Ubiquitination Patterns in Cancer: From Molecular Mechanisms to Clinical Applications in Biomarker and Therapy Development
This comprehensive review synthesizes current research on dysregulated ubiquitination patterns in cancer versus normal tissues, exploring their profound implications for tumor biology and clinical practice.
Ubiquitination Patterns in Cancer: From Molecular Mechanisms to Clinical Applications in Biomarker and Therapy Development
Abstract
This comprehensive review synthesizes current research on dysregulated ubiquitination patterns in cancer versus normal tissues, exploring their profound implications for tumor biology and clinical practice. It examines foundational mechanisms by which ubiquitination drives oncogenesis, details advanced methodologies for profiling the cancer ubiquitinome, analyzes challenges in therapeutic targeting, and evaluates clinical validation strategies for ubiquitination-based biomarkers. By integrating findings from recent pancancer analyses and tissue-specific studies, this article provides researchers and drug development professionals with a critical resource for understanding ubiquitination as a dynamic regulatory layer in cancer, highlighting its emerging role in prognostic stratification, immunotherapy response prediction, and the development of novel targeted therapies like PROTACs.
The Ubiquitin Code in Malignancy: Decoding Cancer-Specific Patterns and Biological Consequences
The ubiquitin system represents a crucial post-translational modification pathway that maintains cellular homeostasis by regulating the stability, activity, and localization of a vast array of intracellular proteins [1]. This system encompasses a coordinated enzymatic cascade that conjugates the small protein ubiquitin to substrate proteins, thereby generating a complex "ubiquitin code" that dictates diverse cellular outcomes [2]. The process is highly reversible, with deubiquitinating enzymes (DUBs) counterbalancing ubiquitination to ensure dynamic regulation [3]. While initially recognized for its role in targeting proteins for degradation via the proteasome, the ubiquitin system is now known to govern virtually all aspects of cellular function, including cell cycle progression, DNA repair, immune response, and signal transduction [4]. Notably, dysregulation of this finely tuned system is increasingly implicated in human pathologies, particularly in cancer, where mutations in ubiquitination pathway genes contribute to tumorigenesis, immune evasion, and therapeutic resistance [5] [6]. This technical guide examines the core components of the ubiquitination machinery—E1, E2, E3 enzymes, and DUBs—with emphasis on their mechanisms, interactions, and relevance to oncogenic processes.
The Ubiquitination Cascade: E1, E2, and E3 Enzymes
Fundamental Mechanism
Protein ubiquitination occurs through a sequential, ATP-dependent enzymatic cascade comprising three distinct steps catalyzed by ubiquitin-activating (E1), ubiquitin-conjugating (E2), and ubiquitin-ligase (E3) enzymes [4]. This process initiates with ubiquitin activation, followed by conjugation, and culminates in ligation to specific substrate proteins.
Table 1: Core Enzymes in the Ubiquitination Cascade
| Enzyme Type | Key Function | Representative Family Members | Catalytic Mechanism |
|---|---|---|---|
| E1 (Activating) | Activates ubiquitin in ATP-dependent manner | UBA1, UBA6 | Forms thioester bond with ubiquitin |
| E2 (Conjugating) | Accepts and carries activated ubiquitin | UBE2T, UBE2N, UBE2B | Transient E2~Ub thioester intermediate |
| E3 (Ligase) | Recognizes substrates and catalyzes ubiquitin transfer | RING, HECT, RBR types | Direct transfer (RING) or intermediate (HECT) |
The process initiates when the E1 enzyme activates ubiquitin through an ATP-dependent reaction that adenylates the ubiquitin C-terminal glycine, subsequently forming a high-energy thioester bond between E1's catalytic cysteine and ubiquitin [1] [3]. Activated ubiquitin is then transferred to a cysteine residue on an E2 conjugating enzyme via transesterification [4]. The final step involves an E3 ubiquitin ligase that recognizes specific substrate proteins and facilitates the transfer of ubiquitin from the E2 to a lysine residue on the substrate, forming an isopeptide bond [1]. Humans possess approximately 40 E2 enzymes and over 600 E3 ligases, which confer substrate specificity and determine the nature of ubiquitin modifications [3] [5].
E3 Ligase Classification and Mechanisms
E3 ubiquitin ligases are categorized into three major families based on their structural domains and mechanisms of ubiquitin transfer:
RING-type E3 ligases (Really Interesting New Gene) represent the largest class and function primarily as scaffolds that simultaneously bind both the E2~Ub complex and the substrate protein, facilitating direct ubiquitin transfer without forming a covalent intermediate [3] [7]. Prominent examples include the tripartite motif (TRIM) family proteins such as TRIM8 and TRIM31, which have been implicated in cancer-relevant signaling pathways [3].
HECT-type E3 ligases (Homologous to E6-AP Carboxyl Terminus) employ a two-step mechanism wherein ubiquitin is first transferred from the E2 to a conserved cysteine residue within the HECT domain, forming a thioester intermediate, before final transfer to the substrate [3] [7].
RBR-type E3 ligases (RING-Between-RING) represent a hybrid class that utilizes both RING-like domains for E2 binding and a catalytic domain that transiently accepts ubiquitin similar to HECT-type E3s [3].
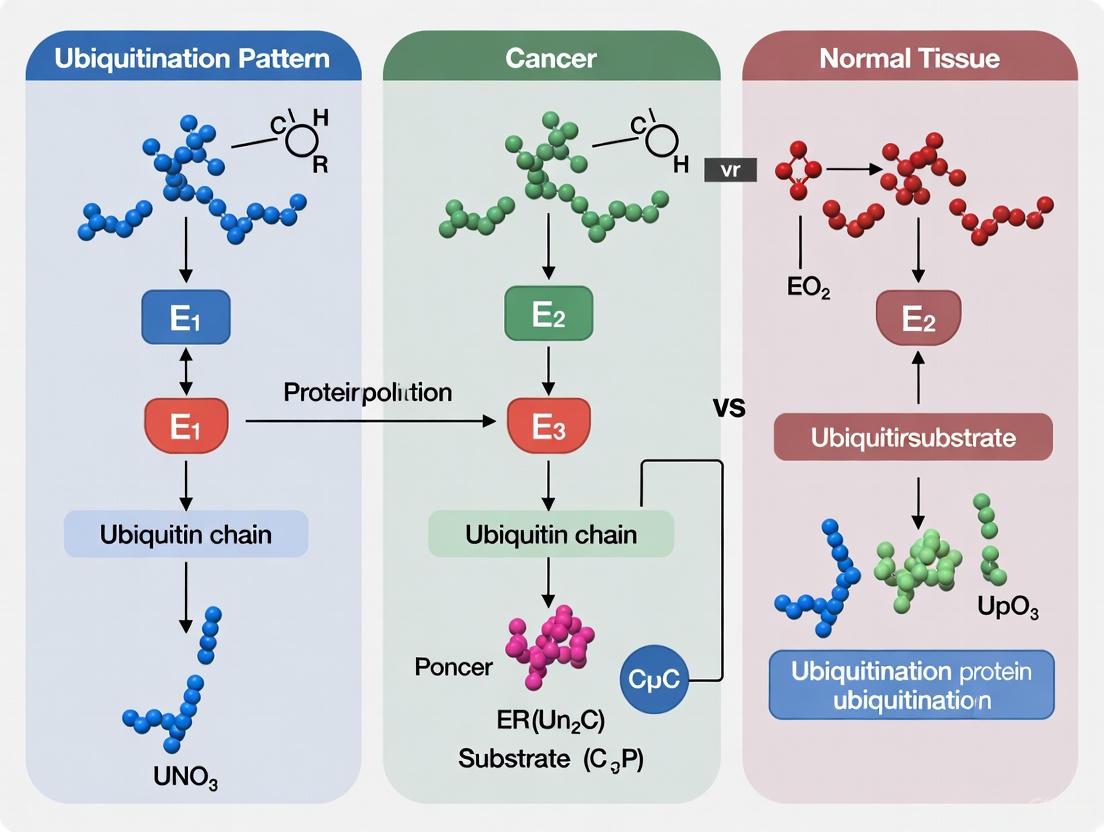
Figure 1: Ubiquitination Enzymatic Cascade. E1 activates ubiquitin in an ATP-dependent process, E2 carries the activated ubiquitin, and E3 facilitates transfer to the substrate protein.
Deubiquitinating Enzymes (DUBs): Reversibility and Regulation
Deubiquitinating enzymes (DUBs) constitute a diverse family of proteases that counterbalance ubiquitination by removing ubiquitin modifications from substrate proteins, thereby providing critical regulatory control over ubiquitin signaling [3]. DUBs are categorized into two major classes based on their catalytic mechanisms: cysteine proteases and metalloproteases [7]. The cysteine protease class includes multiple subfamilies, with ubiquitin-specific proteases (USPs) representing the largest group with over 60 members in humans [7]. These enzymes perform several essential functions, including processing ubiquitin precursors, reversing ubiquitin signals to regulate pathways, rescuing proteins from degradation, and maintaining ubiquitin homeostasis by recycling ubiquitin from substrates targeted to the proteasome or lysosome [3].
A well-characterized example is USP22, a catalytic component of the human Spt-Ada-Gcn5 Acetyltransferase (hSAGA) complex, which plays a vital role in transcriptional regulation through histone modification [7]. USP22 removes monoubiquitin from histone H2B, facilitating transcriptional elongation and affecting additional histone modifications. This DUB has been implicated in various cancers, where its elevated expression correlates with poor patient outcomes, positioning it as a potential biomarker and therapeutic target [7]. Beyond histone modification, DUBs regulate key signaling pathways relevant to cancer, including p53 signaling, NF-κB pathway, and MAPK cascade, highlighting their broad impact on cellular homeostasis and disease processes [3] [6].
The Ubiquitin Code: Complexity and Signaling Diversity
The ubiquitin system generates remarkable complexity through diverse ubiquitin modifications that constitute a sophisticated "ubiquitin code" [2]. Ubiquitin itself contains seven lysine residues (K6, K11, K27, K29, K33, K48, K63) and an N-terminal methionine (M1) that can serve as attachment points for subsequent ubiquitin molecules, forming polyubiquitin chains with distinct structures and functions [2]. The specific linkage types within these chains determine the fate and function of the modified protein:
Table 2: Major Ubiquitin Linkage Types and Their Cellular Functions
| Linkage Type | Primary Cellular Function | Key Recognizers/Effectors |
|---|---|---|
| K48-linked | Proteasomal degradation | Proteasome receptors |
| K63-linked | Signal transduction, DNA repair, endocytosis | Proteins with UBDs in signaling complexes |
| M1-linked (linear) | NF-κB activation, inflammation | LUBAC, NEMO |
| K11-linked | Proteasomal degradation, cell cycle regulation | Proteasome receptors |
| K27-linked | DNA damage response, mitophagy | Autophagy receptors |
| K29-linked | Proteasomal degradation, Wnt signaling | Proteasome receptors |
| K33-linked | Kinase modification, trafficking | Undefined |
Beyond homogeneous chains, ubiquitin modifications can form heterotypic chains (mixed linkages) or branched chains (multiple ubiquitins attached to a single ubiquitin molecule), creating exceptional diversity in signaling outcomes [2]. Additionally, ubiquitin itself can be modified by phosphorylation, acetylation, or other ubiquitin-like proteins (SUMO, NEDD8), adding further layers of regulation [2]. This complex ubiquitin code enables precise control over numerous cellular processes, with different chain architectures recruiting specific ubiquitin-binding proteins that dictate downstream consequences such as proteasomal degradation, altered subcellular localization, or modified activity [1] [2].
Experimental Approaches for Studying Ubiquitination
Key Methodologies and Workflows
Investigating the ubiquitination process requires specialized methodologies to identify substrates, characterize enzymatic activities, and decipher the ubiquitin code. Several well-established experimental approaches include:
In Vitro Ubiquitination Assays: These reconstitution experiments utilize purified E1, E2, E3 enzymes, ubiquitin, and ATP to examine specific ubiquitination events. Reactions are typically analyzed by immunoblotting to detect ubiquitinated species, often under denaturing conditions to preserve the thioester linkages between E2 and ubiquitin [4]. This approach allows researchers to dissect the minimal components required for ubiquitination and test the effects of mutations or inhibitors on the enzymatic cascade.
Global Protein Stability (GPS) Profiling: This genome-wide screening strategy employs reporter proteins fused with hundreds of potential substrates to systematically identify E3 ligase substrates [4]. By inhibiting E3 ligase activity and monitoring reporter accumulation, researchers can map E3-substrate regulatory networks on a global scale, revealing previously unknown relationships in the ubiquitin system.
Mass Spectrometry-Based Ubiquitinomics: Advanced proteomic techniques represent powerful tools for comprehensively characterizing the ubiquitin code. These approaches typically involve enrichment of ubiquitinated peptides using ubiquitin remnant motifs or linkage-specific antibodies, followed by high-resolution mass spectrometry analysis [2]. Quantitative methods such as SILAC (Stable Isotope Labeling with Amino Acids in Cell Culture) or TMT (Tandem Mass Tag) enable comparative analysis of ubiquitination sites and chain topology under different physiological conditions or in response to perturbations.
Figure 2: Ubiquitinomics Workflow. Mass spectrometry-based approach for system-wide analysis of ubiquitination sites and chain architectures.
The Scientist's Toolkit: Essential Research Reagents
Table 3: Essential Research Reagents for Ubiquitination Studies
| Reagent Category | Specific Examples | Application and Function |
|---|---|---|
| Linkage-Specific Antibodies | Anti-K48-Ub, Anti-K63-Ub, Anti-M1-Ub | Immunoblotting, immunofluorescence to detect specific chain types |
| Activity-Based Probes | Ubiquitin-vinylsulfone, HA-Ub-VS | DUB activity profiling and identification |
| Recombinant Enzymes | Purified E1, E2, E3 complexes | Reconstitution of ubiquitination cascades in vitro |
| Proteasome Inhibitors | Bortezomib, MG132 | Stabilize ubiquitinated proteins by blocking degradation |
| DUB Inhibitors | PR-619, P22077 | Pan-DUB inhibitors to study ubiquitination dynamics |
| Ubiquitin Mutants | K48R, K63R, K0 (all lysines mutated) | Define chain specificity and requirements |
| CRISPR Libraries | E3/DUB knockout pools | Functional genomic screens for ubiquitin pathway components |
Ubiquitination Machinery in Cancer: Pathophysiological and Therapeutic Implications
Dysregulation in Oncogenesis
Dysregulation of ubiquitination enzymes is a hallmark of many cancers, with mutations in E2s, E3s, and DUBs contributing to tumor initiation, progression, and therapeutic resistance [5]. For instance, UBE2T, an E2 conjugating enzyme, demonstrates elevated expression across multiple tumor types where its upregulation correlates with poor clinical outcomes [8]. UBE2T functions in the Fanconi anemia DNA repair pathway and promotes oncogenesis through stabilization of proto-oncogenes and cell cycle regulators [8]. Another E2 enzyme, UBE2N, which primarily synthesizes K63-linked ubiquitin chains to stabilize proteins or alter their function, has been identified as a critical dependency in acute myeloid leukemia (AML) [9]. Inhibition of UBE2N catalytic function suppresses leukemic cells through selective degradation of critical proteins, revealing its potential as a therapeutic target [9].
E3 ligases also play pivotal roles in cancer pathogenesis. The TRIM family of RING-type E3 ligases exhibits diverse functions in oncogenesis. TRIM8 expression is increased in metabolic dysfunction-associated steatohepatitis (MASH) and promotes hepatic lipid accumulation, inflammation, and fibrosis by activating TAK1 through ubiquitination [3]. Conversely, TRIM31 exerts protective effects against MASH progression by promoting the degradation of RHBDF2 via K48-linked polyubiquitination, thereby attenuating inflammatory signaling [3]. In von Hippel-Lindau (VHL) disease, loss-of-function mutations in the VHL E3 ligase result in accumulation of hypoxia-inducible factors (HIFs), driving renal cell carcinoma and other tumors [4].
Emerging Therapeutic Strategies
The therapeutic potential of targeting ubiquitination pathways is being realized through several innovative approaches:
Proteolysis-Targeting Chimeras (PROTACs) are bifunctional molecules that recruit E3 ubiquitin ligases to target proteins of interest, inducing their ubiquitination and subsequent degradation [6]. PROTACs such as ARV-110 (targeting androgen receptor) and ARV-471 (targeting estrogen receptor) have advanced to clinical trials, demonstrating promising results in cancer treatment [6]. These molecules offer advantages over traditional inhibitors by catalytically inducing protein degradation rather than merely inhibiting function.
Molecular Glues represent another class of degraders that induce neo-interactions between E3 ligases and target proteins, leading to ubiquitination and degradation [6]. CC-90009, which promotes degradation of GSPT1 by recruiting the CRL4CRBN E3 ligase complex, is currently in phase II trials for leukemia therapy [6].
Small-Molecule Inhibitors targeting specific components of the ubiquitin system continue to be developed. For instance, inhibitors of the E1 enzyme have shown antitumor activity, while specific inhibitors targeting oncogenic E3 ligases or DUBs are under investigation [5]. The clinical success of proteasome inhibitor bortezomib in multiple myeloma and mantle cell lymphoma validates the ubiquitin-proteasome system as a viable therapeutic target in oncology [4].
A comprehensive pan-cancer analysis has revealed that ubiquitination-related gene signatures can effectively stratify patients into prognostic subgroups and predict response to immunotherapy [10]. Specifically, the OTUB1-TRIM28 ubiquitination axis was found to modulate MYC pathway activity and influence tumor histology, suggesting novel strategies for targeting traditionally "undruggable" oncoproteins like MYC through their ubiquitination regulatory networks [10]. These advances highlight the growing importance of understanding ubiquitination machinery for developing targeted cancer therapies.
Ubiquitination is a crucial post-translational modification that governs virtually all cellular processes in eukaryotes, serving as a master regulatory mechanism for protein stability, function, and localization. This sophisticated signaling system employs a 76-amino acid protein, ubiquitin, which can be conjugated to substrate proteins as a single moiety (monoubiquitination) or as polymeric chains (polyubiquitination) through an enzymatic cascade involving E1 activating, E2 conjugating, and E3 ligating enzymes [11] [12]. The diversity of ubiquitin signaling stems from the various topological arrangements possible when ubiquitin molecules form chains, with all seven lysine residues (K6, K11, K27, K29, K33, K48, K63) and the N-terminal methionine (M1) serving as potential linkage sites [13] [14]. In human cells, this complex system is orchestrated by a limited set of enzymes: only two E1 enzymes, approximately 40 E2 enzymes, and over 600 E3 enzymes, which work in concert to achieve remarkable substrate specificity [14] [12]. The resulting "ubiquitin code" is interpreted by specialized receptors containing ubiquitin-binding domains (UBDs), with more than 20 distinct UBD families identified to date [13]. When decoded incorrectly or dysregulated, this intricate system contributes significantly to human diseases, particularly cancer, making it a compelling area for therapeutic intervention [14] [8] [12].
Ubiquitin Linkage Types and Their Functional Consequences
The ubiquitination system generates remarkable functional diversity through variations in chain linkage and architecture. The specific lysine residues used to connect ubiquitin molecules create structurally and functionally distinct signals that are interpreted differently by cellular machinery [13] [15].
Table 1: Ubiquitin Linkage Types and Their Primary Cellular Functions
| Linkage Type | Structural Features | Primary Cellular Functions | Representative E2/E3 Enzymes |
|---|---|---|---|
| Monoubiquitination | Single ubiquitin attached | DNA damage repair, chromatin remodeling, endocytosis [11] [12] | Rad18 (E3) for PCNA [12] |
| K48-linked | Compact "closed" conformation | Proteasomal degradation [11] [15] | Cdc34/SCF complexes [11] |
| K63-linked | Extended "open" conformation | Kinase activation, DNA repair, endocytosis, inflammation [11] [15] | UBC13/MMS2 heterodimer (E2) [13] |
| K11-linked | Mixed open/closed states | Cell cycle regulation, ER-associated degradation [14] [12] | UBE2S with APC/C (E3) [13] |
| K6-linked | Not well characterized | DNA damage repair, mitochondrial homeostasis [12] | BRCA1/BARD1 (E3) [13] |
| K27-linked | Heterogeneous structures | Mitophagy, innate immunity [12] | - |
| K29-linked | Not well characterized | Proteasomal degradation, lysosomal degradation [14] | - |
| K33-linked | Not well characterized | Endosomal sorting, kinase regulation [12] | - |
| M1-linked | Linear chains | NF-κB signaling, inflammation [12] | LUBAC complex (E3) [12] |
| Branched | Multiple linkage types in single chain | Enhanced signaling complexity [14] | Multiple E2 combinations [13] |
The functional specificity of different ubiquitin linkages arises from their distinct three-dimensional structures, which create unique interaction surfaces for ubiquitin-binding domains. For instance, K48-linked chains predominantly adopt a "closed" conformation where the hydrophobic patches are sequestered at ubiquitin-ubiquitin interfaces, while K63-linked chains maintain an extended "open" structure that exposes these hydrophobic surfaces for recognition by specific receptors [13]. This structural diversity enables the ubiquitin system to coordinate a vast array of cellular processes, with distinct chain types directing proteins to different fates—K48 linkages typically target substrates for proteasomal degradation, whereas K63 linkages generally serve non-proteolytic roles in signaling complex assembly [11] [15].
The Ubiquitination Enzyme Cascade
The process of ubiquitination involves a sequential enzymatic cascade that begins with ubiquitin activation and culminates in its transfer to specific substrate proteins [11] [12].
Diagram 1: Ubiquitin Enzymatic Cascade (55 characters)
The cascade initiates when the E1 activation enzyme utilizes ATP to adenylate ubiquitin's C-terminus, forming a ubiquitin-adenylate intermediate. The E1 then captures activated ubiquitin via a thioester bond between its catalytic cysteine and ubiquitin's C-terminal glycine [12]. This activated ubiquitin is subsequently transferred to the E2 conjugating enzyme, which forms a similar thioester bond with ubiquitin through its conserved catalytic cysteine residue [11]. Finally, E3 ligases orchestrate the final transfer of ubiquitin from the E2 to specific substrate proteins, facilitating the formation of an isopeptide bond between ubiquitin's C-terminus and a lysine ε-amino group on the substrate [11] [12].
Table 2: Classification of Human Ubiquitination Enzymes
| Enzyme Class | Subtypes | Representative Members | Catalytic Mechanism | Human Genes |
|---|---|---|---|---|
| E1 Activating Enzymes | - | UBA1, UBA6 | Ubiquitin activation via ATP-dependent adenylation, forms E1~Ub thioester [12] | 2 |
| E2 Conjugating Enzymes | Class I (UBC only) | Cdc34, UBE2T, Ube2c | Accepts Ub from E1, forms E2~Ub thioester, often determines chain topology [11] [14] | ~40 |
| Class II (C-terminal extension) | - | - | - | |
| Class III (N-terminal extension) | - | - | - | |
| Class IV (both extensions) | - | - | - | |
| E3 Ligase Enzymes | RING-type | SCF complexes, MDM2 | Brings E2~Ub and substrate together, direct Ub transfer [11] [14] | >500 |
| HECT-type | Nedd4 family | Forms HECT-Ub thioester intermediate before substrate transfer [14] | ~30 | |
| RBR-type | HOIP, HOIL-1 | Hybrid mechanism with RING1 and RING2 domains [14] | 14 |
The exceptional specificity of ubiquitin signaling is largely achieved through the combinatorial action of E2 and E3 enzymes. While E2 enzymes often determine chain topology, E3 enzymes provide substrate recognition through specialized protein-protein interaction domains [11] [14]. For example, in the well-characterized SCFCdc4/Cdc34 system, the RING E3 SCFCdc4 binds the substrate Sic1 while the E2 Cdc34 catalyzes ubiquitin transfer, with specific residues in Cdc34's catalytic core determining whether Sic1 undergoes monoubiquitination or K48-linked polyubiquitination [11]. This sophisticated division of labor enables the ubiquitin system to achieve remarkable regulatory precision with a limited set of components.
Experimental Methods for Studying Ubiquitination
Investigating ubiquitination mechanisms requires specialized methodologies that can capture transient enzyme-substrate interactions and determine linkage specificity. The following protocols represent core experimental approaches in the field.
In Vitro Ubiquitination Assay Protocol
Purpose: To reconstitute ubiquitination using purified components and identify specific E2-E3-substrate combinations responsible for particular ubiquitin chain types [11].
Reagents and Equipment:
- Purified E1, E2, E3 enzymes
- Ubiquitin (wild-type and mutant forms)
- ATP regeneration system
- Substrate protein
- Reaction buffer (50 mM Tris-HCl pH 7.5, 50 mM NaCl, 10 mM MgCl₂, 1 mM DTT)
- SDS-PAGE equipment
- Immunoblotting apparatus
- Ubiquitin linkage-specific antibodies
Procedure:
- Prepare master mix containing 100 nM E1, 1-5 μM E2, 5-20 μM ubiquitin, and ATP regeneration system in reaction buffer
- Aliquot master mix into separate tubes containing different E3 enzymes (100-500 nM) and substrate (1-2 μM)
- Incubate reactions at 30°C for 60-90 minutes
- Terminate reactions by adding SDS-PAGE sample buffer with DTT
- Analyze by immunoblotting with ubiquitin antibodies or substrate-specific antibodies
- For linkage determination, include ubiquitin mutants (e.g., K48R, K63R) or use linkage-specific antibodies
Key Controls:
- Omit individual components (E1, E2, E3, or substrate) to confirm requirement of all factors
- Include catalytically inactive E2 (Cys-to-Ser mutant) to verify enzymatic activity requirement
- Test ubiquitin lysine mutants to determine linkage specificity [11]
Acceptor Lysine Identification Protocol
Purpose: To identify specific lysine residues targeted for ubiquitination and characterize sequence determinants influencing lysine selection [11].
Reagents and Equipment:
- Substrate protein with wild-type and mutant lysine residues
- In vitro ubiquitination components (as above)
- Mass spectrometry equipment
- Site-directed mutagenesis kit
Procedure:
- Perform in vitro ubiquitination reaction with wild-type substrate
- Resolve ubiquitinated products by SDS-PAGE and excise bands
- Digest with trypsin and analyze by mass spectrometry to identify modified lysines
- Create point mutants converting target lysines to arginine
- Test ubiquitination efficiency of lysine mutants compared to wild-type
- Create chimeric proteins swapping sequences around poorly and efficiently ubiquitinated lysines
- Quantify ubiquitination efficiency via immunoblotting and densitometry
Applications: This approach revealed that residues surrounding Sic1 lysines are critical for ubiquitination efficiency, and that amino acid determinants in Cdc34's catalytic region specify whether Sic1 undergoes monoubiquitination or polyubiquitination [11].
Ubiquitin Signaling in Cancer Biology
Dysregulation of ubiquitin signaling is implicated in numerous cancers, with specific E3 ligases and deubiquitinases acting as oncogenes or tumor suppressors. The functional consequences of ubiquitination in cancer depend critically on both the substrate and the linkage type.
Diagram 2: Ubiquitination in Cancer (34 characters)
The tumor suppressor p53 provides a classic example of ubiquitin-mediated regulation in cancer. The E3 ligase MDM2 binds to p53 through its N-terminus to ubiquitinate p53 protein, with monoubiquitination promoting nuclear export and polyubiquitination mediating degradation in the nucleus [14]. MDM2 overexpression, detected in various human cancers including osteosarcoma and neuroblastoma, results in excessive p53 degradation and diminished tumor suppressor activity [14]. Beyond p53, numerous other critical cancer regulators are controlled by ubiquitination, including the core stem cell factors Nanog, Oct4, and Sox2, whose ubiquitination status helps maintain cancer stem cell stemness [12].
Table 3: Selected Ubiquitination Enzymes Dysregulated in Cancer
| Enzyme | Gene | Cancer Type | Molecular Function | Therapeutic Implications |
|---|---|---|---|---|
| MDM2 | MDM2 | Osteosarcoma, Neuroblastoma, Lung Cancer | E3 ligase for p53 degradation [14] | Nutlin, MI-219 (MDM2 inhibitors) [12] |
| UBE2T | UBE2T | Multiple Myeloma, Breast Cancer, Ovarian Cancer | E2 enzyme in Fanconi anemia pathway, interacts with FANCL [8] | Potential biomarker for prognosis and immunotherapy response [8] |
| Ube2c | UBE2C | Hepatocellular Carcinoma, Esophageal Cancer, Breast Cancer | E2 cooperating with APC/C for cell cycle regulation [14] | Overexpression enhances proliferation; inhibition induces apoptosis [14] |
| Gp78 | AMFR | Sarcomas, Metastatic Cancers | Endoplasmic reticulum-associated E3 ligase for KA11/CD82 [14] | Inhibition reduces metastasis by stabilizing KA11 [14] |
| OTUB1 | OTUB1 | Pan-cancer (Ubiquitination Regulatory Network) | Deubiquitinase regulating MYC pathway with TRIM28 [10] | High expression associated with immunotherapy resistance [10] |
Recent pan-cancer analyses have revealed that ubiquitination patterns effectively stratify patients into molecular subtypes with distinct clinical outcomes. A comprehensive study integrating data from 4,709 patients across 26 cohorts identified a conserved ubiquitination-related prognostic signature (URPS) that effectively stratified patients into high-risk and low-risk groups with distinct survival outcomes across all analyzed cancers [10]. This signature demonstrated significant associations with tumor immune markers, checkpoint genes, and immune cell infiltration, highlighting the immune-modulatory functions of ubiquitination in cancer [8] [10]. Furthermore, ubiquitination scores showed a positive correlation with squamous or neuroendocrine transdifferentiation in adenocarcinoma, suggesting ubiquitination pathways help drive histological fate decisions in cancer cells [10].
Research Reagent Solutions
Table 4: Essential Research Reagents for Ubiquitination Studies
| Reagent Category | Specific Examples | Research Applications | Key Features |
|---|---|---|---|
| Ubiquitin Mutants | K48-only, K63-only, K48R, K63R | Linkage specificity determination [11] | Single lysine ubiquitins prevent alternative chain formation; arginine mutants block specific linkages |
| E2 Enzyme Inhibitors | CC0651, Leucettamol A [12] | E2 functional studies | Target E2-ubiquitin thioester formation; demonstrate therapeutic potential in preclinical models |
| E1 Enzyme Inhibitors | MLN7243, MLN4924 [12] | Global ubiquitination blockade | MLN4924 inhibits NEDD8-activating enzyme; causes apoptosis in hematological malignancies |
| Proteasome Inhibitors | Bortezomib, Carfilzomib, Ixazomib [12] | Clinical translation; K48-linked pathway studies | FDA-approved for multiple myeloma; validate ubiquitin system as drug target |
| Linkage-Specific Antibodies | K48-linkage specific, K63-linkage specific | Immunoblotting, immunohistochemistry | Recognize unique epitopes formed by specific ubiquitin linkages |
| DUB Inhibitors | Compounds G5, F6 [12] | Deubiquitination pathway studies | Target ubiquitin-specific proteases; show potential in preclinical cancer models |
| Activity-Based Probes | Ubiquitin-based probes with reactive groups | DUB substrate profiling | Covalently trap active DUBs for identification and characterization |
The diverse signaling capabilities of monoubiquitination and polyubiquitin chains represent a sophisticated regulatory language that coordinates cellular homeostasis. The structural plasticity of ubiquitin chains—from monoubiquitination to complex polyubiquitin architectures—enables this system to direct an extraordinary range of biological outcomes, with specific chain topologies recruiting distinct receptor proteins to initiate appropriate downstream responses [13] [15]. In cancer biology, dysregulation of ubiquitination contributes fundamentally to tumorigenesis through multiple mechanisms, including excessive degradation of tumor suppressors, stabilization of oncoproteins, and rewiring of signaling networks [14] [12]. The expanding repertoire of ubiquitin-targeting therapeutics, particularly those exploiting linkage-specific vulnerabilities, represents a promising frontier in precision oncology [12] [16]. As our understanding of ubiquitin signaling complexity deepens through multiomics approaches and single-cell technologies, we anticipate increasingly sophisticated strategies for manipulating this system to overcome therapeutic resistance and improve patient outcomes across diverse cancer types [10] [17] [16].
