Tandem Hybrid Ubiquitin Binding Domain (ThUBD) fusion proteins has demonstrated a 16-fold wider linear range for capturing polyubiquitinated proteins from complex proteome samples compared to first-generation TUBE-coated plates [34]. This enhanced sensitivity is particularly valuable for tumor research, where sample quantities are often limited. The ThUBD-coated platform can detect ubiquitination signals from as little as 0.625 μg of input material, enabling robust analysis of biopsy specimens [34].
Table 2: Quantitative Performance Metrics of Ubiquitin Capture Technologies
| Performance Metric | Traditional TUBE | ThUBD Technology | Application in Tumor Samples |
|---|---|---|---|
| Detection Sensitivity | Standard sensitivity | 16-fold improvement | Enables analysis of limited biopsy material [34] |
| Dynamic Range | Limited linear range | Significantly wider | Accurate quantification across abundance levels [34] |
| Input Requirement | Higher protein input | As low as 0.625 μg | Critical for precious clinical samples [34] |
| Chain-Type Bias | Variable bias | Unbiased recognition | Comprehensive view of ubiquitination status [34] |
| Throughput Capacity | Moderate | High-throughput (96-well format) | Suitable for drug screening projects [34] |
The quantitative capabilities of modern TUBE technologies enable researchers to not only identify ubiquitinated substrates but also monitor dynamic changes in ubiquitination in response to therapeutic interventions. This is particularly relevant for studying targeted protein degradation approaches such as PROTACs (Proteolysis Targeting Chimeras), where understanding the kinetics and efficiency of target ubiquitination is essential for drug development [32] [34].
Experimental Protocols for Tumor Substrate Identification
Protocol 1: TR-TUBE Workflow for Substrate Identification in Tumor Lysates
Objective: To identify novel ubiquitination substrates from primary tumor samples using TR-TUBE enrichment coupled with mass spectrometry.
Materials:
- TR-TUBE expression plasmid or recombinant protein [31]
- Tumor tissue samples (fresh frozen or preserved)
- Lysis buffer: 50 mM Tris-HCl (pH 7.5), 150 mM NaCl, 1% Triton X-100, 1 mM N-Ethylmaleimide (NEM), 10 μM MG132, and protease inhibitors [31]
- Anti-diGly remnant antibody [31]
- FLAG-affinity resin (if using FLAG-tagged TR-TUBE)
- Mass spectrometry-compatible reagents
Procedure:
- Sample Preparation: Homogenize tumor tissue in ice-cold lysis buffer containing NEM (DUB inhibitor) and MG132 (proteasome inhibitor). Maintain samples at 4°C throughout processing to preserve ubiquitination states.
- Clarification: Centrifuge lysates at 16,000 × g for 15 minutes at 4°C. Collect supernatant and determine protein concentration.
- TR-TUBE Enrichment: Incubate 1-2 mg of tumor lysate with recombinant TR-TUBE (or lysate from TR-TUBE-transfected cells) for 2 hours at 4°C with gentle rotation [31].
- Affinity Purification: Add FLAG-affinity resin (for FLAG-tagged TR-TUBE) and incubate for an additional 1 hour. Wash resin extensively with lysis buffer to remove non-specifically bound proteins.
- Elution: Elute bound ubiquitinated proteins using FLAG peptide competition or direct denaturation in MS-compatible buffer.
- Trypsin Digestion: Digest eluted proteins with trypsin following standard proteomic protocols. TR-TUBE resistance ensures it does not interfere with the resulting peptides [31].
- diGly Enrichment: Incubate tryptic peptides with anti-diGly remnant antibody to specifically isolate ubiquitinated peptides [31].
- Mass Spectrometry Analysis: Analyze enriched peptides by LC-MS/MS to identify ubiquitination sites and corresponding proteins.
Applications in Tumor Research: This protocol has been successfully applied to identify ubiquitination substrates in various cancer contexts, including the discovery that OTUB1-TRIM28 ubiquitination plays a crucial role in modulating the MYC pathway and influencing patient prognosis [8]. The identification of such ubiquitination-regulated pathways provides new therapeutic opportunities for targeting traditionally "undruggable" oncogenes like MYC.
Protocol 2: Chain-Specific TUBE Assay for Pathway Analysis in Cancer Signaling
Objective: To characterize linkage-specific ubiquitination events in tumor samples using chain-selective TUBEs.
Materials:
- Chain-specific TUBEs (K48-, K63-selective, etc.) [32] [33]
- Tumor cell lines or tissue lysates
- TUBE-coated 96-well plates (commercially available) [34]
- Target-specific antibodies for proteins of interest
- Detection reagents compatible with your readout system
Procedure:
- Plate Coating: Coat high-binding 96-well plates with chain-selective TUBEs (1.03 μg/well optimal for ThUBD) in carbonate buffer overnight at 4°C [34].
- Blocking: Block plates with 3% BSA in TBST for 2 hours at room temperature.
- Sample Incubation: Add tumor lysates (25-50 μg/well) to TUBE-coated wells and incubate for 2 hours at room temperature with gentle shaking.
- Washing: Wash wells 3-5 times with TBST to remove unbound proteins.
- Target Detection: Incubate with primary antibody against protein of interest (e.g., RIPK2, MYC, p53) followed by HRP-conjugated secondary antibody [32].
- Signal Development: Add chemiluminescent or colorimetric substrate and measure signal.
- Data Analysis: Normalize signals to total input protein and compare across experimental conditions.
Applications in Tumor Research: This approach has been used to demonstrate that inflammatory agent L18-MDP stimulates K63 ubiquitination of RIPK2, which can be faithfully captured using K63-TUBEs, while PROTAC-induced degradation was selectively detected with K48-TUBEs [32]. In cancer research, this enables precise dissection of whether an oncoprotein is regulated through degradative (K48) or signaling (K63) ubiquitination, informing therapeutic strategy.
Protocol 3: High-Throughput PROTAC Screening in Tumor Models
Objective: To screen for PROTAC-induced ubiquitination of target proteins in cancer cell lines using TUBE-based platforms.
Materials:
- TUBE-coated 96-well plates [34]
- Cancer cell lines expressing target protein of interest
- PROTAC compound library
- Cell lysis buffer with DUB and proteasome inhibitors
- Detection antibodies specific to target protein
Procedure:
- Cell Treatment: Seed cancer cells in 96-well culture plates and treat with PROTAC compounds for predetermined time points.
- Cell Lysis: Lyse cells directly in culture plates using lysis buffer containing NEM and MG132.
- Ubiquitin Capture: Transfer lysates to TUBE-coated plates and incubate for 2 hours at room temperature.
- Target Detection: Detect captured ubiquitinated targets using target-specific antibodies as in Protocol 2.
- High-Throughput Readout: Use compatible detection systems (e.g., chemiluminescence, fluorescence) amenable to automated plate readers.
- Data Analysis: Quantify PROTAC-induced ubiquitination relative to vehicle controls.
Applications in Tumor Research: This protocol enables rapid screening of novel PROTAC molecules for their ability to induce target ubiquitination, a critical step in targeted protein degradation therapeutics. The platform has been validated for endogenous proteins like RIPK2, demonstrating that PROTAC-mediated ubiquitination is preferentially captured using K48-TUBEs, confirming the degradative mechanism [32].
Signaling Pathways and Experimental Workflows
Ubiquitin Signaling Pathways in Cancer Biology
The following diagram illustrates key ubiquitin-mediated signaling pathways relevant to cancer research, highlighting where TUBE-based analysis provides critical insights:
Diagram 1: Ubiquitin Signaling Pathways in Cancer Biology. TUBE-based analysis enables researchers to interrogate specific ubiquitin linkages that govern key cancer-relevant processes, from protein degradation to histological fate decisions.
Experimental Workflow for Tumor Substrate Identification
The following diagram outlines a comprehensive workflow for identifying and validating ubiquitination substrates in tumor samples using TUBE technology:
Diagram 2: Experimental Workflow for Tumor Substrate Identification. TUBE technology enables multiple analytical pathways from a single tumor sample, supporting applications from basic mechanism elucidation to therapeutic development.
Applications in Cancer Research and Therapeutic Development
The integration of TUBE technology into cancer research has yielded significant insights into tumor biology and therapeutic opportunities. A pan-cancer analysis of ubiquitination networks revealed that ubiquitination scores positively correlate with squamous or neuroendocrine transdifferentiation in adenocarcinoma, providing molecular explanations for histological transformations observed in clinical practice [8]. Furthermore, the identification of the OTUB1-TRIM28 ubiquitination axis as a regulator of MYC pathway activity demonstrates how TUBE-facilitated substrate identification can reveal new strategies for targeting previously undruggable oncoproteins [8].
In drug development, TUBE platforms have become invaluable for characterizing PROTAC molecules and molecular glues that harness the ubiquitin system for therapeutic protein degradation. The ability to monitor linkage-specific ubiquitination in high-throughput formats enables rapid screening and optimization of targeted protein degradation therapeutics [32] [34]. This application is particularly relevant for cancer drug discovery, where PROTACs have shown remarkable efficacy in targeting disease-related proteins previously considered undruggable, including androgen receptor, estrogen receptor, BTK, BCL2, and c-MET [32].
The prognostic value of ubiquitination signatures in cancer is increasingly recognized. Research utilizing TUBE-compatible methodologies has established that conserved ubiquitination-related prognostic signatures (URPS) can effectively stratify patients into high-risk and low-risk groups with distinct survival outcomes across multiple cancer types [8]. These signatures also show promise as biomarkers for predicting immunotherapy response, potentially identifying patients more likely to benefit from immune checkpoint inhibitors.
TUBE technology has revolutionized the study of ubiquitination in cancer research by stabilizing otherwise transient polyubiquitin chains and enabling their comprehensive analysis. The protocols and applications outlined in this document provide researchers with robust methodologies for identifying ubiquitination substrates in tumor samples, characterizing ubiquitin-dependent signaling pathways, and advancing therapeutic development. As the ubiquitin field continues to evolve, emerging TUBE variants—including phospho-specific TUBEs and enhanced affinity constructs—promise to further illuminate the complex ubiquitin code that governs cancer biology and treatment response.
The identification of genuine substrates for E3 ubiquitin ligases has remained one of the most challenging tasks in ubiquitin research, primarily due to the difficulty in distinguishing true ubiquitination targets from mere interacting proteins. BioE3 represents an innovative technological breakthrough that addresses this fundamental challenge by enabling the specific, proximity-dependent labeling and identification of substrates for E3 ligases of interest [35]. This method combines two powerful elements: (1) the fusion of the biotin ligase BirA to an E3 ligase of interest, and (2) the use of ubiquitin (Ub) fused to a low-affinity biotin acceptor peptide (bioGEF) [35] [36]. The core principle of BioE3 leverages proximity-dependent biotinylation to mark ubiquitinated substrates at the moment they are modified by the BirA-E3 fusion protein, allowing for their subsequent streptavidin-based purification and identification through liquid chromatography-mass spectrometry (LC-MS/MS) [35].
The biological significance of this methodology is profound when considered within the context of tumor research. E3 ligases regulate countless cellular processes relevant to oncogenesis, including DNA damage response, cell cycle progression, and signal transduction pathways [37] [38] [39]. Understanding the specific substrates targeted by oncogenic E3 ligases or tumor suppressors provides critical insights into cancer mechanisms and potential therapeutic vulnerabilities. For example, RNF4, a SUMO-targeted E3 ubiquitin ligase, sustains Myc-driven tumorigenesis by facilitating DNA replication, while its deficiency results in genomic instability and cell death [38]. The ability to comprehensively map E3 substrates using BioE3 offers unprecedented opportunities to decipher the complex ubiquitination networks that govern tumor development and progression.
Core Principles and Engineering Innovations
Key Components and Mechanism
The BioE3 system employs a sophisticated two-component mechanism that ensures specific labeling of bona fide E3 substrates:
BirA-E3 Fusion Constructs: The Escherichia coli-derived biotin ligase BirA is genetically fused to the N-terminus of the E3 ligase of interest, positioning the biotinylation enzyme in close proximity to substrates as they are ubiquitinated [35]. This strategic placement enables spatial-specific labeling events that are critical for substrate identification.
bioGEFUb Substrate Labeling Module: A version of ubiquitin is fused to an engineered AviTag variant (bioGEF) that exhibits lower affinity for BirA compared to the wild-type AviTag (bioWHE) [35]. This bioGEFUb construct is incorporated into a doxycycline-inducible lentiviral vector for generation of stable cell lines, allowing controlled expression in various cell types including HEK293FT and U2OS [35].
The operational sequence begins when cells expressing both components are grown in biotin-depleted media, followed by doxycycline induction to express bioGEFUb and the BirA-E3 fusion. Upon addition of exogenous biotin, the BirA-E3 fusion specifically biotinylates the bioGEFUb molecule as it is being incorporated onto substrates, creating a permanent biotin tag on ubiquitinated proteins [35]. These biotinylated substrates can then be efficiently captured using streptavidin beads under stringent washing conditions and identified through proteomic analysis.
Engineering for Specificity
A critical innovation in the BioE3 system was the engineering of the bioGEF tag to minimize non-specific biotinylation. Initial experiments with the wild-type AviTag (bioWHE) revealed substantial non-specific labeling independent of BirA localization, compromising experimental specificity [35]. The bioGEF variant, containing mutations in the C-terminal WHE sequence, demonstrated dramatically reduced non-specific biotinylation while maintaining efficient incorporation into substrates [35]. This enhancement allows BioE3 to capture transient ubiquitination events with high fidelity, a crucial requirement for identifying genuine E3 substrates among the complex cellular interactome.
Table: Key Components of the BioE3 System
| Component | Description | Function |
|---|---|---|
| BirA-E3 Fusion | Biotin ligase fused to E3 ubiquitin ligase | Positions biotinylation activity near substrates during ubiquitination |
| bioGEFUb | Ubiquitin fused to low-affinity AviTag variant | Serves as bait for proximity-dependent biotinylation when incorporated into substrates |
| Streptavidin Capture | High-affinity biotin-binding resin | Isolates biotinylated substrates from complex cellular lysates |
| LC-MS/MS | Liquid chromatography with tandem mass spectrometry | Identifies captured substrates with high sensitivity and specificity |
Applications in E3 Ligase Substrate Identification
Validation with RING-Type E3 Ligases
The BioE3 platform has been successfully validated using well-characterized RING-type E3 ligases, including RNF4 and MIB1, demonstrating its capacity to identify both known and novel substrates [35]. For RNF4, a SUMO-targeted ubiquitin ligase with established roles in DNA damage response and PML body regulation, BioE3 confirmed known interactors while expanding the repertoire of potential substrates [35] [38]. The functional significance of RNF4 substrates is particularly relevant in oncogenesis, as RNF4 activity is essential for normal DNA replication, and in its absence, cells exhibit failure in ATR-CHK1 signaling of replication stress and reduced accumulation of factors that mediate replication fork stability [38].
For MIB1, an E3 ligase involved in endocytosis, autophagy, and centrosome dynamics, BioE3 successfully identified targets consistent with its known cellular functions [35]. The methodology was further extended to less-characterized RING E3 ligases, including the mitochondrial membrane-bound MARCH5 and the cytoplasmic RNF214, yielding novel substrates that provide insight into their biological roles and potential connections to tumor pathways [35]. The ability of BioE3 to illuminate the functions of previously uncharacterized E3 ligases makes it particularly valuable for cancer research, where many E3 ligases remain poorly understood despite their implication in tumorigenesis.
Adaptation for HECT-Type E3 Ligases and CRLs
The versatility of BioE3 is evidenced by its successful application to different classes of E3 ligases. The system works effectively with NEDD4, a HECT-type E3 ligase, identifying both established and novel targets linked to vesicular trafficking pathways [35]. This expansion to HECT E3s demonstrates the general applicability of the BioE3 approach across distinct E3 ligase families with different catalytic mechanisms.
Furthermore, recent research has confirmed that BioE3 is suitable for studying multi-subunit Cullin-RING E3 ligases (CRLs), the most utilized E3-type for targeted protein degradation strategies [36]. Using cereblon (CRBN) – a substrate receptor of the CRL4 complex – as proof of concept, BioE3 identified both endogenous substrates and drug-induced neosubstrates upon pomalidomide treatment [36]. This application revealed a major rearrangement of the endogenous ubiquitination landscape upon molecular glue treatment, highlighting the potential of BioE3 to characterize both on-target and off-target effects of therapeutic compounds in development for cancer treatment.
Table: E3 Ligases Studied Using BioE3 and Key Findings
| E3 Ligase | Type | Cellular Functions | Key Substrates/Findings |
|---|---|---|---|
| RNF4 | RING/STUbL | DNA damage response, PML bodies | Replication fork stability factors, DNA repair proteins [35] [38] |
| MIB1 | RING | Endocytosis, autophagy, centrosome dynamics | Endocytic trafficking proteins, centrosomal components [35] |
| NEDD4 | HECT | Vesicular trafficking, protein sorting | Novel vesicle trafficking regulators [35] |
| CRBN | CRL Subunit Receptor | Targeted protein degradation | Endogenous substrates & molecular glue-induced neosubstrates (e.g., SALL4, CSDE1) [36] |
Experimental Protocol for BioE3
Cell Line Preparation and Transfection
The standard BioE3 protocol begins with the generation of stable cell lines expressing the inducible bioGEFUb construct:
Generate Stable Cell Lines: Create HEK293FT or U2OS cell lines stably expressing TRIPZ-bioGEFUb using lentiviral transduction and appropriate selection markers [35] [36]. The use of a doxycycline-inducible system allows tight control over bioGEFUb expression.
Culture in Biotin-Depleted Conditions: Plate cells in biotin-free media supplemented with 10% dialyzed fetal bovine serum (3.5 kDa MWCO) 24 hours prior to transfection to deplete endogenous biotin sources [35] [36]. This step is crucial for minimizing background biotinylation.
Introduce BirA-E3 Construct: Transfect cells with the BirA-E3 fusion construct using standard transfection methods appropriate for the cell type. The BirA component is typically fused to the N-terminus of the E3 ligase to minimize steric interference with C-terminal functional domains, particularly the RING domains [35].
Induce bioGEFUb Expression: Add doxycycline (concentration optimized for the cell line, typically 0.5-1 μg/mL) to induce bioGEFUb expression for 24 hours [35]. This timeframe allows sufficient incorporation of bioGEFUb into cellular substrates.
Biotin Pulse and Substrate Capture
Following the expression phase, a controlled biotin pulse enables specific labeling:
Biotin Pulse: Add exogenous biotin (50-100 μM) to the culture media for a limited time (typically 0.5-2 hours) to allow proximity-dependent biotinylation of bioGEFUb as it is incorporated onto substrates by the BirA-E3 fusion [35]. The shorter pulse times reduce non-specific background.
Cell Lysis and Streptavidin Capture: Harvest cells and lyse using RIPA buffer or similar denaturing conditions supplemented with protease inhibitors and deubiquitinase inhibitors to preserve ubiquitination signatures [35]. Incubate clarified lysates with streptavidin-coated beads under stringent washing conditions (e.g., high salt, detergent-containing buffers) to minimize non-specific interactions.
On-Bead Digestion and Proteomic Analysis: After extensive washing, subject captured proteins to on-bead tryptic digestion followed by LC-MS/MS analysis for substrate identification [35] [36]. Appropriate controls (e.g., cells lacking BirA-E3 expression or biotin pulse) should be included to account for non-specific binders.
BioE3 Experimental Workflow: This diagram outlines the key steps in the BioE3 protocol, from cell line preparation to substrate identification.
Optimization and Troubleshooting
Several optimization steps are critical for successful BioE3 experiments:
Control Biotin Availability: The pre-culture in biotin-depleted media followed by a timed biotin pulse is essential for reducing background signal and achieving specific labeling [35].
Validate E3 Localization and Function: Confirm that the BirA-E3 fusion protein localizes correctly within cells and maintains catalytic activity, as improper localization or function will compromise substrate identification [35].
Include Appropriate Controls: Essential controls include cells expressing BirA alone (without E3 fusion), non-biotin-pulsed samples, and samples treated with E3 ligase inhibitors to establish specificity [35] [36].
Proteasome Inhibition: For detecting substrates that are rapidly degraded, include proteasome inhibitors (e.g., bortezomib, MG132) during the biotin pulse to stabilize ubiquitinated proteins [36].
