Proteasome Inhibition and Ubiquitin Homeostasis: Mechanisms, Measurement, and Clinical Implications in Disease Therapy
This article provides a comprehensive analysis of how proteasome inhibition directly impacts cellular ubiquitin levels and dynamics, a critical consideration in both basic research and drug development.
Proteasome Inhibition and Ubiquitin Homeostasis: Mechanisms, Measurement, and Clinical Implications in Disease Therapy
Abstract
This article provides a comprehensive analysis of how proteasome inhibition directly impacts cellular ubiquitin levels and dynamics, a critical consideration in both basic research and drug development. We explore the foundational principles of the ubiquitin-proteasome system (UPS), detailing the enzymatic cascade from E1 activation to E3 ligase-mediated substrate targeting. Methodological sections cover established and emerging techniques for quantifying ubiquitination and proteasome activity, including reporter constructs and mass spectrometry-based approaches. The content addresses common experimental challenges, such as distinguishing specific from global protein degradation and interpreting ubiquitin chain linkages. Finally, we validate these concepts with clinical and commercial data on proteasome inhibitors, examining their efficacy, adverse event profiles, and the growing market driven by their application in hematologic cancers. This resource is tailored for researchers, scientists, and drug development professionals seeking to deepen their understanding of UPS modulation.
The Ubiquitin-Proteasome System: Core Machinery and Consequences of Inhibition
The ubiquitin conjugation cascade represents a crucial enzymatic pathway for post-translational modification, directing cellular proteins toward degradation or functional alteration. This E1-E2-E3 enzyme cascade enables precise targeting of substrates through a coordinated mechanism of ubiquitin activation, conjugation, and ligation. Within proteasome inhibition research, understanding this cascade is fundamental, as inhibited proteasomes cause accumulation of polyubiquitinated proteins, depleting free ubiquitin pools and disrupting protein homeostasis. This technical guide examines the molecular mechanisms of ubiquitin transfer, experimental methodologies for studying ubiquitination, and the cascade's integration with proteasome function, providing researchers with essential tools for investigating ubiquitin-proteasome system dynamics.
The ubiquitin-proteasome system (UPS) constitutes the primary pathway for targeted intracellular protein degradation in eukaryotic cells, operating through a highly regulated process that involves tagging proteins with ubiquitin for proteasomal destruction [1]. This system controls the degradation of over 80% of cellular proteins, including short-lived, misfolded, and damaged proteins, thereby maintaining cellular homeostasis [2]. The UPS encompasses two major components: the ubiquitin conjugation cascade that marks substrates, and the 26S proteasome that executes degradation.
Ubiquitin itself is a small, 76-amino acid protein (8.6 kDa) that is highly conserved across eukaryotes and ubiquitously expressed in most tissues [3]. Its name derives from this ubiquitous distribution. The ubiquitin protein features seven lysine residues (K6, K11, K27, K29, K33, K48, and K63) and an N-terminal methionine (M1) that serve as potential linkage sites for polyubiquitin chain formation [2]. The modification of proteins with ubiquitin involves the covalent attachment of ubiquitin to target proteins, most commonly through an isopeptide bond between ubiquitin's C-terminal glycine (Gly76) and the ε-amino group of a lysine residue on the substrate protein [4].
The 26S proteasome is a 2.5 MDa multi-subunit complex that recognizes and degrades polyubiquitinated proteins [5]. It consists of a 20S catalytic core particle capped by one or two 19S regulatory particles. The 20S core contains three primary proteolytic activities: chymotrypsin-like (cleavage after hydrophobic residues), caspase-like (cleavage after acidic residues), and trypsin-like (cleavage after basic residues) [1]. The 19S regulatory cap recognizes ubiquitinated proteins, unfolds them, and translocates them into the catalytic core for degradation [1].
In the context of proteasome inhibition research, understanding the ubiquitin conjugation cascade is paramount. When proteasome function is compromised, polyubiquitinated proteins accumulate, leading to depletion of free ubiquitin pools and disruption of protein homeostasis—a cellular state with significant implications for cancer therapy and neurodegenerative disease [6]. This review comprehensively examines the enzymatic cascade responsible for ubiquitin conjugation, with particular emphasis on its relevance to proteasome inhibition studies.
The Ubiquitin Conjugation Cascade: Mechanism and Key Enzymes
The ubiquitin conjugation cascade comprises three sequential enzymatic steps that activate and transfer ubiquitin to substrate proteins. This pathway involves ubiquitin-activating enzymes (E1), ubiquitin-conjugating enzymes (E2), and ubiquitin ligases (E3), working in concert to ensure specific substrate targeting [5]. The hierarchical nature of this cascade—with few E1s, more E2s, and hundreds of E3s—allows for precise regulation of the ubiquitination machinery while enabling diverse substrate recognition [3].
E1: Ubiquitin-Activating Enzyme
The initial step in the ubiquitin cascade involves ubiquitin activation by E1 enzymes in an ATP-dependent process [7]. This reaction occurs through a two-step mechanism: first, ubiquitin is adenylated, then transferred to the active-site cysteine of E1 to form a ubiquitin-E1 thioester bond [3]. During this process, the E1 enzyme catalyzes the acyl-adenylation of the C-terminus of ubiquitin, followed by trans-thioesterification that links ubiquitin to the E1 cysteine sulfhydryl group via a high-energy thioester bond [3].
The human genome encodes only two E1 enzymes capable of activating ubiquitin: UBA1 and UBA6 [3]. This limited repertoire contrasts with the expanding number of downstream enzymes, reflecting E1's role as the central entry point for ubiquitin activation. The E1 enzyme must recognize and interact with all downstream E2 conjugating enzymes, necessitating both specificity and versatility in its function.
E2: Ubiquitin-Conjugating Enzyme
Following ubiquitin activation, the ubiquitin moiety is transferred from E1 to the active-site cysteine of an E2 conjugating enzyme, again forming a thioester linkage [8]. This trans-thioesterification reaction requires the E2 to bind both activated ubiquitin and the E1 enzyme [3]. The human genome encodes approximately 35 E2 enzymes, each characterized by a highly conserved ubiquitin-conjugating (UBC) catalytic domain fold [3] [8].
E2 enzymes demonstrate varying specificity for different E3 ligases and substrates, contributing to the diversity of ubiquitination outcomes. Some E2s specialize in building specific ubiquitin chain types, while others collaborate with particular E3 families. The table below summarizes key E2 enzymes and their characteristics:
Table 1: Selected Human Ubiquitin-Conjugating Enzymes (E2s)
| Gene Name | Synonyms | Protein Length (aa) | Ubiquitin-Loading Capacity | Primary Function |
|---|---|---|---|---|
| UBE2A | RAD6A | 152 | Yes | Ubiquitylation |
| UBE2D1 | UBCH5A | 147 | Yes | Ubiquitylation |
| UBE2L3 | UBCH7 | 154 | Yes | Ubiquitylation |
| UBE2N | UBC13 | 152 | Yes | K63-linked chains |
| UBE2S | E2-EPF | 225 | Yes | Ubiquitylation |
| CDC34 | UBE2R1 | 236 | Yes | Cell cycle regulation |
E3: Ubiquitin Ligase
The final step in the cascade involves E3 ubiquitin ligases, which facilitate the transfer of ubiquitin from E2 to substrate proteins [2]. E3s serve as matchmakers that recognize specific substrates and bring them into proximity with ubiquitin-charged E2s, enabling ubiquitin transfer [4]. With over 600 members in humans, E3 ligases provide the primary determinant of substrate specificity in the ubiquitin system [2].
E3 ligases are categorized into several families based on their structural features and mechanisms of action:
RING-type E3 ligases constitute the largest family, characterized by a Really Interesting New Gene (RING) domain that binds E2s [2]. Unlike other E3 types, RING E3s catalyze the direct transfer of ubiquitin from E2 to substrate without forming a covalent E3-ubiquitin intermediate [2]. Multi-subunit cullin-RING ligases (CRLs) represent an important subclass that utilize cullin scaffolds to bring together substrate-recognition modules and RING domain proteins [2].
HECT-type E3 ligases contain a Homologous to E6-AP C-Terminus (HECT) domain that forms a thioester intermediate with ubiquitin before transferring it to substrates [2] [7]. These enzymes first accept ubiquitin from E2 onto their active-site cysteine before catalyzing substrate ubiquitination. The NEDD4 family of HECT E3s contains WW domains that mediate protein-protein interactions and C2 domains involved in membrane targeting [2].
RBR-type E3 ligases (RING-Between-RING) utilize a hybrid mechanism, combining features of both RING and HECT E3s [2]. They contain two RING domains with an intermediate domain, and like HECT E3s, form a thioester intermediate with ubiquitin before substrate transfer.
Table 2: Major E3 Ubiquitin Ligase Families
| E3 Family | Transfer Mechanism | Representative Members | Key Features |
|---|---|---|---|
| RING | Direct transfer from E2 to substrate | MDM2, CBL, APC/C | Largest E3 family; functions as scaffolding proteins |
| HECT | Via E3-ubiquitin thioester intermediate | NEDD4, HERC, E6AP | C-terminal catalytic HECT domain; diverse N-terminal domains for substrate recognition |
| RBR | Via E3-ubiquitin thioester intermediate | HOIP, HOIL-1, PARKIN | Two RING domains with intermediate region; hybrid mechanism |
The sequential action of E1-E2-E3 enzymes results in the covalent attachment of ubiquitin to substrate proteins. Additional ubiquitin molecules can then be added to the first ubiquitin, forming polyubiquitin chains with diverse functions based on their linkage types [2].
Experimental Methods for Studying Ubiquitination
Investigating the ubiquitin conjugation cascade requires specialized methodologies to detect ubiquitinated proteins, analyze degradation kinetics, and identify specific ubiquitination sites. This section details key experimental protocols used in ubiquitination research, particularly relevant to studying the effects of proteasome inhibition on cellular ubiquitin levels.
Detecting Protein Ubiquitination
Ubiquitin Enrichment and Western Blotting: To determine if a specific protein of interest (POI) has been ubiquitinated, researchers commonly employ co-immunoprecipitation (co-IP) followed by Western blot analysis [5]. The protocol involves:
- Treating cells with proteasome inhibitors (e.g., MG132, bortezomib) to accumulate ubiquitinated proteins by blocking their degradation [5].
- Lysing cells under denaturing conditions to preserve ubiquitin-substrate conjugates and prevent deubiquitination.
- Immunoprecipitating the POI using a specific antibody.
- Separating immunoprecipitated proteins by SDS-PAGE and transferring to membranes.
- Probing with anti-ubiquitin antibodies to detect ubiquitin conjugates of the POI.
This approach allows researchers to confirm whether their protein of interest has been ubiquitinated and to observe changes in ubiquitination status under different experimental conditions, such as proteasome inhibition.
High-Throughput Ubiquitination Assays: For screening applications, LanthaScreen conjugation assay reagents enable monitoring ubiquitin conjugation rates or extent in a high-throughput format [5]. These assays utilize time-resolved fluorescence resonance energy transfer (TR-FRET) to quantitatively measure ubiquitination in vitro, facilitating rapid screening of compounds that modulate E1-E2-E3 activity.
Analyzing Polyubiquitinated Proteins
Ubiquitin Enrichment Kits: Commercial ubiquitin enrichment kits employ high-affinity resins to isolate polyubiquitinated proteins from cell or tissue lysates [5]. The basic protocol includes:
- Preparing cell lysates in appropriate buffers.
- Incubating lysates with ubiquitin-binding resins.
- Washing away non-specifically bound proteins.
- Eluting bound polyubiquitinated proteins for downstream analysis.
- Detecting specific proteins of interest by Western blotting with target-specific antibodies.
This method provides a global view of polyubiquitinated proteins and can be used to monitor changes in the ubiquitinome in response to proteasome inhibition.
Tandem Mass Tag (TMT) Proteomics: For comprehensive, quantitative analysis of protein ubiquitination, tandem mass tag labeling combined with mass spectrometry enables large-scale ubiquitinome profiling [5]. This approach allows simultaneous measurement of ubiquitination changes across thousands of proteins in multiple samples, providing systems-level insights into UPS dynamics.
Monitoring Protein Degradation
Pulse-Chase Analysis: To measure protein degradation kinetics, pulse-chase experiments track the fate of radiolabeled or tagged proteins over time [5]. The standard protocol involves:
- "Pulsing" cells with labeled amino acids (e.g., 35S-methionine/cysteine) or methionine analogs for a defined period.
- Replacing the labeling medium with excess unlabeled amino acids ("chase").
- Harvesting cells at various time points during the chase period.
- Immunoprecipitating the protein of interest and quantifying remaining labeled protein.
Click-iT Plus technology provides a non-radioactive alternative using methionine analogs with click chemistry tags for fluorescence detection [5]. This approach enables real-time measurement of protein synthesis and degradation in live cells.
Global Protein Degradation Assessment: To distinguish targeted degradation of specific proteins from general proteolysis, researchers can measure overall protein degradation rates using radioactive pulse-chase methodology [5]. Monitoring the release of acid-soluble radioactivity from pre-labeled cellular proteins over time provides an assessment of global protein turnover.
Experimental Workflow for Ubiquitination Studies
The Scientist's Toolkit: Essential Research Reagents
Studying the ubiquitin conjugation cascade requires specialized reagents and tools. The following table compiles essential research materials for investigating ubiquitination mechanisms, particularly in the context of proteasome inhibition research.
Table 3: Research Reagent Solutions for Ubiquitination Studies
| Reagent Category | Specific Examples | Function/Application |
|---|---|---|
| Proteasome Inhibitors | MG132, Bortezomib (PS-341), Carfilzomib | Block proteasomal degradation, causing accumulation of ubiquitinated proteins for detection and analysis [5]. |
| E1 Enzyme Inhibitors | PYR-41, TAK-243 | Inhibit ubiquitin activation, blocking the entire ubiquitination cascade for mechanistic studies [1]. |
| Ubiquitin Antibodies | Anti-ubiquitin, Anti-polyubiquitin, Anti-K48/K63-linkage specific | Detect ubiquitinated proteins in Western blot, immunofluorescence, and immunoprecipitation applications [5]. |
| E2 Enzyme Assays | Recombinant E2 enzymes (UBE2D, UBE2L3, UBE2N) | In vitro ubiquitination assays to study E2 specificity and function [8]. |
| E3 Expression Constructs | Plasmids encoding RING, HECT, RBR E3 ligases | Overexpression or knockdown of specific E3s to identify substrates and study mechanisms [2]. |
| Deubiquitinase Inhibitors | PR-619, P5091, G5 | Block deubiquitinating enzymes to stabilize ubiquitin signals and study ubiquitination dynamics [5]. |
| Ubiquitin Enrichment Kits | Agarose-tandem ubiquitin-binding entities (TUBEs) | Isolate and purify polyubiquitinated proteins from complex lysates for proteomic analysis [5]. |
| Activity Assay Kits | LanthaScreen ubiquitination assays | High-throughput screening for modulators of E1-E2-E3 activity using TR-FRET technology [5]. |
| Cell Lines | HEK293, HCT116, specialized ubiquitin-reporters | Model systems for studying ubiquitination in cellular contexts, including reporter lines with engineered degradation signals. |
| Mass Spectrometry Reagents | Tandem Mass Tags (TMT), ubiquitin remnant motifs | Quantitative proteomics to identify ubiquitination sites and quantify changes in ubiquitinome [5]. |
These reagents enable researchers to dissect specific components of the ubiquitin cascade and investigate how proteasome inhibition affects ubiquitin dynamics. For instance, combining proteasome inhibitors with ubiquitin enrichment techniques allows comprehensive mapping of accumulated ubiquitinated proteins under proteasome stress conditions [5] [6].
Ubiquitin Conjugation in the Context of Proteasome Inhibition Research
The relationship between the ubiquitin conjugation cascade and proteasome function is fundamental to cellular homeostasis. When proteasomes are inhibited, the careful balance between ubiquitination and deubiquitination is disrupted, leading to profound cellular consequences. Understanding this relationship is crucial for both basic research and therapeutic development.
Interplay Between Ubiquitination and Proteasome Function
The ubiquitin conjugation cascade and the proteasome operate in a tightly coordinated manner. Under normal conditions, polyubiquitinated proteins are rapidly recognized and degraded by the 26S proteasome, with ubiquitin molecules recycled for reuse [5]. This continuous cycle maintains free ubiquitin pools and prevents accumulation of ubiquitinated proteins.
When proteasome activity is compromised—whether through pharmacological inhibition, genetic manipulation, or pathological conditions—this equilibrium is disturbed. The immediate effect is accumulation of polyubiquitinated proteins, as the degradation endpoint is blocked while ubiquitination continues [1] [5]. This accumulation has two significant consequences: sequestration of ubiquitin into stalled conjugates, and activation of compensatory cellular responses.
Research has demonstrated that human cancer cells often possess elevated proteasome activity and show heightened sensitivity to proteasome inhibitors compared to normal cells [1]. This differential sensitivity forms the basis for therapeutic applications of proteasome inhibitors in oncology, particularly for hematological malignancies.
Cellular Response to Ubiquitin Stress
Cells mount specific adaptive responses when ubiquitin homeostasis is disrupted. Unlike proteasome stress, which upregulates proteasome biogenesis, ubiquitin stress triggers alternative compensatory mechanisms [6]. A key finding is that ubiquitin depletion does not increase proteasome abundance but instead alters proteasome composition by enhancing association with the deubiquitinating enzyme Ubp6 (USP14 in mammals) [6].
This compositional change improves ubiquitin recycling efficiency from proteasome-bound substrates, sparing ubiquitin from degradation and replenishing free ubiquitin pools. The adaptation represents a sophisticated feedback mechanism that optimizes ubiquitin usage under stress conditions. Understanding this response is particularly relevant for cancer therapy, as prolonged proteasome inhibitor treatment may induce resistance through such adaptive mechanisms.
Ubiquitin- Proteasome Dynamics Under Inhibition
Therapeutic Implications and Research Applications
The intimate connection between the ubiquitin conjugation cascade and proteasome function has significant therapeutic implications. Proteasome inhibitors like bortezomib, carfilzomib, and ixazomib are established cancer therapies that exploit the dependence of certain malignancies on efficient proteasome function [1]. These compounds create an imbalance in protein homeostasis that preferentially kills cancer cells.
More recently, researchers have developed complementary strategies that target earlier steps in the ubiquitin pathway. These include:
- Inhibitors of E1 enzymes to globally block ubiquitin activation
- Specific E3 modulators to target individual substrates for stabilization or degradation
- PROTACs (Proteolysis-Targeting Chimeras) that hijack E3 ligases to degrade target proteins of interest [2]
For researchers studying proteasome inhibition, monitoring the ubiquitin conjugation cascade provides crucial insights into mechanism of action and resistance patterns. Assaying changes in E1, E2, and E3 activities; quantifying ubiquitin pool dynamics; and profiling the ubiquitinome under treatment conditions all contribute to a comprehensive understanding of how cells respond to proteasome stress.
The ubiquitin conjugation cascade comprising E1, E2, and E3 enzymes represents a sophisticated biological system for targeted protein modification and degradation. Its precise molecular mechanisms—from ubiquitin activation through E1, conjugation via E2, and substrate-specific ligation by E3s—enable exquisite control over protein fate. In the context of proteasome inhibition research, understanding this cascade is paramount, as disrupted equilibrium between ubiquitination and degradation triggers profound cellular stress responses with important implications for disease therapy.
The experimental methodologies and research tools detailed in this guide provide scientists with robust approaches for investigating ubiquitination mechanisms, particularly under conditions of proteasome impairment. As research advances, deepening our knowledge of the ubiquitin conjugation cascade will continue to illuminate cellular homeostasis mechanisms and reveal new therapeutic opportunities for manipulating protein degradation pathways.
The 26S proteasome serves as the central proteolytic machine in eukaryotic cells, responsible for the regulated degradation of the vast majority of intracellular proteins [9] [10]. As the endpoint of the ubiquitin-proteasome system (UPS), it controls vital processes ranging from cell cycle progression and signal transduction to stress response and general protein homeostasis [9] [11]. Understanding its intricate structure and mechanistic function is fundamental to biomedical research, particularly in the context of drug development, where the proteasome has emerged as a validated therapeutic target. This whitepaper provides an in-depth technical examination of the 26S proteasome, with its content framed specifically to support research on how proteasome inhibition impacts cellular ubiquitin levels and proteostasis.
Architectural Organization of the 26S Proteasome
The 26S proteasome is a ∼2.5 MDa complex consisting of two primary subcomplexes: the 20S core particle (CP) and the 19S regulatory particle (RP), with the RP often capping one or both ends of the CP [9] [12] [10].
The 20S Core Particle (CP)
The 20S CP is a barrel-shaped structure composed of 28 subunits arranged in four stacked heptameric rings [12] [10]. The configuration of these rings follows an α-β-β-α pattern. The two outer α-rings, formed by subunits α1-α7, function as a tightly regulated gate, controlling substrate access to the proteolytic chamber [10]. The N-terminal tails of specific α-subunits form a constricted pore that prevents unregulated entry of native proteins [10]. The two inner β-rings, formed by subunits β1-β7, house the proteolytic active sites. Three of these β-subunits—β1 (caspase-like activity), β2 (trypsin-like activity), and β5 (chymotrypsin-like activity)—contain N-terminal threonine residues that confer the proteasome's distinct peptidase activities [12] [10].
Table 1: Catalytic Subunits of the 20S Core Particle
| Subunit | Proteolytic Activity | Catalytic Residue | Primary Cleavage Preference |
|---|---|---|---|
| β1 | Caspase-like | N-terminal Threonine | Acidic residues |
| β2 | Trypsin-like | N-terminal Threonine | Basic residues |
| β5 | Chymotrypsin-like | N-terminal Threonine | Hydrophobic residues |
The 19S Regulatory Particle (RP)
The 19S RP is a multifunctional complex that identifies, prepares, and translocates ubiquitinated substrates into the 20S CP [9] [10]. It is further divided into two subcomplexes: the base and the lid.
The base subcomplex comprises:
- Six AAA-ATPase subunits (Rpt1-Rpt6): Form a heterohexameric ring that uses ATP hydrolysis to unfold substrates and translocate them into the 20S CP [9] [13].
- Three non-ATPase subunits (Rpn1, Rpn2, Rpn13): Rpn1 and Rpn13 function as primary ubiquitin receptors, while Rpn2 serves as a structural scaffold [9] [12].
The lid subcomplex consists of nine non-ATPase subunits (Rpn3, Rpn5-Rpn9, Rpn11, Rpn12, and Sem1) [9] [10]. A crucial component is Rpn11, a Zn²⁺-dependent deubiquitinase (DUB) that catalyzes the en bloc removal of ubiquitin chains from substrates prior to their degradation [9] [13].
Additionally, the proteasome harbors other important subunits not strictly confined to the base or lid. Rpn10 is a ubiquitin receptor that bridges the two subcomplexes [9] [12]. Two associated DUBs, Usp14 (Ubp6 in yeast) and Uch37, bind to Rpn1 and Rpn13, respectively, and function in editing ubiquitin chains and recycling ubiquitin [9] [14].
Functional Mechanism of Substrate Degradation
The degradation of a protein by the 26S proteasome is a multistep, ATP-dependent process that requires precise coordination between the RP and CP.
Substrate Recognition and Ubiquitin Sensing
Most proteasome substrates are marked for degradation by covalent attachment of a polyubiquitin chain, typically linked through lysine 48 (K48) of ubiquitin [15]. The proteasome contains multiple ubiquitin receptors—Rpn1, Rpn10, and Rpn13—that recognize these chains, providing redundancy and versatility in substrate engagement [9] [12]. This multi-receptor system allows the proteasome to handle a vast and diverse array of ubiquitinated proteins.
Conformational Dynamics and Substrate Commitment
The 26S proteasome is a highly dynamic machine that exists in several conformational states. Key states include the resting state (s1 or RS) and multiple processing states (s3/s4 or PS) [9] [13].
- In the resting state, the substrate entrance channel is accessible, but the gate to the 20S CP is closed, and the ATPase motor is inactive.
- Upon ubiquitin binding and substrate engagement, the proteasome undergoes a major conformational change to a processing state. This involves rotation of the lid subcomplex, a shift of Rpn11 to a central position above the ATPase pore, and opening of the 20S CP gate [13]. This state is primed for processive substrate translocation.
These conformational changes represent a critical substrate commitment step, ensuring that only properly engaged proteins are degraded and preventing nonspecific proteolysis [9] [11].
Deubiquitination, Unfolding, and Translocation
Once committed, the substrate is processed through coordinated actions:
- Deubiquitination: The Rpn11 deubiquitinase, positioned directly above the ATPase pore, removes the entire ubiquitin chain from the substrate en bloc just before the polypeptide is translocated into the ATPase motor [9] [13]. This coupling ensures the bulky ubiquitin chain does not enter the degradation chamber and allows for ubiquitin recycling.
- Unfolding and Translocation: The Rpt1-Rpt6 AAA-ATPase hexamer uses the energy from ATP hydrolysis to mechanically unfold the substrate protein. Recent cryo-EM studies have revealed that the ATPase subunits adopt a spiral-staircase arrangement around the substrate polypeptide [13]. Conserved pore loops in the central channel of the ring engage the substrate and, through a concerted "hand-over-hand" mechanism, apply mechanical force to unfold the protein and translocate the unfolded polypeptide into the 20S CP for degradation [13].
Research Toolkit: Methods for Studying Proteasome Function
This section outlines key experimental methodologies for investigating proteasome structure, function, and the effects of its inhibition.
Structural Analysis by Cryo-Electron Microscopy (Cryo-EM)
Protocol Overview: The application of single-particle cryo-EM has been instrumental in elucidating the conformational landscape of the 26S proteasome.
- Sample Preparation: Purify endogenous or recombinant 26S proteasomes. To capture intermediate states, proteasomes can be incubated with substrate (e.g., FAT10-Eos3.2), cofactors (e.g., NUB1, TXNL1), and/or ATPγS (a non-hydrolyzable ATP analog) to stall the cycle [13].
- Vitrification: Apply the sample to an EM grid and rapidly freeze it in liquid ethane to preserve its native state.
- Data Collection & Processing: Acquire thousands of micrographs. Use advanced 3D classification to separate particles into distinct conformational states (e.g., resting state vs. various processing states with different ATPase staircase registers) [13].
- Model Building: Build atomic models into the high-resolution density maps to visualize subunit interactions and substrate engagement.
Application: This approach has revealed how cofactors like TXNL1 bind with high affinity specifically to substrate-engaged proteasomes, coordinating degradation steps [13].
Functional Assays for Degradation and Deubiquitination Activity
Protocol Overview: In Vitro Degradation Assay
- Reconstitution: Incubate purified 26S proteasome with an ATP-regenerating system and a ubiquitinated model substrate (e.g., ubiquitinated Sic1 or a fluorescently tagged substrate) [14].
- Reaction Monitoring: Take aliquots at time intervals and stop the reaction with SDS-PAGE loading buffer.
- Analysis: Analyze samples by SDS-PAGE and immunoblotting to monitor the disappearance of the substrate and/or the appearance of degradation products.
Protocol Overview: Deubiquitination Assay
- Reaction Setup: Incubate proteasomes with polyubiquitin chains or a ubiquitinated substrate.
- Inhibition Control: To specifically assess Rpn11 activity, include the specific inhibitor OPA-1 or use proteasomes with a catalytically inactive Rpn11 mutant [13].
- Analysis: Resolve reaction products by SDS-PAGE and visualize by immunoblotting with anti-ubiquitin antibodies or Coomassie staining to monitor ubiquitin chain cleavage.
Investigating Proteasome Autoregulation
Protocol Overview: Analyzing In Situ Ubiquitination
- Proteasome Purification: Rapidly purify 26S proteasomes under denaturing conditions (using SDS buffer) or in the presence of deubiquitinase inhibitors to preserve native ubiquitination states of proteasome subunits [14].
- Immunoblotting: Probe for specific proteasomal subunits (e.g., Rpt5, Rpn13/Adrm1, S5a/Rpn10, Uch37) to detect slower-migrating ubiquitinated forms.
- Functional Correlation: Compare the activity of ubiquitinated proteasomes against non-ubiquitinated ones in binding, deubiquitination, and degradation assays to determine the functional consequence of autoregulation [14].
Table 2: Key Research Reagents for 26S Proteasome Studies
| Reagent / Method | Category | Primary Function in Research | Key Experimental Insight |
|---|---|---|---|
| Cryo-EM with 3D Classification | Structural Biology | Resolves conformational states and cofactor binding | Revealed spiral-staircase ATPase mechanism and conformation-specific cofactor binding [13]. |
| ATPγS (Adenosine 5′-O-[γ-thio]triphosphate) | Small Molecule | Non-hydrolyzable ATP analog; stalls ATPase cycle | Allows trapping of proteasome in substrate-engaged intermediate states for structural studies [13]. |
| OPA-1 | Inhibitor | Specific, active-site inhibitor of Rpn11 deubiquitinase | Blocks deubiquitination, stalling ubiquitinated substrates for structural and functional analysis [13]. |
| MG132 / Bortezomib | Small Molecule Inhibitor | Reversible/irreversible 20S CP active-site inhibitor | Validates UPS dependency in degradation assays; used therapeutically to induce ER stress and apoptosis [16] [15]. |
| Carfilzomib | Small Molecule Inhibitor | Irreversible 20S CP active-site inhibitor | Rescued expression and function of pathogenic pendrin variants in disease models [16]. |
| Rapid Denaturing Purification | Biochemical Method | Preserves labile post-translational modifications | Enabled discovery of in situ ubiquitination of proteasomal subunits (Rpt5, Rpn13) [14]. |
Implications for Proteasome Inhibition and Ubiquitin Homeostasis
The detailed mechanistic understanding of the 26S proteasome directly informs research on proteasome inhibition and its consequences. A key concept emerging from recent studies is proteasome autoregulation. The 26S proteasome itself can be ubiquitinated in situ on subunits such as Rpt5, Rpn13/Adrm1, and Uch37 [14]. This self-modification impairs the proteasome's ability to bind and degrade ubiquitinated substrates, creating a negative feedback loop. This mechanism is proposed to adjust proteasomal activity in response to fluctuating cellular ubiquitination levels [14].
When proteasome activity is pharmacologically inhibited (e.g., by Bortezomib or Carfilzomib), this feedback is disrupted. The result is a dual impact on cellular ubiquitin economy:
- Substrate Accumulation: Ubiquitinated proteins that are normally degraded begin to accumulate.
- Ubiquitin Depletion: The continuous cycle of ubiquitin conjugation and deubiquitination is halted, as the Rpn11-mediated deubiquitination step is coupled to degradation. This can lead to the sequestering of ubiquitin on undegraded substrates, effectively depleting the free ubiquitin pool.
This model explains why proteasome inhibition can lead to a rapid accumulation of high-molecular-weight ubiquitin conjugates while simultaneously causing stress through a lack of free ubiquitin. Furthermore, novel small molecules like BRD1732, which was recently found to be directly ubiquitinated by E3 ligases RNF19A/B, exacerbate this effect by acting as a ubiquitin "sink," leading to dramatic accumulation of ubiquitin-BRD1732 conjugates and broad inhibition of the UPS [17]. Understanding the proteasome's native structure and regulation is therefore paramount for developing next-generation therapeutics that target the UPS and for interpreting the complex cellular phenotypes that arise from its inhibition.
The ubiquitin-proteasome system (UPS) is the primary pathway for the selective degradation of intracellular proteins, a process essential for maintaining cellular homeostasis. Proteasome inhibitors, a class of therapeutic agents predominantly used in hematological malignancies, function by selectively targeting the proteolytic core of the 26S proteasome. This in-depth technical review examines the molecular mechanisms through which these inhibitors induce the characteristic accumulation of polyubiquitinated proteins. We detail the sequential process from initial proteasome engagement to the disruption of protein turnover, highlighting the critical conformational and biochemical changes involved. The document further provides a comprehensive analysis of experimental methodologies for quantifying ubiquitin accumulation and discusses the implications of these findings for drug development and therapeutic applications, particularly within the broader research context of cellular ubiquitin level modulation.
The ubiquitin-proteasome system (UPS) represents a sophisticated, ATP-dependent proteolytic pathway responsible for the controlled degradation of the majority of intracellular proteins [18] [19]. This system regulates a diverse array of cellular processes, including cell cycle progression, gene expression, and the removal of misfolded or damaged proteins [18] [20]. The UPS operates through two discrete, successive steps: a highly specific ubiquitin conjugation cascade that marks target proteins for destruction, and an indiscriminate destruction process mediated by the proteasome [18].
The ubiquitination process involves a sequential enzymatic cascade. First, the ubiquitin-activating enzyme (E1) activates ubiquitin in an ATP-dependent reaction, forming a high-energy thioester intermediate. The activated ubiquitin is then transferred to a ubiquitin-conjugating enzyme (E2). Finally, a ubiquitin-protein ligase (E3) facilitates the transfer of ubiquitin from E2 to a lysine residue on the target protein substrate [18]. This process is repeated to form a polyubiquitin chain, which serves as the primary recognition signal for the 26S proteasome [18] [19].
The 26S proteasome is a multi-subunit complex comprising a 20S core particle (CP) flanked by one or two 19S regulatory particles (RP) [19] [20]. The 20S core particle is a barrel-shaped structure composed of four stacked rings (two identical outer α-rings and two identical inner β-rings) that contain the proteolytic active sites. The three primary catalytic activities within the β-rings are the caspase-like (β1), trypsin-like (β2), and chymotrypsin-like (β5) activities [20]. The 19S regulatory particle is responsible for recognizing polyubiquitinated proteins, cleaving the ubiquitin chains, unfolding the target protein, and translocating the unfolded polypeptide into the 20S core for degradation [19].
Table 1: Core Components of the 26S Proteasome
| Component | Subunit Examples | Primary Function |
|---|---|---|
| 20S Core Particle (CP) | β1, β2, β5 catalytic subunits | Proteolytic degradation of substrate proteins |
| 19S Regulatory Particle (RP) - Base | Rpt1-Rpt6 ATPases | Substrate unfolding, translocation, and CP gating |
| 19S Regulatory Particle (RP) - Lid | Rpn11 deubiquitinase | Ubiquitin chain removal prior to degradation |
| Ubiquitin Receptors | Rpn1, Rpn10, Rpn13 | Polyubiquitinated substrate recognition |
Molecular Mechanism of Proteasome Inhibitors
Proteasome inhibitors function by directly binding to the catalytic subunits of the 20S core particle, thereby blocking its ability to degrade target proteins [18] [20]. These compounds are typically classified based on their chemical structure and mode of interaction with the proteasome's active sites.
Pharmacological Targeting of the Proteasome
Most clinically relevant proteasome inhibitors, including bortezomib, carfilzomib, and ixazomib, primarily target the chymotrypsin-like (β5) activity of the proteasome [20]. At higher concentrations, they also inhibit the caspase-like (β1) and trypsin-like (β2) activities. The inhibitors exhibit different binding kinetics: bortezomib and ixazomib act as reversible inhibitors, while carfilzomib forms an irreversible, covalent bond with the β5 subunit [20].
The binding of an inhibitor to the catalytic sites physically occludes the proteolytic chamber, preventing the insertion and cleavage of polypeptide substrates. This direct steric blockade is the initiating event that triggers the downstream accumulation of ubiquitinated proteins [20].
