Ubiquitin Signaling in the Tumor Microenvironment: Mechanisms, Therapeutic Targeting, and Clinical Frontiers
This article provides a comprehensive analysis of the ubiquitin signaling network's critical role in shaping the tumor microenvironment (TME).
Ubiquitin Signaling in the Tumor Microenvironment: Mechanisms, Therapeutic Targeting, and Clinical Frontiers
Abstract
This article provides a comprehensive analysis of the ubiquitin signaling network's critical role in shaping the tumor microenvironment (TME). It explores foundational mechanisms by which E3 ligases and deubiquitinases regulate cellular and non-cellular TME components, including immune cells, cancer-associated fibroblasts, and the extracellular matrix. The content covers methodological advances in targeting the ubiquitin-proteasome system, troubleshooting for therapeutic resistance, and comparative validation of emerging strategies like PROTACs and molecular glues. Synthesizing recent research and clinical insights, this review serves as a strategic resource for researchers and drug development professionals aiming to exploit ubiquitination for novel cancer therapeutics.
Decoding the Ubiquitin Code: Core Mechanisms and Key Regulators in the TME
The Ubiquitin-Proteasome System (UPS) represents a highly complex, temporally controlled, and conserved pathway that maintains cellular protein homeostasis through the targeted degradation of short-lived, misfolded, or damaged proteins [1] [2]. This selective proteolysis mechanism regulates a myriad of critical cellular processes, including immune response, apoptosis, cell cycle progression, and differentiation [1]. The UPS operates through a hierarchical enzymatic cascade that conjugates the small, 76-amino acid protein ubiquitin to substrate proteins, marking them for destruction by the 26S proteasome [3] [4].
Within the context of tumor biology, the UPS has emerged as a critical regulator of the tumor microenvironment (TME), influencing immune cell function, cancer cell survival, and response to therapy [5]. Dysregulation of UPS components contributes significantly to oncogenesis and tumor immune evasion by altering the stability of key regulatory proteins [6] [7]. The intricate role of ubiquitination signaling in the TME underscores the therapeutic potential of targeting specific UPS elements to overcome resistance to cancer treatments, particularly immunotherapy [8] [5].
The Core Enzymatic Machinery of the UPS
The Ubiquitination Cascade: E1, E2, and E3 Enzymes
Protein ubiquitination involves a sequential three-step enzymatic cascade that requires ATP and culminates in the covalent attachment of ubiquitin to substrate proteins [2] [4]. This process is mediated by the coordinated actions of ubiquitin-activating (E1), ubiquitin-conjugating (E2), and ubiquitin-ligase (E3) enzymes [1] [3].
E1: Ubiquitin-Activating Enzymes - The initiating step involves E1 enzymes, which activate ubiquitin in an ATP-dependent manner. The E1 forms a high-energy thioester bond between its active-site cysteine residue and the C-terminal glycine of ubiquitin [2] [4]. This "charged" ubiquitin is then transferred to the next enzyme in the cascade. E1 function is crucial for cellular homeostasis, as chemical inhibition of E1 activity results in the almost immediate shutdown of the entire UPS [3].
E2: Ubiquitin-Conjugating Enzymes - The intermediate step involves E2 enzymes, which receive the activated ubiquitin from E1 via a trans-thioesterification reaction, forming an E2-ubiquitin conjugate intermediate [2] [3]. E2s function as the central ubiquitin carriers of the system, working in conjunction with E3 ligases to ultimately transfer ubiquitin to the target protein [3].
E3: Ubiquitin Ligases - The final and most diverse step involves E3 ubiquitin ligases, which provide substrate specificity by recognizing and binding target proteins while simultaneously interacting with the E2-ubiquitin complex [1] [4]. E3s facilitate the direct transfer of ubiquitin from the E2 to a lysine residue on the substrate protein [2]. Humans possess hundreds of E3 ligases, enabling the recognition of a vast array of specific substrates [7].
Table 1: Core Enzymes of the Ubiquitin-Proteasome System
| Enzyme Class | Number in Humans | Primary Function | Key Features |
|---|---|---|---|
| E1 (Activating) | Limited number (e.g., UBE1) | Ubiquitin activation via ATP hydrolysis | Forms E1-Ub thioester; essential for all downstream UPS function [2] [3] |
| E2 (Conjugating) | ~40 members (e.g., UBE2D2) | Ubiquitin carrier protein | Forms E2-Ub thioester; determines ubiquitin chain topology with E3 [2] [3] |
| E3 (Ligase) | ~600 members (e.g., MurRF1) | Substrate recognition and ubiquitin transfer | Determines substrate specificity; largest class with diverse domains [1] [7] |
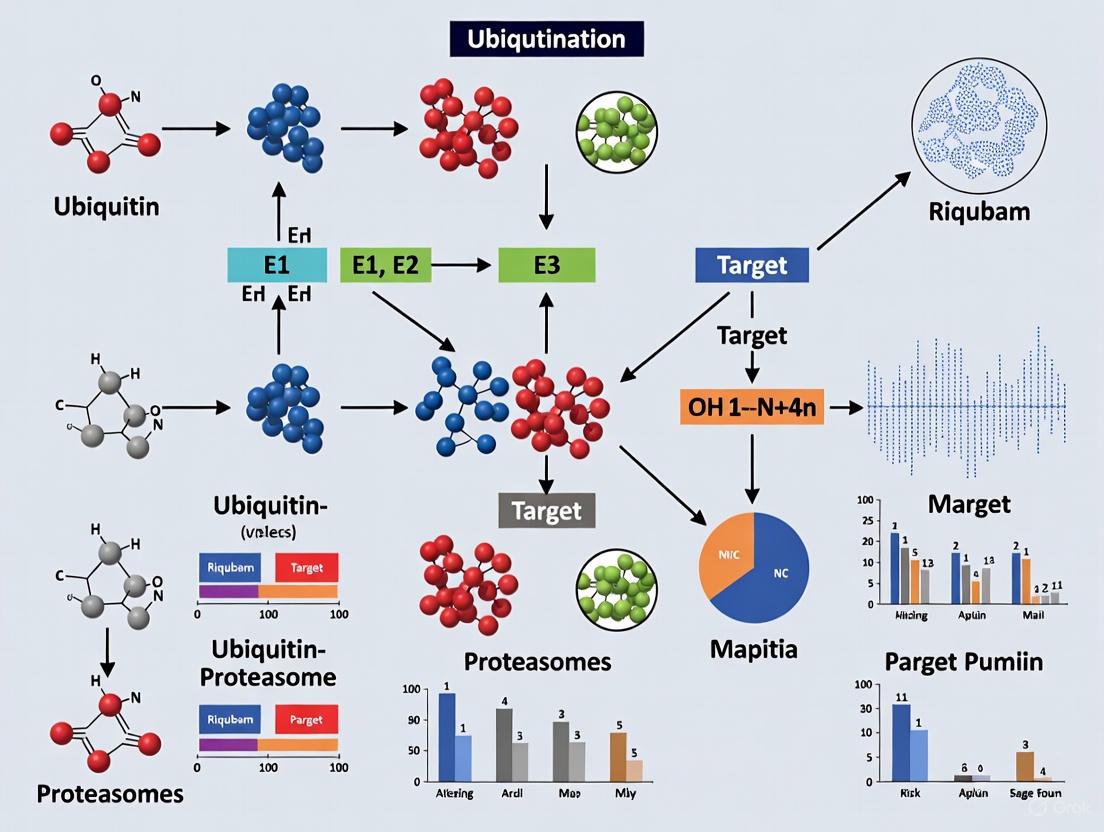
The following diagram illustrates the sequential flow of the ubiquitin conjugation cascade:
E3 Ubiquitin Ligases: Masters of Specificity
E3 ubiquitin ligases constitute the most diverse and specialized component of the UPS, functioning as critical decision-makers in determining which proteins are targeted for degradation [1]. They can be broadly categorized into three major families based on their structural characteristics and mechanisms of action:
RING (Really Interesting New Gene) E3s: Function primarily as scaffolds that simultaneously bind the E2-ubiquitin complex and the substrate, facilitating the direct transfer of ubiquitin from the E2 to the substrate without forming a covalent intermediate [4]. A prominent subclass is the Cullin-RING Ligases (CRLs), multi-subunit complexes that represent the largest family of E3s [7].
HECT (Homologous to the E6AP C-terminus) E3s: Form a catalytic intermediate by accepting ubiquitin from the E2 onto a conserved cysteine residue in their HECT domain before transferring it to the substrate [6].
RBR (RING-Between-RING-RING) E3s: Utilize a hybrid mechanism that combines features of both RING and HECT E3s [6].
A particularly well-characterized subset of CRLs is the SCF (SKP1-CUL1-F-box protein) complex, which exemplifies the modularity and specificity of the UPS. The SCF complex consists of a constant core (CUL1, RBX1, SKP1) and a variable substrate recognition module, the F-box protein [7]. The approximately 70 human F-box proteins are categorized into three subfamilies based on their protein-protein interaction domains: FBXW (WD repeat domain), FBXL (Leucine-rich repeat), and FBXO (other or uncharacterized domains) [7]. These F-box proteins typically recognize their substrates by binding to specific degrons—short, defined motifs within the substrate proteins—often requiring specific post-translational modifications such as phosphorylation for efficient recognition [7].
Deubiquitinating Enzymes (DUBs): The Editors of Ubiquitination
Deubiquitinating enzymes (DUBs) perform the reverse reaction of E3 ligases, countering ubiquitination by removing ubiquitin molecules from substrate proteins [1] [4]. This editing function serves several critical purposes: (1) maintaining cellular pools of free ubiquitin; (2) rescuing substrate proteins from degradation by reversing ubiquitin tagging; and (3) processing ubiquitin precursors to generate mature ubiquitin [5]. DUBs are categorized into five major subfamilies based on their catalytic mechanisms: USP (ubiquitin-specific proteases), UCH (ubiquitin C-terminal hydrolases), OTU (ovarian tumor proteases), MJD (Machado-Joseph disease proteases), and JAMM (JAB1/MPN/Mov34 metalloenzymes) [4]. Within the proteasome itself, three DUBs—PSMD14 (POH1/RPN11), UCH37 (UCH-L5), and USP14—work to recycle ubiquitin molecules before substrate degradation [4].
The Proteasome: Terminal Destination for Ubiquitinated Proteins
The 26S proteasome is the final executioner of the UPS pathway, responsible for the actual degradation of ubiquitinated proteins into short peptides [5]. This macromolecular protease complex consists of two primary components:
The 20S Core Particle (CP): A barrel-shaped structure containing proteolytically active sites (caspase-like, trypsin-like, and chymotrypsin-like activities) within its interior chamber, where protein digestion occurs [5].
The 19S Regulatory Particle (RP): Caps one or both ends of the 20S core and performs three key functions: (i) recognizing ubiquitinated substrates; (ii) cleaving off ubiquitin chains via its resident DUBs; and (iii) unfolding the target protein and translocating it into the 20S core for degradation [5] [4].
The proteasome's recognition of ubiquitinated substrates is a key regulatory step in the degradation process. The 19S RP contains ubiquitin receptors that specifically bind polyubiquitin chains, initiating the degradation sequence [3].
The Ubiquitin Code: A Language of Signals
The functional consequences of ubiquitination are determined by the type of ubiquitin chain assembled on the substrate protein—a concept often referred to as the "ubiquitin code" [2]. Ubiquitin contains seven lysine residues (K6, K11, K27, K29, K33, K48, K63) and an N-terminal methionine (M1), each serving as potential linkage sites for polyubiquitin chain formation [1] [7]. Different chain topologies encode distinct functional outcomes for the modified substrate:
- K48-linked chains: Primarily target substrates for proteasomal degradation and represent the most abundant degradation signal [1] [2].
- K11-linked chains: Also serve as potent signals for proteasomal degradation, particularly for substrates involved in endoplasmic reticulum-associated degradation (ERAD) and during cell cycle regulation [1].
- K63-linked chains: Typically mediate non-proteolytic functions, including regulation of signal transduction, DNA repair, endocytic trafficking, and inflammation [5] [4].
- M1-linked (linear) chains: Important for regulating NF-κB signaling and immune and inflammatory responses [4].
- K6, K27, K29, K33-linked chains: Less characterized but implicated in various processes including DNA damage response, autophagy, and kinase signaling [7].
Table 2: Major Ubiquitin Chain Linkages and Their Cellular Functions
| Linkage Type | Primary Function | Key Roles and Processes |
|---|---|---|
| K48 | Proteasomal Degradation | Primary signal for degradation; regulates most short-lived proteins, cell cycle regulators [1] [2] |
| K11 | Proteasomal Degradation | Targets misfolded ER proteins (ERAD); regulates cell cycle proteins [1] |
| K63 | Non-degradative Signaling | DNA repair, endocytosis, NF-κB and kinase activation, inflammatory signaling [5] [4] |
| M1 (Linear) | Non-degradative Signaling | NF-κB activation, immune regulation, inflammation [4] |
| K29/K33 | Diverse Functions | Atypical degradation signals; implicated in autophagy [1] |
The following diagram summarizes the ubiquitin code and the fates of ubiquitinated proteins:
Experimental Analysis of the UPS
Key Methodologies for UPS Research
Investigating the components and functions of the UPS requires a combination of molecular, biochemical, and cellular techniques. Below are detailed protocols for key experiments commonly used in the field.
Protocol 1: Immunoprecipitation (IP) and Ubiquitination Assay
- Purpose: To detect and characterize ubiquitination of a specific protein of interest.
- Procedure:
- Cell Lysis: Harvest and lyse cells in RIPA buffer supplemented with N-ethylmaleimide (NEM) to inhibit deubiquitinating enzymes (DUBs) and preserve ubiquitin conjugates.
- Immunoprecipitation: Incubate cell lysates with an antibody specific to your protein of interest. Use Protein A/G beads to pull down the antibody-protein complex.
- Washing: Wash beads extensively with lysis buffer to remove non-specifically bound proteins.
- Denaturation: Elute proteins from beads by boiling in SDS-PAGE sample buffer.
- Immunoblotting: Resolve proteins by SDS-PAGE, transfer to a membrane, and probe with an anti-ubiquitin antibody to detect ubiquitinated forms of the protein, which appear as higher molecular weight smears.
- Key Controls: Include a negative control using normal IgG or beads alone. For chain linkage specificity, use ubiquitin mutants (K48-only, K63-only) or linkage-specific antibodies.
Protocol 2: In Vitro Ubiquitination Assay
- Purpose: To reconstitute the ubiquitination cascade using purified components and define the minimal requirements for substrate ubiquitination.
- Procedure:
- Reaction Setup: In a tube, combine purified E1 enzyme, E2 enzyme, E3 ligase, ubiquitin, and the substrate protein in a reaction buffer containing ATP and an energy-regenerating system.
- Incubation: Incubate the reaction at 30°C for 1-2 hours.
- Termination and Analysis: Stop the reaction by adding SDS-PAGE sample buffer and boiling. Analyze the products by immunoblotting for the substrate to detect upward mobility shifts indicative of ubiquitination.
- Key Controls: Omit individual components (E1, E2, E3, or ATP) one at a time to confirm the requirement for each factor.
Protocol 3: Cycloheximide Chase Assay to Measure Protein Half-Life
- Purpose: To determine the in vivo half-life of a protein and assess the impact of UPS perturbation on its stability.
- Procedure:
- Inhibition of Translation: Treat cells with cycloheximide to block new protein synthesis.
- Time-Course Sampling: Harvest cells at various time points after cycloheximide addition (e.g., 0, 15, 30, 60, 120 minutes).
- Analysis: Prepare lysates from each time point and analyze the levels of the protein of interest by immunoblotting. Quantify band intensities and plot the natural logarithm of protein level versus time.
- Proteasome Inhibition: To confirm UPS involvement, parallel experiments can be performed using proteasome inhibitors like MG132 or bortezomib. Stabilization of the protein upon inhibitor treatment suggests UPS-mediated degradation.
The Scientist's Toolkit: Key Reagents for UPS Research
Table 3: Essential Research Reagents for UPS Investigation
| Reagent Category | Specific Examples | Function and Application |
|---|---|---|
| Proteasome Inhibitors | MG132, Bortezomib, Carfilzomib | Block proteolytic activity of the 20S proteasome; used to validate UPS-dependent degradation and accumulate ubiquitinated proteins [5]. |
| E1 Inhibitor | PYR-41, TAK-243 | Inhibit ubiquitin activation; used to shut down the entire UPS pathway for functional studies [3]. |
| DUB Inhibitors | PR-619 (broad-spectrum), P5091 (USP7 inhibitor) | Block deubiquitinating enzyme activity; used to study DUB function and increase global ubiquitination levels [5]. |
| Linkage-Specific Ub Antibodies | K48-linkage specific, K63-linkage specific | Identify specific ubiquitin chain topologies on substrates via immunoblotting or immunofluorescence [2]. |
| Ubiquitin Mutants | K48R, K63R, K48-only, K63-only | Define the role of specific lysine residues in ubiquitin chain formation in cellular and in vitro assays [5]. |
| PROTACs | ARV-471, ARV-110 | Bifunctional molecules that recruit E3 ligases to target non-enzyme proteins for degradation; used as chemical tools and therapeutic agents [1]. |
The UPS in the Tumor Microenvironment: Therapeutic Implications
The UPS plays a multifaceted role in shaping the tumor microenvironment (TME), influencing the behavior of both cancer cells and immune cells. A key mechanism of tumor immune evasion involves the UPS-mediated regulation of immune checkpoint proteins, particularly PD-1/PD-L1 [5]. The E3 ubiquitin ligase SPOP has been identified as a critical regulator that promotes the ubiquitination and proteasomal degradation of PD-L1 in various cancers, including colorectal cancer [5]. However, tumor cells can counteract this by upregulating proteins like ALDH2 or the transcription factor BCLAF1, which competitively bind to SPOP or PD-L1, thereby stabilizing PD-L1 and enhancing immune evasion [5]. This dynamic interplay presents a promising therapeutic avenue, as demonstrated by studies showing that the SGLT2 inhibitor canagliflozin can disrupt the SGLT2-PD-L1 interaction, restoring SPOP-mediated degradation of PD-L1 and enhancing T cell-mediated anti-tumor activity [5].
Beyond immune checkpoints, F-box proteins within the SCF E3 ligase complex are increasingly recognized as master regulators of cancer hallmarks within the TME. They control critical processes such as cancer cell proliferation, epithelial-to-mesenchymal transition (EMT), metabolic reprogramming, and the integrated stress response [7]. The adaptability and wide coverage of F-box proteins, governed by a sophisticated regulatory hierarchy, make them attractive potential targets for cancer therapy. Emerging therapeutic strategies are moving beyond broad proteasome inhibition (e.g., bortezomib) toward more precise targeting of specific E3 ligases or DUBs. The development of PROTACs (Proteolysis-Targeting Chimeras) and molecular glues represents a paradigm shift, enabling the re-purposing of E3 ligases to selectively degrade disease-driving proteins that have been historically difficult to target with conventional inhibitors [1]. These approaches hold significant potential for modulating the TME and overcoming resistance to current immunotherapies.
Ubiquitination is a critical post-translational modification that regulates virtually every cellular process in eukaryotes, with particular significance in cancer biology. This modification involves the covalent attachment of a small 76-amino acid protein, ubiquitin, to substrate proteins, thereby altering their fate, function, or localization [9] [10]. The remarkable functional diversity of ubiquitin signaling stems from the ability of ubiquitin molecules to form polymers (polyubiquitin chains) of different topologies—defined by the linkage type between ubiquitin monomers, chain length, and branching patterns—creating a sophisticated "ubiquitin code" that can be interpreted by cellular machinery [9] [11]. Within the context of the tumor microenvironment (TME), understanding this code is paramount, as ubiquitination regulates key processes including immune cell function, hypoxia response, angiogenesis, and cancer stemness [12] [13].
The seven lysine residues in ubiquitin (K6, K11, K27, K29, K33, K48, K63) plus its N-terminal methionine (M1) serve as potential linkage sites for chain formation [10]. Among these, K48-linked chains represent the most abundant linkage type and typically target substrates for proteasomal degradation, while K63-linked chains generally serve non-proteolytic functions in signaling pathways related to DNA repair, inflammation, and protein trafficking [9] [14]. Beyond these well-characterized homotypic chains, heterotypic chains including mixed linkage and branched chains dramatically expand the complexity of ubiquitin signaling, enabling sophisticated regulation of cellular processes [9] [11]. This review comprehensively examines ubiquitin chain topology from classical K48/K63 linkages to monoubiquitination, with special emphasis on their functional consequences in the context of tumor microenvironment regulation.
Ubiquitin Chain Topologies: Structures and Functions
Monoubiquitination and Multi-Monoubiquitination
Monoubiquitination, the attachment of a single ubiquitin molecule to a substrate lysine residue, represents the simplest form of ubiquitin modification. Despite its simplicity, monoubiquitination regulates crucial cellular processes including DNA damage repair, histone function, chromatin remodeling, and receptor endocytosis [10] [15]. In the DNA damage response, the E3 ligase Rad18 mediates monoubiquitination of proliferating cell nuclear antigen (PCNA), facilitating the recruitment of specialized DNA polymerases [10]. Similarly, TRAF6-driven monoubiquitination of H2AX serves as a prerequisite for recruiting ataxia telangiectasia mutated (ATM) to DNA damage sites [10]. Membrane protein monoubiquitination can modulate interactions with autophagy adapter proteins such as p62, thereby promoting organelle-specific autophagy including mitophagy and pexophagy [10].
Multi-monoubiquitination, wherein multiple single ubiquitin molecules attach to different lysine residues on the same substrate, further expands the regulatory potential of monoubiquitination. This modification type can create specialized interaction surfaces for proteins containing multiple ubiquitin-binding domains, allowing for fine-tuned regulation of processes such as endocytosis and protein sorting [11].
Homotypic Polyubiquitin Chains
Table 1: Major Homotypic Polyubiquitin Chain Linkages and Their Functions
| Linkage Type | Primary Functions | Cellular Processes | Key Effectors/Readers |
|---|---|---|---|
| K48-linked | Proteasomal degradation | Protein turnover, cell cycle progression | Proteasome, RAD23B [9] |
| K63-linked | Non-proteolytic signaling | DNA repair, NF-κB signaling, endocytosis, autophagy | EPN2, TAB2/3 [9] [14] |
| K11-linked | Proteasomal degradation (ERAD), cell cycle regulation | Mitosis, endoplasmic reticulum-associated degradation | Proteasome, CDC48/p97 [10] |
| K6-linked | DNA damage response, mitophagy | DNA repair, mitochondrial quality control | Parkin, BRCA1-BARD1 [10] |
| K27-linked | Mitochondrial autophagy, immune signaling | Mitophagy, NF-κB pathway | - |
| K29-linked | Proteasomal degradation (less common) | Protein quality control | - |
| K33-linked | Kinase modification, trafficking | Endosomal sorting, kinase regulation | - |
| M1-linked | Inflammatory signaling, cell death | NF-κB activation, necroptosis | LUBAC complex, NEMO [13] |
K48-linked polyubiquitination serves as the principal signal for proteasomal degradation, representing one of the best-characterized ubiquitin signals [9] [10]. This chain type facilitates the recognition and degradation of myriad regulatory proteins, including cell cycle regulators, transcription factors, and damaged proteins. The proteasome recognizes K48-linked chains typically containing at least four ubiquitin monomers, though the importance of chain length specificity continues to be elucidated [9].
In contrast, K63-linked polyubiquitination typically serves non-proteolytic functions across diverse signaling pathways [14]. In DNA damage response, K63 chains facilitate the recruitment of repair proteins to damage sites. In inflammatory signaling, K63 ubiquitination of key signaling molecules such as RIP kinases and IKK complex components activates NF-κB signaling pathways [14]. Additionally, K63 chains play crucial roles in endocytic trafficking and selective autophagy, wherein they serve as recognition signals for autophagy receptors [14] [10].
Other linkage types including K11, K27, K29, and K33 constitute specialized ubiquitin signals with more restricted functions. K11-linked chains, for instance, collaborate with K48 chains to target cell cycle regulators for degradation during mitosis and participate in endoplasmic reticulum-associated degradation (ERAD) [10]. M1-linked linear chains, assembled by the linear ubiquitin chain assembly complex (LUBAC), play specialized roles in inflammatory signaling and cell death pathways [13].
Heterotypic and Branched Ubiquitin Chains
Table 2: Characterized Branched Ubiquitin Chains and Their Proposed Functions
| Branched Chain Type | Biosynthesis Mechanism | Proposed Functions | Biological Context |
|---|---|---|---|
| K48/K63-branched | TRAF6 + HUWE1; ITCH + UBR5 [11] | Enhanced degradation signal; regulation of NF-κB signaling [9] | Apoptosis regulation, immune signaling |
| K11/K48-branched | APC/C with UBE2C + UBE2S [11] | Enhanced substrate degradation during mitosis [11] [15] | Cell cycle progression |
| K29/K48-branched | Ufd4 + Ufd2 collaboration [11] | Protein quality control, ubiquitin fusion degradation pathway | Ubiquitin fusion degradation |
| K6/K48-branched | Parkin, NleL [11] | Mitochondrial quality control, unknown functions | Mitophagy, bacterial infection |
Branched ubiquitin chains represent the most topologically complex ubiquitin signals, wherein a single ubiquitin monomer serves as the branching point for two or more distinct chain types [11]. These structures exponentially increase the coding potential of ubiquitin signaling and have recently emerged as important regulatory signals, particularly in the context of protein degradation and signal transduction [9] [11].
The biosynthesis of branched chains frequently involves collaboration between E3 ligases with distinct linkage specificities. For instance, during NF-κB signaling, TRAF6 (a K63-specific E3) collaborates with HUWE1 (a K48-specific E3) to synthesize K48/K63-branched chains on signaling components [11]. Similarly, in the ubiquitin fusion degradation pathway, Ufd4 (K29-specific) and Ufd2 (K48-specific) cooperate to assemble K29/K48-branched chains [11]. Alternatively, single E3 ligases can synthesize branched chains, such as the APC/C which collaborates with distinct E2 enzymes (UBE2C and UBE2S) to assemble K11/K48-branched chains during mitosis [11].
Branched chains appear to function as specialized degradation signals that enhance substrate targeting to the proteasome. K11/K48-branched chains assembled by the APC/C more efficiently target mitotic regulators for destruction compared to homotypic K48 chains [11]. Similarly, K48/K63-branched chains can convert non-proteolytic K63-linked ubiquitination into a degradation signal, as demonstrated in the regulation of the apoptotic regulator TXNIP, where ITCH-mediated K63 ubiquitination is subsequently branched with K48 linkages by UBR5 to trigger proteasomal degradation [11].
Diagram 1: Ubiquitin chain topologies and their primary functional associations. Different chain architectures encode distinct biological information, with branched chains representing particularly complex signaling entities.
The Ubiquitin Code in Tumor Microenvironment Regulation
Ubiquitination in Tumor-Immune Cell Interactions
The tumor microenvironment represents a complex ecosystem wherein cancer cells interact with various stromal components, including immune cells, cancer-associated fibroblasts, endothelial cells, and extracellular matrix components [12] [13]. Ubiquitination plays pivotal roles in regulating these interactions, particularly in controlling immune cell function and immune checkpoint expression.
Programmed death-ligand 1 (PD-L1) stability represents a key node of ubiquitin-dependent regulation in the TME. Multiple E3 ligases including CHIP (STUB1), β-TrCP, HRD1, and SPOP mediate the ubiquitination and degradation of PD-L1, thereby influencing tumor immune evasion [12]. Conversely, the deubiquitinase CSN5 removes ubiquitin from PD-L1, stabilizing it and enabling tumors to escape T-cell-mediated immune surveillance [12]. Additionally, CMTM6 stabilizes PD-L1 through a non-enzymatic mechanism, protecting it from ubiquitin-mediated degradation [12].
Tumor-associated macrophages (TAMs) represent another crucial component of the TME regulated by ubiquitination. Macrophage polarization toward the pro-tumorigenic M2 phenotype is controlled by ubiquitin-dependent signaling pathways, particularly those involving NF-κB and inflammatory cytokine receptors [12] [13]. E3 ligases such as TRAF6 mediate K63-linked ubiquitination events that promote M2 polarization, thereby fostering an immunosuppressive TME conducive to tumor progression [13].
Ubiquitin-Dependent Signaling Pathways in Cancer Progression
Multiple oncogenic signaling pathways operating within the TME are subject to ubiquitin-dependent regulation. The PI3K/AKT pathway, frequently hyperactivated in cancer, is regulated by K63-linked ubiquitination of AKT itself. The E3 ligases Skp2 and TRAF6 mediate K63 ubiquitination of AKT, promoting its membrane translocation and activation, thereby driving tumorigenesis [14]. Similarly, the Wnt/β-catenin pathway is regulated by K63 ubiquitination events that control β-catenin stability and nuclear localization, as exemplified by Rad6B-mediated K63 ubiquitination of β-catenin at K394 in breast cancer [14].
The Hippo-YAP/TAZ pathway, which controls tissue growth and organ size, is similarly regulated by ubiquitination. The E3 ligase complex SKP2 mediates non-proteolytic K63-linked ubiquitination of YAP, controlling its nuclear localization and oncogenic activity, while the deubiquitinase OTUD1 reverses this modification [14]. Additionally, TAK1 inhibits YAP/TAZ proteasomal degradation by promoting TRAF6-mediated K63 ubiquitination in contrast to K48 ubiquitination [14].
Diagram 2: Key nodes of ubiquitin-dependent regulation in the tumor microenvironment. Multiple E3 ligases and deubiquitinases control critical processes in tumor progression and immune evasion.
Methodological Approaches for Ubiquitin Chain Analysis
Ubiquitin Interactor Pull-Down and Mass Spectrometry
Comprehensive analysis of ubiquitin chain functions requires specialized methodological approaches. Ubiquitin interactor pull-down coupled with mass spectrometry represents a powerful technique for identifying linkage-specific ubiquitin-binding proteins [9]. This approach typically involves immobilizing specific ubiquitin chain types (e.g., K48-Ub2, K63-Ub3, branched K48/K63-Ub3) on solid supports followed by incubation with cell lysates to enrich for specific ubiquitin-binding proteins, which are subsequently identified by liquid chromatography-mass spectrometry (LC-MS/MS) [9].
Critical methodological considerations include the use of deubiquitinase inhibitors to prevent chain disassembly during experiments. Commonly used inhibitors include chloroacetamide (CAA) and N-ethylmaleimide (NEM), though each presents distinct advantages and limitations [9]. NEM more completely inhibits chain disassembly but has potential off-target effects, while CAA is more cysteine-specific but permits partial chain disassembly [9]. Comparative studies using both inhibitors can identify inhibitor-dependent interactors, highlighting the importance of methodological considerations in experimental design.
Advanced Mass Spectrometry for Topology Determination
Top-down tandem mass spectrometry approaches enable detailed structural analysis of polyubiquitin chains without requiring proteolytic digestion [16]. This methodology preserves post-translational modifications and linkage information that would be lost with traditional bottom-up approaches. The protocol typically involves liquid chromatography separation followed by tandem MS analysis using fragmentation techniques such as electron transfer dissociation (ETD) combined with collision-induced dissociation (CID) or higher-energy CID (HCD) [16].
This approach facilitates discrimination between ubiquitin chain linkage types and can identify branched chains based on their unique fragmentation patterns [16]. The methodology is universally applicable to all chain linkage types and can be extended to ubiquitin-like proteins, providing a powerful tool for comprehensive ubiquitinome characterization.
Table 3: Key Research Reagents and Methodologies for Ubiquitin Chain Analysis
| Reagent/Methodology | Specific Application | Key Features and Considerations |
|---|---|---|
| Linkage-specific Ubiquitin Chains | Ubiquitin interactor pull-downs | Native isopeptide bonds; susceptible to DUBs; requires DUB inhibitors [9] |
| Chloroacetamide (CAA) | DUB inhibition in pull-downs | Cysteine-specific; partial chain disassembly may occur [9] |
| N-ethylmaleimide (NEM) | DUB inhibition in pull-downs | More potent cysteine alkylator; potential off-target effects [9] |
| Liquid Chromatography-Mass Spectrometry | Ubiquitin interactor identification | High sensitivity; requires specialized statistical analysis [9] |
| Top-down Tandem MS | Ubiquitin chain topology analysis | Preserves linkage information; identifies branched chains [16] |
| UbiCRest Assay | Linkage composition confirmation | Uses linkage-specific DUBs (OTUB1 for K48, AMSH for K63) [9] |
| Surface Plasmon Resonance | Binding affinity validation | Quantitative analysis of ubiquitin-binding protein interactions [9] |
Therapeutic Targeting of Ubiquitin Signaling
The ubiquitin-proteasome system represents a promising therapeutic target in cancer treatment, with several FDA-approved drugs already in clinical use. Proteasome inhibitors including bortezomib, carfilzomib, and ixazomib have demonstrated efficacy in hematological malignancies, particularly multiple myeloma [10]. These agents disrupt protein homeostasis, leading to accumulation of polyubiquitinated proteins and ultimately apoptosis in cancer cells.
Beyond proteasome inhibition, targeted approaches against specific components of the ubiquitin system are under active development. Inhibitors targeting E1 enzymes (e.g., MLN7243 and MLN4924), E2 enzymes (e.g., Leucettamol A and CC0651), and specific E3 ligases (e.g., nutlin and MI-219 targeting MDM2) have shown promise in preclinical models [10]. Additionally, deubiquitinase inhibitors represent emerging therapeutic opportunities, with compounds such as G5 and F6 demonstrating potential in preclinical cancer models [10].
Novel therapeutic strategies including proteolysis-targeting chimeras (PROTACs) hijack the endogenous ubiquitin machinery to selectively target oncoproteins for degradation [15]. These bifunctional molecules simultaneously bind to a target protein and an E3 ubiquitin ligase, facilitating target ubiquitination and degradation. This approach expands the druggable proteome to include proteins traditionally considered undruggable, representing a promising frontier in cancer therapeutics.
Ubiquitin chain topology constitutes a sophisticated regulatory system that governs protein fate and function through diverse structural configurations. From the classical degradation signal of K48-linked chains to the non-proteolytic signaling functions of K63 linkages and the emerging complexity of branched chains, the ubiquitin code represents a fundamental regulatory layer in cellular homeostasis. Within the tumor microenvironment, ubiquitin-dependent regulation impacts virtually all aspects of tumor biology, from cancer cell-intrinsic signaling to immune cell function and stromal interactions.
Ongoing methodological advances, particularly in mass spectrometry and interactome analysis, continue to reveal new dimensions of ubiquitin signaling complexity. The expanding toolkit for ubiquitin research, combined with developing therapeutic approaches targeting the ubiquitin-proteasome system, promises to yield new insights and treatment strategies for cancer and other diseases characterized by ubiquitin pathway dysregulation. As our understanding of the ubiquitin code deepens, so too will our ability to therapeutically manipulate this system for cancer treatment, particularly in the complex context of the tumor microenvironment.
The tumor microenvironment (TME) is a complex ectopic ecosystem composed of multiple cell types, including immune cells, fibroblasts, and endothelial cells, along with non-cellular components such as the extracellular matrix and secreted mediators [17]. Bidirectional communication between tumor cells and the TME is directly responsible for tumor genesis, progression, and metastasis, and is closely related to therapeutic efficacy and patient prognosis [17]. Ubiquitination, an essential and reversible post-translational modification, plays a vital role in modulating the stability, activity, and localization of proteins through a three-enzyme cascade involving E1 activating, E2 conjugating, and E3 ligase enzymes [17]. E3 ubiquitin ligases are particularly crucial as they confer substrate specificity, determining which proteins are targeted for ubiquitination and subsequent degradation or functional modification [18] [10]. Recognition of specific substrates is achieved through degrons—short peptide motifs that serve as minimal but sufficient elements for recognition by the degradation machinery within substrate proteins [17]. The ubiquitin-proteasome system (UPS) represents a major regulatory axis in cellular homeostasis, and its dysregulation contributes significantly to carcinogenesis [19] [10]. Emerging evidence indicates that E3 ligases extensively regulate the TME by controlling key cellular processes in both tumor and stromal cells, making them attractive therapeutic targets for cancer treatment [17] [19].
Classification and Mechanisms of E3 Ubiquitin Ligases
E3 ubiquitin ligases are categorized into several families based on their structural domains and mechanisms of action. The four principal families are RING, HECT, RBR, and CRLs (Cullin-RING Ligases), each employing distinct mechanisms to transfer ubiquitin to substrate proteins [17] [19].
Table 1: Major E3 Ubiquitin Ligase Families and Their Characteristics
| E3 Family | Mechanism of Action | Representative Members | Structural Features |
|---|---|---|---|
| RING | Direct transfer of Ub from E2~Ub to substrate [20] | MDM2, MARCH1 [19] | Characterized by a RING fold domain with zinc-binding sites; functions via monomers, homodimers, heterodimers, or multiple subunits [19] |
| HECT | Forms catalytic intermediate (HECT~Ub) before substrate transfer [20] | NEDD4, WWP2, Mule [19] | Bilobal HECT domain: N-lobe binds E2, C-lobe contains catalytic cysteine [19] |
| RBR | Hybrid mechanism; RING1 recruits E2~Ub, ubiquitin transferred to catalytic cysteine in Rcat domain, then to substrate [17] [20] | Parkin, HOIP, HHARI [17] [20] | Triad of RING1, BRcat (benign-catalytic), and Rcat (required-for-catalysis) domains [20] |
| CRLs | Multisubunit RING E3s; scaffold cullin protein binds substrate adapter and RING protein [21] | CUL1-5 complexes with FBXO17, FBXW [19] | Modular assembly: cullin scaffold, substrate-binding module (e.g., F-box protein), and RING protein (RBX1/2) [21] |
The following diagram illustrates the fundamental mechanistic differences in ubiquitin transfer among the major E3 ligase families:
RING E3 Ubiquitin Ligases
RING (Really Interesting New Gene) E3 ligases represent the largest family of E3 ubiquitin ligases and function primarily as scaffolds that simultaneously bind to E2~Ub complexes and substrate proteins, facilitating the direct transfer of ubiquitin from the E2 enzyme to the substrate without forming a covalent intermediate [20]. These ligases are characterized by a RING fold domain that coordinates two zinc ions in a cross-brace formation, which is essential for their structural integrity and function [20]. RING E3s can function as monomers, homodimers, heterodimers, or multi-subunit complexes, with Cullin-RING ligases (CRLs) representing a particularly important and diverse subclass of multi-subunit RING E3s [19]. The modular nature of CRLs allows for tremendous diversity in substrate recognition, as different substrate-binding modules can associate with the core cullin-RING scaffold [21].
HECT E3 Ubiquitin Ligases
HECT (Homologous to E6-AP C-terminus) E3 ligases employ a two-step catalytic mechanism that involves the formation of a covalent thioester intermediate between a conserved cysteine residue in the HECT domain and ubiquitin before ultimate transfer to the substrate [20] [19]. Structurally, the HECT domain consists of an N-terminal lobe that binds the E2 enzyme and a C-terminal lobe containing the catalytic cysteine residue, connected by a flexible linker [19]. This distinct mechanism allows HECT E3s to determine the topology of the ubiquitin chain being assembled, as the chain-building process occurs while ubiquitin is attached to the HECT domain itself. The human genome encodes approximately 28 HECT E3 ligases, which regulate diverse cellular processes and have been implicated in various pathological conditions, including cancer [19].
RBR E3 Ubiquitin Ligases
RBR (RING-BetweenRING-RING) E3 ligases represent a unique family that employs a hybrid mechanism combining features of both RING and HECT-type E3s [17] [20]. Recent structural and biochemical studies have prompted a revision in the nomenclature of RBR domains to more accurately reflect their structures and functions: the former RING2 domain is now designated Rcat (Required-for-catalysis) domain, while the intermediate IBR domain is renamed BRcat (benign-catalytic) domain [20]. Mechanistically, the RING1 domain first recruits the E2~Ub complex in a manner similar to canonical RING E3s, following which ubiquitin is transferred to a conserved cysteine residue in the Rcat domain through a trans-thioesterification reaction, forming a covalent intermediate analogous to HECT E3s [20]. Finally, the Rcat domain catalyzes the transfer of ubiquitin to the substrate protein. This sophisticated mechanism allows RBR E3s to precisely control the ubiquitination of specific substrates involved in critical cellular processes.
Cullin-RING Ligases (CRLs)
Cullin-RING ligases constitute the largest family of multi-subunit E3 ubiquitin ligases, characterized by a modular architecture assembled around a cullin scaffold protein (CUL1-5, CUL7, or CUL9) that serves as a molecular platform [21]. The cullin protein binds a substrate-recognition module at its N-terminus and a RING-domain protein (RBX1 or RBX2) at its C-terminus, which in turn recruits the E2 enzyme [21]. CRL activity is primarily regulated by neddylation—the covalent attachment of the ubiquitin-like protein NEDD8 to a specific lysine residue on the cullin subunit [21]. Neddylation induces a conformational change that enhances the recruitment and activation of the E2 enzyme, thereby increasing ubiquitination efficiency by up to 1000-fold [21]. The modular nature of CRLs allows for tremendous diversity, with hundreds of distinct CRL complexes possible through combinatorial assembly of different substrate-recognition modules, enabling precise control over the degradation of a vast array of cellular proteins.
Experimental Approaches for Studying E3 Ligases in TME Regulation
Conformation-Specific Profiling of CRL Networks
Recent advances in profiling E3 ligase activities have enabled more precise assessment of their functional states in biological systems. For CRLs, a key regulatory mechanism involves neddylation, which activates these complexes by inducing a specific conformational state. The following experimental workflow has been developed to profile active CRL repertoires using conformation-specific probes:
This approach utilizes synthetic antibodies (Fabs) generated through phage display that specifically recognize the active conformation of NEDD8-linked cullins [21]. The selection process involves a negative>negative>positive strategy that enriches Fabs binding specifically to neddylated cullin–RING complexes while depleting binders to unneddylated cullins or NEDD8 alone [21]. These conformation-specific probes enable:
- Activity-based profiling: Direct assessment of neddylated CRL complexes without requiring genetic manipulation [21]
- Network analysis: Identification of CRL complexes responding to cellular stimuli or targeted protein degradation [21]
- Cell-type specific repertoires: Comparison of baseline neddylated CRL landscapes across different cell types [21]
Table 2: Key Research Reagents for E3 Ligase Studies in TME
| Reagent/Category | Specific Examples | Function/Application | Experimental Use |
|---|---|---|---|
| Conformation-Specific Probes | N8C_Fab series [21] | Recognize active NEDD8-linked cullins with nanomolar affinity | Activity-based profiling of CRL networks; immunoprecipitation of neddylated CRLs |
| E3 Ligase Inhibitors | MLN4924 (Neddylation inhibitor) [21] | Inhibits NEDD8-activating enzyme, blocking CRL activation | Validation of CRL-dependent processes; studying neddylation dynamics |
| Targeted Degraders | PROTACs, Molecular Glues [18] [22] | Harness E3 ligases to degrade specific target proteins | Therapeutic exploration; studying substrate degradation mechanisms |
| Activity-Based Probes | Catalytic cysteine-reactive probes [21] | Label active HECT, RBR, and other cysteine-dependent E3s | Profiling enzymatic activities of cysteine-dependent E3 ligases |
Methodologies for Assessing E3 Ligase Function in TME
Comprehensive analysis of E3 ligase functions in the tumor microenvironment requires integrated experimental approaches:
- Genetic manipulation: Knockdown or knockout of specific E3 ligases in tumor or stromal cells to assess effects on TME composition and function [19]
- Substrate identification: Ubiquitinome profiling through mass spectrometry to identify novel E3 substrates in TME contexts [17]
- Functional assays: Assessment of tumor cell proliferation, apoptosis, migration, and immune cell functions following E3 modulation [19]
- Therapeutic validation: Testing E3-targeting agents in combination with immunotherapies to overcome treatment resistance [19]
E3 Ligase Regulation of Tumor Microenvironment Components
E3 ubiquitin ligases extensively regulate the tumor microenvironment by controlling the stability and function of key proteins in various TME components. The following sections detail specific mechanisms through which different E3 families influence TME dynamics.
Immune Cell Regulation in TME
E3 ligases play pivotal roles in modulating immune cell composition and function within the TME. In hepatocellular carcinoma (HCC), RNF125 expression levels show positive correlation with infiltration of CD4+ and CD8+ T cells as well as macrophages [19]. Similarly, WD repeat 4 (WDR4), when serving as a substrate receptor for CRL complexes, promotes degradation of the tumor suppressor PML protein, leading to expansion of Treg cells and M2 macrophages while reducing CD8+ T cells, thereby establishing an immunosuppressive TME [19]. Parkin, an RBR family E3 ligase, exhibits tumor-suppressive functions in HCC through direct degradation of TRAF2 and TRAF6, which drives HCC cell apoptosis by inhibiting the NF-κB pathway [19]. These examples illustrate how specific E3 ligases can shape the immunological landscape of tumors, potentially influencing response to immunotherapy.
Cancer Cell Signaling Pathways in TME
E3 ligases extensively regulate oncogenic signaling pathways that influence TME communication. In HCC, the HECT-type E3 ligase NEDD4 targets LATS1, a core component of the Hippo pathway, for ubiquitin-mediated degradation, thereby increasing YAP transcriptional activity and promoting tumor progression [19]. The RING-type E3 ligase MDM2 diminishes YAP's interaction with other proteins and promotes its cytoplasmic translocation and degradation, thereby inhibiting tumorigenesis [19]. Monomeric MARCH1 upregulates the PI3K-AKT-β-catenin pathway, promoting HCC growth and progression [19]. These pathway regulations not only affect cancer cell-intrinsic properties but also alter secretory profiles that influence stromal and immune cells within the TME.