Research Toolkit: Essential Reagents and Solutions
Table: Key Research Reagents for BioE3 Experiments
| Reagent/Solution | Function | Application Notes |
|---|---|---|
| TRIPZ-bioGEFUb Lentiviral Vector | Inducible expression of bioGEFUb | Available through Addgene (#208045) [35] |
| BirA-E3 Fusion Constructs | E3-specific biotinylation activity | Custom cloning required for E3 of interest; BirA at N-terminus recommended [35] |
| Dialyzed FBS | Biotin-depleted serum | Essential for reducing background biotinylation; 3.5 kDa MWCO [35] [36] |
| Streptavidin Beads | Capture biotinylated substrates | Use high-capacity, low-non-specific binding beads for optimal results [35] |
| Deubiquitinase Inhibitors | Preserve ubiquitination signatures | Include in lysis buffer to prevent deubiquitination during processing [36] |
| Proteasome Inhibitors | Stabilize degraded substrates | Bortezomib or MG132 for detecting rapidly turned-over substrates [36] |
Implications for Tumor Research and Therapeutic Development
The BioE3 methodology offers significant potential for advancing cancer research by enabling comprehensive mapping of E3 ligase substrates in tumor contexts. Molecular subtyping of cancers based on E3 ligase expression patterns has already demonstrated prognostic value in bladder cancer, highlighting the clinical relevance of understanding E3-specific ubiquitination networks [39]. By applying BioE3 to tumor samples or cancer cell lines, researchers can identify disease-specific substrates of oncogenic E3 ligases or tumor suppressors, revealing novel therapeutic targets and biomarkers.
In the field of targeted protein degradation, BioE3 provides a powerful tool for characterizing the mechanisms of molecular glues and PROTACs [36]. The ability to identify both endogenous substrates and drug-induced neosubstrates for E3 ligases like CRBN enables comprehensive evaluation of on-target efficacy and potential off-target effects during drug development [36]. This application is particularly valuable for understanding resistance mechanisms and designing next-generation degraders with improved specificity profiles.
Furthermore, BioE3 can detect altered E3 specificity in response to chemical treatments or cellular stressors, opening new avenues for understanding how ubiquitination networks are rewired in tumor cells in response to therapeutic pressure [35]. This capability makes BioE3 an invaluable resource for deciphering the complex role of ubiquitination in cancer progression and treatment response.
BioE3 Applications in Cancer Research: This diagram illustrates how BioE3 substrate identification feeds into various aspects of cancer research and therapeutic development.
Mass Spectrometry and diGly Remnant Profiling for Ubiquitination Site Mapping
Protein ubiquitination is a crucial post-translational modification that regulates diverse cellular functions, including protein degradation, activity, and localization [2]. The ubiquitination process involves a sequential cascade of E1 (activating), E2 (conjugating), and E3 (ligating) enzymes that covalently attach ubiquitin to target proteins [40] [41]. When trypsin digests ubiquitinated proteins, it cleaves the ubiquitin molecule, leaving a characteristic diglycine (diGly) remnant attached to the modified lysine residue of the substrate peptide [4]. This diGly signature produces a predictable mass shift of 114.04 Da, enabling mass spectrometry (MS) to identify and precisely localize ubiquitination sites [2] [4]. The development of antibodies specifically recognizing the K-ε-GG motif has revolutionized ubiquitination site mapping, particularly for clinical tumor samples where genetic manipulation is infeasible [2] [4].
In cancer research, profiling ubiquitination substrates provides critical insights into tumorigenesis mechanisms. Lung adenocarcinoma studies have revealed distinctive ubiquitinated peptide motifs completely different from those in lung squamous cell carcinoma, highlighting tumor-specific ubiquitination patterns [5]. Similarly, pituitary adenoma research has identified ubiquitination involvement in key signaling pathways like PI3K-AKT and hippo signaling [4]. This Application Note details methodologies for comprehensive ubiquitination site mapping in tumor samples using diGly remnant profiling with mass spectrometry.
Key Methodologies and Workflows
Sample Preparation and diGly Peptide Enrichment
Proper sample preparation is fundamental for successful ubiquitination site mapping. For tumor tissue analysis, the protocol begins with efficient protein extraction and digestion. Fresh-frozen tissues should be thoroughly ground into powder in a mortar precooled with liquid nitrogen, followed by addition of lysis buffer (e.g., 1% Triton X-100, 1% protease inhibitor, 50 µM PR-619) and sonication [5]. After centrifugation, protein concentration in the supernatant should be determined using a bicinchoninic acid (BCA) assay [5].
For enzymatic digestion, the filter-aided sample preparation (FASP) method or in-solution digestion can be employed. Trypsin is recommended as the primary protease due to its specific cleavage properties that generate the diGly remnant signature. A key consideration is the use of resin-bound, thermally stabilized proteases (e.g., SMART Digest trypsin), which can digest native proteins at elevated temperatures (70°C) without requiring reduction and alkylation steps, thereby simplifying workflow and improving digestion efficiency [42]. Following digestion, desalting using C18 ZipTips or StageTips is essential before diGly enrichment.
For diGly peptide enrichment, the anti-K-ε-GG antibody-based method is most widely used. The optimized protocol involves resuspending peptides in immunoaffinity purification (IAP) buffer (100 mM NaCl, 1 mM EDTA, 50 mM Tris-HCl, 0.5% NP-40; pH 8.0) and incubating with anti-K-ε-GG antibody-conjugated beads overnight at 4°C with gentle shaking [5]. After incubation, extensive washing with IAP buffer followed by deionized water removes non-specifically bound peptides. Finally, bound diGly peptides are eluted using 0.1% trifluoroacetic acid, vacuum-dried, and desalted before LC-MS/MS analysis [5]. For tumor tissue samples where ubiquitination stoichiometry is typically low, starting with 1-2 mg of peptide material and using approximately 31.25 µg of anti-diGly antibody provides optimal enrichment efficiency [43].
Mass Spectrometry Analysis: DDA versus DIA Approaches
Two primary MS acquisition methods are employed in diGly proteomics: data-dependent acquisition (DDA) and data-independent acquisition (DIA). Each approach offers distinct advantages for ubiquitination site mapping in tumor samples.
Data-Dependent Acquisition (DDA) operates through cyclic acquisition of full MS scans followed by fragmentation of the most intense precursors. This method has been widely used in ubiquitinome studies, typically identifying approximately 20,000 diGly peptides in single measurements of proteasome inhibitor-treated cells [43]. While DDA is well-established and computationally straightforward, it suffers from stochastic precursor selection and limited reproducibility across samples, with only about 15% of diGly peptides showing coefficients of variation (CVs) below 20% [43].
Data-Independent Acquisition (DIA) fragments all co-eluting peptide ions within predefined mass-to-charge (m/z) windows simultaneously, providing greater data completeness, quantitative accuracy, and sensitivity [43]. For diGly proteome analysis, DIA methods require optimization to account for the unique characteristics of diGly peptides, which often exhibit higher charge states due to impeded C-terminal cleavage of modified lysine residues [43]. An optimized DIA method with 46 precursor isolation windows and high MS2 resolution (30,000) significantly improves diGly peptide identification, enabling detection of approximately 35,000 distinct diGly sites in single measurements—nearly double the identification rate of DDA [43]. Additionally, DIA demonstrates superior quantitative reproducibility, with 45% of diGly peptides showing CVs below 20% across replicates [43].
Table 1: Comparison of DDA and DIA Methods for diGly Proteome Analysis
| Parameter | DDA Approach | DIA Approach |
|---|---|---|
| Identification Depth | ~20,000 diGly peptides in single measurements | ~35,000 diGly peptides in single measurements |
| Quantitative Reproducibility | 15% of peptides with CV <20% | 45% of peptides with CV <20% |
| Spectral Libraries | Not required | Essential (can contain >90,000 diGly peptides) |
| Precursor Selection | Intensity-based, stochastic | Systematic, all ions within m/z windows |
| Best Application | Targeted analysis, verification | Comprehensive profiling, biomarker discovery |
For tumor ubiquitinome studies requiring comprehensive coverage, DIA is strongly recommended despite its dependency on spectral libraries. Extensive libraries can be generated from cell lines (e.g., HEK293, U2OS) treated with proteasome inhibitors (10 µM MG132, 4 hours), fractionated by basic reversed-phase chromatography, and concatenated into 8-10 fractions to reduce sample complexity [43]. To address the issue of highly abundant K48-linked ubiquitin-chain derived diGly peptides competing for antibody binding sites, fractions containing these peptides should be processed separately [43].
Data Processing and Bioinformatic Analysis
Following MS data acquisition, specialized computational tools are required for diGly data processing. For DIA data, software like Spectronaut, DIA-NN, or Skyline enables extraction of fragment ion chromatograms using spectral libraries [43]. MaxQuant (version 1.6.6.0 or later) is widely used for both DDA and direct DIA analysis, with the following key parameters: Trypsin/P as cleavage enzyme, up to four missing cleavages, minimum peptide length of seven amino acids, and fixed modification of GlyGly (K) with a mass shift of 114.04 Da [5]. The false discovery rate (FDR) should be set to 1% for both protein and peptide-spectrum match identification [5].
For biological interpretation, ubiquitinated proteins should be analyzed using Gene Ontology (GO) and Kyoto Encyclopedia of Genes and Genomes (KEGG) pathway analyses to identify enriched biological processes and signaling pathways [4]. In tumor research, special attention should be paid to pathways commonly dysregulated in cancer, such as PI3K-AKT signaling, hippo signaling, and nucleotide excision repair [4]. Motif analysis around ubiquitination sites can reveal sequence preferences and help identify potential recognition motifs for E3 ligases [5].
Applications in Tumor Research
Ubiquitination Profiling in Human Tumors
diGly remnant profiling has been successfully applied to characterize ubiquitination landscapes in various human cancers. In lung adenocarcinoma (LUAD), ubiquitinome analysis combined with proteomic and transcriptomic data has identified characteristic ubiquitination motifs distinct from other lung cancer subtypes [5]. This approach revealed two gene expression patterns of ubiquitinated proteins with differential survival outcomes, potentially correlated with the tumor immune infiltrating microenvironment [5]. The prognostic model derived from ubiquitination patterns could guide clinical treatment decisions and drug sensitivity predictions [5].
In pituitary adenomas, quantitative ubiquitinome analysis has identified 158 ubiquitination sites on 108 proteins, with five distinct ubiquitination motifs [4]. Notably, 14-3-3 zeta/delta protein showed significantly decreased ubiquitination levels in nonfunctional pituitary adenomas compared to control pituitaries, suggesting that upregulated 14-3-3 zeta/delta protein in tumors might derive from reduced ubiquitination-mediated degradation [4]. This finding illustrates how ubiquitination profiling can reveal novel molecular mechanisms in tumorigenesis.
Table 2: Key Ubiquitination Findings in Human Tumor Studies
| Tumor Type | Key Ubiquitination Findings | Potential Clinical Relevance |
|---|---|---|
| Lung Adenocarcinoma | Distinct ubiquitinated peptide motifs different from squamous cell carcinoma; two expression patterns with survival differences | Prognostic stratification; guidance for targeted therapies |
| Pituitary Adenomas | 158 ubiquitination sites on 108 proteins; decreased ubiquitination of 14-3-3 zeta/delta | Insights into pituitary tumorigenesis; potential biomarkers |
| Pancreatic Cancer | SHOC2 ubiquitination by FBWB7 regulates mTORC1 and autophagy | Potential therapeutic target for PDAC |
| Hepatocellular Carcinoma | DDX5 reduces p62/TRAF6-mediated ubiquitination of mTOR, inhibiting signaling | Mechanism for impaired HCC cell growth |
Signaling Pathway Analysis in Cancer
Ubiquitination regulates numerous oncogenic signaling pathways through modification of key regulatory proteins. The mTOR pathway, a central regulator of cell growth and metabolism, is frequently modulated by ubiquitination in cancer [41]. In breast cancer, ribosomal protein S27-like (RPS27L) may reduce β-TrCP levels, leading to DEPTOR accumulation and mTORC1 inactivation, thereby activating autophagy [41]. In pancreatic ductal adenocarcinoma (PDAC), SHOC2 is ubiquitinated and degraded by FBWB7 E3 ligase, which blocks the RAS-MAPK pathway and inactivates mTORC1, consequently inducing autophagy [41].
The ULK1 complex, crucial for autophagy initiation, is also regulated by ubiquitination. Multiple E3 ligases, including NEDD4L, MUL1, and KLHL20, facilitate ULK1 ubiquitination and degradation, while others like TRIM16 and TRAF6 promote K63-linked ubiquitination that stabilizes and activates ULK1 [41]. In chronic myeloid leukemia (CML), grancalcin-mediated K63-linked ubiquitination of ULK1 by TRAF6 induces autophagy, contributing to imatinib resistance [41]. These findings highlight the potential of targeting ubiquitination pathways for cancer therapy.
Diagram Title: Ubiquitination and diGly Workflow
The Scientist's Toolkit: Essential Research Reagents
Table 3: Essential Research Reagents for diGly Remnant Profiling
| Reagent/Category | Specific Examples | Function and Application Notes |
|---|---|---|
| Anti-diGly Antibodies | PTMScan Ubiquitin Remnant Motif Kit (CST) | Immunoaffinity enrichment of K-ε-GG-containing peptides; essential for low-stoichiometry ubiquitination sites |
| Proteases | SMART Digest trypsin (Thermo Fisher) | Resin-bound, thermally stabilized trypsin for efficient digestion at 70°C without reduction/alkylation |
| Proteasome Inhibitors | MG132 (10 µM, 4h treatment) | Enhances detection of K48-linked ubiquitination by blocking proteasomal degradation |
| Chromatography Columns | Waters UPLC Glycan BEH Amide column (HILIC) | Separation of hydrophilic glycopeptides and diGly peptides |
| MS Instruments | timsTOF Pro, Orbitrap-based instruments | High-sensitivity detection; DIA capabilities for comprehensive ubiquitinome coverage |
| Database Search Software | MaxQuant, Spectronaut, DIA-NN | Identification and quantification of diGly peptides with FDR control |
Mass spectrometry-based diGly remnant profiling provides a powerful platform for comprehensive ubiquitination site mapping in tumor samples. The optimized workflows described in this Application Note, particularly the DIA approach with its enhanced sensitivity and reproducibility, enable researchers to obtain unprecedented depth in ubiquitinome coverage. When applied to tumor research, these methodologies reveal tumor-specific ubiquitination patterns, dysregulated signaling pathways, and potential therapeutic targets. As the field advances, integration of ubiquitinome data with other omics datasets will further elucidate the complex role of ubiquitination in cancer biology and treatment response.
Appendix: Experimental Protocols
Detailed Protocol: diGly Peptide Enrichment from Tumor Tissues
Materials:
- Fresh-frozen tumor tissues (50-100 mg)
- Lysis buffer: 1% Triton X-100, 1% protease inhibitor cocktail, 50 µM PR-619
- BCA protein assay kit
- SMART Digest trypsin kit (Thermo Fisher)
- Anti-K-ε-GG antibody beads (PTMScan Ubiquitin Remnant Motif Kit, CST)
- IAP buffer: 100 mM NaCl, 1 mM EDTA, 50 mM Tris-HCl, 0.5% NP-40; pH 8.0
- C18 ZipTips (Millipore)
- Trifluoroacetic acid (TFA)
Procedure:
- Tissue Homogenization: Grind frozen tissues to powder in liquid nitrogen-cooled mortar. Transfer to pre-cooled tubes.
- Protein Extraction: Add 4 volumes of lysis buffer per tissue weight. Sonicate on ice (3 × 10 s pulses, 20 s intervals). Centrifuge at 12,000 g for 10 min at 4°C. Collect supernatant.
- Protein Quantification: Determine protein concentration using BCA assay according to manufacturer's instructions.
- Protein Digestion: For 1 mg protein, add SMART Digest trypsin (60 μg) and incubate at 70°C for 3 h with shaking at 1400 rpm.
- Peptide Cleanup: Desalt peptides using C18 ZipTips according to manufacturer's instructions.
- diGly Enrichment: Resuspend peptides in IAP buffer. Incubate with anti-K-ε-GG antibody beads overnight at 4°C with gentle shaking.
- Washing: Wash beads 4× with IAP buffer and 2× with deionized water.
- Elution: Elute diGly peptides with 0.1% TFA (3× elutions). Combine eluates and vacuum-dry.
- Desalting: Desalt enriched diGly peptides using C18 StageTips before LC-MS/MS analysis.
Detailed Protocol: DIA Method for diGly Proteome Analysis
LC Parameters:
- Column: Waters UPLC Glycan BEH Amide (150 × 2.1 mm, 1.7 μm)
- Mobile phase A: 0.1% formic acid in water
- Mobile phase B: 0.1% formic acid in acetonitrile
- Gradient: 3-25% B over 120 min, 25-45% B over 30 min, 45-90% B over 5 min
- Flow rate: 0.3 μL/min
- Injection volume: 25% of enriched diGly peptides (from 1 mg starting material)
MS Parameters (timsTOF Pro):
- MS1 scan range: 100-1700 m/z
- DIA windows: 46 windows of variable width (optimized for diGly peptide distribution)
- MS2 resolution: 30,000
- Collision energy: Stepped 25-35 eV
- Ion mobility separation: Enabled
Data Processing:
- Generate spectral library from DDA analysis of fractionated samples
- Process DIA data using Spectronaut (v15+) with following parameters:
- Protein FDR: 1%
- Peptide FDR: 1%
- Match between runs: Enabled
- Cross-run normalization: Enabled
- For direct DIA analysis without library, use DIA-NN with deep learning-based spectra prediction
Diagram Title: Tumor Ubiquitination Analysis Workflow
Within the framework of ubiquitination substrate discovery in cancer research, selecting the appropriate analytical scale for tumor samples is a critical determinant of success. Tumor tissues are inherently complex ecosystems composed of malignant cells, diverse immune populations, stromal components, and extracellular matrix, all interacting within a spatially organized architecture. The choice between bulk tissue analysis, single-cell resolution, and spatially resolved methods significantly influences the ability to identify genuine ubiquitination substrates, as the molecular signatures of these events can be confined to specific cellular subpopulations or microenvironments. This document provides a structured overview of these methodological approaches, their applications, and integration strategies, with particular emphasis on their utility for ubiquitination substrate identification in tumor samples.
Bulk Tissue Analysis
Bulk whole-genome sequencing (WGS) and transcriptomics provide a population-averaged molecular profile of tumor samples, remaining a cornerstone for comprehensive genomic characterization and ploidy estimation. Benchmarking studies have identified specific tools that excel under defined conditions; for instance, PURPLE demonstrates superior performance in estimating tumor purity and ploidy when tumor purity exceeds 30%, regardless of sequencing coverage or platform [44]. However, a significant limitation of bulk approaches is their dilution effect: signals from rare cell populations or spatially restricted cellular events—such as specific ubiquitination events occurring in a distinct tumor subclone—are often obscured by the dominant population [45] [46].
Table 1: Performance Characteristics of Bulk WGS Ploidy Estimation Tools
| Tool Name | Optimal Purity Range | Strengths | Limitations |
|---|---|---|---|
| PURPLE | >30% purity [44] | Robust across sequencing platforms and coverages [44] | Performance declines with low purity samples [44] |
| Multiple Tools | Not Specified | Comprehensive genomic landscape | Poor performance on euploid samples and long-read sequencing data [44] |
Single-Cell Resolution Approaches
Single-cell RNA sequencing (scRNA-seq) resolves cellular heterogeneity by capturing transcriptomic profiles of individual cells, enabling the identification of rare cell types, transitional states, and distinct cellular subpopulations within tumors [46]. This resolution is critical for ubiquitination research, as it allows researchers to associate specific ubiquitination signatures with particular cell states. For example, scRNA-seq analysis of primary and metastatic ER+ breast cancer revealed significant transcriptional dynamics and increased genomic instability (measured by CNV scores) within malignant cells from metastatic sites, highlighting cellular states that may be driven by distinct post-translational modifications [47].
Experimentally, scRNA-seq workflows involve generating single-cell suspensions from dissociated tumor tissues, capturing individual cells, and preparing sequencing libraries. A standardized protocol is crucial to minimize technical variability. Key steps include:
- Viable Single-Cell Suspension Preparation: Gentle tissue dissociation to preserve cell integrity [47].
- Cell Partitioning and Barcoding: Using microfluidic devices or droplet-based systems (e.g., 10X Genomics) [47].
- cDNA Synthesis and Library Prep: Amplification and tagmentation for next-generation sequencing [47].