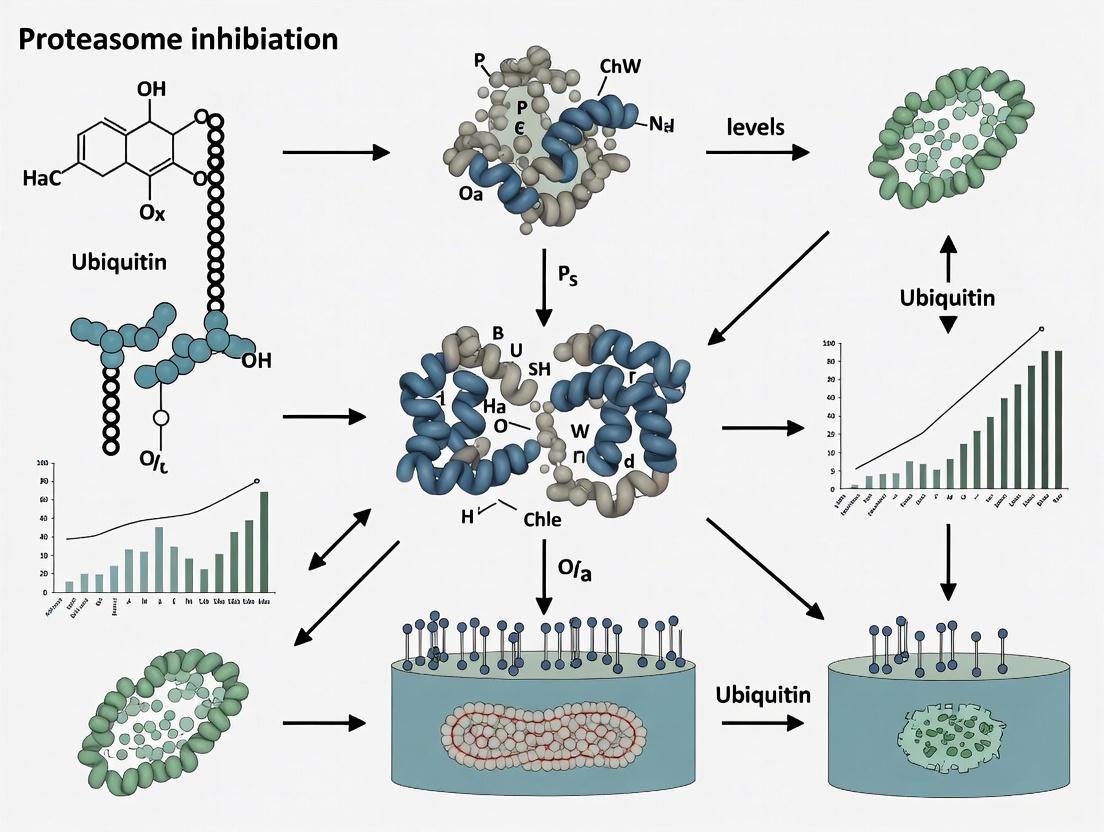
Figure 1: Mechanism of Ubiquitin Accumulation via Proteasome Inhibition. Proteasome inhibitors bind the 20S core, blocking degradation and causing polyubiquitinated protein buildup.
Consequences of Proteasomal Blockade
The inhibition of the proteolytic core triggers a cascade of cellular events. With the degradation machinery incapacitated, polyubiquitinated proteins that are continuously produced by the ubiquitination cascade can no longer be processed and thus begin to accumulate within the cell [18] [21]. This accumulation is not merely a passive consequence but actively contributes to cellular stress and death signaling.
The resulting accumulation of undegraded proteins, particularly in the endoplasmic reticulum (ER), leads to ER stress and the activation of the unfolded protein response (UPR) [20]. The UPR initially attempts to restore proteostasis by reducing global protein synthesis and upregulating chaperone production. However, sustained proteasome inhibition overwhelms this adaptive response, pushing the cell toward apoptosis via several pathways, including JNK activation and caspase-8 and caspase-3 activation [20]. Furthermore, proteasome inhibition stabilizes various pro-apoptotic proteins (e.g., NOXA, Bim, Bid) that are normally short-lived and rapidly turned over by the UPS, further tilting the cellular balance toward programmed cell death [20].
Table 2: Clinically Approved Proteasome Inhibitors and Their Properties
| Inhibitor | Primary Target | Binding Kinetics | Key Clinical Indications |
|---|---|---|---|
| Bortezomib | β5 subunit | Reversible | Multiple Myeloma, Mantle Cell Lymphoma |
| Carfilzomib | β5 subunit | Irreversible | Relapsed/Refractory Multiple Myeloma |
| Ixazomib | β5 subunit | Reversible | Multiple Myeloma (oral administration) |
Experimental Analysis of Ubiquitin Accumulation
Standardized Methodologies for Detection
The experimental validation of ubiquitin accumulation following proteasome inhibition relies on well-established biochemical and cellular techniques. The most fundamental approach involves treating cells with a proteasome inhibitor and analyzing cell lysates via western blotting using anti-ubiquitin antibodies.
Protocol 1: Western Blot Analysis of Ubiquitinated Proteins
- Cell Treatment: Incubate cells (e.g., SK-N-SH, MelJuSo) with a proteasome inhibitor (e.g., 1-10 µM MG132, 100 nM bortezomib, or 100 nM epoxomicin) for a defined period (typically 4-24 hours) [21] [22]. DMSO is used as a vehicle control.
- Cell Lysis: Harvest cells and lyse in RIPA buffer or 1x SDS sample buffer containing protease inhibitors.
- Protein Separation and Immunoblotting: Resolve equal amounts of protein by SDS-PAGE (e.g., 4-12% Bis-Tris gels), transfer to PVDF or nitrocellulose membranes, and probe with a monoclonal anti-ubiquitin antibody (e.g., Cell Signaling Technology #3933) [22]. An anti-β-actin or anti-GAPDH antibody should be used as a loading control.
- Expected Outcome: A characteristic smear of high-molecular-weight bands, representing accumulated polyubiquitinated proteins, is observed in inhibitor-treated samples but not in controls [21].
Protocol 2: Functional Assessment Using Reporter Cell Lines To quantitatively assess UPS function, specialized reporter cell lines can be utilized.
- Reporter Constructs: Generate or obtain cell lines (e.g., MelJuSo) stably expressing UPS reporter substrates such as Ub-YFP, Ub-R-GFP, or YFP-CL1 [22]. These fusion proteins are constitutively ubiquitinated and targeted for rapid proteasomal degradation.
- Experimental Procedure: Treat reporter cells with the proteasome inhibitor. Inhibition of the proteasome will block the degradation of the reporter, leading to its intracellular accumulation.
- Quantification: Measure fluorescence accumulation over time using flow cytometry or fluorescence microscopy. Alternatively, measure protein levels by western blotting with an anti-GFP antibody [22].
Quantitative Data and Comparative Inhibition
Experimental evidence consistently demonstrates a strong quantitative increase in ubiquitinated proteins upon proteasome inhibition. One study directly compared different classes of inhibitors and found that the proteasome inhibitor epoxomicin raised ubiquitinated protein levels at least 3-fold higher than the lysosomotropic agent chloroquine, which inhibits autophagy [21]. This underscores the primary role of the proteasome in the clearance of ubiquitinated proteins under normal conditions.
Furthermore, genetic inhibition of autophagy (e.g., in Atg5 −/− MEFs) failed to elevate ubiquitinated protein levels unless the proteasome was concurrently impaired [21]. These findings highlight the distinct roles of the proteasome and autophagy in protein quality control, with the proteasome serving as the primary pathway for ubiquitin-dependent proteolysis.
Figure 2: Experimental Workflow for Detecting Ubiquitin Accumulation via Western Blot.
The Scientist's Toolkit: Key Research Reagents
Table 3: Essential Reagents for Studying Proteasome Inhibition and Ubiquitin Accumulation
| Reagent / Assay | Function / Purpose | Example Products / Citations |
|---|---|---|
| Pharmacological Inhibitors | Chemically inhibit proteasome activity to induce ubiquitin accumulation. | MG132 (investigational); Bortezomib, Carfilzomib (clinical) [23] [16] [20] |
| Anti-Ubiquitin Antibodies | Detect global ubiquitinated proteins in western blot, immunofluorescence. | Cell Signaling Technology #3933; P4D1 [22] |
| UPS Reporter Cell Lines | Real-time, quantitative assessment of UPS function in live cells. | Stably expressing Ub-YFP, YFP-CL1, ZsGreen-ODC [22] |
| Proteasome Activity Assays | Directly measure chymotrypsin-like, trypsin-like, and caspase-like activity. | Fluorogenic substrates (e.g., Suc-LLVY-AMC) [20] |
| Lysosomal Inhibitors | Control experiments to distinguish UPS from autophagic degradation. | Bafilomycin A1, Chloroquine, Ammonium Chloride [21] |
Research Implications and Therapeutic Context
The accumulation of ubiquitinated proteins is more than a simple biomarker of proteasome inhibition; it represents a critical node in the mechanism of action for this drug class. This effect is strategically exploited in oncology, particularly in multiple myeloma, where malignant plasma cells exhibit high protein synthesis rates and are exceptionally dependent on the UPS to manage their proteotoxic stress [20]. The resulting accumulation of misfolded proteins triggers irreversible ER stress and apoptosis, creating a favorable therapeutic window.
Beyond cancer therapy, understanding this mechanism is crucial for researching neurodegenerative diseases. Conditions like Alzheimer's disease, Parkinson's disease, and cerebral ischemia are associated with impaired proteasomal activity and the prominent accumulation of ubiquitinated proteins in inclusion bodies [24]. Interestingly, a pathogenic feed-forward loop has been identified in which impaired proteasomal activity leads to the accumulation of a cytosolic PINK1 fragment (sPINK1), which in turn phosphorylates ubiquitin. This S65-phosphorylated ubiquitin (pUb) further inhibits proteasome function by interfering with ubiquitin chain elongation and proteasome-substrate interactions, exacerbating protein aggregation and neurodegeneration [24].
Conversely, modulating the UPS presents therapeutic opportunities beyond inhibition. Recent research demonstrates that proteasome activators, such as those in the ZFAND family, can enhance the degradation of misfolded proteins and may have therapeutic potential in conditions like tauopathy and cardiac failure [25]. Furthermore, a novel approach for treating genetic disorders like Pendred syndrome involves using proteasome inhibitors to rescue the expression and function of pathogenic pendrin protein variants by slowing their degradation, highlighting the nuanced and context-dependent applications of UPS modulation [23] [16].
Proteasome inhibition triggers a cascade of intracellular events, beginning with the acute disruption of protein homeostasis and culminating in the initiation of apoptotic cell death. This whitepaper delineates the molecular mechanisms underlying this critical transition, with a specific focus on the resultant fluctuations in cellular ubiquitin levels. By synthesizing findings from recent high-impact studies, we provide a technical guide detailing the experimental frameworks and quantitative assessments essential for researchers investigating the ubiquitin-proteasome system (UPS) and its therapeutic targeting in oncology and beyond.
The ubiquitin-proteasome system (UPS) serves as the primary pathway for regulated intracellular protein degradation in eukaryotic cells, responsible for approximately 80–90% of cellular protein turnover [26]. This system orchestrates the timely destruction of damaged, misfolded, and short-lived regulatory proteins, thereby playing a pivotal role in maintaining cellular homeostasis. The canonical degradation pathway involves a three-enzyme cascade (E1-E2-E3) that tags target proteins with polyubiquitin chains, which are then recognized and degraded by the 26S proteasome complex into short peptides [20] [27]. The 26S proteasome itself is a multiprotein complex comprising a 20S catalytic core particle (CP) capped by one or two 19S regulatory particles (RP) [20]. The 20S core possesses three primary catalytic activities: chymotrypsin-like (β5), trypsin-like (β2), and caspase-like (β1), with the chymotrypsin-like site being the principal target of most clinically approved proteasome inhibitors [20]. Given its central role in controlling protein stability and abundance, targeted inhibition of the UPS presents a powerful strategy for probing cellular physiology and a validated therapeutic approach for hematological malignancies.
Molecular Architecture of the UPS
Proteasome Composition and Regulatory Complexes
The 20S core proteasome is a barrel-shaped structure composed of 28 subunits arranged in four stacked heptameric rings (αββα) [26]. The outer α-rings regulate substrate entry, while the inner β-rings contain the proteolytic active sites. Beyond the standard constitutive proteasome, cells can express the immunoproteasome, which incorporates inducible catalytic subunits (β1i, β2i, β5i) upon stimulation by inflammatory cytokines like interferon-γ, enhancing peptide generation for major histocompatibility complex (MHC) class I antigen presentation [26].
Proteasome activity is further modulated by associated regulatory particles:
- 19S Regulatory Particle (PA700): Binds in an ATP-dependent manner to form the 26S proteasome, responsible for recognizing ubiquitinated substrates, deubiquitinating them (via Rpn11 and USP14), and unfolding them for translocation into the 20S core [26].
- PA28αβ (11S REG): A heptameric activator induced by interferon-γ that binds the 20S core in an ATP-independent manner, facilitating the degradation of small, unfolded peptides and playing a key role in antigen presentation [26].
- PA200 and PSMF1 (PI31): Nuclear and cytoplasmic regulators, respectively, with PA200 involved in DNA repair and spermatogenesis, and PSMF1 acting as an endogenous proteasome inhibitor whose activity can be counteracted by p97/VCP ATPase [26].
Table 1: Major Proteasome Complexes and Their Regulators
| Complex/Regulator | Structure | Binding | Primary Function |
|---|---|---|---|
| 26S Proteasome | 20S CP + 19S RP(s) | ATP-dependent | Degradation of polyubiquitinated proteins |
| Immunoproteasome | 20S with β1i, β2i, β5i | - | Antigen presentation; stress response |
| 19S RP (PA700) | Base (Rpt1-6, Rpn1/2/10/13) + Lid (Rpn3/5-9/11/12/15) | ATP-dependent | Substrate recognition, deubiquitination, unfolding |
| PA28αβ (11S REG) | Heteroheptamer | ATP-independent | Peptide hydrolysis enhancement; antigen presentation |
| PA200 | Monomer | ATP-independent | Nuclear functions; DNA repair; spermatogenesis |
| PSMF1 (PI31) | Monomer | - | Proteasome inhibition; regulation of CP-RP assembly |
Ubiquitin-Dependent and Independent Degradation
While the UPS is synonymous with ubiquitin-dependent degradation, the proteasome can also degrade certain substrates in a ubiquitin-independent manner (UbInPD). This pathway typically targets proteins with intrinsically disordered regions or specific C-terminal sequences. A key example is the oncogenic phosphatase PPM1D, whose rapid degradation is mediated directly by the 20S proteasome via its C-terminal 35 amino acids, without requiring ubiquitination [28]. This UbInPD pathway is estimated to account for up to 20% of intracellular protein degradation and can be activated by regulatory subunits like PSMD14 and PSME3 [28].
Core Mechanisms: From Proteasome Inhibition to Apoptosis
Proteasome inhibitors (e.g., Bortezomib, Carfilzomib, Ixazomib) primarily target the chymotrypsin-like activity of the β5 subunit. This inhibition triggers a multi-faceted cellular stress response, culminating in apoptosis through several interconnected mechanisms.
Disruption of Protein Homeostasis and ER Stress
Cells with high protein synthesis rates, such as multiple myeloma plasma cells producing immunoglobulins, are particularly reliant on efficient UPS function. Proteasome inhibition causes an accumulation of misfolded and polyubiquitinated proteins, leading to proteotoxic stress. A critical consequence is Endoplasmic Reticulum (ER) Stress. The ER relies on the UPS to dislocate and degrade misfolded proteins via ER-associated degradation (ERAD). When this process is blocked, misfolded proteins accumulate within the ER lumen, triggering the Unfolded Protein Response (UPR) [20]. While initially pro-survival, persistent UPR signaling shifts toward pro-apoptotic outcomes, including cell cycle arrest and activation of caspase cascades [20].
Modulation of Apoptotic Signaling Pathways
The accumulation of regulatory proteins due to blocked degradation directly activates both intrinsic and extrinsic apoptotic pathways.
- Stabilization of Pro-Apoptotic Regulators: Key pro-apoptotic Bcl-2 family proteins, such as Bim, Bid, and NOXA, are normally short-lived and rapidly turned over by the proteasome. Their stabilization upon proteasome inhibition tips the mitochondrial balance toward apoptosis [20]. NOXA, in particular, binds and neutralizes the anti-apoptotic protein Mcl-1, promoting Bak/Bax activation and mitochondrial outer membrane permeabilization (MOMP) [29].
- Activation of Intrinsic Apoptosis: MOMP leads to cytochrome c release, formation of the apoptosome, and sequential activation of caspase-9 and caspase-3, executing the cell death program [29].
- c-Jun NH2-terminal Kinase (JNK) and p53 Pathways: Proteasome inhibition activates JNK, which promotes apoptosis via caspase-8 and caspase-3. It also stabilizes the tumor suppressor p53, either directly or through interaction with MDM2, further amplifying pro-apoptotic signals [20].
- Inhibition of NF-κB Survival Signaling: The NF-κB transcription factor is normally activated by the degradation of its inhibitor, IκBα, via the UPS. Proteasome inhibition prevents IκBα degradation, sequestering NF-κB in the cytoplasm and blocking its pro-survival, anti-apoptotic transcriptional program [20].
Diagram 1: Apoptotic signaling cascade triggered by proteasome inhibition, showing key pathways and regulatory proteins.
Quantitative Profiling of Proteasome Inhibitors
The efficacy and cellular impact of proteasome inhibitors are defined by their pharmacodynamic properties. The table below summarizes quantitative and characteristic data for FDA-approved inhibitors.
Table 2: Clinically Approved Proteasome Inhibitors: Mechanisms and Toxicities
| Name (Brand) | Inhibition Kinetics | Active Moiety | Primary Target | Common Clinical Toxicities |
|---|---|---|---|---|
| Bortezomib (Velcade) | Slowly reversible | Boronate | β5 > β1 > β2 | Peripheral neuropathy, nausea, diarrhea, cytopenias |
| Carfilzomib (Kyprolis) | Irreversible | Epoxyketone | β5 > β2/β1 | Dyspnea, cytopenias, nausea, fatigue, peripheral edema |
| Ixazomib (Ninlaro) | Reversible | Boronate | β5 > β1 | Diarrhea, constipation, cytopenias, peripheral neuropathy |
Experimental Frameworks for Investigating UPS Dysfunction
Protocol 1: CRISPR-Cas9 Screens for UPS Modulator Identification
Objective: To identify genes conferring resistance or sensitivity to proteasome inhibitors or novel UPS-targeting compounds. Methodology: This protocol is based on the genome-wide CRISPR-Cas9 resistance screen used to identify mediators of the novel compound BRD1732 [17].
- Cell Line Preparation: Generate a Cas9-expressing cell line (e.g., HAP1, MelJuSo) via lentiviral transduction and antibiotic selection (e.g., blasticidin). Validate Cas9 expression by western blot.
- Library Transduction: Transduce the cell population at a low MOI (e.g., ~0.3) with a genome-wide lentiviral sgRNA library (e.g., Brunello or GeCKO) to ensure single integration. Use a coverage of >500 cells per sgRNA.
- Selection and Treatment: After puromycin selection, split cells into treatment and control arms. Treat the experimental arm with the compound of interest (e.g., BRD1732 at IC50-IC90) for several population doublings. Maintain the control arm in parallel with vehicle (DMSO).
- Genomic DNA Extraction and Sequencing: Harvest genomic DNA from both arms. Amplify the integrated sgRNA sequences by PCR and subject them to next-generation sequencing.
- Bioinformatic Analysis: Align sequences to the sgRNA library. Use algorithms (e.g., MAGeCK) to compare sgRNA abundance between treatment and control arms. Significantly enriched sgRNAs indicate genes whose knockout confers resistance.
Protocol 2: Assessing Ubiquitination and Protein Half-Life
Objective: To measure the turnover rate and ubiquitination status of a specific protein (e.g., PPM1D, Mcl-1) under proteasome inhibition. Methodology: This combines cycloheximide chase assays and ubiquitination assessment as applied in recent studies [29] [28].
Cycloheximide Chase Assay:
- Seed cells expressing the protein of interest. Prior to assay, treat with a proteasome inhibitor (e.g., 10 μM MG132) or vehicle for 4-6 hours to establish a baseline.
- Add cycloheximide (e.g., 100 μg/mL) to inhibit new protein synthesis. Harvest cell pellets at defined time points (e.g., 0, 30, 60, 120, 240 minutes).
- Prepare whole-cell lysates and perform SDS-PAGE and western blotting for the target protein and a loading control (e.g., GAPDH, β-actin).
- Quantify band intensity to plot protein decay and calculate half-life.
Ubiquitination Dependency Assay:
- To distinguish ubiquitin-dependent from independent degradation, repeat the chase assay in the presence of TAK-243 (1 μM), a specific E1 ubiquitin-activating enzyme inhibitor [28].
- Stabilization of the protein upon TAK-243 treatment indicates ubiquitin-dependent degradation. If the protein remains unstable, it suggests UbInPD.
In Vitro Degradation Assay:
- Purify the recombinant protein of interest (e.g., PPM1D) and incubate it with purified 20S proteasome in a degradation buffer.
- Monitor protein degradation over time via western blot or other detection methods. Direct degradation confirms UbInPD and identifies the protein as a direct proteasome substrate [28].
Diagram 2: Workflow for a genome-wide CRISPR-Cas9 screen to identify genes involved in the cellular response to proteasome inhibition or UPS-targeting compounds.
The Scientist's Toolkit: Key Research Reagents
Table 3: Essential Reagents for Investigating UPS and Apoptosis
| Reagent / Assay | Function / Application | Example Compounds & Targets |
|---|---|---|
| Proteasome Inhibitors | Inhibit catalytic activity of the 20S core; induce ER stress and apoptosis. | Bortezomib (β5), Carfilzomib (β5), MG132 (β5), Epoxomicin (β5) [20] [22] |
| E1 Ubiquitination Inhibitor | Globally blocks ubiquitin activation; tests ubiquitin-dependency of degradation. | TAK-243 (E1 UBA1 inhibitor) [28] |
| CRISPR-Cas9 Libraries | Genome-wide forward genetic screens for modifier gene identification. | Brunello/GeCKO libraries; sgRNAs targeting RNF19A, RNF19B, UBE2L3 [17] |
| Ubiquitin Reporters | Live-cell or endpoint reporters for ubiquitin-dependent proteolysis. | Ub-YFP, Ub-R-GFP, YFP-CL1 [22] |
| Apoptosis Assays | Quantify caspase activation and cell death. | Caspase-3/7 activity assays, Annexin V staining [20] [29] |
| Lysosome Inhibitors | Distinguish proteasomal from lysosomal degradation pathways. | Bafilomycin A1, Chloroquine [28] |
| DUB Inhibitors | Investigate the role of deubiquitinating enzymes in UPS function. | USP14 inhibitors, PR-619 (pan-DUB inhibitor) [26] |
Emerging Frontiers and Novel Mechanisms
Recent research has uncovered non-canonical mechanisms of UPS disruption. A landmark study identified a first-in-class small molecule, BRD1732, which is itself directly ubiquitinated within cells [17]. This stereospecific process is dependent on the E3 ligases RNF19A/RNF19B and the E2 enzyme UBE2L3. Ubiquitination occurs on a secondary amine of BRD1732, leading to the accumulation of inert ubiquitin-BRD1732 conjugates and non-canonical K27-linked polyubiquitin chains. This sequestration of ubiquitin pools results in a broad collapse of the UPS, independent of direct proteasome inhibition, and represents a novel MOA for inducing proteotoxic stress [17].
Furthermore, the UPS is increasingly implicated in regulating cancer immunotherapy outcomes. The stability of immune checkpoint proteins like PD-L1 is controlled by E3 ligases such as SPOP and TRIM21, which mediate its ubiquitination and proteasomal degradation [30]. Tumor cells can evade this regulation, leading to increased PD-L1 surface expression and immune evasion. Targeting these E3 ligases or associated DUBs presents a promising strategy to enhance the efficacy of anti-PD-1/PD-L1 immunotherapy [30].
Ubiquitination is a pivotal post-translational modification that extends far beyond its canonical role in targeting proteins for proteasomal degradation. While K48-linked ubiquitin chains are well-established as definitive degradation signals, a diverse array of "atypical" ubiquitin linkages—including K63, K11, K29, K33, K6, K27, M1, and various branched forms—orchestrate a complex spectrum of non-degradative cellular processes. These atypical chains function as sophisticated molecular codes that regulate inflammatory signaling, DNA repair, endocytosis, and autophagy. This whitepaper examines the architecture, synthesis, and functional roles of these atypical ubiquitin chains, with particular emphasis on their implications for therapeutic strategies involving proteasome inhibition. Understanding this ubiquitin code is essential for advancing drug development in oncology, neurodegenerative diseases, and inflammatory disorders.
Ubiquitin chains are classified into three structural categories based on their linkage patterns: homotypic (uniformly linked through the same ubiquitin residue), mixed (containing different linkages but each ubiquitin modified at only one site), and branched (featuring ubiquitin monomers simultaneously modified at two or more distinct sites) [31]. Atypical ubiquitin chains encompass all ubiquitin polymers except the classical K48-linked homotypic chains traditionally associated with proteasomal degradation [32].
The diversity of atypical chains arises from ubiquitin's seven lysine residues (K6, K11, K27, K29, K33, K48, K63) and its N-terminal methionine (M1), each capable of forming distinct isopeptide linkages that generate unique three-dimensional structures [32] [31]. This structural diversity enables the transmission of specific biological information, allowing ubiquitin to function as a multifunctional signaling molecule. Beyond protein degradation, atypical ubiquitin chains regulate essential processes including NF-κB signaling, kinase activation, DNA damage repair, protein trafficking, and autophagy [32] [31].
Table 1: Classification of Atypical Ubiquitin Chain Linkages
| Linkage Type | Structural Class | Primary Functions | Key Assembling Enzymes |
|---|---|---|---|
| K63-linked | Homotypic | NF-κB signaling, DNA repair, endocytosis, kinase activation | TRAF6, UBC13-UEV1A complex |
| K11-linked | Homotypic/Branched | Cell cycle regulation, ERAD | UBE2S, APC/C, UBE2C |
| M1-linked (linear) | Homotypic | NF-κB activation, inflammatory signaling | LUBAC complex |
| K29/K48-branched | Branched | Proteasomal degradation (enhanced efficiency) | UBE3C, Ufd4/Ufd2 collaboration |
| K48/K63-branched | Branched | Signaling-to-degradation switch, proteasomal processing | TRAF6/HUWE1, ITCH/UBR5 collaboration |
| K6-linked | Homotypic/Branched | DNA damage response, mitophagy | Parkin, BRCA1-BARD1 |
| K27-linked | Homotypic | Immune signaling, kinase activation | Uncharacterized |
| K33-linked | Homotypic | Kinase regulation, TCR signaling | Uncharacterized |
Structural Diversity and Synthesis of Atypical Chains
Homotypic and Mixed Linkage Chains
Homotypic atypical chains are uniformly connected through a single lysine residue other than K48. Among these, K63-linked chains represent one of the most extensively studied atypical linkages. These chains adopt an extended, open conformation that differs dramatically from the compact structure of K48-linked chains, enabling their recognition by proteins containing specific ubiquitin-binding domains (UBDs) that translate the ubiquitin signal into downstream cellular responses [32]. K63 linkages primarily function in non-degradative signaling pathways, including activation of the NF-κB pathway, DNA damage repair mechanisms, and regulation of receptor endocytosis [32].
The synthesis of homotypic chains is governed by specific E2-E3 enzyme pairs that determine linkage specificity. For instance, the MMS2-UBC13 complex specifically generates K63-linked chains through a mechanism that positions the acceptor ubiquitin such that only K63 is accessible for ubiquitin transfer [32]. Similarly, the linear ubiquitin chain assembly complex (LUBAC) exclusively generates M1-linked linear chains that play critical roles in NF-κB signaling and inflammatory responses [31].
Branched Ubiquitin Chains
Branched ubiquitin chains represent a sophisticated level of complexity in the ubiquitin code, where a single ubiquitin moiety serves as a branch point by being simultaneously modified at two or more distinct lysine residues [31]. These branched architectures can be generated through two primary mechanisms:
Collaborative E3 mechanisms: Pairs of E3 ligases with distinct linkage specificities work sequentially to build branched structures. For example, in the ubiquitin fusion degradation (UFD) pathway in yeast, Ufd4 first assembles K29-linked chains on substrates, which are then recognized by Ufd2 through specialized binding loops to add K48-linked ubiquitins, creating K29/K48-branched chains [31]. Similarly, during NF-κB signaling, TRAF6 synthesizes K63-linked chains that are subsequently recognized by HUWE1, which attaches K48 linkages through its UIM and UBA domains to form K48/K63-branched chains [31].
Single E3 mechanisms: Certain E3 ligases possess intrinsic capability to generate branched chains. The anaphase-promising complex/cyclosome (APC/C) collaborates with two different E2s (UBE2C and UBE2S) to form branched K11/K48 chains during mitosis [31]. Additionally, some HECT-family E3s like WWP1 can synthesize branched chains containing both K48 and K63 linkages when paired with a single E2 enzyme (UBE2L3) [31].
Diagram 1: Branch ubiquitin chain formation process.
The functional significance of branched chains often lies in their ability to integrate multiple signals or enhance degradation efficiency. For instance, branched K48/K63 chains on the pro-apoptotic regulator TXNIP facilitate a conversion from non-degradative K63 signaling to degradative K48 signaling, enabling precise temporal control of protein stability during apoptotic responses [31]. Recent research using the UbiREAD technology has demonstrated that in K48/K63-branched chains, the identity of the substrate-anchored chain determines the functional outcome, establishing that "branched chains are not the sum of their parts" [33].
Functional Roles in Cell Signaling
NF-κB and Inflammatory Signaling
Atypical ubiquitin chains play indispensable roles in the activation and regulation of NF-κB signaling pathways. Both K63-linked and M1-linear chains function as critical scaffolds that facilitate the assembly of signaling complexes. K63-linked chains activate IκB kinase (IKK) by promoting the phosphorylation and activation of TAK1 through specific adaptor proteins, while M1-linear chains generated by LUBAC stabilize the signaling complex and prevent its dissociation [32] [31].
The integration of different chain types creates a sophisticated regulatory network. For example, branched K48/K63 chains formed through collaboration between TRAF6 and HUWE1 enable crosstalk between inflammatory signaling and degradation pathways, potentially serving as a mechanism to terminate NF-κB activation after the signaling event [31]. This demonstrates how branched ubiquitin chains can integrate multiple signals to fine-tune cellular responses.
Kinase Activation and DNA Repair
In kinase activation pathways, atypical ubiquitin chains frequently function as allosteric regulators rather than degradation signals. K63-linked ubiquitination of both receptor tyrosine kinases (e.g., EGFR) and cytoplasmic kinases (e.g., MEKK3) can enhance their catalytic activity or promote their translocation to specific cellular compartments where they interact with downstream effectors [32].
The DNA damage response employs multiple atypical ubiquitin linkages to coordinate repair processes. K63-linked chains facilitate the recruitment of DNA repair proteins to damage sites, while K6-linked chains assembled by BRCA1-BARD1 play roles in DNA double-strand break repair [31]. Additionally, K29/K48-branched chains have been implicated in the regulation of DNA repair proteins, potentially modulating their stability or activity in response to genotoxic stress [31].
Selective Autophagy and Membrane Trafficking
Atypical ubiquitin chains serve as specific recognition signals for selective autophagy pathways. During mitophagy, K6-linked chains on mitochondrial proteins can be recognized by autophagy receptors that target damaged mitochondria for degradation [31]. Similarly, K63-linked chains often function as signals for various selective autophagy processes, including aggrephagy (clearance of protein aggregates) and xenophagy (clearance of intracellular pathogens) [32].
In membrane trafficking, monoubiquitination and K63-linked chains function as sorting signals that direct transmembrane proteins to lysosomal degradation via the endosomal system, independent of proteasomal degradation [32]. This is particularly important for the downregulation of activated growth factor receptors and the modulation of immune receptor signaling.
Experimental Approaches and Methodologies
UbiREAD Technology for Functional Analysis
The Ubiquitinated Reporter Evaluation After Intracellular Delivery (UbiREAD) platform represents a technological breakthrough for systematically deciphering the ubiquitin code, particularly for understanding how chain linkage and topology influence intracellular degradation kinetics [33].
Experimental Workflow:
- Preparation of defined ubiquitin chains: Recombinant ubiquitin chains of defined length and linkage composition are synthesized in vitro using specific E2/E3 enzyme combinations or semisynthetic approaches. Chain length is fixed by incorporating a distal ubiquitin bearing point mutations (e.g., K48R for K48 chains) that prevent further elongation [33].
Substrate conjugation: The pre-assembled ubiquitin chains are enzymatically conjugated to a mono-ubiquitinated GFP-based degradation reporter substrate that has been engineered for efficient proteasomal recognition [33].
Intracellular delivery: The defined ubiquitin-GFP conjugates are introduced into mammalian cells (e.g., RPE-1, THP-1, U2OS) via electroporation, which enables rapid cytoplasmic delivery without significant protein processing or loss of viability [33].
Degradation kinetics monitoring: The fate of the ubiquitinated reporter is tracked using multiple complementary approaches:
- Flow cytometry to measure GFP fluorescence loss over time (as fast as 20-second intervals)
- In-gel fluorescence to distinguish between input, degraded, and deubiquitinated species
- Pharmacological inhibition using specific inhibitors (MG132 for proteasome, TAK243 for E1, CB5083/NMS873 for p97) to validate degradation mechanisms [33]
Key Insights from UbiREAD:
- K48 chains with three or more ubiquitins trigger degradation with half-lives of 1-2 minutes
- K63-ubiquitinated substrates are rapidly deubiquitinated rather than degraded
- In K48/K63-branched chains, the substrate-anchored chain identity determines degradation vs. deubiquitination outcomes [33]
Table 2: Intracellular Degradation Kinetics of Different Ubiquitin Chain Types
| Ubiquitin Chain Type | Intracellular Half-life | Primary Fate | DUB Sensitivity | Proteasome Dependency |
|---|---|---|---|---|
| K48-Ub4 | 1-2 min | Degradation | Low | High (MG132-sensitive) |
| K48-Ub3 | ~2 min | Degradation | Moderate | High |
| K63-Ub4 | >60 min | Deubiquitination | High | Low |
| K48/K63-branched | Variable (anchor-dependent) | Mixed | Moderate | Partial |
| MonoUb | >120 min | Stable | Low | None |
Structural Biology Approaches
Cryo-EM and Structural Analysis of full-length E3 ligases has provided unprecedented insights into the mechanisms of ubiquitin chain assembly and specificity. For example, structural studies of the HECT-type E3 HACE1 have revealed:
Autoinhibition mechanism: Full-length HACE1 forms a yin-yang-like dimer that constrains the catalytic HECT domain in an autoinhibited state, with dimerization mediated by contacts between the N-helix of one subunit and the small wing of the HECT N-lobe of the other subunit [34].
Activation process: Upon activation, HACE1 transitions to a monomeric state that enables substrate recognition and ubiquitin transfer [34].
Substrate specificity: Activated monomeric HACE1 selectively recognizes GTP-bound RAC1 through specific interaction interfaces, explaining its selectivity for the active form of this GTPase [34].
Hydrogen-Deuterium Exchange Mass Spectrometry (HDX-MS) complements structural approaches by mapping protein dynamics and interaction interfaces, revealing how E3 ligases like HACE1 undergo conformational changes during activation and substrate engagement [34].
Proteomics and Enrichment Strategies
Mass spectrometry-based ubiquitinomics enables system-wide profiling of ubiquitination sites and chain linkages. Key methodological considerations include:
Di-Glycine remnant immunoaffinity enrichment: Antibodies specific for the Lys-ε-GG remnant left after tryptic digestion of ubiquitinated proteins enable enrichment of ubiquitinated peptides for MS identification and quantification [35]. This approach has revealed that aging prominently affects protein ubiquitylation in the mouse brain, with 29% of altered ubiquitylation sites changing independently of protein abundance [35].
Linkage-specific antibodies: Antibodies that recognize specific ubiquitin linkages (e.g., K63, K48, M1) enable the enrichment and detection of particular chain types.
UbiCRest assay: This approach uses linkage-specific deubiquitinases (DUBs) as "restriction enzymes" to fingerprint ubiquitin chain topology by analyzing characteristic cleavage patterns [33].
Research Reagent Solutions
Table 3: Essential Research Tools for Studying Atypical Ubiquitin Chains
| Research Tool | Specific Example | Application/Function | Key Features |
|---|---|---|---|
| Defined ubiquitin chains | K48-Ub4-GFP, K63-Ub4-GFP | Substrate degradation kinetics | Pre-assembled chains of specific linkage and length |
| Linkage-specific DUBs | OTUB1 (K48-specific), AMSH (K63-specific) | Chain linkage analysis, UbiCRest | Cleave specific ubiquitin linkages |
| Proteasome inhibitors | MG132, Bortezomib, Carfilzomib | Block proteasomal degradation | Varying specificity and mechanisms |
| E1 inhibitors | TAK243 | Block global ubiquitination | Prevents ubiquitin activation |
| p97/VCP inhibitors | CB5083, NMS873 | Disrupt p97-mediated extraction | Affects ERAD and substrate processing |
| Linkage-specific antibodies | Anti-K63, Anti-K48, Anti-M1 | Immunodetection and enrichment | Specific recognition of chain linkages |
| Activity-based probes | Ubiquitin-based electrophilic probes | DUB activity profiling | Covalently label active DUBs |
| Recombinant E2/E3 enzymes | UBC13-UEV1A, TRAF6, HACE1 | In vitro ubiquitination assays | Defined linkage specificity |
Implications for Proteasome Inhibition Therapy
The expanding understanding of atypical ubiquitin chains has profound implications for therapeutic strategies involving proteasome inhibitors, particularly in oncology. Multiple myeloma treatment with bortezomib and other PIs exploits the heightened dependency of antibody-producing cells on proteasomal function, but resistance frequently develops through adaptation of the ubiquitin-proteasome system [36].