The ubiquitin-proteasome system (UPS) is a critical post-translational regulatory mechanism responsible for controlling approximately 80-90% of intracellular proteolysis in eukaryotic cells [8] [10]. This system employs a precise enzymatic cascade comprising E1 (activating), E2 (conjugating), and E3 (ligating) enzymes to tag substrate proteins with ubiquitin chains, ultimately determining their stability, localization, and function [16]. Dysregulation of this finely tuned system has emerged as a hallmark of cancer pathogenesis, driving uncontrolled proliferation, metabolic reprogramming, immune evasion, and therapeutic resistance across diverse malignancies [16] [18].
Global ubiquitinome remodeling represents a fundamental molecular process wherein cancer cells systematically rewire ubiquitination networks to acquire malignant capabilities. Unlike genetic mutations, which are static alterations, the ubiquitinome constitutes a dynamic, adaptable layer of regulation that enables tumors to fine-tune oncogenic and tumor-suppressive pathways in response to selective pressures [16]. Recent pan-cancer analyses have begun to illuminate conserved patterns of ubiquitin pathway alterations that transcend tissue-of-origin classifications, revealing both universal vulnerabilities and context-specific dependencies [8] [10] [19].
This technical review synthesizes current evidence quantifying ubiquitinome alterations across solid tumors, delineates the experimental methodologies enabling these discoveries, and explores the therapeutic implications of targeting the ubiquitin system in oncology. By framing these findings within the context of a broader thesis on ubiquitination patterns in cancer versus normal tissues, we aim to provide researchers and drug development professionals with a comprehensive reference for understanding and exploiting ubiquitin-based mechanisms in cancer biology.
Quantitative Landscape of Ubiquitin Pathway Alterations in Solid Tumors
Systematic pan-cancer analyses have revealed consistent patterns of ubiquitin pathway dysregulation across diverse solid tumors. The integration of genomic, transcriptomic, and proteomic datasets has enabled researchers to quantify these alterations at multiple molecular levels, from gene expression changes to protein abundance and post-translational modifications.
Table 1: Ubiquitin Enzyme Expression Alterations Across Solid Tumors
| Ubiquitin Enzyme | Cancer Types with Significant Overexpression | Associated Clinical Outcomes | Primary Functional Consequences |
|---|---|---|---|
| UBE2T [8] | Multiple myeloma, breast cancer, renal cell carcinoma, ovarian cancer, cervical cancer, retinoblastoma, pancreatic cancer | Reduced overall and progression-free survival | Enhanced proliferation, invasion, epithelial-mesenchymal transition, DNA repair dysregulation |
| UBD [19] | 29 cancer types including glioma, colorectal carcinoma, hepatocellular carcinoma, breast cancer | Poor prognosis, higher histological grades | Promotion of chromosomal instability, interaction with NF-κB, Wnt, and SMAD2 pathways |
| OTUB1 [10] | Lung cancer, esophageal cancer, cervical cancer, urothelial cancer, melanoma | Immunotherapy resistance, poor prognosis | Modulation of MYC pathway, oxidative stress alteration, squamous/neuroendocrine transdifferentiation |
| E3 Ligases [20] | HERC5 (esophageal cancer), RNF5 (liver cancer) | Cancer type-specific progression | Tumor type-specific substrate targeting, potential therapeutic vulnerabilities |
The ubiquitin-conjugating enzyme UBE2T demonstrates particularly widespread oncogenic roles across solid tumors. Comprehensive analyses using TIMER 2.0, GEPIA2, and TCGA datasets have revealed elevated UBE2T expression in numerous malignancies compared to adjacent normal tissues [8]. This overexpression correlates strongly with adverse clinical outcomes, including reduced overall survival and progression-free survival across multiple cancer types. Functional studies indicate that UBE2T upregulation drives key oncogenic processes including enhanced cellular proliferation, invasion, epithelial-mesenchymal transition, and dysregulation of DNA repair mechanisms [8].
Table 2: Genetic and Epigenetic Alterations in Ubiquitin Pathway Genes
| Alteration Type | Representative Genes | Frequency Across Cancers | Functional Impact |
|---|---|---|---|
| Gene amplification [8] [19] | UBE2T, UBD | High frequency in pan-cancer cohorts | Increased enzyme dosage, enhanced oncogenic signaling |
| Somatic mutations [8] | UBE2T | Relatively infrequent | Potential functional alterations, neoantigen generation |
| Promoter hypomethylation [19] | UBD | 16 cancer types | Transcriptional derepression, increased expression |
| Copy number variations [8] | UBE2T | Predominant alteration type | Gene dosage effects, pathway amplification |
Beyond individual enzyme dysregulation, ubiquitination-related prognostic signatures (URPS) have demonstrated remarkable utility in stratifying patients across multiple cancer types. A comprehensive study integrating data from 4,709 patients across 26 cohorts and five solid tumor types (lung cancer, esophageal cancer, cervical cancer, urothelial cancer, and melanoma) established that URPS effectively identifies high-risk and low-risk patient groups with distinct survival outcomes [10]. This signature further correlates with immunotherapy response, enabling identification of patients most likely to benefit from immune checkpoint blockade [10].
Experimental Methodologies for Ubiquitinome Profiling
Multi-Omics Data Integration Frameworks
Advanced bioinformatics pipelines integrating data from multiple omics layers have proven essential for comprehensive ubiquitinome characterization. The following experimental protocol outlines a standardized approach for pan-cancer ubiquitinome analysis:
Data Acquisition and Preprocessing
- Source transcriptomic data and clinical metadata from TCGA (The Cancer Genome Atlas) and GTEx (Genotype-Tissue Expression) projects using platforms such as GEPIA2.0, UALCAN, and Sangerbox [8] [19].
- Implement rigorous quality control measures including log2(x + 0.001) transformation of expression values, exclusion of samples with zero expression levels, and removal of cancer types with fewer than three representative samples [19].
- For ubiquitination-focused analyses, obtain reference ubiquitin enzyme catalogs from specialized databases such as the Unified Ubiquitin-Code Database (UUCD), typically comprising approximately 929 genes categorized into E1 (8 genes), E2 (39 genes), and E3 (882 genes) enzyme classes [21].
Differential Expression Analysis
- Identify differentially expressed ubiquitination-related genes (Ubi-DEGs) using the 'edgeR' package in R, applying thresholds of |logFC| ≥ 1 and adjusted p-value < 0.01 [21].
- Validate findings across multiple independent cohorts (e.g., GSE165808, GSE26712 for ovarian cancer) to ensure reproducibility [21].
- Correlate expression patterns with clinicopathological parameters including histological grade, clinical stage, and T-stage using logistic regression models [19].
Genetic and Epigenetic Alteration Mapping
- Interrogate mutation frequency, amplification events, and other genetic alterations using cBioPortal with data sourced from TCGA Pan-Cancer Atlas Studies [19].
- Analyze promoter DNA methylation levels in both normal tissues and pan-cancer samples using UALCAN to identify epigenetic deregulation mechanisms [19].
- Employ single nucleotide variation (SNV) analysis using "maftools" to characterize somatic mutation patterns in ubiquitin pathway genes [21].
Proteomic Profiling of Ubiquitination Networks
Mass spectrometry-based proteomics has emerged as a cornerstone technology for directly quantifying ubiquitinome alterations in cancer:
The Pan-Cancer Proteome Atlas (TPCPA) Framework
- Utilize data-independent acquisition mass spectrometry (DIA-MS) to enable high-throughput proteome characterization without sample multiplexing limitations [20].
- Process 9,670 proteins from 999 primary tumors representing 22 cancer types to ensure comprehensive coverage [20].
- Implement co-expression analysis to identify protein modules, including those centered on ubiquitin pathway components, using weighted gene co-expression network analysis (WGCNA) [20].
- Validate cancer type-enriched E3 ubiquitin ligases (e.g., HERC5 in esophageal cancer, RNF5 in liver cancer) through orthogonal methods including immunohistochemistry and functional assays [20].
Ubiquitin Chain Typing and Functional Characterization
- Employ chain-specific antibodies and ubiquitin binding domains to differentiate between ubiquitin linkage types (K48, K63, monoubiquitination) in tumor samples [16].
- Integrate phosphoproteomic data to map crosstalk between phosphorylation and ubiquitination events, particularly relevant for DNA damage response pathways [16].
- Analyze ubiquitin chain hierarchies in therapy-resistant tumors, with particular focus on K48-linked proteolysis, K63-linked signaling scaffolds, and monoubiquitylation [16].
Functional Validation Approaches
In Vitro and In Vivo Models
- Conduct reverse transcription-quantitative PCR (RT-qPCR) and western blotting in cancer cell lines (e.g., pancreatic cancer lines PANC1, ASPC, BXPC3) compared to normal epithelial cells (e.g., HPDE) to validate expression findings [8].
- Perform gene silencing (siRNA/shRNA) and overexpression studies to establish causal relationships between ubiquitin enzyme expression and oncogenic phenotypes [8] [21].
- Utilize patient-derived xenograft (PDX) models and genetically engineered mouse models (GEMMs) to assess therapeutic targeting of ubiquitin pathway components in physiologically relevant contexts [10].
Immune Microenvironment Characterization
- Analyze correlations between ubiquitin enzyme expression and immune cell infiltration using algorithms such as TIMER and QUANTISEQ [19].
- Assess relationships with immune checkpoint genes, microsatellite instability (MSI), tumor mutational burden (TMB), and neoantigen load [19].
- Employ single-cell RNA sequencing to resolve ubiquitination patterns across distinct cell types within the tumor microenvironment [10].
Visualization of Core Ubiquitin Signaling Networks in Cancer
The following diagrams illustrate key ubiquitin-mediated signaling pathways commonly altered in solid tumors, generated using Graphviz DOT language.
Ubiquitin Enzymatic Cascade and Outcomes
Ubiquitin Pathway Alterations in Cancer
Table 3: Key Research Reagent Solutions for Ubiquitinome Studies
| Reagent/Resource | Function | Example Applications | Key Considerations |
|---|---|---|---|
| TCGA & GTEx Databases [8] [19] | Source of multi-omics cancer data | Differential expression analysis, survival correlations | Requires sophisticated bioinformatics pipelines for integration |
| DIA Mass Spectrometry [20] | High-throughput protein quantification | Pan-cancer proteome atlas construction, E3 ligase discovery | Enables analysis of >9,000 proteins across 22 cancer types |
| CCLE Cell Lines [8] | Ubiquitin enzyme expression profiling | Validation of cancer-specific targets | Provides mRNA profiles across diverse cancer cell lines |
| UUCD Database [21] | Curated ubiquitin enzyme catalog | Reference for ubiquitination-related gene sets | Contains 929 genes categorized into E1, E2, E3 classes |
| cBioPortal [19] | Genetic alteration analysis | Mutation frequency, amplification events | Integrates data from TCGA Pan-Cancer Atlas |
| TIMER/QUANTISEQ Algorithms [19] | Immune infiltration estimation | Correlation with immune cell abundance | Links ubiquitin enzymes to tumor microenvironment |
| Chain-Specific Ub Antibodies [16] | Differentiation of ubiquitin linkage types | Functional characterization of ubiquitin signatures | Critical for understanding non-proteolytic ubiquitination |
| PROTAC Molecules [16] [21] | Targeted protein degradation | Therapeutic exploitation of ubiquitin system | Recruit E3 ligases to neo-substrates |
Therapeutic Implications and Clinical Translation
The systematic characterization of ubiquitinome remodeling in solid tumors has unveiled numerous therapeutic opportunities. Several targeting strategies have emerged with significant clinical potential:
Direct Targeting of Ubiquitin Pathway Components
Small molecule inhibitors targeting specific E3 ligases and deubiquitinating enzymes (DUBs) have demonstrated preclinical efficacy across multiple cancer types. However, functional redundancy and contextual duality present significant challenges. For instance, FBXW7 exhibits tumor-suppressive or oncogenic functions depending on cellular context—promoting radioresistance in p53-wild type colorectal tumors by degrading p53, while enhancing radiosensitivity in non-small cell lung cancer with SOX9 overexpression [16]. This highlights the critical importance of patient stratification biomarkers when targeting ubiquitin pathway components.
Immunomodulation Through Ubiquitin Pathway Manipulation
Ubiquitination plays a pivotal role in regulating tumor-immune interactions, making it an attractive target for enhancing immunotherapy efficacy. Key mechanisms include:
- Regulation of PD-L1 stability through ubiquitin-mediated degradation, potentially reversing immune evasion [18]
- Modulation of interferon signaling pathways that control tumor cell susceptibility to immune-mediated cytotoxicity [18]
- Influence on macrophage infiltration and functional polarization within the tumor microenvironment [10]
The ubiquitination-related prognostic signature (URPS) has demonstrated particular utility in predicting immunotherapy response, potentially identifying patients most likely to benefit from immune checkpoint inhibitors [10].
PROTACs and Targeted Protein Degradation
Proteolysis-targeting chimeras (PROTACs) represent a revolutionary therapeutic modality that exploits the ubiquitin system for targeted protein degradation. These bifunctional molecules simultaneously bind to E3 ubiquitin ligases and target proteins of interest, inducing selective ubiquitination and degradation [16] [21]. Recent advances include:
- Radiation-responsive PROTAC (RT-PROTAC) prodrugs activated by tumor-localized X-rays to degrade specific oncoproteins [16]
- EGFR-directed PROTACs that selectively degrade β-TrCP substrates in EGFR-dependent tumors [16]
- Nanomicelle-based delivery systems for spatially controlled PROTAC release within irradiated tumors [16]
To date, 50 ubiquitination-related genes have been targeted by PROTACs, with several emerging as promising clinical drug targets for cancer treatment [21].
Global ubiquitinome remodeling represents a fundamental layer of cancer pathophysiology that transcends individual cancer types. Pan-cancer analyses have revealed consistent patterns of ubiquitin pathway alteration, including overexpression of specific E2 enzymes (e.g., UBE2T), E3 ligases, and deubiquitinating enzymes across diverse solid tumors. These alterations drive oncogenic transformation through multiple mechanisms, including dysregulation of DNA repair, cell cycle control, immune evasion, and metabolic reprogramming.
The ongoing development of sophisticated proteomic technologies, particularly DIA mass spectrometry, coupled with advanced bioinformatics pipelines, continues to expand our understanding of ubiquitin-based signaling networks in cancer. These insights are now being translated into novel therapeutic modalities, including PROTACs and ubiquitin pathway inhibitors, that offer promising approaches for targeting previously "undruggable" oncoproteins.
Future research directions should focus on elucidating context-specific functions of ubiquitin pathway components, developing predictive biomarkers for patient stratification, and optimizing combination strategies that integrate ubiquitin-targeting agents with conventional therapies, immunotherapy, and radiation. As our understanding of the cancer ubiquitinome continues to mature, it promises to yield increasingly precise and effective therapeutic strategies for diverse malignancies.
Ubiquitination, a critical post-translational modification, serves as a master regulator of oncogenic signaling pathways by controlling the stability, localization, and activity of key cancer-associated proteins. This technical review examines the intricate mechanisms through which the ubiquitin-proteasome system (UPS) orchestrates the delicate balance of MYC, RAS, and p53 signaling networks in cancer pathogenesis. We provide a comprehensive analysis of the E3 ligases and deubiquitinases (DUBs) that fine-tune these pathways, alongside quantitative data on their dysregulation across cancer types. The resource integrates detailed experimental methodologies for investigating ubiquitination dynamics and presents visual schematics of critical regulatory networks. Furthermore, we catalog emerging therapeutic strategies that target ubiquitination machinery to manipulate oncogenic signaling, offering researchers a foundational framework for developing novel cancer therapeutics aimed at overcoming the traditional "undruggability" of major oncogenic drivers.
The ubiquitin-proteasome system represents a sophisticated hierarchical mechanism for post-translational regulation, comprising ubiquitin-activating (E1), ubiquitin-conjugating (E2), and ubiquitin-ligating (E3) enzymes that collectively coordinate the covalent attachment of ubiquitin to substrate proteins [12]. This enzymatic cascade culminates in the specific recognition of substrates by E3 ligases, of which over 600 exist in human cells, providing exceptional specificity to the process [14]. The functional consequences of ubiquitination are remarkably diverse, ranging from proteasomal degradation to modulation of protein activity, localization, and complex formation, dependent on the topology of ubiquitin chain linkage [14] [12].
In the context of oncogenesis, ubiquitination serves as a pivotal regulatory mechanism that governs the precise control of tumor suppressors and oncoproteins. The balanced regulation of the tumor suppressor p53 ("yin") and the oncoprotein c-Myc ("yang") exemplifies this critical control system, whose disruption represents a fundamental event in cellular transformation [22]. As a library, NLM provides access to scientific literature. Inclusion in an NLM database does not imply endorsement of, or agreement with, the contents by NLM or the National Institutes of Health. Recent pan-cancer analyses have revealed that ubiquitination-related prognostic signatures can effectively stratify patients across multiple cancer types, including lung cancer, esophageal cancer, cervical cancer, urothelial cancer, and melanoma, highlighting the broad clinical relevance of ubiquitination networks in oncology [10]. This review systematically examines the specific ubiquitination mechanisms regulating MYC, RAS, and p53 pathways, integrating quantitative data, experimental approaches, and therapeutic implications for research and drug development.
Molecular Mechanisms of Ubiquitination in Core Oncogenic Pathways
p53 Ubiquitination and Regulatory Networks
The p53 tumor suppressor, often termed the "guardian of the genome," is extensively regulated by ubiquitination, with its stability and activity controlled by multiple E3 ubiquitin ligases [22] [23]. As the most frequently mutated gene in human cancers, p53's tight regulation is essential for maintaining genomic integrity, with the MDM2 E3 ligase serving as its primary negative regulator [22] [23]. MDM2 mediates both multiple monoubiquitination to promote nuclear export and polyubiquitination for nuclear degradation of p53 [14]. The critical balance in this regulatory circuit is evidenced by the rescue of embryonic lethality in mdm2 knockout mice through concomitant p53 deletion [22].
Beyond MDM2, several other E3 ligases contribute to p53 regulation, including PirH2, COP1, CHIP, ARF-BP1/HectH9, and complexes containing Cullin 7 [22]. This multilayered regulatory network ensures precise control of p53 activity in response to diverse cellular stresses. The functional diversity of ubiquitination is exemplified by MDM2's ability to not only promote p53 degradation but also directly inhibit its transcriptional activity by binding to its N-terminal transactivation domain and promoting histone monoubiquitination on target gene promoters [22]. Furthermore, MDM2 collaborates with its homolog MDMX to enhance p53 ubiquitylation and degradation, though MDMX lacks intrinsic E3 ligase activity [22].
Table 1: E3 Ubiquitin Ligases Regulating p53 Stability and Activity
| E3 Ligase | Type | Effect on p53 | Role in Cell Growth | Cancer Association |
|---|---|---|---|---|
| MDM2 | RING | Degradation, nuclear export, inhibition of transactivation | Promotes cell growth | Oncogene |
| PirH2 | RING | Degradation | Uncertain | Uncertain |
| COP1 | RING | Degradation | Uncertain | Uncertain |
| ARF-BP1/HectH9 | HECT | Degradation | Promotes cell growth | Uncertain |
| Cullin 7 | Cullin-based | Degradation | Uncertain | Uncertain |
MYC Ubiquitination and Stability Control
The MYC oncoprotein is regulated by several E3 ubiquitin ligases that control its stability and oncogenic activity. Skp2, Fbw7, and ARF-BP1/HectH9 have been identified as key regulators of c-Myc turnover [22]. The balance between these enzymes determines c-Myc protein levels and consequently its transcriptional activity. Skp2 promotes cell growth and exhibits oncogenic properties, while Fbw7 acts as a tumor suppressor by targeting c-Myc for degradation [22]. ARF-BP1/HectH9 similarly promotes cell growth and may function as an oncogene [22].
Recent research has identified the OTUB1-TRIM28 ubiquitination axis as a crucial regulator of MYC pathway activity [10]. This regulatory module influences cancer cell fate by modulating MYC and its downstream targets while altering oxidative stress responses, ultimately contributing to immunotherapy resistance and poor patient prognosis [10]. The ubiquitination score derived from this regulatory network positively correlates with squamous or neuroendocrine transdifferentiation in adenocarcinoma, highlighting the clinical relevance of MYC ubiquitination in tumor progression and subtype specification [10].
RAS Ubiquitination and Signaling Modulation
RAS proteins, representing the most frequently mutated oncoproteins in human cancers, are subject to complex ubiquitination regulation that controls their stability, membrane localization, and signaling transduction [24]. The ubiquitination of RAS proteins exhibits significant heterogeneity across different isoforms (KRAS4A, KRAS4B, NRAS, and HRAS), contributing to their functional disparities in cancer pathogenesis [24]. This regulatory mechanism profoundly impacts RAS-driven oncogenic functions, including tumor proliferation, metastasis, and therapeutic resistance.
The functional consequences of RAS ubiquitination extend beyond protein degradation, encompassing modulation of GTPase activity, subcellular localization, and interaction with effector proteins. This regulatory complexity presents both challenges and opportunities for therapeutic intervention in RAS-driven cancers. Current research efforts are focused on exploiting the ubiquitination pathway to develop novel strategies to overcome RAS-driven malignant phenotypes, particularly through combination approaches with direct RAS inhibitors or immunotherapy [24].
Table 2: Ubiquitin Linkage Types and Their Functional Consequences in Oncogenic Regulation
| Ubiquitin Linkage | Primary Functions | Oncogenic Pathway Examples |
|---|---|---|
| K48 | Proteasomal degradation | p53 degradation by MDM2 |
| K63 | Activity and localization regulation | DNA damage response, kinase activation |
| K11 | Cell cycle regulation, trafficking | β-catenin stabilization in colorectal cancer |
| K29 | Uncertain, potential degradation role | Uncertain in oncogenic pathways |
| K6 | DNA damage repair | Uncertain in oncogenic pathways |
| K27 | Mitochondrial autophagy | Regulation of mitophagy |
| M1 | NF-κB signaling activation | Inflammatory response regulation |
Quantitative Analysis of Ubiquitination Patterns in Cancer
Comprehensive pan-cancer analyses have revealed consistent dysregulation of ubiquitination pathways across multiple cancer types. A study integrating data from 4,709 patients across 26 cohorts and five solid tumor types (lung cancer, esophageal cancer, cervical cancer, urothelial cancer, and melanoma) identified key nodes and prognostic pathways within the ubiquitination-modification network [10]. This research established a conserved ubiquitination-related prognostic signature (URPS) that effectively stratified patients into high-risk and low-risk groups with distinct survival outcomes across all analyzed cancers [10].
The clinical utility of ubiquitination signatures extends beyond prognostic stratification. URPS demonstrates significant potential as a novel biomarker for predicting immunotherapy response, with the capacity to identify patients most likely to benefit from immunotherapy in clinical settings [10]. Analysis of URPS-associated proteins has revealed novel cancer-related interaction partners as potential drug targets, expanding the therapeutic landscape for ubiquitination-focused interventions [10].
In ovarian cancer, a prognostic model based on 17 ubiquitination-related genes demonstrated high predictive performance (1-year AUC = 0.703, 3-year AUC = 0.704, 5-year AUC = 0.705) [21]. Patients in the high-risk group had significantly lower overall survival, and immune analysis revealed distinct tumor microenvironment profiles between risk groups, with the low-risk group showing higher levels of CD8+ T cells, M1 macrophages, and follicular helper cells [21]. This model further identified distinct mutation patterns between risk groups, with high-risk patients having more mutations in MUC17 and LRRK2, while low-risk patients had more RYR2 mutations [21].
Table 3: Ubiquitination-Related Prognostic Models Across Cancer Types
| Cancer Type | Number of Genes in Signature | Predictive Performance (AUC) | Clinical Utility |
|---|---|---|---|
| Multiple Cancers (Pan-cancer) | URPS (unspecified number) | Not specified | Stratifies patients into high/low risk groups, predicts immunotherapy response |
| Ovarian Cancer | 17 | 1-year: 0.703, 3-year: 0.704, 5-year: 0.705 | Prognostic stratification, immune microenvironment characterization |
| Colorectal Cancer | USP48-focused | Not specified | Associated with autophagy inhibition, promotes proliferation, migration, and invasion |
Experimental Protocols for Ubiquitination Research
Ubiquitination Regulatory Network Construction
The construction of pancancer ubiquitination regulatory networks involves systematic integration of multi-omics data from large patient cohorts. A standardized methodology includes the following steps [10]:
Data Collection and Integration: Collect RNA-seq data and clinicopathological features from relevant cancer databases (e.g., TCGA, GEO). For immunotherapy-focused studies, include datasets from patients receiving immune checkpoint inhibitors.
Network Mapping: Map molecular profiles to interaction networks using correlation coefficient matrices standardized through significance screening (p-value < 0.05).
Prognostic Analysis: Employ Cox regression and Kaplan-Meier survival analysis for prognostic assessment of ubiquitination scores. Apply LASSO algorithm to identify key prognostic genes.
Functional Validation: Validate findings using independent patient cohorts, cell line models, and in vivo experiments to confirm biological significance.
Ubiquitination Assay Protocols
Several experimental approaches are essential for characterizing ubiquitination events in cancer pathways:
Co-immunoprecipitation and Ubiquitination Assays [25]:
- Transfect cells with plasmids encoding the E3 ligase (e.g., FBXO22) and potential substrate (e.g., KLF10)
- Treat cells with proteasome inhibitor (e.g., MG132) for 4-6 hours before harvesting to stabilize ubiquitinated proteins
- Lyse cells in RIPA buffer containing protease and deubiquitinase inhibitors
- Perform immunoprecipitation with antibody against the substrate protein
- Analyze ubiquitination by western blotting with anti-ubiquitin antibody
In Vivo Ubiquitination Assay:
- Express His-tagged ubiquitin in cells along with the E3 ligase and substrate
- Harvest cells under denaturing conditions (6M guanidine-HCl)
- Purify His-ubiquitinated proteins using nickel-nitrilotriacetic acid (Ni-NTA) beads
- Detect specific substrate ubiquitination by western blotting
Functional Validation Assays:
- Conduct proliferation assays (CCK-8, colony formation)
- Perform invasion assays (Transwell with Matrigel)
- Analyze apoptosis (Annexin V staining)
- Validate in vivo using xenograft models in immunodeficient mice
Visualization of Ubiquitination Pathways
p53 Ubiquitination Regulation Network
Diagram 1: p53 Ubiquitination Regulation Network. Multiple E3 ubiquitin ligases, particularly MDM2, target p53 for ubiquitination and subsequent proteasomal degradation under normal conditions. Cellular stress stabilizes p53 by disrupting this regulatory balance [22] [23].
MYC-OTUB1-TRIM28 Regulatory Axis
Diagram 2: MYC-OTUB1-TRIM28 Regulatory Axis. The OTUB1-TRIM28 ubiquitination complex modulates MYC pathway activity and oxidative stress responses, driving histological transdifferentiation and therapy resistance [10].
The Scientist's Toolkit: Essential Research Reagents
Table 4: Essential Research Reagents for Ubiquitination Studies
| Reagent Category | Specific Examples | Research Application | Key Functions |
|---|---|---|---|
| E3 Ligase Inhibitors | Nutlin, MI-219 (MDM2 inhibitors) | p53 pathway studies | Block MDM2-p53 interaction, stabilize p53 |
| Proteasome Inhibitors | Bortezomib, Carfilzomib, MG132 | Ubiquitination assays | Stabilize ubiquitinated proteins by blocking degradation |
| Ubiquitin System Modulators | MLN7243 (E1 inhibitor), MLN4924 (NEDD8-activating enzyme inhibitor) | Pathway validation | Block ubiquitin activation or neddylation pathway |
| Deubiquitinase Inhibitors | Compounds G5 and F6 | DUB functional studies | Inhibit deubiquitinating enzyme activity |
| Expression Plasmids | His-tagged ubiquitin, E3 ligase constructs, substrate genes | In vivo ubiquitination assays | Enable detection and manipulation of ubiquitination |
| Cell Line Models | BJ fibroblasts with inducible H-RASV12 and MycER | Oncogene cooperation studies | Study senescence and apoptosis in controlled systems |
| Antibodies | Anti-ubiquitin, anti-substrate specific, anti-E3 ligases | Immunoprecipitation, western blot | Detect ubiquitination and protein interactions |
Therapeutic Implications and Drug Development
Targeting ubiquitination pathways represents a promising strategic approach for anticancer drug development, particularly for addressing traditionally "undruggable" targets like MYC [10]. Several therapeutic classes have emerged:
Proteasome Inhibitors: Bortezomib, carfilzomib, oprozomib, and ixazomib have demonstrated tangible clinical success, particularly in hematological malignancies, by disrupting protein homeostasis and inducing endoplasmic reticulum stress [14] [12].
E1-Targeting Compounds: MLN7243 and MLN4924 inhibit E1 enzymes, with MLN4924 specifically blocking the NEDD8-activating enzyme to modulate cullin-RING ligase activity [12].
E2-Targeting Agents: Leucettamol A and CC0651 represent early-stage inhibitors targeting specific E2 enzymes [12].
E3-Targeting Strategies: Nutlin and MI-219 specifically disrupt MDM2-p53 interaction, stabilizing p53 in cancers with wild-type TP53 [12]. Emerging PROTAC (Proteolysis-Targeting Chimera) technology leverages E3 ligases to selectively degrade target proteins, with 50 ubiquitination-related genes currently targeted by PROTACs in development [21].
DUB Inhibitors: Compounds G5 and F6 represent early-stage inhibitors of deubiquitinating enzyme activity [12].
The therapeutic potential of targeting ubiquitination pathways extends beyond direct anticancer effects to modulating immunotherapy response. Recent research indicates that ubiquitination scores may predict immunotherapy efficacy, offering opportunities for patient stratification and combination therapy development [10]. Furthermore, the identification of specific ubiquitination regulators like USP48 in colorectal cancer provides novel targets for intervention, with preliminary success demonstrated using tetrahedral DNA nanomaterials loaded with USP48 siRNA [26].
Ubiquitination represents a master regulatory mechanism that orchestrates the activity of fundamental oncogenic pathways, including MYC, RAS, and p53. The intricate balance of E3 ligases and deubiquitinases that control these pathways offers unprecedented opportunities for therapeutic intervention in cancer. Quantitative ubiquitination signatures demonstrate robust prognostic and predictive value across diverse cancer types, while emerging technologies like PROTACs leverage the ubiquitin-proteasome system for targeted protein degradation. Future research directions should focus on elucidating the context-specific functions of ubiquitination regulators, developing isoform-selective ubiquitination modulators, and exploring rational combination therapies that exploit ubiquitination dependencies in cancer cells. The systematic characterization of ubiquitination networks presented in this review provides a foundation for advancing these efforts and overcoming the therapeutic challenges posed by traditionally intractable oncogenic drivers.
The ubiquitin-proteasome system (UPS) represents a sophisticated regulatory mechanism that governs protein stability and function through post-translational modification. In cancer, this system undergoes profound dysregulation, leading to the aberrant degradation of tumor suppressor proteins that normally maintain cellular homeostasis. This review examines the molecular mechanisms underlying tumor suppressor destabilization, focusing on the E3 ubiquitin ligases and deubiquitinating enzymes that orchestrate these processes. We explore how cancer cells exploit the ubiquitin network to eliminate key protective proteins, thereby gaining proliferative advantages, evading growth suppression, and resisting therapeutic interventions. The clinical implications of these mechanisms are substantial, offering novel avenues for targeted therapeutic strategies aimed at restoring tumor suppressor function through modulation of ubiquitination pathways.