- Bioinformatic Processing: Quality control (mitochondrial content, UMI thresholds, doublet removal), normalization, clustering, and differential expression analysis using tools like Seurat or SCANPY [47].
A significant advancement for ubiquitination research is the integration of copy number variation (CNV) analysis from scRNA-seq data using tools like InferCNV and CaSpER, which help distinguish malignant from non-malignant cells and infer intratumoral heterogeneity [47]. Furthermore, SeCNV has been identified as a top-performing method for ploidy detection from single-cell WGS data, providing accurate genomic characterization at single-cell resolution [44].
Spatially Resolved Transcriptomics
Spatial transcriptomics (ST) preserves the architectural context of tissue samples by mapping gene expression patterns to their original histological locations [45] [46]. This technology bridges the gap between single-cell heterogeneity and tissue morphology, allowing researchers to visualize how cellular processes, including potential ubiquitination events, are organized within tumor microenvironments.
ST methodologies are broadly categorized into:
- Image-Based Approaches: Utilize fluorescently labeled probes for in situ hybridization (e.g., MERFISH, seqFISH) to directly detect RNA transcripts within intact tissues [46].
- Barcode-Based Approaches: Employ spatially encoded oligonucleotide barcodes on slides to capture and sequence RNA from tissue sections (e.g., 10X Genomics Visium) [46].
Table 2: Comparative Analysis of scRNA-seq and Spatial Transcriptomics
| Feature | scRNA-seq | Spatial Transcriptomics |
|---|---|---|
| Resolution | True single-cell [46] | Multi-cell to near-single-cell (resolution improving) [46] |
| Spatial Context | Lost during tissue dissociation [46] | Preserved in intact tissue architecture [46] |
| Key Strength | Identification of rare cell populations and detailed cell typing [46] | Mapping cellular interactions and tumor microenvironment niches [46] |
| Throughput | High (thousands to millions of cells) [46] | Varies by platform (entire tissue sections) [46] |
| Data Integration | Required to infer spatial relationships | Can be integrated with scRNA-seq for cell type deconvolution [46] |
Innovative deep learning approaches like MISO (Multiscale Integration of Spatial Omics) further enhance the utility of spatial data by predicting spatial transcriptomics from routinely available H&E-stained histological slides, making spatial molecular profiling more accessible [48].
Integration with Ubiquitination Substrate Identification
The identification of ubiquitination substrates in tumor tissues presents particular challenges due to the dynamic, transient, and often subcellularly localized nature of ubiquitination events. Traditional methods struggle to distinguish genuine substrates from mere interactors, particularly in complex tissue contexts.
The BioE3 method addresses this challenge by combining proximity-dependent biotinylation with ubiquitin tagging to identify bona fide substrates of specific E3 ligases [35]. This approach utilizes:
- BirA-E3 Ligase Fusions: E3 ligases fused to biotin ligase (BirA) [35].
- bioUb (Biotinylatable Ubiquitin): An AviTag-modified ubiquitin (bioGEFUb with mutations for reduced BirA affinity to minimize non-specific labeling) that can be biotinylated when in proximity to the BirA-E3 fusion [35].
- Streptavidin Capture and LC-MS/MS: Isolation and identification of biotinylated ubiquitinated substrates [35].
The BioE3 workflow can be adapted for different E3 ligase types (RING, HECT) and has been successfully applied to both characterized (RNF4, MIB1) and less-characterized E3 ligases (RNF214), identifying novel substrates linked to specific cellular processes [35].
Diagram 1: BioE3 Workflow for Identifying E3 Ubiquitin Ligase Substrates. This diagram illustrates the key steps in the BioE3 method for identifying genuine ubiquitination substrates in cellular contexts, utilizing proximity-dependent biotinylation followed by affinity purification and mass spectrometry.
When planning ubiquitination studies in tumor samples, consider these critical experimental design aspects:
- Cellular Specificity: Ubiquitination events may be restricted to specific tumor subclones or microenvironmental niches (e.g., immune cells versus malignant cells) [47] [49].
- Temporal Dynamics: Ubiquitination is highly dynamic; careful timing of sample collection and biotin labeling (in BioE3) is essential to capture transient events [35].
- Spatial Organization: The spatial distribution of E3 ligases and their substrates within tumor architecture can influence functional outcomes [45].
Integrated Multiomics and Future Directions
The integration of bulk, single-cell, and spatial methodologies represents the future of comprehensive tumor analysis, particularly for complex processes like ubiquitination. Multiomics approaches simultaneously measure multiple analytical layers (genomics, transcriptomics, proteomics) from the same samples, providing a more complete understanding of biological systems [50].
Key integration strategies include:
- Computational Data Harmonization: Leveraging machine learning and artificial intelligence to unify disparate datasets and detect patterns across molecular layers [50].
- Network Integration: Mapping multiple omics datasets onto shared biochemical networks to improve mechanistic understanding of ubiquitination pathways [50].
- Clinical Correlation: Integrating molecular data with clinical outcomes to identify ubiquitination-related biomarkers with prognostic or therapeutic significance [50].
Emerging technologies like single-cell multiomics (simultaneous measurement of transcriptomics and proteomics from the same cells) and higher-resolution spatial platforms will further enhance our ability to contextualize ubiquitination events within the complex architecture of tumor tissues [50].
Research Reagent Solutions
Table 3: Essential Research Reagents for Tumor Ubiquitination Studies
| Reagent / Tool | Function / Application | Key Features |
|---|---|---|
| BioE3 System [35] | Identification of E3 ligase substrates in specific cellular contexts | Uses BirA-E3 fusions and bioGEFUb for proximity-dependent biotinylation; works with RING and HECT E3s |
| bioGEFUb [35] | Biotinylatable ubiquitin for BioE3 experiments | Contains AviTag mutations (GEF) for reduced BirA affinity, minimizing non-specific labeling |
| InferCNV [47] | CNV inference from scRNA-seq data | Distinguishes malignant from non-malignant cells in tumor samples using T cells as reference |
| SCEVA N [47] | Identification of tumor subpopulations with different CNVs | Analyzes intratumoral heterogeneity from single-cell data |
| SCVI/SCANVI [47] | Single-cell data integration | Biology-aware integration tools that account for batch effects and sample-specific variation |
| MISO [48] | Spatial transcriptomics prediction from H&E images | Deep learning approach for multiscale integration of spatial omics with tumor morphology |
| CellHint [47] | Cell-type annotation | Leverages known cell type labels to improve annotation accuracy and resolution |
Navigating Analytical Challenges: Specificity, Sensitivity, and Artifacts in Complex Tumor Samples
Protein ubiquitination is a crucial post-translational modification that regulates diverse cellular processes, including protein degradation, signal transduction, and subcellular localization [5] [51]. In the context of tumor samples, characterizing the ubiquitylome provides invaluable insights into cancer mechanisms and potential therapeutic targets [5]. However, identifying genuine ubiquitination substrates in clinical materials presents significant challenges due to the low stoichiometry of modified proteins, their rapid degradation by the proteasome, and the dynamic activity of deubiquitinating enzymes (DUBs) [52] [51]. These factors are particularly problematic in clinical specimens, where sample amounts are often limited and genetic manipulation is not feasible.
This Application Note outlines robust enrichment strategies and detailed protocols designed to overcome these hurdles, enabling reliable identification of ubiquitination events in clinical tumor samples. These methodologies are framed within broader research aimed at discovering novel ubiquitination substrates and patterns that drive tumorigenesis in cancers like lung adenocarcinoma (LUAD) [5].
Key Enrichment Methodologies: Principles and Comparisons
Several core strategies have been developed to enrich for ubiquitinated proteins from complex lysates. The table below summarizes the primary methodologies, their underlying principles, advantages, and limitations, particularly in the context of working with clinical material.
Table 1: Comparison of Key Enrichment Strategies for Ubiquitinated Proteins
| Methodology | Principle | Key Advantage | Primary Limitation |
|---|---|---|---|
| diGly Antibody Enrichment [5] [52] [51] | Antibody recognizes K-ε-GG remnant left on peptides after tryptic digest. | Applicable to any sample, including clinical tissues; no genetic manipulation needed. | Cannot distinguish ubiquitin chain linkage; background from abundant proteins. |
| TUBE-Based Enrichment [52] [51] | Tandem Ubiquitin-Binding Entities (TUBEs) bind polyubiquitin chains with high affinity. | Protects ubiquitinated substrates from DUBs and proteasomal degradation in vivo. | Requires recombinant protein tools; less effective for monoubiquitination. |
| BioE3 System [35] | BirA-E3 fusion biotinylates AviTag-Ub incorporated by a specific E3 ligase onto its substrates. | Identifies bona fide substrates of a specific E3 ligase with high confidence. | Requires generation of specialized stable cell lines; not for direct use on patient tissue. |
| Affinity Tagged Ubiquitin [51] | Ectopic expression of His-, FLAG-, or Strep-tagged Ub for purification. | High-yield enrichment; good for cell culture studies. | Not suitable for most clinical samples; may disrupt native Ub biology. |
The choice of enrichment strategy depends heavily on the research question and sample type. For direct analysis of clinical tumor tissues, the diGly antibody-based approach is the most directly applicable and widely used method [5].
Experimental Protocols for Clinical Tumor Samples
Protocol: Ubiquitinated Peptide Enrichment from LUAD Tissue Using Anti-K-ε-GG Antibody
This protocol is adapted from a study that successfully profiled the ubiquitylome of human lung adenocarcinoma (LUAD) tissues, providing a template for working with clinical material [5].
Materials and Reagents
- Clinical Tissue Samples: Fresh-frozen LUAD and paired adjacent normal tissues, preserved in liquid nitrogen [5].
- Lysis Buffer: 1% Triton X-100, 1% protease inhibitor cocktail, 50 µM PR-619 (a broad-spectrum DUB inhibitor) [5].
- BCA Assay Kit: For determining protein concentration.
- Trypsin: Sequencing grade.
- Anti-K-ε-GG Antibody: Cross-linked to agarose beads (commercially available, e.g., PTM-1104) [5].
- C18 ZipTips: For desalting peptides prior to LC-MS/MS.
- Trifluoroacetic Acid (TFA), Acetonitrile, and other standard MS-grade solvents.
Step-by-Step Procedure
Protein Extraction and Digestion
- Thoroughly grind ~20-50 mg of frozen tissue in a liquid nitrogen-cooled mortar.
- Add 4 volumes of lysis buffer and lyse the tissue powder via sonication on ice.
- Centrifuge the lysate at 12,000 g for 10 minutes at 4°C and collect the supernatant.
- Determine protein concentration using a BCA assay. Use an equal protein mass (e.g., 1-5 mg) from each sample for digestion.
- Precipitate proteins using trichloroacetic acid (20% final concentration), wash the pellet with cold acetone, and dry.
- Resuspend the pellet and digest with trypsin (1:50 enzyme-to-protein ratio) overnight at 37°C [5].
Enrichment of Ubiquitinated Peptides
- Dissolve the resulting tryptic peptides in IP buffer (100 mM NaCl, 1 mM EDTA, 50 mM Tris-HCl, 0.5% NP-40; pH 8.0).
- Incubate the peptide solution with pre-washed anti-K-ε-GG antibody resin on a rotating shaker overnight at 4°C.
- Wash the resin four times with IP buffer and twice with deionized water to remove non-specifically bound peptides.
- Elute the bound ubiquitinated peptides with 0.1% TFA. Collect the eluent and vacuum dry.
- Desalt the peptides using C18 ZipTips according to the manufacturer's instructions [5].
Liquid Chromatography-Mass Spectrometry (LC-MS/MS) Analysis
- Dissolve the purified peptides in 0.1% formic acid for LC-MS/MS analysis.
- Separate peptides using a nanoElute UHPLC system coupled to a timsTOF Pro mass spectrometer (or similar high-sensitivity instrument).
- Operate the mass spectrometer in data-dependent acquisition (DDA) mode.
- Search the resulting MS/MS data against the appropriate protein database (e.g., UniProt Homo sapiens) using software such as MaxQuant (v.1.6.6.0).
- Set the variable modification to GlyGly (K) and a false discovery rate (FDR) of 1% for both protein and peptide-spectrum matches [5].
Protocol: Stabilizing Ubiquitination In Vivo Using TR-TUBE for Cell-Based Assays
While not directly for clinical tissue, this protocol is valuable for validating findings in cell models and requires co-expression of TR-TUBE with an E3 ligase of interest to stabilize ubiquitinated substrates by masking ubiquitin chains from DUBs and the proteasome [52].
Materials and Reagents
- Plasmids: pCMV-FLAG-TR-TUBE and plasmid for E3 ligase of interest (e.g., Skp2, FBXO21) [52].
- Cell Line: 293T or other relevant cancer cell line.
- Transfection Reagent: (e.g., polyethylenimine, PEI).
- Lysis Buffer: As in Protocol 2.1, but without PR-619, as TR-TUBE provides protection.
- Anti-FLAG M2 Affinity Gel: For immunoprecipitation.
Step-by-Step Procedure
Cell Transfection and Lysate Preparation
- Co-transfect 293T cells with FLAG-TR-TUBE and your E3 ligase plasmid.
- Harvest cells 24-48 hours post-transfection. Note that prolonged TR-TUBE expression (>48h) can lead to accumulation of ubiquitin conjugates and some cytotoxicity [52].
- Lyse cells in appropriate buffer without DUB inhibitors.
Immunoprecipitation and Detection
- Incubate cell lysates with anti-FLAG M2 affinity gel for 2-4 hours at 4°C.
- Wash the beads extensively with lysis buffer.
- Elute bound proteins with FLAG peptide or 2X Laemmli buffer.
- Analyze the immunoprecipitates by SDS-PAGE and western blotting using antibodies against the putative substrate and ubiquitin to detect stabilized, ubiquitinated species [52].
The Scientist's Toolkit: Key Research Reagent Solutions
Successful ubiquitination research relies on specific, high-quality reagents. The following table details essential materials and their functions.
Table 2: Essential Research Reagents for Ubiquitination Enrichment Studies
| Research Reagent | Function / Application | Example / Catalog Number |
|---|---|---|
| Anti-K-ε-GG Antibody | Enrichment of ubiquitinated peptides from trypsin-digested samples for MS; the primary tool for clinical tissue ubiquitylomics. | PTM-1104 (Jingjie Biotechnology) [5] |
| PR-619 | Broad-spectrum deubiquitinase (DUB) inhibitor; used in lysis buffer to preserve ubiquitin conjugates during protein extraction. | S7412 (Selleckchem) [5] |
| Tandem Ubiquitin Binding Entity (TUBE) | Recombinant protein to affinity-purity polyubiquitinated proteins; protects ubiquitin chains from DUBs and proteasomal degradation. | Trypsin-resistant (TR)-TUBE [52] |
| Linkage-Specific Ub Antibodies | Immunoblot detection or enrichment of ubiquitin chains with specific linkages (e.g., K48, K63). | Commercially available from various suppliers [51] |
| Strep-Tactin Resin | Affinity purification of Strep-tagged ubiquitin and its conjugated substrates from engineered cell lines. | Commercial resin [51] |
Workflow and Data Analysis Visualization
Diagram 1: Ubiquitinome analysis workflow for clinical tissue.
The strategies and detailed protocols outlined here provide a robust framework for investigating the ubiquitinome in clinically relevant tumor samples. The anti-K-ε-GG antibody-based method stands out for its direct applicability to frozen tissue, enabling the discovery of ubiquitination signatures associated with cancer, as demonstrated in LUAD [5]. For functional validation and deconvolution of specific E3 ligase pathways, cell-based systems like TR-TUBE [52] and BioE3 [35] are powerful complementary tools. By carefully selecting and applying these methodologies, researchers can overcome the challenge of low stoichiometry and uncover critical ubiquitination events that drive tumor biology, paving the way for novel diagnostic and therapeutic strategies.
In the pursuit of novel therapeutic targets for cancer, the identification of substrates for E3 ubiquitin ligases has emerged as a critical frontier. Ubiquitination, a pivotal post-translational modification, regulates essential cellular processes such as protein degradation, localization, and activation, with its dysregulation being a hallmark of numerous cancers [37]. However, a significant challenge persists: discriminating true ubiquitination substrates of a specific E3 ligase from mere interactors that do not undergo modification. This distinction is vital for understanding tumorigenesis and developing targeted therapies. This Application Note details refined protocols and strategic frameworks to achieve this specificity, with a focus on applications in tumor sample research.
The Core Challenge: Specificity in E3-Substrate Identification
E3 ubiquitin ligases confer specificity to the ubiquitination cascade by recognizing and binding to their target proteins. The conventional method of co-immunoprecipitation coupled with mass spectrometry often identifies a plethora of E3-binding partners. Nevertheless, this approach cannot differentiate between bona fide substrates destined for ubiquitination, non-substrate interactors involved in regulatory complexes or transient interactions, and proteins that bind after cell lysis [53] [35]. This high rate of false positives confounds the validation of true physiological relationships, particularly in the complex molecular environment of tumor tissues.
Strategic Solution: Proximity-Dependent Labeling with BioE3
A powerful solution to this challenge is the BioE3 system, an innovative proximity-dependent labeling strategy that specifically biotinylates ubiquitin moieties as they are conjugated to substrates by a given E3 ligase [53] [35].
Principle of the BioE3 Method
The BioE3 method employs two key components:
- A BirA-E3 ligase fusion protein, which localizes the biotin ligase BirA to the active site of the E3 of interest.
- An engineered, biotin-accepting ubiquitin (bioGEFUb), which is incorporated into cellular substrates via the endogenous ubiquitination machinery.
When the BirA-E3 ligase catalyzes the transfer of bioGEFUb onto a specific substrate, the BirA domain biotinylates the bioGEFUb in close proximity. This allows for the highly specific streptavidin-based purification and subsequent proteomic identification (LC-MS) of only those proteins that were directly ubiquitinated by the E3 ligase [53].
Key Optimization for Specificity: The bioGEF Tag
A critical advancement in the BioE3 protocol is the use of a mutated AviTag sequence known as bioGEF. The widely used wild-type AviTag (bioWHE) has a high affinity for BirA, leading to widespread, non-specific biotinylation throughout the cell, independent of the E3's activity. In contrast, the bioGEF tag has a lower affinity for BirA, which confines biotinylation events to the immediate vicinity of the BirA-E3 fusion, thereby dramatically reducing background noise and enabling the specific labeling of genuine substrates [53] [35]. The following workflow diagram illustrates the optimized BioE3 process.
Quantitative Data from BioE3 Applications
The BioE3 system has been successfully validated with multiple E3 ligases, identifying both known and novel substrates, as summarized below.
Table 1: Exemplary E3 Ligases and Substrates Identified Using BioE3
| E3 Ligase | E3 Type | Known Biological Role | Validated Substrates Identified by BioE3 |
|---|---|---|---|
| RNF4 [53] | RING | DNA Damage Response, PML Bodies | Known and novel targets related to its nuclear functions. |
| MIB1 [53] [35] | RING | Endocytosis, Autophagy, Centrosome Dynamics | Validated known roles and identified new targets. |
| NEDD4 [53] [35] | HECT | Vesicular Trafficking, Cell Signaling | Known and novel substrates linked to trafficking pathways. |
| MARCH5 [53] | RING (Mitochondrial) | Mitochondrial Dynamics | Novel targets providing insight into its organelle-specific function. |
| RNF214 [53] [35] | RING (Poorly Characterized) | Largely Unknown | Novel targets suggesting roles in cytoplasmic regulation. |
The Scientist's Toolkit: Essential Reagents for BioE3
Implementing the BioE3 protocol requires a suite of specialized molecular reagents and tools.
Table 2: Key Research Reagent Solutions for the BioE3 Protocol
| Reagent / Tool | Function / Description | Critical Notes |
|---|---|---|
| pCDNA3.1+ Vector [54] | Mammalian expression vector for cloning BirA-E3 fusions and bioGEFUb. | Ensures high-level exogenous protein expression. |
| BirA Enzyme | Proximity biotin ligase; fused to the N-terminus of the E3. | N-terminal fusion minimizes steric hindrance with the E3's C-terminal catalytic domain [53]. |
| bioGEFUb | Engineered ubiquitin with a mutated AviTag (GEF sequence). | Essential for specificity. The bioGEF mutant prevents non-specific biotinylation [53] [35]. |
| Lentiviral TRIPZ Vector [53] | Doxycycline-inducible system for stable integration of bioGEFUb. | Allows controlled, temporal expression of bioGEFUb to minimize cellular stress. |
| Dialyzed, Biotin-depleted FBS | Serum for cell culture during the labeling phase. | Removes free biotin to minimize background labeling prior to the experimental pulse [53]. |
| Streptavidin Beads | High-affinity capture of biotinylated proteins. | Used under stringent, denaturing conditions to pull down only covalently biotinylated substrates. |
| TMT or iTRAQ Reagents [55] | Isobaric mass tags for multiplexed quantitative proteomics. | Enables relative quantification of ubiquitinated substrates across multiple conditions or time points. |
Detailed Protocol: Implementing BioE3 for Substrate Identification
This protocol outlines the key steps for applying the BioE3 method, incorporating critical steps to ensure specificity.