Compensatory Mechanisms and Resistance
Cancer cells employ multiple adaptive responses to proteasome inhibition:
- NRF1-mediated proteasome bounce-back: Upon proteasome inhibition, the transcription factor NRF1 is stabilized and activates the expression of proteasome subunit genes, enabling cells to compensate for inhibited proteasomes by synthesizing new ones [36].
- Ubiquitin chain editing: Changes in the balance of ubiquitin chain types, particularly increased non-degradative chains, may allow cancer cells to redirect proteins from degradation to alternative fates.
- Enhanced autophagy: When proteasomal function is compromised, cells may increase their reliance on autophagy as an alternative degradation pathway [36].
Therapeutic Opportunities
Understanding atypical ubiquitin chains reveals several promising therapeutic approaches:
- Combination targeting: Simultaneous inhibition of proteasomes and compensatory pathways (e.g., p97/VCP, autophagy, NRF1 activation) may overcome resistance mechanisms [36].
- Chain linkage-specific interventions: Developing agents that specifically modulate the formation or recognition of particular atypical ubiquitin linkages could enable more precise manipulation of specific pathways without global disruption of protein homeostasis.
- Branched chain manipulation: Targeting the E3 ligases that create branched degradation signals (e.g., HUWE1, UBR5) might enhance the efficacy of proteasome inhibitors by promoting the formation of more efficient degradation signals on specific oncoproteins.
Diagram 2: UPS adaptation and therapeutic strategy.
Atypical ubiquitin chains represent a sophisticated language of post-translational modification that extends far beyond the traditional degradation paradigm. The diversity of ubiquitin chain linkages and architectures—including homotypic atypical chains, mixed chains, and branched polymers—enables precise control over numerous cellular signaling pathways. Understanding this "ubiquitin code" is not merely an academic exercise but has direct implications for therapeutic development, particularly in the context of proteasome inhibitor treatments for cancer.
Future research directions should focus on developing more sophisticated tools for monitoring ubiquitin chain dynamics in living cells, elucidating the structural basis of branched chain recognition by proteasomal and non-proteosomal effectors, and designing therapeutic strategies that specifically target the formation or interpretation of disease-relevant ubiquitin signals. As our understanding of atypical ubiquitin chains continues to evolve, so too will our ability to manipulate this system for therapeutic benefit across a range of human diseases.
Quantifying the Impact: Tools and Techniques for Monitoring Ubiquitin Dynamics
The ubiquitin-proteasome system (UPS) serves as the primary pathway for targeted intracellular protein degradation, playing a central role in maintaining cellular protein homeostasis (proteostasis). This sophisticated biochemical machinery is responsible for the selective degradation of abnormal, misfolded, or damaged proteins, as well as the controlled turnover of key regulatory proteins involved in critical processes such as cell cycle progression, transcriptional regulation, apoptosis, and stress response [37] [18]. The UPS operates through a two-step mechanism: first, target proteins are marked for destruction through the covalent attachment of ubiquitin chains in an enzymatic cascade involving E1 (activating), E2 (conjugating), and E3 (ligating) enzymes; second, the polyubiquitinated proteins are recognized and degraded by the 26S proteasome, a massive multi-catalytic protease complex [18]. Given its pivotal role in cellular physiology, it is not surprising that UPS dysfunction has been implicated in the pathogenesis of numerous human diseases, including cancer, neurodegenerative disorders, and metabolic conditions [37] [38].
Within the context of investigating the impact of proteasome inhibition on cellular ubiquitin levels, the ability to quantitatively monitor UPS activity in living cells is paramount. Pharmacological inhibition of the proteasome creates a proteostatic imbalance, leading to the accumulation of polyubiquitinated proteins and potentially triggering adaptive cellular responses. To study these dynamic processes in real-time, researchers have developed genetically-encoded fluorescent reporter constructs that serve as indicators of UPS functionality. Among these, the GFPu (Green Fluorescent Protein-based ubiquitin-proteasome system reporter) and related UbV-GFP (Ubiquitin-variant-GFP) constructs have emerged as powerful tools for monitoring proteasome activity directly in the live cell environment, providing unprecedented spatial and temporal resolution [39] [38]. This technical guide examines the design principles, implementation, and applications of these reporter systems in the study of UPS function and the cellular responses to proteasome inhibition.
Fundamentals of UPS Reporter Design
Core Principles of Degradation Reporters
UPS reporter constructs are based on the fundamental principle of targeting an otherwise stable fluorescent protein for proteasomal degradation through the introduction of specific degradation signals, known as degrons [38]. These degrons are recognized by the ubiquitination machinery, leading to the polyubiquitination of the reporter and its subsequent degradation by the 26S proteasome. Under normal conditions, this results in low steady-state levels of the fluorescent protein. However, when proteasome activity is impaired, the reporter accumulates, leading to a measurable increase in fluorescence intensity [37] [40]. This elegant design allows researchers to monitor UPS functionality in real-time by simply measuring fluorescence levels using techniques such as epifluorescence microscopy or flow cytometry [37].
The utility of these reporters extends beyond simple inhibition studies. They can reveal spatial aspects of proteasome function within different cellular compartments, track changes in UPS activity during cellular processes such as differentiation or stress response, and identify subpopulations of cells with varying proteasome capacity [39] [41]. Furthermore, transgenic models expressing these reporters enable the study of UPS function in physiological and pathological contexts in vivo [40].
The GFPu Reporter Family
The GFPu family of UPS reporters consists of fluorescent proteins (typically GFP or its variants) that have been engineered to include constitutive degradation signals, rendering them ubiquitin-dependent proteasome substrates [39]. These reporters can be tailored to monitor different aspects of UPS function:
- Global UPS Reporters: These constructs typically contain degrons that are recognized by ubiquitin ligases present throughout the cell, providing an overall assessment of UPS capacity.
- Compartment-Specific Reporters: By incorporating targeting sequences or using degrons with specific subcellular localization, these reporters can monitor UPS activity in particular compartments such as the nucleus or cytoplasm [39].
One particularly well-characterized GFPu variant utilizes the CL1 degron, a short C-terminal peptide extension identified in a yeast screen for sequences that target proteins for ER-associated degradation [38]. When fused to GFP (creating GFP-CL1), this hydrophobic sequence converts the otherwise stable GFP into a short-lived protein that is continuously degraded by the UPS. The degradation of GFP-CL1 is dependent on functional ubiquitination machinery and proteasome activity, making it a sensitive indicator of global UPS function [38].
UbV-GFP and Engineered Ubiquitin Fusion Reporters
Ubiquitin fusion degradation (UFD) substrates represent another important class of UPS reporters. These constructs are based on the observation that fusion proteins with an N-terminal ubiquitin moiety are rapidly cleaved by ubiquitin-specific proteases (DUBs), exposing a residue that may function as a degron according to the N-end rule pathway [38]. When the cleavage between ubiquitin and the reporter is prevented (e.g., by mutating the critical glycine residue at the C-terminus of ubiquitin to valine, creating Ub(^{G76V})), the uncleaved fusion protein itself becomes a target for polyubiquitination and proteasomal degradation [38].
The Ub(^{G76V})-GFP (UbV-GFP) reporter exploits this UFD pathway by fusing a non-cleavable ubiquitin mutant to the N-terminus of GFP. This fusion protein is recognized by specific ubiquitin ligases, polyubiquitinated on the ubiquitin moiety, and subsequently degraded by the proteasome [38]. The accumulation of UbV-GFP upon proteasome inhibition provides a quantitative measure of UPS activity that is complementary to the GFPu reporters.
Table 1: Comparison of Major UPS Reporter Constructs
| Reporter Type | Degradation Signal | Degradation Pathway | Key Features | Primary Applications |
|---|---|---|---|---|
| GFPu (e.g., GFP-CL1) | C-terminal degron (CL1) | Ubiquitin-dependent proteasomal degradation | Sensitive to global UPS function; can form aggregates due to hydrophobic degron | Monitoring overall UPS capacity; identifying cells with low proteasome activity [38] |
| UbV-GFP (Ub(^{G76V})-GFP) | N-terminal non-cleavable ubiquitin | Ubiquitin fusion degradation (UFD) pathway | Based on engineered ubiquitin fusion; avoids some aggregation issues | Studying UFD pathway; monitoring nuclear and cytoplasmic UPS activity [38] |
| GFP-dgn | Destabilizing domain (dgn) | Ubiquitin-dependent proteasomal degradation | Can be used with lentiviral delivery for high efficiency transduction | Monitoring UPS activity in primary cells and senescent cells [37] |
| ZsGreen-mODC | Ornithine decarboxylase degron | Ubiquitin-independent proteasomal degradation | Reports on ubiquitin-independent degradation; useful for distinguishing degradation mechanisms | Identifying tumor-initiating cells with low proteasome activity [41] |
Experimental Implementation and Methodologies
Reporter Delivery and Expression Systems
The method of introducing UPS reporters into cells is critical for obtaining reliable and interpretable results. While traditional transfection methods can be used, lentiviral delivery systems offer significant advantages, particularly for primary cells or hard-to-transfect cell types [37].
Lentiviral Transduction Protocol:
- Vector Construction: Clone the reporter gene (e.g., GFPu or UbV-GFP) into a lentiviral expression vector. Most modern systems use self-inactivating (SIN) designs for enhanced biosafety.
- Virus Production: Co-transfect packaging cells (typically HEK293T) with the lentiviral transfer vector and packaging plasmids (psPAX2 and pMD2.G) using a transfection reagent such as Lipofectamine.
- Virus Harvesting: Collect virus-containing supernatant at 48 and 72 hours post-transfection, filter through a 0.45μm membrane to remove cellular debris, and concentrate if necessary.
- Cell Transduction: Incubate target cells with the viral supernatant in the presence of polybrene (4-8μg/mL) to enhance transduction efficiency. The multiplicity of infection (MOI) should be optimized to achieve good expression while minimizing multiple integrations.
- Selection and Expansion: If using vectors with selection markers, apply appropriate antibiotics (e.g., puromycin, blasticidin) 48 hours post-transduction to select for stably expressing populations [37] [41].
This lentiviral approach "guarantees a very high transfection efficiency independent of the cell type or the age of the donor," making it particularly valuable for studying UPS function in specialized primary cells or in the context of cellular senescence [37].
Quantitative Assessment of Proteasome Activity
The activity of the UPS can be quantified by comparing the fluorescence intensity of the destabilized reporter (e.g., GFPu) to that of a stable control (e.g., GFP-dgnFS, which contains a frameshift mutation that stabilizes the protein) [37]. This internal control accounts for variations in expression levels and enables accurate measurement of UPS activity.
Flow Cytometry Protocol:
- Sample Preparation: Harvest cells expressing the UPS reporter 24-72 hours post-transduction or treatment. Include appropriate controls: untransduced cells (background fluorescence), cells expressing stable GFP (maximum signal), and cells treated with proteasome inhibitors (positive control for reporter accumulation).
- Data Acquisition: Analyze samples using a flow cytometer with appropriate excitation/emission settings for GFP (typically 488nm excitation, 530/30nm emission). Collect a minimum of 10,000 events per sample.
- Data Analysis:
- Gate cells based on forward and side scatter to exclude debris and dead cells.
- Measure the geometric mean fluorescence intensity (MFI) of the GFP-positive population.
- Calculate the normalized proteasome activity using the formula: [ \text{Proteasome Activity} = 1 - \left( \frac{\text{MFI}{\text{sample}} - \text{MFI}{\text{min}}}{\text{MFI}{\text{max}} - \text{MFI}{\text{min}}} \right) ] where MFI({}{\text{min}}) represents background fluorescence (untransduced cells) and MFI({}{\text{max}}) represents fluorescence under complete proteasome inhibition [37] [41].
Live-Cell Imaging Protocol:
- Cell Preparation: Plate reporter-expressing cells on glass-bottom dishes or chambered coverslips at an appropriate density (typically 50-70% confluency).
- Image Acquisition: Use an epifluorescence or confocal microscope with environmental control (37°C, 5% CO₂) to maintain cell viability during imaging. Acquire images using identical exposure settings across all experimental conditions.
- Image Analysis: Quantify fluorescence intensity using image analysis software (e.g., ImageJ, CellProfiler). Measure mean intensity per cell after background subtraction. For time-course experiments, normalize fluorescence to baseline levels [37] [42].
Table 2: Quantitative Parameters for UPS Reporter Analysis
| Parameter | Measurement Method | Interpretation | Considerations |
|---|---|---|---|
| Fluorescence Intensity | Flow cytometry or microscopy | Direct measure of reporter accumulation; inversely correlated with UPS activity | Must be normalized to controls; affected by expression level and autofluorescence |
| Reporter Half-life | Time-course after inhibition of protein synthesis | Kinetic measure of degradation rate | Requires cycloheximide or other translation inhibitors; more physiologically relevant |
| Nuclear/Cytoplasmic Ratio | Quantitative image analysis with compartmental segmentation | Spatial information on UPS activity | Requires high-quality segmentation; may reveal compartment-specific regulation |
| Cell-to-Cell Variability | Coefficient of variation of fluorescence | Heterogeneity in UPS activity within populations | May identify subpopulations with differential proteasome capacity [41] |
Controls and Validation Experiments
Proper experimental design requires inclusion of critical controls to ensure that changes in reporter fluorescence specifically reflect alterations in UPS activity rather than confounding factors:
- Proteasome Inhibition Control: Treat cells with established proteasome inhibitors (e.g., 1μM bortezomib, 1μM epoxomicin, or 10μM MG132) for 4-24 hours to demonstrate that reporter accumulation occurs as expected when the proteasome is inhibited [22].
- Stable Reporter Control: Express a mutated version of the reporter that lacks the degron or contains stabilizing mutations (e.g., GFP-dgnFS) to control for variations in expression and overall protein synthesis [37].
- Ubiquitination Dependency Test: Co-treat with inhibitors of E1 ubiquitin-activating enzymes (e.g., PYR-41) to confirm that reporter degradation requires functional ubiquitination [18].
- Specificity Controls: Test whether the reporter responds to perturbations known to affect UPS activity, such as oxidative stress, energy depletion, or expression of dominant-negative ubiquitin mutants [22].
The following diagram illustrates the experimental workflow for implementing and validating UPS reporter systems:
Applications in Proteasome Inhibition Research
Monitoring Dynamic Responses to Proteasome Inhibition
GFPu and UbV-GFP reporters enable real-time monitoring of cellular responses to proteasome inhibition, providing insights into the kinetics and heterogeneity of these responses. For example, in studies of the bioactivatable UPS inhibitor CBK77, UPS reporters demonstrated that this compound causes "an irreversible collapse of the UPS, accompanied by a general accumulation of ubiquitylated proteins and caspase-dependent cell death" [22]. The reporters allowed researchers to distinguish this mechanism from other proteasome inhibitors and to establish the concentration and time dependence of UPS inhibition.
In cancer research, these reporters have been instrumental in identifying subpopulations of cells with differential sensitivity to proteasome inhibitors. For instance, in breast cancer models, "a small subpopulation of cells with low proteasome activity that divided asymmetrically to produce daughter cells with low or high proteasome activity" was identified using a ZsGreen-ODC reporter [41]. This heterogeneity in UPS function may contribute to the variable therapeutic responses observed in clinical applications of proteasome inhibitors.
Identifying Tumor-Initiating Cells
UPS reporters have revealed fascinating connections between proteasome activity and cancer stem cell biology. Multiple studies have demonstrated that "cells with low proteasome activity had greater local tumor formation and metastasis in immunocompromised and immunocompetent mice" across various cancer types, including breast cancer and glioblastoma [41]. This discovery has important implications for understanding treatment resistance, as tumor-initiating cells with low proteasome activity may survive conventional therapies that target more differentiated cancer cells with higher proteasome activity.
The application of these reporters in patient-derived samples further strengthens their translational relevance. In glioblastoma models, "patient-derived glioblastoma cells with low proteasome activity have higher frequency of tumor formation in mouse xenografts," suggesting that proteasome activity could serve as a functional biomarker for tumor-initiating capacity [41].
High-Throughput Screening for UPS Modulators
The quantitative nature of GFP-based UPS reporters makes them ideal tools for high-throughput screening campaigns aimed at identifying novel modulators of proteasome activity. These screens can target either inhibition or enhancement of UPS function:
Inhibitor Screening: Identifies compounds that block UPS activity, potentially useful for cancer therapy. For example, a screen of 5,720 small molecules using UPS reporters led to the discovery of CBK77, an NQO1-activatable UPS inhibitor [22].
Enhancer Screening: Seeks compounds that stimulate UPS activity, potentially beneficial for neurodegenerative diseases characterized by protein aggregation. As noted by Gierisch et al., "enhancing UPS activity may be desirable in diseases where accumulation of misfolded proteins is responsible for cellular dysfunction and decay, which is the case for a broad variety of neurodegenerative diseases" [38].
The following diagram illustrates the central role of UPS reporters in studying proteasome inhibition and its cellular consequences:
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Research Reagents for UPS Reporter Studies
| Reagent Category | Specific Examples | Function in UPS Reporter Studies | Notes and Considerations |
|---|---|---|---|
| Reporter Plasmids | GFPu (GFP-CL1), Ub(^{G76V})-GFP, GFP-dgn, ZsGreen-mODC | Core degradation reporters for monitoring UPS activity | Select based on degradation pathway of interest; consider aggregation propensity of CL1-based reporters [38] |
| Lentiviral Systems | pLVX-IRES-Cherry, pLenti6.4/R4R2/V5-DEST | High-efficiency delivery of reporters to diverse cell types | Enable stable expression; allow transduction of primary and senescent cells [37] [41] |
| Proteasome Inhibitors | Bortezomib, Epoxomicin, MG132, Carfilzomib | Positive controls for reporter validation; tools for studying UPS inhibition mechanisms | Different inhibitors have distinct specificities for catalytic subunits [22] |
| E1 Enzyme Inhibitors | PYR-41, TAK-243 | Controls for ubiquitination-dependency of reporter degradation | Confirm that reporter stabilization requires functional ubiquitination system [18] |
| Fluorescence Detection Tools | Flow cytometers, Fluorescence microscopes, Microplate readers | Quantification of reporter accumulation and UPS activity | Flow cytometry enables population analysis; microscopy provides spatial information [37] [42] |
| Cell Line Models | HEK293T (virus production), MelJuSo (reporter validation), Primary cells (physiological relevance) | Cellular contexts for UPS studies | Consider using multiple models to ensure generalizability of findings [22] |
Technical Considerations and Limitations
While GFPu and UbV-GFP reporters provide powerful approaches for monitoring UPS activity, researchers must be aware of several important technical considerations:
Reporter Aggregation: Some destabilized reporters, particularly those containing hydrophobic degrons like CL1, may form aggregates when their degradation is impaired [38]. These aggregates can complicate fluorescence quantification and potentially exert proteotoxic stress independent of the experimental manipulation. This issue can be mitigated by using alternative degrons (e.g., Ub(^{G76V})) or regularly monitoring cells for the appearance of punctate fluorescence indicative of aggregation.
Potential Artifacts from Overexpression: High-level expression of UPS reporters may saturate the degradation machinery, potentially leading to underestimation of UPS activity or induction of stress responses. Using the lowest practical expression level, employing inducible promoters, or comparing multiple reporters with different degradation kinetics can help address this concern.
Pathway Specificity: Different UPS reporters may be degraded through distinct pathways—some through the N-end rule pathway, others via UFD or other specialized mechanisms [38]. A compound that appears to generally inhibit UPS activity based on a single reporter might actually specifically affect one degradation pathway. Using multiple reporters with different degrons can provide a more comprehensive assessment of UPS function.
Spatial Considerations: The UPS operates in multiple cellular compartments, and proteasome activity may be regulated differently in each. Reporters that localize to specific compartments (e.g., nuclear-targeted vs. cytoplasmic-restricted) can reveal these spatial aspects of UPS regulation [39] [43].
GFPu and UbV-GFP reporter constructs represent versatile and powerful tools for monitoring proteasome activity in living cells, providing unprecedented insights into the dynamics of the ubiquitin-proteasome system. Their application in the study of proteasome inhibition has revealed fundamental aspects of cellular responses to proteostatic stress, including the kinetics of UPS impairment, heterogeneity in cellular sensitivity, and connections to broader physiological processes such as apoptosis and adaptation. Furthermore, these reporters have enabled the identification of clinically relevant cellular subpopulations, such as tumor-initiating cells with characteristically low proteasome activity.
As research on the ubiquitin-proteasome system continues to evolve, these reporter technologies will undoubtedly play an increasingly important role in drug discovery efforts aimed at modulating UPS function for therapeutic benefit. The ongoing refinement of these tools—including the development of new degrons with improved characteristics, reporters with different spectral properties for multiplexing, and advanced imaging approaches for single-molecule tracking—will further enhance our ability to probe the intricacies of protein degradation in health and disease.
Protein ubiquitination is a fundamental post-translational modification that regulates nearly all cellular processes in eukaryotes, including protein degradation, DNA repair, cell cycle progression, and immune responses [44] [45]. This modification involves the covalent attachment of ubiquitin, a 76-amino acid protein, to lysine residues on target proteins through a sequential enzymatic cascade involving E1 activating, E2 conjugating, and E3 ligase enzymes [45]. The versatility of ubiquitination arises from its ability to form diverse polyubiquitin chains through different linkage types (K6, K11, K27, K29, K33, K48, K63, and M1), each encoding distinct functional outcomes [45].
Understanding the global ubiquitination landscape has become crucial for elucidating molecular mechanisms in health and disease. Dysregulation of the ubiquitin-proteasome system (UPS) is implicated in numerous pathologies, including cancer, neurodegenerative disorders, and autoimmune diseases [46] [15]. Furthermore, the development of proteasome-targeting therapies such as PROTACs (Proteolysis-Targeting Chimeras) has heightened the need for precise methods to monitor changes in cellular ubiquitination levels [46]. This technical guide outlines contemporary methodologies for large-scale mapping of ubiquitination sites, with particular emphasis on affinity enrichment strategies coupled with mass spectrometry-based proteomics.
Principles of Ubiquitination Site Analysis
The identification of ubiquitination sites presents several technical challenges. First, the stoichiometry of modification is typically low compared to unmodified proteins. Second, ubiquitinated lysine residues can be modified by single ubiquitin molecules (monoubiquitination), multiple single ubiquitins (multiubiquitination), or polyubiquitin chains of various lengths and linkage types [44] [45]. Third, the dynamic nature of ubiquitination, with continuous attachment by ligases and removal by deubiquitinases (DUBs), creates a rapidly changing cellular landscape [45].
Traditional biochemical approaches, such as immunoblotting with anti-ubiquitin antibodies followed by site-directed mutagenesis of putative modified lysines, are low-throughput and time-consuming [45]. The advent of high-sensitivity mass spectrometry has revolutionized this field, enabling system-wide identification of thousands of ubiquitination sites in a single experiment [47]. Central to these advances has been the development of methods to enrich for ubiquitinated peptides from complex proteomic samples, dramatically increasing the detection sensitivity for these low-abundance modifications.
Key Affinity Enrichment Methodologies
Ubiquitin Remnant Immunoaffinity Enrichment
The most widely employed method for large-scale ubiquitin site mapping utilizes antibodies specific for the diglycine (K-ε-GG) remnant left on modified lysine residues after tryptic digestion [47]. This approach enables enrichment of endogenous ubiquitination sites without genetic manipulation of the target cells or tissues.
Table 1: Comparison of Major Affinity Enrichment Strategies
| Method | Principle | Throughput | Advantages | Limitations |
|---|---|---|---|---|
| K-ε-GG Antibody | Immunoaffinity enrichment of diglycine remnant after trypsin digestion | High | Works with endogenous ubiquitin; applicable to clinical samples; identifies exact modification sites | Cannot distinguish linkage types; may miss peptides with atypical cleavage |
| Tagged Ubiquitin | Expression of epitope-tagged ubiquitin (His, Strep, FLAG) | High | Strong enrichment; relatively low cost | Potential artifacts from tagged ubiquitin expression; not suitable for clinical tissues |
| UBD-Based Capture | Use of ubiquitin-binding domains (TUBEs, ThUBDs) to enrich ubiquitinated proteins | Medium | Preserves ubiquitin chain architecture; can be linkage-specific | Lower affinity for some chains; may not identify exact modification sites |
| Linkage-Specific Antibodies | Antibodies targeting specific ubiquitin chain linkages | Medium to low | Provides linkage information; biologically relevant | Limited to specific chain types; high cost |
The experimental workflow for K-ε-GG remnant enrichment typically involves the following steps [47]:
- Cell Lysis and Protein Extraction: Preparation of protein lysates under denaturing conditions to preserve ubiquitination states and inhibit DUB activity.
- Protein Digestion: Tryptic cleavage of proteins, which simultaneously generates the K-ε-GG signature on modified lysines.
- Peptide Immunoaffinity Enrichment: Incubation of peptides with anti-K-ε-GG antibodies covalently cross-linked to beads.
- Peptide Fractionation: Offline high-pH reversed-phase chromatography to reduce sample complexity.
- LC-MS/MS Analysis: Liquid chromatography coupled to tandem mass spectrometry for peptide identification and quantification.
For quantitative applications, researchers can incorporate SILAC (Stable Isotope Labeling by Amino Acids in Cell Culture) prior to cell lysis, enabling precise comparison of ubiquitination dynamics across different conditions, including proteasome inhibition [47].
Tagged Ubiquitin Expression Systems
An alternative approach involves expressing epitope-tagged ubiquitin (e.g., His, FLAG, Strep, or HA tags) in cells, which becomes incorporated into the endogenous ubiquitination machinery [45]. Tagged ubiquitin constructs allow purification under denaturing conditions using affinity resins such as Ni-NTA for His-tags or Strep-Tactin for Strep-tags [45]. While this method enables strong enrichment of ubiquitinated proteins, it requires genetic manipulation of cells and may not perfectly recapitulate endogenous ubiquitination dynamics due to potential artifacts from the tag itself [45].
Ubiquitin-Binding Domain (UBD) Based Approaches
UBDs are protein domains that naturally recognize and bind to ubiquitin moieties. Tandem hybrid UBD (ThUBD) technology represents a recent advancement, combining multiple UBDs to create high-affinity capture reagents with reduced linkage bias compared to earlier TUBE (Tandem Ubiquitin Binding Entity) designs [46]. ThUBD-coated plates demonstrate a 16-fold wider linear range for capturing polyubiquitinated proteins compared to TUBE-based methods, significantly enhancing detection sensitivity [46]. These approaches are particularly valuable for studying ubiquitin chain architecture and for applications where preserving native ubiquitin configurations is essential.
Experimental Protocol: K-ε-GG Remnant Enrichment
This protocol provides a detailed methodology for large-scale identification of ubiquitination sites using the K-ε-GG antibody enrichment approach, adaptable for studying proteasome inhibition effects [47].
Sample Preparation
- Cell Culture and Treatment: Culture approximately 5 × 10^7 cells per condition. For proteasome inhibition studies, treat cells with inhibitors (e.g., MG132, bortezomib, carfilzomib) at appropriate concentrations and durations [16].
- Cell Lysis: Lyse cells in urea-based buffer (8 M urea, 50 mM Tris-HCl pH 8.0) supplemented with protease and phosphatase inhibitors. Maintain pH >8.0 to prevent lysine carbamylation.
- Protein Digestion:
- Reduce disulfide bonds with 5 mM dithiothreitol (30 minutes, 25°C).
- Alkylate with 10 mM iodoacetamide (30 minutes, 25°C in darkness).
- Dilute urea concentration to 2 M with 50 mM Tris-HCl pH 8.0.
- Digest with trypsin (1:50 enzyme-to-substrate ratio) overnight at 25°C.
Peptide Enrichment
- Antibody Cross-linking:
- Incubate anti-K-ε-GG antibody with protein A/G agarose beads.
- Cross-link using dimethyl pimelimidate (20 mM in 0.2 M triethanolamine pH 8.9) for 30 minutes at 25°C.
- Quench with 50 mM Tris-HCl pH 8.0.
- Immunoaffinity Purification:
- Incubate digested peptides with cross-linked antibody beads (1-2 mg peptides per 10 μg antibody).
- Use 1.5 mL of IgG binding buffer (50 mM MOPS/NaOH pH 7.5, 10 mM Na2HPO4, 50 mM NaCl).
- Rotate mixture for 4-16 hours at 4°C.
- Wash and Elution:
- Wash beads sequentially with IgG binding buffer, water, and 50 mM Tris-HCl pH 8.0.
- Elute peptides with 0.1% trifluoroacetic acid (3 × 100 μL).
Mass Spectrometric Analysis
- Peptide Fractionation:
- Perform offline high-pH reversed-phase chromatography using a C18 column.
- Fractionate peptides using a shallow acetonitrile gradient (5-35% over 60 minutes).
- Combine fractions into 12-24 samples for LC-MS/MS analysis.
- LC-MS/MS Parameters:
- Use a nanoflow LC system coupled to a high-resolution tandem mass spectrometer.
- Employ a 120-minute linear gradient from 5% to 30% acetonitrile in 0.1% formic acid.
- Operate the mass spectrometer in data-dependent acquisition mode.
- Set MS1 resolution to at least 60,000 and MS2 resolution to 15,000.
- Data Analysis:
- Search MS/MS spectra against appropriate protein databases using search engines (e.g., MaxQuant, SEQUEST).
- Include variable modifications for K-ε-GG (glycyl-glycine remnant, +114.0429 Da) on lysine.
- Apply false discovery rate thresholds (typically <1% at peptide and protein levels).
The Scientist's Toolkit: Essential Research Reagents
Table 2: Key Research Reagents for Ubiquitination Studies
| Reagent Category | Specific Examples | Function & Application |
|---|---|---|
| Proteasome Inhibitors | MG132, Bortezomib, Carfilzomib, Delanzomib [16] | Increase global ubiquitination levels by blocking proteasomal degradation; used to study ubiquitin dynamics |
| K-ε-GG Antibodies | Commercial monoclonal antibodies (Cell Signaling Technology, etc.) | Immunoaffinity enrichment of ubiquitinated peptides for mass spectrometry |
| Ubiquitin Tags | His-tagged ubiquitin, Strep-tagged ubiquitin, HA-ubiquitin [45] | Affinity purification of ubiquitinated proteins from engineered cell systems |
| UBD-Based Reagents | TUBEs, ThUBD-coated plates [46] | Unbiased capture of polyubiquitinated proteins with high affinity; minimal linkage bias |
| Linkage-Specific Antibodies | K48-linkage specific, K63-linkage specific, M1-linear specific [45] | Detection and enrichment of specific ubiquitin chain types |
| Deubiquitinase Inhibitors | b-AP15, PR-619 [15] | Prevent removal of ubiquitin modifications; stabilize ubiquitination signals |
| E1/E2/E3 Inhibitors | PYR-41 (E1), NSC697923 (E2), MLN4924 (NEDD8-activating enzyme) [15] | Modulate specific steps in ubiquitination cascade; mechanistic studies |
Integration with Proteasome Inhibition Research
The methodologies described above are particularly relevant for investigating the impact of proteasome inhibition on cellular ubiquitin levels. Proteasome inhibitors, including clinical agents like bortezomib and carfilzomib, disrupt the normal degradation of ubiquitinated proteins, leading to their accumulation within cells [16]. This effect has been demonstrated in various pathological models. For instance, in Pendred syndrome, proteasome inhibitors rescued the expression and function of pathogenic pendrin variants by counteracting their excessive ubiquitination and degradation [16].
When designing experiments to study proteasome inhibition effects, researchers should consider:
- Temporal Dynamics: Ubiquitin accumulation occurs rapidly after proteasome inhibition, with optimal timepoints typically between 2-8 hours post-treatment.
- Inhibitor Specificity: Different inhibitors (e.g., MG132 vs. bortezomib vs. carfilzomib) exhibit varying specificity profiles and cellular toxicities.
- Dose Optimization: Use the minimum effective concentration to avoid pleiotropic effects while achieving sufficient proteasome inhibition.
- Validation Methods: Correlate mass spectrometry findings with orthogonal techniques like western blotting with ubiquitin-specific antibodies.
Technical Considerations and Future Perspectives
Several factors critically influence the success of large-scale ubiquitination studies:
- Sample Quality: Prevent artificial deubiquitination during sample preparation through use of DUB inhibitors and rapid processing.
- Enrichment Efficiency: Optimize antibody-to-peptide ratios to maximize recovery while minimizing non-specific binding.
- Data Quality Controls: Implement careful false discovery rate controls and validate identified sites through independent methods.
Emerging technologies are further advancing the field. ThUBD-based platforms offer significantly improved sensitivity and dynamic range for ubiquitinated protein capture [46]. Cross-linking mass spectrometry provides insights into ubiquitin chain architecture and interactions with ubiquitin-binding proteins. Additionally, improved bioinformatics tools are enhancing our ability to distinguish true ubiquitination sites from isobaric modifications and to interpret the functional consequences of ubiquitination patterns.
When these methodologies are applied within the context of proteasome inhibition research, they enable comprehensive mapping of the cellular ubiquitin landscape, revealing how disrupted protein degradation influences ubiquitination dynamics and contributes to both therapeutic effects and resistance mechanisms. This knowledge is invaluable for developing next-generation UPS-targeting therapies and biomarkers for clinical application.
The ubiquitin-proteasome system (UPS) represents a crucial pathway for intracellular protein degradation and homeostasis. This system involves the covalent attachment of ubiquitin molecules to target proteins, which can then be recognized and degraded by the 26S proteasome complex. The process of ubiquitination involves a sequential enzymatic cascade comprising E1 (activating), E2 (conjugating), and E3 (ligating) enzymes that collectively mediate the attachment of ubiquitin to substrate proteins [45]. Ubiquitin itself contains eight potential linkage sites (M1, K6, K11, K27, K29, K33, K48, and K63), with K48-linked polyubiquitin chains being the primary signal for proteasomal degradation, while K63-linked chains are primarily involved in regulating signal transduction and protein trafficking [48].
Within the context of proteasome inhibition research, monitoring global ubiquitin levels and polyubiquitinated proteins provides critical insights into UPS function and disruption. Pharmacological proteasome inhibitors (e.g., MG132, bortezomib, carfilzomib) cause the accumulation of polyubiquitinated proteins by blocking their degradation, creating a measurable indicator of UPS inhibition [45]. This technical guide details methodologies for the detection and quantification of these changes using western blot analysis, framed within research investigating the impact of proteasome inhibition on cellular ubiquitin homeostasis.
Methodological Considerations for Ubiquitin Detection
Enrichment Strategies for Ubiquitinated Proteins
The relatively low stoichiometry of protein ubiquitination necessitates effective enrichment strategies prior to western blot analysis. The following table summarizes the primary approaches for isolating ubiquitinated proteins:
Table 1: Enrichment Methods for Ubiquitinated Proteins
| Method | Principle | Advantages | Limitations |
|---|---|---|---|
| Ubiquitin Tagging [45] | Expression of epitope-tagged Ub (e.g., His, HA, Flag) in cells; purification via affinity resins. | Easy implementation, relatively low-cost. | May not mimic endogenous Ub; artifacts possible; infeasible for tissue samples. |
| Antibody-Based Enrichment [45] | Use of anti-Ub antibodies (e.g., P4D1, FK1/FK2) or linkage-specific antibodies to immunoprecipitate ubiquitinated proteins. | Works under physiological conditions; no genetic manipulation needed; can provide linkage information. | High cost of antibodies; potential for non-specific binding. |
| UBD-Based Enrichment (TUBEs) [48] [45] | Use of Tandem Ubiquitin Binding Entities (TUBEs) with high affinity for polyubiquitin chains to pull down ubiquitinated proteins. | Protects ubiquitin chains from deubiquitinases (DUBs); preserves labile ubiquitination; can be linkage-specific. | Requires optimization of binding and wash conditions. |
For proteasome inhibition studies, TUBEs are particularly valuable as they preserve the often-labile ubiquitin signatures that accumulate upon inhibition [48]. Furthermore, chain-specific TUBEs (e.g., K48- or K63-specific) enable researchers to delineate the specific type of polyubiquitin chain accumulated in response to proteasome inhibition, providing deeper mechanistic insight [48].