Table 3: E3 Ligase Functions in Hepatocellular Carcinoma and TME Regulation
| E3 Ligase | E3 Family | Substrate(s) | Function in HCC/TME | Mechanism |
|---|---|---|---|---|
| FBXO17 | RING (CRL) | Unknown Wnt pathway component [19] | Promoter | Inhibits Wnt/β-catenin signaling [19] |
| MARCH1 | RING | PI3K-AKT pathway components [19] | Promoter | Upregulates PI3K-AKT-β-catenin pathway [19] |
| Hakai | RING (Dimer) | E-cadherin [19] | Promoter | Promotes E-cadherin degradation, driving EMT [19] |
| MDM2 | RING | YAP [19] | Suppressor | Promotes YAP cytoplasmic translocation and degradation [19] |
| WWP2 | HECT | Caspase-7, caspase-8, Bax [19] | Promoter | Regulates apoptosis; knockdown increases apoptosis markers [19] |
| Mule | HECT | β-catenin [19] | Suppressor | Targets β-catenin for degradation, suppressing cancer stem cell activity [19] |
| NEDD4 | HECT | LATS1 [19] | Promoter | Targets LATS1 for degradation, increasing YAP activity [19] |
| Parkin | RBR | TRAF2, TRAF6 [19] | Suppressor | Drives apoptosis via NF-κB pathway inhibition [19] |
Extracellular Matrix and Stromal Component Regulation
E3 ligases directly and indirectly regulate extracellular matrix (ECM) composition and stromal cell functions within the TME. Matrix metalloproteinases (MMPs), key enzymes involved in ECM remodeling and cancer invasion, are regulated by E3 ligases [19]. Additionally, E3 ligases influence epithelial-mesenchymal transition (EMT), a critical process in cancer progression that alters tumor-stroma interactions. For instance, the Hakai E3 ligase promotes degradation of E-cadherin, resulting in nuclear translocation of β-catenin proteins and ultimately driving EMT in HCC [19]. Similar mechanisms operate in other cancer types, highlighting conserved roles for E3 ligases in regulating ECM dynamics and stromal-tumor interactions across different TME contexts.
Therapeutic Targeting of E3 Ligases in TME
Targeted Protein Degradation Strategies
The understanding of E3 ligase mechanisms has enabled the development of innovative therapeutic strategies that harness the ubiquitin-proteasome system for targeted protein degradation. Several approaches have shown significant promise:
PROTACs (Proteolysis-Targeting Chimeras): Heterobifunctional molecules that simultaneously bind to an E3 ligase and a target protein of interest, thereby recruiting the target for ubiquitination and degradation [18] [22]. PROTACs have shown efficacy against various cancer-associated proteins previously considered "undruggable."
Molecular Glues: Small molecules that induce or stabilize interactions between E3 ligases and target proteins, leading to selective degradation [18] [22]. Unlike PROTACs, molecular glues are monovalent and typically function by altering the surface of either the E3 or target protein to create novel protein-protein interfaces.
Antibody-Based Degraders: Emerging technologies that utilize antibody-mediated targeting to deliver degradation signals to specific proteins or cell types [18].
These targeted degradation approaches offer several advantages over traditional inhibition strategies, including event-driven pharmacology, potential targeting of non-enzymatic functions, and ability to achieve profound and sustained target suppression.
E3 Ligase Inhibitors and Modulators
Beyond degradation strategies, direct targeting of E3 ligases themselves represents a viable therapeutic approach:
Neddylation Inhibitors: MLN4924 (Pevonedistat) inhibits the NEDD8-activating enzyme, blocking activation of CRL complexes and inducing apoptosis in various cancer models [21] [10].
E3-Specific Inhibitors: Compounds such as nutlin and MI-219 target the MDM2 E3 ligase, disrupting its interaction with p53 and stabilizing this critical tumor suppressor [10].
DUB Inhibitors: Compounds targeting deubiquitinating enzymes that counteract E3 ligase function, such as G5 and F6, have shown potential in preclinical cancer models [10].
Therapeutic targeting of E3 ligases in the TME context offers the potential for dual benefit—direct antitumor effects combined with TME modulation that may enhance response to conventional therapies and overcome resistance mechanisms.
E3 ubiquitin ligases represent master regulators of the tumor microenvironment, extensively controlling protein stability and function across cancer cells, immune cells, and stromal components. The four major E3 families—RING, HECT, RBR, and CRLs—employ distinct mechanistic strategies to achieve substrate specificity, enabling precise regulation of key cellular processes in the TME. Advanced experimental approaches, including conformation-specific probes and activity-based profiling, have revealed the dynamic nature of E3 networks and their complex regulation in biological systems. Growing understanding of E3 functions in TME regulation has catalyzed the development of innovative therapeutic strategies, particularly targeted protein degradation technologies that hijack endogenous E3 machinery to eliminate disease-driving proteins. As research continues to elucidate the intricate relationships between specific E3 ligases and TME components, promising opportunities emerge for developing novel cancer therapeutics that simultaneously target tumor cells and modulate the supportive microenvironment, potentially overcoming limitations of current treatment modalities.
This whitepaper provides a comprehensive analysis of phosphodegrons—phosphorylation-dependent recognition motifs that serve as pivotal regulatory elements in the ubiquitin-proteasome system (UPS). Within the context of the tumor microenvironment (TME), phosphodegrons integrate signaling inputs to control the stability of oncoproteins, tumor suppressors, and immune regulators, thereby influencing tumor progression and therapeutic responses. We detail the molecular mechanisms of phosphodegron recognition, present quantitative proteomic methodologies for their system-wide identification, and discuss emerging therapeutic strategies, including proteolysis-targeting chimeras (PROTACs), that exploit these motifs for targeted protein degradation. The content is structured to serve researchers, scientists, and drug development professionals working at the intersection of ubiquitination signaling and cancer biology.
Post-translational modifications (PTMs) constitute a critical regulatory layer that controls protein stability, function, and localization. Among these, phosphorylation and ubiquitination engage in extensive crosstalk to direct the timed degradation of cellular proteins [23] [24]. The ubiquitin-proteasome system (UPS), responsible for the degradation of most intracellular proteins, relies on E3 ubiquitin ligases to recognize specific degradation signals, or degrons, on their substrates [24] [25]. A phosphodegron is a specific type of degron that becomes activated upon phosphorylation of its serine, threonine, or tyrosine residues, creating a high-affinity binding site for a cognate E3 ligase [26] [25]. This phosphorylation event acts as a molecular switch, converting a stable protein into a target for polyubiquitination and subsequent proteasomal destruction [24].
The functional importance of phosphodegrons lies in their ability to confer precise, rapid, and reversible control over the abundance of key regulatory proteins. They are essential for fundamental processes including cell cycle progression, DNA damage response, apoptosis, and signal transduction [26]. Within the complex signaling networks of the tumor microenvironment (TME), dysregulation of phosphodegron-mediated degradation is frequently implicated in oncogenesis, immune evasion, and therapy resistance [27] [28] [29]. For instance, the stability of transcription factor FOXP3 in regulatory T cells (Tregs), a critical mediator of immunosuppression, is controlled by a complex balance of ubiquitin ligases and opposing PTMs on its phosphodegron [27]. Therefore, understanding the dynamics of phosphodegrons is not only fundamental to cell biology but also paramount for developing novel cancer therapeutics.
Molecular Mechanisms and Biological Significance
Structural Basis of Phosphodegron Recognition
Phosphodegrons are not merely phosphorylated residues; they consist of specific primary sequences surrounding the phosphorylatable residue that are complementary to the binding pocket of a specific E3 ubiquitin ligase [26]. The SCF (SKP1-CUL1-F-box protein) complex represents one of the best-characterized classes of E3 ligases that recognize phosphodegrons. Within the SCF complex, the variable F-box protein subunit (e.g., FBXW7, β-TrCP) acts as the substrate receptor that directly binds the phosphorylated motif [30] [26].
- Conserved Phosphodegron Motifs: Different F-box proteins recognize distinct, phosphorylated consensus sequences.
- FBXW7 recognizes the motif TPPx(S/T) (where S/T is phosphorylated) [30] [26]. This motif is found in oncoproteins such as MYC, NOTCH, and cyclin E, facilitating their regulated degradation.
- β-TrCP typically binds to the DpSGXXpS motif (where both serine residues are phosphorylated) [30] [25]. Substrates include β-catenin, IκBα, and CDC25A.
- FBXO22 was recently shown to recognize the motif XXPpSPXPXX (where pS is phospho-serine) to target proteins like the co-chaperone BAG3 for degradation [30].
The following diagram illustrates the generalized mechanism of phosphodegron recognition and subsequent protein degradation.
Phosphodegrons in the Tumor Microenvironment
The TME is a complex ecosystem where tumor cells interact with immune cells, fibroblasts, and other components. Phosphodegron-mediated regulation of protein stability is a key mechanism exploited by both tumor and stromal cells to adapt and survive.
Regulation of Immune Cell Function: In Tregs, the stability of the transcription factor FOXP3 is controlled by a battle between competing E3 ligases and deubiquitinating enzymes (DUBs) acting on its phosphodegron. The E3 ligase STUB1 promotes FOXP3 degradation, weakening Treg immunosuppressive function. Conversely, the E3 ligase Itch catalyzes non-degradative K63-linked ubiquitination, promoting FOXP3's nuclear localization and activity [27]. Targeting this axis with a KLHDC2-recruiting PROTAC to degrade FOXP3 is a potential strategy to enhance anti-tumor immunity [27].
Therapeutic Resistance: The ubiquitin system, including phosphodegron recognition, is a master regulator of radiotherapy resistance [28]. For example, the E3 ligase FBXW7 exhibits contextual duality: in p53-wild type tumors, it can promote radioresistance by degrading p53, whereas in SOX9-overexpressing non-small cell lung cancer (NSCLC), it enhances radiosensitivity by degrading SOX9 [28]. This highlights that the functional outcome of phosphodegron recognition is highly dependent on the genetic and signaling context of the TME.
Metabolic Reprogramming: Protein stability controlled by phosphodegrons directly impacts cancer metabolism. For instance, ERK-dependent phosphorylation of BAG3 at S377 creates a phosphodegron for SCFFBXO22, targeting this pro-survival co-chaperone for degradation. Disruption of this ERK-FBXO22-BAG3 axis promotes tumor growth by impairing apoptosis and cell cycle progression [30].
Table 1: Key E3 Ligases and Their Phosphodegron Substrates in Cancer
| E3 Ligase | Phosphodegron Motif | Key Substrate(s) | Role in Tumor Microenvironment | Ref. |
|---|---|---|---|---|
| FBXW7 | TPPx(pS/pT) | c-MYC, Cyclin E, NOTCH | Controls proliferation and growth; function is context-dependent (can be tumor suppressive or promote resistance). | [26] [28] |
| β-TrCP | DpSGXXpS | β-catenin, CDC25A, IκBα | Regulates WNT signaling, cell cycle checkpoints, and NF-κB-mediated inflammation. | [26] [25] |
| SCFFBXO22 | XXPpSPXPXX | BAG3 | Targets pro-survival co-chaperone BAG3; axis is involved in tumorigenesis. | [30] |
| STUB1 | Not fully defined | FOXP3 | Destabilizes FOXP3 in Tregs, potentially reducing immunosuppression. | [27] |
Experimental Protocols for System-Wide Identification
Mass spectrometry (MS)-based proteomics has become the mainstay technology for the system-wide, unbiased identification of phosphodegrons and phosphorylation-dependent substrates of E3 ligases [23] [30]. The following section outlines a detailed protocol for a quantitative phosphoproteomic screen to identify phospho-dependent SCF substrates.
Protocol: Quantitative Phosphoproteomic Screen for SCF Substrates
This protocol, adapted from a 2021 study, uses a neddylation inhibitor to inactivate Cullin-RING Ligases (CRLs), including SCF complexes, combined with Stable Isotope Labeling by Amino acids in Cell culture (SILAC) for quantitative MS [30].
Objective: To globally identify phosphorylation-dependent substrates of SCF E3 ligases by quantifying changes in the proteome and phosphoproteome upon CRL inhibition.
Key Reagent Solutions: Table 2: Essential Research Reagents for Phosphoproteomic Screening
| Reagent / Tool | Function / Explanation |
|---|---|
| MLN4924 (Neddylation Inhibitor) | Inhibits the neddylation of cullins, thereby inactivating CRL E3 ligases. This prevents the degradation of phosphorylated substrates, causing their accumulation. |
| SILAC (Stable Isotope Labeling) | Metabolic labeling for quantitative proteomics. "Light" and "Heavy" isotope-labeled amino acids allow for precise comparison of protein/phosphosite abundance between control and treated samples. |
| Immunoaffinity Phosphopeptide Enrichment | Enrichment of phosphorylated peptides from complex protein digests using titanium dioxide (TiO2) or anti-phosphomotif antibodies, enabling comprehensive phosphosite mapping. |
| LC-MS/MS (Liquid Chromatography-Tandem MS) | High-resolution separation and identification of peptides, and localization of phosphorylation sites with high confidence. |
| Motif Analysis (e.g., Motif-X) | Bioinformatics tool to identify statistically overrepresented phosphorylation motifs (e.g., potential novel phosphodegrons) from the list of upregulated phosphosites. |
Step-by-Step Workflow:
Cell Culture and SILAC Labeling: Grow two populations of HEK 293T cells (or other relevant cell lines) in SILAC "light" (L-lysine/L-arginine) and "heavy" (L-lysine-13C6/L-arginine-13C6) media until full isotopic incorporation is achieved [30].
CRL Inhibition and Cell Lysis:
- Treat the "heavy"-labeled cells with 1 µM MLN4924 for 4 hours.
- Treat the "light"-labeled control cells with vehicle (e.g., DMSO).
- Harvest cells and mix the light (control) and heavy (MLN4924-treated) populations at a 1:1 protein ratio.
- Lyse the combined cells and perform protein digestion with trypsin.
Phosphopeptide Enrichment: Subject the resulting peptide mixture to phosphopeptide enrichment using TiO2 beads or immunoaffinity purification with phosphomotif antibodies to isolate phosphorylated peptides for analysis [23] [30].
LC-MS/MS Analysis and Data Processing:
- Analyze the enriched phosphopeptides by high-resolution LC-MS/MS.
- Use database search engines (e.g., MaxQuant) to identify peptides and localize phosphorylation sites, calculating the Heavy/Light (H/L) ratio for each phosphosite and protein.
- Apply statistical analysis (e.g., t-test) to identify significant changes.
Bioinformatic Triage of Candidate Substrates:
- Apply screening criteria to identify potential phospho-dependent substrates. A successful screen identified candidates showing a >1.2-fold increase in both protein abundance and specific phosphorylation site intensity upon MLN4924 treatment [30].
- Integrate the resulting list with external datasets (e.g., BioGRID for SCF interactors, GPS for global protein stability data) to prioritize high-confidence candidates.
- Perform Kinase Enrichment Analysis (KEA) on upregulated phosphosites to identify kinases responsible for creating the phosphodegrons [30].
- Use motif analysis tools to discover enriched phosphorylation motifs that may represent novel phosphodegrons.
The experimental workflow for this protocol is summarized below.
Biochemical Validation of Candidate Phosphodegrons
Following the proteomic screen, putative phosphodegrons require rigorous biochemical validation.
Site-Directed Mutagenesis: Mutate the identified phosphorylated serine/threonine residue to alanine (S/T → A) to create a phosphorylation-deficient mutant. Compare the stability of the wild-type and mutant protein upon inhibition of the UPS (e.g., with MG132) or upon CRL inactivation (e.g., with MLN4924 or DN-CUL1). A true phosphodegron mutant will show increased basal stability and fail to accumulate further with MLN4924 treatment [30].
In Vitro Ubiquitination Assay: Purify the SCF E3 ligase complex and its substrate. Perform an in vitro reaction with E1, E2, ubiquitin, and ATP. Assess whether ubiquitination of the wild-type substrate is enhanced by its prior phosphorylation (e.g., using an active kinase) and whether this effect is abolished in the phospho-mutant [30].
Quantitative Data and Therapeutic Targeting
Quantitative Insights from Global Studies
High-throughput phosphoproteomic studies provide a systems-level view of phosphodegron dynamics. One systematic screen for phospho-dependent SCF substrates quantified over 12,276 phosphorylation sites across 4,322 proteins. Upon CRL inhibition, 369 phosphosites met the criteria for potential phosphodegron-associated sites (increased in both phosphorylation and total protein abundance) [30]. This data richness underscores the vast regulatory network controlled by phosphorylation-dependent degradation. Furthermore, kinase analysis revealed that CDKs, GSK3B, and MAPKs were significantly enriched upstream of the accumulated phosphosites, highlighting these kinases as primary drivers of phosphodegron creation [30].
Therapeutic Exploitation: PROTACs and Beyond
The understanding of phosphodegron biology has directly enabled the development of novel therapeutic modalities, most notably Proteolysis-Targeting Chimeras (PROTACs) [27] [28] [25].
PROTAC Mechanism: PROTACs are heterobifunctional molecules with one ligand that binds an E3 ubiquitin ligase (e.g., VHL or CRBN) and another that binds a protein of interest (POI), connected by a linker. The PROTAC induces proximity between the E3 ligase and the POI, leading to the POI's ubiquitination and degradation, bypassing the need for a native phosphodegron [27] [25].
Application in the TME: In cancer immunotherapy, a proposed strategy involves designing PROTACs that recruit the E3 ligase KLHDC2 to degrade FOXP3 in Tregs, thereby potentially reversing immunosuppression in the TME [27]. Additionally, radiation-responsive PROTACs (RT-PROTACs) are being developed to achieve spatially controlled degradation of oncoproteins like BRD4 specifically within irradiated tumors, enhancing radiotherapy efficacy [28].
Table 3: Targeting the Ubiquitin System in Cancer Therapy
| Therapeutic Class | Example(s) | Molecular Target / Mechanism | Clinical/Preclinical Context |
|---|---|---|---|
| Proteasome Inhibitor | Bortezomib, Carfilzomib | Inhibit the proteasome's proteolytic activity, causing accumulation of polyubiquitinated proteins. | Approved for multiple myeloma and mantle cell lymphoma. [27] [31] |
| E3 Ligase Inhibitor | P5091 (USP7 inhibitor) | Inhibits a deubiquitinase (DUB), leading to degradation of its substrates (e.g., MDM2, activating p53). | Preclinical promise in multiple myeloma. [27] |
| PROTAC | ARV-471, FOXP3-targeting PROTACs | Recruit E3 ligase to target oncoproteins or immune regulators for degradation. | Clinical trials and preclinical investigation for solid tumors and immuno-oncology. [27] [28] |
Phosphodegrons represent a fundamental mechanism of cellular information processing, where phosphorylation signals are translated into proteolytic outcomes. Within the dynamic and complex tumor microenvironment, the precise regulation of protein stability via phosphodegrons governs cell fate decisions, immune responses, and therapeutic susceptibility. The integration of quantitative mass spectrometry-based proteomics with sophisticated biochemical validation provides a powerful framework for decoding the global landscape of phosphodegron networks. As our mechanistic understanding deepens, so does the potential for innovative therapies. The transformative success of PROTAC technology exemplifies how hijacking the cell's intrinsic degradation machinery can lead to novel treatment strategies for cancer and other diseases, heralding a new era in targeted protein degradation.
F-box proteins, the critical substrate-recognition subunits of the SKP1-CUL1-F-box (SCF) ubiquitin ligase complex, have emerged as pivotal regulators at the intersection of cancer cell plasticity and immune evasion. These proteins mediate the ubiquitination and subsequent degradation of specific target proteins, playing essential roles in cell cycle regulation, signal transduction, and immune homeostasis. Within the tumor microenvironment, F-box proteins demonstrate remarkable functional heterogeneity, dynamically modulating key oncogenic processes including epithelial-mesenchymal transition, metabolic reprogramming, and immune checkpoint functionality. This whitepaper systematically examines the molecular mechanisms through which F-box proteins coordinate cancer cell adaptation and immunosuppression, reviews current experimental methodologies for their investigation, and discusses emerging therapeutic strategies targeting F-box proteins for combination immunotherapy. The comprehensive analysis presented herein aims to provide researchers and drug development professionals with both foundational knowledge and advanced insights into this crucial protein family's role in tumor progression.
The ubiquitin-proteasome system (UPS) represents a crucial post-translational modification pathway that regulates diverse cellular processes through the targeted degradation of specific proteins. Ubiquitination involves a sequential enzymatic cascade catalyzed by ubiquitin-activating (E1), ubiquitin-conjugating (E2), and ubiquitin ligase (E3) enzymes [7]. E3 ubiquitin ligases, the most critical components of this cascade, directly bind substrates and determine specificity. Among the hundreds of E3 ligases encoded in the human genome, the Cullin-RING ligase (CRL) complex family constitutes the largest group, with CRL1 (also known as the SCF complex) being the best-characterized member [7].
F-box proteins serve as the variable substrate-recognition components of the SCF complex, which consists of four essential subunits: the scaffold protein CUL1, the RING-finger protein RBX1, the adaptor protein SKP1, and an F-box protein that provides specificity [7]. The F-box domain, a characteristic motif of approximately 50 amino acids, facilitates binding to SKP1, while diverse C-terminal domains enable recognition of specific substrates [32] [33]. The human genome encodes approximately 69 F-box proteins, classified into three subfamilies based on their C-terminal domain structures: FBXW (WD40 repeats, 10 members), FBXL (leucine-rich repeats, 21 members), and FBXO (other domains, 38 members) [7].
Table 1: Classification of F-box Protein Subfamilies
| Subfamily | Distinguishing Feature | Number of Members | Representative Functions |
|---|---|---|---|
| FBXW | WD40 repeats at C-terminus | 10 | Cell cycle regulation, targeting of oncoproteins like c-MYC |
| FBXL | Leucine-rich repeats (LRRs) at C-terminus | 22 | Regulation of multiple signaling pathways, metabolic control |
| FBXO | Diverse C-terminal domains not fitting FBXW or FBXL categories | 38 | Broad regulatory roles in various cellular processes |
The evolutionary pattern of the F-box gene family primarily follows the birth-death model, characterized by gene duplication and loss events [32] [33]. Population genetic analyses reveal that domain regions within F-box genes experience significantly stronger purifying selection compared to non-domain regions, highlighting the critical functional importance of these conserved structural elements [32] [33].
Molecular Mechanisms of F-box Proteins in Cancer Cell Plasticity
Regulation of Epithelial-Mesenchymal Transition (EMT)
F-box proteins extensively regulate cancer cell phenotypic plasticity, particularly through epithelial-mesenchymal transition (EMT), during which epithelial cells lose their junctions and apical-basal polarity and remodel their cytoskeleton to acquire mesenchymal characteristics [7]. This process enhances cell motility and invasiveness, critical steps in metastasis. Multiple F-box proteins target key regulators of EMT for ubiquitin-mediated degradation:
β-TrCP (FBXW1/FBXW11): This F-box protein demonstrates dual functionality in EMT regulation. It activates NF-κB signaling by degrading IκB (NF-κB inhibitors), promoting pro-inflammatory factors that enhance tumor cell survival and metastasis [32] [33]. Simultaneously, β-TrCP mediates the ubiquitination and degradation of β-catenin to inhibit the classical Wnt pathway. Dysfunction in this regulatory axis leads to β-catenin accumulation, promoting EMT and the formation of an immunosuppressive microenvironment [32] [33].
FBXO25: Recent research has identified FBXO25 as a promoter of ovarian cancer progression through its interaction with α-actinin 1 (ACTN1) [34]. The FBXO25/ACTN1 axis activates ERK1/2 signaling and promotes EMT, driving tumor cell invasion and metastasis. This pathway exemplifies how F-box proteins can directly influence the mesenchymal transition of cancer cells through specific substrate interactions [34].
The complexity of F-box protein function is highlighted by their context-dependent roles, where individual F-box proteins can target different substrates to exert either pro-tumorigenic or anti-tumorigenic effects depending on cellular conditions [7].
Metabolic Reprogramming and Phenotypic Adaptation
Cancer cells exhibit remarkable metabolic plasticity, and F-box proteins serve as critical regulators of this adaptive capability. Through targeted protein degradation, they modulate key metabolic enzymes and signaling pathways that enable cancer cells to survive in challenging microenvironmental conditions:
β-TrCP in Pancreatic Cancer: In the low-glucose and hypoxic microenvironment of pancreatic cancer, β-TrCP indirectly regulates HIF1α and c-MYC signaling, both central drivers of metabolic adaptation [33]. The gene BZW1, functionally related to β-TrCP, enhances glycolytic metabolism by stabilizing HIF1α and c-MYC, exacerbating the formation of an immunosuppressive microenvironment [33].
β-TrCP-Mediated Lipid Metabolism: Research led by Wei Wenyi demonstrated that β-TrCP degrades Lipin1, a key enzyme in lipid metabolism, through ubiquitination, thereby regulating liver lipid metabolism homeostasis [32] [33]. Lipid overload in the tumor microenvironment can induce M2-type macrophage polarization and inhibit T cell function, creating an immunosuppressive niche [32] [33].
Table 2: F-box Proteins Regulating Cancer Cell Plasticity
| F-box Protein | Molecular Target | Biological Outcome | Cancer Context |
|---|---|---|---|
| β-TrCP (FBXW1) | IκB, β-catenin, Lipin1 | NF-κB activation, Wnt regulation, metabolic reprogramming | Pan-cancer (LUAD, KIRC, Pancreatic) |
| FBXO25 | α-actinin 1 (ACTN1) | ERK1/2 activation, EMT promotion | Ovarian cancer |
| FBXW7 | c-MYC, Cyclin E | Cell cycle control, stemness regulation | Multiple cancers |
| FBXO32 | Cyclin D1 | Cell cycle progression | Under investigation |
Diagram 1: F-box Protein Regulation of Cancer Cell Plasticity. F-box proteins integrate microenvironmental signals to drive plastic phenotypes through multiple signaling pathways.
F-box Proteins in Immune Evasion and Tumor Microenvironment Remodeling
Direct Regulation of Immune Checkpoint Molecules
F-box proteins directly regulate tumor immune microenvironments by targeting immune-related molecules for degradation, thereby modulating T-cell activation, macrophage polarization, and immune checkpoint functionality [32] [33] [35]. Specifically, they impact the PD-1/PD-L1 axis and CTLA-4 signaling, although the complete mechanistic details remain an active area of investigation [32] [33]. The regulatory dimensions of F-box proteins in the tumor immune microenvironment are increasingly recognized as critically important, particularly their mechanisms in mediating immune escape through reshaping immune cell metabolism or regulating immune checkpoint molecules [32] [33].
Control of Immune Cell Infiltration and Function
Pan-cancer analyses have revealed significant correlations between specific F-box protein expression patterns and immune cell infiltration:
β-TrCP and Immune Exclusion: Expression of FBXW1 (β-TrCP) shows significant negative correlation with immune score and matrix score, and positive correlation with tumor purity [32] [33]. In lung adenocarcinoma (LUAD) and kidney renal clear cell carcinoma (KIRC), high FBXW1 expression associates with reduced infiltration of immunocompetent cells including NK cells and CD8+ T cells, suggesting it promotes immunosuppression by inhibiting anti-tumor immune responses [32] [33].
Macrophage Polarization: The FBXO25/ACTN1/ERK1/2 axis in ovarian cancer not only promotes tumor progression but also facilitates M2 macrophage polarization [34]. When ovarian cancer cells were co-cultured with macrophages, ACTN1 overexpression promoted M2 polarization, as evidenced by increased CD163 expression, an effect reversible with ERK1/2 inhibition [34]. This demonstrates how F-box protein-mediated signaling in cancer cells can directly shape the immune landscape.
The functional heterogeneity of F-box proteins in tumor development has led to their classification into three categories: tumor-suppressive F-box proteins, proto-oncogenic F-box proteins, and context-dependent F-box proteins [32] [33]. This classification reflects their adaptable roles in different cancer types and stages.
Experimental Approaches for Investigating F-box Protein Functions
Model Systems for Studying F-box Proteins in Tumor-Immune Interactions
Research into F-box protein functions employs diverse model systems that recapitulate different aspects of the tumor microenvironment:
Organoid Cultures: Tumor organoids maintain the 3D structure of tumors and can incorporate multiple cell types from the tumor immune microenvironment [36]. Differences have been observed in therapeutic intervention efficacy between 2D models and 3D organoids, emphasizing the importance of modeling complex 3D cellular interactions when studying F-box protein function [36].
Genetically Engineered Mouse Models: Both syngeneic tumor models and genetically engineered mice enable investigation of F-box proteins in the context of an intact immune system [36]. Conditional knockout or overexpression systems allow tissue-specific manipulation of F-box protein expression to dissect their physiological functions.
Lineage Tracing Models: Given the importance of phenotypic plasticity in F-box protein function, lineage tracing models that follow markers like N-cadherin expression or employ genetic barcoding provide powerful tools for monitoring EMT and other plasticity events during tumor progression [36].
Methodologies for Identifying F-box Protein Substrates
A major challenge in the field remains the identification of specific ubiquitin ligase-substrate pairs, as most F-box proteins remain "orphans" without known substrates [37]. Several experimental approaches have proven effective:
Co-immunoprecipitation and Mass Spectrometry: As demonstrated in the identification of the SCFFbx23-Ace1 pair in Penicillium oxalicum, co-immunoprecipitation followed by mass spectrometry can reveal physical interactions between F-box proteins and their substrates [37]. In this study, deleting the Pofbx23 gene resulted in remarkable accumulation of all versions of the PoAce1 protein, confirming the functional relationship [37].
Ubiquitination Assays: In vitro ubiquitination assays using purified SCF complexes can demonstrate direct substrate ubiquitination. These assays typically require E1 and E2 enzymes, ubiquitin, ATP, and the reconstituted SCF complex with the specific F-box protein of interest.
Functional Validation: After identifying potential substrates, functional validation through genetic manipulation (knockdown/overexpression) of the F-box protein and assessment of substrate stability is essential. For example, in the FBXO25-ACTN1 interaction study, FBXO25 upregulation partially reversed cell proliferation and migration inhibited by ACTN1 knockdown, confirming their functional relationship [34].
Table 3: Experimental Approaches for F-box Protein Research
| Methodology | Key Applications | Technical Considerations |
|---|---|---|
| Co-immunoprecipitation + Mass Spectrometry | Identification of novel F-box protein substrates | Requires specific antibodies; may miss transient interactions |
| Genetic Knockout/Knockdown | Functional analysis of F-box proteins | Compensation by related family members may obscure phenotypes |
| Ubiquitination Assays | Direct demonstration of substrate modification | Requires purified components; optimized reaction conditions |
| Organoid Co-cultures | Study of F-box proteins in tumor-immune crosstalk | Maintains tissue architecture; complex to establish |
| Lineage Tracing | Monitoring plasticity events in real-time | Suitable for in vivo studies; requires genetic manipulation |
The Scientist's Toolkit: Research Reagent Solutions
Table 4: Essential Research Reagents for F-box Protein Investigations
| Reagent Category | Specific Examples | Research Applications | Key Functions |
|---|---|---|---|
| Genetic Manipulation Tools | CRISPR/Cas9 systems, siRNA/shRNAs, Conditional knockout mice | Functional studies of specific F-box proteins | Targeted gene disruption, conditional deletion in specific cell types |
| Detection Reagents | Anti-F-box protein antibodies, Anti-ubiquitin antibodies, Phospho-specific antibodies | Protein expression analysis, ubiquitination detection | Immunoprecipitation, Western blot, immunohistochemistry |
| Model Systems | Patient-derived organoids, Syngeneic mouse models, Humanized mouse models | Tumor-immune interaction studies | Preclinical testing, microenvironment recapitulation |
| Proteomics Tools | Tandem mass tag (TMT) reagents, Ubiquitin remnant motifs antibodies | Substrate identification, ubiquitinome analysis | Quantitative proteomics, ubiquitination site mapping |
| Small Molecule Inhibitors | SCF complex inhibitors, Kinase inhibitors targeting degron phosphorylation | Pathway modulation, therapeutic exploration | Mechanistic studies, combination therapy screening |
Therapeutic Implications and Future Perspectives
Targeting F-box Proteins in Combination Immunotherapy
The strategic targeting of F-box proteins represents a promising approach for enhancing cancer immunotherapy efficacy. Several potential strategies are emerging:
PROTAC-Based Approaches: Proteolysis-Targeting Chimeras (PROTACs) that selectively intervene in pathological substrate interactions offer a potential avenue for targeting specific F-box protein functions [32] [33]. Based on structural biology insights, these degradants could achieve selective modulation of F-box protein activity.
Combination with Immune Checkpoint Inhibitors: Given their roles in regulating immune checkpoint functionality and immune cell infiltration, F-box protein inhibition may sensitize tumors to existing immunotherapies [32] [33] [35]. For instance, targeting β-TrCP might reverse immune exclusion in tumors with high β-catenin signaling.
Metabolic Interventions: Since F-box proteins like β-TrCP regulate key metabolic enzymes, combining F-box protein modulation with metabolic interventions represents another promising strategy [32] [33].
Future Research Directions
Despite significant advances, critical knowledge gaps remain in our understanding of F-box protein functions:
Substrate Recognition Dynamics: More than 70% of F-box proteins still lack complete substrate identification [32] [33]. Systematic analysis of dynamic substrate recognition rules among family members represents a priority research area.
Non-degradative Ubiquitination: Emerging research indicates that F-box proteins can mediate non-proteolytic ubiquitination events. For example, FBXO32 can stabilize substrates through K27-linked ubiquitination, suggesting F-box proteins may constitute a new "ubiquitin code" decoding system [32] [33].
Single-Cell Multiomics: Application of single-cell multiomics technologies will help clarify tumor type-specific regulation patterns of F-box proteins and their cell-type-specific functions within the tumor microenvironment [32] [33].
Diagram 2: Therapeutic Targeting and Future Research Directions for F-box Proteins. The diagram outlines emerging therapeutic strategies and priority research areas for advancing F-box protein-based interventions.
F-box proteins represent multifunctional switches that coordinate cancer cell plasticity and immune evasion through sophisticated regulation of protein stability and function. Their position at the crossroads of ubiquitination signaling and tumor immunity makes them particularly attractive targets for therapeutic intervention. As our understanding of their complex regulatory networks deepens, particularly through advanced technologies like single-cell multiomics and structural biology, we anticipate rapid progress in targeting F-box proteins for combination immunotherapy approaches. The continued elucidation of F-box protein functions in specific cancer types and immune contexts will undoubtedly yield novel strategies for precision cancer treatment, ultimately improving patient outcomes in immunotherapy-resistant malignancies.
The tumor microenvironment (TME) represents a complex ecosystem where stromal components, particularly cancer-associated fibroblasts (CAFs) and endothelial cells (ECs), undergo extensive reprogramming to support tumor progression. Ubiquitination, a crucial post-translational modification, has emerged as a master regulator of stromal cell functionality within the TME. This whitepaper comprehensively analyzes how the ubiquitin-proteasome system (UPS) orchestrates CAF activation, endothelial cell function, and metabolic reprogramming through precise control of protein stability and signaling pathways. We detail molecular mechanisms whereby specific E3 ligases and deubiquitinases (DUBs) regulate key stromal processes, including CAF differentiation, angiogenesis, and immune evasion. Experimental methodologies for investigating ubiquitination in stromal cells are presented, alongside visualization of critical signaling networks and research reagent solutions. Understanding ubiquitin-mediated stromal reprogramming provides novel therapeutic avenues for disrupting tumor-stroma crosstalk and improving cancer treatment outcomes.
The tumor microenvironment is a dynamic network comprising malignant cells and various stromal components, including cancer-associated fibroblasts (CAFs), endothelial cells (ECs), immune cells, and extracellular matrix [38]. Stromal cells are not passive bystanders but active participants in tumor progression, undergoing extensive reprogramming to support cancer growth, metastasis, and therapy resistance [39] [40]. Central to this reprogramming is ubiquitination, a reversible post-translational modification that governs protein stability, activity, and localization through covalent attachment of ubiquitin molecules [13] [12].
The ubiquitination process involves a sequential enzymatic cascade: E1 ubiquitin-activating enzymes, E2 ubiquitin-conjugating enzymes, and E3 ubiquitin ligases which confer substrate specificity [12]. The human genome encodes over 600 E3 ligases, categorized into three major families: homologous to the E6AP carboxyl terminus (HECT), really interesting new gene (RING), and RING-between-RING (RBR) families [12]. Conversely, deubiquitinases (DUBs) remove ubiquitin modifications, providing dynamic regulation of protein fate. DUBs are classified into six families based on conserved catalytic domains: ubiquitin-specific proteases (USPs), ubiquitin C-terminal hydrolases (UCHs), ovarian tumor proteases (OTUs), Machado-Joseph disease proteases (MJDs), JAB1/MPR/Mov34 metalloproteases (JAMMs), and motif interacting with ubiquitin-containing novel DUB family (MINDY) [12].
Ubiquitin chain topology determines functional outcomes: Lys48-linked polyubiquitination typically targets proteins for proteasomal degradation, while Lys63-linked chains mediate non-proteolytic functions including signal transduction and DNA repair [28] [12]. Monoubiquitination and methionine 1-linked linear ubiquitin chains also participate in diverse cellular processes [13]. Within the TME, ubiquitination has emerged as a critical regulator of stromal cell reprogramming, influencing CAF activation, endothelial cell function, metabolic adaptation, and immune modulation [13] [12] [41]. This review examines the intricate mechanisms whereby ubiquitination orchestrates stromal cell reprogramming, with emphasis on CAFs and endothelial cells as key stromal components.
Ubiquitination in Cancer-Associated Fibroblast (CAF) Reprogramming
Molecular Mechanisms of CAF Activation and Heterogeneity
Cancer-associated fibroblasts represent the most abundant stromal cell type in many solid tumors, originating from various precursor cells including resident fibroblasts, bone marrow-derived mesenchymal stem cells, endothelial cells (via EndMT), and epithelial cells (via EMT) [39] [42]. CAFs exist in multiple functional states, primarily characterized by expression markers including α-smooth muscle actin (α-SMA), fibroblast activation protein (FAP), fibroblast-specific protein 1 (FSP1), platelet-derived growth factor receptors (PDGFRα/β), and caveolin-1 (Cav-1) [39] [42]. CAF activation is driven by soluble factors secreted by tumor cells, particularly TGF-β, which induces a myofibroblastic phenotype through metabolic reprogramming and oxidative stress [39].
Ubiquitination plays a fundamental role in regulating CAF differentiation and function through control of key signaling pathways. The UPS governs TGF-β signaling, a central pathway in CAF activation, through regulation of SMAD proteins and TGF-β receptors [13]. Additionally, ubiquitination modulates ROS production in CAFs by controlling NOX-4 stability, with TGF-β triggering NOX-4 upregulation and ROS production that promotes CAF differentiation [39]. The UPS also regulates inflammatory signaling in CAFs; for instance, USP14 degrades IκBα to activate NF-κB in head and neck cancers, promoting a pro-inflammatory CAF phenotype [28].
Table 1: Key E3 Ligases and DUBs Regulating CAF Biology
| Enzyme | Category | Target | Function in CAFs | Cancer Context |
|---|---|---|---|---|
| FBXW7 | E3 Ligase | p53, SOX9 | Context-dependent role in radiosensitivity | Breast cancer, NSCLC |
| USP14 | DUB | ALKBH5, IκBα | Stabilizes ALKBH5 to maintain stemness; degrades IκBα to activate NF-κB | Glioma, HNSCC |
| SMURF2 | E3 Ligase | HIF1α | Promotes HIF1α degradation under hypoxia | Multiple cancers |
| TRAF4 | E3 Ligase | JNK/c-Jun pathway | Activates anti-apoptotic pathways | Colorectal, oral cancers |
| USP28 | DUB | c-Myc | Stabilizes c-Myc to suppress ATM/ATR checkpoints | Esophageal, breast cancer |
Ubiquitin-Dependent Metabolic Reprogramming in CAFs
CAFs undergo extensive metabolic reprogramming to support tumor growth, predominantly shifting toward aerobic glycolysis (the "Warburg effect") even in oxygen-sufficient conditions [39]. This metabolic switch enables CAFs to produce and export high-energy metabolites (lactate, pyruvate, ketone bodies) that adjacent cancer cells utilize for oxidative phosphorylation and biosynthesis [39]. Ubiquitination regulates this metabolic reprogramming through control of key metabolic enzymes and transcription factors.
The UPS governs hypoxia adaptation in CAFs through regulation of hypoxia-inducible factors (HIFs). The von Hippel-Lindau (VHL) E3 ligase targets HIF-α subunits for proteasomal degradation under normoxic conditions [13] [12]. In hypoxic TME, HIF stabilization induces expression of glycolytic enzymes and monocarboxylate transporters, enhancing CAF glycolytic flux [39]. Additionally, ubiquitination regulates antioxidant defense in CAFs; for instance, impaired TGF-β signaling in CAFs suppresses the antioxidant enzyme glutathione peroxidase 1 (GPx1), leading to increased ROS levels that maintain CAF activation [39].
Ferroptosis regulation represents another ubiquitin-dependent process in CAFs. OTUB1 stabilizes GPX4 to suppress ferroptosis in gastric cancer, while TRIM26 stabilizes GPX4 via K63-linked ubiquitination in glioma [28]. These mechanisms protect CAFs from lipid peroxidation-induced cell death, maintaining their tumor-supportive functions within the TME.
Ubiquitination in Endothelial Cell Reprogramming
Regulation of Tumor Angiogenesis by Ubiquitination
Endothelial cells lining blood vessels undergo extensive reprogramming in the TME, forming abnormal, leaky vasculature that supports tumor growth and metastasis [40] [38]. Tumor-associated ECs (TECs) display marked phenotypic alterations characterized by high proliferative potential, genetic instability, and abnormal expression of adhesion molecules and immune regulators [40]. The ubiquitin system precisely controls multiple aspects of endothelial biology, including VEGF signaling, endothelial-to-mesenchymal transition (EndMT), and immune cell recruitment.
The VEGF/VEGFR axis represents a crucial ubiquitination target in endothelial cells. The UPS regulates VEGF receptor stability and signaling through multiple E3 ligases including CBL family proteins, which negatively regulate PD-L1 expression through inactivation of STAT, AKT, and ERK signaling [12]. Additionally, the ubiquitin system controls hypoxia response in ECs; for instance, VHL-mediated HIF-α degradation maintains endothelial homeostasis under normoxic conditions [13]. During hypoxia, HIF stabilization induces VEGF expression, driving angiogenic switching in the TME [38].
Table 2: Ubiquitin Enzymes Regulating Endothelial Cell Function
| Enzyme | Category | Target | Function in Endothelial Cells | Therapeutic Implication |
|---|---|---|---|---|
| VHL | E3 Ligase | HIF-α | Degrades HIF-α under normoxia | Anti-angiogenic therapy |
| β-TrCP | E3 Ligase | PD-L1 | Regulates PD-L1 stability in T cells | Combination immunotherapy |
| CHIP/STUB1 | E3 Ligase | PD-L1 | Destabilizes PD-L1 in Tregs | Immune checkpoint regulation |
| CSN5 | DUB | PD-L1 | Stabilizes PD-L1 to escape immune surveillance | Immunotherapy resistance |
| FBW7 | E3 Ligase | Notch4 | Regulates Notch signaling in angiogenesis | Vascular normalization |
Ubiquitin-Mediated Control of Endothelial-Immune Cell Crosstalk
Tumor-associated endothelial cells actively regulate immune cell infiltration and function through expression of adhesion molecules, chemokines, and immune checkpoint proteins [40] [38] [43]. The UPS governs this immunomodulatory function through control of key immune regulators. PD-L1 stability on endothelial cells is regulated by multiple E3 ligases (CHIP, β-TrCP, HRD1, SPOP) and DUBs (CSN5), influencing T cell activity and immune surveillance [12]. CMTM6, while not a DUB, protects PD-L1 from ubiquitination and degradation, enhancing immune evasion [12].
The ubiquitin system also controls adhesion molecule expression on endothelial cells. Pro-angiogenic factors (VEGF-A, FGF2, EGFL7) downregulate leukocyte adhesion molecules (P/E-selectin, ICAM1, VCAM1) on TECs, impairing immune cell infiltration [43]. Meanwhile, TECs selectively upregulate specific adhesion molecules (MAdCAM1, CLEVER-1) that promote infiltration of immunosuppressive cells like Tregs [43]. Ubiquitination likely regulates the stability of these adhesion molecules, though specific mechanisms require further elucidation.
Experimental Methodologies for Studying Ubiquitination in Stromal Cells
Proteomic Approaches for Ubiquitin Substrate Identification
Mass spectrometry-based ubiquitinome analysis enables system-wide identification of ubiquitination substrates in stromal cells. The following protocol outlines key steps for ubiquitinome profiling in CAFs and endothelial cells:
Cell Isolation and Culture: Primary CAFs are isolated from fresh tumor tissues via enzymatic digestion (collagenase/dispase) and differential centrifugation. Endothelial cells are isolated using magnetic bead-based separation with CD31 or CD144 antibodies. Cells are cultured under normoxic (21% O₂) or hypoxic (1-2% O₂) conditions to mimic TME [39] [40].
Ubiquitin Enrichment: Cells are lysed in denaturing buffer (6M guanidine-HCl, 100mM Na₂HPO₄/NaH₂PO₄, 10mM Tris-HCl, 5mM N-ethylmaleimide, pH 8.0). Ubiquitinated proteins are enriched using ubiquitin remnant motif antibodies (e.g., K-ε-GG antibody) or tandem ubiquitin-binding entities (TUBEs) [28] [12].
Mass Spectrometry Analysis: Enriched peptides are analyzed by LC-MS/MS on a Q-Exactive HF mass spectrometer. Data processing includes database searching (MaxQuant, Andromeda), quantification (LFQ algorithm), and statistical analysis (Perseus software) [28].
