Ubiquitination in Cancer Stem Cell Maintenance: Molecular Mechanisms and Therapeutic Targeting
This article comprehensively examines the critical role of the ubiquitin-proteasome system (UPS) in regulating cancer stem cell (CSC) maintenance, a key driver of tumor progression, metastasis, and therapy resistance.
Ubiquitination in Cancer Stem Cell Maintenance: Molecular Mechanisms and Therapeutic Targeting
Abstract
This article comprehensively examines the critical role of the ubiquitin-proteasome system (UPS) in regulating cancer stem cell (CSC) maintenance, a key driver of tumor progression, metastasis, and therapy resistance. Tailored for researchers and drug development professionals, it synthesizes foundational mechanisms—including the regulation of core stemness transcription factors (SOX2, OCT4, Nanog, c-Myc) and key signaling pathways (Notch, Wnt/β-catenin, Hedgehog)—with emerging methodological applications such as PROTACs and molecular glues. It further addresses challenges in therapeutic targeting, including functional redundancy and biomarker identification, and validates these approaches through preclinical and clinical evidence. The review aims to provide a framework for developing novel UPS-targeted strategies to eliminate the CSC population and overcome treatment resistance in oncology.
The Ubiquitin Code: Mastering Core Mechanisms in Cancer Stem Cell Biology
The Core Enzymatic Cascade of the UPS
The Ubiquitin-Proteasome System (UPS) is the primary pathway for targeted protein degradation in eukaryotic cells, governing essential cellular processes through a sophisticated enzymatic cascade. This system regulates the stability, function, and localization of a vast array of proteins, making it a critical determinant of cellular homeostasis [1] [2].
Ubiquitination initiates with a three-step enzymatic cascade involving E1 (ubiquitin-activating enzyme), E2 (ubiquitin-conjugating enzyme), and E3 (ubiquitin ligase) enzymes [1] [3] [2]. The process begins when E1 activates ubiquitin, a 76-amino acid protein, in an ATP-dependent reaction, forming a high-energy thiol ester intermediate [4] [5]. The activated ubiquitin is then transferred to an E2 enzyme. Finally, an E3 ligase facilitates the transfer of ubiquitin from the E2 to a lysine residue on the target substrate protein, culminating in substrate ubiquitination [4].
This modification is dynamically reversible through the action of deubiquitinases (DUBs), which cleave ubiquitin from substrate proteins, providing a crucial regulatory counterbalance to ubiquitination [1] [3]. Collectively, these components form a precise regulatory system that controls protein fate and function.
Table 1: Core Components of the Ubiquitin-Proteasome System
| Component | Key Function | Representative Examples | Mechanistic Role |
|---|---|---|---|
| E1 (Activating Enzyme) | Activates ubiquitin via ATP hydrolysis | UBA1, UBA6, UBA7 | Forms ubiquitin-adenylate intermediate, initiates catalytic cascade [5] |
| E2 (Conjugating Enzyme) | Carries activated ubiquitin | UBE2T, UBE2B, UBE2C | Transfers ubiquitin from E1 to E3 or directly to substrate [3] |
| E3 (Ligase) | Confers substrate specificity | MDM2, PARKIN, TRIM family, CRLs | Recognizes specific substrates and catalyzes ubiquitin transfer [1] [4] |
| DUBs (Deubiquitinases) | Removes ubiquitin modifications | USP2, OTUB2, OTULIN, BAP1 | Cleaves ubiquitin from substrates, recycles ubiquitin [1] [3] |
E3 Ubiquitin Ligases: Architects of Specificity
E3 ubiquitin ligases represent the most diverse and specialized component of the UPS, with over 600 identified in the human genome [4]. These enzymes are categorized into three major families based on their structural domains and mechanisms of ubiquitin transfer: RING (Really Interesting New Gene), HECT (Homologous to the E6AP C terminus), and RBR (RING-Between-RING) [4].
RING-type E3 ligases, the largest class, function as scaffolds that directly catalyze ubiquitin transfer from E2-ubiquitin complexes to substrate proteins [4]. In contrast, HECT-type E3 ligases employ a two-step mechanism where the HECT domain first receives ubiquitin on a cysteine residue from the E2 enzyme before transferring it to the substrate [4] [6]. RBR-type E3 ligases incorporate features of both, possessing RING domains but utilizing a HECT-like catalytic mechanism [4].
This classification system reflects the diverse evolutionary strategies for achieving substrate specificity in ubiquitination, with different E3 families employing distinct molecular mechanisms to ensure precise target selection.
Table 2: Major Families of E3 Ubiquitin Ligases
| E3 Family | Representative Members | Catalytic Mechanism | Biological Functions in Cancer |
|---|---|---|---|
| RING-type | MDM2, CBL, TRIM8, TRIM31 | Direct transfer of ubiquitin from E2 to substrate [4] | Regulates p53 stability (MDM2), modulates inflammatory signaling (TRIM8) [1] [4] |
| HECT-type | NEDD4, SMURF, E6AP | Two-step mechanism with ubiquitin-thioester intermediate on E3 cysteine residue [4] [6] | Controls cell growth, signal transduction; implicated in various cancers [1] |
| RBR-type | PARKIN, HOIP, HOIL-1L | Hybrid mechanism with RING domains and HECT-like catalysis [4] | Regulates mitophagy (PARKIN), linear ubiquitin chain assembly (HOIP) [3] |
Deubiquitinases (DUBs): Regulators of Reversibility
Deubiquitinases (DUBs) constitute a family of approximately 100 enzymes that counterbalance ubiquitination by removing ubiquitin modifications from substrate proteins [3] [6]. DUBs perform two essential functions: they disassemble polyubiquitin chains from substrate proteins, thereby rescuing them from degradation, and they recycle ubiquitin molecules by processing ubiquitin precursors or editing ubiquitin chains [3].
DUBs are classified into several families based on their catalytic domains and mechanisms, including ubiquitin-specific proteases (USPs), ovarian tumor proteases (OTUs), Josephin domain-containing proteases, and JAB1/MPN/Mov34 metalloenzymes (JAMMs) [7] [3]. Each family exhibits distinct preferences for specific ubiquitin chain linkages and cellular localizations, enabling precise regulation of ubiquitin signaling [3].
The balanced interplay between E3 ligases and DUBs creates a dynamic regulatory system that allows cells to rapidly respond to changing environmental conditions and maintain protein homeostasis.
The Ubiquitin Code: Molecular Language of Fate Determination
Ubiquitination represents a sophisticated molecular code that extends far beyond a simple degradation signal. This complexity arises from the ability of ubiquitin to form diverse polymeric chains through its seven internal lysine residues (K6, K11, K27, K29, K33, K48, K63) or its N-terminal methionine (M1) [3] [2]. These structurally distinct ubiquitin modifications are recognized as functionally discrete signals that determine specific protein fates [2].
K48-linked polyubiquitin chains typically target substrates for proteasomal degradation, serving as the canonical degradation signal [4] [8]. In contrast, K63-linked chains generally mediate non-proteolytic functions including protein-protein interactions, activation of kinase pathways, and DNA repair processes [4] [4]. Monoubiquitination (attachment of a single ubiquitin molecule) and multimonoubiquitination (multiple single ubiquitins on different lysines) regulate processes such as DNA repair, signal transduction, and protein trafficking [3].
The emerging understanding of heterotypic polyubiquitin chains (mixed linkage), branched chains, and ubiquitin-like modifications (e.g., NEDD8, SUMO) further expands the complexity of this regulatory system, creating a sophisticated signaling network that controls virtually all aspects of cell biology [3].
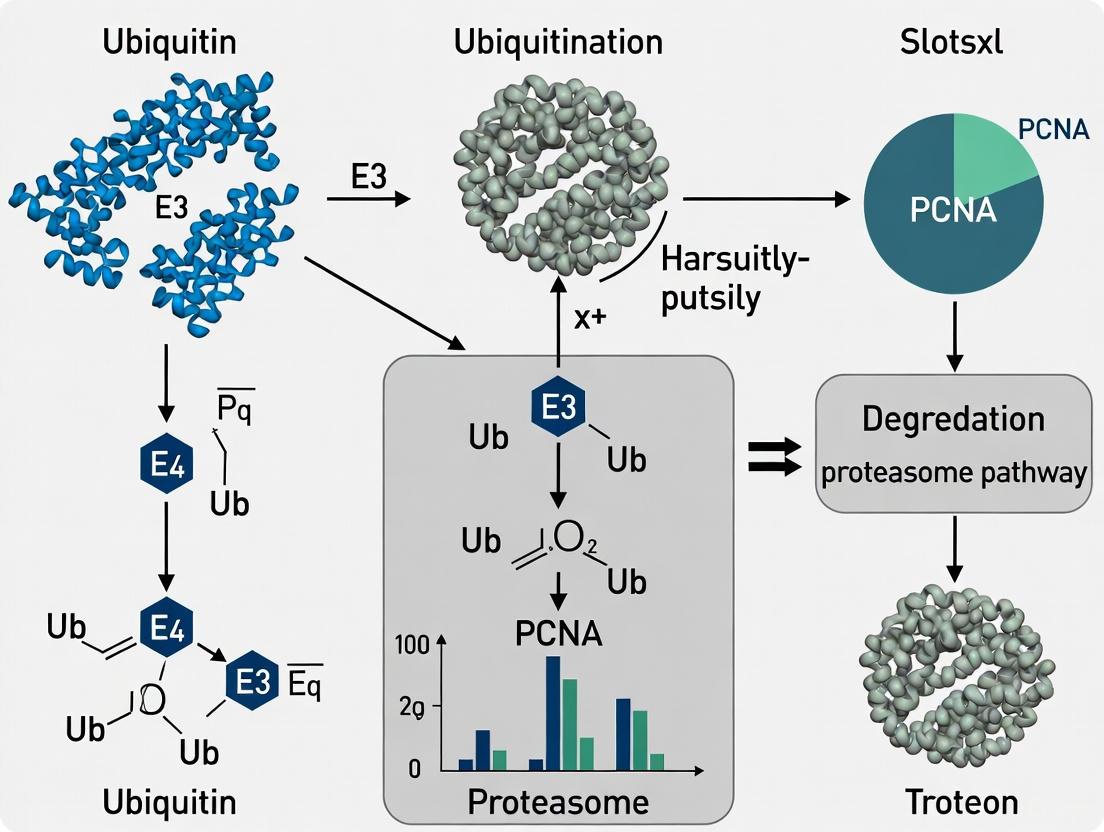
Diagram Title: UPS Enzymatic Cascade and Regulatory Dynamics
UPS in Cancer Stem Cell Maintenance: Mechanistic Insights
The Ubiquitin-Proteasome System plays a pivotal role in maintaining cancer stem cell (CSC) populations, which drive tumor initiation, metastasis, recurrence, and therapeutic resistance [9] [5]. CSCs typically constitute approximately 1% of total cells in various malignancies, though this proportion can escalate to 30% in metastatic contexts, correlating with enhanced treatment resistance [5].
E3 ubiquitin ligases and DUBs precisely regulate core transcription factors governing CSC self-renewal and pluripotency, including SOX2, OCT4, KLF4, and c-MYC [9] [5]. Quantitative proteomics analyses have revealed that these core transcription factors are themselves ubiquitination targets, suggesting that ubiquitination plays a fundamental role in maintaining stemness and pluripotency [5]. For instance, the CSN6-TRIM21 axis regulates colorectal cancer stemness by stabilizing OCT1 through modulation of TRIM21 E3 ligase activity [5].
The UPS also interfaces with key developmental signaling pathways essential for CSC maintenance, including Notch, Wnt/β-catenin, Hedgehog, and Hippo-YAP pathways [9] [10]. In non-small cell lung cancer, PKMYT1 stabilizes β-catenin protein and activates Wnt signaling, thereby bolstering CSC self-renewal capacity [5]. Similarly, dysregulation of ubiquitination in these pathways can promote the acquisition and maintenance of stem-like properties in cancer cells.
Diagram Title: UPS Regulation of Cancer Stem Cell Properties
Experimental Methodologies for UPS Research
Ubiquitin Variant (UbV) Technology
UbV technology employs a structure-based protein engineering strategy to develop ubiquitin variants that selectively modulate UPS components in human cells [1]. This approach involves generating UbV phage display libraries followed by screening against target E3 ligases or DUBs to identify high-affinity binders [1]. For instance, Hewitt et al. utilized computational approaches to create UbV-based activity-based probes (ABPs) for UCHL1, a DUB overexpressed in various cancers and neurodegenerative disorders [1]. Subsequently, the same research group generated a selective triple-mutant UbV-ABP for UCHL3, validating its function across multiple human cell lines [1].
Protocol: UbV Generation and Validation
- Library Construction: Generate UbV phage display libraries with randomized ubiquitin surface residues
- Biopanning: Screen libraries against purified target E3 ligases or DUBs over multiple rounds
- Hit Characterization: Sequence positive clones and characterize binding affinity using surface plasmon resonance (SPR)
- Functional Validation: Test UbV effects on enzyme activity in vitro using ubiquitination/deubiquitination assays
- Cellular Studies: Express selected UbVs in human cell lines and assess target modulation and phenotypic outcomes
Proteolysis-Targeting Chimeras (PROTACs)
PROTACs represent an innovative therapeutic strategy that artificially recruits E3 ligases to non-native substrates, inducing targeted protein degradation [1] [8]. These bifunctional molecules consist of a target-binding moiety linked to an E3 ligase-recruiting ligand, enabling selective degradation of disease-causing proteins [1]. Aminu et al. utilized structure-based protein engineering to create Ubiquitin Variant Induced Proximity (UbVIP), generating non-inhibitory UbV binders for selected E3 ligases and screening UbVIP libraries to identify novel E3 ligases capable of degrading target proteins like 53BP1 [1].
Protocol: PROTAC Development and Testing
- Design: Synthesize bifunctional molecules linking target protein ligand to E3 ligase recruiter
- Binding Validation: Confirm simultaneous binding to target protein and E3 ligase using pull-down assays
- Degradation Assessment: Treat cells with PROTACs and measure target protein levels by immunoblotting
- Specificity Profiling: Use quantitative proteomics to assess degradation selectivity across the proteome
- Functional Consequences: Evaluate phenotypic effects of target degradation in disease-relevant models
Mass Spectrometry-Based Ubiquitomics
Mass spectrometry-based proteomics has been instrumental in mapping ubiquitination sites and understanding the ubiquitin code [1] [3]. Lacoursiere et al. employed biochemical, biophysical, and proteomics assays to reveal the comprehensive Ub and UPS post-translational modification landscape, providing insights into how these modifications impact ubiquitin signaling in human diseases [1]. These approaches typically involve enrichment of ubiquitinated peptides using ubiquitin remnant motifs (e.g., diGly residues) followed by high-resolution mass spectrometry analysis.
Table 3: Key Experimental Approaches in UPS Research
| Methodology | Key Application | Technical Output | Research Utility |
|---|---|---|---|
| Ubiquitin Variants (UbVs) | Selective inhibition/modulation of E3s or DUBs [1] | High-affinity protein binders | Functional dissection of specific UPS components; therapeutic development [1] |
| Activity-Based Probes (ABPs) | Profiling enzyme activity in complex proteomes [1] | Active-site directed chemical probes | Target engagement studies; inhibitor screening; mechanistic studies [1] |
| PROTACs | Targeted protein degradation [1] [8] | Bifunctional degradation molecules | Therapeutic development; target validation; chemical genetics [1] |
| Mass Spectrometry Ubiquitomics | System-wide identification of ubiquitination sites [1] [3] | Quantitative ubiquitin site maps | Discovery of novel regulatory mechanisms; biomarker identification [1] |
Research Reagent Solutions for UPS Investigation
Table 4: Essential Research Tools for UPS Studies
| Reagent Category | Specific Examples | Research Application | Experimental Function |
|---|---|---|---|
| E3 Ligase Inhibitors | Hinokiflavone (MDM2 inhibitor) [1] | Functional studies of specific E3 ligases | Validated natural product inhibitor identified through virtual screening of compound libraries [1] |
| DUB Probes | UbV-based ABPs for UCHL1/UCHL3 [1] | DUB activity profiling and inhibition | Selective triple-mutant UbV-ABPs enable cell-specific DUB targeting and functional characterization [1] |
| PROTAC Molecules | ARV-110, ARV-471 [3] | Targeted protein degradation research | Clinical-stage PROTACs that recruit E3 ligases to degrade target oncoproteins [3] |
| Ubiquitin Linkage-Specific Antibodies | K48-linkage, K63-linkage antibodies [3] | Ubiquitin chain type determination | Immunoblotting and immunofluorescence detection of specific polyubiquitin chain architectures [3] |
| Proteasome Inhibitors | Bortezomib, Carfilzomib [9] | UPS functional blockade | Clinical inhibitors used to validate UPS-dependent processes and as cancer therapeutics [9] |
Therapeutic Targeting and Clinical Implications
Targeting the UPS represents a promising strategic approach for eliminating therapy-resistant cancer stem cells in multiple cancer types [9] [5]. Existing proteasome inhibitors, including bortezomib and carfilzomib, have demonstrated efficacy in certain hematological malignancies, though their application in solid tumors remains challenging [9]. More precise targeting of specific E3 ligases and DUBs offers potential for enhanced therapeutic specificity with reduced off-target effects [9].
The integration of UPS-targeted therapies with conventional chemotherapy, immunotherapy, and molecularly-targeted drugs represents an emerging frontier in oncological treatment strategies [9] [5]. For instance, targeting DUBs that stabilize immune checkpoints like PD-1/PD-L1 could synergize with existing immunotherapies to overcome resistance mechanisms [3]. USP2, a DUB that stabilizes PD-1 and promotes tumor immune escape through deubiquitination, represents one such promising target [3].
Advanced therapeutic modalities including PROTACs and molecular glue degraders offer innovative approaches to target traditionally "undruggable" oncoproteins by hijacking the endogenous UPS [1] [8]. ARV-110 and ARV-471 represent pioneering PROTAC drugs that have progressed to phase II clinical trials, demonstrating the clinical viability of this approach [3]. Molecular glue degraders such as CC-90009, which promotes GSPT1 degradation by recruiting the CRL4CRBN E3 ligase complex, further expand the toolkit for targeted protein degradation [3].
As research continues to decipher the complex roles of the UPS in cancer stem cell biology, therapeutic interventions targeting this system hold significant promise for addressing the persistent challenges of tumor recurrence, metastasis, and therapeutic resistance that characterize advanced malignancies.
Cancer Stem Cells (CSCs), also referred to as tumor-initiating cells (TICs), represent a distinct subpopulation within tumors that exhibit stem cell-like properties, including self-renewal capability, multi-lineage differentiation, and enhanced tumor-driving capacity [11] [12]. Although they constitute only a minority of tumor cells, CSCs have been identified as the central drivers of tumor initiation, progression, metastasis, therapeutic resistance, and relapse [12] [13]. The CSC concept challenges the traditional view of tumor homogeneity, proposing instead that tumors are organized hierarchically, with CSCs at the apex capable of regenerating the entire tumor heterogeneity [12]. The existence of CSCs was first definitively demonstrated in acute myeloid leukemia (AML) in the 1990s by John Edgar Dick and colleagues, who showed that only a specific subpopulation with a CD34⁺CD38⁻ phenotype could reconstitute leukemia in immunodeficient mice [13]. This foundational discovery has since been extended to various solid tumors, including breast cancer, glioblastoma, lung cancer, and head and neck squamous cell carcinoma, establishing CSCs as a fundamental component of tumor biology across cancer types [13] [14].
Biological Properties and Identification of CSCs
Defining Functional Properties of CSCs
CSCs possess three defining functional characteristics that distinguish them from the bulk of tumor cells. These properties collectively enable CSCs to initiate and maintain tumors, adapt to therapeutic pressures, and drive disease progression:
- Self-Renewal Capacity: The ability to undergo symmetrical or asymmetrical division to generate identical daughter cells that maintain the stem cell pool indefinitely [12]. This property ensures the long-term persistence of CSCs within tumors.
- Multi-Lineage Differentiation Potential: The capacity to differentiate into the heterogeneous cell populations that constitute the entire tumor mass, thereby establishing and maintaining tumor heterogeneity [12].
- Tumor-Initiating Ability: The potential to initiate and sustain tumor growth when transplanted into suitable host environments, which represents the functional gold standard for identifying CSCs [12] [13]. This capacity has been demonstrated through limiting dilution assays in immunodeficient mice, where CSCs can form tumors with far fewer cells compared to non-CSC populations [12].
CSC Markers and Identification
The identification and isolation of CSCs rely on specific surface markers and functional assays, though these markers vary significantly across different cancer types, reflecting tissue-specific origins and microenvironmental influences [13]. The table below summarizes key CSC markers across various cancer types:
Table 1: Cancer Stem Cell Markers Across Different Cancer Types
| Cancer Type | Key CSC Markers | Additional Functional Markers | References |
|---|---|---|---|
| Acute Myeloid Leukemia (AML) | CD34⁺CD38⁻ | - | [13] |
| Breast Cancer | CD44⁺CD24⁻/low | ALDH1⁺ | [11] [12] |
| Glioblastoma (GBM) | CD133⁺ | Nestin⁺, SOX2⁺ | [13] |
| Head and Neck Squamous Cell Carcinoma (HNSCC) | CD44⁺ | - | [14] |
| Gastrointestinal Cancers | LGR5⁺, CD166⁺ | - | [13] |
| Multiple Solid Tumors | CD133⁺ | - | [13] |
It is important to note that no universal CSC marker exists, and CSC identity appears to be shaped by both intrinsic genetic programs and extrinsic microenvironmental cues [13]. Furthermore, non-CSCs can acquire stem-like characteristics de novo in response to environmental stimuli such as hypoxia, inflammation, or therapeutic pressure, indicating that the CSC state represents a dynamic functional status rather than a fixed cellular hierarchy [13].
Molecular Mechanisms Governing CSC Maintenance
Core Signaling Pathways in CSC Regulation
CSCs utilize several evolutionarily conserved signaling pathways that normally regulate stem cell maintenance in development and adult tissues. These pathways form complex interconnected networks that sustain CSC self-renewal, survival, and plasticity:
- Wnt/β-catenin Signaling: Promotes self-renewal and maintains stemness by regulating key transcription factors. In the absence of Wnt, β-catenin is targeted for ubiquitination and degradation by the destruction complex [15]. Wnt activation stabilizes β-catenin, allowing its nuclear translocation and activation of stemness-associated genes [15].
- Notch Signaling: Regulates cell fate decisions and maintains CSC populations through cell-cell interactions. Notch activation leads to proteolytic cleavage of the receptor and release of the Notch intracellular domain (NICD), which translocates to the nucleus and activates target genes [9].
- Hedgehog Signaling: Contributes to CSC maintenance, particularly in cancers like glioblastoma and pancreatic cancer. The pathway is initiated when Hedgehog ligands bind to Patched receptors, relieving suppression of Smoothened and activating GLI transcription factors [12].
- Hippo-YAP Signaling: Regates organ size and stem cell function. In CSCs, YAP/TAZ activation promotes stemness and survival. The pathway is regulated by a kinase cascade that ultimately controls the localization and stability of YAP/TAZ transcriptional coactivators [9].
The diagram below illustrates the core regulatory network of these signaling pathways in maintaining CSC properties:
Ubiquitination in CSC Regulation
Ubiquitination, a fundamental post-translational modification, has emerged as a critical regulatory mechanism governing CSC functionality [9]. The ubiquitin-proteasome system (UPS) consists of a cascade of enzymes including ubiquitin-activating enzymes (E1), ubiquitin-conjugating enzymes (E2), and ubiquitin ligases (E3) that work in concert to attach ubiquitin molecules to target proteins, determining their stability, activity, and localization [3]. The reverse process, deubiquitination, is mediated by deubiquitinating enzymes (DUBs) that remove ubiquitin chains, providing an additional layer of regulation [7].
In CSCs, the ubiquitin system exerts precise control over key stemness transcription factors and signaling pathways:
- Stemness Transcription Factors: E3 ubiquitin ligases and DUBs modulate the stability of core pluripotency factors including SOX2, OCT4, KLF4, and c-MYC, which play crucial roles in CSC self-renewal and differentiation [9]. For instance, the E3 ligase FBXW7 targets c-MYC for degradation, while various DUBs can stabilize these factors to maintain stemness.
- Signaling Pathway Components: Ubiquitination regulates core CSC signaling pathways including Notch, Wnt/β-catenin, Hedgehog, and Hippo-YAP by controlling the turnover of key pathway components [9]. The E3 ligase Itch, for example, ubiquitinates Notch receptors, influencing Notch signaling activity in CSCs.
- Metabolic Regulators: The UPS controls metabolic enzymes crucial for CSC maintenance, such as pyruvate kinase M2 (PKM2). The E3 ligase Parkin facilitates PKM2 ubiquitination, while the DUB OTUB2 inhibits this process, enhancing glycolysis and promoting colorectal cancer progression [3].
The table below summarizes key ubiquitin system components involved in CSC regulation:
Table 2: Ubiquitination System Components Regulating Cancer Stem Cells
| Component Type | Specific Elements | Targets/Function in CSCs | References |
|---|---|---|---|
| E3 Ubiquitin Ligases | FBXW7 | Targets c-MYC for degradation | [9] |
| Parkin | Ubiquitinates PKM2 to regulate CSC metabolism | [3] | |
| Itch | Regulates Notch signaling in CSCs | [9] | |
| Deubiquitinases (DUBs) | OTUB2 | Inhibits PKM2 ubiquitination, enhancing glycolysis | [3] |
| USP2 | Stabilizes PD-1, promoting immune escape | [3] | |
| Ubiquitin Chains | K48-linked chains | Target proteins for proteasomal degradation | [7] |
| K63-linked chains | Regulate signal transduction and endocytosis | [7] | |
| Linear ubiquitin chains | Regulate NF-κB signaling through LUBAC complex | [3] |
The intricate regulation of CSCs by the ubiquitin system offers promising therapeutic opportunities. Existing proteasome inhibitors such as bortezomib and carfilzomib have shown promise in certain cancers, and more targeted approaches focusing on specific E3 ligases and DUBs are under development to selectively disrupt CSC maintenance while sparing normal stem cells [9].
CSCs in Tumor Initiation, Metastasis, and Drug Resistance
Role in Tumor Initiation and Progression
CSCs are defined by their remarkable tumor-initiating capacity, which represents the functional hallmark of this cellular subpopulation [12]. When transplanted into immunodeficient mice, CSCs can regenerate tumors that recapitulate the heterogeneity of the original tumor, while non-CSC populations lack this capacity [12] [13]. The tumor-initiating potential of CSCs is strongly correlated with the expression of specific genes and transcription factors. For instance:
- In glioblastoma, adenosine deaminase RNA-specific binding protein (ADAR1) promotes tumor initiation by enhancing ganglioside GM2 activator (GM2A) expression and inducing specific mutations in GLI1 that improve its nuclear localization [12].
- The transcription factor SOX9 plays a crucial role in regulating mammary stem and progenitor cells, with SOX9high cells exhibiting significantly higher tumor-inducing capacity compared to SOX9low counterparts [12].
- In melanoma, colon, and pancreatic cancers, CDK1 expression regulates the phosphorylation, localization, and transcriptional activity of the pluripotency-associated transcription factor SOX2, thereby influencing tumor initiation capacity [12].
Role in Metastasis
CSCs play a central role in the metastatic cascade, from initial departure from the primary tumor to successful colonization of distant organs [15]. The metastatic process involves multiple steps including local invasion, intravasation into blood or lymphatic vessels, survival in circulation, extravasation at distant sites, and eventual colonization [16]. CSCs contribute to each of these stages through several mechanisms:
- Epithelial-to-Mesenchymal Transition (EMT): CSCs can undergo EMT, a process where cells lose epithelial characteristics and gain mesenchymal properties, enhancing migratory capacity and invasiveness [16]. EMT is regulated by transcription factors such as Snail, Slug, and Twist, which are activated by pathways like TGF-β and Wnt/β-catenin [16].
- Proteolytic Enzyme Systems: CSCs utilize proteolytic systems including the urokinase plasminogen activator (uPA) system and matrix metalloproteinases (MMPs) to degrade extracellular matrix components and facilitate invasion and intravasation [16]. The uPA system is particularly significant, as it activates plasminogen to plasmin and subsequently activates MMPs like MMP-2 and MMP-9 that degrade basement membranes [16].
- Stem Cell-Like Migratory Properties: CSCs share molecular mechanisms with normal stem cell migration, utilizing overlapping sets of molecules and pathways that facilitate movement and colonization [15].
- Pre-Metastatic Niche Formation: Primary tumors can prepare distant sites for metastasis by secreting factors that create a supportive "pre-metastatic niche." CSCs subsequently colonize these prepared microenvironments [15].
The diagram below illustrates the role of CSCs in the metastatic cascade:
Mechanisms of Therapy Resistance
CSCs employ multiple sophisticated mechanisms to evade conventional cancer therapies, making them central players in treatment failure and disease recurrence:
- Enhanced DNA Repair Capacity: CSCs possess more efficient DNA repair mechanisms than non-CSCs, enabling them to survive DNA-damaging therapies like radiation and chemotherapy [14].
- Drug Efflux Transporters: CSCs highly express ATP-binding cassette (ABC) transporters that actively pump chemotherapeutic drugs out of the cell, reducing intracellular drug accumulation [12].
- Quiescence: A subset of CSCs can enter a quiescent or dormant state, making them resistant to therapies that target rapidly dividing cells [14].
- Epigenetic Plasticity: CSCs exhibit dynamic epigenetic modifications that allow for adaptive responses to therapeutic stress, including transitions between drug-sensitive and resistant states [12].
- Metabolic Flexibility: CSCs can switch between different metabolic pathways (glycolysis, oxidative phosphorylation, and alternative fuel sources) to survive under diverse environmental conditions, including therapy-induced stress [13].
- Interaction with the Tumor Microenvironment (TME): The TME provides protective niches that shield CSCs from therapies. Components such as tumor-associated macrophages (TAMs), cancer-associated fibroblasts (CAFs), and other stromal cells secrete factors that promote CSC survival and drug resistance [12].
Experimental Models and Methodologies for CSC Research
In Vitro Models and Functional Assays
The study of CSCs relies on specialized experimental models and functional assays that enable the identification, isolation, and characterization of this critical cellular subpopulation:
- Sphere Formation Assays: Under non-adherent, serum-free conditions, CSCs form three-dimensional spheroids that enrich for stem-like cells and demonstrate self-renewal capacity in vitro [17]. This assay serves as a fundamental method for assessing CSC frequency and functional properties.
- Flow Cytometry and Cell Sorting: Surface markers such as CD44, CD24, CD133, and ALDH1 activity are used to identify and isolate CSC populations using fluorescence-activated cell sorting (FACS) [11] [12].
- Organoid Cultures: Three-dimensional organoid models derived from patient tumors or cancer cell lines maintain CSC populations and recapitulate tumor heterogeneity more effectively than traditional 2D cultures [13]. These models enable long-term expansion of CSCs while preserving their stemness properties.
- Migration and Invasion Assays: Transwell assays with or without Matrigel coating are used to evaluate the migratory and invasive capabilities of CSCs, which are critical for metastatic potential [16].
- Extracellular Matrix (ECM) Degradation Assays: These assays assess the ability of CSCs to degrade ECM components using fluorescently-labeled matrix proteins, evaluating the activity of proteolytic systems like uPA and MMPs [16].
In Vivo Models for CSC Study
In vivo models provide essential physiological context for studying CSC biology and therapeutic responses:
- Xenograft Models: Immunodeficient mice (such as SCID or NSG strains) are transplanted with human tumor cells to assess tumor-initiating capacity through limiting dilution assays [12] [13]. This represents the gold standard for functional validation of CSCs.
- Genetically Engineered Mouse Models (GEMMs): These models enable the study of CSCs in their native microenvironment, with spontaneous tumor development that recapitulates the natural history of human cancers [16].
- Lineage Tracing: Advanced genetic approaches allow tracking of CSC fate and dynamics in living animals, providing insights into CSC hierarchy, plasticity, and contribution to tumor maintenance [12].
- Patient-Derived Xenografts (PDX): Tumors obtained directly from patients are engrafted into immunodeficient mice, preserving the original tumor heterogeneity and CSC characteristics better than cell line-derived models [16].
The Scientist's Toolkit: Essential Research Reagents
Table 3: Essential Research Reagents for CSC Investigations
| Reagent/Category | Specific Examples | Primary Research Application | References |
|---|---|---|---|
| Surface Marker Antibodies | Anti-CD44, Anti-CD24, Anti-CD133 | Identification and isolation of CSCs by FACS | [12] [13] |
| ALDH Activity Assay | ALDEFLUOR Kit | Functional identification of CSCs based on ALDH enzyme activity | [12] |
| CSC Culture Media | Serum-free media with growth factors (EGF, FGF) | Sphere formation assays and CSC expansion | [17] |
| Proteasome Inhibitors | Bortezomib, Carfilzomib | Investigating ubiquitin system in CSC regulation | [9] |
| Pathway Inhibitors | Wnt, Notch, Hedgehog inhibitors | Targeting core stemness signaling pathways | [9] [14] |
| 3D Culture Matrices | Matrigel, Collagen I | Organoid and spheroid cultures for CSC maintenance | [13] [16] |
| CSC Reporter Systems | GFP/Luciferase under stemness promoters | Lineage tracing and in vivo CSC tracking | [12] [16] |
Therapeutic Targeting of CSCs and Clinical Implications
Emerging Therapeutic Strategies
The development of effective therapies targeting CSCs represents a promising frontier in oncology, with multiple approaches under investigation:
- Ubiquitin System-Targeted Therapies: Small molecules targeting specific E3 ubiquitin ligases or deubiquitinases (DUBs) offer precision approaches to disrupt CSC maintenance [9]. Proteolysis-targeting chimeras (PROTACs) represent an innovative technology that harnesses the ubiquitin system to degrade specific oncoproteins in CSCs [3].
- Immunotherapy Approaches: Chimeric antigen receptor T-cell (CAR-T) therapies targeting CSC-specific surface markers such as EpCAM have shown promise in preclinical models [13]. Immune checkpoint inhibitors combined with CSC-targeted vaccines are also being explored to overcome CSC-mediated immune evasion [12].
- Differentiation Therapy: Agents that induce CSC differentiation into more mature, therapy-sensitive states represent a promising strategy to reduce the CSC pool [14].
- Metabolic Interventions: Targeting CSC metabolic vulnerabilities, such as dual inhibition of glycolysis and oxidative phosphorylation, can exploit the metabolic dependencies of CSCs [13].
- Nanoparticle-Based Delivery Systems: Nanotechnology enables targeted delivery of CSC-active agents to tumor sites, improving efficacy while reducing systemic toxicity [17].
- Epigenetic Modulators: Inhibitors of DNA methyltransferases and histone deacetylases can reverse epigenetic modifications that maintain CSC stemness [14].
Current Challenges and Future Perspectives
Despite significant advances, several challenges remain in translating CSC-targeted therapies to clinical practice:
- Biomarker Development: The lack of universal, reliable CSC biomarkers hampers patient stratification and treatment monitoring [13]. Developing robust biomarkers to track CSC dynamics in real-time represents a critical need.
- Therapeutic Toxicity: Achieving selective toxicity against CSCs while sparing normal stem cells remains challenging due to shared signaling pathways and regulatory mechanisms [13].
- Tumor Heterogeneity and Plasticity: The dynamic nature of CSCs and their ability to transition between states complicates therapeutic targeting [12].
- Microenvironmental Protection: The TME provides sanctuary for CSCs, necessitating combination approaches that simultaneously target CSCs and their supportive niches [12].
Future research directions include the integration of multi-omics technologies (single-cell sequencing, spatial transcriptomics) with artificial intelligence to decipher CSC heterogeneity and identify novel vulnerabilities [13]. Additionally, advanced preclinical models that better recapitulate human tumor biology and the development of rational combination therapies will be essential for overcoming CSC-mediated therapy resistance [14].
Cancer Stem Cells represent a critical subpopulation within tumors that drive tumor initiation, metastasis, therapy resistance, and recurrence. Their unique biological properties, including self-renewal capacity, differentiation potential, and remarkable plasticity, are maintained by complex molecular networks involving core signaling pathways and precise regulation through mechanisms such as ubiquitination. While significant challenges remain in targeting CSCs therapeutically, advances in our understanding of CSC biology, coupled with innovative therapeutic approaches targeting their specific vulnerabilities, offer promising avenues for overcoming treatment resistance and improving patient outcomes. The continued integration of basic mechanistic studies with translational and clinical research will be essential for developing effective CSC-targeted therapies that can ultimately change the landscape of cancer treatment.
Cancer stem cells (CSCs) constitute a minor subpopulation within tumors characterized by unlimited self-renewal, differentiation potential, and enhanced resistance to conventional therapies. These cells drive tumor initiation, metastasis, and recurrence, presenting a significant challenge in oncology [5] [18]. The molecular foundation of CSC maintenance relies on a network of core stemness transcription factors, primarily SOX2, OCT4, and Nanog, alongside the pleiotropic regulator c-Myc [19]. These factors coordinate a transcriptional program that sustains the undifferentiated, self-renewing state of CSCs, mirroring their roles in embryonic stem cells [20].
Post-translational modifications, particularly ubiquitination, provide a critical regulatory layer controlling the stability and activity of these core stemness factors. The ubiquitin-proteasome system (UPS) precisely governs the "quantity" and "quality" of specific proteins to ensure cellular homeostasis, making it a fundamental process in determining CSC fate [5]. Ubiquitination involves a sequential enzymatic cascade comprising ubiquitin-activating (E1), conjugating (E2), and ligase (E3) enzymes, with E3 ligases conferring substrate specificity [21]. The reverse process, deubiquitination, is catalyzed by deubiquitinating enzymes (DUBs) that remove ubiquitin moieties, protecting proteins from degradation [21]. Dysregulation of this balance directly influences CSC properties by modulating the key transcription factors that define their identity, offering promising therapeutic avenues for selectively targeting this resilient cell population [5] [9].
Ubiquitination Landscapes of Core Stemness Transcription Factors
The stability and activity of core stemness transcription factors are precisely regulated by specific E3 ubiquitin ligases and deubiquitinating enzymes. The following table summarizes the key regulatory mechanisms for each factor.