Key Reagents and Materials
Table 2: Essential Research Reagents for Ubiquitin Western Blotting
| Reagent / Material | Function / Application |
|---|---|
| Proteasome Inhibitors (e.g., MG132, Bortezomib) | Induce accumulation of polyubiquitinated proteins for detection. |
| Lysis Buffer (RIPA or NP-40 based) [49] | Extraction and solubilization of proteins while preserving ubiquitination. |
| Protease & Deubiquitinase (DUB) Inhibitors (e.g., N-Ethylmaleimide) | Prevent deubiquitination and protein degradation during sample preparation. |
| Tandem Ubiquitin Binding Entities (TUBEs) [48] [45] | High-affinity enrichment of polyubiquitinated proteins from cell lysates. |
| Primary Antibodies: Pan-Ubiquitin (e.g., P4D1), Linkage-specific (e.g., K48, K63) [45] | Detection of total or specific linkage types of ubiquitin chains. |
| Primary Antibodies: Anti-Ubiquitin (from various hosts) | Standard detection of ubiquitin in western blots. |
| Fluorescently-Labeled Secondary Antibodies [49] | Enable quantitative fluorescent western blotting (QFWB). |
| Total Protein Stain/Label (e.g., No-Stain Protein Labeling Reagent) [50] | For Total Protein Normalization (TPN), the gold standard for quantitation. |
| Pre-stained Molecular Weight Markers [49] | Essential for orientation and estimating molecular weights. |
Experimental Workflow and Protocols
Comprehensive Experimental Workflow
The following diagram illustrates the logical flow of a complete experiment designed to detect global ubiquitin levels in response to proteasome inhibition, from cell treatment to data analysis.
Detailed Protocols for Key Steps
Cell Treatment and Protein Extraction
- Treatment: Treat cells with a proteasome inhibitor (e.g., 10-20 μM MG132) or vehicle control (e.g., DMSO) for a predetermined time (typically 4-8 hours).
- Lysis: Lyse cells in an appropriate volume of RIPA buffer (25 mM Tris-HCl pH 7.6, 150 mM NaCl, 1% NP-40, 1% sodium deoxycholate, 0.1% SDS) or NP-40 lysis buffer, supplemented with a complete protease inhibitor cocktail and 1-10 mM N-Ethylmaleimide (NEM) to inhibit DUBs [49] [45].
- Clarification: Centrifuge lysates at 20,000 x g for 20 minutes at 4°C. Collect the supernatant containing solubilized proteins.
- Quantification: Determine protein concentration using a compatible assay (e.g., BCA or Bradford). Ensure all samples are compared against the same standard curve with an R-squared value ≥ 0.99 [49].
Electrophoresis and Transfer
- Sample Preparation: Dilute protein lysates (typically 15-30 μg per lane) in loading buffer. Heat at 98°C for 2 minutes [49].
- Gel Loading: Load samples and a pre-stained protein ladder onto a 4-12% Bis-Tris gradient gel. Use MES running buffer for optimal resolution of proteins between 3.5-160 kDa [49].
- Electrophoresis: Run the gel at 80 V for 4 minutes, then increase to 180 V for approximately 50 minutes, or until the dye front reaches the bottom.
- Transfer: Transfer proteins to a nitrocellulose or PVDF membrane using a standard wet or semi-dry transfer system.
Immunodetection and Quantitative Fluorescent Western Blotting (QFWB)
For truly quantitative results, a fluorescent detection method is superior to chemiluminescence (ECL) due to its linear dynamic range [49].
- Blocking: Block the membrane with a suitable blocking buffer (e.g., Odyssey Blocking Buffer) for 1 hour at room temperature.
- Primary Antibody Incubation: Incubate with primary antibodies diluted in blocking buffer overnight at 4°C. A typical panel includes:
- Pan-ubiquitin antibody (e.g., mouse P4D1) to detect total ubiquitinated proteins.
- Linkage-specific antibodies (e.g., K48-linkage or K63-linkage specific).
- Optional Housekeeping Protein (H KP) antibody (e.g., GAPDH, β-Actin), though TPN is preferred.
- Secondary Antibody Incubation: Incubate with fluorescently-labeled secondary antibodies (e.g., IRDye 680LT or 800CW) diluted in blocking buffer for 1 hour at room temperature, protected from light.
- Total Protein Normalization (TPN): Perform TPN by staining the membrane with a total protein stain (e.g., No-Stain Protein Labeling Reagent) according to the manufacturer's protocol. TPN is now considered the gold standard for normalization as it accounts for loading variations more reliably than HKPs, which can vary with experimental conditions [50].
- Imaging: Image the membrane using a fluorescent imaging system (e.g., LI-COR Odyssey, iBright Imaging System) at a resolution of at least 169-174 dpi (equivalent to 300 dpi at final print size) [51] [50]. Acquire images in the 700 nm and 800 nm channels.
Data Analysis, Normalization, and Presentation
Quantification and Normalization Strategy
- Signal Quantification: Use the imaging system's software to quantify the band or lane intensities for your target signals (ubiquitin smears/specific bands) and the total protein stain.
- Normalization: Normalize the ubiquitin signal to the total protein signal from the same lane. This corrects for any minor loading inaccuracies. The formula is:
Normalized Ubiquitin Level = (Ubiquitin Signal Intensity) / (Total Protein Signal Intensity for the same lane)
- Data Presentation: Compare the normalized ubiquitin levels between the proteasome-inhibited samples and the control samples. Data can be presented as fold-change relative to the control.
Table 3: Comparison of Western Blot Normalization Methods
| Method | Principle | Advantages | Disadvantages |
|---|---|---|---|
| Total Protein Normalization (TPN) [50] | Normalizes target protein signal to the total protein in the lane. | Not affected by experimental manipulations; larger dynamic range; superior accuracy; increasingly required by journals. | Requires an extra staining/labeling step. |
| Housekeeping Protein (HKP) Normalization [50] | Normalizes target protein signal to a constitutively expressed protein (e.g., GAPDH, Actin). | Widely used and familiar. | HKP expression can vary with cell type, treatment, and disease; signal saturation is common; narrow linear range. |
Publication Guidelines and Data Integrity
Adherence to journal-specific publication guidelines is critical. Key universal requirements include:
- Image Capture: Capture original, unmanipulated images at a minimum of 300 dpi resolution and at least 190 mm wide [51] [50].
- Data Manipulation: Adjustments to brightness/contrast must be applied evenly across the entire image and must not obscure, eliminate, or misrepresent any information present in the original. Non-linear adjustments should be avoided and must be disclosed if used [51] [50].
- Figure Preparation: Avoid excessive cropping. All important bands and molecular weight markers must be visible. Spliced lanes from different parts of the same gel or different gels must be clearly indicated with dividing lines in the figure [51] [50].
- Data Availability: Many journals, including those from the Nature portfolio, require that original, unprocessed images of all blots be published as Supplementary Information [51].
Troubleshooting Common Issues
- High Background: Optimize antibody concentrations and increase the number and stringency of washes.
- Weak or No Signal: Confirm antibody specificity and activity. Increase protein load or primary antibody incubation time. Ensure the proteasome inhibitor was active.
- Smearing of Ubiquitin Signal: This is expected, as ubiquitinated proteins form a heterogeneous population of different molecular weights. The "smear" is a key characteristic of global ubiquitination. However, over-transfer can also cause smearing; ensure optimal transfer conditions.
- Poor Reproducibility: Implement TPN instead of HKP normalization. Use analytical replication by running samples in duplicate or triplicate across multiple gels to account for gel-to-gel variation [52].
Western blot analysis remains a cornerstone technique for detecting global ubiquitin levels and polyubiquitinated proteins in the study of proteasome inhibition. The successful application of this method relies on careful experimental design, robust sample preparation with appropriate controls, the use of enrichment tools like TUBEs for sensitive detection, and the adoption of quantitative fluorescent detection coupled with total protein normalization. By following the detailed protocols, data analysis frameworks, and publication guidelines outlined in this whitepaper, researchers can generate reliable, reproducible, and publication-ready data that accurately reflects the impact of proteasome inhibition on cellular ubiquitin homeostasis.
The ubiquitin-proteasome system (UPS) serves as the primary pathway for selective intracellular protein degradation in eukaryotic cells, playing a critical role in maintaining protein homeostasis (proteostasis) and regulating numerous cellular processes including cell cycle progression, stress responses, and DNA repair [53]. This sophisticated system involves a cascade of enzymatic reactions: ubiquitin is first activated by an E1 enzyme, transferred to an E2 conjugating enzyme, and finally delivered to target proteins via E3 ligases, forming polyubiquitin chains that mark substrates for degradation by the 26S proteasome [53]. The proteasome itself consists of a 20S catalytic core particle capped by 19S regulatory particles that recognize ubiquitinated proteins [53]. Given its central role in controlling protein turnover, pharmacological inhibition of the UPS has emerged as a powerful strategy for investigating its function and as a therapeutic approach for cancers such as multiple myeloma [53].
MG-132 (carbobenzoxyl-L-leucyl-L-leucyl-leucinal) is a potent, reversible proteasome inhibitor that primarily targets the chymotrypsin-like activity of the β-subunit of the 20S proteasome core [54]. As a pharmacological probe, MG-132 has proven invaluable for elucidating UPS function by inducing the accumulation of polyubiquitinated proteins and disrupting proteostasis, thereby allowing researchers to study the consequences of impaired protein degradation on cellular signaling pathways, stress responses, and viability [54] [55]. This technical guide examines the mechanistic basis, experimental applications, and methodological considerations for employing MG-132 in UPS research, with particular emphasis on its utility within investigations exploring the impact of proteasome inhibition on cellular ubiquitin dynamics.
Mechanism of Action of MG-132
Molecular Targeting and Proteasome Inhibition
MG-132 functions as a peptide aldehyde that specifically inhibits the proteasome's chymotrypsin-like activity by targeting the β-subunit of the 20S catalytic core [54]. This inhibition prevents the degradation of polyubiquitinated proteins, leading to their rapid intracellular accumulation and disruption of protein homeostasis. Within hours of treatment, MG-132 causes a dose-dependent increase in polyubiquitinated proteins, which can be readily detected by western blot analysis using ubiquitin-specific antibodies [54] [55]. This accumulation creates a state of proteotoxic stress that triggers subsequent cellular responses, including the unfolded protein response (UPR) and apoptosis [55].
The specificity of MG-132 for the proteasome, while notable, is not absolute. At higher concentrations, MG-132 may also inhibit certain cysteine and calpain proteases, necessitating appropriate controls in experimental designs [54]. Nevertheless, its well-characterized proteasome inhibition profile makes it an excellent tool for investigating UPS function, particularly when used at optimized concentrations and with verification experiments using alternative proteasome inhibitors.
Signaling Pathway Alterations
MG-132 exerts profound effects on multiple cellular signaling pathways through the stabilization of key regulatory proteins that are normally rapidly turned over by the proteasome. Mechanistic studies in A375 melanoma cells have revealed that MG-132 displays dual regulatory capacity:
MDM2-p53 Pathway Modulation: MG-132 inhibits MDM2, leading to activation of the p53/p21/caspase-3 axis while simultaneously suppressing CDK2 and Bcl-2 expression. This cascade triggers cell cycle arrest and promotes DNA damage-mediated apoptosis [54].
MAPK Pathway Activation: MG-132 activates the MAPK pathway, which serves as a critical driver of apoptosis in response to proteasome inhibition. Western blot analyses have confirmed dose-responsive modulation of these molecular targets, demonstrating pathway specificity [54].
Table 1: Key Signaling Pathways Affected by MG-132-Induced Proteasome Inhibition
| Pathway | Effect | Functional Outcome | Experimental Validation |
|---|---|---|---|
| MDM2-p53 | Inhibition of MDM2, stabilization of p53 | Activation of p21, cell cycle arrest, apoptosis | Western blot, flow cytometry [54] |
| MAPK | Phosphorylation of MAPK components | Apoptosis induction | Western blot with phospho-specific antibodies [54] |
| Bcl-2/CDK2 | Downregulation | Reduced anti-apoptotic signaling, impaired cell cycle progression | Western blot, apoptosis assays [54] |
| Ubiquitin-Proteasome | Direct inhibition of 20S proteasome | Accumulation of polyubiquitinated proteins | Ubiquitin western blot, reporter assays [54] [55] |
The diagram below illustrates the core mechanism of MG-132 action and its downstream effects on key cellular pathways:
Experimental Approaches for Monitoring UPS Function
Assessing Cytotoxicity and Anti-Tumor Activity
Determining the cytotoxic profile of MG-132 is a fundamental first step in establishing appropriate experimental conditions. The CCK-8 assay provides a reliable method for quantifying cell viability and calculating inhibitor potency:
Protocol: CCK-8 Cytotoxicity Assay
- Seed target cells (e.g., A375, MCF-7, HeLa) in 96-well plates at 70-80% confluence [54].
- Treat with serial dilutions of MG-132 (typical range: 0.1-10 μM) for 8, 12, 24, and 48 hours, including DMSO vehicle controls [54].
- Add CCK-8 reagent and incubate for 1-4 hours at 37°C [54].
- Measure absorbance at 450 nm using a plate reader [54].
- Calculate IC50 values using non-linear regression analysis of dose-response curves [54].
In A375 melanoma cells, MG-132 demonstrates potent anti-tumor activity with a calculated IC50 of 1.258 ± 0.06 μM [54]. Similar cytotoxicity has been observed across various cancer cell lines, underscoring its broad applicability in oncology research.
Apoptosis and Cell Cycle Analysis
Flow cytometry-based apoptosis assays provide quantitative data on cell death mechanisms triggered by proteasome inhibition:
Protocol: Annexin V/PI Apoptosis Assay
- Seed cells in 6-well plates and treat with MG-132 (0.5, 1, 2 μM) for 24 hours [54].
- Collect cells by gentle trypsinization and centrifugation [54].
- Resuspend in binding buffer containing Annexin V-FITC and propidium iodide (PI) [54].
- Incubate for 15 minutes in the dark at room temperature [54].
- Analyze by flow cytometry within 1 hour, using appropriate fluorescence channels [54].
- Analyze data using FlowJo software, distinguishing early apoptotic (Annexin V+/PI-), late apoptotic (Annexin V+/PI+), and necrotic (Annexin V-/PI+) populations [54].
MG-132 induces concentration-dependent apoptosis, with 2 μM treatment resulting in early apoptosis in 46.5% of cells and total apoptotic response in 85.5% of A375 cells within 24 hours [54]. Complementary cell cycle analysis through DNA content measurement (using PI staining and RNase treatment) typically reveals G1 or G2/M phase arrest, consistent with the activation of checkpoint controls [54].
Table 2: Quantitative Effects of MG-132 on A375 Melanoma Cells
| Parameter | Concentration | Exposure Time | Effect | Measurement Method |
|---|---|---|---|---|
| Viability (IC50) | 1.258 ± 0.06 μM | 48 hours | 50% growth inhibition | CCK-8 assay [54] |
| Early Apoptosis | 2 μM | 24 hours | 46.5% Annexin V+/PI- | Flow cytometry [54] |
| Total Apoptosis | 2 μM | 24 hours | 85.5% combined apoptotic cells | Flow cytometry [54] |
| Migration | 0.125-0.5 μM | 24 hours | Significant suppression | Wound healing assay [54] |
| Ubiquitinated proteins | 0.5-2 μM | 24 hours | Dose-dependent accumulation | Western blot [54] |
Monitoring Protein Ubiquitination and Turnover
Direct assessment of UPS inhibition involves monitoring the accumulation of polyubiquitinated proteins and stabilization of short-lived regulatory proteins:
Protocol: Western Blot Analysis of Ubiquitinated Proteins
- Treat cells (2×10⁴/well in 6-well plates) with MG-132 (0.5, 1, 2 μM) for 24 hours [54].
- Lyse cells in denaturing buffer (e.g., 50 mM Tris-HCl pH 7.4, 150 mM NaCl, 1% Triton X-100, 20 mM NaF, 2 mM Na₃VO₄, 0.1 mM leupeptin, 2 mM PMSF) to preserve ubiquitination states [54].
- Resolve proteins by 10% SDS-PAGE and transfer to PVDF membranes [54].
- Block with 5% skimmed milk for 2 hours at room temperature [54].
- Incubate with primary antibodies (e.g., anti-ubiquitin, anti-p53, anti-β-actin) overnight at 4°C [54].
- Incubate with HRP-conjugated secondary antibodies for 1 hour at room temperature [54].
- Develop using ECL luminescent reagent and image with a chemiluminescence analyzer [54].
Advanced methodologies for comprehensive ubiquitinome assessment have emerged, employing monoclonal antibodies that recognize diglycine (diGly) remnants following trypsin digestion of ubiquitinated proteins. This approach allows for systematic identification and quantification of ubiquitination sites, with recent studies identifying approximately 19,000 diGly-modified lysine residues within ~5,000 proteins [56]. Quantitative diGly proteomics following MG-132 treatment reveals temporal changes in site abundance, with approximately 58% of quantified sites increasing by more than 2-fold after proteasome inhibition [56].
Functional Consequences: Migration and Protein Homeostasis Assays
Protocol: Wound Healing Migration Assay
- Culture A375 cells in 6-well plates for 24 hours to form confluent monolayers [54].
- Create a scratch "wound" using a sterile pipette tip [54].
- Wash away detached cells and add fresh serum-free medium containing MG-132 (0.125, 0.25, 0.5 μM) [54].
- Capture images at 0, 12, and 24 hours using an inverted microscope [54].
- Quantify migration distance or wound closure percentage using ImageJ software [54].
MG-132 significantly suppresses cellular migration at subtoxic concentrations (0.125-0.5 μM), demonstrating its anti-metastatic potential [54]. For monitoring protein homeostasis disruption, recent approaches combine MG-132 with other agents like propolin G to synergistically induce proteotoxic stress, significantly reducing proteasome activity and activating the PERK/ATF4/CHOP signaling pathway and autophagy [55].
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Research Reagents for MG-132 Experiments
| Reagent/Category | Specific Examples | Function/Application | Considerations |
|---|---|---|---|
| Proteasome Inhibitors | MG-132 (CAS 133407-82-6), Bortezomib, Carfilzomib | Induce accumulation of polyubiquitinated proteins, study UPS function | MG-132 reversible; Carfilzomib irreversible; different specificity profiles [54] [57] |
| Cell Lines | A375 melanoma, HeLa, MCF-7, HCT116, 293T | Model systems for studying UPS inhibition | Varying sensitivity (IC50 1.258 μM for A375); tissue-specific responses [54] [56] |
| Apoptosis Detection | Annexin V-FITC/PI kits, caspase inhibitors (Q-VD-OPh) | Quantify apoptotic vs. necrotic cell death | Distinguish early (Annexin V+/PI-) and late (Annexin V+/PI+) apoptosis [54] |
| Protein Analysis | Ubiquitin antibodies, HRP-conjugated secondaries, ECL reagents | Detect ubiquitinated proteins, pathway effectors | Use denaturing lysis to preserve ubiquitination state; β-actin loading control [54] |
| Pathway Reporters | Ub-YFP, Ub-R-GFP, ZsGreen-ODC | Real-time monitoring of UPS function in live cells | Fluorescent substrates for proteasome activity [22] |
| Proteasome Activity Assays | Fluorogenic substrates (Suc-LLVY-AMC) | Direct measurement of proteasome catalytic activity | Distinguish chymotrypsin-like, caspase-like, trypsin-like activities [57] |
Advanced Applications and Integration with Other Techniques
Combination Studies with Other Therapeutic Agents
MG-132 has demonstrated synergistic effects when combined with other anti-cancer compounds, enhancing proteotoxic stress and expanding its research applications. In breast cancer models, combination treatment with MG-132 (1 μM) and propolin G (10 μM) resulted in synergistic suppression of proliferation and induction of apoptosis, as indicated by a combination index (CI) of 0.63 [55]. This combination significantly reduced proteasome activity, leading to accumulation of polyubiquitinated proteins and activation of both the PERK/ATF4/CHOP signaling pathway and autophagy-mediated cell death [55].
The experimental workflow for such combination studies typically involves:
- Determining individual agent IC50 values
- Testing combinations at fixed ratios based on IC50
- Calculating combination indices using the Chou-Talalay method
- Mechanistic validation through pathway analysis
CRISPR-Based Screening for Mechanism Elucidation
Genome-wide CRISPR screening has emerged as a powerful approach for identifying novel mediators of MG-132 activity. In one such screen, the redox enzyme NAD(P)H:quinone oxidoreductase 1 (NQO1) was identified as a critical mediator of the bioactivatable UPS inhibitor CBK77 [22], highlighting how similar approaches could be applied to MG-132 mechanism studies. The general workflow includes:
- Generating Cas9-expressing cell lines
- Transducing with genome-wide sgRNA libraries
- Selecting with MG-132 treatment
- Sequencing surviving cells to identify enriched/depleted sgRNAs
- Validating hits through individual knockout experiments
Quantitative Ubiquitinome Profiling
Advanced mass spectrometry-based techniques now enable quantitative assessment of changes in the ubiquitinome following MG-132 treatment. The methodology involves:
- Metabolic labeling with heavy lysine (SILAC or related approaches)
- MG-132 treatment (typically 1-10 μM for 2-24 hours)
- Denaturing lysis to preserve ubiquitination states
- Trypsin digestion to generate diGly remnants
- Immunoaffinity enrichment of diGly-containing peptides
- LC-MS/MS analysis and quantitative profiling [56]
This approach has revealed that approximately 58% of quantified ubiquitination sites increase by more than 2-fold following proteasome inhibition, while about 13% decrease by similar magnitudes, indicating complex remodeling of the ubiquitinome beyond simple accumulation [56].
MG-132 remains an indispensable pharmacological probe for investigating ubiquitin-proteasome system function, offering researchers a well-characterized means to induce proteotoxic stress and study subsequent cellular responses. Its defined mechanism of action, concentration-dependent effects on apoptosis and cell cycle progression, and compatibility with diverse experimental endpoints make it particularly valuable for both basic research and drug discovery applications. When employing MG-132 in UPS studies, researchers should carefully consider dose-response relationships, temporal dynamics of inhibition, and appropriate verification experiments to ensure specific interpretation of results. As quantitative proteomic and genetic screening technologies continue to advance, MG-132 will undoubtedly maintain its position as a fundamental tool for elucidating the complexities of cellular protein homeostasis.
The ubiquitin-proteasome system (UPS) represents a complex network of enzymes and signaling pathways responsible for controlled protein degradation and the maintenance of cellular homeostasis. Traditional methods for identifying UPS modulators have primarily focused on direct enzyme inhibition. However, emerging strategies now explore more sophisticated approaches, including bioactivatable inhibitors that leverage intracellular enzymes for activation and the groundbreaking discovery of small molecules that act as direct substrates for ubiquitination. This technical guide examines cutting-edge screening methodologies that are expanding our understanding of UPS modulation, with particular emphasis on their implications for cellular ubiquitin dynamics and proteasome function. These innovative approaches are revealing novel therapeutic opportunities for diseases characterized by proteotoxic stress, including cancer and neurodegenerative disorders.
The ubiquitin-proteasome system comprises an elaborate enzymatic cascade that regulates protein turnover through the covalent attachment of ubiquitin to substrate proteins. This system involves E1 activating enzymes, E2 conjugating enzymes, E3 ligases (numbering over 600 in humans), deubiquitinating enzymes (DUBs, approximately 100), and the proteasome itself [58] [59]. The complexity of this system offers numerous potential targets for therapeutic intervention, yet also presents significant challenges for specific modulation.
Traditional UPS drug discovery has primarily employed high-throughput screening (HTS) of large compound libraries against predefined molecular targets. However, this approach has limitations, particularly in identifying compounds with novel mechanisms of action or those requiring intracellular bioactivation. Recent advances have shifted toward more sophisticated phenotypic screening strategies that can uncover unexpected mechanisms, including bioactivatable compounds that are transformed into active inhibitors by cellular enzymes and small molecules that directly participate in the ubiquitination cascade [22] [17].
Research into proteasome inhibition has consistently demonstrated a direct impact on cellular ubiquitin levels, as impaired degradation capacity leads to accumulation of ubiquitinated proteins and depletion of free ubiquitin pools. This relationship positions ubiquitin homeostasis as a critical indicator of UPS function and a valuable biomarker in screening campaigns for novel UPS modulators.
Bioactivatable UPS Inhibitors
Mechanism of Bioactivation
Bioactivatable UPS inhibitors are compounds that require enzymatic transformation within the cell to exert their inhibitory effects on the UPS. Unlike direct inhibitors, these prodrug-like molecules leverage the intracellular environment of specific cell types, particularly cancer cells, for selective activation, offering potential therapeutic windows.
One identified mechanism involves the enzyme NAD(P)H:quinone oxidoreductase 1 (NQO1), which is frequently overexpressed in malignant cells. The compound CBK77 serves as a prototype for this class, requiring NQO1-mediated bioactivation to inhibit the UPS effectively [22]. Genome-wide CRISPR interference screens have validated NQO1 as the critical activator, where genetic ablation of NQO1 confers resistance to CBK77, while overexpression sensitizes cells to its effects.
Screening Methodologies for Bioactivatable Inhibitors
Identification of bioactivatable UPS inhibitors employs phenotypic screening approaches that monitor UPS function in living cells. Key methodological components include:
Reporter Cell Lines: Engineered cell lines expressing ubiquitin-dependent degradation reporters, such as Ub-YFP, Ub-R-GFP, YFP-CL1, and ZsGreen-ODC, enable quantitative assessment of proteasomal activity through fluorescence measurement [22].
Functional Endpoints: Primary screens typically measure accumulation of ubiquitinated proteins via western blotting or reporter fluorescence, followed by secondary assays assessing cell viability, caspase activation, and global protein synthesis.
CRISPR-Based Target Deconvolution: Genome-wide CRISPR-Cas9 knockout or interference screens identify genes essential for compound activity, as demonstrated by the identification of NQO1 as the activator for CBK77 [22].
Table 1: Key Assays for Identifying Bioactivatable UPS Inhibitors
| Assay Type | Measured Parameters | Applications |
|---|---|---|
| Reporter Accumulation | Fluorescence intensity of UPS reporters | Primary high-throughput screening |
| Immunoblotting | Polyubiquitinated protein accumulation | Secondary confirmation |
| CRISPR Screens | Gene essentiality for compound activity | Target identification |
| Viability Assays | IC50 determination, caspase activation | Cytotoxicity profiling |
| Enzymatic Assays | NQO1 activity, proteasome activity | Mechanistic studies |
Experimental Protocol: CRISPR Screen for Bioactivatable UPS Inhibitors
The following protocol outlines the key steps for identifying mediators of bioactivatable UPS inhibitor activity:
Generate Reporter Cell Line: Stably express a UPS degradation reporter (e.g., Ub-GFP) in human cancer cells (e.g., MelJuSo) [22].
Establish CRISPR Platform: Introduce stable Cas9 expression via lentiviral transduction and selection with blasticidin.
Perform Genome-wide Screen: Transduce cells with a genome-wide sgRNA library at low MOI (≈0.3) followed by puromycin selection.
Compound Treatment: Treat cells with the bioactivatable compound at predetermined concentrations (e.g., IC50-IC80).
FACS Analysis and Sorting: Isolate resistant populations based on reporter fluorescence (e.g., GFP-high for UPS inhibitors).
Sequencing and Hit Identification: Extract genomic DNA, amplify sgRNA regions, and sequence to identify enriched sgRNAs.
Validation: Confirm candidate genes using individual sgRNAs and orthogonal assays.
Small-Molecule Substrates for Ubiquitination
Discovery of Ubiquitinated Small Molecules
A paradigm-shifting discovery in UPS research emerged with the identification of BRD1732, a small molecule that undergoes direct ubiquitination in cells [17]. This finding challenges the long-standing paradigm that ubiquitination is exclusively restricted to protein substrates and reveals a novel mechanism of UPS inhibition.
BRD1732 is a synthetic compound featuring an azetidine scaffold identified from a diversity-oriented synthesis (DOS) library. Its cytotoxicity is stereospecific, with the (2S,3R,4R) stereoisomer demonstrating potent activity (IC50 1-3 µM) while stereoisomers show 10-40-fold reduced potency [17]. This stereospecificity suggests a specific interaction with biological macromolecules.
Mechanism of Small-Molecule Ubiquitination
Ubiquitination of BRD1732 occurs through a canonical enzymatic cascade, despite the non-protein nature of the substrate:
Enzyme Requirements: Genetic screens revealed that BRD1732 ubiquitination depends on the E3 ubiquitin ligases RNF19A and RNF19B and their shared E2 conjugating enzyme UBE2L3 [17].
Site of Modification: Structure-activity relationship studies using methylated analogs demonstrated that ubiquitination occurs specifically at the azetidine secondary amine, not the primary alcohol [17].
Conjugate Structure: Mass spectrometry analysis confirmed a covalent linkage between the C-terminus of ubiquitin and BRD1732, with a measured mass increase of 387 Da corresponding to ubiquitin-BRD1732 minus water [17].
Cellular Consequences: BRD1732 ubiquitination leads to dramatic accumulation of mono- and di-ubiquitin conjugates, depletion of free ubiquitin, and impairment of ubiquitin-dependent proteasomal degradation.
Screening Approaches for Ubiquitinable Small Molecules
Identification of small molecules that undergo ubiquitination requires specialized screening approaches:
Phenotypic Screening: DOS libraries are screened for compounds causing ubiquitin accumulation, as detected by western blotting with anti-ubiquitin antibodies.
Genetic Dependency Mapping: Genome-wide CRISPR resistance screens identify E3 ligases and E2 enzymes required for compound activity.
Metabolic Profiling: Affinity purification of ubiquitin conjugates followed by LC-MS analysis detects unusual ubiquitin adducts.
Chemoproteomic Approaches: Activity-based protein profiling can identify small molecules that interact with ubiquitination machinery.
Table 2: Characteristics of Ubiquitinated Small Molecules
| Property | BRD1732 | Traditional UPS Inhibitors |
|---|---|---|
| Molecular Target | Becomes ubiquitination substrate | Binds directly to UPS enzymes |
| Ubiquitin Fate | Accumulates as conjugates | Accumulates as free ubiquitin or chains |
| Genetic Requirements | RNF19A/B, UBE2L3 | Varies by specific inhibitor |
| Stereospecificity | High (>10-fold) | Variable |
| Cellular Phenotype | Ubiquitin conjugate accumulation | Ubiquitinated protein accumulation |
Diagram 1: Mechanism of BRD1732 Ubiquitination and UPS Inhibition. The small molecule BRD1732 is recognized by the E2 enzyme UBE2L3 and E3 ligases RNF19A/B, leading to its direct ubiquitination. The resulting ubiquitin-BRD1732 conjugate accumulation inhibits the UPS, causing cytotoxicity.
Advanced Screening Technologies
Fragment-Based Drug Discovery for the UPS
Fragment-based drug discovery (FBDD) has emerged as a powerful alternative to HTS for targeting UPS components. FBDD utilizes small molecular fragments (MW <300 Da) that cover chemical space more efficiently than traditional drug-like compounds [59].
Key advantages of FBDD for UPS targets include:
Improved Ligand Efficiency: Fragments typically have higher binding efficiency per atom, providing better starting points for optimization.
Covalent Fragment Screening: Electrophilic "warheads" (e.g., acrylamides, chloroacetamides) enable targeting of catalytic cysteines in DUBs and E3 ligases.
Structural Insights: Crystallographic screening platforms like XChem provide direct structural information on fragment binding.
Successful applications of FBDD to the UPS include the development of inhibitors for E1 enzymes, E2 enzymes, E3 ligases, and DUBs [59].
CRISPR-Based Screening for E3 Ligase Discovery
CRISPR-based screening approaches have revolutionized the identification of E3 ligases capable of supporting targeted protein degradation. A novel CRISPR activation screen identified FBXO22 as an E3 ligase that supports heterobifunctional compound-mediated target degradation when transcriptionally activated [60].
The experimental workflow involves:
Cell Line Engineering: Generate cells expressing the target protein (e.g., FKBP12-EGFP) along with dCas9-VP64 and MS2-P65-HSF1 transcriptional activation systems.
Focused sgRNA Library: Design sgRNAs targeting promoter regions of approximately 680 human E3 ligases.
Activation and Selection: Transduce cells with the sgRNA library, treat with candidate PROTACs, and sort cells showing enhanced degradation.
Hit Validation: Confirm E3 ligase involvement using individual sgRNAs and functional degradation assays.
This approach successfully identified FBXO22 as an E3 ligase that supports degradation of multiple substrates when engaged by electrophilic PROTACs [60].
Diagram 2: CRISPR Activation Screening for E3 Ligase Discovery. An sgRNA library targeting E3 ligase promoters enables CRISPR-mediated transcriptional activation. Enhanced E3 expression facilitates PROTAC-mediated target degradation, identifying functional E3 ligases for targeted protein degradation.
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Research Reagents for Novel UPS Screening Approaches
| Reagent/Cell Line | Application | Key Features |
|---|---|---|
| Ubiquitin Reporters (Ub-GFP, Ub-R-GFP, YFP-CL1) | Monitoring UPS activity in live cells | Quantifiable fluorescence, tunable degradation kinetics |
| CRISPR Activation System (dCas9-VP64, MS2-P65-HSF1) | E3 ligase discovery | Enhanced transcriptional activation, compatible with pooled screens |
| DOS Libraries | Identifying ubiquitinable small molecules | 3D complexity, diverse stereochemistry, novel scaffolds |
| Linkage-Specific Ub Antibodies | Detecting specific ubiquitin chain types | Specificity for K48, K63, M1, and other linkages |
| NQO1-Expressing Cell Lines | Bioactivatable compound screening | Model for cancer-selective activation, validated bioactivation platform |
| Tandem UBD Affinity Reagents | Enriching ubiquitinated proteins/compounds | High affinity for ubiquitin conjugates, reduced background |
The landscape of UPS screening is evolving beyond traditional inhibition approaches to encompass novel mechanisms including bioactivatable inhibitors and small-molecule substrates. These innovative strategies leverage advanced technologies such as CRISPR screening, fragment-based discovery, and diversity-oriented synthesis to explore previously inaccessible areas of UPS biology. The discovery that small molecules can serve as direct substrates for ubiquitination represents a paradigm shift with profound implications for both basic research and therapeutic development. As these approaches mature, they promise to unlock new opportunities for targeting the UPS in diseases characterized by proteotoxic stress, while providing powerful tools for fundamental research into ubiquitin biology. Future directions will likely focus on expanding the repertoire of E3 ligases that can be harnessed for targeted degradation, developing increasingly selective bioactivatable compounds, and exploring the full potential of small-molecule ubiquitination as a therapeutic strategy.
Navigating Complexities: Challenges and Refinements in UPS Research and Therapy
Within the context of proteasome inhibition research, a central challenge persists: differentiating the specific degradation of a target protein from global perturbations to the ubiquitin-proteasome system (UPS). Proteasome inhibitors, while invaluable tools, trigger complex compensatory and indirect effects that can obfuscate interpretation. This technical guide outlines rigorous experimental methodologies and critical pitfalls to accurately delineate specific degradation events from system-wide UPS alterations, enabling more precise target validation and therapeutic development.
Quantitative Profiling of the Ubiquitinome: A Systems View
Proteasome inhibition causes a massive restructuring of the cellular ubiquitin landscape, or "ubiquitinome." Comprehensive quantitative assessment is essential to understand the global scale of these changes and to identify specific, regulated substrates.
Key Experimental Methodology: diGly Capture and Quantitative Proteomics
The most robust method for system-wide profiling relies on immunoprecipitation of peptides containing the diglycine (diGly) remnant, which remains on lysine residues after tryptic digestion of ubiquitylated proteins [56]. This is coupled with quantitative mass spectrometry.
Detailed Protocol:
- Cell Culture and Metabolic Labeling: Grow two populations of cells (e.g., HCT116 or 293T). Culture one population in "light" media containing natural abundance lysine (K0) and the other in "heavy" media containing stable isotope-labeled lysine (K8, Lys +8 Da) [56].
- Experimental Perturbation: Treat the "heavy" population with the proteasome inhibitor (e.g., 1µM Bortezomib for 8 hours). The "light" population serves as an untreated control [56].
- Cell Lysis and Protein Digestion: Mix the cell populations in a 1:1 ratio. Lyse cells in a denaturing buffer (e.g., SDS) to instantly inactivate deubiquitylating enzymes (DUBs) and preserve the ubiquitin-modified proteome. Digest the combined protein extract with trypsin [56].
- Enrichment of diGly-Modified Peptides: Use a monoclonal antibody specific for the diGly-Lys remnant to immunoprecipitate ubiquitylated peptides. Perform multiple sequential immunoprecipitations (e.g., 4x) to maximize depth of coverage [56].
- LC-MS/MS and Data Analysis: Analyze the enriched peptides by liquid chromatography coupled to tandem mass spectrometry (LC-MS/MS). The relative abundance of specific ubiquitylation sites is determined by comparing the heavy-to-light (H:L) ratio of the peptide pairs. Bioinformatic analysis identifies sites that significantly increase or decrease upon inhibition [56].
Quantitative Insights from Global Ubiquitinome Analysis
Application of this methodology reveals the extensive scope of UPS remodeling. One study identified approximately 19,000 diGly-modified lysine residues within ~5,000 proteins in response to proteasome inhibition [56]. Quantitative analysis shows that not all ubiquitylation events are equivalent.