Validation: Candidate substrates are validated by immunoprecipitation and western blotting using ubiquitin antibodies under conditions of E3 ligase/DUB overexpression or knockdown.
Functional Assays for Ubiquitin Enzyme Activity
Determining functional consequences of ubiquitination in stromal cells requires specialized assays:
In Vitro Ubiquitination Assay: Recombinant E3 ligase/DUB is incubated with E1/E2 enzymes, ubiquitin, ATP, and substrate in reaction buffer (50mM Tris-HCl, pH 7.5, 5mM MgCl₂, 2mM ATP, 0.5mM DTT). Reactions are terminated with SDS sample buffer and analyzed by western blotting [12].
Cycloheximide Chase Assay: Stromal cells transfected with E3/DUB constructs are treated with cycloheximide (100μg/mL) to inhibit protein synthesis. Cells are harvested at time points and target protein degradation is monitored by western blotting [28] [12].
Co-immunoprecipitation: Cell lysates are incubated with target protein antibodies followed by protein A/G beads. Immunoprecipitates are analyzed by western blotting with ubiquitin or interacting protein antibodies [13].
Functional Phenotyping: Following E3/DUB modulation, stromal cell functions are assessed through migration (transwell assay), angiogenesis (tube formation assay), metabolic profiling (Seahorse analyzer), and cytokine secretion (ELISA/multiplex arrays) [39] [40].
Visualization of Ubiquitin Signaling Networks
Ubiquitin Signaling in CAF Activation: This diagram illustrates key ubiquitination pathways in cancer-associated fibroblast reprogramming, highlighting E3 ligases (red) and their targets in metabolic adaptation and activation.
Ubiquitin Regulation of Endothelial Function: This diagram depicts ubiquitin-mediated control of angiogenesis and immune regulation in tumor-associated endothelial cells, highlighting the balance between E3 ligases and DUBs.
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Research Reagents for Studying Ubiquitination in Stromal Cells
| Reagent Category | Specific Examples | Function/Application | Key Considerations |
|---|---|---|---|
| E3 Ligase Inhibitors | MLN4924 (NEDD8 activator inhibitor), SCF-I2 (Skp-Cullin-F-box complex inhibitor) | Block specific E3 ligase activities; study substrate stabilization | Monitor on-target toxicity; assess compensatory mechanisms |
| DUB Inhibitors | b-AP15 (proteasome DUB inhibitor), P5091 (USP7 inhibitor), VLX1570 (USP14/UCHL5 inhibitor) | Inhibit deubiquitinating enzymes; accelerate substrate degradation | Evaluate selectivity across DUB families; assess effects on protein turnover |
| Ubiquitin Probes | HA-Ubiquitin, TUBE (Tandem Ubiquitin Binding Entity), Ub-AMC (fluorogenic substrate) | Detect ubiquitinated proteins; measure DUB activity | Consider chain linkage specificity; optimize delivery methods |
| PROTACs | dBET1 (BRD4 degrader), ARV-771 (BET degrader), radiation-responsive PROTACs | Targeted protein degradation; study functional consequences of substrate loss | Assess tissue penetration; monitor degradation kinetics |
| Stromal Cell Isolation Kits | CD31+ microbeads (endothelial cells), FAP+ selection (CAFs), collagenase-based digestion | Isolate pure stromal cell populations from tumor tissues | Maintain cell viability; preserve native phenotype during isolation |
| Metabolic Assays | Seahorse XF Glycolysis Stress Test, LC-MS for metabolomics, glucose uptake probes | Characterize metabolic reprogramming in stromal cells | Correlate with ubiquitination status; compare normoxic vs hypoxic conditions |
Therapeutic Implications and Future Perspectives
Targeting ubiquitin signaling in stromal cells represents a promising therapeutic approach for cancer treatment. Several strategies are emerging:
Combination Therapies: Co-targeting stromal ubiquitin pathways with conventional therapies may overcome treatment resistance. For instance, inhibiting USP28 disrupts c-Myc/HIF-1α signaling and enhances radiotherapy response [28]. Similarly, targeting the OTUB1-GPX4 interaction sensitizes cells to ferroptosis inducers [28].
PROTAC Applications: Proteolysis-targeting chimeras (PROTACs) that engage E3 ligases to degrade specific targets in stromal cells show considerable promise. EGFR-directed PROTACs selectively degrade β-TrCP substrates in EGFR-dependent tumors, suppressing DNA repair while minimizing impact on normal tissues [28]. Radiation-responsive PROTAC platforms activated by tumor-localized X-rays offer spatial control of protein degradation [28].
Immunotherapy Combinations: Targeting ubiquitin pathways in endothelial cells may enhance immunotherapy efficacy. Normalizing tumor vasculature through modulation of ubiquitin enzymes improves T cell infiltration and function [40] [38] [43]. Combining anti-angiogenic agents with immune checkpoint blockers represents a promising strategy currently in clinical trials.
Future research should focus on developing more selective ubiquitin enzyme modulators with improved stromal cell targeting. Understanding cell-type specific functions of ubiquitin enzymes will be crucial, as evidenced by USP14's opposing roles in different cancers [28]. Advanced delivery systems including nanoparticles and antibody-drug conjugates may enable precise targeting of stromal ubiquitin pathways while minimizing systemic toxicity.
Ubiquitination serves as a master regulatory mechanism governing stromal cell reprogramming in the tumor microenvironment. Through precise control of protein stability and signaling networks, the ubiquitin-proteasome system orchestrates CAF activation, metabolic adaptation, endothelial cell function, and angiogenesis. The complex interplay between E3 ligases and DUBs creates a dynamic regulatory network that responds to TME cues including hypoxia, oxidative stress, and cytokine signaling.
Advancing our understanding of ubiquitin-mediated stromal reprogramming requires sophisticated experimental approaches including ubiquitinome profiling, functional validation of substrates, and physiological models of stromal-tumor interactions. The development of selective ubiquitin enzyme modulators and targeted degradation technologies offers promising therapeutic avenues for disrupting pro-tumorigenic stromal functions. Integrating stromal-targeting agents with conventional therapies and immunotherapies may ultimately improve outcomes for cancer patients by addressing the critical role of the tumor microenvironment in cancer progression and treatment resistance.
Therapeutic Exploitation: From Targeted Degradation to Clinical Translation
Targeted protein degradation (TPD) represents a revolutionary strategy in therapeutic development that hijacks the body's natural protein disposal systems to eliminate disease-causing proteins. Unlike traditional small molecule inhibitors that merely block protein activity, degraders catalytically destroy target proteins, offering potential advantages for addressing drug resistance and targeting previously "undruggable" proteins [44]. This approach primarily utilizes the ubiquitin-proteasome system (UPS), the primary pathway for regulated intracellular protein degradation in eukaryotic cells [18].
The UPS employs a sophisticated enzymatic cascade to mark proteins for destruction. This process begins with ubiquitin activation by an E1 enzyme in an ATP-dependent manner, followed by transfer to an E2 conjugating enzyme, and culminates with an E3 ubiquitin ligase facilitating the transfer of ubiquitin to specific substrate proteins [15]. E3 ligases are particularly crucial as they confer substrate specificity—the human genome encodes over 600 E3 ligases that recognize distinct sets of protein targets through specific degradation motifs called "degrons" [15]. Once a protein is tagged with a chain of at least four ubiquitin molecules linked through lysine 48 (K48), it is recognized and degraded by the 26S proteasome into small peptides [13].
The two primary TPD strategies—PROTACs (Proteolysis-Targeting Chimeras) and molecular glues—exploit this natural system differently. PROTACs are heterobifunctional molecules that physically link a target protein to an E3 ligase, while molecular glues induce or stabilize interactions between E3 ligases and target proteins that would not naturally occur [45] [46]. Both modalities have demonstrated significant potential for cancer therapy, particularly in modulating the tumor microenvironment (TME), where they can reprogram cellular components to overcome immunosuppression and enhance anti-tumor immunity [47] [15].
Molecular Mechanisms and Classifications
PROTACs: Heterobifunctional Degraders
PROTACs are rationally designed chimera molecules consisting of three key components: a ligand that binds the protein of interest (POI), a ligand that recruits an E3 ubiquitin ligase, and a linker connecting these two moieties [44]. This structure enables the PROTAC to form a ternary complex between the POI and E3 ligase, bringing them into close proximity and enabling ubiquitin transfer from the E2 enzyme to the POI. Crucially, PROTACs function catalytically—a single PROTAC molecule can facilitate the degradation of multiple POI copies, offering potential advantages in potency over occupancy-driven inhibitors [45].
The degradation efficiency of PROTACs depends on several factors beyond simple binary binding affinities. The stability of the ternary complex, the geometry of ubiquitin transfer, and the subcellular localization of all components significantly influence degradation efficacy [46]. Optimal linker length and composition are critical for ensuring proper orientation between the E3 ligase and POI, with insufficient or excessive distances between binding motifs reducing degradation efficiency [44].
Molecular Glues: Monovalent Inducers
Molecular glues are typically smaller, monovalent molecules that induce neo-interactions between E3 ligases and target proteins. Unlike the modular design of PROTACs, molecular glues work by altering the surface topography of an E3 ligase to create new binding interfaces for substrate proteins [45] [46]. A prominent example includes immunomodulatory imide drugs (IMiDs) such as thalidomide derivatives that reprogram the CRL4(^\text{CRBN}) E3 ligase to recognize novel protein substrates including transcription factors Ikaros and Aiolos [18].
The discovery of molecular glues has often been serendipitous, though recent advances in screening technologies are enabling more systematic identification. For instance, high-throughput proteomic approaches can now rapidly identify novel molecular glue interactions by monitoring changes in global protein stability, while biophysical methods like Spectral Shift technology directly characterize ternary complex formation [46].
E3 Ligase Families and Their Hijacking
The human proteome contains diverse E3 ubiquitin ligase families that can be co-opted for TPD:
- RING E3 Ligases: The largest family, characterized by a Really Interesting New Gene domain that directly cataly ubiquitin transfer from E2 to substrate. RING E3s include multi-subunit complexes like SCF (Skp1-Cullin1-F-box) and CRL (Cullin-RING Ligases) [48] [15].
- HECT E3 Ligases: Contain a Homologous to E6-AP C-Terminus domain that forms an obligate thioester intermediate with ubiquitin before transferring it to substrates [15].
- RBR E3 Ligases: Hybrid RING-HECT ligases (Ring Between Ring) that employ a two-step mechanism combining aspects of both RING and HECT families [15].
Current TPD platforms predominantly utilize a limited set of E3 ligases, primarily Cereblon (CRBN) and Von Hippel-Lindau (VHL), which together account for nearly 90% of developed degraders [45]. However, expanding the E3 ligase toolbox is an active research area, with investigations underway targeting MDM2, KEAP1, RNF114, and members of the SCF complex including Skp2, β-TrCP, and FBXW7 [45] [48].
Figure 1: Comparative Mechanisms of PROTACs and Molecular Glues
Quantitative Profiling of Degrader Properties
Table 1: Key Properties of PROTACs Versus Molecular Glues
| Property | PROTACs | Molecular Glues |
|---|---|---|
| Structure | Heterobifunctional: Target binder + E3 ligase binder + linker | Monovalent, single pharmacophore |
| Molecular Weight | High (often >700 Da), beyond "Rule of 5" | Lower, typically drug-like |
| Mechanism | Forms ternary complex by bridging E3 and target | Induces surface complementarity between E3 and target |
| Design Approach | Rational, modular design | Often serendipitous discovery; emerging rational design |
| Oral Bioavailability | Challenging due to size and efflux pumps [45] | More favorable due to smaller size |
| Resistance Mechanism | E3 ligase loss, efflux pumps [45] | Mutations in E3 ligase binding interface |
| E3 Ligases Targeted | CRBN, VHL, with expansion to others | Primarily CRBN, with growing diversity |
Table 2: Experimentally Determined Resistance Profiles of Targeted Protein Degraders
| Resistance Mode | Small Molecule Inhibitors | PROTAC Degraders |
|---|---|---|
| Primary Mechanism | Target mutation (e.g., T790M in EGFR) - active site changes [45] | Machinery loss (e.g., CRBN/VHL mutation) - ligase downregulation [45] |
| "Hook" Mutation Risk | High (requires high affinity binding) [45] | Low (can function with weak affinity) [45] |
| Cross-Resistance | Often limited to same-class inhibitors [45] | Class-wide (e.g., CRBN loss kills all CRBN degraders) [45] |
| Overcoming Strategy | Design tighter binders; Type II inhibitors [45] | Switch E3 ligase; use molecular glues [45] |
Applications in Tumor Microenvironment Research
The tumor microenvironment (TME) represents a complex ecosystem comprising malignant cells, immune cells, fibroblasts, endothelial cells, extracellular matrix, and signaling molecules [13] [15]. Ubiquitination signaling plays a pivotal role in regulating the delicate balance between anti-tumor and pro-tumor activities within the TME, making E3 ligases attractive targets for therapeutic intervention.
Remodeling Immune Cell Functions
PROTACs and molecular glues can reprogram immune cell functions within the TME by degrading key regulatory proteins:
- T-cell Regulation: The E3 ligase FBXO38 targets the immune checkpoint protein PD-1 for degradation, potentially enhancing anti-tumor T-cell activity [47]. Conversely, PROTAC-mediated degradation of Siglec-7 and Siglec-9 on T-cells rescues T-cell effector function by preventing dephosphorylation of TCR signaling cascades [46].
- Macrophage Polarization: E3 ligases regulate the balance between pro-inflammatory M1 macrophages and anti-inflammatory M2 macrophages. Targeted degradation of M2-polarizing factors could shift the balance toward anti-tumor phenotypes [13] [47].
- Myeloid Cell Manipulation: Myeloid-derived suppressor cells (MDSCs) inhibit anti-tumor immunity through multiple mechanisms including arginase production and PD-L1 expression [13]. Degrading key mediators of MDSC suppressive functions could enhance immune responses.
Targeting Angiogenesis and Stromal Components
The UPS regulates hypoxia response and angiogenesis through E3 ligases like VHL that target HIF-α subunits for degradation under normoxic conditions [13]. PROTACs targeting angiogenic signaling components or cancer-associated fibroblasts (CAFs) could normalize tumor vasculature and reduce desmoplasia, improving drug delivery and reducing immunosuppression.
Practical Implementation: Experimental Case Studies
Case Study 1: Development of Orally Bioavailable MDM2 Degraders Researchers at the University of Michigan developed highly potent and orally efficacious MDM2 PROTAC degraders for treating acute myeloid leukemia (AML) [46]. While traditional MDM2 inhibitors disrupt the MDM2-p53 interaction, MDM2 degraders eliminate the oncoprotein entirely, potentially overcoming limitations of insufficient efficacy and clinical resistance observed with MDM2 inhibitors.
Case Study 2: BTK Molecular Glue Degraders A recent study identified PS-10, a molecular glue that induces degradation of Bruton's tyrosine kinase (BTK) by recruiting the CRBN E3 ligase [46]. Cryo-EM analysis revealed unique protein interactions in the ternary complex, demonstrating that PS-10 binds CRBN and reshapes its surface to recognize BTK as a neosubstrate, despite showing no direct binding to BTK alone.
Case Study 3: Siglec Degraders for Immune-Resistant Tumors For anti-PD-1 and anti-CTLA-4 refractory tumors, Siglec-7/9 degraders that target these inhibitory receptors to the lysosome for degradation have shown promise in rescuing T-cell effector function and reprogramming the TME, resulting in productive tumor control [46].
Research Reagent Solutions
Table 3: Essential Research Tools for Targeted Protein Degradation Studies
| Research Tool | Function/Application | Example Uses |
|---|---|---|
| High-Throughput Proteomic Screening | Systematic discovery of novel degraders and their targets | NEOsphere Biotechnologies' platform screening 50,000 ubiquitination sites [46] |
| Spectral Shift Technology | Direct characterization of ternary complex formation | Eurofins Discovery's approach to identify WEE1 molecular glues [46] |
| E3scan Assay | Orthogonal validation of E3 ligase engagement | Confirming compound interaction with specific E3 ligases [46] |
| KinaseProfiler | Selectivity screening against kinase panels | Profiling molecular glue specificity across kinome [46] |
| Mechanistic PK/PD Modeling | Prediction of in vivo degradation profiles from in vitro data | Bayer's framework for degrader design optimization [46] |
| Electrostatic Complementarity Analysis | In silico evaluation of degrader-protein interactions | Cresset's platform for linker optimization in PROTAC design [46] |
Experimental Protocols and Methodologies
Assessing Degradation Efficiency
Western Blot Protocol for Target Protein Degradation
- Cell Treatment: Plate appropriate cancer cell lines (e.g., MM.1S for multiple myeloma studies) in 6-well plates at 60-70% confluence. Treat with serial dilutions of PROTAC or molecular glue compounds for 16-24 hours. Include DMSO vehicle control and positive controls if available.
- Protein Extraction: Lyse cells in RIPA buffer supplemented with protease and phosphatase inhibitors. Centrifuge at 14,000 × g for 15 minutes at 4°C and collect supernatant.
- Immunoblotting: Separate 20-30 μg protein by SDS-PAGE, transfer to PVDF membrane, and block with 5% non-fat milk. Incubate with primary antibodies against target protein (e.g., CDK8/CDK19, BTK) and loading control (e.g., GAPDH, β-actin) overnight at 4°C.
- Detection: Incubate with HRP-conjugated secondary antibodies, develop with ECL reagent, and quantify band intensity using densitometry software. Calculate DC(_{50}) values (concentration causing 50% degradation) using nonlinear regression analysis [46].
Ternary Complex Formation Assays
Surface Plasmon Resonance (SPR) for Ternary Complex Analysis
- Immobilization: Covalently immobilize E3 ligase (e.g., CRBN-DDB1 complex) on CMS sensor chip using amine coupling chemistry.
- Ligand Binding: Inject molecular glue or PROTAC E3-binding moiety at varying concentrations to confirm direct binding.
- Ternary Complex Assessment: Pre-incubate target protein with fixed concentration of degrader, then inject over immobilized E3 ligase. Measure response units compared to target protein alone to confirm enhanced binding indicative of ternary complex formation [46].
Global Ubiquitinomics Profiling
Mass Spectrometry-Based Ubiquitinome Analysis
- Sample Preparation: Treat cells with degraders or DMSO control, followed by lysis in denaturing buffer. Digest proteins with trypsin.
- Ubiquitin Peptide Enrichment: Use anti-diGly remnant antibodies to immunoaffinity purify ubiquitinated peptides.
- LC-MS/MS Analysis: Separate peptides by reverse-phase liquid chromatography followed by tandem mass spectrometry.
- Data Analysis: Identify and quantify diGly-modified peptides using search engines like MaxQuant. Compare ubiquitination site abundances between treatment conditions to identify degrader-induced changes [46].
Figure 2: PROTAC Resistance Mechanisms and Resolution Strategies
Challenges and Future Perspectives
Despite significant progress, several challenges remain in the clinical translation of PROTACs and molecular glues. Resistance mechanisms pose a substantial hurdle, with cancer cells employing multiple strategies to evade degradation, including E3 ligase downregulation, efflux pump upregulation, and proteasome mutations [45]. The current overreliance on just two E3 ligases (CRBN and VHL) creates a strategic vulnerability, as tumors can develop cross-resistance to entire drug classes through a single resistance mechanism [45].
Pharmacokinetic optimization presents another challenge, as the large molecular size of PROTACs often results in poor oral bioavailability and high efflux pump susceptibility [45]. Emerging solutions include the development of molecular glues with more drug-like properties and advanced formulation strategies. Computational approaches like mechanistic modeling and machine learning are being employed to predict in vivo degradation profiles and guide compound optimization [46].
Future directions in the field include:
- Expanding the E3 Ligase Toolbox: Diversifying beyond CRBN and VHL to include tissue-specific E3 ligases that may offer improved therapeutic windows and overcome resistance [45] [48].
- Novel Degrader Modalities: Developing autophagosome-targeting chimeras (AUTACs), lysosome-targeting chimeras (LYTACs), and antibody-based degraders to expand the scope of degradable targets beyond intracellular proteins [18].
- Combination Therapies: Rational pairing of degraders with immunotherapy, targeted therapy, and conventional chemotherapy to enhance efficacy and prevent resistance [47].
- Predictive Biomarkers: Identifying biomarkers for patient selection, particularly indicators of E3 ligase functionality and efflux pump expression to guide treatment decisions [45].
As the field matures, PROTACs and molecular glues are poised to transform cancer therapy by enabling targeting of previously intractable oncoproteins and modulating the tumor immune microenvironment. With multiple degraders in clinical trials and continued technological innovations, these modalities represent a promising frontier in the ongoing battle against cancer.
The tumor microenvironment (TME) represents a complex ecosystem where cancer cells evade immune destruction through multiple mechanisms, notably the activation of immune checkpoint pathways. The programmed cell death protein 1 (PD-1) and its ligand PD-L1 constitute a critical immunosuppressive axis that tumors exploit to suppress T-cell mediated cytotoxicity and achieve immune escape [49] [50]. While antibody-based blockade of PD-1/PD-L1 has revolutionized cancer treatment, therapeutic resistance remains a substantial clinical challenge, with response rates below 30% for single-agent therapy across many malignancies [51] [50]. Consequently, research has intensified toward understanding the fundamental molecular regulation of these immune checkpoints, particularly through post-translational modifications (PTMs).
The ubiquitin-proteasome system (UPS) has emerged as a master regulator of PD-1/PD-L1 protein dynamics and stability within the TME [49] [52]. As the primary pathway for intracellular protein degradation in eukaryotic cells, the UPS employs a sophisticated enzymatic cascade to tag target proteins with ubiquitin molecules, marking them for proteasomal destruction [53] [51]. This highly specific process involves the sequential action of ubiquitin-activating enzymes (E1), ubiquitin-conjugating enzymes (E2), and ubiquitin ligases (E3), which collectively determine substrate specificity and polyubiquitin chain topology [53] [51]. The reverse reaction, catalyzed by deubiquitinating enzymes (DUBs), removes ubiquitin chains and can rescue proteins from degradation [54] [51]. The intricate balance between ubiquitination and deubiquitination constitutes a crucial regulatory mechanism for PD-1/PD-L1 expression and function, presenting novel therapeutic opportunities to enhance the efficacy of cancer immunotherapy.
Molecular Mechanisms of PD-1/PD-L1 Regulation via Ubiquitination
The Ubiquitin-Proteasome System: Core Components and Function
The UPS operates through a conserved enzymatic cascade that conjugates ubiquitin to substrate proteins. Initially, the E1 enzyme activates ubiquitin in an ATP-dependent manner, forming a thioester bond between its catalytic cysteine residue and the C-terminal glycine of ubiquitin [51]. The activated ubiquitin is then transferred to a cysteine residue on an E2 enzyme. Finally, an E3 ubiquitin ligase recruits both the E2~ubiquitin complex and the target protein, facilitating the transfer of ubiquitin to a lysine residue on the substrate [53] [51]. E3 ligases demonstrate remarkable specificity, with over 600 identified in humans, recognizing distinct substrate proteins through specialized domains [51].
The consequences of ubiquitination depend heavily on the polyubiquitin chain topology. K48-linked polyubiquitin chains typically target substrates for proteasomal degradation, while K63-linked chains predominantly regulate non-proteolytic functions including signal transduction, endocytic trafficking, and DNA repair [49] [55]. Other linkage types, such as K11, K29, and linear M1 chains, mediate diverse cellular processes including endoplasmic reticulum-associated degradation, lysosomal degradation, and NF-κB signaling, respectively [51]. This "ubiquitin code" enables precise spatiotemporal control over protein fate and function within cellular networks.
Figure 1: The Ubiquitin-Proteasome System Cascade. This diagram illustrates the sequential enzymatic reactions of ubiquitination, from E1-mediated ubiquitin activation to E3-mediated substrate ligation, culminating in proteasomal degradation for K48-linked polyubiquitinated proteins.
E3 Ubiquitin Ligases Regulating PD-L1 Stability
Multiple E3 ubiquitin ligases directly target PD-L1 for ubiquitination and subsequent proteasomal degradation, functioning as critical negative regulators of this immunosuppressive molecule. The speckle-type POZ protein (SPOP) represents a well-characterized E3 ligase that promotes K48-linked ubiquitination of PD-L1 in colorectal cancer and hepatocellular carcinoma [49] [53]. SPOP-mediated degradation is competitively inhibited by aldehyde dehydrogenase 2 (ALDH2) in colorectal cancer cells, while the transcription factor BCLAF1 binds and sequesters SPOP in hepatocellular carcinoma, thereby stabilizing PD-L1 and promoting immune evasion [49] [53]. Additionally, sodium-glucose cotransporter 2 (SGLT2) stabilizes PD-L1 by competing with SPOP binding, an interaction that can be disrupted by the SGLT2 inhibitor canagliflozin to restore PD-L1 degradation [49] [53].
Beyond SPOP, several other E3 ligases contribute to PD-L1 regulation. TRIM21 promotes PD-L1 ubiquitination in non-small cell lung cancer (NSCLC), with its activity enhanced by CDK5 interaction [53]. The E3 ligase ARIH1 recognizes PD-L1 phosphorylated at Ser279 and Ser283 by glycogen synthase kinase 3 alpha (GSK3α), promoting its ubiquitination [53]. Beta-transducin repeat-containing protein (β-TrCP) also targets PD-L1 in a GSK3β-dependent manner, specifically recognizing nonglycosylated forms of PD-L1 [50]. These findings reveal a complex network of E3 ligases that maintain PD-L1 homeostasis, with tumor cells frequently exploiting regulatory mechanisms to stabilize PD-L1 and evade immune destruction.
Table 1: E3 Ubiquitin Ligases Regulating PD-L1 Stability
| E3 Ligase | Cancer Type | Regulatory Mechanism | Functional Outcome |
|---|---|---|---|
| SPOP | Colorectal Cancer, Hepatocellular Carcinoma | Direct binding to PD-L1; inhibited by ALDH2, BCLAF1, or SGLT2 competition | K48-linked ubiquitination and proteasomal degradation of PD-L1 |
| TRIM21 | Non-Small Cell Lung Cancer (NSCLC) | Activity enhanced by CDK5; LINC02418 acts as molecular sponge | Promotes PD-L1 ubiquitination and degradation |
| ARIH1 | Lymphosarcoma, NSCLC | Recognizes GSK3α-phosphorylated PD-L1 (Ser279/Ser283) | GSK3α-enhanced ubiquitination and degradation |
| β-TrCP | Multiple Cancers | Recognizes GSK3β-phosphorylated nonglycosylated PD-L1 | Phosphorylation-dependent ubiquitination and degradation |
E3 Ubiquitin Ligases Regulating PD-1 Stability
The PD-1 receptor on immune cells similarly undergoes ubiquitin-mediated regulation, though this mechanism has been less extensively characterized than PD-L1 regulation. F-box only protein 38 (FBXO38) has been identified as a critical E3 ligase that promotes PD-1 ubiquitination and degradation in activated T cells [52]. This process is essential for maintaining functional T-cell responses, as FBXO38 deficiency results in PD-1 accumulation and consequent T-cell exhaustion. Similarly, c-Cbl and Cbl-b (casitas B-lineage lymphoma) E3 ligases have been implicated in PD-1 ubiquitination, potentially through indirect mechanisms involving receptor internalization and degradation [52].
The regulation of PD-1 stability appears particularly important in the context of chronic antigen exposure, where sustained PD-1 expression drives T-cell exhaustion and dysfunctional anti-tumor immunity. Therapeutic strategies aimed at enhancing E3 ligase activity toward PD-1 could potentially reverse this exhausted phenotype and restore T-cell function, representing a promising approach to improve immunotherapeutic outcomes.
Deubiquitinating Enzymes Stabilizing PD-1/PD-L1
Counterbalancing the action of E3 ubiquitin ligases, deubiquitinating enzymes (DUBs) remove ubiquitin chains from target proteins, thereby stabilizing them against proteasomal degradation. Several DUBs have been identified that directly stabilize PD-L1 in cancer cells. CSN5 (constitutive photomorphogenesis 9 signalosome 5) binds to and deubiquitinates PD-L1, preventing its proteasomal degradation [52]. Similarly, ubiquitin-specific protease 7 (USP7) and USP22 have been shown to deubiquitinate PD-L1, enhancing its stability and promoting immune evasion [52].
The DUB OTUB1 (OTU domain-containing ubiquitin aldehyde-binding protein 1) stabilizes PD-L1 through a non-catalytic mechanism, inhibiting PD-L1 ubiquitination by binding to the E2 enzyme [52]. On the T-cell side, USP9X stabilizes the PD-1 receptor, contributing to T-cell exhaustion, while USP5 has been implicated in PD-1 stabilization in chronically stimulated T cells [52]. These DUBs represent attractive therapeutic targets, as their inhibition could simultaneously reduce PD-L1 expression in tumor cells and decrease PD-1 levels on T cells, potentially enhancing anti-tumor immunity through dual mechanisms.
Table 2: Deubiquitinating Enzymes Regulating PD-1/PD-L1 Stability
| Deubiquitinating Enzyme | Target | Regulatory Mechanism | Functional Outcome |
|---|---|---|---|
| CSN5 | PD-L1 | Direct binding and deubiquitination | Stabilizes PD-L1 protein |
| USP7 | PD-L1 | Catalytic deubiquitination | Prevents PD-L1 degradation |
| USP22 | PD-L1 | Catalytic deubiquitination | Enhances PD-L1 stability |
| OTUB1 | PD-L1 | Non-catalytic inhibition of E2 enzyme | Stabilizes PD-L1 |
| USP9X | PD-1 | Catalytic deubiquitination | Stabilizes PD-1 on T cells |
Experimental Approaches for Studying PD-1/PD-L1 Ubiquitination
Assessing Protein Ubiquitination Status
Determining the ubiquitination status of PD-1 and PD-L1 represents a fundamental methodology in this research field. The co-immunoprecipitation (co-IP) assay followed by western blotting serves as the gold standard technique for detecting protein ubiquitination. In this protocol, cells expressing the protein of interest (PD-1 or PD-L1) are treated with proteasome inhibitors (e.g., MG132) to accumulate ubiquitinated species. Following cell lysis, the target protein is immunoprecipitated using specific antibodies, and the immunoprecipitates are subsequently analyzed by western blotting with anti-ubiquitin antibodies [49] [53] [50].
For enhanced specificity in detecting particular ubiquitin chain topologies, researchers employ ubiquitin mutants where all lysine residues except one (e.g., K48-only or K63-only ubiquitin) are mutated to arginine. These constructs allow definitive identification of chain linkage types involved in regulating PD-1/PD-L1 stability [49] [55]. Additionally, cycloheximide chase assays provide complementary data on protein half-life, measuring the degradation kinetics of PD-1/PD-L1 following inhibition of new protein synthesis. Stabilization of these proteins upon proteasomal inhibitor treatment strongly suggests UPS-mediated regulation.
Identifying Regulatory E3 Ligases and DUBs
Systematic approaches to identify E3 ligases and DUBs that regulate PD-1/PD-L1 stability have proven invaluable. RNA interference (RNAi) screens targeting known E3 ligases or DUBs can reveal modifiers of PD-1/PD-L1 protein levels. In these experiments, target cells are transfected with siRNA or shRNA libraries, followed by quantification of PD-1/PD-L1 expression via western blotting or flow cytometry [53] [50].
For candidate validation, co-immunoprecipitation assays determine physical interactions between PD-1/PD-L1 and putative regulatory enzymes. Reciprocal co-IPs, where either the immune checkpoint molecule or the enzyme is immunoprecipitated, provide compelling evidence for direct interaction [49] [50]. Functional ubiquitination assays reconstitute the reaction in vitro using purified E1, E2, E3 enzymes, and PD-1/PD-L1 substrates to demonstrate direct ubiquitination without potential confounding factors from cellular environments [50].
In Vivo Validation and Therapeutic Assessment
Mouse tumor models represent essential tools for validating the physiological relevance of PD-1/PD-L1 ubiquitination regulators. Syngeneic mouse models, wherein immunocompetent mice are inoculated with tumor cells, allow investigation of immune responses in the context of genetic or pharmacological manipulation of ubiquitination pathway components [49] [53]. Key endpoints include tumor growth kinetics, immune cell infiltration analyzed by flow cytometry or immunohistochemistry, and functional assessments of T-cell activity through cytokine production or cytotoxicity assays.
For therapeutic evaluation, small-molecule inhibitors targeting specific E3 ligases or DUBs are administered alone or in combination with PD-1/PD-L1 blockade antibodies. The UPS-enhanced immunotherapy response can be quantified through comparison of tumor regression, survival benefit, and immune parameters between treatment groups [49] [53] [51]. These preclinical studies provide critical proof-of-concept for translating ubiquitination-targeting strategies into clinical applications.
Figure 2: Experimental Workflow for Studying PD-1/PD-L1 Ubiquitination. This diagram outlines the integrated experimental approaches from in vitro mechanistic studies to in vivo therapeutic validation that characterize the ubiquitination-mediated regulation of immune checkpoints.
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Research Reagents for Studying PD-1/PD-L1 Ubiquitination
| Reagent Category | Specific Examples | Research Application |
|---|---|---|
| Proteasome Inhibitors | MG132, Bortezomib, Carfilzomib | Block degradation of ubiquitinated proteins, allowing accumulation for detection |
| Ubiquitin System Modulators | PYR-41 (E1 inhibitor), MLN7243 (E1 inhibitor), Compound A (DUB inhibitor) | Tool compounds to interrogate specific components of ubiquitination machinery |
| Ubiquitin Constructs | Wild-type ubiquitin, K48-only ubiquitin, K63-only ubiquitin, Ubiquitin mutants (K0, K48R, K63R) | Determine ubiquitin chain topology and linkage specificity in ubiquitination assays |
| Antibodies for Detection | Anti-ubiquitin, anti-K48-linkage specific, anti-K63-linkage specific, anti-PD-1, anti-PD-L1 | Immunoprecipitation and western blot analysis of ubiquitination status |
| Kinase Modulators | GSK3α/β inhibitors (CHIR99021), CDK4/5 inhibitors (Palbociclib, Roscovitine) | Investigate phosphorylation-dependent ubiquitination mechanisms |
| Gene Manipulation Tools | siRNA/shRNA libraries, CRISPR/Cas9 systems, cDNA overexpression vectors | Knockdown or overexpression of specific E3 ligases, DUBs, or PD-1/PD-L1 |
Therapeutic Implications and Future Perspectives
The intricate regulation of PD-1/PD-L1 stability via ubiquitination presents compelling therapeutic opportunities to enhance cancer immunotherapy. Small molecules that modulate the activity of specific E3 ligases or DUBs could potentially normalize PD-1/PD-L1 expression levels in the TME, overcoming a key mechanism of resistance to current immune checkpoint inhibitors [49] [51] [52]. Several strategic approaches show particular promise for clinical translation.
First, enhancing the activity of E3 ligases that target PD-L1 for degradation, such as SPOP or TRIM21, could reduce PD-L1 expression on tumor cells and enhance T-cell-mediated killing. Similarly, boosting FBXO38 activity might decrease PD-1 levels on exhausted T cells, potentially reversing their dysfunctional state [52]. Second, inhibiting specific DUBs that stabilize PD-L1, such as CSN5 or USP7, represents an attractive strategy to promote PD-L1 degradation and sensitize tumors to immune attack [52]. The development of selective DUB inhibitors has advanced considerably, with several candidates entering clinical trials for various indications.
The integration of ubiquitination modulators with existing PD-1/PD-L1 blockade antibodies may yield synergistic therapeutic effects. Preclinical studies have demonstrated that SGLT2 inhibition with canagliflozin enhances SPOP-mediated PD-L1 degradation and augments the efficacy of anti-PD-1 therapy [49] [53]. Similarly, EGFR inhibition promotes GSK3α-mediated phosphorylation and ARIH1-dependent ubiquitination of PD-L1, suggesting that combination regimens with EGFR inhibitors may enhance responses to immunotherapy in EGFR-driven cancers [53].
Looking forward, emerging technologies promise to accelerate both fundamental understanding and therapeutic targeting of ubiquitin-mediated immune checkpoint regulation. Proteolysis-targeting chimeras (PROTACs) represent a particularly promising modality, enabling targeted degradation of specific proteins by recruiting them to E3 ubiquitin ligases [55]. PROTACs designed to target PD-L1 for degradation could potentially overcome the limitations of antibody-based approaches. Additionally, advances in quantitative mass spectrometry and structural biology will provide unprecedented insights into the molecular details of PD-1/PD-L1 recognition by regulatory enzymes, facilitating rational drug design.
As these therapeutic strategies advance toward clinical application, careful consideration of potential toxicities will be essential. The ubiquitin-proteasome system regulates countless cellular processes, and systemic modulation may produce off-target effects. Innovative delivery approaches, such as nanoparticle-based systems or tumor-targeting conjugates, may enhance specificity while minimizing adverse events. With thoughtful development, ubiquitin-based immunotherapeutic combinations hold significant potential to expand the population of cancer patients who derive durable benefit from immune checkpoint modulation.
The ubiquitin-mediated regulation of PD-1 and PD-L1 stability represents a crucial mechanism controlling immune checkpoint abundance and function within the tumor microenvironment. A sophisticated network of E3 ubiquitin ligases and deubiquitinating enzymes dynamically controls the turnover of these immunoregulatory proteins, influencing the balance between immune activation and tolerance. Malignant cells frequently exploit this regulatory system to stabilize PD-L1 expression and evade immune destruction, contributing to resistance against current immunotherapies.
The expanding mechanistic understanding of these processes reveals numerous therapeutic opportunities through targeted modulation of specific ubiquitination pathway components. Both laboratory research and emerging clinical evidence suggest that combining ubiquitin system modulators with existing immune checkpoint inhibitors can enhance anti-tumor immunity and overcome treatment resistance. As research in this field advances, the integration of ubiquitin-targeting strategies with standard immunotherapy regimens holds significant promise for improving outcomes for cancer patients.
The ubiquitin-proteasome system (UPS) is a crucial post-translational regulatory mechanism that maintains cellular homeostasis by controlling protein degradation, localization, and activity [56]. This enzymatic cascade, involving E1 (activating), E2 (conjugating), and E3 (ligating) enzymes, culminates in the attachment of ubiquitin to substrate proteins, marking them for proteasomal degradation or functional modification [57] [56]. The reverse process, deubiquitination, is carried out by deubiquitinases (DUBs), which remove ubiquitin chains and stabilize substrate proteins [58] [12]. In the context of the tumor microenvironment (TME), ubiquitination signaling regulates fundamental processes including immune cell function, cytokine signaling, hypoxia response, and metabolic adaptation [12] [59]. Cancer cells exploit this system to create an immunosuppressive TME, primarily by stabilizing immune checkpoint proteins such as PD-L1 and modulating the function of tumor-infiltrating lymphocytes [12] [5]. Consequently, targeted inhibition of specific components of the ubiquitin system has emerged as a promising therapeutic strategy to overcome immune evasion and enhance anti-tumor immunity.
The Ubiquitination Cascade and Therapeutic Targeting Sites
The ubiquitination process follows a precise enzymatic cascade. E1 enzymes activate ubiquitin in an ATP-dependent manner, forming a thioester bond. Activated ubiquitin is then transferred to an E2 conjugating enzyme. Finally, E3 ligases facilitate the transfer of ubiquitin from E2 to specific substrate proteins, with different E3 families employing distinct mechanisms [57] [56]. RING-type E3s function as scaffolds that bring the E2 and substrate into proximity, while HECT-type E3s form an intermediate thioester with ubiquitin before transferring it to the substrate [57]. Deubiquitinases (DUBs) counterbalance this process by cleaving ubiquitin chains, thereby regulating ubiquitin recycling and protein stability [58].
The following diagram illustrates this catalytic cascade and the primary sites for therapeutic intervention using small molecule inhibitors:
Small Molecule Inhibitors in Clinical Development
E3 Ubiquitin Ligase Inhibitors
E3 ligases represent particularly attractive therapeutic targets due to their substrate specificity, which potentially enables precise modulation of specific pathways with reduced off-target effects [57]. The majority of clinical-stage E3 inhibitors focus on MDM2 and IAP family proteins, with several candidates demonstrating promising anti-tumor activity.
Table 1: Selected E3 Ubiquitin Ligase Inhibitors in Development
| Target | Compound | Development Stage | Key Mechanisms & Notes |
|---|---|---|---|
| MDM2 | Nutlins, MI-63, Mel 23, HL198, TDP521252, TDP665759 | Preclinical & Clinical | Stabilize p53 tumor suppressor by blocking MDM2-mediated ubiquitination [57] |
| Skp2 | NSC689857, NSC681152 | Preclinical | Target SCF complex component; induce cell cycle arrest [57] |
| IAP (XIAP, cIAP1/2) | SM-406, GDC-0152 | Clinical | Promote apoptosis; overcome immune resistance [57] |
| SCFCdc4 | SCF-12 | Preclinical | Cell cycle regulation [57] |
| Itch | Clomipramine | Preclinical | Modulate immune signaling pathways [57] |
| E6AP | CM11-1 | Preclinical | Target HPV-associated malignancies [57] |
Deubiquitinase (DUB) Inhibitors
DUB inhibitors have gained significant attention for their ability to modulate protein stability in the TME. Several DUB targets have emerged as promising candidates for cancer therapy, with inhibitors advancing through preclinical development.
Table 2: Selected Deubiquitinase (DUB) Inhibitors in Development
| DUB Target | Compound Examples | Development Stage | Key Mechanisms in TME |
|---|---|---|---|
| USP1 | Pyrido[2,3-d]pyrimidin-7(8H)-one derivatives | Preclinical | Interfere with DNA damage repair; synergize with DNA-damaging agents [58] |
| USP7 | P5091, HBX 19818, P22077 | Preclinical | Modulate p53 stability and immune regulation; overcome bortezomib resistance in multiple myeloma [58] |
| USP14 | IU1 compounds | Preclinical | Enhance proteasome activity; potentially sensitize to proteasome inhibitors [58] |
| USP2a | Lithocholic acid hydroxyamide | Preclinical | Destabilize cyclin D1; induce G0/G1 arrest [58] |
| USP8 | Novel inhibitors via high-throughput screening | Preclinical | Regulate ERα expression in breast cancer [58] |
| USP9X | WP1130 derivatives | Preclinical | Induce apoptosis in FLT3-ITD-positive AML; promote c-Myc aggregation [58] |
Emerging Technologies: DUBTACs and Novel Modalities
Beyond conventional inhibitors, novel therapeutic platforms are emerging that leverage the ubiquitin system for targeted protein stabilization. Deubiquitinase-targeting chimeras (DUBTACs) represent a groundbreaking approach to rescue protective proteins from aberrant degradation in human diseases [60]. These heterobifunctional molecules consist of a target protein-binding ligand connected via a linker to a DUB-recruiting ligand, enabling selective stabilization of proteins of interest [60].
The mechanism of DUBTAC action involves:
- Simultaneous binding to both the protein of interest (POI) and a specific DUB
- Formation of a POI-DUBTAC-DUB ternary complex
- Deubiquitination of the polyubiquitinated POI by the recruited DUB
- Stabilization of the POI and restoration of its physiological function [60]
This platform shows particular promise for stabilizing tumor suppressor proteins (e.g., p53, CDKN1A), mutated proteins (e.g., ΔF508-CFTR in cystic fibrosis), and other protective proteins that are aberrantly degraded in disease states [60]. The following diagram illustrates the DUBTAC mechanism compared to traditional inhibition:
Experimental Protocols for Inhibitor Development
High-Throughput Screening for DUB Inhibitors
The discovery of novel DUB inhibitors typically employs sophisticated screening methodologies:
Ubiquitin-Rho-110 Fluorometric Assay: This high-throughput screening approach utilizes ubiquitin conjugated to the fluorogenic substrate Rhodamine-110. When DUB activity is present, cleavage occurs, generating a fluorescent signal. Inhibition of DUB activity reduces fluorescence in a dose-dependent manner, enabling quantitative assessment of inhibitor potency [58].
Mechanism of Action:
- Ubiquitin-Rho-110 substrate remains non-fluorescent when intact
- Active DUBs cleave the ubiquitin-Rho-110 conjugate
- Released Rho-110 generates measurable fluorescence (excitation ~500 nm, emission ~525 nm)
- Test compounds that inhibit DUB activity reduce fluorescence signal
- Z-factor validation for high-throughput screening suitability
Secondary Validation:
- Counter-screening against related DUBs to establish selectivity
- Cellular activity assessment using substrate stabilization assays
- Specificity profiling using activity-based protein profiling (ABPP) [58]
E3 Ligase Inhibitor Screening Strategies
Global Protein Stability (GPS) Profiling: This genome-wide screening strategy identifies E3 ligase substrates using reporter proteins fused with hundreds of potential substrates. By inhibiting ligase activity and monitoring reporter accumulation, researchers can comprehensively map E3-substrate regulatory networks [56].
CRISPR-Cas9 Screening: Genome-wide knockout screens help identify synthetic lethal interactions and validate E3 ligases as therapeutic targets in specific cancer contexts [56].
In Vitro Ubiquitination Assays: Reconstituted systems containing purified E1, E2, E3 enzymes, ubiquitin, ATP, and candidate substrates enable direct assessment of inhibitor effects on ubiquitin chain formation [56].