Table 1: Ubiquitination Regulation of Core Stemness Transcription Factors
| Transcription Factor | Regulating E3 Ubiquitin Ligases | Regulating DUBs (if mentioned) | Ubiquitination Type & Function | Biological Outcome in CSCs |
|---|---|---|---|---|
| OCT4 | WWP2, ITCH, CHIP [20] | Information not covered in search results | K48-linked degradation [20] | Reduces OCT4 stability, inhibits breast CSC production [20] |
| SOX2 | Information not covered in search results | Information not covered in search results | Information not covered in search results | Information not covered in search results |
| Nanog | Information not covered in search results | Information not covered in search results | Target of ubiquitination [5] | Role in maintaining stemness and pluripotency [5] |
| c-Myc | FBW7 (SCF complex) [22] | Information not covered in search results | K48-linked degradation [22] | FBW7 deletion causes c-Myc overexpression; can induce apoptosis in leukemic initiating cells [22] |
OCT4 Ubiquitination
OCT4 is a pivotal transcription factor for maintaining pluripotency, and its protein stability is controlled by several E3 ubiquitin ligases. The E3 ligase WWP2 promotes the ubiquitination and degradation of OCT4 in human embryonic stem cells (hESCs) [20]. Similarly, ITCH regulates OCT4 transcription and degradation in mouse embryonic stem cells (mESCs) [20]. Notably, the E3 ligase CHIP (Carboxy terminus of HSP70-interacting protein) ubiquitinates OCT4 at lysine 284, which reduces OCT4 stability and subsequently inhibits human breast CSC production [20]. Furthermore, OCT4 is subject to other post-translational modifications that influence its activity, including phosphorylation and SUMOylation, which can interact with ubiquitination to fine-tune its function [20].
Nanog and SOX2 as Ubiquitination Targets
Quantitative proteomic analyses have revealed that core transcription factors, including Nanog and SOX2, are targets for ubiquitination, hinting at a crucial role for this modification in sustaining stemness and pluripotency [5]. While the specific E3 ligases and DUBs for SOX2 are not detailed in the provided search results, its regulatory partnership with OCT4 is emphasized. Acetylation of both OCT4 and SOX2 can attenuate their transcriptional activity by impairing heterodimer formation, indicating a complex interplay between different post-translational modifications [20].
c-Myc Ubiquitination by the SCFFBW7 Complex
The stability of the c-Myc oncoprotein is rigorously controlled by the ubiquitin-proteasome system. The SCF (SKP1-CUL1-F-box protein) complex, a major class of RING-type E3 ligases, targets c-Myc for degradation. Specifically, FBW7 (F-box and WD repeat domain-containing 7), the substrate-recognition component of the SCF complex, directs the ubiquitination and proteasomal degradation of c-Myc [22]. This regulation is critical in CSC populations; for instance, the ablation of Fbw7 in leukemic initiating cells (LICs) results in c-Myc overexpression, which, contrary to expectations, can lead to p53-dependent apoptosis and exhaustion of LICs, demonstrating the context-dependent effects of ubiquitination regulation [22].
Experimental Methodologies for Studying Ubiquitination
Investigating the ubiquitination of stemness factors requires a combination of molecular biology, biochemistry, and cellular functional assays. Below are detailed protocols for key experiments cited in the literature.
Co-Immunoprecipitation (Co-IP) and Ubiquitination Assays
This protocol is used to identify interactions between an E3 ligase and its substrate (e.g., CHIP and OCT4) and to detect protein ubiquitination.
- Objective: To confirm physical interaction and specific ubiquitination of a target protein.
- Detailed Procedure:
- Cell Lysis and Preparation: Harvest cells expressing the protein of interest (e.g., OCT4). Lyse cells using a non-denaturing RIPA buffer (e.g., 50 mM Tris-HCl pH 8.0, 150 mM NaCl, 1% NP-40, 0.5% sodium deoxycholate, 0.1% SDS) supplemented with protease inhibitors (e.g., PMSF, aprotinin) and 10 mM N-Ethylmaleimide (NEM) to inhibit endogenous DUBs.
- Immunoprecipitation: Pre-clear the cell lysate with Protein A/G agarose beads. Incubate the pre-cleared lysate with an antibody specific to the target protein (e.g., anti-OCT4 antibody) or a control IgG overnight at 4°C with gentle rotation. Then, add Protein A/G beads and incubate for 2-4 hours.
- Bead Washing: Pellet the beads and wash extensively with lysis buffer (3-5 times) to remove non-specifically bound proteins.
- Immunoblotting: Elute the bound proteins by boiling in SDS-PAGE loading buffer. Separate the proteins by SDS-PAGE and transfer to a PVDF membrane. Probe the membrane with an anti-ubiquitin antibody (e.g., P4D1) to detect ubiquitination. To confirm the interaction, reprobe the membrane with an antibody against the suspected E3 ligase (e.g., anti-CHIP antibody) [20].
- Key Controls:
- IgG control for immunoprecipitation specificity.
- Total cell lysate input control.
- Use of proteasome inhibitor (e.g., MG132) to enhance detection of ubiquitinated species.
Cycloheximide (CHX) Chase Assay
This assay measures the half-life of a protein to determine if an E3 ligase or DUB affects its stability.
- Objective: To assess the degradation rate of a protein (e.g., OCT4) upon inhibition of protein synthesis.
- Detailed Procedure:
- Cell Treatment: Culture cells and transfect with plasmids expressing the E3 ligase (e.g., CHIP) or a control vector. Optionally, treat cells with a proteasome inhibitor (MG132, 10-20 µM) or a DUB inhibitor to confirm UPS dependency.
- Inhibition of Protein Synthesis: Add cycloheximide (CHX, typically 100 µg/mL) to the culture medium to block new protein synthesis.
- Time-Course Harvesting: Harvest cell pellets at predetermined time points (e.g., 0, 30, 60, 120, 240 minutes) after CHX addition.
- Protein Level Analysis: Lyse the cells and quantify protein concentration. Analyze the levels of the target protein (OCT4) and a loading control (e.g., GAPDH or Tubulin) by western blotting.
- Quantification: Use densitometry software to quantify band intensities. Plot the relative protein level against time to calculate the half-life [20].
- Key Controls:
- Control vector transfection.
- Untreated (0-hour) time point as a baseline.
In Vitro Ubiquitination Assay
This is a direct, cell-free assay to confirm that an E3 ligase can ubiquitinate a substrate protein.
- Objective: To reconstitute the ubiquitination reaction in vitro using purified components.
- Detailed Procedure:
- Protein Purification: Purify the recombinant E3 ligase (e.g., CHIP), the substrate (e.g., OCT4), E1 enzyme, E2 enzyme (e.g., UbcH5a), and ubiquitin.
- Reaction Setup: In a reaction tube, combine the following components in a suitable buffer (e.g., 50 mM Tris-HCl, pH 7.5, 2 mM ATP, 5 mM MgCl2):
- E1 enzyme (50 nM)
- E2 enzyme (200 nM - 1 µM)
- E3 ligase (1-2 µM)
- Substrate protein (1-2 µM)
- Ubiquitin (10-20 µM)
- Incubation: Incubate the reaction at 30°C for 1-2 hours.
- Reaction Termination: Stop the reaction by adding SDS-PAGE loading buffer and boiling.
- Analysis: Analyze the products by western blotting. A smear or ladder of higher molecular weight species when probed with an anti-substrate (OCT4) or anti-ubiquitin antibody indicates successful polyubiquitination [20].
- Key Controls:
- Omission of E1, E2, E3, or ATP from the reaction as negative controls.
Diagram 1: A flowchart summarizing the key experimental methodologies used to study the ubiquitination of stemness transcription factors, from initial interaction confirmation to functional validation.
The Scientist's Toolkit: Key Research Reagents
The following table lists essential reagents and tools for investigating the ubiquitination of core stemness factors, as derived from the cited research.
Table 2: Essential Research Reagents for Studying Ubiquitination in CSCs
| Reagent/Tool | Specific Example | Function in Research |
|---|---|---|
| E3 Ubiquitin Ligase Constructs | CHIP, WWP2, ITCH, FBW7 expression plasmids [22] [20] | To overexpress or knock down specific E3s and assess their impact on substrate stability and CSC function. |
| Proteasome Inhibitors | MG132, Bortezomib, Carfilzomib [9] | To block proteasomal degradation, allowing accumulation of ubiquitinated proteins for detection and functional studies. |
| Deubiquitinase (DUB) Inhibitors | Information not covered in search results | To prevent deubiquitination, stabilizing ubiquitin chains on substrates and helping identify DUB-substrate relationships. |
| Specific Antibodies | Anti-OCT4, Anti-SOX2, Anti-Nanog, Anti-c-Myc, Anti-Ubiquitin [5] [20] | For detection, immunoprecipitation, and localization of target proteins and their ubiquitinated forms via western blot, immunofluorescence, and Co-IP. |
| Protein Synthesis Inhibitor | Cycloheximide (CHX) [20] | To halt new protein synthesis in chase assays, enabling measurement of protein half-life and degradation kinetics. |
| CSC Functional Assays | Sphere Formation Assay, ALDH Activity Assay [5] [23] | To assess the functional consequences of manipulating ubiquitination on self-renewal and stemness in vitro. |
Therapeutic Implications and Future Perspectives
Targeting the ubiquitination machinery regulating stemness factors presents a promising but complex strategy for eradicating CSCs. The development of PROTACs (Proteolysis-Targeting Chimeras) is a leading therapeutic approach. PROTACs are bifunctional molecules that recruit a target protein (e.g., a stemness transcription factor) to a specific E3 ligase, inducing its degradation [21]. This offers the potential to directly dismantle the core regulatory network of CSCs. Furthermore, existing proteasome inhibitors like bortezomib and carfilzomib have shown efficacy in some cancers, but their broad activity limits specificity [9]. Future efforts are focused on developing small-molecule inhibitors or activators that target specific E3 ligases or DUBs, offering a more precise method to modulate the stability of individual oncoproteins like c-Myc or OCT4 [21] [24].
A significant challenge in this field is the context-dependent duality of many E3 ligases. For example, while FBW7 acts as a tumor suppressor by degrading c-Myc and Notch, its loss in some leukemic models can lead to cell death due to excessive c-Myc accumulation [22]. This highlights the need for a deep understanding of tissue and cancer-type specific effects. The intricate crosstalk between ubiquitination and other PTMs adds another layer of complexity. For instance, phosphorylation of OCT4 can regulate its ubiquitination, and acetylation can affect its partnership with SOX2 [20] [24]. Therefore, successful therapeutic strategies will likely require an integrated approach that considers the entire PTM landscape governing CSC maintenance.
Diagram 2: A regulatory network showing the balance between ubiquitination and deubiquitination in controlling stemness factor stability, its modulation by other PTMs, and potential therapeutic intervention points.
The ubiquitination of core stemness transcription factors represents a critical regulatory node in maintaining the CSC state. As detailed in this review, E3 ligases such as CHIP, WWP2, and FBW7 precisely control the protein levels of OCT4, c-Myc, and other key players, directly influencing self-renewal, tumor initiation, and drug resistance. The experimental frameworks and toolkits outlined provide a roadmap for ongoing research into these complex mechanisms. While challenges remain, particularly regarding the contextual duality of ubiquitin components and their crosstalk with other signaling pathways, the continued development of targeted therapies like PROTACs holds significant promise. By strategically manipulating the ubiquitin system, the scientific community moves closer to the goal of effectively targeting the resilient CSC population, a crucial step toward overcoming cancer recurrence and therapeutic resistance.
Cancer stem cells (CSCs) represent a subpopulation within tumors characterized by high capacities for self-renewal, differentiation, and reconstitution of tumor heterogeneity [25]. These cells are major contributors to tumor initiation, metastasis, and therapy resistance in cancer [25]. The regulation of CSC maintenance and function is controlled by key developmental signaling pathways, including Notch, Wnt/β-catenin, and Hedgehog (HH) [9] [25]. Emerging evidence indicates that ubiquitination-mediated post-translational modification plays a fundamental role in the maintenance of CSC characteristics [25].
The ubiquitin-proteasome system (UPS) comprises a sequential enzymatic network where E3 ubiquitin ligases (E3s) and deubiquitinating enzymes (DUBs) serve as the main actors [26]. The dynamic balance between E3s and DUBs dictates the abundance and fate of cellular proteins, affecting both physiological and pathological processes [26]. This technical review examines the intricate mechanisms through which E3 ligases and DUBs regulate the core CSC signaling pathways, highlighting their implications for targeted therapeutic interventions.
Ubiquitination is a post-translational modification process wherein a highly conserved 76-amino acid ubiquitin protein is covalently conjugated to lysine residues on substrate proteins through a sequential enzymatic cascade [27]. The process involves E1 (ubiquitin-activating), E2 (ubiquitin-conjugating), and E3 (ubiquitin-ligase) enzymes [25] [27]. E3 ligases are particularly crucial as they confer substrate specificity, with approximately 600 identified in humans [25]. These enzymes are classified based on their structural domains and mechanisms of ubiquitin transfer:
- HECT domain E3s: Transfer ubiquitin directly from E2 to the substrate [25]
- RING domain E3s: Facilitate ubiquitin transfer by binding both E2 and substrate [25]
- RBR E3s: Utilize a hybrid RING-HECT mechanism [25]
Ubiquitination is reversible through the action of DUBs, which cleave ubiquitin from substrate proteins [25] [27]. Approximately 100 DUBs have been identified in the human genome, categorized into several families including ubiquitin-specific proteases (USPs), ubiquitin carboxy-terminal hydrolases (UCHs), ovarian-tumor proteases (OTUs), and JAMM/MPN domain-associated metallopeptidases [27].
Table 1: Major Enzyme Classes in the Ubiquitin-Proteasome System
| Enzyme Class | Representative Members | Function in Ubiquitination | Role in Reversal |
|---|---|---|---|
| E1 Activating Enzymes | UBA1, UBA6 | Activates ubiquitin in ATP-dependent manner | - |
| E2 Conjugating Enzymes | ~30 members in humans | Carries activated ubiquitin | - |
| E3 Ligases | ~600 members in humans | Confers substrate specificity | - |
| HECT-type E3s | SMURF1/2, ITCH, WWP1/2, NEDD4 | Direct ubiquitin transfer to substrate | - |
| RING-type E3s | RNF43, ZNRF3, β-TrCP | Facilitates ubiquitin transfer | - |
| DUBs | USP22, OTUB2, CYLD | - | Removes ubiquitin from substrates |
Regulation of Notch Signaling by E3 Ligases and DUBs
The Notch signaling pathway is highly conserved throughout evolution and plays crucial roles in cell fate determination, embryonic development, organ formation, and tissue repair [28]. In mammals, four Notch receptors (Notch1-4) and five ligands (JAG1, JAG2, DLL1, DLL3, DLL4) have been identified [28]. The canonical Notch signaling activation involves a series of proteolytic cleavages upon ligand-receptor interaction, resulting in the release of the Notch intracellular domain (NICD) which translocates to the nucleus and activates transcription of target genes [28].
Figure 1: Regulation of Notch Signaling by E3 Ligases and DUBs. The diagram illustrates the canonical Notch signaling pathway and its regulation by ubiquitination machinery. E3 ligases (green) promote NICD degradation, while DUBs (red) stabilize NICD.
Key Regulatory E3 Ligases and DUBs in Notch Signaling
The stability and activity of Notch signaling components are tightly regulated by E3 ligases and DUBs. FBXW7 (a subunit of the SCF E3 ubiquitin ligase complex) targets NICD for proteasomal degradation, acting as a critical negative regulator of Notch signaling [28]. Additionally, several E3 ligases including CBL, ITCH, and DELTEX have been implicated in regulating Notch receptor turnover and activity [28].
On the reversal side, specific DUBs counteract E3 ligase activity to maintain Notch signaling homeostasis. While the search results do not specify all DUBs regulating Notch, the intricate balance between ubiquitination and deubiquitination is crucial for proper pathway function [27] [28].
Table 2: E3 Ligases and DUBs Regulating Notch Signaling in CSCs
| Regulator | Type | Target | Functional Outcome | Role in CSCs |
|---|---|---|---|---|
| FBXW7 | E3 Ligase | NICD | Promotes degradation of activated NICD | Suppresses stemness; loss promotes CSC maintenance |
| CBL | E3 Ligase | Notch Receptor | Regulates receptor turnover | Modulates CSC self-renewal |
| ITCH | E3 Ligase | Notch Components | Controls pathway activity | Affects CSC proliferation |
| Unspecified DUBs | DUB | NICD/Notch Receptor | Stabilizes signaling components | Promotes stemness properties |
Regulation of Wnt/β-catenin Signaling by E3 Ligases and DUBs
The Wnt/β-catenin pathway plays critical roles in embryonic development, adult tissue homeostasis, cell proliferation, and stem cell regulation [29] [30]. In the absence of Wnt ligands, cytoplasmic β-catenin is phosphorylated by a destruction complex comprising AXIN, adenomatous polyposis coli (APC), glycogen synthase kinase-3β (GSK-3β), and casein kinase 1 (CK1), leading to its ubiquitination and proteasomal degradation [29] [30]. When Wnt ligands bind to Frizzled (Fz) receptors and LRP5/6 coreceptors, the destruction complex is disrupted, allowing β-catenin to accumulate and translocate to the nucleus where it activates target gene expression through TCF/LEF transcription factors [29] [30].
Key Regulatory E3 Ligases and DUBs in Wnt/β-catenin Signaling
Multiple E3 ligases and DUBs precisely regulate Wnt/β-catenin signaling components:
E3 Ligases:
- β-TrCP: Recognizes phosphorylated β-catenin, targeting it for ubiquitination and degradation [29]
- RNF43/ZNRF3: Membrane-associated E3 ligases that ubiquitinate Frizzled receptors, promoting their endocytosis and degradation [29]
- APC: Component of the destruction complex that facilitates β-catenin recognition by E3 ligases [30]
DUBs:
- USP22: Promotes stemness and tumor progression; identified as a promising therapeutic target in CSCs [31]
- CYLD: Removes ubiquitin chains from multiple Wnt pathway components [3]
- OTULIN: Regulates genotoxic Wnt/β-catenin pathway activation through linear deubiquitination [3]
Figure 2: Regulation of Wnt/β-catenin Signaling by E3 Ligases and DUBs. The diagram illustrates key regulatory points in the Wnt pathway where E3 ligases (green) promote degradation of pathway components, while DUBs (red) stabilize them.
Table 3: E3 Ligases and DUBs Regulating Wnt/β-catenin Signaling in CSCs
| Regulator | Type | Target | Functional Outcome | Role in CSCs |
|---|---|---|---|---|
| β-TrCP | E3 Ligase | β-catenin | Targets phosphorylated β-catenin for degradation | Limits CSC self-renewal |
| RNF43/ZNRF3 | E3 Ligase | Frizzled Receptors | Promotes receptor degradation | Negative regulators of Wnt signaling in CSCs |
| APC | E3 Ligase Complex Component | β-catenin | Facilitates β-catenin recognition | Tumor suppressor in CSC maintenance |
| USP22 | DUB | Unspecified Wnt Components | Stabilizes pathway components | Promotes stemness; therapeutic target |
| CYLD | DUB | Multiple Wnt Components | Removes ubiquitin chains | Suppresses CSC properties |
| OTULIN | DUB | Linear Ubiquitin Chains | Activates Wnt/β-catenin pathway | Enhances CSC signaling |
Regulation of Hedgehog Signaling by E3 Ligases and DUBs
The Hedgehog (HH) pathway governs cell proliferation and patterning during embryonic development and is involved in regeneration, homeostasis, and stem cell maintenance in adult tissues [26]. In mammals, three HH ligands (SHH, IHH, DHH) bind to the Patched (PTCH) receptor, relieving its inhibition of Smoothened (SMO) [26]. Activated SMO triggers the nuclear localization of GLI transcription factors (GLI1, GLI2, GLI3), which activate target gene expression [26]. The primary cilium plays a crucial role in coordinating HH signal transduction in vertebrates [26].
Key Regulatory E3 Ligases and DUBs in Hedgehog Signaling
HH signaling is finely modulated at multiple levels by E3 ligases and DUBs:
E3 Ligases:
- SCFβ-TrCP: Promotes proteolytic processing of GLI proteins into repressor forms and degradation of GLI1 [26]
- HIB/Roadkill/SPOP: Cullin3-based E3 ligase complex that targets GLI proteins for degradation [26]
- ITCH: HECT-type E3 ligase that mediates degradation of GLI1 and PTCH1 [26]
- SMURF: Regulates SMO ubiquitylation and trafficking in Drosophila [26]
DUBs:
- USP48: Stabilizes GLI proteins, enhancing HH signaling output [26]
- USP7: Modulates GLI1 stability and activity [26]
- UCHL5: Regulates SMO ciliary accumulation and HH pathway activation [26]
Table 4: E3 Ligases and DUBs Regulating Hedgehog Signaling in CSCs
| Regulator | Type | Target | Functional Outcome | Role in CSCs |
|---|---|---|---|---|
| SCFβ-TrCP | E3 Ligase | GLI Proteins | Promotes processing into repressors & degradation | Limits CSC maintenance |
| SPOP Complex | E3 Ligase | GLI Proteins | Targets GLI for degradation | Suppresses stemness |
| ITCH | E3 Ligase | GLI1, PTCH1 | Mediates degradation of key pathway components | Negative regulator of HH in CSCs |
| SMURF | E3 Ligase | SMO | Regulates SMO trafficking and stability | Modulates HH signaling in CSCs |
| USP48 | DUB | GLI Proteins | Stabilizes GLI transcription factors | Enhances HH signaling in CSCs |
| USP7 | DUB | GLI1 | Modulates GLI1 stability and activity | Promotes CSC maintenance |
| UCHL5 | DUB | SMO | Regulates SMO ciliary accumulation | Activates HH pathway in CSCs |
Experimental Approaches for Studying Ubiquitination in CSC Pathways
Methodologies for Assessing Protein Ubiquitination
Ubiquitination Assays:
- Co-immunoprecipitation (Co-IP) with Ubiquitin Detection: Cells are transfected with tagged ubiquitin (HA-Ub, FLAG-Ub, Myc-Ub) and target plasmids. After treatment with proteasome inhibitor (MG132), cell lysates are immunoprecipitated with target protein antibody and probed with ubiquitin antibody to detect ubiquitination [29] [26].
- Tandem Ubiquitin Binding Entities (TUBEs): Utilize recombinant UBA domains with high affinity for polyubiquitin chains to isolate ubiquitinated proteins from cell lysates, protecting them from DUBs during extraction [26].
- In vivo Denaturation Techniques: Use of strong denaturants (SDS, Guanidine HCl) in lysis buffers to preserve labile ubiquitin linkages while disrupting non-covalent interactions [26].
Pulse-Chase Experiments: Measure protein half-life by metabolic labeling with 35S-methionine/cysteine followed by immunoprecipitation of target protein at time intervals. Treatment with cycloheximide to block new protein synthesis enhances assessment of degradation kinetics [26].
Identification of E3 Ligases and DUBs
RNA Interference Screens:
- siRNA/shRNA Libraries: Targeted or genome-wide screens to identify E3s/DUBs regulating specific CSC pathways. Readouts include luciferase reporters (TOPFlash for Wnt, GLI-luc for HH), target gene expression (qRT-PCR), and protein stability (Western blot) [26] [27].
Yeast Two-Hybrid Screening: Identification of novel E3-DUB interactions using known pathway components as bait against human E3/DUB libraries [26].
CRISPR-Cas9 Screening:
- GeCKO Libraries: Genome-wide knockout screens to identify essential E3s/DUBs for CSC maintenance using viability, sphere formation, and drug resistance as endpoints [26] [27].
Functional Validation in Cancer Stem Cells
In vitro CSC Models:
- Tumor Sphere Formation: Primary tumorspheres are dissociated and plated as single cells in ultra-low attachment plates with growth factors (EGF, bFGF). Sphere number and size are quantified after E3/DUB modulation [25].
- Flow Cytometry for CSC Markers: Analysis of ALDH activity (ALDEFLUOR assay) and surface markers (CD44, CD133, CD24) following E3/DUB targeting [25].
- Clonogenic Assays: Assessment of self-renewal capacity through limiting dilution assays in semisolid media [25].
In vivo Tumorigenesis Models:
- Limiting Dilution Transplantation: Serial dilutions of control vs. E3/DUB-modified cells injected into immunocompromised mice (NSG) to assess CSC frequency using extreme limiting dilution analysis (ELDA) software [25].
- Patient-Derived Xenografts (PDXs): Treatment of established PDX tumors with E3/DUB inhibitors to assess effects on tumor growth and CSC frequency [25].
The Scientist's Toolkit: Research Reagent Solutions
Table 5: Essential Research Reagents for Studying Ubiquitination in CSC Pathways
| Reagent Category | Specific Examples | Experimental Application | Key Considerations |
|---|---|---|---|
| Ubiquitin Expression Constructs | HA-Ub, FLAG-Ub, Myc-Ub, K-only mutants (K48R, K63R) | Ubiquitination assays | K-only mutants determine chain topology specificity |
| Proteasome Inhibitors | MG132, Bortezomib, Carfilzomib | Stabilize ubiquitinated proteins | Cytotoxic at prolonged exposures; optimize treatment duration |
| E3 Ligase Modulators | MLN4924 (NEDD8 activator inhibitor), PROTACs | Functional studies of E3 activity | MLN4924 inhibits cullin-RING ligases broadly |
| DUB Inhibitors | PR-619 (pan-DUB inhibitor), USP-specific inhibitors | Functional validation of DUB targets | Pan-inhibitors lack specificity; use with validation controls |
| CSC Culture Supplements | B27, N2, EGF, bFGF, Noggin | Tumorsphere assays | Serum-free conditions essential for stem cell maintenance |
| Pathway Reporters | TOPFlash (Wnt), GLI-luc (HH), CBF1-luc (Notch) | Pathway activity screening | Normalize to constitutive controls (Renilla luciferase) |
| Antibody Resources | Anti-ubiquitin (P4D1, FK2), anti-K48/K63 linkage-specific | Detection of ubiquitinated proteins | FK2 recognizes polyUb chains; linkage-specific for topology |
Therapeutic Implications and Future Perspectives
The strategic targeting of E3 ligases and DUBs regulating CSC pathways represents a promising approach for cancer therapy. Several strategies have emerged:
Proteolysis-Targeting Chimeras (PROTACs): These bifunctional molecules recruit target proteins to E3 ligases for ubiquitination and degradation. ARV-110 and ARV-471 represent advanced PROTACs in clinical trials for cancer therapy [3].
DUB Inhibitors: Selective inhibition of oncogenic DUBs such as USP22 presents a viable strategy for eliminating CSCs [31]. Computational drug repurposing approaches have identified Ergotamine as a potential USP22 inhibitor with anticancer properties [31].
Combination Therapies: Targeting ubiquitination regulators in combination with conventional chemotherapy, immunotherapy, or pathway-specific inhibitors may overcome therapy resistance mediated by CSCs [9] [3].
The continued elucidation of E3 ligase and DUB functions in CSC regulation will provide novel insights into tumor biology and enable the development of more effective therapeutic strategies against treatment-resistant cancers.
The ubiquitin system, a crucial post-translational modification platform, governs cancer stem cell (CSC) maintenance through specialized chain topologies. K48-linked ubiquitination primarily targets key regulatory proteins for proteasomal degradation, K63-linked chains coordinate non-proteolytic signaling processes driving stemness, and monoubiquitination regulates protein trafficking and chromatin dynamics. This whitepaper examines how these distinct ubiquitin codes integrate to control CSC fate, therapy resistance, and metastatic potential. We present quantitative analyses of linkage-specific functions, detailed experimental methodologies for topology interrogation, and visualization of ubiquitin signaling networks in CSCs, providing a technical framework for targeting ubiquitin signaling in cancer stem cell populations.
Cancer stem cells (CSCs) represent a subpopulation of tumor cells with capabilities for self-renewal, differentiation, and driving tumor initiation, progression, and therapy resistance [27] [32]. The functional properties of CSCs are regulated by post-translational modifications, with ubiquitination emerging as a master regulator of stemness pathways. Ubiquitin topology—the spatial arrangement of ubiquitin monomers and polymers on substrate proteins—encodes specific biological outcomes that determine CSC fate decisions [33] [27].
The ubiquitin system comprises E1 activating enzymes, E2 conjugating enzymes, and E3 ligases that work in concert to attach ubiquitin to substrate proteins, with approximately 600 E3 ligases providing substrate specificity in humans [34] [35]. Deubiquitinating enzymes (DUBs) reverse this process, creating a dynamic regulatory system. The seven lysine residues in ubiquitin (K6, K11, K27, K29, K33, K48, K63) and the N-terminal methionine (M1) serve as linkage sites for polyubiquitin chain formation, each generating distinct structural signatures recognized by specific effector proteins [34] [27].
Table 1: Major Ubiquitin Chain Types and Their General Functions in Cellular Regulation
| Chain Type | Primary Functions | Key Effectors/Receptors |
|---|---|---|
| K48-linked | Proteasomal degradation | Proteasome, RAD23B [36] |
| K63-linked | Kinase activation, DNA repair, endocytosis, signaling complexes | EPN2, TAB2/3, CYLD [36] [34] |
| Monoubiquitination | Endocytosis, protein trafficking, histone regulation, chromatin modulation | Tsg101, ESCRT complex [37] [33] |
| K11/K48-branched | Enhanced proteasomal degradation, protein quality control | Bispecific antibodies, proteasome [38] [39] |
| K11-linked | ER-associated degradation, cell cycle regulation | Proteasome, CCDC50 [36] [27] |
| K27/K29-linked | DNA damage response, stress signaling | RNF168 [33] [27] |
Within CSC populations, the balance between different ubiquitin chain types regulates key stemness pathways including Wnt, Notch, Hedgehog, and TGF-β signaling [27]. Understanding the functional consequences of specific ubiquitin topologies provides critical insights into CSC maintenance and reveals potential therapeutic vulnerabilities for eradicating this therapy-resistant cell population.
Functional Specialization of Ubiquitin Chain Types
K48-Linked Ubiquitination: Proteostatic Control of Stemness Factors
K48-linked polyubiquitin chains represent the canonical degradation signal, targeting proteins for proteasomal destruction. In CSCs, K48-linked ubiquitination regulates the stability of transcription factors, cell cycle regulators, and metabolic enzymes that control stem cell identity and proliferation [33] [27].
The context-dependent function of K48 chains in CSC regulation is exemplified by FBXW7, an E3 ligase that displays dual roles in radiation response. In p53-wild type colorectal tumors, FBXW7 promotes radioresistance by degrading p53 and inhibiting apoptosis. Conversely, in non-small cell lung cancer (NSCLC) with SOX9 overexpression, FBXW7 enhances radiosensitivity by destabilizing SOX9 and alleviating p21 repression [33]. This functional switch underscores how tissue-specific genetic backgrounds influence ubiquitin signaling outcomes in CSC populations.
K48-linked ubiquitination also intersects with CSC metabolism through SMURF2-mediated HIF1α degradation, which compromises hypoxic survival, and SOCS2/Elongin B/C-driven SLC7A11 destruction, which increases ferroptosis sensitivity in liver cancer [33]. Additionally, TRIM21 utilizes K48 ubiquitination to degrade VDAC2 in nasopharyngeal carcinoma, suppressing cGAS/STING-mediated immune surveillance and potentially enabling CSC immune evasion [33].
Table 2: K48-Linked Ubiquitination in CSC-Regulatory Proteins
| E3 Ligase | CSC Substrate | Functional Consequence | Cancer Context |
|---|---|---|---|
| FBXW7 | p53 | Promotes radioresistance | Colorectal cancer [33] |
| FBXW7 | SOX9 | Enhances radiosensitivity | Non-small cell lung cancer [33] |
| SMURF2 | HIF1α | Compromises hypoxic survival | Multiple cancer types [33] |
| SOCS2/Elongin B/C | SLC7A11 | Increases ferroptosis sensitivity | Liver cancer [33] |
| TRIM21 | VDAC2 | Suppresses cGAS/STING immunity | Nasopharyngeal carcinoma [33] |
K63-Linked Ubiquitination: Signaling Amplification in Stemness Pathways
K63-linked ubiquitin chains serve as non-proteolytic signaling scaffolds that activate kinase pathways and assemble macromolecular complexes essential for CSC maintenance. Unlike K48 linkages, K63 chains function in NF-κB activation, protein trafficking, DNA repair, and kinase activation—processes frequently hijacked in CSCs to promote survival and self-renewal [34] [35].
In CSCs, K63 ubiquitination directly regulates prosurvival signaling cascades. TRAF4 utilizes K63 modifications to activate the JNK/c-Jun pathway, driving overexpression of anti-apoptotic Bcl-xL in colorectal cancer and MCL-1 in oral cancers [33]. K63 chains can also repurpose tumor suppressors; TRAF6 modifies p53 with K63 linkages, converting it into a pro-survival mitochondrial factor that may enhance CSC resistance to apoptosis [33]. Furthermore, K63 ubiquitination integrates metabolic and immune regulation in CSCs: TRIM26 stabilizes GPX4 via K63 ubiquitination to prevent ferroptosis in gliomas, while USP14 inhibition leads to accumulation of K63-modified IRF3, triggering STING-dependent antitumor immunity [33].
The E3 ligase TRAF6 exemplifies the specialized role of K63-specific enzymes in CSC signaling. As one of only two known E3s that selectively target substrates for K63-linked ubiquitination (along with RNF168), TRAF6 activates AKT through K63-linked ubiquitination, promoting CSC survival and expansion across multiple cancer types [34]. This signaling function depends on the unique structural properties of K63 chains, which create extended interfaces for protein-protein interactions without triggering proteasomal degradation.
Figure 1: K63-Linked Ubiquitin Chains Coordinate Multiple Pro-Survival Pathways in CSCs. K63 linkages serve as molecular scaffolds for complex assembly in kinase activation, DNA damage response, and metabolic regulation—processes essential for CSC maintenance.
Monoubiquitination: Trafficking and Epigenetic Control in CSCs
Monoubiquitination—the attachment of a single ubiquitin molecule to substrate proteins—regulates protein trafficking, endocytosis, and epigenetic programming in CSCs. Unlike polyubiquitin chains, monoubiquitination typically alters protein interaction landscapes and subcellular localization without triggering degradation [38] [27].
A paradigm for monoubiquitination in CSC regulation is CD133 (PROM1), a well-established CSC marker in multiple malignancies. CD133 undergoes monoubiquitination at lysine 848 within its intracellular carboxyl terminus, which facilitates its interaction with tumor susceptibility gene 101 (Tsg101) and subsequent incorporation into extracellular vesicles [37]. This monoubiquitination-dependent vesicle secretion promotes cell migration and potentially establishes metastatic niches for CSCs. Knockdown of the E3 ubiquitin protein ligase Nedd4 significantly impairs CD133 ubiquitination and vesicle secretion, confirming the importance of this modification for CSC trafficking and communication [37].
Monoubiquitination also regulates chromatin dynamics and DNA damage responses in CSCs through histone modifications. UBE2T/RNF8-mediated H2AX monoubiquitylation accelerates DNA damage detection in hepatocellular carcinoma, while RNF40-generated H2Bub1 recruits the FACT complex (SUPT16H) to relax nucleosomes [33]. For non-histone targets, FANCD2 monoubiquitylation resolves carbon ion-induced DNA crosslinks, and γ-tubulin monoubiquitylation maintains centrosome integrity—processes that may be co-opted by CSCs to maintain genomic stability despite heightened replication stress [33].
Branched Ubiquitin Chains: Complex Topologies in CSC Regulation
Branched ubiquitin chains, containing ubiquitin molecules modified on two or more residues simultaneously, represent an emerging layer of complexity in ubiquitin coding. These heterotypic polymers integrate signals from different linkage types and can encode qualitative and quantitative information beyond homotypic chains [38] [40] [39].
K11/K48-branched chains exemplify the specialized functions of branched topologies in CSC-relevant processes. These heterotypic polymers are synthesized by coordinated actions of E2 enzymes and E3 ligases, such as the anaphase-promoting complex (APC/C) working with UBE2C and UBE2S during mitosis [38] [39]. K11/K48-branched chains promote rapid proteasomal degradation of aggregation-prone proteins and mitotic regulators, serving as potent degradation signals that may be critical for maintaining proteostasis in rapidly dividing CSCs [38]. Endogenous substrates of K11/K48-branched chains include misfolded nascent polypeptides and pathological Huntingtin variants, suggesting a role in protein quality control pathways relevant to CSC stress adaptation [38].
K48/K63-branched chains represent another functionally significant heterotypic topology that integrates degradative and non-degradative signaling. These branched chains are produced by collaboration between E3s with distinct specificities, such as TRAF6 and HUWE1 during NF-κB signaling, or ITCH and UBR5 during apoptotic responses [39]. In the case of the pro-apoptotic regulator TXNIP, ITCH first modifies the substrate with non-proteolytic K63-linked chains before UBR5 attaches K48 linkages to produce branched K48/K63 chains, resulting in proteasomal degradation [39]. This conversion from non-degradative to degradative signaling may provide a regulatory switch for controlling protein stability in response to CSC microenvironmental cues.
Experimental Approaches for Ubiquitin Topology Analysis
Bispecific Antibody Technology for Heterotypic Chain Detection
The development of linkage-specific antibodies has revolutionized ubiquitin chain analysis. For branched chain detection, bispecific antibodies that recognize two different linkage types simultaneously provide unprecedented specificity. The K11/K48-bispecific antibody was engineered using knobs-into-holes heterodimerization technology, pairing one arm that recognizes K11-linkages with another that binds K48-linkages [38].
This bispecific antibody functions as a coincidence detector, gaining avidity from simultaneous recognition of K11 and K48 linkages. Surface plasmon resonance (SPR) analyses demonstrated ~500–1,000-fold higher affinity for K11/K48-branched ubiquitin trimers compared to control antibodies [38]. The antibody efficiently recognizes K11/K48-branched trimers but fails to detect monomeric or dimeric ubiquitin, including homotypic K11- or K48-linked di-ubiquitin species, confirming its specificity for branched topology [38].
Table 3: Key Research Reagents for Ubiquitin Chain Topology Studies
| Research Tool | Specificity/Function | Experimental Applications |
|---|---|---|
| K11/K48-bispecific antibody | Recognizes K11 and K48 linkages simultaneously | Detection of endogenous K11/K48-branched chains by Western blot, immunoprecipitation [38] |
| Linkage-specific DUBs | Cleave specific ubiquitin linkage types (e.g., OTUB1 for K48, AMSH for K63) | Ubiquitin chain linkage verification (UbiCRest assay) [36] |
| Ubiquitin variant mutants | Lysine-to-arginine mutations prevent specific chain formation | Determining chain linkage requirements in functional assays [38] |
| Tandem Ubiquitin Binding Entities (TUBEs) | Multi-domain ubiquitin-associated domains with avidity for polyubiquitin | Protection of ubiquitin chains from DUBs during purification, enrichment of polyubiquitinated proteins [36] |
| Di-Gly antibody | Recognests diglycine remnant left after tryptic digestion of ubiquitin | Mass spectrometry identification of ubiquitination sites [36] |
Ubiquitin Interactor Pull-Down and Mass Spectrometry
Ubiquitin interactor pulldown coupled with mass spectrometry enables system-level mapping of ubiquitin chain interactions. This approach uses immobilized ubiquitin chains of defined topologies as bait to enrich linkage-specific binding proteins from cell lysates, followed by identification via liquid chromatography-mass spectrometry (LC-MS) [36].