Table 1: Quantitative Changes in the Ubiquitinome Following Proteasome Inhibition
| Metric of Change | Quantitative Finding | Technical Implication |
|---|---|---|
| Overall Site Regulation | ~58% of sites increased >2-fold; ~13% decreased >2-fold [56]. | Inhibition has a net stabilizing effect but also triggers active deubiquitylation of a protein subset. |
| Linkage-Type Dynamics | K11, K29, and K48 linkages increased >2-fold; K63 linkages were largely unaffected [56]. | Specific ubiquitin chain types are preferentially involved in proteasomal targeting. |
| Multi-site Protein Regulation | In 60% of proteins with multiple sites, individual lysines showed divergent regulation (≥2-fold increase and decrease) [56]. | Ubiquitylation sites on a single protein can be functionally distinct; site-specific quantification is critical. |
| Inhibitor Specificity | 92% of sites increased by Bortezomib were also increased by Epoxomycin [56]. | Observed effects are due to proteasome inhibition itself, not inhibitor-specific off-target effects. |
Discerning Specific Substrates from Global Effects
With the global ubiquitinome mapped, the next challenge is to determine which accumulating proteins are direct proteasome substrates and which are indirect consequences of the inhibition.
Experimental Workflow for Substrate Validation
The following diagram outlines a logical pathway for progressing from initial observation to validated substrate, incorporating key validation steps to avoid common pitfalls.
Pitfall 1: Misinterpreting Indirect Stabilization
A protein may accumulate post-inhibition not because it is a direct substrate, but because a stabilizing protein that is a proteasome substrate is itself being stabilized. This is a classic indirect effect.
Mitigation Protocol: Cycloheximide Chase to Measure Half-Life
- Treat cells with cycloheximide to halt de novo protein synthesis.
- Harvest cells at multiple time points (e.g., 0, 1, 2, 4, 8 hours) after cycloheximide addition.
- In parallel, repeat the time course in the presence of a proteasome inhibitor.
- Quantify the protein of interest by immunoblotting. A direct substrate will show a significantly extended half-life only in the presence of the proteasome inhibitor. If the half-life remains short despite inhibition, its accumulation is likely indirect [56].
Pitfall 2: Overlooking E3 Ligase Specificity
The accumulation of a ubiquitylated protein upon proteasome inhibition does not automatically identify its regulating E3 ligase. The system contains significant redundancy.
Mitigation Protocol: Genetic Validation of E3 Ligase Involvement
- CRISPR-Cas9 Screening: A genome-wide CRISPR screen can identify E3 ligases (or other UPS components) whose loss confers resistance to the accumulation or toxicity phenotype. For instance, sgRNAs targeting RNF19A and RNF19B were enriched in cells treated with a specific compound, identifying these E3s as essential for its mechanism of action [17].
- Focused Knockdown/Knockout: Use siRNA, shRNA, or CRISPR to individually deplete candidate E3 ligases in cells. A true specific substrate will show reduced ubiquitylation and stabilized half-life upon knockdown of its cognate E3 ligase. As demonstrated in yeast, knockout of the ubiquitin receptor Rpn10 led to the accumulation of specific ubiquitylated substrates, defining its unique repertoire [61].
Pitfall 3: Confounding UBL Modifications
The diGly remnant is not exclusive to ubiquitin. The ubiquitin-like modifiers (UBLs) NEDD8 and ISG15 also generate diGly signatures upon trypsinization.
Mitigation Protocol: Distinguishing Ubiquitin from NEDD8/ISG15 Modifications
- ISG15: Assess expression levels via immunoblotting. ISG15 is typically absent in unstimulated cells [56].
- NEDD8 vs. Ubiquitin: Treat cell lysates with the catalytic domain of USP2 (USP2cc), a deubiquitylating enzyme that selectively removes ubiquitin but does not affect NEDD8 conjugates.
- Incubate lysate with USP2cc prior to trypsin digestion and diGly enrichment.
- A ≥50% reduction in the H:L ratio of a diGly peptide after USP2cc treatment confirms it is a ubiquitin modification. Retention of the signal indicates a NEDD8 modification (e.g., neddylated CUL1) [56].
The Scientist's Toolkit: Essential Research Reagents
Table 2: Key Reagents for Differentiating Specific from Global UPS Degradation
| Reagent / Tool | Function | Application in Specificity Research |
|---|---|---|
| Proteasome Inhibitors (Bortezomib, Carfilzomib, MG132) | Reversibly or irrereversibly block the proteasome's proteolytic activity. | Used to trigger global accumulation of ubiquitylated proteins and identify potential substrates [56] [16]. |
| α-diGly Remnant Antibody | Monoclonal antibody for immunoprecipitating tryptic peptides derived from ubiquitylated proteins. | Core reagent for quantitative ubiquitinome profiling via LC-MS/MS [56]. |
| USP2 Catalytic Domain (USP2cc) | Deubiquitylating enzyme that specifically cleaves ubiquitin chains but not NEDD8. | Critical for confirming that an observed diGly signal originates from ubiquitin and not the UBL NEDD8 [56]. |
| Cycloheximide | Inhibitor of protein translation. | Used in chase experiments to measure a protein's half-life independent of new synthesis [56]. |
| CRISPR-Cas9 Libraries | Enables genome-wide knockout screening. | Identifies E3 ligases and UPS components whose loss rescues a degradation phenotype, revealing specificity [17]. |
| Metabolic Labeling (SILAC) | Incorporation of stable isotopes into proteins for quantitative MS. | Allows precise comparison of protein and ubiquitin site abundance between control and treated samples [56] [61]. |
Case Study: Rescuing Pathogenic Pendrin Variants
Research on Pendred syndrome provides a clear example of distinguishing specific from global degradation. Pathogenic pendrin (SLC26A4) variants exhibit reduced expression due to premature degradation, not defective production. The key findings were [16]:
- Specific Ubiquitination: Wild-type and variant pendrin showed different ubiquitination patterns, with a specific pathogenic variant (p.R409H) ubiquitinated preferentially on lysine 77.
- Specific Pathway: Only proteasome inhibition (via clinical inhibitors like carfilzomib), and not lysosomal inhibition, rescued pendrin protein levels and ion transport function.
- Therapeutic Specificity: Carfilzomib specifically rescued the function of the p.R409H variant to wild-type levels, demonstrating a targeted rescue of a specific degradation event within the complex UPS environment.
Emerging Frontiers and Novel Mechanisms
Recent discoveries reveal even greater complexity. The finding that a small molecule (BRD1732) can be directly ubiquitinated on a secondary amine by the E2 enzyme UBE2L3 and E3 ligases RNF19A/B represents a novel mechanism that globally inhibits the UPS by sequestering ubiquitin [17]. This highlights a potential pitfall in screening campaigns where small-molecule effects can directly perturb the UPS machinery, leading to widespread downstream effects that can be mistaken for specific substrate stabilization.
Accurately distinguishing specific protein degradation from global UPS dysfunction demands a multi-faceted approach. Reliance solely on inhibitor-based accumulation is insufficient. Robust conclusions require the integration of quantitative global ubiquitinome profiling, direct half-life measurements, and genetic validation of regulating enzymes. By adhering to these technical considerations and acknowledging the inherent pitfalls, researchers can confidently validate specific proteasome substrates, leading to more reliable insights into disease mechanisms and more effective therapeutic development.
The ubiquitin-proteasome system (UPS) is a vital proteolytic pathway responsible for degrading 80-90% of intracellular proteins, including regulatory proteins critical for cell cycle control, apoptosis, and DNA repair [62]. Proteasome inhibitors, such as bortezomib and carfilzomib, have been validated as anticancer therapeutics, particularly for hematological malignancies like multiple myeloma [62]. These agents function primarily by binding to the proteolytic β-subunits of the 20S core particle, disrupting protein homeostasis and leading to apoptosis in malignant cells [62].
Despite initial clinical success, the efficacy of proteasome inhibitor therapy is often limited by the emergence of resistance. Tumor cells employ diverse adaptation mechanisms to circumvent proteasome inhibition, including proteasome subunit mutations, upregulation of alternative degradation pathways, and modulation of the tumor immune microenvironment [62] [30]. Understanding these resistance mechanisms is crucial for developing novel therapeutic strategies and improving patient outcomes. This review synthesizes current knowledge on tumor adaptations to proteasome inhibitor therapy within the broader context of cellular ubiquitin level dynamics.
Core Resistance Mechanisms and Quantitative Data
Tumors evade proteasome inhibitor cytotoxicity through several well-characterized molecular adaptations. The table below summarizes the primary resistance mechanisms and their functional consequences.
Table 1: Key Tumor Resistance Mechanisms to Proteasome Inhibitors
| Resistance Mechanism | Molecular Components | Functional Consequence | Experimental Evidence |
|---|---|---|---|
| Proteasome Subunit Mutations | PSMB5 (β5 subunit) | Reduced drug-binding affinity, maintains proteolytic activity [62] | Site-directed mutagenesis, crystal structure analysis |
| Immunoproteasome Upregulation | LMP2, LMP7, MECL-1 | Altered catalytic specificity and inhibitor sensitivity [62] | RNA-seq, proteasome activity profiling |
| Efflux Pump Activation | P-glycoprotein (MDR1) | Active cellular efflux of proteasome inhibitors [63] | Drug accumulation assays, inhibitor synergy studies |
| UPS Component Upregulation | Proteasome-assembling chaperones (PACs), 19S RP | Increased proteasome abundance and assembly [62] | Immunoblotting, gene expression analysis |
| Activation of Alternative Degradation | Autophagy-lysosome pathway, TRIM21 E3 ligase | Compensatory protein clearance independent of proteasome [30] | LC3 puncta assay, lysosome inhibition experiments |
Quantitative data further elucidates the dynamics of these adaptations. The following table compiles key experimental findings from resistance studies.
Table 2: Quantitative Data on Proteasome Inhibitor Resistance
| Experimental Parameter | Sensitive Cell Model | Resistant Cell Model | Change Magnitude |
|---|---|---|---|
| PSMB5 Mutation Frequency | <5% | >60% | >12-fold increase [62] |
| Immunoproteasome mRNA | Baseline (1x) | 3-5x elevated | 3 to 5-fold upregulation [62] |
| Intracellular Drug Accumulation | High (100%) | ~30% | ~70% reduction [63] |
| Chymotrypsin-like Activity | 10% of baseline | 60-80% of baseline | 6 to 8-fold recovery [62] |
| Autophagy Flux | Baseline (1x) | 2.5-4x elevated | 2.5 to 4-fold increase [30] |
The Scientist's Toolkit: Essential Research Reagents
Research into proteasome inhibitor resistance relies on a specialized toolkit of reagents and methodologies.
Table 3: Key Research Reagents for Studying Resistance Mechanisms
| Reagent/Method | Specific Example | Primary Function in Research |
|---|---|---|
| Specific Proteasome Inhibitors | Bortezomib, Carfilzomib, MG-132 | Tool compounds for in vitro and in vivo proteasome inhibition [62] |
| Proteasome Activity Probes | Fluorogenic substrates (Suc-LLVY-AMC) | Quantify chymotrypsin-like, trypsin-like, and caspase-like activities [62] |
| Antibodies for Immunoblotting | Anti-PSMB5, Anti-LMP2, Anti-PD-L1 | Detect protein expression levels and post-translational modifications [62] [30] |
| Gene Silencing Tools | siRNA against SPOP, TRIM21 | Functional validation of specific E3 ligases in PD-L1 regulation [30] |
| Chemical Modulators | Chloroquine (autophagy inhibitor), Verapamil (MDR1 inhibitor) | Probe compensatory pathways and efflux mechanisms [30] [63] |
Experimental Protocols for Key Methodologies
Protocol: Generating an Isogenic Resistant Cell Line
- Culture Setup: Initiate cultures of a proteasome inhibitor-sensitive cancer cell line (e.g., MM.1S for multiple myeloma) in standard growth medium.
- Dose Escalation: Continuously expose cells to a low, sub-lethal concentration of the proteasome inhibitor (e.g., 5 nM bortezomib). Maintain this culture for 2-3 weeks or until >90% cell viability is restored.
- Selection Pressure: Gradually increase the inhibitor concentration in a stepwise manner (e.g., 5 nM → 10 nM → 20 nM), allowing cells to stabilize and proliferate at each new concentration for 2-3 weeks.
- Clonal Selection: After achieving resistance to a target concentration (e.g., 40-50 nM bortezomib, ~10x IC50 of parental line), isolate single-cell clones by limiting dilution or colony picking.
- Validation: Expand clones and validate the resistant phenotype by comparing IC50 values to the parental line using cell viability assays (e.g., MTT, CellTiter-Glo). Confirm sustained resistance over at least 5 passages in drug-free medium.
Protocol: Measuring Proteasome Activity in Cell Lysates
- Lysate Preparation: Harvest 1x10^6 cells by centrifugation. Wash with cold PBS and lyse in a non-denaturing buffer (e.g., 50 mM Tris-HCl, pH 7.5, 250 mM sucrose, 5 mM MgCl2, 1 mM DTT, 0.5% NP-40) on ice for 30 minutes. Clarify by centrifugation at 16,000 x g for 20 minutes at 4°C. Determine the protein concentration of the supernatant.
- Reaction Setup: In a black 96-well plate, combine 10-20 µg of total protein lysate with 100 µL of reaction buffer (50 mM HEPES, pH 7.5, 5 mM EDTA) containing 100 µM of a fluorogenic proteasome substrate.
- Substrate Specificity:
- Chymotrypsin-like activity: Suc-LLVY-AMC
- Caspase-like activity: Z-LLE-AMC
- Trypsin-like activity: Boc-LRR-AMC
- Substrate Specificity:
- Control Wells: Include replicate wells pre-incubated for 30 minutes with a specific proteasome inhibitor (e.g., 10 µM MG-132) to confirm signal specificity.
- Kinetic Measurement: Immediately transfer the plate to a pre-warmed (37°C) fluorescence microplate reader. Measure the release of the fluorescent AMC group (excitation 380 nm, emission 460 nm) every 5 minutes for 60-120 minutes.
- Data Analysis: Calculate the velocity of the reaction from the linear range of the fluorescence curve. Normalize activity to total protein content and express as a percentage of activity in untreated control samples.
Protocol: Evaluating PD-L1 Ubiquitination and Stability
- Cell Treatment: Treat relevant cancer cells (e.g., HCT116 colorectal cancer or A549 non-small cell lung cancer) with a proteasome inhibitor (e.g., 100 nM carfilzomib) for 4-16 hours. Include a DMSO vehicle control.
- Immunoprecipitation: Harvest cells and lyse in a mild RIPA buffer. Incubate 500 µg of total protein with 2 µg of anti-PD-L1 antibody overnight at 4°C with gentle rotation. Add Protein A/G beads for 2 hours to capture the immune complexes.
- Ubiquitin Detection: Wash the beads extensively to remove non-specifically bound proteins. Elute the immunoprecipitated proteins by boiling in 2X Laemmli buffer. Resolve the proteins by SDS-PAGE and transfer to a PVDF membrane.
- Immunoblotting: Probe the membrane with an anti-ubiquitin antibody (e.g., P4D1) to detect ubiquitinated PD-L1 species, which will appear as high-molecular-weight smears above the core PD-L1 band. Re-probe the membrane with anti-PD-L1 antibody to confirm equal pulldown.
- Cycloheximide Chase: To measure protein half-life, treat cells with 100 µg/mL cycloheximide to block new protein synthesis. Harvest cells at 0, 1, 2, 4, and 6 hours post-treatment. Perform immunoblotting for PD-L1 and a loading control (e.g., GAPDH). Densitometry analysis will reveal the stabilization of PD-L1 in resistant models.
Signaling Pathways in Resistance
The development of resistance involves interconnected signaling networks that allow tumor cells to survive proteasome inhibition. The following diagrams, generated using Graphviz DOT language, illustrate two key pathways.
Diagram 1: Intrinsic Resistance via Proteasome Adaptation and Drug Efflux. This pathway shows tumor cell adaptations including proteasome subunit mutations, immunoproteasome upregulation, and drug efflux that collectively sustain protein degradation and promote survival under proteasome inhibitor pressure [62] [63].
Diagram 2: UPS-Mediated Immune Evasion via PD-L1 Stabilization. This pathway illustrates how proteasome inhibition can disrupt the normal ubiquitination and degradation of PD-L1, leading to its accumulation on tumor cells and subsequent suppression of anti-tumor T-cell immunity [30] [64].
Tumor resistance to proteasome inhibitors is a multifaceted phenomenon driven by intrinsic adaptations within the cancer cell and extrinsic interactions with the tumor immune microenvironment. Key mechanisms include genetic alterations of the proteasome itself, activation of compensatory degradation pathways, and immune evasion through checkpoint protein stabilization. Overcoming this resistance requires combination therapies that simultaneously target the proteasome and these adaptive survival pathways. Future research should focus on elucidating the precise molecular triggers that initiate these resistance programs and developing next-generation inhibitors that are less susceptible to common resistance mechanisms, such as immunoproteasome-specific agents or dual-targeting molecules. A deep understanding of the interplay between proteasome inhibition and cellular ubiquitin dynamics will be fundamental to guiding these innovative therapeutic strategies.
Proteasome inhibitors have revolutionized the treatment landscape for multiple myeloma, a malignant clonal plasma cell disease and the second most common hematologic malignancy in adults [65]. By targeting the ubiquitin-proteasome system (UPS)—the primary proteolytic machinery responsible for degrading intracellular proteins—these therapeutics promote apoptosis in malignant cells by inhibiting the NF-κB signaling pathway and upregulating pro-apoptotic proteins [65]. The UPS maintains cellular homeostasis by degrading a vast array of regulatory proteins, with the majority of substrates marked for degradation through the covalent attachment of multiple ubiquitin molecules, which provides the recognition signal for the 26S proteasome [18]. This system divides protein destruction into two discrete steps: a specific recognition process via the ubiquitin conjugation cascade, followed by an indiscriminate destruction process mediated by the proteolytic proteasome core [18].
The clinical utility of proteasome inhibitors (PIs) is tempered by their characteristic adverse event profiles, which can hinder treatment adherence and limit therapeutic efficacy. Understanding these safety profiles within the context of real-world clinical practice provides essential insights for researchers and clinicians managing treated populations. This technical guide examines the real-world safety data for the three most commonly used PIs—bortezomib (BTZ), carfilzomib (CFZ), and ixazomib (IXZ)—and frames their adverse event profiles within the broader research context of proteasome inhibition's impact on cellular ubiquitin levels and protein homeostasis.
The Ubiquitin-Proteasome Pathway: Molecular Framework for Therapeutic Intervention
The Ubiquitin-Conjugation Cascade
The ubiquitin-proteasome pathway represents a sophisticated cellular mechanism for targeted protein degradation. The process initiates with ubiquitin activation, where the E1 enzyme activates ubiquitin in an ATP-dependent manner, forming a thioester bond with ubiquitin's C-terminal glycine [18]. Subsequently, activated ubiquitin is transferred to an E2 ubiquitin-conjugating enzyme, which then collaborates with an E3 ubiquitin ligase to facilitate the covalent attachment of ubiquitin to a lysine residue on the target protein [18]. This modular system, employing different combinations of E2 and E3 enzymes, provides exquisite specificity for recognizing diverse protein substrates. Polyubiquitin chains, typically linked through Lys48 of ubiquitin, serve as the recognition signal for the 26S proteasome [18].
The Proteasome and Proteasome Inhibition
The 26S proteasome consists of a 20S catalytic core particle and one or two 19S regulatory particles. The 20S proteasome contains multiple proteolytic activities, including chymotrypsin-like, trypsin-like, and caspase-like activities, which are all targeted by clinical proteasome inhibitors with varying specificity [65]. Malignant cells exhibit heightened sensitivity to proteasome inhibition due to their increased protein synthesis and reliance on the UPS to manage proteotoxic stress [22]. This differential sensitivity creates a therapeutic window that can be exploited for cancer treatment, particularly in hematological malignancies like multiple myeloma [22].
Diagram: The Ubiquitin-Proteasome Pathway and Proteasome Inhibition. This diagram illustrates the sequential enzymatic cascade of ubiquitination and subsequent proteasomal degradation of target proteins, with the site of therapeutic proteasome inhibitor intervention highlighted in red.
Methodology for Pharmacovigilance Analysis
Data Source and Extraction
Real-world safety data for proteasome inhibitors were obtained through analysis of the U.S. Food and Drug Administration Adverse Event Reporting System (FAERS) database, the largest publicly available pharmacovigilance database [65]. This analysis encompassed reports from January 2004 through December 2023, totaling 20,629,811 adverse event reports [65]. Researchers extracted reports for the three proteasome inhibitors using standardized query terms: "bortezomib," "Velcade," "LDP341," "PS341" for bortezomib; "carfilzomib," "Kyprolis," "PR171" for carfilzomib; and "ixazomib," "Ninlaro," "MLN9708" for ixazomib [65]. Only reports where the proteasome inhibitor was designated as the 'primary suspect' drug were included in the analysis to strengthen causal inference.
Adverse Event Coding and Statistical Analysis
Adverse events in FAERS are coded using the Medical Dictionary for Regulatory Activities (MedDRA) terminology, which organizes events into System Organ Classes (SOCs) and more specific Preferred Terms (PTs) [65]. To detect safety signals, researchers employed the Reporting Odds Ratio (ROR) algorithm, a disproportionality analysis method that compares the reporting rate of a specific adverse event for a drug of interest versus all other drugs in the database [65]. A significant safety signal was detected when the lower bound of the 95% confidence interval for the ROR exceeded 1, with additional criteria of at least 3 reported cases [65]. Statistical analyses were performed using Microsoft Excel 2021 and R version 4.4.0 software, with data visualization conducted using the "ggplot2" package in R [65].
Diagram: Pharmacovigilance Analysis Workflow. This diagram outlines the sequential steps in processing FAERS data for proteasome inhibitor safety signal detection, from initial database query through to final safety signal identification.
Comparative Safety Profiles of Clinical Proteasome Inhibitors
Descriptive Analysis and Patient Demographics
During the 19-year study period, FAERS contained 29,395 (0.12%) reports for bortezomib, 12,753 (0.05%) for carfilzomib, and 8,594 (0.03%) for ixazomib [65]. Adverse events were reported slightly more frequently in males than females, with a higher proportion of patients aged >65 years across all three agents [65]. The primary reporting countries for bortezomib and carfilzomib included the United States, France, and Japan, while ixazomib reports primarily originated from the United States and Japan [65]. Physicians submitted the majority of reports for bortezomib (54.3%) and carfilzomib (54.8%), but accounted for a smaller proportion for ixazomib (38.5%) [65].
Table 1: Adverse Event Reporting Characteristics for Proteasome Inhibitors
| Parameter | Bortezomib | Carfilzomib | Ixazomib |
|---|---|---|---|
| Total Reports | 29,395 (0.12%) | 12,753 (0.05%) | 8,594 (0.03%) |
| Gender Distribution | Slightly more males | Slightly more males | Slightly more males |
| Age Distribution | >65 years predominant | >65 years predominant | >65 years predominant |
| Primary Reporting Countries | United States, France, Japan | United States, France, Japan | United States, Japan |
| Physician-Submitted Reports | 54.3% | 54.8% | 38.5% |
System Organ Class Safety Signals
Analysis by System Organ Class (SOC) revealed distinct safety profiles for the three proteasome inhibitors. Bortezomib demonstrated its most significant SOC signal in "blood and lymphatic system disorders" (ROR = 3.47, 95% CI 3.37–3.57), while carfilzomib showed an even stronger signal in the same category (ROR = 4.34, 95% CI 4.17–4.53) [65]. In contrast, ixazomib's most significant SOC signal was "gastrointestinal disorders" (ROR = 2.04, 95% CI 1.96–2.12) [65]. These differential safety profiles likely reflect variations in molecular structure, administration routes, and metabolic pathways among the three agents.
Table 2: Significant System Organ Class (SOC) Safety Signals for Proteasome Inhibitors
| Proteasome Inhibitor | Most Significant SOC | Reporting Odds Ratio (95% CI) | Other Significant SOCs |
|---|---|---|---|
| Bortezomib | Blood and lymphatic system disorders | 3.47 (3.37–3.57) | Nervous system disorders, Gastrointestinal disorders |
| Carfilzomib | Blood and lymphatic system disorders | 4.34 (4.17–4.53) | Cardiac disorders, Respiratory disorders |
| Ixazomib | Gastrointestinal disorders | 2.04 (1.96–2.12) | General disorders, Metabolism and nutrition disorders |
Preferred Term Analysis and Unexpected Adverse Events
At the more specific Preferred Term (PT) level, bortezomib demonstrated its strongest signal for "enteric neuropathy" (ROR = 134.96, 95% CI 45.67–398.79), consistent with its known association with peripheral neuropathy [65]. Both carfilzomib and ixazomib showed their most significant PT signals for "light chain analysis increased" (ROR = 76.65, 95% CI 57.07–102.96 and ROR = 67.15, 95% CI 45.36–99.42, respectively), potentially reflecting disease monitoring rather than true adverse drug reactions [65]. For bortezomib and carfilzomib, the top 20 reported PTs were consistent with known adverse events described in their prescribing information [65]. However, for ixazomib, six unexpected adverse events not currently listed on the drug label were observed: asthenia, malaise, pyrexia, decreased appetite, dehydration, and falls [65].
Time-to-Onset of Adverse Events
The time-to-onset analysis revealed distinct temporal patterns for adverse events associated with each proteasome inhibitor. For bortezomib, the median time-to-onset was 38 days (interquartile range [IQR] 12–109 days), with 44.4% of adverse reactions occurring within the first treatment cycle [65]. Carfilzomib exhibited a longer median time-to-onset of 57 days (IQR 13–190 days), while ixazomib demonstrated the most delayed onset profile with a median of 81 days (IQR 23–222 days) [65]. These temporal patterns align with the early failure type model in time-to-onset analysis and provide clinically valuable information for monitoring schedules across the treatment continuum.
Table 3: Time-to-Onset Profiles for Proteasome Inhibitor Adverse Events
| Proteasome Inhibitor | Median Time-to-Onset (Days) | Interquartile Range (IQR) | Early Adverse Events (First Cycle) |
|---|---|---|---|
| Bortezomib | 38 | 12–109 | 44.4% |
| Carfilzomib | 57 | 13–190 | Not specified |
| Ixazomib | 81 | 23–222 | Not specified |
Mechanistic Insights: Linking UPS Inhibition to Adverse Events
Molecular Mechanisms of Toxicity
The adverse events associated with proteasome inhibitors stem from the fundamental role of the UPS in maintaining cellular homeostasis. Hematological toxicities, particularly prominent with bortezomib and carfilzomib, likely result from the rapid turnover of hematopoietic cells and the sensitivity of this system to perturbations in protein degradation [65]. Gastrointestinal disorders, which characterize ixazomib's safety profile, may reflect the high rate of protein turnover in gastrointestinal mucosal cells and their consequent vulnerability to proteasome inhibition [65]. Peripheral neuropathy, a hallmark toxicity of bortezomib, may involve disrupted protein degradation in neuronal cells, leading to accumulation of misfolded proteins and cellular dysfunction [65].
Structural Considerations and Target Specificity
The structural differences among proteasome inhibitors contribute to their distinct safety profiles. Bortezomib, a dipeptide boronic acid, reversibly inhibits the chymotrypsin-like activity of the proteasome [65]. Ixazomib shares boronate-like structure with bortezomib but was designed with improved pharmacological properties, including oral bioavailability [65]. Carfilzomib possesses a unique tetrapeptide epoxide ketone structure that enables highly selective, irreversible covalent binding to the proteasome's β5 subunit [65]. This irreversible binding and sustained inhibition may contribute to carfilzomib's stronger hematological toxicity signals observed in the FAERS analysis.
The Scientist's Toolkit: Essential Research Reagents and Methodologies
Table 4: Essential Research Reagents for Studying Proteasome Inhibition
| Research Tool | Function/Application | Representative Examples |
|---|---|---|
| Reporter Substrates | Monitor UPS function via fluorescent or luminescent tags | Ub-YFP, Ub-R-GFP, YFP-CL1, CD3δ-YFP, ZsGreen-ODC [22] |
| Proteasome Activity Assays | Measure chymotrypsin-like, trypsin-like, and caspase-like proteasome activities | Fluorogenic peptides (e.g., Suc-LLVY-AMC), luminogenic substrates [22] |
| Ubiquitin Probes | Detect ubiquitin conjugates and profile ubiquitinated proteins | Anti-ubiquitin antibodies, ubiquitin binding domains [22] |
| CRISPR/Cas9 Screening | Identify genetic modifiers of proteasome inhibitor sensitivity | Genome-wide sgRNA libraries, NQO1 knockout cells [22] |
| Pharmacological Inhibitors | Specific inhibition of UPS components for mechanistic studies | Bortezomib, Carfilzomib, Epoxomicin, CBK77 [65] [22] |
| Cell Viability Assays | Assess cytotoxicity and proliferation following proteasome inhibition | WST-1 tetrazolium salt, ATP-based luminescence assays [22] |
Real-world safety data from the FAERS database reveals distinct adverse event profiles for the three primary proteasome inhibitors used in multiple myeloma treatment. Bortezomib and carfilzomib demonstrate significant hematological toxicity signals, while ixazomib is characterized predominantly by gastrointestinal disorders. These safety profiles reflect the fundamental role of the ubiquitin-proteasome system in maintaining cellular homeostasis across different tissue types. The association between ixazomib and unexpected adverse events such as asthenia, malaise, and falls warrants further clinical investigation and consideration in risk management strategies. As proteasome inhibition continues to represent a cornerstone of multiple myeloma therapy, understanding these distinct safety profiles enables optimized treatment selection, appropriate monitoring, and proactive management of adverse events, ultimately improving patient outcomes and quality of life during treatment.
The therapeutic window, defined as the range of drug doses that effectively treats disease without causing unacceptable toxicity, represents a central challenge in oncology drug development. Within the context of proteasome inhibition research, optimizing this window is paramount for selectively targeting malignant cells while sparing healthy tissues. This whitepaper explores advanced strategies—encompassing molecular, computational, and clinical approaches—to maximize the therapeutic window of cancer therapies. We examine how targeted agent dose optimization, exploitation of differential pathway dependencies, and innovative trial designs can improve patient outcomes by enhancing efficacy and reducing off-target effects. The integration of precision medicine principles with a deep understanding of the ubiquitin-proteasome system (UPS) offers promising avenues for developing more selective and effective cancer treatments.
The concept of the therapeutic window is critically important in oncology, where the biological processes targeted by therapies often exist in both malignant and healthy cells. Traditional chemotherapy approaches have typically relied on the maximum tolerated dose (MTD), operating under the assumption that higher drug exposure will yield greater tumor cell kill, albeit with significant toxicity to normal tissues [66]. However, with the advent of molecularly targeted therapies and precision medicine, a broader therapeutic window is achievable through more sophisticated approaches to dose selection and combination strategies.
The ubiquitin-proteasome system (UPS) serves as an illustrative model for therapeutic window optimization challenges. As the main non-lysosomal protein degradation pathway in eukaryotic cells, the UPS regulates critical cellular processes including cell cycle progression, apoptosis, and inflammatory responses [67] [53]. Malignant cells, particularly those in hematological malignancies like multiple myeloma, often exhibit increased proteasome activity and greater dependence on protein homeostasis mechanisms compared to normal cells [68]. This differential dependence creates a theoretical therapeutic window that can be exploited through targeted inhibition.
Research demonstrates that optimized therapeutic windows can be achieved through multiple strategic approaches: (1) precision dosing based on target engagement rather than pure toxicity endpoints; (2) exploitation of pathway addiction in cancer cells; (3) sophisticated combination therapies that selectively sensitize malignant cells; and (4) advanced patient stratification using genomic and network dynamics biomarkers. The following sections explore these strategies in technical detail, with particular emphasis on UPS-targeting therapies and their implications for cancer treatment.
The Ubiquitin-Proteasome System: A Therapeutic Framework
System Architecture and Function
The ubiquitin-proteasome system represents a complex, multi-step pathway for regulated protein degradation in eukaryotic cells. This sophisticated system involves a cascade of enzymatic reactions that ultimately lead to the targeted degradation of proteins, providing precise control over cellular protein levels [53]. The UPS begins with ubiquitin activation by E1 enzymes, proceeds through ubiquitin conjugation by E2 enzymes, and culminates in substrate-specific ubiquitination by E3 ligases, which identify target proteins for degradation [53].
The 26S proteasome serves as the catalytic core of the UPS, consisting of a 20S proteolytic core particle capped by one or two 19S regulatory particles [67]. The 20S core contains three distinct active sites—caspase-like (β1), trypsin-like (β2), and chymotrypsin-like (β5)—that collectively cleave ubiquitinated proteins into small peptides [67]. Importantly, specialized immunoproteasomes (i20S), containing inducible catalytic subunits (β1i/LMP2, β2i/MECL-1, and β5i/LMP7), are constitutively expressed in immune cells and can be induced in other cell types by inflammatory cytokines like interferon-γ (IFN-γ) and tumor necrosis factor-α (TNF-α) [67].
Table 1: Core Components of the Ubiquitin-Proteasome System
| Component | Number in Humans | Primary Function |
|---|---|---|
| E1 Activating Enzymes | 2 | Initiate ubiquitination by activating ubiquitin in an ATP-dependent manner |
| E2 Conjugating Enzymes | ~30 | Carry activated ubiquitin and mediate transfer to target proteins |
| E3 Ligases | >700 | Provide substrate specificity by recognizing target proteins and facilitating ubiquitin transfer |
| Deubiquitinating Enzymes (DUBs) | ~100 | Reverse ubiquitination by removing ubiquitin from substrates |
| 20S Proteasome Core | 1 complex | Catalyzes the proteolytic degradation of tagged proteins |
| 19S Regulatory Particle | 1 complex | Recognizes ubiquitinated proteins and facilitates their entry into the 20S core |
Malignant vs. Healthy Cell Differential Dependence
Cancer cells frequently develop heightened dependence on the UPS due to several factors. Rapid proliferation generates increased levels of misfolded and damaged proteins that require efficient clearance [53]. Oncogenic signaling pathways often rely on tight regulation of key proteins through controlled degradation [69]. Additionally, the increased metabolic and oxidative stress in tumor cells creates greater proteotoxic burden [53].
Multiple myeloma cells exemplify this differential dependence, as they produce massive quantities of monoclonal immunoglobulins, creating exceptional endoplasmic reticulum stress and protein processing demands [68]. This vulnerability has been successfully targeted by proteasome inhibitors, which induce apoptosis by disrupting protein homeostasis, activating the unfolded protein response, and inhibiting NF-κB signaling [68]. The differential effect on malignant versus normal cells forms the basis for the therapeutic window of proteasome inhibitors in clinical use.
Quantitative Approaches to Therapeutic Window Optimization
Potency-Guided Dosing Strategies
Traditional oncology drug development has emphasized maximum tolerated dose (MTD) determination, often proceeding with dose escalation until unacceptable toxicity is observed [66]. However, for molecularly targeted agents, this approach may overlook potentially effective lower doses with improved safety profiles. Analysis of 25 targeted therapies revealed that the average free steady-state concentration (Css) at approved doses frequently approximates the in vitro IC50 value, with a median Css/IC50 ratio of 1.2 [66]. This suggests many targeted drugs are dosed to achieve concentrations near their biological potency threshold.
Notably, significant outliers exist in this analysis, with three drugs (encorafenib, erlotinib, and ribociclib) demonstrating Css/IC50 values exceeding 25 [66]. These findings indicate that certain kinase inhibitors may have substantial therapeutic windows that remain unexploited, as lower doses might maintain efficacy while reducing toxicity. This supports a paradigm shift toward potency-guided dosing, where dose selection is informed by target engagement and pathway modulation rather than toxicity alone [66].
Table 2: Comparative Steady-State Concentration and Potency Ratios for Selected Targeted Therapies
| Drug | Target | Css/IC50 Ratio | Therapeutic Window Implications |
|---|---|---|---|
| Encorafenib | BRAF | >25 | Potential for dose reduction with maintained efficacy |
| Erlotinib | EGFR | >25 | Possible improved tolerability at lower doses |
| Ribociclib | CDK4/6 | >25 | Unexploited therapeutic window |
| Imatinib | ABL | ~1.2 | Narrow therapeutic window |
| Vemurafenib | BRAF | 0.5-4 | Moderate therapeutic window |
| PARP Inhibitors | PARP | ~1 | Narrow therapeutic window |
Network Dynamics-Based Therapeutic Window Estimation
Computational approaches integrating genomic profiles with network dynamics modeling offer sophisticated methods for therapeutic window estimation. One such framework employs Boolean network modeling of the p53 signaling pathway combined with cancer-specific genomic alterations to simulate dose-response relationships [70]. This method evaluates both efficacy (maximal response) and potency (IC50) while incorporating toxicity estimates through comparison to normal tissue network models.