The Scientist's Toolkit: Key Research Reagents
Table 3: Essential Research Reagents for Ubiquitin System Studies
| Reagent Category | Specific Examples | Research Applications |
|---|---|---|
| Activity Assays | Ubiquitin-Rho-110, Activity-based probes (ABPs) | High-throughput screening, selectivity profiling, mechanistic studies [58] |
| Proteasome Inhibitors | Bortezomib, Carfilzomib, Ixazomib | Control compounds, validation of UPS-dependent processes, combination studies [58] |
| E1 Inhibitors | PYR-41, TAK-243 | Pathway validation, control experiments [57] |
| MDM2-p53 Interaction Inhibitors | Nutlins, MI-63 | Positive controls for E3 inhibition studies [57] |
| DUB-Targeting Compounds | WP1130, P5091, HBX 19818 | Benchmark compounds, tool compounds for pathway validation [58] |
| Ubiquitin Variants (UbVs) | Engineered ubiquitin mutants | Specific inhibition of E3 ligases or DUBs; mechanistic studies [12] |
| PROTAC/DUBTAC Components | E3 ligands, DUB ligands, linkers | Bifunctional molecule development, targeted protein degradation/stabilization [60] |
Targeting the ubiquitin system with small molecule inhibitors represents a promising frontier in cancer therapeutics, particularly within the complex landscape of the tumor microenvironment. The continued development of E1, E2, E3, and DUB inhibitors, coupled with emerging technologies such as DUBTACs, offers unprecedented opportunities to precisely modulate protein stability for therapeutic benefit. Current challenges include achieving sufficient selectivity, overcoming compensatory mechanisms, and identifying predictive biomarkers for patient stratification. Future directions will likely focus on combination strategies with immunotherapy, expansion of the degradome and stabilome toolbox, and translation of mechanistic insights into clinical breakthroughs for cancer patients. As our understanding of ubiquitin signaling in the TME deepens, so too will our ability to develop increasingly sophisticated therapeutic interventions that exploit this fundamental regulatory system.
The ubiquitin-proteasome system (UPS) has emerged as a master regulator of tumor biology, orchestrating critical processes in the tumor microenvironment (TME) that influence responses to both radiotherapy and immunotherapy [55] [12]. Ubiquitination, a reversible post-translational modification involving the sequential action of E1 activating, E2 conjugating, and E3 ligase enzymes, regulates protein stability, localization, and function through diverse chain topologies [12] [49]. The strategic manipulation of this system offers promising avenues for overcoming therapy resistance. K48-linked polyubiquitination primarily targets proteins for proteasomal degradation, while K63-linked chains facilitate non-proteolytic signaling complexes, and monoubiquitylation regulates chromatin dynamics and DNA damage responses [55] [28]. Deubiquitinases (DUBs) provide counter-regulation by removing ubiquitin modifications, creating a dynamic equilibrium that tumors exploit for adaptation [55]. This review examines mechanistic insights and combination strategies targeting the ubiquitin system to enhance radiotherapy and immunotherapy efficacy, providing a technical framework for researchers and drug development professionals working at this intersection.
Molecular Mechanisms of Ubiquitin Signaling in Therapy Resistance
Ubiquitin-Mediated Regulation of Radiotherapy Response
Radiotherapy resistance remains a major clinical challenge, largely driven by tumors' ability to dynamically adapt through ubiquitin-mediated networks [55]. The ubiquitin system orchestrates radioresistance through spatiotemporal control of DNA repair fidelity, metabolic reprogramming, and immune evasion [55] [28]. Distinct ubiquitin chain architectures govern tumor radioresistance through specialized mechanisms:
K48 Ubiquitination in Radiation Response: The effects of K48-linked ubiquitination demonstrate significant context dependency. FBXW7 exemplifies this duality: in p53-wild type colorectal tumors, it promotes radioresistance by degrading p53 and inhibiting apoptosis, whereas in non-small cell lung cancer (NSCLC) with SOX9 overexpression, FBXW7 enhances radiosensitivity by destabilizing SOX9 and alleviating p21 repression [55] [28]. This functional switch hinges on tumor-specific genetic backgrounds, as FBXW7 preferentially degrades substrates bearing phosphorylated degrons [55].
K63 Ubiquitination in Adaptive Survival: Beyond structural roles, K63-linked ubiquitin chains directly orchestrate cell survival pathways. FBXW7 employs K63 chains to modify XRCC4, enhancing the accuracy of non-homologous end joining (NHEJ) repair [55]. TRAF4 utilizes K63 modifications to activate the JNK/c-Jun pathway, driving overexpression of anti-apoptotic Bcl-xL in colorectal cancer and MCL-1 in oral cancers [55] [28]. Intriguingly, these chains can repurpose tumor suppressors; TRAF6 modifies p53 with K63 linkages, converting it into a pro-survival mitochondrial factor [55].
Monoubiquitylation in Genome Stability: Monoubiquitylation of both histones and non-histone proteins critically regulates radiation adaptation. UBE2T/RNF8-mediated H2AX monoubiquitylation accelerates damage detection in hepatocellular carcinoma, while RNF40-generated H2Bub1 recruits the FACT complex (SUPT16H) to relax nucleosomes [55]. For non-histone targets, FANCD2 monoubiquitylation specifically resolves carbon ion-induced DNA crosslinks, and γ-tubulin monoubiquitylation maintains centrosome integrity, whose disruption by high-LET radiation triggers mitotic catastrophe [55].
Table 1: Key E3 Ligases and DUBs in Radiotherapy Response
| Enzyme | Tumor Type | Function in Radioresistance | Therapeutic Vulnerability |
|---|---|---|---|
| FBXW7 | Colorectal cancer | Radioresistance: Degrades p53 to block apoptosis | MDM2/FBXW7 co-inhibition prevents compensatory resistance |
| FBXW7 | NSCLC | Radiosensitization: Degrades SOX9 to relieve p21 repression | Targeting SOX9 |
| TRIM21 | Nasopharyngeal carcinoma | K48-linked degradation of VDAC2 inhibits cGAS-STING pathway | Combined immunotherapy to overcome immune suppression |
| USP14 | Glioma | Radioresistance: Stabilizes ALKBH5 to maintain stemness | USP14 inhibitors |
| OTUB1 | Lung cancer | Radioresistance: Stabilizes CHK1 to enhance repair fidelity | Inhibiting OTUB1 to destabilize CHK1 |
Ubiquitin-Mediated Regulation of Tumor Immune Evasion
The UPS plays a pivotal role in tumor immune evasion by dynamically regulating immune checkpoint expression and immune cell function within the TME [27] [12] [49]. The stability of PD-L1 is intricately regulated by various E3 ligases and DUBs:
E3 Ligases Targeting PD-L1: Several E3 ligases catalyze the ubiquitination and degradation of PD-L1. The E3 ligase β-TrCP recognizes the typical DSG phospho-degron in substrates and catalyzes phosphorylation-dependent ubiquitination of non-glycosylated PD-L1 [12]. Glycogen synthase kinase 3β (GSK3β) phosphorylates β-catenin and facilitates recognition of PD-L1 by β-TrCP [12]. Speckle-type POZ protein (SPOP), an adaptor protein from the CRL E3 family, interacts with PD-L1, and Cullin3-SPOP polyubiquitinates and destabilizes PD-L1 [12] [49]. Malfunction of SPOP results in decreased tumor-infiltrating cells in mouse models [12]. Additionally, HRD1, a component of the endoplasmic reticulum-associated protein degradation (ERAD) complex, acts upon Ser195 phosphorylated PD-L1 in the ERAD process [12].
Regulation of PD-1 Expression: Beyond PD-L1 regulation, the UPS also controls PD-1 expression. FBXO38, belonging to the SCF subfamily, catalyzes Lys48-linked polyubiquitination to induce proteasome degradation of PD-1 in tumor-infiltrating T cells [12]. This mechanism provides a potential avenue for enhancing T cell function in the TME.
DUBs Stabilizing Immune Checkpoints: Counteracting E3 ligase activity, DUBs stabilize immune checkpoint proteins. COP9 signalosome complex subunit 5 (CSN5), a JAMM-family DUB, deubiquitinates and stabilizes PD-L1, thereby escaping T cell-mediated immune surveillance [12]. Expression of CSN5 is induced by NF-κB, which is activated by proinflammatory cytokine TNF-α [12]. Another protein that stabilizes PD-L1 is CMTM6, which, while not a DUB, can interact with PD-L1 on tumor cell surfaces and protect PD-L1 from ubiquitination and degradation [12].
Regulation of Treg Function: The UPS significantly influences regulatory T cell (Treg) biology, which is crucial for maintaining immune homeostasis and suppressing excessive immune responses [27]. The stability of FOXP3, the master transcription factor of Tregs, is vital for their immunosuppressive function, and its dysregulation can contribute to tumor immune evasion [27]. Various E3 ubiquitin ligases regulate FOXP3 stability and function through different mechanisms. Itch promotes the nuclear translocation and transcriptional activity of FOXP3 through K63-linked ubiquitination modification (a non-degradative type) [27]. In Itch-deficient mice, the nuclear localization of FOXP3 in Treg cells is reduced by 50%, leading to an autoimmune phenotype [27]. TRAF6 catalyzes the K63 ubiquitination of FOXP3 at Lys227, promoting the binding and stabilization of the deubiquitinase USP7 [27]. Conversely, RNF31 catalyzes M1-linked linear ubiquitination of FOXP3, antagonizing the K48 degradation signal [27]. The RNF31 inhibitor HOIPIN-8 reduces the FOXP3 level in Treg cells by 60%, enhancing anti-tumor immunity [27]. As a component of the CRL2^(KLHDC2) complex, KLHDC2 mediates the K48-linked ubiquitination degradation of FOXP3 [27].
Strategic Combination Approaches
Ubiquitin-Targeting Agents with Radiotherapy
Targeting the ubiquitin system shows significant promise for enhancing radiotherapy efficacy through multiple mechanisms:
PROTAC Platforms for Radio-sensitization: Capitalizing on the druggable nature of the ubiquitin system, significant progress has been made with proteolysis-targeting chimeras (PROTACs), which demonstrate compelling radiosensitizing effects [55] [28]. The specificity of these agents is exemplified by EGFR-directed PROTACs that selectively degrade β-TrCP substrates in EGFR-dependent tumors (e.g., lung and head/neck squamous cell carcinomas), suppressing DNA repair while minimizing impact on normal tissues [55]. Innovative radiation-responsive PROTAC platforms are emerging to overcome radioresistance, including radiotherapy-triggered PROTAC (RT-PROTAC) prodrugs activated by tumor-localized X-rays to degrade BRD4/2, synergizing with radiotherapy in breast cancer models [55]. Additionally, X-ray-responsive nanomicelles (e.g., diselenide-bridged RCNprotac) selectively release PROTACs (such as MZ1 targeting BRD4) within irradiated tumors [55].
Targeting DNA Repair Mechanisms: The ubiquitin system offers numerous targets for disrupting DNA repair pathways in combination with radiotherapy. RNF126-mediated K27/K29 polyubiquitin of MRE11 activates the ATM-CHK1 axis in TNBC, thereby promoting error-prone repair [55]. Structural studies illuminate this process, demonstrating that radiation-induced ATM phosphorylation induces conformational changes in RNF168, facilitating K63-linked ubiquitination of H2A/H2AX to open chromatin and recruit BRCA1-A complexes [55]. Targeting these ubiquitin-mediated DNA repair mechanisms presents opportunities for selective radio-sensitization.
Metabolic Reprogramming Approaches: Ubiquitination critically regulates cancer metabolism, reprogramming processes such as ferroptosis susceptibility, hypoxia adaptation, and nutrient flux, thereby creating targetable vulnerabilities for radio-sensitization [55] [28]. TRIM26 stabilizes GPX4 via K63 ubiquitination to prevent ferroptosis in gliomas [55] [28]. Similarly, OTUB1 stabilizes GPX4 to suppress ferroptosis in gastric cancer [28]. Targeting the OTUB1-GPX4 interaction or inhibiting the FTO-OTUB1 axis in nasopharyngeal carcinoma increases ferroptosis sensitivity when combined with radiotherapy [28].
Table 2: Experimental Combination Strategies in Preclinical Development
| Combination Approach | Molecular Target | Proposed Mechanism | Experimental Model |
|---|---|---|---|
| RT-PROTAC platform | BRD4/2 degradation | Radiotherapy-triggered PROTAC activation enhances tumor-specific protein degradation | Breast cancer models |
| EGFR-directed PROTAC | β-TrCP substrate degradation | Selective degradation in EGFR-dependent tumors suppresses DNA repair | Lung and HNSCC models |
| USP14 inhibition | K63-ubiquitinated IRF3 stabilization | Accumulation of K63-modified IRF3 triggers STING-dependent antitumor immunity | Preclinical models |
| TRIM21 inhibition | VDAC2 stabilization | Prevents degradation of VDAC2, activating cGAS/STING pathway | Nasopharyngeal carcinoma models |
| HOIPIN-8 (RNF31 inhibitor) | FOXP3 degradation in Tregs | Reduces FOXP3 levels in Treg cells by 60%, enhancing anti-tumor immunity | Preclinical models |
Ubiquitin-Targeting Agents with Immunotherapy
The combination of ubiquitin-targeting agents with immunotherapy represents a promising strategy for overcoming immune resistance:
Enhancing Immune Checkpoint Blockade: Combining UPS-targeted therapies with immune checkpoint inhibitors (ICIs) shows significant potential for enhancing anti-tumor immune responses [27] [61] [49]. The stability of PD-L1 is regulated by various E3 ligases, and targeting these regulators can enhance the efficacy of PD-1/PD-L1 blockade therapy [12] [49]. For example, targeting the E3 ligase SPOP, which promotes ubiquitination and degradation of PD-L1, represents a promising combination strategy with ICIs [49]. In colorectal cancer cells, SPOP promotes ubiquitination and degradation of PD-L1, while ALDH2 expressed at high levels in cancer cells competitively binds to PD-L1 with SPOP, inhibiting PD-L1 ubiquitination [49]. Similarly, in hepatocellular carcinoma, the transcription factor BCLAF1 inhibits PD-L1 ubiquitination by SPOP by targeting and binding to SPOP, enhancing PD-L1 stability and promoting tumor immune evasion [49]. Targeting these interactions could enhance ICI efficacy.
Modulating Treg Function: Targeting E3 ligases that regulate FOXP3 stability presents opportunities for enhancing anti-tumor immunity. KLHDC2 mediates K48-linked ubiquitination degradation of FOXP3, and knockout of KLHDC2 extends the half-life of FOXP3 by 4 times and enhances the inhibitory function of Treg cells by 2.3 times [27]. Identification of small-molecule PROTACs targeting KLHDC2 and FOXP3 is a potential strategy for immunotherapy [27]. Additionally, inhibition of USP5 alongside PD-(L)1 blockade represents a promising cancer treatment strategy [27].
DUB Inhibition for Immune Enhancement: Targeting DUBs that stabilize immune checkpoints or regulatory proteins provides another combination approach. The USP7 inhibitor P5091 has shown promise in treating multiple myeloma by promoting ubiquitination and degradation of MDM2, thereby activating the p53 pathway [27]. Similarly, USP14 inhibition leads to accumulation of K63-modified IRF3, triggering STING-dependent type I interferon responses and synergizing with radiotherapy to overcome immune evasion [55]. These approaches demonstrate the potential of DUB inhibitors in combination with immunotherapy.
Experimental Protocols and Methodologies
Assessing Ubiquitin-Mediated PD-L1 Regulation
Protocol: Co-immunoprecipitation for E3 Ligase-PD-L1 Interaction Studies
Cell Lysis and Preparation: Harvest cancer cells (e.g., colorectal cancer cell lines) and lyse in RIPA buffer (50 mM Tris-HCl pH 7.4, 150 mM NaCl, 1% NP-40, 0.5% sodium deoxycholate, 0.1% SDS) supplemented with protease inhibitors (e.g., PMSF, leupeptin, aprotinin) and 20 mM N-ethylmaleimide to inhibit endogenous DUBs [49].
Immunoprecipitation: Incubate cell lysates (500-1000 μg total protein) with anti-PD-L1 antibody (1-2 μg) overnight at 4°C with gentle rotation. Add Protein A/G agarose beads and incubate for an additional 2-4 hours [49].
Western Blot Analysis: Resolve immunoprecipitates by SDS-PAGE and transfer to PVDF membranes. Probe with antibodies against SPOP, ALDH2, or other E3 ligases of interest to detect interactions [49].
Ubiquitination Assay: Treat cells with MG132 (10 μM, 6 hours) before lysis to stabilize ubiquitinated proteins. Immunoprecipitate PD-L1 and probe with anti-ubiquitin antibody to detect ubiquitination levels under different experimental conditions [49].
Protocol: Cycloheximide Chase Assay for PD-L1 Protein Stability
Treatment: Treat cells with cycloheximide (100 μg/mL) to inhibit protein synthesis. Harvest cells at various time points (0, 1, 2, 4, 8 hours) [49].
Western Blot Analysis: Lyse cells and quantify PD-L1 protein levels by Western blotting. Normalize to loading controls (e.g., GAPDH, β-actin) [49].
Half-life Calculation: Quantify band intensities using densitometry software. Plot relative PD-L1 levels versus time and calculate half-life using exponential decay models [49].
Functional T-cell Activation Assays
Protocol: Co-culture Assay for T-cell Mediated Cytotoxicity
T-cell Isolation and Activation: Isolate human peripheral blood mononuclear cells (PBMCs) from healthy donors by density gradient centrifugation. Isolate CD8+ T cells using magnetic bead-based negative selection. Activate T cells with anti-CD3/CD28 antibodies (1 μg/mL each) for 3 days in RPMI-1640 medium with 10% FBS and 100 U/mL IL-2 [12].
Tumor Cell Preparation: Culture tumor cells expressing PD-L1 and treat with E3 ligase agonists, DUB inhibitors, or vehicle control for 24 hours. Label tumor cells with Calcein-AM (5 μM) for 30 minutes at 37°C [12].
Co-culture Assay: Seed labeled tumor cells (1×10^4 cells/well) in 96-well plates. Add activated CD8+ T cells at various effector:target ratios (5:1 to 20:1). Co-culture for 4-6 hours at 37°C [12].
Cytotoxicity Measurement: Measure fluorescence release in supernatant using a plate reader. Calculate specific lysis using the formula: (Experimental release - Spontaneous release) / (Maximum release - Spontaneous release) × 100% [12].
In Vivo Radiation-Immunotherapy Combination Studies
Protocol: Preclinical Evaluation of Ubiquitin-Targeting Agents with Radiotherapy
Animal Model Establishment: Implant syngeneic tumor cells (e.g., MC38, CT26) subcutaneously into the flanks of 6-8 week old immunocompetent mice. Randomize mice into treatment groups when tumors reach 100-150 mm³ [55].
Treatment Protocol:
- Group 1: Vehicle control
- Group 2: Radiotherapy alone (e.g., 2-8 Gy × 5 fractions)
- Group 3: Ubiquitin-targeting agent alone (e.g., PROTAC, E3 ligase modulator, DUB inhibitor)
- Group 4: Combination therapy
- Group 5: Combination therapy + anti-PD-1/PD-L1 antibody (200 μg, IP, twice weekly) [55]
Tumor Monitoring and Immune Profiling: Measure tumor dimensions 2-3 times weekly using calipers. Calculate volume as (length × width²)/2. At endpoint, harvest tumors for flow cytometry analysis of immune cell infiltration (CD8+ T cells, Tregs, macrophages) and IHC staining for PD-L1 expression and DNA damage markers (γH2AX) [55].
Abscopal Effect Assessment: In bilateral tumor models, treat the primary tumor and monitor response in distant, non-irradiated tumors to evaluate systemic immune effects [55].
Signaling Pathways and Molecular Interactions
Diagram 1: Ubiquitin Signaling in Therapy Response and Targeting Strategies. This diagram illustrates how radiation-induced DNA damage activates E3 ligases, leading to different ubiquitination outcomes that influence therapy response. K48-linked ubiquitination can either promote immune activation through degradation of immunosuppressive proteins or contribute to immune evasion by stabilizing PD-L1. K63-linked ubiquitination enhances DNA repair, leading to radioresistance. Targeted interventions including PROTACs, DUB inhibitors, and E3 modulators can manipulate these pathways to improve therapeutic outcomes.
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Research Tools for Investigating Ubiquitin Pathways in Therapy Combinations
| Research Tool | Specific Examples | Application/Function | Experimental Context |
|---|---|---|---|
| PROTAC Platforms | RT-PROTAC (BRD4/2 degradation), EGFR-directed PROTAC (β-TrCP substrate degradation) | Tumor-specific protein degradation activated by radiation or tumor context | Breast cancer, lung cancer, HNSCC models |
| E3 Ligase Modulators | HOIPIN-8 (RNF31 inhibitor), SPOP agonists | Target specific E3 ligases to modulate substrate stability | FOXP3 degradation in Tregs, PD-L1 destabilization |
| DUB Inhibitors | P5091 (USP7 inhibitor), USP14 inhibitors | Stabilize ubiquitinated proteins by preventing deubiquitination | Multiple myeloma, glioma, immune activation |
| Ubiquitination Assay Systems | MG132 proteasome inhibitor, N-ethylmaleimide (DUB inhibitor) | Stabilize ubiquitinated proteins for detection | PD-L1 ubiquitination studies, protein half-life assays |
| Immune Monitoring Tools | CD8+ T cell isolation kits, PD-1/PD-L1 blockade antibodies, cytokine detection arrays | Assess immune cell function and checkpoint inhibition | Co-culture assays, in vivo immune profiling |
| Radiation Platforms | Clinical linear accelerators, FLASH radiotherapy systems | Deliver conventional or ultra-high dose rate radiation | In vivo radiation therapy models |
The strategic combination of ubiquitin-targeting agents with radiotherapy and immunotherapy represents a paradigm shift in cancer treatment, moving beyond conventional approaches to address the dynamic adaptability of tumors. The ubiquitin system's central role in regulating DNA repair, metabolic adaptation, and immune evasion makes it an ideal target for enhancing therapeutic efficacy [55] [28]. Future developments in this field will likely focus on several key areas: First, the refinement of biomarker-guided approaches to identify patients most likely to benefit from specific ubiquitin-targeting combinations, potentially through assessment of tumor E3 ligase/DUB expression profiles or ubiquitin chain topology signatures [55]. Second, the advancement of conditional activation technologies, such as radiation-activated PROTACs, to achieve unprecedented spatial and temporal precision in target degradation [55]. Third, the integration of emerging technologies including AI-driven analytics to optimize combination strategies and predict treatment responses [61]. Finally, addressing the challenges of therapeutic redundancy, on-target toxicity, and adaptive resistance will be crucial for successful clinical translation [55]. As our understanding of ubiquitin signaling networks in the TME continues to deepen, so too will our ability to strategically manipulate this system to overcome therapy resistance and improve patient outcomes across multiple cancer types.
The ubiquitin system, a crucial post-translational regulatory mechanism, governs virtually all cellular processes in eukaryotic cells. Its dysregulation is a hallmark of cancer, influencing tumorigenesis, progression, and therapy resistance through complex rewiring of the tumor microenvironment (TME). This whitepaper explores the convergence of ubiquitin biology and artificial intelligence (AI) as a transformative paradigm in oncology drug discovery. We detail how AI-driven approaches are accelerating the identification of ubiquitin-related therapeutic targets, the design of novel modulators—including ubiquitin variants—and the stratification of patients for precision therapy. Supported by structured data, detailed experimental protocols, and pathway visualizations, this review provides a technical guide for researchers and drug development professionals seeking to leverage these emerging technologies for breakthrough cancer therapeutics.
Ubiquitination is a dynamic and reversible post-translational modification involving a cascade of E1 (activating), E2 (conjugating), and E3 (ligase) enzymes that attach ubiquitin to substrate proteins, with reversal mediated by deubiquitinases (DUBs) [62]. This system regulates protein stability, localization, and activity, thereby controlling fundamental processes such as cell cycle, DNA repair, metabolism, and immune responses [6] [62]. The TME is a complex ecosystem where cancer cells interact with immune cells, fibroblasts, and signaling molecules. Ubiquitination has emerged as a master regulator of this landscape, modulating immune checkpoint expression, antigen presentation, and cytokine signaling [63] [61].
Dysregulation of ubiquitin signaling contributes to tumor immune evasion and therapy resistance. For instance, the ubiquitin-proteasome system tightly regulates the stability of key immune checkpoints like PD-L1, presenting a therapeutic opportunity [61]. The functional outcome of ubiquitination is exquisitely dependent on the topology of ubiquitin chains. For example, K48-linked chains typically target proteins for proteasomal degradation, whereas K63-linked chains and monoubiquitination often serve non-proteolytic roles in signaling and trafficking [55]. Understanding this "ubiquitin code" within the context of the TME is critical for developing novel anti-cancer strategies [55] [62].
Molecular Mechanisms of Ubiquitination in Cancer
Ubiquitination orchestrates cancer hallmarks through distinct chain topologies and substrate modifications. The following table summarizes the key linkages and their roles in cancer biology.
Table 1: Ubiquitin Chain Linkages and Their Roles in Cancer
| Linkage Type | Primary Function | Role in Cancer & TME | Key Examples |
|---|---|---|---|
| K48-linked | Proteasomal degradation | Contextual duality in tumor suppression/oncogenesis [55]. | FBXW7 degrades SOX9 (radiosensitizer) or p53 (radioresistor) [55]. |
| K63-linked | Non-proteolytic signaling | Promotes survival, DNA repair, and immune evasion [55]. | TRAF4 activates JNK/c-Jun for anti-apoptotic Bcl-xL expression [55]. |
| K27/K29-linked | Atypical signaling | Activates DNA damage response in resistant cancers [55]. | RNF126 ubiquitinates MRE11 to activate ATM-CHK1 axis in TNBC [55]. |
| Monoubiquitination | Alters activity/localization | Regulates DNA damage response and chromatin dynamics [55]. | UBE2T/RNF8 monoubiquitinates H2AX for damage detection in HCC [55]. |
Ubiquitination in Immune Regulation
The ubiquitin system is a pivotal regulator of anti-tumor immunity. E3 ligases and DUBs control the stability of PD-L1 on cancer cells and PD-1 on T cells, directly influencing the efficacy of immune checkpoint blockade therapy [61]. For example, the small molecule PIK-93 has been shown to enhance PD-L1 ubiquitination and degradation, thereby improving T-cell activation [64]. Furthermore, ubiquitination modulates key immune signaling pathways, such as the cGAS-STING pathway. TRIM21, for instance, promotes the K48-linked degradation of VDAC2, inhibiting mitochondrial DNA release and cGAS-STING activation, thereby suppressing anti-tumor immunity in nasopharyngeal carcinoma [55]. Conversely, inhibition of the DUB USP14 leads to accumulation of K63-ubiquitinated IRF3, which triggers STING-dependent type I interferon responses and can synergize with radiotherapy [55].
AI-Driven Approaches in Ubiquitin-Targeted Drug Discovery
Traditional drug discovery is hampered by lengthy timelines, high costs, and high failure rates [65]. AI is transforming this landscape by enhancing target identification, virtual screening, and lead optimization, offering dramatic improvements in speed and predictive power [64] [65].
AI for Target Identification and Ubiquitination Site Prediction
AI models, particularly deep learning (DL), excel at analyzing complex multi-omics datasets to identify novel oncogenic vulnerabilities and ubiquitination-related targets [65]. For example, integrative multi-omics analysis of lung adenocarcinoma (LUAD) identified 17 hub ubiquitination regulators (UBRs) from protein-protein interaction networks, whose expression is detrimental to patient survival [63]. Beyond target identification, ML models are crucial for predicting ubiquitination sites (Ubi-sites) on proteins. DL approaches that use both raw amino acid sequences and hand-crafted features have achieved performance metrics exceeding 0.9 in F1-score and 0.87 in precision, outperforming conventional ML methods [66]. These models help decipher the ubiquitin code and identify novel substrate targets.
Table 2: Performance of Machine Learning Models in Ubiquitination Site Prediction
| Model Category | Example Algorithms | Key Features | Reported Performance (Best) | Reference |
|---|---|---|---|---|
| Conventional ML | Random Forest (RF), Support Vector Machine (SVM) | Physicochemical properties (PCPs), Amino Acid Composition (AAC) | AUC: 0.80 (UbPred tool on yeast) [66]. | [66] |
| Deep Learning (DL) | Convolutional Neural Networks (CNNs) | Raw amino acid sequences, sequence profiles | AUC: 0.99 (DeepUni) [66]. | [66] |
| Hybrid DL | Multimodal Deep Architecture | Combination of raw sequences and hand-crafted PCPs | F1-score: 0.902, Accuracy: 0.8198 [66]. | [66] |
AI-Accelerated Virtual Screening and De Novo Design
Structure-based virtual screening is a key tool in early drug discovery. AI-accelerated platforms, such as the open-source OpenVS platform, now enable the screening of multi-billion compound libraries in days rather than years [67]. These platforms use active learning to train target-specific neural networks that triage the most promising compounds for more expensive physics-based docking calculations, dramatically improving efficiency [67]. For de novo design, generative models like Variational Autoencoders (VAEs) and Generative Adversarial Networks (GANs) can create novel, drug-like molecular structures with optimized properties for specific biological targets, such as E3 ligases or DUBs [64]. Reinforcement learning (RL) further fine-tunes these AI-generated compounds toward desired therapeutic goals [64].
Experimental Protocols for Validation
The transition from in silico prediction to biological validation requires rigorous experimental workflows.
Protocol: AI-Guided Virtual Screening for a Ubiquitin Ligase Inhibitor
This protocol is adapted from a study that successfully discovered hits for the ubiquitin ligase target KLHDC2 using the RosettaVS method and the OpenVS platform [67].
- Target Preparation (Day 1): Obtain a high-resolution crystal structure of the target E3 ubiquitin ligase (e.g., KLHDC2). Prepare the protein structure by adding hydrogen atoms, assigning protonation states, and defining the binding pocket.
- Library Curation (Day 1): Select an ultra-large chemical library for screening (e.g., multi-billion compound libraries like ZINC20).
- AI-Accelerated Docking (Days 2-4):
- Utilize a platform like OpenVS that integrates active learning.
- Initial Triage (VSX mode): Perform rapid, initial docking of the entire library using a fast scoring function to sample billions of poses.
- Neural Network Training: Simultaneously train a target-specific neural network on the docking results to predict binding affinity.
- Focused Screening (VSH mode): Use the trained model to select a subset of top-ranking compounds (e.g., thousands) for high-precision docking that includes full receptor side-chain flexibility.
- Hit Selection and In Vitro Testing (Days 5-7): Select the top 100-500 compounds based on the final ranking for experimental validation. Procure compounds and test their binding affinity (e.g., using Surface Plasmon Resonance) and functional activity in a ubiquitination assay. The cited study achieved a 14% hit rate for KLHDC2 with single-digit micromolar affinity [67].
- Structural Validation: For top hits, solve a co-crystal structure of the ligand bound to the target to confirm the predicted binding pose, as was done for the KLHDC2 hit [67].
Protocol: Functional Validation of a Ubiquitin RegulatorIn Vivo
This protocol is based on the functional characterization of the E3 ligase FBXO8 in Acute Lymphoblastic Leukemia (ALL) models [68].
- Knockdown in Cell Lines: Transduce relevant cancer cell lines (e.g., ALL cell lines) with lentiviral vectors expressing shRNAs targeting the UBR of interest (e.g., FBXO8) or a non-targeting control shRNA.
- In Vitro Functional Assays:
- Proliferation: Measure cell proliferation over 3-5 days using assays like CCK-8 or MTT. FBXO8 knockdown significantly enhanced ALL cell proliferation [68].
- Apoptosis: Induce apoptosis (e.g., with serum starvation or chemotherapeutic agents) and quantify the percentage of apoptotic cells using flow cytometry with Annexin V/propidium iodide staining. FBXO8 knockdown suppressed apoptosis [68].
- In Vivo Tumorigenesis Model:
- Xenograft Establishment: Subcutaneously inject FBXO8-knockdown cells and control cells into immunodeficient mice (e.g., NOD/SCID).
- Tumor Monitoring: Measure tumor volume twice weekly for 4-6 weeks.
- Endpoint Analysis: Harvest tumors and perform immunohistochemistry for proliferation (Ki-67) and apoptosis (TUNEL) markers. The study on FBXO8 showed that knockdown led to increased tumor growth, reduced apoptosis, and diminished survival rates in mice [68].
Signaling Pathways and Therapeutic Targeting
The following diagram illustrates how ubiquitination and AI-driven discovery intersect to regulate key pathways in the Tumor microenvironment.
Diagram 1: AI and Ubiquitin Signaling in the TME. This map shows how AI identifies ubiquitin regulators and designs inhibitors, which target ubiquitin-mediated control of immune and DNA repair pathways to overcome therapy resistance and immune evasion in the TME.
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Reagents for Ubiquitin and AI-Driven Cancer Research
| Reagent / Tool | Function / Application | Example Use Case |
|---|---|---|
| OpenVS Platform | An open-source, AI-accelerated virtual screening platform for ultra-large compound libraries [67]. | Screening for small-molecule inhibitors of E3 ligases like KLHDC2 [67]. |
| UB_risk Score | A scoring system based on hub UBR expression to evaluate individual patient ubiquitination status [63]. | Stratifying LUAD patients for immunotherapy response; low-score patients show better advantage [63]. |
| PROTACs (Proteolysis-Targeting Chimeras) | Bifunctional molecules that recruit E3 ligases to target proteins for degradation [55]. | EGFR-directed PROTACs degrade β-TrCP substrates to suppress DNA repair in lung cancer [55]. |
| Mass Spectrometry with Ubiquitin Remnant Antibodies | Enrichment and identification of ubiquitination sites from complex protein samples [66]. | High-throughput mapping of Ubi-sites for training and validating ML prediction models [66]. |
| shRNA/sgRNA Libraries | For targeted knockdown or knockout of ubiquitination-related genes (URGs) in functional studies. | Validating the role of FBXO8 as a tumor suppressor in ALL models [68]. |
The integration of ubiquitin biology and AI is forging a new frontier in precision oncology. AI is no longer just an auxiliary tool but is becoming central to deciphering the complexity of the ubiquitin code, identifying novel drug targets, and designing precise chemical modulators at an unprecedented pace. The development of biomarkers like the UB_risk score highlights a move towards patient stratification based on ubiquitination network status, which could significantly improve the efficacy of immunotherapies and targeted treatments [63]. Future efforts will focus on refining multi-omics integration, developing more sophisticated generative AI models for bifunctional degraders like PROTACs, and validating these approaches in complex preclinical models that faithfully recapitulate the human TME. For researchers, mastering the confluence of these technologies is essential for developing the next generation of cancer therapeutics.
The ubiquitin-proteasome system (UPS) has emerged as a critical regulatory network in oncology, governing the controlled degradation of cellular proteins and fundamentally shaping the tumor microenvironment (TME). Ubiquitination, a post-translational modification, directs protein fate through a sophisticated enzymatic cascade involving E1 activating, E2 conjugating, and E3 ligase enzymes. This process determines the stability, function, and trafficking of key proteins that regulate immune cell function, tumor cell survival, and drug resistance. The clinical translation of strategies targeting the UPS represents a paradigm shift in cancer therapeutics, moving beyond traditional inhibition to targeted protein degradation. This whitepaper provides a comprehensive technical analysis of the current clinical trial landscape for FDA-approved agents and investigational therapies, with particular emphasis on how ubiquitination signaling influences therapeutic efficacy and resistance mechanisms within the TME. The integration of UPS-targeting approaches with established modalities like immune checkpoint inhibitors (ICIs) and kinase-targeted therapies is creating novel opportunities to overcome the immunosuppressive TME and improve patient outcomes [61] [69].
FDA-Approved Oncology Agents (2025)
The first three quarters of 2025 have witnessed significant regulatory advancements across multiple cancer types, with approvals encompassing novel molecular targets, new drug modalities, and enhanced delivery systems. These approvals reflect a continued trend toward precision medicine and patient-centric dosing options.
First-in-Class Agents and New Molecular Targets
Table 1: Novel FDA-Approved Oncology Agents (July-September 2025)
| Generic Name (Brand) | Target/MOA | Indication | Key Trial Data |
|---|---|---|---|
| Dordaviprone (Modeyso) | First-in-class protease activator; inhibits D2/3 dopamine receptor & activates mitochondrial ClpP [70] | H3 K27M-mutated diffuse midline glioma (progressed after prior therapy) | Accelerated approval for patients ≥1 year; first FDA-approved therapy specifically for H3 K27M-mutated DMG [70] [71] |
| Zongertinib (Hernexeos) | HER2 tyrosine kinase inhibitor (TKI) [70] | HER2-mutated non-squamous NSCLC (post-prior therapy) | Accelerated approval; "very favorable safety profile"; oral administration; effective against broad HER2 mutations [70] [71] |
| Sunvozertinib (Zegfrovy) | EGFR TKI targeting exon 20 insertion mutations [70] | EGFR exon 20-mutated NSCLC (post-chemotherapy) | Accelerated approval; activity against T790M resistance mutation [70] |
| Imlunestrant (Inluriyo) | Selective estrogen receptor degrader (SERD) [70] | ER-positive, HER2-negative, ESR1-mutated advanced/metastatic breast cancer (post-endocrine therapy) | Approved based on Phase III EMBER-3 trial [70] [71] |
| Linvoseltamab-gcpt (Lynozyfic) | BCMA x CD3 bispecific T-cell engager [70] | Relapsed/refractory multiple myeloma (≥4 prior lines) | Accelerated approval; third BCMA-targeting bispecific approved [70] |
The latter part of 2025 introduced additional significant approvals. In October, the menin inhibitor revumenib (Revuforj) was approved for relapsed/refractory NPM1-mutant acute myeloid leukemia (AML), supported by the AUGMENT-101 trial [72] [71]. November brought the traditional approval of tarlatamab-dlle (Imdelltra) for extensive-stage small cell lung cancer (ES-SCLC) post-platinum therapy and the accelerated approval of another HER2 TKI, sevabertinib (Hyrnuo), for HER2-mutant NSCLC [71].
Advanced Formulations and Delivery Methods
Recent approvals have also focused on improving patient convenience, tolerability, and drug exposure through novel formulations and delivery systems:
- Gemcitabine Intravesical System (Inlexzo): A continuous delivery system for non-muscle invasive bladder cancer providing sustained intravesical chemotherapy, overcoming limitations of bolus instillation [70] [71].
- Selumetinib (KOSELUGO) Granules: New granule formulation allows administration to pediatric neurofibromatosis type 1 patients as young as 1 year by mixing with food [70] [71].
- Subcutaneous Pembrolizumab (Keytruda Qlex): Hyaluronidase-facilitated subcutaneous injection approved as an alternative to intravenous infusion across all adult and pediatric (≥12 years) solid tumor indications for pembrolizumab, significantly reducing administration time [70] [71].
Investigational Therapies and Clinical Trial Pipeline
The oncology drug development pipeline is robust with investigational agents employing novel mechanisms to target oncogenic drivers and modulate the TME. Key emerging classes include protein degradation technologies, next-generation immunotherapies, and novel small molecule inhibitors.
Protein-Targeting Chimerics (PROTACs)
PROTACs represent a revolutionary class of bifunctional molecules that harness the UPS to achieve targeted protein degradation.
Table 2: Select PROTAC Degraders in Advanced Clinical Trials (2025)
| PROTAC (Company) | Target | Indication | Phase | Key Updates |
|---|---|---|---|---|
| Vepdegestrant (ARV-471) (Arvinas/Pfizer) | Estrogen Receptor (ER) | ER+/HER2- breast cancer | Phase III | Met primary PFS endpoint in ESR1-mutant pts in VERITAC-2; regulatory submission planned H2 2025 [69] |
| BMS-986365 (CC-94676) (Bristol Myers Squibb) | Androgen Receptor (AR) | mCRPC | Phase III | First AR-targeting PROTAC in Phase III; ~100x more potent than enzalutamide in preclinical models [69] |
| BGB-16673 (BeiGene) | Bruton's Tyrosine Kinase (BTK) | R/R B-cell malignancies | Phase III | BTK-degrading PROTAC; potential option for patients with resistance to covalent BTK inhibitors [69] |
| NX-1607 (Nurix Therapeutics) | Casitas B-lineage lymphoma proto-oncogene B (CBL-B) E3 ligase [73] | Advanced solid tumors | Phase I | Oral CBL-B inhibitor; demonstrates immune activation & TME remodeling; data presented at SITC 2025 [73] |
Novel Immuno-Oncology Targets
Research continues to identify and validate new immunomodulatory targets within the TME. Triggering Receptor Expressed on Myeloid Cells 2 (TREM2) has emerged as a key regulator of immunosuppressive tumor-associated macrophages (TAMs) and myeloid-derived suppressor cells (MDSCs) [74]. TREM2 signaling promotes an immunosuppressive TME through modulation of cellular metabolism, antigen presentation, and cytokine secretion (e.g., IL-10, TGF-β) [74]. Preclinical studies demonstrate that TREM2 blockade can reprogram the TME, enhance T-cell infiltration, and synergize with PD-1/PD-L1 checkpoint inhibitors [74]. Several TREM2-targeting agents are in early-stage development.
Other promising investigational immunotherapies include:
- Ivonescimab: A novel PD-1/VEGF bispecific antibody. Phase III HARMONi-A trial showed improved overall survival combined with chemotherapy versus chemotherapy alone in EGFR-mutated NSCLC post-targeted therapy [75].
- Ficerafusp alfa (BCA101): An EGFR/TGF-β-trapping bifunctional antibody granted Breakthrough Therapy Designation for HPV-negative head and neck squamous cell carcinoma (HNSCC) in combination with pembrolizumab [72].
- Sonrotoclax (BGB-11417): A BCL2 inhibitor with Breakthrough Therapy Designation for relapsed/refractory mantle cell lymphoma post-BTK inhibitor and anti-CD20 therapy [72].
Experimental Protocols for Key Mechanistic Studies
Understanding the mechanism of action for UPS-targeting therapies requires specialized experimental approaches. Below are detailed protocols for key assays.
Protocol: Target Engagement and Ubiquitination Assay for PROTACs
Objective: To confirm PROTAC-induced target protein ubiquitination and degradation in tumor cells. Background: This protocol validates the core mechanism of PROTACs, which recruit an E3 ubiquitin ligase to the protein of interest (POI), leading to its polyubiquitination and subsequent proteasomal degradation [69].
Materials:
- Research Reagent Solutions:
- Cell line relevant to target indication (e.g., breast cancer line for ER-targeting PROTACs)
- PROTAC molecule and inactive analog control
- Proteasome inhibitor (e.g., MG132)
- Lysis Buffer: RIPA buffer supplemented with protease and deubiquitinase inhibitors
- Antibodies: Anti-target protein (e.g., anti-ERα), anti-ubiquitin, anti-E3 ligase (e.g., anti-VHL or anti-CRBN), and species-specific HRP-conjugated secondary antibodies
- Protein A/G magnetic beads
- SDS-PAGE and Western Blotting system
- Cycloheximide (to block new protein synthesis)
Methodology:
- Cell Treatment: Seed cells in 6-well plates. At ~70% confluence, treat with:
- Vehicle control (DMSO)
- PROTAC at varying concentrations (e.g., 1 nM - 1 µM)
- Inactive control compound
- PROTAC + MG132 (10 µM) for the final 6 hours of treatment to block degradation.
- For degradation kinetics, pre-treat with cycloheximide (100 µg/mL) for 30 minutes before adding PROTAC.
Protein Extraction: After treatment (e.g., 4, 8, 24 hours), lyse cells in ice-cold lysis buffer. Centrifuge at 14,000 x g for 15 minutes at 4°C. Collect supernatant and determine protein concentration.
Immunoprecipitation (IP): Incubate 500 µg of total protein with 2 µg of anti-target protein antibody overnight at 4°C. Add protein A/G beads and incubate for 2 hours. Wash beads 3x with lysis buffer.
Western Blot Analysis:
- Elute proteins from beads with Laemmli buffer.
- Resolve proteins by SDS-PAGE and transfer to PVDF membrane.
- Probe membranes with:
- Anti-ubiquitin antibody to detect ubiquitinated POI.
- Anti-target protein antibody to assess total POI levels and IP efficiency.
- Anti-E3 ligase antibody to confirm recruitment to the POI complex.
- Use appropriate secondary antibodies and chemiluminescence for detection.
Data Interpretation: Successful PROTAC activity is indicated by a concentration-dependent increase in high-molecular-weight smearing (polyubiquitinated species) of the POI in the anti-ubiquitin blot, and a corresponding decrease in total POI levels in the whole-cell lysate blot. This degradation should be rescued by co-treatment with MG132. Recruitment of the E3 ligase should be evident in the IP complex from PROTAC-treated but not control-treated cells [69].
Protocol: Tumor Microenvironment Immune Profiling via Flow Cytometry
Objective: To evaluate immune cell composition and activation状态 in the TME following therapy with immune-modulating agents (e.g., CBL-B inhibitors, ICIs). Background: This protocol is crucial for assessing the pharmacodynamic effects of therapies designed to remodel the immunosuppressive TME, such as the CBL-B inhibitor NX-1607 [73].
Materials:
- Research Reagent Solutions:
- Single-cell suspension from dissociated tumor tissue
- Fluorescently conjugated antibodies: Anti-mouse/human CD45, CD3, CD4, CD8, CD19, CD11b, F4/80, Ly6G, Ly6C, CD206, MHC-II, PD-1, Ki67, ICOS
- Viability dye (e.g., Zombie NIR)
- Cell staining buffer (PBS + 2% FBS)
- Intracellular fixation and permeabilization buffer set
- Flow cytometer with ≥12 colors
Methodology:
- Tumor Processing: Generate single-cell suspensions from harvested tumors using a combination of mechanical dissociation and enzymatic digestion (e.g., collagenase/DNase). Filter through a 70-µm cell strainer. Lyse red blood cells if necessary.