Recent applications of this methodology have revealed novel heterotypic branch-specific ubiquitin interactors, including histone ADP-ribosyltransferase PARP10/ARTD10, E3 ligase UBR4, and huntingtin-interacting protein HIP1 [36]. The screen also identified interactors with chain length preference, such as Ub-directed endoprotease DDI2, autophagy receptor CCDC50, and p97 adaptor FAF1, which show preference for Ub3 over Ub2 chains [36]. This methodology has proven particularly valuable for characterizing the K48/K63-branched ubiquitin interactome, revealing branch-specific readers that potentially decode this complex topology in CSC signaling pathways.
Figure 2: Experimental Workflow for Ubiquitin Interactor Pull-Down Screens. This methodology enables identification of linkage-specific, chain length-dependent, and branch-selective ubiquitin-binding proteins from complex biological samples.
Methodological Considerations and Controls
Accurate interpretation of ubiquitin topology experiments requires careful methodological controls. Deubiquitinating enzyme (DUB) inhibition is critical during ubiquitin interactor pulldowns to prevent chain disassembly. Commonly used cysteine alkylators include chloroacetamide (CAA) and N-ethylmaleimide (NEM), each with distinct advantages and limitations [36].
NEM provides more complete DUB inhibition but has potential off-target effects due to alkylation of non-DUB cysteines and frequent side reactions with N-termini and lysine side chains. CAA is more cysteine-specific but allows partial chain disassembly during experiments [36]. Comparative studies using both inhibitors are recommended to distinguish true ubiquitin interactors from inhibitor-dependent artifacts.
Linkage verification of synthesized ubiquitin chains is essential and typically performed using the UbiCRest method, which employs linkage-specific DUBs like OTUB1 (K48-specific) and AMSH (K63-specific) to selectively disassemble chains of defined topology [36]. For branched chains, sequential digestion with multiple DUBs can confirm the presence of different linkage types within the same polymer.
Therapeutic Targeting of Ubiquitin Signaling in CSCs
The ubiquitin system presents attractive therapeutic vulnerabilities for CSC-directed therapies. Several targeting strategies have emerged, including small molecule inhibitors of E3 ligases, DUB inhibitors, and proteolysis-targeting chimeras (PROTACs) that redirect endogenous ubiquitin machinery toward specific CSC drivers [33].
PROTAC platforms represent a particularly promising approach for targeting CSCs. These bifunctional molecules simultaneously bind to E3 ubiquitin ligases and target proteins of interest, inducing target ubiquitination and degradation. EGFR-directed PROTACs selectively degrade β-TrCP substrates in EGFR-dependent tumors (e.g., lung and head/neck squamous cell carcinomas), suppressing DNA repair while minimizing impact on normal tissues [33]. Radiation-responsive PROTAC platforms are also emerging, including radiotherapy-triggered PROTAC (RT-PROTAC) prodrugs activated by tumor-localized X-rays to degrade BRD4/2, synergizing with radiotherapy in breast cancer models [33].
DUB inhibition provides another strategic approach for targeting CSC populations. USP14 inhibition stabilizes K63-ubiquitinated IRF3, triggering STING-dependent type I interferon responses and potentially overcoming CSC-mediated immune evasion [33]. However, therapeutic targeting requires consideration of contextual duality, as USP14 stabilizes ALKBH5 to maintain glioblastoma stemness but degrades IκBα to activate NF-κB in head/neck cancers [33]. Such opposing functions highlight the critical need for precision therapies that selectively disrupt detrimental ubiquitination events while preserving protective pathways in CSCs.
The topology of ubiquitin chains constitutes a sophisticated regulatory code that controls CSC maintenance through degradation, signaling, and trafficking mechanisms. K48-linked ubiquitination directs proteasomal degradation of stemness regulators, K63-linked chains coordinate pro-survival signaling networks, and monoubiquitination regulates protein localization and epigenetic states. Branched ubiquitin chains integrate these signals, creating complex topological signatures that potentially amplify degradation signals or coordinate multiprotein complex assembly in CSCs.
Technological advances in bispecific antibodies, ubiquitin interactor screens, and mass spectrometry are decoding this ubiquitin landscape with increasing resolution. These tools reveal the remarkable specificity of ubiquitin topology in controlling CSC functions and identify novel therapeutic entry points for targeting this treatment-resistant population. As our understanding of ubiquitin coding in CSCs deepens, topology-specific interventions may provide novel paradigms for combinatorial therapies that simultaneously target multiple ubiquitin-dependent processes in cancer stem cells.
From Bench to Bedside: Therapeutic Strategies Targeting the UPS in CSCs
Cancer stem cells (CSCs) represent a formidable challenge in oncology, driving tumor initiation, metastasis, and therapeutic resistance. The ubiquitin-proteasome system (UPS) has emerged as a critical regulator of CSC maintenance and survival, making it a promising therapeutic target. This whitepaper provides a comprehensive evaluation of two prominent proteasome inhibitors—bortezomib and carfilzomib—in the context of CSC targeting. We examine their distinct mechanisms of action, differential effects on CSC populations, and efficacy in preclinical models. The analysis integrates current understanding of UPS dysregulation in CSCs, detailed experimental methodologies for investigating proteasome inhibitor effects, and visualization of key signaling pathways. Our synthesis reveals that while both agents demonstrate anti-CSC activity, their efficacy is context-dependent and influenced by factors such as drug-specific resistance mechanisms and differential effects on CSC subpopulations. This resource aims to equip researchers and drug development professionals with the technical foundation necessary to advance next-generation strategies targeting the UPS in CSCs.
The ubiquitin-proteasome system (UPS) serves as the primary pathway for controlled intracellular protein degradation in eukaryotic cells, regulating approximately 80-90% of cellular proteins [41] [42]. This sophisticated system involves a cascade of enzymes (E1 activating, E2 conjugating, and E3 ligase enzymes) that tag target proteins with ubiquitin chains, marking them for recognition and degradation by the 26S proteasome [41]. The 26S proteasome consists of a 20S core particle containing proteolytic active sites (β1 caspase-like, β2 trypsin-like, and β5 chymotrypsin-like activities) and 19S regulatory particles that govern substrate recognition, deubiquitination, and translocation [42]. The UPS maintains precise control over fundamental cellular processes including cell cycle progression, apoptosis, DNA repair, and stress response through regulated protein turnover [41].
Cancer stem cells (CSCs), also termed cancer-initiating cells, constitute a minor subpopulation within tumors that possess self-renewal capacity, differentiation potential, and enhanced resistance to conventional therapies [43]. CSCs act as hidden reservoirs that drive tumor recurrence and metastasis following initially successful treatments. Recent evidence establishes that the UPS plays an essential role in maintaining the CSC phenotype through regulation of key stemness transcription factors, cell cycle regulators, and apoptotic proteins [43]. UPS dysregulation in CSCs can lead to aberrant stabilization of oncoproteins or accelerated degradation of tumor suppressors, creating a cellular environment conducive to tumor maintenance and progression.
Targeting the UPS with proteasome inhibitors has emerged as a promising strategy to disrupt CSC survival mechanisms. By interfering with proteasomal degradation, these agents cause accumulation of polyubiquitinated proteins, induction of proteotoxic stress, and disruption of multiple signaling pathways critical for CSC maintenance [43]. This whitepaper focuses on two clinically relevant proteasome inhibitors—bortezomib and carfilzomib—evaluating their potential as anti-CSC therapeutics within the broader context of ubiquitination pathways in cancer stem cell biology.
Molecular Mechanisms of Proteasome Inhibitors
Bortezomib: Mechanism of Action
Bortezomib is a first-generation proteasome inhibitor that reversibly binds to the chymotrypsin-like site of the 26S proteasome's β5 subunit [42] [44]. Its mechanism of action involves multiple interconnected pathways that collectively induce anti-cancer effects:
Cell Cycle Disruption: Bortezomib stabilizes cyclin-dependent kinase inhibitors (p21, p27) and tumor suppressor p53, leading to cell cycle arrest in the G0/G1 phase [45] [44]. This is accompanied by suppressed expression of CDK4 and CDK6, crucial regulators of G1 to S phase progression [45].
Apoptosis Induction: Treatment stabilizes pro-apoptotic proteins (Bid, Bax) while increasing the Bax to Bcl-2 ratio, promoting mitochondrial outer membrane permeabilization (MOMP) and cytochrome C release [45] [46]. This activates the intrinsic apoptotic pathway through caspase-9 and caspase-3 activation, with PARP cleavage serving as a hallmark of execution-phase apoptosis [45].
SKP2/p53 Axis Regulation: In non-melanoma skin cancer models, bortezomib downregulates SKP2 (an oncogenic ubiquitin ligase) while upregulating p53 expression, resulting in impaired cellular growth and caspase-dependent cell death [45]. SKP2 silencing experiments confirmed p53 as a direct target of this pathway.
Reactive Oxygen Species (ROS) Generation: Bortezomib generates significant ROS, and blocking ROS production substantially reduces apoptotic cell death, indicating ROS-mediated toxicity contributes to its mechanism [45].
Immunomodulatory Effects: Bortezomib upregulates stress ligands MICA/B and death receptors (DR5, Fas) on tumor cells, enhancing natural killer (NK) cell-mediated killing, particularly against aldehyde dehydrogenase (ALDH)-positive CSCs [47].
NF-κB Pathway Inhibition: By preventing IκB degradation, bortezomib inhibits nuclear factor kappa-B (NF-κB) activation, thereby suppressing expression of anti-apoptotic and pro-survival genes [44].
Carfilzomib: Mechanism of Action
Carfilzomib represents a second-generation proteasome inhibitor with distinct biochemical properties and mechanisms:
Irreversible Binding: Unlike bortezomib's reversible inhibition, carfilzomib forms irreversible covalent bonds with the β5 subunit, resulting in sustained proteasome inhibition even after drug clearance [42] [48].
Selectivity Profile: At lower concentrations, carfilzomib primarily inhibits the β5 subunit, but at higher doses it also substantially inhibits the β2 trypsin-like activity, which may contribute to both enhanced efficacy and distinct toxicity profiles [48].
Apoptosis Pathways: Carfilzomib induces concentration-dependent apoptosis through multiple mechanisms, including increased expression of cleaved caspase-3, caspase-9, and Bax, while decreasing Bcl-2 levels [49]. This shifts the balance toward pro-apoptotic signaling.
STAT1/COX-2/iNOS Pathway Inhibition: In multiple myeloma models, carfilzomib suppresses the STAT1 signaling pathway, subsequently downregulating COX-2 and iNOS expression, which correlates with both proliferation inhibition and apoptosis induction [49].
Unfolded Protein Response (UPR) Activation: Like bortezomib, carfilzomib induces ER stress through accumulation of unfolded proteins, triggering the UPR and ultimately apoptosis when proteotoxic stress exceeds compensatory capacity [42].
Table 1: Comparative Molecular Mechanisms of Bortezomib and Carfilzomib
| Mechanistic Aspect | Bortezomib | Carfilzomib |
|---|---|---|
| Binding Mechanism | Reversible | Irreversible |
| Primary Target | β5 subunit (chymotrypsin-like) | β5 subunit (chymotrypsin-like) |
| Secondary Targets | Limited β1 activity at higher concentrations | β2 subunit (trypsin-like) at higher concentrations |
| Effect on Apoptotic Proteins | Increases Bax/Bcl-2 ratio; stabilizes p53 | Increases cleaved caspases-3, -9; modulates Bax/Bcl-2 ratio |
| Effect on Cell Cycle | G0/G1 arrest via p21/p27 stabilization | G2/M arrest observed in some models |
| Unique Pathway Effects | SKP2/p53 axis regulation; NK cell activation via MICA/B upregulation | STAT1/COX-2/iNOS pathway inhibition |
| ROS Generation | Significant contributor to cytotoxicity | Less pronounced |
Experimental Models and Methodologies
In Vitro Assessment of Anti-CSC Effects
Research into proteasome inhibitor effects on CSCs employs specialized methodologies to evaluate stem cell populations and their functional properties:
CSC Enrichment and Identification:
- ALDH Activity Assay: ALDHbright cells are identified using the ALDEFLUOR kit, which measures intracellular aldehyde dehydrogenase activity [47]. Cells are incubated with BODIPY-aminoacetaldehyde substrate, and the brightly fluorescent population representing CSCs is isolated via fluorescence-activated cell sorting (FACS).
- Sphere Formation Assay: To evaluate self-renewal capacity, single cells are plated in ultra-low attachment plates with serum-free media supplemented with growth factors (EGF, bFGF) [47]. Sphere number and size are quantified after 7-14 days following bortezomib or carfilzomib treatment.
Viability and Apoptosis assays:
- CCK-8/MTT Assays: Cells are treated with varying concentrations of proteasome inhibitors (typically 1-100 nM) for 24-72 hours [45] [49]. IC50 values are calculated from dose-response curves.
- Annexin V/PI Dual Staining: Following drug treatment, cells are stained with Annexin V-FITC and propidium iodide, then analyzed by flow cytometry to distinguish early apoptotic (Annexin V+/PI-), late apoptotic (Annexin V+/PI+), and necrotic (Annexin V-/PI+) populations [45].
- Caspase Activity Assays: Cleaved caspase-3, caspase-9, and PARP are detected via western blotting or flow cytometry using specific antibodies [45] [49]. Pan-caspase inhibitors like z-VAD-FMK are used to confirm caspase-dependent apoptosis.
Mechanistic Studies:
- Western Blot Analysis: Protein extracts from treated cells are subjected to SDS-PAGE, transferred to PVDF membranes, and probed with antibodies against targets of interest (SKP2, p53, Bcl-2 family proteins, STAT1, COX-2, iNOS) [45] [49].
- RNA Interference: siRNA-mediated knockdown of specific targets (e.g., SKP2) confirms their role in mediating drug effects [45].
- ROS Detection: Intracellular ROS levels are measured using fluorescent probes like DCFH-DA following drug treatment with or without ROS scavengers such as N-acetylcysteine [45].
In Vivo Models
Mouse Xenograft Models:
- CSC-Enriched Tumors: ALDHbright cells or primary tumor cells are implanted orthotopically or subcutaneously into immunodeficient mice (e.g., NSG mice) [47].
- Drug Administration: Bortezomib (0.5-1.5 mg/kg) or carfilzomib (2-8 mg/kg) are administered intravenously on varying schedules [47] [48].
- Endpoint Analyses: Tumor growth is monitored regularly. At study endpoint, tumors are excised for analysis of CSC markers (ALDH, CD133), proliferation (Ki-67), and apoptosis (TUNEL staining) [47].
C. elegans Model:
- Germline Apoptosis Assay: Bortezomib-induced apoptosis is quantified in C. elegans germlines using acridine orange staining or GFP-tagged CED-1 [45].
- Genetic Analysis: CEP-1 (p53 ortholog) mutant strains confirm conservation of p53-mediated apoptosis mechanisms [45].
Table 2: Experimental Details for Key Proteasome Inhibitor Studies
| Experimental Aspect | Bortezomib Studies | Carfilzomib Studies |
|---|---|---|
| Typical Concentration Range (in vitro) | 10-50 nM (IC50: 8.69-37.3 nM in NMSC cells) [45] | 1-25 nM (concentration-dependent effects in MM cells) [49] |
| Treatment Duration | 24-72 hours | 48 hours standard |
| Primary Cell Models | A431, A388 (NMSC); U87 (glioblastoma); SW982 (sarcoma); PANC-1 (pancreatic) [45] [47] | RPMI-8226, MOLP-8, NCI-H929, OPM-2 (multiple myeloma) [49] |
| CSC Identification Method | ALDEFLUOR assay; sphere formation [47] | Side population analysis; colony formation |
| In Vivo Dosing | 0.5-1.5 mg/kg IV [47] | 2-8 mg/kg IV [48] |
| Key Readout Assays • Viability (CCK-8) • Apoptosis (Annexin V/PI, caspase cleavage) • CSC frequency (ALDH, sphere formation) • Protein changes (western blot) | • Viability (MTT) • Apoptosis (TUNEL, caspase/bax/bcl-2 western) • Proliferation (BrdU) • Pathway analysis (STAT1/COX-2/iNOS) |
Signaling Pathways in Proteasome Inhibition
The following diagram illustrates key signaling pathways affected by proteasome inhibitors in cancer stem cells:
Diagram 1: Signaling pathways of proteasome inhibitors in CSCs. Proteasome inhibition affects multiple pathways converging on cell cycle arrest and apoptosis, with specific effects on CSC populations.
Research Reagent Solutions
Table 3: Essential Research Reagents for Studying Proteasome Inhibitors in CSCs
| Reagent/Category | Specific Examples | Research Application |
|---|---|---|
| Proteasome Inhibitors | Bortezomib, Carfilzomib | Primary investigational compounds for targeting UPS in CSCs |
| CSC Identification | ALDEFLUOR Kit, Anti-CD44, Anti-CD133, Anti-CD34 | Identification and isolation of CSC populations via FACS |
| Apoptosis Detection | Annexin V/Propidium Iodide, TUNEL Assay, Caspase Activity Assays | Quantification of programmed cell death |
| Cell Viability/Proliferation Assays | CCK-8, MTT, BrdU Incorporation Assay | Assessment of cytotoxic and anti-proliferative effects |
| Protein Analysis | Antibodies against: p53, SKP2, Bcl-2 family, STAT1, COX-2, iNOS, Cleaved Caspases, PARP | Western blot analysis of molecular mechanisms |
| Pathway Modulators | z-VAD-FMK (pan-caspase inhibitor), N-acetylcysteine (ROS scavenger) | Mechanistic studies to confirm specific pathways |
| In Vivo Models | Immunodeficient mice (NSG, NOD/SCID), Patient-derived xenografts | Preclinical evaluation of anti-CSC efficacy |
| Specialized Cell Culture | Ultra-low attachment plates, Serum-free media with EGF/bFGF | Sphere formation assays for CSC functional analysis |
Comparative Efficacy Against Cancer Stem Cells
Differential Effects on CSC Subpopulations
Research demonstrates that proteasome inhibitors exhibit variable effects on CSC populations depending on cancer type and specific agent:
Bortezomib-CSC Interactions:
- Differential Sensitivity: In glioblastoma (U87), synovial sarcoma (SW982), and pancreatic adenocarcinoma (PANC-1) models, ALDHbright CSCs demonstrate relative resistance to bortezomib's cytotoxic effects compared to ALDHdim cells [47]. This results in enrichment of ALDHbright cells following treatment with lower concentrations (10-20 nM).
- Immunomodulatory Sensitization: Despite initial resistance, bortezomib pre-treatment significantly sensitizes CSCs to NK cell-mediated killing through upregulation of stress ligands MICA/B and death receptor DR5 on both ALDHbright and ALDHdim populations [47].
- In Vivo Efficacy: Combination therapy with bortezomib and allogeneic NK cell adoptive transfer in immunodeficient mice enhances CSC elimination and delays tumor growth in orthotopic glioblastoma models [47].
Carfilzomib-CSC Interactions:
- Limited Direct Data: While specific studies examining carfilzomib's effects on defined CSC populations are more limited, its potent and irreversible proteasome inhibition suggests potential efficacy against CSCs dependent on UPS function.
- Overcoming Resistance: Evidence suggests carfilzomib may overcome bortezomib resistance in multiple myeloma, potentially including CSC subpopulations [42] [43].
- Toxicity Considerations: Carfilzomib-specific cardiotoxicity at higher doses (mediated through β2 inhibition and disruption of retinol metabolism) may limit dosing strategies required to target resistant CSC populations [48].
Resistance Mechanisms
CSCs employ multiple resistance mechanisms against proteasome inhibitors:
- Proteasomal Mutations: Mutations in catalytic β-subunits can reduce inhibitor binding affinity [43].
- Enhanced Proteasome Expression: Increased proteasome subunit production compensates for inhibited complexes [43].
- Autophagy Activation: CSCs upregulate autophagy as an alternative protein clearance pathway when proteasome function is impaired [45] [43].
- Efflux Transporters: Elevated ABC transporter activity in CSCs may enhance drug efflux [43].
- Anti-oxidant Defense Systems: Enhanced ROS detoxification capabilities protect against proteasome inhibitor-induced oxidative stress [45].
Proteasome inhibitors represent a promising therapeutic strategy for targeting CSCs through disruption of the ubiquitin-proteasome system. Bortezomib and carfilzomib exhibit distinct mechanistic profiles—with reversible versus irreversible binding, differential effects on proteasome subunits, and unique pathway interactions—that influence their efficacy against CSC populations. Current evidence suggests that while CSCs may demonstrate initial resistance to single-agent proteasome inhibition, combination approaches that leverage immunomodulatory effects or target complementary pathways show enhanced anti-CSC activity.
Future research directions should focus on several critical areas: First, elucidating UPS dysregulation patterns specific to CSCs across different tumor types may identify predictive biomarkers for proteasome inhibitor sensitivity. Second, developing optimized combination strategies that simultaneously target UPS and compensatory pathways (such as autophagy) may prevent resistance development. Third, addressing the cardiotoxicity limitations of carfilzomib through dose optimization or cardioprotective approaches could enhance its therapeutic window against CSCs. Finally, advancing UPS-targeting technologies beyond conventional proteasome inhibitors—including specific E3 ligase modulators and PROTACs—holds significant promise for precision targeting of CSC maintenance mechanisms.
The continued investigation of proteasome inhibitors in CSC biology, employing the sophisticated methodologies and reagents outlined in this whitepaper, will be essential for developing more effective therapeutic strategies capable of eliminating this critical population of treatment-resistant cells.
Cancer stem cells (CSCs) represent a subpopulation within tumors characterized by infinite reproductive capacity, continuous self-renewal, and multi-directional differentiation potential [5]. These cells are major contributors to tumor initiation, metastasis, and therapy resistance in cancer [25]. The "stem" state of CSCs is maintained through intricate regulatory networks, with ubiquitination emerging as a crucial post-translational modification governing CSC functionality [5] [9]. Ubiquitination, a process mediated by a cascade of E1, E2, and E3 enzymes, controls the stability, activity, and localization of proteins central to stemness pathways [25]. Dysregulation of the ubiquitin system drives tumorigenesis and metastasis by altering the delicate balance of CSC regulatory factors [5] [9]. This technical guide explores the strategic application of targeted protein degradation technologies, specifically PROTACs and Molecular Glues, to dismantle the ubiquitin-dependent maintenance mechanisms of CSCs.
Biological Rationale: Targeting the Ubiquitin System in CSCs
Key CSC Factors Regulated by Ubiquitination
The core transcription factors and signaling pathways that maintain CSC pluripotency and self-renewal are heavily influenced by ubiquitin-mediated regulation. Understanding these relationships provides the foundation for rational degrader design.
Table 1: Key CSC Factors and Their Regulation by Ubiquitination
| CSC Factor/Pathway | Role in CSC Maintenance | Ubiquitination Regulation |
|---|---|---|
| Transcription Factors | ||
| OCT4 | Maintains self-renewal and pluripotency [5] | Ubiquitination target; affects stemness maintenance [5] [25] |
| SOX2 | Regulates self-renewal and differentiation [5] | Ubiquitination target; affects stemness maintenance [5] [25] |
| NANOG | Critical for pluripotency [5] | Ubiquitination target; affects stemness maintenance [5] [25] |
| c-MYC | Promotes proliferation and survival [9] | Modulated by ubiquitin ligases and DUBs [9] |
| Signaling Pathways | ||
| Wnt/β-catenin | Regulates self-renewal and cell fate [5] [25] | β-catenin stability controlled by E3 ligases [5] |
| Notch | Controls cell fate decisions and proliferation [5] [25] | Pathway components regulated by ubiquitination [9] |
| Hedgehog | Patterns tissue development and stemness [5] [25] | Key components modulated by UPS [9] |
| Hippo-YAP | Regulates organ size and stem cell expansion [5] | Central components influenced by ubiquitination [9] |
The Ubiquitin-Proteasome System in CSC Homeostasis
The ubiquitin-proteasome system (UPS) maintains cellular homeostasis through a precise enzymatic cascade [5] [25]:
- E1 Ubiquitin-Activating Enzymes: Initiate ubiquitination by activating ubiquitin in an ATP-dependent manner (only 2 known in humans) [25]
- E2 Ubiquitin-Conjugating Enzymes: Receive and carry activated ubiquitin (approximately 30 known in humans) [25]
- E3 Ubiquitin Ligases: Confer substrate specificity by recognizing target proteins and facilitating ubiquitin transfer (over 600 known in humans) [25]
- Deubiquitinases (DUBs): Reverse ubiquitination by removing ubiquitin molecules, providing dynamic regulation [5] [25]
In CSCs, this system precisely controls the "quantity" and "quality" of specific proteins that govern self-renewal, maintenance, and differentiation [5] [25]. The overexpression of adenosine triphosphate-binding transporter proteins in CSCs, which actively efflux drugs, can be modulated by targeting ubiquitination components, thereby enhancing CSC sensitivity to chemotherapeutic agents [5].
PROTACs: Rational Design for CSC-Specific Degradation
PROTAC Mechanism and Catalytic Advantage
Proteolysis-Targeting Chimeras (PROTACs) are bifunctional molecules designed to induce targeted protein degradation [50] [51]. Each PROTAC consists of three distinct components:
- POI-binding ligand: A chemical moiety that selectively binds to the target protein intended for degradation
- E3 ligase-recruiting ligand: A moiety that binds to a specific E3 ubiquitin ligase
- Chemical linker: A flexible chain connecting the two ligands, optimizing spatial arrangement [51]
The core mechanism involves the PROTAC simultaneously binding to both the protein of interest (POI) and an E3 ubiquitin ligase, inducing formation of a ternary complex (E3 ligase–PROTAC–POI) [51]. This forced proximity facilitates transfer of ubiquitin molecules from the E3 ligase to the POI. Once poly-ubiquitinated, the POI is recognized and degraded by the 26S proteasome [51]. A key advantage is their catalytic nature – the PROTAC is not consumed in the degradation process, enabling a single molecule to degrade multiple POI copies, providing potent and sustained protein knockdown at low concentrations [51].
Design Considerations for CSC-Targeting PROTACs
Table 2: E3 Ligase Options for PROTAC Design Against CSCs
| E3 Ligase | Native Biological Function | Ligand Examples | Considerations for CSC Targeting |
|---|---|---|---|
| Cereblon (CRBN) | Target of immunomodulatory drugs (IMiDs) [52] | Thalidomide, Lenalidomide, Pomalidomide derivatives [51] [53] | Widely utilized; known to degrade transcription factors like IKZF1/3 [51] |
| Von Hippel-Lindau (VHL) | Regulates HIF-1α under normoxic conditions [52] | VHL ligands based on HIF-1α peptide modifications [52] | Well-characterized ligand binding; used in numerous PROTAC designs |
| MDM2 | Negative regulator of p53 tumor suppressor [52] | Nutlin-3 derivatives [52] | Potential for p53 stabilization in p53 wild-type CSCs [52] |
| IAP (cIAP/XIAP) | Regulates apoptosis and NF-κB signaling [52] | LCL-161, Bestatin, MV1 derivatives [52] | Can induce dual degradation of POI and IAPs themselves [52] |
Linker Optimization: The chemical linker is not merely a connector but critically influences degradation efficiency [51] [53]. Optimization involves empirical testing of:
- Length: Typically 5-25 atoms to enable proper ternary complex formation
- Composition: PEG-based, alkyl chains, or rigid aromatic groups
- Attachment points: Location on both warheads affects molecular geometry and binding
Addressing CSC Challenges: When designing PROTACs against CSC-specific factors:
- Target Transcription Factors: Utilize DNA-binding domain inhibitors or protein-protein interaction disruptors as warheads against OCT4, SOX2, NANOG
- Overcome Quiescence: Leverage catalytic mechanism to degrade targets in slowly-dividing CSCs where occupancy-driven inhibitors fail
- Counteract Resistance: Design PROTACs against mutated or overexpressed targets that confer resistance to conventional therapies [50] [51]
Figure 1: PROTAC Mechanism of Action: The catalytic degradation cycle enables a single PROTAC molecule to mediate multiple degradation events
Experimental Protocol: PROTAC Screening and Validation
Phase 1: Initial Degradation Screening
- Cell Model Selection: Use CSC-enriched populations (e.g., tumorsphere cultures, marker-sorted cells)
- PROTAC Treatment: Apply PROTAC candidates across concentration range (1 nM - 10 µM) for 4-24 hours
- Western Blot Analysis: Assess target protein degradation and confirm specificity
- Viability Assessment: Measure cell viability over 72-96 hours using ATP-based or resazurin assays
Phase 2: Mechanistic Validation
- Ternary Complex Confirmation:
- Co-immunoprecipitation of POI and E3 ligase in PROTAC-treated cells
- Cellular thermal shift assays (CETSA) to confirm stabilization
- Ubiquitin-Dependence Tests:
- Pre-treatment with proteasome inhibitor (MG132, bortezomib) to block degradation
- Pre-treatment with neddylation inhibitor (MLN4924) to disrupt E3 ligase activity
- Selectivity Assessment:
- Global proteomics (e.g., TMT or label-free quantification) to identify off-target degradation
- RNA-seq to monitor transcriptional responses
Phase 3: Functional CSC Assessment
- Tumorsphere Formation: Evaluate primary and secondary sphere formation capacity
- Lineage Tracing: Monitor differentiation potential upon PROTAC treatment
- In Vivo Limiting Dilution: Transplant PROTAC-treated CSCs into immunocompromised mice to assess tumor-initiating capacity reduction
Molecular Glue Degraders: Harnessing Natural Ubiquitin Pathways
Mechanism and Advantages for CSC Targeting
Molecular Glue Degraders (MGDs) are monovalent small molecules that induce or stabilize novel protein-protein interactions between an E3 ubiquitin ligase and a protein of interest, leading to ubiquitination and degradation [51] [54]. Unlike bifunctional PROTACs, MGDs typically bind to one protein (often the E3 ligase), inducing a conformational change that creates a "neosurface" complementary to a specific region on the POI, effectively "gluing" the E3 ligase and POI together [51]. This induced proximity reprograms the E3 ligase's substrate specificity, enabling ubiquitination of the POI [51].
Key advantages for CSC targeting:
- Lower Molecular Weight: Typically <500 Da, improving cellular permeability and pharmacokinetic properties [51]
- Enhanced Blood-Brain Barrier Penetration: Potentially beneficial for targeting CSCs in brain tumors or brain metastases [51]
- Natural Protein-Protein Interactions: Often leverage more natural binding interfaces compared to the forced proximity of PROTACs
Design Strategies for CSC-Focused Molecular Glues
The discovery of molecular glues has historically been serendipitous, but rational approaches are emerging:
Leveraging Known E3 Ligase Binders:
- CRBN-Based Glues: Expand beyond IMiDs (thalidomide, lenalidomide, pomalidomide) to target CSC-specific transcription factors
- Non-CRBN Glues: Develop compounds targeting DCAF15, DCAF16, and other E3 ligases abundant in CSCs
Structure-Based Design:
- Utilize X-ray crystallography and cryo-EM structures of E3 ligases to design small molecules that create neomorphic surfaces
- Employ computational modeling to predict compound-induced protein-protein interfaces
High-Throughput Screening Approaches:
- Ternary Complex Formation Assays: Use FRET or AlphaScreen technologies to identify molecules promoting E3-POI interactions
- Degradation-Based Screens: Monitor endogenous protein levels using high-content imaging or luciferase-tagged endogenous genes
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Research Tools for Developing CSC-Targeted Degraders
| Reagent Category | Specific Examples | Research Application | Key Considerations |
|---|---|---|---|
| E3 Ligase Ligands | Thalidomide analogs, VHL ligands, MDM2 inhibitors (Nutlin-3) [51] [52] [53] | PROTAC assembly and molecular glue optimization | Select based on E3 ligase expression in target CSC population |
| CSC Factor Binders | BET inhibitors (JQ1), kinase inhibitors, protein-protein interaction disruptors | Warheads for PROTAC design against specific CSC factors | Confirm binding to native, non-activated protein conformations |
| Linker Libraries | PEG-based chains, alkyl spacers, rigid aromatic linkers | PROTAC linker optimization | Systematically vary length and composition for ternary complex efficiency |
| Proteomic Tools | TMT/Label-free proteomics, ubiquitin remnant profiling [51] | Global degradation selectivity assessment | Critical for identifying on/off-target degradation in CSCs |
| CSC Functional Assays | Tumorsphere formation, ALDEFLUOR, in vivo limiting dilution | Validate functional impact on CSC populations | Use multiple complementary assays to confirm stemness reduction |
Visualization of Core Signaling Pathways
Figure 2: Ubiquitin System Regulation of CSC Signaling Pathways: The ubiquitin-proteasome system controls core pathways and transcription factors that maintain the CSC state
Emerging Technologies and Future Directions
Advanced PROTAC Modalities
Pro-PROTACs/Photo-PROTACs: Latent PROTACs protected with labile groups (e.g., photocleavable DMNB) enable spatiotemporal control of activation [53]. This allows precise targeting within complex tumor environments and minimizes off-tumor effects.
Dual-Action-Only PROTACs (DAO-PROTACs): Engineered to only function when both warheads are engaged, reducing off-target effects and hook effect [51].
Homo-PROTACs: Utilize two identical E3 ligase ligands to induce dimerization and degradation of the E3 ligase itself, potentially useful for reducing specific E3 ligases overactive in CSCs [52].
Combination Strategies
The future of CSC-targeted degradation lies in rational combinations:
- PROTAC + Chemotherapy: Degrade resistance factors to resensitize CSCs to conventional agents
- PROTAC + Immunotherapy: Eliminate CSC populations that evade immune surveillance
- Multi-Pathway Degradation: Simultaneously target multiple CSC maintenance pathways with complementary degraders
Targeted protein degradation represents a paradigm shift in addressing the challenging biology of cancer stem cells. By harnessing the natural ubiquitin-proteasome system, PROTACs and Molecular Glues offer innovative strategies to eliminate CSC-specific factors that have historically resisted conventional therapeutic approaches. The modular nature of PROTAC design enables systematic targeting of transcription factors and pathway components central to stemness maintenance, while the emerging rational design approaches for Molecular Glues promise increasingly sophisticated degradation tools. As our understanding of ubiquitination in CSC regulation deepens, these technologies hold exceptional promise for overcoming therapy resistance and preventing tumor recurrence—ultimately transforming cancer treatment paradigms.
The ubiquitin-proteasome system (UPS) is a master regulator of protein homeostasis, orchestrating the controlled degradation of key cellular proteins and thereby influencing virtually every cellular process. This system's precise function is critical in cancer stem cells (CSCs), a subpopulation of tumor cells responsible for tumor initiation, metastasis, therapeutic resistance, and relapse [9] [18]. The UPS regulates core stemness pathways—including Wnt/β-catenin, Hedgehog, Notch, and Hippo—and directly controls the stability of pivotal transcription factors such as SOX2, OCT4, KLF4, and c-Myc that maintain the self-renewing, pluripotent state of CSCs [9]. The balance between ubiquitination, catalyzed by E3 ubiquitin ligases, and deubiquitination, mediated by deubiquitinating enzymes (DUBs), therefore represents a crucial regulatory node in CSC maintenance. Disrupting this balance by specifically inhibiting these enzymes offers a promising therapeutic strategy to eradicate the root cause of tumors. This whitepaper provides an in-depth technical guide to the current state of small molecule development for targeting specific E3 ligases and DUBs, framed within the context of CSC research, and outlines the significant challenges that remain.
E3 Ubiquitin Ligases: Mechanisms and Targeted Inhibition
E3 Ligase Biology and Function
E3 ubiquitin ligases are the substrate-recognition components of the ubiquitination cascade, conferring specificity to the process of tagging proteins for proteasomal degradation or functional modification. They operate sequentially with E1 (activating) and E2 (conjugating) enzymes [55]. The human genome encodes over 600 E3s, categorized primarily into three structural families: RING (Really Interesting New Gene), HECT (Homologous to E6AP C-terminus), and RBR (RING-Between-RING) [56] [55]. Recent structural and biochemical studies have revealed new mechanistic classes, such as the RING-Cys-Relay and RZ finger ligases, expanding our understanding of ubiquitin transfer [56]. A critical function of E3s, particularly relevant in oncology, is the regulation of oncoproteins and tumor suppressors; for instance, the E3 ligase MDM2 promotes tumor cell survival by mediating the degradation of p53, while CRL4CRBN targets the degradation of key transcription factors like IKZF1/3 [55].
Key E3 Ligase Targets in Cancer and CSC Pathways
Several E3 ligases have been identified as critical players in cancer pathogenesis and CSC regulation, making them attractive therapeutic targets. The table below summarizes prominent E3 ligase targets, their mechanisms, and roles in cancer, with particular attention to CSC contexts.
Table 1: Key E3 Ubiquitin Ligase Targets in Cancer and CSC Pathways
| E3 Ligase | Family | Key Substrates & Pathways | Role in Cancer & CSC Regulation | Therapeutic Approach/Challenge |
|---|---|---|---|---|
| HUWE1 [57] [55] | HECT | c-Myc, p53, MCL-1 | Regulates proliferation; dual role (oncogenic/tumor suppressive) context-dependent. | Conventional inhibitors can be ubiquitinated themselves, acting as substrates and limiting efficacy [57]. |
| CRL4CRBN [55] | RING | IKZF1, IKZF3 (degraded via IMiDs) | Not a direct CSC regulator, but its modulation by drugs alters transcriptional programs in cancer cells. | Clinically validated by immunomodulatory drugs (lenalidomide, pomalidomide); resistance can occur [55]. |
| MDM2 [55] | RING | p53 (K48-linked degradation) | Promotes cell survival & proliferation by degrading key tumor suppressor p53. | Small-molecule inhibitors (e.g., nutlins) disrupt MDM2-p53 interaction; specificity is key. |
| FBXW7 [55] | RING | p100 (Non-canonical NF-κB) | Acts as a tumor suppressor; regulates cell proliferation and survival. | Loss-of-function mutations are common in cancers; difficult to target therapeutically with inhibitors. |
Experimental Protocol for Profiling E3 Ligase Inhibitors
The discovery and mechanistic characterization of E3 ligase inhibitors require a multi-faceted biochemical and cellular approach. The following protocol, inspired by studies on HUWE1 inhibitors, outlines a standard workflow for profiling compound activity [57].