Pre-experimental Preparation
- Plasmid Preparation: Clone your E3 ligase of interest into a BirA fusion vector. Clone the bioGEFUb sequence into a doxycycline-inducible lentiviral vector (e.g., TRIPZ). Prepare high-quality, endotoxin-free plasmid DNA using commercial kits [54].
- Cell Line Engineering: Generate a stable cell line (e.g., HEK293FT, U2OS) with inducible bioGEFUb expression via lentiviral transduction and selection. For tumor research, consider using relevant cancer cell lines.
- Critical Pre-culture: 24 hours before transfection and induction, switch the stable cell line to a medium containing dialyzed, biotin-depleted serum to deplete endogenous biotin pools [53].
Transfection, Induction, and Biotin Labeling
- Transfection: Transfect the BirA-E3 fusion construct (or a BirA-only control) into the pre-cultured bioGEFUb-inducible cells.
- Induction: Induce the expression of bioGEFUb by adding doxycycline (DOX) for approximately 24 hours. This allows for the concomitant expression of the BirA-E3 fusion and the incorporation of bioGEFUb into cellular substrates.
- Biotin Pulse: Add exogenous biotin to the culture medium for a limited time (e.g., 2 hours). This time-limited pulse is crucial for capturing transient ubiquitination events and reducing background.
Substrate Capture and Identification
- Cell Lysis: Harvest and lyse cells in a denaturing lysis buffer (e.g., containing RIPA buffer and 1% SDS) to disrupt all non-covalent interactions and preserve only the covalent biotinylation mark.
- Streptavidin Pull-down: Incubate the clarified lysates with streptavidin-conjugated beads. Perform stringent washing to eliminate non-specifically bound proteins.
- Proteomic Analysis: Elute the bound proteins and digest them with trypsin. Analyze the resulting peptides by Liquid Chromatography with Tandem Mass Spectrometry (LC-MS/MS) to identify the enriched substrates.
The following diagram summarizes the molecular mechanism of the BioE3 system, highlighting the critical interaction that ensures specificity.
Application in Tumor Research: From Discovery to Validation
The BioE3 protocol is particularly suited for the molecular dissection of oncogenic and tumor-suppressive E3 ligases. For instance, it can be applied to:
- Identify novel oncogenic substrates of ligases that are amplified in cancer.
- Uncover lost degradation pathways in tumors harboring mutations in tumor-suppressor E3s.
- Investigate the rewiring of ubiquitination networks in response to therapeutic agents or under conditions of therapy resistance [53].
Following BioE3 screening, candidate substrates must be validated in a tumor context.
- Validation Assays: Employ standard in vivo ubiquitination assays [54]. This involves co-expressing the E3, the substrate, and His-tagged ubiquitin in tumor cell lines, treating with a proteasome inhibitor (e.g., MG-132), immunoprecipitating the substrate, and detecting poly-ubiquitination via anti-His or anti-Ub western blotting.
- Functional Studies: Validate the functional impact of ubiquitination on the substrate using CCK-8 assays for cell proliferation, transwell migration assays, and colony formation assays to assess the biological consequences in vitro [54] [56].
The ability to definitively distinguish genuine E3 ubiquitin ligase substrates from non-specific interactors is a cornerstone for advancing our understanding of cancer biology. The BioE3 method, with its engineered bioGEF tag and controlled biotinylation workflow, provides a robust and specific solution to this long-standing challenge. By implementing this detailed protocol, researchers in oncology and drug development can reliably map the ubiquitination networks that drive tumorigenesis, thereby uncovering new, high-confidence targets for the next generation of cancer therapeutics.
The ubiquitin-proteasome system (UPS) represents a crucial regulatory mechanism in eukaryotic cells, controlling protein stability, function, and localization through a dynamic equilibrium between ubiquitination and deubiquitination [57] [9]. This balance is particularly significant in cancer biology, where dysregulation of ubiquitinating and deubiquitinating enzymes is a common feature across various malignancies [9]. The ubiquitination process involves a sequential enzymatic cascade: ubiquitin-activating enzymes (E1) activate ubiquitin, which is then transferred to ubiquitin-conjugating enzymes (E2), and finally attached to specific substrate proteins via ubiquitin ligases (E3) [57] [58]. Conversely, deubiquitinating enzymes (DUBs) reverse this process by removing ubiquitin chains, thereby stabilizing proteins [57].
Recent research has firmly established that ubiquitination regulates all cancer hallmarks, including "evading growth suppressors," "reprogramming energy metabolism," and "unlocking phenotypic plasticity" [9]. In urological tumors, which account for approximately 10% of total tumor incidence, the UPS plays a critical role in regulating oncogenes, tumor suppressors, and therapeutic targets [57]. The dynamic reversibility of ubiquitination makes it particularly challenging to preserve in biological samples, as DUBs remain active during sample collection and processing [59]. This application note provides detailed methodologies for optimizing sample preparation from tumor tissues to maintain authentic ubiquitination states for accurate research outcomes.
Biological Significance of Ubiquitination in Tumors
Ubiquitination Mechanisms and Cancer Relevance
Ubiquitination encompasses multiple forms with distinct functional consequences. Monoubiquitination regulates DNA repair mechanisms and signal transduction, with clinical relevance demonstrated by UBE2T/RNF8-mediated H2AX monoubiquitination accelerating damage detection in hepatocellular carcinoma [59]. K48-linked polyubiquitination primarily targets proteins for proteasomal degradation, while K63-linked chains facilitate non-proteolytic signaling complexes involved in DNA repair and cell survival pathways [59]. The functional outcomes are highly context-dependent; for instance, FBXW7-mediated ubiquitination promotes radioresistance in p53-wild type colorectal tumors but enhances radiosensitivity in non-small cell lung cancer with SOX9 overexpression [59].
The SPOP E3 ubiquitin ligase, a substrate-interacting adapter within the Cullin 3-based E3 complex, demonstrates a mutation rate of 10-15% in prostate cancer and regulates lipid metabolism by reducing FASN expression and fatty acid synthesis [57] [58]. In bladder and kidney cancers, ubiquitination processes influence various aspects of signaling, protein stability, and cellular metabolism, making accurate preservation essential for understanding disease mechanisms [57].
Challenges in Presuring Ubiquitination States
The labile nature of ubiquitin modifications presents significant technical challenges. DUBs remain enzymatically active during sample collection and processing, potentially rapidly reversing ubiquitination events within minutes of tissue ischemia [59]. Additionally, the diversity of ubiquitin chain topologies (K48, K63, K11, K27, K29, K33, M1) with distinct functional consequences necessitates preservation methods that maintain this structural diversity [9] [59]. Tumor tissues exhibit considerable heterogeneity in the expression of ubiquitin ligases and DUBs, further complicating accurate profiling [59].
Materials and Reagents
Research Reagent Solutions
Table 1: Essential Reagents for Preserving Ubiquitination States in Tumor Tissues
| Reagent Category | Specific Examples | Function and Application |
|---|---|---|
| DUB Inhibitors | PR-619, N-ethylmaleimide (NEM), Iodoacetamide | Broad-spectrum DUB inhibition; alkylating agents that modify cysteine residues in active sites of multiple DUB families |
| Proteasome Inhibitors | MG-132, Bortezomib, Carfilzomib | Prevent degradation of ubiquitinated proteins by blocking the 26S proteasome |
| Phosphatase Inhibitors | Sodium fluoride, β-glycerophosphate, Sodium orthovanadate | Preserve phosphorylation status which often interfaces with ubiquitination signaling |
| Lysis Buffers | RIPA buffer with fresh inhibitors, NP-40 alternatives | Efficient extraction of ubiquitinated proteins while maintaining complex integrity |
| Denaturing Agents | SDS, Urea | Rapid denaturation of enzymes to "freeze" ubiquitination states at collection |
| Ubiquitin Affinity Reagents | TUBE (Tandem Ubiquitin Binding Entities), K48- or K63-linkage specific antibodies | Enrichment and detection of specific ubiquitin chain topologies |
Protocols for Sample Collection and Processing
Rapid Tissue Collection and Stabilization Protocol
- Pre-chill all equipment: Maintain tubes, solutions, and instruments on dry ice or at 4°C throughout the procedure.
- Ischemia time documentation: Record exact time from devascularization to freezing. Limit this interval to ≤5 minutes for optimal preservation.
- Rapid tissue dissection: Using pre-chilled instruments, rapidly dissect tumor tissue into appropriate segments for:
- Flash-freezing: Place 50-100 mg tissue fragments in pre-chilled cryovials and immediately submerge in liquid nitrogen (2-3 minutes).
- Denaturing lysis: For immediate processing, transfer tissue to 5-10 volumes of hot SDS lysis buffer (95°C, 1% SDS, 50 mM Tris pH 7.5).
- Homogenization under denaturing conditions: For SDS-lysed samples, immediately homogenize using a pre-heated mechanical homogenizer (95°C, 1-2 minutes).
- Clarification: Centrifuge at 16,000 × g for 15 minutes at 4°C and transfer supernatant to fresh tubes.
- Quality assessment: Aliquot samples for ubiquitination pattern validation before storage at -80°C.
Optimized Lysis Buffer Formulations
Table 2: Lysis Buffer Compositions for Ubiquitination Studies
| Buffer Type | Composition | Application | Advantages | Limitations |
|---|---|---|---|---|
| Denaturing Lysis Buffer | 1% SDS, 50 mM Tris-HCl (pH 7.5), 1 mM NEM, 5 mM iodoacetamide, 10 μM MG-132, Phosphatase inhibitors | Preserving instantaneous ubiquitination states; MS sample prep | Complete enzyme inactivation; preserves labile modifications | Incompatible with some functional assays; requires dilution for IP |
| Non-denaturing Lysis Buffer | 1% NP-40, 0.5% sodium deoxycholate, 0.1% SDS, 50 mM Tris-HCl (pH 8.0), 150 mM NaCl, plus fresh inhibitors | Co-immunoprecipitation studies; enzyme complex isolation | Maintains protein-protein interactions; suitable for functional assays | Potential DUB/E3 activity if inhibitors are incomplete |
| Urea-Based Buffer | 8 M Urea, 50 mM Tris-HCl (pH 8.0), 1 mM NEM, 5 mM iodoacetamide | Phosphoproteomics with ubiquitination analysis; insoluble proteins | Strong denaturation while maintaining solubility; compatible with digestion | Protein carbamylation with prolonged exposure |
Inhibitor Cocktail Formulation
Prepare fresh inhibitor cocktails according to the following formulation:
- DUB Inhibitor Cocktail: 5 mM NEM, 1 mM PR-619, 10 μM PYR-41 (E1 inhibitor)
- Protease/Proteasome Inhibitor Cocktail: 10 μM MG-132, 1 μM Bortezomib, 1× complete protease inhibitor (without EDTA)
- Phosphatase Inhibitor Cocktail: 1 mM sodium orthovanadate, 10 mM β-glycerophosphate, 5 mM sodium fluoride
- Reducing Environment Control: 1 mM TCEP (alternative to DTT to avoid DUB inhibition interference)
Workflow Visualization
Diagram 1: Sample Preparation Workflow for Ubiquitination Preservation
Quality Assessment and Validation
Ubiquitination Pattern Verification
- Western Blot Analysis: Use linkage-specific ubiquitin antibodies (K48, K63, K11) to confirm preservation of chain topologies.
- TUBE-based Affinity Purification: Employ Tandem Ubiquitin Binding Entities to enrich ubiquitinated proteins and assess global ubiquitination levels.
- Target Protein Validation: Immunoprecipitate proteins of interest (e.g., SPOP substrates, HIF-1α) to verify ubiquitination state preservation.
Troubleshooting Common Issues
Table 3: Troubleshooting Guide for Ubiquitination Preservation
| Problem | Potential Causes | Solutions | Preventive Measures |
|---|---|---|---|
| Loss of ubiquitin signal | Prolonged ischemia time; insufficient DUB inhibition | Increase inhibitor concentrations; implement rapid freezing | Pre-prepare inhibitor cocktails; train team on rapid processing |
| High background or smearing | Incomplete denaturation; proteolysis during processing | Increase SDS concentration; optimize heating time | Use hot lysis buffer; verify homogenization efficiency |
| Specific linkage loss | Selective DUB activity; improper handling | Add specific DUB inhibitors (e.g., OTUB inhibitors) | Include broad-spectrum and specific DUB inhibitors |
| Inconsistent results | Variable ischemia times; inhibitor degradation | Standardize collection protocol across all samples | Prepare fresh inhibitors weekly; use single-use aliquots |
Application in Experimental Design
Integration with Downstream Analyses
The optimized sample preparation methods described enable accurate assessment of ubiquitination states in various experimental contexts:
- Drug Mechanism Studies: For investigating compounds like PROTACs (e.g., ARV-110, ARV-471) that utilize the ubiquitin system for targeted protein degradation [9].
- Metabolic Reprogramming Studies: To examine ubiquitination-mediated regulation of lipid metabolism enzymes such as ACLY and FASN in cancers [58].
- Therapeutic Response Monitoring: For tracking dynamic changes in ubiquitination in response to treatments, including radiotherapy where ubiquitination regulates resistance mechanisms [59].
Concluding Recommendations
Successful preservation of ubiquitination states in tumor tissues requires:
- Speed: Minimize ischemia time to ≤5 minutes through careful planning and team coordination.
- Inhibition: Use comprehensive, fresh inhibitor cocktails targeting DUBs, proteasomes, and phosphatases.
- Appropriate Lysis: Match lysis conditions to experimental goals—denaturing for detection, non-denaturing for functional studies.
- Validation: Always include quality control measures to verify ubiquitination pattern preservation.
These protocols provide a foundation for reliable investigation of the ubiquitin system in cancer biology, enabling researchers to accurately capture this dynamic post-translational modification for mechanistic studies and therapeutic development.
Protein ubiquitination is a fundamental post-translational modification that regulates virtually every cellular process in eukaryotes, with particular significance in cancer biology [60]. The ubiquitin system's complexity extends beyond simple substrate modification to include diverse polyubiquitin chain architectures that encode distinct functional consequences—often termed the "ubiquitin code" [61]. In tumor samples, deciphering this code is essential for understanding oncogenic signaling pathways, resistance mechanisms, and developing targeted therapies.
Polyubiquitin chains are classified by their linkage patterns: homotypic chains (single linkage type), mixed chains (multiple linkages in tandem), and branched chains (multiple linkages at a single ubiquitin moiety) [62]. The development of tools to deconvolute these complex architectures has accelerated, enabling researchers to probe their roles in cancer-relevant processes such as protein degradation, DNA damage response, and mitophagy [37]. This Application Note details current methodologies for analyzing ubiquitin chain linkage and topology, with emphasis on applications in tumor sample research and drug discovery.
The Complexity of Polyubiquitin Chain Architectures
Chain Typology and Functional Consequences
The eight possible ubiquitin linkage types (Lys6, Lys11, Lys27, Lys29, Lys33, Lys48, Lys63, and Met1) create an extraordinary diversity of polyubiquitin signals with distinct biological functions [62] [61]. K48-linked chains typically target substrates for proteasomal degradation, while K63-linked chains more often regulate protein-protein interactions, endocytosis, and DNA repair [63]. The recently characterized branched chains further expand this signaling capacity, with K11-K48, K29-K48, and K48-K63 branched linkages performing specialized regulatory functions [62].
In cancer research, understanding these chain architectures is particularly relevant for characterizing oncoprotein regulation. For example, RAS proteins—the most frequently mutated oncoproteins in human cancers—are regulated by ubiquitination that controls their stability, membrane localization, and signaling transduction [64]. Different chain architectures on RAS isoforms can drive divergent tumor behaviors, making deconvolution of these signals a priority for therapeutic development.
Table 1: Functional Roles of characterized Branched Ubiquitin Chains
| Branched Chain Type | Key Functions | Relevance to Cancer Research |
|---|---|---|
| K11-K48 | Regulates protein degradation and cell cycle progression [62] | Potential target for cell cycle-directed therapies |
| K29-K48 | Mediates proteasomal degradation [62] | Substrate-specific degradation mechanisms |
| K48-K63 | Enhances NF-κB signaling; regulates p97/VCP processing [62] | Inflammation-driven cancer pathways; protein homeostasis |
Visualizing Ubiquitin Chain Complexity
The following diagram illustrates the major polyubiquitin chain architectures and their functional significance in cancer-relevant signaling pathways:
Mass Spectrometry-Based Approaches for Ubiquitin Chain Analysis
Ub-AQUA/PRM for Linkage Quantification
The Ubiquitin-Absolute Quantification/Parallel Reaction Monitoring (Ub-AQUA/PRM) method represents the gold standard for comprehensive ubiquitin linkage analysis [61]. This targeted mass spectrometry approach enables simultaneous quantification of all eight ubiquitin linkage types with high sensitivity and accuracy.
Workflow Principle: Trypsin digestion of ubiquitin chains generates signature peptides specific to each linkage type. Synthetic, isotopically labeled versions of these peptides (AQUA peptides) are spiked into samples as internal standards for absolute quantification [61]. The PRM methodology, implemented on quadrupole-equipped Orbitrap instruments, provides superior quantitative accuracy across a wide dynamic range—essential for detecting subtle changes in ubiquitin signaling within tumor samples.
Protocol Modifications for Tumor Samples:
- Tissue Lysis: Utilize sodium deoxycholate (SDC)-based lysis buffer supplemented with chloroacetamide (CAA) for immediate cysteine protease inactivation, improving ubiquitin site coverage by approximately 38% compared to urea-based methods [63].
- Sample Input: For limited tumor material, optimize input to 2mg protein for maximal K-GG peptide identification (>30,000 peptides).
- Digestion and Enrichment: Perform tryptic digestion followed by immunoaffinity purification of K-GG remnant peptides using anti-diglycine antibodies.
- LC-MS Analysis: Implement 75-minute nanoLC gradients with optimized MS parameters for DIA acquisition.
- Data Processing: Utilize DIA-NN software with specialized scoring modules for modified peptide identification, enabling quantification of >68,000 ubiquitinated peptides in single runs [63].
DIA-MS for Deep Ubiquitinome Profiling
Data-Independent Acquisition Mass Spectrometry (DIA-MS) has revolutionized ubiquitinome profiling by significantly improving coverage, reproducibility, and quantitative precision compared to traditional data-dependent acquisition (DDA) approaches [63].
Table 2: Performance Comparison of Ubiquitinomics Methods
| Method | Typical K-GG Peptide IDs | Reproducibility (Median CV) | Sample Throughput | Best Application Context |
|---|---|---|---|---|
| DDA-MS with Urea Lysis | 19,403 | ~20-30% | Moderate | Targeted studies with abundant sample |
| DDA-MS with SDC Lysis | 26,756 | ~15-25% | Moderate | Studies requiring maximal depth from limited samples |
| DIA-MS with SDC Lysis | 68,429 | ~10% | High | Large cohort studies; temporal dynamics |
| Ub-AQUA/PRM | Linkage-specific | <10% | Lower | Absolute quantification of specific linkages |
Key Advantages for Cancer Research:
- Comprehensive Coverage: DIA-MS more than triples identification numbers compared to DDA (68,429 vs. 21,434 K-GG peptides on average) [63].
- Temporal Resolution: Enables monitoring of ubiquitination dynamics following therapeutic interventions (e.g., DUB inhibition).
- High Precision: Median coefficient of variation <10% across replicates provides statistical power for detecting significant changes in heterogeneous tumor samples.
The workflow diagram below illustrates the optimized DIA-MS method for deep ubiquitinome profiling:
Biochemical and Proteomic Methods for Substrate Identification
E3-Substrate Tagging by Ubiquitin Biotinylation (E-STUB)
The E-STUB method addresses the critical challenge of identifying substrates for specific E3 ubiquitin ligases—highly relevant for understanding oncogenic pathways and developing targeted protein degraders [65].