Cell Staining:
- Viability and Surface Staining: Resuspend cells in staining buffer. Incubate with viability dye for 15 minutes in the dark. Wash. Incubate with a pre-titrated master mix of surface antigen antibodies for 30 minutes at 4°C. Wash twice.
- Intracellular Staining (for Ki67): Fix and permeabilize cells using the commercial buffer set according to the manufacturer's instructions. Incubate with anti-Ki67 antibody for 30 minutes at 4°C. Wash and resuspend in staining buffer for acquisition.
Flow Cytometric Acquisition: Acquire data on a flow cytometer, collecting at least 50,000 live CD45+ events per sample. Include fluorescence-minus-one (FMO) controls for accurate gating.
Data Analysis: Use flow cytometry analysis software (e.g., FlowJo). Gate on live, single cells. Identify major immune populations:
- T cells: CD45+CD3+; subset into CD8+ cytotoxic T cells and CD4+ helper T cells.
- B cells: CD45+CD19+.
- Myeloid cells: CD45+CD11b+; subset into TAMs (CD11b+F4/80+), monocytic MDSCs (M-MDSCs: CD11b+Ly6G-Ly6Chi), and granulocytic MDSCs (G-MDSCs: CD11b+Ly6G+Ly6Clo).
- Assess activation states using markers like PD-1, Ki67, and ICOS on T cells, and M1/M2 polarization markers (MHC-II, CD206) on TAMs.
Data Interpretation: A successful TME-reprogramming therapy, like a CBL-B inhibitor, should show an increase in the CD8+/Treg ratio and an increase in activated (ICOS+, Ki67+) CD8+ T cells. A shift in TAMs from an M2-like (CD206hi) to an M1-like (MHC-IIhi) phenotype is also a positive indicator of immune activation [73] [74].
Signaling Pathways and Conceptual Workflows
Ubiquitin-Mediated Regulation of PD-L1 in the Tumor Microenvironment
The stability of PD-L1, the critical ligand for the immune checkpoint PD-1, is heavily regulated by ubiquitination. This pathway offers multiple nodal points for therapeutic intervention to modulate the PD-1/PD-L1 axis and enhance anti-tumor immunity [61].
Diagram 1: Ubiquitin-Mediated Regulation of PD-L1. Multiple E3 ligases (e.g., SPOP, c-CBL) can promote the ubiquitination and proteasomal degradation of PD-L1, potentially enhancing anti-tumor immunity. Conversely, deubiquitinating enzymes (DUBs) can stabilize PD-L1, contributing to immune evasion. Investigational PROTAC molecules are designed to hijack this system by co-opting E3 ligases to force the degradation of PD-L1 [61].
CBL-B Inhibition as a Novel Immune Checkpoint
The E3 ubiquitin ligase CBL-B functions as an intracellular checkpoint in T cells, and its inhibition represents a novel mechanism to enhance anti-tumor immunity, potentially overcoming resistance to PD-1/PD-L1 blockade [73].
Diagram 2: Mechanism of CBL-B Checkpoint Inhibition. (Top) In normal T-cell signaling, CBL-B is activated by the T-cell receptor (TCR) and ubiquitinates key signaling proteins, attenuating the immune response and preventing autoimmunity. (Bottom) CBL-B inhibitors block this ubiquitination, leading to enhanced and sustained TCR and CD28 co-stimulation. This lowers the threshold for T-cell activation, resulting in potent anti-tumor activity, even in the absence of co-stimulation, and can help reverse T-cell exhaustion [73].
The Scientist's Toolkit: Key Research Reagents
Table 3: Essential Reagents for Investigating Ubiquitination in Cancer Therapy
| Reagent Category | Specific Examples | Research Function |
|---|---|---|
| E3 Ligase Modulators | CBL-B inhibitors (NX-1607); PROTACs recruiting CRBN/VHL | To experimentally manipulate the UPS; study loss/gain-of-function of specific E3 ligases; validate on-target drug effects [73] [69]. |
| Proteasome Inhibitors | MG132, Bortezomib, Carfilzomib | To block the proteasome, allowing accumulation of ubiquitinated proteins and distinguishing degradation-dependent from -independent effects in mechanistic studies [69]. |
| Ubiquitination Assay Kits | Ubiquitin Remnant Motif Kits; TUBE (Tandem Ubiquitin Binding Entity) reagents | To enrich, detect, and quantify protein ubiquitination via Western blot or mass spectrometry. |
| Immune Profiling Panels | Fluorochrome-conjugated antibodies against CD45, CD3, CD8, CD4, FoxP3, CD11b, F4/80, PD-1, TIM-3, LAG-3, Ki67, ICOS | To characterize immune cell populations, activation states, and exhaustion profiles in the TME by flow cytometry [73] [74]. |
| Phospho-Specific Antibodies | Anti-pSYK, anti-pAKT, anti-pERK, anti-pHS1 | To monitor proximal signaling events downstream of key receptors (e.g., TCR, growth factor receptors) and confirm target engagement of kinase inhibitors and upstream modulators [73]. |
The clinical oncology landscape is being reshaped by a deeper understanding of the ubiquitin-proteasome system and its profound influence on the tumor microenvironment. The advent of FDA-approved degraders like SERDs and the advanced clinical development of PROTAC technology herald a new era of therapeutic intervention that moves beyond simple inhibition to complete elimination of pathogenic proteins. Simultaneously, the targeting of intracellular immune checkpoints like the E3 ligase CBL-B and TME-modulating targets like TREM2 represents a promising frontier for overcoming resistance to existing immunotherapies. For researchers and drug developers, success in this complex field requires the integration of sophisticated mechanistic tools—from detailed ubiquitination assays to comprehensive immune monitoring—to fully elucidate drug mechanisms and validate novel therapeutic hypotheses. The continued translation of ubiquitination-focused research into clinical practice holds significant potential for delivering more effective and durable treatments for cancer patients.
Overcoming Therapeutic Hurdles: Resistance, Specificity, and Toxicity Challenges
The ubiquitin-proteasome system (UPS) represents a crucial regulatory network in cellular homeostasis, with E3 ubiquitin ligases serving as the pivotal determinants of substrate specificity. Within the tumor microenvironment, cancer cells develop resistance to targeted therapies through sophisticated mechanisms involving E3 ligase mutations and activation of compensatory pathways. This technical review examines the molecular underpinnings of these resistance mechanisms, highlighting the complex interplay between genetic alterations in E3 ligases, tumor cell adaptation, and the development of novel therapeutic strategies to overcome treatment resistance. We synthesize current understanding of how tumors exploit the ubiquitin code to bypass targeted interventions and provide experimental frameworks for investigating these pathways in preclinical models.
E3 ubiquitin ligases constitute a large family of enzymes that mediate the transfer of ubiquitin to specific substrate proteins, thereby determining their stability, localization, and function. With approximately 600 members in the human genome, E3 ligases are classified into three major groups based on structural domains and mechanism of ubiquitin transfer: Really Interesting New Gene (RING), Homology to E6AP C-terminus (HECT), and RING-in-Between-RING (RBR) [76] [10]. The RING-E3 class is the most prevalent and extensively researched, functioning as a scaffold that brings E2 enzymes into proximity with substrate proteins to promote ubiquitin transfer [76]. Through their substrate specificity, E3 ligases regulate virtually all cellular processes, including cell cycle progression, DNA damage repair, apoptosis, and metabolic signaling—pathways frequently dysregulated in cancer [10] [77].
The ubiquitination process involves a sequential enzymatic cascade: ubiquitin is initially activated by an E1 activating enzyme, transferred to an E2 conjugating enzyme, and finally delivered to the target protein by an E3 ligase [76] [10]. The functional outcome of ubiquitination depends on the pattern of ubiquitin modification, including monoubiquitination (single ubiquitin attachment), multi-monoubiquitination (multiple single ubiquitins on different lysines), and polyubiquitination (ubiquitin chains linked through specific lysine residues) [10] [77]. Table 1 summarizes the diverse functions associated with different ubiquitin linkage types.
Table 1: Ubiquitin Linkage Types and Their Functional Consequences in Cancer
| Linkage Type | Primary Functions | Role in Cancer Pathways |
|---|---|---|
| K48-linked | Proteasomal degradation | Degradation of tumor suppressors (p53) and cell cycle regulators |
| K63-linked | Signaling complexes, DNA repair, endocytosis | Activation of NF-κB, DNA damage response, kinase activation |
| K11-linked | Cell cycle regulation, endoplasmic reticulum-associated degradation | Mitotic regulation, proliferation signaling |
| K27-linked | Mitochondrial autophagy, immune signaling | Tumor microenvironment modulation |
| K29-linked | Proteasomal degradation, kinase modification | Wnt signaling pathway regulation |
| K33-linked | Kinase inactivation, intracellular trafficking | mTOR signaling modulation |
| K6-linked | DNA damage repair | Genomic instability response |
| M1-linked (Linear) | NF-κB activation, inflammation | Immune cell signaling in tumor microenvironment |
| Monoubiquitination | Endocytosis, DNA repair, histone regulation | Receptor internalization, chromatin remodeling |
In oncogenesis, E3 ligases function as either tumor suppressors or oncogenes, depending on their specific substrates and cellular context [10] [77]. For instance, E3 ligases such as MDM2 promote tumor cell survival by mediating K48-linked ubiquitination and degradation of the tumor suppressor p53 [78]. Conversely, E3 ligases like HUWE1 can exhibit dual roles—depletion of HUWE1 in multiple myeloma shifts ubiquitination patterns, reducing K63-linked polyubiquitination while enhancing K48-linked polyubiquitination, specifically promoting c-Myc degradation and inhibiting cancer cell growth [78]. This functional duality underscores the complex nature of E3 ligases in malignant progression and therapy resistance.
E3 Ligase Mutations as Mechanisms of Resistance
Genetic Alterations and Loss-of-Function Mutations
Cancer cells accumulate genetic alterations in E3 ligases that disrupt their normal regulatory functions, enabling uncontrolled proliferation and survival. These mutations include frameshift mutations, splice site variants, and missense mutations that collectively impair ligase activity, substrate recognition, or protein-protein interactions [78]. In multiple myeloma, genomic studies have revealed a landscape of E3 ligase mutations with varying frequencies across patients, including alterations in HUWE1, RNF114, and other ligases that converge on critical oncogenic pathways [78]. The functional consequence of these mutations is frequently the stabilization of oncoproteins that would normally be targeted for degradation.
A prime example of this mechanism is the mutation of the CRL4CRBN E3 ligase complex, which mediates the therapeutic effects of immunomodulatory drugs (IMiDs) like lenalidomide and pomalidomide in multiple myeloma [78]. Under normal physiological conditions, IMiDs bind CRBN, inducing conformational changes that alter its substrate specificity toward transcription factors IKZF1 and IKZF3, leading to their ubiquitination and degradation [78]. However, mutations in CRBN or associated pathway components can confer resistance to IMiDs by preventing the degradation of these critical targets, thereby maintaining survival signals through IRF4 and c-Myc [78]. This molecular adaptation highlights how specific alterations in E3 ligases can directly drive therapeutic resistance.
Expression Dysregulation and Oncogenic Hijacking
Beyond genetic mutations, cancer cells dysregulate E3 ligase expression through epigenetic mechanisms, transcriptional control, and post-translational modifications. Both overexpression and suppression of specific E3 ligases can promote resistance depending on their normal function. For instance, the E3 ligase TRIM22 functions as a tumor suppressor in breast cancer by targeting the copper chaperone for superoxide dismutase (CCS) for degradation via K27-linked ubiquitination, thereby inhibiting STAT3 signaling [79]. Downregulation of TRIM22 expression in aggressive breast cancers leads to CCS accumulation, enhanced STAT3 phosphorylation, and increased proliferation and invasion [79].
Conversely, overexpression of oncogenic E3 ligases can drive resistance by enhancing the degradation of tumor suppressor proteins. In glioma, TRIM26 stabilizes GPX4 via K63-linked ubiquitination to suppress ferroptosis, a form of iron-dependent cell death, thereby promoting radioresistance [28] [55]. Similarly, in non-small cell lung cancer (NSCLC), FBXW7 can exhibit context-dependent functions—while it typically acts as a tumor suppressor by degrading oncoproteins, in p53-wild type colorectal tumors, it promotes radioresistance by degrading p53 and inhibiting apoptosis [28] [55]. This functional switch underscores the critical influence of tumor genetics and signaling microenvironment on E3 ligase activity in therapy response.
Table 2: E3 Ligase Alterations in Cancer Therapy Resistance
| E3 Ligase | Cancer Type | Alteration Type | Functional Consequence | Therapeutic Resistance |
|---|---|---|---|---|
| CRL4CRBN | Multiple Myeloma | Mutations, reduced expression | Impaired IKZF1/3 degradation | IMiD resistance |
| MDM2 | Various Cancers | Amplification, overexpression | Enhanced p53 degradation | Radiotherapy, chemotherapy |
| TRIM22 | Breast Cancer | Downregulation | CCS stabilization, STAT3 activation | Enhanced proliferation, invasion |
| HUWE1 | Multiple Myeloma | Mutations, expression changes | Altered c-Myc stability | Altered proliferation |
| FBXW7 | Colorectal Cancer | Context-dependent function | p53 degradation | Radioresistance |
| TRIM26 | Glioma | Overexpression | GPX4 stabilization, ferroptosis suppression | Radioresistance |
| RNF125 | Various Cancers | Dysregulated expression | Enhanced oncogene stability | Targeted therapy resistance |
| RNF114 | Colorectal, Gastric | Overexpression | Enhanced proliferation pathways | Chemotherapy resistance |
Compensatory Pathways in Resistance
Bypass Signaling and Pathway Redundancy
When specific E3 ligases are inhibited or mutated, cancer cells frequently activate compensatory pathways that bypass the need for the targeted ligase. This redundancy is particularly evident in the regulation of key oncogenic transcription factors. For example, in multiple myeloma, the CRL4CRBN complex regulates the transcription factors IKZF1 and IKZF3, which subsequently control IRF4 and c-Myc expression [78]. Resistance to IMiDs that target this pathway often coincides with alternative stabilization of c-Myc through other E3 ligases such as HUWE1, which normally regulates c-Myc through balanced K63 and K48 ubiquitination [78]. When CRBN function is compromised, the cell leverages HUWE1-mediated ubiquitination switching to maintain c-Myc stability, thereby sustaining proliferative signals.
This compensatory mechanism extends to DNA damage response pathways, where multiple E3 ligases can regulate similar substrates. In triple-negative breast cancer (TNBC), RNF126 mediates K63-linked ubiquitination to activate the ATR-CHK1 axis, promoting error-prone DNA repair and radioresistance [28] [55]. When RNF126 is inhibited, tumors can exploit alternative E3 ligases like TRAF4, which utilizes K63 modifications to activate the JNK/c-Jun pathway, driving overexpression of anti-apoptotic Bcl-xL in colorectal cancer and MCL-1 in oral cancers [28] [55]. This redundancy in E3 ligase functions enables tumors to maintain essential survival signaling despite therapeutic interventions targeting specific ligases.
Deubiquitinase-Mediated Compensation
The ubiquitination process is dynamically reversible through the action of deubiquitinating enzymes (DUBs), which remove ubiquitin chains from substrate proteins. Cancer cells frequently exploit DUB activity as a compensatory mechanism when E3 ligase function is compromised. The human genome encodes approximately 100 DUBs, categorized into seven subfamilies, with ubiquitin-specific proteases (USPs) representing the largest and most diverse group [80]. These enzymes counterbalance E3 ligase activity, and their upregulation can stabilize proteins that would otherwise be targeted for degradation.
In lung cancer, USP51 upregulation diminishes γH2AX formation and increases CHK1 phosphorylation, conferring cisplatin resistance by ensuring effective cell cycle progression despite DNA damage [80]. Similarly, USP14 stabilizes ALKBH5 to maintain glioblastoma stemness, contributing to therapy resistance [28] [55]. The functional opposition between E3 ligases and DUBs creates a dynamic equilibrium that tumors can manipulate—when E3 ligase activity is compromised, either genetically or therapeutically, corresponding DUBs are often upregulated to stabilize critical oncoproteins, maintaining survival signaling through alternative means.
Ubiquitin Code Plasticity and Signaling Rewiring
Tumors exhibit remarkable plasticity in their manipulation of the ubiquitin code, dynamically reprogramming ubiquitin signaling in response to therapeutic pressure. This rewiring manifests through altered chain formation, with cancer cells strategically manipulating K63-linked chains to stabilize DNA repair factors while concurrently inhibiting K48-mediated degradation of survival proteins [55]. For instance, in nasopharyngeal carcinoma, TRIM21 utilizes K48 ubiquitination to degrade VDAC2, suppressing cGAS/STING-mediated immune surveillance and contributing to immune evasion [28] [55].
This ubiquitin code plasticity extends to metabolic adaptation, where E3 ligases and DUBs collaboratively reprogram cellular metabolism to support survival under stress conditions. In gastric cancer, OTUB1 stabilizes GPX4 to suppress ferroptosis, while in breast cancer, UCHL1 stabilizes HIF-1α to activate the pentose phosphate pathway, enhancing antioxidant defense and conferring radioresistance [28] [80]. The dynamic interplay between different ubiquitin linkages and their modifying enzymes creates a robust, adaptable system that tumors exploit to overcome targeted therapies.
Experimental Approaches for Investigating E3 Ligase Resistance Mechanisms
Functional Genomics and CRISPR Screening
Comprehensive identification of E3 ligase-related resistance mechanisms requires systematic functional genomic approaches. CRISPR-based screens enable genome-wide identification of E3 ligases and DUBs that contribute to therapy resistance when genetically altered.
Protocol 1: CRISPR Screening for E3 Ligase Mediated Resistance
- Design a sgRNA library targeting all known E3 ligase and DUB genes with multiple guides per gene
- Transduce target cancer cells with the sgRNA library at low MOI to ensure single integration
- Treat cells with the therapeutic agent of interest (e.g., targeted therapy, chemotherapy, radiation) for 2-4 weeks
- Harvest genomic DNA from surviving cells and amplify integrated sgRNA sequences
- Sequence amplified products and quantify sgRNA abundance compared to untreated controls
- Validate hits using individual sgRNAs in secondary viability assays
- Mechanistically investigate validated targets through ubiquitination assays and substrate identification
This approach has identified novel radiosensitization targets, such as TRIM21, whose inhibition synergizes effectively with radiotherapy [28]. The power of functional genomics lies in its ability to uncover both known and previously uncharacterized E3 ligases involved in resistance pathways.
Ubiquitination Assays and Substrate Identification
Defining the specific substrates through which E3 ligases mediate resistance is crucial for understanding compensatory pathways. Multiple biochemical approaches can identify and validate E3 ligase substrates.
Protocol 2: In Vitro and In Vivo Ubiquitination Assays In Vitro Ubiquitination Assay:
- Purify recombinant E3 ligase, E2 enzyme, and substrate protein
- Set up reaction with E1 enzyme, ubiquitin, ATP in reaction buffer
- Incubate at 30°C for 1-2 hours
- Stop reaction with SDS loading buffer
- Analyze by Western blot with anti-ubiquitin and substrate-specific antibodies
Co-Immunoprecipitation for In Vivo Ubiquitination:
- Transfect cells with plasmids expressing E3 ligase, substrate, and HA- or MYC-tagged ubiquitin
- Treat cells with proteasome inhibitor (MG132) for 4-6 hours before harvesting
- Lyse cells in RIPA buffer containing protease and deubiquitinase inhibitors
- Immunoprecipitate substrate protein with specific antibody
- Analyze immunoprecipitates by Western blot with anti-HA or anti-MYC antibody to detect ubiquitinated species
For identification of novel substrates, label-free proteomics following E3 ligase perturbation can reveal changes in protein stability. As demonstrated in the study of TRIM22 in breast cancer, this approach identified CCS as a novel substrate degraded via K27-linked ubiquitination [79]. Mass spectrometry analysis of immunoprecipitated proteins can further define the ubiquitination sites, such as the identification of lysine 76 as the critical ubiquitination site on CCS [79].
The Scientist's Toolkit: Key Research Reagents
Table 3: Essential Research Reagents for Investigating E3 Ligase Resistance Mechanisms
| Reagent Category | Specific Examples | Application/Function |
|---|---|---|
| CRISPR Libraries | E3 ligase/DUB-focused sgRNA libraries | Genome-wide screening for resistance genes |
| Ubiquitin Variants | HA-Ub, MYC-Ub, K48-only Ub, K63-only Ub | Detecting specific ubiquitin linkages in assays |
| Proteasome Inhibitors | MG132, Bortezomib, Carfilzomib | Stabilizing ubiquitinated proteins for detection |
| E3 Ligase Inhibitors | Nutlin (MDM2), MLN4924 (NEDD8-activating enzyme) | Specific perturbation of E3 ligase activity |
| DUB Inhibitors | Compounds G5, F6, USP14 inhibitors | Investigating DUB-mediated compensation |
| Ubiquitin Binding Reagents | TUBE (Tandem Ubiquitin Binding Entities) | Enrichment and detection of ubiquitinated proteins |
| Antibody Panels | Anti-K48-Ub, Anti-K63-Ub, Anti-M1-Ub | Distinguishing ubiquitin linkage types |
| PROTAC Molecules | ARV-110, ARV-471 | Targeted protein degradation research tools |
Visualization of E3 Ligase Resistance Mechanisms
The following diagrams illustrate key concepts and pathways discussed in this review, providing visual representations of the complex relationships between E3 ligase mutations, compensatory pathways, and therapeutic resistance.
E3 Ligase Mutation Consequences: This diagram illustrates how E3 ligase mutations initiate multiple compensatory mechanisms that collectively drive therapy resistance.
PROTAC Mechanism: This diagram shows the molecular mechanism of PROTACs, which recruit E3 ligases to target proteins for degradation, overcoming specific resistance mechanisms.
Therapeutic Implications and Future Directions
Targeting Compensatory Networks
Overcoming E3 ligase-mediated resistance requires therapeutic strategies that address the compensatory networks tumors employ. Combination approaches that simultaneously target primary E3 ligases and backup pathways show particular promise. For instance, in tumors with FBXW7 mutations that confer radioresistance through p53 degradation, combined MDM2/FBXW7 co-inhibition prevents compensatory resistance [28]. Similarly, in gliomas where TRIM26 stabilizes GPX4 via K63 ubiquitination to suppress ferroptosis, combining TRIM26 inhibition with ferroptosis inducers presents a synergistic therapeutic opportunity [28].
The development of PROTACs (Proteolysis-Targeting Chimeras) represents a paradigm shift in addressing E3 ligase-related resistance [81]. These bifunctional molecules consist of a ligand that binds to the target protein and another that recruits an E3 ubiquitin ligase, bringing the two into proximity to trigger ubiquitination and subsequent degradation by the 26S proteasome [81]. Since their introduction in 2001, PROTACs have evolved from academic research to clinical trials, with several candidates demonstrating efficacy in treatment-resistant settings [81]. Notably, ARV-110 (for prostate cancer) and ARV-471 (for breast cancer) have shown promising results in clinical trials, even in patients who have developed resistance to conventional therapies [81].
Biomarker-Driven Therapy and Personalized Approaches
The contextual duality of E3 ligase function underscores the necessity for biomarker-guided therapeutic strategies. The same E3 ligase can exert opposing effects in different genetic backgrounds or tissue contexts. For example, FBXW7 promotes radioresistance in p53-wild type colorectal tumors by degrading p53, yet enhances radiosensitivity in non-small cell lung cancer with SOX9 overexpression by destabilizing SOX9 and alleviating p21 repression [28] [55]. This functional switch highlights the critical importance of comprehensive molecular profiling to guide E3-targeted therapies.
Future research directions should focus on mapping the complete E3 ligase-substrate network in different cancer types, understanding contextual E3 ligase functions within specific tumor microenvironments, and developing innovative delivery systems for E3-targeting agents. Nanoparticle-based PROTACs, radiation-responsive PROTAC platforms, and dual-targeting PROTACs represent promising technological advances that may overcome current limitations in bioavailability and tumor-specific targeting [28] [81]. As our understanding of E3 ligase biology deepens, these sophisticated therapeutic approaches will increasingly enable precision targeting of the ubiquitin system to overcome therapy resistance in cancer.
Functional Redundancy and Context-Dependent Roles of Ubiquitin Enzymes
The ubiquitin-proteasome system (UPS) represents a sophisticated post-translational regulatory network that governs virtually all cellular processes through targeted protein degradation and signal modulation. Within the tumor microenvironment, ubiquitin enzymes demonstrate remarkable functional plasticity, exhibiting both redundant and context-dependent behaviors that significantly influence tumorigenesis, therapeutic resistance, and immune evasion. This technical review examines the molecular mechanisms underlying ubiquitin enzyme duality, incorporating quantitative analyses of enzyme-substrate relationships, detailed experimental methodologies for probing ubiquitin networks, and visual representations of critical signaling pathways. The complex interplay between E1, E2, and E3 enzymes and deubiquitinating enzymes (DUBs) creates a regulatory landscape that tumors exploit for adaptation and survival, presenting both challenges and opportunities for targeted therapeutic intervention in oncology.
Ubiquitination involves a sequential enzymatic cascade comprising E1 (activating), E2 (conjugating), and E3 (ligating) enzymes that conjugate ubiquitin to substrate proteins, while deubiquitinating enzymes (DUBs) reverse this process [82] [10]. The human genome encodes approximately 2 E1 enzymes, 40 E2 enzymes, over 600 E3 ligases, and nearly 100 DUBs, creating a complex regulatory network with immense functional potential [83] [10]. Within the tumor microenvironment, this system orchestrates critical cancer hallmarks including immune evasion, metabolic reprogramming, DNA damage response, and maintenance of cancer stem cell populations [28] [77].
The ubiquitin code—defined by variation in chain topology, linkage types, and substrate specificity—generates sophisticated signaling outcomes that extend far beyond simple proteasomal targeting [77]. K48-linked polyubiquitination primarily targets substrates for proteasomal degradation, while K63-linked chains typically facilitate non-proteolytic signaling functions in processes like DNA repair and immune signaling [28]. Monoubiquitination, multimonoubiquitination, and heterotypic polyubiquitination further expand the regulatory scope of ubiquitin signaling, enabling precise control over protein localization, activity, and interactions within malignant and stromal compartments of the tumor ecosystem [77].
Quantitative Landscape of Ubiquitin Enzyme Families
Enzyme-Substrate Relationships and Functional Capacity
Table 1: Quantitative Distribution of Ubiquitin System Components
| Component | Number in Human Genome | Primary Functions | Representative Cancer-Relevant Examples |
|---|---|---|---|
| E1 Activating Enzymes | 2 [10] | Ubiquitin activation via ATP hydrolysis | UBA1, UBA6 [10] |
| E2 Conjugating Enzymes | ~40 [83] | Ubiquitin chain formation, linkage specificity | UBE2N (K63 chains) [84], UBE2T (DNA repair) [77] |
| E3 Ligases | >600 [10] | Substrate recognition, specificity | FBXW7, TRIM21, MDM2 [28] [6] |
| Deubiquitinases (DUBs) | ~100 [85] | Ubiquitin chain removal, reversal of ubiquitination | USP14, USP7, OTUB1 [28] [85] |
The quantitative disparity between E2 enzymes (~40) and E3 ligases (>600) creates an inherent structural basis for functional redundancy, wherein multiple E3s may operate through shared E2 partners [83]. This architecture enables both specialized functions and backup mechanisms within the ubiquitin system. For instance, E2 enzymes such as UBE2N specialize in forming specific ubiquitin linkages (K63-linked chains) that can be utilized by numerous E3 ligases for distinct signaling functions across different tissue contexts [84].
The functional implications of this enzyme distribution become particularly evident in cancer, where perturbation of specific E3 ligases or DUBs can often be compensated by related family members, maintaining essential ubiquitin-dependent processes despite therapeutic targeting [28]. This compensatory capacity represents a significant mechanism of adaptive resistance in tumors and underscores the challenge of achieving durable responses with single-agent therapies targeting individual ubiquitin pathway components.
Mechanisms of Functional Redundancy
Structural and Biochemical Foundations
Functional redundancy within the ubiquitin system arises from conserved structural domains and catalytic mechanisms across enzyme families. E2 enzymes share a conserved ubiquitin-conjugating (UBC) catalytic domain of approximately 150 amino acids that facilitates ubiquitin transfer, while still enabling functional diversification through variation in non-conserved regions [83]. This structural conservation creates a platform for interchangeable functions while allowing evolutionary specialization.
The limited number of E2 enzymes relative to the extensive repertoire of E3 ligases establishes a fundamental redundancy architecture, wherein multiple E3s operate through shared E2 partners [83]. For example, various RING-family E3 ligases can utilize the same E2 enzyme to ubiquitinate distinct substrates, creating parallel signaling pathways with common mechanistic elements. This organization provides built-in compensatory capacity when individual components are disrupted.
Network-Level Redundancy in Cancer Pathways
Table 2: Examples of Functional Redundancy in Ubiquitin Enzymes Across Cancer Types
| Redundant Enzyme Group | Biological Process | Cancer Context | Compensatory Mechanism |
|---|---|---|---|
| USP14, USP7, OTUB1 [28] | DNA damage repair, CHK1 stabilization | Glioma, NSCLC, Breast cancer | Multiple DUBs stabilize key DNA repair proteins |
| TRIM26, OTUB1 [28] | Ferroptosis suppression (GPX4 stabilization) | Glioma, Gastric cancer | Independent stabilization of GPX4 via K63 ubiquitination or protein interaction |
| FBXW7, β-TrCP [28] | Substrate degradation (K48-linked) | Multiple solid tumors | Recognition of similar phosphodegron motifs in overlapping substrates |
| USP28, USP25 [85] | Wnt/β-catenin signaling | Pancreatic cancer | Independent stabilization of pathway components |
In the DNA damage response network, multiple DUBs including USP14, USP7, and OTUB1 demonstrate overlapping functionality in stabilizing CHK1 and other core DNA repair proteins [28]. When OTUB1 is inhibited in lung cancer models, compensatory stabilization through USP7 or USP14 can maintain CHK1 levels and preserve DNA repair fidelity, enabling continued radioresistance. This redundancy creates resilience in the face of genotoxic stress and targeted therapies.
Similarly, in metabolic adaptation, tumors employ multiple ubiquitin-dependent mechanisms to suppress ferroptosis. In glioblastoma, TRIM26 stabilizes GPX4 through K63-linked ubiquitination, while in gastric cancer, OTUB1 stabilizes GPX4 through direct protein-protein interactions [28]. Though the molecular mechanisms differ, both pathways converge on ferroptosis suppression, providing alternative routes to the same protective outcome across different tissue contexts.
Context-Dependent Functions in Tumor Biology
Tissue and Genetic Context Determinants
Ubiquitin enzymes exhibit remarkable functional plasticity based on cellular context, with the same enzyme performing opposing functions in different tumor environments. The F-box protein FBXW7 exemplifies this context duality, functioning as either an oncogene or tumor suppressor depending on genetic background [28]. In p53-wild type colorectal tumors, FBXW7 promotes radioresistance by degrading p53 and inhibiting apoptosis. Conversely, in non-small cell lung cancer (NSCLC) with SOX9 overexpression, FBXW7 enhances radiosensitivity by destabilizing SOX9 and alleviating p21 repression [28]. This functional switch underscores how tissue-specific signaling environments and genetic backgrounds reshape ubiquitin enzyme activity.
The deubiquitinase USP9X demonstrates similarly context-dependent behavior in pancreatic ductal adenocarcinoma (PDAC), where it can function as either an oncogene or tumor suppressor depending on cellular context [85]. In human pancreatic tumor cells, USP9X promotes malignant phenotypes and cell survival, while in KPC (KrasLSL-G12D/+; Trp53LSL-R172H/+; Pdx1-Cre) mouse models, it acts as a tumor suppressor through regulation of the Hippo pathway and YAP/TAZ activity [85]. This stark contrast highlights the limitations of extrapolating ubiquitin enzyme function across model systems and tumor types.
Subcellular Localization and Signaling Microenvironments
The functional outcome of ubiquitin enzyme activity is further refined by subcellular localization and dynamic changes in the signaling microenvironment. For instance, USP14 exhibits compartment-specific functions, stabilizing ALKBH5 to maintain glioblastoma stemness in nuclear contexts while degrading IκBα to activate NF-κB signaling in cytoplasmic environments in head and neck cancers [28]. This spatial regulation enables single enzymes to participate in distinct biological processes within the same cellular context.
Hypoxia and other tumor microenvironmental stresses further reshape ubiquitin enzyme function through post-translational modifications and altered interaction networks. UCHL1 stabilizes HIF-1α specifically in hypoxic tumor regions, activating the pentose phosphate pathway and enhancing antioxidant defense in breast cancer models [28]. This spatial restriction of function creates metabolic heterogeneity within tumors and illustrates how microenvironmental cues dictate context-specific ubiquitin enzyme activity.
Experimental Approaches for Delineating Ubiquitin Functions
Methodologies for Assessing Functional Redundancy
CRISPR-Cas9 Synthetic Lethality Screens: Systematic knockout of ubiquitin enzyme families identifies compensatory relationships and redundant functions. Pooled CRISPR libraries targeting all DUBs or E3 ligases are transduced into cancer cell lines, followed by treatment with specific inhibitors or environmental stressors [28]. Sequencing of guide RNA abundance reveals dropout patterns that identify enzymes with overlapping functions. Essential controls include: (1) non-targeting guide RNA controls for normalization, (2) multiple time points to distinguish primary from secondary effects, and (3) validation with pharmacologic inhibitors where available.
Biomolecular Fluorescence Complementation (BiFC) Assays: Visualizing E2-E3 interaction networks in live cells enables mapping of redundant interaction partners. E2 enzymes are fused to non-fluorescent N-terminal fragments of fluorescent proteins, while potential E3 partners are fused to C-terminal fragments [83]. Interaction-induced fluorescence complementation identifies preferential binding partnerships and competitive relationships. Critical optimization parameters include: (1) expression level titration to minimize non-specific interactions, (2) co-localization markers to verify subcellular context, and (3) time-lapse imaging to capture dynamic complex formation.
Approaches for Evaluating Context-Dependency
Proximity-Dependent Biotin Identification (BioID): Mapping context-dependent protein interaction networks using biotin ligase fusion proteins reveals how microenvironmental cues reshape ubiquitin enzyme function. E3 ligases or DUBs are fused to promiscuous biotin ligases (BirA* or TurboID) and expressed in different cancer models or under varying environmental conditions [28]. Biotinylated proteins are captured with streptavidin and identified by mass spectrometry. Methodological considerations include: (1) minimum expression time for biotinylation (typically 6-24 hours), (2) controls for non-specific biotinylation, and (3) normalization across different cellular contexts.
Ubiquitin Chain Termination (UCT) Assay: Specific interrogation of ubiquitin chain topology preferences across cellular contexts reveals how linkage specificity contributes to functional outcomes. HA-tagged ubiquitin mutants containing a single lysine residue (e.g., K48-only, K63-only) are expressed in cells along with candidate E3 ligases or DUBs [77]. Chain formation and editing preferences are analyzed by anti-HA immunoprecipitation and mass spectrometry. Technical requirements include: (1) verification of equal expression across mutants, (2) protease inhibition to prevent artifactural cleavage, and (3) quantitative normalization to total ubiquitin levels.
Visualization of Ubiquitin Network Relationships
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Research Reagents for Investigating Ubiquitin Enzyme Functions
| Reagent Category | Specific Examples | Research Application | Technical Considerations |
|---|---|---|---|
| Activity-Based Probes | HA-Ub-VS (vinyl sulfone), Ub-AMC (7-amido-4-methylcoumarin) [85] | DUB activity profiling, inhibitor screening | Cell permeability varies; requires optimization of concentration and incubation time |
| Linkage-Specific Antibodies | K48-linkage specific, K63-linkage specific, Mono-Ub antibodies [77] | Western blot detection of specific ubiquitin chain types | Cross-reactivity can occur; verification with linkage-specific mutants recommended |
| Ubiquitin Mutants | K48-only, K63-only, K0 (no lysines) [77] | Determining chain specificity of E3s/DUBs | Requires careful expression level control; may disrupt endogenous ubiquitin dynamics |
| PROTAC Molecules | ARV-110, ARV-471, RT-PROTAC systems [28] | Targeted protein degradation, studying E3 ligase function | Specificity depends on E3 ligase expression; off-target degradation possible |
| CRISPR Libraries | Whole-genome, DUB-focused, E3 ligase-focused libraries [28] | Genetic screens for redundant functions | Requires deep coverage (>500x); multiple time points enhance hit identification |
| Mass Spectrometry Standards | SILAC (stable isotope labeling with amino acids in cell culture), TMT (tandem mass tags) [84] | Quantitative ubiquitinomics, interaction studies | Heavy amino acids can affect cell physiology; appropriate labeling efficiency required |
Therapeutic Implications and Future Directions
The dual nature of ubiquitin enzymes—balancing functional redundancy with context-dependent specificity—presents both challenges and opportunities for cancer therapeutics. While redundancy complicates targeted inhibition by enabling compensatory mechanisms, it also creates synthetic lethal opportunities when multiple family members are simultaneously disrupted [28]. Conversely, context-dependent functions enable more precise therapeutic targeting of tumor-specific vulnerabilities while sparing normal tissues.
Emerging strategies leverage these principles through polypharmacology approaches that simultaneously target multiple ubiquitin pathway components, or through context-specific activation of ubiquitin-dependent protein degradation [28]. Radiation-triggered PROTAC (RT-PROTAC) prodrugs represent a promising example, wherein X-ray activation specifically within irradiated tumors enables spatially-controlled degradation of BRD4/2 in breast cancer models [28]. Similarly, nanoparticle-encapsulated PROTAC systems (e.g., diselenide-bridged RCNprotac) achieve selective release within irradiated tumors, exploiting the unique tumor microenvironment for precision targeting [28].
Future research directions should focus on comprehensive mapping of ubiquitin enzyme interaction networks across diverse tumor contexts, development of conditional degradation technologies that leverage tissue-specific biomarkers, and combinatorial approaches that integrate ubiquitin-targeting agents with conventional therapies to overcome adaptive resistance mechanisms. The integration of high-resolution structural data with functional genomics will further illuminate the molecular determinants of context-dependency, enabling rational design of next-generation ubiquitin-targeted therapeutics with enhanced specificity and efficacy within the complex tumor microenvironment.
The ubiquitin-proteasome system (UPS) represents a pivotal therapeutic target, particularly within the complex signaling networks of the tumor microenvironment. However, achieving precise modulation of ubiquitination without triggering off-target effects remains a formidable challenge in drug development. This technical review examines cutting-edge strategies designed to enhance the specificity of ubiquitin modulation, with a dedicated focus on minimizing collateral damage to non-target proteins and pathways. We synthesize recent advances in structural biology, chemical design, and delivery technologies that collectively enable researchers to exert unprecedented control over ubiquitin signaling networks. The protocols and frameworks presented herein provide a methodological foundation for developing next-generation ubiquitin-targeting therapies with improved safety and efficacy profiles for cancer treatment.
The ubiquitin system comprises approximately 100 deubiquitinating enzymes (DUBs), 600 E3 ubiquitin ligases, and numerous E2 conjugating enzymes that collectively regulate protein stability, localization, and function through post-translational modification [86] [55]. Within the tumor microenvironment, ubiquitination governs critical processes including immune checkpoint expression, metabolic reprogramming, and DNA damage response [8] [5] [41]. However, the inherent complexity and functional redundancy of ubiquitin networks present significant obstacles to specific therapeutic intervention. Conventional approaches that broadly inhibit E1 activating enzymes or proteasomal activity inevitably disrupt global protein homeostasis, resulting in dose-limiting toxicities and narrow therapeutic windows.
Off-target effects in ubiquitin modulation manifest through multiple mechanisms: (1) unintended recognition of structurally similar degrons by E3 ligases; (2) collateral disruption of ubiquitin-dependent processes in non-malignant cells; and (3) temporal mismatches between therapeutic action and target vulnerability windows [87] [7]. Addressing these challenges requires sophisticated strategies that exploit structural nuances within the ubiquitin machinery while incorporating spatial and temporal control mechanisms. The following sections detail emerging approaches that collectively represent a paradigm shift from broad inhibition to precision modulation of ubiquitin signaling.
Molecular-Specific Strategies
Advanced PROTAC Design and Engineering
Proteolysis-Targeting Chimeras (PROTACs) represent a revolutionary approach in targeted protein degradation, but their conventional designs often lack sufficient specificity. Recent innovations have yielded several engineered PROTAC systems with enhanced precision:
Aptamer-PROTAC Conjugates: These conjugates utilize nucleic acid aptamers that recognize tumor-specific cell surface receptors, facilitating selective internalization into malignant cells. Upon receptor-mediated endocytosis, the PROTAC component engages intracellular E3 ligases to degrade oncoproteins, significantly reducing off-target effects in healthy tissues [87].
Drugtamer-PROTAC Conjugates: This platform enables co-delivery of PROTACs with small-molecule agents, optimizing synergistic effects while minimizing systemic exposure. The approach allows for tailored combination therapies that address compensatory resistance mechanisms often triggered by single-agent treatments [87].
RGD Peptide-Based Systems: By incorporating arginine-glycine-aspartate (RGD) motifs that preferentially bind αvβ3 integrins overexpressed on tumor vasculature, these PROTACs achieve enhanced tumor penetration and cellular uptake, concentrating degradation activity within the tumor microenvironment [87].
Table 1: Engineered PROTAC Platforms for Enhanced Specificity
| Platform | Key Component | Specificity Mechanism | Applications |
|---|---|---|---|
| Aptamer-PROTAC | Nucleic acid aptamer | Tumor-specific receptor recognition and internalization | Solid tumors with defined surface markers |
| Drugtamer-PROTAC | Small molecule partner | Coordinated delivery with synergistic agents | Overcoming compensatory resistance pathways |
| RGD-PROTAC | RGD peptide | αvβ3 integrin-mediated tumor homing | Tumors with angiogenic vasculature |
| Photo-controlled PROTAC | Light-responsive group | Spatiotemporal activation by external light | Precision neurobiology and dermatological oncology |
Molecular Glues and Natural Compounds
Molecular glues facilitate induced protein-protein interactions between E3 ubiquitin ligases and target substrates, often exhibiting superior pharmacological properties compared to heterobifunctional PROTACs:
Immunomodulatory Imides: Clinical agents including thalidomide, lenalidomide, and pomalidomide function by recruiting novel substrates to the CRL4CRBN E3 ligase complex. Their relatively compact molecular architecture promotes favorable bioavailability while maintaining specificity through precise interfacial stabilization [88].
Polyphenol-Derived Metabolites: Natural compounds such as urolithins (from ellagitannins) and valerolactones (from flavan-3-ols) demonstrate selective UPS modulation at physiological concentrations. These metabolites exhibit tissue-specific effects on proteasome function, potentially leveraging endogenous metabolic pathways for targeted activity [89].
Spatiotemporal Control Strategies
Light-Activated Systems
Photocontrolled PROTACs incorporate light-responsive elements that remain inert until activated by specific wavelengths, enabling precise temporal regulation of protein degradation in vivo. These systems permit researchers to trigger degradation at defined timepoints, facilitating mechanistic studies of protein function and creating therapeutic interventions that align with circadian rhythms or cell cycle dynamics [87].
Radiation-Responsive Platforms
Emerging radiotherapy-activated systems create spatial specificity within irradiated fields:
- RT-PROTAC Prodrugs: These inactive precursors undergo conversion to active PROTACs upon exposure to tumor-localized X-rays, enabling degradation of specific targets like BRD4/2 in conjunction with radiotherapy [55].
- X-Ray-Responsive Nanomicelles: Diselenide-bridged RCNprotac micelles selectively release PROTAC payloads within irradiated tumors, combining the precision of radiotherapy with targeted protein degradation while sparing healthy tissues [55].
Experimental Protocols for Specificity Validation
Activity-Based Protein Profiling (ABPP) for DUB Specificity Assessment
ABPP utilizes chemical probes to directly monitor the functional state of enzymes in complex biological systems, providing critical data on selectivity patterns [86].
Protocol: Diubiquitin Probe Screening for DUB Specificity
- Probe Synthesis: Generate diubiquitin activity-based probes mimicking natural linkage types (K48, K63, etc.) by coupling warhead-bearing linkers to HA-tagged ubiquitin thioesters, followed by copper-catalyzed azide-alkyne cycloaddition with azidohomoalanine-incorporated proximal ubiquitin [86].
- Lysate Preparation: Prepare clarified lysates from target cell lines (e.g., HEK293, Jurkat) or patient-derived tumor specimens using non-denaturing conditions (25mM HEPES, 150mM NaCl, 1% NP-40, pH 7.4) with protease inhibitors.
- Labeling Reaction: Incubate lysates (50μg total protein) with diubiquitin probes (1μM) for 30 minutes at 37°C in reaction buffer.
- Click Chemistry Conjugation: Add biotin-azide (50μM), Tris(2-carboxyethyl)phosphine (1mM), Tris[(1-benzyl-1H-1,2,3-triazol-4-yl)methyl]amine (100μM), and CuSO4 (1mM) to the labeling mixture, incubate for 1 hour at room temperature.
- Streptavidin Enrichment and Analysis: Capture biotinylated proteins using streptavidin beads, followed by on-bead trypsin digestion and LC-MS/MS analysis to identify specifically labeled DUBs.
- Validation: Confirm functional consequences of DUB engagement through complementary ubiquitin cleavage assays and substrate stabilization monitoring.
Ternary Complex Stability Assessment
PROTAC efficiency correlates directly with the stability of the POI-PROTAC-E3 ternary complex. This protocol quantifies complex formation and degradation specificity.
Protocol: Cellular Thermal Shift Assay (CETSA) for Ternary Complex Evaluation
- Sample Preparation: Treat cells (1×10⁶/mL) with PROTAC compounds at varying concentrations (1nM-10μM) for 3 hours in complete medium.