In Vitro Ubiquitination Assay: Reconstitute the ubiquitination cascade in a purified system.
- Reagents: E1 (UBA1), E2 (UBE2L3 or UBE2D3), purified E3 ligase (e.g., HUWE1HECT), Ubiquitin, ATP, and the test compound.
- Method: Incubate the reaction mixture with a fluorescent Ub tracer. Resolve products via SDS-PAGE and visualize to monitor the inhibition of E3 autoubiquitination, E2~Ub thioester formation, and free poly-Ub chain synthesis. Dose-response curves (e.g., low-μM IC50 for BI8626/BI8622) determine potency [57].
Single-Turnover & Binding Assays: Pinpoint the exact step of inhibition.
- Reagents: Pre-formed E2~Ub thioester or stable E3~Ub proxy (e.g., vinylthioether-linked HUWE1HECT~Ub).
- Method: In single-turnover assays, test if the compound blocks Ub transfer from E2 to E3 (first step) or from E3 to substrate (second step). Use techniques like Differential Scanning Fluorimetry (DSF) or Isothermal Titration Calorimetry (ITC) with the E3~Ub proxy to probe for direct binding, which may be transient or weak [57].
Identification of Compound Ubiquitination: A key counter-screening assay.
- Reagents: Complete ubiquitination reaction mixture, LysC protease.
- Method: After reaction, separate proteins by SDS-PAGE. Excise the ~9 kDa Ub band and analyze via LC-MS/MS after LysC digestion. Identify Ub-derived peptides with a mass shift corresponding to the covalently linked compound (+408.21 Da for BI8622; +422.23 Da for BI8626), confirming the compound is a substrate rather than a pure inhibitor [57].
Cellular Validation:
- Method: Transfer the compound into a relevant cancer cell line. Use methods to detect ubiquitinated compounds and assess downstream effects, such as global proteomics to measure changes in ubiquitination at specific protein sites or stabilization of known E3 substrates (e.g., MCL1) [57].
Deubiquitinating Enzymes (DUBs): Reversing Ubiquitin Signals
DUB Biology and Oncogenic Roles
Deubiquitinating enzymes (DUBs) perform the reverse reaction of E3 ligases, cleaving ubiquitin from substrate proteins to rescue them from degradation or alter their activity. The approximately 100 human DUBs are classified into seven families: USP, UCH, OTU, MJD, JAMM, MINDY, and ZUP [58] [59]. With the exception of the JAMM family, which are zinc-dependent metalloproteases, DUBs are cysteine proteases that rely on a catalytic triad for activity [58]. In cancer and CSCs, DUBs frequently exhibit dysregulated expression and stabilize key oncoproteins. For example, in pancreatic ductal adenocarcinoma (PDAC), USP28 stabilizes FOXM1 to promote cell cycle progression, USP21 stabilizes TCF7 to maintain stemness, and USP5 stabilizes FOXM1 to accelerate tumor growth [60]. Inhibiting these DUBs can lead to the degradation of their oncogenic substrates, providing a compelling therapeutic strategy.
Key DUB Targets in Cancer and CSC Pathways
The development of small-molecule DUB inhibitors has progressed rapidly, with several candidates entering preclinical and clinical studies. The table below highlights key DUB targets and the status of their inhibition.
Table 2: Key Deubiquitinating Enzyme (DUB) Targets and Inhibitors in Cancer
| DUB Target | Family | Key Substrates & Pathways | Role in Cancer & CSC Regulation | Inhibitor (Status) |
|---|---|---|---|---|
| USP1 [61] [58] | USP | DNA damage repair proteins | Stabilizes oncogenic proteins; promotes cancer development. | Small-molecule inhibitors (Preclinical/Clinical) for cancer therapy. |
| USP7 [61] [60] [58] | USP | p53, MDM2 (fine-tunes the pathway) | Context-dependent roles; regulates cell cycle, apoptosis, and is implicated in PDAC. | P22077 (preclinical); multiple inhibitors in development. |
| USP14 [61] [58] [59] | USP | Proteasome-associated | Promotes tumorigenesis and is implicated in osteoarthritis. | IU1 (preclinical tool compound). |
| USP9X [60] [58] | USP | Regulator of Hippo pathway, LATS kinase, YAP/TAZ | Dual role (oncogenic/suppressive) context-dependent; critical in PDAC. | WP1130 (Derivative, preclinical). |
| BAP1 [60] | UCH | - | Frequently mutated in "BAP1 cancer syndrome"; tumor suppressor. | - |
The Scientist's Toolkit: Research Reagent Solutions
To conduct research in this field, scientists rely on a suite of essential reagents and tools. The following table details key components for studying E3 ligases and DUBs.
Table 3: Essential Research Reagents for E3 and DUB Studies
| Reagent / Tool | Function / Application | Example / Note |
|---|---|---|
| Recombinant E1, E2, E3 Enzymes | Reconstitute ubiquitination cascade in in vitro assays. | Purified HUWE1HECT domain, UBE2L3 (E2), UBA1 (E1) [57]. |
| Activity-Based Probes (ABPs) | Label and detect active DUBs in complex proteomes; chemoproteomics. | Ubiquitin-based probes with electrophilic traps for covalent binding to active site cysteine. |
| DNA-Encoded Libraries (DELs) | Screen billions of compounds for ligands against E3 ligases or DUBs. | Core technology in Nurix's DELigase platform for degrader discovery [62]. |
| Stable E3~Ub Proxies | Mechanistic studies of the E3 ubiquitin transfer step. | Vinylthioether-linked HUWE1HECT~Ub for DSF/ITC binding studies [57]. |
| Fluorescent Ubiquitin Tracers | Visualize and quantify ubiquitination activity in real-time. | Used in HTS assays to monitor E3 auto-ubiquitination inhibition [57]. |
| Cell-Based Screening Platforms | Identify degraders and their mechanisms in a physiologically relevant live-cell context. | Plexium's platform evaluates thousands of protein-ligase interactions [62]. |
Technical and Conceptual Challenges in Inhibitor Development
The path to developing clinically viable E3 and DUB inhibitors is fraught with challenges that extend beyond conventional drug discovery.
Specificity and Selectivity: The high structural homology, particularly within DUB families, and the presence of shallow, surface-exposed substrate-binding sites make achieving selectivity extremely difficult. Poor selectivity can lead to off-target toxicity and obscure the interpretation of phenotypic results [58].
Compound-Mediated Ubiquitination: A paradoxical challenge emerged with the discovery that some reported E3 ligase "inhibitors" are, in fact, substrates for their target enzyme. This was demonstrated for HUWE1 inhibitors BI8622 and BI8626, which contain a primary amine that gets ubiquitinated, complicating their mechanism of action and potentially limiting cellular efficacy [57].
Ligand Discovery for Undruggable Pockets: Many E3 ligases and DUBs lack deep, druggable pockets for high-affinity small-molecule binding. This necessitates advanced screening technologies like DELs and AI-guided design to discover novel, weak-binding starting points [62].
Cellular Activity and Delivery: For bifunctional degraders like PROTACs, large molecular weight and poor drug-like properties often hinder cell permeability and oral bioavailability. Designing smaller, more efficient degraders, such as molecular glues or monovalent Targeted Glues, is a major focus of current research [62].
Resistance Mechanisms: Cancer cells can develop resistance to targeted ubiquitin system drugs through various mechanisms, including mutations in the E3 ligase (e.g., CRBN) that prevent degrader binding, or upregulation of compensatory pathways that bypass the inhibition [55].
Signaling Pathways in CSCs Regulated by Ubiquitination
The core signaling pathways that maintain cancer stemness are heavily regulated by ubiquitination. The following diagram illustrates how key E3 ligases and DUBs intersect with these pathways to control the stability of critical proteins.
Diagram 1: Ubiquitination Regulation of Core CSC Pathways. E3 ligases (blue) promote degradation, while DUBs (yellow) stabilize key components of stemness pathways. Arrows indicate activation/stabilization (green) or degradation/inhibition (red).
Future Perspectives and Concluding Remarks
The field of targeting E3 ligases and DUBs is rapidly evolving beyond simple inhibition. The most significant advance is the development of Targeted Protein Degradation (TPD), exemplified by PROTACs and molecular glues, which hijack E3 ligases to eliminate disease-causing proteins [56] [62]. This approach has moved from concept to clinical reality, with companies like Nurix Therapeutics and Kymera Therapeutics advancing oral degraders into trials for cancer and other diseases [62]. Furthermore, the discovery that small molecules can be ubiquitinated opens avenues for creating novel chemical modalities within cells [57].
For CSC-focused research, the future lies in combining the deep understanding of stemness pathways with these novel therapeutic modalities. Identifying E3 ligases and DUBs with restricted expression in CSCs, or that stabilize core stemness factors, will enable more precise targeting. While no DUB-targeted drugs have yet reached the market, the intense investment and scientific progress indicate that modulating the ubiquitin system will remain a cornerstone of next-generation oncology therapeutics, holding the potential to overcome therapeutic resistance and prevent relapse by targeting the root of the tumor.
The Ubiquitin-Proteasome System (UPS) represents a sophisticated regulatory network that controls protein stability and function, thereby governing fundamental cellular processes. In cancer, and particularly in cancer stem cells (CSCs), this system undergoes significant dysregulation, contributing to the maintenance of stemness, enhanced survival mechanisms, and therapeutic resistance [9] [13]. CSCs constitute a highly plastic and therapy-resistant subpopulation that drives tumor initiation, progression, metastasis, and relapse [13]. Their ability to evade conventional treatments, adapt to metabolic stress, and interact with the tumor microenvironment makes them critical targets for innovative therapeutic strategies [13] [63].
The UPS operates through a sequential enzymatic cascade involving E1 (activating), E2 (conjugating), and E3 (ligating) enzymes that coordinate the attachment of ubiquitin chains to target proteins [64]. The specificity of this process is largely determined by E3 ubiquitin ligases, which recognize particular substrates, while deubiquitinases (DUBs) reverse this modification by removing ubiquitin chains [65] [64]. The functional outcome of ubiquitination depends on the chain topology; for instance, K48-linked polyubiquitination typically targets proteins for proteasomal degradation, whereas K63-linked chains primarily facilitate non-proteolytic signaling processes [65] [64]. In CSCs, the UPS precisely regulates the stability of core transcription factors such as SOX2, OCT4, KLF4, and c-Myc, all of which play crucial roles in CSC self-renewal and differentiation [9]. Furthermore, ubiquitination modulates key signaling pathways including Notch, Wnt/β-catenin, Hedgehog, and Hippo-YAP, which collectively sustain stem-like properties in cancer cells [9] [18]. The strategic targeting of specific UPS components thus presents a promising avenue for disrupting CSC maintenance and overcoming therapy resistance.
Molecular Mechanisms: UPS Regulation of CSC Pathways and Therapeutic Resistance
Ubiquitin Chain Diversity in CSC Maintenance
The ubiquitin system orchestrates CSC maintenance through distinct chain topologies that control protein fate and function. The contextual duality of K48-linked ubiquitination significantly influences radiation response in CSCs. For instance, FBXW7 exemplifies this complexity by promoting radioresistance in p53-wild type colorectal tumors through p53 degradation, while enhancing radiosensitivity in non-small cell lung cancer (NSCLC) with SOX9 overexpression by destabilizing SOX9 and alleviating p21 repression [65]. This functional switch underscores the critical influence of tumor genetics and signaling microenvironment on UPS function in therapy response.
Beyond proteolytic signaling, K63-linked ubiquitin chains serve as architectural scaffolds that directly orchestrate cell survival pathways in CSCs. FBXW7 employs K63 chains to modify XRCC4, enhancing the accuracy of non-homologous end joining (NHEJ) repair [65]. TRAF4 utilizes K63 modifications to activate the JNK/c-Jun pathway, driving overexpression of anti-apoptotic Bcl-xL in colorectal cancer and MCL-1 in oral cancers [65]. Intriguingly, these chains can repurpose tumor suppressors; TRAF6 modifies p53 with K63 linkages, converting it into a pro-survival mitochondrial factor [65]. K63 chains also integrate metabolic and immune regulation, as demonstrated by TRIM26, which stabilizes GPX4 via K63 ubiquitination to prevent ferroptosis in glioma [65].
UPS-Mediated Therapy Resistance Mechanisms
CSCs employ multiple UPS-dependent mechanisms to resist conventional therapies. They exhibit enhanced DNA repair fidelity through ubiquitin-mediated regulation of repair proteins like CHK1, stabilized by OTUB1 in lung cancer, and DNA-PKcs, stabilized by USP7 in HPV+ tumors [65]. Metabolic reprogramming represents another key resistance strategy; UCHL1 stabilizes HIF-1α to activate the pentose phosphate pathway in breast cancer, enhancing antioxidant defense [65]. Furthermore, CSCs manipulate immune surveillance through UPS-mediated mechanisms, as evidenced by TRIM21, which utilizes K48 ubiquitination to degrade VDAC2 in nasopharyngeal carcinoma, thereby suppressing cGAS/STING-mediated immune surveillance [65].
Table 1: Key UPS Enzymes Regulating Therapy Resistance in Cancer
| Enzyme | Tumor Type | Function in Therapeutic Resistance | Therapeutic Vulnerability |
|---|---|---|---|
| FBXW7 | Breast Cancer | Degrades p53 to block apoptosis | MDM2/FBXW7 co-inhibition [65] |
| TRIM26 | Glioma | K63-linked ubiquitination stabilizes GPX4 to suppress ferroptosis | GPX4-K63 ubiquitination as biomarker; ferroptosis inducers [65] |
| USP14 | Glioma | Stabilizes ALKBH5 to maintain stemness | USP14 inhibitors [65] |
| OTUB1 | Lung Cancer | Stabilizes CHK1 to enhance repair fidelity | Inhibiting OTUB1 to destabilize CHK1 [65] |
| UCHL1 | Breast Cancer | Stabilizes HIF-1α to activate antioxidant defense | UCHL1 inhibition in hypoxic tumors [65] |
The plasticity of CSCs is further maintained through dynamic ubiquitination of key developmental pathways. The Wnt/β-catenin pathway, crucial for CSC self-renewal, is regulated by multiple E3 ligases that target β-catenin for degradation, while DUBs such as USP7 can stabilize it, promoting stemness [9] [13]. Similarly, Notch signaling is finely tuned by ubiquitin-mediated regulation of Notch intracellular domain stability, with E3 ligases like FBXW7 targeting it for proteasomal degradation [9]. The intricate modulation of these pathways by the UPS establishes it as a master regulator of CSC plasticity and therapeutic resistance.
Strategic Integration: UPS-Targeted Agents with Conventional Chemotherapy
Overcoming Chemoresistance in CSCs
CSCs exhibit inherent resistance to conventional chemotherapy through multiple UPS-dependent mechanisms, including enhanced drug efflux, activation of survival pathways, efficient DNA damage repair, and epigenetic adaptations [63]. The ATP-binding cassette (ABC) transporter family, particularly P-glycoprotein (P-gp/MDR1/ABCB1), plays a crucial role in chemoresistance by actively expelling chemotherapeutic agents from cancer cells [64] [63]. The ubiquitination system regulates the stability and function of these transporters, with certain E3 ligases and DUBs controlling their degradation or stabilization [64]. Additionally, CSCs often exhibit altered cell cycle kinetics with prolonged quiescence in the G0 phase, enabling them to evade cell cycle-specific chemotherapeutic agents [13] [63]. The UPS regulates key cell cycle checkpoints and DNA repair mechanisms, allowing CSCs to survive genotoxic stress induced by chemotherapy.
Strategic combination approaches leverage UPS-targeted agents to sensitize CSCs to conventional chemotherapy. Proteasome inhibitors, such as bortezomib and carfilzomib, disrupt protein degradation, leading to the accumulation of pro-apoptotic proteins and cell cycle regulators [9] [64]. This accumulation can override the anti-apoptotic mechanisms and enhanced DNA repair capabilities of CSCs. Furthermore, specific E3 ligase inhibitors and DUB inhibitors can be employed to target individual components of the UPS that are critical for CSC survival under chemotherapeutic stress [64]. For instance, targeting USP1, which regulates DNA damage repair and the stability of stemness factors, has shown promise in sensitizing CSCs to DNA-damaging agents [64].
Experimental Models and Protocol Design
In vitro models for evaluating combination therapies typically employ CSC-enriched populations, which can be obtained through methods such as sphere-forming assays under non-adherent conditions or fluorescence-activated cell sorting (FACS) using established CSC surface markers (e.g., CD44+/CD24-, CD133+) [18] [13] [63]. A representative experimental protocol involves:
- CSC Enrichment: Culture cancer cells in serum-free medium supplemented with growth factors (EGF, bFGF) in low-attachment plates to form tumorspheres [63].
- Pre-treatment Viability Assessment: Determine baseline viability via ATP-based assays (e.g., CellTiter-Glo).
- Drug Treatment:
- Arm 1: Chemotherapeutic agent alone (e.g., cisplatin, doxorubicin) at varying concentrations.
- Arm 2: UPS-targeted agent alone (e.g., proteasome inhibitor, E3 ligase inhibitor, DUB inhibitor).
- Arm 3: Combination of both agents.
- Include vehicle control.
- Incubation: Treat cells for 72-96 hours.
- Endpoint Analysis:
- Cell viability assays (MTT, CellTiter-Glo).
- Apoptosis detection (Annexin V/PI staining followed by flow cytometry).
- Evaluation of stemness markers (qPCR or flow cytometry for CD44, CD133, ALDH1 activity).
- Colony formation assay to assess long-term self-renewal capacity.
In vivo validation utilizes patient-derived xenograft (PDX) models or immunocompromised mice transplanted with human CSCs. Animals are randomized into treatment groups mirroring the in vitro design. Tumor volume is monitored regularly, and at endpoint, tumors are excised for analysis of proliferation markers (Ki67), apoptosis (TUNEL staining), and stemness marker expression [13] [63].
Table 2: Quantitative Analysis of UPS-Targeting Agents in Combination with Chemotherapy
| UPS-Targeting Agent | Combination Chemotherapy | Cancer Model | Efficacy Outcomes | Proposed Mechanism |
|---|---|---|---|---|
| Proteasome Inhibitors (e.g., Bortezomib) | DNA-damaging agents (e.g., Cisplatin) | Multiple (e.g., Multiple Myeloma) | Synergistic reduction in viability; Increased apoptosis [9] [64] | Accumulation of pro-apoptotic proteins; Disruption of protein homeostasis [64] |
| E3 Ligase Inhibitors | Standard Cytotoxic Agents | Preclinical models | Enhanced sensitization; Reduced tumor growth [64] | Prevention of degradation of tumor suppressors or DNA repair proteins [65] [64] |
| DUB Inhibitors (e.g., targeting USP1, USP7, USP14) | Platinum-based agents | Preclinical models | Suppression of sphere formation; Reduced stemness marker expression [65] [64] | Impairment of DNA damage repair; Destabilization of stemness transcription factors [65] [64] |
The following diagram illustrates the experimental workflow for evaluating UPS-targeted drugs in combination with chemotherapy:
Synergizing UPS-Targeted Drugs with Immunotherapy
Modulating the Immune Microenvironment
The UPS plays a pivotal role in regulating immune checkpoint molecules and antigen presentation, thereby shaping the tumor immune microenvironment [64]. A key mechanism of immune evasion involves the ubiquitin-mediated regulation of PD-L1. Tumor cells can upregulate deubiquitinase activity to remove ubiquitin chains from PD-L1, increasing its stability and expression on the cell surface, which facilitates T-cell exhaustion [64]. Conversely, E3 ligases such as membrane-associated RING-CH1 (MARCH1) can promote the degradation of PD-L1, potentially enhancing antitumor immunity [64]. This dynamic regulation presents a strategic opportunity for combination therapy, where UPS-targeted agents can be used to modulate PD-L1 levels and improve the efficacy of immune checkpoint inhibitors.
Beyond PD-L1, the UPS regulates other critical aspects of the cancer-immunity cycle. Antigen presentation by major histocompatibility complex (MHC) class I molecules is essential for CD8+ T-cell recognition of tumor cells. The ubiquitin-proteasome pathway generates antigenic peptides for loading onto MHC-I molecules, while certain viral E3 ligases and cancer cells can exploit ubiquitination to downregulate MHC-I surface expression, enabling immune escape [64]. Furthermore, the stability and function of key immune cells within the tumor microenvironment, including T-cells and dendritic cells, are influenced by ubiquitin-mediated processes. Targeting specific E3 ligases or DUBs can therefore reprogram the immune landscape to favor antitumor immunity.
Promising Combination Regimens
The combination of UPS-targeted agents with immunotherapies is an emerging frontier in cancer treatment, with several promising approaches:
PROTACs (Proteolysis-Targeting Chimeras) with Immune Checkpoint Inhibitors: PROTACs are heterobifunctional molecules that recruit E3 ligases to target specific proteins for degradation [65] [64]. They offer a unique advantage by enabling the degradation of oncoproteins previously considered "undruggable." Radiotherapy-triggered PROTAC (RT-PROTAC) prodrugs, activated by tumor-localized X-rays to degrade BRD4/2, have shown synergy with radiotherapy in breast cancer models [65]. Combining such PROTACs with anti-PD-1/PD-L1 antibodies can simultaneously eliminate CSCs and block immune inhibitory pathways. EGFR-directed PROTACs that selectively degrade β-TrCP substrates in EGFR-dependent tumors (e.g., lung and head/neck squamous cell carcinomas) can suppress DNA repair while potentially enhancing immune recognition [65].
DUB Inhibitors with Adoptive Cell Therapy: Inhibiting specific DUBs can destabilize oncoproteins and stemness factors in CSCs [64]. For instance, targeting USP7, which stabilizes CHK1 to maintain genomic stability in breast cancer, or USP14, which stabilizes ALKBH5 to maintain stemness in glioma, can sensitize CSCs to T-cell-mediated killing [65]. When combined with adoptive cell therapies like CAR-T cells targeting CSC antigens (e.g., EpCAM, CD133), DUB inhibition may enhance the elimination of CSCs [13].
Ubiquitin-Targeted Vaccines: The dynamic reversibility of the ubiquitin system and its chain topology diversity present unique clinical advantages for vaccine development [65]. Vaccines designed to target neoantigens derived from dysregulated ubiquitination pathways in CSCs could induce specific immune responses against the CSC population.
Table 3: UPS-Immunotherapy Combinations in Clinical Development
| Combination Strategy | Targeted UPS Component | Immunotherapy Partner | Cancer Type (Example) | Reported Outcome/Mechanism |
|---|---|---|---|---|
| PROTACs | E3 Ligase (e.g., for BRD4, β-TrCP substrates) | Immune Checkpoint Inhibitors (e.g., anti-PD-1) | Breast Cancer, NSCLC [65] | Radiosensitization; Suppressed DNA repair; Enhanced tumor cell killing [65] |
| DUB Inhibitors | USP7, USP14, etc. | Adoptive Cell Therapy (e.g., CAR-T) | Glioma, Breast Cancer [65] | Destabilization of stemness/DNA repair factors (e.g., CHK1, ALKBH5); potential enhancement of CSC susceptibility to immune cells [65] [64] |
| E3 Ligase Modulation | MARCH1 (hypothetical) | Anti-PD-1/PD-L1 | Preclinical Concept [64] | Potential degradation of PD-L1, preventing T-cell exhaustion [64] |
The signaling pathways involved in USP7 inhibition combined with anti-PD-L1 immunotherapy can be visualized as follows:
The Scientist's Toolkit: Research Reagent Solutions
The development and evaluation of UPS-targeted combination therapies rely on a specialized set of research tools and reagents. The following table details key resources essential for experimental investigations in this field.
Table 4: Essential Research Reagents for Investigating UPS-Targeted Combinations
| Reagent Category | Specific Examples | Key Function in Research | Research Application Context |
|---|---|---|---|
| UPS-Targeted Compounds | Proteasome Inhibitors (Bortezomib, Carfilzomib) [9] [64] | Inhibit proteasome activity, causing accumulation of polyubiquitinated proteins. | Induce ER stress and apoptosis; test synergy with chemo/immunotherapy. |
| E3 Ligase Inhibitors (e.g., MDM2 inhibitors) [64] | Block specific E3 ligase-substrate interactions. | Stabilize tumor suppressors (e.g., p53); assess impact on CSC viability. | |
| DUB Inhibitors (e.g., targeting USP7, USP14, OTUB1) [65] [64] | Inhibit deubiquitinating enzyme activity, promoting substrate degradation. | Destabilize oncoproteins and stemness factors; overcome therapy resistance. | |
| PROTACs [65] [64] | Bifunctional molecules that recruit E3 ligases to degrade target proteins. | Degrade specific proteins of interest (e.g., BRD4, oncogenic transcription factors). | |
| CSC Markers & Detection | Antibodies for FACS/Sorting (CD44, CD24, CD133, ALDH1) [18] [13] [63] | Identify and isolate CSC subpopulations from heterogeneous tumors. | CSC enrichment for functional assays; tracking CSC population dynamics post-treatment. |
| Functional Assay Kits | Sphere Formation Assay Reagents [63] | Serum-free media with growth factors (EGF, bFGF) in low-attachment plates. | Assess self-renewal and tumor-initiating capacity of CSCs in vitro. |
| ATP-based Viability/Cytotoxicity Assays (e.g., CellTiter-Glo) [63] | Quantify metabolically active cells via luminescence. | Measure cell viability and proliferation in response to drug treatments. | |
| Apoptosis Detection Kits (Annexin V/Propidium Iodide) [63] | Distinguish between live, early apoptotic, and late apoptotic/necrotic cells. | Evaluate mechanism of cell death induced by single or combination agents. | |
| In Vivo Models | Patient-Derived Xenograft (PDX) Models [13] [63] | Immunocompromised mice transplanted with human tumor tissue. | Preclinically validate drug efficacy and CSC targeting in a physiologically relevant context. |
| CSC-Derived Xenograft Models [13] | Immunocompromised mice transplanted with FACS-sorted human CSCs. | Specifically study the effect of therapies on the tumor-initiating CSC population. |
The integration of UPS-targeted drugs with chemotherapy and immunotherapy represents a paradigm shift in the strategic pursuit of eradicating CSCs and overcoming therapeutic resistance. The molecular complexity of the ubiquitin system, with its nuanced regulation of CSC maintenance, DNA repair, metabolic adaptation, and immune evasion, provides a rich landscape for therapeutic intervention [65] [9] [64]. The clinical translation of these strategies, while promising, faces significant challenges. Functional redundancy within the UPS, potential on-target toxicity, and the adaptive responses of tumors necessitate the development of precise, biomarker-guided approaches [65].
Future directions will likely focus on several key areas. First, the advancement of PROTAC technology offers the potential to target a wider array of oncoproteins and CSC-specific factors with high selectivity, including those previously considered undruggable [65] [64]. Second, the application of artificial intelligence and multi-omics integration will be crucial for identifying predictive biomarkers of response, deciphering the dynamic ubiquitination network, and designing optimal combination regimens [66] [13]. Finally, the development of novel drug delivery systems, such as nanomaterials and nanoparticles, holds promise for improving the specificity and efficacy of UPS-targeted agents while minimizing systemic toxicity [63]. By leveraging these innovative tools and deepening our understanding of ubiquitin biology in CSCs, the goal of developing durable and curative combination therapies becomes increasingly attainable.
Radiation-Responsive PROTACs and Nanotechnology-Based Delivery Systems
The ubiquitin-proteasome system (UPS) represents a pivotal regulatory network in cellular homeostasis, and its dysregulation is increasingly recognized as a critical factor in oncogenesis. This is particularly evident in cancer stem cells (CSCs), which utilize ubiquitination pathways to maintain their pluripotency, self-renewal capacity, and resistance to conventional therapies [67]. Within this conceptual framework, Proteolysis-Targeting Chimeras (PROTACs) have emerged as a revolutionary therapeutic modality capable of hijacking the UPS to selectively degrade disease-causing proteins [53] [50]. These bifunctional molecules consist of a target protein-binding ligand connected to an E3 ubiquitin ligase-recruiting moiety via a synthetic linker, enabling the targeted ubiquitination and subsequent proteasomal degradation of specific proteins of interest (POIs) [53].
Despite their transformative potential, conventional PROTACs face substantial pharmacological challenges, including off-target toxicity, poor solubility, and limited bioavailability [68]. To address these limitations, researchers are developing stimulus-activated "pro-PROTACs" or latent PROTACs that remain inert until activated by specific physiological or external triggers [53]. Among these advanced approaches, radiation-responsive PROTAC systems represent a particularly promising frontier, offering spatiotemporal control over protein degradation activity. Concurrently, nanotechnology-driven delivery platforms are being engineered to overcome the pharmacological barriers that have hindered the clinical translation of PROTAC therapeutics [69] [68]. This review examines the integration of these emerging technologies, focusing on their application in disrupting ubiquitination-dependent pathways that sustain cancer stem cell populations.
PROTAC Technology: Mechanism and Therapeutic Rationale
Fundamental Principles of Targeted Protein Degradation
PROTACs function through a catalytic mechanism distinct from traditional occupancy-based inhibitors. A typical PROTAC molecule comprises three essential components: (1) a ligand that binds specifically to the protein of interest (POI), (2) an E3 ubiquitin ligase-recruiting ligand, and (3) a linker connecting these two moieties [53]. The PROTAC molecule facilitates the formation of a ternary complex between the POI and an E3 ubiquitin ligase, such as Cereblon (CRBN) or Von Hippel-Lindau (VHL). This complex proximity enables the transfer of ubiquitin chains from the E2 conjugating enzyme to lysine residues on the POI's surface [53] [50]. The ubiquitinated POI is then recognized and degraded by the 26S proteasome, freeing the PROTAC molecule to catalyze additional degradation cycles [53].
This catalytic mode of action provides significant advantages over conventional small-molecule inhibitors. PROTACs can achieve efficacy at sub-stoichiometric concentrations and effectively target proteins previously considered "undruggable," including non-enzymatic scaffolds and transcription factors [50]. Notably, PROTACs have demonstrated particular utility in overcoming resistance mechanisms driven by protein overexpression or mutation, as they remove the target protein entirely rather than merely inhibiting its function [53].
PROTACs in Cancer Stem Cell Targeting
The therapeutic potential of PROTACs extends significantly to targeting CSC maintenance pathways. CSCs frequently exploit ubiquitination networks to regulate core self-renewal pathways, and PROTACs offer a unique strategy to disrupt these signaling cascades through targeted protein degradation rather than mere inhibition [70]. For instance, in colorectal cancer, KDM3 family histone demethylases (KDM3A and KDM3B) epigenetically regulate CSC properties through the Wnt/β-catenin signaling pathway [70]. Research has demonstrated that PROTACs designed to degrade KDM3 proteins can effectively suppress oncogenic Wnt signaling and eliminate colorectal CSCs with approximately 10- to 35-fold increased potency compared to traditional inhibitors like IOX1 [70]. This approach validates the strategic advantage of protein degradation over inhibition for disrupting critical CSC maintenance pathways.
Table 1: Representative PROTACs in Oncology Research and Development
| PROTAC Target | E3 Ligase Ligand | Cancer Type | Development Stage | Key Findings |
|---|---|---|---|---|
| KDM3A/KDM3B | Pomalidomide (CRBN) | Colorectal Cancer | Preclinical | Selective degradation suppresses Wnt/β-catenin signaling; eliminates CSCs [70] |
| BRD4 | Thalidomide (CRBN) | Multiple Cancers | Preclinical/Clinical | First breakthrough PROTAC target; several candidates in development [53] [50] |
| Androgen Receptor (AR) | CRBN/VHL | Prostate Cancer | Phase III (ARV-110) | Degrades AR in castration-resistant prostate cancer [53] |
| Estrogen Receptor (ER) | CRBN/VHL | Breast Cancer | Phase III (ARV-471) | Demonstrates efficacy in hormone-resistant breast cancer [53] |
| BTK | CRBN/VHL | Hematologic Cancers | Preclinical/Clinical | Overcomes resistance mutations in B-cell malignancies [53] |
Radiation-Responsive PROTAC Systems
Pro-PROTAC Strategies for Spatiotemporal Control
The concept of "pro-PROTACs" or latent PROTACs involves engineering biologically inactive PROTAC precursors that can be selectively activated under specific conditions [53]. This strategy addresses key limitations of conventional PROTACs, particularly off-target effects and uncontrolled activity duration. Pro-PROTACs are designed with labile protecting groups that mask critical functional elements required for ternary complex formation, such as the E3 ligase-binding moiety or the target protein-binding domain [53]. These protecting groups remain stable under physiological conditions but are cleaved in response to specific stimuli, releasing the active PROTAC molecule precisely where and when needed.
Several pro-PROTAC approaches have been successfully demonstrated, with photocaged PROTACs (opto-PROTACs) representing the most advanced technology in this category. These systems utilize photolabile groups such as 4,5-dimethoxy-2-nitrobenzyl (DMNB), diethylamino coumarin (DEACM), or 6-nitropiperonyloxymethyl (NPOM) to cage critical functional groups on either the E3 ligase ligand or the POI-binding warhead [53]. For instance, researchers have installed DMNB groups on the glutarimide nitrogen of thalidomide-based CRBN ligands, effectively preventing essential hydrogen bonding interactions with the E3 ligase until UV light exposure removes the caging group [53]. Similarly, caging the hydroxyproline residue of VHL ligands with DEACM via a carbonate linkage has yielded light-activatable PROTAC systems [53].
Radiation as an Activation Stimulus
While optical activation represents a powerful research tool, its clinical utility is limited by poor tissue penetration of light. Radiation-responsive PROTAC systems offer a more translatable approach for deep-seated tumors by leveraging clinically relevant radiation sources. Although direct references to radiation-responsive PROTACs are limited in the provided search results, the fundamental principles of radiation-activated prodrugs can be extrapolated to PROTAC design based on the established pro-PROTAC paradigm.
Two primary strategies can be envisioned for radiation-activated PROTAC systems:
Radiolabile Protecting Groups: Incorporating radiation-cleavable linkers or protecting groups that fragment upon radiation exposure, particularly in response to clinical radiotherapy energies (e.g., X-rays). These systems could utilize radiation-sensitive moieties such as azobenzene derivatives, nitroaromatic compounds, or gold nanoparticles that enhance radiosensitivity.
Radiation-Induced Expression: Utilizing radiation-responsive promoters to drive the expression of enzymes that activate pro-PROTACs or components of the ubiquitin-proteasome system, thereby creating amplified degradation cascades in irradiated tissues.
The integration of nanotechnology further enhances this approach by enabling the targeted delivery of pro-PROTACs to tumor sites, where localized radiation therapy can trigger their activation specifically within the tumor microenvironment while minimizing systemic exposure [71].
Diagram 1: Radiation-Responsive PROTAC Mechanism for CSC Targeting. This diagram illustrates the sequential activation and mechanism of radiation-responsive PROTACs, from stimulus-induced activation to disruption of cancer stem cell maintenance pathways.
Nanotechnology Platforms for PROTAC Delivery
Nanoparticle Design Considerations for PROTAC Delivery
The effective delivery of PROTACs presents unique challenges that nanotechnology aims to address. Most PROTAC molecules exhibit poor aqueous solubility, limited cellular permeability, and unfavorable pharmacokinetic profiles [68]. Nanoparticle-based delivery systems can overcome these limitations through several design strategies:
Size Optimization: Nanoparticles in the 50-200 nm range optimally balance circulation time and tumor accumulation via the Enhanced Permeability and Retention (EPR) effect [72]. This size range exceeds the renal clearance threshold (~5 nm) while allowing extravasation through leaky tumor vasculature.
Surface Functionalization: PEGylation creates a hydrophilic stealth layer that reduces opsonization and recognition by the mononuclear phagocyte system, significantly extending circulation half-life [72]. Additionally, surface modification with targeting ligands (e.g., antibodies, peptides, aptamers) enables active targeting of specific cell populations, including CSCs.
Stimuli-Responsive Release: Advanced nanocarriers can be engineered to release their PROTAC payload in response to tumor-specific stimuli such as pH, enzymatic activity, or external triggers like radiation [69] [71].
Table 2: Nanocarrier Platforms for PROTAC Delivery
| Nanocarrier Type | Composition | Advantages for PROTAC Delivery | Representative Examples |
|---|---|---|---|
| Liposomal Nanoparticles | Phospholipid bilayers | Improved solubility of hydrophobic PROTACs; enhanced stability and circulation time [69] [72] | Doxil (liposomal doxorubicin) [72] |
| Polymeric Nanoparticles | Biodegradable polymers (PLGA, chitosan) | Controlled release kinetics; protection from enzymatic degradation [69] [72] | Experimental PLGA-based systems [69] |
| Inorganic Nanoparticles | Silica, gold, iron oxide | High drug loading capacity; multifunctionality for combination therapy [69] [73] | Silica nanoparticles with lactate-gated release [71] |
| Hybrid Nanosystems | Composite materials | Tunable properties; synergistic functionality [73] | ZAP-Brucine nanoparticles [73] |
Radiation-Enhanced Nanocarriers for Tumor-Specific Delivery
Nanotechnology platforms can be specifically engineered to respond to radiation, creating synergistic systems for spatially controlled PROTAC activation and release. Several innovative approaches demonstrate this principle:
The lactate-gated nanosystem developed by Wu and colleagues exemplifies stimulus-responsive delivery [71]. This platform exploits the Warburg effect, wherein cancer cells exhibit elevated lactate production. The nanoparticle incorporates lactate oxidase, which converts lactate to hydrogen peroxide, and a hydrogen peroxide-sensitive molecular cap that controls drug release. In lactate-rich tumor microenvironments, hydrogen peroxide production triggers degranulation of the capping material and subsequent PROTAC release [71]. Since radiation therapy can further increase lactate production in tumors, this system offers inherent potential for radiation-enhanced activation.
Radiation-responsive nanocarriers can be designed using materials that undergo structural changes or generate reactive oxygen species upon radiation exposure. For instance, gold nanoparticles can enhance radiosensitivity through energy absorption and secondary electron emission, while certain polymeric systems can incorporate radiation-cleavable linkers that fragment upon exposure, triggering payload release specifically in irradiated tissues.
These advanced nanoplatforms enable the precise spatial and temporal control of PROTAC activity, potentially overcoming the therapeutic index limitations that have hindered conventional protein degradation approaches.
Diagram 2: Nanotechnology-Mediated Delivery of PROTACs to CSCs. This workflow illustrates the integration of passive and active targeting strategies with stimulus-responsive release mechanisms for precise CSC targeting.