Protocol Overview:
- Proximity Labeling: Engineered E3 ligases label nearby ubiquitylated substrates with biotin.
- Biotin-Based Affinity Purification: Streptavidin capture isolates biotinylated substrates.
- Mass Spectrometry Identification: LC-MS/MS identifies E3 ligase substrates with high specificity.
Applications in Cancer Drug Discovery:
- Characterize mechanisms of protein degraders (PROTACs and molecular glues)
- Identify collateral ubiquitylation events beyond primary targets
- Reveal non-degradative ubiquitylation events that modulate protein function [65]
Ub-ProT for Chain Length Determination
The Ubiquitin Chain Protection from Trypsinization (Ub-ProT) method addresses the challenging dimension of ubiquitin chain length, which significantly influences functional outcomes [61].
Method Principle: A "chain protector" molecule shields a specific region of ubiquitin chains from trypsin digestion, enabling determination of chain length through analysis of protected fragments.
Workflow Steps:
- Complex Preparation: Isolate ubiquitin conjugates of interest using TUBEs (tandem ubiquitin-binding entities) or immunoprecipitation.
- Chain Protection: Incubate with chain protector specific to ubiquitin chain type.
- Limited Trypsin Digestion: Perform controlled digestion to cleave unprotected regions.
- Mass Analysis: Quantify protected fragments by MS to determine chain length.
Cancer Research Application: Determining whether oncogenic substrates bear short vs. long ubiquitin chains provides insights into their regulation and potential therapeutic vulnerabilities.
Research Reagent Solutions
Table 3: Essential Research Reagents for Ubiquitin Chain Deconvolution
| Reagent Category | Specific Examples | Function/Application | Considerations for Tumor Samples |
|---|---|---|---|
| Linkage-Specific Antibodies | K11, K48, K63, M1 antibodies | Immunoblotting and immunofluorescence | Validation required for tumor tissue; potential cross-reactivity |
| Ubiquitin Mutants | Ub1-72, UbK48R, K63R, UbD77 | Enzymatic chain assembly | Enable defined branched chain synthesis [62] |
| Activity-Based Probes | DUB probes with warheads | Profiling deubiquitinase activity | Reveals DUB activities in tumor lysates |
| Tandem Ubiquitin-Binding Entities (TUBEs) | Based on ubiquitin-associated domains | Purification of ubiquitinated proteins | Preserve labile ubiquitination in dilute tumor extracts |
| AQUA Peptides | Isotopically labeled signature peptides | Absolute quantification by MS | Enable precise measurement of linkage abundance [61] |
| E3 Ligase Tools | E-STUB components [65] | Substrate identification | Critical for pathway-specific analysis in tumors |
The expanding toolkit for deconvoluting homotypic and heterotypic polyubiquitin chains is transforming our ability to decipher the ubiquitin code in cancer biology. Integration of mass spectrometry advancements like DIA-MS with biochemical methods for substrate identification and chain architecture analysis provides unprecedented insight into ubiquitin signaling networks dysregulated in tumors.
For drug development professionals, these methodologies enable:
- Comprehensive target validation through understanding of ubiquitin-dependent regulation
- Mechanistic understanding of protein degraders (PROTACs) and molecular glues
- Identification of resistance mechanisms through altered ubiquitin signaling
- Development of combination therapies targeting E3 ligases or DUBs alongside conventional treatments
As these tools continue to evolve, particularly through improved sensitivity for limited tumor samples and ability to characterize complex branched chains, they will undoubtedly uncover new therapeutic opportunities in cancer treatment by targeting the ubiquitin system with unprecedented precision.
Within the context of identifying ubiquitination substrates in tumor samples, controlling for experimental artifacts is not merely a procedural step but a fundamental requirement for data integrity. The overexpression of tagged ubiquitin and the use of proteasome inhibitors are ubiquitous techniques in ubiquitin-proteasome system (UPS) research. However, these interventions can introduce significant confounding effects, including the disruption of endogenous ubiquitin dynamics, alteration of substrate specificity, and induction of cellular stress pathways. These artifacts are particularly critical in tumor research, where accurately identifying disease-relevant substrates is essential for understanding immune evasion mechanisms and developing targeted therapies, such as those involving the PD-1/PD-L1 axis [17] [66]. This application note provides a structured framework to identify, quantify, and mitigate these artifacts, ensuring the reliability of substrate identification data in oncological research.
Artifacts from Tagged Ubiquitin Expression and Mitigation Strategies
The expression of tagged ubiquitin (e.g., HA-Ub, FLAG-Ub, BioUb) is a cornerstone of proteomic studies aiming to isolate and identify ubiquitinated substrates. Nevertheless, the introduction of these constructs can perturb the very system under investigation.
Key Artifacts and Biological Consequences
- Saturation of Endogenous Machinery: Overexpression can overwhelm the free ubiquitin pool, saturating cellular deubiquitinases (DUBs) and ubiquitin-binding proteins, which leads to a generalized accumulation of ubiquitinated proteins that may not reflect physiological conditions [35].
- Altered Substrate Specificity: The tag itself can sterically hinder interactions between ubiquitin and specific E3 ligases or DUBs, potentially skewing the observed ubiquitome. This is critical when studying E3 ligases like E6AP/UBE3A, implicated in Angelman syndrome and cervical cancer, or SPOP, which regulates PD-L1 stability in colorectal cancer [67] [17].
- Non-Specific Biotinylation: When using biotin-tagged ubiquitin (BioUb), a key artifact is non-specific, proximity-independent biotinylation. This occurs when the BirA biotin ligase biotinylates BioUb molecules that are not in the immediate vicinity of the E3 ligase complex, leading to false-positive substrate identification [35].
An Engineered Solution: The BioE3 System
The BioE3 system was specifically developed to address the challenge of non-specific biotinylation and to enhance the identification of bona fide E3 ligase substrates [35]. The core innovation involves using an AviTag mutant with lower affinity for BirA.
- bioGEFUb vs. bioWHEUb: The wild-type AviTag (bioWHE) has high affinity for BirA, causing widespread biotinylation regardless of E3 ligase proximity. The engineered bioGEF tag, with mutations that lower its affinity for BirA, ensures that biotinylation occurs only when the BioUb is in very close proximity to the BirA-E3 fusion protein, thereby conferring spatial specificity to the labeling event [35].
- Experimental Workflow for Specificity:
- Generate a stable cell line (e.g., HEK293FT, U2OS) with a doxycycline-inducible bioGEFUb construct.
- Transfert these cells with a BirA-E3 ligase fusion construct.
- Culture cells in biotin-depleted media to control the timing of biotinylation.
- Induce bioGEFUb and BirA-E3 expression with doxycycline for 24 hours.
- Add exogenous biotin for a limited time (e.g., 2 hours) to allow for proximity-dependent biotinylation of substrates being ubiquitinated by the BirA-E3 fusion.
- Perform streptavidin-based affinity enrichment and LC-MS/MS analysis [35].
Table 1: Quantitative Comparison of Tagged Ubiquitin Systems and Associated Artifacts
| System / Parameter | Conventional BioUb (bioWHE) | BioE3 System (bioGEF) | Impact on Data Quality |
|---|---|---|---|
| Non-Specific Biotinylation | High | Effectively eliminated | bioGEF drastically reduces false-positive substrate identification [35] |
| Spatial Specificity | Low | High | bioGEF ensures labeling only near the BirA-E3 ligase [35] |
| Dependency on Overexpression | High | Moderate (controlled by inducible system) | Both systems can saturate endogenous pathways; inducible expression is recommended |
| Identification of Known E3 Substrates | May be obscured by background | Reliable identification (e.g., PSMD4, UCHL5 for E6AP) | Enhanced signal-to-noise ratio is critical for validating method accuracy [67] [35] |
Artifacts from Proteasome Inhibition and Alternative Approaches
Proteasome inhibitors (e.g., MG132, Bortezomib) are widely used to stabilize ubiquitinated proteins and facilitate their detection. However, their application induces broad cellular changes that can confound data interpretation.
Key Artifacts and Compounding Effects
- Global Disruption of Protein Homeostasis: Inhibiting the proteasome causes the accumulation of a vast number of ubiquitinated proteins beyond the pathway of immediate interest. This can mask specific substrate-ligase relationships and activate stress response pathways, such as the unfolded protein response and integrated stress response [68] [66].
- Induction of Alternative Degradation Pathways: Cellular compensation can occur through the upregulation of autophagy or the ubiquitin-independent REGγ-proteasome pathway. This is particularly relevant in KRAS-mutant cancers, where the REGγ-proteasome is often overactive and can degrade substrates like the tumor suppressor p21, even when the canonical proteasome is inhibited [68].
- Perturbation of Apoptotic Signaling: Proteasome inhibition leads to the accumulation of pro-apoptotic proteins, potentially inducing rapid cell death in tumor samples. This alters the cellular context and truncates the experimental window, making it difficult to distinguish primary ubiquitination events from secondary effects of apoptosis [66].
Strategic Use of Proteasome Inhibition
Given these artifacts, a more nuanced approach to proteasome inhibition is required.
- Titration and Time-Course Experiments: Instead of using a single, high dose, perform a dose-response and time-course analysis to identify the minimal concentration and shortest duration of inhibition that yield detectable levels of the substrate of interest. This helps minimize compensatory mechanisms and global stress responses.
- Combining with E3-Centric Methods: For a more targeted approach, combine mild proteasome inhibition with E3-specific methods like BioE3. The inhibitor helps stabilize the ubiquitinated substrate, while BioE3 provides the specificity to attribute it to a particular E3 ligase [35].
- Monitoring Compensatory Pathways: Always include controls to monitor the activation of alternative pathways. For instance, assess the levels of LC3 (autophagy marker) and REGγ substrates to gauge the extent of compensation in your experimental system, especially in KRAS-mutant cancer models [68].
Table 2: Artifacts and Compensatory Mechanisms Induced by Proteasome Inhibition
| Artifact / Compensatory Mechanism | Key Mediators / Pathways | Experimental Monitoring Strategy |
|---|---|---|
| Global Ubiquitinated Protein Accumulation | K48-linked ubiquitin chains | Western blot for poly-ubiquitinated proteins; proteomic depth as a confounder |
| Activation of Unfolded Protein Response | IRE1, ATF6, PERK pathways | qPCR for BiP, CHOP; Western for XBP1 splicing [66] |
| Upregulation of Autophagy | LC3-I/II, p62/SQSTM1 | Western blot for LC3 lipidation and p62 turnover; immunofluorescence [69] |
| Activation of Ubiquitin-Independent Proteasome | REGγ-20S proteasome | Assess stability of known REGγ substrates (e.g., p21, SRC-3) [68] |
| Induction of Apoptosis | Bcl-2 family proteins, caspases | Western for cleaved caspase-3; PARP cleavage [66] |
Integrated Experimental Protocol for Tumor Samples
This protocol integrates the BioE3 system with controlled proteasome inhibition for the specific identification of E3 ligase substrates in tumor-derived cell lines, with a focus on controlling artifacts.
Stage 1: Cell Line Preparation and Validation
Materials:
Procedure:
- Generate a stable polyclonal cell line expressing the inducible bioGEFUb construct via lentiviral transduction and puromycin selection.
- Validate inducibility by treating cells with 1 µg/mL doxycycline for 24 hours and analyzing AviTag expression via Western blot.
- Introduce the BirA-E3 ligase construct into the bioGEFUb cell line via a second round of transduction/transfection and selection.
- For all experiments preceding biotinylation, culture cells in media supplemented with biotin-depleted serum for at least 48 hours to deplete endogenous biotin.
Stage 2: Controlled Substrate Trapping and Enrichment
- Induction and Inhibition: Induce bioGEFUb and BirA-E3 expression with 1 µg/mL doxycycline. After 20 hours, add a low concentration of MG132 (e.g., 5 µM) to gently stabilize ubiquitinated substrates. Incubate for 4 hours.
- Proximity Biotinylation: Add 50 µM D-biotin to the culture media for a precise, limited time (e.g., 2 hours) to allow labeling of substrates captured by the BirA-E3.
- Cell Lysis and Enrichment: Wash cells with cold PBS and lyse in a stringent RIPA buffer containing protease inhibitors, DUB inhibitors (e.g., 10 mM N-Ethylmaleimide), and phosphatase inhibitors.
- Clarify the lysate by centrifugation. Incubate the supernatant with high-capacity streptavidin-agarose beads for 2 hours at 4°C.
- Wash Beads sequentially with lysis buffer, high-salt buffer (1 M NaCl), and detergent-only buffer to remove non-specifically bound proteins.
- On-bead digestion for mass spectrometry analysis.
Stage 3: Data Analysis and Artifact Assessment
- Proteomic Data Processing: Identify proteins from LC-MS/MS data and use the following criteria to prioritize high-confidence substrates:
- Proteins significantly enriched in
bioGEFUb + BirA-E3 + Biotinsamples overbioWHEUb + BirA-E3 + Biotincontrols. - Proteins enriched over
bioGEFUb + BirA-E3 (No Biotin)controls.
- Proteins significantly enriched in
- Validation: Confirm key hits using orthogonal methods such as co-immunoprecipitation and Western blotting under conditions of mild proteasome inhibition.
- Artifact Monitoring: Actively check for markers of stress response (e.g., CHOP for ER stress) and compensatory pathways (e.g., LC3 for autophagy) in your whole-cell lysates to contextualize your proteomic findings.
Visualization of Experimental Workflows and Signaling Context
BioE3 Workflow for Specific Substrate Identification
This diagram illustrates the key steps and critical controls in the BioE3 protocol for identifying genuine E3 ligase substrates while minimizing artifacts.
UPS in Tumor Immunity & Therapy
This diagram places the experimental method within the broader biological context of the Ubiquitin-Proteasome System in tumor immunity and therapy.
The Scientist's Toolkit: Key Research Reagent Solutions
Table 3: Essential Reagents for Controlling Artifacts in Ubiquitin Substrate Identification
| Reagent / Tool | Primary Function | Key Consideration for Artifact Control |
|---|---|---|
| Inducible bioGEFUb System | Enables proximity-dependent, specific biotinylation of ubiquitinated substrates. | The bioGEF mutant tag is critical to prevent non-specific biotinylation by BirA, a major source of false positives [35]. |
| BirA-E3 Ligase Fusions | Targets biotinylation activity to substrates of a specific E3 ligase. | N-terminal fusion is often preferred to avoid steric hindrance of the C-terminal RING/HECT catalytic domain [35]. |
| Biotin-Depleted Serum | Allows precise temporal control over the biotinylation reaction. | Essential for minimizing background labeling; use for at least 48 hours prior to biotin addition [35]. |
| Titrated Proteasome Inhibitors | Stabilizes ubiquitinated substrates by blocking their degradation. | Use the lowest effective concentration for the shortest duration to minimize global stress and activation of compensatory pathways [68] [66]. |
| DUB-Inhibiting Lysis Buffers | Preserves ubiquitin conjugates during cell processing. | Inclusion of N-Ethylmaleimide (NEM) or other DUB inhibitors is crucial to prevent deubiquitination after lysis. |
| Stringent Wash Buffers | Removes non-specifically bound proteins after affinity enrichment. | Washes with high-salt (e.g., 1 M NaCl) and detergent are necessary to reduce background and increase specificity for MS. |
From Candidate to Validated Substrate: Functional Assays and Cross-Technique Corroboration
Protein ubiquitination is a crucial post-translational modification that regulates the stability, activity, and localization of a vast array of cellular proteins. This process involves a sequential enzymatic cascade whereby ubiquitin is activated by an E1 enzyme, transferred to an E2 conjugating enzyme, and finally delivered to a substrate protein by an E3 ligase [58] [1]. The reverse reaction is catalyzed by deubiquitinases (DUBs), which remove ubiquitin modifications, adding a further layer of regulation [58]. In the context of cancer, ubiquitination plays a fundamental role in controlling oncogenic and tumor-suppressive pathways, influencing tumor metabolism, the immunological tumor microenvironment, and cancer stem cell stemness [1]. The identification of specific ubiquitination substrates and regulators in tumor samples is therefore a critical research focus, as it can reveal novel therapeutic targets and biomarkers. For instance, recent pancancer analyses have identified prognostic signatures and key regulatory nodes, such as the OTUB1-TRIM28 ubiquitination axis that modulates MYC signaling and influences patient prognosis and immunotherapy response [8]. This application note provides a structured validation workflow, detailing the integration of in vitro ubiquitylation assays with cellular and in vivo models to functionally characterize putative ubiquitination substrates identified in tumorigenesis research.
Integrated Validation Workflow: From In Vitro Biochemistry to In Vivo Confirmation
A robust validation workflow for a putative ubiquitination substrate progresses through three sequential phases, each designed to answer a specific set of questions about the ubiquitination event, its functional consequences, and its pathological relevance. The following diagram illustrates this integrated, tiered strategy.
Phase 1: In Vitro Ubiquitylation Assays
Objective and Rationale
The primary objective of Phase 1 is to establish a direct, biochemical relationship between a substrate and the ubiquitination machinery, free from the complexities of the cellular environment. This confirms whether the E3 ligase or DUB can directly modify the substrate without requiring intermediary proteins.
Detailed Protocol: Reconstituted Ubiquitination Assay
3.2.1 Reagent Setup
- Purified Components: Recombinant E1 enzyme (e.g., UBA1), E2 enzyme (e.g., UbcH5a, UbcH5b, UbcH5c, UbcH13-Mms2), E3 ligase (full-length or catalytic domain, e.g., TRIM28, SPOP), and substrate protein. Proteins should be purified to >90% homogeneity.
- Reaction Buffer: 50 mM Tris-HCl (pH 7.5), 5 mM MgCl₂, 2 mM ATP, 0.5 mM DTT.
- Ubiquitin Source: 5-10 µg of recombinant wild-type Ub or mutant Ub (e.g., K48-only, K63-only, K0).
- Energy Regeneration System: 10 mM Creatine Phosphate, 1 U Creatine Kinase (optional, for prolonged reactions).
3.2.2 Procedure
- Master Mix Preparation: On ice, combine in a 1.5 mL microcentrifuge tube:
- 5 µL 10X Reaction Buffer
- 1 µL 100 mM ATP
- 0.5 µL 1 M DTT
- 2 µL 5 mg/mL Ubiquitin
- 100 ng E1
- 200 ng E2
- 500 ng E3
- 1 µg Substrate
- Nuclease-free water to a final volume of 50 µL.
- Incubation: Mix gently and incubate the reaction at 30°C for 60-90 minutes.
- Termination: Stop the reaction by adding 15 µL of 4X Laemmli sample buffer and heating at 95°C for 5-10 minutes.
- Analysis: Resolve the reaction by SDS-PAGE (4-12% Bis-Tris gradient gel recommended). Analyze via:
- Immunoblotting: Transfer to PVDF membrane and probe with anti-substrate, anti-ubiquitin (e.g., P4D1), or anti-polyubiquitin linkage-specific (e.g., K48, K63) antibodies.
- Coomassie/Silver Staining: To visualize total protein ubiquitination.
3.2.4 Controls: Include reactions missing individual components (e.g., -E1, -E2, -E3, -ATP) to confirm the specificity of the ubiquitination cascade.
Key Research Reagents for In Vitro Ubiquitylation
Table 1: Essential Reagents for In Vitro Ubiquitination Assays
| Reagent Category | Specific Examples | Function in Assay |
|---|---|---|
| Enzymes | UBA1 (E1), UbcH5b (E2), TRIM28 (E3) | Catalyze the sequential activation, conjugation, and ligation of ubiquitin to the substrate protein. |
| Ubiquitin | Wild-type Ubiquitin, K48-only Ub, K63-only Ub, K0 (no-lysine) Ub | The modifying protein; mutant forms determine chain linkage specificity and requirement. |
| Substrate | Recombinant protein of interest (e.g., ACLY, MYC) | The target protein whose ubiquitination is being investigated. |
| Detection Antibodies | Anti-Ubiquitin (P4D1), Anti-K48-linkage, Anti-K63-linkage, Anti-HA (for HA-Ub) | Detect ubiquitinated species and characterize the topology of polyubiquitin chains. |
| Buffer Components | ATP, MgCl₂, DTT, Tris Buffer | Provide essential cofactors and maintain optimal pH and reducing environment for enzyme activity. |
Phase 2: Cellular Functional Validation
Objective and Rationale
This phase aims to verify the ubiquitination event within a cellular context and determine its functional consequences on substrate stability, downstream signaling, and cellular phenotype.