The ubiquitin-proteasome system serves as the primary pathway for controlled protein degradation in eukaryotic cells, regulating approximately 80-90% of cellular proteolysis [6]. This sophisticated system employs a sequential enzymatic cascade to mark specific proteins for destruction: ubiquitin-activating enzymes (E1) initiate the process through ATP-dependent ubiquitin activation, ubiquitin-conjugating enzymes (E2) serve as intermediaries, and ubiquitin ligases (E3) provide substrate specificity by recognizing target proteins and facilitating ubiquitin transfer [27] [6]. The resulting polyubiquitin chains, particularly those linked through lysine 48 (K48) of ubiquitin, signal the 26S proteasome to degrade the tagged protein into small peptides [28].
Beyond its role in protein quality control, the UPS precisely regulates the abundance of critical regulatory proteins, including tumor suppressors that constrain uncontrolled cell growth. The specificity of ubiquitination primarily resides with E3 ubiquitin ligases, which recognize distinct degradation signals (degrons) on target proteins [29]. The human genome encodes over 600 E3 ligases, each capable of binding specific subsets of substrates, thereby creating an intricate network of protein stability control [30]. This system is counterbalanced by deubiquitinating enzymes (DUBs), which remove ubiquitin chains and can rescue proteins from degradation, adding another layer of regulation [28] [6].
In cancer pathogenesis, tumor cells frequently hijack this精密调控system to selectively eliminate tumor suppressor proteins. Through overexpression of specific E3 ligases, downregulation of protective DUBs, or mutation of ubiquitination sites on tumor suppressors, cancer cells achieve uncontrolled proliferation and survival [29]. Understanding these mechanisms provides crucial insights for developing novel cancer therapies that target the ubiquitin network to restore tumor suppressor function.
Molecular Mechanisms of Aberrant Ubiquitination in Cancer
Ubiquitin Chain Topology and Functional Diversity
Ubiquitination represents a versatile regulatory mechanism whose functional outcome depends critically on the topology of the ubiquitin chain formed on substrate proteins. The eight linkage types (K6, K11, K27, K29, K33, K48, K63, and M1) create a sophisticated "ubiquitin code" that determines the fate of modified proteins [6]. K48-linked polyubiquitin chains predominantly target proteins for proteasomal degradation and serve as the principal mechanism for tumor suppressor destruction [28]. In contrast, K63-linked chains typically mediate non-proteolytic functions, including signal transduction, DNA repair, and endocytic trafficking, while monoubiquitination can regulate protein activity, localization, and interactions [28] [6].
Cancer cells exploit this ubiquitin code to eliminate tumor suppressors through multiple mechanisms. The contextual duality of certain E3 ligases allows them to function as either oncogenes or tumor suppressors depending on cellular context. FBXW7 exemplifies this complexity: in p53-wild type colorectal tumors, it promotes radioresistance by degrading p53, whereas in non-small cell lung cancer with SOX9 overexpression, it enhances radiosensitivity by destabilizing SOX9 and alleviating p21 repression [28]. This functional switching hinges on tumor-specific genetic backgrounds and signaling microenvironments, highlighting the nuanced regulation of ubiquitination in cancer.
The spatial and temporal control of ubiquitination further contributes to its functional diversity. Linear ubiquitination (M1-linked), assembled exclusively by the linear ubiquitin chain assembly complex (LUBAC), activates NF-κB signaling and promotes lymphoma progression [6]. Additionally, heterotypic ubiquitin chains (mixed or branched) increase the complexity of ubiquitin signaling, although their roles in tumor suppressor regulation remain incompletely characterized [6].
E3 Ubiquitin Ligases in Tumor Suppressor Degradation
E3 ubiquitin ligases serve as the critical determinants of specificity in the ubiquitination cascade, recognizing particular tumor suppressor proteins and facilitating their ubiquitination. These enzymes fall into three major classes: RING, HECT, and RBR ligases, each employing distinct catalytic mechanisms [31]. The RING-type E3 ligase MDM2 (HDM2 in humans) represents the most extensively characterized regulator of p53 stability. MDM2 binds directly to p53, inhibiting its transcriptional activity and promoting its polyubiquitination and nuclear export [29]. The biological significance of this interaction is underscored by studies demonstrating that Mdm2-null mice die early in development, but this embryonic lethality is rescued by co-disruption of the Tp53 gene [29].
Other E3 ligases contribute to the regulation of diverse tumor suppressor proteins. UBE3A (E6AP), in partnership with the HPV E6 oncoprotein, targets p53 for degradation in HPV-associated cancers [29]. The LUBAC complex, comprising HOIP, HOIL-1L, and SHARPIN, mediates linear ubiquitination of signaling components and promotes NF-κB activation in lymphoma [6]. RNF2 monoubiquitinates histone H2A at lysine 119, leading to transcriptional repression of E-cadherin and enhanced metastatic potential in hepatocellular carcinoma [6].
The regulation of E3 ligase activity itself represents a critical control point in tumor suppressor stability. MDM2 activity depends on its association with MDMX/MDM4, while phosphorylation of MDM2 by ATM kinase inhibits its function in response to DNA damage, promoting p53 stabilization [29]. Furthermore, many E3 ligases participate in autoregulatory feedback loops; for instance, MDM2 is itself a transcriptional target of p53, creating an oscillatory circuit that maintains p53 at appropriate levels in normal cells [29].
Deubiquitinating Enzymes as Tumor Suppressor Stabilizers
Deubiquitinating enzymes (DUBs) counterbalance E3 ligase activity by removing ubiquitin chains from substrate proteins, thereby preventing proteasomal degradation. Approximately 100 DUBs encoded in the human genome regulate diverse cellular processes, and their dysregulation contributes significantly to tumor suppressor destabilization in cancer [28]. The USP family of DUBs demonstrates particularly important roles in tumor suppressor regulation. USP14 stabilizes ALKBH5 to maintain glioblastoma stemness but degrades IκBα to activate NF-κB in head and neck cancers, illustrating the context-dependent functions of these enzymes [28].
Other DUB families also participate in tumor suppressor stabilization. OTUB1 stabilizes CHK1 to enhance DNA repair fidelity in lung cancer and stabilizes GPX4 to suppress ferroptosis in gastric cancer [28]. USP7 stabilizes CHK1 to maintain genomic stability in breast cancer and counteracts ubiquitination of DNA-PKcs to maintain repair competence in HPV-positive tumors [28]. UCHL1 stabilizes HIF-1α to activate the pentose phosphate pathway and enhance antioxidant defense in breast cancer [28].
The therapeutic targeting of DUBs presents both challenges and opportunities. While inhibition of specific DUBs could potentially stabilize tumor suppressors, functional redundancy among DUB family members may limit efficacy. Additionally, many DUBs exhibit tissue-specific or context-dependent functions, necessitating precise therapeutic strategies [28].
Table 1: Major E3 Ubiquitin Ligases in Tumor Suppressor Regulation
| E3 Ligase | Tumor Suppressor Target | Cancer Type | Functional Outcome |
|---|---|---|---|
| MDM2 | p53 | Various cancers with wild-type p53 | Promotes p53 degradation, enabling unchecked proliferation |
| UBE3A (with HPV E6) | p53 | HPV-associated cancers | Viral oncoprotein-directed p53 degradation |
| FBXW7 | p53, SOX9 | Colorectal cancer, NSCLC | Context-dependent roles in radioresistance or sensitization |
| RNF2 | Histone H2A (K119) | Hepatocellular carcinoma | Transcriptional repression of E-cadherin, enhanced metastasis |
| LUBAC complex | NEMO, other NF-κB signaling components | B-cell lymphoma | Linear ubiquitination and NF-κB activation |
| β-TrCP | Radioprotective LZTS3 | Lung cancer | K48-linked degradation enhances radiation sensitivity |
Key Signaling Pathways and Experimental Analysis
The p53-MDM2 Axis as Paradigm
The regulatory circuit between p53 and MDM2 represents the prototypical example of ubiquitin-mediated tumor suppressor control. This axis exemplifies the sophisticated feedback mechanisms that maintain cellular homeostasis in normal cells and the vulnerability of this system to hijacking in cancer. In normal physiology, p53 activates MDM2 transcription, creating a negative feedback loop that prevents excessive p53 accumulation [29]. Cellular stress signals, such as DNA damage, disrupt this interaction through phosphorylation of both proteins, leading to p53 stabilization and activation of cell cycle arrest, apoptosis, or senescence programs [29].
Cancer cells subvert this regulatory circuit through multiple mechanisms. MDM2 amplification occurs in numerous cancers, resulting in excessive p53 degradation even in the presence of wild-type TP53 genes [29]. Additionally, MDM2 polymorphisms that enhance its expression or activity have been associated with accelerated tumorigenesis [29]. The physical interaction between p53 and MDM2 is driven by key residues of p53 (Phe19, Trp23, Leu26) in its N-terminal transactivation domain burying into a hydrophobic cleft in the N-terminal domain of MDM2 [29]. This precise molecular interaction has enabled the development of therapeutic inhibitors that disrupt the p53-MDM2 interface.
The following diagram illustrates the core regulation and cancer hijacking of the p53-MDM2 axis:
DNA Damage Response Pathway Ubiquitination
The DNA damage response (DDR) represents another critical pathway regulated by ubiquitination that is frequently compromised in cancer. Multiple tumor suppressors in the DDR pathway, including BRCA1, CHK1, and ATM, undergo ubiquitin-mediated regulation. RNF126 catalyzes K63-linked ubiquitination to activate ATR-CHK1 signaling in triple-negative breast cancer, promoting radioresistance [28]. Conversely, USP14 disrupts non-homologous end joining (NHEJ) and promotes homologous recombination (HR) in non-small cell lung cancer, with USP14 inhibition disrupting DNA damage response [28].
The interplay between different ubiquitin chain types fine-tunes the DNA damage response. K63-linked ubiquitination of histone H2A and H2AX facilitates the recruitment of DNA repair proteins to damage sites, while K48-linked ubiquitination limits the duration of DDR activation by degrading key mediators [28]. Deubiquitinating enzymes such as USP7 and OTUB1 further modulate this process by stabilizing DDR components, with OTUB1 stabilizing CHK1 to enhance repair fidelity in lung cancer [28].
The following workflow maps the ubiquitin networks in DNA damage response and therapeutic targeting:
Therapeutic Targeting Strategies
Stabilization of Tumor Suppressor Proteins
Therapeutic strategies to stabilize tumor suppressor proteins primarily focus on inhibiting the E3 ubiquitin ligases responsible for their degradation. MDM2 inhibitors represent the most advanced approach, with multiple compounds in clinical development. Nutlin-3a, a cis-imidazoline derivative, was the first small-molecule inhibitor developed to target the p53-MDM2 interaction by mimicking the three key residues of p53 that bind MDM2's hydrophobic cleft [29]. Subsequent compounds, including RG7112, idasanutlin, and AMG-232, have improved potency and pharmacokinetic properties, with several advancing to clinical trials [29].
Combination therapies represent a promising approach to enhance the efficacy of E3 inhibitors. MDM2 inhibitors combined with chemotherapy agents demonstrate synergistic effects in preclinical models, particularly in tumors retaining wild-type p53 [29]. Additionally, co-targeting MDM2 and its homolog MDMX may overcome resistance mechanisms that limit single-agent efficacy [29]. The development of dual MDM2/MDMX inhibitors such as ALRN-6924 represents an innovative strategy to completely disrupt p53 regulation [29].
Beyond p53-directed therapies, efforts to target other tumor suppressor-E3 ligase axes are emerging. Inhibitors of the CRL4^CRBN complex, which degrades multiple tumor suppressive transcription factors, show promise in hematological malignancies [30]. Similarly, developing compounds that disrupt the interaction between HPV E6 and E6AP could restore p53 function in HPV-associated cancers [29].
Targeted Protein Degradation Technologies
Targeted protein degradation technologies, particularly PROteolysis-TArgeting Chimeras (PROTACs), represent a revolutionary approach to eliminate oncoproteins by hijacking the ubiquitin-proteasome system. PROTACs are heterobifunctional molecules consisting of a target protein-binding ligand connected via a linker to an E3 ligase-recruiting moiety [30]. This structure facilitates the formation of a ternary complex that brings the E3 ligase into proximity with the target protein, leading to its ubiquitination and degradation [30].
PROTACs offer several advantages over traditional inhibitors:
- Catalytic activity: A single PROTAC molecule can facilitate the degradation of multiple target protein molecules
- Targeting undruggable proteins: PROTACs can degrade proteins without defined active sites
- Overcoming resistance: Degradation eliminates all functions of the target protein, circumventing mutation-based resistance
Significant progress has been made in developing PROTACs that target oncoproteins. ARV-110 and ARV-471 represent pioneering PROTACs that target the androgen receptor and estrogen receptor, respectively, with both advancing to phase II clinical trials [6]. MDM2-recruiting PROTACs have demonstrated the ability to stabilize p53 by degrading oncogenic targets, leading to significant anti-proliferative effects in cancer cells without adversely affecting normal cells [30].
The following diagram illustrates the PROTAC mechanism compared to standard E3 inhibition:
Table 2: Experimental Toolkit for Studying Tumor Suppressor Ubiquitination
| Research Tool | Application | Key Features | Experimental Considerations |
|---|---|---|---|
| PROTAC molecules | Induce targeted protein degradation | Catalytic mode of action; targets "undruggable" proteins | Hook effect at high concentrations; molecular size affects permeability |
| MG-132 (and other proteasome inhibitors) | Block proteasomal degradation | Stabilizes ubiquitinated proteins; confirms UPS involvement | Broad-spectrum effects; cytotoxicity at prolonged exposures |
| CRISPR screening for E3 ligases/DUBs | Identify novel regulators of tumor suppressors | Genome-wide functional assessment; identifies dependencies | Validation required in multiple models; potential compensatory mechanisms |
| Ubiquitin variant libraries | Disrupt specific ubiquitin interactions | High specificity for particular E2-E3 pairs | Limited coverage of all possible interactions |
| Tandem Ubiquitin Binding Entities (TUBEs) | Isolate and analyze ubiquitinated proteins | Protects ubiquitin chains from DUBs; enrichment of polyUb proteins | May bias toward certain chain types; requires optimization |
| NEDD8-activating enzyme inhibitors | Block cullin-RING ligase activity | Specifically inhibits CRL family of E3 ligases | Affects multiple CRLs; potential pleiotropic effects |
Experimental Approaches and Methodologies
Assessing Tumor Suppressor Ubiquitination
The experimental analysis of tumor suppressor ubiquitination requires specialized methodologies to detect and characterize these transient modifications. Immunoprecipitation followed by immunoblotting remains the cornerstone technique, typically employing antibodies against the tumor suppressor protein under conditions that stabilize ubiquitin conjugates (e.g., proteasome inhibition). The appearance of higher molecular weight species on SDS-PAGE indicates ubiquitinated forms, with confirmation requiring ubiquitin immunoblotting or expression of epitope-tagged ubiquitin [27] [6].
Pulse-chase experiments provide critical information about tumor suppressor protein half-life and the impact of ubiquitination on turnover rates. By metabolically labeling proteins with radioactive amino acids and monitoring their decay over time, researchers can quantify stabilization or destabilization resulting from experimental manipulations of the ubiquitin system [29]. Combining this approach with proteasome inhibition helps distinguish UPS-mediated degradation from other proteolytic pathways.
In vitro ubiquitination assays reconstitute the ubiquitination cascade using purified E1, E2, and E3 enzymes, ubiquitin, and the tumor suppressor substrate. This reductionist approach establishes direct regulatory relationships and characterizes enzymatic mechanisms without confounding cellular factors [29]. Similarly, deubiquitination assays with purified DUBs demonstrate their ability to reverse tumor suppressor ubiquitination.
Advanced mass spectrometry techniques, particularly ubiquitin remnant profiling, enable system-wide identification of ubiquitination sites and quantification of modification dynamics. This approach employs anti-diglycine antibodies to enrich ubiquitin-derived peptides following tryptic digestion, allowing precise mapping of modification sites and relative quantification across experimental conditions [6].
Functional Validation of Ubiquitination Events
Establishing the functional consequences of tumor suppressor ubiquitination requires rigorous validation approaches. Mutagenesis of ubiquitination sites (lysine to arginine substitutions) represents the most direct method to assess the functional importance of specific modification sites. Rescue experiments with ubiquitination-deficient mutants can demonstrate whether impaired degradation underlies functional changes [29].
RNA interference and CRISPR-Cas9 approaches enable functional characterization of specific E3 ligases and DUBs in tumor suppressor regulation. Knockdown or knockout of candidate regulators followed by assessment of tumor suppressor stability and function establishes physiological relevance [28] [29]. Complementary overexpression studies can determine whether specific enzymes are sufficient to modulate tumor suppressor levels.
Animal models provide critical in vivo validation of ubiquitin-mediated tumor suppressor regulation. Genetically engineered mice with conditional knockout of E3 ligases or DUBs in specific tissues can reveal their roles in tumor suppression and tumorigenesis [29]. Xenograft models employing cancer cells with modulated expression of ubiquitin system components further establish therapeutic potential.
High-throughput screening approaches facilitate the discovery of small molecules that modulate tumor suppressor ubiquitination. Cell-based screens monitoring tumor suppressor protein levels or reporter activity can identify compounds that stabilize tumor suppressors by inhibiting their ubiquitination [29]. Direct binding assays such as surface plasmon resonance or thermal shift assays can confirm compound engagement with target E3 ligases.
The aberrant ubiquitination of tumor suppressor proteins represents a fundamental mechanism driving oncogenesis across diverse cancer types. Understanding the molecular players and regulatory principles governing this process has unveiled new therapeutic opportunities to restore tumor suppressor function. While significant progress has been made in targeting the p53-MDM2 axis, numerous other tumor suppressor-E3 ligase relationships remain underexplored as therapeutic targets.
Future research directions should prioritize several key areas:
- Comprehensive mapping of tumor suppressor ubiquitination networks across cancer types
- Development of selective inhibitors for oncogenic E3 ligases beyond MDM2
- Exploration of combination therapies that synergize with E3 inhibition
- Advanced delivery strategies for ubiquitin-targeting therapeutics
The expanding toolkit for modulating protein stability, including PROTACs, molecular glues, and DUB inhibitors, offers unprecedented opportunities to pharmacologically restore tumor suppressor function. As our understanding of the ubiquitin code deepens, so too will our ability to develop precision interventions that rewrite the ubiquitination programs driving tumor suppressor destruction in cancer.
Metabolic reprogramming is a established hallmark of cancer, enabling rapidly proliferating tumor cells to meet their heightened demands for energy, biosynthetic precursors, and cellular building blocks [32]. The ubiquitin-proteasome system (UPS) has emerged as a master regulator of this process, precisely controlling the stability and activity of key metabolic enzymes and signaling pathways [32] [33]. Ubiquitination, a versatile post-translational modification, extends beyond its canonical role in protein degradation to regulate diverse cellular processes including metabolic adaptation, tumor progression, and immune evasion [34]. This technical review examines the mechanisms by which ubiquitination governs cancer cell metabolism, with particular focus on glucose, lipid, and amino acid metabolic pathways, and explores the translational potential of targeting ubiquitin-related mechanisms for cancer therapy.
The Ubiquitin-Proteasome System: Molecular Machinery
Core Enzymatic Cascade
The ubiquitination process involves a sequential enzymatic cascade [32] [35]:
- E1 (Ubiquitin-activating enzyme): Initiates the pathway by activating ubiquitin in an ATP-dependent manner, forming a thioester bond between its catalytic cysteine residue and the C-terminal glycine of ubiquitin. Mammalian systems possess only two E1 enzymes, creating an initial bottleneck in the pathway.
- E2 (Ubiquitin-conjugating enzyme): Receives the activated ubiquitin from E1 via a trans-thioesterification reaction. Approximately 40 E2 enzymes exist in humans, providing moderate substrate specificity.
- E3 (Ubiquitin ligase): Catalyzes the final transfer of ubiquitin to lysine residues on target substrates. With over 600 members, E3 ligases confer exquisite substrate specificity and are classified into three major families based on their structural domains and mechanisms: RING (Really Interesting New Gene), HECT (Homologous to the E6AP Carboxyl Terminus), and RBR (RING-between-RING) ligases [34].
Table 1: Major E3 Ubiquitin Ligase Families and Characteristics
| Ligase Family | Mechanism of Action | Representative Members | Key Features |
|---|---|---|---|
| RING | Directly transfers ubiquitin from E2 to substrate | MDM2, CBL, FBXW7 | Largest family, often require adapter proteins for substrate recognition |
| HECT | Forms thioester intermediate with ubiquitin before substrate transfer | NEDD4, SMURF, E6AP | Catalytically active, can build diverse ubiquitin chains |
| RBR | Hybrid mechanism combining RING and HECT features | PARKIN, HOIP | Requires two-step catalytic process |
Ubiquitin Signaling Diversity
Ubiquitination generates diverse signals through different ubiquitin chain linkages [32]:
- K48-linked chains: Primarily target proteins for proteasomal degradation
- K63-linked chains: Regulate non-proteolytic functions including signal activation, protein trafficking, and DNA repair
- Mono-ubiquitination: Influences subcellular localization, protein activity, and endocytosis
- Atypical linkages (K6, K11, K27, K29, K33): Mediate specialized functions including mitophagy, cell cycle regulation, and immune signaling
Deubiquitinating Enzymes (DUBs)
Deubiquitinating enzymes constitute a diverse family of proteases that reverse ubiquitination by cleaving ubiquitin from modified substrates [32] [35]. DUBs are categorized into six subfamilies: ubiquitin-specific proteases (USPs), ubiquitin carboxyl-terminal hydrolases (UCHs), ovarian tumor proteases (OTUs), Machado-Joseph disease proteases (MJDs), motif interacting with ubiquitin-containing DUB family (MINDY), and JAMM/MPN+ metalloenzymes. These enzymes process ubiquitin precursors, recycle ubiquitin during proteasomal degradation, edit ubiquitin chains, and remove ubiquitin from substrate proteins, providing critical counter-regulation to E3 ligase activity.
Ubiquitination in Glucose Metabolic Reprogramming
Regulation of Glycolytic Enzymes
Cancer cells preferentially utilize glycolysis for energy production even under normoxic conditions, a phenomenon known as the Warburg effect [32]. Ubiquitination precisely regulates key glycolytic enzymes:
- Hexokinase 2 (HK2): The TRAF6 E3 ligase promotes K63-linked ubiquitination of HK2, enhancing its stability and enzymatic activity, thereby reinforcing glycolytic flux in glioma cells.
- Pyruvate Kinase M2 (PKM2): The CHIP E3 ligase (C-terminus of HSC70-interacting protein) mediates ubiquitination and degradation of PKM2, influencing the metabolic switch between glycolysis and oxidative phosphorylation.
- Phosphofructokinase-Platelet (PFKP): The SKP2 E3 ligase stabilizes PFKP through K63-linked ubiquitination, promoting glycolytic flow and breast cancer cell proliferation.
Control of Glucose Transporter and Signaling Pathways
The UPS regulates glucose uptake and metabolic signaling through multiple mechanisms:
- GLUT1 Stability: The membrane-associated RING-CH (MARCH) family E3 ligases control the ubiquitination and degradation of glucose transporter GLUT1, directly influencing glucose uptake capacity.
- HIF-1α Regulation: The VHL (von Hippel-Lindau) E3 ligase complex targets hypoxia-inducible factor 1α (HIF-1α) for proteasomal degradation under normoxic conditions. During hypoxia, HIF-1α stabilization promotes expression of glycolytic enzymes and glucose transporters.
- AMPK Signaling: The praja2 RING E3 ligase ubiquitylates and degrades kinase suppressor of Ras 2 (KSR2), subsequently restraining AMP-dependent protein kinase (AMPK) activity and attenuating oxidative metabolism in glioblastoma [36].
Table 2: Ubiquitination-Mediated Regulation of Key Metabolic Enzymes in Cancer
| Metabolic Pathway | Enzyme/Transporter | Regulating E3 Ligase/DUB | Functional Outcome |
|---|---|---|---|
| Glycolysis | HK2 | TRAF6 | K63-linked ubiquitination enhances stability and activity |
| Glycolysis | PKM2 | CHIP | Ubiquitination promotes degradation |
| Glycolysis | PFKP | SKP2 | K63-linked ubiquitination enhances stability |
| Lipid Synthesis | ACLY | NEDD4, UBR4, CUL3/KLHL25 | Degradation via K48-linked ubiquitination |
| Lipid Synthesis | FASN | COP1, TRIM21, SPOP | Degradation via K48-linked ubiquitination |
| Fatty Acid Uptake | CD36 | Multiple E3 ligases | Regulates membrane abundance and function |
| Cholesterol Synthesis | HMGCR | GP78, TRC8 | Degradation feedback regulation |
Ubiquitination in Lipid Metabolism Rewiring
Regulation of Fatty Acid Synthesis Enzymes
Lipid metabolic reprogramming in cancer involves enhanced de novo lipogenesis to support membrane biosynthesis and energy storage [34] [35]. Ubiquitination plays a crucial role in regulating key lipogenic enzymes:
- ACLY (ATP-citrate lyase): Multiple E3 ligases including NEDD4, UBR4, and the CUL3/KLHL25 complex target ACLY for ubiquitin-mediated degradation, thereby controlling the critical step of cytosolic acetyl-CoA production from citrate [35]. ACLY stability is further modulated by acetylation-deacetylation cycles that influence its interaction with E3 ligases.
- FASN (Fatty acid synthase): The COP1 E3 ligase, facilitated by Shp2 as an adapter, promotes FASN ubiquitination and degradation. Additionally, deacetylation of FASN by HDAC3 enhances its binding with TRIM21 E3 ligase, leading to reduced lipogenesis and inhibited cancer cell growth [35].
- SCD1 (Stearoyl-CoA desaturase 1): The FBXW7 E3 ligase targets SCD1 for degradation, modulating the balance between saturated and unsaturated fatty acids.
Control of Cholesterol Homeostasis and Lipid Uptake
Cholesterol metabolism and extracellular lipid acquisition are equally critical for cancer cell proliferation:
- HMGCR (3-Hydroxy-3-methylglutaryl-coenzyme A reductase): This rate-limiting enzyme in cholesterol synthesis is targeted by GP78 and TRC8 E3 ligases, providing feedback regulation based on cellular sterol levels [35].
- CD36 fatty acid transporter: Ubiquitination regulates CD36 membrane abundance and function, influencing fatty acid uptake and utilization in cancer cells [34].
- SREBP transcription factors: These master regulators of lipogenic gene expression are controlled by multiple ubiquitin ligases including Fbw7 and RNF145, which respond to cellular sterol status.
Experimental Methodologies for Investigating Ubiquitination in Cancer Metabolism
Ubiquitination Assay Protocols
In Vivo Ubiquitination Assay
Purpose: To detect ubiquitination of endogenous or exogenously expressed proteins in cellular systems.
Procedure:
- Transfert cells with expression plasmids for target protein, ubiquitin, and relevant E3 ligase or control vector.
- Treat cells with proteasome inhibitor (e.g., MG132, 10-20 μM for 4-6 hours) prior to harvesting to prevent degradation of ubiquitinated species.
- Lyse cells in RIPA buffer supplemented with N-ethylmaleimide (NEM, 10-25 mM) to inhibit deubiquitinating enzymes.
- Perform immunoprecipitation of target protein using specific antibody and protein A/G beads.
- Analyze immunoprecipitates by SDS-PAGE and immunoblotting with anti-ubiquitin antibody.
- Reverse membrane and reprobe with antibody against target protein to confirm equal precipitation.
Key Controls:
- Include ligase-deficient E3 mutant as negative control
- Test ubiquitin K48R and K63R mutants to determine chain linkage specificity
- Include sample without proteasome inhibitor to demonstrate degradation
In Vitro Ubiquitination Assay
Purpose: To reconstitute ubiquitination using purified components and demonstrate direct substrate targeting.
Procedure:
- Purify recombinant E1, E2, E3, ubiquitin, and substrate proteins.
- Set up reaction mixture containing: 50 mM Tris-HCl (pH 7.5), 2 mM ATP, 5 mM MgCl₂, 0.5 mM DTT, 10-50 nM E1, 100-500 nM E2, 500 nM-1 μM E3, 10-20 μM ubiquitin, and 1-2 μM substrate protein.
- Incubate at 30°C for 1-3 hours.
- Terminate reaction by adding SDS-PAGE sample buffer.
- Analyze by immunoblotting with anti-substrate and anti-ubiquitin antibodies.
Variations:
- Use different E2 enzymes to determine chain linkage specificity
- Incorporate different ubiquitin mutants (K48-only, K63-only) to establish chain topology
Metabolic Phenotyping coupled with Ubiquitination Manipulation
Purpose: To determine functional consequences of ubiquitination on cellular metabolism.
Procedure:
- Generate stable knockdown or knockout of specific E3 ligases/DUBs using shRNA or CRISPR/Cas9 systems.
- Validate target depletion by immunoblotting and assess effects on substrate protein stability.
- Perform metabolic profiling:
- Seahorse Extracellular Flux Analysis: Measure extracellular acidification rate (ECAR) and oxygen consumption rate (OCR) to assess glycolytic flux and mitochondrial respiration.
- Isotope Tracing: Use 13C-labeled glucose, glutamine, or fatty acids to track nutrient utilization through metabolic pathways.
- Lipidomic Analysis: Quantify lipid species composition and abundance by mass spectrometry.
- Cholesterol Measurement: Apply enzymatic or chromatographic methods to assess cellular cholesterol content.
Integration: Correlate ubiquitination status of metabolic enzymes with functional metabolic outputs to establish mechanistic links.
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Research Reagents for Investigating Ubiquitination in Cancer Metabolism
| Reagent Category | Specific Examples | Key Applications | Considerations |
|---|---|---|---|
| Proteasome Inhibitors | MG132, Bortezomib, Carfilzomib | Stabilize ubiquitinated proteins for detection, study proteasome-dependent degradation | MG132 for experimental use; Bortezomib for clinical relevance |
| Deubiquitinase Inhibitors | PR-619 (broad-spectrum), P5091 (USP7-specific), ML364 (USP2-specific) | Investigate DUB functions in metabolic regulation | Varying specificity profiles require careful control experiments |
| E3 Ligase Modulators | MLN4924 (NAE inhibitor), Nutlin-3 (MDM2 inhibitor), HLI373 (HDM2 inhibitor) | Target specific E3 ligase families or individual ligases | MLN4924 blocks neddylation, affecting CRL ligase activity |
| Ubiquitin Mutants | K48-only, K63-only, K48R, K63R, Ub(G76V) | Determine chain linkage specificity and function | K48R and K63R act as dominant-negative mutants |
| Metabolic Assay Kits | Seahorse XF Glycolysis Stress Test, Cholesterol/Triglyceride Quantification Kits, ATP Assay Kits | Functional metabolic phenotyping | Normalize to protein/cell number for accurate comparisons |
| Tagged Ubiquitin Constructs | HA-Ub, FLAG-Ub, Myc-Ub, GFP-Ub | Detect ubiquitinated proteins in pulldown and imaging experiments | Tandem tags (e.g., HA-FLAG) enable sequential purification |
| CRISPR Libraries | E3 ligase-focused, DUB-focused, whole genome | High-throughput screening for ubiquitination regulators | Use metabolic reporters (e.g., glucose consumption, lipid accumulation) for phenotypic screening |
Therapeutic Targeting and Clinical Implications
Targeting UPS Components in Cancer Metabolism
The strategic targeting of ubiquitination pathways offers promising therapeutic opportunities:
- Proteasome Inhibitors: Bortezomib and carfilzomib are FDA-approved for multiple myeloma and mantle cell lymphoma, demonstrating clinical efficacy partially through disruption of cancer metabolic pathways [33].