Experimental Protocols and Methodologies
Design and Synthesis of Radiation-Responsive Pro-PROTACs
The development of radiation-activated PROTACs requires a multidisciplinary approach combining synthetic chemistry, radiobiology, and nanomaterial science. Below is a representative protocol for creating and evaluating such systems:
Step 1: Molecular Design and Computational Modeling
- Conduct molecular docking studies to identify optimal attachment points for radiation-labile groups that minimally interfere with ternary complex formation in the active state [70]. Tools like AutoDock Vina or GOLD are commonly used for this purpose.
- Perform molecular dynamics simulations to assess the stability of the pro-PROTAC conformation and predict cleavage efficiency under radiation exposure [69].
- Select appropriate radiation-sensitive moieties based on the energy levels of clinical radiotherapy systems (typically 6-15 MeV for linear accelerators).
Step 2: Synthetic Chemistry and Characterization
- Synthesize pro-PROTAC derivatives by incorporating radiation-cleavable linkers (e.g., azobenzene, nitroaromatic compounds) at strategic positions that disrupt E3 ligase binding [53] [70].
- Purify compounds using flash chromatography and confirm structures via NMR and high-resolution mass spectrometry.
- Evaluate photophysical properties and radiation sensitivity using spectrophotometric methods following irradiation at clinical relevant doses (2-10 Gy).
Step 3: Nanocarrier Formulation and Drug Loading
- Prepare nanoparticle formulations using appropriate methods (e.g., solvent evaporation, microfluidics) [72].
- Load pro-PROTACs into nanocarriers and determine loading efficiency and encapsulation efficiency using HPLC.
- Characterize nanoparticle size, zeta potential, and morphology using dynamic light scattering and electron microscopy.
In Vitro and In Vivo Evaluation
Cellular Assays:
- Validate pro-PROTAC inertness and radiation-induced activation in relevant cancer cell lines, including CSC-enriched populations [70].
- Assess target protein degradation via western blotting and immunofluorescence at various time points post-irradiation.
- Evaluate anticancer efficacy using viability assays (MTT, CellTiter-Glo) and CSC-specific functional assays (sphere formation, ALDH activity) [70].
- Confirm mechanism of action through rescue experiments with proteasome inhibitors (MG132) and E3 ligase competitors.
Animal Studies:
- Establish xenograft models using CSC-enriched tumor cells [70].
- Evaluate biodistribution and tumor accumulation of radiolabeled pro-PROTAC nanocarriers via IVIS or PET imaging.
- Assess therapeutic efficacy by monitoring tumor growth and survival in cohorts receiving: (1) vehicle control, (2) radiation alone, (3) pro-PROTAC nanocarriers alone, (4) conventional PROTACs, and (5) pro-PROTAC nanocarriers + radiation.
- Analyze tumor tissues for evidence of target protein degradation, apoptosis, and CSC marker expression via immunohistochemistry.
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Research Reagents for Radiation-Responsive PROTAC Development
| Reagent/Category | Specific Examples | Research Function | Experimental Context |
|---|---|---|---|
| E3 Ligase Ligands | Thalidomide, Pomalidomide, VHL Ligands | Recruit E3 ubiquitin ligase to form ternary complex | PROTAC design [53] [70] |
| Target Protein Binders | IOX1 (for KDM3), BET inhibitors (for BRD4) | Bind protein of interest and bring it into proximity with E3 ligase | PROTAC warhead selection [70] |
| Linker Systems | PEG chains, alkyl chains | Connect warhead to E3 ligase ligand at optimal distance and orientation | PROTAC optimization [70] |
| Radiation-Cleavable Groups | Azobenzene, nitroaromatics | Provide radiation sensitivity for controlled activation | Pro-PROTAC design |
| Nanocarrier Components | PLGA, phospholipids, silica | Formulate delivery vehicles for improved PROTAC pharmacokinetics | Nanotechnology integration [69] [72] |
| Characterization Tools | Surface plasmon resonance, isothermal titration calorimetry | Evaluate binding affinity and ternary complex formation | PROTAC validation [70] |
The integration of radiation-responsive PROTAC technology with advanced nanotechnology delivery platforms represents a paradigm shift in targeted cancer therapy, particularly for addressing the therapeutic challenge of cancer stem cells. This convergent approach leverages the catalytic efficiency and target range of PROTACs, the spatiotemporal control of radiation activation, and the enhanced pharmacokinetics of nanocarrier systems. By specifically disrupting ubiquitination-dependent pathways that maintain CSC populations, these innovative therapeutic strategies offer potential solutions to the problems of tumor recurrence and therapeutic resistance.
Future developments in this field will likely focus on optimizing radiation-sensitive chemistries for clinical energy sources, engineering multifunctional nanocarriers with enhanced tumor targeting capabilities, and identifying novel E3 ligases with restricted expression patterns for improved tissue specificity. Additionally, the combination of radiation-responsive PROTACs with immunotherapy approaches represents a promising frontier for achieving sustained antitumor responses. As these technologies mature, they hold significant potential to transform the therapeutic landscape for aggressive, treatment-resistant cancers by directly targeting the CSC populations that drive disease progression and recurrence.
Navigating Roadblocks: Overcoming Functional Redundancy and Toxicity in UPS Targeting
Addressing Functional Redundancy and Compensation in the Ubiquitin System
The ubiquitin system, a master regulator of protein stability and function, exhibits extensive functional redundancy and compensatory mechanisms that pose significant challenges for therapeutic intervention, particularly in the context of cancer stem cell (CSC) maintenance. This technical review examines the molecular basis of redundancy within the ubiquitin-proteasome system (UPS), focusing on the hierarchical E1-E2-E3 enzyme cascade, diverse polyubiquitin chain topologies, and the balancing role of deubiquitinating enzymes (DUBs). Through structured analysis of quantitative data and experimental methodologies, we provide a framework for addressing these challenges in CSC research, where ubiquitination precisely controls core transcription factors and signaling pathways essential for stemness maintenance. The insights presented herein aim to guide researchers in developing strategies to overcome redundancy-related obstacles in targeting the UPS for cancer therapy.
The ubiquitin system represents one of the most sophisticated post-translational regulatory networks in eukaryotic cells, coordinating the precise spatiotemporal control of protein degradation, activity, and localization. This system operates through a sequential enzymatic cascade involving E1 (activating), E2 (conjugating), and E3 (ligating) enzymes that conjugate the 76-amino acid ubiquitin protein to specific substrate proteins [2] [74]. The outcome of ubiquitination is determined by the topology of ubiquitin modifications, which range from monoubiquitination to various polyubiquitin chain architectures linked through specific lysine residues (K6, K11, K27, K29, K33, K48, K63) or the N-terminal methionine (M1) [2] [3]. This "ubiquitin code" is further deciphered by ubiquitin receptors and reversed by deubiquitinating enzymes (DUBs), creating a dynamic, reversible regulatory system [2].
In the context of cancer stem cells (CSCs)—a subpopulation of tumor cells with self-renewal capacity and therapeutic resistance—the ubiquitin system regulates core transcription factors (Nanog, Oct4, Sox2) and signaling pathways (Notch, Hedgehog, Wnt/β-catenin, Hippo-YAP) that maintain stemness and pluripotency [5] [9]. The functional redundancy inherent in the ubiquitin system creates resilience that protects CSC maintenance networks from therapeutic perturbation. Understanding and addressing this redundancy is therefore essential for developing effective strategies to eliminate CSCs and prevent tumor recurrence.
Molecular Foundations of Redundancy and Compensation
Hierarchical Enzyme Architecture
The ubiquitin system employs a pyramidal hierarchy where a limited number of E1 enzymes (2 in humans) activate ubiquitin for transfer to approximately 35 E2 enzymes, which subsequently partner with over 600 E3 ligases to confer substrate specificity [2] [75]. This architecture inherently creates multiple parallel pathways for substrate ubiquitination, as illustrated in Table 1.
Table 1: Redundancy in Human Ubiquitin System Enzymes
| Enzyme Class | Number of Human Genes | Functional Redundancy Mechanisms |
|---|---|---|
| E1 (Activating) | 2 (UBA1, UBA6) | Broad specificity for all E2s; essential cellular functions |
| E2 (Conjugating) | ~35 | Partial overlap in E3 partnerships and substrate specificity |
| E3 (Ligating) | 600+ | Substrate promiscuity; shared degradation signals |
| DUBs (Deubiquitinating) | ~100 | Overlap in chain type specificity; compensatory expression |
This enzymatic hierarchy creates built-in redundancy, where the inhibition of specific E3s may be compensated by related E3s with overlapping substrate specificities or through adaptive overexpression of alternative enzymes. For instance, multiple E3 ligases can target the same core transcription factors in CSCs, creating fail-safe mechanisms that maintain stemness regulatory networks despite therapeutic intervention [5].
Diverse Ubiquitin Chain Topologies
The ubiquitin code's complexity arises from the various chain architectures that determine substrate fate. While K48-linked chains typically target proteins for proteasomal degradation, other chain types regulate non-proteolytic functions including signal transduction, DNA repair, and endocytosis [2] [74]. This functional diversity enables compensatory mechanisms when specific ubiquitination pathways are disrupted.
Table 2: Functional Diversity of Ubiquitin Chain Linkages
| Linkage Type | Primary Functions | Compensatory Potential |
|---|---|---|
| K48 | Proteasomal degradation | High - Multiple degradation signals |
| K63 | DNA repair, endocytosis, signaling | Medium - Context-dependent redundancy |
| K11 | Proteasomal degradation, cell cycle | Medium - Overlap with K48 functions |
| K29 | Proteasomal degradation, basal metabolism | Low - Specialized functions |
| M1 (Linear) | NF-κB signaling, inflammation | Low - Specialized assembly complex |
| K27 | DNA damage response, mitophagy | Emerging redundancy mechanisms |
| K6 | DNA damage response, mitophagy | Not well characterized |
| K33 | Kinase regulation, trafficking | Not well characterized |
The functional outcomes of different ubiquitin modifications create a system where alternative chain types can partially compensate when primary degradation signals are impaired, particularly in stress adaptation responses crucial for CSC survival [3].
Experimental Approaches for Dissecting Redundancy
Comprehensive E3 Ligase Profiling
Protocol: CRISPR-Cas9 Synthetic Lethality Screening for Redundant E3s
Library Design: Utilize a genome-wide sgRNA library targeting all known E3 ubiquitin ligases and DUBs, including multiple guides per gene to ensure coverage.
Cell Line Selection: Employ isogenic pairs of CSC-enriched and differentiated cancer cells from the same tumor origin. CSC enrichment can be achieved through fluorescence-activated cell sorting (FACS) for established surface markers (CD44+CD24- for breast CSCs, CD133+ for various solid tumors).
Screening Conditions: Transduce cells with the sgRNA library at low multiplicity of infection (MOI = 0.3) to ensure single integration events. Include both baseline and negative control sgRNAs.
Selection and Analysis: Maintain cells for at least 14 population doublings under normal culture conditions. Harvest genomic DNA at multiple time points and sequence the integrated sgRNAs to quantify enrichment/depletion.
Hit Validation: Identify synthetic lethal pairs where simultaneous knockout of two or more E3s significantly impairs CSC viability but not differentiated cells. Validate hits using individual sgRNAs and rescue experiments with cDNA constructs.
This approach can reveal compensatory relationships between E3 ligases that maintain essential CSC functions, identifying nodal points where redundancy creates therapeutic vulnerabilities.
Ubiquitin Chain-Type Specific Proteomics
Protocol: Quantitative Proteomics with Linkage-Specific Ubiquitin Antibodies
Sample Preparation: Generate stable cell lines expressing tagged ubiquitin mutants (K48-only, K63-only, etc.) under inducible promoters. Alternatively, use linkage-specific ubiquitin antibodies for immunopurification.
Ubiquitin Enrichment: Lyse cells under denaturing conditions (1% SDS, 50mM Tris pH 7.5) to preserve ubiquitin modifications. Dilute SDS to 0.1% and incubate with linkage-specific antibodies (e.g., K48-, K63-specific) conjugated to protein A/G beads overnight at 4°C.
Proteomic Analysis: Wash beads extensively, elute ubiquitinated proteins, and digest with trypsin. Analyze peptides by liquid chromatography-tandem mass spectrometry (LC-MS/MS) using data-independent acquisition (DIA) for quantitative precision.
Data Processing: Identify ubiquitination sites and chain types using software platforms like MaxQuant with integrated ubiquitin remnant motif analysis. Normalize data and perform statistical analysis to identify significant changes in ubiquitination patterns following E3 inhibition.
Functional Validation: Confirm proteomic findings by immunoblotting with linkage-specific antibodies and functional assays for pathway activity.
This methodology enables researchers to map how ubiquitin chain usage adapts when specific components of the ubiquitin system are inhibited, revealing compensatory mechanisms that maintain critical signaling pathways in CSCs.
Visualization of Ubiquitin System Redundancy
Diagram 1: Ubiquitin System Architecture Showing Redundancy Mechanisms. This visualization illustrates the hierarchical enzyme structure and multiple points where functional redundancy occurs, from E2-E3 partnerships to substrate targeting and diverse chain-type outcomes.
Research Reagent Solutions for Redundancy Studies
Table 3: Essential Research Tools for Investigating Ubiquitin System Redundancy
| Reagent Category | Specific Examples | Research Application | Considerations for Redundancy Studies |
|---|---|---|---|
| E1 Inhibitors | PYR-41, TAK-243 | System-wide ubiquitination blockade | Useful for establishing baseline effects but lacks specificity |
| E2 Enzyme Kits | UBE2L3, UBE2D3, UBE2R1 panels | In vitro ubiquitination assays | Test multiple E2s to identify compensatory partnerships |
| E3 Ligase Inhibitors | MLN4924 (NEDD8-activating enzyme inhibitor) | CRL complex disruption | Targets multiple cullin-RING ligases simultaneously |
| Linkage-Specific Antibodies | K48-, K63-, M1-linked ubiquitin antibodies | Chain-type specific immunoblotting | Essential for detecting ubiquitin code rewiring |
| DUB Inhibitors | PR-619 (pan-DUB inhibitor), specific USP7/46 inhibitors | DUB activity blockade | Pan-inhibitors reveal system compensation mechanisms |
| Activity-Based Probes | Ubiquitin-VS, HA-Ub-VME | DUB profiling and identification | Identify DUBs with overlapping substrate specificities |
| PROTAC Molecules | ARV-110, ARV-471 | Targeted protein degradation | Can bypass resistance from E3 redundancy |
| CRISPR Libraries | E3/DUB-focused sgRNA libraries | Synthetic lethality screening | Identify compensatory gene pairs systematically |
| Ubiquitin Mutants | K48R, K63R, K48-only, K63-only | Chain-type function studies | Dissect specific chain functionality in compensation |
| Mass Spectrometry Grade | Trypsin/Lys-C, TMT reagents | Ubiquitin remnant profiling | Quantify ubiquitination site changes comprehensively |
These research tools enable systematic dissection of redundancy mechanisms in the ubiquitin system. When designing studies focused on CSCs, researchers should employ multiple complementary approaches to overcome the limitations of individual reagents, particularly given the context-dependent nature of ubiquitin system compensation.
Therapeutic Implications and Future Directions
The functional redundancy within the ubiquitin system presents both challenges and opportunities for CSC-targeted therapies. Combination approaches that simultaneously target multiple nodes in the ubiquitin system may overcome compensatory mechanisms that maintain CSC survival. Emerging strategies include:
Polypharmacology Agents: Developing small molecules that inhibit multiple E3 ligases with shared substrate specificities, potentially through targeting common protein-protein interaction domains.
PROTAC Platforms: Utilizing proteolysis-targeting chimeras that recruit multiple E3 ligases to the same oncogenic substrate, exploiting rather than fighting redundancy.
Systems-Level Targeting: Identifying master regulatory E3s or DUBs that sit at nodal points in CSC maintenance networks, where inhibition cannot be easily compensated.
Adaptive Response Blockade: Combining E3 inhibitors with agents that prevent compensatory overexpression of alternative ubiquitin system components.
Future research should focus on mapping the complete redundancy network in specific CSC subtypes, developing more sophisticated tools to monitor real-time ubiquitin code dynamics, and creating computational models that predict compensatory mechanisms before they emerge in therapeutic settings. As our understanding of ubiquitin system redundancy matures, so too will our ability to strategically disrupt this critical regulatory system in CSCs while sparing normal stem cell populations.
Managing On-Target Toxicity and Identifying Therapeutic Windows for CSC Eradication
Cancer stem cells (CSCs) represent a subpopulation within tumors characterized by self-renewal capacity, differentiation potential, and enhanced resistance to conventional therapies. These properties drive tumor initiation, progression, metastasis, and recurrence [76] [18]. The ubiquitin-proteasome system (UPS) has emerged as a critical regulatory mechanism governing CSC functionality through post-translational control of protein stability, signaling pathway activity, and stemness transcription factors [9]. Ubiquitination, a highly versatile enzymatic process involving E1 activating, E2 conjugating, and E3 ligase enzymes, determines the fate of proteins essential for CSC maintenance, including those involved in Wnt/β-catenin, Notch, and Hedgehog pathways [77] [9]. While targeting ubiquitination processes offers promising therapeutic avenues for CSC eradication, the development of these approaches must carefully address the challenge of on-target toxicity—where inhibiting essential UPS components in normal stem cells and healthy tissues causes unacceptable adverse effects [78] [13]. This technical guide examines strategies to manage these toxicities and identify therapeutic windows for CSC-directed therapies targeting ubiquitination pathways.
Ubiquitination Mechanisms in CSC Regulation: Key Targets and Toxicities
The Ubiquitin-Proteasome Machinery
The ubiquitination cascade involves sequential action of E1, E2, and E3 enzymes, with E3 ubiquitin ligases providing substrate specificity by recognizing target proteins [77]. More than 600 E3 ligases exist in humans, categorized into four main classes: really interesting new gene (RING)-type, U-box-type, homologous to E6AP carboxyl terminus (HECT)-type, and RING-between-RING (RBR)-type E3 ligases [77]. Additionally, deubiquitinases (DUBs) counter-regulate this process by removing ubiquitin chains, providing a dynamic control mechanism for protein stability [9]. In CSCs, this system regulates key transcription factors (SOX2, OCT4, KLF4, c-Myc), signaling pathways, and metabolic enzymes that maintain stemness properties [9].
Table 1: Ubiquitination Enzyme Classes and Their Roles in CSC Maintenance
| Enzyme Class | Representative Members | Role in CSC Maintenance | Potential Toxicity Concerns |
|---|---|---|---|
| E1 Activators | UBA1, UBA6 | Initial ubiquitin activation; essential for all ubiquitination | High toxicity risk due to universal function in protein degradation |
| E2 Conjugators | ~40 members (e.g., CDC34, UBCH5) | Ubiquitin shuttle to specific substrates | Variable risk depending on tissue expression and specificity |
| E3 Ligases | RING-type (e.g., CRL family), HECT-type (e.g., NEDD4), RBR-type | Substrate recognition; precise targeting of stemness factors | Better therapeutic window with careful selection of tissue-specific E3s |
| Deubiquitinases | ~100 members (e.g., USP22, BAP1) | Ubiquitin chain removal; stabilization of CSC factors | Emerging targets with potential for pathway-specific modulation |
CSC-Specific Signaling Pathways Regulated by Ubiquitination
Ubiquitination critically regulates several key signaling pathways that maintain CSC stemness and survival. The Wnt/β-catenin pathway, essential for CSC self-renewal, is tightly controlled by a destruction complex containing GSK3β that promotes β-catenin ubiquitination and degradation [79]. Notch signaling, which maintains CSC populations in various cancers, is similarly regulated by ubiquitin-mediated degradation of Notch intracellular domain [79] [9]. The Hedgehog pathway and Hippo-YAP pathway, the latter being crucial for CSC generation in bladder cancer and lung adenocarcinoma, also undergo ubiquitination regulation [78] [9]. The interconnected nature of these pathways creates both challenges and opportunities for therapeutic intervention, as inhibition of specific E3 ligases or DUBs may simultaneously modulate multiple stemness pathways while potentially causing broad physiological effects.
Diagram 1: Ubiquitination Regulation of CSC Stemness Pathways. The ubiquitin-proteasome system, comprising E1, E2, E3 enzymes and deubiquitinases (DUBs), regulates key stemness pathways and transcription factors in cancer stem cells. Strategic targeting of specific components (highlighted in red and green) can disrupt CSC maintenance while potentially sparing normal stem cells.
Managing On-Target Toxicity in CSC-Targeted Therapies
Therapeutic Window Challenges in UPS Targeting
The fundamental challenge in targeting ubiquitination processes for CSC eradication lies in the essential nature of UPS components for normal cellular homeostasis, particularly in healthy stem cells that share regulatory mechanisms with CSCs [78] [13]. First-generation proteasome inhibitors like bortezomib and carfilzomib demonstrated that broad UPS inhibition can have efficacy in hematological malignancies but often with significant toxicity profiles that limit their utility in solid tumors [9]. These observations highlight the critical need for strategies that maximize therapeutic windows by exploiting meaningful biochemical and biological differences between normal and cancer stem cells.
Strategies for Toxicity Mitigation
Targeting CSC-Specific E3 Ligases and DUBs
The large number of E3 ligases (>600) and DUBs (~100) provides opportunities to identify specific enzymes with preferential importance in CSCs versus normal stem cells. For example, targeting E3 ligases that regulate CSC-specific variants of stemness transcription factors or targeting DUBs that stabilize oncogenic versions of signaling proteins may provide enhanced selectivity [9]. Research has identified specific E3 ligases that regulate transcription factors such as SOX2, OCT4, and NANOG in CSCs, suggesting potential targets with reduced impact on normal stem cell function [9].
Exploiting Differential Pathway Dependency
While normal and cancer stem cells may share signaling pathways, they often exhibit differential dependency on specific regulatory nodes. For instance, the YAP1 pathway appears particularly critical for CSC maintenance in bladder cancer and lung adenocarcinoma, with pharmacological inhibition using verteporfin showing efficacy in attenuating CSC properties and enhancing chemotherapy response [78]. Similarly, targeting ubiquitination enzymes specifically involved in hyperactive Wnt/β-catenin signaling in CSCs may provide therapeutic windows, as normal stem cells utilize this pathway but with different regulation and feedback mechanisms [77] [79].
Combination Therapy Approaches
Lower-dose combination therapies represent a promising strategy for managing on-target toxicity while maintaining efficacy. Combining ubiquitination-targeting agents with conventional chemotherapy or targeted therapies can enable dose reduction of each component while simultaneously targeting both CSCs and bulk tumor cells [78] [80]. For example, combining YAP1 inhibition with conventional chemotherapy in bladder cancer models enhanced therapeutic response while potentially reducing individual drug toxicity [78]. Similarly, nanotechnology approaches can enhance targeted delivery of ubiquitination modulators to CSCs, further improving therapeutic indices [76] [80].
Table 2: Strategies for Managing On-Target Toxicity in CSC-Targeted Therapies
| Strategy | Mechanism | Examples | Toxicity Mitigation Approach |
|---|---|---|---|
| Specific E3 Ligase Targeting | Inhibit E3 ligases with preferential CSC expression or function | CRL family inhibitors; RING-type E3 specific compounds | Avoid broad proteasome inhibition; exploit tissue-specific E3 expression |
| DUB Inhibition | Target deubiquitinases stabilizing oncogenic CSC factors | USP family inhibitors; preclinical DUB-targeting compounds | Selective targeting of DUBs with minimal normal stem cell function |
| Pathway-Specific Intervention | Exploit differential pathway dependency between normal and CSCs | Verteporfin (YAP inhibition); Wnt pathway inhibitors | Leverage synthetic lethal interactions in CSCs |
| Combination Therapy | Lower doses of multiple agents targeting complementary pathways | YAP1 + chemotherapy; E3 inhibitors + differentiation agents | Reduced individual drug exposure while maintaining efficacy |
| Nanoparticle Delivery | Enhance targeted delivery to CSCs and tumor microenvironment | CD44-targeted nanoparticles; CSC marker-conjugated nanocarriers | Reduced systemic exposure and improved tumor accumulation |
Experimental Protocols for Assessing Therapeutic Windows
In Vitro Assessment of CSC-Specific Toxicity
Protocol 1: Comparative Toxicity Screening in Normal Stem Cells versus CSCs
Objective: Evaluate differential toxicity of ubiquitination-targeting compounds in normal stem cells and CSCs.
Materials:
- Patient-derived CSCs and matched normal stem cells (e.g., mesenchymal stem cells)
- Ubiquitination-targeting compounds (E1/E2/E3/DUB inhibitors)
- Aldefluor assay kit for ALDH activity assessment
- Flow cytometry equipment with appropriate antibodies for CSC surface markers (CD44, CD133, CD24)
- Sphere formation assay materials (ultra-low attachment plates, defined serum-free media)
Methodology:
- Establish cultures of CSCs (from patient-derived xenografts or sphere cultures) and normal stem cells with comparable passage numbers.
- Treat parallel cultures with serial dilutions of ubiquitination-targeting compounds for 72 hours.
- Assess viability using multiplexed assays: ATP-based viability, apoptosis markers (Annexin V/PI), and colony formation capacity.
- Evaluate CSC-specific functional properties: sphere-forming capacity in ultra-low attachment plates, ALDH activity via Aldefluor assay, and surface marker expression by flow cytometry.
- Calculate selective toxicity indices (STI) as: STI = IC50 (normal stem cells) / IC50 (CSCs)
- Perform counter-screening against differentiated cell types (fibroblasts, epithelial cells) to identify general cytotoxic effects.
Data Interpretation: Compounds with STI >3.0 suggest potential therapeutic windows for further development. Additional validation through pathway-specific assays (Wnt/β-catenin, Notch activity) should confirm mechanism-based differential effects.
In Vivo Therapeutic Window Determination
Protocol 2: Maximum Tolerated Dose (MTD) and Efficacy Studies in PDX Models
Objective: Establish therapeutic window of ubiquitination-targeting compounds in patient-derived xenograft (PDX) models.
Materials:
- Immunocompromised mice (NSG or similar)
- Patient-derived xenograft models with characterized CSC populations
- Test compounds formulated for in vivo administration
- In vivo imaging system (IVIS) for tumor monitoring
- Tissue processing equipment for immunohistochemistry and flow cytometry
Methodology:
- Conduct dose-range finding studies in non-tumor-bearing mice to determine maximum tolerated dose (MTD) and identify dose-limiting toxicities.
- Establish PDX models with documented CSC content (by flow cytometry for CD44+/CD24-, CD133+, or ALDH+ cells).
- Randomize mice into treatment groups: vehicle control, MTD, ½ MTD, and ¼ MTD of test compound, with appropriate positive controls.
- Administer compounds via predetermined route and schedule (e.g., daily oral gavage, intermittent intravenous).
- Monitor tumor volume twice weekly and overall animal health daily.
- At study endpoint, analyze tumors for:
- CSC frequency by flow cytometry and sphere-forming assays
- Proliferation (Ki67) and apoptosis (cleaved caspase-3) markers
- Pathway modulation (nuclear β-catenin, YAP localization) by IHC
- Assess normal tissues (bone marrow, intestinal crypts) for evidence of on-target toxicity to normal stem cell compartments.
Data Interpretation: The therapeutic index is calculated as MTD / ED50 (effective dose for 50% tumor growth inhibition). Successful candidates demonstrate >50% reduction in CSC frequency with minimal toxicity to normal stem cell compartments at efficacious doses.
Research Reagent Solutions for Ubiquitination-CSC Studies
Table 3: Essential Research Tools for Investigating Ubiquitination in CSCs
| Research Tool Category | Specific Examples | Research Application | Considerations for Toxicity Studies |
|---|---|---|---|
| E1 Inhibitors | TAK-243 (MLN7243), PYR-41 | Pan-UPS inhibition controls; assess broad ubiquitination disruption | High toxicity expected; useful for establishing maximum effect boundaries |
| E2 Inhibitors | CC0651 (Cdc34-specific); Leucettamol A (Ubc13-specific) | Pathway-specific ubiquitination inhibition | Variable selectivity; assess effects on specific E2-E3 pairs important in CSCs |
| E3 Ligase Modulators | MLN4924 (NEDD8-activating enzyme inhibitor); Nutlin-3 (MDM2 inhibitor) | Targeted protein stabilization or degradation | More specific than broad UPS inhibition; evaluate tissue-specific E3 expression |
| DUB Inhibitors | b-AP15 (USP14/UCHL5); PR-619 (broad DUB inhibitor); P5091 (USP7 inhibitor) | Stabilization of ubiquitinated substrates | Emerging target class; assess effects on CSC transcription factor stability |
| CSC Functional Assays | Sphere formation kits; ALDEFLUOR kits; CSC marker antibody panels | Quantification of CSC frequency and functional properties | Essential for evaluating selective effects on CSCs vs. normal stem cells |
| Pathway Reporters | TCF/LEF luciferase reporters (Wnt); Notch luciferase reporters | Monitoring stemness pathway activity | Critical for confirming mechanism of action and selective pathway inhibition |
| Animal Models | Patient-derived xenografts; genetically engineered mouse models | In vivo therapeutic window assessment | Select models with validated CSC populations and relevant stroma interactions |
Targeting ubiquitination processes in CSCs represents a promising but challenging therapeutic approach. The strategies outlined here—including specific E3 ligase or DUB targeting, exploitation of differential pathway dependencies, rational combination therapies, and advanced delivery systems—provide frameworks for managing on-target toxicity while effectively eradicating CSCs. As our understanding of ubiquitination mechanisms in CSC biology advances, particularly through single-cell analyses and CRISPR-based functional screens, new opportunities will emerge for identifying targets with enhanced therapeutic windows. The experimental approaches described enable systematic evaluation of both efficacy and toxicity, supporting the development of ubiquitination-targeting therapies that can overcome CSC-mediated resistance while maintaining acceptable safety profiles. Success in this endeavor will require continued attention to the fundamental differences between normal and cancer stem cells, innovative approaches to compound delivery, and rigorous assessment of therapeutic windows throughout the drug development process.
The ubiquitin-proteasome system (UPS) represents a crucial regulatory mechanism for post-translational protein modification and degradation, governing diverse cellular processes from cell cycle progression to differentiation. In cancer biology, particularly in the maintenance of cancer stem cells (CSCs), the UPS exerts context-dependent influences that either suppress or promote tumorigenesis depending on specific components and cellular environments. CSCs constitute a minor subpopulation within tumors capable of self-renewal, differentiation, and driving tumor initiation, metastasis, and therapeutic resistance. The intricate balance of ubiquitination and deubiquitination processes orchestrated by UPS components serves as a critical determinant of CSC fate. This review examines two pivotal UPS components—the E3 ubiquitin ligase FBXW7 and the deubiquitinase USP14—as exemplars of the context-dependent functionality within cancer stemness regulation, highlighting their mechanistic substrates, signaling pathway influences, and emerging therapeutic implications.
FBXW7: A Tumor Suppressor in CSC Regulation
Molecular Structure and Canonical Functions
FBXW7 (F-box and WD repeat domain-containing 7) serves as the substrate recognition component of the SKP1-CUL1-F-box (SCF) E3 ubiquitin ligase complex. It targets numerous proto-oncoproteins for proteasomal degradation via recognition of phosphorylated degron motifs, establishing its role as a critical tumor suppressor [81]. Three isoforms—FBXW7α (nucleoplasmic), FBXW7β (cytoplasmic), and FBXW7γ (nucleolar)—provide subcellular compartment-specific regulation of distinct substrates [81]. The canonical function of FBXW7 depends on glycogen synthase kinase 3β (GSK3β)-mediated phosphorylation of substrates, which creates binding sites for FBXW7 recognition, leading to polyubiquitination and subsequent degradation [82] [81].
Table 1: Key Oncogenic Substrates of FBXW7
| Substrate | Role in Oncogenesis | Phosphorylation Sites | Cancer Context |
|---|---|---|---|
| c-Myc | Master transcription regulator of proliferation | Thr58, Ser62 | T-ALL, CML [81] |
| Notch1 | Regulates differentiation and stemness | Thr2512, Ser2514, Ser2517 | T-ALL [82] [81] |
| Cyclin E | Controls G1-S cell cycle transition | Thr380, Ser384 | Multiple cancers [81] |
| c-Jun | AP-1 transcription factor component | Multiple serine residues | Neural stem cells [82] |
| mTOR | Growth and metabolic regulator | Serine residues | Various cancers [81] |
| Mcl-1 | Anti-apoptotic Bcl-2 family member | Multiple sites | Hematologic malignancies [81] |
| ACTL6A | Chromatin remodeling factor | Not fully characterized | Hepatocellular carcinoma [83] |
| CHD4 | Chromatin remodeling enzyme | Not fully characterized | Triple-negative breast cancer [84] |
FBXW7 Mechanisms in Cancer Stem Cell Suppression
FBXW7 exerts tumor-suppressive functions across multiple cancer types through distinct mechanisms targeting CSC properties:
Hematopoietic Malignancies: In T-cell acute lymphoblastic leukemia (T-ALL), FBXW7 is mutated in up to 30% of cases, leading to stabilization of oncoproteins like Notch1 and c-Myc [82] [81]. FBXW7 deletion in hematopoietic stem cells (HSCs) promotes cell cycle entry and disrupts quiescence maintenance through c-Myc accumulation, though this also triggers p53-dependent apoptosis that limits leukemogenesis. Approximately 30% of Fbxw7-null mice develop rapid HSC exhaustion and pancytopenia, while those that evade this apoptotic pathway develop T-ALL [82].
Solid Tumors: In hepatocellular carcinoma (HCC), FBXW7 expression is significantly reduced and negatively correlates with invasion and migration capabilities. FBXW7 overexpression suppresses stemness properties, tumorigenicity, and sorafenib resistance by targeting the novel substrate ACTL6A, a component of chromatin remodeling complexes [83]. The ubiquitin-dependent degradation of ACTL6A by FBXW7 disrupts CSC maintenance, and ACTL6A overexpression reverses the tumor-suppressive effects of FBXW7 [83].
In triple-negative breast cancer (TNBC), FBXW7 expression is reduced and correlates positively with patient prognosis [84]. FBXW7 overexpression inhibits colony formation, migration, epithelial-mesenchymal transition (EMT), and stemness properties. Mechanistically, FBXW7 targets chromodomain-helicase-DNA-binding protein 4 (CHD4) for ubiquitin-mediated degradation, subsequently inhibiting Wnt/β-catenin pathway activation and suppressing CSC maintenance [84].
Stem Cell Differentiation: Beyond cancer, FBXW7 regulates normal stem cell differentiation. In embryonic stem cells (ESCs), Fbxw7 is maintained at low levels during self-renewal but upregulated during differentiation, where it targets c-Myc for degradation [82]. Fbxw7 knockdown during differentiation maintains self-renewal markers and inhibits differentiation [82]. Similarly, in neural stem cells, Fbxw7 deletion results in Notch1 accumulation, impaired neuronal differentiation, enhanced astroglial differentiation, and increased neurosphere formation [82].
USP14: An Oncogenic Promoter in CSC Regulation
Structural Regulation and Activation Mechanisms
Ubiquitin-specific protease 14 (USP14) belongs to the ubiquitin-specific proteases (USPs) family of deubiquitinating enzymes (DUBs) and is unique among DUBs for its association with the 19S proteasome regulatory particle [85] [86]. The full-length human USP14 contains 494 amino acids with an N-terminal ubiquitin-like (UBL) domain that regulates proteasomal activity and a C-terminal catalytic USP domain responsible for deubiquitinating activity [85].
USP14 exists in an autoinhibited state when free in the cytoplasm, with two surface loops (BL1 and BL2) partially blocking the active site cleft [85]. Proteasome binding induces conformational changes that activate USP14 by repositioning these loops to accommodate ubiquitin C-terminus access [85]. USP14 preferentially cleaves K48-linked ubiquitin chains, which typically target proteins for proteasomal degradation, thereby stabilizing substrate proteins [85] [87].
USP14 Mechanisms in Cancer Stem Cell Promotion
USP14 exhibits oncogenic functions across multiple cancer types through distinct stabilization of pro-tumorigenic factors:
Glioblastoma (GBM): USP14 is highly expressed in mesenchymal GBM stem cells (GSCs) compared to proneural GSCs and normal neural cells, with high expression correlating with poor patient prognosis [86]. USP14 knockdown impairs GSC proliferation, sphere-forming capacity, tumorigenicity, and radioresistance. Catalytically inactive USP14 (C114A) fails to rescue these phenotypes, indicating dependence on deubiquitinating activity [86].
Mechanistically, USP14 stabilizes the m6A RNA demethylase ALKBH5 by removing K48-linked ubiquitin chains, preventing its proteasomal degradation via the E3 ligase HECW2 [86]. The kinase MST4 phosphorylates ALKBH5 at serine residues 64 and 69, enhancing its interaction with USP14 and subsequent deubiquitination. This MST4-USP14-ALKBH5 signaling axis promotes homologous recombination-mediated DNA repair, stemness maintenance, and radioresistance in GSCs [86].
Gastric Cancer: USP14 is significantly upregulated in gastric cancer tissues and cell lines, with overexpression correlating with poor prognosis [87]. USP14 knockdown suppresses proliferation, migration, and invasion of gastric cancer cells. USP14 interacts with and stabilizes KPNA2, a nuclear transporter protein, by removing K48-linked ubiquitin chains [87]. This stabilization facilitates c-MYC nuclear translocation, driving oncogenic progression.
Additional Cancers: USP14 also stabilizes IDO1 in colorectal cancer, promoting immune evasion, and deubiquitinates TAZ in pancreatic ductal adenocarcinoma, creating a positive feedback loop that drives tumor progression and metastasis [86].
Table 2: Key Substrates Stabilized by USP14 in Cancer
| Substrate | Stabilization Mechanism | Functional Consequence | Cancer Context |
|---|---|---|---|
| ALKBH5 | Removes K48-linked ubiquitin chains | Enhances m6A demethylation, DNA repair, and radioresistance | Glioblastoma [86] |
| KPNA2 | Deubiquitinates via K48 linkage | Promotes c-MYC nuclear translocation | Gastric cancer [87] |
| IDO1 | Inhibits TRIM21-mediated ubiquitination | Facilitates immune evasion | Colorectal cancer [86] |
| TAZ | Removes ubiquitin chains | Enhances stemness and metastasis | Pancreatic cancer [86] |
Experimental Methodologies for Studying FBXW7 and USP14
Loss-of-Function and Gain-of-Function Approaches
Gene Manipulation: Lentiviral vectors encoding cDNA for overexpression or shRNA for knockdown represent standard approaches. For FBXW7 studies in TNBC, Flag-tagged FBXW7 constructs were generated by inserting coding sequences into lentiviral vector GV341, with stable cell lines established through puromycin selection [84]. Similarly, for USP14 studies in GBM, multiple distinct shRNA constructs were used to downregulate endogenous USP14, with rescue experiments performed by reintroducing wild-type or catalytically inactive (C114A) USP14 [86].