Detailed Protocol: Co-immunoprecipitation (Co-IP) and Cycloheximide Chase
4.2.1 Co-IP to Verify Endogenous Interaction
- Cell Culture & Transfection: Culture relevant cancer cells (e.g., HEK293T, A549, MCF-7). Transfect with plasmids encoding E3, DUB, or empty vector control.
- Cell Lysis: At 24-48 hours post-transfection, lyse cells in 1 mL of NP-40 or RIPA lysis buffer supplemented with 1X protease inhibitor cocktail and 20 µM N-ethylmaleimide (NEM, a DUB inhibitor).
- Pre-clearing & Immunoprecipitation: Pre-clear lysate with 20 µL Protein A/G beads for 30 minutes at 4°C. Incubate supernatant with 1-2 µg of target antibody (anti-substrate or anti-E3) overnight at 4°C. Add 30 µL Protein A/G beads the next day and incubate for 2-4 hours.
- Washing and Elution: Wash beads 3-4 times with cold lysis buffer. Elute proteins by boiling in 2X Laemmli buffer.
- Immunoblotting: Probe the immunoprecipitates and whole-cell lysate (input) for the substrate, E3/DUB, and ubiquitin.
4.2.2 Cycloheximide Chase Assay to Measure Protein Half-Life
- Treatment: Treat cells (transfected or with modulated E3/DUB expression) with 100 µg/mL cycloheximide to inhibit new protein synthesis.
- Time-Course Harvesting: Harvest cell pellets at defined time points (e.g., 0, 1, 2, 4, 8 hours) post-cycloheximide addition.
- Lysis and Immunoblotting: Lyse pellets and perform immunoblotting for the substrate protein.
- Densitometry Analysis: Quantify band intensity and plot relative protein levels over time to calculate half-life.
The following diagram illustrates the cellular decision-making process triggered by different ubiquitin linkages, a key functional outcome validated in this phase.
Key Research Reagents for Cellular Validation
Table 2: Essential Reagents for Cellular Ubiquitination Studies
| Reagent Category | Specific Examples | Function in Assay |
|---|---|---|
| Expression Plasmids | HA-Ubiquitin, MYC-E3 Ligase, FLAG-Substrate, DUB shRNA | To overexpress or knock down components of the ubiquitination machinery in cells. |
| Cell Lines | HEK293T, Cancer cell lines relevant to tumor samples (e.g., A549, HCT116) | Provide a cellular context to study endogenous and exogenous ubiquitination. |
| Inhibitors | MG132/ Bortezomib (Proteasome), MLN7243 (E1), Cycloheximide (Translation) | Block protein degradation or synthesis to study substrate turnover and stability. |
| Critical Antibodies | Antibodies against endogenous substrate, E3, DUB, Ubiquitin | For immunoblotting and immunoprecipitation to detect proteins and interactions. |
| Lysis Buffers & Additives | RIPA Buffer, NP-40 Buffer, Protease Inhibitors, NEM (DUB inhibitor) | Extract proteins while preserving post-translational modifications and interactions. |
Phase 3: In Vivo Pathophysiological Validation
Objective and Rationale
The final phase seeks to establish the pathophysiological relevance of the ubiquitination event in a complex, whole-organism system, assessing its impact on tumorigenesis, metastasis, and therapy response.
Detailed Protocol: Xenograft Tumor Models and Immunohistochemistry
5.2.1 Animal Model Generation
- Cell Preparation: Use cancer cells with stable knockdown/knockout of the E3 ligase or DUB, or control cells. Use CRISPR-Cas9 or lentiviral shRNA systems.
- Xenograft Implantation: Resuspend 1-5 x 10^6 cells in 100 µL of PBS/Matrigel (1:1) mixture. Inject subcutaneously into the flanks of immunodeficient mice (e.g., NOD/SCID or NSG mice). Assign mice randomly to experimental groups.
- Tumor Monitoring: Measure tumor dimensions with calipers 2-3 times per week. Calculate tumor volume using the formula: Volume = (Length x Width²) / 2.
- Endpoint Analysis: Harvest tumors at a predetermined endpoint (e.g., 4-6 weeks or when tumor volume reaches ~1500 mm³). Weigh tumors and divide them for subsequent molecular analysis (snap-freezing for immunoblotting, RNA extraction; fixation for IHC).
5.2.2 Tumor Tissue Analysis via Immunohistochemistry (IHC)
- Fixation and Sectioning: Fix tumor tissues in 10% neutral buffered formalin for 24-48 hours, then embed in paraffin. Section at 4-5 µm thickness.
- Antigen Retrieval and Staining: Deparaffinize and rehydrate sections. Perform heat-induced epitope retrieval in citrate or EDTA buffer. Block endogenous peroxidases and nonspecific sites.
- Primary and Secondary Antibody Incubation: Incubate with primary antibodies (e.g., anti-substrate, anti-K48 ubiquitin, anti-Ki67) overnight at 4°C. The next day, apply appropriate HRP-conjugated secondary antibodies.
- Detection and Counterstaining: Develop the signal using DAB substrate, which produces a brown precipitate. Counterstain with hematoxylin to visualize nuclei.
- Scoring and Analysis: Score slides by a pathologist or using automated image analysis software for staining intensity and percentage of positive cells. Correlate with tumor volume and grade.
Data Integration with Clinical Cohorts
Correlate the findings from the in vivo models with human tumor data from public repositories like The Cancer Genome Atlas (TCGA). Analyze whether the expression levels of the E3 ligase, DUB, and substrate are correlated with patient overall survival, cancer stage, or histological subtype, as demonstrated in pancancer studies [8].
Troubleshooting and Technical Considerations
- Specificity of Antibodies: A common challenge is the specificity of ubiquitin antibodies for immunoblotting. Using linkage-specific antibodies requires rigorous validation with controls.
- Inhibitor Specificity: The effects of proteasome inhibitors like MG132 are global. Results should be interpreted with caution and combined with genetic (e.g., siRNA) approaches to modulate specific E3s/DUBs.
- Chain Linkage Complexity: In vitro assays may not fully recapitulate the complexity of ubiquitin chain formation in cells. Using a panel of ubiquitin mutants (K48R, K63R, K48-only, etc.) can help decipher linkage specificity.
- Dynamic Range of Assays: Ubiquitinated species are often transient and low-abundance. Enrichment strategies, such as Tandem Ubiquitin Binding Entities (TUBEs) or the use of DUB inhibitors (NEM, PR-619) during lysis, are critical for successful detection.
This application note provides a detailed comparative analysis of substrate specificity between the closely related E3 ubiquitin ligases Nedd4-1 (Nedd4) and Nedd4-2 (Nedd4L). Within the context of identifying ubiquitination substrates in tumor samples, we present structured quantitative data, experimental protocols for substrate profiling, and visualization of key signaling pathways. Our analysis demonstrates that while these ligases share structural similarities and some common substrates, they exhibit distinct preferences with significant implications for cancer signaling pathways, tumor metabolism, and immune regulation. The methodologies outlined herein provide a framework for researchers investigating E3 ligase function in oncogenesis and targeted drug discovery.
The neural precursor cell-expressed developmentally downregulated gene 4 (Nedd4) family of HECT-type E3 ubiquitin ligases represents crucial regulators of cellular homeostasis whose dysfunction is increasingly implicated in tumorigenesis. Of the nine mammalian Nedd4 family members, Nedd4-1 and Nedd4-2 share the closest evolutionary relationship and structural architecture, yet mounting evidence indicates they perform distinct physiological functions [70]. Both enzymes feature an N-terminal C2 domain that mediates membrane localization, 2-4 WW domains that recognize proline-rich PY motifs (L/PPxY) in substrate proteins, and a C-terminal HECT domain that catalyzes ubiquitin transfer [71] [70]. Despite these structural similarities, emerging research reveals they target distinct subsets of proteins with significant implications for cancer biology, including regulation of receptor tyrosine kinases, ion channels, and apoptotic regulators.
In the context of tumor samples, understanding E3 ligase-substrate relationships is paramount, as ubiquitination plays a fundamental role in regulating cancer hallmarks such as evading growth suppressors, reprogramming energy metabolism, and unlocking phenotypic plasticity [1] [9]. The ubiquitin-proteasome system (UPS) regulates the stability of approximately 80-90% of cellular proteins, making E3 ligases like Nedd4-1 and Nedd4-2 attractive therapeutic targets for cancer treatment [9]. This application note provides a comprehensive resource for researchers aiming to decipher the specific functions of these ligases in tumorigenesis through comparative substrate profiling.
Comparative Substrate Specificity: Nedd4-1 vs. Nedd4-2
Global Substrate Profiling Using Proteome Arrays
A landmark study employing protein microarray technology spotted with approximately 8,200 human proteins provided the first comprehensive comparison of Nedd4-1 and Nedd4-2 substrate specificity [71] [72]. This systematic approach revealed that while both ligases primarily recognize substrates containing PY motifs, they exhibit distinct preferences:
Table 1: Comparative Substrate Specificity of Nedd4-1 and Nedd4-2
| Ligase Feature | Nedd4-1 | Nedd4-2 |
|---|---|---|
| Preferred Substrate Types | Tyrosine kinases (e.g., FGFR) | Ion channels, transporters (e.g., ENaC, NCC) |
| Shared Substrates | Multiple common substrates identified | Multiple common substrates identified |
| Validated In Vivo Targets | FGFR (knockdown increases signaling) | ENaC (regulation linked to Liddle's syndrome) |
| Structural Basis | WW domains recognize PY motifs | WW domains recognize PY motifs |
| Tumor Relevance | Sustained tyrosine kinase signaling | Ion homeostasis affecting tumor microenvironment |
The proteome array data demonstrated that Nedd4-1 preferentially ubiquitinates tyrosine kinases such as FGFR, and subsequent validation experiments confirmed that Nedd4-1 knockdown sustains signaling through these receptors [71]. This finding positions Nedd4-1 as a potential negative regulator of oncogenic signaling. Conversely, Nedd4-2 showed preference for ion channels and transporters, including the epithelial sodium channel (ENaC) and sodium chloride transporter (NCC), with important implications for cellular homeostasis and the tumor microenvironment [71] [73].
Novel Substrate Identification in Cancer Context
Recent research has continued to expand the known substrate repertoire for these ligases, particularly in disease contexts. A 2025 study identified phospholipid scramblase 1 (PLSCR1) as a novel Nedd4-2 substrate through affinity purification mass spectrometry in kidney cells [73]. This finding connects Nedd4-2 to the regulation of phosphatidyl serine exposure and apoptotic cell clearance – processes with significant implications for tumor immune evasion and therapy resistance.
The interaction between Nedd4-2 and PLSCR1 depends on the canonical PY motif recognition, as mutation of the PPPY motif in PLSCR1 substantially reduced both binding and ubiquitination efficiency [73]. Functionally, Nedd4-2 deficiency resulted in increased PLSCR1 protein levels, enhanced phosphatidyl serine exposure in response to calcium and apoptotic stimuli, and higher rates of macrophage clearance of apoptotic cells [73]. This regulatory relationship exemplifies how E3 ligase profiling can reveal novel connections to cancer-relevant processes, including immunogenic cell death and phagocytosis.
Experimental Protocols for E3 Ligase Substrate Identification
Proteome Array-Based Ubiquitylation Assay
The proteome array approach provides a high-throughput method for initial substrate screening [71]:
Materials:
- Protein microarrays spotted with ~8,200 human proteins
- Purified E3 ligases (Nedd4-1 and Nedd4-2)
- Ubiquitination reaction mix: E1 enzyme, E2 enzyme, ubiquitin, ATP
- Detection reagents (antibodies, fluorescence labels)
Procedure:
- Array Preparation: Block protein microarrays with suitable blocking buffer (e.g., 1% BSA in TBST) for 1 hour at room temperature.
- Ligase Binding: Incubate arrays with purified Nedd4-1 or Nedd4-2 (1-5 µg/mL in binding buffer) for 2 hours at 4°C with gentle agitation.
- Ubiquitination Reaction: Add ubiquitination reaction mix containing 50 nM E1, 100 nM E2 (UbcH5b or similar), 10 µg/mL ubiquitin, and 5 mM ATP in reaction buffer. Incubate for 90 minutes at 30°C.
- Detection: Wash arrays and incubate with anti-ubiquitin primary antibody (1:1000) for 1 hour, followed by fluorescently labeled secondary antibody (1:2000) for 45 minutes.
- Image Acquisition: Scan arrays using a fluorescence scanner and quantify signal intensity for each spot.
- Data Analysis: Normalize signals, subtract background, and identify high-confidence substrates based on statistical thresholds.
Validation: Top hits should be validated through co-immunoprecipitation and in vitro ubiquitination assays, followed by functional validation in cellular models (e.g., knockdown/knockout studies) [71].
Affinity Purification Mass Spectrometry for Novel Substrate Discovery
This protocol identifies novel E3 ligase interactors in relevant cellular contexts [73]:
Materials:
- Cell lines expressing tagged E3 ligase (e.g., NEDD4-2-myc)
- Cross-linking reagent (if required)
- Lysis/wash buffers, affinity resin (anti-myc or similar)
- Mass spectrometry equipment and reagents
Procedure:
- Cell Culture and Lysis: Culture CCD (cortical collecting duct) cells or other relevant cell lines. Transfect with NEDD4-2-myc plasmid. Harvest cells and lyse in appropriate lysis buffer containing protease inhibitors.
- Affinity Purification: Incubate cell lysates with anti-myc agarose beads for 4 hours at 4°C with rotation.
- Wash and Elution: Wash beads extensively with lysis buffer, followed by an additional wash with low-salt buffer. Elute bound proteins with myc peptide or low-pH elution buffer.
- Sample Preparation for MS: Denature eluted proteins, reduce with DTT, alkylate with iodoacetamide, and digest with trypsin overnight.
- Mass Spectrometry Analysis: Desalt peptides and analyze by LC-MS/MS using a high-resolution instrument.
- Data Processing: Search MS data against appropriate protein databases, apply statistical filters to identify high-confidence interactors.
Validation: Confirm interactions through co-immunoprecipitation and assess functional consequences through ubiquitination assays and phenotypic analysis [73].
Ubiquitylome Analysis of Tumor Tissues
This protocol enables system-wide identification of ubiquitinated substrates in clinical samples [5]:
Materials:
- Tumor and matched normal tissues (fresh frozen)
- K-ε-GG antibody-conjugated resin
- Protein extraction and digestion reagents
- Liquid chromatography-mass spectrometry system
Procedure:
- Protein Extraction: Grind tissue samples in liquid nitrogen. Lyse powder in buffer containing 1% Triton X-100, protease inhibitors, and deubiquitinase inhibitor PR-619.
- Protein Digestion: Determine protein concentration by BCA assay. Precipitate proteins with TCA, then digest with trypsin (1:50 ratio) overnight.
- Ubiquitinated Peptide Enrichment: Incubate digested peptides with K-ε-GG antibody resin overnight at 4°C. Wash resin extensively, then elute bound peptides with 0.1% TFA.
- LC-MS/MS Analysis: Desalt eluted peptides and analyze by LC-MS/MS using instruments such as timsTOF Pro.
- Data Analysis: Process raw data using software such as MaxQuant, searching against human protein databases. Identify differentially ubiquitinated peptides between tumor and normal tissues.
This approach has revealed distinctive ubiquitination patterns in lung adenocarcinoma (LUAD) compared to other cancer types, providing insights into tumor-specific ubiquitination events [5].
Visualization of Nedd4-1 and Nedd4-2 Regulatory Networks
Figure 1: Nedd4-1 and Nedd4-2 Regulatory Networks in Cancer. This diagram illustrates the distinct substrate preferences and downstream oncogenic consequences of Nedd4-1 and Nedd4-2 regulation.
Research Reagent Solutions for E3 Ligase Studies
Table 2: Essential Research Reagents for E3 Ligase Substrate Identification
| Reagent/Category | Specific Examples | Function/Application |
|---|---|---|
| Protein Microarrays | Human Proteome Microarray (~8,200 proteins) | High-throughput in vitro substrate screening [71] |
| Affinity Purification Resins | Anti-myc, Anti-GFP, Anti-FLAG agarose | Immunoprecipitation of tagged E3 ligases and interactors [73] |
| Ubiquitination Assay Components | E1 enzyme, E2 enzymes (UbcH5 family), Ubiquitin, ATP | In vitro and cellular ubiquitination reactions [71] [73] |
| Mass Spectrometry Platforms | LC-MS/MS with timsTOF Pro | Identification of ubiquitinated peptides and interacting proteins [73] [5] |
| Ubiquitin Enrichment Reagents | K-ε-GG antibody resin | Enrichment of ubiquitinated peptides for ubiquitylome analysis [5] |
| Proteasome Inhibitors | MG132, Bortezomib | Stabilize ubiquitinated proteins and assess proteasomal degradation [73] |
| Lysosomal Inhibitors | Chloroquine, Bafilomycin A1 | Assess lysosomal degradation pathways [73] |
| E3 Ligase Expression Constructs | NEDD4-2-myc, PLSCR1-GFP, PY mutants | Functional studies of E3-substrate interactions [73] |
Implications for Tumor Biology and Therapeutic Development
The distinct substrate preferences of Nedd4-1 and Nedd4-2 have significant implications for understanding tumor biology and developing targeted therapies. Nedd4-1's regulation of tyrosine kinases such as FGFR positions it as a potential tumor suppressor in certain contexts, as its loss or inhibition would sustain mitogenic signaling [71]. This is particularly relevant given the importance of receptor tyrosine kinase signaling in numerous cancer types.
Conversely, Nedd4-2's regulation of ion channels and apoptotic regulators like PLSCR1 suggests roles in modulating the tumor microenvironment and immunogenic cell death [73]. The finding that Nedd4-2 deficiency enhances phosphatidyl serine exposure and macrophage clearance indicates potential applications in immunotherapy, where enhancing immune recognition of tumor cells is a therapeutic goal.
From a translational perspective, understanding E3 ligase-substrate relationships enables several therapeutic approaches:
- Targeted protein degradation using PROTACs or molecular glues that recruit specific E3 ligases to oncoproteins [74] [75] [9]
- Small molecule inhibitors of E3 ligases that inappropriately target tumor suppressors
- Activators of E3 ligases that could enhance degradation of oncoproteins
Recent advances in chemoproteomics and fragment-based screening have enabled identification of ligands for E3 ligases with restricted expression patterns, opening possibilities for tumor-selective degraders that minimize on-target toxicity in healthy tissues [75]. Additionally, high-throughput screening approaches like COMET (combinatorial mapping of E3 targets) provide frameworks for systematically testing E3-substrate relationships [76].
This application note demonstrates that despite their structural similarities, Nedd4-1 and Nedd4-2 exhibit distinct substrate preferences with different implications for cancer biology. The experimental protocols outlined provide researchers with robust methodologies for identifying novel E3-substrate relationships in tumor samples, while the visualization tools and reagent tables offer practical resources for experimental design. As research in this field advances, understanding the nuanced functions of closely related E3 ligases will be crucial for developing targeted therapeutic strategies that exploit the ubiquitin-proteasome system in cancer treatment.
Within the framework of identifying ubiquitination substrates in tumor samples, functional assays are indispensable for connecting molecular modifications to phenotypic outcomes. The ubiquitin-proteasome system (UPS) catalyzes the tagging of proteins for degradation, a process critically involved in regulating cancer cell proliferation, apoptosis, and metabolic reprogramming [58]. Alterations in ubiquitination of key metabolic and signaling proteins can occur early in tumorigenesis, influencing cellular responses to stressors and therapeutics [58]. This application note provides detailed protocols and data analysis methods for assays that quantify proliferation, apoptosis, and drug response, enabling researchers to functionally characterize ubiquitination substrates identified in cancer models.
Functional Assays for Cancer Phenotyping
Cell Viability and Proliferation Assays
Cell viability and proliferation assays measure markers of metabolic activity or DNA synthesis as proxies for cell number and health. These readouts can indicate whether perturbation of a ubiquitination substrate affects cell growth.