- E3 Ligase Modulators: Molecular glues and PROTACs (Proteolysis-Targeting Chimeras) represent emerging technologies that redirect E3 ligase activity toward specific oncoproteins and metabolic enzymes [33].
- DUB Inhibitors: Small molecule inhibitors targeting USP7, USP14, and UCHL1 are under investigation for their ability to modulate cancer-relevant metabolic pathways.
Case Study: Targeting Praja2 in Glioblastoma
A compelling example of therapeutic targeting comes from glioblastoma research [36]. The E3 ligase praja2 is overexpressed in IDH1 wild-type GBM lesions and promotes tumor growth by degrading KSR2, resulting in suppressed AMPK activity and attenuated oxidative metabolism. Experimental therapeutic approach:
- Target Validation: Demonstrated preferential praja2 expression in primary GBM tissues carrying wild-type IDH1 compared to mutant IDH1 low-grade gliomas.
- Mechanistic Elucidation: Identified direct interaction between praja2 and KSR2, with praja2 mediating KSR2 ubiquitination and degradation.
- Therapeutic Development: Employed transferrin-targeted self-assembling nanoparticles (SANPs) to deliver siRNA targeting praja2 to the brain.
- Efficacy Assessment: Showed that praja2 knockdown prevented KSR2 degradation, inhibited GBM growth, reduced tumor size, and prolonged survival in mouse models.
This case demonstrates the feasibility of targeting ubiquitin-related metabolic regulators and highlights nanoparticle-mediated RNA delivery as a promising strategy for challenging malignancies like GBM.
Ubiquitination-mediated control of cancer cell metabolism represents a rapidly advancing field with significant basic science and translational implications. The precise regulation of metabolic enzymes and pathways by the UPS enables cancer cells to adapt to nutrient availability, hypoxic stress, and therapeutic challenges. Future research directions should include:
- Systematic Mapping: Comprehensive identification of ubiquitination substrates in specific metabolic pathways across different cancer types.
- Context Dependency: Understanding how tissue of origin, oncogenic drivers, and tumor microenvironment influence ubiquitination-mediated metabolic regulation.
- Therapeutic Development: Advancing isoform-specific UPS-targeting agents with improved pharmacological properties and tissue-specific delivery.
- Combination Strategies: Rational design of therapies combining UPS-targeting agents with conventional chemotherapy, radiation, or other metabolic inhibitors.
The integration of ubiquitination biology with cancer metabolism research continues to reveal novel regulatory mechanisms and therapeutic vulnerabilities, offering promising avenues for innovative cancer treatments.
The tumor microenvironment (TME) is a complex ecosystem comprising tumor cells, non-tumor cells, and critical non-cellular components that collectively influence tumor progression and therapeutic response [37]. Within this intricate landscape, ubiquitination has emerged as a pivotal post-translational modification that governs protein stability, function, and localization in virtually all cellular processes. As a substantial part of post-translational protein modification, ubiquitination serves as a crucial player in maintaining protein stability during cell signaling, cell growth, and a series of cellular life activities, making it essential for regulating both tumor cells and non-tumor cells in the TME [37]. The ubiquitin-proteasome system (UPS), comprising E1 activating enzymes, E2 conjugating enzymes, and E3 ligases, along with deubiquitinating enzymes (DUBs), precisely controls substrate modification through a reversible enzymatic cascade [37]. Recent advances have illuminated how ubiquitination modulates immune cell function within the TME, creating either permissive or restrictive environments for tumor growth. This regulatory mechanism affects immune recognition, cytokine signaling, and cellular differentiation, positioning the ubiquitin system as a critical determinant of anti-tumor immunity and a promising therapeutic target for cancer intervention [38].
Molecular Mechanisms of Ubiquitin Signaling
The Ubiquitination Machinery
Ubiquitin modification involves a coordinated enzymatic cascade that tags target proteins with ubiquitin molecules, fundamentally altering their fate and function. The process begins with E1 ubiquitin-activating enzymes that initiate the cascade through ATP-dependent ubiquitin activation. The activated ubiquitin is then transferred to E2 ubiquitin-conjugating enzymes, which subsequently collaborate with E3 ubiquitin ligases to mediate substrate-specific ubiquitination [37]. The human genome encodes approximately 40 E2s and over 600 E3 ligases, providing tremendous specificity in substrate recognition and regulatory potential [8].
E3 ubiquitin ligases are categorized into three major families based on their structural characteristics and operational mechanisms: RING (really interesting new gene) E3s, HECT (homologous to E6-AP carboxyl terminus) E3s, and RBR (RING-between-RING) E3s [37]. RING E3s facilitate the direct transfer of ubiquitin from E2 to substrate lysine residues, while HECT and RBR E3s form catalytic intermediates by transferring ubiquitin to a conserved cysteine residue before substrate modification. This enzymatic diversity enables precise control over protein stability, interaction networks, and functional states of immune cells within the TME.
The reverse reaction, deubiquitination, is equally crucial for maintaining ubiquitin homeostasis and dynamic signaling. Deubiquitinating enzymes (DUBs) remove ubiquitin molecules from substrate proteins by hydrolyzing peptide or isopeptide bonds at the carboxyl-terminal end of ubiquitin [37]. Based on sequence and structural domain characteristics, DUBs are classified into five families: UCH (ubiquitin carboxy-terminal hydrolases), USP/UBP (ubiquitin-specific protease and ubiquitin-binding protein), OTU (ovarian tumor proteases), MJD (Machado-Joseph domain), and JAMM (JAB1/MPN/MOV34) families [37].
Ubiquitin Code Diversity and Signaling Outcomes
Ubiquitination generates remarkable functional diversity through different ubiquitin chain architectures. When a single ubiquitin molecule is added to a substrate's lysine residue, monoubiquitination occurs, typically affecting protein localization and interactions. In polyubiquitination, ubiquitin molecules are added to a single ubiquitin molecule to form polyubiquitin chains [37]. The seven lysine residues in ubiquitin (K6, K11, K27, K29, K33, K48, and K63) enable formation of structurally and functionally distinct polyubiquitin chains.
K48-linked and K11-linked polyubiquitin chains primarily mediate proteasomal degradation, representing the canonical fate for many ubiquitinated proteins. In contrast, K63-linked polyubiquitination is typically less common in tumors and is usually not involved in proteasomal degradation but is associated with cellular signal assembly, transduction, and repair of damaged cells [37]. This non-degradative ubiquitination serves as a platform for assembling signaling complexes and modulating pathway activation, particularly in immune signaling networks.
Figure 1: Ubiquitin Signaling Cascade. The enzymatic cascade of ubiquitination involving E1, E2, and E3 enzymes, and the opposing action of deubiquitinating enzymes (DUBs), leading to either proteasomal degradation or signaling activation depending on ubiquitin chain topology.
Ubiquitin-Mediated Regulation of Immune Cells in the TME
Myeloid Cell Regulation
Myeloid cells, including tumor-associated macrophages (TAMs), dendritic cells (DCs), and myeloid-derived suppressor cells (MDSCs), undergo extensive ubiquitin-mediated programming within the TME. TREM2 (Triggering Receptor Expressed on Myeloid Cells 2) has emerged as a key regulator of myeloid cell function, with TREM2+ TAMs exhibiting potent immunosuppressive properties [39]. TREM2 signaling depends on its association with the adapter protein DAP12, which contains an immunoreceptor tyrosine-based activation motif (ITAM) that recruits spleen tyrosine kinase (SYK) upon phosphorylation. This triggers downstream signaling cascades including PI3K/AKT, NF-κB, and ERK pathways, ultimately promoting an immunosuppressive phenotype [39].
The PI3K/AKT/mTOR pathway activated by TREM2 signaling supports metabolic adaptation in myeloid cells, enhancing lipid metabolism and oxidative phosphorylation to sustain immune suppression in the nutrient-deprived TME [39]. Additionally, TREM2-dependent NF-κB signaling differs from classical NF-κB activation by preferentially inducing immunosuppressive cytokines like IL-10 and TGF-β rather than pro-inflammatory cytokines, thereby reinforcing immune tolerance [39].
E3 ubiquitin ligases also directly shape myeloid cell fate. In hepatocellular carcinoma, the deubiquitinating enzyme OTUB1 blocks ubiquitination of PD-L1, prolonging its cell surface retention and promoting immune evasion [40]. This mechanism represents a direct ubiquitin-mediated strategy for sustaining immune checkpoint expression and limiting T-cell mediated killing.
T Cell and B Cell Regulation
Ubiquitination profoundly influences T cell activation, differentiation, and function within the TME. The anaphase-promoting complex/cyclosome (APC/C) and Skp1-Cul1-F-box (SCF) complexes, both cullin RING E3 ligase family members, play crucial roles in regulating cell cycle proteins that govern T cell proliferation [37]. APC/C regulates G1 phase cell activity by binding to coactivators CDC20 and CDH1, subsequently controlling mitotic progression, while SCF complexes address DNA damage in the cell cycle by binding to ubiquitin ligases including FBXW7, β-Trcp, and SKP2 [37].
The PD-1/PD-L1 axis, a critical immune checkpoint, is subject to ubiquitin-mediated regulation. The stability, trafficking, and degradation of both PD-1 on T cells and PD-L1 on tumor and immune cells are controlled by various E3 ligases and DUBs. In breast cancer models, ubiquitination-related genes significantly influence tumor immune microenvironment composition and response to immunotherapies [41]. Comprehensive analyses reveal that ubiquitin-conjugating enzyme UBE2T expression shows significant associations with tumor immune markers, checkpoint genes, and immune cell infiltration across multiple cancer types [8].
Table 1: Key Ubiquitination Enzymes Regulating Immune Cells in the TME
| Enzyme | Type | Immune Cell Target | Molecular Function | Cancer Context |
|---|---|---|---|---|
| TREM2 | Signaling Adapter | Myeloid cells | Activates SYK-PI3K/AKT/mTOR pathway | Multiple cancers [39] |
| OTUB1 | DUB | Myeloid cells | Stabilizes PD-L1 by deubiquitination | Hepatocellular carcinoma [40] |
| UBE2T | E2 conjugating enzyme | Multiple immune cells | Correlates with immune checkpoint expression | Pan-cancer [8] |
| APC/C | E3 ligase complex | T cells | Regulates cell cycle progression via CDH1 | Multiple cancers [37] |
| SCF/FBXW7 | E3 ligase complex | T cells | Controls cell cycle checkpoints | Multiple cancers [37] |
| USP14 | DUB | Multiple immune cells | Stabilizes oncoproteins like c-Myc | Hepatocellular carcinoma [40] |
Ubiquitin-Based Therapeutic Targeting in the TME
Experimental Models and Methodologies
Studying ubiquitination in the TME requires sophisticated experimental approaches that capture the complexity of both the ubiquitin system and tumor-immune interactions. Single-cell RNA sequencing (scRNA-seq) has proven invaluable for identifying novel TAMC subsets, including TREM2+ myeloid cells with distinct functional properties [39]. This technology enables researchers to deconstruct the heterogeneity of immune populations within tumors and correlate ubiquitination-related gene expression with functional states.
For functional validation, genetic manipulation of ubiquitin system components in specific immune cell populations provides mechanistic insights. In pancreatic cancer models, UBE2T expression was assessed in multiple cell lines (PANC1, ASPC, BXPC3, MIA2, SW1990, and CAPAN1) compared to normal pancreatic epithelial cells (HPDE) using reverse transcription-quantitative PCR (RT-qPCR) and western blotting [8]. Similarly, in breast cancer research, stable knockdown of FBXL6 and overexpression of PDZRN3 were achieved through lentivirus infection in MDA-MB-231 cells, followed by validation of knockdown and overexpression efficiency via western blot analysis [41].
Drug sensitivity analyses using computational approaches like the "prophetic" R package predict differences in therapeutic response between subgroups based on ubiquitination-related gene signatures [41]. These analyses help identify patients most likely to benefit from specific interventions and reveal connections between ubiquitination states and treatment efficacy.
Figure 2: Experimental Workflow for Studying Ubiquitination in the TME. A representative methodology for investigating ubiquitin-mediated immune regulation, from initial discovery to functional validation and therapeutic testing.
Therapeutic Applications and Clinical Translation
Targeting ubiquitination pathways offers promising strategies for cancer immunotherapy. Small-molecule inhibitors of specific E3 ligases or DUBs show preclinical efficacy in modulating the immune TME. In hepatocellular carcinoma models, the E3 ligase inhibitor ML323 reduced NEDD4 activity, inducing apoptosis (30% vs. 5% in controls) and suppressing migration by 80% in vitro [40]. Similarly, the DUB inhibitor WP1130 combined with sorafenib synergistically reduced HCC cell viability (20% vs. 40% for sorafenib alone, p<0.01) by destabilizing c-Myc and enhancing drug sensitivity [40].
Immunotherapy combinations represent another promising application. TREM2 blockade has shown potential to reprogram the immunosuppressive TME, enhance T-cell infiltration, and augment the efficacy of immune checkpoint inhibitors [39]. Preclinical studies demonstrate that targeting TREM2+ myeloid cells can overcome resistance to anti-PD-1/PD-L1 therapies, suggesting combination approaches might benefit patients with immunologically "cold" tumors.
Table 2: Quantitative Effects of Ubiquitin-Targeting Therapies in Preclinical Models
| Therapeutic Agent | Target | Cancer Model | Key Effects | Reference |
|---|---|---|---|---|
| ML323 | E3 ligase NEDD4 | Hepatocellular carcinoma | Reduced tumor volume by 40%; induced 30% apoptosis (vs 5% control) | [40] |
| WP1130 + Sorafenib | DUBs | Hepatocellular carcinoma | Reduced cell viability to 20% (vs 40% with sorafenib alone) | [40] |
| TREM2 blockade | TREM2 signaling | Multiple cancer models | Enhanced T-cell infiltration; improved response to anti-PD-1 | [39] |
| Anti-UBE2T strategies | UBE2T | Pancreatic cancer models | Correlated with trametinib and selumetinib sensitivity | [8] |
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Research Reagents for Studying Ubiquitination in the TME
| Reagent Category | Specific Examples | Research Application | Key Functions |
|---|---|---|---|
| Primary Antibodies | Anti-UBB (HPA049132), Anti-UBC (HPA041344), Anti-β-Catenin | Immunohistochemistry/ Western blot | Protein localization and expression analysis [42] |
| Cell Lines | MDA-MB-231, MCF10A, CAL51, PANC1, ASPC, BXPC3 | In vitro modeling | Functional assays for proliferation, invasion, drug response [8] [41] |
| Inhibitors | ML323, WP1130, Trametinib, Selumetinib | Therapeutic targeting | Modulation of ubiquitination pathways; combination therapies [40] |
| Genetic Tools | siFBXL6-1, siFBXL6-2, PDZRN3 overexpression plasmids | Mechanistic studies | Gene-specific knockdown/overexpression to establish causality [41] |
| Databases | TCGA, GTEx, UCSC Xena, cBioPortal, GSCALite | Bioinformatic analysis | Ubiquitination gene expression, mutations, clinical correlations [8] [43] |
Ubiquitin signaling represents a master regulatory system that shapes immune cell function within the tumor microenvironment through precise control of protein stability, localization, and activity. The intricate interplay between E3 ligases, deubiquitinating enzymes, and their substrates creates a responsive network that tumors co-opt to evade immune surveillance. Understanding these mechanisms provides not only fundamental insights into cancer biology but also unveils new therapeutic opportunities.
Future research directions should prioritize the integration of multi-omics approaches to map ubiquitination networks across different immune cell populations in human tumors. Spatial transcriptomics will be essential for understanding how geographical relationships within the TME influence ubiquitin-mediated regulation. Additionally, advancing the specificity of ubiquitin-targeting therapeutics remains a critical challenge, requiring structural insights and sophisticated delivery strategies to minimize off-target effects.
As the field progresses, combining ubiquitin-directed therapies with established immunotherapies represents a promising strategy for overcoming resistance and expanding the repertoire of effective cancer treatments. The continued elucidation of ubiquitin signaling in the TME will undoubtedly yield novel biomarkers, therapeutic targets, and combination approaches to improve patient outcomes across multiple cancer types.
Mapping the Cancer Ubiquitinome: Advanced Profiling Techniques and Biomarker Discovery
Ubiquitin remnant profiling, often termed ubiquitinomics, is a powerful mass spectrometry (MS)-based proteomic strategy for the system-wide identification and quantification of protein ubiquitination. This approach specifically targets the diglycine (K-ε-GG) remnant that remains on lysine residues after tryptic digestion of ubiquitin-modified proteins, serving as a detectable signature for ubiquitination sites [44]. The ubiquitin-proteasome system (UPS) consists of approximately 750 enzymes that mediate the attachment and cleavage of ubiquitin, regulating virtually every intracellular process from cell cycle progression to autophagy [45]. The versatility of ubiquitin signaling arises from the complexity of ubiquitin conjugates, which can range from single ubiquitin monomers to polymers with different lengths and linkage types, each encoding distinct cellular signals [44]. For instance, K48-linked chains typically target substrates for proteasomal degradation, while K63-linked chains often modulate protein-protein interactions and kinase activation [12].
The disturbance of ubiquitination plays a fundamental role in the initiation and development of numerous pathologies, particularly cancer [46] [12]. In colorectal cancer alone, global ubiquitinome analyses have revealed significant alterations in thousands of ubiquitination sites compared to normal adjacent tissues [46] [47]. Consequently, comprehensive ubiquitinome profiling provides critical insights into molecular mechanisms of carcinogenesis and offers promising avenues for biomarker discovery and targeted therapeutic development [47]. This technical guide details the core methodologies, experimental workflows, and applications of ubiquitin remnant profiling with a specific focus on revealing ubiquitination patterns in cancer versus normal tissues.
Core Methodological Framework
Sample Preparation and Lysis Protocols
Optimal sample preparation is crucial for deep and reproducible ubiquitinome coverage. Recent advancements have demonstrated that sodium deoxycholate (SDC)-based lysis protocols significantly outperform conventional urea-based methods. When supplemented with chloroacetamide (CAA) for immediate cysteine protease inactivation during boiling, SDC lysis yielded approximately 38% more K-ε-GG peptides compared to urea buffer while maintaining excellent enrichment specificity [45]. This protocol improvement is particularly valuable for clinical tissue samples where material may be limited, as it enables the quantification of approximately 30,000 ubiquitinated peptides from just 2 mg of protein input material [45].
For tissue samples, including colorectal cancer specimens, a standard protocol involves rapid collection following surgery, immediate freezing in liquid nitrogen, and storage at -80°C until processing [46] [48]. Protein extraction typically utilizes lysis buffer containing 8 M urea, 10 mM EDTA, 10 mM DTT, and protease inhibitors, followed by sonication and centrifugation to remove debris [48]. The extracted proteins are then reduced, alkylated with iodoacetamide, and digested with trypsin, which cleaves proteins after lysine and arginine residues while leaving the K-ε-GG signature on modified lysines [46].
Affinity Enrichment Strategies
The low stoichiometry of endogenous ubiquitination necessitates efficient enrichment of K-ε-GG-containing peptides prior to LC-MS/MS analysis. The predominant method utilizes anti-K-ε-GG remnant motif antibodies conjugated to beads for immunoaffinity purification [46] [48] [47]. The commercial PTMScan Ubiquitin Remnant Motif Kit (Cell Signaling Technology) is widely employed for this purpose, enabling specific isolation of ubiquitinated peptides from complex tryptic digests [48] [47].
Following tryptic digestion, peptides are dissolved in NETN buffer (100 mM NaCl, 1 mM EDTA, 50 mM Tris-HCl, 0.5% NP-40, pH 8.0) and incubated with antibody-conjugated beads at 4°C overnight with gentle shaking. After extensive washing with NETN buffer and water, bound peptides are eluted with 0.1% trifluoroacetic acid, desalted using C18 ZipTips, and prepared for LC-MS/MS analysis [48]. This enrichment strategy typically achieves sufficient specificity and sensitivity to identify thousands of ubiquitination sites from limited biological material, making it suitable for clinical tissue samples where quantity may be restricted.
Table 1: Comparison of Ubiquitinated Peptide Enrichment Methods
| Method | Principle | Advantages | Limitations | Typical Applications |
|---|---|---|---|---|
| Antibody-based Enrichment | Immunoaffinity purification using K-ε-GG-specific antibodies | High specificity; applicable to any biological sample; identifies endogenous ubiquitination | Antibody cost; potential non-specific binding | Clinical tissues; cell lines; animal models |
| Ubiquitin Tagging | Expression of tagged ubiquitin (e.g., His, Strep) in living cells | Easy implementation; relatively low cost | Genetic manipulation required; may not mimic endogenous ubiquitin | Engineered cell lines; mechanistic studies |
| UBD-based Approaches | Enrichment using ubiquitin-binding domains | Linkage-specific isolation possible | Lower affinity requiring tandem domains; limited availability | Specialized studies on specific ubiquitin linkages |
Mass Spectrometry Acquisition Methods
Two primary MS acquisition methods are employed in ubiquitin remnant profiling: data-dependent acquisition (DDA) and data-independent acquisition (DIA). DDA, the conventional approach, involves selecting the most abundant precursor ions from MS1 scans for fragmentation, generating MS2 spectra for peptide identification [45]. While DDA with match-between-runs (MBR) can quantify approximately 21,434 K-ε-GG peptides on average per sample, it suffers from semi-stochastic sampling that leads to missing values across sample series [45].
DIA has emerged as a superior alternative for ubiquitinome analyses, overcoming the limitations of DDA by systematically fragmenting all ions within predetermined m/z windows [45]. When coupled with neural network-based data processing tools like DIA-NN, this method more than triples identification numbers to over 70,000 ubiquitinated peptides in single MS runs while significantly improving quantitative precision and reproducibility [45]. The median coefficient of variation (CV) for all quantified K-ε-GG peptides using DIA is approximately 10%, with the majority of peptides quantifiable across replicate samples [45].
For DIA analysis of ubiquitinomes, specific MS parameters should be optimized, including: using a nanoLC system with C18 columns (75 μm × 25 cm, 3 μm particles), implementing a 40-60 minute gradient from 5% to 35% buffer B (98% ACN, 0.1% FA), setting MS1 resolution to 60,000 with an m/z range of 350-1800, and employing HCD fragmentation with MS2 resolution at 30,000 [45] [48]. These parameters ensure optimal peptide separation, ionization, and fragmentation for comprehensive ubiquitinome coverage.
Ubiquitin Remnant Profiling Workflow
The following diagram illustrates the complete experimental workflow for ubiquitin remnant profiling, from sample preparation to data analysis:
Analytical Considerations and Bioinformatics
Ubiquitination Motif Analysis
Ubiquitination site analysis frequently reveals conserved sequence motifs surrounding modified lysine residues. In human colorectal cancer tissues, common motifs include acidic residues such as glutamic acid (E) and aspartic acid (D) positioned adjacent to ubiquitinated lysines [46]. Similarly, large-scale profiling in rice panicles identified E-Kub, Kub-D, and E-X-X-X-Kub as significantly enriched motifs (where Kub represents the ubiquitinated lysine) [49]. These conserved features suggest underlying sequence preferences for ubiquitin machinery and can inform prediction algorithms for novel ubiquitination sites.
Data Processing and False Discovery Control
Robust data processing pipelines are essential for confident ubiquitination site identification. For DDA data, MaxQuant is widely used with parameters including: false discovery rate (FDR) < 1% at peptide and protein levels, mass tolerance of 20 ppm for precursor ions (first search) and 5 ppm (main search), and fragment ion mass tolerance of 0.02 Da [46] [48]. Variable modifications should include GlyGly lysine and methionine oxidation, while carbamidomethylation is typically set as a fixed modification [48].
For DIA data, the DIA-NN software incorporates specialized scoring modules for modified peptides, providing rigorous FDR control specifically for K-ε-GG peptide identification [45]. This approach has been experimentally validated to achieve identification confidence comparable to DDA workflows while delivering substantially higher coverage and quantitative precision [45]. DIA-NN can operate in "library-free" mode against sequence databases or utilize project-specific spectral libraries generated through fractionation, with both approaches yielding similar performance for ubiquitinome analyses [45].
Functional Interpretation and Pathway Analysis
Following ubiquitination site identification, functional annotation tools extract biological insights from ubiquitinome datasets. Gene Ontology (GO) analysis typically reveals enrichment in biological processes such as G-protein coupling, antigen presentation, metabolic pathways, and immune regulation in cancer tissues [46] [47]. Kyoto Encyclopedia of Genes and Genomes (KEGG) pathway analysis frequently implicates ubiquitination in critical cancer-relevant pathways including RNA transport, cell cycle regulation, glycolysis/gluconeogenesis, and ferroptosis [48] [47].
Protein-protein interaction network construction further elucidates functional relationships among ubiquitinated proteins, highlighting densely connected modules with potential cooperative functions in carcinogenesis [47]. Integration with transcriptomic and proteomic data enables the identification of discordant regulation patterns, such as increased ubiquitination coupled with decreased protein abundance (indicative of degradation) or increased ubiquitination with stable protein levels (suggesting non-degradative functions) [45] [47].
Cancer Ubiquitinome Applications
Analytical Workflow for Cancer Research
The application of ubiquitin remnant profiling in cancer research follows a structured pathway from discovery to validation:
Key Findings in Colorectal Cancer
Ubiquitin remnant profiling has revealed profound alterations in ubiquitination patterns across various cancer types, with particularly extensive characterization in colorectal cancer (CRC). Comprehensive ubiquitinome analyses of CRC tissues have identified thousands of differentially ubiquitinated proteins compared to normal adjacent tissues [46] [47]. For example, one study quantified 1,690 ubiquitination sites on 870 proteins in CRC patient tissues, finding that highly ubiquitinated proteins (containing ≥10 modification sites) were specifically involved in biological processes including G-protein coupling, glycoprotein coupling, and antigen presentation [46].
In sigmoid colon cancer, the first ubiquitinome analysis identified 1,249 ubiquitinated sites within 608 differentially ubiquitinated proteins (DUPs) [47]. Bioinformatic analysis of these DUPs revealed 35 statistically significant signaling pathways, including salmonella infection, glycolysis/gluconeogenesis, and ferroptosis [47]. Survival analysis further identified 46 DUPs with significant correlation to overall survival, highlighting their potential as prognostic biomarkers and therapeutic targets [47].
Comparative analysis of primary and metastatic colon adenocarcinoma tissues revealed 375 differentially regulated ubiquitination sites on 341 proteins, with 132 sites upregulated and 243 downregulated in metastases [48]. Pathway analysis indicated enrichment in metastasis-relevant processes including RNA transport and cell cycle regulation, with specific identification of altered ubiquitination on CDK1 as a potential pro-metastatic factor [48].
Table 2: Quantification of Ubiquitination Sites in Cancer Studies
| Study Focus | Sample Type | Total Ubiquitination Sites | Differentially Regulated Sites | Key Technologies |
|---|---|---|---|---|
| Colorectal Cancer [46] | Cancerous vs. para-cancerous tissues (n=6) | 5,537 identified sites; 1,690 quantifiable sites | 1,172 up-regulated; 1,700 down-regulated proteins | DDA-MS, MaxQuant |
| Primary vs. Metastatic Colon Adenocarcinoma [48] | Primary (n=3) vs. metastatic (n=3) tissues | Not specified | 375 differentially modified sites (132 up, 243 down) | Anti-K-ε-GG enrichment, LC-MS/MS |
| Sigmoid Colon Cancer [47] | Cancerous vs. para-carcinoma tissues | 1,249 ubiquitinated sites within 608 DUPs | 608 differentially ubiquitinated proteins | Label-free quantification, Anti-K-ε-GG beads |
| USP7 Inhibition [45] | HCT116 cells with USP7 inhibitor | >70,000 ubiquitinated peptides | Hundreds with increased ubiquitination within minutes | DIA-MS, DIA-NN, SDC lysis |
Integration with Multi-Omics Data
Integrating ubiquitinome data with complementary genomic, transcriptomic, and proteomic datasets significantly enhances the biological insights gained from cancer studies. Relationship analyses between differentially ubiquitinated proteins (DUPs) and their corresponding gene expression patterns have revealed four distinct regulatory models: (1) DUP-up with gene expression up; (2) DUP-up with gene expression down; (3) DUP-down with gene expression up; and (4) DUP-down with gene expression down [47]. Similarly, comparing ubiquitination changes with protein abundance changes helps distinguish degradative from non-degradative ubiquitination events [45] [47].
A prominent example of this integrated approach identified increased ubiquitination of FOCAD at Lys583 and Lys587 as potentially associated with patient survival in colorectal cancer [46]. Subsequent analysis depicted the mutation map of FOCAD and elucidated its potential functions in RNA localization and translation in CRC, demonstrating how ubiquitinome findings can guide functional validation studies [46].
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Reagents and Resources for Ubiquitin Remnant Profiling
| Reagent/Resource | Function | Examples/Specifications |
|---|---|---|
| Anti-K-ε-GG Antibody Beads | Immunoaffinity enrichment of ubiquitinated peptides | PTMScan Ubiquitin Remnant Motif Kit (Cell Signaling Technology); enrichment specificity >90% [48] [47] |
| SDC Lysis Buffer | Protein extraction with enhanced ubiquitinome coverage | 5% SDC, 50 mM Tris-HCl (pH 8.5), 10 mM chloroacetamide; immediate boiling after lysis [45] |
| DIA-NN Software | Data processing for DIA ubiquitinomics | Deep neural network-based; specialized scoring for modified peptides; library-free and library-based modes [45] |
| High-pH Reverse-Phase Fractions | Spectral library generation | Fractionation into 8-12 fractions; enables deep library generation (>100,000 ubiquitinated peptides) [45] |
| NanoLC System | Peptide separation prior to MS | C18 columns (75μm × 25cm, 3μm particles); 40-60min gradients; flow rates 250-300nL/min [45] [48] |
| Q-Exactive HF-X Mass Spectrometer | High-resolution mass spectrometry | MS1 resolution: 60,000; MS2 resolution: 30,000; HCD fragmentation; DIA or DDA modes [48] |
Ubiquitin remnant profiling has matured into an indispensable methodology for system-wide ubiquitination analysis, with particular transformative potential in cancer research. The ongoing development of DIA-MS approaches coupled with neural network-based data processing has dramatically enhanced the depth, precision, and throughput of ubiquitinome analyses, enabling quantification of over 70,000 ubiquitinated peptides in single LC-MS runs [45]. These technical advances now permit rapid mode-of-action profiling for drug candidates targeting ubiquitin pathway components, including deubiquitinases and ubiquitin ligases, at unprecedented resolution [45].
In the context of cancer research, ubiquitinome profiling has revealed extensive reprogramming of ubiquitination networks across diverse cancer types, highlighting potential biomarkers and therapeutic targets. The integration of ubiquitinome data with genomic, transcriptomic, and proteomic datasets provides a multidimensional perspective on cancer biology, distinguishing degradative from non-degradative ubiquitination events and revealing complex regulatory relationships [45] [47]. These insights are particularly valuable for advancing predictive, preventive, and personalized medicine (PPPM) approaches in oncology, enabling patient stratification based on ubiquitination signatures and facilitating targeted therapeutic interventions [47].