Functional Assays for CSC Properties:
- Sphere Formation Assay: Cells are cultured in serum-free medium supplemented with growth factors (EGF, bFGF) in low-attachment plates to assess self-renewal capability [86] [84]. Sphere number and size are quantified after 7-14 days.
- Flow Cytometry for CSC Markers: Surface markers like CD133 (HCC, GBM) or CD44/CD24 (TNBC) are detected using fluorochrome-conjugated antibodies and analyzed by flow cytometry [83] [86].
- Chemotherapy and Radiotherapy Resistance: For sorafenib resistance in HCC, cells are treated with increasing drug concentrations and viability assessed by MTT assays [83]. For radioresistance in GBM, cells are irradiated at various doses and clonogenic survival determined [86].
- In Vivo Tumorigenicity: Limiting dilution assays in immunodeficient mice evaluate tumor-initiating capacity [83] [86]. Cells are injected subcutaneously or intracranially, with tumor growth monitored and stem cell frequency calculated using extreme limiting dilution analysis (ELDA).
Molecular Interaction and Substrate Identification
Co-immunoprecipitation (Co-IP) and Mass Spectrometry: For identifying novel substrates, Co-IP is performed using antibodies against the protein of interest (FBXW7 or USP14) followed by mass spectrometric analysis of interacting proteins [83] [84] [87]. In FBXW7-CHD4 interaction studies, NP-40 lysis buffer was used for immunoprecipitation with anti-FBXW7 antibody, followed by Western blotting with anti-CHD4 antibody [84].
Ubiquitination Assays: To demonstrate direct ubiquitination, cells are co-transfected with substrates and ubiquitin plasmids, treated with proteasome inhibitor MG132 (20μM) for 4-6 hours before harvesting, and immunoprecipitation is performed under denaturing conditions to preserve ubiquitination [83] [84]. Western blotting with anti-ubiquitin antibody confirms polyubiquitination.
Protein Stability Assays: Cycloheximide (CHX) chase assays assess protein half-life. Cells are treated with protein synthesis inhibitor CHX (10-100μg/mL) and harvested at different time points for Western blot analysis [83] [84] [87]. MG132 treatment should stabilize proteins degraded via proteasome.
Signaling Pathway Visualization
FBXW7 and USP14 Regulatory Networks
Research Reagent Solutions
Table 3: Essential Research Reagents for Studying FBXW7 and USP14
| Reagent Category | Specific Examples | Research Application | Key Considerations |
|---|---|---|---|
| Inhibitors | IU1 (USP14 inhibitor) | Specifically inhibits USP14 catalytic activity | Reversible inhibitor; use at 10-100μM concentration [86] [87] |
| MG132 (proteasome inhibitor) | Blocks proteasomal degradation | Stabilizes ubiquitinated proteins; use at 10-20μM [83] [84] | |
| Cycloheximide (protein synthesis inhibitor) | Measures protein half-life | Use at 10-100μg/mL for time-course experiments [83] [84] | |
| Expression Vectors | Lentiviral vectors (GV341, GV112) | Stable overexpression or knockdown | Include puromycin selection marker; confirm efficiency by WB/qPCR [83] [84] |
| Catalytically inactive mutants (USP14 C114A) | Controls for enzyme activity dependence | Essential for rescue experiments [86] | |
| Antibodies | Anti-FBXW7 (Abcam ab109617) | Detection, IP, IHC | Distinguish isoforms when possible [83] |
| Anti-USP14 (multiple sources) | Detection, IP, IHC | Validate specificity with knockdown controls [86] [87] | |
| Anti-ubiquitin (K48-linkage specific) | Detection of specific ubiquitin chains | Critical for mechanistic studies [86] [87] | |
| Cell Culture Models | Patient-derived GSCs | Maintain stemness properties in vitro | Culture as neurospheres with EGF/FGF2 [86] |
| CSC-enriched populations | Study stemness mechanisms | Isolate via FACS (CD133+, CD44+/CD24-) or ALDH activity [83] [84] |
Discussion and Therapeutic Implications
The opposing functions of FBXW7 and USP14 in cancer stem cell regulation highlight the context-dependent nature of UPS components in tumor biology. FBXW7 serves predominantly as a tumor suppressor by targeting multiple oncoproteins for degradation, while USP14 typically exerts oncogenic functions by stabilizing cancer-promoting factors. However, both converge on critical pathways governing stemness, including Wnt/β-catenin, Notch, and c-Myc signaling.
Therapeutic targeting of these UPS components presents distinct challenges and opportunities. For FBXW7-deficient tumors, restoration of function represents an ideal approach, though pharmacologically challenging. Alternative strategies include targeting stabilized substrates like Notch1 with γ-secretase inhibitors or exploiting synthetic lethal interactions. For USP14, the specific inhibitor IU1 provides a proof-of-concept, showing enhanced radiosensitivity in GSC-derived xenografts [86]. Developing more potent and specific USP14 inhibitors represents a promising therapeutic avenue.
The opposing functions of FBXW7 and USP14 extend beyond cancer to neurodevelopmental disorders, as evidenced by FBXW7 mutations causing global developmental delay and USP14 variants associated with syndromic neurodevelopmental disorders [88] [89]. These findings underscore the critical balance of ubiquitination in stem cell fate determination and tissue development.
Future research should focus on identifying novel context-specific substrates, understanding compensatory mechanisms within the UPS network, and developing isoform-specific targeting strategies. The integration of ubiquitin-proteasome targeting with conventional chemotherapy, radiotherapy, and emerging immunotherapies may provide synergistic benefits for eradicating CSCs and overcoming treatment resistance.
FBXW7 and USP14 exemplify the context-dependent functionality of UPS components in cancer stem cell regulation. FBXW7 acts as a multi-faceted tumor suppressor by targeting key oncoproteins for degradation across diverse cancer types, while USP14 promotes tumorigenesis by stabilizing oncogenic factors. The intricate balance between these opposing forces significantly influences CSC maintenance, therapeutic resistance, and tumor progression. Understanding their mechanistic substrates, regulatory networks, and contextual dependencies provides valuable insights for developing novel therapeutic strategies aimed at targeting the ubiquitin-proteasome system in cancer and beyond.
Strategies to Counter CSC Plasticity and Adaptive Responses to UPS Inhibition
Cancer stem cells (CSCs) represent a formidable challenge in oncology due to their intrinsic plasticity, capacity for self-renewal, and role in driving tumor recurrence and therapeutic resistance. The ubiquitin-proteasome system (UPS) plays a crucial role in maintaining CSC function by regulating key stemness pathways. However, targeting the UPS in CSCs triggers adaptive survival mechanisms that limit therapeutic efficacy. This technical review examines the molecular interplay between CSC plasticity and UPS function, analyzes current strategies to overcome resistance mechanisms, and provides detailed experimental frameworks for developing next-generation therapies. We integrate the latest research on combinatorial approaches that simultaneously disrupt UPS function while blocking compensatory pathways, offering a roadmap for researchers and drug development professionals working to eradicate the CSC population in malignant diseases.
The ubiquitin-proteasome system (UPS) serves as a critical regulatory mechanism in cancer stem cell biology, governing the stability and activity of proteins essential for CSC maintenance and survival. The UPS consists of a cascade of enzymes (E1, E2, and E3) that mediate the attachment of ubiquitin chains to target proteins, marking them for degradation by the 26S proteasome [41] [90]. This system regulates virtually all cellular processes, including cell cycle progression, signal transduction, and stress response pathways.
In CSCs, the UPS exerts precise control over core stemness transcription factors (SOX2, OCT4, KLF4, c-Myc) and key signaling pathways (Notch, Wnt/β-catenin, Hedgehog) that maintain the undifferentiated, self-renewing state [9] [91]. E3 ubiquitin ligases and deubiquitinases (DUBs) function as molecular switches that determine the abundance and activity of these critical factors, making the UPS a central regulator of CSC identity [9] [43]. Dysregulation of specific UPS components has been identified as a driving force behind tumorigenesis and metastasis, positioning the UPS as a compelling therapeutic target in CSC-directed therapies [41] [9].
Mechanisms of CSC Plasticity and Adaptation to UPS Inhibition
CSC Plasticity and Heterogeneity
CSCs exhibit remarkable phenotypic plasticity, enabling them to transition between states of quiescence and proliferation, epithelial and mesenchymal characteristics, and differentiated and stem-like states [13] [92]. This plasticity is regulated by both intrinsic factors (genetic, epigenetic) and extrinsic cues from the tumor microenvironment (TME) [92] [91]. The dynamic nature of CSCs allows them to adapt to therapeutic pressures, including UPS inhibition, through multiple mechanisms:
Therapeutic-induced dedifferentiation: Non-CSCs can acquire stem-like properties in response to environmental stressors, including therapy-induced damage [92] [91]. This state transition is mediated through epigenetic reprogramming and activation of core pluripotency networks, effectively replenishing the CSC pool after therapeutic challenge.
Metabolic flexibility: CSCs can switch between glycolysis, oxidative phosphorylation, and alternative fuel sources (glutamine, fatty acids) to survive under diverse conditions, including proteotoxic stress induced by UPS impairment [13].
Interaction with the TME: Crosstalk with stromal cells, particularly tumor-associated macrophages (TAMs), myeloid-derived suppressor cells (MDSCs), and regulatory T cells (Tregs), creates a supportive niche that enhances CSC survival following UPS disruption [93] [91].
Adaptive Responses to UPS Impairment
When the UPS is compromised, CSCs activate compensatory mechanisms to maintain protein homeostasis and viability. Understanding these adaptations is crucial for designing effective combination therapies:
Autophagic induction: UPS impairment triggers upregulation of the autophagosome-lysosome pathway (ALP) as an alternative protein clearance mechanism [94]. This adaptive response involves increased expression of LC3-I/II and Beclin 1, coupled with reduced mTOR signaling, enabling cells to survive proteotoxic stress [94].
Epigenetic reprogramming: CSCs undergo rapid epigenetic modifications in response to UPS inhibition, altering chromatin accessibility and gene expression patterns to promote survival [13] [14]. These changes can stabilize the CSC state and enhance resistance mechanisms.
Enhanced DNA repair capacity: CSCs possess robust DNA damage response systems that are further activated under UPS impairment, allowing them to withstand the genomic stress associated with proteasome dysfunction [13] [14].
Metabolic rewiring: UPS inhibition alters energy requirements and nutrient utilization in CSCs, prompting shifts toward metabolic pathways that support survival under proteotoxic stress [13] [93].
Table 1: Adaptive Mechanisms of CSCs to UPS Inhibition
| Adaptive Mechanism | Key Molecular Players | Functional Consequences |
|---|---|---|
| Autophagic Induction | LC3-I/II, Beclin 1, p62/SQSTM1, mTOR | Alternative protein degradation, cell survival |
| Epigenetic Reprogramming | DNMTs, HDACs, chromatin modifiers | Altered gene expression, enhanced stemness |
| Enhanced DNA Repair | ATM, ATR, RAD51, BRCA1/2 | Genomic stability maintenance |
| Metabolic Rewiring | GLUT1, glutaminase, fatty acid synthase | Energy production, redox balance |
| Immune Evasion | PD-L1, B7-H4, MHC-I downregulation | Escape from immune surveillance |
Therapeutic Strategies to Overcome Resistance
Dual-Targeting of UPS and Compensatory Pathways
Simultaneously targeting the UPS and adaptive survival mechanisms presents a promising approach to overcome CSC resistance:
UPS and autophagy inhibition: Combining proteasome inhibitors with autophagy blockers (e.g., chloroquine, hydroxychloroquine) prevents the activation of this key compensatory pathway, leading to enhanced accumulation of toxic protein aggregates and CSC death [94].
UPS and epigenetic modulation: Co-administration of proteasome inhibitors with epigenetic drugs (DNMT inhibitors, HDAC inhibitors) blocks the reprogramming capacity of CSCs, limiting their adaptive potential [93] [14].
UPS and metabolic targeting: Dual inhibition of the proteasome and key metabolic enzymes (e.g., glutaminase with CB-839) exploits the metabolic vulnerabilities of CSCs under proteotoxic stress [93].
Advanced UPS-Targeting Modalities
Moving beyond broad proteasome inhibition to more precise strategies represents the next frontier in CSC-directed therapies:
E3 ligase-specific targeting: Rather than general proteasome inhibition, targeting specific E3 ubiquitin ligases that regulate core CSC factors offers greater precision [9] [43]. This approach minimizes off-target effects while effectively disrupting CSC maintenance.
Targeted protein degradation (TPD): Proteolysis-targeting chimaera (PROTAC) technology enables selective degradation of oncogenic proteins essential for CSC survival by hijacking the UPS machinery [41] [43]. This modality specifically targets proteins that maintain CSC identity while sparing normal cellular components.
DUB inhibition: Targeting deubiquitinating enzymes that stabilize oncogenic CSC factors provides an alternative UPS-directed approach [9] [43]. DUB inhibitors can promote the degradation of key stemness regulators, effectively compromising CSC viability.
Table 2: Therapeutic Strategies Targeting UPS and CSC Plasticity
| Therapeutic Approach | Molecular Targets | Representative Agents | Development Status |
|---|---|---|---|
| Proteasome Inhibition | 20S proteasome core | Bortezomib, Carfilzomib | FDA-approved (multiple myeloma) |
| E3 Ligase Modulation | CRL, HECT, RBR-type E3s | Experimental compounds | Preclinical development |
| PROTAC Technology | E3 ligases + oncoproteins | ARV-825, ARV-110 | Early clinical trials |
| DUB Inhibition | USP7, USP22, UCH-L1 | HBX 41-108, P5091 | Preclinical studies |
| UPS-Autophagy Dual Inhibition | Proteasome + autophagy machinery | Bortezomib + Chloroquine | Phase I/II trials |
| UPS-Epigenetic Combination | Proteasome + DNMTs/HDACs | Carfilzomib + Guadecitabine | Phase I trials |
Experimental Models and Methodologies
In Vitro Assessment of UPS Inhibition Efficacy
Protocol 1: Evaluating CSC Response to UPS Inhibition
Materials and Reagents:
- CSC-enriched cultures (grown as tumorspheres)
- Proteasome inhibitors (e.g., bortezomib, carfilzomib, MG132)
- Autophagy inhibitors (e.g., chloroquine, bafilomycin A1)
- Apoptosis detection reagents (Annexin V, propidium iodide)
- ALDEFLUOR assay kit for ALDH activity
- Western blot reagents for ubiquitinated proteins, LC3, p62, and stemness markers
Methodology:
- CSC enrichment: Culture patient-derived xenograft cells or established cancer cell lines in serum-free, growth factor-supplemented media to form tumorspheres, enriching for the CSC population [13] [91].
- Compound treatment: Treat tumorspheres with titrated concentrations of UPS inhibitors alone and in combination with autophagy inhibitors for 24-72 hours.
- Viability assessment: Measure cell viability using ATP-based assays (e.g., CellTiter-Glo) and apoptosis via Annexin V/propidium iodide staining followed by flow cytometry.
- Functional CSC analysis: Evaluate CSC frequency using ALDEFLUOR assay and tumorsphere-forming capacity in secondary passages.
- Mechanistic studies: Analyze protein extracts by Western blotting for ubiquitin conjugates, autophagy markers (LC3 conversion, p62 degradation), and stemness transcription factors (SOX2, OCT4, Nanog).
- Autophagic flux measurement: Treat parallel samples with and without lysosomal inhibitors to quantify autophagic activity following UPS impairment.
In Vivo Evaluation of Combination Therapies
Protocol 2: Assessing Therapeutic Efficacy in Preclinical Models
Materials and Reagents:
- Immunocompromised mice (NSG, NOG strains)
- Patient-derived xenograft (PDX) models or CSC-enriched cell lines
- Proteasome inhibitors (bortezomib, carfilzomib)
- Autophagy/epigenetic inhibitors (chloroquine, panobinostat)
- In vivo imaging system (IVIS) for bioluminescence tracking
- Tissue processing reagents for immunohistochemistry
Methodology:
- Model establishment: Implant luciferase-labeled PDX tumors or CSC-enriched cell lines subcutaneously or orthotopically into immunocompromised mice.
- Treatment protocol: Once tumors reach 100-150 mm³, randomize animals into treatment groups (n=8-10):
- Vehicle control
- UPS inhibitor alone
- Secondary inhibitor alone
- Combination therapy
- Drug administration: Administer compounds via appropriate routes (intraperitoneal, oral) at established maximum tolerated doses.
- Efficacy monitoring: Measure tumor dimensions 2-3 times weekly and image weekly via bioluminescence to track metastatic spread.
- Endpoint analyses: At study conclusion, harvest tumors for:
- Immunohistochemical staining of CSC markers (CD44, CD133, ALDH1)
- Western blot analysis of pathway modulation
- Tumorsphere assays to quantify residual CSC frequency
- Histopathological assessment of toxicity in normal tissues
- Serial transplantation: Implant limited numbers of cells from treated tumors into secondary recipients to assess CSC depletion by limiting dilution analysis.
Research Tools and Visualization
Essential Research Reagents
Table 3: Key Reagents for Studying UPS in CSCs
| Reagent Category | Specific Examples | Research Applications |
|---|---|---|
| Proteasome Inhibitors | Bortezomib, Carfilzomib, MG132, Lactacystin | Base UPS suppression, mechanism studies |
| Autophagy Inhibitors | Chloroquine, Bafilomycin A1, 3-Methyladenine | Block compensatory protein degradation |
| E3 Ligase Modulators | MLN4924 (NEDD8 inhibitor), PROTACs | Targeted protein degradation |
| DUB Inhibitors | P5091, HBX 41-108, PR-619 | Study ubiquitin chain stabilization |
| CSC Marker Antibodies | Anti-CD44, Anti-CD133, Anti-ALDH1 | Identify and isolate CSC populations |
| Stemness Transcription Factor Antibodies | Anti-SOX2, Anti-OCT4, Anti-Nanog | Evaluate CSC phenotype maintenance |
| Ubiquitin Detection Reagents | FK2 antibody, TUBE reagents | Measure global ubiquitination changes |
| Apoptosis Detection Kits | Annexin V, Caspase 3/7 assays | Quantify cell death mechanisms |
Signaling Pathway Visualizations
Diagram 1: CSC Adaptive Responses to UPS Inhibition and Therapeutic Countermeasures. This diagram illustrates how CSCs activate survival mechanisms (red) in response to UPS disruption (yellow) and how targeted therapies (green) can block these adaptive pathways.
Diagram 2: Experimental Workflow for Evaluating UPS-Targeting Therapies in CSCs. This diagram outlines the sequential process for evaluating UPS-directed therapies, from in vitro mechanism studies (blue) to in vivo efficacy assessment (red) and clinical translation (green).
Targeting the UPS in cancer stem cells represents a promising but complex therapeutic approach. The remarkable plasticity of CSCs and their capacity to activate compensatory survival mechanisms necessitate multi-faceted strategies that simultaneously disrupt protein homeostasis while blocking adaptive pathways. The experimental frameworks and technical approaches outlined in this review provide a roadmap for advancing this promising therapeutic paradigm.
Future progress will depend on developing more sophisticated models of CSC biology, including advanced 3D culture systems that better recapitulate the tumor microenvironment and its role in therapeutic resistance [13]. Additionally, the application of single-cell technologies to map the dynamic responses of CSCs to UPS impairment at unprecedented resolution will identify new vulnerabilities and combination therapy opportunities [13] [92]. As targeted protein degradation technologies mature, particularly PROTACs and molecular glues, we anticipate more precise approaches to dismantling the core regulatory networks that maintain CSC identity and plasticity [41] [43].
Ultimately, successfully countering CSC plasticity and adaptive responses will require temporally controlled combination therapies that preempt resistance mechanisms while exploiting the inherent vulnerabilities of CSCs under proteotoxic stress. The integration of UPS-targeting approaches with immunotherapy, metabolic intervention, and epigenetic modulation holds particular promise for achieving durable responses in advanced malignancies.
The ubiquitin system, a master regulator of protein stability and function, has emerged as a central player in oncogenesis and therapy resistance. Its role is particularly critical in the maintenance of cancer stem cells (CSCs), a subpopulation of tumor cells responsible for recurrence, metastasis, and treatment failure [9]. The ubiquitin network orchestrates CSC functionality by tightly regulating the stability of key transcription factors like SOX2, OCT4, KLF4, and c-Myc, as well as core signaling pathways such as Notch, Wnt/β-catenin, and Hedgehog [9]. Targeting this system offers a promising strategy to eradicate these resilient cells. However, the clinical success of ubiquitin-targeted therapies hinges on precise patient stratification. The inherent complexity and contextual duality of ubiquitin signaling necessitate robust biomarker-driven approaches to identify patient subgroups most likely to benefit from specific interventions, thereby ushering in a new era of precision oncology.
Scientific Rationale: Biomarkers for Ubiquitin-Targeted Therapies
The development of biomarkers for ubiquitin-targeted therapies is grounded in the molecular mechanisms of ubiquitin ligases (E3s) and deubiquitinases (DUBs). These enzymes determine the specificity of protein ubiquitination, a post-translational modification that can target a substrate for proteasomal degradation or alter its function and localization.
- Genetic Alterations in E3 Ligases and DUBs: Somatic mutations or copy number variations in genes encoding E3 ligases and DUBs can serve as direct biomarkers. A prime example is FBXW7, a tumor-suppressive E3 ligase that is frequently mutated in cancers. Its mutation status is a predictive biomarker, as tumors with wild-type FBXW7 may respond to strategies that stabilize its tumor-suppressive substrates [95].
- Substrate Protein Status: The genetic and functional status of an E3 ligase's substrate is a critical companion biomarker. The most validated example is TP53. Inhibitors of the E3 ligase MDM2 (or HDM2 in humans) are only effective in tumors that retain wild-type p53, as the therapy aims to stabilize the existing functional protein [95]. In p53-mutant cancers, this approach is ineffective.
- Ubiquitin Chain Topology: The functional outcome of ubiquitination depends on the topology of the polyubiquitin chain. K48-linked chains typically target proteins for degradation, while K63-linked chains are often involved in non-proteolytic signaling [65] [33]. The presence of specific chain types on key proteins can thus serve as a functional biomarker. For instance, K63-linked ubiquitination of GPX4 by TRIM26 stabilizes it and suppresses ferroptosis, a vulnerability that can be targeted in gliomas [65].
Key Biomarkers and Clinical Applications
The following table summarizes established and emerging biomarkers for patient stratification in ubiquitin-targeted therapy.
Table 1: Key Biomarkers for Patient Stratification in Ubiquitin-Targeted Therapy
| Biomarker Category | Specific Example | Associated Cancer Type(s) | Therapeutic Implication | Clinical/Preclinical Context |
|---|---|---|---|---|
| Tumor Suppressor Status | Wild-type TP53 status [95] | Various (e.g., leukemias, sarcomas) | Predicts response to MDM2 inhibitors | Stabilizes functional p53 to induce apoptosis [95] |
| E3 Ligase Mutation | FBXW7 mutation status [95] [65] | Colorectal cancer, others | Loss of FBXW7 function leads to accumulation of oncogenic substrates (e.g., c-Myc); dictates response to co-targeting strategies [65] | In p53-wildtype contexts, FBXW7 mutation confers radioresistance [65] |
| Ubiquitin Chain Signal | K63-linked ubiquitination of GPX4 [65] | Glioma | Biomarker for sensitivity to TRIM26 inhibition and ferroptosis inducers | TRIM26 stabilizes GPX4 via K63 chains to suppress ferroptosis [65] |
| E3/Substrate Axis | UBE3A/E6AP and HPV status [95] | Cervical cancer, Head and Neck cancer | HPV-driven UBE3A activation degrades p53; strategies to inhibit this axis are relevant | Targeted degradation of p53 in HPV+ cancers [95] |
| DUB Overexpression | USP14 overexpression [65] | Glioma, NSCLC, HNSCC | Biomarker for USP14 inhibitor sensitivity; role in stabilizing oncoproteins and maintaining CSC stemness [65] [9] | Stabilizes ALKBH5 in glioma to maintain stemness; degrades IκBα to activate NF-κB in HNSCC [65] |
Methodologies for Biomarker Discovery and Validation
The identification and validation of biomarkers require a multi-faceted experimental approach.
3.1. Genomic and Transcriptomic Profiling
- Objective: To identify genetic mutations, copy number alterations, and gene expression signatures in the ubiquitin-proteasome system associated with drug response.
- Protocol:
- NGS Panel Sequencing: Utilize targeted next-generation sequencing (NGS) panels that include genes for key E3 ligases (e.g., MDM2, FBXW7, TRIM family), DUBs, and their critical substrates (e.g., TP53, PTEN) [96].
- Whole Transcriptome Analysis: Perform RNA sequencing (RNA-Seq) on tumor and matched normal tissue to quantify differential gene expression [96] [97].
- Algorithmic Analysis: Apply machine learning algorithms, such as the Digital Display Precision Predictor (DDPP), to identify multi-gene predictors of treatment outcome. The DDPP algorithm involves: (a) selecting key genes from literature; (b) ranking them based on their correlation with progression-free survival (PFS) using Pearson correlation; and (c) building a predictor through vectorial summation of the top-ranking genes' expression [96].
3.2. Functional Proteomics for Ubiquitin Signaling
- Objective: To characterize the ubiquitin-modified proteome (ubiquitinome) and identify specific ubiquitin chain linkages involved in therapy resistance.
- Protocol:
- Ubiquitin Affinity Purification: Use tandem ubiquitin-binding entities (TUBEs) to enrich for ubiquitinated proteins from cell or tissue lysates under denaturing conditions.
- Mass Spectrometry (MS) Analysis: Digest enriched proteins and analyze them by liquid chromatography-tandem mass spectrometry (LC-MS/MS). Use di-glycine remnant (Gly-Gly) profiling to identify ubiquitination sites.
- Linkage-Specific Antibodies: Employ antibodies specific for K48-linked or K63-linked ubiquitin chains in western blotting or immunohistochemistry (IHC) to assess chain topology in patient samples [65] [33].
Diagram 1: Biomarker Discovery Workflow
The Scientist's Toolkit: Essential Research Reagents
The following table lists key reagents essential for experimental research in ubiquitin biology and biomarker validation.
Table 2: Research Reagent Solutions for Ubiquitin Biomarker Studies
| Research Reagent | Function and Application | Key Examples/Context |
|---|---|---|
| E3 Ligase Inhibitors | Small molecules that block the activity of specific E3 ligases, used to validate targets and model therapy. | MDM2 inhibitors (e.g., idasanutlin) for p53 stabilization [95]. |
| DUB Inhibitors | Small molecules that inhibit deubiquitinating enzymes, used to study the effect of stabilizing DUB substrates. | USP14 inhibitors for probing its role in radioresistance and CSC maintenance [65]. |
| PROTACs | Proteolysis-Targeting Chimeras are heterobifunctional molecules that hijack E3 ligases to degrade target proteins of interest. | EGFR-directed PROTACs to degrade β-TrCP substrates; BRD4-targeting PROTACs (MZ1) [65] [33]. |
| Linkage-Specific Ubiquitin Antibodies | Antibodies that recognize specific polyubiquitin chain linkages (e.g., K48, K63), used in WB, IHC, and ELISA. | Critical for detecting K63-ubiquitination of GPX4 or K48-ubiquitination of VDAC2 in patient samples [65] [33]. |
| Tandem Ubiquitin Binding Entities (TUBEs) | Recombinant proteins with high affinity for polyubiquitin chains, used to enrich ubiquitinated proteins from lysates for proteomics. | Essential for ubiquitinome studies to identify novel ubiquitination substrates and sites [65]. |
Integrated Signaling Pathways and Therapeutic Stratification
The complex interplay between ubiquitin enzymes and their substrates in CSCs can be visualized as an integrated network. A key pathway involves the E3 ligase FBXW7, which exhibits contextual duality based on p53 status. In p53-wild-type backgrounds, FBXW7 can promote the degradation of p53, leading to radioresistance. Therefore, FBXW7 wild-type status in a p53-wild-type tumor is a biomarker indicating potential sensitivity to MDM2/FBXW7 co-inhibition. Conversely, in a p53-null context, FBXW7 can degrade oncogenic substrates like SOX9, exerting a tumor-suppressive effect [65]. This highlights the absolute necessity of stratifying patients based on the genetic context of both the E3 and its substrate.
Diagram 2: FBXW7 Contextual Duality in Therapy
Biomarker-driven patient stratification is the cornerstone for realizing the full potential of precision ubiquitin-targeted therapies. As research continues to unravel the complexities of the ubiquitin code, particularly its role in CSC maintenance, the biomarker toolkit will expand. Future directions will involve the integration of multi-omics data through advanced machine learning models to develop composite biomarker scores that more accurately predict patient responses [96] [97]. Furthermore, the clinical translation of novel modalities like PROTACs and DUB inhibitors will be profoundly guided by biomarkers that account for the contextual duality and tissue-specific functions of ubiquitin enzymes. By rigorously applying these stratification strategies, we can selectively target the ubiquitin network in the right patient populations, moving beyond broad inhibition to precise molecular interventions that ultimately overcome therapy resistance and improve cancer outcomes.
Evidence and Evaluation: Preclinical Models and Clinical Translation of UPS Modulators
The ubiquitin-proteasome system (UPS) represents a crucial regulatory network for protein homeostasis, and its dysregulation is increasingly recognized as a fundamental mechanism in cancer stem cell (CSC) maintenance. CSCs constitute a minor subpopulation within tumors characterized by self-renewal capacity, differentiation potential, and enhanced therapy resistance, contributing significantly to tumor recurrence and metastatic spread [98] [18]. The UPS governs the stability of key transcription factors and regulatory proteins that maintain CSC stemness through precisely controlled ubiquitination and deubiquitination processes [7] [9].
Targeting specific UPS components to eliminate CSCs represents a promising therapeutic strategy to overcome conventional therapy resistance. This technical guide comprehensively examines contemporary in vitro and in vivo models used to assess the efficacy of UPS-targeting agents against CSC populations, providing detailed methodologies and analytical frameworks for researchers investigating ubiquitination in CSC maintenance.
UPS Regulation of CSC Maintenance
Molecular Mechanisms of Ubiquitination in CSC Signaling
The UPS exerts precise control over CSC maintenance through regulation of core stemness pathways. E3 ubiquitin ligases and deubiquitinating enzymes (DUBs) determine the protein stability of key transcriptional regulators including β-catenin, Twist1, SOX2, OCT4, and NANOG [99] [9]. These factors are central to the maintenance of stem-like properties and are frequently stabilized in CSCs through dysregulated ubiquitination.
Table 1: Key UPS Components Regulating CSC Maintenance
| UPS Component | Target Protein | Biological Effect in CSCs | Therapeutic Implications |
|---|---|---|---|
| USP4 | β-catenin, Twist1 | Stabilizes proteins; promotes stemness, EMT, and chemoresistance | USP4 inhibition promotes target degradation; reduces stemness [100] |
| FBXW7 | c-MYC, NOTCH | Promotes degradation of oncoproteins; tumor suppressor | Loss enhances CSC properties; restoration inhibits CSC [7] |
| β-TrCP | β-catenin, SOX2 | Regulates stemness factor degradation | Dysregulation stabilizes CSC transcription factors [7] |
| USP22 | SOX2, c-MYC | Stabilizes pluripotency factors | Overexpressed in CSCs; inhibition reduces self-renewal [9] |
| PARK2 | Multiple substrates | Mitochondrial quality control; tumor suppressor | Loss promotes CSC phenotype in multiple cancers [7] |
USP4 as a Key Regulatory Node in CSC Maintenance
Ubiquitin-specific peptidase 4 (USP4) has emerged as a critical DUB regulating CSC maintenance, particularly in colorectal cancer. USP4 directly stabilizes β-catenin and Twist1 by removing ubiquitin chains, preventing their proteasomal degradation [100]. This stabilization enhances WNT/β-catenin signaling and epithelial-mesenchymal transition (EMT), two fundamental processes in CSC maintenance. In colorectal cancer models, USP4 expression correlates strongly with chemoresistance and CSC marker expression, identifying it as a promising therapeutic target [100].
Diagram 1: USP4 regulates CSC stemness by stabilizing β-catenin and Twist1. The diagram illustrates how USP4 removes ubiquitin chains from β-catenin and Twist1, preventing their proteasomal degradation and thereby promoting cancer stemness properties and chemotherapy resistance.
In Vitro Models for Assessing UPS-Targeting Agents
CSC Enrichment and Characterization Methods
Reliable in vitro CSC models require robust enrichment strategies and validation methodologies. The most common approaches include:
Sphere Formation Assays: Culturing dissociated tumor cells in serum-free, non-adherent conditions with growth factors (EGF, bFGF) enriches for CSCs capable of anchorage-independent growth [100] [18]. These tumorspheres demonstrate self-renewal capacity upon serial passaging and express elevated levels of stemness markers including OCT4, SOX2, NANOG, and CD44/CD133 [99].
Flow Cytometry-Based CSC Isolation: Fluorescence-activated cell sorting (FACS) using established CSC surface markers (CD44, CD133, CD24, EpCAM, Lgr5) enables purification of specific CSC subpopulations [100] [18]. Multi-marker strategies (e.g., CD44+ Lgr5+ EpCAM+ in colorectal cancer) typically provide higher specificity for true CSCs [100].
Aldefluor Assay: Detection of high aldehyde dehydrogenase (ALDH) activity identifies CSCs across multiple cancer types, providing a functional enrichment method complementary to surface marker expression [18].
Experimental Protocols for UPS-Targeting Agent Evaluation
Primary Screening Protocol - Tumorsphere Formation Assay:
- Dissociate monolayer cultures of cancer cell lines (e.g., SW620, LoVo for colorectal cancer) to single-cell suspension using enzymatic digestion
- Plate 500-1000 cells/well in ultra-low attachment 24-well plates with serum-free DMEM/F12 medium supplemented with B27, 20ng/mL EGF, and 10ng/mL bFGF
- Treat with UPS-targeting compounds (e.g., USP4 inhibitor U4-I05 at nanomolar concentrations) or DMSO vehicle control
- Refresh media and compounds every 3-4 days
- Quantify spheres (>50μm diameter) after 7-14 days using automated image analysis or manual counting
- Calculate sphere formation efficiency: (number of spheres / number of cells seeded) × 100% [100]
Secondary Validation - Flow Cytometric CSC Quantification:
- Culture CSC-enriched populations as tumorspheres or in specialized media
- Treat with UPS-targeting agents for 72-96 hours
- Dissociate to single cells and stain with fluorescently-conjugated antibodies against CSC markers (e.g., CD44-APC, Lgr5-PE, EpCAM-FITC) and viability dye
- Include appropriate isotype controls for gating standardization
- Analyze using flow cytometry (minimum 10,000 events/sample) and quantify percentage of marker-positive CSC population [100]
Molecular Mechanism - Western Blot Analysis of UPS Targets:
- Lyse treated cells in RIPA buffer with protease and phosphatase inhibitors
- Resolve 20-30μg protein by SDS-PAGE and transfer to PVDF membrane
- Probe with primary antibodies against target proteins (β-catenin, Twist1), ubiquitin, and stemness transcription factors (SOX2, OCT4, NANOG)
- Use appropriate secondary antibodies and develop with enhanced chemiluminescence
- Quantify band intensity normalized to loading controls (β-actin, GAPDH) [100]
Table 2: Quantitative Effects of USP4 Inhibition in Colorectal Cancer Models
| Model System | USP4 Inhibition Method | Effect on CSC Markers | Impact on Sphere Formation | Chemosensitization |
|---|---|---|---|---|
| LoVo cells | siRNA knockdown | ~60% reduction in CD44+Lgr5+EpCAM+ cells | ~70% reduction in sphere number | Enhanced oxaliplatin sensitivity [100] |
| SW620 cells | siRNA knockdown | ~55% reduction in CD44+Lgr5+EpCAM+ cells | ~65% reduction in sphere number | Enhanced oxaliplatin sensitivity [100] |
| Patient-derived organoids | USP4 inhibitor U4-I05 | ~50% reduction in CD44 expression | ~60% reduction in organoid formation | Synergy with 5-fluorouracil [100] |
| MC38 mouse model in vivo | siRNA knockdown | N/A | N/A | ~80% reduction in tumor initiation capacity [100] |
In Vivo Models for UPS-Targeting Agent Validation
Mouse Models of Tumor Initiation and Metastasis
In vivo models provide critical assessment of UPS-targeting agents against CSCs in physiological contexts, evaluating effects on tumor initiation, metastatic potential, and therapy resistance.
Tumor Initiation Assay:
- Knock down USP4 or treat CSCs with UPS-targeting agents in vitro (e.g., 7-day pretreatment with U4-I05)
- Prepare serial dilutions of treated cells (e.g., 10³, 10⁴, 10⁵ cells) in PBS:Matrigel (1:1)
- Inject subcutaneously into immunocompromised mice (NOD/SCID or NSG)
- Monitor weekly for tumor formation; record latency period and tumor incidence
- USP4 knockdown in MC38 cells significantly impaired tumor initiation capacity, with ~80% reduction even at higher cell inoculums [100]
Orthotopic Metastasis Models:
- Establish CSCs expressing luciferase for bioluminescent tracking
- Pretreat with UPS-targeting agent or vehicle control
- Inject directly into the organ of origin (e.g., intrasplenic for liver metastasis, intracecal for colorectal cancer)
- Monitor metastatic progression weekly via bioluminescent imaging
- Quantify metastatic burden at endpoint through ex vivo organ analysis [100]
Genetic Engineered Mouse Models (GEMMs)
GEMMs enable evaluation of UPS-targeting agents in autochthonous, immunocompetent settings that recapitulate human disease progression:
- Utilize tissue-specific promoters to drive oncogene expression or tumor suppressor deletion
- Treat with UPS-targeting compounds during tumor initiation or progression phases
- Assess effects on CSC populations through flow cytometry of dissociated tumors
- Evaluate metastasis to distant organs [100]
Treatment with the USP4 inhibitor U4-I05 in a genetically engineered CRC mouse model inhibited tumor metastasis and extended survival, demonstrating the therapeutic potential of targeting USP4 [100].
Diagram 2: Integrated experimental workflow for evaluating UPS-targeting agents. The diagram outlines the complementary in vitro and in vivo models used to comprehensively assess the efficacy of UPS-targeting compounds against cancer stem cell populations.