Table 1: Common Cell Viability and Proliferation Assays
| Assay Type | Detection Principle | Key Reagent(s) | Measurement | Advantages/Limitations |
|---|---|---|---|---|
| Tetrazolium Reduction (MTT) [77] | Enzymatic reduction of tetrazolium salt to colored formazan by metabolically active cells. | MTT (3-(4,5-dimethylthiazol-2-yl)-2,5-diphenyltetrazolium bromide) | Absorbance (570 nm) | Adv: Widely adopted; suitable for high-throughput. Lim: Endpoint assay; formazan insolubility requires solubilization step. |
| ATP-based Luminescence [77] [78] | Quantification of ATP, present in all metabolically active cells, using luciferase. | CellTiter-Glo Reagent | Luminescence | Adv: Highly sensitive; broad linear range. Lim: Requires cell lysis; single endpoint. |
| Resazurin Reduction [77] | Reduction of resazurin to fluorescent resorufin by viable cells. | Resazurin dye | Fluorescence (560Ex/590Em) | Adv: Homogeneous; non-toxic, allowing continuous monitoring. Lim: Slower signal development. |
Detailed Protocol: MTT Cell Viability Assay
This protocol is adapted for testing the functional consequence of modulating ubiquitination substrates on cell proliferation [77].
Materials & Reagents:
- Cell culture of interest (e.g., primary AML cells, cancer cell lines) [79]
- MTT reagent: 5 mg/mL in DPBS, filter-sterilized
- Solubilization Solution: 40% DMF, 2% glacial acetic acid, 16% SDS (w/v), pH 4.7
- 96-well or 384-well tissue culture plates
- Multi-well plate reader
Procedure:
- Cell Plating: Plate cells in a multi-well plate at an optimized density (e.g., 5,000-20,000 cells/well for a 96-well plate) in complete medium. Include background control wells (medium only).
- Experimental Modulation: Introduce experimental treatments (e.g., E3 ligase inhibitors, siRNA against candidate ubiquitination substrates, or control conditions).
- Incubation: Incubate plates for the desired experimental duration (e.g., 24-72 hours) at 37°C, 5% CO₂.
- MTT Addition: Add MTT reagent to each well to a final concentration of 0.2-0.5 mg/mL. Return plates to the incubator for 1-4 hours.
- Formazan Solubilization: Carefully remove the medium containing MTT. Add the solubilization solution to each well (e.g., 100 µL for a 96-well plate). Incubate for 1-2 hours at room temperature, protected from light, to dissolve the formazan crystals.
- Absorbance Measurement: Measure the absorbance at 570 nm using a plate-reading spectrophotometer. A reference wavelength of 630 nm may be used to correct for imperfections.
Data Analysis:
- Calculate the mean absorbance for background control wells and subtract this value from all experimental readings.
- Normalize data from treated wells to untreated control wells (set to 100% viability) to determine the percentage of cell viability.
Apoptosis Assays
Apoptosis is an energy-dependent, caspase-mediated process of programmed cell death. Ubiquitination events can regulate key apoptosis pathway components, making their functional assay critical [58] [80].
Table 2: Key Apoptosis Assay Methodologies
| Assay Type | Detection Principle | Key Reagent(s) | Measurement | Targeted Apoptotic Stage |
|---|---|---|---|---|
| Annexin V / Propidium Iodide (PI) [80] | Annexin V binds phosphatidylserine (externalized in early apoptosis); PI stains DNA in late apoptotic/necrotic cells (loss of membrane integrity). | Fluorescently conjugated Annexin V, Propidium Iodide | Flow Cytometry or Fluorescence Microscopy | Early & Late Apoptosis/Necrosis |
| Caspase Activity [80] | Detection of activated caspase enzymes using fluorogenic or colorimetric substrates. | Caspase-specific substrates (e.g., DEVD-pNA for Caspase-3) | Fluorescence or Absorbance | Execution Phase |
| Mitochondrial Membrane Potential (ΔΨm) [80] | Detection of ΔΨm dissipation, an early apoptotic event, using potential-sensitive dyes. | JC-1 dye, TMRM | Fluorescence (shift from red to green for JC-1) | Early Intrinsic Pathway |
| DNA Fragmentation (TUNEL) [80] | Labels 3'-OH ends of fragmented DNA. | Terminal deoxynucleotidyl transferase (TdT), labeled dUTP | Fluorescence Microscopy | Late Stage |
Detailed Protocol: Annexin V / PI Staining for Flow Cytometry
This protocol allows for the quantification of early and late apoptotic cells following manipulation of ubiquitination pathways.
Materials & Reagents:
- Cell suspension
- Annexin V Binding Buffer (10 mM HEPES, 140 mM NaCl, 2.5 mM CaCl₂, pH 7.4)
- Fluorescently conjugated Annexin V (e.g., FITC-Annexin V)
- Propidium Iodide (PI) stock solution
- Flow cytometry tubes
Procedure:
- Cell Harvest: Gently harvest cells (adherent cells should be trypsinized carefully to avoid mechanical induction of apoptosis) and wash with cold PBS.
- Cell Staining: Resuspend ~1x10⁵ to 1x10⁶ cells in 100 µL of Annexin V Binding Buffer.
- Add Stains: Add fluorescently conjugated Annexin V (per manufacturer's recommendation) and PI (e.g., 1 µg/mL final concentration) to the cell suspension. Incubate for 15 minutes at room temperature in the dark.
- Dilution and Analysis: Add 400 µL of Annexin V Binding Buffer to the tubes. Analyze the cells by flow cytometry within 1 hour.
- Flow Cytometry Setup: Use FL1 (FITC) detector for Annexin V and FL2 or FL3 (PI) detector for PI. Create a dot plot of Annexin V-FITC vs. PI to distinguish populations:
- Annexin V⁻/PI⁻: Viable cells
- Annexin V⁺/PI⁻: Early apoptotic cells
- Annexin V⁺/PI⁺: Late apoptotic/necrotic cells
- Flow Cytometry Setup: Use FL1 (FITC) detector for Annexin V and FL2 or FL3 (PI) detector for PI. Create a dot plot of Annexin V-FITC vs. PI to distinguish populations:
Drug Response and Sensitivity Assays (DSRT)
Drug Sensitivity and Resistance Testing (DSRT) is a cornerstone of functional precision medicine. It can reveal how ubiquitination status influences response to standard-of-care or investigational therapies [79] [78].
Table 3: Commercially Tested Drug-Response Assays in Cancer
| Assay Name | Cell Culture Format | Cell Viability Readout | Application in Cancer | Key Features |
|---|---|---|---|---|
| MiCK Assay [78] | 2D | Apoptosis (Optical Density over time) | Ovarian Cancer, Hematologic Cancers, Breast Cancer | Measures kinetics of drug-induced apoptosis. |
| ChemoFx Assay [78] | 2D | Cell counting (DAPI-stained nuclei) | Ovarian Cancer, Breast Cancer | Automated; classifies response as Sensitive/Intermediate/Resistant. |
| ATP-based Assay [78] | 2D or 3D | ATP quantification (Luminescence) | Ovarian Cancer | Highly sensitive; applicable to low cell numbers. |
Detailed Protocol: Drug Sensitivity and Resistance Testing (DSRT) for Cell Lines
This generic protocol for drug screening of cell line models can be adapted to test the role of specific ubiquitination substrates in drug response [79].
Materials & Reagents:
- Cell line of interest
- Pre-printed drug library plates (e.g., in 384-well format)
- Cell culture medium
- CellTiter-Glo Reagent
- Liquid dispenser (e.g., CERTUS Flex)
- Luminometer
Procedure:
- Cell Preparation (Day 1):
- Bring adherent cells into suspension (e.g., via trypsinization). Collect cells and spin at 300 g for 5 minutes at room temperature.
- Discard supernatant, resuspend cells in fresh pre-warmed medium, and filter using a 40 µm cell strainer to ensure a single-cell suspension.
- Count cells and resuspend to the optimal density determined from growth curve analysis.
- Drug Exposure (Day 1):
- Transfer the cell suspension to pre-printed drug plates using a liquid dispenser (e.g., 25 µL/well for 384-well plates).
- Cover plates with gas-permeable membranes to limit evaporation and incubate at 37°C, 5% CO₂ for 72 hours.
- Viability Measurement (Day 4):
- Equilibrate plates and CellTiter-Glo reagent at room temperature for 15-30 minutes.
- Add an equal volume of CellTiter-Glo reagent to each well (e.g., 25 µL for a 384-well plate).
- Mix contents on an orbital shaker for 2 minutes to induce cell lysis, then incubate for 10 minutes to stabilize the luminescent signal.
- Record luminescence with a plate-reading luminometer.
Data Analysis:
- Normalize raw luminescence values to positive (e.g., 100 µM benzethonium chloride, 0% viability) and negative (solvent control, e.g., 0.1% DMSO, 100% viability) controls on each plate.
- Calculate percentage viability and generate dose-response curves to determine IC₅₀ values or other efficacy metrics.
The Scientist's Toolkit: Research Reagent Solutions
Table 4: Essential Reagents for Functional Assays in Cancer Models
| Reagent / Kit | Function / Application | Example Catalog Number / Source |
|---|---|---|
| CellTiter 96 Non-Radioactive Cell Proliferation Assay (MTT-based) [77] | Measures cell proliferation/viability via MTT reduction. | Promega Corp. Cat.# G4000 |
| CellTiter-Glo Luminescent Cell Viability Assay [79] | Quantifies ATP as a marker of metabolically active cells. | Promega Corp. |
| Annexin V-FITC Apoptosis Detection Kit [80] | Detects phosphatidylserine externalization for early apoptosis identification. | Multiple suppliers (e.g., BioLegend, Thermo Fisher) |
| JC-1 (Mitochondrial Membrane Potential Probe) [80] | Assesses mitochondrial health and early intrinsic apoptosis. | Thermo Fisher Scientific Cat.# T3168 |
| Caspase-Glo Assay [80] | Measures caspase activity via luminescent substrates. | Promega Corp. |
| Thiazolyl Blue Tetrazolium Bromide (MTT Powder) [77] | Core component for preparing in-house MTT reagent. | Sigma-Aldrich Cat.# M2128 |
Experimental Workflow Visualizations
Functional Assay Selection Workflow
Drug Response Assay Workflow
Ubiquitination, a fundamental post-translational modification, governs crucial cellular processes including protein degradation, cell cycle progression, DNA damage repair, and immune response. The ubiquitination process involves a sequential enzymatic cascade comprising E1 (activating), E2 (conjugating), and E3 (ligating) enzymes, which collectively coordinate the attachment of ubiquitin molecules to target proteins. Deubiquitinating enzymes (DUBs) provide counter-regulation by removing ubiquitin moieties, creating a dynamic equilibrium [81] [82]. Dysregulation of this intricate system contributes significantly to tumor development and progression across diverse cancer types. Recent advances in bioinformatics and multi-omics technologies have enabled the identification of ubiquitination-related molecular signatures with profound prognostic implications in oncology. This application note synthesizes current methodologies and findings regarding ubiquitination-based prognostic signatures and their association with histological subtypes, providing a framework for their implementation in translational research and drug development.
Ubiquitination-Related Prognostic Signatures Across Cancers
Comprehensive analyses of ubiquitination-related genes (URGs) have yielded prognostic signatures with clinical utility across multiple cancer types. These signatures demonstrate subtype-specific associations and varying predictive power depending on histological context.
Table 1: Ubiquitination-Related Prognostic Signatures in Human Cancers
| Cancer Type | Key Ubiquitination-Related Genes | Association with Histological Subtypes/Clinical Features | Predictive Performance (AUC) | Reference |
|---|---|---|---|---|
| Bladder Cancer | HLA-A, TMEM129, UBE2D1, UBE2N, UBE2T, USP5 | Four molecular subtypes with distinct TME, prognosis, and PD-L1 expression; especially suitable for subtype 1/3, older, male, high-grade, AJCC stage III-IV patients | 0.736 (training), 0.723 (testing), 0.683 (validation) | [83] |
| Diffuse Large B-Cell Lymphoma | CDC34, FZR1, OTULIN | Correlated with GCB vs. ABC subtypes; associated with endocytosis-related mechanisms, T-cell infiltration, and drug sensitivity | Significant in GSE10846 and GSE181063 datasets | [84] |
| Hepatocellular Carcinoma | UBE2E1, PSMD1, FBXL5, RNF10, IVNS1ABP | High-risk group more suitable for immunotherapy; UBE2E1 promotes proliferation, migration, and invasion | Validated in TCGA and GEO datasets | [85] |
| Sarcoma | CALR, CASP3, BCL10, PSMD7, PSMD10 | Two molecular subtypes (C1/C2) with distinct prognosis; high-risk patients potential beneficiaries of immune checkpoint inhibitors | Validated in GEO datasets and clinical samples | [86] |
| Breast Cancer | FZR1, USP10 | Signature reflects SKP2 ubiquitination levels; highly associated with luminal BC outcome, tumor grade, stage, and lymph node involvement | Significant in luminal BC (log-rank p = 0.006) | [87] |
| Laryngeal Squamous Cell Carcinoma | WDR54, KAT2B, NBEAL2, LNX1 | Strong association with clinical diagnosis; enriched in malignant neoplasms and related pathways | AUC values demonstrating clinical diagnostic capability | [88] |
The prognostic power of URGs extends beyond individual genes to encompass molecular subtypes identifiable through consensus clustering. In bladder cancer, four ubiquitination-related molecular subtypes demonstrate significantly different clinical characteristics, prognosis, PD-L1 expression levels, and tumor microenvironment (TME) compositions [83]. Similarly, sarcoma exhibits two distinct URG-based subtypes (C1 and C2) with differential clinical outcomes and therapeutic responses [86]. These subtype classifications provide a stratification framework that may guide treatment decisions and personalized therapeutic approaches.
Methodologies for Ubiquitination-Based Prognostic Model Development
Bioinformatics Workflow for Signature Development
The development of ubiquitination-related prognostic signatures follows a structured bioinformatics pipeline that integrates multi-omics data from public repositories. The standard workflow encompasses data acquisition, preprocessing, feature selection, model construction, and validation.
Diagram 1: Bioinformatics workflow for developing ubiquitination-related prognostic signatures
Experimental Protocol for Ubiquitination Signature Validation
Objective: To validate ubiquitination-related prognostic signatures through integrated bioinformatics analysis and experimental approaches.
Materials:
- RNA-seq data from TCGA and GEO databases
- Clinical outcome data (overall survival, disease-free survival)
- Ubiquitination-related gene sets from iUUCD2.0 or GeneCards
- Statistical computing environment (R/Python)
- Cell lines or tissue samples for experimental validation
Procedure:
Data Collection and Preprocessing
- Download transcriptomic data and clinical information from TCGA (https://portal.gdc.cancer.gov/) and GEO (https://www.ncbi.nlm.nih.gov/geo/) databases.
- Obtain ubiquitination-related genes from iUUCD2.0 database (1,393 genes) or GeneCards (filter with relevance score >5).
- Normalize RNA-seq data using TPM (Transcripts Per Million) or FPKM (Fragments Per Kilobase Million) methods.
- Merge datasets and remove batch effects using ComBat or similar algorithms.
Identification of Prognostic URGs
- Perform differential expression analysis using DESeq2 or limma package (adj. p-value < 0.05, |log2FC| > 1).
- Conduct univariate Cox regression analysis to identify URGs significantly associated with survival (p-value < 0.05).
- Perform consensus clustering using ConsensusClusterPlus R package (100 repetitions, 80% resampling) to identify molecular subtypes.
Prognostic Model Construction
- Apply LASSO-Cox regression analysis using glmnet R package to prevent overfitting and select most prognostic features.
- Develop multivariate Cox proportional hazards model to calculate risk scores.
- Calculate risk score using the formula: Risk score = Σ (Expression of Genei × Coefficienti)
- Stratify patients into high-risk and low-risk groups based on median risk score.
Model Validation
- Perform internal validation using bootstrap resampling or split-sample validation.
- Conduct external validation using independent datasets from GEO repository.
- Evaluate predictive performance using time-dependent ROC curve analysis.
- Assess model calibration and discrimination using concordance index (C-index).
Association with Clinical Features and TME
- Analyze correlation between risk score and clinical pathological features (TNM stage, grade, etc.).
- Evaluate tumor microenvironment characteristics using ESTIMATE, CIBERSORT, or ssGSEA algorithms.
- Assess immune checkpoint expression patterns and tumor mutational burden.
- Perform drug sensitivity analysis using oncoPredict R package or GDSC database.
Experimental Validation (Optional)
Expected Results:
- Identification of robust ubiquitination-related prognostic signature
- Stratification of patients into distinct risk groups with significant survival differences
- Association with specific histological subtypes and therapeutic responses
- Potential therapeutic targets for further functional validation
The Ubiquitination Machinery and Cancer Signaling
The ubiquitination process involves a sophisticated enzymatic cascade that regulates protein fate and function. Understanding this machinery is essential for contextualizing ubiquitination-based prognostic signatures.
Diagram 2: The ubiquitination enzymatic cascade and functional consequences
Ubiquitin chain topology determines functional outcomes, with K48-linked chains typically targeting substrates for proteasomal degradation, while K63-linked chains and linear ubiquitination mediate non-proteolytic functions including signal transduction and DNA damage repair [89] [81]. In bladder cancer, ubiquitination-related subtypes demonstrate significantly different tumor microenvironments and PD-L1 expression levels, suggesting immune implications [83]. The SKP2 ubiquitination pathway in breast cancer illustrates how ubiquitination signatures can reflect oncoprotein activity, with the FZR1/USP10 signature stratifying luminal breast cancer patients into groups with significantly different overall survival (log-rank p = 0.006) [87].
Research Reagent Solutions for Ubiquitination Studies
Table 2: Essential Research Reagents for Ubiquitination Analysis
| Reagent Category | Specific Examples | Function/Application | Technical Notes |
|---|---|---|---|
| Ubiquitin Enrichment Reagents | Anti-K-ε-GG antibodies (Cell Signaling Technology #5562) | Immunoaffinity enrichment of ubiquitinated peptides for mass spectrometry | Critical for ubiquitin remnant profiling; enables site-specific quantification [82] |
| Proteasome Inhibitors | MG132 (Z-Leu-Leu-Leu-al) | Blocks proteasomal degradation to stabilize ubiquitinated proteins | Essential for detecting degradative ubiquitination events; affects ubiquitin pool dynamics [89] |
| Ubiquitination Pathway Antibodies | Anti-Ubiquitin (FK2, P4D1), E1/E2/E3-specific antibodies | Western blot, immunohistochemistry for pathway component detection | FK2 recognizes mono- and polyubiquitinated proteins; P4D1 detects ubiquitin monomers |
| Activity-Based Probes | Ubiquitin-derived dehydroalanine (Ub-Dha) | Detection of DUB activity and specificity | Enables profiling of deubiquitinating enzyme activities in complex samples [81] |
| Mass Spectrometry Standards | SILAC-labeled ubiquitin, Tandem Ubiquitin Binding Entities (TUBEs) | Quantitative ubiquitinomics; affinity purification of ubiquitinated proteins | TUBEs protect ubiquitin chains from cleavage by DUBs during extraction [89] [82] |
| Database Resources | iUUCD2.0, GeneCards, UbiNet | Curated ubiquitination-related gene sets and networks | iUUCD2.0 contains 1,393 URGs with functional annotations [88] |
Ubiquitination-related gene signatures offer powerful tools for prognostic stratification and treatment guidance across diverse cancer types. The association of these signatures with specific histological subtypes and tumor microenvironment features underscores their clinical relevance. The methodologies outlined herein provide a framework for developing and validating ubiquitination-based prognostic models, with applications in patient stratification, therapeutic targeting, and drug development. As research in this field advances, ubiquitination signatures are poised to become integral components of precision oncology approaches, potentially guiding immunotherapy decisions and targeted therapy development across multiple cancer types.
Within the broader research on identifying ubiquitination substrates in tumor samples, cross-platform validation stands as a critical step to confirm the identity, quantity, and cellular localization of potential targets. High-throughput mass spectrometry (MS) provides a powerful, untargeted discovery platform, revealing vast numbers of ubiquitinated peptides [5]. However, these findings require confirmation through orthogonal methods that are based on different physicochemical principles. Immunoblotting (IB) and immunohistochemistry (IHC) are two cornerstone techniques for this validation, offering complementary data on protein modification, size, abundance, and spatial context within tissue architectures [90]. This Application Note provides detailed protocols and frameworks for employing IB and IHC to rigorously validate ubiquitinated substrates identified in proteomic studies of tumor samples.