As the field continues to evolve, future developments will likely focus on enhancing spatial resolution through ubiquitinome analysis of specific subcellular compartments, improving quantification accuracy for low-abundance regulatory ubiquitination events, and expanding the integration of ubiquitinome data with other post-translational modification datasets to decipher complex signaling networks. Through these advances, ubiquitin remnant profiling will continue to illuminate the intricate role of ubiquitination in cancer pathogenesis and treatment response, ultimately contributing to improved diagnostic, prognostic, and therapeutic strategies.
The integration of transcriptomic and ubiquitinomic data represents a transformative approach in molecular biology, particularly for elucidating the complex regulatory mechanisms underlying carcinogenesis. The ubiquitin-proteasome system (UPS), responsible for the post-translational regulation of 80-90% of cellular proteins, is frequently dysregulated in cancer, yet its interplay with transcriptional networks remains poorly characterized at a systems level [8] [50]. This technical guide outlines comprehensive bioinformatics methodologies for the synergistic analysis of these data modalities, providing a structured framework for identifying critical regulatory nodes and therapeutic vulnerabilities within oncogenic networks. We detail specific pipelines for data processing, multi-omics integration, and functional validation, with particular emphasis on applications in cancer biology and drug discovery.
Ubiquitination is a critical, reversible post-translational modification mediated by a coordinated enzyme cascade comprising E1 (activating), E2 (conjugating), and E3 (ligating) enzymes, alongside deubiquitinating enzymes (DUBs) that remove ubiquitin modifications [51] [50]. This system regulates virtually all cellular processes, including protein degradation, cell cycle progression, signal transduction, and DNA damage response [50]. The dysregulation of ubiquitination machinery is increasingly implicated in tumorigenesis, with accumulating evidence demonstrating elevated expression of specific UPS components like ubiquitin-conjugating enzyme UBE2T across multiple cancer types, where it correlates with poor clinical outcomes [8].
Transcriptomic profiling provides a powerful tool for mapping global gene expression patterns but offers limited insight into post-translational regulatory mechanisms. The integration of ubiquitinomic data—which captures the activity and targets of the ubiquitination system—with transcriptomic profiles enables a more comprehensive understanding of cancer pathophysiology. Recent pan-cancer analyses reveal that ubiquitination regulators (UBRs) exhibit widespread genetic alterations and expression perturbations across malignancies, with more than 90% of UBRs significantly affecting patient survival [50]. This integration is particularly crucial for understanding mechanisms of therapeutic resistance and for identifying novel biomarker signatures, such as ubiquitination-related prognostic signatures (URPS) that effectively stratify patients based on survival outcomes and immunotherapy response potential [10].
Computational Workflows for Data Integration
Data Acquisition and Preprocessing
The foundation of any integrated analysis is robust data acquisition from publicly available repositories and experimental sources. Key resources include:
- Transcriptomic Data: The Cancer Genome Atlas (TCGA), Genotype-Tissue Expression (GTEx) consortium, and Gene Expression Omnibus (GEO) provide bulk RNA-seq data across diverse cancer types and normal tissues [8] [50]. For single-cell resolution, databases like the Human Cell Atlas offer cell-type-specific expression profiles.
- Ubiquitinomic Data: Protein-level ubiquitination data can be sourced from mass spectrometry-based ubiquitinome datasets, while genetic alterations in UBRs are available through TCGA mutation and copy number variation (CNV) files [50]. The UbiBrowser database provides curated ubiquitin ligase-substrate interactions [50].
- Proteomic Data: The Clinical Proteomic Tumor Analysis Consortium (CPTAC) and Cancer Cell Line Encyclopedia (CCLE) offer protein abundance data critical for validating transcriptional observations at the proteomic level [51].
Preprocessing should include quality control, normalization, and batch effect correction using established tools. For ubiquitinomic data, this involves identifying ubiquitination sites and quantifying ubiquitin conjugates.
Core Integration Methodologies
Several computational approaches enable the effective integration of transcriptomic and ubiquitinomic datasets:
- Correlation-Based Analysis: Calculate Pearson correlation coefficients between the expression of UBRs (writers, erasers, readers) and cancer hallmark pathway activities derived from transcriptomic data [50]. Regulator-pathway pairs with |PCC| > 0.5 and adjusted p-value < 0.01 represent significant associations worthy of further investigation.
- Gene Set Variation Analysis (GSVA): Transform gene expression matrices of UBRs into enrichment scores for specific biological pathways using the GSVA package in R [50] [10]. This non-parametric, unsupervised method evaluates pathway activity variations across samples without requiring predefined gene sets.
- Network-Based Integration: Construct protein-protein interaction (PPI) networks using databases like STRING, then apply molecular complex detection (MCODE) algorithms to identify densely connected regions representing functional modules [50]. Integration with transcriptomic data helps prioritize hub genes with both network significance and expression perturbations in cancer.
- Multi-Omics Factor Analysis: Employ statistical frameworks like MOFA+ to identify latent factors that capture shared and unique variations across transcriptomic and ubiquitinomic data modalities, revealing coordinated biological programs.
The workflow diagram below illustrates the logical sequence and decision points in a standard integration pipeline:
Analytical Outputs and Visualization
Effective visualization of integrated data is critical for interpretation. The following table summarizes key analytical outputs and recommended visualization approaches:
Table 1: Analytical Outputs and Visualization Strategies for Integrated Data
| Analytical Output | Description | Visualization Method | Biological Insight |
|---|---|---|---|
| UBR Expression Heatmaps | Comparative expression of ubiquitination regulators across cancer vs. normal tissues | ComplexHeatmap R package [50] | Tissue-specific UBR dysregulation patterns |
| Pathway Correlation Networks | Interconnections between UBR expression and oncogenic pathway activities | Correlation network diagrams (Cytoscape) | Key regulatory UBRs in cancer signaling |
| Survival Signatures | Ubiquitination-related prognostic models stratifying patient outcomes | Kaplan-Meier survival curves [10] | Clinical relevance of UBR dysregulation |
| Genetic Alteration Landscapes | Mutation and CNV profiles of UBRs across pan-cancer cohorts | Oncoprints (maftools R package) [50] | Somatic alteration patterns in UPS |
| Immune Cell Correlations | Associations between UBR expression and tumor-infiltrating immune cells | TIMER2.0 database outputs [8] | UBR roles in tumor microenvironment |
When creating visualizations, adhere to established color guidelines: use qualitative palettes for categorical data, sequential palettes for ordered values, and diverging palettes for spectra [52]. Ensure sufficient color contrast and limit palettes to approximately seven distinguishable colors to avoid cognitive overload [52].
Experimental Protocols for Validation
Functional Validation of UBR Candidates
Bioinformatic predictions require experimental validation to establish biological relevance. The following protocols provide frameworks for validating integrated transcriptomic-ubiquitinomic findings:
Table 2: Key Research Reagent Solutions for Experimental Validation
| Reagent/Category | Specific Examples | Function/Application | Example Usage |
|---|---|---|---|
| CRISPR-Cas9 Libraries | Arrayed libraries targeting DUBs/UBRs [51] | Gene knockout to assess essentiality and phenotype | Determine proliferation impact of UBR loss |
| DUB Inhibitors | Selective compounds for USP1, USP7, USP14, USP30 [51] | Pharmacological inhibition of deubiquitinating enzymes | Validate DUB substrate relationships and therapeutic potential |
| Antibodies for Detection | UBE2T (Abclonal A6853) [8] | Protein detection via western blot, immunohistochemistry | Confirm protein-level expression of UBR candidates |
| Cell Line Panels | Cancer Cell Line Encyclopedia (CCLE) [51] [8] | Models for genetic and pharmacological screens | Assess UBR expression and dependency across lineages |
| Ubiquitination Assays | TUBE (Tandem Ubiquitin Binding Entity) pulldowns | Enrichment and detection of ubiquitinated proteins | Identify specific substrates of UBRs of interest |
Protocol 1: CRISPR-Cas9 Knockout of Candidate UBRs
- Library Design: Utilize arrayed CRISPR-Cas9 libraries targeting UBRs (e.g., 81 DUB targets with 4 guides per target) [51].
- Transfection Optimization: Optimize delivery conditions using western blotting to validate protein knockdown efficiency.
- Phenotypic Screening: Assess impact on proliferation (DepMap dependency scores), apoptosis, and migration in relevant cancer models.
- Transcriptomic Profiling: Conduct RNA-seq on knockout cells to identify differentially expressed genes and pathways.
- Validation: Confirm phenotypes with complementary approaches (RNAi, rescue experiments).
Protocol 2: Pharmacological Triaptosis Induction
- Compound Treatment: Treat hepatocellular carcinoma (HCC) cell lines (Huh7, HCCLM3) with menadione sodium bisulfite (MSB; 0-50 μM, 12 hours) to induce triaptosis [53].
- Viability Assessment: Measure IC50 values (typically ~12-14 μM for HCC) using CellTiter-Glo or MTT assays [53].
- Pathway Inhibition: Co-treat with cell death inhibitors (e.g., NAC for ROS scavenging) to confirm mechanism [53].
- ROS Measurement: Quantify intracellular reactive oxygen species using DCFDA assays [53].
- In Vivo Validation: Administer MSB (150 μg/mL in drinking water) to Huh7 xenograft models for two weeks; measure tumor volume reduction and TUNEL staining [53].
Protocol 3: Ubiquitination-Regulated Pathway Analysis
- Identify Correlation: Detect significant correlations between UBR expression and pathway activities (e.g., OTUB1-TRIM28 with MYC signaling) [10].
- Genetic Manipulation: Knock down or overexpress UBR candidates in appropriate cell models.
- Pathway Assessment: Monitor downstream pathway activity using western blotting (phospho-specific antibodies) and qPCR for target genes.
- Ubiquitination Status: Examine substrate ubiquitination through immunoprecipitation followed by ubiquitin immunoblotting.
- Functional Assays: Assess impact on proliferation (colony formation), cell cycle (flow cytometry), and invasion (Transwell assays).
The signaling pathway diagram below illustrates a validated ubiquitination-regulated pathway in cancer:
Applications in Cancer Research and Therapeutics
Biomarker Discovery and Prognostic Modeling
Integrated transcriptomic-ubiquitinomic analyses have enabled the development of robust prognostic signatures with clinical utility:
- Ubiquitination-Related Prognostic Signature (URPS): Constructed through LASSO Cox regression analysis of UBR expression across multiple cancer types (lung, esophageal, cervical cancer, melanoma) [10]. This signature effectively stratifies patients into high-risk and low-risk groups with distinct survival outcomes and immunotherapy responses.
- Triaptosis-Associated lncRNA Signature: A 5-lncRNA signature (LINC01134, HPN-AS1, DDX11-AS1, AC009283.1, AC009005.1) derived from TCGA data demonstrates superior predictive power for hepatocellular carcinoma prognosis compared to conventional clinical parameters [53].
- UBE2T as Pan-Cancer Biomarker: Comprehensive analyses reveal elevated UBE2T expression across multiple tumors, association with poor outcomes, correlation with immune markers, and involvement in key oncogenic pathways including cell cycle, ubiquitin-mediated proteolysis, and p53 signaling [8].
Therapeutic Target Identification
The integration pipeline facilitates prioritization of therapeutic targets:
- DUB Inhibition: Systematic analysis identifies DUBs with cancer-specific essentiality, supporting development of inhibitors against USP1 (advanced solid tumors), USP30 (kidney disease), USP7 (TP53 stabilization), and USP28 (c-Myc regulation) [51].
- Triaptosis Induction: MSB-mediated triaptosis induction represents a novel therapeutic approach for HCC, with functional studies revealing LINC01134 as an oncogenic driver that sensitizes cells to triaptosis via MTM1-mediated PI(3)P catabolism [53].
- Immune Modulation: UBR expression correlates with immune checkpoint markers and infiltrating immune cells, suggesting opportunities for combination therapies targeting ubiquitination pathways to enhance immunotherapy efficacy [8] [10].
The experimental workflow below outlines the process from data integration to therapeutic application:
The integration of transcriptomic and ubiquitinomic data through the bioinformatics pipelines detailed in this guide provides a powerful systematic approach for deciphering the complex regulatory landscape of cancer. These methodologies enable the identification of novel prognostic biomarkers, therapeutic targets, and functional mechanisms linking ubiquitination pathways to oncogenic processes. As multi-omics datasets continue to expand, refinement of these integration strategies will further accelerate the development of ubiquitination-targeted therapeutics and personalized medicine approaches for cancer treatment. The protocols and workflows outlined here offer researchers a comprehensive framework for implementing these analyses in their own investigations of ubiquitination patterns in cancer biology.
Ubiquitination, the second most abundant post-translational modification in cells after phosphorylation, represents a crucial regulatory mechanism in cellular homeostasis and disease pathogenesis [54]. This process involves the covalent attachment of ubiquitin molecules to target proteins through a sequential enzymatic cascade involving E1 (activating), E2 (conjugating), and E3 (ligating) enzymes [55] [54]. The ubiquitin-proteasome system (UPS) maintains precise control over fundamental cellular processes including cell cycle progression, DNA damage repair, apoptosis, and immune response [56] [54]. In cancer biology, dysregulation of ubiquitination pathways contributes significantly to tumor initiation, progression, metastasis, and therapeutic resistance through aberrant degradation of tumor suppressors, stabilization of oncoproteins, and modulation of the tumor microenvironment [16] [54]. The comprehensive analysis of ubiquitination-related genes (URGs) has recently emerged as a promising approach for developing prognostic biomarkers across various cancer types [57] [56] [21].
The development of Ubiquitination-Related Prognostic Signatures (URPS) represents an innovative intersection of cancer biology, bioinformatics, and machine learning. These signatures quantify the collective expression patterns of URGs to stratify patients into distinct risk categories with differential clinical outcomes [57] [56]. The reversibility and dynamic nature of the ubiquitin system, coupled with the recent advent of targeted therapies such as proteolysis-targeting chimeras (PROTACs), have further heightened the clinical relevance of URPS in the era of precision oncology [16] [21]. This technical guide comprehensively outlines the methodological framework, computational approaches, and validation strategies for developing and implementing URPS in cancer research and therapeutic development.
Molecular Foundations of Ubiquitination in Cancer
The Ubiquitin Code and Cancer Hallmarks
Ubiquitination complexity extends beyond simple protein degradation, encompassing diverse chain topologies that constitute a sophisticated "ubiquitin code" with distinct functional consequences [16] [54]. Table 1 summarizes the major ubiquitin linkage types and their primary biological functions in cancer contexts.
Table 1: Ubiquitin Linkage Types and Their Cancer-Related Functions
| Linkage Type | Primary Function | Role in Cancer Hallmarks | Representative Examples |
|---|---|---|---|
| K48-linked | Proteasomal degradation | Stabilizes oncoproteins; degrades tumor suppressors | p53 degradation, SOX9 stabilization in NSCLC [16] |
| K63-linked | Signaling scaffolds; DNA repair | Activates survival pathways; DNA damage tolerance | FBXW7-modified XRCC4 in NHEJ repair; TRAF4 activation of JNK/c-Jun [16] |
| K11/K48-branched | Enhanced degradation | Cell cycle regulation | Rapid turnover of cell cycle regulators [54] |
| Monoubiquitination | Protein activity/localization | Chromatin remodeling; DNA damage response | H2AX monoubiquitylation in hepatocellular carcinoma [16] |
| K6-linked | DNA damage response | Genomic instability | DNA damage response regulation [54] |
| K27/K29-linked | DNA repair activation | Error-prone repair in therapy resistance | RNF126-mediated MRE11 activation in TNBC [16] |
Ubiquitination Enzymes as Oncogenic Drivers and Suppressors
The enzymes constituting the ubiquitination cascade exhibit both oncogenic and tumor-suppressive properties across cancer types. E3 ubiquitin ligases, which confer substrate specificity, are particularly prominent in cancer pathogenesis, with mutations identified in numerous malignancies [54]. For instance, in ovarian cancer, the E3 ligase FBXO45 promotes tumor growth, spread, and migration via the Wnt/β-catenin pathway [21]. In diffuse large B-cell lymphoma (DLBCL), elevated expression of the E2 enzyme CDC34 and the E3 ligase regulator FZR1 correlates with poor prognosis, while low expression of the deubiquitinase OTULIN is associated with unfavorable outcomes [57]. The tissue-specific and context-dependent functions of these enzymes underscore the complexity of ubiquitination networks in cancer and highlight the importance of developing cancer-type-specific URPS.
Computational Methodology for URPS Development
Data Acquisition and Preprocessing
The development of a robust URPS begins with comprehensive data acquisition from multiple sources. Transcriptomic data from large-scale consortiums such as The Cancer Genome Atlas (TCGA) and the Genotype-Tissue Expression (GTEx) project provide the foundational datasets for initial model development [19] [56]. Supplementary data from Gene Expression Omnibus (GEO) repositories serve as valuable validation cohorts [57] [56]. The ubiquitination-related gene sets are typically compiled from specialized databases such as the Ubiquitin and Ubiquitin-like Conjugation Database (UUCD) or iUUCD 2.0, which catalog E1, E2, E3, and deubiquitinating enzymes [56] [21].
Essential Preprocessing Steps:
- Data Filtering: Remove samples with poor quality, formalin-fixed specimens, recurrent tissues, and patients with survival times shorter than 3 months to reduce confounding factors [56].
- Normalization: Apply appropriate normalization methods (e.g., log2 transformation with a small constant to handle zeros) to ensure comparability across datasets [19] [21].
- Batch Effect Correction: Address technical variations between different sequencing batches or platforms using established computational methods.
- Differential Expression Analysis: Identify URGs differentially expressed between tumor and normal tissues using packages such as 'limma' or 'edgeR' with thresholds typically set at |logFC| ≥ 1-2 and adjusted p-value < 0.05 [57] [21].
Feature Selection Using Machine Learning Algorithms
Feature selection represents a critical step in URPS development, aiming to identify the most prognostically relevant URGs from hundreds of candidates. Table 2 summarizes the core machine learning algorithms employed in URPS development with their specific implementations.
Table 2: Machine Learning Algorithms for URPS Feature Selection
| Algorithm | Primary Function | Key Parameters | Advantages | R Package/Implementation |
|---|---|---|---|---|
| Univariate Cox Regression | Initial screening of prognostic genes | P-value threshold (<0.05) | Computational efficiency; identifies individually significant genes | survival package [57] [21] |
| LASSO Cox Regression | Dimension reduction and feature selection | Optimal lambda via cross-validation | Prevents overfitting; handles multicollinearity | glmnet with cv.glmnet (family='cox', type.measure='deviance') [57] [56] |
| Random Survival Forest | Non-linear feature importance | ntree=100, nsplit=5, variable importance >0.25 | Handles complex interactions; robust to outliers | randomForestSRC package [56] |
| Consensus Clustering | Molecular subtype identification | maxK=5-10, reps=1000, pItem=0.8, pFeature=1 | Identifies distinct ubiquitination patterns | ConsensusClusterPlus [56] [21] |
The application of these algorithms follows a sequential approach. For instance, in lung adenocarcinoma (LUAD) research, univariate Cox regression initially identified prognostic URGs, followed by Random Survival Forests to select features with importance >0.25, and finally LASSO Cox regression for further refinement, ultimately yielding a 4-gene signature (DTL, UBE2S, CISH, STC1) [56]. Similarly, in DLBCL, LASSO Cox analysis of 7 ubiquitination-survival-related differentially expressed genes identified a final 3-gene signature (CDC34, FZR1, OTULIN) [57].
Figure 1: Comprehensive Workflow for URPS Development. The process encompasses data preparation, feature selection using machine learning algorithms, and multi-dimensional validation.
Signature Construction and Risk Stratification
Following feature selection, the URPS is constructed using a multivariate Cox regression model. The risk score for each patient is calculated using the formula:
Risk score = Σ(βi × Expi)
Where βi represents the regression coefficient for each gene from multivariate Cox analysis, and Expi represents the expression level of the corresponding gene [56] [21]. Patients are subsequently stratified into high-risk and low-risk groups based on the median risk score or optimized cut-off values determined using algorithms such as the "surv_cutpoint" function from the survminer R package [57].
The prognostic performance of the URPS is evaluated using Kaplan-Meier survival analysis with log-rank tests to assess significant differences in overall survival (OS) or disease-specific survival (DSS) between risk groups [19] [56]. Time-dependent receiver operating characteristic (ROC) curves analyze the predictive accuracy at 1-, 3-, and 5-year intervals, with area under the curve (AUC) values quantifying discrimination ability [56] [21]. For enhanced clinical utility, the URPS is often integrated with clinical parameters (e.g., age, stage, grade) to construct nomograms that provide individualized survival probability estimates [21] [58].
Analytical Validation and Functional Characterization
Multi-dimensional Validation Strategies
Robust validation of URPS requires a multi-faceted approach encompassing technical, biological, and clinical dimensions:
- External Validation: Apply the URPS to independent validation cohorts from GEO databases (e.g., GSE181063 for DLBCL; GSE165808 and GSE26712 for ovarian cancer) to assess generalizability [57] [21].
- Subgroup Analysis: Evaluate the prognostic performance across various clinical subgroups stratified by age, gender, cancer stage, and molecular subtypes to ensure broad applicability [58].
- Experimental Validation: Conduct in vitro and in vivo studies to confirm the biological roles of signature genes. For example, in ovarian cancer, FBXO45 was experimentally validated using Western blot, qRT-PCR, and ELISA to demonstrate its role in promoting tumor growth via the Wnt/β-catenin pathway [21].
- Single-cell RNA Sequencing: Analyze signature gene expression at single-cell resolution to identify cell-type-specific expression patterns within the tumor microenvironment [57] [21].
Tumor Microenvironment and Immune Landscape Analysis
The URPS demonstrates significant utility in characterizing the tumor immune microenvironment, which critically influences therapeutic response and clinical outcomes. Comprehensive immune analyses typically include:
- Immune Cell Infiltration: Quantify immune cell abundances using computational algorithms such as CIBERSORT, ESTIMATE, or QUANTISEQ to compare immune profiles between risk groups [57] [19] [21]. In ovarian cancer, the low-risk URPS group showed significantly higher infiltration of CD8+ T cells, M1 macrophages, and follicular helper T cells [21].
- Immunomodulator Expression: Analyze expression patterns of immune checkpoints (e.g., PD-1, PD-L1, CTLA-4) and cytokines to identify potential mechanisms of immune evasion [56] [58]. In lung adenocarcinoma, the high URRS group had significantly higher PD-1/PD-L1 expression levels [56].
- Tumor Mutational Burden (TMB) and Neoantigens: Assess correlations between URPS risk scores and TMB/tumor neoantigen load (TNB), which influence immunotherapy response [19] [56].
Figure 2: URPS Correlation with Tumor Microenvironment and Therapeutic Implications. The risk score correlates with multiple TME components, genomic features, and treatment responses.
Therapeutic Response Prediction
A critical application of URPS lies in predicting response to various therapeutic modalities:
- Chemotherapy Sensitivity: Using computational tools such as oncoPredict, researchers can calculate the half-maximal inhibitory concentration (IC50) of chemotherapeutic agents for different risk groups [57] [56]. In lung adenocarcinoma, the high URRS group exhibited lower IC50 values for various chemotherapy drugs, suggesting enhanced sensitivity [56].
- Immunotherapy Response: Correlations between URPS risk scores and immune checkpoint expression, TMB, and TNB provide insights into likely immunotherapy efficacy [56] [58]. In laryngeal cancer, the low-risk group demonstrated more activated immune function and higher infiltration of anti-cancer immune cells, suggesting greater potential benefit from immune checkpoint inhibitors [58].
- Targeted Therapy Opportunities: Identification of key ubiquitination enzymes within signatures reveals potential targets for emerging therapeutic strategies, particularly PROTACs and small-molecule inhibitors targeting specific E3 ligases or deubiquitinases [16] [21] [54].
Table 3: Essential Research Reagents and Computational Resources for URPS Development
| Category | Specific Resource | Application | Key Features |
|---|---|---|---|
| Bioinformatics Databases | TCGA (https://www.cancer.gov/) | Transcriptomic and clinical data | Pan-cancer molecular data with clinical annotations [19] [56] |
| GTEx (https://www.gtexportal.org/) | Normal tissue reference | Normal tissue gene expression reference [19] [21] | |
| GEO (https://www.ncbi.nlm.nih.gov/geo/) | Validation datasets | Repository of gene expression datasets [57] [56] | |
| UUCD/iUUCD 2.0 (http://iuucd.biocuckoo.org/) | Ubiquitination-related gene sets | Comprehensive catalog of ubiquitination enzymes [56] [21] | |
| Computational Tools | R/Bioconductor | Statistical analysis and modeling | Open-source environment for statistical computing [57] [56] |
| glmnet package | LASSO Cox regression | Efficient implementation of regularized models [57] [56] | |
| randomForestSRC package | Random Survival Forests | Machine learning for survival analysis [56] | |
| oncoPredict package | Drug sensitivity prediction | Computational prediction of IC50 values [57] [56] | |
| CIBERSORT/ESTIMATE | Immune infiltration analysis | Deconvolution of immune cell populations [57] [21] | |
| Experimental Validation Reagents | qRT-PCR assays | Gene expression validation | Quantitative validation of signature genes [21] [58] |
| Western blot reagents | Protein expression analysis | Protein-level validation of ubiquitination enzymes [21] [58] | |
| ELISA kits | Cytokine quantification | Measurement of immune markers [21] [58] | |
| Cell lines (e.g., A2780, HEY) | Functional studies | In vitro models for experimental validation [21] |
The development of Ubiquitination-Related Prognostic Signatures represents a cutting-edge approach in cancer prognostication and treatment stratification. By leveraging machine learning algorithms to distill complex ubiquitination networks into clinically actionable signatures, URPS models provide powerful tools for personalized oncology. The integration of these signatures with multi-omics data, comprehensive immune profiling, and drug sensitivity predictions creates a robust framework for guiding therapeutic decisions.
Future directions in URPS development will likely focus on several key areas: (1) incorporation of single-cell and spatial transcriptomics data to resolve intratumoral heterogeneity in ubiquitination patterns; (2) integration of ubiquitin linkage-specific information to enhance biological interpretability; (3) development of pan-cancer URPS models to identify common ubiquitination themes across malignancies; and (4) application of deep learning architectures to model complex non-linear relationships within ubiquitination networks. Furthermore, the rapid advancement of ubiquitination-targeted therapies, particularly PROTACs and molecular glues, will increasingly position URPS as essential biomarkers for identifying patients most likely to benefit from these novel therapeutic approaches [16] [21] [54].
As the field progresses, standardized methodologies for URPS development and validation will be crucial for ensuring reproducibility and clinical translation. The methodological framework outlined in this technical guide provides a comprehensive foundation for researchers developing ubiquitination-related prognostic signatures across diverse cancer types, ultimately contributing to more precise and effective cancer management strategies.
Protein ubiquitination, a fundamental post-translational modification, has emerged as a critical regulator of oncogenesis, tumor progression, and therapeutic response. This process, which involves the covalent attachment of ubiquitin to target proteins, governs nearly all cellular processes including metabolism, cell cycle progression, and immune response [59] [50]. The dysregulation of ubiquitination signals is closely associated with the initiation and progression of multiple cancers, making ubiquitination-related regulators (UBRs) promising candidates for prognostic modeling [50]. Recent advances in multi-omics technologies and computational biology have enabled the development of Ubiquitination-Related Prognostic Signatures (URPS) that can stratify patients across different cancer types based on their molecular profiles rather than traditional histology alone [10]. This technical review comprehensively examines the construction, validation, and clinical application of URPS across lung, ovarian, and gastrointestinal cancers, providing researchers with detailed methodological frameworks and comparative performance metrics.
Ubiquitination-Related Prognostic Signatures (URPS): Pan-Cancer Principles
Theoretical Foundation of URPS
The ubiquitin-proteasome system (UPS) comprises writers (E1-E3 enzymes), erasers (deubiquitinases), and readers (proteins with ubiquitin-binding domains) that collectively maintain protein homeostasis [50]. Ubiquitination controls 80-90% of cellular proteolysis and is a reversible modification dynamically regulated by these enzymes [10]. In cancer, widespread genetic alterations and expression perturbations in UBRs lead to dysfunctional degradation of oncoproteins and tumor suppressors, ultimately driving malignant progression [50]. The URPS framework leverages these molecular perturbations to create predictive models that reflect the underlying biological state of tumors beyond what conventional staging systems can capture.
Core Analytical Framework for URPS Development
The construction of URPS follows a standardized bioinformatics pipeline with specific adaptations for ubiquitination-related components:
Data Acquisition and Preprocessing: Transcriptomic data from The Cancer Genome Atlas (TCGA) and Gene Expression Omnibus (GEO) form the foundation for URPS development. Normal ovarian tissue RNAseq data are often obtained from the Genotype-Tissue Expression (GTEx) project (180 control samples) to establish baseline ubiquitination patterns [60]. Harmonization of transcriptomic profiles between TCGA and GTEX is achieved through empirical Bayes-based batch effect correction using the ComBat function from the sva R package [60].
UBR Gene Selection: Ubiquitination-related genes are curated from databases such as UbiBrowser, with subsequent differential expression analysis between tumor and normal tissues performed using the R package "limma" (P-value < 0.05 and |log2FC| ≥ 1) [60] [50]. Protein-protein interaction (PPI) networks for differentially expressed UBRs are constructed using the STRING database and visualized with Cytoscape to identify hub genes [60].
Model Construction via Machine Learning: LASSO Cox regression analysis with 10-fold cross-validation is employed to construct the prognostic model, selecting the optimal penalty parameter (λ) based on the largest λ within 1 standard error of the minimum mean squared error [60] [10]. A risk score formula is then generated incorporating expression values of selected genes weighted by their regression coefficients from LASSO analysis [60].
Table 1: Core Components of URPS Development Pipeline
| Component | Description | Tools/Databases |
|---|---|---|
| Data Sources | Transcriptomic data from TCGA, GTEx, GEO | TCGA portal, GTEx portal, GEO database |
| UBR Curation | Collection of ubiquitination-related genes | UbiBrowser, STRING, published literature |
| Feature Selection | Identification of prognostic UBRs | Limma, univariate Cox, LASSO-Cox |
| Model Validation | Internal and external performance assessment | TCGA training, GEO validation sets |
| Pathway Analysis | Biological interpretation of URPS | GSVA, GSEA, clusterProfiler |
URPS Validation in Lung Cancer
Molecular Stratification and Prognostic Performance
In lung cancer, URPS has demonstrated remarkable utility in stratifying patients with distinct survival outcomes and therapeutic responses. A comprehensive pancancer study analyzing 4,709 patients across 26 cohorts established that URPS effectively categorized lung cancer patients into high-risk and low-risk groups with significantly different overall survival [10]. The high-risk group exhibited upregulation of oxidative phosphorylation and MYC signaling pathways, both known drivers of aggressive tumor behavior. The prognostic model was further validated in independent lung cancer cohorts (GSE30219, GSE135222, GSE126044), confirming its robust performance across diverse patient populations [10].
Integration with Radiomic Features
Recent advances have integrated URPS with radiomic features from preoperative CT scans to enhance prognostic accuracy. A machine learning model incorporating both clinical variables and CT radiomic features demonstrated superior performance compared to conventional TNM staging alone, particularly for stage I patients [61]. The model achieved higher hazard ratios for disease-free survival in both internal (HR = 1.71 vs 1.22) and external (HR = 3.34 vs 1.98) validation compared to tumor size-based stratification [61]. Significantly, the machine learning-derived risk scores correlated with established pathologic risk factors including poor differentiation (P < 0.0001), lymphovascular invasion (P < 0.0001), and pleural invasion (P < 0.0001) [61].