The Scientist's Toolkit: Essential Research Reagents
Table 3: Essential Research Reagents for UPS-CSC Studies
| Reagent Category | Specific Examples | Application & Function |
|---|---|---|
| UPS-Targeting Compounds | U4-I05 (USP4 inhibitor), Bortezomib, Carfilzomib | Selective targeting of deubiquitinases or proteasome; induces degradation of CSC-maintaining proteins [41] [100] |
| CSC Surface Markers | Anti-CD44, Anti-CD133, Anti-EpCAM, Anti-Lgr5 | Identification and isolation of CSC subpopulations via flow cytometry [100] [18] |
| Stemness Transcription Factor Antibodies | Anti-OCT4, Anti-SOX2, Anti-NANOG, Anti-KLF4 | Detection of pluripotency network activation in CSCs via Western blot/immunofluorescence [99] |
| Signaling Pathway Reporter Systems | TOPFlash WNT/β-catenin reporter, Notch reporter constructs | Functional assessment of stemness pathway activity in response to UPS targeting [99] |
| Proteasome Activity Assays | Fluorogenic substrates (Suc-LLVY-AMC), LIVE Cell Proteasome Sensor | Quantification of proteasome function in live cells or lysates [41] |
| Ubiquitination Assay Reagents | HA-Ubiquitin, GST-Ubiquitin, TUBE reagents | Assessment of protein ubiquitination status; identification of UPS targets [7] |
| Patient-Derived Model Culture Systems | Tumor organoid media, Basement membrane matrix (Matrigel) | Maintenance of CSC populations in physiologically relevant 3D cultures [100] |
The strategic targeting of specific UPS components, particularly regulatory enzymes like USP4, represents a promising approach to disrupt CSC maintenance and overcome therapy resistance. The integration of complementary in vitro and in vivo models, including tumorsphere assays, patient-derived organoids, tumor initiation studies, and genetically engineered mouse models, provides a robust framework for evaluating UPS-targeting agents. These experimental systems enable comprehensive assessment of effects on CSC self-renewal, stemness pathways, and tumorigenic potential at molecular, cellular, and organismal levels. As research advances, UPS-targeted therapies in combination with conventional chemotherapy may offer enhanced efficacy against refractory cancers by addressing the fundamental role of CSCs in treatment resistance and disease recurrence.
Proteolysis-Targeting Chimeras (PROTACs) represent a transformative class of heterobifunctional small molecules that harness the body's natural ubiquitin-proteasome system (UPS) to achieve targeted protein degradation. Unlike traditional occupancy-based inhibitors that merely block protein function, PROTACs catalytically eliminate entire disease-causing proteins, offering a promising therapeutic strategy for previously "undruggable" targets, including transcription factors, scaffolding proteins, and mutant oncoproteins [101]. This targeted protein degradation (TPD) approach has created new therapeutic possibilities across multiple disease areas, with oncology serving as the primary testing ground for initial clinical applications [101].
The significance of PROTAC technology extends deeply into cancer stem cell (CSC) research, where the ubiquitin system plays a critical regulatory role. Ubiquitination governs the stability and function of key transcription factors essential for CSC maintenance and survival, including SOX2, OCT4, KLF4, and c-Myc [9]. The dysregulation of specific E3 ubiquitin ligases and deubiquitinases (DUBs) has been identified as a driving force behind tumorigenesis and metastasis, making the ubiquitin system a crucial area of investigation for developing novel anti-cancer therapies aimed at eradicating the treatment-resistant CSC subpopulation [9]. PROTACs offer the unprecedented ability to directly target and eliminate these critical regulatory proteins, potentially disrupting the mechanisms that allow CSCs to perpetuate tumor growth and evade conventional therapies.
PROTAC Mechanism and Design Principles
Molecular Mechanism of Targeted Degradation
PROTACs function through a unique event-driven pharmacological mechanism rather than traditional occupancy-based inhibition [101]. A canonical PROTAC molecule consists of three covalently linked components: a ligand that binds the protein of interest (POI), a ligand that recruits an E3 ubiquitin ligase, and a linker that bridges the two [101]. This structure enables the formation of a productive POI-PROTAC-E3 ternary complex [101].
Upon ternary complex formation, the recruited E3 ligase facilitates the transfer of ubiquitin chains to lysine residues on the target protein [101]. The specific architecture of these ubiquitin chains determines the cellular outcome, with K48-linked polyubiquitination primarily targeting proteins for proteasomal degradation [65]. Once ubiquitinated, the target protein is recognized and degraded by the 26S proteasome, while the PROTAC molecule can dissociate and catalyze additional degradation cycles, enabling sub-stoichiometric activity and potentially reducing systemic exposure requirements [101].
Critical Design Parameters for Effective PROTACs
Successful PROTAC design depends on several interdependent factors beyond simple target binding affinity:
Ternary Complex Stability: The cooperative interaction between the POI, PROTAC, and E3 ligase often proves more critical than high-affinity binding of individual components. Even weak-affinity ligands can drive potent degradation if the linker supports favorable ternary complex geometry [101].
Linker Optimization: Linker properties—including length, flexibility, polarity, and spatial orientation—directly influence the protein-protein interface and determine whether the ternary complex adopts a ubiquitination-competent conformation [101]. The linker serves as a tunable element that significantly impacts both pharmacokinetics and target selectivity [101].
E3 Ligase Selection: While CRBN- and VHL-based recruiters are most commonly used in current clinical-stage PROTACs, emerging E3 ligases such as IAPs, MDM2, and DCAF family members are being explored to enhance tissue selectivity, reduce off-target toxicity, and broaden therapeutic scope [101].
Cellular Context: Critical parameters influencing PROTAC efficacy include target protein localization, E3 ligase expression patterns, DUB activity, and the broader ubiquitin machinery present in specific cellular environments [102]. The subcellular compartment where degradation occurs can significantly impact PROTAC sensitivity and therapeutic outcomes [102].
Clinical Trial Landscape of PROTAC Therapeutics
Advanced-Stage PROTAC Clinical Candidates
The PROTAC clinical landscape has matured rapidly, with multiple candidates advancing through late-stage development. The following table summarizes the key clinical-stage PROTACs, their targets, and current development status.
Table 1: PROTACs in Clinical Trials for Cancer Therapy
| Drug Candidate | Company/Sponsor | Target | Indication | Development Status |
|---|---|---|---|---|
| Vepdegestrant (ARV-471) | Arvinas/Pfizer | Estrogen Receptor (ER) | ER+/HER2- Advanced or Metastatic Breast Cancer | Phase 3 (NDA submitted, PDUFA date: Jun 5, 2026) [103] [104] |
| BMS-986365 (CC-94676) | Bristol Myers Squibb | Androgen Receptor (AR) | Metastatic Castration-Resistant Prostate Cancer (mCRPC) | Phase 3 [105] |
| BGB-16673 | BeiGene | Bruton's Tyrosine Kinase (BTK) | Relapsed/Refractory B-cell Malignancies | Phase 3 [105] |
| ARV-110 | Arvinas | Androgen Receptor (AR) | mCRPC | Phase 2 [105] |
| ARV-766 | Arvinas/Novartis | Androgen Receptor (AR) | mCRPC | Phase 2 [105] [102] |
| KT-474 (SAR444656) | Kymera | IRAK4 | Hidradenitis Suppurativa and Atopic Dermatitis | Phase 2 [105] |
| ARV-393 | Arvinas | BCL6 | Relapsed/Refractory Non-Hodgkin Lymphoma | Phase 1 [105] [104] |
| ARV-806 | Arvinas | KRAS G12D | KRAS G12D-Mutated Solid Tumors | Phase 1 [104] |
Detailed Analysis of Key Clinical-Stage PROTACs
Vepdegestrant (ARV-471): Pioneering ER-Targeted Degradation
Vepdegestrant represents the most advanced PROTAC in clinical development and the first oral PROTAC molecule to advance into Phase 3 trials [105]. This investigational PROTAC estrogen receptor degrader is being developed as a potential monotherapy for estrogen receptor positive (ER+)/HER2- advanced or metastatic breast cancer, particularly in patients with ESR1 mutations in the second-line plus setting [103].
The pivotal VERITAC-2 Phase 3 trial (NCT05654623) demonstrated statistically significant and clinically meaningful improvement in progression-free survival (PFS) compared to fulvestrant in patients with ESR1 mutations, exceeding the target hazard ratio of 0.60 in this predefined subgroup [103] [105]. Although the trial did not reach statistical significance in the overall intent-to-treat population, the compelling activity in ESR1-mutated patients underscores the potential of vepdegestrant to address a significant unmet need in this resistant population [105]. The U.S. Food and Drug Administration (FDA) has accepted the New Drug Application (NDA) for vepdegestrant and assigned a Prescription Drug User Fee Act (PDUFA) action date of June 5, 2026 [103] [104].
Beyond monotherapy development, vepdegestrant is being evaluated in combination strategies. Ongoing studies are assessing its potential as part of combination therapy for ER+/HER2- breast cancer, including investigations with letrozole or abemaciclib in the I-SPY2 Endocrine Optimization Pilot trial [103]. Additional combination trials include a Phase 1/2 study evaluating vepdegestrant with the KAT6 inhibitor PF-07248144 in patients with ER+/HER2- locally advanced or metastatic breast cancer [103].
Androgen Receptor-Targeting PROTACs for Prostate Cancer
The androgen receptor (AR) has been a prime target for PROTAC development, with multiple candidates demonstrating clinical activity in metastatic castration-resistant prostate cancer (mCRPC):
BMS-986365 (CC-94676): As the second PROTAC to enter Phase 3 trials and the first AR-targeting PROTAC to reach this stage, BMS-986365 represents a potent ligand-directed degrader that promotes CRL4^CRBN E3 ubiquitin ligase-dependent ubiquitination and degradation of AR [105]. Preclinical data demonstrated approximately 100 times greater potency in suppressing AR-driven gene transcription compared to the AR antagonist enzalutamide, with 10- to 120-fold higher efficacy in inhibiting AR-dependent proliferation across various prostate cancer cell lines [105]. Phase 1 clinical data presented at ASCO GU 2024 showed a dose-dependent increase in the proportion of patients achieving a ≥30% decline in PSA levels (PSA30), with 55% of patients receiving the 900 mg twice-daily dose achieving PSA30 [105].
ARV-110 and ARV-766: These earlier AR-targeting PROTACs have demonstrated potent and selective degradation of their targets in preclinical models and have progressed to Phase 2 trials [102]. Both compounds have shown activity against AR variants that drive resistance to standard antagonists, highlighting a key advantage of degradation-based strategies over traditional inhibition [101].
Emerging PROTACs in Early-Stage Development
The PROTAC clinical pipeline continues to expand with novel targets and indications:
BGB-16673: This BTK-targeting PROTAC from BeiGene has advanced to Phase 3 development for relapsed/refractory B-cell malignancies, representing one of the three most advanced PROTACs in clinical testing [105].
ARV-393: An oral PROTAC BCL6 degrader being evaluated in a first-in-human Phase 1 trial in patients with non-Hodgkin lymphoma (NHL). Early data has shown multiple responses in early cohorts of both B- and T-cell lymphomas, with dose escalation ongoing as the anticipated effective exposure level has not yet been achieved [104].
ARV-806: A novel PROTAC targeting the challenging KRAS G12D mutation demonstrates the potential of TPD for addressing previously undruggable oncogenes. Preclinical data showed dose-dependent, selective, robust anti-tumor activity with regressions across models of KRAS G12D-mutant cancers, with in vitro potency approximately 25 times greater than KRAS inhibitors and 40 times greater than the leading clinical-stage degrader [104]. A Phase 1 trial in patients with solid tumors harboring KRAS G12D mutations is now underway (NCT07023731) [104].
PROTACs in Cancer Stem Cell Regulation: Mechanistic Insights
Ubiquitination Networks in Cancer Stem Cell Maintenance
The ubiquitin-proteasome system plays a fundamental role in governing the functionality of cancer stem cells (CSCs), making PROTAC technology particularly relevant for targeting this treatment-resistant cell population. Ubiquitination regulates key pathways essential for CSC maintenance and survival through several mechanisms:
Transcription Factor Stability: E3 ubiquitin ligases and deubiquitinases (DUBs) modulate the stability of core transcription factors that maintain stemness, including SOX2, OCT4, KLF4, and c-Myc [9]. The balanced regulation of these factors through ubiquitination determines their abundance and activity, directly influencing CSC self-renewal and differentiation capacity.
Signaling Pathway Modulation: The ubiquitin system regulates key developmental signaling pathways implicated in CSC maintenance, including Notch, Wnt/β-catenin, Hedgehog, and Hippo-YAP [9]. By influencing the components of these pathways, ubiquitination emerges as a powerful regulatory mechanism controlling stem-like properties in cancer cells.
Metabolic Reprogramming: CSCs exhibit distinct metabolic preferences, and the ubiquitin system plays a crucial role in regulating cancer lipid metabolism and other metabolic pathways [106]. Key enzymes in lipid synthesis, including ACLY and FASN, are regulated by ubiquitination, creating potential vulnerabilities that could be exploited through targeted degradation approaches [106].
PROTAC-Mediated Disruption of CSC Maintenance Pathways
PROTACs offer a strategic approach to disrupt CSC maintenance by targeting the core regulatory proteins that control stemness. The catalytic degradation mechanism provides distinct advantages over traditional inhibition for addressing the dynamic adaptive capabilities of CSCs:
Overcoming Adaptive Resistance: Unlike inhibitors that block specific functional domains, protein degradation removes the entire target protein, preventing compensatory signaling through alternative domains or conformational adaptations that often underlie treatment resistance in CSCs [101].
Targeting Multiple Functions: Many CSC regulators, such as c-Myc, perform pleiotropic functions through different protein domains and interaction networks. Complete degradation simultaneously eliminates all functional aspects of these proteins, potentially leading to more comprehensive disruption of CSC maintenance mechanisms [101].
Addressing Protein Overexpression: In cases where CSC survival depends on overexpression of specific anti-apoptotic or pro-survival proteins, degradation can reset the cellular balance toward apoptosis, potentially overcoming the heightened survival thresholds characteristic of CSCs [101].
Research Toolkit: Experimental Approaches for PROTAC Development
Essential Research Reagents and Methodologies
Table 2: Key Research Reagent Solutions for PROTAC Development
| Research Reagent/Category | Function and Application in PROTAC Research |
|---|---|
| E3 Ligase Ligands (VHL, CRBN, IAP, MDM2) | Recruit specific E3 ubiquitin ligase complexes to enable target ubiquitination; choice of E3 ligand influences degradation efficiency and tissue specificity [101]. |
| Target Protein Binders (Warheads) | High-affinity ligands for the protein of interest; determine target specificity and influence ternary complex formation efficiency [101]. |
| Linker Libraries | Chemical spacers connecting E3 and target ligands; optimized for length, composition, and flexibility to enable productive ternary complex formation [101]. |
| Ubiquitination Assays (in vitro) | Measure efficiency of target ubiquitination; typically employ purified E1, E2, E3 enzymes, ubiquitin, and target protein with PROTAC [101]. |
| Cellular Viability Assays | Assess functional consequences of target degradation; determine anti-proliferative effects and potency in relevant cell lines [101]. |
| Western Blot/Immunofluorescence | Quantify target protein degradation kinetics and efficiency; confirm mechanism of action and specificity in cellular models [101]. |
| Mass Spectrometry Proteomics | Evaluate global proteome changes following PROTAC treatment; assess selectivity and identify potential off-target effects [101]. |
| Ternary Complex Assays (SPR, FRET, etc.) | Measure stability and cooperativity of POI-PROTAC-E3 interactions; critical parameter predicting degradation efficiency [101]. |
Experimental Workflow for PROTAC Evaluation
A systematic approach to PROTAC development and validation involves multiple stages from initial design through mechanistic evaluation, as visualized in the following workflow:
Key Methodological Protocols
Ternary Complex Formation Analysis
Surface Plasmon Resonance (SPR) and FRET-Based Assays:
- Immobilize either the target protein or E3 ligase complex on sensor chips
- Measure binding kinetics and affinity of PROTAC-induced ternary complex formation
- Assess cooperativity by comparing binary versus ternary interactions
- Utilize varying linker lengths and compositions to optimize complex stability [101]
Degradation Kinetics and Efficiency Assessment
Time-Course Western Blot Analysis:
- Treat relevant cell lines with PROTAC compounds across a concentration range (typically 1 nM - 10 μM)
- Harvest cells at multiple time points (1-48 hours) post-treatment
- Quantify target protein levels relative to loading controls
- Calculate DC₅₀ (half-maximal degradation concentration) and Dmax (maximal degradation) values
- Assess degradation selectivity through proteomic analysis or evaluation of related protein family members [101]
Functional Consequences in Cancer Stem Cell Models
Tumor Sphere Formation Assays:
- Isolate CSCs through fluorescence-activated cell sorting (FACS) or magnetic-activated cell sorting (MACS) using established CSC surface markers
- Culture primary tumor cells or established cancer cell lines under ultra-low attachment conditions with CSC-selective media
- Treat sphere cultures with PROTAC compounds and monitor sphere formation, size, and number over 7-21 days
- Assess self-renewal capacity through serial sphere formation assays
- Evaluate stemness marker expression (SOX2, OCT4, NANOG, etc.) via qRT-PCR or immunofluorescence [9]
The clinical landscape of PROTACs has evolved rapidly from concept to late-stage clinical development in under two decades. With vepdegestrant (ARV-471) positioned as the potential first-in-class PROTAC therapeutic awaiting FDA decision in 2026, and multiple additional candidates advancing through Phase 3 and Phase 2 trials, targeted protein degradation is poised to become an established therapeutic modality [103] [105].
The unique mechanistic approach of PROTACs offers particular promise for addressing the challenges of cancer stem cell maintenance and therapeutic resistance. By catalytically eliminating key regulatory proteins rather than merely inhibiting their activity, PROTACs can potentially disrupt the complex signaling networks that maintain CSC populations and drive tumor recurrence [9]. The ongoing clinical development of PROTACs targeting critical oncogenic drivers—including ER, AR, BTK, and KRAS—will provide crucial validation of this approach and potentially establish a new paradigm for targeting the most resilient cellular populations in cancer therapy.
Future directions in PROTAC development will likely focus on expanding the E3 ligase toolbox, improving tissue-specific targeting, addressing emerging resistance mechanisms, and combining PROTACs with complementary therapeutic approaches to achieve more durable anti-cancer responses, particularly against the treatment-resistant cancer stem cell compartments that often underlie disease recurrence and metastasis [101] [9].
Targeted protein degradation (TPD) represents a paradigm shift in therapeutic strategy, moving beyond the transient inhibition offered by conventional small-molecule inhibitors to achieve complete and irreversible elimination of disease-causing proteins. This review provides a comparative analysis of proteolysis-targeting chimeras (PROTACs), molecular glues, and conventional inhibitors, with a specific focus on their mechanisms, applications, and potential to disrupt the ubiquitin-mediated pathways critical for cancer stem cell (CSC) maintenance. By examining the distinct pharmacological profiles of each modality, we aim to guide researchers in selecting and developing appropriate therapeutic strategies to target the previously "undruggable" proteome, with particular emphasis on overcoming therapy resistance rooted in CSC populations.
The ubiquitin-proteasome system (UPS) is a highly regulated cellular pathway responsible for maintaining protein homeostasis, governing the degradation of approximately 80-90% of cellular proteins [3]. This process involves a coordinated enzymatic cascade where ubiquitin-activating (E1), conjugating (E2), and ligase (E3) enzymes work in concert to tag specific proteins with ubiquitin chains, marking them for destruction by the 26S proteasome [3] [107]. The dysregulation of this system is a hallmark of various cancers, underscoring the therapeutic potential of targeting ubiquitination pathways.
Within the realm of oncology, CSCs represent a subpopulation of cells with self-renewal capacity and pluripotency that are inherently linked to tumor initiation, dissemination, relapse, and drug resistance [9] [108]. The maintenance and survival of CSCs are regulated by key transcription factors including SOX2, OCT4, KLF4, and c-Myc, as well as signaling pathways such as Notch, Wnt/β-catenin, and Hedgehog [9]. These proteins and pathways are predominantly controlled through ubiquitination, presenting a critical vulnerability that can be therapeutically exploited [9].
Traditional small-molecule inhibitors, which operate on an "occupancy-driven" model, have demonstrated limited success against these challenging targets due to their transient effects and requirement for well-defined binding pockets [109] [52]. In contrast, TPD strategies, including PROTACs and molecular glues, leverage the cell's intrinsic degradation machinery to catalytically remove target proteins, offering a promising approach to eradicate CSCs and overcome therapeutic resistance [109] [52].
Conventional Small-Molecule Inhibitors
Conventional small-molecule inhibitors represent the traditional approach in pharmacology, functioning primarily through an "occupancy-driven" model [51]. These molecules are designed to bind directly to the active sites or allosteric pockets of target proteins, thereby transiently suppressing their activity [109]. This approach requires sustained, often high, dosing regimens to maintain therapeutic efficacy due to the reversible nature of the binding [109]. A significant limitation is that many disease-causing proteins, particularly non-enzymatic scaffolding proteins and transcription factors, lack well-defined ligand-binding pockets, rendering them "undruggable" by conventional means [109] [107]. Furthermore, even when effective binding occurs, these inhibitors may fail to completely abolish all pathological functions of the target protein, leading to residual activity and potential compensatory mechanisms that limit therapeutic outcomes [109].
PROTACs: Catalytic Protein Degraders
PROTACs (Proteolysis-Targeting Chimeras) are heterobifunctional molecules that represent a novel "event-driven" therapeutic modality [51]. These compounds consist of three distinct components: a target protein-binding ligand, an E3 ubiquitin ligase-recruiting ligand, and a chemical linker that connects these two moieties [51]. The mechanism of action involves the simultaneous binding of the PROTAC to both the protein of interest (POI) and an E3 ubiquitin ligase, forming a ternary complex that brings the POI into proximity with the ubiquitination machinery [109] [51]. This forced proximity facilitates the transfer of ubiquitin chains to the POI, marking it for recognition and degradation by the 26S proteasome [51].
A key advantage of PROTACs is their catalytic nature; after facilitating the ubiquitination and degradation of one target molecule, the PROTAC is released and can engage additional POI molecules, enabling potent protein depletion at sub-stoichiometric concentrations [109] [51]. This catalytic mode confers significant advantages in potency and dosing frequency compared to conventional inhibitors [109]. However, PROTAC activity is highly dependent on linker design, requiring careful optimization to balance ternary complex stability, minimize off-target effects, and maintain favorable pharmacokinetic properties [109].
Molecular Glues: Induced-Proximity Degraders
Molecular glues are monovalent small molecules that induce targeted protein degradation through a distinct mechanism from PROTACs [109] [110]. These compounds typically function by binding to a specific surface on an E3 ubiquitin ligase or its substrate receptor, inducing conformational changes or creating a "neosurface" that becomes complementary to a particular protein of interest [109] [51]. This surface remodeling facilitates novel protein-protein interactions that would not otherwise occur, effectively "gluing" the E3 ligase and the target protein together into a stable ternary complex [109].
Unlike the rational design approach possible with PROTACs, molecular glues have historically been discovered serendipitously, with thalidomide and its analogs (lenalidomide, pomalidomide) serving as prototypical examples [109]. These immunomodulatory drugs (IMiDs) function by binding to the E3 ligase cereblon (CRBN) and reprogramming its substrate specificity to target specific transcription factors (IKZF1, IKZF3) for degradation [109] [111]. Molecular glues are characterized by their lower molecular weight and simpler chemical structure compared to PROTACs, which often translates to improved pharmacokinetic properties, including better cell permeability and potential for blood-brain barrier penetration [51].
Comparative Pharmacological Profiles
Table 1: Comparative Analysis of Therapeutic Modalities
| Feature | Conventional Inhibitors | PROTACs | Molecular Glues |
|---|---|---|---|
| Molecular Mechanism | Occupancy-driven inhibition | Event-driven degradation | Event-driven degradation |
| Molecular Weight | Low (typically <500 Da) | High (typically 700-1200 Da) [51] | Low (typically <500 Da) [51] |
| Structural Features | Single binding moiety | Heterobifunctional + linker [51] | Monovalent [109] |
| Pharmacological Mode | Stoichiometric | Catalytic [109] [51] | Catalytic [109] [51] |
| Target Scope | Proteins with defined binding pockets | Greatly expanded ("undruggable" targets) [109] | Expanded, but discovery challenging [109] |
| Duration of Effect | Transient (requires sustained exposure) | Prolonged (substoichiometric activity) [109] | Prolonged (substoichiometric activity) [109] |
| Oral Bioavailability | Generally favorable | Often challenging [51] | Generally improved [51] |
| BBB Penetration | Target-dependent | More challenging [51] | Generally better [51] |
| Hook Effect | Not applicable | Yes (at high concentrations) [51] | No [51] |
| Resistance Mechanisms | Target mutations, overexpression | E3 ligase downregulation, mutations [51] | E3 ligase alterations, mutation [51] |
Table 2: Clinical-Stage TPD Candidates in Oncology
| Compound | Modality | Target | E3 Ligase | Indication | Development Phase |
|---|---|---|---|---|---|
| ARV-110 (Bavdegalutamide) | PROTAC | Androgen Receptor (AR) [3] [51] | Not specified | Metastatic Castration-Resistant Prostate Cancer [3] [51] | Phase II [3] |
| ARV-471 (Vepdegestrant) | PROTAC | Estrogen Receptor (ER) [3] [51] | Not specified | Breast Cancer [3] [51] | Phase II [3] |
| CC-90009 | Molecular Glue | GSPT1 [3] | CRL4CRBN [3] | Leukemia [3] | Phase II [3] |
| KT-253 | PROTAC | MDM2 [52] | MDM2 [52] | Hematologic Malignancies | Phase I [52] |
Targeting Cancer Stem Cells through Ubiquitination Pathways
Ubiquitin-Mediated Regulation of CSC Maintenance
Cancer stem cells possess unique molecular dependencies that make them particularly vulnerable to targeted protein degradation approaches. The core transcription factors governing stemness and pluripotency—including SOX2, OCT4, KLF4, and c-Myc—are tightly regulated through ubiquitin-mediated degradation pathways [9]. In normal cellular contexts, this regulation maintains appropriate stem cell populations, but in CSCs, dysregulation of these pathways contributes to their persistence and therapy resistance.
The E3 ubiquitin ligases and deubiquitinases (DUBs) that modulate these transcription factors represent critical intervention points for CSC-directed therapies [9]. For instance, the E3 ligase complexes CRL4CRBN and CRL2VHL, which are hijacked by molecular glues and PROTACs respectively, can be redirected to target CSC maintenance factors that are otherwise recalcitrant to conventional inhibition [109] [107]. This approach offers the potential to directly eliminate the cells responsible for tumor recurrence and metastasis.
Key Signaling Pathways in CSCs Amenable to TPD
Multiple developmental signaling pathways that maintain CSC populations are regulated through ubiquitination, making them prime targets for degradation-based approaches:
Wnt/β-catenin Pathway: The stability of β-catenin, a central transcriptional co-activator in this pathway, is controlled by a destruction complex that targets it for ubiquitination and proteasomal degradation [3] [9]. Dysregulation of this process is common in CSCs, and targeted degradation of β-catenin or pathway components could suppress stemness.
Notch Signaling: Notch intracellular domain (NICD) stability and activity are regulated by ubiquitin-mediated processes [9] [108]. As Notch signaling maintains the undifferentiated state of CSCs in various cancers, including triple-negative breast cancer, its targeted degradation represents a promising therapeutic strategy.
Hedgehog Pathway: Components of the Hedgehog signaling cascade, including GLI transcription factors, undergo ubiquitin-mediated regulation [9] [108]. Targeting these factors for degradation could disrupt a critical self-renewal pathway in CSCs.
MYC Oncoproteins: c-MYC and other MYC family proteins are notoriously difficult to target with conventional inhibitors but are regulated through ubiquitin-mediated degradation [9]. Both PROTACs and molecular glues offer potential strategies to directly target these pivotal CSC regulators.
Experimental Protocols for TPD Research
Assessing Degradation Efficiency and Kinetics
Purpose: To quantitatively measure target protein degradation over time and determine degrader potency (DC50) and maximum degradation efficacy (Dmax).
Procedure:
- Cell Treatment: Plate appropriate cancer cells (e.g., multiple myeloma cells for IMiDs, prostate cancer cells for AR-targeting PROTACs) in multi-well plates and allow to adhere overnight.
- Compound Administration: Treat cells with a concentration gradient of PROTAC or molecular glue degraders (typically ranging from 1 nM to 10 μM) alongside appropriate vehicle controls.
- Time-Course Sampling: Harvest cells at multiple time points (e.g., 2, 4, 8, 12, 24, 48 hours) post-treatment to assess kinetic profile.
- Protein Extraction and Quantification: Lyse cells, quantify total protein content, and perform Western blot analysis for target protein.
- Normalization and Analysis: Normalize target protein levels to housekeeping controls (e.g., GAPDH, actin) and plot degradation curves to calculate DC50 and Dmax values using appropriate software (e.g., GraphPad Prism).
- Validation: Confirm degradation mechanism through rescue experiments with proteasome inhibitors (e.g., MG132) or E1 ubiquitin-activating enzyme inhibitors (e.g., TAK-243) [109] [52].
Key Considerations: Include controls for potential off-target effects by assessing related protein family members. Monitor for "hook effect" in PROTAC treatments by including high concentration points (≥10 μM) [51].
Ternary Complex Formation Assays
Purpose: To demonstrate and characterize the formation of ternary complexes between E3 ligase, degrader, and target protein.
Procedure:
- Surface Plasmon Resonance (SPR):
- Immobilize E3 ligase complex (e.g., CRBN-DDB1) on sensor chip.
- Pre-incubate target protein with varying concentrations of degrader molecule.
- Inject pre-formed complexes over immobilized E3 ligase surface.
- Measure binding responses and calculate affinity constants for ternary complex formation [109].
Cellular Thermal Shift Assay (CETSA):
- Treat cells with degrader compounds or vehicle control.
- Heat cell lysates or intact cells to different temperatures (e.g., 37-65°C).
- Separate soluble protein and detect target protein and E3 ligase stability shifts by Western blot.
- Stabilization indicates compound engagement and potential complex formation [52].
Co-immunoprecipitation (Co-IP):
Global Proteomics for Selectivity Profiling
Purpose: To comprehensively assess degrader selectivity and identify potential off-target effects across the proteome.
Procedure:
- Sample Preparation:
- Treat cells with degraders at multiple concentrations (including DC50 and 10× DC50) for 6-24 hours.
- Include vehicle controls and compound-negative controls (e.g., target-binding incompetent analogs).
- Harvest cells, lyse, and digest proteins using trypsin.
Mass Spectrometry Analysis:
- Perform quantitative proteomics using data-independent acquisition (DIA) mass spectrometry.
- Label-free quantitation or isobaric tagging (TMT, iTRAQ) can be employed.
- Analyze 5,000-10,000 proteins per sample for comprehensive coverage.
Data Analysis:
- Normalize protein abundance across samples.
- Identify significantly changed proteins (p < 0.05, fold change > 2).
- Exclude proteins that change in negative control treatments.
- Validate key off-target hits by Western blot [51].
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Research Reagents for TPD Studies
| Reagent/Category | Specific Examples | Application/Function |
|---|---|---|
| E3 Ligase Ligands | VHL ligands [52], CRBN ligands (e.g., pomalidomide) [109], MDM2 ligands (e.g., Nutlin-3) [52] | Recruit specific E3 ubiquitin ligase complexes for targeted degradation |
| Target Protein Binders | Kinase inhibitors, BET bromodomain inhibitors, AR/ER antagonists [52] | Provide target binding moiety for PROTAC design; determine target engagement |
| Linker Chemistry | PEG chains, alkyl chains, piperazine-based linkers [109] | Connect E3 and target ligands in PROTACs; optimize ternary complex formation |
| Proteasome Inhibitors | MG132, bortezomib, carfilzomib [9] | Validate UPS-dependent degradation mechanism; rescue experiments |
| Ubiquitination System Inhibitors | TAK-243 (E1 inhibitor) [52] | Confirm ubiquitin cascade dependency in degradation mechanism |
| CSC Model Systems | Patient-derived xenografts, sphere-forming assays [9] [108] | Evaluate efficacy against therapy-resistant cancer stem cell populations |
| Proteomics Platforms | DIA mass spectrometry, TMT/iTRAQ labeling [51] | Global assessment of degradation selectivity and off-target effects |
| Structural Biology Tools | X-ray crystallography, Cryo-EM [109] | Elucidate ternary complex structures for rational degrader design |
Future Perspectives and Clinical Implications
The field of targeted protein degradation continues to evolve rapidly, with several promising directions emerging for cancer therapy, particularly in targeting CSCs. Future developments will likely focus on expanding the repertoire of E3 ligases beyond the currently utilized CRBN, VHL, MDM2, and IAP families [107]. With over 600 E3 ligases in the human genome, tissue-specific or tumor-selective ligases could enable more precise targeting with reduced off-tissue effects [107]. Additionally, the combination of TPD agents with conventional chemotherapy, immunotherapy, and targeted agents represents a promising strategy to overcome the therapeutic resistance mediated by CSCs [9].
Emerging technologies such as lysosome-targeting degraders (e.g., LYTACs, AUTACs) and bifunctional modulators that recruit E3 ligases to extracellular or membrane-bound proteins are expanding the reach of TPD beyond the intracellular proteome [110]. Furthermore, advances in computational modeling, artificial intelligence, and structure-based drug design are progressively overcoming the historical challenges in degrader discovery, particularly for molecular glues [109] [51].
In the context of CSC-targeted therapies, the ability of TPD modalities to simultaneously degrade multiple components of stemness pathways or key transcription factors provides a unique advantage over single-target inhibitors. This multi-faceted approach may be necessary to completely eradicate the resilient CSC populations that drive tumor recurrence and metastasis. As clinical validation of PROTACs and molecular glues progresses, their integration into cancer treatment paradigms, particularly for targeting the CSC niche, holds tremendous promise for improving long-term patient outcomes in aggressive and therapy-resistant cancers.
PROTACs and molecular glues represent a transformative advance in therapeutic strategy, moving beyond the limitations of conventional occupancy-driven inhibitors to achieve catalytic degradation of disease-causing proteins. While PROTACs offer a more rational design approach for targeting specific proteins of interest, molecular glues provide advantages in size and drug-like properties. Both modalities demonstrate particular promise in targeting the ubiquitin-dependent regulatory pathways that maintain cancer stem cell populations, offering potential solutions to the challenges of therapy resistance and tumor recurrence. As research in this field advances, the strategic application of these degradation technologies, guided by comprehensive mechanistic understanding and rigorous selectivity profiling, will undoubtedly expand the therapeutic landscape for cancer treatment and beyond.
Ubiquitination-Related Gene Signatures as Prognostic and Predictive Biomarkers in Cancers
The ubiquitin-proteasome system represents a complex and highly regulated post-translational modification network that governs virtually all cellular processes in eukaryotic cells. Recent advances in bioinformatics and high-throughput technologies have revealed that ubiquitination-related gene (URG) signatures provide powerful prognostic and predictive biomarkers across diverse cancer types. This technical review synthesizes current methodologies for developing URG signatures, summarizes validated multi-gene panels for major malignancies, and delineates their clinical utility in predicting patient survival, therapeutic response, and tumor microenvironment characteristics. Furthermore, we frame these findings within the context of cancer stem cell maintenance, where ubiquitination dynamics regulate key pathways governing self-renewal and differentiation. The comprehensive analysis presented herein establishes URG signatures as indispensable tools for advancing personalized cancer medicine.
Ubiquitination is an essential post-translational modification process involving the covalent attachment of ubiquitin, a 76-amino acid protein, to target substrates through a sequential enzymatic cascade involving E1 activating, E2 conjugating, and E3 ligase enzymes [112] [113]. The human genome encodes approximately 40 E2 enzymes and at least 600 E3 ligases, which collectively regulate thousands of protein substrates through diverse ubiquitin chain topologies [112]. The specificity of ubiquitin signaling is mediated through distinct chain linkages (K48, K63, K11, etc.), with K48-linked chains primarily targeting proteins for proteasomal degradation while K63 linkages facilitate non-proteolytic signaling complexes [65] [112]. The ubiquitin system exhibits remarkable plasticity in cancer cells, where altered expression of ubiquitination enzymes reprograms critical oncogenic and tumor suppressive pathways. Mounting evidence establishes that ubiquitination plays a pivotal role in cancer stem cell (CSC) maintenance through regulation of self-renewal pathways, DNA damage response, metabolic adaptation, and drug efflux mechanisms. The dynamic reversibility of ubiquitination, mediated by deubiquitinating enzymes (DUBs), creates a regulatory network that CSCs exploit to maintain plasticity and withstand therapeutic stress [65].
Methodological Framework for URG Signature Development
Data Acquisition and Preprocessing
The construction of URG signatures begins with comprehensive data acquisition from publicly available repositories. Standard practice involves obtaining transcriptomic data and corresponding clinical information from The Cancer Genome Atlas (TCGA) and Gene Expression Omnibus (GEO) databases [114] [115] [116]. Ubiquitination-related gene sets are typically compiled from specialized databases such as iUUCD 2.0, MSigDB, or GeneCards, with relevance score thresholds applied to filter high-confidence URGs [115] [117] [118]. Data preprocessing includes quality control, normalization (e.g., FPKM, TPM), and filtering of samples with survival time less than 3 months to avoid perioperative mortality bias [115].
Identification of Prognostic URGs
Differential expression analysis between tumor and normal tissues identifies ubiquitination-related DEGs using established R packages (limma) with criteria typically set at |log2FC| > 1-2 and FDR < 0.05 [114] [117]. Survival-associated URGs are identified through univariate Cox regression analysis. Machine learning approaches, particularly Least Absolute Shrinkage and Selection Operator (LASSO) Cox regression, are then applied to select the most informative genes for signature development while preventing overfitting [114] [115] [119]. The LASSO algorithm employs ten-fold cross-validation to determine the optimal penalty parameter (λ) that minimizes cross-validation error [114] [117]. Complementary approaches include Random Survival Forests, which provide variable importance metrics for feature selection [115] [117].
Risk Model Construction and Validation
Risk scores are calculated using the formula: Risk score = Σ(βi * Expi), where β represents the coefficient from multivariate Cox regression and Exp denotes gene expression level [114] [115] [118]. Patients are stratified into high-risk and low-risk groups based on the median risk score. Model performance is validated through Kaplan-Meier survival analysis, time-dependent receiver operating characteristic (ROC) curves, and decision curve analysis [115] [119] [118]. External validation across multiple independent cohorts is essential to demonstrate robustness [115] [119]. Additional validation may include single-cell RNA sequencing analysis to examine URG distribution across cell types [114] [116] and experimental confirmation using reverse transcription quantitative polymerase chain reaction (RT-qPCR) in clinical specimens [115] [117] [118].