- Heat Denaturation: Aliquot cell suspensions into PCR tubes, heat at temperatures ranging from 37°C to 65°C for 3 minutes using a thermal cycler.
- Cell Lysis and Fractionation: Freeze-thaw samples three times using liquid nitrogen and a 37°C water bath, followed by centrifugation at 20,000×g for 20 minutes at 4°C.
- Western Blot Analysis: Resolve soluble fractions by SDS-PAGE, transfer to PVDF membranes, and immunoblot for targets of interest and potential off-targets.
- Data Analysis: Quantify band intensities to generate melting curves, calculating Tm shifts indicative of compound engagement. Specificity is validated by comparing Tm shifts between intended targets and structurally related off-target proteins.
Diagram 1: Integrated strategies for enhancing specificity in ubiquitin modulation, showing the relationship between molecular design, spatiotemporal control, and experimental validation approaches.
The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential Research Reagents for Specific Ubiquitin Modulation Studies
| Reagent Category | Specific Examples | Function and Application | Specificity Features |
|---|---|---|---|
| Activity-Based Probes | Diubiquitin vinyl sulfone probes; Ubiquitin variant (UbV) probes with C-terminal alkyne warheads [86] | Covalent labeling of active DUBs; identification of enzyme activity patterns in complex lysates | Linkage-specific diubiquitin probes distinguish K48- vs K63-specific DUBs; UbV mutants selective for individual DUBs like USP7 |
| Selective E3 Ligase Modulators | FBXW7-directed molecular glues; SPOP-recruiting PROTACs [7] [5] | Targeted degradation of substrates bearing specific phosphodegrons | FBXW7 recognizes canonical CPD motif (L-X-pT-P-P-X-pS); SPOP targets melanoma-associated antigens |
| UPS-Modulating Metabolites | Urolithin A (Ellagitannin metabolite); Ferulic acid (Hydroxycinnamic acid) [89] | Natural proteasome modulation at physiological concentrations | Tissue-specific effects on UPS; differential activity in cancerous vs. normal cells |
| Chain-Linkage Specific Antibodies | K48-linkage specific antibodies; K63-linkage specific antibodies [55] | Detection of specific ubiquitin chain architectures in cells and tissues | Distinguishes degradative (K48) from signaling (K63) ubiquitination in immunofluorescence and Western blot |
The evolving toolkit for precise ubiquitin modulation represents a paradigm shift in targeted protein degradation therapeutics. By integrating structure-guided design, innovative delivery platforms, and rigorous validation methodologies, researchers can now address specificity challenges that have historically limited the clinical translation of UPS-targeting agents. The convergence of these approaches—from molecular glues that exploit natural protein interfaces to spatiotemporally controlled PROTACs that respond to external stimuli—creates unprecedented opportunities for therapeutic intervention in the tumor microenvironment.
Future developments will likely focus on patient-specific degron profiling to match ubiquitin modulators with individual tumor signatures, as well as multi-specific platforms that simultaneously engage multiple E3 ligases for enhanced selectivity. As our understanding of ubiquitin chain plasticity and context-dependent E3 ligase function deepens, the next generation of ubiquitin modulators will achieve increasingly sophisticated control over protein fate, ultimately enabling more precise and effective cancer therapies with minimal off-target consequences.
Addressing Adaptive Tumor Responses and Metabolic Rewiring
The tumor microenvironment (TME) is a complex ecosystem wherein cancer cells exhibit remarkable adaptability through metabolic rewiring—a hallmark of cancer that supports uncontrolled proliferation, survival, and metastasis [90] [91]. This reprogramming encompasses altered glucose, amino acid, and lipid metabolism, enabling tumors to thrive under hypoxic and nutrient-deficient conditions [90]. Central to regulating these adaptive responses is the ubiquitin-proteasome system (UPS), which governs the stability, activity, and localization of key metabolic enzymes and signaling proteins through post-translational modification [6] [92]. Ubiquitination, the covalent attachment of ubiquitin to target proteins, has emerged as a pivotal mechanism controlling fundamental cellular processes in tumor biology, including metabolic pathway modulation and immune evasion [6] [8]. This intricate interplay between ubiquitination signaling and metabolic rewiring represents a critical frontier in understanding tumor adaptation and developing targeted therapeutic strategies.
The UPS consists of a cascade of enzymes—E1 (ubiquitin-activating), E2 (ubiquitin-conjugating), and E3 (ubiquitin-ligase)—that work in concert to tag proteins for proteasomal degradation or functional modification [92] [10]. With over 600 E3 ligases conferring substrate specificity, the UPS can precisely regulate metabolic enzymes and oncoproteins [10]. Conversely, deubiquitinating enzymes (DUBs) reverse this process, providing an additional layer of regulation [92]. The dysregulation of ubiquitination pathways in cancer creates dependencies that can be therapeutically exploited, making the UPS an attractive target for intervention [6] [10].
Metabolic Rewiring in the Tumor Microenvironment
Hallmarks of Tumor Metabolic Reprogramming
Cancer cells undergo profound metabolic alterations to meet the biosynthetic and bioenergetic demands of rapid proliferation. These adaptations include:
- Dysregulated nutrient uptake: Increased glucose and amino acid consumption even under oxygen-sufficient conditions [93].
- Glycolytic dominance: Preference for glycolysis over oxidative phosphorylation (Warburg effect), supporting rapid ATP generation and biomass production [90] [92].
- Metabolic flexibility: Utilization of diverse nutrient sources including lipids, amino acids, and metabolic byproducts [91].
- Enhanced anabolic metabolism: Activation of biosynthetic pathways for nucleotides, non-essential amino acids, and lipids [91].
These reprogrammed metabolic pathways are not isolated events but form an integrated network that interacts with immune cells and stromal components within the TME, creating an immunosuppressive milieu that facilitates immune evasion and tumor progression [91].
Key Metabolic Pathways in Tumor Adaptation
Table 1: Major Metabolic Pathways in Cancer Cells and Their Functional Roles
| Metabolic Pathway | Key Enzymes/Regulators | Role in Tumor Progression | Ubiquitination Regulation |
|---|---|---|---|
| Glucose Metabolism | HK2, PKM2, LDHA, GLUT1 [90] [91] | Warburg effect, lactate production, immune suppression [92] [91] | STING targets HK2; UPS regulates glycolytic enzymes [92] [91] |
| Amino Acid Metabolism | IDO1, ASS1, GLS, ASNS [91] | Tryptophan/kynurenine pathway, arginine dependency, glutaminolysis [91] | UPS regulates stability of metabolic enzymes [6] [92] |
| Lipid Metabolism | ACAT1, FASN, CPT1A, SCD [90] [91] | Membrane biosynthesis, energy storage, signal transduction [91] | c-MYC regulates fatty acid enzymes; UPS modulation [90] [92] |
The coordination of these metabolic pathways is orchestrated by oncogenes and tumor suppressor genes. For instance, the c-MYC oncogene enhances glycolysis by regulating GLUT1, LDHA, and HK2 expression, while simultaneously promoting glutamine metabolism and fatty acid synthesis [90]. Similarly, KRAS mutations drive glucose uptake and divert glycolytic intermediates into biosynthetic pathways like the hexosamine biosynthesis pathway and pentose phosphate pathway [90]. These oncogenic drivers are themselves regulated by ubiquitination, creating complex feedback loops within the TME [6] [10].
Ubiquitination Regulation of Tumor Metabolism
The Ubiquitin-Proteasome System: Molecular Machinery
The ubiquitination process involves a sequential enzymatic cascade that conjugates ubiquitin to target proteins. E1 activating enzymes initiate the process through ATP-dependent ubiquitin activation, which is then transferred to E2 conjugating enzymes. E3 ligases provide substrate specificity by facilitating ubiquitin transfer from E2 enzymes to target proteins [92] [10]. The human genome encodes approximately 40 E2 enzymes and over 600 E3 ligases, enabling precise substrate selection [10]. Deubiquitinating enzymes (DUBs) counterbalance this process by removing ubiquitin chains, providing dynamic regulation of protein stability and function [92].
Diagram 1: Ubiquitin-Proteasome System Cascade. The enzymatic cascade of ubiquitination and subsequent proteasomal degradation of target substrates.
Ubiquitination of Metabolic Enzymes and Regulators
The UPS exerts precise control over metabolic reprogramming through the regulation of key metabolic enzymes, transcription factors, and signaling proteins:
Glycolytic Enzymes: Multiple glycolytic enzymes are regulated by ubiquitination. HK2 (hexokinase 2), the first rate-limiting enzyme of glycolysis, is targeted by the STING pathway, linking DNA damage sensing to metabolic regulation [91]. PKM2 (pyruvate kinase M2), which influences glycolytic flux and nucleotide synthesis, is regulated by ubiquitination that can trigger its degradation [91].
Oncogenic Metabolic Regulators: The stability of powerful oncogenic drivers like c-MYC is controlled by ubiquitin-mediated degradation [90] [10]. Similarly, HIF-1α (hypoxia-inducible factor 1-alpha), a master regulator of hypoxia response and metabolic adaptation, is targeted for proteasomal degradation under normoxic conditions [91].
Lipid Metabolic Enzymes: Enzymes involved in lipid metabolism such as FASN (fatty acid synthase) and ACC (acetyl-CoA carboxylase) are regulated by ubiquitination, influencing de novo lipogenesis in cancer cells [90].
Amino Acid Transporters and Enzymes: Proteins involved in amino acid metabolism, including glutamine transporters and catabolic enzymes, undergo ubiquitin-mediated regulation that adapts nutrient utilization to support tumor growth [92].
The impact of ubiquitination on metabolic enzymes creates vulnerabilities that can be targeted therapeutically. For instance, the E3 ligase SPOP mediates the ubiquitination and degradation of PD-L1, linking metabolic regulation to immune checkpoint control [5]. When this regulatory mechanism is disrupted, either through competitive binding or mutations, PD-L1 stability increases, promoting immune evasion [5].
Experimental Approaches for Studying Ubiquitination in Tumor Metabolism
In Vivo Ubiquitination Assay Protocol
The detection of protein ubiquitination is essential for understanding UPS-mediated metabolic regulation. Below is an optimized protocol for in vivo ubiquitination assays [94]:
Key Reagents and Materials:
- Plasmids: His-tagged ubiquitin, Flag-tagged E3 ligase (e.g., FBXO45), HA-tagged substrate protein (e.g., IGF2BP1)
- Cell lines: HEK293T (for transfection), cancer cell lines relevant to study (e.g., HepG2, HCCLM3)
- Proteasome inhibitor: MG-132
- Lysis buffer: Containing protease inhibitors and 1% Triton X-100
- Ni-NTA Agarose for His-ubiquitin pulldown
- Antibodies: Anti-HA, anti-Flag, anti-GAPDH, species-specific HRP-conjugated secondary antibodies
Procedure:
- Plasmid Preparation: Generate endotoxin-free expression plasmids for His-Ub, Flag-E3, and HA-substrate using EndoFree Plasmid kits. Verify concentration and purity (A260/A280 ratio of 1.8-2.0) [94].
- Cell Culture and Transfection: Maintain HEK293T and relevant cancer cell lines in complete DMEM. At 80-90% confluency, transfect cells with plasmid combinations using Lipofectamine 2000. Include controls with empty vector and substrate mutants (e.g., K190A, K450A) [94].
- Proteasome Inhibition: Treat cells with 10μM MG-132 for 4-6 hours before harvesting to prevent degradation of ubiquitinated proteins.
- Cell Lysis and Protein Extraction: Harvest cells and lyse in buffer containing protease inhibitors and 1% Triton X-100. Clarify lysates by centrifugation at 12,000 × g for 15 minutes.
- Affinity Purification: Incubate lysates with Ni-NTA Agarose for 4 hours at 4°C to capture His-tagged ubiquitinated proteins.
- Western Blot Analysis: Resolve purified proteins by SDS-PAGE, transfer to membranes, and probe with anti-HA antibody to detect ubiquitinated substrate. Use anti-Flag for E3 ligase expression and anti-GAPDH as loading control.
Troubleshooting Notes: High background can be reduced by increasing salt concentration in wash buffer. Incomplete ubiquitination detection may require optimization of MG-132 concentration and treatment duration.
The Scientist's Toolkit: Essential Research Reagents
Table 2: Key Research Reagents for Studying Ubiquitination and Metabolism
| Reagent Category | Specific Examples | Research Application | Key Function |
|---|---|---|---|
| Expression Plasmids | His-Ub, Flag-E3 ligases, HA-substrates [94] | In vivo ubiquitination assays | Tagged proteins for detection and purification |
| Proteasome Inhibitors | MG-132, Bortezomib [94] [10] | Stabilize ubiquitinated proteins | Block proteasomal degradation |
| E1 Inhibitors | MLN7243, MLN4924 [10] | Investigate UPS dependency | Block ubiquitin activation |
| E3 Ligase Modulators | Nutlin, MI-219 [10] | Target specific ubiquitination pathways | Modulate substrate degradation |
| DUB Inhibitors | Compounds G5, F6 [10] | Study deubiquitination processes | Prevent ubiquitin removal |
| Metabolic Assay Kits | CCK-8 assay [94] | Measure cell proliferation | Assess functional outcomes |
Functional Validation Assays
Following ubiquitination detection, functional validation is crucial for establishing biological significance:
- Cell Proliferation Assays: Using CCK-8 or similar reagents to measure the impact of ubiquitination on substrate-mediated cell growth [94].
- Metabolic Flux Analysis: Employing Seahorse Analyzers or isotope tracing to quantify changes in glycolysis, oxidative phosphorylation, or nutrient utilization.
- Immune Co-culture Assays: Evaluating how ubiquitination of metabolic enzymes or immune checkpoints affects T-cell mediated killing [5].
Therapeutic Targeting Strategies
Current Clinical Agents and Development Candidates
The intimate connection between ubiquitination and tumor metabolism has inspired several therapeutic approaches:
Table 3: Therapeutic Agents Targeting Ubiquitination and Metabolic Pathways
| Therapeutic Category | Representative Agents | Molecular Target | Clinical Status |
|---|---|---|---|
| Proteasome Inhibitors | Bortezomib, Carfilzomib, Ixazomib [10] | 20S proteasome core particle | Approved for hematologic malignancies |
| E1 Inhibitors | MLN4924 (Pevonedistat) [10] | NEDD8-activating enzyme | Clinical trials |
| E3 Ligase Modulators | Nutlin, MI-219 [10] | MDM2-p53 interaction | Preclinical/Clinical development |
| DUB Inhibitors | Compounds G5, F6 [10] | Deubiquitinating enzymes | Preclinical development |
| Metabolic Enzyme Inhibitors | ADI-PEG20, CB-839 [91] | Arginine metabolism, glutaminase | Clinical trials |
| SGLT2 Inhibitors | Canagliflozin [5] | SGLT2/PD-L1 interaction | Preclinical research |
Combination Strategies and Resistance Mechanisms
Promising therapeutic approaches include combining ubiquitination-targeted agents with conventional treatments or immunotherapy:
- PROTACs (Proteolysis-Targeting Chimeras): Bifunctional molecules that recruit E3 ligases to target proteins for degradation, enabling targeting of previously "undruggable" oncoproteins [6].
- Immunometabolic Combinations: Simultaneous targeting of PD-1/PD-L1 and metabolic checkpoints such as IDO1 or glutaminase to overcome immune resistance [91] [5].
- Resistance Mechanisms: Tumors develop resistance to UPS-targeted therapies through proteasome subunit mutations, upregulated antioxidant pathways, and activation of alternative protein degradation mechanisms like autophagy [10].
Diagram 2: Therapeutic Targeting Landscape. Key interconnected nodes in the tumor microenvironment for therapeutic intervention, highlighting the interface between ubiquitination, metabolism, and immune regulation.
The intricate interplay between ubiquitination signaling and metabolic rewiring represents a critical axis of tumor adaptation that offers promising therapeutic opportunities. As research continues to unravel the complex regulatory networks connecting the UPS to metabolic pathway control, several emerging areas warrant particular attention:
First, the development of tissue-specific and tumor-selective E3 ligase modulators could enable more precise targeting of oncogenic metabolism while minimizing off-target effects. Second, understanding the temporal dynamics of ubiquitination in response to metabolic stress and therapy will be crucial for optimizing treatment scheduling and combination strategies. Third, exploring the role of non-degradative ubiquitination (e.g., K63-linked chains) in metabolic regulation may reveal novel regulatory mechanisms. Finally, advancing proteomic technologies for mapping ubiquitination events across different tumor types will enable patient stratification and personalized therapeutic approaches.
The integration of ubiquitination-targeting agents with conventional chemotherapy, radiotherapy, and immunotherapy represents a promising frontier in cancer treatment. By simultaneously addressing multiple adaptive mechanisms—metabolic plasticity, immune evasion, and protein homeostasis—these combinatorial approaches may overcome the limitations of single-modality therapies and provide durable responses for cancer patients.
Biomarker Development for Patient Stratification and Treatment Selection
Ubiquitination, a dynamic and reversible post-translational modification, has emerged as a master regulatory mechanism in oncology, orchestrating critical processes including immune evasion, DNA repair fidelity, and metabolic reprogramming within the tumor microenvironment (TME) [5] [55]. The ubiquitin-proteasome system (UPS) mediates the precise degradation of cellular proteins through a coordinated enzymatic cascade involving E1 (activating), E2 (conjugating), and E3 (ligase) enzymes, ultimately tagging substrates for proteasomal destruction [5]. Conversely, deubiquitinases (DUBs) reverse this process, stabilizing target proteins [63]. The functional outcome of ubiquitination depends critically on ubiquitin chain topology, with K48-linked chains typically targeting proteins for proteasomal degradation, while K63-linked chains and monoubiquitination predominantly regulate non-proteolytic signaling complexes, endocytic trafficking, and DNA damage responses [5] [55].
Mounting evidence firmly establishes the ubiquitin system as a pivotal regulator of tumor immune resistance, largely through its modulation of immune checkpoint molecules such as programmed cell death protein 1 (PD-1) and its ligand (PD-L1) [5] [63]. The strategic manipulation of this system offers novel avenues for therapeutic intervention. This technical guide examines biomarker development strategies that leverage our growing understanding of ubiquitination signaling to achieve precise patient stratification and optimize treatment selection in oncology.
Ubiquitination-Mediated Regulation of Immune Checkpoints
Molecular Mechanisms of PD-1/PD-L1 Control via Ubiquitination
The cell surface expression and stability of PD-1/PD-L1 are critically regulated by ubiquitin-mediated degradation, presenting a key mechanism of immune evasion exploited by tumors [5]. Multiple E3 ubiquitin ligases directly target PD-L1 for ubiquitination and subsequent proteasomal degradation. Speckle-type POZ protein (SPOP) has been identified as a crucial E3 ligase promoting PD-L1 ubiquitination in colorectal cancer [5]. However, competitive binding by proteins such as ALDH2 and BCLAF1 in hepatocellular carcinoma can disrupt SPOP-PD-L1 interaction, thereby stabilizing PD-L1 and promoting immune escape [5].
Beyond SPOP, other regulatory mechanisms exist. The sodium-glucose cotransporter 2 (SGLT2) can stabilize PD-L1 by competitively binding to it, thereby preventing SPOP recognition. Notably, the SGLT2 inhibitor canagliflozin can disrupt this interaction, restoring SPOP-mediated PD-L1 ubiquitination and degradation, and consequently enhancing T-cell mediated antitumor activity [5]. These findings illustrate the complex regulatory networks controlling PD-L1 stability and highlight potential therapeutic strategies to modulate immune checkpoint expression.
Ubiquitination Chain Topology and Functional Consequences
The biological consequences of ubiquitination are profoundly influenced by chain linkage type, creating a sophisticated "ubiquitin code" that governs protein fate within the TME [55].
Table 1: Ubiquitin Chain Linkages and Their Functional Impact in Cancer
| Linkage Type | Primary Function | Impact on Tumor Biology | Therapeutic Implication |
|---|---|---|---|
| K48-linked | Targets substrates for proteasomal degradation [5] | Context-dependent roles in radioresistance; FBXW7 degrades p53 (radioresistance) or SOX9 (radiosensitization) depending on cellular context [55] | High specificity potential but requires careful patient stratification |
| K63-linked | Facilitates signaling complexes, DNA repair, endocytosis [5] | Promotes error-prone DNA repair (e.g., FBXW7-XRCC4 in NHEJ); activates pro-survival pathways (e.g., TRAF4-JNK/c-Jun) [55] | Targets for combination therapy to overcome treatment resistance |
| Monoubiquitination | Regulates histone function, DNA repair, protein trafficking [55] | Maintains genome integrity (e.g., UBE2T/RNF8-mediated H2AX monoubiquitylation); critical for DNA damage response [55] | Emerging target for precision radio-sensitization strategies |
This functional diversity establishes ubiquitin networks as central hubs coordinating DNA repair, immune modulation, and cell survival simultaneously [55]. The complexity of this regulatory system necessitates sophisticated biomarker strategies to identify patients most likely to benefit from ubiquitination-targeted therapies.
Multi-Omics Approaches for Ubiquitination Biomarker Discovery
Integrating Omics Technologies for Comprehensive Profiling
Tumor heterogeneity remains a formidable challenge in clinical oncology, driving drug resistance through variations in treatment targets and TME composition [95]. Multi-omics approaches provide a powerful solution by delivering a comprehensive, multidimensional view of tumor biology that captures this complexity. The integration of genomics, transcriptomics, proteomics, and spatial biology enables researchers to identify distinct patient subgroups based on molecular and immune profiles [95].
Table 2: Multi-Omics Technologies for Ubiquitination Biomarker Discovery
| Omics Layer | Analytical Focus | Relevant Technologies | Application in Ubiquitination Research |
|---|---|---|---|
| Genomics | Identifies mutations, structural variations, and copy number variations (CNVs) that drive tumorigenesis [95] | Whole Genome Sequencing (WGS), Whole Exome Sequencing (WES) | Detection of mutations and CNVs in ubiquitination regulators (UBRs) such as E3 ligases and DUBs [63] |
| Transcriptomics | Analyzes gene expression patterns and regulatory networks [95] | RNA sequencing, single-cell RNA sequencing, spatial transcriptomics | Assessment of UBR expression across tissue architecture, revealing TME dynamics [95] [63] |
| Proteomics | Profiles functional protein states, including post-translational modifications [95] | Mass spectrometry, immunofluorescence, multiplex immunohistochemistry (IHC) | Direct measurement of ubiquitinated proteins; mapping of ubiquitination networks and interactions [95] |
| Spatial Biology | Preserves tissue architecture to study cellular interactions and immune infiltration [95] | Spatial transcriptomics, spatial proteomics, multiplex IHC/IF | Contextualization of ubiquitination signaling within tumor ecosystem; identification of spatially-resolved biomarkers [95] |
Ubiquitination-Based Patient Stratification in Lung Adenocarcinoma
Integrative multi-omics analysis has demonstrated the clinical utility of ubiquitination-based stratification in lung adenocarcinoma (LUAD) [63]. One study identified 17 hub ubiquitination regulators (UBRs) from protein-protein interaction networks correlated with cancer hallmark-related pathways. These UBRs exhibited widespread genetic alterations, with somatic mutations occurring in 11.04% of LUAD patients (68/616) and prevalent copy number variations (CNVs) [63].
Based on the expression profiles of these hub UBRs, LUAD patients can be classified into two distinct ubiquitination subtypes with significantly different clinical characteristics [63]. These subtypes demonstrate marked differences in:
- Patient survival outcomes
- Mutation burden and patterns
- Gender distribution (female predominance in one subtype)
- Immune infiltration levels and profiles
- Therapeutic response to various treatments [63]
This stratification approach enabled the development of a ubiquitination-related risk (UBrisk) scoring system, which effectively evaluates ubiquitination status at the individual patient level. Importantly, patients with low UBrisk scores demonstrated increased likelihood of benefiting from immunotherapy, providing a clinically actionable biomarker for treatment selection [63].
Biomarker Classification and Clinical Validation Frameworks
Defining Biomarker Types and Clinical Applications
Biomarkers are objectively measured characteristics that indicate normal biological processes, pathogenic processes, or pharmacological responses to therapeutic intervention [96]. In clinical oncology, they are broadly classified based on their specific applications in drug development and patient management.
Prognostic Biomarkers provide information about the natural history of the disease regardless of therapy. They identify patients with differing risks of specific outcomes, such as disease progression or death [96]. For example, a validated prognostic biomarker would distinguish populations with poor versus favorable outcomes following both test and standard treatments.
Predictive Biomarkers identify patients who are more likely to respond to a particular treatment. They indicate differential outcomes based on specific therapies, enabling treatment selection tailored to individual patient biology [96]. A classic example includes ER status in breast cancer, which predicts benefit from tamoxifen therapy [96].
Some biomarkers demonstrate both prognostic and predictive characteristics. For instance, in breast cancer, estrogen receptor (ER)-negative status is prognostic (indicating higher relapse risk) and predictive (indicating reduced benefit from tamoxifen) [96]. This dual functionality underscores the importance of comprehensive biomarker validation.
Statistical Considerations in Biomarker Development
Robust statistical methodology is paramount in biomarker research to minimize bias and maximize precision [96]. Common challenges include:
- Confounding factors that may distort the relationship between biomarker status and clinical outcomes
- Multiplicity issues arising from multiple statistical testing without appropriate correction
- Overestimation of effects in small, early-stage discovery studies [96]
Prospective-validation in large, independent cohorts is essential to establish clinical utility before widespread implementation. Randomized controlled trials provide the most definitive evidence for biomarker utility, as non-randomized studies cannot distinguish between prognostic and predictive effects [96].
Experimental Protocols for Ubiquitination Biomarker Validation
Flow Cytometry for Immune Cell Profiling and Checkpoint Expression
Flow cytometry represents a cornerstone technology for validating immune-related biomarkers in the TME. The following protocol outlines a standardized approach for characterizing immune cell populations and PD-1/PD-L1 expression:
Cell Preparation and Staining Protocol:
- Prepare single-cell suspensions from fresh tumor tissue using appropriate dissociation techniques [97].
- Assess cell viability using fluorescent dyes (e.g., propidium iodide, 7-AAD) to exclude dead cells from analysis [97].
- Stimulate immune cells as needed using cell activation cocktails (e.g., PMA/ionomycin with protein transport inhibitors for cytokine detection) [97].
- Perform surface staining with fluorochrome-conjugated antibodies against immune markers (CD3, CD4, CD8, CD45, PD-1, PD-L1) in staining buffer for 30 minutes at 4°C [97].
- For intracellular targets (cytokines, transcription factors), fix and permeabilize cells using commercial fixation/permeabilization kits before intracellular staining [97].
- Acquire data on a flow cytometer configured for multicolor analysis, ensuring proper compensation controls [97].
- Analyze data using flow cytometry software to quantify immune cell subsets and activation markers.
Multi-Omics Data Integration and Ubiquitination Signature Development
The development of ubiquitination-based biomarker signatures requires sophisticated computational approaches for integrating diverse data types:
Data Integration and Analysis Workflow:
- Data Generation: Collect matched genomic (WES/WGS), transcriptomic (RNA-seq), and proteomic (mass spectrometry) data from patient samples [95] [63].
- Quality Control: Apply stringent QC filters to each data modality to ensure data integrity [63].
- Ubiquitination Regulator Expression: Quantify expression of E3 ligases, DUBs, and other UBRs from transcriptomic and proteomic data [63].
- Pathway Activity Analysis: Correlate UBR expression with cancer hallmark pathway activities using gene set enrichment analysis (GSEA) or similar approaches [63].
- Network Construction: Build protein-protein interaction networks of correlated UBRs using databases such as STRING [63].
- Hub Gene Identification: Apply topological algorithms (EPC, Degree, MNC, Closeness) to identify hub UBRs within the network [63].
- Patient Stratification: Perform consensus clustering based on hub UBR expression to define molecular subtypes [63].
- Signature Validation: Validate ubiquitination signatures in independent cohorts and functional models [63].
Visualization of Ubiquitination Signaling Networks
Ubiquitin-Mediated PD-L1 Regulation Pathway
Multi-Omics Biomarker Discovery Workflow
Research Reagent Solutions for Ubiquitination Studies
Table 3: Essential Research Reagents for Ubiquitination Biomarker Development
| Reagent Category | Specific Examples | Research Application | Technical Considerations |
|---|---|---|---|
| Ubiquitination Assays | Ubiquitin remnant motifs (K-ε-GG) antibodies, TUBE (Tandem Ubiquitin Binding Entity) reagents, activity-based DUB probes [63] | Detection and enrichment of ubiquitinated proteins; DUB activity profiling | Specificity for different ubiquitin chain linkages; compatibility with mass spectrometry |
| Flow Cytometry Reagents | Fluorochrome-conjugated antibodies against PD-1, PD-L1, immune cell markers; cell viability dyes; intracellular staining kits [97] | Immune profiling; checkpoint protein quantification; phospho-flow signaling analysis | Panel design for high-parameter cytometry; compensation controls; fixation/permeabilization optimization |
| Multi-Omics Platforms | RNA sequencing kits; single-cell RNA-seq solutions; mass spectrometry reagents; multiplex IHC/IF panels [95] | Comprehensive molecular profiling; spatial context preservation; single-cell resolution analysis | Sample quality requirements; data integration frameworks; computational infrastructure needs |
| Preclinical Models | Patient-derived xenografts (PDX); organoid cultures; CRISPR-modified cell lines [95] | Functional validation of biomarker candidates; therapeutic efficacy testing; mechanism of action studies | Maintenance of original tumor characteristics; scalability for high-throughput screening |
| Small Molecule Inhibitors | MLN4924 (E1 inhibitor), nutlin (E3 targeter), compound G5 (DUB inhibitor), canagliflozin (indirect modulator) [5] [63] | Functional modulation of ubiquitination pathways; therapeutic intervention studies | Specificity for target enzymes; potential off-target effects; combinatorial synergy with immunotherapies |
The integration of ubiquitination signaling knowledge with advanced biomarker development holds transformative potential for precision oncology. As detailed in this technical guide, ubiquitination networks provide a rich source of biomarkers for patient stratification, particularly in the context of immunotherapy response prediction. The continued refinement of multi-omics technologies, coupled with robust computational frameworks for data integration, will enable increasingly sophisticated classification of patients based on their tumor's ubiquitination status.
Future directions in this field include the development of standardized ubiquitination signature panels for clinical deployment, the validation of ubiquitination-based companion diagnostics for targeted therapies, and the implementation of real-time ubiquitination monitoring to track treatment response and resistance evolution. By leveraging the strategic position of ubiquitination signaling within critical cancer pathways, researchers and clinicians can advance toward truly personalized treatment approaches that maximize efficacy while minimizing toxicity.
Formulation and Delivery Challenges for Ubiquitin-Targeting Therapeutics
The ubiquitin-proteasome system (UPS) is a crucial regulatory mechanism for protein degradation in eukaryotic cells, involving a cascade of enzymes (E1, E2, and E3) that tag target proteins with ubiquitin for proteasomal destruction [82]. Within the tumor microenvironment (TME), this system exerts profound influence on cancer progression through multiple mechanisms, including the regulation of immune checkpoint proteins such as PD-1/PD-L1 [5]. The emergence of targeted protein degradation (TPD) technologies, particularly proteolysis-targeting chimeras (PROTACs), represents a paradigm shift in therapeutic strategy by harnessing the UPS to eliminate disease-causing proteins rather than merely inhibiting their function [98] [99]. These heterobifunctional molecules simultaneously bind to a protein of interest (POI) and an E3 ubiquitin ligase, facilitating ubiquitination and subsequent degradation of the target [100]. While this approach offers significant advantages for tackling traditionally "undruggable" targets and overcoming drug resistance, the translation of ubiquitin-targeting therapeutics from bench to bedside faces substantial formulation and delivery challenges that must be addressed to realize their full clinical potential [101] [98].
Core Challenges in PROTAC Formulation and Delivery
Inherent Physicochemical Properties
PROTACs possess molecular characteristics that inherently complicate their delivery and formulation. Their high molecular weight (often 700-1,200 Da), extensive polar surface area, and multiple hydrogen bond donors and acceptors contribute to what has been termed 'molecular obesity' [101]. These properties directly impact critical pharmaceutical parameters:
- Low Aqueous Solubility: The complex molecular structure comprising a target protein ligand, E3 ligase ligand, and linker creates highly hydrophobic compounds with poor water solubility, impeding absorption and bioavailability [101] [98].
- Limited Cell Permeability: The high molecular weight and polar surfaces hinder passive diffusion across cell membranes, restricting access to intracellular UPS machinery [100] [101].
- Suboptimal Pharmacokinetics: Rapid clearance and poor stability in physiological environments further limit therapeutic exposure and efficacy [100].
Table 1: Key Physicochemical Challenges of PROTACs
| Challenge | Structural Basis | Impact on Delivery |
|---|---|---|
| High Molecular Weight | Bifunctional structure with linker | Poor membrane permeability |
| High Hydrophobicity | Aromatic rings, hydrocarbon chains | Low aqueous solubility |
| Polar Surface Area | Multiple H-bond donors/acceptors | Limited cellular uptake |
| Molecular Flexibility | Rotatable bonds in linker | Conformational instability |
Pharmacological Challenges
Beyond physicochemical barriers, PROTACs exhibit unique pharmacological behaviors that complicate their clinical application:
- Hook Effect: A concentration-dependent phenomenon where high PROTAC concentrations favor the formation of non-productive binary complexes (PROTAC-POI or PROTAC-E3) over functional ternary complexes, paradoxically reducing degradation efficacy [100] [101].
- Off-Target Effects: Potential degradation of proteins with structural similarities to the intended target, leading to unintended toxicities [100].
- On-Target Side Effects: Excessive degradation of proteins that play essential roles in normal physiological processes can cause adverse effects [100].
Advanced Delivery Strategies and Formulation Technologies
Nano-Delivery Systems
Nanoparticle-based delivery approaches have shown significant promise in overcoming PROTAC limitations:
- Lipid-Based Nanoparticles: These systems enhance solubility and protect PROTACs from premature degradation, with some formulations demonstrating improved therapeutic outcomes in preclinical cancer models [101].
- Polymeric Micelles: Amphiphilic block copolymers that self-assemble into core-shell structures, encapsulating hydrophobic PROTACs in the core while providing a hydrophilic exterior for improved biocompatibility and circulation time [101].
- Liposomes and Exosomes: Spherical vesicles with lipid bilayers that can encapsulate both hydrophilic and hydrophobic compounds, offering enhanced tissue targeting and reduced clearance [101].
Chemical Modification and Conjugation Approaches
- Targeted Modifications: Attachment of targeting ligands (e.g., antibodies, peptides) to enhance accumulation in specific tissues or cell types [100].
- Prodrug Strategies: Design of inactive PROTAC precursors that undergo enzymatic activation in the target tissue, improving specificity and reducing off-target effects [100].
- Stimuli-Responsive Systems: Incorporation of cleavable linkers that respond to tumor microenvironment cues (e.g., pH, enzymes) for controlled release [100].
Solubility-Enhancing Formulation Techniques
Several established formulation technologies have been adapted to address PROTAC solubility challenges:
- Amorphous Solid Dispersions: Created through hot-melt extrusion or spray drying to transform crystalline PROTACs into amorphous forms with higher apparent solubility [98].
- Nano-Milling: Reduction of particle size to increase surface area and dissolution rate [98].
- Lipid-Based Formulations: Utilization of self-emulsifying drug delivery systems (SEDDS) that leverage natural lipid absorption pathways [98].
Table 2: Formulation Technologies for PROTAC Delivery
| Technology | Mechanism | Advantages |
|---|---|---|
| Spray Drying | Creates amorphous solid dispersions | Enhanced bioavailability, processing flexibility |
| Hot-Melt Extrusion | Generates molecular dispersions in polymer matrix | Continuous processing, solvent-free |
| Nano-Milling | Reduces particle size to nanoscale | Significantly increased dissolution rate |
| Lipid-Based Formulations | Enhances solubility via lipid digestion | Leverages natural absorption pathways |
Experimental Protocols for Assessing Delivery Challenges
Permeability and Cellular Uptake Studies
Protocol 1: Assessment of Cell Membrane Permeability
- Cell Culture: Grow appropriate cell lines (e.g., Caco-2 for intestinal absorption models) on transwell inserts until tight junction formation (typically 21 days).
- Dosing: Apply PROTAC formulation to the apical compartment at physiologically relevant concentrations.
- Sampling: Collect samples from the basolateral compartment at predetermined time points (e.g., 0.5, 1, 2, 4, 8 hours).
- Analysis: Quantify PROTAC concentration using LC-MS/MS to determine apparent permeability (Papp).
- Integrity Monitoring: Measure transepithelial electrical resistance (TEER) before and after experiments to confirm monolayer integrity [101].
Ternary Complex Formation and Hook Effect Evaluation
Protocol 2: Characterization of Hook Effect
- Dilution Series: Prepare a broad concentration range of PROTAC (e.g., 1 nM to 100 µM) in assay buffer.
- Incubation: Add fixed concentrations of POI and E3 ligase components to each PROTAC dilution.
- Detection: Employ techniques such as surface plasmon resonance (SPR) or fluorescence polarization to quantify ternary complex formation.
- Data Analysis: Plot degradation efficiency versus PROTAC concentration to identify the optimal concentration range and hook effect threshold [100] [101].
- Validation: Confirm findings in cellular models by measuring target protein degradation via western blotting across the same concentration range.
In Vivo Pharmacokinetic and Biodistribution Studies
Protocol 3: Preclinical PK/BD Assessment
- Formulation Preparation: Develop physiologically compatible formulations (e.g., nanoformulations, solubilized preparations) for intended administration route.
- Dosing Administration: Administer PROTAC to animal models (typically rodents) via relevant routes (oral, intravenous).
- Sample Collection: Collect blood samples at predetermined time points and euthanize subsets of animals at various intervals to harvest tissues of interest.
- Sample Processing: Extract PROTACs from biological matrices (plasma, tissue homogenates) using appropriate techniques (e.g., protein precipitation, liquid-liquid extraction).
- Bioanalysis: Quantify PROTAC concentrations using validated LC-MS/MS methods with stable isotope-labeled internal standards [101].
Diagram 1: PROTAC Delivery Challenge Solutions
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Key Research Reagents for PROTAC Delivery Studies
| Reagent/Material | Function | Application Examples |
|---|---|---|
| Caco-2 cell line | Model for intestinal permeability screening | Prediction of oral absorption potential |
| Surface Plasmon Resonance (SPR) | Quantification of binding kinetics and ternary complex formation | Assessment of hook effect and binding affinities |
| LC-MS/MS systems | Bioanalytical quantification of PROTACs in biological matrices | Pharmacokinetic studies and biodistribution analysis |
| Transwell inserts | Permeability assessment across cellular barriers | Measurement of apparent permeability (Papp) |
| Lipid nanoparticles (LNPs) | Nano-delivery vehicle for hydrophobic compounds | Solubility enhancement and targeted delivery |
| Poly(lactic-co-glycolic acid) (PLGA) | Biodegradable polymer for controlled release | Sustained release formulations for PROTACs |
The formulation and delivery of ubiquitin-targeting therapeutics represent both a significant challenge and opportunity in advancing cancer treatment, particularly within the complex context of the tumor microenvironment. While PROTACs and related TPD technologies offer unprecedented potential for targeting previously undruggable proteins in oncology, their translation to clinical application requires sophisticated formulation approaches that address their inherent physicochemical limitations. The convergence of advanced delivery technologies—including nanoformulations, lipid-based systems, and stimuli-responsive platforms—with increasingly sophisticated PROTAC design holds promise for overcoming these hurdles. As the field progresses, key areas for future development include expanding the repertoire of E3 ligase ligands, enhancing tissue-specific targeting, and optimizing administration routes to maximize therapeutic efficacy while minimizing off-target effects. With continued innovation in formulation science and delivery technology, ubiquitin-targeting therapeutics are poised to revolutionize cancer treatment and potentially address other complex diseases driven by pathological protein accumulation.
Comparative Efficacy and Future Directions in Ubiquitin-Targeted Therapies
Targeted protein degradation (TPD) represents a transformative approach in drug discovery that fundamentally challenges the conventional pharmacology model. Unlike traditional small-molecule inhibitors that merely block protein activity, TPD strategies leverage the cell's intrinsic protein quality control machinery to achieve complete and irreversible removal of disease-causing proteins [102] [88]. This paradigm shift moves therapeutic intervention from an "occupancy-driven" model, where continuous drug presence is required to suppress protein function, to an "event-driven" model, where a single drug molecule can catalyze multiple rounds of protein degradation [103]. Within the specific context of tumor microenvironment research, the ubiquitin-proteasome system (UPS) offers unprecedented opportunities for modulating immune checkpoint proteins, transcription factors, and other challenging targets that drive tumor immune evasion and cancer progression [5].
The ubiquitin-proteasome system serves as the primary executioner for intracellular protein degradation in eukaryotic cells. This sophisticated machinery involves a cascade of enzymes (E1 activating, E2 conjugating, and E3 ubiquitin ligase enzymes) that tag target proteins with ubiquitin chains, marking them for destruction by the 26S proteasome [88] [103]. The specificity of this process is largely determined by E3 ubiquitin ligases, which recognize specific substrate proteins. The therapeutic exploitation of this natural process has given rise to two prominent TPD modalities: PROteolysis TArgeting Chimeras (PROTACs) and Molecular Glues, each with distinct mechanisms, advantages, and limitations when compared to conventional inhibitors [102] [88].
Molecular Mechanisms and Signaling Pathways
The Ubiquitin-Proteasome System in Protein Homeostasis
The ubiquitin-proteasome system maintains cellular proteostasis through a highly coordinated enzymatic cascade. The process begins with E1 ubiquitin-activating enzyme that activates ubiquitin in an ATP-dependent manner. The activated ubiquitin is then transferred to an E2 conjugating enzyme, and finally, an E3 ubiquitin ligase facilitates the transfer of ubiquitin to the target protein [88] [5]. Repeated cycles of this process result in polyubiquitination, with K48-linked ubiquitin chains serving as the primary signal for proteasomal recognition and degradation [88]. The 26S proteasome, composed of a 20S core particle and 19S regulatory particles, recognizes polyubiquitinated proteins, deubiquitinates them, and unfolds and degrades them into short peptides [5].
Figure 1: The Ubiquitin-Proteasome System Pathway. This diagram illustrates the sequential enzymatic cascade involving E1, E2, and E3 enzymes that results in polyubiquitination of target proteins and their subsequent degradation by the 26S proteasome.
Comparative Mechanisms of Action
Conventional inhibitors operate through an occupancy-driven mechanism where the drug molecule binds directly to an active site or allosteric pocket on the target protein, temporarily inhibiting its function. This approach requires sustained drug exposure and high target occupancy to maintain therapeutic effect [102] [104]. The efficacy is directly proportional to drug concentration and binding affinity, necessitating high doses that often lead to off-target effects and dose-limiting toxicities.
PROTACs (Proteolysis-Targeting Chimeras) are heterobifunctional molecules consisting of three key elements: a target protein-binding ligand, an E3 ubiquitin ligase-recruiting ligand, and a chemical linker that connects these two moieties [88] [81]. The PROTAC molecule simultaneously engages both the target protein and an E3 ubiquitin ligase, forming a ternary complex that induces ubiquitin transfer to the target protein. This ubiquitination marks the target for proteasomal degradation [103]. The catalytic nature of PROTACs enables a single molecule to facilitate the degradation of multiple target proteins, providing sustained effects at sub-stoichiometric concentrations [81].
Molecular Glue Degraders are typically monovalent small molecules that induce or stabilize protein-protein interactions between an E3 ubiquitin ligase and a target protein that would not naturally interact [102] [105]. Unlike PROTACs, molecular glues lack a linker and often function by binding to one protein (frequently the E3 ligase) and inducing conformational changes that create a novel binding surface complementary to the target protein [106]. This "surface remodeling" facilitates the formation of a ternary complex leading to ubiquitination and degradation of the target protein [102].
Figure 2: Comparative Mechanisms of Conventional Inhibitors, PROTACs, and Molecular Glues. This diagram illustrates the fundamental differences in how each modality engages with its target protein and E3 ubiquitin ligase to achieve therapeutic effects.
Comparative Analysis of Therapeutic Modalities
Structural and Physicochemical Properties
The structural differences between these therapeutic modalities directly influence their drug-like properties and development considerations. Conventional small-molecule inhibitors typically have low molecular weights (<500 Da) and are designed to comply with Lipinski's Rule of Five, resulting in favorable oral bioavailability and membrane permeability [102]. PROTACs, as heterobifunctional molecules with a connecting linker, have significantly higher molecular weights (typically 700-1200 Da), which can challenge their cellular permeability, oral bioavailability, and overall drug-likeness [103] [81]. Molecular glues occupy a middle ground with molecular weights generally below 500 Da, resembling conventional drugs in size while functioning through a degradation mechanism [105].
Table 1: Structural and Physicochemical Properties Comparison
| Property | Conventional Inhibitors | PROTACs | Molecular Glues |
|---|---|---|---|
| Molecular Structure | Monovalent | Heterobifunctional (two ligands + linker) | Monovalent |
| Molecular Weight | Low (<500 Da) | High (700-1200 Da) | Low (<500 Da) |
| Linker Requirement | Not applicable | Required for connecting ligands | Linker-less |
| Oral Bioavailability | Generally favorable | Often challenging due to size/lipophilicity | Generally favorable |
| Blood-Brain Barrier Penetration | Achievable with careful design | More challenging for CNS targets | Generally more favorable |
| Catalytic Activity | No (stoichiometric) | Yes (event-driven) | Yes (event-driven) |
Pharmacological and Therapeutic Advantages
Conventional Inhibitors benefit from well-established development paradigms, predictable structure-activity relationships, and generally favorable pharmacokinetic profiles. However, they typically require high systemic exposure to maintain target inhibition, which increases the risk of off-target effects [102]. They are also limited to targets with well-defined binding pockets and may produce incomplete inhibition or compensatory adaptive responses [104].