Experimental Validation of Key Mechanisms
Functional validation in lung cancer models identified the OTUB1-TRIM28 ubiquitination axis as a critical modulator of MYC pathway activity and histological fate determination [10]. Both in vitro and in vivo experiments demonstrated that this ubiquitination pair influences squamous or neuroendocrine transdifferentiation in adenocarcinoma, ultimately leading to immunotherapy resistance and poor prognosis [10]. These findings provide a mechanistic foundation for the prognostic capability of URPS in lung cancer and highlight potential therapeutic targets for high-risk patients.
Figure 1: OTUB1-TRIM28 Ubiquitination Axis in Lung Cancer Prognosis
URPS Implementation in Ovarian Cancer
Multi-Omics Approach to URPS Development
Ovarian cancer (OV) research has demonstrated the particular utility of multi-omics approaches for URPS development. A comprehensive study utilizing data from extensive public cohorts and machine learning methods identified 17 differentially expressed prognostic genes between OV and normal ovarian tissue [60]. The resulting risk score was positively correlated with poor survival (P < 0.001) and associated with key oncological pathways, immune-related processes, and genomic alterations [60]. Patients with higher risk scores exhibited increased levels of immune cell infiltration and significant remodeling of the immune microenvironment, suggesting distinct biological states captured by the URPS.
Immune Microenvironment and Therapeutic Implications
The ovarian cancer URPS demonstrated strong correlations with immune checkpoint molecules, including PD-1/PD-L1, suggesting potential benefits from immune checkpoint blockade strategies in high-risk patients [60]. Computational analysis of immune cell infiltration using the CIBERSORT algorithm revealed distinct patterns of immune cell distribution between high-risk and low-risk groups, with high-risk patients showing increased M2 macrophage polarization and regulatory T-cell infiltration [60]. The risk score also proved to be a stable and sensitive indicator for predicting sensitivity to various chemotherapeutic drugs, with high-risk patients showing potential resistance to conventional platinum-based therapies but increased sensitivity to PARP inhibitors [60].
Methodological Workflow for OV URPS
Table 2: Ovarian Cancer URPS Development Protocol
| Step | Method | Parameters | Output |
|---|---|---|---|
| Data Collection | TCGA-OV (377 samples), GTEx (180 normal) | FPKM normalization, batch correction | Harmonized expression matrix |
| DEG Identification | Limma package | P < 0.05, |log2FC| ≥ 1 | 17 prognostic UBRs |
| Pathway Analysis | clusterProfiler, GSVA | GO, KEGG, HALLMARK | Immune/oncogenic pathways |
| Risk Model | LASSO-Cox, 10-fold CV | λ.1se selection | 17-gene signature |
| Validation | External cohorts (GSE14764, GSE17260) | Kaplan-Meier, log-rank | Prognostic performance |
Gastrointestinal Cancer URPS Applications
Pancreatic Adenocarcinoma URPS
Pancreatic adenocarcinoma (PAAD) represents a particularly compelling application for URPS given its aggressive nature and limited therapeutic options. A specialized URPS incorporating both mRNA and lncRNA components was developed using multi-omics data from TCGA and validated through in vitro and in vivo experiments [62]. Unsupervised hierarchical clustering based on ubiquitination-related mRNAs and lncRNAs identified two PAAD subtypes with distinct clinical outcomes, ubiquitination pathway activities, and immune microenvironment characteristics [62]. The URPS demonstrated superior prognostic performance compared to four other recognized panels in evaluating PAAD patient survival status.
Experimental validation confirmed the functional significance of URPS components, with real-time PCR revealing that AC005062.1 expression was elevated several thousand-fold in all three tested PAAD cell lines [62]. Drug sensitivity analysis predicted that FTI-277 (a farnesyltransferase inhibitor) had better efficacy in high-risk patients, while MK-2206 (an Akt allosteric inhibitor) showed superior therapeutic effects in low-risk patients, highlighting the potential for URPS-guided therapy selection [62].
Esophageal and Gastric Cancers
In esophageal cancer, circular RNAs have been identified as key regulators of protein ubiquitination networks. CircPDE5A, significantly down-regulated in esophageal squamous cell carcinoma (ESCC), encodes a protein (PDE5A-500aa) that stabilizes phosphatidylinositol-3-kinase interacting protein 1 (PIK3IP1) by facilitating USP14-mediated deubiquitination [63]. This process consequently attenuates the PI3K/AKT signaling pathway in ESCC cells, leading to inhibition of proliferation and metastasis [63]. Another circRNA, circ0026611, was upregulated in ESCC cells and exosomes, promoting cancer progression through NAA10-mediated ubiquitination pathways [63].
Ubiquitination Patterns Across GI Malignancies
A systematic analysis of ubiquitination mechanisms revealed tissue-specific signatures across gastrointestinal cancers, with distinct ubiquitination patterns observed in esophageal, gastric, hepatocellular, pancreatic, and colorectal cancers [50]. The expression of 79 UBRs was closely correlated with the activity of 32 cancer hallmark-related pathways across these malignancies, and more than 90% of UBRs significantly affected patient survival in specific cancer types [50].
Figure 2: Gastrointestinal Cancer URPS Development Workflow
Technical Protocols and Methodological Standards
Ubiquitination Score Calculation
The ubiquitination score, a key quantitative metric in URPS, is computed using single-sample gene set enrichment analysis (ssGSEA) based on the expression profiles of UBRs [62]. This method transforms the gene-level expression matrix into a pathway-level enrichment score for each sample, representing the overall activity of ubiquitination-related pathways. Samples scoring in the top 30% and bottom 30% of ubiquitination scores are typically selected as representative high-risk and low-risk groups for subsequent comparative analysis of pathway activities using Gene Set Enrichment Analysis (GSEA) [62].
Immune Microenvironment Characterization
Comprehensive analysis of the tumor immune microenvironment in URPS studies employs multiple complementary approaches. RNA-seq data from patients in high and low-risk groups are analyzed using the CIBERSORT algorithm to infer the relative proportions of 22 immune-infiltrating cell types [60]. Simultaneously, the TISIDB database (http://cis.hku.hk/TISIDB/index.php) is utilized to explore interactions between tumors and the immune system, integrating heterogeneous data types from TCGA, UniProt, GO, and DrugBank [60]. These analyses collectively provide a detailed view of immune contexture associated with different URPS risk groups.
Drug Sensitivity Prediction
The R package "pRRophetic" is employed to predict chemosensitivity based on the largest available public pharmacogenomics database (Genomics of Cancer Drug Sensitivity - GDSC) [60]. The estimated half-maximal inhibitory concentration (IC50) for each chemotherapeutic drug is obtained by linear regression analysis, with prediction accuracy tested by 10-fold cross-validation using the GDSC training set [60]. This approach enables the identification of potential therapeutic options tailored to specific URPS risk categories.
Table 3: Key Research Reagent Solutions for URPS Investigation
| Reagent/Resource | Function | Application in URPS Research |
|---|---|---|
| TCGA & GTEx Datasets | Provide transcriptomic profiles | Foundation for initial URPS development and training |
| CIBERSORT Algorithm | Deconvolutes immune cell populations | Characterizes immune microenvironment in risk groups |
| LASSO-Cox Regression | Performs feature selection and survival modeling | Identifies most prognostic UBRs and constructs risk score |
| GDSC Database | Contains drug sensitivity genomics data | Predicts therapeutic response based on URPS risk |
| STRING Database | Maps protein-protein interactions | Identifies hub genes within ubiquitination networks |
| CytoTRACE2 | Computes cellular differentiation states | Analyzes single-cell trajectories in URPS context |
The validation of Ubiquitination-Related Prognostic Signatures across lung, ovarian, and gastrointestinal cancers represents a significant advancement in molecular oncology. By capturing the essential biological processes driven by ubiquitination networks, URPS provides a powerful framework for patient stratification that transcends conventional histopathological classifications. The consistent performance of URPS across multiple cancer types underscores the fundamental role of ubiquitination in oncogenesis and highlights the potential for targeted interventions that modulate specific components of the ubiquitin-proteasome system.
Future research directions should focus on integrating URPS with other molecular data types, including epigenomic profiles and radiomic features, to create more comprehensive prognostic models. Additionally, prospective clinical trials are needed to validate the utility of URPS in guiding therapeutic decisions, particularly in the context of immunotherapy and targeted therapy selection. As our understanding of ubiquitination networks continues to expand, so too will the refinement and application of these prognostic tools, ultimately advancing the field toward more personalized and effective cancer management strategies.
The ubiquitin-proteasome system (UPS) is a critical post-translational modification machinery responsible for degrading 80-90% of intracellular proteins, thereby maintaining cellular homeostasis and genomic stability [8]. This enzymatic cascade involves E1 (activating), E2 (conjugating), and E3 (ligating) enzymes that collectively tag substrate proteins with ubiquitin for proteasomal degradation. Recent pan-cancer analyses reveal that dysregulation of ubiquitination pathways constitutes a fundamental mechanism in tumorigenesis and profoundly shapes the tumor immune microenvironment (TIME) [10]. The ubiquitination process directly regulates key immune checkpoint proteins, modulates cytokine signaling, and influences immune cell activation states, positioning ubiquitination patterns as critical determinants of anti-tumor immunity [8] [10]. Assessment of ubiquitination-mediated immunomodulation provides novel insights into cancer biology and unveils potential therapeutic targets for enhancing immunotherapy efficacy.
Computational Assessment of Ubiquitination Patterns in the Immune Microenvironment
Data Acquisition and Preprocessing
Comprehensive analysis begins with acquiring multi-omics data from public repositories including The Cancer Genome Atlas (TCGA), Gene Expression Omnibus (GEO), and Cancer Cell Line Encyclopedia (CCLE) [8] [64]. RNA sequencing data from tumor tissues and matched normal samples should be processed using standardized pipelines. For ubiquitination-focused analyses, identify ubiquitination-related genes (UbLGs) from databases such as GeneCards with relevance scores ≥3, typically yielding approximately 465 genes [64]. Differential expression analysis between tumor and normal samples can be performed using DESeq2 (v1.36.0) with thresholds of p-value <0.05 and |log2FoldChange| >0.5 [64]. For immune cell infiltration quantification, utilize algorithms such as CIBERSORT, EPIC, or TIMER2.0 to estimate abundances of specific immune cell populations from bulk transcriptome data [8].
Ubiquitination-Inmmune Correlation Analysis
To establish significant associations between ubiquitination patterns and immune infiltration, conduct systematic correlation analyses comparing expression levels of key ubiquitination enzymes with immune cell signatures. For example, UBE2T expression demonstrates significant correlation with various immune markers across multiple cancer types [8]. Similarly, multi-gene ubiquitination signatures encompassing MMP1, RNF2, TFRC, SPP1, and CXCL8 effectively stratify patients into distinct risk groups with differential immune profiles [64]. Implement statistical methods including Pearson or Spearman correlation tests with appropriate multiple testing correction. Survival analysis via Kaplan-Meier curves and Cox regression models further validates the clinical relevance of identified ubiquitination-immune relationships [64] [10].
Table 1: Key Ubiquitination-Related Genes with Established Roles in Immune Regulation
| Gene Symbol | Protein Name | Function in Ubiquitination | Immune Correlates | Cancer Context |
|---|---|---|---|---|
| UBE2T | Ubiquitin-conjugating enzyme E2 T | E2 conjugating enzyme | Correlates with immune checkpoint expression and T cell infiltration | Pan-cancer [8] |
| RNF2 | Ring finger protein 2 | E3 ubiquitin ligase | Differential infiltration of memory B cells and M0 macrophages | Cervical cancer [64] |
| OTUB1 | OTU deubiquitinase, ubiquitin aldehyde binding 1 | Deubiquitinating enzyme | Modulates MYC pathway; influences macrophage infiltration | Lung cancer, esophageal cancer [10] |
| TRIM28 | Tripartite motif containing 28 | E3 ubiquitin ligase | Co-regulator with OTUB1; affects TME composition | Multiple solid tumors [10] |
| CXCL8 | C-X-C motif chemokine ligand 8 | Ubiquitination substrate | Upregulated in tumor tissues; chemotaxis for immune cells | Cervical cancer [64] |
Functional Enrichment and Pathway Analysis
To elucidate biological mechanisms linking ubiquitination to immune modulation, perform functional enrichment analysis using Gene Ontology (GO), Kyoto Encyclopedia of Genes and Genomes (KEGG), and Gene Set Enrichment Analysis (GSEA) [8]. Ubiquitination-related gene signatures typically enrich pathways including 'cell cycle', 'ubiquitin-mediated proteolysis', 'p53 signaling', 'mismatch repair', and immune-related pathways such as 'T cell receptor signaling' and 'PD-L1 expression/PD-1 checkpoint pathway' [8] [10]. Protein-protein interaction networks constructed using databases like STRING can identify hub genes within ubiquitination-immune networks [10]. Single-cell RNA sequencing analysis further resolves ubiquitination patterns across distinct cell subpopulations within the TME, revealing cell-type specific ubiquitination activities [10].
Experimental Methodologies for Validating Ubiquitination-Immune Relationships
In Vitro Cellular Assays
Immune Cell Coculture Systems: Establish direct and indirect coculture systems using cancer cell lines and primary immune cells. For mitochondrial transfer studies, tag cancer cell mitochondria with fluorescent proteins (MitoDsRed) and coculture with T cells for 24-48 hours [65]. Assess transfer efficiency via flow cytometry and confocal microscopy. To elucidate transfer mechanisms, apply specific inhibitors: cytochalasin B (TNT formation inhibitor), GW4869 (small EV release blocker), or Y-27632 (microEV inhibitor) [65]. Use transwell inserts (3μm and 0.4μm) to distinguish direct cell-contact-mediated transfer from extracellular vesicle-mediated transfer [65].
Gene Manipulation Techniques: Employ CRISPR/Cas9 or RNA interference to knockdown ubiquitination enzymes in cancer cells. Validate knockdown efficiency via western blotting and RT-qPCR. Following manipulation, assess impacts on immune cell function through transwell migration assays, T cell proliferation assays, and cytokine production measurements (e.g., IFN-γ, IL-2) via ELISA [8] [10].
Protein-Protein Interaction Studies: Conduct co-immunoprecipitation assays to identify novel ubiquitination substrates within immune signaling pathways. For example, investigate OTUB1-TRIM28 ubiquitination axis using co-IP followed by mass spectrometry [10]. Validate interactions via Western blotting with specific antibodies.
Table 2: Experimental Models for Ubiquitination-Immune Microenvironment Studies
| Experimental System | Key Applications | Technical Readouts | Considerations |
|---|---|---|---|
| Cancer cell-immune cell coculture | Mitochondrial transfer, immune cell function | Flow cytometry, confocal microscopy, cytokine assays | Maintain appropriate cell ratios; include controls for indirect effects |
| Ubiquitination enzyme knockdown/knockout | Functional validation of specific genes | Western blot, RT-qPCR, immune cell activation assays | Monitor compensatory mechanisms; use multiple targeting approaches |
| Patient-derived organoids | Personalized immunomodulation assessment | Single-cell sequencing, imaging, drug screening | Preserves tumor heterogeneity; technically challenging |
| Animal tumor models (syngeneic, PDX) | In vivo validation of ubiquitination-immune axis | Tumor growth, immune profiling, survival analysis | Consider species-specific ubiquitination differences |
| Proteomic analysis of immune cells | Ubiquitinome characterization | Mass spectrometry, ubiquitin remnant profiling | Requires specialized sample preparation |
Molecular Profiling Techniques
Transcriptomic Analysis: Isolve RNA from tumor tissues or immune cell populations using TRIzol reagent with quality verification via NanoDrop spectrophotometry and agarose gel electrophoresis [64]. For bulk RNA-seq, prepare libraries with average insert sizes of 300±50 bp and sequence on Illumina platforms (e.g., NovaSeq 6000) [64]. Align sequences to reference genomes (GRCh38.105) and quantify gene expression. For ubiquitination-focused analyses, specifically examine ubiquitination-related gene sets.
Mitochondrial DNA Sequencing: To investigate mitochondrial transfer between cancer and immune cells, sequence mtDNA from paired tumor-infiltrating lymphocytes (TILs) and cancer cells [65]. Design specific primers for mtDNA regions and compare mutations between cell types. Identify shared mutations indicating transfer events.
Single-Cell RNA Sequencing: Prepare single-cell suspensions from tumor tissues and perform scRNA-seq using 10X Genomics platform. Analyze ubiquitination gene expression patterns across different immune cell subtypes to identify cell-type specific ubiquitination activities within the TME [10].
Immune Monitoring Approaches
Flow Cytometry: Comprehensive immunophenotyping of TILs using antibody panels targeting CD45 (pan-immune), CD3 (T cells), CD4 (helper T cells), CD8 (cytotoxic T cells), CD19 (B cells), CD56 (NK cells), and CD11b/CD33 (myeloid cells) [65]. Include analysis of activation markers (CD69, CD25), exhaustion markers (PD-1, TIM-3, LAG-3), and memory differentiation markers (CD45RO, CD62L). Intracellular staining for cytokines (IFN-γ, TNF-α) assesses functional capacity.
Immunohistochemistry/Immunofluorescence: Tissue staining for ubiquitination enzymes (e.g., UBE2T), immune cell markers (CD3, CD8, CD68), and immune checkpoints (PD-L1) [8]. Spatial analysis determines colocalization of ubiquitination patterns with specific immune populations.
Metabolic Profiling: Assess metabolic consequences of ubiquitination modulation in immune cells via Seahorse Analyzer to measure oxidative phosphorylation and glycolysis [65]. Compare metabolic profiles of T cells with and without exposure to cancer cell-derived mitochondria containing ubiquitination-related mutations.
Table 3: Key Research Reagent Solutions for Ubiquitination-Immune Studies
| Reagent/Resource | Specific Example | Application | Considerations |
|---|---|---|---|
| Ubiquitination enzyme antibodies | UBE2T (cat. no. A6853; Abclonal) [8] | Western blotting, immunohistochemistry | Validate specificity with knockout controls |
| Immune cell isolation kits | CD3+ T cell isolation kits (e.g., Miltenyi) | Purification of specific immune populations | Maintain cell viability and function during isolation |
| Mitochondrial dyes | MitoTracker Green, MitoDsRed [65] | Tracking mitochondrial transfer | Optimize loading concentrations to avoid toxicity |
| Ubiquitination inhibitors | MG132 (proteasome inhibitor), PYR-41 (E1 inhibitor) | Functional perturbation studies | Assess specificity and off-target effects |
| EV isolation reagents | GW4869 (small EV inhibitor) [65] | Extracellular vesicle studies | Characterize EV size and composition |
| Cytokine detection assays | ELISA kits for IFN-γ, IL-2, TGF-β | Immune functional assessment | Use appropriate standard curves and controls |
| scRNA-seq platforms | 10X Genomics Chromium | Single-cell transcriptomics | Process samples immediately to preserve RNA integrity |
| Metabolic assay systems | Seahorse XF Analyzer kits | Metabolic profiling of immune cells | Optimize cell numbers and assay conditions |
Concluding Perspectives
The intricate relationship between ubiquitination patterns and immune cell infiltration represents a burgeoning frontier in cancer immunology. Comprehensive assessment requires integration of computational approaches with experimental validation across molecular, cellular, and functional dimensions. The methodologies outlined herein provide a framework for deciphering ubiquitination-mediated immunomodulation in the tumor microenvironment. As research advances, ubiquitination-based biomarkers may stratify patients for immunotherapy while ubiquitination enzymes emerge as promising therapeutic targets for overcoming immunosuppression. Future studies should emphasize spatial characterization of ubiquitination patterns within tissue contexts and develop targeted interventions to manipulate ubiquitination for enhanced anti-tumor immunity.
In the evolving landscape of oncology, the prediction of therapeutic response remains a critical challenge in clinical management. The ubiquitin-proteasome system, once primarily recognized for its role in protein degradation, has emerged as a rich source of prognostic biomarkers across cancer types. Ubiquitination signatures—multigene expression patterns derived from ubiquitin-related genes (UbRGs)—demonstrate remarkable utility in stratifying patients based on their likely response to chemotherapy and immunotherapy [57] [66]. These signatures reflect fundamental biological processes that govern tumor behavior, including cell cycle regulation, DNA repair mechanisms, and immune modulation [67] [68]. The integration of ubiquitination signatures into clinical prediction models represents a paradigm shift from traditional histopathological classification toward molecularly-guided treatment strategies, potentially unlocking more personalized and effective therapeutic approaches for cancer patients.
Table 1: Overview of Ubiquitination-Related Prognostic Signatures Across Cancers
| Cancer Type | Key Ubiquitination-Related Genes in Signature | Predictive Value | Reference |
|---|---|---|---|
| Diffuse Large B-Cell Lymphoma | CDC34, FZR1, OTULIN | Chemotherapy response; Poor prognosis with elevated CDC34/FZR1 and low OTULIN | [57] |
| Hepatocellular Carcinoma | UBE2C, CPY26B1, MCM10, SPINK4, TRIM54 | Immunotherapy response; High risk = poor survival | [67] [69] |
| Epithelial Ovarian Carcinoma | HSP90AB1, FBXO9, SIGMAR1, STAT1, SH3KBP1, EPB41L2, DNAJB6, VPS18, PPM1G, AKAP12, FRK, PYGB | Chemoresistance; B-cell receptor signaling, focal adhesion | [66] |
| Laryngeal Cancer | PPARG, LCK, LHX1 | Immune microenvironment; Chemotherapy vs. immunotherapy benefit | [70] |
| Breast Cancer | TCN1, DIRAS3, IZUMO4 | Immunotherapy response; Cell cycle and DNA replication pathways | [71] |
| Ovarian Cancer | 17-gene signature including FBXO45 | CD8+ T-cell and M1 macrophage infiltration; Wnt/β-catenin pathway | [21] |
Methodological Framework for Ubiquitination Signature Development
Bioinformatics Pipeline Construction
The development of ubiquitination signatures follows a structured bioinformatics workflow that integrates multi-omics data. The process begins with differential expression analysis using R packages such as limma to identify ubiquitination-related genes (UbRGs) with significant expression changes between tumor and normal tissues [57] [70]. The standard threshold employs a false discovery rate (FDR) < 0.05 and |log2 fold change| > 1 [70] [21]. Subsequently, univariate Cox regression analysis identifies UbRGs with significant association with overall survival (OS), followed by Least Absolute Shrinkage and Selection Operator (LASSO) Cox regression to prevent overfitting and select the most robust prognostic genes [57] [66] [71]. The final risk score model is constructed using the formula: Risk score = Σ(Coefi × Expri), where Coefi represents the regression coefficient and Expri denotes the gene expression level [70] [21]. Patients are stratified into high-risk and low-risk groups based on the median risk score, enabling prognostic prediction.
Experimental Validation Approaches
Bioinformatic discoveries require rigorous experimental validation through both in vitro and in vivo models. For ubiquitination-related genes of interest, knockdown experiments using small interfering RNA (siRNA) or short hairpin RNA (shRNA) demonstrate functional relevance. For instance, UBE2C knockdown in hepatocellular carcinoma (HCC) cell lines (Huh7 and Hep3B) significantly reduced cell proliferation, invasion, and migration capacity [67]. Conversely, overexpression systems using eukaryotic expression vectors establish gain-of-function effects, as demonstrated with USP2 in gastric cancer, where overexpression suppressed proliferation and enhanced apoptosis [72]. Functional assays including Transwell migration and invasion assays, CCK-8 proliferation assays, wound healing assays, and flow cytometric apoptosis analysis provide mechanistic insights into how specific UbRGs influence malignant phenotypes and treatment responses [67] [72].
Ubiquitination Signatures in Chemotherapy Response Prediction
Molecular Mechanisms Underlying Chemoresistance
Ubiquitination signatures demonstrate remarkable predictive power for chemotherapy response through their association with key resistance pathways. In epithelial ovarian carcinoma (EOC), a 12-gene ubiquitination signature strongly predicts chemoresistance, with high-risk patients showing reduced sensitivity to conventional chemotherapeutic agents except dasatinib [66]. The underlying mechanisms involve enrichment in B-cell receptor signaling, ECM-receptor interactions, and focal adhesion pathways that collectively create a protective tumor microenvironment [66]. Similarly, in diffuse large B-cell lymphoma (DLBCL), the ubiquitination signature comprising CDC34, FZR1, and OTULIN correlates with significant differences in drug sensitivity, particularly to Osimertinib and Boehringer Ingelheim compound 2536 [57]. These signatures reflect fundamental biological processes: CDC34 and FZR1 associate with cell cycle progression, while OTULIN regulates linear ubiquitination in inflammatory signaling, collectively influencing how tumor cells respond to cytotoxic insults [57].
Pathway-Based Chemotherapy Response Stratification
The predictive capacity of ubiquitination signatures extends beyond simple risk stratification to pathway-specific therapeutic implications. In breast cancer, ubiquitination-related risk scores show distinct IC50 values for multiple targeted agents: the low-risk group demonstrates higher sensitivity to rapamycin, while high-risk patients show increased sensitivity to axitinib, AZD6244, erlotinib, GDC0941, and lapatinib [71]. This differential drug sensitivity profile enables clinicians to select more effective treatment regimens based on a patient's molecular ubiquitination profile. The high-risk breast cancer ubiquitination signature is notably enriched in cell cycle and DNA replication pathways, explaining the observed resistance to DNA-damaging chemotherapeutic agents [71]. This pathway-level understanding transforms ubiquitination signatures from mere prognostic indicators to functional biomarkers that can guide therapeutic selection.
Table 2: Ubiquitination Signature-Based Drug Sensitivity Predictions
| Cancer Type | High-Risk Group Sensitive Drugs | Low-Risk Group Sensitive Drugs | Enriched Pathways in High-Risk |
|---|---|---|---|
| Breast Cancer | Axitinib, AZD6244, Erlotinib, GDC0941, Lapatinib | Rapamycin | Cell cycle, DNA replication [71] |
| Liver Cancer | Erlotinib | VX-11e, AKT inhibitor VIII, Bortezomib | Cell cycle, cancer-related miRNAs [69] |
| Ovarian Cancer | Dasatinib | Multiple conventional agents | B-cell receptor signaling, focal adhesion [66] |
| Diffuse Large B-Cell Lymphoma | Osimertinib, Boehringer Ingelheim 2536 | Not specified | Endocytosis, immune response [57] |
Ubiquitination Signatures in Immunotherapy Response Prediction
Modulation of the Tumor Immune Microenvironment
Ubiquitination signatures exert profound influence on immunotherapy response primarily through their regulation of the tumor immune microenvironment (TIME). In hepatocellular carcinoma, ubiquitination-related genes are significantly upregulated in tumor tissues and correlate with an immunosuppressive TIME characterized by reduced anti-tumor immune cell infiltration [67] [69]. The UBE2C gene emerges as a central regulator in this process, promoting immune evasion by inhibiting anti-tumor immune responses and reducing immune system recognition of tumor cells [67]. Similarly, in laryngeal cancer, the ubiquitination-related signature comprising PPARG, LCK, and LHX1 accurately discriminates between "immune-hot" and "immune-cold" tumors, with the low-risk group demonstrating more activated immune function, higher infiltration of anti-cancer immune cells, and stronger expression of immune-promoting cytokines [70]. Specifically, PPARG and LHX1 show negative correlation with immuno-promoting microenvironments, whereas LCK exhibits positive correlation, highlighting the complex regulatory networks through which ubiquitination processes shape anti-tumor immunity [70].
Predictive Biomarkers for Immune Checkpoint Inhibitor Response
The clinical utility of ubiquitination signatures extends to predicting response to immune checkpoint inhibitors (ICIs), addressing a critical need in precision immuno-oncology. In breast cancer, the ubiquitination-related risk score demonstrates significant negative correlation with immunotherapy response, with high-risk patients showing elevated tumor microenvironment scores but diminished potential benefit from ICIs [71]. This paradoxical relationship suggests that while ubiquitination-related processes may promote an inflamed TIME, they simultaneously establish compensatory immunosuppressive mechanisms that limit ICI efficacy. Supporting this concept, in ovarian cancer, ubiquitination signatures reveal distinct immune infiltration patterns, with low-risk patients exhibiting significantly higher levels of CD8+ T cells, M1 macrophages, and follicular helper cells—all associated with improved response to ICIs [21]. Additionally, mutation patterns differ between risk groups, with high-risk ovarian cancer patients showing more mutations in MUC17 and LRRK2, while low-risk patients have more RYR2 mutations, providing genomic correlates for the observed differential immunotherapy responses [21].
Table 3: Key Research Reagents and Databases for Ubiquitination Signature Development
| Resource Category | Specific Tools/Reagents | Application/Purpose | Reference |
|---|---|---|---|
| Bioinformatics Databases | TCGA, GEO, ICGC, CPTAC | Omics data acquisition for model development | [57] [71] [69] |
| Ubiquitin Gene Databases | UUCD 2.0, UbiBrowser 2.0, MSigDB | Reference ubiquitination-related gene sets | [70] [71] [21] |
| Computational R Packages | limma, survminer, survival, glmnet, ConsensusClusterPlus | Differential expression, survival analysis, clustering | [57] [66] [71] |
| Immune Analysis Tools | CIBERSORT, ESTIMATE, MCPcounter, TIMER | Tumor microenvironment deconvolution | [57] [66] [21] |
| Drug Sensitivity Prediction | oncoPredict, pRRophetic | In silico chemotherapeutic response prediction | [57] [71] |
| Experimental Validation Kits | CCK-8, Transwell assays, Annexin V/PI apoptosis kits | Functional validation of ubiquitination genes | [67] [72] |
Ubiquitination signatures represent a transformative approach to predicting therapeutic response in oncology, integrating complex biological processes into clinically actionable biomarkers. The consistent demonstration of their prognostic value across diverse cancer types—including lymphomas, carcinomas, and sarcomas—underscores the fundamental role of ubiquitination processes in shaping tumor behavior and treatment resistance [57] [66] [71]. As drug development increasingly targets the ubiquitin-proteasome system with novel modalities such as proteolysis-targeting chimeras (PROTACs), these signatures will play dual roles as both predictive biomarkers and pharmacodynamic indicators [21]. Future research directions should focus on standardizing ubiquitination signature assays for clinical implementation, validating them in prospective clinical trials, and integrating them with existing biomarkers to create comprehensive predictive models that maximize therapeutic efficacy while minimizing unnecessary toxicity for cancer patients.
Ubiquitination, a critical reversible post-translational modification, regulates protein stability, localization, and activity through a coordinated enzymatic cascade involving E1 activating, E2 conjugating, and E3 ligase enzymes, alongside deubiquitinating enzymes (DUBs) [35]. The tumor microenvironment (TME) comprises a complex ecosystem of malignant, immune, and stromal cells, each contributing differently to tumor progression. Single-cell RNA sequencing (scRNA-seq) has revolutionized our ability to dissect this heterogeneity by profiling gene expression at individual cell resolution [73]. Recent advances now enable researchers to investigate ubiquitination patterns across these cellular compartments, revealing how differential ubiquitination regulates driver pathways within specific cell populations [74] [67] [10].
Integrating scRNA-seq with ubiquitination analysis provides unprecedented insights into cancer biology by mapping the ubiquitin-modified landscape across distinct cell types. This approach has identified novel therapeutic targets and mechanisms of therapy resistance that were previously obscured in bulk tissue analyses [75]. For instance, pancreatic cancer studies have revealed endothelial cell subpopulations with high ubiquitination scores exhibiting enriched interactions with fibroblasts and macrophages through WNT, NOTCH, and integrin pathways [74]. Similarly, hepatocellular carcinoma analyses demonstrate how ubiquitination-related genes significantly upregulated in tumor tissues correlate with poor prognosis by modulating immune evasion and metabolic reprogramming [67].