Figure 1: Bioinformatics workflow for developing ubiquitination-related gene signatures
Validated URG Signatures Across Cancer Types
Comprehensive studies have established cancer-type specific URG signatures with prognostic utility. The table below summarizes validated multi-gene signatures across major malignancies.
Table 1: Validated Ubiquitination-Related Gene Signatures in Human Cancers
| Cancer Type | Key URG Signature Genes | Prognostic Value | Biological Pathways | Citation |
|---|---|---|---|---|
| Diffuse Large B-Cell Lymphoma | CDC34, FZR1, OTULIN | Elevated CDC34/FZR1 + low OTULIN = poor prognosis | Endocytosis, T-cell signaling, drug sensitivity | [114] |
| Lung Adenocarcinoma | DTL, UBE2S, CISH, STC1 | High risk = worse prognosis (HR=0.54, CI:0.39-0.73) | Immune infiltration, PD1/L1 expression | [115] |
| Breast Cancer | ATG5, FBXL20, DTX4, BIRC3, TRIM45, WDR78 | Significant survival differences (p<0.05) | Tumor microenvironment, microbial diversity | [119] |
| Sarcoma | CALR, CASP3, BCL10, PSMD7, PSMD10 | Low-risk = better prognosis | Cell cycle, focal adhesion, ECM-receptor interaction | [116] |
| Hepatocellular Carcinoma | CYP26B1, MCM10, SPINK4, TRIM54 | High risk = poor survival | Cell cycle, cancer-related miRNAs | [118] |
| Ovarian Cancer | TOP2A, MYLIP | Significant survival difference | Ion channels, neuroactive ligand-receptor interactions | [120] |
| Crohn's Disease | UBE2R2, NEDD4L | Diagnostic efficacy | Autophagy, Wnt signaling, lysosome pathways | [117] |
URG Signatures in Cancer Stem Cell Maintenance
Within the context of cancer stem cell biology, ubiquitination networks regulate core pathways governing self-renewal and therapeutic resistance. In glioblastoma, USP14 stabilizes ALKBH5 to maintain stemness properties, while in breast cancer, FBXW7-mediated degradation of SOX9 relieves p21 repression, impacting CSC populations [65]. The TRIM family proteins, including TRIM26 and TRIM21, employ K63-linked ubiquitination to stabilize GPX4 and suppress ferroptosis—a regulated cell death process particularly relevant to CSC survival under oxidative stress [65]. Additionally, the OTUB1-GPX4 axis stabilizes GPX4 to suppress ferroptosis in gastric cancer, potentially contributing to CSC maintenance [65]. URG signatures effectively capture these regulatory dynamics, providing readouts of CSC activity within tumors. Single-cell transcriptomic analyses have revealed profound intratumoral heterogeneity in the expression of ubiquitin ligases and DUBs, uncovering distinct therapy-resistant subpopulations with stem-like properties [65].
Figure 2: Ubiquitination networks regulating cancer stem cell properties
Technical Implementation and Research Toolkit
Experimental Protocols for URG Signature Validation
Ubiquitinated Proteome Profiling Using Mass Spectrometry
Comprehensive analysis of ubiquitination patterns employs anti-ubiquitin antibody-based label-free quantitative proteomics. The standard protocol involves: (1) Protein extraction from tumor and control tissues; (2) Trypsin digestion to generate peptides; (3) Enrichment of ubiquitinated peptides using anti-K-ε-GG antibody immunoaffinity purification; (4) Liquid chromatography-tandem mass spectrometry (LC-MS/MS) analysis; (5) Database searching and ubiquitination site identification using MaxQuant algorithms; (6) Quantification of ubiquitination levels based on spectral counts or label-free intensity measurements [112] [113]. The GG remnant on modified lysine residues creates a distinct mass shift (114.04 Da) that enables precise localization of ubiquitylation sites based on peptide fragmentation patterns [113].
Single-Cell RNA Sequencing for URG Expression Analysis
Single-cell analysis of URG expression follows this workflow: (1) Tissue dissociation and single-cell suspension preparation; (2) Cell viability assessment (>80% required); (3) Library preparation using 10x Genomics platform; (4) Sequencing on Illumina platform to depth of 50,000 reads/cell; (5) Data processing using Seurat package in R with quality control filtering (cells with <200 or >6,000 genes excluded); (6) Dimensionality reduction using t-distributed stochastic neighbor embedding (t-SNE) or UMAP; (7) Cell clustering and annotation using SingleR package and manual curation; (8) Analysis of URG expression distribution across cell types [114].
Essential Research Reagents and Computational Tools
Table 2: Research Reagent Solutions for URG Signature Studies
| Category | Specific Tool/Reagent | Application | Key Features |
|---|---|---|---|
| Bioinformatics Packages | Limma R package | Differential expression analysis | Fold change >2, FDR <0.05 [114] [115] |
| ConsensusClusterPlus | Molecular subtyping | Unsupervised clustering, 1000 repetitions [114] [118] | |
| glmnet package | LASSO Cox regression | Feature selection, ten-fold cross-validation [114] [117] | |
| CIBERSORT | Immune cell infiltration | Leukocyte signature matrix [114] [118] | |
| oncoPredict R package | Drug sensitivity prediction | IC50 calculation for 198 drugs [114] | |
| Experimental Assays | Anti-K-ε-GG antibody | Ubiquitinated peptide enrichment | Specific to diglycine remnant [113] |
| SYBR Green Real-time PCR Master Mix | RT-qPCR validation | URG expression confirmation [117] [118] | |
| Single-cell RNA sequencing | Cellular heterogeneity analysis | 10x Genomics platform [114] | |
| Database Resources | TCGA database | Multi-omics cancer data | Clinical, genomic, transcriptomic data [115] [118] |
| GEO database | Expression datasets | Independent validation cohorts [114] [115] | |
| iUUCD 2.0 database | Ubiquitination-related genes | E1, E2, E3 enzyme catalog [115] | |
| STRING database | Protein-protein interactions | PPI network construction [117] [116] |
Clinical Applications and Therapeutic Implications
URG signatures demonstrate significant clinical utility in predicting immunotherapy response across multiple cancer types. In lung adenocarcinoma, high URRS groups showed elevated PD1/L1 expression levels (p<0.05), higher tumor mutation burden (p<0.001), and increased tumor neoantigen load (p<0.001), suggesting enhanced responsiveness to immune checkpoint inhibitors [115]. Similarly, in sarcoma, high-risk patients were identified as potential beneficiaries of immune checkpoint inhibitor therapy [116]. URG signatures also predict response to conventional chemotherapy, with distinct IC50 values for various chemotherapeutic agents observed between high-risk and low-risk groups in hepatocellular carcinoma [118].
The integration of URG signatures with CSC biology opens new avenues for therapeutic intervention. PROTACs (proteolysis-targeting chimeras) represent a promising class of therapeutics that exploit the ubiquitin system for targeted protein degradation. EGFR-directed PROTACs selectively degrade β-TrCP substrates in EGFR-dependent tumors, suppressing DNA repair while minimizing impact on normal tissues [65]. Radiation-responsive PROTAC platforms, including radiotherapy-triggered PROTAC (RT-PROTAC) prodrugs activated by tumor-localized X-rays, demonstrate synergistic effects with radiotherapy in breast cancer models [65]. These approaches specifically target the ubiquitination networks that maintain CSC populations, potentially overcoming therapy resistance.
URG signatures have emerged as robust prognostic and predictive biomarkers across diverse malignancies, providing insights into tumor biology that extend beyond conventional clinicopathological features. The integration of these signatures with cancer stem cell research illuminates the molecular mechanisms underlying therapy resistance and tumor recurrence. Future research directions should focus on single-cell ubiquitinome profiling to resolve cellular heterogeneity, development of URG-based liquid biopsies for non-invasive monitoring, and combinatorial therapeutic strategies that simultaneously target multiple nodes of ubiquitination networks in CSCs. As our understanding of ubiquitination dynamics in cancer deepens, URG signatures will increasingly guide clinical decision-making and therapeutic development, ultimately advancing precision oncology.
Cancer Stem Cells (CSCs) represent a subpopulation within tumors characterized by their ability to self-renew, differentiate into constitutive tumor cells, and drive tumor initiation, metastasis, and recurrence. Mounting evidence identifies CSCs as the primary instigators of therapeutic resistance in cancer treatments. Conventional therapies proficiently target proliferating cells but often fail to eradicate quiescent CSCs, explaining the perplexing phenomenon of tumor recurrence despite initial treatment success. CSCs typically constitute around 1% of total cells in various malignancies, but this proportion can escalate to approximately 30% in metastatic sites, correlating with heightened treatment resistance. Their resilience stems from multiple mechanisms, including enhanced expression of drug efflux transporters, epigenetic modifications, and interactions with the tumor microenvironment.
The regulation of CSC maintenance involves intricate signaling networks and post-translational modifications, with ubiquitination emerging as a central governing mechanism. Ubiquitination, a fundamental post-translational modification, precisely controls protein stability, functionality, and degradation, thereby regulating key transcription factors and signaling pathways essential for CSC self-renewal and survival. The ubiquitin-proteasome system (UPS) comprises a cascade of enzymes—E1 activating enzymes, E2 conjugating enzymes, and E3 ubiquitin ligases—alongside deubiquitinases (DUBs) that reverse this process. Dysregulation of specific E3 ligases and DUBs has been identified as a critical driver of tumorigenesis and CSC maintenance, presenting promising therapeutic targets for overcoming drug resistance.
Functional Genomics Approaches for Target Identification
Genome-Wide CRISPR Screening in Primary Cells
Functional genomics approaches, particularly genome-wide CRISPR screens, have revolutionized the identification of genetic regulators of CSC therapy resistance. These screens enable systematic interrogation of gene function across the entire genome in relevant biological contexts. Recent advances have demonstrated the feasibility of performing multiple genome-wide CRISPR screens directly in primary human immune cells, such as natural killer (NK) cells, to identify critical checkpoints regulating resistance to immunosuppressive pressures within the tumor microenvironment.
The experimental workflow involves transducing primary cells with a genome-wide lentiviral CRISPR library, followed by selection and application of specific functional or survival pressures relevant to CSC biology. For instance, screens can be designed to identify genes whose loss enhances cell survival under chemotherapeutic stress or enriches for CSC populations after treatment. One such screen identified MED12, ARIH2, and CCNC as critical regulators whose ablation significantly improved NK cell antitumor activity against multiple treatment-refractory human cancers both in vitro and in vivo. The validation process requires a multi-step approach confirming that genetic ablation of identified targets genuinely enhances therapeutic efficacy against resistant CSC populations.
Table: Key Genetic Targets Identified via CRISPR Screening in Therapy-Resistant Models
| Target Gene | Biological Function | Impact on Therapy Resistance | Validation Models |
|---|---|---|---|
| MED12 | Transcriptional regulation | Enhanced antitumor activity | Primary human NK cells, in vivo xenografts |
| ARIH2 | E3 ubiquitin ligase | Overcame immunosuppression | Refractory solid tumors |
| CCNC | Cell cycle regulation | Improved metabolic fitness | CAR-NK cell therapies |
| PKMYT1 | Kinase regulating β-catenin | Stabilized β-catenin, enhanced CSC self-renewal | Non-small cell lung cancer |
| TRIM21 | E3 ubiquitin ligase | Regulated OCT1 stability, modulated cancer stemness | Colorectal cancer |
Experimental Protocol: Genome-Wide CRISPR Screen
Materials and Reagents:
- Genome-wide lentiviral CRISPR library (e.g., Brunello or GeCKO v2)
- Primary human NK cells or patient-derived CSCs
- Polybrene (8 μg/mL)
- Puromycin (selection marker)
- Flow cytometry antibodies for CSC markers (CD44, CD133, ALDH)
- Cell culture media with appropriate cytokines (IL-2, IL-15)
Methodology:
- Library Amplification and Titering: Amplify the CRISPR library in E. coli to maintain representation and determine viral titer using HEK293T cells.
- Cell Transduction: Seed primary cells at optimal density (0.5-1×10^6 cells/mL) and transduce with lentiviral library at MOI 0.3-0.5 in the presence of polybrene using spinfection (1000×g, 32°C, 60 minutes).
- Selection and Expansion: After 24 hours, replace media and begin puromycin selection (1-2 μg/mL) for 5-7 days to eliminate non-transduced cells.
- Application of Selective Pressure: Split transduced cells into experimental arms—untreated control versus chemotherapeutic agent at IC90 concentration—for 14-21 days, maintaining cell coverage of >500x library representation throughout.
- Genomic DNA Extraction and Sequencing: Harvest cells and extract genomic DNA using QIAamp DNA Blood Maxi Kit. Amplify integrated sgRNA sequences via PCR with barcoded primers for multiplexing and sequence on Illumina platform.
- Bioinformatic Analysis: Align sequences to reference library, count sgRNA reads, and identify significantly enriched/depleted guides using MAGeCK or BAGEL algorithms.
Diagram 1: CRISPR Screening Workflow. The schematic outlines the key steps in a functional genomics screen for identifying genetic regulators of therapy resistance.
Ubiquitination in Cancer Stem Cell Regulation
Ubiquitin-Proteasome System in CSC Maintenance
The ubiquitin-proteasome system (UPS) constitutes a sophisticated regulatory network that governs protein stability and functionality, playing an indispensable role in maintaining CSC properties. Ubiquitination involves a sequential enzymatic cascade: E1 activating enzymes initiate the process by forming a thioester bond with ubiquitin in an ATP-dependent manner; E2 conjugating enzymes then carry the activated ubiquitin; finally, E3 ubiquitin ligases facilitate the transfer of ubiquitin to specific substrate proteins. This system exhibits remarkable specificity, with humans encoding approximately 600 E3 ligases that recognize distinct substrates, thereby enabling precise control over protein fate.
The UPS regulates core transcription factors essential for CSC maintenance, including SOX2, OCT4, KLF4, and c-MYC. Quantitative proteomics analyses have revealed discernible differences in ubiquitination levels between pluripotent and differentiated stem cells, with core transcription factors identified as direct ubiquitination targets. For instance, the CSN6-TRIM21 axis drives cancer stemness during tumorigenesis by stabilizing OCT1 through down-regulation of TRIM21 E3 ubiquitin ligase activity, consequently heightening aldehyde dehydrogenase 1A1 expression and modulating colorectal cancer stemness. Similarly, PKMYT1 physically interacts with β-catenin, stabilizing the β-catenin protein and activating Wnt signaling, thereby bolstering non-small cell lung cancer CSC self-renewal.
Table: Key Ubiquitination Components Regulating CSC Pathways
| Ubiquitin System Component | Type | Target/Pathway | Role in CSCs |
|---|---|---|---|
| TRIM21 | E3 Ubiquitin Ligase | OCT1 | Regulates stemness in colorectal cancer |
| β-TrCP | E3 Ubiquitin Ligase | β-catenin (Wnt pathway) | Controls self-renewal capacity |
| CSN6 | COP9 Signalosome Subunit | TRIM21 regulation | Enhances stemness by stabilizing OCT1 |
| PKMYT1 | Kinase (Regulates Ubiquitination) | β-catenin stabilization | Promotes CSC self-renewal in NSCLC |
| USP22 | Deubiquitinase | Multiple substrates | Maintains stem cell properties |
Ubiquitination in Key CSC Signaling Pathways
Ubiquitination serves as a critical regulatory mechanism across all major signaling pathways that govern CSC biology. The Wnt/β-catenin pathway is precisely controlled by ubiquitination, with β-catenin degradation mediated by a destruction complex containing GSK3β, CK1, AXIN, and APC. When Wnt signaling is inactive, β-catenin is phosphorylated and targeted for ubiquitination by β-TrCP, leading to its proteasomal degradation. In CSCs, various mechanisms disrupt this regulatory process, resulting in stabilized β-catenin that translocates to the nucleus and activates transcription of genes promoting self-renewal.
Similarly, the Notch, Hedgehog, and Hippo-YAP pathways—all crucial for CSC maintenance—are extensively regulated by ubiquitination. Notch intracellular domain (NICD) stability is controlled by ubiquitin-mediated degradation, while Hedgehog signaling involves ubiquitination of Gli transcription factors. The Hippo-YAP pathway, which regulates organ size and stem cell proliferation, is similarly modulated by ubiquitination events that control the stability of pathway components. The intricate involvement of ubiquitination across these diverse pathways highlights its fundamental role as a central processing unit coordinating CSC signaling networks.
Diagram 2: Ubiquitination Regulates Core CSC Pathways. The diagram illustrates how ubiquitination controls key signaling pathways essential for cancer stem cell maintenance.
Target Validation and Therapeutic Translation
Functional Validation of CRISPR-Idenfied Targets
Following initial identification through CRISPR screens, potential targets require rigorous validation to confirm their role in CSC therapy resistance. Validation employs a multi-faceted approach combining genetic, biochemical, and functional assays. For targets identified in immune cells like NK cells, validation includes assessing both innate and CAR-mediated antitumor function, metabolic fitness, proinflammatory cytokine secretion, and expansion of cytotoxic cell subsets. For targets directly validated in CSCs, researchers employ sphere-forming assays, in vivo limiting dilution transplantation, and drug resistance profiling.
The validation pipeline for MED12, ARIH2, and CCNC exemplifies this comprehensive approach. Ablation of these targets significantly improved NK cell antitumor activity against multiple treatment-refractory human cancers in vitro and in vivo. CRISPR editing augmented both innate and CAR-mediated NK cell function, associated with enhanced metabolic fitness, increased secretion of proinflammatory cytokines, and expansion of cytotoxic NK cell subsets. For targets involving ubiquitination pathways, validation must include demonstration of direct effects on protein stability of known CSC regulators, assessment of E3 ligase or DUB activity, and evaluation of downstream pathway modulation.
Experimental Protocol: Target Validation in CSCs
Materials and Reagents:
- Patient-derived CSC cultures or established CSC lines
- Lentiviral or retroviral constructs for shRNA/CRISPR-mediated gene knockdown/knockout
- Antibodies for Western blot (target protein, ubiquitin, CSC markers)
- Proteasome inhibitor (MG132, 10μM)
- Cycloheximide (100μg/mL) for protein stability assays
- Flow cytometry antibodies for ALDH activity and surface markers
Methodology:
- Genetic Modulation: Transduce CSCs with lentiviral vectors encoding CRISPR-Cas9/sgRNA complexes or shRNAs targeting candidate genes. Include non-targeting controls.
- Sphere Formation Assay: Seed 500-1000 cells/well in ultra-low attachment plates with serum-free media supplemented with EGF (20ng/mL) and bFGF (10ng/mL). Count spheres >50μm after 7-14 days.
- Drug Sensitivity Profiling: Treat engineered CSCs with gradient concentrations of relevant chemotherapeutics for 72 hours. Assess viability using CellTiter-Glo 3D assay.
- Protein Stability Assay: Treat cells with cycloheximide to inhibit new protein synthesis. Harvest cells at 0, 2, 4, and 8 hours. Analyze target protein levels by Western blotting. Repeat in presence of MG132 to confirm ubiquitin-proteasome dependence.
- In Vivo Limiting Dilution Transplantation: Serially dilute engineered CSCs (from 10^5 to 10^2 cells) and transplant into immunodeficient mice (NOD/SCID/IL2Rγ-/-). Monitor tumor formation for 12-16 weeks. Calculate CSC frequency using ELDA software.
- Co-immunoprecipitation: Lysate cells in RIPA buffer with protease inhibitors. Incubate with target protein antibody overnight at 4°C. Pull down complexes with protein A/G beads, wash, and elute. Analyze by Western blotting for ubiquitin and interacting partners.
Therapeutic Development and Combination Strategies
The ultimate goal of target validation is therapeutic development. For ubiquitination-related targets, several strategies exist: small molecule inhibitors of specific E3 ligases or DUBs; proteolysis-targeting chimeras (PROTACs) that hijack the ubiquitin system to degrade target proteins; and combination therapies with existing treatments. Existing proteasome inhibitors, such as bortezomib and carfilzomib, have shown promise in certain cancers but lack specificity for CSCs. More targeted approaches focusing on specific E3 ligases or DUBs could pave the way for more precise and effective cancer treatments.
Combining ubiquitination-targeted therapies with conventional chemotherapy, immunotherapy, and other targeted drugs represents a promising frontier in oncological treatment strategies. For instance, targeting MED12 or ARIH2 in adoptive cell therapies could enhance persistence and function in the immunosuppressive tumor microenvironment. Similarly, combining CSC-specific ubiquitination modulators with standard chemotherapy could address both bulk tumor cells and the therapy-resistant CSC population, potentially preventing recurrence and metastasis.
Table: Research Reagent Solutions for CSC Target Validation
| Research Tool | Type | Function in Validation | Example Applications |
|---|---|---|---|
| Genome-wide CRISPR Libraries | Lentiviral Pool | Unbiased identification of genetic regulators | KO library screens under therapeutic pressure |
| Patient-derived CSC Models | Primary Cells | Biologically relevant validation system | Functional assays with clinical relevance |
| Proteasome Inhibitors (MG132) | Small Molecule | Confirms ubiquitin-dependent degradation | Protein stability assays |
| ALDEFLUOR Assay | Fluorescent Substrate | Identifies and isolates CSCs | Flow cytometry-based CSC enumeration |
| Sphere Formation Assay | Functional Assay | Measures self-renewal capacity | In vitro assessment of stemness |
| In Vivo Limiting Dilution | Animal Model | Quantifies tumor-initiating frequency | Gold standard for CSC validation |
| Ubiquitin Binding Modules | Affinity Reagents | Detects and purifies ubiquitinated proteins | Ubiquitination status assessment |
The integration of functional genomics approaches, particularly genome-wide CRISPR screens, with our growing understanding of ubiquitination mechanisms in CSC regulation provides a powerful framework for identifying and validating novel therapeutic targets. This synergistic approach has already yielded promising candidates such as MED12, ARIH2, and CCNC that enhance cell-based therapies, as well as ubiquitination components like TRIM21 and associated regulators that directly impact CSC maintenance. The continued refinement of CRISPR screening methodologies in relevant primary cell models, coupled with advanced mechanistic studies of ubiquitination pathways, will accelerate the discovery of transformative therapeutic strategies to overcome therapy resistance in cancer stem cells.
Conclusion
The intricate regulation of CSCs by the ubiquitin system presents a formidable yet promising frontier in oncology. This synthesis underscores that targeting specific E3 ligases, DUBs, and employing novel degradation technologies like PROTACs can effectively disrupt the core stemness machinery and signaling pathways that sustain CSCs. Future research must prioritize overcoming the challenges of redundancy, toxicity, and CSC plasticity through biomarker-guided, combinatorial approaches. Advancing our understanding of the 'ubiquitin code' in CSCs will be instrumental in translating these insights into next-generation therapies that prevent tumor recurrence and metastasis, ultimately improving long-term patient outcomes.
References
- 1. The Multifaceted Role of the Ubiquitin in... Proteasome System [https://pmc.ncbi.nlm.nih.gov/articles/PMC9313328/]
- 2. The ubiquitin system: from cell signalling to disease ... [https://www.nature.com/articles/s41418-020-00703-w]
- 3. Ubiquitination and deubiquitination in cancer [https://molecular-cancer.biomedcentral.com/articles/10.1186/s12943-024-02046-3]
- 4. The emerging role of E ligases and 3 in... ubiquitin deubiquitinases [https://translational-medicine.biomedcentral.com/articles/10.1186/s12967-025-06255-2]
- 5. Key roles of ubiquitination in regulating critical regulators of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11875185/]
- 6. The role of ubiquitin - proteasome (UPS) in asthma pathology system [https://www.dovepress.com/the-role-of-ubiquitin-proteasome-system-ups-in-asthma-pathology-peer-reviewed-fulltext-article-JAA]
- 7. Ubiquitination in cancer: mechanisms and therapeutic ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12479132/]
- 8. Targeting the ubiquitin-proteasome system and drug ... [https://pubmed.ncbi.nlm.nih.gov/40844830/]
- 9. The role of ubiquitination in cancer stem cell regulation [https://ecancer.org/en/news/26126-the-role-of-ubiquitination-in-cancer-stem-cell-regulation]
- 10. Key roles of ubiquitination in regulating critical ... [https://www.sciencedirect.com/science/article/pii/S2352304224001089]
- 11. The role and mechanism of cancer in breast... stem cells [https://pubmed.ncbi.nlm.nih.gov/41139464/]
- 12. Cancer stem cells: Bridging microenvironmental interactions ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12264091/]
- 13. Cancer stem cells: landscape, challenges and emerging ... [https://www.nature.com/articles/s41392-025-02360-2]
- 14. Cancer stem cell mechanisms and targeted therapeutic ... [https://www.sciencedirect.com/science/article/pii/S0304383525005853]
- 15. Beyond tumorigenesis: cancer in stem cells metastasis [https://www.nature.com/articles/7310118?error=cookies_not_supported&code=441ce1e7-7532-46fa-a256-55ac8d632f17]
- 16. Epithelial-to-mesenchymal transition (EMT) and cancer ... metastasis [https://molecular-cancer.biomedcentral.com/articles/10.1186/s12943-025-02338-2]
- 17. : New insights in Biomarkers, Cancer Targets and... Stem Cells Drug [https://www.frontiersin.org/research-topics/45100/cancer-stem-cells-new-insights-in-biomarkers-drug-targets-and-therapeutics/magazine]
- 18. Cancer stem cells: advances in knowledge and ... [https://www.nature.com/articles/s41392-024-01851-y]
- 19. Transcriptional regulation of cancer stem cell: regulatory ... [https://jeccr.biomedcentral.com/articles/10.1186/s13046-024-03021-y]
- 20. The Role and Specific Mechanism of OCT4 in Cancer Stem ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7691851/]
- 21. E3 ubiquitin ligases in cancer stem cells - PubMed Central - NIH [https://pmc.ncbi.nlm.nih.gov/articles/PMC10910623/]
- 22. Regulation of cancer stem cells by RING finger ubiquitin ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4923516/]
- 23. The involvement of E3 ubiquitin ligases in the development ... [https://www.nature.com/articles/s41420-023-01760-z]
- 24. Unlocking the Role of OCT4 in Cancer Lineage Plasticity [https://www.mdpi.com/2227-9059/13/7/1642]
- 25. Protein Degradation by E3 Ubiquitin Ligases in Cancer Stem ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8870109/]
- 26. DUBs Activating the Hedgehog Signaling Pathway [https://pmc.ncbi.nlm.nih.gov/articles/PMC7352588/]
- 27. Deubiquitinating Enzyme-Mediated Signaling Networks in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7694198/]
- 28. Notch signaling pathway in cancer: from mechanistic ... [https://www.nature.com/articles/s41392-024-01828-x]
- 29. Regulation of Wnt Signaling through Ubiquitination and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7311976/]
- 30. Wnt/β-catenin signalling: function, biological mechanisms ... [https://www.nature.com/articles/s41392-021-00762-6]
- 31. Targeting ubiquitin-specific peptidase 22 (USP22) as a ... [https://pubmed.ncbi.nlm.nih.gov/40847643/]
- 32. in Stem growth, progression... | Nature Reviews cell fate cancer Cancer [https://www.nature.com/articles/s41568-018-0056-x?error=cookies_not_supported&code=f852929d-7747-49f4-b1e0-9f372a202f3d]
- 33. Decoding the ubiquitin network: molecular mechanisms and... [https://molecular-cancer.biomedcentral.com/articles/10.1186/s12943-025-02433-4]
- 34. K63-Linked Ubiquitination in Kinase Activation and Cancer [https://pmc.ncbi.nlm.nih.gov/articles/PMC3355940/]
- 35. Frontiers | K -Linked 63 in Kinase Activation and Ubiquitination Cancer [https://www.frontiersin.org/journals/oncology/articles/10.3389/fonc.2012.00005/full]
- 36. K48- and K63-linked ubiquitin chain interactome reveals ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11109483/]
- 37. of Monoubiquitination Marker CD133 at Lysine... Cancer Stem Cell [https://pmc.ncbi.nlm.nih.gov/articles/PMC6048314/]
- 38. Assembly and Function of Heterotypic Ubiquitin Chains in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5669814/]
- 39. Emerging functions of branched ubiquitin chains [https://www.nature.com/articles/s41421-020-00237-y]
- 40. Review Assembly and function of branched ubiquitin chains [https://www.sciencedirect.com/science/article/abs/pii/S0968000422000883]
- 41. Targeting the Ubiquitin–Proteasome System for Cancer - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC12495026/]
- 42. Carfilzomib: A Promising Proteasome Inhibitor for the ... [https://www.frontiersin.org/journals/oncology/articles/10.3389/fonc.2021.740796/full]
- 43. Targeting the ubiquitin proteasome system in cancer stem ... [https://www.sciencedirect.com/science/article/abs/pii/S0962892424002538]
- 44. Bortezomib in cancer therapy: Mechanisms, side effects ... [https://www.sciencedirect.com/science/article/pii/S002432052400715X]
- 45. Bortezomib exerts its anti-cancer activity through ... - Nature [https://www.nature.com/articles/s41420-024-01992-7]
- 46. A new era in cancer therapy: targeting the Proteasome-Bcl ... [https://jeccr.biomedcentral.com/articles/10.1186/s13046-025-03505-5]
- 47. Bortezomib Augments Natural Killer Cell Targeting of Stem ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6356940/]
- 48. Carfilzomib-specific proteasome β5/β2 inhibition drives ... [https://www.sciencedirect.com/science/article/pii/S2589004225014890]
- 49. Carfilzomib inhibits the proliferation and apoptosis of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8841661/]
- 50. Design and development of PROTACs: A new paradigm in ... [https://www.sciencedirect.com/science/article/pii/S2590098625000181]
- 51. Targeted Protein Degradation with PROTACs and ... [https://blog.crownbio.com/targeted-protein-degradation-with-protacs-and-molecular-glues]
- 52. Targeted protein degradation: advances in drug discovery ... [https://www.nature.com/articles/s41392-024-02004-x]
- 53. Recent Advances in the Development of Pro-PROTAC for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12473374/]
- 54. The “three body solution”: Structural insights into molecular ... [https://www.sciencedirect.com/science/article/pii/S0959440X25000259]
- 55. Regulatory role of E3 ubiquitin ligases in multiple myeloma [https://pmc.ncbi.nlm.nih.gov/articles/PMC12343653/]
- 56. E3 ubiquitin ligases in signaling, disease, and therapeutics [https://www.sciencedirect.com/science/article/pii/S0968000425001860]
- 57. Selective ubiquitination of drug-like small molecules by the ... [https://www.nature.com/articles/s41467-025-63442-x]
- 58. Recent advances in small molecule inhibitors of ... [https://www.sciencedirect.com/science/article/abs/pii/S0223523425000893]
- 59. Deubiquitinating Enzymes in Osteoarthritis: From Mechanisms ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12488074/]
- 60. The multifaceted roles of deubiquitinating enzymes (DUBs) ... [https://www.nature.com/articles/s41419-025-08052-7]
- 61. Recent advances in small molecule inhibitors of ... [https://pubmed.ncbi.nlm.nih.gov/39908798/]
- 62. Five Small Biotechs to Watch: June 2025 [https://www.pharmasalmanac.com/articles/five-small-biotechs-to-watch-june-2025]
- 63. Nanomaterials targeting cancer stem cells to overcome drug ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12178904/]
- 64. The advancement of ubiquitination regulation in apoptosis ... [https://www.sciencedirect.com/science/article/abs/pii/S0003986125002103]
- 65. Decoding the ubiquitin network: molecular mechanisms and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12492556/]
- 66. Experts Forecast Cancer Research and Treatment ... [https://www.aacr.org/blog/2025/01/10/experts-forecast-cancer-research-and-treatment-advances-in-2025/]
- 67. Targeting the Ubiquitin System in Glioblastoma - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC7724090/]
- 68. Targeted protein degradation technologies: Emerging ... [https://www.sciopen.com/article/10.26599/NR.2025.94907983]
- 69. Nanotechnology‐Driven Drug Delivery Systems for Lung Cancer [https://pmc.ncbi.nlm.nih.gov/articles/PMC12274165/]
- 70. Novel PROTAC probes targeting KDM3 degradation to eliminate... [https://pubs.rsc.org/en/content/articlehtml/2024/md/d4md00122b]
- 71. Nanoparticle-based targeted delivery unleashes the full ... [https://www.uchicagomedicine.org/forefront/cancer-articles/2025/may/nanoparticle-based-targeted-delivery-unleashes-the-full-power-of-anti-cancer-drugs]
- 72. Developments in nanotechnology approaches for the ... [https://ehoonline.biomedcentral.com/articles/10.1186/s40164-025-00656-1]
- 73. Nanotechnology in oncology: advances in biosynthesis, ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12182552/]
- 74. Ubiquitin and Ubiquitin-Like Protein Resources [https://www.cellsignal.com/pathways/by-research-area/ubiquitin-protein-resources-pathways?srsltid=AfmBOopA0N0oCjSyhjdqYG5YjHCnRTXdpttcmSTflMmu8nBoVZytpsTm]
- 75. Ubiquitin [https://en.wikipedia.org/wiki/Ubiquitin]
- 76. Unveiling the future of cancer stem cell therapy [https://pmc.ncbi.nlm.nih.gov/articles/PMC11929669/]
- 77. The cross talk of ubiquitination and chemotherapy tolerance in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10960765/]
- 78. Targeting Cancer Stem Cells: A Strategy for Effective ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6562442/]
- 79. Therapeutic potential of natural compounds in targeting ... [https://link.springer.com/article/10.1007/s12672-025-03190-y]
- 80. Targeting Cancer Stem Cells: Therapeutic and diagnostic ... [https://www.sciencedirect.com/science/article/abs/pii/S016836592200342X]
- 81. FBXW7: a critical tumor suppressor of human cancers [https://molecular-cancer.biomedcentral.com/articles/10.1186/s12943-018-0857-2]
- 82. Emerging roles for the FBXW7 ubiquitin ligase in leukemia ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4687017/]
- 83. FBXW7 Reduces the Cancer Stem Cell-Like Properties of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9492413/]
- 84. Fbxw7 suppresses carcinogenesis and stemness in triple ... [https://translational-medicine.biomedcentral.com/articles/10.1186/s12967-024-04897-2]
- 85. USP14: Structure, Function, and Target Inhibition - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC8766727/]
- 86. USP14 modulates stem-like properties, tumorigenicity, and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11840735/]
- 87. The deubiquitination enzyme USP14 promotes ... [https://www.nature.com/articles/s41419-025-08065-2]
- 88. Article Biallelic USP14 variants cause a syndromic ... [https://www.sciencedirect.com/science/article/pii/S1098360024000534]
- 89. Case report: A novel FBXW7 gene variant causes global ... [https://www.frontiersin.org/journals/genetics/articles/10.3389/fgene.2024.1436462/full]
- 90. The Ubiquitin-Proteasome System: Potential Therapeutic ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4727241/]
- 91. Biology of stem cell paradox: a double-edged sword ... [https://cancerci.biomedcentral.com/articles/10.1186/s12935-025-03981-x]
- 92. Cancer cell plasticity and therapeutic resistance [https://pmc.ncbi.nlm.nih.gov/articles/PMC12465352/]
- 93. Targeting CSC-immune cell crosstalk to overcome ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12325370/]
- 94. Adaptive changes in autophagy after UPS impairment ... [https://pubmed.ncbi.nlm.nih.gov/23503475/]
- 95. A Perspective on Therapeutic Targeting Against Ubiquitin ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11853300/]
- 96. Digital Display Precision Predictor: the prototype of a ... [https://www.nature.com/articles/s41698-021-00171-6]
- 97. Machine learning-driven multi-targeted drug discovery in ... [https://www.nature.com/articles/s41698-025-01058-6]
- 98. Biology of stem cell paradox: a double-edged sword ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12560468/]
- 99. Transcriptional regulation of cancer stem cell - PubMed Central [https://pmc.ncbi.nlm.nih.gov/articles/PMC10986082/]
- 100. A novel USP4 inhibitor that suppresses colorectal cancer ... [https://translational-medicine.biomedcentral.com/articles/10.1186/s12967-024-06001-0]
- 101. Proteolysis‐Targeting Chimera (PROTAC) - PubMed Central [https://pmc.ncbi.nlm.nih.gov/articles/PMC12495453/]
- 102. Cellular parameters shaping pathways of targeted protein ... [https://www.nature.com/articles/s42003-025-08104-w]
- 103. Press Release Details [https://ir.arvinas.com/news-releases/news-release-details/arvinas-announces-data-presentations-vepdegestrant-arv-471]
- 104. Arvinas Reports Third Quarter 2025 Financial Results and ... [https://ir.arvinas.com/news-releases/news-release-details/arvinas-reports-third-quarter-2025-financial-results-and]
- 105. PROTAC Degraders in Clinical Trails: 2025 Update [https://www.biochempeg.com/article/434.html]
- 106. The role of ubiquitination and deubiquitination in cancer ... [https://www.frontiersin.org/journals/oncology/articles/10.3389/fonc.2025.1464914/full]
- 107. Advancing targeted protein degradation for cancer therapy [https://pmc.ncbi.nlm.nih.gov/articles/PMC8463487/]
- 108. Translational drugs targeting cancer stem cells in triple- ... [https://www.sciencedirect.com/science/article/pii/S2950329925000773]
- 109. Review Molecular glues and PROTACs in targeted protein ... [https://www.sciencedirect.com/science/article/abs/pii/S0006295225005623]
- 110. Molecular glue-mediated targeted protein degradation [https://www.sciencedirect.com/science/article/pii/S2589004224019370]
- 111. PROTAC targeted protein degraders: the past is prologue [https://www.nature.com/articles/s41573-021-00371-6]
- 112. Quantitative proteomics to decipher ubiquitin signaling - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC3498854/]
- 113. Quantitative Analysis of Ubiquitinated Proteins in Human ... [https://www.frontiersin.org/journals/endocrinology/articles/10.3389/fendo.2019.00328/full]
- 114. A novel ubiquitination-based molecular signature predicts ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12619766/]
- 115. Construction of ubiquitination-related risk model for ... [https://www.nature.com/articles/s41598-025-92177-4]
- 116. Integration of ubiquitination-related genes in predictive ... [https://www.frontiersin.org/journals/oncology/articles/10.3389/fonc.2024.1446522/full]
- 117. Identification of ubiquitination-related key biomarkers and ... [https://www.nature.com/articles/s41598-025-88148-4]
- 118. Prognostic implication and immunotherapy response ... [https://www.aging-us.com/article/205926/text]
- 119. Construction and validation of a ubiquitination-related ... [https://www.sciencedirect.com/science/article/pii/S2405844024115848]
- 120. Identification of ubiquitin markers for survival and ... [https://www.sciencedirect.com/science/article/pii/S2405844024133191]