PROTACs offer several transformative advantages, including the ability to target proteins previously considered "undruggable" due to the lack of functional binding pockets [81]. Their catalytic mechanism enables potent and sustained target suppression at sub-stoichiometric concentrations, potentially reducing dosing frequency and toxicity [103]. PROTACs can achieve more complete pathway suppression by eliminating all protein functions (scaffolding, enzymatic, structural) rather than just inhibiting a single activity [88]. This complete elimination may also help overcome drug resistance mechanisms such as target overexpression or mutations that reduce drug binding affinity [81].
Molecular Glues share the catalytic degradation advantages of PROTACs while maintaining more drug-like properties due to their smaller size [105]. Their monovalent structure typically results in better oral bioavailability, tissue penetration, and potentially enhanced blood-brain barrier penetration for central nervous system targets [103]. Molecular glues can induce degradation of proteins that lack deep binding pockets by surface manipulation, further expanding the druggable proteome [102].
Table 2: Therapeutic Advantages and Limitations
| Parameter | Conventional Inhibitors | PROTACs | Molecular Glues |
|---|---|---|---|
| Target Scope | Limited to proteins with suitable binding pockets | Expanded to many "undruggable" targets | Expanded to proteins without deep binding pockets |
| Resistance Potential | Higher (target mutations, overexpression) | Lower (target elimination) | Lower (target elimination) |
| Dosing Requirements | High, sustained exposure | Lower, less frequent dosing | Lower, less frequent dosing |
| Discovery Approach | Rational design, high-throughput screening | Rational, modular design | Historically serendipitous, increasingly rational |
| Major Challenges | Off-target effects, incomplete inhibition | Poor permeability, hook effect | Limited E3 ligase repertoire, discovery difficulty |
Applications in Tumor Microenvironment and Cancer Immunotherapy
The tumor microenvironment represents a particularly promising application for TPD strategies, especially given the critical role of ubiquitination in regulating immune checkpoint proteins [5]. Research has demonstrated that the ubiquitin-proteasome system dynamically regulates the surface expression of PD-1/PD-L1, a fundamental immune checkpoint axis in tumor immune evasion [5].
Several E3 ubiquitin ligases, including SPOP, have been shown to mediate PD-L1 ubiquitination and degradation. In colorectal cancer cells, SPOP promotes ubiquitination and degradation of PD-L1, while ALDH2 competes with SPOP for PD-L1 binding, thereby stabilizing PD-L1 and promoting immune evasion [5]. Similarly, in hepatocellular carcinoma, BCLAF1 inhibits SPOP-mediated PD-L1 ubiquitination, enhancing PD-L1 stability and facilitating immune escape [5]. These findings highlight the potential of targeted degradation approaches to modulate immune checkpoint expression in the tumor microenvironment.
PROTACs and molecular glues offer distinct advantages in this context. PROTACs could be designed to specifically target and degrade immune checkpoint proteins like PD-L1, potentially overcoming limitations of antibody-based therapies [5]. Molecular glues such as thalidomide analogs (lenalidomide, pomalidomide) have already demonstrated clinical efficacy in hematological malignancies by degrading transcription factors IKZF1 and IKZF3 through cereblon recruitment [88] [105]. These clinically validated examples provide proof-of-concept for TPD approaches in cancer therapy.
Experimental Approaches and Research Methodologies
Screening Strategies for Degrader Discovery
The discovery and development of degraders requires specialized screening approaches that differ significantly from conventional inhibitor development.
For PROTACs, the development process typically follows a more rational design approach [103]. It begins with the identification of suitable ligands for the target protein and selected E3 ubiquitin ligase. These ligands are connected via synthetic linkers of varying composition and length, followed by systematic optimization of the ternary complex formation and degradation efficiency [102]. Key parameters evaluated during PROTAC development include DC50 (concentration required for half-maximal degradation), Dmax (maximum degradation achievable), and catalytic efficiency [106].
For Molecular Glues, discovery has historically been serendipitous but is increasingly incorporating systematic approaches [106] [105]. Phenotype-based screening in live-cell systems enables identification of compounds that induce target degradation without prior knowledge of the mechanism or involved E3 ligases [106]. Follow-up mechanistic studies using CRISPR screening, chemoproteomics, and quantitative proteomics help identify the relevant E3 ligase and degradation machinery [106]. Alternative approaches include screening focused compound libraries derived from known E3 ligase or target ligands with strategic appendages to explore molecular glue chemical space [106].
Key Assays and Validation Methods
Degradation Efficiency Assessment:
- Immunoblotting: Time- and concentration-dependent measurement of target protein levels [106]
- Quantitative Proteomics: Global profiling of protein abundance changes to assess selectivity [103] [106]
- Pulse-Chase Analysis: Direct measurement of protein half-life and degradation kinetics [102]
Mechanistic Validation:
- Ternary Complex Formation: Techniques such as surface plasmon resonance (SPR) and isothermal titration calorimetry (ITC) to characterize complex stability [102]
- Genetic Validation: CRISPR-based knockout of candidate E3 ligases or other UPS components to confirm mechanistic requirements [106]
- Ubiquitination Assays: Direct detection of target protein ubiquitination using mass spectrometry or ubiquitin pulldown approaches [5]
Functional Consequences:
- Cellular Proliferation/Viability Assays: Correlation of degradation with functional outcomes [104]
- Pathway Modulation: Assessment of downstream signaling consequences of target elimination [81]
- Immune Function Assays: For immunooncology targets, evaluation of T-cell activation, cytokine production, and cytotoxicity [5]
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Research Reagents for TPD Investigations
| Reagent Category | Specific Examples | Research Applications |
|---|---|---|
| E3 Ligase Ligands | Thalidomide analogs (CRBN), VHL ligands, MDM2 ligands | PROTAC construction, E3 engagement validation |
| Proteasome Inhibitors | Bortezomib, MG132, Carfilzomib | Confirmation of proteasome-dependent degradation |
| Ubiquitination Assay Reagents | Ubiquitin mutants (K48-only, K63-only), DUB inhibitors | Mechanism validation, ubiquitin chain topology determination |
| CRISPR Libraries | E3 ligase knockout pools, UPS component libraries | Identification of required degradation machinery |
| Protein Degradation Reporters | HaloTag, NanoLuc fusion constructs | High-throughput degradation screening |
| Proteomics Platforms | TMT/iTRAQ labeling, DIA mass spectrometry | Global assessment of degradation selectivity |
Clinical Translation and Therapeutic Applications
Current Clinical Status and Case Studies
PROTAC Clinical Advancements: Several PROTACs have advanced to clinical trials, demonstrating proof-of-concept for this modality in humans. Bavdegalutamide (ARV-110), an androgen receptor (AR) degrader, has shown efficacy in metastatic castration-resistant prostate cancer patients who progressed on standard therapies [81]. Similarly, vepdegestrant (ARV-471), an oral estrogen receptor (ER) degrader, has progressed to phase 3 clinical trials for ER-positive/HER2-negative breast cancer [81]. These candidates demonstrate the ability of PROTACs to achieve therapeutic target degradation in humans, even in treatment-resistant settings.
Molecular Glue Clinical Success: The immunomodulatory drugs (IMiDs) thalidomide, lenalidomide, and pomalidomide represent the most successful examples of molecular glue degraders, approved for multiple myeloma and other hematological malignancies [88] [105]. These compounds bind to the CRBN E3 ligase and induce degradation of transcription factors IKZF1 and IKZF3, demonstrating the therapeutic potential of targeted degradation [88]. Interestingly, these agents were used clinically for years before their degradation mechanism was fully elucidated [88].
Emerging Trends and Future Directions
The TPD field is rapidly evolving with several promising developments. Expanding the E3 Ligase Toolbox is a priority, as current approaches predominantly utilize a limited set of E3s (CRBN, VHL, IAP) [103]. Discovering ligands for tissue-specific or disease-associated E3 ligases could enable more precise targeting. Dual-targeting Approaches including dual-PROTACs and heterobifunctional degraders that simultaneously engage multiple targets or pathways offer potential for addressing complex diseases and overcoming redundancy [88].
Tissue-Specific Delivery Strategies such as antibody-PROTAC conjugates, nanoparticle formulations, and cell-penetrating peptide conjugates are being explored to improve the pharmacokinetic profiles and tissue specificity of degraders [81]. Additionally, Novel Degradation Modalities including lysosome-targeting chimeras (LYTACs), antibody-based PROTACs (AbTACs), and autophagy-targeting chimeras (AUTACs) are expanding the scope of TPD beyond the ubiquitin-proteasome system to target extracellular proteins, membrane receptors, and organelles [88].
The head-to-head analysis of PROTACs, molecular glues, and conventional inhibitors reveals a compelling evolution in therapeutic paradigms. Conventional inhibitors remain valuable for targets with well-defined binding pockets where transient inhibition suffices. PROTACs offer a modular, rational approach to target elimination that dramatically expands the druggable proteome, albeit with significant pharmacokinetic challenges. Molecular glues represent an elegant compromise, combining the catalytic efficiency of degradation with favorable drug-like properties, though their discovery remains challenging.
Within the context of tumor microenvironment research and ubiquitination signaling, TPD strategies offer unprecedented opportunities to manipulate previously intractable targets, particularly immune checkpoint proteins, transcription factors, and scaffolding proteins that drive cancer progression and immune evasion. As the field advances, the integration of structural biology, computational prediction, and sophisticated screening methodologies will likely accelerate the discovery and optimization of both PROTACs and molecular glues.
The ongoing clinical validation of these modalities, particularly the PROTAC candidates in advanced trials and the established clinical benefits of molecular glue degraders like lenalidomide, suggests that targeted protein degradation will play an increasingly prominent role in cancer therapy and beyond. For research professionals and drug developers, understanding the distinct advantages, limitations, and appropriate applications of each modality is essential for leveraging their full potential in the development of next-generation therapeutics.
Comparative Clinical Outcomes Across Cancer Types and TME Subtypes
Abstract The tumor microenvironment (TME) is a complex and dynamic ecosystem where the interplay between cancer cells, immune cells, and stromal components dictates disease progression and therapeutic response. Within this niche, post-translational modifications, particularly ubiquitination, have emerged as master regulators of immune checkpoint expression and cellular crosstalk. This whitepaper synthesizes recent clinical and single-cell evidence to delineate how TME subtypes, modulated by the ubiquitin-proteasome system, influence clinical outcomes across cancers. We provide a comparative analysis of immune checkpoint inhibitor (ICI) efficacy, detail experimental protocols for TME deconvolution, and visualize key signaling networks, offering a resource for developing novel ubiquitination-targeted therapies.
The clinical success of cancer immunotherapy, particularly immune checkpoint inhibitors (ICIs) targeting the PD-1/PD-L1 axis, has reshaped oncology landscapes. However, positive response rates remain low, generally around only 15% in many cases, highlighting the critical need for predictive biomarkers and combination strategies [61]. The TME is no longer a passive bystander but an active participant in tumorigenesis, immune evasion, and therapy resistance. Its composition—encompassing heterogeneous immune cells like tumor-associated macrophages (TAMs) and regulatory T cells (Tregs), cancer-associated fibroblasts (CAFs), and the extracellular matrix (ECM)—creates distinct functional subtypes that correlate with patient prognosis [107].
Central to regulating the protein stability and function of key players within the TME is the ubiquitin-proteasome system (UPS). The UPS is responsible for 80-90% of cellular proteolysis and involves a sequential cascade mediated by E1 (activating), E2 (conjugating), and E3 (ligating) enzymes, which tag proteins for degradation [77]. Conversely, deubiquitinating enzymes (DUBs) can reverse this process. Dysregulation of this system is a feature of various cancers. For instance, the deubiquitinase USP2 can stabilize PD-1, promoting tumor immune escape, while the E2 enzyme UBE2T is associated with poor clinical outcomes and immune cell infiltration in pan-cancer analyses [77] [108]. This positions the ubiquitin machinery as a pivotal layer of control over the TME and a promising frontier for therapeutic intervention.
Clinical Outcomes: A Tale of Tumors and Their Microenvironments
Clinical outcomes following ICI therapy vary significantly across cancer types and are intimately linked to the specific cellular and molecular makeup of the TME. Metrics such as the Tumor Proportion Score (TPS) and Combined Positive Score (CPS) for PD-L1 expression are used as predictive biomarkers for ICI response [61].
Table 1: Selected FDA-Approved PD-1/PD-L1 Inhibitors and Associated Cancers
| Generic Name | Target | Key Cancer Indications | Notable Clinical Outcomes |
|---|---|---|---|
| Pembrolizumab [61] | PD-1 | Melanoma, NSCLC, HNSCC, RCC | In high PD-L1 (TPS ≥50%) NSCLC, monotherapy improved OS to 30.0 mo vs. 14.2 mo with chemo [61]. |
| Nivolumab [61] | PD-1 | Melanoma, NSCLC, RCC, cHL | Superior to docetaxel in post-platinum NSCLC; combined with ipilimumab, benefits patients with TPS ≥1% [61]. |
| Atezolizumab [61] | PD-L1 | NSCLC, SCLC, HCC, Bladder Cancer | Improves outcomes as monotherapy in metastatic NSCLC and as consolidation after chemoradiation in stage III disease [61]. |
| Durvalumab [61] | PD-L1 | NSCLC, SCLC, HCC | Demonstrates prolonged PFS and OS versus placebo in specific settings [61]. |
| Cemiplimab [61] | PD-1 | CSCC, NSCLC | With platinum chemo in 1st-line NSCLC, increased OS (21.9 vs. 13.0 mo) and PFS (8.2 vs. 5.0 mo) [61]. |
The TME's cellular composition is a critical determinant of these outcomes. Single-cell transcriptomic analyses have revealed that specific immune cell subtypes within the TME are linked to metastasis and poor prognosis.
Table 2: TME Cell Subtypes and Their Impact on Clinical Outcomes
| Cell Subtype | Pro-Tumorigenic Role | Association with Clinical Outcomes |
|---|---|---|
| CCL18+ TAMs [107] | Express PD-L1 and VEGF-A; facilitate immune evasion and angiogenesis. | Promotes metastasis; associated with immunosuppressive TME. |
| FCN1+ TAMs [107] | Secrete IL-1β and TNF-α; enhance CD8+ T cell activation. | May be associated with improved anti-tumor immunity. |
| M2-like TAMs [109] | Exhibit immunosuppressive activity. | Presence in papillary thyroid carcinoma (PTC) is associated with lymph node metastasis [109]. |
| Tregs [107] [109] | Inhibit effector T cell activation via non-coding RNAs (e.g., miR-155, FOXP3-AS1). | Contribute to immune evasion; enriched in metastatic PTC [109]. |
| DC2s (LAMP3+ CCL22+) [109] | Recruit CD4+ T cells and possess various immune-related ligands. | Associated with advanced stage and metastasis in PTC [109]. |
The Ubiquitin-Mediated Molecular Underpinnings of the TME
Ubiquitination and deubiquitination are rapid and reversible mechanisms that precisely control the abundance of proteins critical for TME function. This regulation impacts immune checkpoint expression, metabolic reprogramming, and cell signaling pathways.
3.1 Regulating Immune Checkpoints The stability of PD-L1 on cancer cells and PD-1 on T cells is directly controlled by the UPS. For example, the E3 ligase AIP4 mediates the monoubiquitination of PD-L1 at K263, leading to its internalization and lysosomal degradation, thereby inhibiting immune escape in lung adenocarcinoma [77]. Conversely, the deubiquitinase USP2 can remove ubiquitin from PD-1, stabilizing it and promoting T cell exhaustion and tumor immune escape [77].
3.2 Controlling TME Cell Fate and Metabolism The UPS also dictates the behavior of TME components. In hepatocellular carcinoma, the E3 ligase RNF2 monoubiquitinates histone H2A, repressing E-cadherin transcription and enhancing metastatic potential [77]. Metabolic reprogramming, a hallmark of cancer, is similarly regulated. The E3 ligase Parkin facilitates the ubiquitination of the glycolytic enzyme PKM2, while the deubiquitinase OTUB2 inhibits this process, enhancing glycolysis and accelerating colorectal cancer progression [77].
Experimental Protocols for TME and Ubiquitination Analysis
To investigate the TME and the role of ubiquitination, researchers employ a suite of advanced molecular and bioinformatic techniques.
4.1 Single-Cell RNA Sequencing (scRNA-seq) Workflow This protocol allows for the deconvolution of the TME at a single-cell resolution [109].
- Tissue Dissociation: Fresh tumor and adjacent normal tissues are minced and digested enzymatically (e.g., with sCelLive Tissue Dissociation Solution) using a tissue dissociation system at 37°C for 15 minutes.
- Cell Suspension Preparation: The digest is filtered through a 40μm strainer, centrifuged, and the cell pellet is resuspended in PBS. Cell viability is assessed using Trypan blue staining.
- Library Preparation: Single-cell suspensions are loaded onto a microwell chip. Barcoding beads capture mRNA from individual cells. The process includes reverse transcription, cDNA amplification, fragmentation, and adapter ligation to create sequencing libraries using kits like GEXSCOPE.
- Sequencing and Data Analysis: Libraries are sequenced on a platform such as Illumina Novaseq 6000. Raw data is processed through pipelines (e.g., CeleScope) for quality control, read alignment (to GRCh38 with STAR), and generation of a gene expression matrix using featureCounts.
- Bioinformatic Analysis: Using Seurat in R, data undergoes quality control (filtering cells with <200 genes, high mitochondrial content), normalization, dimensional reduction (PCA, UMAP), and cluster identification. Differential expression analysis then defines cell subtypes and states.
4.2 Analyzing Ubiquitin-Related Enzyme Expression in Pan-Cancer This bioinformatic protocol assesses the role of enzymes like UBE2T across cancers [108].
- Data Acquisition: Download RNA sequencing data from public repositories like The Cancer Genome Atlas (TCGA) and the Genotype-Tissue Expression (GTEx) project.
- Expression Analysis: Use tools like TIMER 2.0 and GEPIA2 to compare UBE2T expression between tumor and normal tissues across multiple cancer types. Statistical significance is assessed with the Wilcoxon test.
- Survival Analysis: Perform Kaplan-Meier analysis using patient data from TCGA to correlate UBE2T expression levels with overall survival (OS) and progression-free survival (PFS).
- Genetic Alteration Analysis: Utilize cBioPortal or GSCALite to determine the frequency and type of genetic alterations (e.g., amplification, mutations) in UBE2T.
- Immune Correlation: Employ the TIMER 2.0 database to investigate correlations between UBE2T expression and levels of immune cell infiltration or immune checkpoint gene expression.
4.3 In Vitro Validation of Ubiquitination
- Cell Culture: Culture relevant cancer cell lines and normal epithelial controls in standard media (e.g., DMEM with 10% FBS) [108].
- Gene/Protein Expression Analysis:
- RT-qPCR: Extract total RNA, reverse transcribe to cDNA, and perform qPCR with primers specific to the target gene (e.g., UBE2T) to measure mRNA levels [108].
- Western Blotting: Lyse cells in RIPA buffer with protease inhibitors. Separate proteins by SDS-PAGE, transfer to a PVDF membrane, and incubate with primary antibodies (e.g., anti-UBE2T) and HRP-conjugated secondary antibodies. Detect signals using chemiluminescence [108].
- Ubiquitination Assay: Transfect cells with plasmids expressing the protein of interest (e.g., PD-L1) and His-tagged ubiquitin. Treat cells with a proteasome inhibitor (e.g., MG132) for several hours. Lyse cells and perform immunoprecipitation under denaturing conditions with an antibody against the protein. Detect ubiquitination via western blot using an anti-Ub or anti-His antibody [77].
Visualization of Signaling Pathways and Experimental Workflows
Diagram 1: UPS regulation of PD-1/PD-L1. E3 ligases promote PD-L1 degradation via ubiquitination, while DUBs stabilize it. Stable PD-L1 binds PD-1, leading to T cell exhaustion [61] [77].
Diagram 2: scRNA-seq workflow for TME. Key steps from tissue processing to sequencing and data analysis reveal cellular heterogeneity [109].
Table 3: Key Reagents and Tools for TME and Ubiquitination Research
| Research Tool / Reagent | Function / Application | Example Use Case |
|---|---|---|
| GEXSCOPE Kit [109] | Library construction for single-cell RNA sequencing. | Profiling the immune cell atlas of papillary thyroid carcinoma [109]. |
| Seurat (R Package) [109] | Comprehensive toolkit for single-cell genomics data analysis. | Quality control, normalization, clustering, and differential expression analysis of scRNA-seq data [109]. |
| TCGA & GTEx Datasets [108] | Publicly available genomic data for pan-cancer analysis. | Comparing UBE2T expression between tumor and normal tissues across cancers [108]. |
| TIMER 2.0 & GEPIA2 [108] | Web-based tools for analyzing tumor-infiltrating immune cells and gene expression. | Correlating UBE2T expression with immune cell infiltration levels [108]. |
| Anti-UBE2T Antibody [108] | Detecting UBE2T protein levels via Western Blot. | Validating elevated UBE2T expression in pancreatic cancer cell lines vs. normal controls [108]. |
| Proteasome Inhibitor (MG132) [77] | Blocks proteasomal degradation, enriching for ubiquitinated proteins. | Used in ubiquitination assays to detect levels of ubiquitinated substrates like PD-L1 [77]. |
| cBioPortal [108] | Web resource for exploring and visualizing multidimensional cancer genomics data. | Analyzing the frequency and type of genetic alterations in UPS components like UBE2T [108]. |
The comparative analysis of clinical outcomes firmly establishes that TME subtypes are decisive factors in patient responses to therapy. The integration of scRNA-seq and pan-cancer genomic data provides an unprecedented view of this heterogeneity. The ubiquitin-proteasome system emerges as a central regulatory layer, controlling key immune checkpoints and cellular processes within the TME by fine-tuning protein stability. Future research must focus on integrating 4D spatiotemporal omics with AI-driven predictive models to dynamically monitor TME evolution [107]. Therapeutically, combining ICIs with agents that target the ubiquitin machinery—such as PROTACs, molecular glues, or inhibitors of specific E3 ligases and DUBs—represents a compelling strategy to reprogram the TME from immunosuppressive to immunopermissive, ultimately improving clinical outcomes for a broader range of cancer patients.
Validation of Novel Targets Through Preclinical Models and Functional Genomics
Ubiquitination, a crucial post-translational modification, has emerged as a central regulatory mechanism in tumorigenesis and the remodeling of the tumor microenvironment (TME). This process involves the covalent attachment of ubiquitin molecules to target proteins, thereby regulating their stability, activity, localization, and interactions [110] [111]. The ubiquitin-proteasome system (UPS) maintains precise control over numerous cellular proteins, with dysregulation contributing significantly to cancer pathogenesis [112]. Within the TME, ubiquitination modulates key biological processes including tumor metabolism, immune cell infiltration, and cancer stem cell maintenance [110]. The versatility of ubiquitination stems from its complexity—ranging from mono-ubiquitination to poly-ubiquitin chains with various linkage types—each generating distinct functional outcomes [111]. Understanding these intricate mechanisms provides a foundation for identifying and validating novel therapeutic targets in oncology.
Table 1: Key Ubiquitination-Related Processes in the Tumor Microenvironment
| Process | Key Molecular Regulators | Functional Impact in TME |
|---|---|---|
| Tumor Metabolism | RagA, mTOR, PTEN, AKT, c-Myc, P53 | Regulates mTORC1, AMPK, and PTEN-AKT signaling pathways [110] |
| Immunological TME | TLR, RLR, STING-dependent signaling | Modulates immune recognition and response [110] |
| Cancer Stem Cell Stemness | Nanog, Oct4, Sox2, Wnt, Hippo-YAP signaling | Maintains self-renewal and differentiation capacity [110] |
| Iron Metabolism & Ferroptosis | TFRC, FPN, NCOA4 | Regulates iron-dependent cell death in hepatocellular carcinoma [113] |
Target Identification: Ubiquitination-Related Biomarkers in Cancer
The initial phase of target validation relies on comprehensive identification of ubiquitination-related biomarkers across cancer types. Advanced genomic and transcriptomic analyses have revealed numerous ubiquitination-related genes (UbRGs) with significant diagnostic and prognostic value. In cervical cancer, integrative bioinformatics approaches identified five key biomarkers (MMP1, RNF2, TFRC, SPP1, and CXCL8) strongly associated with disease progression [112]. Similarly, in laryngeal squamous cell carcinoma (LSCC), researchers identified four ubiquitination-related biomarkers (WDR54, KAT2B, NBEAL2, and LNX1) through combined differential expression analysis and weighted gene co-expression network analysis (WGCNA) [114]. These biomarkers demonstrated significant diagnostic capability with area under curve (AUC) values exceeding 0.7 in receiver operating characteristic (ROC) analysis [114].
In lung adenocarcinoma (LUAD), a ubiquitination-related risk score (URRS) model was developed based on four genes (DTL, UBE2S, CISH, and STC1), effectively stratifying patients into high-risk and low-risk subgroups with distinct clinical outcomes [115]. The prognostic value of this model was validated across six external datasets, confirming its robustness [115]. Mantle cell lymphoma studies have further demonstrated the clinical relevance of ubiquitination pathways, with TP53 alterations and ATM mutations defining distinct prognostic subgroups that exhibit differential responses to immunochemotherapy [116]. These findings highlight the expanding repertoire of ubiquitination-related targets across diverse malignancies.
Table 2: Experimentally Validated Ubiquitination-Related Biomarkers in Human Cancers
| Cancer Type | Identified Biomarkers | Validation Method | Clinical Utility |
|---|---|---|---|
| Cervical Cancer | MMP1, RNF2, TFRC, SPP1, CXCL8 | RT-qPCR, Immune infiltration analysis, ROC curves (AUC >0.6 for 1/3/5 years) [112] | Prognostic stratification, immune microenvironment assessment [112] |
| Laryngeal Squamous Cell Carcinoma | WDR54, KAT2B, NBEAL2, LNX1 | RT-qPCR, ROC analysis (AUC ~0.7), Survival analysis [114] | Diagnostic prediction, therapeutic target identification [114] |
| Lung Adenocarcinoma | DTL, UBE2S, CISH, STC1 | Multivariate Cox regression, External validation (6 GEO datasets), RT-qPCR [115] | Risk stratification, treatment response prediction [115] |
| Mantle Cell Lymphoma | TP53, ATM, KMT2D, SMARCA4 | Whole exome sequencing, Targeted sequencing, Immunohistochemistry [116] | Molecular subtyping, therapy selection [116] |
Functional Validation: Methodologies and Experimental Protocols
Genomic and Transcriptomic Profiling Techniques
Comprehensive molecular profiling forms the foundation for functional validation of ubiquitination targets. DNA and RNA sequencing technologies enable the systematic identification of ubiquitination-related alterations across cancer genomes. For whole exome sequencing (WES), DNA samples are typically sequenced to an average coverage of 100-150x using platforms such as Illumina NovaSeq 6000 [116]. Somatic variants are identified through paired analysis of tumor and normal samples using validated bioinformatics pipelines like GATK. For transcriptomic analysis, RNA sequencing libraries are prepared from total RNA extracted with TRIzol reagent, with quality assessment performed using NanoDrop spectrophotometry and agarose gel electrophoresis [112]. Differential expression analysis of ubiquitination-related genes is conducted using DESeq2 with thresholds set at |log2Fold Change| > 2 and adjusted p-value < 0.05 [114]. Weighted gene co-expression network analysis (WGCNA) further identifies gene modules significantly associated with cancer phenotypes, with soft thresholding parameters optimized to achieve scale-free topology (R² > 0.9) [114].
Ubiquitination-Specific Proteomic Methodologies
Mass spectrometry-based proteomics has revolutionized the detection and characterization of ubiquitination events. Two primary enrichment strategies enable comprehensive ubiquitinome profiling: ubiquitin tagging-based approaches and antibody-based methods [111]. The ubiquitin tagging approach involves expressing affinity-tagged ubiquitin (6×His or Strep-tag) in cells, followed by purification under denaturing conditions using Ni-NTA or Strep-Tactin resins [111]. After tryptic digestion, ubiquitination sites are identified by mass spectrometry detection of the characteristic 114.04 Da mass shift on modified lysine residues [111]. Alternatively, antibody-based approaches utilize pan-specific ubiquitin antibodies (e.g., P4D1, FK1/FK2) or linkage-specific antibodies (e.g., K48-, K63-specific) to enrich endogenously ubiquitinated proteins from clinical samples without genetic manipulation [111]. For tissue samples, formalin-fixed paraffin-embedded (FFPE) sections are deparaffinized, rehydrated, and subjected to antigen retrieval before ubiquitin immunoprecipitation [116].
In Vitro and Preclinical Functional Assays
Functional validation of ubiquitination targets requires sophisticated cellular and animal models that recapitulate the tumor microenvironment. For in vitro studies, gene editing technologies including CRISPR/Cas9 enable precise manipulation of candidate ubiquitination regulators in cancer cell lines. Knockout and knockdown efficiencies are validated through Western blotting and quantitative RT-PCR [116]. Functional assays assess proliferation (CellTiter-Glo), apoptosis (Annexin V staining), cell cycle distribution (propidium iodide staining), and colony formation capacity [116]. For ubiquitination-specific functional assessment, cycloheximide chase experiments determine protein half-life, while co-immunoprecipitation assays identify E3 ligase-substrate relationships [111]. Preclinical validation employs patient-derived xenograft (PDX) models that maintain the original tumor's biological characteristics. Animals are monitored for tumor growth, metastasis, and overall survival, with tissues harvested for immunohistochemical analysis of ubiquitination markers and TME components [116]. Imaging mass cytometry (IMC) enables multiplexed spatial analysis of up to 40 markers simultaneously, providing insights into immune cell infiltration and exhaustion states within the TME [116].
Table 3: Research Reagent Solutions for Ubiquitination Studies
| Reagent/Category | Specific Examples | Function/Application |
|---|---|---|
| Ubiquitin Tagging Systems | 6×His-tagged Ub, Strep-tagged Ub, HA-Ub | Affinity purification of ubiquitinated proteins for mass spectrometry analysis [111] |
| Ubiquitin Antibodies | P4D1, FK1/FK2, Linkage-specific antibodies (K48, K63, M1) | Immunoprecipitation and detection of ubiquitinated proteins; linkage-specific analysis [111] |
| Ubiquitination Enzymes | E1 inhibitors (MLN7243, MLN4924), E2 inhibitors (Leucettamol A, CC0651), E3 inhibitors (Nutlin, MI-219) | Pharmacological modulation of ubiquitination cascade; target validation [110] |
| Proteasome Inhibitors | Bortezomib, Carfilzomib, Oprozomib, Ixazomib | Clinical validation of UPS targeting; induction of ER stress and apoptosis [110] |
| Deubiquitinase Inhibitors | Compounds G5, F6 | Targeting deubiquitination processes; stabilization of specific protein substrates [110] |
| Functional Assay Kits | Cycloheximide chase assay kits, Ubiquitination assay kits, Proteasome activity assays | Assessment of protein stability, ubiquitination status, and proteasomal function [111] |
Therapeutic Translation: Targeting Ubiquitination in Cancer
The ubiquitin-proteasome system presents multiple therapeutic opportunities for cancer intervention, with several classes of compounds demonstrating preclinical and clinical efficacy. Small molecule inhibitors targeting the proteasome, including bortezomib, carfilzomib, oprozomib, and ixazomib, have achieved tangible success in hematological malignancies [110]. Emerging therapeutic strategies focus on specific components of the ubiquitination machinery, including E1 enzymes (inhibited by MLN7243 and MLN4924), E2 enzymes (targeted by Leucettamol A and CC0651), and E3 ligases (inhibited by nutlin and MI-219) [110]. Additionally, deubiquitinase (DUB) inhibitors such as compounds G5 and F6 show promising antitumor activity in preclinical models [110].
The integration of ubiquitination-targeting agents with immunotherapies represents a promising frontier. Studies in lung adenocarcinoma demonstrate that high ubiquitination-related risk scores correlate with increased PD-1/PD-L1 expression, tumor mutation burden (TMB), and tumor neoantigen load (TNB), suggesting enhanced sensitivity to immune checkpoint blockade [115]. Similarly, mantle cell lymphoma analyses reveal distinct immune microenvironments in TP53-perturbed tumors, characterized by CD4⁺ T-cell exhaustion and M2-like myeloid skewing, presenting opportunities for combination therapies [116]. Ferroptosis induction through ubiquitination-mediated regulation of iron metabolism proteins (TFRC, FPN) offers another therapeutic avenue, particularly in hepatocellular carcinoma [113]. These approaches highlight the potential of ubiquitination-targeting strategies across cancer types with distinct molecular features.
The validation of novel ubiquitination-related targets through functional genomics and preclinical models represents a transformative approach in cancer therapeutics. The integration of multi-omics data, sophisticated bioinformatics analyses, and mechanistic studies in physiologically relevant models has uncovered critical regulators of tumor progression and TME remodeling. As our understanding of the ubiquitin code expands, so too does the repertoire of therapeutic strategies capable of selectively targeting oncogenic proteins while sparing normal cellular functions. The continued refinement of validation methodologies and preclinical models will accelerate the translation of ubiquitination-based discoveries into effective cancer therapies that ultimately improve patient outcomes.
Integrating Multi-Omics Data for Target Prioritization and Validation
The integration of multi-omics data represents a transformative approach for identifying and validating disease-relevant molecular targets, particularly within complex biological systems such as the ubiquitination signaling network in the tumor microenvironment (TME). This technical guide outlines a systematic framework that leverages cutting-edge computational strategies, including artificial intelligence and network-based analysis, to prioritize ubiquitination regulators with high therapeutic potential. Detailed experimental methodologies are provided for subsequent functional validation of candidate targets, with a focus on their roles in tumor progression and immune modulation. By bridging high-dimensional molecular data with rigorous experimental confirmation, this whitepaper provides researchers and drug development professionals with a comprehensive roadmap for target discovery in the context of ubiquitination signaling.
Ubiquitination, a critical reversible post-translational modification, regulates diverse cellular processes including protein stability, cell differentiation, and immunity through a complex enzymatic cascade involving E1 activating enzymes, E2 conjugating enzymes, E3 ligases, and deubiquitinases (DUBs). Dysregulation of ubiquitination regulators (UBRs) leads to destabilization of biological processes and contributes significantly to oncogenesis [63]. The tumor microenvironment represents a complex ecosystem where ubiquitination modulates critical processes including immune cell infiltration, stromal interactions, and therapeutic resistance [117]. However, the specific roles of UBRs within the TME remain inadequately characterized, creating a knowledge gap that impedes the development of targeted therapies.
Multi-omics integration has emerged as a powerful strategy to address this complexity, moving beyond traditional single-omics approaches that often fail to capture the interconnected nature of molecular regulation [118]. The staggering molecular heterogeneity of cancer demands innovative approaches that integrate diverse data types including genomics, transcriptomics, epigenomics, proteomics, and metabolomics to recover system-level signals often missed by single-modality studies [119]. When applied to ubiquitination research, multi-omics integration enables researchers to identify critical UBRs, delineate their regulatory networks, and prioritize the most promising therapeutic targets based on multidimensional evidence.
Table 1: Key Ubiquitination Regulator Categories and Functions
| Category | Function | Examples | Role in Cancer |
|---|---|---|---|
| Writers (E1/E2/E3) | Add ubiquitin molecules to substrate proteins | UBE2C, UBE2T, UBE2N | Promote degradation of tumor suppressors; drive cell cycle progression |
| Erasers (DUBs) | Remove ubiquitin from substrate proteins | USP7, USP10 | Stabilize oncoproteins; confer therapy resistance |
| Readers | Recognize ubiquitination modifications | Proteins with UBD/ULD domains | Link ubiquitination substrates to downstream events |
Computational Frameworks for Multi-Omics Data Integration
Data Preprocessing and Harmonization
The foundation of robust multi-omics integration begins with comprehensive data preprocessing to address the significant technical challenges inherent in combining diverse molecular datasets. Multi-omics data encounter formidable computational and statistical challenges rooted in intrinsic data heterogeneity, including dimensional disparities (from millions of genetic variants to thousands of metabolites), temporal heterogeneity, analytical platform diversity, and pervasive missing data [119]. Effective preprocessing requires rigorous quality control pipelines and normalization methods such as ComBat for batch correction, DESeq2 for RNA-seq, and quantile normalization for proteomics to enhance signal fidelity [119]. For ubiquitination-focused analyses, researchers should curate comprehensive UBR catalogs from existing literature and databases, then map multi-omics features to these regulatory components.
Integration Strategies and Algorithm Selection
Three primary integration strategies govern multi-omics analysis: early integration (combining raw data), intermediate integration (integrating at feature selection or extraction stages), and late integration (analyzing datasets separately before combining results) [118]. For UBR target prioritization, intermediate integration has demonstrated particular utility as it allows flexibility in handling modality-specific characteristics while identifying cross-omic patterns.
Artificial intelligence (AI), particularly machine learning (ML) and deep learning (DL), has emerged as the essential scaffold bridging multi-omics data to clinical decisions [119]. Unlike traditional statistics, AI excels at identifying non-linear patterns across high-dimensional spaces, making it uniquely suited for multi-omics integration. Advanced methods include:
- Graph Neural Networks (GNNs): Model protein-protein interaction networks perturbed by somatic mutations, prioritizing druggable hubs in cancer networks [119] [120].
- Multi-modal Transformers: Fuse diverse data types such as MRI radiomics with transcriptomic data to predict cancer progression [119].
- Genetic Programming: An evolutionary algorithm that optimizes feature selection and integration strategies, enabling identification of robust biomarkers [118].
Table 2: Multi-Omics Integration Methods for Ubiquitination Research
| Method Category | Key Algorithms | Strengths | Applications in UBR Research |
|---|---|---|---|
| Network-Based | MOGLAM, MoAGL-SA, DeepProg | Captures complex interactions; incorporates prior biological knowledge | Identifying hub UBRs in PPI networks; pathway enrichment analysis |
| Similarity-Based | Similarity Network Fusion | Preserves data structure; handles heterogeneous data | Identifying patient subgroups based on ubiquitination patterns |
| AI-Driven | Graph Neural Networks, Transformers | Scalable; identifies non-linear relationships | Predicting novel UBR-substrate relationships; drug response prediction |
| Latent Factor Models | MOFA+, Bayesian Group Factor Analysis | Distinguishes shared from modality-specific signals | Decomposing ubiquitination variation across omics layers |
Target Prioritization Through Network Analysis
Biological networks provide an organizational framework for multi-omics integration, as biomolecules do not perform their functions alone but rather interact to form complex networks [120]. For ubiquitination research, protein-protein interaction (PPI) networks offer particularly valuable insights, as UBRs frequently function within multi-protein complexes. A recent study on lung adenocarcinoma (LUAD) demonstrated the power of this approach, identifying 17 hub UBRs from high-confidence PPI networks using four topological algorithms (EPC, Degree, MNC, and Closeness) [63]. These hub UBRs showed widespread genetic alterations and expression perturbations in LUAD, with high expression typically detrimental to patient survival.
Diagram 1: Multi-omics target prioritization workflow for ubiquitination research.
Application to Ubiquitination Signaling in Tumor Microenvironment
Identifying Clinically Relevant Ubiquitination Regulators
When applying multi-omics integration to ubiquitination signaling in the TME, researchers can identify UBRs with significant clinical relevance through systematic analysis. A pan-cancer study of ubiquitin D (UBD) exemplifies this approach, revealing UBD overexpression in 29 cancer types linked to poor prognosis and higher histological grades [121]. The most common genetic variation was gene amplification, and patients with these alterations exhibited significantly reduced overall survival rates. Epigenetically, 16 cancer types showed reduced UBD promoter methylation, suggesting a potential mechanism for overexpression.
Another study focusing on hepatocellular carcinoma (HCC) revealed that ubiquitination-related genes are significantly upregulated in HCC tissues, with high expression levels correlating with poor patient prognosis [117]. Pathway analysis showed that these genes are enriched in key processes including cell cycle regulation, DNA repair, metabolic reprogramming, and p53 signaling. These UBRs contribute to the TME by promoting tumor cell proliferation, facilitating matrix remodeling, and enhancing angiogenesis.
Stratification by Ubiquitination Signatures
Multi-omics approaches enable molecular stratification based on ubiquitination patterns, revealing clinically distinct subgroups. Research in lung adenocarcinoma demonstrated that based on the expression profiles of hub UBRs, patients can be classified into two ubiquitination subtypes with significantly different characteristics [63]. These subtypes exhibit dramatic differences across multiple dimensions, including survival, expression level, mutation burden, female predominance, infiltration level, immune profile, and drug response.
The establishment of scoring systems based on ubiquitination signatures provides a quantitative framework for patient stratification. In LUAD, researchers developed a ubiquitination-related risk (UB_risk) score and found that patients with low scores are more likely to benefit from immunotherapy [63]. Similarly, in hepatocellular carcinoma, ubiquitination scores calculated across various TME cell types revealed how different levels of ubiquitination influence HCC progression [117].
Diagram 2: Ubiquitination cascade and functional outcomes.
Experimental Validation of Prioritized Targets
In Vitro Functional Assays
Following computational prioritization of UBR targets, rigorous experimental validation is essential to confirm their functional roles in oncogenesis and TME modulation. A comprehensive validation pipeline should include assays assessing proliferation, invasion, migration, and viability:
CCK-8 Assay: Cell viability can be assessed using the Cell Counting Kit-8 (CCK8) assay. After transfection with UBR-targeting constructs, cells are seeded into 96-well plates at optimal density (e.g., 2500 cells per well) and incubated at 37°C. CCK8 reagent is added to each well, followed by additional incubation for 4 hours at 37°C. The optical density value (OD450) is then measured using a microplate reader to quantify viable cells [117].
Transwell Assay: Cell migration and invasion can be evaluated using Transwell chambers, either coated with Matrigel for invasion assessment or uncoated for migration evaluation. Typically, 5 × 10^4 transfected cells are seeded into the upper chamber with serum-free medium, while complete medium is placed in the lower chamber. After 24 hours of culture, cells that have migrated or invaded through the membrane are fixed with 4% paraformaldehyde, stained with 0.1% crystal violet, and quantified using light microscopy [117].
Wound Healing Assay: Cellular migratory behavior can be analyzed using a wound healing assay, which provides detailed observations of movement patterns. Transfected cells are grown in six-well plates until approximately 80% confluence. A sterile pipette tip is used to create a linear scratch through the cell layer, establishing a uniform wound. After washing to remove detached cells, serum-free medium is added, and wound closure is documented at 0h and 24h using an inverted microscope, allowing measurement of migration distance [117].
Clonogenic Formation Assay: This assay evaluates the long-term proliferative potential and colony-forming efficiency of cells following UBR perturbation, providing insights into self-renewal capacity and cytotoxic effects.
Table 3: Experimental Protocols for UBR Functional Validation
| Assay Type | Key Steps | Parameters Measured | Interpretation |
|---|---|---|---|
| CCK-8 | Cell seeding, CCK8 reagent incubation, OD450 measurement | Cell viability and proliferation | UBR knockdown/overexpression impact on cell growth |
| Transwell | Chamber setup with/without Matrigel, cell fixation and staining | Migration and invasion capacity | UBR role in metastatic potential |
| Wound Healing | Scratch formation, time-lapse imaging, migration distance calculation | Cell migratory behavior | UBR function in cell motility |
| Clonogenic | Low-density plating, colony formation, staining and counting | Long-term proliferative potential | UBR effect on self-renewal capacity |
Molecular Validation Techniques
Molecular validation confirms the mechanistic relationships between prioritized UBRs and their proposed functions within the TME:
Knockdown/Overexpression Systems: Plasmid-based systems expressing shRNA specifically designed to target UBRs of interest (e.g., UBE2C) are constructed. During cultivation, cells are treated with viral supernatants and polybrene in the culture medium. After 24h incubation, cells are transferred to fresh medium containing puromycin for selection. Knockdown efficiency is confirmed 2 days later using qRT-PCR analysis [117].
qPCR Analysis: Total RNA extraction is performed using commercial kits according to manufacturer's guidelines. cDNA synthesis is conducted using reverse transcription kits, followed by real-time PCR analysis with appropriate reagents and primer sequences. The PCR reaction typically includes an initial pre-denaturation phase at 95°C for 15min, followed by 40 amplification cycles comprising denaturation at 95°C for 10s, annealing at 72°C for 20s, and extension at 60°C for 20s. PCR signals are calculated using the 2^−ΔΔCT method to determine relative gene expression levels [117].
The Scientist's Toolkit: Research Reagent Solutions
Table 4: Essential Research Reagents for Ubiquitination Studies
| Reagent/Category | Specific Examples | Function/Application | Implementation Notes |
|---|---|---|---|
| Cell Culture | DMEM with 10% FBS, penicillin/streptomycin | Maintenance of HCC cell lines (Huh7, Hep3B) | Standard cell culture conditions at 37°C in 5% CO2 environment |
| Transfection | Lipofectamine 3000, viral supernatants with polybrene | Introduction of UBR-targeting constructs | Puromycin selection post-transfection; efficiency confirmation via qPCR |
| RNA Analysis | RNA extraction kits, reverse transcription kits, SYBR Green reagents | Quantification of UBR expression levels | Primer design for specific UBRs (e.g., UBE2C: F-5'-GACCTCTCCTTGTTGCTGCC-3') |
| Functional Assays | CCK-8 reagent, Transwell chambers, Matrigel, crystal violet | Assessment of proliferation, migration, invasion | Optimal cell seeding density (5×10^4 for Transwell); 24h incubation periods |
| Antibodies | UBD/FAT10 antibodies, ubiquitin remnant motifs | Detection and quantification of ubiquitination | Validation in multiple cancer types (pan-cancer applications) |
The integration of multi-omics data provides an unprecedented opportunity to prioritize and validate ubiquitination regulators as therapeutic targets within the complex landscape of the tumor microenvironment. This technical guide outlines a systematic framework that combines computational approaches with experimental validation, enabling researchers to navigate the complexity of ubiquitination signaling in oncogenesis. As single-cell multi-omics technologies continue to advance, they offer increasingly refined resolution for dissecting tumor heterogeneity at the cellular level, further enhancing our ability to identify context-specific UBR dependencies [122].