Core Methodologies for Single-Cell Ubiquitination Analysis
Experimental Workflow and Technical Considerations
Single-cell ubiquitination analysis requires specialized wet-lab and computational approaches. The foundational workflow begins with high-quality single-cell suspension preparation from tumor tissues, followed by cell isolation using microfluidic technologies, fluorescence-activated cell sorting (FACS), or magnetic-activated cell sorting (MACS) [73]. Following cell isolation, scRNA-seq libraries are prepared using platforms such as 10x Genomics, which incorporate unique molecular identifiers (UMIs) and cell-specific barcodes to minimize technical noise and enable high-throughput analysis [73].
Critical quality control measures must be implemented, including:
- Cell filtering: Retain features between 200-5,000 genes; exclude cells with >15% mitochondrial gene expression [75]
- Normalization: Use methods like SCTransform to normalize sequencing depth [75]
- Integration: Apply canonical correlation analysis (CCA) to correct batch effects across samples [76]
For ubiquitination-specific analysis, researchers typically curate ubiquitination-related gene sets from databases like GeneCard (relevance score >10) or the integrated Ubiquitin and Ubiquitin-like Conjugation Database (iUUCD), which contains 27 E1s, 109 E2s, 1,153 E3s, and 164 DUBs [74] [75]. The AUCell, irGSEA, and UCell packages then calculate ubiquitination scores across cell populations [74].
Computational Analysis Framework
Table 1: Key Computational Tools for Single-Cell Ubiquitination Analysis
| Tool/Package | Primary Function | Application in Ubiquitination Analysis |
|---|---|---|
| Seurat | Single-cell data processing and clustering | Cell type identification, differential expression [74] [75] |
| CellChat | Cell-cell communication analysis | Ligand-receptor interactions between cell types with different ubiquitination scores [74] |
| InferCNV | Copy number variation inference | Malignant cell identification from epithelial cells [75] |
| AUCell/UCell | Gene set enrichment scoring | Ubiquitination activity quantification at single-cell level [74] [75] |
| SCENIC | Regulatory network inference | Transcription factor activity in high-ubiquitination cells [10] |
| Spacexr | Spatial transcriptomics deconvolution | Mapping single-cell ubiquitination patterns to spatial tissue context [74] |
| scRepertoire | Immune receptor profiling | Paired analysis of immune receptor diversity and ubiquitination [77] |
Advanced analytical approaches include Weighted Gene Co-expression Network Analysis (WGCNA) to identify ubiquitination-related gene modules associated with cancer traits, and Summary-data-based Mendelian Randomization (SMR) to prioritize causal ubiquitination genes for functional validation [74]. Spatial transcriptomics integration through packages like spacexr enables mapping ubiquitination patterns within tissue architecture, revealing how spatial organization influences ubiquitination-mediated signaling [74].
Key Experimental Findings and Ubiquitination Patterns
Cell-Type-Specific Ubiquitination in Cancer
Single-cell analyses have revealed striking cell-type-specific ubiquitination patterns across cancer types. In pancreatic cancer, scRNA-seq of patient samples (GSE155698) identified 12 distinct cell types, with endothelial cells exhibiting particularly high ubiquitination scores ("High_ubiquitin-Endo") [74]. These high-ubiquitination endothelial cells showed enriched interactions with fibroblasts and macrophages via WNT, NOTCH, and integrin pathways, suggesting specialized ubiquitination-mediated signaling in tumor vasculature [74].
In hepatocellular carcinoma, ubiquitination-related genes are significantly upregulated in tumor tissues, with distinct patterns observed across plasma cells, fibroblasts, endothelial cells, and epithelial-mesenchymal transition (EMT) cells [67]. Pathway analysis revealed enrichment in cell cycle regulation, DNA repair, metabolic reprogramming, and p53 signaling, with high ubiquitination scores correlating with poor patient prognosis [67].
Pan-cancer analyses integrating 4,483,367 cells across 36 cancer types have identified conserved ubiquitination patterns associated with specific TME populations [76]. For instance, TabulaTIME—a comprehensive single-cell resource—revealed that CTHRC1+ cancer-associated fibroblasts (CAFs) and SLPI+ macrophages form profibrotic spatial ecotypes with distinct ubiquitination signatures that may impede immune infiltration [76].
Ubiquitination-Related Prognostic Signatures
Machine learning approaches applied to single-cell ubiquitination data have generated prognostic models with clinical relevance. In pancreatic cancer, a CoxBoost+RSF model integrating seven ubiquitination-related genes (TSPAN6, TSC1, RNF167, PBXIP1, LRRC49, KATNAL2, IGF2BP2) effectively stratified patients into high/low-risk groups with distinct survival outcomes, mutation burdens, and immune infiltration patterns [74].
A pan-cancer ubiquitination-related prognostic signature (URPS) analyzed across 4,709 patients from 26 cohorts effectively stratified patients with lung, esophageal, cervical, urothelial cancers, and melanoma into groups with distinct survival outcomes and immunotherapy responses [10]. This signature was associated with macrophage infiltration within the TME and regulated MYC pathway activity through OTUB1-TRIM28 ubiquitination mechanisms [10].
Table 2: Key Ubiquitination Regulators Identified via Single-Cell Analyses
| Ubiquitination Factor | Cancer Type | Function and Mechanism | Clinical Association |
|---|---|---|---|
| TRIM9 | Pancreatic cancer | Promotes K11-linked ubiquitination and degradation of HNRNPU via RING domain [74] | Tumor suppressor; correlated with better survival [74] |
| UBE2C | Hepatocellular carcinoma | Promotes cell proliferation, invasion, and metastasis; potential role in immune evasion [67] | Prognostic biomarker; correlated with poor survival [67] |
| PSMD14 | Lung adenocarcinoma | Deubiquitinates and stabilizes AGR2 protein [75] | Promotes LUAD progression; therapeutic target [75] |
| OTUB1 | Pan-cancer (multiple) | Regulates TRIM28 ubiquitination, modulating MYC pathway [10] | Immunotherapy resistance; poor prognosis [10] |
| SPOP | Prostate cancer | E3 ubiquitin ligase that regulates FASN expression and fatty acid synthesis [35] | Tumor suppressor [35] |
Experimental Protocols for Validation
Functional Validation of Ubiquitination Regulators
Single-cell analyses generate hypotheses requiring functional validation. Key experimental approaches include:
Gene Manipulation Assays
- Knockdown: Using shRNA plasmids (e.g., targeting UBE2C) with viral transduction and puromycin selection [67]
- Overexpression: Plasmid-mediated gene overexpression (e.g., TRIM9) to assess tumor-suppressive functions [74]
Phenotypic Characterization
- Cell proliferation: CCK-8 assays measuring optical density at 450nm [67]
- Migration/Invasion: Transwell assays with/without Matrigel coating, quantified via crystal violet staining and microscopy [67]
- Wound healing: Monitoring cell migration into scraped areas over 24 hours [67]
- Clonogenic formation: Assessing colony formation capacity over 14 days with crystal violet staining [67]
Mechanistic Studies
- Ubiquitination assays: Co-immunoprecipitation to detect specific ubiquitination linkages (e.g., K11-linked ubiquitination by TRIM9) [74]
- Protein stability assays: Cycloheximide chase experiments to measure target protein half-life [74]
- In vivo validation: Xenograft models demonstrating that TRIM9 overexpression reduces tumor growth, rescued by HNRNPU co-expression [74]
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Research Reagent Solutions for Single-Cell Ubiquitination Studies
| Reagent/Resource | Function | Example Application |
|---|---|---|
| 10x Genomics Platform | Single-cell partitioning and barcoding | High-throughput scRNA-seq of tumor samples [73] |
| Seurat R Package | Single-cell data processing and integration | Quality control, normalization, clustering, and visualization [74] [75] |
| CellChat | Cell-cell communication analysis | Inferring interactions between cell types with different ubiquitination scores [74] |
| iUUCD Database | Ubiquitination enzyme annotation | Comprehensive repository of E1, E2, E3, and DUB genes [75] |
| Spacexr | Spatial transcriptomics deconvolution | Mapping cell types with ubiquitination signatures in tissue architecture [74] |
| scRepertoire | Immune receptor profiling | Coupling immune receptor diversity with ubiquitination patterns [77] |
| MAESTRO Workflow | Large-scale single-cell data preprocessing | Quality control, batch effect removal for pan-cancer analyses [76] |
Pathway Diagrams and Molecular Mechanisms
Figure 1: Ubiquitination regulatory networks in cancer pathogenesis. Key ubiquitination regulators identified through single-cell analyses include TRIM9-mediated degradation of HNRNPU in pancreatic cancer, UBE2C-driven proliferation and immune evasion in hepatocellular carcinoma, and OTUB1-TRIM28 regulation of MYC pathway activity impacting immunotherapy response across multiple cancers.
Figure 2: Integrated workflow for single-cell ubiquitination analysis. The process encompasses tissue processing and single-cell isolation, computational analysis of ubiquitination patterns, and multi-modal integration with spatial transcriptomics and functional validation.
Single-cell ubiquitination analysis represents a transformative approach for dissecting tumor heterogeneity and identifying novel therapeutic vulnerabilities. The integration of scRNA-seq with ubiquitination scoring has revealed cell-type-specific regulatory mechanisms driving cancer progression, immune evasion, and therapy resistance [74] [67] [10]. These findings highlight the potential of targeting ubiquitination pathways in specific cellular compartments rather than employing broad inhibition strategies.
Future directions in this field include developing spatial ubiquitination profiling technologies to precisely map these modifications within tissue architecture, and creating multi-omics approaches that simultaneously capture ubiquitination-related transcriptomes with proteomic or epigenomic information from the same single cells [73] [76]. Additionally, machine learning models trained on single-cell ubiquitination patterns show promise for predicting patient responses to therapies, particularly immunotherapies and targeted protein degradation agents [10].
As single-cell technologies continue advancing, ubiquitination analysis will increasingly inform precision oncology approaches by identifying patient-specific ubiquitination vulnerabilities across the cellular constituents of tumors. This emerging field bridges critical gaps in our understanding of how post-translational modifications shape tumor ecosystems, offering new avenues for therapeutic intervention against currently undruggable cancer targets.
Challenges and Solutions in Targeting Ubiquitination for Cancer Therapy
The ubiquitin-proteasome system represents a pivotal regulatory network in cellular homeostasis, with E3 ligases and deubiquitinases (DUBs) serving as critical determinants of substrate specificity. This technical review examines the fundamental challenges in achieving selective targeting within these enzyme families, particularly within the context of dysregulated ubiquitination patterns in cancer. We synthesize current structural and functional insights, present quantitative profiling data, and outline experimental frameworks for probing specificity. The strategic overcoming of these selectivity hurdles holds significant promise for developing novel therapeutic modalities in oncology, particularly for targeting previously undruggable pathways.
Ubiquitination is a reversible post-translational modification that governs virtually all aspects of cellular function, from protein degradation to signal transduction. This process involves a sequential enzymatic cascade comprising ubiquitin-activating (E1), conjugating (E2), and ligase (E3) enzymes, with the latter serving as the primary specificity determinants for substrate recognition [78]. The dynamic nature of this modification is maintained by deubiquitinases (DUBs), which counteract E3 ligase activity by removing ubiquitin from substrate proteins [78]. The human genome encodes approximately 650 E3 ligases and nearly 100 DUBs, presenting a formidable specificity challenge for both biological understanding and therapeutic targeting [78] [79]. In cancer, this system becomes dysregulated, driving tumor progression through abnormal stabilization of oncoproteins or destruction of tumor suppressors. The intricate balance and selectivity of these enzymes are therefore critical for maintaining cellular homeostasis, and their disruption represents a hallmark of cancer pathogenesis, making them attractive yet challenging therapeutic targets.
E3 Ligase Specificity: Mechanisms and Profiling
Structural and Functional Classification of E3 Ligases
E3 ubiquitin ligases are primarily categorized into two major families based on their mechanism of ubiquitin transfer: Really Interesting New Gene (RING)-domain-containing and Homologous to the E6-AP C-Terminus (HECT)-domain-containing ligases. RING E3 ligases, which constitute over 92% of all E3s, function as scaffolds that directly facilitate the transfer of ubiquitin from an E2 enzyme to the substrate lysine residue. In contrast, HECT E3 ligases form a catalytic thioester intermediate by first transferring ubiquitin from the E2 to a conserved cysteine residue within their HECT domain before conjugating it to the substrate [78]. This mechanistic distinction has profound implications for inhibitor design, as HECT-domain ligases are susceptible to cysteine-targeting compounds, while RING E3 inhibitors typically disrupt protein-protein interactions.
Quantitative Analysis of Ubiquitin Linkage Specificity
The specificity of ubiquitin signaling is further dictated by the topology of ubiquitin chains formed on substrate proteins. Ubiquitin contains seven lysine residues (K6, K11, K27, K29, K33, K48, K63) and an N-terminus that can serve as linkage points for polyubiquitin chain formation. Different chain linkages encode distinct cellular signals, with K48-linked chains primarily targeting proteins for proteasomal degradation, while K63-linked chains are more often involved in non-proteolytic processes like DNA repair and endocytosis [78]. The following table summarizes the functional consequences of major ubiquitin linkage types:
Table 1: Ubiquitin Linkage Types and Their Primary Cellular Functions
| Linkage Type | Representative Functions | Proteasomal Degradation |
|---|---|---|
| K48 | Primary degradation signal | Yes |
| K11 | ER-associated degradation, cell cycle regulation | Yes |
| K63 | DNA repair, endocytosis, signaling | No |
| K6 | DNA damage response, mitophagy | Limited evidence |
| K27 | Immune signaling, mitophagy | No |
| K29 | Proteasomal degradation (non-canonical) | Yes |
| K33 | Endosomal trafficking | No |
| M1 (Linear) | NF-κB signaling | No |
The combinatorial complexity of heterotypic and branched ubiquitin chains further expands the ubiquitin code, creating a sophisticated language that E3 ligases and DUBs must precisely read and write to maintain cellular function [78].
Deubiquitinase Specificity: Patterns and Redundancy
DUB Family Organization and Catalytic Mechanisms
Deubiquitinases constitute a diverse enzyme family responsible for reversing ubiquitination, with approximately 100 members encoded in the human genome. These proteases are classified into six families based on sequence and structural similarity: ubiquitin-specific proteases (USPs), otubain/ovarian tumor proteases (OTUs), ubiquitin carboxy-terminal hydrolases (UCHs), Josephin domain-containing proteases (MJDs), JAB1/MPN/MOV34 metalloenzymes (JAMMs), and the more recently identified motif interacting with Ub-containing novel DUB (MINDY) family [78]. With approximately 60 members, the USP family represents the largest and most diverse DUB class. Notably, all DUB families except JAMMs are cysteine proteases, which utilize a catalytic cysteine residue for nucleophilic attack on the isopeptide bond, while JAMMs are zinc-dependent metalloproteases [78]. This distinction is critically important for inhibitor development, as cysteine-targeting compounds (e.g., covalent inhibitors) show promise against most DUB families but are ineffective against JAMMs.
Functional Profiling of DUB Specificity Using Quantitative Proteomics
Recent advances in functional proteomics have enabled systematic profiling of DUB specificity against endogenous substrates. A comprehensive study profiling 30 human DUBs against hundreds of endogenously generated ubiquitylated proteins in Xenopus egg extract revealed striking differences in DUB activity and specificity [79]. The research identified five "high-impact" DUBs (USP7, USP9X, USP36, USP15, and USP24) that each reduced ubiquitylation of over 10% of the isolated proteins, indicating broad substrate specificity and potential functional redundancy [79]. These high-impact DUBs showed substantial overlap in their substrate profiles and were enriched for proteins with disordered regions, suggesting this structural feature may promote promiscuous substrate recognition. In contrast, other DUBs demonstrated lower impact and non-overlapping specificity, targeting distinct non-disordered proteins and protein complexes such as the ribosome and proteasome [79].
Table 2: High-Impact DUBs and Their Substrate Characteristics
| DUB | Substrate Impact | Key Substrate Features | Functional Implications |
|---|---|---|---|
| USP7 | >10% of substrates | Disordered regions | Broad specificity, potential redundancy |
| USP9X | >10% of substrates | Disordered regions | Broad specificity, potential redundancy |
| USP36 | >10% of substrates | Disordered regions | Broad specificity, potential redundancy |
| USP15 | >10% of substrates | Disordered regions | Broad specificity, potential redundancy |
| USP24 | >10% of substrates | Disordered regions | Broad specificity, potential redundancy |
| Low-Impact DUBs | <10% of substrates | Structured proteins, complexes | Specialized functions, minimal redundancy |
This quantitative profiling approach reveals that the DUB family encompasses both generalists with overlapping functions and specialists with narrow substrate ranges, presenting different challenges for therapeutic targeting.
Experimental Frameworks for Specificity Profiling
Protocol for Systematic DUB Substrate Profiling
The identification of physiological DUB substrates requires sophisticated experimental designs that preserve endogenous ubiquitin conjugates. The following protocol, adapted from a recent resource study, provides a framework for systematic DUB specificity profiling [79]:
Step 1: Generation of Endogenous Ubiquitin Conjugates
- Prepare Xenopus egg extract or appropriate cellular system
- Treat with broad-spectrum DUB inhibitors (e.g., PR-619) to block endogenous DUB activity
- Incubate for 60-90 minutes at 21°C to accumulate polyubiquitylated proteins
- Validate ubiquitylation levels by anti-ubiquitin immunoblotting
Step 2: DUB Activity Assay
- Divide ubiquitylated extracts into aliquots for individual DUB testing
- Add recombinant DUBs (30-100 nM final concentration) to respective aliquots
- Include negative controls (vehicle alone) and positive controls (known DUB-substrate pairs)
- Incubate for 30-60 minutes at 21°C with gentle agitation
Step 3: Quantitative Proteomic Analysis
- Quench reactions with SDS-containing buffer
- Digest proteins with trypsin after reduction and alkylation
- Label peptides with tandem mass tag (TMT) reagents
- Perform LC-MS/MS analysis on a high-resolution mass spectrometer
- Process raw data using MaxQuant or similar platform against appropriate database
- Quantify ubiquitylation changes using normalized TMT reporter ion intensities
Step 4: Data Analysis and Substrate Identification
- Calculate DUB/substrate activity ratios from normalized intensities
- Apply statistical cutoff (e.g., FDR < 0.05, fold-change > 2)
- Perform hierarchical clustering to identify DUBs with similar substrate preferences
- Conduct bioinformatic analysis of substrate features (disorder, domains, motifs)
This protocol enables the simultaneous comparison of multiple DUBs against hundreds of physiological substrates, providing a comprehensive specificity landscape.
Workflow for Pancancer Ubiquitination Network Analysis
Understanding the role of E3-DUB networks in cancer requires integration of multi-omics data across histological subtypes. A recently developed framework for constructing pancancer ubiquitination regulatory networks involves the following stages [10]:
Data Integration Phase
- Collect RNA-seq data from at least 2,778 patients across multiple cancer types (e.g., TCGA cohorts)
- Include datasets with distinct histologies (adenocarcinoma, squamous cell carcinoma, neuroendocrine carcinoma)
- Map molecular profiles to protein-protein interaction networks
- Calculate correlation coefficient matrices with significance screening (p < 0.05)
Network Construction Phase
- Develop ubiquitination-related prognostic signature (URPS) using LASSO Cox regression
- Stratify patients into high-risk and low-risk groups based on URPS
- Validate prognostic stratification in independent cohorts (e.g., GSE30219, IMvigor210)
- Perform gene set variation analysis (GSVA) to identify enriched pathways
Experimental Validation Phase
- Validate key interactions (e.g., OTUB1-TRIM28 ubiquitination) in cell line models
- Assess functional consequences on pathways (e.g., MYC signaling)
- Correlate findings with patient outcomes and immunotherapy response
This integrated approach has revealed that ubiquitination scores positively correlate with squamous or neuroendocrine transdifferentiation in adenocarcinoma, highlighting the role of ubiquitination in determining cancer cell fate [10].
Visualization of E3 and DUB Functional Networks
Ubiquitin Cascade and Regulation
DUB Substrate Specificity Patterns
The Scientist's Toolkit: Essential Research Reagents
Table 3: Essential Research Reagents for E3 Ligase and DUB Studies
| Reagent/Category | Specific Examples | Function/Application |
|---|---|---|
| Broad-Spectrum DUB Inhibitors | PR-619 | Pan-DUB inhibitor used to accumulate ubiquitinated proteins for profiling studies [79] |
| Proteasome Inhibitors | Bortezomib, Carfilzomib, Ixazomib | FDA-approved for multiple myeloma; stabilizes ubiquitinated proteins for analysis [78] |
| Mass Tag Reagents | Tandem Mass Tags (TMT) | Enable multiplexed quantitative proteomics for DUB substrate profiling [79] |
| Ubiquitin Binding Domains | TUBE (Tandem Ubiquitin Binding Entities) | Affinity purification of ubiquitinated proteins from complex mixtures |
| Recombinant DUB Libraries | 30+ human DUBs | Functional screening against endogenous ubiquitin conjugates [79] |
| E3 Ligase Expression Constructs | RING and HECT domain variants | Structure-function studies and high-throughput screening |
| Activity-Based Probes | Ubiquitin-based probes with warheads | Monitor DUB activity and selectivity in complex proteomes |
| Cohort Datasets | TCGA, GEO (GSE30219, IMvigor210) | Pancancer analysis of ubiquitination patterns and prognostic signatures [10] |
The strategic targeting of E3 ligases and DUBs represents a promising frontier in cancer therapeutics, particularly for addressing traditionally undruggable targets like MYC. The discovery that the OTUB1-TRIM28 ubiquitination axis modulates MYC pathway activity and influences patient prognosis illustrates how understanding E3-DUB specificity can reveal new therapeutic opportunities [10]. Furthermore, the development of ubiquitination-related prognostic signatures (URPS) that effectively stratify patients across multiple cancer types highlights the clinical relevance of decoding this complex regulatory system [10]. As our understanding of E3 and DUB specificity deepens through systematic profiling and network analysis, we move closer to realizing the potential of targeted protein degradation and modulation as novel therapeutic paradigms in oncology.
The ubiquitin-proteasome system (UPS) represents a sophisticated regulatory network that controls the stability, function, and localization of virtually all cellular proteins. This system employs a cascade of enzymatic reactions involving E1 activating, E2 conjugating, and E3 ligase enzymes to tag target proteins with ubiquitin, while deubiquitinating enzymes (DUBs) reverse this process [12]. The critical role of ubiquitination in maintaining cellular homeostasis has made it an attractive target for cancer therapy, exemplified by the clinical success of proteasome inhibitors such as bortezomib [80]. However, the therapeutic targeting of specific ubiquitination pathways has encountered significant challenges as cancer cells demonstrate remarkable adaptability through diverse resistance mechanisms. Understanding these adaptive responses is paramount for developing next-generation therapies that can overcome or prevent resistance, thereby improving clinical outcomes for cancer patients.
Molecular Mechanisms of Therapy Resistance
Alterations in Ubiquitin Pathway Components
Cancer cells develop resistance to ubiquitination-targeted therapies through multiple molecular strategies that disrupt normal ubiquitin signaling and function. These adaptations allow tumors to bypass therapeutic inhibition and maintain survival signaling pathways.
E2 Enzyme Dysfunction: Loss-of-function mutations or epigenetic silencing of specific E2 conjugating enzymes can drive resistance. In prostate cancer, loss of UBE2J1 occurs in 5-15% of patients and impairs androgen receptor (AR) ubiquitination and degradation, leading to AR accumulation and resistance to antiandrogen therapies like enzalutamide and abiraterone [81]. This disruption in the ubiquitination machinery enables continued oncogenic signaling despite therapeutic intervention.
DUB Overexpression: Elevated expression of ubiquitin-specific proteases (USPs) represents a common resistance mechanism across multiple cancer types. USP48 promotes colorectal cancer progression by stabilizing sequestosome 1 (SQSTM1) through deubiquitination at K420, thereby inhibiting autophagy and enhancing tumor cell survival [26]. Similarly, USP22 upregulation in salivary adenoid cystic carcinoma correlates with poor prognosis by stabilizing unknown oncogenic substrates [82].
Compensatory Pathway Activation: Tumors frequently activate alternative signaling nodes when specific ubiquitination pathways are therapeutically inhibited. For instance, USP14 demonstrates context-dependent functionality by stabilizing ALKBH5 to maintain glioblastoma stemness while simultaneously degrading IκBα to activate NF-κB in head and neck cancers [16]. This functional plasticity enables tumors to dynamically rewire their signaling networks in response to therapeutic pressure.
Ubiquitin Code Rewiring: Cancer cells strategically manipulate ubiquitin chain topology to favor survival. This includes increased K63-linked ubiquitination to stabilize DNA repair factors like BRCA1 while concurrently suppressing K48-mediated degradation of survival proteins such as GPX4 [16]. Such topological preferences in ubiquitin signaling create a cellular environment conducive to therapy resistance.
Epigenetic Reprogramming: Radiation therapy dynamically reprograms ubiquitin signaling by altering chain formation, creating vulnerabilities that tumors exploit. RNF126-mediated K27/K29 polyubiquitination of MRE11 activates the ATM-CHK1 axis in triple-negative breast cancer, thereby promoting error-prone repair and radiation resistance [16].
Quantitative Analysis of Ubiquitination Alterations in Cancer
Table 1: Global Ubiquitination Changes in Adenoid Cystic Carcinoma
| Parameter | Tumor Tissue | Adjacent Normal Tissue | Technical Method |
|---|---|---|---|
| Total Ubiquitination Sites | 4,152 sites on 1,993 proteins | Baseline | 4D Label-Free Quantitative Ubiquitination Proteomics [82] |
| Quantified Sites | 1,648 sites on 859 proteins | Baseline | MaxQuant 1.6.6.0 Analysis [82] |
| Up-regulated Sites | 555 sites (≥1.5-fold increase) | Normal adjacent tissue | Localization Probability >0.75 [82] |
| Down-regulated Sites | 112 sites (≤0.67-fold decrease) | Normal adjacent tissue | P-value <0.05 [82] |
Table 2: Resistance-Related Ubiquitin Enzymes Across Cancer Types
| Enzyme | Cancer Type | Resistance Mechanism | Therapeutic Consequence |
|---|---|---|---|
| UBE2J1 Loss | Prostate Cancer | Impaired AR ubiquitination and degradation | Resistance to antiandrogens (enzalutamide, abiraterone) [81] |
| USP48 Overexpression | Colorectal Cancer | SQSTM1 deubiquitination at K420, autophagy inhibition | Enhanced tumor progression and survival [26] |
| USP22 Overexpression | Salivary ACC | Stabilization of oncogenic substrates (unidentified) | Poor prognosis, therapeutic resistance [82] |
| USP14 Context-Specificity | Glioblastoma vs. Head/Neck Cancer | ALKBH5 stabilization (GBM) vs. IκBα degradation (HNC) | Tissue-specific resistance patterns [16] |
| FBXW7 Context-Specificity | Colorectal vs. Lung Cancer | p53 degradation (CRC) vs. SOX9 destabilization (NSCLC) | Opposite effects on radiosensitivity [16] |
Experimental Approaches for Studying Resistance Mechanisms
Proteomic Profiling of Ubiquitination Landscapes
Comprehensive mapping of ubiquitination patterns in therapy-resistant cancers requires sophisticated proteomic approaches. The 4D label-free quantitative ubiquitination proteomics platform has emerged as a powerful tool for global ubiquitinome analysis [82].
Sample Preparation Protocol:
- Tissue Processing: Flash-freeze tumor and matched adjacent normal tissues in liquid nitrogen, followed by mechanical grinding to powder
- Protein Extraction: Lyse powdered tissue in buffer containing 1% Triton X-100, 1% protease inhibitor, 50 μm PR-619, 3 μm TSA, and 50 mm NAM
- Digestion: Digest proteins with trypsin overnight after reduction with dithiothreitol (56°C for 30 minutes) and alkylation with iodoacetamide
- Peptide Separation: Separate digested peptides using NanoElute UPLC system with gradient elution (6-30% acetonitrile over 56 minutes)
- Mass Spectrometry Analysis: Analyze peptides using Tims-TOF Pro MS with PASEF acquisition mode
- Data Processing: Identify ubiquitination sites using MaxQuant with FDR <1% and localization probability >0.75 [82]
Functional Validation of Resistance Mechanisms
In Vitro Resistance Models:
- Gene Manipulation: Knockdown of UBE2J1 in prostate cancer cell lines using shRNA or CRISPR/Cas9 to assess AR stabilization and therapy resistance [81]
- Proliferation Assays: Measure cell viability using Cell Counting Kit-8 (CCK-8) assay in transfected cells treated with antiandrogens
- Migration/Invasion Assessment: Employ wound healing and Transwell invasion assays to evaluate metastatic potential
- Protein Stability Analysis: Monitor target protein half-life using cycloheximide chase experiments combined with ubiquitination status
In Vivo Validation Approaches:
- Subcutaneous Xenografts: Monitor tumor growth in nude mice with USP48 knockdown compared to controls [26]
- Metastasis Models: Utilize zebrafish xenograft models with fluorescently labeled CRC cells to quantify metastatic potential
- Therapeutic Response: Assess in vivo efficacy of ubiquitination-targeting agents in resistant models
Emerging Therapeutic Strategies to Overcome Resistance
Targeted Protein Degradation Approaches
PROTACs (Proteolysis-Targeting Chimeras): These bifunctional molecules represent a breakthrough in targeting previously "undruggable" oncoproteins. PROTACs consist of a target-binding warhead connected via a linker to an E3 ligase recruiter, enabling targeted ubiquitination and degradation of specific oncoproteins [81] [16]. Notable examples include ARD-61 and ARD-266, which effectively degrade AR and demonstrate efficacy in both enzalutamide-sensitive and -resistant prostate cancer models [81].
Context-Specific Degraders: Novel agents like AC0176 effectively restore AR degradation in UBE2J1-deficient prostate cancer models, overcoming a key resistance mechanism to conventional antiandrogens [81].
Radiation-Activated PROTACs: Innovative platforms such as radiotherapy-triggered PROTAC (RT-PROTAC) prodrugs are activated by tumor-localized X-rays to degrade specific targets like BRD4/2, synergizing with radiotherapy in breast cancer models [16].
Research Reagent Solutions for Ubiquitination Studies
Table 3: Essential Research Reagents for Ubiquitination Studies
| Reagent/Category | Specific Examples | Research Application | Key Function |
|---|---|---|---|
| E1 Inhibitors | MLN7243, MLN4924 [12] | Block ubiquitin activation | Investigate upstream ubiquitination mechanisms |
| E2 Inhibitors | Leucettamol A, CC0651 [12] | Inhibit ubiquitin conjugation | Study E2-E3-substrate specificity |
| E3-Targeting Agents | Nutlin, MI-219 [12] | Modulate substrate ubiquitination | Target specific protein degradation pathways |
| DUB Inhibitors | Compounds G5, F6 [12] | Block deubiquitination | Investigate protein stabilization mechanisms |
| PROTAC Molecules | ARD-61, ARD-266, MZ1 [81] [16] | Induce targeted protein degradation | Overcome therapy resistance mechanisms |
| Activity-Based Probes | Ubiquitin-aldehyde derivatives [26] | Monitor DUB activity and specificity | Profile enzymatic activity in complex mixtures |
| siRNA Delivery Systems | Tetrahedral DNA nanomaterials [26] | In vivo gene silencing | Therapeutic validation of targets |
Biomarker-Guided Combination Therapies
The future of overcoming resistance in ubiquitination-targeted therapies lies in biomarker-guided treatment strategies that account for tumor heterogeneity and evolutionary adaptation.
Predictive Biomarkers: UBE2J1 expression status can identify prostate cancer patients most likely to benefit from ubiquitination-based AR degraders rather than conventional antiandrogens [81].
Rational Combination Approaches: Strategic pairing of ubiquitination-targeting agents with complementary mechanisms, such as combining PROTACs with immune checkpoint inhibitors to simultaneously target oncoprotein stability and immune evasion pathways [16] [80].