The approach involves six key steps: (1) obtaining functional genomic alterations from cancer databases; (2) constructing cell-specific network models by mapping alterations to interaction networks; (3) simulating dose-dependent perturbations; (4) scoring efficacy and toxicity responses; (5) evaluating therapeutic windows; and (6) screening optimal drug-target combinations [70]. This methodology enables stratification of patients based on network-specific determinants of drug response, moving beyond tissue-based classification to wiring-specific categorization.
Diagram 1: Network dynamics workflow for therapeutic window estimation
Experimental Strategies and Methodologies
Research Reagent Solutions for UPS Studies
Table 3: Essential Research Reagents for Ubiquitin-Proteasome System Investigations
| Reagent/Category | Specific Examples | Research Application |
|---|---|---|
| Proteasome Inhibitors | Bortezomib, Carfilzomib, Ixazomib, Marizomib | Investigate proteasome function; induce proteotoxic stress |
| E1 Enzyme Inhibitors | PYR-41, TAK-243 | Block ubiquitin activation; study upstream UPS regulation |
| E3 Ligase Modulators | BC-1215 (Fbxo3 inhibitor), Pevonedistat (NEDD8 inhibitor) | Target specific substrate degradation pathways |
| Immunoproteasome Inhibitors | ONX 0914, PR-924, KZR-504 | Selective immunoproteasome inhibition; immune response studies |
| Deubiquitinase Inhibitors | b-AP15, VLX1570 | Investigate ubiquitin chain editing and substrate stabilization |
| Activity Reporters | Proteasome-Glo Assays, Ubiquitin Probes | Measure proteasome activity in cellular contexts |
| Protein Degradation Inducers | PROTACs, Molecular Glues | Induce targeted protein degradation |
Detailed Methodologies for Key Experiments
Potency-Guided Dose Optimization Protocol
The potency-guided approach to dose selection involves comprehensive pharmacokinetic-pharmacodynamic (PK-PD) characterization during early clinical development. The experimental workflow includes:
In Vitro Potency Determination:
- Conduct cell proliferation assays using genetically characterized cell lines relevant to the drug target (e.g., H3255 for EGFR, A375 for BRAF) [66].
- Calculate IC50 values from dose-response curves using 72-hour CellTiter-Glo viability assays.
- Determine fraction of unbound drug (fup) using equilibrium dialysis or ultrafiltration methods.
Clinical PK/PD Modeling:
- Measure steady-state total drug AUCtau in phase I trials.
- Calculate free average steady-state concentration (Css) using the formula: Css = (AUCtau/dosing interval) × fup [66].
- Compare Css to IC50 to derive Css/IC50 ratio.
- Establish preliminary efficacy thresholds based on target engagement biomarkers.
Dose Cohort Expansion:
- Implement multiple expansion cohorts at doses achieving Css exceeding potency thresholds.
- Include doses below MTD when evidence of clinical activity is observed.
- Compare efficacy and toxicity across dose levels to identify optimal therapeutic window [66].
Proteasome Inhibition Resistance Overcoming Protocol
Recent research demonstrates that proteasome inhibitors can overcome resistance to targeted therapies in B-cell malignancies [71]. The experimental methodology includes:
Resistance Model Development:
- Generate drug-resistant cell lines (e.g., idelalisib-resistant KARPAS1718 and VL51 models) through prolonged exposure to IC90 concentrations of the targeted agent [71].
- Maintain resistant cultures for >3 months with continuous drug pressure.
- Validate resistance phenotype through dose-response confirmation.
High-Throughput Compound Screening:
- Perform dose-response experiments using 384-well plate format.
- Seed cells at optimized density (5,000 cells/well for cell lines; 10,000 cells/well for primary CLL cells).
- Co-culture primary CLL cells with irradiated APRIL/BAFF/CD40L-expressing fibroblasts for 24 hours prior to screening [71].
- Incubate with compound libraries for 72 hours at 37°C.
- Measure viability using CellTiter-Glo luminescent assay.
- Process dose-response data using specialized software (e.g., KNIME).
Mechanistic Validation Studies:
- Perform (phospho)protein profiling using fluorescent cell barcoding at 24 hours post-treatment.
- Analyze Bcl-2 family protein expression and phosphorylation (Bcl-2, Bim, Mcl-1).
- Conduct immunophenotyping of primary patient samples pre- and post-treatment.
- Evaluate cytokine production using ELISA (e.g., IL-10 measurement).
Diagram 2: Proteasome inhibition overcomes targeted therapy resistance
Clinical Translation and Therapeutic Applications
Proteasome Inhibitors in Hematologic Malignancies
Proteasome inhibitors have demonstrated significant clinical success in hematologic malignancies, particularly multiple myeloma and mantle cell lymphoma [68]. The therapeutic window of these agents stems from the differential proteotoxic stress between malignant plasma cells and normal tissues. First-generation proteasome inhibitor bortezomib achieves clinical responses by disrupting protein homeostasis, leading to endoplasmic reticulum stress and apoptosis in myeloma cells [68].
Second-generation agents have expanded the therapeutic window through improved specificity and reduced off-target effects. Carfilzomib, an irreversible epoxyketone inhibitor, demonstrates reduced neurotoxicity compared to bortezomib while maintaining efficacy in refractory/relapsed multiple myeloma [68]. Ixazomib, the first oral proteasome inhibitor, offers convenience with a toxicity profile characterized primarily by manageable hematologic side effects and hepatic enzyme elevations [68].
Novel proteasome inhibitors continue to emerge with potentially enhanced therapeutic indices. Marizomib, a non-peptide irreversible inhibitor, targets all three catalytic subunits with distinctive activity against the immunoproteasome [68]. Investigational agents like oprozomib and KZR-616 aim to further optimize the balance of efficacy and safety through improved pharmacological properties.
Strategic Combination Approaches
Rational combination therapies represent a powerful strategy for expanding therapeutic windows. Research demonstrates that proteasome inhibitors can overcome resistance to targeted agents like PI3K inhibitors and Bcl-2 antagonists in B-cell malignancy models [71]. The underlying mechanism involves modulation of Bcl-2 family members, with proteasome inhibition consistently upregulating Bim and Mcl-1 while increasing Bcl-2 in certain cellular contexts [71].
In a clinical application, a multi-refractory chronic lymphocytic leukemia patient treated with the combination of Bcl-2 inhibitor venetoclax and proteasome inhibitor bortezomib achieved initial clinical improvement through the IMPRESS-Norway trial (NCT04817956) [71]. This approach highlights the potential of targeting complementary vulnerabilities to restore therapeutic sensitivity while managing toxicity through appropriate dosing schedules.
The combination of proteasome inhibitors with targeted therapies requires careful management of overlapping toxicities. Strategies include sequential administration, dose modification, and prophylactic support measures. For instance, the combination of carfilzomib with lenalidomide and dexamethasone (KRd) has demonstrated efficacy as consolidation therapy after autologous stem cell transplantation, achieving minimal residual disease negativity while managing hematologic toxicity through appropriate dosing intervals [68].
Emerging Frontiers and Future Directions
Novel UPS-Targeting Modalities
Beyond catalytic proteasome inhibition, several innovative approaches to targeting the UPS are emerging with potential for enhanced therapeutic windows:
Immunoproteasome-Specific Inhibitors: Selective inhibition of immunoproteasome subunits (LMP2, LMP7, MECL-1) offers potential for targeted immunomodulation with reduced effects on constitutive proteasome function in normal tissues [67]. Compounds like ONX 0914 and KZR-504 demonstrate subunit specificity that may translate to improved safety profiles.
E3 Ligase-Targeted Therapies: The development of small molecules targeting specific E3 ligases represents a promising approach for precision intervention. Unlike kinase inhibitors that often target structurally similar ATP-binding pockets, E3 ligase inhibitors can exploit distinct substrate-binding interfaces, potentially offering greater specificity [67]. Challenges include the potential for off-target effects due to multiple substrate recognition by individual E3s and incomplete characterization of the E3-substrate interactome [67].
Targeted Protein Degradation: Proteolysis-targeting chimeras (PROTACs) represent a revolutionary approach that hijacks the UPS for selective degradation of target proteins [53]. These bifunctional molecules simultaneously bind a target protein and an E3 ubiquitin ligase, facilitating target ubiquitination and degradation. This modality offers potential advantages in targeting traditionally "undruggable" proteins and achieving sustained pharmacological effects through event-driven pharmacology rather than occupancy-based inhibition.
Advanced Therapeutic Window Assessment Technologies
Innovative technologies are enhancing our ability to predict and monitor therapeutic windows in both preclinical and clinical settings:
Network Dynamics-Based Patient Stratification: Computational approaches that model signaling network behavior in response to perturbations enable prediction of individual patient therapeutic windows [70]. By integrating genomic data with dynamic network modeling, these methods can identify patients most likely to respond to specific targeted therapies while experiencing minimal toxicity.
Functional Proteasome Activity Monitoring: Advanced assays for measuring tissue-specific proteasome activity in real time may enable more precise dosing of proteasome inhibitors. Such approaches could facilitate dose optimization based on target engagement rather than purely toxicity endpoints.
Biomarker-Guided Dosing Strategies: Identification and validation of biomarkers that predict both efficacy and toxicity are critical for therapeutic window optimization. For proteasome inhibitors, potential biomarkers include markers of proteotoxic stress, immunoglobulin free light chains, and specific genetic polymorphisms affecting drug metabolism [68].
Optimizing the therapeutic window for cancer therapies requires a multifaceted approach that integrates deep understanding of biological pathways, sophisticated dosing strategies, and innovative clinical trial designs. The ubiquitin-proteasome system provides a compelling model for therapeutic window optimization, demonstrating how differential dependence between malignant and healthy cells can be exploited for therapeutic benefit. Moving beyond traditional maximum tolerated dose paradigms toward potency-guided dosing, rational combination strategies, and personalized network dynamics-based approaches promises to enhance the efficacy and safety of cancer therapies. As our understanding of the complex interplay between targeted agents and cellular networks deepens, so too will our ability to design treatments that maximally engage malignant targets while sparing healthy tissues, ultimately improving outcomes for cancer patients.
The ubiquitin-proteasome system (UPS) represents a complex regulatory network that controls protein stability, function, and localization. This technical guide examines the sophisticated methodologies required to interpret ubiquitin landscapes, with particular emphasis on quantifying low-stoichiometry ubiquitination sites and mapping the dynamic changes induced by proteasome inhibition. Within the broader context of UPS research, understanding these intricate landscapes provides critical insights into cellular stress responses, proteotoxic stress management in malignancies, and the mechanistic actions of therapeutic agents. We present comprehensive experimental frameworks, quantitative data analysis strategies, and visualization tools to empower researchers in deciphering the complex ubiquitin code that governs cellular homeostasis.
Ubiquitin (UB)-driven signaling systems permeate biology and are frequently integrated with other post-translational modifications, most notably phosphorylation, to control the flux of information through cellular networks [72]. The 76-amino acid ubiquitin protein can be conjugated to substrate proteins as a single moiety (monoubiquitination) or as polymers (polyubiquitin chains) through an enzymatic cascade involving E1 activating, E2 conjugating, and E3 ligase enzymes [18]. The versatility of ubiquitination is reflected in the complexity of ubiquitin conjugates, which range from single ubiquitin monomers to polymers with different lengths and linkage types [45]. This complexity creates a sophisticated "ubiquitin code" that regulates diverse fundamental features of protein substrates, including stability, activity, and localization [45].
A central challenge in ubiquitin research involves detecting and quantifying low-stoichiometry modification sites—those occurring on a small percentage of a target protein population at any given time. These transient modifications often escape detection by conventional methods yet play crucial regulatory roles. Furthermore, proteasome inhibition induces dramatic shifts in ubiquitin landscapes by blocking the terminal step of ubiquitin-dependent proteolysis, resulting in accumulation of ubiquitinated proteins that provides a snapshot of UPS dynamics [22]. Interpreting these inhibitor-induced changes requires sophisticated methodological approaches that can distinguish meaningful signaling events from nonspecific accumulation.
Methodological Frameworks for Ubiquitin Landscape Analysis
Enrichment Strategies for Ubiquitinated Proteins
Identifying ubiquitinated proteins presents significant technical challenges due to low stoichiometry, transient nature, and structural diversity of modifications. Three primary enrichment strategies have emerged to address these challenges:
Ubiquitin Tagging-Based Approaches: These methods involve expressing ubiquitin containing affinity tags (e.g., His, Strep, HA) in living cells, enabling purification of ubiquitinated substrates using commercially available resins. The Strep-tag II system demonstrates particular utility, binding strongly to Strep-Tactin matrices with minimal non-specific interactions [45]. A cell line stably expressing Strep-tagged ubiquitin enabled identification of 753 lysine ubiquitylation sites on 471 proteins in U2OS and HEK293T cells [45]. While cost-effective and relatively straightforward, these approaches may introduce artifacts as tagged ubiquitin cannot completely mimic endogenous ubiquitin behavior.
Ubiquitin Antibody-Based Approaches: For profiling endogenous ubiquitination without genetic manipulation, pan-specific anti-ubiquitin antibodies (e.g., P4D1, FK1/FK2) enable enrichment of ubiquitinated proteins from native sources, including clinical samples [45]. Linkage-specific antibodies targeting M1-, K11-, K27-, K48-, or K63-linked chains further facilitate analysis of chain architecture. For instance, a K48-linkage specific antibody revealed abnormal accumulation of K48-linked polyubiquitination on tau proteins in Alzheimer's disease [45]. Limitations include the high cost of quality antibodies and potential non-specific binding.
Ubiquitin-Binding Domain (UBD)-Based Approaches: Proteins containing ubiquitin-binding domains (some E3 ubiquitin ligases, deubiquitinases, and ubiquitin receptors) can be utilized to bind and enrich endogenously ubiquitinated proteins [45]. Tandem-repeated ubiquitin-binding entities (TUBEs) exhibit significantly improved affinity compared to single UBDs, enabling more efficient capture of ubiquitinated species while simultaneously protecting ubiquitin chains from deubiquitinase activity during purification [45].
Quantitative Mass Spectrometry Approaches
Accurate quantification of ubiquitination dynamics requires sophisticated mass spectrometry methods that can distinguish subtle changes in modification status amid complex biological backgrounds:
Stable Isotope Labeling with Amino Acids in Cell Culture (SILAC): This metabolic labeling approach incorporates stable isotopes (e.g., (^{13})C, (^{15})N) into cellular proteins during cell division, allowing precise relative quantification between experimental conditions (e.g., proteasome inhibitor-treated vs. control cells) [72]. SILAC provides high quantitative accuracy as samples are combined early in the workflow, minimizing technical variability.
Tandem Mass Tagging (TMT): This isobaric labeling strategy enables multiplexing of up to 10 samples, significantly improving throughput for complex experimental designs [72]. Each TMT tag contains a reporter ion fragment (mass range 126-131) released upon high-energy collision-induced dissociation (HCD). Signal compression issues inherent in LC-MS2 approaches can be mitigated through LC-MS3 methodologies with synchronous precursor selection (MultiNotch MS3), which increases reporter ion detection approximately 10-fold [72].
Label-Free Quantification: While requiring extensive instrument time and rigorous normalization, label-free approaches avoid potential artifacts introduced by chemical labeling and can be applied to any sample type, including primary tissues [72]. Advanced computational algorithms now enable relatively robust quantification, particularly when combined with targeted acquisition methods like parallel reaction monitoring.
Table 1: Comparison of Quantitative Proteomics Methods for Ubiquitin Studies
| Method | Principle | Throughput | Advantages | Limitations |
|---|---|---|---|---|
| SILAC | Metabolic incorporation of stable isotopes | Medium (2-3 plex) | High quantitative accuracy; early sample combination reduces variability | Limited to cell culture systems; incomplete labeling possible |
| TMT | Isobaric chemical tags | High (up to 10-plex) | Excellent throughput; reduces missing values | Reporter ion interference/compression; requires specialized instrumentation for MS3 |
| Label-Free | Spectral counting or intensity-based | Low | Applicable to any sample type; no chemical modifications | Extensive instrument time required; higher technical variability |
Absolute Quantification and Stoichiometry Determination
While relative quantification reveals changes in ubiquitination between conditions, understanding biological significance often requires determination of modification stoichiometry—the fraction of target protein molecules modified at a specific site. Absolute quantification approaches, using heavy isotope-labeled synthetic peptides as internal standards, enable calculation of site-specific stoichiometries [72]. This information is crucial for distinguishing functionally important regulatory sites from bystander modifications and for understanding flux through ubiquitin-driven signaling pathways.
Proteasome Inhibition and Ubiquitin Landscape Remodeling
Mechanisms of Inhibitor Action
Proteasome inhibitors function by blocking the proteolytic activity of the 20S core particle, preventing degradation of ubiquitinated proteins and causing their accumulation. Different inhibitor classes exhibit distinct mechanisms:
CBK77 and NQO1-Mediated Activation: The bioactivatable compound CBK77 requires the redox enzyme NAD(P)H:quinone oxidoreductase 1 (NQO1)—often upregulated in malignant cells—for activation [22]. Once activated, CBK77 causes irreversible collapse of the UPS, accompanied by general accumulation of ubiquitylated proteins and caspase-dependent cell death. Affinity-based proteomics revealed that CBK77 covalently interacts with ubiquitin itself, and CBK77-treated ubiquitin conjugates show reduced susceptibility to disassembly by deubiquitinating enzymes [22].
Clinical Proteasome Inhibitors: FDA-approved agents including bortezomib, carfilzomib, and ixazomib primarily target the chymotrypsin-like activity of the proteasome, with varying specificity, reversibility, and clinical applications [73]. Cancer cells display heightened sensitivity to these agents due to increased reliance on UPS function to manage proteotoxic stress resulting from hyperactive protein synthesis and accumulation of aberrant proteins [22].
Quantifying Inhibitor-Induced Changes
Proteasome inhibition induces complex remodeling of the ubiquitin landscape that can be quantified through integrated methodologies:
Ubiquitination Site Dynamics: Quantitative proteomics following proteasome inhibition reveals both expected and unexpected changes. While most ubiquitinated proteins accumulate due to blocked degradation, some sites may show decreased ubiquitination due to disrupted processivity or compensatory deubiquitinase activity.
Chain Linkage Specificity: Different proteasome inhibitors can induce distinct patterns of chain linkage accumulation. For example, bortezomib treatment primarily increases K48-linked chains (typically associated with proteasomal degradation), while other inhibitors might promote accumulation of atypical chains (K63, K11, etc.) with different signaling functions.
Temporal Dynamics: The kinetics of ubiquitin accumulation following proteasome inhibition provide insights into protein half-lives and turnover rates. Time-course experiments with quantitative proteomics can distinguish rapidly turned over substrates from stable proteins that become ubiquitinated in response to proteotoxic stress.
Table 2: Representative Ubiquitination Changes Following Proteasome Inhibition
| Protein Category | Example Proteins | Ubiquitination Response to Inhibition | Functional Consequences |
|---|---|---|---|
| Cell Cycle Regulators | Cyclins, CDK inhibitors | Rapid accumulation | Cell cycle arrest |
| Apoptosis Regulators | MCL-1, NOXA, p53 | Increased ubiquitination | Caspase-dependent apoptosis |
| ER Stress Components | Misfolded ER proteins | Marked accumulation | Unfolded protein response activation |
| Transcriptional Regulators | NF-κB inhibitors (IκB) | Altered degradation patterns | Modulated signaling pathway activity |
| DNA Repair Factors | BRCA1, RAD51 | Variable responses | Impaired DNA damage response |
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Research Reagents for Ubiquitin Landscape Studies
| Reagent Category | Specific Examples | Function/Application |
|---|---|---|
| Proteasome Inhibitors | Bortezomib, Carfilzomib, MG-132, Epoxomicin | Block proteasomal activity to stabilize ubiquitinated proteins for analysis |
| DUB Inhibitors | PR-619 | Block deubiquitinating enzyme activity to preserve ubiquitin chains during extraction |
| Affinity Tags | 6×His, Strep-tag II, HA, FLAG | Enable purification of ubiquitinated proteins from complex lysates |
| Ubiquitin Antibodies | P4D1, FK1, FK2, Linkage-specific antibodies | Detect and enrich ubiquitinated proteins; distinguish chain linkage types |
| CRISPR/Cas9 Components | Cas9 nucleases, guide RNAs | Generate knockout cell lines to validate ubiquitination enzymes and substrates |
| Mass Spectrometry Standards | Stable isotope-labeled peptides (AQUA) | Enable absolute quantification of ubiquitination sites |
| Expression Vectors | Tagged-ubiquitin constructs, E3 ligase plasmids | Manipulate ubiquitination pathways; express tagged ubiquitin for enrichment |
Experimental Workflow Visualization
Ubiquitin Enrichment and Quantification Workflow
Proteasome Inhibition Signaling Pathway
Data Interpretation and Analytical Considerations
Distinguishing Functional Sites from Bystander Modifications
Interpreting ubiquitin landscapes requires distinguishing functionally relevant ubiquitination events from non-specific bystander modifications. Several analytical strategies support this discrimination:
Stoichiometry Calculations: Combining absolute quantification of ubiquitination sites with total protein abundance enables calculation of modification stoichiometry. Low-stoichiometry sites with high functional impact typically show increased fractional occupancy following pathway activation or proteasome inhibition [72].
Evolutionary Conservation: Bioinformatics analysis of sequence conservation across species can identify functionally constrained ubiquitination sites more likely to have regulatory significance.
Mutational Validation: Site-directed mutagenesis of candidate ubiquitination sites, followed by functional assays, provides direct evidence of biological relevance. Substituting lysine with arginine (preserving charge while preventing ubiquitination) tests necessity, while lysine-to-glutamine mutations (mimicking constitutive ubiquitination) can test sufficiency [45].
Contextualizing Inhibitor-Induced Changes
Proteasome inhibition creates a complex cellular response extending beyond simple accumulation of ubiquitinated proteins:
Compensatory Mechanisms: Cells activate multiple adaptive responses to proteasome inhibition, including upregulated deubiquitinase expression, increased autophagic flux, and enhanced expression of molecular chaperones. These compensatory mechanisms reshape the ubiquitin landscape in ways that must be considered during data interpretation.
Off-Target Effects: Some proteasome inhibitors, particularly at higher concentrations, can affect other proteolytic systems or cellular processes. Controlled dose-response experiments and orthogonal validation methods are essential for distinguishing UPS-specific effects.
Cell Type-Specific Responses: Malignant cells often exhibit heightened sensitivity to proteasome inhibition due to pre-existing proteotoxic stress, while non-transformed cells may demonstrate more robust adaptive responses. These differential sensitivities create therapeutic windows but complicate comparative analyses.
Interpreting ubiquitin landscapes requires integrated methodological approaches that address the complexity and dynamic nature of this essential post-translational modification system. The frameworks presented here—combining sophisticated enrichment strategies, quantitative mass spectrometry, and contextual data analysis—provide powerful tools for deciphering low-stoichiometry ubiquitination sites and understanding the multifaceted cellular responses to proteasome inhibition. As research in this field advances, continued refinement of these methodologies will further illuminate the intricate ubiquitin code and its manipulation for therapeutic benefit in cancer and other diseases characterized by proteostasis dysfunction.
From Bench to Bedside: Clinical Validation and Market Analysis of Proteasome Inhibitors
The ubiquitin-proteasome system (UPS) represents a critical therapeutic target in oncology, particularly for hematologic malignancies characterized by high protein turnover. Proteasome inhibitors (PIs) exploit this vulnerability by disrupting protein homeostasis, leading to apoptosis in malignant cells. This whitepaper provides a comprehensive technical analysis of the clinical efficacy, molecular mechanisms, and experimental methodologies for PIs in multiple myeloma (MM) and mantle cell lymphoma (MCL), framed within the context of UPS inhibition research. We synthesize clinical trial data, detail relevant experimental protocols, and visualize key signaling pathways to serve as a resource for researchers and drug development professionals.
The ubiquitin-proteasome pathway is the principal mechanism for regulated intracellular protein degradation in eukaryotic cells. This pathway controls the turnover of proteins critical for cell cycle progression, signal transduction, and apoptosis [1] [18]. The 26S proteasome complex consists of a 20S catalytic core particle capped by one or two 19S regulatory particles. The 20S core, a barrel-shaped structure of four stacked rings (α7β7β7α7), contains three primary proteolytic activities on its inner β-rings: chymotrypsin-like (CT-L, β5 subunit), trypsin-like (T-L, β2 subunit), and caspase-like (C-L, β1 subunit) [1] [74]. Proteins destined for degradation are first tagged with polyubiquitin chains through a sequential enzymatic cascade involving E1 (activating), E2 (conjugating), and E3 (ligating) enzymes. The 19S regulatory particle recognizes these ubiquitinated proteins, unfolds them, and translocates them into the 20S core for proteolysis [1] [20].
Malignant cells, particularly those derived from hematologic lineages, exhibit heightened dependence on UPS function due to increased protein synthesis and metabolic stress. MM plasma cells produce massive quantities of immunoglobulins, creating exceptional endoplasmic reticulum (ER) stress and reliance on proteasomal clearance of misfolded proteins [20]. Similarly, MCL cells demonstrate sensitivity to proteasome disruption through multiple mechanisms [75]. This differential dependence creates a therapeutic window that PIs effectively exploit. The impact of proteasome inhibition on cellular ubiquitin levels and protein homeostasis is profound, resulting in the accumulation of polyubiquitinated proteins and triggering multiple pro-apoptotic signaling cascades [22].
Clinical Efficacy of Approved Proteasome Inhibitors
Key Agents and Their Properties
Three PIs are currently approved for clinical use in MM and/or MCL, each with distinct pharmacophores, binding kinetics, and toxicity profiles.
Table 1: Approved Proteasome Inhibitors in Hematologic Malignancies
| Name (Brand) | Pharmacophore | Binding Mechanism | Primary Indications | Common Toxicities |
|---|---|---|---|---|
| Bortezomib (Velcade) | Boronic acid | Reversible inhibition (β5>β1>β2) | Newly diagnosed & relapsed/refractory MM; Relapsed/refractory MCL | Peripheral neuropathy, thrombocytopenia, gastrointestinal disturbances [20] [65] |
| Carfilzomib (Kyprolis) | Epoxyketone | Irreversible inhibition (β5>β2/β1) | Relapsed/refractory MM | Dyspnea, cytopenias, fatigue, hypertension [74] [65] |
| Ixazomib (Ninlaro) | Boronic acid | Reversible inhibition (β5>β1) | Relapsed/refractory MM (oral) | Diarrhea, thrombocytopenia, rash, peripheral neuropathy [74] [65] |
Efficacy Outcomes in Multiple Myeloma
In MM, PIs have fundamentally improved treatment paradigms and patient outcomes. As single agents, they demonstrate significant activity, but their efficacy is enhanced in combination regimens.
Bortezomib: The landmark APEX trial established bortezomib's superiority over high-dose dexamethasone in relapsed MM, with a significantly higher response rate (38% vs 18%, p<0.001) and longer time to progression (6.22 vs 3.49 months; HR 0.55; p<0.001) [20]. Subsequent studies confirmed its role in newly diagnosed MM, both in transplant-eligible and ineligible patients.
Carfilzomib: This next-generation agent demonstrates efficacy in bortezomib-resistant disease due to its irreversible binding mechanism. In the ENDEAVOR trial, carfilzomib-dexamethasone outperformed bortezomib-dexamethasone in relapsed/refractory MM, achieving superior median progression-free survival (PFS) (18.7 vs 9.4 months; HR 0.53, p<0.0001) [74].
Ixazomib: As the first oral PI, ixazomib offers convenience with maintained efficacy. The TOURMALINE-MM1 trial showed that adding ixazomib to lenalidomide-dexamethasone significantly improved PFS in relapsed/refractory MM (20.6 vs 14.7 months; HR 0.74, p=0.01) [74].
Meta-analyses of randomized controlled trials (RCTs) confirm that PI-based maintenance or consolidation therapy post-induction or autologous stem cell transplantation (ASCT) significantly improves depth of response and survival outcomes. PI-based regimens significantly improve rates of complete response (CR) and very good partial response or better (≥VGPR), and are associated with significantly prolonged PFS and overall survival (OS) compared to control groups [76].
Efficacy Outcomes in Mantle Cell Lymphoma
MCL represents another lymphoid malignancy with demonstrated susceptibility to PIs. Bortezomib received approval for relapsed/refractory MCL based on the PINNACLE trial, a phase II study in which patients achieved an overall response rate of 33% with a median duration of response of 9.2 months [75] [77]. MCL's sensitivity to PIs is particularly noteworthy given its generally poor prognosis with conventional chemotherapy. The efficacy in MCL is attributed to multiple mechanisms, including disruption of NF-κB signaling and induction of oxidative stress, as discussed in subsequent sections [75].
Table 2: Selected Clinical Trial Outcomes for Proteasome Inhibitors
| Trial/Agent | Patient Population | Regimen | Key Efficacy Endpoint | Result |
|---|---|---|---|---|
| APEX (Bortezomib) | Relapsed MM | Bortezomib vs High-Dose Dexamethasone | Time to Progression | 6.22 vs 3.49 months (HR 0.55; p<0.001) [20] |
| ENDEAVOR (Carfilzomib) | Relapsed/Refractory MM | Carfilzomib+Dex vs Bortezomib+Dex | Median PFS | 18.7 vs 9.4 months (HR 0.53; p<0.0001) [74] |
| TOURMALINE-MM1 (Ixazomib) | Relapsed/Refractory MM | Ixazomib+Len+Dex vs Placebo+Len+Dex | Median PFS | 20.6 vs 14.7 months (HR 0.74; p=0.01) [74] |
| PINNACLE (Bortezomib) | Relapsed/Refractory MCL | Bortezomib single-agent | Overall Response Rate | 33% (CR+CRu: 8%) [75] |
| Meta-analysis (PIs) | MM Maintenance/Consolidation | PI-based vs Control | Progression-Free Survival | Significant improvement (HR <1; p<0.05) [76] |
Molecular Mechanisms of Action
Proteasome inhibitors exert pleiotropic effects on malignant cells, triggering cell death through multiple interconnected pathways. The primary consequence of proteasome inhibition is the accumulation of polyubiquitinated proteins, disrupting cellular homeostasis.
Key Signaling Pathways in Proteasome Inhibitor Cytotoxicity
The following diagram illustrates the major molecular mechanisms activated by proteasome inhibition, leading to apoptosis in MM and MCL cells.
Detailed Mechanistic Analysis
Unfolded Protein Response and ER Stress: MM cells experience high ER stress due to immunoglobulin production. PIs prevent clearance of misfolded proteins from the ER, exacerbating this stress and switching the unfolded protein response from pro-survival to pro-apoptotic signaling, ultimately leading to caspase activation [75] [20].
NF-κB Pathway Inhibition: Constitutive NF-κB activation promotes survival in many hematologic malignancies. NF-κB is normally sequestered in the cytoplasm by IκBα. Signal-induced phosphorylation targets IκBα for ubiquitin-dependent proteasomal degradation, freeing NF-κB. PIs prevent IκBα degradation, thereby trapping NF-κB in the cytoplasm and blocking transcription of anti-apoptotic genes like Bcl-2 and XIAP [75] [78].
Cell Cycle and Apoptosis Regulation: PIs disrupt the tightly controlled degradation of cell cycle regulators. Accumulation of cyclin-dependent kinase inhibitors (e.g., p21, p27) induces cell cycle arrest. Furthermore, PIs prevent the degradation of pro-apoptotic proteins like Noxa and Bim, shifting the balance toward mitochondrial apoptosis. Noxa upregulation is particularly critical in MCL, where it neutralizes the anti-apoptotic protein Mcl-1, releasing Bak and triggering apoptosis [75] [77].
Oxidative Stress: PIs induce the generation of reactive oxygen species (ROS) in malignant cells. Antioxidants can partially reverse PI lethality, confirming the role of oxidative injury. In MCL, the cellular antioxidant defense capacity is a key determinant of sensitivity to bortezomib [75].
Experimental Protocols for Investigating Proteasome Inhibition
This section provides detailed methodologies for key experiments used to evaluate proteasome function and inhibitor efficacy in a research setting.
Assessing Proteasome Inhibition and UPS Function
Workflow for Evaluating UPS Inhibition
Protocol 1: Measuring Proteasome Activity and Ubiquitinated Protein Accumulation
- Objective: To quantify chymotrypsin-like proteasome activity and detect the accumulation of polyubiquitinated proteins in cells treated with a proteasome inhibitor.
- Materials:
- Cell line of interest (e.g., MM.1S multiple myeloma cells)
- Proteasome inhibitor (e.g., Bortezomib, dissolved in DMSO)
- Fluorogenic proteasome substrate (e.g., Suc-LLVY-AMC for CT-L activity)
- Lysis buffer (e.g., 50 mM Tris-HCl, pH 7.5, 250 mM sucrose, 5 mM MgCl2, 1 mM DTT, 0.5% NP-40)
- Assay buffer (50 mM HEPES, pH 7.5, 5 mM EDTA)
- SDS-PAGE and Western blot equipment
- Primary antibodies: Anti-ubiquitin, Anti-β-actin (loading control)
- Method:
- Cell Treatment: Seed cells and allow to adhere. Treat with a concentration range of the PI (e.g., 1-100 nM bortezomib) and a DMSO vehicle control for a predetermined time (e.g., 4-16 hours).
- Cell Lysis: Harvest cells, wash with PBS, and lyse in ice-cold lysis buffer containing protease inhibitors. Centrifuge at high speed (e.g., 16,000 × g) for 15 minutes at 4°C to remove insoluble debris. Determine protein concentration of the supernatant.
- Proteasome Activity Assay:
- In a black 96-well plate, combine cell lysate (10-20 µg protein), assay buffer, and fluorogenic substrate (e.g., 100 µM Suc-LLVY-AMC) in a final volume of 100 µL.
- Immediately measure the increase in fluorescence (excitation ~380 nm, emission ~460 nm for AMC) kinetically over 60-90 minutes using a plate reader.
- Calculate activity relative to the DMSO control after subtracting background from a no-lysate control.
- Western Blot Analysis:
- Separate equal amounts of protein (20-30 µg) from the lysates by SDS-PAGE.
- Transfer to PVDF membrane and probe with anti-ubiquitin antibody. A characteristic "smear" of high molecular weight proteins indicates accumulation of polyubiquitinated substrates.
- Strip and re-probe membrane with anti-β-actin to confirm equal loading [22].
Protocol 2: Cell Viability and Apoptosis Assay
- Objective: To determine the cytotoxic effect of a proteasome inhibitor and confirm induction of apoptosis.
- Materials:
- WST-1 or MTT tetrazolium salt
- Annexin V-FITC / Propidium Iodide (PI) staining kit
- Flow cytometer
- Caspase inhibitor (e.g., Q-VD-OPh)
- Method:
- Cell Viability (Proliferation):
- Seed cells at low density (1500-5000 cells/well) in a 96-well plate.
- The next day, treat with a serial dilution of the PI. Incubate for 48-72 hours.
- Add WST-1 reagent and incubate for 1-4 hours. Measure absorbance at 440-480 nm. Calculate IC50 values using non-linear regression analysis [22].
- Apoptosis Detection:
- Treat cells with PI for 16-24 hours.
- Harvest cells and stain with Annexin V-FITC and PI according to manufacturer's instructions.
- Analyze by flow cytometry within 1 hour. Annexin V+/PI- cells are in early apoptosis; Annexin V+/PI+ cells are in late apoptosis/necrosis.
- To confirm caspase-dependence, pre-treat cells with a pan-caspase inhibitor like Q-VD-OPh (10-20 µM) for 1 hour before adding the PI [22].