Future developments in this field will likely focus on incorporating temporal and spatial dynamics of ubiquitination signaling, improving model interpretability through explainable AI techniques, and establishing standardized evaluation frameworks for multi-omics integration methods [120] [123]. Additionally, the growing application of semantic technologies including ontologies and knowledge graphs will enhance data standardization, integration, and analysis in multi-omics research [123]. As these methodologies mature, they will accelerate the development of ubiquitination-targeted therapies, ultimately advancing precision oncology through personalized therapeutic interventions based on comprehensive molecular profiling.
Therapeutic efficacy in oncology is fundamentally gauged through rigorous benchmarking of response rates and the delineation of resistance patterns. Within the context of ubiquitination signaling in the tumor microenvironment (TME), these metrics are not merely descriptive but are profoundly influenced by the dynamic post-translational modifications orchestrated by E3 ligases and deubiquitinases (DUBs). This whitepaper provides an in-depth technical guide on the methodologies for benchmarking therapeutic efficacy, with a specialized focus on how the ubiquitin network dictates both initial treatment responsiveness and the emergence of resistance. We synthesize current data into structured tables, detail essential experimental protocols for profiling ubiquitination in the TME, and provide pathway visualizations and reagent lists to equip researchers and drug development professionals with the tools necessary to advance targeted therapies.
The ubiquitin-proteasome system (UPS) is a master regulator of protein stability and function, governing key cellular processes in the TME such as immune cell infiltration, polarization, and checkpoint molecule expression [12] [10]. Ubiquitination involves a sequential enzymatic cascade: an E1 activating enzyme, an E2 conjugating enzyme, and an E3 ligase, which collectively confer substrate specificity. This process is reversible through the action of deubiquitinases (DUBs) [10] [51]. The functional outcome of ubiquitination is critically dependent on the topology of the ubiquitin chain. For instance, Lys48-linked polyubiquitination typically targets proteins for proteasomal degradation, whereas Lys63-linked chains are primarily involved in non-proteolytic signaling processes, such as activating the NF-κB pathway [12] [10].
The strategic importance of benchmarking therapeutic efficacy—quantifying response rates and mapping resistance patterns—becomes apparent when considering the UPS. The TME is a dynamic ecosystem where ubiquitination continuously modulates the stability of oncoproteins, tumor suppressors, and immune checkpoint receptors [12] [51]. Consequently, a deep understanding of ubiquitin signaling networks is indispensable for interpreting clinical response data, predicting resistance mechanisms, and designing next-generation combination therapies that target the UPS to overcome immune evasion and treatment failure.
Ubiquitination Signaling in the Tumor Microenvironment and Its Impact on Therapy Response
The cellular and non-cellular components of the TME are prime targets for regulation by ubiquitination. The efficacy of immunotherapies, in particular, is heavily influenced by the ubiquitin-driven stability of key immune checkpoint proteins.
Regulation of Immune Checkpoints by E3 Ligases and DUBs
The stability of programmed death-ligand 1 (PD-L1) on tumor and immune cells is a critical determinant of the response to immune checkpoint blockade (ICB). Multiple E3 ligases and DUBs intricately control PD-L1 levels [12] [51].
E3 Ligases Promoting PD-L1 Degradation:
- β-TrCP: Recognizes a phosphorylated degron on non-glycosylated PD-L1, leading to its Lys48-linked polyubiquitination and proteasomal degradation. Glycogen synthase kinase 3β (GSK3β) is often the kinase that primes PD-L1 for β-TrCP recognition [12].
- SPOP: As an adaptor for the Cullin3-RING ligase complex, SPOP directly binds to PD-L1 and promotes its polyubiquitination and degradation. The stability of SPOP itself is regulated by the APC/CCdh1 complex and cyclin D/CDK4-mediated phosphorylation [12].
- c-Cbl and Cbl-b: These RING-type E3 ligases negatively regulate PD-L1 expression indirectly by inactivating signaling pathways like STAT, AKT, and ERK [12].
- HRD1: This ER-resident E3 ligase targets phosphorylated PD-L1 (at Ser195) for endoplasmic reticulum-associated degradation (ERAD) [12].
- STUB1: A U-box E3 ligase that destabilizes PD-L1, particularly in regulatory T cells (Tregs) [12].
Regulators Promoting PD-L1 Stability:
- CSN5: A JAMM-family DUB that deubiquitinates and stabilizes PD-L1, allowing tumors to escape immune surveillance. Its expression is induced by TNF-α via the NF-κB pathway [12].
- CMTM6: While not a DUB, this transmembrane protein interacts with PD-L1 and protects it from ubiquitination and degradation, potentially by interfering with the STUB1 E3 ligase [12].
Table 1: Key Regulators of PD-L1 Stability in the Tumor Microenvironment
| Regulator | Type | Mechanism of Action on PD-L1 | Impact on Protein Stability |
|---|---|---|---|
| β-TrCP | E3 Ligase (SCF complex) | Recognizes phosphorylated, non-glycosylated PD-L1 | ↓ Degradation |
| SPOP | E3 Ligase Adaptor (CRL3 complex) | Direct binding and polyubiquitination | ↓ Degradation |
| HRD1 | E3 Ligase (ERAD) | Ubiquitinates phosphorylated PD-L1 (Ser195) in the ER | ↓ Degradation |
| STUB1 | E3 Ligase (U-box) | Ubiquitinates PD-L1 in Tregs | ↓ Degradation |
| CSN5 | Deubiquitinase (JAMM) | Removes ubiquitin chains from PD-L1 | ↑ Stabilization |
| CMTM6 | Transmembrane Protein | Binds PD-L1 and shields it from ubiquitination | ↑ Stabilization |
Control of Tumor-Infiltrating Immune Cells
Beyond checkpoint molecules, ubiquitination directly controls the polarization and function of immune cells within the TME.
- Tumor-Associated Macrophages (TAMs): E3 ligases and DUBs regulate the polarization of macrophages towards the pro-tumor M2 phenotype or the anti-tumor M1 phenotype, though the specific molecular players are still being elucidated [12].
- T cells: The E3 ligase FBXO38 catalyzes the Lys48-linked polyubiquitination and degradation of PD-1 in activated T cells. Loss of FBXO38 function leads to PD-1 accumulation and T cell exhaustion, a primary resistance mechanism to ICB [12].
The diagram below illustrates the core ubiquitination cascade and its impact on key immune checkpoint proteins within the TME.
Quantitative Frameworks for Benchmarking Therapeutic Efficacy
Robust benchmarking is essential for evaluating the success of cancer therapies in both clinical trials and preclinical research. This requires a clear understanding of standardized metrics and the value of biomarker-guided strategies.
Key Metrics for Benchmarking
Therapeutic efficacy is primarily quantified through a set of well-defined clinical and translational endpoints.
- Response Rate (RR): The percentage of patients whose tumor burden is reduced by a predefined amount. This is often categorized using criteria like RECIST (Response Evaluation Criteria in Solid Tumors) into complete response (CR), partial response (PR), stable disease (SD), and progressive disease (PD) [124].
- Progression-Free Survival (PFS): The length of time during and after treatment that a patient lives with the disease but it does not get worse [124].
- Overall Survival (OS): The gold standard efficacy endpoint, measuring the time from treatment initiation until death from any cause.
A meta-analysis of phase 1 cancer trials underscores the transformative impact of a biomarker-based personalized treatment strategy. This analysis demonstrated that a personalized approach, which often involves targeting specific genetic alterations or signaling pathways like the UPS, was independently associated with a significantly higher median RR and longer median PFS compared to a non-personalized approach [124].
Table 2: Benchmarking Efficacy of Personalized vs. Non-Personalized Therapy in Refractory Cancers (Meta-Analysis Data) [124]
| Therapeutic Strategy | Median Response Rate (RR) | Median Progression-Free Survival (PFS) |
|---|---|---|
| Biomarker-Based (Personalized) | 30.6% (95% CI, 25.0%-36.9%) | 5.7 months (95% CI, 2.6-13.8) |
| Non-Personalized (All Comers) | 4.9% (95% CI, 4.2%-5.7%) | 2.95 months (95% CI, 2.3-3.7) |
| Personalized using Genomic (DNA) Biomarker | 42.0% (95% CI, 33.7%-50.9%) | Data not specified in source |
| Personalized using Protein Biomarker | 22.4% (95% CI, 15.6%-30.9%) | Data not specified in source |
The Critical Role of Biomarker-Guided Strategies
The data in Table 2 highlights several critical points for modern drug development:
- Superior Efficacy: Biomarker-based selection nearly doubles the response rate and significantly extends PFS.
- Precision of Genomic Biomarkers: Personalized arms using genomic (DNA) biomarkers achieved a significantly higher median RR than those using protein biomarkers, suggesting deeper molecular stratification can lead to better outcomes [124].
- Ineffectiveness of Untargeted Use: Targeted therapy arms that did not use a biomarker-based strategy had outcomes comparable to cytotoxic chemotherapy, emphasizing that the mere use of a targeted agent is insufficient without proper patient selection [124].
Experimental Protocols for Profiling Ubiquitination in the TME
To mechanistically link therapeutic efficacy to ubiquitination, specific experimental methodologies are required to profile the activity and targets of the UPS within the TME.
Protocol: Immunoprecipitation and Immunoblotting for Ubiquitination Status
Objective: To detect the ubiquitination status and linkage type of a specific protein of interest (e.g., PD-L1) from tumor cell lysates or immune cells isolated from the TME.
- Cell Lysis and Preparation: Lyse cells or minced tumor tissue in a RIPA buffer supplemented with protease inhibitors, 10mM N-Ethylmaleimide (NEM) to inhibit endogenous DUBs, and 1% SDS to disrupt non-covalent interactions. Boil samples to denature proteins.
- Immunoprecipitation (IP): Dilute the lysate to 0.1% SDS. Pre-clear with protein A/G beads. Incubate the supernatant with an antibody specific to your protein of interest (e.g., anti-PD-L1) overnight at 4°C. Add protein A/G beads the next day and incubate for 2-4 hours.
- Ubiquitin Detection by Western Blot: Wash the beads extensively to remove non-specifically bound proteins. Elute the immunoprecipitated proteins by boiling in Laemmli buffer. Resolve proteins by SDS-PAGE and transfer to a PVDF membrane.
- Membrane Probing: Probe the membrane with:
- Primary antibody: Anti-ubiquitin antibody (to detect total ubiquitination), or linkage-specific antibodies (e.g., anti-K48-ubiquitin, anti-K63-ubiquitin).
- Secondary antibody: HRP-conjugated anti-mouse/rabbit IgG.
- Stripping and Re-probing: Strip the membrane and re-probe with an antibody against the original immunoprecipitated protein (e.g., PD-L1) to confirm equal pulldown and visualize non-ubiquitinated species.
Protocol: In Vivo Resistance Modeling via CRISPR/Cas9 Screens
Objective: To identify E3 ligases or DUBs whose loss confers resistance to a given therapy (e.g., ICB, radiotherapy) in a syngeneic mouse model.
- Library Design and Transduction: Use a pooled lentiviral CRISPR/Cas9 library targeting all known E3 ligases and DUBs. Transduce a murine cancer cell line that is sensitive to the therapy of interest at a low MOI to ensure single guide RNA (sgRNA) integration.
- In Vivo Selection: Inject the transduced pool of cells into immunocompetent mice. Once tumors are established, treat the mice with the therapeutic agent (e.g., anti-PD-1 antibody) or a vehicle control.
- Tumor Harvest and Sequencing: Harvest tumors upon vehicle-treated tumors reaching endpoint. Isolate genomic DNA from all tumors.
- sgRNA Amplification and NGS: Amplify the integrated sgRNA sequences by PCR and subject them to next-generation sequencing (NGS).
- Bioinformatic Analysis: Compare the abundance of each sgRNA in the treatment group versus the control group. sgRNAs that are significantly enriched in the treatment group identify E3 ligases or DUBs whose knockout conferred a survival advantage (resistance), nominating them as key resistance nodes in the ubiquitin network.
The Scientist's Toolkit: Essential Reagents for Ubiquitin Research in the TME
Profiling the ubiquitin landscape requires a specialized set of reagents and tools.
Table 3: Key Research Reagent Solutions for Ubiquitination Studies
| Reagent/Tool | Function/Application | Example Use-Case in TME Research |
|---|---|---|
| Linkage-Specific Ubiquitin Antibodies | Detect specific polyubiquitin chain topologies (K48, K63, etc.) via Western blot or immunofluorescence. | Determine if a therapy alters the K48-linked degradation of PD-L1 in tumor cells. |
| Proteasome Inhibitors (e.g., Bortezomib, Carfilzomib) | Block the degradation of ubiquitinated proteins, causing their accumulation. | Used in pulse-chase experiments to measure the degradation rate of a protein of interest. |
| DUB Inhibitors (e.g., Compounds G5, F6) | Selectively inhibit deubiquitinating enzyme activity. | Test if pharmacological inhibition of CSN5 destabilizes PD-L1 and re-sensitizes tumors to ICB. |
| CRISPR/Cas9 Knockout Libraries | Enable genome-wide or targeted (e.g., E3/DUB-focused) loss-of-function screens. | Identify ubiquitin-system genes that modulate resistance to radiotherapy or targeted therapy in vivo. |
| PROTACs (Proteolysis-Targeting Chimeras) | Bifunctional molecules that recruit an E3 ligase to a target protein, inducing its degradation. | Degrade a specific oncoprotein or immune checkpoint protein in the TME for therapeutic validation. |
| Active-Site Mutant Ubiquitin Plasmids | Express ubiquitin that cannot form specific chain types (e.g., K48R, K63R). | Mechanistically dissect which ubiquitin linkage is required for a specific signaling event in the TME. |
Advanced Visualization of Ubiquitin-Driven Resistance Pathways
The following diagram synthesizes the complex, multi-faceted role of ubiquitination in driving resistance to cancer therapy, connecting DNA repair, metabolic reprogramming, and immune evasion.
Benchmarking therapeutic efficacy through response rates and resistance profiling is a cornerstone of oncology drug development. This whitepaper establishes that these clinical outcomes are inextricably linked to the molecular circuitry of ubiquitination within the tumor microenvironment. The ubiquitin-signaling cascade, with its over 600 E3 ligases and 100 DUBs, provides a vast and largely untapped reservoir of therapeutic targets and predictive biomarkers. The quantitative frameworks and experimental protocols outlined herein provide a roadmap for researchers to systematically investigate this network. By integrating biomarker-guided patient stratification with a deep mechanistic understanding of ubiquitin-driven resistance, the field can advance towards more durable and effective cancer therapies.
Economic and Developmental Considerations in Ubiquitin-Targeted Therapy Development
The ubiquitin-proteasome system (UPS) represents a sophisticated intracellular protein degradation machinery that maintains cellular homeostasis by selectively eliminating damaged or misfolded proteins through a coordinated enzymatic cascade. This process involves three key enzymes: ubiquitin-activating (E1), ubiquitin-conjugating (E2), and ubiquitin-ligating (E3) enzymes, which collectively tag target proteins with ubiquitin chains for recognition and degradation by the 26S proteasome [82]. In recent years, targeted protein degradation (TPD) has emerged as a revolutionary therapeutic strategy that capitalizes on the UPS to eliminate disease-causing proteins, particularly in oncology [99] [125]. Unlike traditional small molecule inhibitors that merely block protein function, TPD technologies, including proteolysis-targeting chimeras (PROTACs) and molecular glues, facilitate the complete removal of target proteins from cells, offering potential advantages in addressing drug resistance and targeting previously "undruggable" proteins [99]. This paradigm shift in therapeutic intervention has created a rapidly expanding market with significant economic potential and complex developmental challenges, especially within the context of tumor microenvironment research where ubiquitination signaling plays a crucial regulatory role.
Economic Landscape of Ubiquitin-Targeted Therapies
Market Size and Growth Trajectory
The global targeted protein degradation market has demonstrated remarkable growth potential, valued at approximately $532.18 million in 2024 and projected to reach $2.84 billion by 2033, with a robust compound annual growth rate (CAGR) of 20.45% during the forecast period [126]. This expansion significantly outpaces the broader ubiquitin-proteasome market, which is expected to register a more modest CAGR of 5.2% from 2025 to 2031 [127]. The distinct growth rates highlight the particularly high investor confidence and innovation velocity in the TPD segment compared to established UPS-targeting approaches like proteasome inhibitors.
Table 1: Global Market Landscape for Ubiquitin-Targeted Therapeutics
| Market Segment | 2024 Market Size (USD) | Projected 2033 Market Size (USD) | CAGR (%) | Key Drivers |
|---|---|---|---|---|
| Targeted Protein Degradation | $532.18 million | $2.84 billion | 20.45% | High investment, clinical trial successes, addressing undruggable targets [126] |
| Ubiquitin Enzymes | $3.5 billion | $6.0 billion | 7.5% | Rising demand for personalized medicine, cancer research expansion [128] |
| Ubiquitin Proteasome | Not specified | Not specified | 5.2% (2025-2031) | Increasing research in cancer therapies, neurodegenerative diseases [127] |
Regional Investment Patterns and Innovation Hubs
North America currently dominates the TPD market with a 47% share, driven by a robust biotechnology ecosystem, substantial venture capital investment, and a favorable regulatory environment that accelerates clinical translation [126]. The United States serves as the primary hub, with companies like Arvinas, Amgen, and Pfizer pioneering TPD therapeutics. The Asia-Pacific region represents the fastest-growing market, with China emerging as a central player due to government incentives, R&D investments, and a vast oncology patient pool that facilitates clinical trial recruitment [126]. Europe maintains a strong presence through academic-industry partnerships and government-supported research initiatives, particularly in the United Kingdom and Germany [126].
Strategic Partnerships and Investment Trends
The TPD landscape has witnessed significant strategic partnerships and licensing deals, reflecting strong industry confidence in the therapeutic approach. A notable example includes Arvinas' out-licensing of ARV-766, a second-generation PROTAC androgen receptor degrader for prostate cancer, to Novartis AG in May 2024. This deal included a $150 million upfront payment with potential additional payments up to $1.01 billion based on development and commercialization milestones [126]. Similar high-value partnerships between biotechnology startups and pharmaceutical giants have become increasingly common, providing necessary capital for expensive late-stage clinical development while distributing financial risk.
Therapeutic Platforms and Developmental Pipelines
Key Technology Platforms: PROTACs and Molecular Glues
PROTACs represent the most advanced TPD platform, constituting the largest market share segment. These heterobifunctional molecules consist of three structural components: a ligand that binds to the protein of interest (POI), a ligand that recruits an E3 ubiquitin ligase, and a linker connecting these two moieties [99] [125]. The mechanism of action involves the formation of a ternary complex (POI-PROTAC-E3 ligase), leading to polyubiquitination and subsequent proteasomal degradation of the target protein [125]. PROTACs operate catalytically, enabling them to degrade multiple target protein molecules, potentially offering advantages over traditional occupancy-driven inhibitors [99].
Molecular glues constitute another important class of protein degraders, typically smaller molecules that induce or stabilize interactions between E3 ubiquitin ligases and target proteins [99]. Unlike PROTACs, molecular glues do not contain separate ligands connected by a linker, which often results in better drug-like properties and oral bioavailability. However, their discovery has been more challenging as their design relies on unpredictable protein-protein interface modifications [99].
Table 2: Comparison of Major Targeted Protein Degradation Platforms
| Platform Characteristic | PROTACs | Molecular Glues |
|---|---|---|
| Molecular Structure | Heterobifunctional: POI ligand + E3 ligase ligand + linker | Monomeric small molecules |
| Size | Larger molecular weight (>700 Da) | Smaller molecular weight |
| Mechanism | Induced proximity | Surface modulation |
| Design Approach | Rational design | Often serendipitous discovery |
| Hook Effect | Possible at high concentrations | Not observed |
| Oral Bioavailability | Challenging due to size | More favorable |
| Clinical Stage | Multiple candidates in Phase I/II trials | Several approved agents (e.g., immunomodulatory drugs) |
Clinical Trial Landscape and Regulatory Status
As of 2024, the clinical pipeline for ubiquitin-targeted therapies has expanded significantly, with over 40 active clinical trials investigating PROTAC-based therapies [126]. Notable candidates include ARV-110 and ARV-471 from Arvinas, which target the androgen receptor and estrogen receptor for prostate and breast cancer, respectively [125]. These were the first PROTACs to enter phase I clinical trials in 2019 [125]. Additional promising candidates in development include KT-253 (an MDM2-based PROTAC) [99] and NX-2127 (a BTK PROTAC for hematological malignancies) [125].
Despite this robust clinical activity, no PROTAC has yet received full regulatory approval from the U.S. Food and Drug Administration (FDA) as of 2025 [125]. However, several candidates have received Fast Track designation to accelerate their development and review processes. The regulatory pathway for these novel modalities presents unique challenges, particularly regarding the definition of potency and the development of appropriate bioassays, as outlined in FDA's 21 CFR 600.3(s) [125].
Technical and Economic Challenges in Therapy Development
Scientific and Manufacturing Hurdles
The development of ubiquitin-targeted therapies faces several significant technical challenges. The rational design of effective degraders remains complex, with optimization required for ternary complex formation, degradation efficiency, and pharmacokinetic properties [125]. The limited repertoire of utilized E3 ligases presents another constraint—while the human genome encodes over 600 E3 ligases, current TPD platforms primarily exploit only a handful, including cereblon (CRBN), von Hippel-Lindau (VHL), mouse double minute 2 homolog (MDM2), and inhibitors of apoptosis proteins (IAPs) [99]. Expanding this repertoire is crucial for broadening the targetable proteome and addressing tissue-specific expression patterns of E3 ligases.
Manufacturing complexities represent another substantial hurdle. PROTACs, with their large molecular weights and complex structures, often exhibit poor solubility and permeability, requiring advanced formulation strategies [99] [125]. The synthesis of these heterobifunctional molecules typically involves multi-step processes with challenging purification requirements, contributing to high production costs compared to conventional small molecules.
Economic Barriers and Return on Investment Considerations
The development of ubiquitin-targeted therapies requires substantial capital investment, with lengthy research and development timelines increasing financial risk. The high cost of clinical trials, particularly for oncology indications, combined with the novelty of the mechanism of action, necessitates extensive preclinical characterization and safety testing [126] [125]. Additionally, the complexity of the UPS creates challenges in predicting and monitoring therapeutic efficacy, requiring specialized biomarkers and diagnostic tools that further increase development costs [127].
The intellectual property landscape for TPD technologies has become increasingly crowded, with foundational patents creating potential barriers to entry for new players. Navigating this complex IP environment requires strategic planning and may involve licensing agreements that impact profit margins for successful products [126].
The Scientist's Toolkit: Key Research Reagents and Methodologies
Essential Research Tools for Ubiquitin-Targeted Therapy Development
Table 3: Key Research Reagent Solutions for Ubiquitin-Targeted Therapy Development
| Research Tool Category | Specific Examples | Research Applications | Technical Considerations |
|---|---|---|---|
| E3 Ligase Ligands | CRBN ligands (lenalidomide derivatives), VHL ligands, MDM2 ligands (Nutlin-3) | PROTAC design and optimization | Ligand affinity, selectivity, and physicochemical properties critically influence PROTAC efficacy [99] |
| Linker Chemistry | PEG-based linkers, alkyl chains, triazole-based linkers | Connecting POI and E3 ligase ligands | Linker length, composition, and rigidity impact ternary complex formation and degradation efficiency [125] |
| Proteasome Inhibitors | Bortezomib, carfilzomib, ixazomib | Validation of UPS-dependent degradation mechanism | Used as negative controls to confirm proteasome-dependent degradation [82] |
| Ubiquitination Assays | In vitro ubiquitination assays, TUBE (Tandem Ubiquitin Binding Entity) reagents | Monitoring ubiquitination of target proteins | Confirm mechanistic basis of degradation; require purified components or specialized detection reagents [82] |
| Protein Stability Assays | Cycloheximide chase assays, cellular thermal shift assays (CETSA) | Measuring target protein degradation kinetics | Provide quantitative degradation metrics; require optimization of timepoints and detection methods [99] |
| Ternary Complex Assays | Surface plasmon resonance (SPR), isothermal titration calorimetry (ITC) | Characterizing POI-PROTAC-E3 ligase interactions | Technically challenging but provide critical mechanistic insights into PROTAC function [99] |
Experimental Workflow for PROTAC Development and Validation
Diagram 1: PROTAC Development Workflow. This flowchart outlines the key stages in the development and validation of PROTAC-based therapeutics, from initial target identification through candidate selection for clinical development.
Key Signaling Pathways in Ubiquitin-Targeted Cancer Therapy
Diagram 2: Ubiquitin-Proteasome System and PROTAC Mechanism. This diagram illustrates the normal ubiquitin-proteasome pathway (top) and the targeted protein degradation induced by PROTAC molecules (bottom), highlighting how PROTACs hijack the natural degradation machinery.
Future Directions and Strategic Considerations
Emerging Opportunities and Innovation Frontiers
The future development of ubiquitin-targeted therapies will likely focus on several key areas. First, expanding the E3 ligase repertoire beyond the currently utilized CRBN and VHL ligases represents a major opportunity to access novel tissue-specific targets and improve therapeutic windows [99] [125]. Second, the development of conditional degradation technologies (e.g., light-controlled, small molecule-activated) may enable spatial and temporal control of protein degradation, potentially enhancing safety profiles [125]. Third, extending TPD beyond oncology to neurodegenerative disorders, autoimmune diseases, and infectious diseases represents a significant growth opportunity, though this requires overcoming challenges related to blood-brain barrier penetration and tissue-specific delivery [126] [127].
The integration of artificial intelligence and machine learning in degrader design is rapidly advancing, with these tools being employed to predict ternary complex formation, optimize linker properties, and identify novel E3 ligase ligands [128]. Additionally, the exploration of combination therapies that pair protein degraders with other treatment modalities, such as immunotherapy or targeted agents, holds promise for enhanced efficacy and overcoming resistance mechanisms [127].
Strategic Recommendations for Efficient Therapy Development
To navigate the complex landscape of ubiquitin-targeted therapy development, several strategic approaches can maximize efficiency and resource utilization. First, adopting a patient-centric early development strategy that incorporates biomarker identification and patient stratification approaches can increase the probability of clinical success [126]. Second, establishing cross-sector collaborations between academia, biotechnology companies, and pharmaceutical partners can distribute risk and leverage specialized expertise [126] [128]. Third, implementing platform-based approaches to degrader discovery and optimization can create efficiencies across multiple programs, particularly for companies pursuing diverse targets.
From a regulatory perspective, engaging with agencies like the FDA early in development is crucial for novel TPD modalities, particularly regarding potency assays, biomarker strategies, and appropriate preclinical models [125]. Finally, balancing portfolio diversification with focus areas of expertise will be essential for organizations of different sizes—while large pharmaceutical companies may pursue broad TPD pipelines, smaller biotechnology firms may achieve success through specialized approaches targeting specific E3 ligase families or disease areas.
Ubiquitin-targeted therapy development represents a transformative approach in precision medicine, particularly relevant to tumor microenvironment research where ubiquitination signaling governs critical processes. The field has demonstrated substantial economic potential, driven by compelling clinical data and significant investment from both public and private sectors. However, the path to successful commercialization requires navigating complex scientific, manufacturing, and regulatory challenges. Strategic approaches that leverage advancing technologies, expand the toolset of available E3 ligases, and foster collaborative development models will be essential for realizing the full potential of this promising therapeutic modality. As the field matures, ubiquitin-targeted therapies are poised to make significant contributions to the treatment of cancer and other diseases, potentially offering new solutions for patients with limited therapeutic options.
Conclusion
The ubiquitin signaling network represents a master regulatory system that dynamically controls the tumor microenvironment through sophisticated mechanisms. This review synthesizes key insights across foundational biology, therapeutic applications, challenge mitigation, and validation strategies, highlighting the immense potential of targeting this system for cancer therapy. Future directions should focus on developing isoform-specific inhibitors, advancing biomarker-guided precision medicine, exploiting ubiquitin chain specificity, and creating innovative combination regimens. The integration of AI and novel degradation technologies will further accelerate the translation of ubiquitin-focused research into clinical breakthroughs, ultimately reshaping cancer treatment paradigms by reeducating the TME.
References
- 1. Ubiquitin proteasome system in immune regulation and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10163937/]
- 2. Ubiquitin-Proteasome System [https://lifesensors.com/ubiquitinproteasomesystem/]
- 3. Perilous journey: a tour of the ubiquitin–proteasome system [https://www.sciencedirect.com/science/article/abs/pii/S0962892413002274]
- 4. Ubiquitin/Proteasome [https://www.cellsignal.com/pathways/ubiquitin-proteasome-pathway?srsltid=AfmBOooZxK3oi7gpkOEmoyTXqF5uX1N9D0Xd26E4HK8ztGQHKJIHFFbZ]
- 5. Molecular mechanisms and potential targeting strategies of ... [https://www.spandidos-publications.com/10.3892/or.2025.9000]
- 6. Ubiquitination in cancer: mechanisms and therapeutic ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12479132/]
- 7. F-box proteins in cancer: from cancer cells to the tumor ... [https://biosignaling.biomedcentral.com/articles/10.1186/s12964-025-02445-z]
- 8. Editorial: The role of ubiquitination in disease development ... [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2025.1595755/full]
- 9. K48- and K63-linked ubiquitin chain interactome reveals ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11109483/]
- 10. The role of ubiquitination in tumorigenesis and targeted ... [https://www.nature.com/articles/s41392-020-0107-0]
- 11. Emerging functions of branched ubiquitin chains [https://www.nature.com/articles/s41421-020-00237-y]
- 12. Targeting the Ubiquitin Signaling Cascade in Tumor ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7830467/]
- 13. Roles of ubiquitination in the crosstalk between tumors and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9170352/]
- 14. Role of K63-linked ubiquitination in cancer [https://www.nature.com/articles/s41420-022-01204-0]
- 15. Exploiting E3 ubiquitin ligases to reeducate the tumor ... [https://ehoonline.biomedcentral.com/articles/10.1186/s40164-023-00394-2]
- 16. Analysis of the topology of ubiquitin chains - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC6989142/]
- 17. Exploiting E3 ubiquitin ligases to reeducate the tumor ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10061905/]
- 18. E3 ubiquitin ligases in signaling, disease, and therapeutics [https://pubmed.ncbi.nlm.nih.gov/40940201/]
- 19. Role and therapeutic potential of E3s in the tumor ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11560419/]
- 20. RBR E3 ubiquitin ligases: new structures, new insights, new ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3940038/]
- 21. Activity-based profiling of cullin–RING E3 networks by ... [https://www.nature.com/articles/s41589-023-01392-5]
- 22. E3 ubiquitin ligases in signaling, disease, and therapeutics [https://www.sciencedirect.com/science/article/pii/S0968000425001860]
- 23. System level dynamics of post-translational modifications [https://pmc.ncbi.nlm.nih.gov/articles/PMC4097989/]
- 24. Control of protein stability by post-translational modifications [https://www.nature.com/articles/s41467-023-35795-8]
- 25. Recognition of substrate degrons by E3 ubiquitin ligases ... [https://www.sciencedirect.com/science/article/abs/pii/S0959440X16301932]
- 26. Phosphodegrons in Health and Disease: From Cellular ... [https://www.mdpi.com/2813-3757/3/1/3]
- 27. Frontiers | Commentary: The ubiquitin -proteasome system in the... [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2025.1522427/full]
- 28. Decoding the ubiquitin network: molecular mechanisms and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12492556/]
- 29. Involvement of the ubiquitin -proteasome system in the regulation of... [https://pubmed.ncbi.nlm.nih.gov/39759114/]
- 30. Global identification of phospho-dependent SCF substrates ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8738747/]
- 31. Unveiling the role of the ubiquitin -proteasome system in... | EurekAlert! [https://www.eurekalert.org/news-releases/1074633]
- 32. F-box proteins at the crossroads of ubiquitination and ... [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2025.1596344/full]
- 33. F-box proteins at the crossroads of ubiquitination and tumor ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12174096/]
- 34. F-box only protein 25-mediated α-actinin 1 upregulation ... [https://www.sciencedirect.com/science/article/pii/S1567576925004692]
- 35. F-box proteins at the crossroads of ubiquitination and ... [https://pubmed.ncbi.nlm.nih.gov/40534867/]
- 36. How cancer and immune cell plasticity mediates tumor ... [https://journals.plos.org/plosbiology/article?id=10.1371/journal.pbio.3003301&rev=1]
- 37. F-box protein Fbx23 acts as a transcriptional coactivator to ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11750091/]
- 38. Exploring the crosstalk between endothelial cells, immune ... [https://www.nature.com/articles/s41419-023-06119-x]
- 39. Metabolic Reprogramming of Cancer Associated Fibroblasts [https://pmc.ncbi.nlm.nih.gov/articles/PMC6008683/]
- 40. Endothelial cells in tumor microenvironment - PubMed Central [https://pmc.ncbi.nlm.nih.gov/articles/PMC10902062/]
- 41. Involvement of the ubiquitin-proteasome system in ... [https://www.sciencedirect.com/science/article/pii/S2352304224000370]
- 42. Crosstalk between cancer-associated fibroblasts and ... [https://www.nature.com/articles/s41420-024-01958-9]
- 43. Signaling crosstalk between tumor endothelial cells and ... [https://www.frontiersin.org/journals/cell-and-developmental-biology/articles/10.3389/fcell.2024.1387198/full]
- 44. Design and development of PROTACs: A new paradigm in ... [https://www.sciencedirect.com/science/article/pii/S2590098625000181]
- 45. The great escape: How cancer outsmarts PROTACs [https://www.drugdiscoverynews.com/the-great-escape-how-cancer-outsmarts-protacs-16831]
- 46. Degraders & Molecular Glues Part 1 | April 15-16, 2025 [https://www.drugdiscoverychemistry.com/25/protein-degradation-molecular-glues]
- 47. Frontiers | The ubiquitin -proteasome system in the tumor immune... [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2024.1436174/full]
- 48. A patent review of SCF E3 ligases inhibitors for cancer [https://www.sciencedirect.com/science/article/abs/pii/S0223523424007025]
- 49. Molecular mechanisms and potential targeting strategies of... [https://www.spandidos-publications.com/10.3892/or.2025.9000?text=fulltext]
- 50. Emerging Role of Ubiquitination in the Regulation of PD - 1 / PD - L in... 1 [https://pmc.ncbi.nlm.nih.gov/articles/PMC7934629/]
- 51. Targeting the ubiquitination /deubiquitination process to regulate... [https://www.nature.com/articles/s41392-020-00418-x?error=cookies_not_supported&code=c17d2806-6c73-483d-89ab-f0101c8ea551]
- 52. Emerging role of ubiquitination/deubiquitination ... [https://www.sciencedirect.com/science/article/pii/S2352304222000320]
- 53. Molecular mechanisms and potential targeting strategies of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12511930/]
- 54. Frontiers | The role of ubiquitination and deubiquitination in ... cancer [https://www.frontiersin.org/journals/oncology/articles/10.3389/fonc.2025.1464914/full]
- 55. Decoding the ubiquitin : molecular mechanisms and... network [https://molecular-cancer.biomedcentral.com/articles/10.1186/s12943-025-02433-4]
- 56. Biochemistry, Ubiquitination - StatPearls - NCBI Bookshelf - NIH [https://www.ncbi.nlm.nih.gov/books/NBK556052/]
- 57. E1, E2, E3 Enzyme and Their Regulators [https://www.bocsci.com/resources/e1-e2-e3-enzyme-and-their-regulators.html?srsltid=AfmBOor3MTkAkACbYgI0Mg7kZcbEaXXIxLKu0JZ7kbKrK4eShIfhsX8V]
- 58. Recent advances in small molecule inhibitors of ... [https://www.sciencedirect.com/science/article/abs/pii/S0223523425000893]
- 59. Targeting ubiquitin signaling for cancer immunotherapy [https://www.nature.com/articles/s41392-020-00421-2]
- 60. Deubiquitinase-Targeting Chimeras (DUBTACs) as a ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12507175/]
- 61. PD-1/PD-L1 Cancer Immunotherapeutics Reshape Tumor ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12532714/]
- 62. The ubiquitin system: from cell signalling to disease ... [https://www.nature.com/articles/s41418-020-00703-w]
- 63. Integrative Multi-Omics Analysis Reveals the Molecular ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12250011/]
- 64. Integrating artificial intelligence into small molecule ... [https://www.nature.com/articles/s44386-025-00029-y]
- 65. Integrating artificial intelligence in drug discovery and early ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11909971/]
- 66. Machine learning-based approaches for ubiquitination site ... [https://bmcbioinformatics.biomedcentral.com/articles/10.1186/s12859-023-05581-w]
- 67. An artificial intelligence accelerated virtual screening ... [https://www.nature.com/articles/s41467-024-52061-7]
- 68. Ubiquitination and ALL: Identifying FBXO8 as a prognostic ... [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2025.1554231/full]
- 69. PROTAC Degraders in Clinical Trails: 2025 Update [https://www.biochempeg.com/article/434.html]
- 70. FDA Approvals in Oncology: July-September 2025 | Blog [https://www.aacr.org/blog/2025/10/02/fda-approvals-in-oncology-july-september-2025/]
- 71. Oncology (Cancer)/Hematologic Malignancies Approval ... [https://www.fda.gov/drugs/resources-information-approved-drugs/oncology-cancerhematologic-malignancies-approval-notifications]
- 72. October 2025: A Look at FDA Oncology Approvals and ... [https://www.targetedonc.com/view/october-2025-a-look-at-fda-oncology-approvals-and-designations]
- 73. Press releases [https://ir.nurixtx.com/news-releases/news-release-details/nurix-therapeutics-presents-new-translational-data-first-human]
- 74. TREM2-mediated regulation of myeloid cells in the tumor ... [https://www.nature.com/articles/s41698-025-01152-9]
- 75. MD Anderson experts spotlight key immunotherapy ... [https://www.mdanderson.org/newsroom/research-newsroom/md-anderson-experts-spotlight-key-immunotherapy-advances-at-2025.h00-159781179.html]
- 76. The enigma of the RING-UIM E3 ligases - PubMed Central - NIH [https://pmc.ncbi.nlm.nih.gov/articles/PMC12522283/]
- 77. Ubiquitination and deubiquitination in cancer [https://molecular-cancer.biomedcentral.com/articles/10.1186/s12943-024-02046-3]
- 78. Regulatory role of E3 ubiquitin ligases in multiple myeloma [https://www.frontiersin.org/journals/cell-and-developmental-biology/articles/10.3389/fcell.2025.1620097/full]
- 79. The E3 ligase TRIM22 functions as a tumor suppressor in ... [https://www.sciencedirect.com/science/article/pii/S0304383524005524]
- 80. Drug resistance mechanisms and treatment strategies ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11067278/]
- 81. Proteolysis‐targeting chimeras in cancer therapy [https://pmc.ncbi.nlm.nih.gov/articles/PMC12535346/]
- 82. Targeting the Ubiquitin–Proteasome System for Cancer - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC12495026/]
- 83. E2 conjugating enzymes: A silent but crucial player in ... [https://www.sciencedirect.com/science/article/abs/pii/S1568163725000868]
- 84. Ubiquitin-conjugating enzyme UBE2N modulates ... [https://www.jci.org/articles/view/184665]
- 85. The multifaceted roles of deubiquitinating enzymes (DUBs) ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12533248/]
- 86. Strategies to Target Specific Components of the Ubiquitin ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6966607/]
- 87. Strategies for Precise Modulation of Protein Degradation [https://pubmed.ncbi.nlm.nih.gov/40132213/]
- 88. Targeted protein degradation: mechanisms, strategies and ... [https://www.nature.com/articles/s41392-022-00966-4]
- 89. Modulation of the Ubiquitin-Proteasome System by ... [https://www.sciencedirect.com/science/article/pii/S095528632500289X]
- 90. Metabolic reprogramming in cancer: Mechanisms and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10041388/]
- 91. Tumor metabolic regulators: key drivers of ... - Molecular Cancer [https://molecular-cancer.biomedcentral.com/articles/10.1186/s12943-024-02205-6]
- 92. The Ubiquitin–Proteasome System in Tumor Metabolism - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC10136670/]
- 93. Metabolic rewiring in the promotion of cancer metastasis [https://www.nature.com/articles/s41388-020-01432-7]
- 94. An optimized protocol to detect protein ubiquitination ... - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC10050764/]
- 95. The Future of Clinical Trials: Incorporating 'Omics for ... [https://blog.crownbio.com/the-future-of-clinical-trials-incorporating-omics-for-enhanced-stratification]
- 96. Study Designs and Statistical Analyses for Biomarker ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3444086/]
- 97. Flow Cytometry Protocols | Thermo Fisher Scientific - US [https://www.thermofisher.com/us/en/home/references/protocols/cell-and-tissue-analysis/flow-cytometry-protocol.html]
- 98. Targeted Protein Degraders: Transforming Oral Therapeutics [https://pci.com/resources/targeted-protein-degraders-in-oral-therapeutics/]
- 99. Targeted protein degradation: advances in drug discovery ... [https://www.nature.com/articles/s41392-024-02004-x]
- 100. Advancements in delivery Systems for Proteolysis ... [https://www.sciencedirect.com/science/article/abs/pii/S0168365925003396]
- 101. PROTAC Delivery Strategies for Overcoming Physicochemical ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12030311/]
- 102. Review Molecular glues and PROTACs in targeted protein ... [https://www.sciencedirect.com/science/article/abs/pii/S0006295225005623]
- 103. Targeted Protein Degradation with PROTACs and ... [https://blog.crownbio.com/targeted-protein-degradation-with-protacs-and-molecular-glues]
- 104. Inhibitors, PROTACs and Molecular Glues as Diverse ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8583118/]
- 105. Molecular Glues: A New Dawn After PROTAC [https://www.biochempeg.com/article/271.html]
- 106. Mechanisms that matter: unbiased cellular screening for ... [https://www.nature.com/articles/s44386-025-00028-z]
- 107. Frontiers | Editorial: Interaction of cell subtypes in tumor ... [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2025.1600338/full]
- 108. Comprehensive pan‑cancer analysis reveals ubiquitin ... [https://www.spandidos-publications.com/10.3892/ol.2025.15237]
- 109. Single‑cell transcriptomic analysis revealed the tumor ‑associated... [https://www.spandidos-publications.com/10.3892/ol.2025.14876?text=fulltext]
- 110. The role of ubiquitination in tumorigenesis and targeted drug discovery - PubMed [https://pubmed.ncbi.nlm.nih.gov/32296023/]
- 111. Current methodologies in protein ubiquitination ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9373315/]
- 112. Identification and validation of ubiquitination-related genes for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12343280/]
- 113. Frontiers | Research progress of ferroptosis pathway and its related... [https://www.frontiersin.org/journals/oncology/articles/10.3389/fonc.2025.1502673/full]
- 114. Transcriptomics-based exploration of ubiquitination-related biomarkers and potential molecular mechanisms in laryngeal squamous cell carcinoma | BMC Medical Genomics | Full Text [https://bmcmedgenomics.biomedcentral.com/articles/10.1186/s12920-025-02148-x]
- 115. Construction of ubiquitination-related risk model for ... [https://www.nature.com/articles/s41598-025-92177-4]
- 116. Functional genomics and tumor microenvironment analysis ... [https://www.nature.com/articles/s41467-025-64666-7]
- 117. Integrating multi-omics and experimental techniques to ... [https://www.frontiersin.org/journals/pharmacology/articles/10.3389/fphar.2025.1545472/full]
- 118. Adaptive multi-omics integration framework for breast ... [https://www.nature.com/articles/s41598-025-22202-z]
- 119. AI-driven multi-omics integration in precision oncology [https://pmc.ncbi.nlm.nih.gov/articles/PMC12634751/]
- 120. Network-based multi-omics integrative analysis methods in ... [https://biodatamining.biomedcentral.com/articles/10.1186/s13040-025-00442-z]
- 121. Pan-cancer multi-omics profiling reveals ubiquitin D as a ... [https://link.springer.com/article/10.1007/s12672-025-03545-5]
- 122. Single-cell multi-omics in cancer immunotherapy: from tumor ... [https://molecular-cancer.biomedcentral.com/articles/10.1186/s12943-025-02426-3]
- 123. A systematic mapping study of semantic technologies in ... [https://www.sciencedirect.com/science/article/pii/S1532046425000383]
- 124. Association of Biomarker -Based Treatment Strategies With Response ... [https://pubmed.ncbi.nlm.nih.gov/27273579/]
- 125. Exploring the clinical trials, regulatory insights, and ... [https://www.sciencedirect.com/science/article/abs/pii/S0093775425000181]
- 126. Targeted Protein Degradation Market Size, Growth, Trends ... [https://straitsresearch.com/report/targeted-protein-degradation-market]
- 127. Ubiquitin Proteasome Market Growth and Size by 2031 [https://www.theinsightpartners.com/reports/ubiquitin-proteasome-market]
- 128. Ubiquitin Enzymes Market Trends to Watch: Growth and ... [https://www.linkedin.com/pulse/ubiquitin-enzymes-market-trends-watch-growth-ht7zf]