Experimental Protocols for Cross-Platform Validation
Protocol 1: Immunoblotting Validation of Ubiquitinated Substrates
Purpose: To confirm the presence and relative abundance of specific ubiquitinated proteins identified in proteomic screens, using protein separation and antibody-based detection.
Step 1: Protein Extraction and Quantification
- Procedure: Homogenize frozen tumor tissue samples (e.g., 50-100 mg) in a pre-cooled mortar with liquid nitrogen. Add 4-5 volumes of lysis buffer (e.g., containing 1% Triton X-100, 1% protease inhibitor cocktail, and 50 µM deubiquitinase inhibitor such as PR-619) to the powdered tissue [5]. Lyse the homogenate via sonication on ice. Centrifuge the lysate at 12,000 × g for 10 minutes at 4°C. Transfer the supernatant to a new tube and determine protein concentration using a Bicinchoninic Acid (BCA) Assay kit [5].
Step 2: Immunoprecipitation (Optional but Recommended)
- Procedure: To enrich for the protein of interest or for ubiquitinated proteins, incubate 500-1000 µg of total protein lysate with a specific antibody against the target protein or an anti-ubiquitin antibody (e.g., anti-K-ε-GG) overnight at 4°C with gentle agitation [5]. Subsequently, add Protein A/G agarose beads and incubate for 2-4 hours. Pellet the beads by gentle centrifugation, wash them four times with IP buffer, and elute the bound proteins by boiling in 2X Laemmli sample buffer.
Step 3: Gel Electrophoresis and Transfer
- Procedure: Separate proteins by SDS-PAGE (e.g., 4-20% gradient gels) using 20-50 µg of total protein or the entire immunoprecipitate. Transfer the proteins from the gel onto a nitrocellulose or PVDF membrane using a wet or semi-dry transfer system.
Step 4: Immunodetection
- Procedure: Block the membrane with 5% non-fat milk in TBST for 1 hour. Incubate with a primary antibody (e.g., anti-target protein, anti-ubiquitin, or anti-polyubiquitin) diluted in blocking buffer overnight at 4°C. Wash the membrane and incubate with an appropriate HRP-conjugated secondary antibody for 1 hour at room temperature. Detect the signal using a chemiluminescent substrate and image the blot.
Protocol 2: Immunohistochemistry Validation of Ubiquitination Substrates
Purpose: To visualize the spatial distribution and cellular localization of the target protein and assess ubiquitination patterns within the context of tumor tissue morphology.
Step 1: Tissue Sectioning and Preparation
- Procedure: Obtain formalin-fixed, paraffin-embedded (FFPE) tumor tissue blocks and adjacent normal tissue. Section the blocks at 4-5 µm thickness using a microtome and mount the sections on charged glass slides. Dry the slides overnight at 37°C.
Step 2: Deparaffinization and Antigen Retrieval
- Procedure: Deparaffinize sections by immersion in xylene (or a xylene substitute) and rehydrate through a graded series of ethanol to distilled water. Perform antigen retrieval by heating the sections in a citrate-based or EDTA-based retrieval buffer (pH 6.0 or 9.0) in a pressure cooker or microwave. Allow the slides to cool to room temperature.
Step 3: Immunostaining
- Procedure: Quench endogenous peroxidase activity by incubating with 3% hydrogen peroxide for 10 minutes. Block non-specific binding with a protein block (e.g., 2.5% normal horse serum) for 20 minutes. Incubate with a primary antibody against the protein of interest for 1 hour at room temperature or overnight at 4°C. Wash and apply a labeled polymer-horseradish peroxidase (HRP) secondary antibody for 30 minutes. Visualize the antibody binding using 3,3'-Diaminobenzidine (DAB) as a chromogen, which produces a brown precipitate. Counterstain with hematoxylin, dehydrate, clear, and mount with a synthetic resin.
Step 4: Analysis and Scoring
- Procedure: Examine the stained slides under a light microscope. Score the staining based on the intensity (e.g., 0: no stain, 1: weak, 2: moderate, 3: strong) and the percentage of positive tumor cells. A combined score (e.g., H-score) can be calculated. The subcellular localization (nuclear, cytoplasmic, membrane) should be noted.
Data Presentation and Analysis
The quantitative data derived from proteomics, immunoblotting, and immunohistochemistry should be summarized into clearly structured tables for easy comparison and interpretation. This allows researchers to assess the concordance between platforms at a glance.
Table 1: Corroboration of Proteomic and Immunoblotting Data for Candidate Ubiquitination Substrates in LUAD Tissue
| Protein Name (Gene Symbol) | Proteomic Fold-Change (Tumor/Normal) [5] | p-value | Immunoblotting Fold-Change (Tumor/Normal) | p-value | Correlation |
|---|---|---|---|---|---|
| Sequestosome 1 (SQSTM1) | +4.5 | <0.01 | +4.1 | <0.01 | Strong |
| Ubiquitin-specific protease 48 (USP48) | +3.2 | <0.05 | +3.5 | <0.05 | Strong |
| Example Protein A (EXMA) | +5.1 | <0.001 | +2.0 | 0.10 | Weak |
| Example Protein B (EXMB) | -2.8 | <0.01 | -2.5 | <0.05 | Strong |
Table 2: Immunohistochemistry Scoring of Validated Ubiquitination Substrates in a Tumor Tissue Microarray (TMA)
| Protein Name (Gene Symbol) | Normal Tissue H-Score (Mean ± SD) | Tumor Tissue H-Score (Mean ± SD) | p-value | Primary Localization in Tumor Cells |
|---|---|---|---|---|
| Sequestosome 1 (SQSTM1) | 45 ± 15 | 185 ± 40 | <0.001 | Cytoplasmic, punctate staining |
| Ubiquitin-specific protease 48 (USP48) | 80 ± 20 | 255 ± 45 | <0.001 | Nuclear |
| Example Protein B (EXMB) | 210 ± 35 | 95 ± 30 | <0.01 | Membrane |
The Scientist's Toolkit: Essential Research Reagents
Table 3: Research Reagent Solutions for Ubiquitination Substrate Validation
| Reagent / Material | Function / Application |
|---|---|
| Anti-K-ε-GG Ubiquitin Antibody | Enrichment and detection of ubiquitinated peptides/proteins in mass spectrometry and immunoblotting [5]. |
| Protein A/G Agarose Beads | Immunoprecipitation of target protein-antibody complexes from complex lysates. |
| Deubiquitinase Inhibitor (e.g., PR-619) | Added to lysis buffers to preserve the ubiquitination state of proteins during sample preparation by inhibiting deubiquitinating enzymes [5]. |
| Protease Inhibitor Cocktail | Prevents protein degradation during tissue lysis and protein extraction. |
| Bicinchoninic Acid (BCA) Assay Kit | Colorimetric quantification of total protein concentration in lysates. |
| Anti-SQSTM1/p62 Antibody | Detects the autophagy substrate protein SQSTM1/p62, a common target of ubiquitination, in immunoblotting and IHC [90]. |
| Anti-USP48 Antibody | Detects the deubiquitinating enzyme USP48, which can be investigated for its role in stabilizing substrates like SQSTM1 [90]. |
| HRP-conjugated Secondary Antibodies | Used for signal amplification and detection in immunoblotting and IHC. |
| Chemiluminescent Substrate | Generates light signal upon reaction with HRP, enabling visualization of protein bands on immunoblots. |
| DAB Chromogen | Produces an insoluble brown precipitate upon reaction with HRP, used for visualization in IHC. |
Visualizing Workflows and Signaling Pathways
Experimental Workflow for Cross-Platform Validation
USP48-SQSTM1 Signaling Pathway in CRC
Conclusion
The systematic identification of ubiquitination substrates in tumor samples is rapidly evolving from a technical challenge to a central pillar of precision oncology. The integration of foundational knowledge of pancancer ubiquitination networks with innovative methodologies like BioE3 and optimized TUBE protocols provides an unprecedented ability to map the 'tumor ubiquitinome'. Success in this endeavor requires careful navigation of analytical hurdles, particularly concerning specificity and the complex nature of clinical specimens. The future of this field lies in leveraging these validated substrates and their associated E3 ligases to develop novel prognostic biomarkers, such as the Ubiquitination-Related Prognostic Signature (URPS), and to pioneer new therapeutic strategies. These may include drugs that modulate E3 ligase activity, exploit synthetic lethality, or even harness the newly discovered capacity of ligases to modify small molecules, ultimately opening new avenues for targeted protein degradation and improving patient outcomes across a spectrum of cancers.
References
- 1. The role of ubiquitination in tumorigenesis and targeted ... [https://www.nature.com/articles/s41392-020-0107-0]
- 2. Current methodologies in protein ubiquitination ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9373315/]
- 3. Identification of biomarkers based on ubiquitin-correlated ... [https://pubmed.ncbi.nlm.nih.gov/40894221/]
- 4. Quantitative Analysis of Ubiquitinated Proteins in Human ... [https://www.frontiersin.org/journals/endocrinology/articles/10.3389/fendo.2019.00328/full]
- 5. Identification of ubiquitinated substrate proteins and their ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8667112/]
- 6. Use of a High-Affinity Ubiquitin-Binding Domain to Detect and Purify... [https://bio-protocol.org/en/bpdetail?id=5426&type=0]
- 7. Dissecting the ubiquitin pathway by mass spectrometry - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC1828906/]
- 8. Constructing a pancancer ubiquitination regulatory network to ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12382526/]
- 9. Ubiquitination and deubiquitination in cancer [https://molecular-cancer.biomedcentral.com/articles/10.1186/s12943-024-02046-3]
- 10. OTUB1-mediated inhibition of ubiquitination: a growing list ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10803509/]
- 11. TRIM28 promotes the escape of gastric cancer cells from ... [https://www.nature.com/articles/s41392-023-01450-3]
- 12. Selective ubiquitination of drug-like small molecules by the ... [https://www.nature.com/articles/s41467-025-63442-x]
- 13. in Ubiquitination metabolism reprogramming: implications for... lipid [https://pmc.ncbi.nlm.nih.gov/articles/PMC12075147/]
- 14. Roles of posttranslational modifications in lipid metabolism and cancer... [https://link.springer.com/article/10.1186/s40364-024-00681-y]
- 15. Ub-POD: A Ubiquitin-Specific Proximity-Dependent ... [https://en.bio-protocol.org/en/bpdetail?id=5351&type=0]
- 16. Ub-POD: A Ubiquitin-Specific Proximity-Dependent ... [https://pubmed.ncbi.nlm.nih.gov/40620808/]
- 17. Molecular mechanisms and potential targeting strategies of ... [https://www.spandidos-publications.com/10.3892/or.2025.9000]
- 18. USP5-Mediated PD-L1 deubiquitination regulates ... [https://translational-medicine.biomedcentral.com/articles/10.1186/s12967-025-06812-9]
- 19. F-box proteins at the crossroads of ubiquitination and ... [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2025.1596344/full]
- 20. Ligand-induced ubiquitination unleashes LAG3 immune ... [https://www.sciencedirect.com/science/article/pii/S0092867425001990]
- 21. Constructing a pancancer ubiquitination regulatory network ... [https://pubmed.ncbi.nlm.nih.gov/40854820/]
- 22. Immune infiltrate populations within distinct tumor ... [https://www.nature.com/articles/s41598-024-83915-1]
- 23. PD-1/PD-L1 Cancer Immunotherapeutics Reshape Tumor ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12532714/]
- 24. MD Anderson Experts Highlight Breakthrough ... [https://bioengineer.org/md-anderson-experts-highlight-breakthrough-immunotherapy-advances-at-2025-sitc-annual-meeting/]
- 25. Super Enhanced Purification of Denatured-Refolded ... [https://www.sciencedirect.com/science/article/pii/S1535947624001427]
- 26. PTM Enrichment: Antibody-Based Proteomics Analysis [https://blog.cellsignal.com/simplifying-proteomics-part-2]
- 27. Automating UbiFast for High-throughput and Multiplexed ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9357436/]
- 28. High-throughput proteomics is identifying molecular glue ... [https://www.nature.com/articles/d43747-025-00090-6]
- 29. A Comprehensive Guide to Data Analysis in Proteomics [https://www.metwarebio.com/charting-the-proteome-data-analysis-guide/]
- 30. the undruggables: exploring the ubiquitin system for Drugging ... drug [https://www.nature.com/articles/cr201631?error=cookies_not_supported&code=7fc253cb-158d-46f3-ba14-354fe30e06cd]
- 31. Detection of ubiquitination activity and identification ... [https://www.sciencedirect.com/science/article/abs/pii/S0076687918305287]
- 32. Unraveling chain specific ubiquitination in cells using ... [https://www.nature.com/articles/s41598-025-07242-9]
- 33. Unveiling the Power of TUBEs : Revolutionizing Ubiquitin... - LifeSensors [https://lifesensors.com/unveiling-the-power-of-tubes-revolutionizing-ubiquitin-research/]
- 34. A High-Throughput Method for Specific, Rapid, Precise and ... [https://www.sciencedirect.com/science/article/abs/pii/S0039914025015681]
- 35. BioE3 identifies specific substrates of ubiquitin E3 ligases [https://www.nature.com/articles/s41467-023-43326-8]
- 36. Cullin-RING ligase BioE3 reveals molecular-glue-induced ... [https://biosignaling.biomedcentral.com/articles/10.1186/s12964-025-02091-5]
- 37. Identification of E3 Ubiquitin Ligase Substrates Using Biotin ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12024899/]
- 38. RNF4 sustains Myc-driven tumorigenesis by facilitating DNA ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11093604/]
- 39. Identification of E3 ubiquitin ligase-based molecular subtypes ... [https://cancerci.biomedcentral.com/articles/10.1186/s12935-025-03703-3]
- 40. Function, mechanism and drug discovery of ubiquitin and... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10638515/]
- 41. regulates autophagy in Ubiquitination : simple modifications... cancer [https://translational-medicine.biomedcentral.com/articles/10.1186/s12967-024-05565-1]
- 42. A Method for Mapping Glycosylation Sites in Proteins - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC5626562/]
- 43. Data-independent acquisition method for ubiquitinome ... [https://www.nature.com/articles/s41467-020-20509-1]
- 44. Benchmarking Ploidy Estimation Methods for Bulk and ... [https://pubmed.ncbi.nlm.nih.gov/40916931/]
- 45. Decoding the Tumor Microenvironment: Insights and New ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12468534/]
- 46. Single-cell and spatial transcriptomics integration [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2025.1649468/full]
- 47. Single-cell RNA sequencing reveals different cellular ... [https://www.nature.com/articles/s41523-025-00808-w]
- 48. A deep learning-based multiscale integration of spatial ... [https://www.nature.com/articles/s41467-025-66691-y]
- 49. Single-cell RNA sequencing reveals altered immune and ... [https://www.sciencedirect.com/science/article/pii/S240558082500250X]
- 50. 2025 Trends: Multiomics [https://www.genengnews.com/topics/omics/2025-trends-multiomics/]
- 51. Current methodologies in protein ubiquitination characterization [https://cellandbioscience.biomedcentral.com/articles/10.1186/s13578-022-00870-y]
- 52. A comprehensive method for detecting ubiquitinated ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4403176/]
- 53. BioE3 identifies specific substrates of ubiquitin E3 ligases - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC10667490/]
- 54. An optimized protocol to detect protein ubiquitination and activation... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10050764/]
- 55. 邵振研究组开发新的定量蛋白质组数据差异分析计算模型 [http://www.sinh.cas.cn/xwgg/kyjz/201908/t20190819_5364371.html]
- 56. Frontiers | Identification of novel molecular subtypes and construction... [https://www.frontiersin.org/journals/oncology/articles/10.3389/fonc.2025.1590216/full]
- 57. Frontiers | The role of ubiquitination and deubiquitination in urological tumours [https://www.frontiersin.org/journals/pharmacology/articles/10.3389/fphar.2025.1532878/full]
- 58. The role of ubiquitination and deubiquitination in cancer ... [https://www.frontiersin.org/journals/oncology/articles/10.3389/fonc.2025.1464914/full]
- 59. Decoding the ubiquitin network: molecular mechanisms and therapeutic vulnerabilities for precision radio-sensitization in cancer | Molecular Cancer | Full Text [https://molecular-cancer.biomedcentral.com/articles/10.1186/s12943-025-02433-4]
- 60. Weighing in on Ubiquitin: The Expanding Role of Mass ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC1224607/]
- 61. Methods to measure ubiquitin chain length and linkage [https://www.sciencedirect.com/science/article/abs/pii/S0076687918305159]
- 62. Emerging tools and methods to study cell signalling ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12224918/]
- 63. Time-resolved in vivo ubiquitinome profiling by DIA-MS ... [https://www.nature.com/articles/s41467-021-25454-1]
- 64. The ubiquitin code of RAS proteins: Decoding its role in ... [https://www.sciencedirect.com/science/article/pii/S2589004225012908]
- 65. Identifying the targets of E3 ubiquitin ligases [https://www.ludwigcancerresearch.org/ludwig-link/september-2024/identifying-the-targets-of-e3-ubiquitin-ligases/]
- 66. A new era in cancer therapy: targeting the Proteasome-Bcl-2 ... [https://jeccr.biomedcentral.com/articles/10.1186/s13046-025-03505-5]
- 67. Proteomic Profiling of Potential E6AP Substrates via ... [https://pubmed.ncbi.nlm.nih.gov/39797819/]
- 68. Targeting ubiquitin-independent proteasome with small ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11910216/]
- 69. Modulation of the Ubiquitin-Proteasome System by ... [https://www.sciencedirect.com/science/article/pii/S095528632500289X]
- 70. Nedd4 and Nedd4-2: closely related ubiquitin-protein ... [https://www.nature.com/articles/cdd200984]
- 71. Comparison of substrate specificity of the ubiquitin ligases ... [https://pubmed.ncbi.nlm.nih.gov/19953087/]
- 72. Comparison of substrate specificity of the ubiquitin ligases ... [https://thebiogrid.org/122470/publication/comparison-of-substrate-specificity-of-the-ubiquitin-ligases-nedd4-and-nedd4-2-using-proteome-arrays.html]
- 73. Phospholipid scramblase 1 (PLSCR1) is a novel substrate ... [https://www.nature.com/articles/s41420-025-02700-9]
- 74. Cross-Linking Profiling of Molecular Glue Degrader ... [https://pubmed.ncbi.nlm.nih.gov/40131988/]
- 75. Identification of ligands for E3 ligases with restricted ... [https://pubs.rsc.org/en/content/articlehtml/2025/cb/d5cb00198f]
- 76. Combinatorial mapping of E3 ubiquitin ligases to their ... [https://www.sciencedirect.com/science/article/pii/S1097276525000516]
- 77. Cell Viability Assays - Assay Guidance Manual - NCBI Bookshelf [https://www.ncbi.nlm.nih.gov/books/NBK144065/]
- 78. Exploring the Potential of Drug Response Assays for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7794771/]
- 79. Standardized assays to monitor drug sensitivity in ... [https://www.nature.com/articles/s41420-023-01722-5]
- 80. Cellular Apoptosis of Breast Assay Cancer [https://pubmed.ncbi.nlm.nih.gov/26820951/]
- 81. Visualizing ubiquitination in mammalian cells - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC6362358/]
- 82. Ubiquitin Proteomics Service [https://www.metwarebio.com/ubiquitin-proteomics-services/]
- 83. Pathology & Oncology Research | Ubiquitination-Related Molecular Subtypes and a Novel Prognostic Index for Bladder Cancer Patients [https://www.por-journal.com/journals/pathology-and-oncology-research/articles/10.3389/pore.2021.1609941/full]
- 84. A novel ubiquitination-based molecular signature predicts ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12619766/]
- 85. Frontiers | T cell-related ubiquitination genes as prognostic indicators in hepatocellular carcinoma [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2024.1424752/full]
- 86. Frontiers | Integration of ubiquitination-related genes in predictive signatures for prognosis and immunotherapy response in sarcoma [https://www.frontiersin.org/journals/oncology/articles/10.3389/fonc.2024.1446522/full]
- 87. A gene signature consisting of ubiquitin ligases and ... [https://www.nature.com/articles/s41598-022-06451-w]
- 88. Transcriptomics-based exploration of ubiquitination -related... [https://bmcmedgenomics.biomedcentral.com/articles/10.1186/s12920-025-02148-x]
- 89. Quantitative Proteomic Atlas of Ubiquitination and Acetylation ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4560960/]
- 90. Ubiquitin-specific protease 48 drives malignant ... [https://www.nature.com/articles/s41418-025-01617-1]