- Cell Viability (Proliferation):
The Scientist's Toolkit: Key Research Reagents
Table 3: Essential Reagents for Studying Proteasome Inhibition
| Reagent / Assay | Function / Utility | Example Product / Target |
|---|---|---|
| Fluorogenic Proteasome Substrates | Quantify specific proteasome catalytic activities in cell lysates or purified complexes. | Suc-LLVY-AMC (CT-L), Z-LLE-AMC (C-L), Boc-LRR-AMC (T-L) [74] |
| UPS Reporter Cell Lines | Visually monitor global UPS inhibition in live cells via fluorescence accumulation. | Ub-YFP, Ub-R-GFP, YFP-CL1, ZsGreen-ODC [22] |
| Apoptosis Detection Kits | Distinguish stages of apoptosis and necrosis through flow cytometry. | Annexin V-FITC/PI Staining Kit [22] |
| Deubiquitylating (DUB) Enzymes | Study the interplay between proteasome inhibition and ubiquitin chain disassembly. | Recombinant UCHL5, USP14 [22] |
| CRISPR/Cas9 Screening Libraries | Perform unbiased genetic screens to identify mediators of PI sensitivity/resistance. | Whole-genome sgRNA library (e.g., identifies NQO1 as a bioactivator) [22] |
| Specific Antibodies | Detect key molecular events by Western blot or immunofluorescence. | Anti-Ubiquitin, Anti-Noxa, Anti-cleaved Caspase-3, Anti-p-IκBα [75] [22] |
Proteasome inhibitors represent a cornerstone of targeted therapy for MM and MCL, validating the UPS as a critical target in oncology. Their clinical efficacy is firmly rooted in the profound disruption of protein homeostasis, leading to integrated cellular stress and apoptosis. Ongoing research focuses on overcoming resistance to existing PIs through next-generation agents like marizomib and oprozomib, which have distinct inhibitory profiles [74]. Furthermore, combination strategies with other targeted therapies—such as BH3 mimetics to counter Mcl-1 upregulation or histone deacetylase inhibitors—show significant promise in preclinical models [75] [78]. The continued investigation into the relationship between proteasome inhibition, cellular ubiquitin dynamics, and cell death signaling will undoubtedly yield more effective and selective therapeutic strategies for these malignancies, solidifying the role of PIs in the oncologist's arsenal.
Proteasome inhibitors (PIs) have revolutionized the treatment landscape of hematologic malignancies, particularly multiple myeloma (MM) and mantle cell lymphoma, by exploiting the critical dependence of malignant plasma cells on the ubiquitin-proteasome pathway (UPP) for protein homeostasis [20] [79]. The UPP regulates intracellular protein degradation, cell cycle progression, and apoptosis through a coordinated enzymatic cascade that tags unwanted proteins with ubiquitin for destruction by the 26S proteasome [20]. The high protein turnover in myeloma cells resulting from excessive immunoglobulin production creates a therapeutic window that PIs effectively target, leading to the accumulation of misfolded proteins, endoplasmic reticulum (ER) stress, and ultimately apoptosis [20] [79]. Since the initial approval of bortezomib in 2003, followed by carfilzomib in 2012 and ixazomib in 2015, these agents have become cornerstone therapies, significantly improving progression-free and overall survival outcomes [20] [79]. However, their clinical utility is tempered by distinct safety profiles and adverse events (AEs) that necessitate careful management. This analysis comprehensively evaluates the comparative safety and pharmacovigilance signals of these three PIs within the broader context of proteasome inhibition's impact on cellular ubiquitin homeostasis, providing researchers and clinicians with evidence-based guidance for their optimal utilization.
Mechanistic Foundations of Proteasome Inhibitors
The Ubiquitin-Proteasome Pathway and Inhibitor Targeting
The 26S proteasome is a multi-subunit complex consisting of a 20S catalytic core particle flanked by one or two 19S regulatory particles [20]. The 20S core features three primary proteolytic activities: chymotrypsin-like (β5 subunit), trypsin-like (β2 subunit), and caspase-like (β1 subunit) [20] [79]. The chymotrypsin-like activity is the rate-limiting step in protein degradation and represents the primary target for all approved PIs [20] [80]. Inhibition of the proteasome disrupts multiple cellular processes, including NF-κB activation, cell cycle progression, and the unfolded protein response (UPR), ultimately leading to apoptosis through various mechanisms including JNK activation, p53 stabilization, and increased expression of pro-apoptotic proteins like NOXA [20] [81].
Structural and Kinetic Differences Among Proteasome Inhibitors
Although bortezomib, carfilzomib, and ixazomib all primarily target the β5 subunit, they exhibit important differences in chemical structure, binding kinetics, and subunit selectivity that influence their efficacy and safety profiles:
- Bortezomib: A reversible boronate-based inhibitor that targets β5 with some cross-inhibition of β1 at higher concentrations [20]. It can be administered intravenously or subcutaneously.
- Carfilzomib: An irreversible epoxyketone-based inhibitor with greater selectivity for β5 and minimal off-target activity [79]. It requires intravenous administration.
- Ixazomib: A reversible boronate-based inhibitor like bortezomib but designed as the first oral PI [20]. It demonstrates similar subunit selectivity to bortezomib.
Table 1: Fundamental Characteristics of Approved Proteasome Inhibitors
| Characteristic | Bortezomib | Carfilzomib | Ixazomib |
|---|---|---|---|
| Year of FDA Approval | 2003 | 2012 | 2015 |
| Chemical Class | Boronate | Epoxyketone | Boronate |
| Binding Kinetics | Reversible | Irreversible | Reversible |
| Primary Target | β5 subunit | β5 subunit | β5 subunit |
| Administration Route | IV/SC | IV | Oral |
| Half-life (Recovery of β5 activity) | 15-20 hours | <24 hours | <4 hours |
The differential kinetics and administration routes significantly impact both the safety profiles and practical clinical application of these agents. The irreversible binding of carfilzomib provides sustained proteasome inhibition but may contribute to different toxicity patterns compared to the reversible inhibitors [79]. The oral administration of ixazomib offers convenience but introduces variability in drug exposure that may influence both efficacy and safety [20].
Comparative Safety Profiles: Pharmacovigilance Evidence
Analysis of Real-World Safety Data
Large-scale pharmacovigilance studies utilizing the FDA Adverse Event Reporting System (FAERS) database provide robust real-world evidence of the distinct safety profiles associated with each PI. A recent comprehensive analysis of FAERS data demonstrated significant differences in system-organ class (SOC) level adverse events [82]:
- Bortezomib: Showed the most significant SOC signal for "blood and lymphatic system disorders" (ROR = 3.47, 95% CI 3.37-3.57), with the most notable preferred term (PT) being "enteric neuropathy" (ROR = 134.96, 95% CI 45.67-398.79) [82].
- Carfilzomib: Also exhibited significant signals for "blood and lymphatic system disorders" (ROR = 4.34, 95% CI 4.17-4.53), with the most significant PT being "light chain analysis increased" (ROR = 76.65, 95% CI 57.07-102.96) [82].
- Ixazomib: Demonstrated a distinct profile with the most significant SOC signal for "gastrointestinal disorders" (ROR = 2.04, 95% CI 1.96-2.12), while sharing "light chain analysis increased" as a significant PT (ROR = 67.15, 95% CI 45.36-99.42) [82].
Infection-Related Adverse Events
Infection represents a significant concern with PI therapy due to the immunocompromised state of MM patients combined with the immunomodulatory effects of proteasome inhibition. A focused pharmacovigilance study analyzing infection-related AEs revealed distinct patterns [83]:
- Bortezomib: Associated with 43 infection-related AEs, most commonly cytomegalovirus infection [83].
- Carfilzomib: Associated with 23 infection-related AEs, most commonly bacteremia [83].
- Ixazomib: Associated with 10 infection-related AEs, most commonly conjunctivitis [83].
The higher incidence of viral reactivation with bortezomib may relate to its more profound effect on immune cell function, while the association of carfilzomib with bacteremia may reflect its use in more heavily pretreated patients with greater compromise of host defenses.
Table 2: Comparative Safety Signals of Proteasome Inhibitors Based on FAERS Analysis
| Safety Parameter | Bortezomib | Carfilzomib | Ixazomib |
|---|---|---|---|
| Most Significant SOC Signal | Blood and lymphatic system disorders | Blood and lymphatic system disorders | Gastrointestinal disorders |
| SOC ROR (95% CI) | 3.47 (3.37-3.57) | 4.34 (4.17-4.53) | 2.04 (1.96-2.12) |
| Most Significant PT Signal | Enteric neuropathy | Light chain analysis increased | Light chain analysis increased |
| PT ROR (95% CI) | 134.96 (45.67-398.79) | 76.65 (57.07-102.96) | 67.15 (45.36-99.42) |
| Most Common Infection AE | Cytomegalovirus infection | Bacteremia | Conjunctivitis |
| Peripheral Neuropathy | High incidence | Lower incidence | Lower incidence |
| Hematological Toxicity | Significant | Most significant | Moderate |
Characteristic Adverse Events and Management Considerations
Peripheral Neuropathy
Peripheral neuropathy (PN) represents one of the most clinically significant dose-limiting toxicities of PIs, with considerable variation among the class [20] [81]. Bortezomib demonstrates the highest incidence of PN, attributed to its off-target inhibition of neuronal proteasomes and effects on mitochondrial function [81]. Strategies to mitigate bortezomib-induced PN include subcutaneous administration, dose modification, and schedule adjustments [81]. In contrast, carfilzomib and ixazomib show markedly reduced neurotoxicity, likely due to their greater selectivity for the constitutive proteasome over those in neuronal tissue [79]. This improved neurological safety profile makes them preferred options for patients with pre-existing neuropathy or those who develop significant neurotoxicity on bortezomib.
Cardiovascular and Renal Toxicity
Carfilzomib demonstrates a distinct profile of cardiovascular toxicity, including dyspnea, hypertension, and cardiac failure, which necessitates careful monitoring especially in patients with pre-existing cardiac conditions [20] [79]. The mechanism may involve accumulation of pro-apoptotic proteins in cardiomyocytes or endothelial dysfunction. Renal manifestations also differ among the PIs, with carfilzomib associated with acute kidney injury possibly related to its irreversible binding and tumor lysis effects [83] [20]. Bortezomib, in contrast, may be beneficial in myeloma-related renal impairment due to its rapid action and efficacy in reducing monoclonal light chains.
Gastrointestinal Toxicity
Ixazomib demonstrates a higher incidence of gastrointestinal AEs, particularly diarrhea, nausea, and vomiting, consistent with its primary SOC signal in FAERS analysis [82]. This profile likely reflects both its oral administration and potentially local gastrointestinal effects. These symptoms are typically manageable with supportive care and dose modifications, but significantly impact quality of life and adherence. The gastrointestinal effects of ixazomib represent an important consideration when selecting therapy, particularly for frail patients or those with pre-existing gastrointestinal comorbidities.
Mechanisms of Resistance and Impact on Therapeutic Efficacy
Molecular Adaptations to Proteasome Inhibition
Resistance to PIs represents a significant clinical challenge and involves complex adaptive cellular mechanisms beyond simple proteasome mutations [80]. Research using proteasome inhibitor-adapted myeloma cell lines (AMO-BTZ and AMO-CFZ) revealed that resistant cells tolerate subtotal proteasome inhibition through multifaceted adaptations [80]:
- Metabolic reprogramming: Upregulation of proteins involved in metabolic regulation and redox homeostasis, favoring generation of reducing equivalents like NADPH through oxidative glycolysis [80].
- Reduced UPR activation: Uniform demonstration of an 'IRE1/XBP1-low' signature, indicating decreased activation of the unfolded protein response, which normally contributes to PI-induced apoptosis [80].
- Altered protein expression: Quantitative changes in over 600 protein species, with downregulation of apoptotic pathways and upregulation of protein folding and destruction mechanisms [80].
- Efflux pump upregulation: Significant induction of multidrug resistance protein ABCB1 (MDR1) in carfilzomib-resistant cells, with resistance reversible by MDR1 inhibition [80].
These adaptations represent potential targets for overcoming resistance, particularly the metabolic dependencies that enable resistant cells to manage proteotoxic stress.
Ubiquitination-Independent Degradation Pathways
Emerging research indicates that not all proteasomal degradation requires ubiquitination, with approximately 20% of intracellular proteins potentially undergoing ubiquitin-independent proteasomal degradation (UbInPD) [28]. The oncogenic phosphatase PPM1D represents a biologically relevant model substrate for UbInPD, being directly degraded by the 20S proteasome through its C-terminal region without ubiquitination [28]. This finding has significant therapeutic implications, as proteasome inhibition may paradoxically stabilize oncogenic drivers like PPM1D, potentially reducing therapeutic efficacy. Combined proteasome and PPM1D inhibition demonstrates synergistic antitumor effects, suggesting a novel combinatorial approach to overcome this resistance mechanism [28].
Diagram 1: Mechanisms of Sensitivity and Resistance to Proteasome Inhibitors. Resistant cells exhibit metabolic adaptations, reduced UPR activation, and efflux pump upregulation.
Experimental Approaches for Profiling Proteasome Inhibitor Effects
Methodologies for Pharmacovigilance Analysis
The safety profiles presented in this analysis derive primarily from sophisticated statistical analysis of the FAERS database using quantitative signal detection algorithms [83] [82]. Key methodological approaches include:
- Reporting Odds Ratio (ROR): Calculated as the ratio of the odds of reporting a specific adverse event for the drug of interest versus all other drugs in the database. A signal is typically considered when the lower limit of the 95% confidence interval exceeds 1.0 [82].
- Proportional Reporting Ratios (PRR): Compares the proportion of specific adverse events for a drug to the proportion of the same events for all other drugs [83].
- Multi-item Gamma-Poisson Shrinker (MGPS): A Bayesian method that uses empirical Bayes geometric mean to estimate the strength of association between drugs and adverse events [83].
These methodologies enable detection of potential safety signals that may not be evident in pre-marketing clinical trials due to limited sample sizes and restricted patient populations.
Proteomic and Molecular Techniques
Elucidation of resistance mechanisms and differential sensitivity employs advanced proteomic and molecular approaches [80] [84]:
- Quantitative proteomics: Using stable isotope labeling (SILAC) with mass spectrometry to compare protein expression profiles in sensitive versus resistant cell lines [80].
- Activity-based proteasome profiling: Direct measurement of proteasome subunit inhibition using fluorogenic substrates specific for β5, β1, and β2 activities [80].
- Gene expression analysis: Assessment of UPR pathway components including IRE1, XBP1 (spliced and unspliced), and downstream targets [80].
- Viability and apoptosis assays: Determination of IC50 values and correlation with proteasome inhibition levels [84].
These techniques provide comprehensive insights into the molecular adaptations underlying differential responses to PIs.
Table 3: Essential Research Reagents for Studying Proteasome Inhibitor Mechanisms
| Research Reagent | Application/Function | Experimental Context |
|---|---|---|
| Fluorogenic proteasome substrates (Suc-LLVY-AMC for β5, Z-LLE-AMC for β1, Boc-LRR-AMC for β2) | Specific measurement of proteasome catalytic activities | In vitro and cellular proteasome activity assays [80] |
| TAK-243 (MLN7243) | Selective inhibitor of ubiquitin E1 activating enzyme | Distinguishing ubiquitin-dependent and independent degradation [84] [28] |
| Cycloheximide | Protein synthesis inhibitor | Measurement of protein half-life (chase assays) [28] |
| Proteasome inhibitors (MG132, bortezomib, carfilzomib) | Specific proteasome inhibition | Controls for proteasome-dependent degradation experiments [28] |
| Antibodies for UPR markers (IRE1, XBP1s, XBP1u) | Detection of unfolded protein response activation | Western blot, immunohistochemistry [80] |
| Stable isotope labeling (SILAC reagents) | Quantitative mass spectrometry-based proteomics | Global protein expression profiling [80] |
The comparative safety analysis of bortezomib, carfilzomib, and ixazomib reveals distinct profiles that reflect their structural differences, binding kinetics, and administration routes. Bortezomib carries the highest risk of peripheral neuropathy but demonstrates well-characterized management strategies. Carfilzomib shows reduced neurotoxicity but increased cardiovascular and renal concerns, while ixazomib offers convenient oral administration with predominant gastrointestinal toxicity. These differences enable clinicians to tailor PI selection based on individual patient risk factors, comorbidities, and treatment history.
Future research directions should focus on several critical areas. First, deeper understanding of the molecular determinants of differential toxicity may enable development of next-generation PIs with improved therapeutic indices. Second, elucidating the precise mechanisms underlying ubiquitin-independent degradation pathways may reveal novel biomarkers for treatment response and resistance. Third, combinatorial strategies targeting the adaptive responses of myeloma cells to proteasome inhibition, particularly metabolic reprogramming and reduced UPR activation, hold promise for overcoming resistance. Finally, prospective studies directly comparing these agents in defined patient populations would provide valuable evidence to guide optimal sequencing and selection in the context of modern combination regimens.
As proteasome inhibition remains a cornerstone of multiple myeloma therapy, ongoing pharmacovigilance and mechanistic research will continue to refine our understanding of these critical agents, ultimately enhancing their efficacy and safety in clinical practice.
Diagram 2: Adverse Event Spectrum Across Proteasome Inhibitors. Each inhibitor demonstrates a distinct pattern of organ-specific toxicities.
The field of proteasome inhibition represents a cornerstone of modern targeted cancer therapy, with its evolution deeply intertwined with global demographic shifts. The growing prevalence of hematologic malignancies, driven in part by an expanding aging population, serves as a primary catalyst for the proteasome inhibitors market [85] [86]. This in-depth technical guide examines the market trajectory and its underlying drivers, framed within the critical scientific context of ubiquitin-proteasome system (UPS) research. For scientists and drug development professionals, understanding this interplay is essential for guiding the development of next-generation therapies that address not only oncogenic targets but also the demographic realities of patient populations. The proteasome is a sophisticated cellular machinery responsible for the controlled degradation of intracellular proteins, a process predominantly regulated by the covalent attachment of ubiquitin chains [17]. Disruption of this system in cancerous cells leads to the accumulation of pro-apoptotic proteins and cell death, a mechanism harnessed by proteasome inhibitors. Contemporary research continues to refine our understanding of this system, exploring novel mechanisms of inhibition and expanding potential therapeutic applications.
Market Size, Growth Projections, and Key Drivers
Quantitative Market Analysis
The global proteasome inhibitors market is on a robust growth trajectory, fueled by rising disease incidence, drug development advancements, and growing investments in oncology research [85]. The following table synthesizes key market metrics from recent analyses:
| Market Metric | Figures & CAGR | Source & Forecast Period |
|---|---|---|
| Market Size (2024) | USD 2.7 Billion | [85] |
| Projected Market Size (2034) | USD 6.1 Billion | [85] (Forecast 2025-2034) |
| Compound Annual Growth Rate (CAGR) | 8.7% | [85] (Forecast 2025-2034) |
| Alternative CAGR | 8.4% | [86] (Forecast 2025-2029) |
| Alternative Projection | Increase of USD 4.42 Billion | [86] (Forecast 2025-2029) |
This growth is underpinned by several key drivers. The rising prevalence of hematologic cancers, particularly multiple myeloma and mantle cell lymphoma, creates a sustained demand for effective treatments [85] [86]. Furthermore, continuous advancements in drug development are leading to novel inhibitors with improved efficacy and risk profiles, such as the second-generation drug carfilzomib and the oral agent ixazomib [85] [86]. A significant demographic driver is the global aging population, as the incidence of multiple myeloma is strongly correlated with age [85] [87]. The expanding elderly population is projected to substantially increase the patient pool eligible for proteasome inhibitor therapy.
The Impact of an Aging Population
The "age wave" is not a distant future scenario but a current demographic shift with profound implications for healthcare markets. In the United States, the population aged 80 and above is expected to grow from 14.7 million in 2025 to nearly 23 million by 2035, representing a growth rate of over 55% [87]. This demographic will comprise 10% of the total population by 2030, up from 7.5% today [88].
This demographic shift directly fuels the proteasome inhibitor market through several mechanisms:
- Increased Cancer Incidence: Age is a major risk factor for most cancers. The prevalence of multiple myeloma, which accounts for approximately 10% of all hematological malignancies, is expected to rise significantly alongside the growing elderly population [85] [86].
- Evolving Treatment Paradigms: Today's older adults are living longer, healthier lives, creating a demand for effective, targeted therapies that maintain quality of life [87]. This aligns with the clinical profile of newer proteasome inhibitors used in combination regimens.
Scientific Foundations: Ubiquitin-Proteasome System and Inhibition Mechanisms
The Canonical Ubiquitin-Proteasome Pathway
The ubiquitin-proteasome system is the primary pathway for regulated intracellular protein degradation in eukaryotes. The following diagram illustrates the canonical pathway and the points of inhibition by therapeutic agents and research tools.
The canonical pathway involves a cascade of E1 (activating), E2 (conjugating), and E3 (ligating) enzymes that attach a polyubiquitin chain to a target protein, marking it for degradation by the 26S proteasome [17]. This process is critical for maintaining cellular homeostasis by controlling the levels of key regulatory proteins. Clinical proteasome inhibitors, such as bortezomib and carfilzomib, function by directly binding to and inhibiting the proteolytic active sites of the proteasome's 20S core particle, thereby disrupting protein turnover and leading to apoptosis in cancer cells [85] [28].
Expanding Frontiers: Novel Mechanisms and Ubiquitin-Independent Degradation
Recent research has unveiled more complex and nuanced interactions with the UPS, opening new avenues for therapeutic intervention. A groundbreaking study reported the discovery of a small molecule, BRD1732, which is itself directly ubiquitinated in cells by the E3 ligases RNF19A and RNF19B and their E2 enzyme UBE2L3 [17]. This ubiquitination occurs on the molecule's azetidine secondary amine, leading to dramatic accumulation of inactive ubiquitin-BRD1732 conjugates and diubiquitin chains, causing broad inhibition of the UPS through a novel "ubiquitin sequestration" mechanism [17].
Furthermore, a significant subset of cellular proteins is degraded in a ubiquitin-independent manner. The oncogenic phosphatase PPM1D is a key model substrate for this pathway. It is directly degraded by the 20S proteasome through specific recognition of its C-terminal region, without the need for ubiquitin tagging [28]. This has direct therapeutic implications, as proteasome inhibitor treatment can lead to the accumulation of oncogenic PPM1D, potentially reducing therapeutic efficacy. This suggests that combined inhibition of the proteasome and PPM1D could synergistically enhance antitumor effects [28].
Key Experimental Methodologies and Reagent Solutions
Core Experimental Protocols
Research in this field relies on a suite of well-established biochemical and cellular assays. Below are detailed methodologies for key experiments cited in the foundational research.
Protocol 1: Assessing Protein Stability via Cycloheximide Chase Assay This protocol is used to measure the half-life of a protein of interest, such as PPM1D [28].
- Cell Seeding and Treatment: Seed cells (e.g., HCT116, U2OS) in multi-well plates and allow them to adhere overnight.
- Translation Inhibition: Treat cells with cycloheximide (typically at 50-100 µg/mL) to halt de novo protein synthesis.
- Time-Course Harvesting: Lyse cells at predetermined time points (e.g., 0, 1, 2, 4, 8 hours) post-cycloheximide addition.
- Immunoblot Analysis: Resolve proteins by SDS-PAGE and transfer to a membrane. Probe with a target-specific primary antibody (e.g., anti-PPM1D) and a corresponding HRP-conjugated secondary antibody.
- Quantification: Detect signals using enhanced chemiluminescence reagents and quantify band intensity. Plot the relative protein level against time to determine degradation kinetics.
Protocol 2: Identifying UPS Dependencies via CRISPR-Cas9 Screening This genome-wide approach identifies genes required for a small molecule's cytotoxicity, as used for BRD1732 [17].
- Library Transduction: Infect a haploid cell line (e.g., HAP1) expressing Cas9 with a genome-wide lentiviral sgRNA library at a low MOI to ensure single integration.
- Selection and Treatment: Select transduced cells with puromycin. Split the cell population and treat one with the compound (e.g., BRD1732 at its IC50) and another with a vehicle control (DMSO).
- Outgrowth and Harvest: Culture cells for several population doublings to allow outgrowth of resistant clones. Harvest genomic DNA from both treated and control populations.
- PCR Amplification & Sequencing: Amplify the integrated sgRNA sequences by PCR and subject them to high-throughput sequencing.
- Bioinformatic Analysis: Compare sgRNA abundance between treatment and control groups. Significantly enriched sgRNAs in the treated population identify genes whose knockout confers resistance (e.g., RNF19A, RNF19B, UBE2L3).
Protocol 3: Direct Ubiquitin Conjugate Characterization by LC-MS This protocol confirms direct ubiquitination of a small molecule [17].
- Treatment and Ubiquitin Purification: Treat cells (e.g., Expi293F overexpressing RNF19A) with the compound of interest (e.g., 10 µM BRD1732 for 6 hours). Lyse cells under nondenaturing conditions.
- Chromatography: Purify endogenous ubiquitin from the lysate using a two-step process: cation exchange chromatography followed by size-exclusion chromatography (SEC).
- Liquid Chromatography-Mass Spectrometry (LC-MS): Analyze the purified samples by LC-MS.
- Data Analysis: Compare the mass of ubiquitin from treated and untreated cells. An exact mass shift corresponding to the compound minus a water molecule confirms a covalent adduct. For further characterization, perform trypsin digestion under nondenaturing conditions and analyze the resulting fragments (e.g., Gly-Gly-BRD1732).
The Scientist's Toolkit: Key Research Reagents
The following table details essential materials and reagents used in the featured studies, providing a resource for experimental design.
| Reagent / Tool | Function & Application in UPS Research |
|---|---|
| MG132 | A peptide aldehyde that acts as a potent, reversible proteasome inhibitor. Commonly used in in vitro experiments to block proteasomal activity and stabilize short-lived proteins [28]. |
| Bortezomib | A clinically approved dipeptide boronic acid that reversibly inhibits the chymotrypsin-like activity of the proteasome. Used both therapeutically and as a research tool to study proteasome function [16] [28]. |
| Carfilzomib | A second-generation, tetrapeptide epoxyketone that irreversibly inhibits the proteasome. Used in research to achieve sustained inhibition and study its consequences [16] [28]. |
| TAK-243 | A specific inhibitor of the E1 ubiquitin-activating enzyme (UBA1). Used to determine if a protein's degradation is ubiquitin-dependent by globally shutting down the ubiquitination cascade [28]. |
| Bafilomycin A1 / Chloroquine | Inhibitors of lysosomal acidification and autophagic degradation. Used to distinguish proteasomal degradation from lysosomal degradation pathways [16]. |
| Cycloheximide | A protein synthesis inhibitor. Essential for cycloheximide chase assays to measure protein half-life without confounding from new protein synthesis [28]. |
| GSK2830371 | A specific, allosteric inhibitor of PPM1D phosphatase activity. Used to probe the biological functions of PPM1D and explore combination therapies with proteasome inhibitors [28]. |
Future Directions and Research Opportunities
The convergence of market demands and scientific innovation is shaping the future of the proteasome inhibition field. Key trends and opportunities include:
- Next-Generation Inhibitors: Research is focused on developing inhibitors with improved safety profiles, oral bioavailability, and the ability to overcome resistance mechanisms [86] [89]. This includes exploring non-boronic acid based chemistries and targeted delivery systems.
- Expansion into Non-Oncological Indications: Emerging research, such as the rescue of pathogenic pendrin protein variants linked to Pendred syndrome using proteasome inhibitors, suggests potential applications beyond oncology, particularly in genetic and inflammatory diseases [16].
- Combination Therapies and Synthetic Lethality: The synergistic effect observed between proteasome inhibitors and PPM1D inhibitors highlights the promise of rational combination therapies [28]. Combining proteasome inhibitors with other modalities, such as CAR-T cell therapy or checkpoint inhibitors, represents a major frontier in oncology [86].
- Harnessing Novel Mechanisms: The discovery of small-molecule ubiquitination by BRD1732 opens the possibility of "ubiquitin sequestration" as a new therapeutic modality and a powerful research tool for perturbing the UPS [17].
The proteasome inhibitors market is poised for sustained growth, powerfully driven by the undeniable demographic force of an aging global population and continuous scientific advancement. For researchers and drug development professionals, the future lies in leveraging deep mechanistic insights into the UPS—from canonical degradation and ubiquitin-independent pathways to novel inhibition mechanisms—to develop more effective and targeted therapies. The ongoing elucidation of the complex interplay between proteasome inhibition, cellular ubiquitin levels, and oncogenic signaling networks will undoubtedly unlock new therapeutic possibilities and solidify the central role of the UPS in precision medicine.
The ubiquitin-proteasome system (UPS) represents the primary pathway for controlled intracellular protein degradation in eukaryotic cells, playing an indispensable role in maintaining cellular homeostasis by regulating protein turnover, eliminating damaged proteins, and controlling critical processes such as cell cycle progression, apoptosis, and stress response [18] [5]. This complex biochemical machinery operates through a two-step process: first, proteins designated for degradation are covalently tagged with polyubiquitin chains through a sequential enzymatic cascade involving E1 (activating), E2 (conjugating), and E3 (ligating) enzymes; second, these tagged proteins are recognized and degraded by the 26S proteasome, releasing ubiquitin and peptides for recycling [18] [5]. The 26S proteasome itself is a massive multi-subunit complex comprising a barrel-shaped 20S core particle, which contains the proteolytic active sites, capped by one or two 19S regulatory particles that recognize ubiquitinated substrates, unfold them, and facilitate their translocation into the catalytic chamber [74] [90].
The therapeutic targeting of the UPS, particularly through proteasome inhibition, has emerged as a validated strategy for cancer treatment, most notably in multiple myeloma and mantle cell lymphoma [74] [90]. The clinical success of first-generation proteasome inhibitors has demonstrated that despite the proteasome's ubiquitous nature, a therapeutic window exists for selectively targeting malignant cells, particularly those with high protein synthesis rates and dependency on proteostasis networks [91]. However, limitations associated with existing drugs—including resistance development, suboptimal pharmacokinetic profiles, and inadequate tissue distribution—have spurred intensive efforts to develop next-generation inhibitors [74]. This review examines recent advances in irreversible and oral proteasome inhibitors, framed within the broader context of understanding how proteasome inhibition impacts cellular ubiquitin dynamics and protein homeostasis.
Clinically Established Proteasome Inhibitors: Foundations for Next-Generation Development
Currently, three proteasome inhibitors are approved for clinical use, each representing distinct stages in the evolution of this drug class and providing valuable insights that have guided the development of next-generation agents.
Table 1: Clinically Approved Proteasome Inhibitors
| Drug Name (Brand Name) | Pharmacophore | Binding Mechanism | Administration Route | Key Clinical Indications | IC₅₀ for CT-L Activity (nM) |
|---|---|---|---|---|---|
| Bortezomib (Velcade) | Boronic acid | Reversible | Intravenous, Subcutaneous | Multiple Myeloma, Mantle Cell Lymphoma | 5.1-5.7 [74] |
| Carfilzomib (Kyprolis) | Epoxyketone | Irreversible | Intravenous | Multiple Myeloma | 2-31 [74] |
| Ixazomib (Ninlaro) | Boronic acid | Reversible | Oral | Multiple Myeloma | 2.8-4.1 [74] |
Bortezomib, the first-in-class proteasome inhibitor approved in 2003, is a dipeptide boronic acid that reversibly inhibits the chymotrypsin-like (CT-L) activity of the β5 subunit of the proteasome [74] [90]. Its development proved that proteasome inhibition could achieve clinical efficacy with acceptable toxicity, revolutionizing the treatment of multiple myeloma. However, limitations soon emerged, including peripheral neuropathy, development of resistance, and the inconvenience of parenteral administration [74]. Carfilzomib, approved in 2012, addressed some of these limitations through an irreversible epoxyketone mechanism that provides more sustained proteasome inhibition and different toxicity profile, notably reduced peripheral neuropathy [74]. The approval of ixazomib in 2015 marked another significant advancement as the first oral proteasome inhibitor, offering improved convenience for patients [74]. Despite these advances, the therapeutic landscape continues to evolve with next-generation inhibitors designed to overcome persistent challenges.
Next-Generation Proteasome Inhibitors: Addressing Unmet Clinical Needs
Next-generation proteasome inhibitors represent strategic innovations aimed at overcoming the limitations of existing therapies, particularly focusing on irreversible inhibition mechanisms, improved safety profiles, and enhanced delivery methods.
Irreversible Inhibitors: Mechanisms and Advantages
Irreversible proteasome inhibitors, exemplified by carfilzomib and newer agents like oprozomib, form permanent covalent bonds with the catalytic threonine residues of proteasome subunits, offering several theoretical advantages over reversible inhibitors [74]. The irreversible binding mechanism typically results in more prolonged proteasome inhibition, potentially enhancing antitumor activity by persistently disrupting protein homeostasis in malignant cells. This sustained inhibition may be particularly valuable in malignancies with rapid protein turnover or those that have developed adaptive responses to transient proteasome inhibition [74]. Additionally, irreversible inhibitors may demonstrate different resistance profiles, as some resistance mechanisms to bortezomib involve mutations in the β5 subunit that affect drug binding without completely abrogating proteolytic activity; irreversible inhibitors with distinct chemical structures may overcome these specific resistance mechanisms [90].
Research into the cellular consequences of irreversible inhibition has revealed intriguing insights into UPS dynamics. Unlike reversible inhibitors, which allow gradual recovery of proteasome activity, irreversible inhibitors necessitate the synthesis of new proteasome subunits to restore function, creating a more profound and sustained disruption to protein homeostasis [74]. This fundamental difference in mechanism may explain the observed efficacy of carfilzomib in some bortezomib-resistant malignancies and has stimulated interest in developing additional irreversible inhibitors with improved pharmacological properties.
Oral Formulations: Enhancing Treatment Convenience and Flexibility
The development of oral proteasome inhibitors addresses a significant unmet need in long-term cancer management by transitioning treatment from clinical settings to patient homes. Ixazomib, the first oral proteasome inhibitor, demonstrated that oral administration could achieve clinically meaningful proteasome inhibition with comparable efficacy to parenteral agents in multiple myeloma [74]. The boronic acid pharmacophore of ixazomib provides sufficient metabolic stability and bioavailability for oral dosing, overcoming the challenges that initially prevented the development of an oral bortezomib formulation [74].
Oral administration offers several potential benefits beyond patient convenience, including the possibility of more continuous or frequent dosing schedules that maintain steadier levels of proteasome inhibition, potentially improving efficacy while reducing peak-concentration-related toxicities [86]. Additionally, oral formulations facilitate combination regimens with other oral anticancer agents, enabling entirely oral treatment protocols that may enhance adherence and quality of life during extended treatment periods [86]. The commercial success of ixazomib has validated the feasibility of oral proteasome inhibition and stimulated development of additional oral agents, particularly those incorporating irreversible inhibition mechanisms.
Emerging Investigational Agents
Several next-generation proteasome inhibitors are in various stages of clinical development, aiming to improve upon existing agents through novel chemical structures, enhanced selectivity, or optimized pharmacological properties. Marizomib (salinosporamide A) is an irreversible β-lactone inhibitor of natural product origin that exhibits broad proteasome subunit inhibition, potentially overcoming limitations associated with subunit-specific inhibitors [74]. Delanzomib is an oral reversible boronic acid inhibitor designed with improved pharmacokinetic properties [74]. Oprozomib represents a significant innovation as an oral irreversible epoxyketone inhibitor, attempting to combine the pharmacological advantages of carfilzomib with the convenience of oral administration [74].
Table 2: Investigational Next-Generation Proteasome Inhibitors
| Drug Name | Pharmacophore | Binding Mechanism | Administration Route | Development Status | Notable Features |
|---|---|---|---|---|---|
| Marizomib | β-lactone | Irreversible | Intravenous | Clinical Trials | Broad subunit inhibition; natural product origin [74] |
| Delanzomib | Boronic acid | Reversible | Oral | Clinical Trials | Improved pharmacokinetic profile [74] |
| Oprozomib | Epoxyketone | Irreversible | Oral | Clinical Trials | Oral irreversible inhibitor [74] |
These emerging agents reflect the ongoing innovation in proteasome inhibitor design, addressing limitations of existing drugs while expanding the potential applications of proteasome inhibition in oncology and beyond.
Impact of Proteasome Inhibition on Cellular Ubiquitin Levels and Dynamics
The fundamental relationship between proteasome inhibition and cellular ubiquitin dynamics represents a critical aspect of the mechanism of action of proteasome inhibitors and a key consideration in understanding both their efficacy and resistance mechanisms.
Ubiquitin Homeostasis and Proteasome Inhibition
Proteasome inhibition triggers complex perturbations in cellular ubiquitin homeostasis, characterized by rapid accumulation of polyubiquitinated proteins due to continued ubiquitination coupled with impaired degradation [5]. This disruption creates a proteotoxic crisis within cells, particularly affecting malignant cells with high protein synthesis rates and inherent proteostatic stress [74] [91]. The accumulation of polyubiquitinated proteins can be experimentally visualized through Western blot analysis using anti-ubiquitin antibodies, typically showing a characteristic smear of high-molecular-weight conjugates in inhibitor-treated cells [5]. This technique, combined with proteasome activity assays, provides a comprehensive view of the pharmacodynamic effects of proteasome inhibition on its primary biochemical target.
The interplay between proteasome inhibition and ubiquitin dynamics extends beyond simple substrate accumulation. As polyubiquitinated proteins accumulate, they sequester available cellular ubiquitin pools, potentially creating feedback mechanisms that further disrupt ubiquitin-dependent processes [5]. Additionally, the impaired recycling of ubiquitin from proteasome substrates may create ubiquitin depletion that affects other ubiquitin-dependent cellular functions, creating a complex cascade of downstream effects that contribute to both the efficacy and toxicity of proteasome inhibitors.
Resistance Mechanisms and Ubiquitin-Proteasome System Adaptation
Despite initial efficacy, resistance to proteasome inhibitors frequently develops through diverse mechanisms that often involve adaptations within the UPS itself [74] [91]. One well-characterized resistance mechanism involves mutations in the PSMB5 gene encoding the β5 proteasome subunit, the primary target of most inhibitors [90]. These mutations can reduce drug binding affinity while preserving sufficient proteolytic activity for cell survival, particularly in the presence of continued proteasome inhibitor exposure [90].
A paradoxical resistance mechanism identified through functional genetic screens involves reduced expression of 19S regulatory particle subunits [91]. Surprisingly, knockdown of certain 19S subunits confers resistance to proteasome inhibitors rather than sensitizing cells, potentially by reducing the efficiency of substrate processing and thus altering the spectrum of accumulated proteins during proteasome inhibition [91]. This suggests that specific protective factors may be less efficiently degraded when 19S function is impaired, thereby promoting cell survival under proteasome inhibitor treatment. Clinical correlative studies have supported this finding, demonstrating that lower 19S levels in multiple myeloma patients predict diminished response to carfilzomib-based therapies [91].
Figure 1: Proteasome Inhibition Signaling and Resistance Pathways. This diagram illustrates the cascade of cellular events following proteasome inhibition, from initial polyubiquitinated protein accumulation through ER stress and apoptosis induction, alongside adaptive resistance mechanisms that can lead to treatment failure.
Beyond proteasome mutations, resistance can emerge through upregulation of alternative protein degradation pathways, such as autophagy, which can compensate for impaired proteasome function [91]. Additionally, alterations in cellular stress response pathways, including the unfolded protein response and heat shock response, can enhance the capacity of cells to manage proteotoxic stress induced by proteasome inhibitors [91]. The intricate interplay between these adaptive responses highlights the remarkable plasticity of the UPS and underscores the challenge of achieving durable responses with single-agent proteasome inhibition.
Experimental Approaches for Evaluating Next-Generation Inhibitors
The development of next-generation proteasome inhibitors relies on sophisticated experimental methodologies that assess both the pharmacological properties of the inhibitors and their biological effects on the UPS and cellular physiology.
Proteasome Activity and Inhibition Assays
Standardized assays for measuring proteasome activity form the foundation of inhibitor development and characterization. The Proteasome-Glo assay system provides a luminescent method for specifically measuring the chymotrypsin-like, trypsin-like, and caspase-like activities of the proteasome in cell-based or biochemical systems [74]. This assay employs specific fluorogenic substrates that generate luminescent signals upon cleavage by the respective proteasome activities, allowing quantitative assessment of inhibitor potency and selectivity across the different catalytic subunits.
For evaluating proteasome inhibition in living cells, researchers often combine activity assays with techniques that assess the accumulation of polyubiquitinated proteins, typically through Western blot analysis using anti-ubiquitin antibodies [5]. This approach provides complementary data on the functional consequences of proteasome inhibition beyond direct enzymatic measurements. Additionally, pulse-chase experiments using labeled amino acids or click chemistry approaches can quantify global protein degradation rates, offering insights into the overall impact of inhibitors on cellular proteostasis [5].
Functional Genomics in Resistance Mechanism Identification
Advanced functional genomic approaches have proven invaluable in identifying genetic determinants of sensitivity and resistance to proteasome inhibitors. Next-generation RNAi screens, employing complex libraries with multiple shRNAs per target and extensive negative controls, have enabled comprehensive identification of genes that modulate cellular responses to proteasome inhibition [91]. These screens typically involve transducing cells with shRNA libraries followed by selection and division into treated and untreated populations, with sequencing-based quantification of shRNA abundance changes identifying genes whose depletion affects sensitivity.
Table 3: Essential Research Reagents for Proteasome Inhibition Studies
| Research Tool | Specific Examples | Application | Key Utility |
|---|---|---|---|
| Proteasome Activity Assays | Proteasome-Glo Assay System | Biochemical/cellular screening | Quantify chymotrypsin-like, trypsin-like, and caspase-like activity [74] |
| Ubiquitination Detection Antibodies | Anti-ubiquitin, Anti-polyubiquitin | Western blot, Immunoprecipitation | Detect global ubiquitination changes [5] |
| Proteasome Inhibitors (Research Grade) | MG132, Epoxomicin, Lactacystin | Mechanistic studies | Tool compounds for validating proteasome-dependent effects [90] |
| Ubiquitin Enrichment Kits | Ubiquitin Enrichment Kit | Proteomics studies | Isolate polyubiquitinated proteins for mass spectrometry [5] |
| Click Chemistry Protein Labeling | Click-iT Plus Protein Analysis Kits | Pulse-chase degradation assays | Measure nascent protein synthesis and degradation [5] |
These functional genomic approaches have revealed unexpected aspects of proteasome biology, such as the paradoxical protective effect of 19S regulatory particle depletion, highlighting the complexity of cellular responses to proteasome inhibition [91]. The integration of these screening results with clinical data has further validated their relevance, demonstrating that mechanistic insights from genetic screens can predict clinical resistance patterns and inform combination therapy strategies.
Figure 2: Functional Genomics Workflow for Proteasome Inhibitor Mechanism Studies. This diagram outlines the experimental workflow for genome-wide RNAi screens to identify genetic modifiers of proteasome inhibitor sensitivity, from library design through hit validation and clinical correlation.
Future Directions and Therapeutic Applications Beyond Oncology
The development of next-generation proteasome inhibitors continues to evolve, with several promising directions emerging that may expand the therapeutic applications of these agents beyond their current oncology focus.
Novel Therapeutic Applications
While proteasome inhibitors have established efficacy in hematologic malignancies, emerging research suggests potential applications in other pathological conditions. Recent investigations have explored proteasome inhibitors as antimalarial agents, demonstrating potent activity against Plasmodium falciparum and synergy with artemisinin-based therapies [92]. The structural differences between human and plasmodial proteasomes offer the potential for selective targeting, suggesting that pathogen-specific proteasome inhibitors could represent a new class of antimicrobial agents with reduced off-target effects [92].
Additionally, natural product-derived compounds, particularly circulating polyphenol metabolites, have shown modest proteasome-modulating activity that may contribute to their observed health benefits in chronic diseases [93]. While these natural compounds typically exhibit weaker direct proteasome inhibition compared to pharmaceutical agents, their chronic exposure and tissue distribution patterns suggest they might exert subtle modulatory effects on proteasome function that could influence disease progression in conditions like neurodegeneration, cardiovascular disease, and metabolic disorders [93].
Strategic Combination Therapies
The future clinical development of proteasome inhibitors increasingly focuses on rational combination strategies that target complementary pathways or overcome resistance mechanisms. Based on functional genomic screens that identified translation initiation factors and mTOR signaling as modifiers of proteasome inhibitor sensitivity, combinations with translation inhibitors or mTOR pathway antagonists represent a promising approach [91]. Preclinical studies have validated that mTOR inhibition by rapamycin can desensitize cells to carfilzomib, supporting the exploration of such combinations in clinical settings [91].
Similarly, the identification of autophagy as a compensatory degradation pathway during proteasome inhibition has stimulated interest in combining proteasome inhibitors with autophagy inhibitors [91]. This approach aims to simultaneously block both major intracellular degradation pathways, creating an insurmountable proteotoxic stress that preferentially kills malignant cells. However, the challenge remains in achieving sufficient therapeutic windows with such combinations, as normal cells also depend on these pathways for protein homeostasis.
The growing understanding of the interplay between the UPS and apoptotic regulation, particularly through Bcl-2 family proteins, has further informed combination strategies [94]. As proteasome inhibition affects the stability of both pro- and anti-apoptotic Bcl-2 family members, synergistic interactions with BH3 mimetics and other apoptosis-targeting agents represent another promising direction for therapeutic development [94].
The development of next-generation proteasome inhibitors represents a dynamic frontier in targeted cancer therapy and beyond. Advances in irreversible inhibition mechanisms and oral formulations address significant limitations of first-generation agents, potentially expanding the therapeutic utility of proteasome-targeted therapies. The ongoing elucidation of how proteasome inhibition impacts cellular ubiquitin dynamics and protein homeostasis provides critical insights for designing more effective treatment strategies and overcoming resistance. As our understanding of the complex interplay between proteasome inhibition and cellular stress responses deepens, and as functional genomic approaches continue to identify novel modifiers of sensitivity, the rational development of next-generation inhibitors and their strategic deployment in combination regimens will likely further improve outcomes for patients with proteasome inhibitor-sensitive malignancies.
The ubiquitin-proteasome system (UPS) is a master regulator of cellular protein homeostasis, governing the controlled degradation of proteins to modulate virtually every biological process, from cell cycle progression to stress responses [95] [93]. At the heart of this system are E3 ubiquitin ligases, which confer specificity by recognizing target substrate proteins and facilitating their ubiquitination. The human genome encodes an estimated 600-700 E3 ligases, representing a vast but underexplored therapeutic landscape [96] [97] [98]. The critical context for this field is the profound impact that proteasome inhibition exerts on cellular ubiquitin dynamics; impairing the proteasome's degradative capacity does not halt ubiquitination, leading to a rapid accumulation of poly-ubiquitinated proteins and disrupting the delicate balance of the entire UPS [35] [99]. This whitepaper provides an in-depth examination of emerging strategies to therapeutically target E3 ligases and ubiquitin itself, framed within the essential research on proteasome inhibition's cellular consequences. It is designed to equip researchers and drug development professionals with the latest mechanistic insights, experimental data, and methodological protocols driving this rapidly advancing field.
The Ubiquitin-Proteasome System and the Consequences of Proteasome Inhibition
Core Mechanism of the UPS
The ubiquitin-proteasome system operates through a sequential enzymatic cascade:
- Activation: A ubiquitin-activating enzyme (E1) activates ubiquitin in an ATP-dependent reaction.
- Conjugation: The ubiquitin is transferred to a ubiquitin-conjugating enzyme (E2).
- Ligation: An E3 ubiquitin ligase recruits the E2~Ub complex and a specific substrate protein, facilitating the transfer of ubiquitin to a lysine residue on the substrate.
- Degradation: Poly-ubiquitinated proteins (typically with K48-linked chains) are recognized and degraded by the 26S proteasome [100] [101] [95].
E3 ligases are categorized into three major families based on their structure and mechanism: the RING finger family, the HECT family, and the RBR family [100] [95]. The RING family, the largest group, directly transfers ubiquitin from E2 to the substrate. The HECT and RBR families, however, form a covalent thioester intermediate with ubiquitin before transferring it to the substrate [95].
Impact of Proteasome Inhibition on the Ubiquitin Landscape
Proteasome inhibitors, such as MG132 and clinical agents like bortezomib and carfilzomib, are established cancer therapeutics. Their primary effect is the rapid intracellular accumulation of poly-ubiquitinated proteins, as degradation is blocked while ubiquitination continues [16] [99]. Recent research reveals that the consequences extend far beyond simple protein stabilization.
A 2025 study using mass spectrometry to analyze the aging mouse brain—a model of naturally declining proteasome function—found that aging has a "major impact" on protein ubiquitylation, with 29% of quantified ubiquitylation sites being altered independently of changes in the core protein's abundance. This indicates a fundamental shift in ubiquitin stoichiometry and pathway regulation [35]. Furthermore, proteasome inhibition can trigger compensatory transcriptional responses. In breast cancer and multiple myeloma cell lines, proteasome inhibitor treatment unexpectedly caused an ~100-fold increase in APOBEC3A (A3A) mRNA, a known DNA mutator enzyme, thereby increasing its protein levels and associated genomic DNA damage [99]. This demonstrates that proteasome dysfunction can actively rewire cellular signaling and transcriptional networks, with significant implications for both disease progression and therapeutic outcomes.
Figure 1: Proteasome inhibition disrupts cellular ubiquitin levels and signaling. Pharmacological inhibition or age-related decline of proteasome function causes a buildup of ubiquitinated proteins, triggering downstream transcriptional changes and dysregulated signaling that impact cellular health and disease states [35] [99].
Emerging Therapeutic Strategies Targeting E3 Ligases
Proteolysis-Targeting Chimeras (PROTACs)
PROTACs represent a paradigm shift from traditional occupancy-based pharmacology to event-driven catalysis. These heterobifunctional molecules consist of three elements:
- A ligand that binds the Protein of Interest (POI).
- A ligand that recruits a specific E3 ubiquitin ligase.
- A chemical linker tethering the two ligands [97].
By bringing the E3 ligase into proximity with the POI, the PROTAC induces poly-ubiquitination of the POI, leading to its degradation by the proteasome. The catalytic nature of PROTACs allows for sub-stoichiometric activity, potentially leading to more profound and durable effects than traditional inhibitors [96] [97].
Table 1: Canonical and Emerging E3 Ligases for PROTAC Development
| E3 Ligase | Family | Key Ligand(s) | Therapeutic Rationale & Status |
|---|---|---|---|
| CRBN | RING | Thalidomide analogs (Lenalidomide, Pomalidomide) | Most widely used; basis for clinical candidates like ARV-471 [97] [101]. |
| VHL | RING (CRL) | HIF-1α mimetics (e.g., VH032) | Well-validated; used in numerous preclinical & clinical PROTACs [97] [98]. |
| MDM2 | RING | Nutlins, Idasanutlin | Exploited in cancers to reactivate p53; used in PROTACs [97] [101]. |
| RNF114 | RING | Nimbolide, covalent acrylamides | Emerging target; nimbolide-based PROTACs degrade BRD4 [97]. |
| RNF4 | RING | Covalent ligand CCW 16 | Proof-of-concept; PROTACs developed via chemoproteomic screening [97]. |
| CBL-c | RING | Fragment-based ligands (discovered 2025) | Tumor-selective expression may enable wider therapeutic window [98]. |
The field's heavy reliance on CRBN and VHL represents a bottleneck, driving efforts to recruit novel E3 ligases. A key 2025 study used protein-observed NMR fragment screening to identify starting ligands for CBL-c and TRAF-4, two E3 ligases with preferential expression in cancer tissues. This strategy aims to create tumor-selective degraders that minimize on-target, off-tissue toxicity [98].
Molecular Glues
Molecular glues are monovalent small molecules that induce or stabilize the interaction between an E3 ligase and a target protein, leading to the target's ubiquitination and degradation. The immunomodulatory drugs (IMiDs) like lenalidomide are classic examples; they "glue" the CRL4CRBN E3 ligase to novel neosubstrates such as the transcription factors IKZF1 and IKZF3, which are then ubiquitinated and degraded. This mechanism is central to the treatment of multiple myeloma [101].
Direct E3 Ligase Inhibition
Beyond degradation, directly inhibiting the activity of specific E3 ligases remains a valid therapeutic strategy, particularly in oncology. For instance, the E3 ligase MDM2 is a key negative regulator of the tumor suppressor p53. Inhibiting MDM2 leads to p53 stabilization and activation of apoptosis in cancer cells [101]. Similarly, targeting the E3 ligase HUWE1, which regulates oncoproteins like c-Myc and MCL-1, is an active area of investigation for multiple myeloma and other cancers [101].
Quantitative Data on E3 Ligase Targeting
Table 2: Quantitative Assessment of E3 Ligase Targeting in Disease Models
| Disease Context | Key E3 Ligase | Experimental Intervention | Quantitative Outcome | Citation |
|---|---|---|---|---|
| Pendred Syndrome | (Implicated UPS) | Proteasome Inhibitors (Carfilzomib) | Rescued ion transport function of pathogenic pendrin variants to wild-type levels. | [16] |
| Multiple Myeloma | CRBN | Molecular Glues (Lenalidomide) | Alters substrate specificity, leading to degradation of IKZF1/3, suppressing MM cell growth. | [101] |
| Triple-Negative Breast Cancer | RNF114 | PROTAC XH2 (Nimbolide-JQ1 conjugate) | Induced RNF114-dependent, proteasome-mediated degradation of BRD4 with nanomolar potency. | [97] |
| Multiple Cancer Types | CBL-c, TRAF-4 | Fragment-Based Ligand Discovery | Identified E3s with high tumor-to-normal mRNA expression ratios (CBL-c: >4-fold in some cancers). | [98] |
| Aging Brain | (Global UPS) | Natural Proteasome Decline (Mouse Model) | 29% of quantified ubiquitylation sites were altered independently of protein abundance changes. | [35] |
Detailed Experimental Protocols
Protocol 1: Protein-Observed NMR Fragment Screening for E3 Ligand Discovery
This protocol is used to identify small molecule fragments that bind to E3 ligases, providing starting points for developing PROTAC recruiters [98].
- Protein Expression and Purification: Clone the DNA encoding the target E3 ligase (or its specific binding domain) into a suitable expression vector (e.g., pET series). Express the protein in E. coli and purify it using affinity chromatography (e.g., Ni-NTA for His-tagged proteins), followed by size-exclusion chromatography to ensure homogeneity and remove aggregates.
- Sample Preparation: Prepare an NMR sample containing ~100-200 µM of the purified protein in a phosphate or Tris-based buffer (e.g., 20 mM sodium phosphate, 50 mM NaCl, pH 7.0) using D₂O or a H₂O/D₂O mixture. Add 1-10 mM of a reference standard like DSS for chemical shift calibration.
- NMR Data Acquisition (Ligand-Free): Collect 2D ( ^1H )-( ^{15}N ) HSQC or ( ^1H )-( ^{13}C ) HMQC spectra of the protein alone at 25°C. This serves as the reference spectrum.
- Fragment Library Addition: Introduce individual fragments from a curated library (typically 500-1500 Da in size) to the protein sample. A final fragment concentration of 0.5-2 mM is standard, ensuring a molar excess of ligand over protein.
- NMR Data Acquisition (Ligand-Bound): Collect 2D ( ^1H )-( ^{15}N ) HSQC or ( ^1H )-( ^{13}C ) HMQC spectra for each protein-fragment mixture using identical parameters to the reference experiment.
- Hit Identification: Analyze the spectra for chemical shift perturbations (CSPs). A CSP is defined as ( \Delta \delta = \sqrt{(\Delta \deltaH)^2 + (0.1 \cdot \Delta \deltaN)^2} ) for HN experiments. Fragments causing significant CSPs (e.g., > mean + 3 standard deviations of all perturbations) are considered primary hits.
- Validation and Characterization: Validate hits using orthogonal techniques such as:
- Surface Plasmon Resonance (SPR): To determine binding affinity (K_D).
- X-ray Crystallography: To solve the co-crystal structure of the protein-fragment complex and elucidate the binding mode for future optimization.
Figure 2: Workflow for discovering E3 ligase ligands via NMR fragment screening. This process identifies small molecule binders that can serve as starting points for developing PROTACs [98].
Protocol 2: Functional Validation of a PROTAC in Cell-Based Assays
This protocol assesses the efficacy and mechanism of action of a novel PROTAC molecule.
- Cell Culture and Seeding: Culture appropriate cell lines (e.g., cancer lines relevant to the target protein) in recommended media. Seed cells in 6-well or 12-well plates at a density that will ensure ~60-80% confluence at the time of treatment.
- PROTAC Treatment: Prepare a dilution series of the PROTAC (e.g., from 1 nM to 10 µM) in DMSO or culture media. Treat cells for a predetermined period (typically 4-24 hours). Include controls: vehicle (DMSO), a linker-only control, and each warhead (E3 ligand and POI ligand) alone.
- Protein Extraction and Quantification: Lyse cells in RIPA buffer supplemented with protease and phosphatase inhibitors. Quantify total protein concentration using a BCA or Bradford assay.
- Western Blot Analysis:
- Separate equal amounts of protein (20-40 µg) by SDS-PAGE.
- Transfer to a PVDF membrane.
- Block membrane with 5% non-fat milk in TBST.
- Incubate with primary antibodies against: the Protein of Interest (POI), the E3 ligase (to control for loading), and a housekeeping protein (e.g., GAPDH, β-Actin).
- Incubate with HRP-conjugated secondary antibodies.
- Develop using enhanced chemiluminescence (ECL) and image.
- Mechanism of Action Validation:
- Proteasome Dependence: Co-treat cells with the PROTAC and a proteasome inhibitor (e.g., 10 µM MG132 or 100 nM Bortezomib). Degradation should be rescued.
- E3 Ligase Dependence: Co-treat cells with the PROTAC and an excess of the free E3 ligase ligand (e.g., 10 µM) to compete for binding. Degradation should be inhibited.
- Ubiquitination Assay: Perform immunoprecipitation of the POI from PROTAC-treated cells, followed by western blotting with an anti-ubiquitin antibody to detect increased poly-ubiquitination.
- Cellular Phenotype Assays: Depending on the target, perform downstream assays such as cell viability (MTT, CellTiter-Glo), apoptosis (Annexin V staining), or cell cycle analysis (PI staining) to confirm functional consequences of target degradation.
The Scientist's Toolkit: Key Research Reagents
Table 3: Essential Reagents for Research on E3 Ligases and Ubiquitin
| Reagent / Tool | Function / Mechanism | Example Application |
|---|---|---|
| Proteasome Inhibitors (MG132, Bortezomib, Carfilzomib) | Reversibly or irreversibly block the proteasome's chymotrypsin-like activity. | Validating UPS-dependent processes; rescuing protein degradation in negative controls [16] [99]. |
| E3 Ligase Ligands (e.g., VH032 for VHL, Lenalidomide for CRBN) | Bind specifically to an E3 ligase's recognition domain. | Core components for constructing PROTAC molecules; competition assays [97]. |
| Ubiquitin-Activating Enzyme (E1) Inhibitor (e.g., TAK-243/MLN7243) | Inhibits the initial step of the ubiquitin cascade, globally blocking ubiquitination. | Confirming that a process is dependent on ubiquitination [96]. |
| Activity-Based Probes (ABPP) | Covalently label active-site residues of enzymes, including some E3 ligases. | Profiling E3 ligase activity and identifying new ligandable E3s via chemoproteomics [97]. |
| K-ε-GG Ubiquitin Remnant Motif Antibody | Recognizes the di-glycine remnant left on tryptic peptides after ubiquitination. | Enriching and identifying ubiquitinated peptides for mass spectrometry-based ubiquitinome studies [35]. |
The strategic targeting of E3 ligases and the ubiquitin machinery is poised to redefine therapeutic intervention in cancer, neurodegenerative disorders, and beyond. The field is rapidly evolving from a reliance on a handful of established E3 ligases to a broad exploration of the E3 ligome, fueled by advanced screening techniques and a deeper understanding of UPS biology. The critical insight that proteasome inhibition fundamentally alters the cellular ubiquitin landscape—driving not just protein accumulation but also transcriptional and signaling rewiring—demands that new therapeutic strategies be designed and evaluated within this complex physiological context. The tools and data summarized in this whitepaper provide a foundation for researchers to contribute to this dynamic and promising frontier, with the ultimate goal of delivering precise, effective, and novel medicines to patients.
Conclusion
Proteasome inhibition precipitates a profound and measurable increase in cellular ubiquitin levels, a phenomenon that sits at the intersection of fundamental cell biology and transformative cancer therapy. The foundational understanding of the UPS, combined with sophisticated methodological tools for monitoring its activity, has enabled the successful development of proteasome inhibitors. While these drugs have validated the UPS as a critical therapeutic target, challenges such as drug resistance and adverse events underscore the need for continued optimization. The robust market growth and ongoing clinical trials for next-generation inhibitors and novel modalities, including small molecules that are themselves ubiquitinated, highlight the dynamic nature of this field. Future research directions will likely focus on achieving greater specificity by targeting upstream components like E3 ligases, developing personalized treatment regimens based on individual UPS capacity, and expanding the utility of proteasome inhibition beyond hematologic malignancies into solid tumors. A deep understanding of the intricate relationship between proteasome function and ubiquitin homeostasis remains paramount for driving the next wave of innovation in targeted protein degradation.
References
- 1. The Ubiquitin-Proteasome System as a Prospective Molecular ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3306609/]
- 2. E3 ubiquitin ligases: styles, structures and functions - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC8607428/]
- 3. Ubiquitin [https://en.wikipedia.org/wiki/Ubiquitin]
- 4. Site-specific ubiquitination: Deconstructing the degradation ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9208700/]
- 5. Protein Degradation using the Ubiquitin-Proteasome ... [https://www.thermofisher.com/us/en/home/life-science/cell-analysis/cell-analysis-learning-center/protein-degradation-resource-center/protein-degradation-using-ubiquitin-proteasome-pathway.html]
- 6. A Ubiquitin Stress Response Induces Altered Proteasome ... [https://www.sciencedirect.com/science/article/pii/S009286740700459X]
- 7. Protein ubiquitination involving an E1–E2–E3 enzyme ... [https://www.nature.com/articles/373081a0]
- 8. A Human Ubiquitin Conjugating Enzyme (E2)-HECT E3 ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3412965/]
- 9. Structure and Function of the 26S Proteasome - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC6422034/]
- 10. The life cycle of the 26S proteasome: from birth, through ... [https://www.nature.com/articles/cr201686]
- 11. Review The Logic of the 26S Proteasome [https://www.sciencedirect.com/science/article/pii/S0092867417304749]
- 12. The Ubiquitin–26S Proteasome Pathway and Its Role in the ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9917055/]
- 13. Structural landscape of the degrading 26S proteasome ... [https://www.nature.com/articles/s41594-025-01695-2]
- 14. Autoregulation of the 26S proteasome by in situ ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4055262/]
- 15. Ubiquitin-proteasome system: a potential participant and ... [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2025.1523799/full]
- 16. Inhibitors of the ubiquitin‑proteasome system rescue ... [https://pubmed.ncbi.nlm.nih.gov/40052591/]
- 17. Highly specific intracellular ubiquitination of a small molecule [https://www.nature.com/articles/s41589-025-02011-1]
- 18. The Ubiquitin-Proteasome Pathway and Proteasome Inhibitors [https://pmc.ncbi.nlm.nih.gov/articles/PMC2556558/]
- 19. Frontiers | Proteasome dynamics in response to metabolic changes [https://www.frontiersin.org/journals/cell-and-developmental-biology/articles/10.3389/fcell.2025.1523382/full]
- 20. Proteasome Inhibitors: Structure and Function - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC6020165/]
- 21. Dynamics of the Degradation of Ubiquitinated Proteins by ... [https://www.sciencedirect.com/science/article/pii/S0021925819489539]
- 22. Inhibition of the ubiquitin-proteasome system by an NQO1- ... [https://www.nature.com/articles/s41419-021-04191-9]
- 23. of the Inhibitors ‑ ubiquitin system rescue proteasome ... cellular levels [https://www.spandidos-publications.com/10.3892/ijmm.2025.5510?text=fulltext]
- 24. Elevated ubiquitin phosphorylation by PINK1 contributes to... [https://elifesciences.org/articles/103945]
- 25. Activators of the 26S proteasome when protein degradation increases [https://www.nature.com/articles/s12276-024-01385-x?error=cookies_not_supported&code=ce45823a-562f-4447-9516-8db1e10308b2]
- 26. Cellular Responses to Proteasome Inhibition - PubMed Central [https://pmc.ncbi.nlm.nih.gov/articles/PMC6678303/]
- 27. Delineating Crosstalk Mechanisms of the Ubiquitin ... [https://www.frontiersin.org/journals/cell-and-developmental-biology/articles/10.3389/fcell.2018.00011/full]
- 28. PPM1D is directly degraded by proteasomes in a ... [https://jbiomedsci.biomedcentral.com/articles/10.1186/s12929-025-01185-z]
- 29. Ubiquitin-proteasome pathway-mediated regulation of the ... [https://haematologica.org/article/view/haematol.2023.283730]
- 30. Molecular mechanisms and potential targeting strategies of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12511930/]
- 31. Emerging functions of branched ubiquitin chains [https://www.nature.com/articles/s41421-020-00237-y]
- 32. Atypical ubiquitin chains: new molecular signals. 'Protein ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC2427391/]
- 33. UbiREAD deciphers proteasomal degradation code of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7617769/]
- 34. Structural mechanisms of autoinhibition and substrate ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10873202/]
- 35. Aging and diet alter the protein ubiquitylation landscape in ... [https://www.nature.com/articles/s41467-025-60542-6]
- 36. Impact of proteostasis workload on sensitivity to proteasome ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12106538/]
- 37. Monitoring of ubiquitin-proteasome activity in living cells ... [https://pubmed.ncbi.nlm.nih.gov/23169445/]
- 38. Reporter-Based Screens for the Ubiquitin/Proteasome ... [https://www.frontiersin.org/journals/chemistry/articles/10.3389/fchem.2020.00064/full]
- 39. Application and analysis of the GFPu family of ubiquitin ... [https://pubmed.ncbi.nlm.nih.gov/16338377/]
- 40. Functional studies of the ubiquitin-proteasome system using ... [https://openarchive.ki.se/articles/thesis/Functional_studies_of_the_ubiquitin-proteasome_system_using_GFP-based_reporters/26923906]
- 41. Imaging Reporters for Proteasome Activity Identify Tumor [https://pmc.ncbi.nlm.nih.gov/articles/PMC4663702/]
- 42. Probing protein ubiquitination in live cells - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC9757074/]
- 43. Quantitative live-cell imaging reveals spatio-temporal ... [https://www.nature.com/articles/ncomms4396]
- 44. Weighing in on Ubiquitin: The Expanding Role of Mass ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC1224607/]
- 45. Current methodologies in protein ubiquitination characterization [https://cellandbioscience.biomedcentral.com/articles/10.1186/s13578-022-00870-y]
- 46. A High-Throughput Method for Specific, Rapid, Precise and ... [https://www.sciencedirect.com/science/article/abs/pii/S0039914025015681]
- 47. Large-scale identification of ubiquitination sites by mass ... [https://pubmed.ncbi.nlm.nih.gov/24051958/]
- 48. Unraveling chain specific ubiquitination in cells using tandem ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12217038/]
- 49. A Guide to Modern Quantitative Fluorescent Western ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4354265/]
- 50. 2024 Guide to Quantitative Western Blot Publication [https://www.thermofisher.com/blog/life-in-the-lab/2023-guide-to-quantitative-western-blot-publication/]
- 51. 2024 Scientific Publication Requirements for Western Blots ... [https://azurebiosystems.com/blog/publication-requirements-for-western-blots-and-gels/]
- 52. Optimizing reduction of western blotting analytical variations [https://www.sciencedirect.com/science/article/pii/S000326972300163X]
- 53. Targeting the Ubiquitin–Proteasome System for Cancer - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC12495026/]
- 54. Mechanistic insights into proteasome inhibitor MG132 ... [https://www.nature.com/articles/s41598-025-99151-0]
- 55. Proteostasis Disruption by Proteasome Inhibitor MG132 and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12256276/]
- 56. Systematic and quantitative assessment of the ubiquitin ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3200427/]
- 57. Increased cellular uptake and proteasome inhibition of ... [https://pubmed.ncbi.nlm.nih.gov/40680669/]
- 58. Current methodologies in protein ubiquitination ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9373315/]
- 59. Targeting the ubiquitin system by fragment-based drug ... [https://www.frontiersin.org/journals/molecular-biosciences/articles/10.3389/fmolb.2022.1019636/full]
- 60. A CRISPR activation screen identifies FBXO22 supporting ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11581908/]
- 61. Quantitative Profiling of Ubiquitylated Proteins Reveals ... [https://www.sciencedirect.com/science/article/pii/S1535947620319228]
- 62. Targeting the ubiquitin-proteasome system for cancer ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5722705/]
- 63. Ubiquitin proteasome pathway: implications and advances ... [https://www.sciencedirect.com/science/article/abs/pii/S0960740401000184]
- 64. The ubiquitin-proteasome system in the tumor immune ... [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2024.1436174/full]
- 65. Safety assessment of proteasome inhibitors real world ... [https://www.nature.com/articles/s41598-025-96427-3]
- 66. Optimizing the Therapeutic Window of Targeted Drugs in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7993318/]
- 67. The ubiquitin proteasome system as a potential therapeutic ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10231402/]
- 68. Research progress in proteasome inhibitor resistance to ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10929973/]
- 69. Therapeutic strategies within the ubiquitin proteasome ... [https://www.nature.com/articles/cdd200982]
- 70. Evaluating a therapeutic window for precision medicine by ... [https://www.nature.com/articles/s42003-022-03872-1]
- 71. Proteasome inhibition overcomes resistance to targeted ... [https://www.nature.com/articles/s41419-025-07884-7]
- 72. Quantifying Ubiquitin Signaling - PMC - PubMed Central [https://pmc.ncbi.nlm.nih.gov/articles/PMC4441763/]
- 73. The Evolution and Diversification of Proteasome Inhibitors ... [https://chemrxiv.org/engage/chemrxiv/article-details/6853081ac1cb1ecda0b1e33f]
- 74. Next-generation proteasome inhibitors for cancer therapy - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC6151281/]
- 75. in Proteasome - PMC inhibitors mantle cell lymphoma [https://pmc.ncbi.nlm.nih.gov/articles/PMC3374152/]
- 76. Efficacy of maintenance or consolidation therapy for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11993517/]
- 77. Mechanistic Rationale and Clinical Evidence for the Efficacy of... [https://link.springer.com/article/10.2165/00063030-200620010-00002]
- 78. The role of the proteasome in AML | Blood Cancer Journal [https://www.nature.com/articles/bcj2016112?error=cookies_not_supported&code=ca5a407b-3ddf-4dd1-9530-1765d8c01fcf]
- 79. Carfilzomib: A Promising Proteasome Inhibitor for the ... [https://www.frontiersin.org/journals/oncology/articles/10.3389/fonc.2021.740796/full]
- 80. Proteasome inhibitor-adapted myeloma cells are largely ... [https://www.nature.com/articles/leu2016102]
- 81. Bortezomib in cancer therapy: Mechanisms, side effects ... [https://www.sciencedirect.com/science/article/pii/S002432052400715X]
- 82. Safety assessment of proteasome inhibitors real world ... [https://pubmed.ncbi.nlm.nih.gov/40185858/]
- 83. Infection-related adverse events comparison of bortezomib, ... [https://pubmed.ncbi.nlm.nih.gov/40243068/]
- 84. Preclinical comparison of proteasome and ubiquitin E1 ... [https://www.oncotarget.com/article/24750/text/]
- 85. Proteasome Inhibitors Market Size & Share Report, 2025 [https://www.gminsights.com/industry-analysis/proteasome-inhibitors-market]
- 86. Proteasome Inhibitors Market Size 2025-2029 [https://www.technavio.com/report/proteasome-inhibitors-market-industry-size-analysis]
- 87. The Impending Age Wave [https://www.nicmap.com/blog/the-impending-age-wave-navigating-the-urgent-need-for-senior-housing/]
- 88. The gray wave: How an aging population is reshaping ... [https://www.mizuhogroup.com/americas/insights/2025/05/the-gray-wave-how-an-aging-population-is-reshaping-the-economy.html]
- 89. North America Proteasome Inhibitors Market Key ... [https://www.linkedin.com/pulse/north-america-proteasome-inhibitors-market-key-determinants-on3lf/]
- 90. Development of Proteasome Inhibitors as Therapeutic Drugs - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC3546515/]
- 91. Paradoxical resistance of multiple myeloma to proteasome ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4602331/]
- 92. Proteasome inhibitors: The next generation of antimalarial drugs? - PubMed [https://pubmed.ncbi.nlm.nih.gov/37207628/]
- 93. Modulation of the Ubiquitin-Proteasome System by ... [https://www.sciencedirect.com/science/article/pii/S095528632500289X]
- 94. A new era in cancer therapy: targeting the Proteasome-Bcl-2 ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12369272/]
- 95. Targeting E3 ubiquitin ligases and their adaptors as a ... [https://www.nature.com/articles/s12276-023-01087-w]
- 96. E3 ubiquitin ligases in signaling, disease, and therapeutics [https://www.sciencedirect.com/science/article/pii/S0968000425001860]
- 97. The Expanding E3 Ligase-Ligand Landscape for PROTAC ... [https://www.mdpi.com/2813-3137/3/4/30]
- 98. Identification of ligands for E3 ligases with restricted ... [https://pubs.rsc.org/en/content/articlehtml/2025/cb/d5cb00198f]
- 99. An impaired ubiquitin-proteasome system increases ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10753533/]
- 100. Targeting E3 ubiquitin ligases: a new frontier in idiopathic ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12399401/]
- 101. Regulatory role of E3 ubiquitin ligases in multiple myeloma [https://pmc.ncbi.nlm.nih.gov/articles/PMC12343653/]