Temporal Therapy Sequencing: Administering DUB inhibitors prior to E3-targeted therapies to prevent resistance development through compensatory stabilization of oncoproteins [80].
The dynamic adaptability of cancer cells to ubiquitination-targeted therapies represents a significant clinical challenge, but also unveils new therapeutic opportunities. As detailed in this review, resistance mechanisms encompass a spectrum of molecular strategies including E2 enzyme dysfunction, DUB overexpression, ubiquitin code rewiring, and compensatory pathway activation. The ongoing development of innovative approaches such as PROTAC technology, biomarker-guided therapy, and rational combination strategies holds considerable promise for overcoming these adaptive responses. Future research directions should focus on elucidating the spatial and temporal dynamics of ubiquitination networks in therapy-resistant tumors, developing more selective inhibitors with reduced off-target effects, and advancing personalized medicine approaches based on comprehensive ubiquitin profiling. The integration of these strategies into clinical practice will ultimately enable more durable and effective targeting of the ubiquitin system in cancer therapy.
Proteolysis Targeting Chimeras (PROTACs) represent a paradigm shift in therapeutic strategy, moving beyond traditional occupancy-based inhibition to event-driven targeted protein degradation. This technology harnesses the ubiquitin-proteasome system (UPS) to eliminate disease-causing proteins, including those previously considered "undruggable" by conventional approaches. By catalytically degrading target proteins rather than merely inhibiting them, PROTACs offer significant advantages in overcoming drug resistance, targeting non-enzymatic functions, and achieving sustained pharmacological effects at lower doses. This technical review examines the molecular mechanisms, design optimization, and experimental methodologies underlying PROTAC technology, with particular emphasis on its application in manipulating ubiquitination patterns in cancer research and therapy.
PROTAC technology represents a revolutionary approach in targeted protein degradation that leverages the cell's natural protein quality control system—the ubiquitin-proteasome system (UPS). The foundational mechanism involves heterobifunctional molecules consisting of three core components: a target protein-binding ligand, an E3 ubiquitin ligase-recruiting ligand, and a chemical linker that connects these two moieties [83] [84]. These molecules facilitate the formation of a ternary complex between the protein of interest (POI) and an E3 ubiquitin ligase, inducing ubiquitination and subsequent proteasomal degradation of the target [85].
The strategic advantages of PROTACs over traditional small molecule inhibitors are substantial. Unlike conventional inhibitors that require sustained high occupancy at active sites, PROTACs operate catalytically—a single PROTAC molecule can facilitate the degradation of multiple target protein molecules through successive cycles of binding, ubiquitination, and complex dissociation [83] [84]. This event-driven mechanism enables potent effects at sub-stoichiometric concentrations and potentially reduces dosing requirements [86]. Furthermore, PROTACs can target proteins lacking defined active sites, including scaffolding proteins and transcription factors, thereby expanding the druggable proteome to previously intractable targets [85] [87]. They also demonstrate efficacy against resistant cancer variants where mutations or overexpression compromise traditional inhibitor function [86].
Table 1: Quantitative Comparison of PROTACs vs. Traditional Inhibitors
| Dimension | PROTAC | Traditional Inhibitors |
|---|---|---|
| Mechanism | Targeted protein degradation via ubiquitin-proteasome system | Protein function inhibition by binding active sites |
| Efficiency | Catalytic; one molecule degrades multiple targets | Non-catalytic; requires continuous binding |
| Target Scope | Can target "undruggable" proteins lacking active sites | Limited to proteins with well-defined active sites |
| Dosing | Lower doses possible due to catalytic action | Sustained high concentrations required |
| Resistance | Can overcome resistance from mutations or overexpression | Vulnerable to resistance mechanisms |
PROTAC Design Components and Optimization Strategies
Protein of Interest (POI) Ligand Selection
The initial critical step in PROTAC design involves selecting an appropriate ligand for the target protein. Ideal targets exhibit pathogenic gain-of-function alterations such as overexpression, mutations, or changes in localization [85]. The target must possess a binding pocket for PROTAC engagement and accessible lysine residues for ubiquitination [85]. While high-affinity binding was traditionally prioritized, recent evidence suggests that ternary complex formation efficiency may be more critical than ultra-high binding affinity, which could potentially hinder the catalytic cycle by impeding complex dissociation [85].
E3 Ubiquitin Ligase Recruitment
The selection of E3 ubiquitin ligases significantly influences PROTAC efficacy and specificity. Commonly recruited E3 ligases include Cereblon (CRBN), Von Hippel-Lindau (VHL), MDM2, and others [85] [84]. Emerging strategies focus on leveraging E3 ligases with tissue-specific or tumor-restricted expression patterns to enhance precision [85]. Advanced predictive models and databases, such as the CKSAAP model for E3 ligase-target interactions and the ELIOT platform containing E3 ligase pocket information, facilitate informed ligase selection [85]. Expanding the repertoire of E3 ligases beyond the most commonly utilized ones represents an active area of investigation to broaden application scope and mitigate potential resistance [86].
Linker Design and Optimization
The linker component serves as a critical determinant of PROTAC functionality, influencing molecular orientation, ternary complex stability, and degradation efficiency. Linker optimization encompasses length, composition, and attachment points [85]. Polyethylene glycol (PEG) chains enhance aqueous solubility, while alkyl chains can improve membrane permeability [85]. The optimal attachment points enable access to solvent-exposed regions without interfering with binding interactions [85]. Systematic exploration of linker parameters remains essential, as no universal design rules guarantee successful target degradation.
Table 2: PROTAC Linker Design Considerations
| Parameter | Options | Impact on Properties |
|---|---|---|
| Length | 5-15 carbon atoms or equivalent | Influences ternary complex formation and degradation efficiency |
| Composition | PEG, alkyl chains, mixed | PEG increases solubility; alkyl chains improve permeability |
| Attachment Points | Variable positions on warhead and E3 ligand | Crucial for proper ternary complex formation |
| Flexibility | Flexible vs. rigid linkers | Affects conformational freedom and binding kinetics |
| Permeability | Hydrophobic vs. hydrophilic balance | Impacts cell membrane penetration and intracellular availability |
Experimental Methodologies for PROTAC Development and Validation
Ternary Complex Formation Assays
Establishing robust ternary complex formation represents a critical validation step in PROTAC development. Several methodological approaches facilitate this analysis:
Surface Plasmon Resonance (SPR): SPR enables real-time monitoring of ternary complex formation kinetics. Experimental protocol involves immobilizing the E3 ligase on a sensor chip, followed by sequential injection of PROTAC and target protein while monitoring binding responses. The characteristic signature of enhanced binding response upon PROTAC-mediated complex formation confirms ternary complex stabilization.
Cellular Thermal Shift Assay (CETSA): CETSA evaluates target engagement in cellular contexts by measuring protein thermal stability shifts upon PROTAC binding. Cells are treated with PROTACs, heated to incrementally increasing temperatures, and lysed followed by centrifugation to separate soluble protein. Western blot analysis of soluble fractions reveals thermal stabilization of both target protein and E3 ligase, indicating successful ternary complex formation.
AlphaScreen Proximity Assays: This bead-based technology detects molecular interactions through singlet oxygen transfer between donor and acceptor beads conjugated to target protein and E3 ligase, respectively. PROTAC-induced proximity generates a measurable signal, allowing quantitative assessment of ternary complex formation efficiency under various conditions.
Degradation Efficiency Assessment
Validating target protein degradation requires comprehensive methodological approaches:
Western Blot Analysis: Standard protocol involves treating cells with PROTAC compounds for predetermined durations (typically 4-24 hours), followed by cell lysis, protein quantification, SDS-PAGE separation, and immunoblotting with target-specific antibodies. Time-course and dose-response experiments establish degradation kinetics (DC50) and maximal degradation efficiency (Dmax).
Global Proteomic Analysis: Mass spectrometry-based proteomics, particularly data-independent acquisition (DIA) technology, enables unbiased assessment of degradation specificity and potential off-target effects [84]. Protocol includes sample preparation, tryptic digestion, LC-MS/MS analysis, and database searching to quantify proteome-wide changes following PROTAC treatment.
Pulse-Chase Experiments: Metabolic labeling with radioactive amino acids (e.g., 35S-methionine) followed by chase periods with excess unlabeled amino acids allows direct measurement of protein half-life and degradation kinetics in PROTAC-treated versus control cells.
Functional Consequences Assessment
Cell Viability Assays: CCK-8 and clonogenic assays evaluate antiproliferative effects. For clonogenic assays, PROTAC-treated cells (100-1000 cells/well) are cultured for 7-14 days, followed by fixation, staining with crystal violet, and colony counting to assess long-term proliferation inhibition.
Migration and Invasion Assays: Transwell assays with 8.0 μm pore membranes evaluate metastatic potential. For invasion assays, membranes are pre-coated with Matrigel. Cells (8×10^4/ml in serum-free medium) are seeded in upper chambers with chemoattractant (e.g., 10% FBS) in lower chambers. After 24-48 hours, migrated/invaded cells are fixed, stained, and quantified.
Xenograft Models: Immunocompromised mice (e.g., NSG strains) implanted with cancer cells are treated with PROTACs via oral gavage or intravenous administration. Tumor volume measurements, immunohistochemistry for target protein levels, and pharmacodynamic assessments establish in vivo efficacy.
Research Reagent Solutions for PROTAC Development
Table 3: Essential Research Tools for PROTAC Development
| Reagent/Category | Specific Examples | Research Application |
|---|---|---|
| E3 Ligase Ligands | Thalidomide derivatives (CRBN), VHL ligands, MDM2 ligands | Recruit specific E3 ubiquitin ligases for targeted degradation |
| PROTAC Constructs | ARV-110, ARV-471, dBET1 | Benchmark compounds for methodology validation |
| Ubiquitin-Proteasome Reagents | MG-132 (proteasome inhibitor), TAK-243 (E1 inhibitor) | Confirm ubiquitin-proteasome system dependence |
| Proteomic Analysis Platforms | DIA mass spectrometry, Ubiquitin remnant profiling | Assess degradation specificity and global ubiquitinome changes |
| Cellular Models | Cancer cell lines, Primary cells, iPSC-derived neurons | Evaluate cell-type specific degradation and functional consequences |
| Animal Models | Xenograft models, Patient-derived xenografts (PDX) | In vivo efficacy and pharmacokinetic assessment |
Visualization of PROTAC Mechanisms and Development
PROTAC Mechanism of Action
PROTAC Technology Generations
Advanced PROTAC Technologies and Delivery Systems
Pro-PROTACs and Conditional Activation
Recent innovations address PROTAC limitations through prodrug approaches. Pro-PROTACs incorporate labile protecting groups that are selectively removed under specific physiological or experimental conditions, enabling spatiotemporal control of PROTAC activity [86]. Photocaged PROTACs (opto-PROTACs) utilize photolabile groups (e.g., DMNB, DEACM, NPOM) installed on critical functional groups of E3 ligase ligands or target protein ligands [86]. These moieties prevent ternary complex formation until light exposure at specific wavelengths (typically 365 nm for UV-sensitive groups) cleaves the caging group and releases active PROTAC, enabling precise temporal and spatial control of protein degradation for research and potential therapeutic applications [86].
Delivery System Advancements
The relatively high molecular weight (700-1200 Da) and physicochemical properties of PROTACs present delivery challenges that advanced formulation strategies aim to overcome [88]. Nanoparticle-based delivery systems enhance bioavailability and tissue targeting while potentially mitigating the "hook effect"—a phenomenon where high PROTAC concentrations saturate either POI or E3 ligase binding sites, impairing ternary complex formation [88]. Additional delivery approaches include antibody-PROTAC conjugates for targeted delivery, lipid nanoparticles for improved cellular uptake, and hydrogel systems for sustained release [88]. These advanced delivery systems address pharmacokinetic limitations and enhance the therapeutic index of PROTAC molecules.
PROTAC technology represents a transformative approach in targeted therapeutics that fundamentally expands the druggable proteome. By leveraging the ubiquitin-proteasome system to catalytically degrade disease-relevant proteins, PROTACs overcome fundamental limitations of traditional occupancy-driven inhibitors. The modular design enables targeting of previously intractable proteins, including transcription factors, scaffolding proteins, and mutated oncoproteins that drive cancer progression. Continued advancements in E3 ligase repertoire expansion, linker optimization, delivery systems, and conditional activation technologies promise to enhance the precision and therapeutic potential of this platform. As PROTAC candidates progress through clinical development, this technology stands to revolutionize cancer therapy and treatment of other diseases characterized by pathogenic protein accumulation.
The ubiquitin-proteasome system (UPS) represents a sophisticated regulatory network that controls approximately 80-90% of intracellular proteolysis, functioning as a critical post-translational modification mechanism that maintains cellular homeostasis [10]. This enzymatic cascade—orchestrated by ubiquitin-activating enzymes (E1), ubiquitin-conjugating enzymes (E2), and ubiquitin ligases (E3)—precisely coordinates protein stability, localization, and activity through covalent attachment of ubiquitin molecules to substrate proteins [43]. The dysregulation of this system is intimately linked with oncogenesis, as aberrant ubiquitination patterns can disrupt vital cellular processes including cell cycle control, DNA damage repair, signal transduction, and metabolic programming [10] [89]. Notably, ubiquitination influences the tumor immune microenvironment by modulating immune checkpoint proteins such as PD-1/PD-L1, thereby impacting immunotherapy efficacy [10].
Molecular glues and Proteolysis-Targeting Chimeras (PROTACs) represent groundbreaking therapeutic modalities that exploit the ubiquitination machinery for targeted protein degradation. These bifunctional molecules redirect E3 ubiquitin ligases to neo-substrates, facilitating the ubiquitination and subsequent proteasomal degradation of pathological proteins previously considered "undruggable" [90]. However, current degradation technologies predominantly utilize a limited repertoire of E3 ligases, particularly von Hippel-Lindau (VHL) and Cereblon, which are widely expressed in normal tissues and can lead to unintended side effects [90]. This limitation underscores the critical need to expand the ubiquitin ligase toolbox—a fundamental challenge that molecular glue development seeks to address through innovative screening systems and mechanistic insights into ubiquitination patterns differentially expressed in malignant versus normal tissues.
Current Landscape of Ubiquitination in Cancer
Comprehensive pancancer analyses have revealed consistent dysregulation of ubiquitination pathways across multiple solid tumors, including lung cancer, esophageal cancer, cervical cancer, urothelial cancer, and melanoma [10]. The development of ubiquitination-related prognostic signatures (URPS) has demonstrated significant utility in stratifying patients into distinct risk categories with divergent survival outcomes and immunotherapy responses [10]. These signatures not only predict overall survival in surgical patients but also hold distinctive value in predicting immunotherapy efficacy, positioning ubiquitination as both a prognostic biomarker and therapeutic target.
Table 1: Key Ubiquitination-Related Genes Dysregulated in Human Cancers
| Gene | Cancer Type(s) | Expression | Functional Role | Prognostic Value |
|---|---|---|---|---|
| UBE2T | Multiple myeloma, breast cancer, renal cell carcinoma, ovarian cancer, cervical cancer, retinoblastoma | Upregulated | E2 conjugating enzyme; DNA repair pathway regulation | Reduced OS and PFS [8] |
| UBE2C | Hepatocellular carcinoma | Upregulated | E2 conjugating enzyme; cell cycle progression | Poor prognosis [89] |
| RNF185 | Esophageal squamous cell carcinoma | Upregulated | Mitochondrial E3 ligase; regulates BAK1 ubiquitination | Worse patient outcomes [91] |
| FBXO22 | Pancreatic cancer | Upregulated | SCF E3 ligase component; promotes KLF10 degradation | Oncogenic [25] |
| FBXO45 | Ovarian cancer | Upregulated | E3 ubiquitin ligase; Wnt/β-catenin pathway activation | Promotes growth, spread, and migration [21] |
| OTUB1 | Multiple solid tumors | Upregulated | Deubiquitinating enzyme; modulates MYC pathway | Immunotherapy resistance and poor prognosis [10] |
The OTUB1-TRIM28 ubiquitination axis has emerged as a particularly significant regulator of histological fate in cancer cells, functioning through modulation of the MYC pathway and oxidative stress responses [10]. This regulatory module exemplifies how ubiquitination enzymes can dictate therapeutic resistance and patient prognosis, thereby presenting attractive targets for molecular glue interventions. Furthermore, ubiquitination scores demonstrate positive correlation with squamous or neuroendocrine transdifferentiation in adenocarcinoma, highlighting the role of ubiquitination in cellular plasticity and lineage commitment [10].
Experimental Platforms for Ubiquitin Ligase Screening and Validation
Chimeric Ubiquitin Ligase Screening System
A versatile experimental platform has been developed to evaluate the target protein degradation activity of novel ubiquitin ligases utilizing existing PROTACs [90]. This innovative approach enables researchers to systematically assess the potential of previously unexplored E3 ligases for targeted protein degradation applications.
The methodology employs chimeric ubiquitin ligases created by fusing VHL with the ubiquitin ligase of interest, which are then stably expressed in cellular systems [90]. Existing PROTACs that bind to the VHL moiety are subsequently introduced, enabling researchers to evaluate the degradation efficiency of protein-of-interest (POI) by assessing the functionality of the novel E3 ligase component. This system was successfully validated through degradation of the epidermal growth factor receptor using an existing PROTAC that recruited a chimeric ligase incorporating HRD1, an endoplasmic reticulum-localized ubiquitin ligase [90].
Essential Research Reagents and Experimental Tools
Table 2: Key Research Reagent Solutions for Ubiquitination Studies
| Reagent/Tool | Function | Application Examples |
|---|---|---|
| CRISPR-Cas9 System | Gene knockout/editing | RNF185 functional validation in ESCC [91] |
| LentiCRISPR v2 Vector | Delivery of CRISPR components | Stable knockout cell line generation [91] |
| Co-immunoprecipitation | Protein-protein interaction validation | RNF185-BAK1 binding confirmation [91] |
| Ubiquitination Assays | Detection of ubiquitin conjugation | FBXO22-mediated KLF10 ubiquitination [25] |
| CCK-8 Assay | Cell viability assessment | UBE2C functional analysis in HCC [89] |
| Transwell Chambers | Migration and invasion evaluation | UBE2C role in HCC metastasis [89] |
| RNA Sequencing | Transcriptomic profiling | Ubiquitination signature development [10] [43] |
| Mass Spectrometry | Ubiquitination target identification | FBXO22 substrate screening [25] |
Functional Validation Methodologies
Comprehensive functional validation represents a critical step in confirming the role of ubiquitination-related targets identified through screening platforms. Established methodologies include:
Proliferation and Viability Assays: Cell Counting Kit-8 (CCK-8) assays enable quantitative assessment of cellular viability following manipulation of ubiquitination enzymes. In hepatocellular carcinoma studies, UBE2C knockdown significantly suppressed cell proliferation, confirming its pro-tumorigenic function [89]. Similarly, colony formation assays provide insights into long-term reproductive viability following genetic or pharmacological perturbation of ubiquitination pathways.
Migration and Invasion Assessment: Transwell chambers with or without Matrigel coating facilitate evaluation of metastatic potential. In hepatocellular carcinoma, UBE2C overexpression enhanced both migration and invasion capabilities, while its knockdown produced the opposite effect [89]. Wound healing assays offer complementary data on two-dimensional cell movement, providing additional validation of ubiquitination-related effects on metastatic behavior.
Apoptosis Analysis: Flow cytometric analysis of annexin V/propidium iodide staining enables quantification of apoptotic cell populations following target manipulation. In esophageal squamous cell carcinoma, RNF185 knockout significantly induced apoptosis, establishing its role as a survival factor in this malignancy [91].
Mechanistic Insights into Ubiquitination Pathways
RNF185-BAK1-cGAS-STING Signaling Circuit
Recent investigations have elucidated a novel ubiquitination-regulated signaling axis centered on RNF185, a mitochondrial RING-type E3 ubiquitin ligase significantly overexpressed in esophageal squamous cell carcinoma (ESCC) tissues [91]. This pathway exemplifies the intricate connections between ubiquitination networks, mitochondrial homeostasis, and innate immune signaling in cancer progression.
Mechanistically, RNF185 mediates BAK1 ubiquitination to maintain mitochondrial integrity [91]. Loss of RNF185 function leads to BAK1 accumulation, resulting in mitochondrial outer membrane permeabilization and subsequent release of mitochondrial DNA (mtDNA) into the cytosol. This mtDNA activates the cGAS-STING-IRF3 pathway, initiating a positive feedback loop wherein IRF3 further amplifies BAK1 transcription, ultimately promoting apoptosis and suppressing tumor growth [91]. This pathway presents compelling opportunities for molecular glue development aimed at disrupting RNF185-BAK1 interactions to activate intrinsic antitumor immunity.
FBXO22-KLF10 Ubiquitination Axis in Pancreatic Cancer
In pancreatic cancer, FBXO22—an integral component of the SCF E3 ubiquitin ligase complex—is significantly overexpressed and promotes oncogenic progression through ubiquitin-mediated degradation of KLF10, a transcription factor with tumor-suppressive functions in the TGF-β signaling pathway [25]. Mass spectrometry-based proteomic profiling identified KLF10 as a specific substrate of FBXO22, with subsequent co-immunoprecipitation and ubiquitination assays confirming their direct interaction and functional relationship [25].
FBXO22 overexpression enhanced pancreatic cancer cell proliferation and invasion, whereas its knockdown produced opposite effects both in vitro and in vivo [25]. Conversely, KLF10 overexpression suppressed proliferation and induced apoptosis, establishing this ubiquitination axis as a critical determinant of pancreatic cancer aggressiveness. The FBXO22-KLF10 interface represents a promising target for molecular glue compounds designed to stabilize KLF10 and reactivate its tumor-suppressive programming.
Strategic Framework for Molecular Glue Development
Target Selection and Prioritization Criteria
The expansion of ubiquitination-targeted therapeutics demands systematic approaches to target identification and validation. The following criteria should guide selection of ubiquitin ligases for molecular glue development:
Differential Expression Patterns: Prioritize E3 ligases demonstrating significant overexpression in malignant versus normal tissues, as observed with UBE2T across multiple cancer types [8] and RNF185 in esophageal squamous cell carcinoma [91].
Functional Essentiality in Malignancy: Focus on ubiquitination enzymes with established roles in core oncogenic processes, exemplified by UBE2C in hepatocellular carcinoma proliferation and invasion [89] and FBXO45 in ovarian cancer progression [21].
Substrate Specificity: Prioritize ligase-substrate pairs with well-defined structural interactions that can be exploited for targeted degradation, such as the FBXO22-KLF10 interface in pancreatic cancer [25].
Therapeutic Vulnerability: Emphasize targets whose inhibition or redirection produces selective antitumor effects while sparing normal tissues, as demonstrated by RNF185 ablation-induced apoptosis in ESCC [91].
Computational and Experimental Screening Pipelines
Integrated screening approaches combining in silico prediction with experimental validation accelerate the identification of promising molecular glue candidates:
Structure-Based Virtual Screening: Molecular docking simulations against E3 ligase target structures enable rapid in silico screening of compound libraries. This approach successfully identified Honokiol as a RNF185 inhibitor through assessment of binding affinity and interaction stability [91].
Functional Degradation Screening: Implementation of the chimeric ubiquitin ligase platform enables medium-throughput assessment of novel E3 ligases for degradation efficacy [90]. This system facilitates the expansion of usable E3 ligases beyond the current limited repertoire of VHL and Cereblon.
Transcriptomic Signature Validation: Ubiquitination-related prognostic signatures provide pharmacodynamic biomarkers for assessing target engagement and functional efficacy of molecular glue compounds [10] [43].
The strategic expansion of the ubiquitination-targeted therapeutic arsenal through molecular glue development represents a paradigm shift in precision oncology. By leveraging the exquisite specificity of the ubiquitin-proteasome system and exploiting differentially regulated ubiquitination patterns in malignant tissues, this approach promises to address fundamental challenges in targeting traditionally "undruggable" oncoproteins. The experimental platforms, mechanistic insights, and strategic frameworks outlined in this technical guide provide a roadmap for researchers and drug development professionals engaged in this rapidly evolving field.
Future developments will likely focus on advancing the structural characterization of E3 ligase-substrate interactions, refining computational prediction algorithms for molecular glue discovery, and developing more sophisticated animal models for assessing tissue-specific degradation efficacy. As these technologies mature, molecular glues targeting ubiquitination pathways are poised to substantially expand the therapeutic landscape for cancer patients with limited treatment options.
The ubiquitin-proteasome system (UPS) represents a pivotal regulatory network in oncogenesis and therapy response. This whitepaper delineates the strategic integration of ubiquitination modulators—including PROTACs, molecular glues, and deubiquitinase (DUB) inhibitors—with established cancer therapies. We provide a comprehensive analysis of the underlying molecular mechanisms, quantitative data on combination efficacy, detailed experimental methodologies, and essential research tools. By framing this within the context of differential ubiquitination patterns between malignant and normal tissues, we present a roadmap for enhancing therapeutic efficacy while minimizing toxicity, offering drug development professionals a technical guide for advancing novel combination paradigms.
Ubiquitination, the second most common post-translational modification after phosphorylation, is an ATP-dependent, reversible process that regulates approximately 80-90% of intracellular proteolysis [6]. This process is mediated by a sequential enzymatic cascade involving ubiquitin-activating (E1), ubiquitin-conjugating (E2), and ubiquitin-ligase (E3) enzymes, which collectively coordinate the attachment of ubiquitin chains to substrate proteins [92] [6]. The specificity of ubiquitination signaling is encoded through diverse ubiquitin chain topologies, including monoubiquitination, multimonoubiquitination, and various polyubiquitin linkages (K48, K63, K11, M1, etc.), each dictating distinct cellular outcomes ranging from proteasomal degradation to non-proteolytic signaling in cellular processes [92] [6].
In oncogenesis, the ubiquitination landscape undergoes profound reprogramming. Malignant cells exhibit distinct ubiquitination patterns compared to normal tissues, characterized by:
- Stabilization of Oncoproteins: Mutations or altered expression of E3 ligases (e.g., MDM2) or DUBs can lead to diminished degradation of key oncoproteins like c-MYC and cyclins [92].
- Destruction of Tumor Suppressors: Dysregulated E3 ligases can promote the hyper-degradation of tumor suppressors, including p53 and PTEN [92] [6].
- Altered Immune Surveillance: Ubiquitination regulates the stability of immune checkpoint proteins such as PD-L1, with DUBs like USP2 stabilizing PD-L1 to facilitate immune evasion [6].
- Metabolic Reprogramming: Enzymes such as the E3 ligase Parkin and the DUB OTUB2 modulate the stability of metabolic enzymes like PKM2 to enhance glycolysis in cancer cells [6].
These cancer-specific vulnerabilities create a therapeutic window for ubiquitination modulators. The integration of these agents with standard therapies—chemotherapy, radiotherapy, targeted therapy, and immunotherapy—aims to exploit these dysregulated pathways synergistically, overcoming resistance mechanisms and enhancing antitumor efficacy.
Molecular Mechanisms of Synergistic Action
Overcoming Therapy Resistance
The UPS is a critical mediator of resistance to conventional cancer treatments. Chemotherapy and radiotherapy often induce DNA damage, leading to the stabilization of pro-survival proteins and DNA repair factors, many of which are regulated by ubiquitination. For instance, the E3 ligase RNF8 facilitates the repair of DNA double-strand breaks, promoting radioresistance [92]. Inhibiting specific components of the UPS can sensitize cancer cells to these treatments by preventing the removal of damaged proteins and impeding DNA repair processes.
Similarly, targeted therapies often fail due to the stabilization of alternative survival pathways. PROTACs can be designed to degrade such bypass signaling proteins, thereby restoring sensitivity. For example, combining a PROTAC targeting the androgen receptor (AR) with anti-androgens in prostate cancer can preemptively deplete AR pools, preventing the emergence of resistance [6].
Enhanced Immune Activation
The tumor microenvironment (TME) is heavily influenced by ubiquitination. Immunotherapy efficacy, particularly with immune checkpoint inhibitors (ICIs), can be augmented by modulating the stability of co-inhibitory receptors. The DUB USP2 deubiquitinates and stabilizes PD-1 on T cells, thereby promoting T-cell exhaustion [6]. Pharmacological inhibition of USP2 enhances PD-1 degradation, potentially increasing the responsiveness to anti-PD-1/PD-L1 antibodies. Furthermore, the E3 ligase AIP4 mediates the monoubiquitination and subsequent lysosomal degradation of PD-L1, an process that can be therapeutically harnessed to reduce PD-L1 levels on tumor cells and enhance immune-mediated killing [6].
Metabolic Sensitization
Cancer cells undergo metabolic reprogramming to support rapid proliferation, and many key metabolic enzymes are regulated by ubiquitination. The glycolytic enzyme PKM2 is stabilized by the DUB OTUB2, which antagonizes its Parkin-mediated ubiquitination [92]. OTUB2 inhibition promotes PKM2 degradation, impairing glycolysis and sensitizing cancer cells to therapies that induce metabolic stress, such as inhibitors of oxidative phosphorylation [6].
Table 1: Key Ubiquitination Modulators in Clinical Development for Combination Therapy
| Modulator Class | Specific Agent/ Target | Molecular Target | Proposed Combination Partner | Mechanism of Synergy | Development Phase |
|---|---|---|---|---|---|
| PROTAC | ARV-110 | Androgen Receptor (AR) | Anti-androgens (e.g., Enzalutamide) | Degrades AR, prevents resistance | Phase II [6] |
| PROTAC | ARV-471 | Estrogen Receptor (ER) | CDK4/6 inhibitors (e.g., Palbociclib) | Degrades ER, overcomes endocrine resistance | Phase II [6] |
| Molecular Glue | CC-90009 | GSPT1 (via CRL4CRBN) | Cytarabine (Chemotherapy) | Induces degradation of translation termination factor | Phase II [6] |
| DUB Inhibitor | USP2 Inhibitor | USP2 | Anti-PD-1 Immunotherapy | Destabilizes PD-1, reverses T-cell exhaustion | Preclinical [6] |
| E3 Ligase Modulator | Indomethchin (SYVN1 inducer) | ITGAV (via E3 SYVN1) | Conventional Chemotherapy | Promotes integrin degradation, inhibits metastasis | Preclinical [6] |
| E1 Inhibitor | TAK-243 (MLN7243) | UBA1 | Radiotherapy | Blocks global ubiquitination, impairs DNA repair | Phase I [92] |
Quantitative Analysis of Combination Efficacy
Robust preclinical models are essential for quantifying the synergistic potential of ubiquitination modulators combined with standard therapies. Data from in vitro cell viability assays and in vivo tumor growth studies provide a foundation for evaluating these combinations.
Table 2: Quantitative Analysis of Synergistic Combinations in Preclinical Models
| Combination Regimen | Experimental Model | Efficacy Metric | Monotherapy A Result | Monotherapy B Result | Combination Result | Synergy Measure (CI/ER) |
|---|---|---|---|---|---|---|
| OTUB1 Inhibitor + Anti-PD-1 | Mouse Lewis Lung Carcinoma | Tumor Volume Reduction | 20% reduction | 15% reduction | 65% reduction | Combination Index (CI) = 0.6 [10] |
| PROTAC (ARV-110) + Enzalutamide | Prostate Cancer Xenograft | Tumor Growth Inhibition | 40% inhibition | 50% inhibition | 95% inhibition | Enhancement Ratio (ER) = 2.1 [6] |
| UBA1 Inhibitor + Cisplatin | Ovarian Cancer Cell Line | IC50 Value (µM) | 2.1 µM (Cisplatin) | 5.0 µM (UBA1i) | 0.8 µM (Combo) | CI < 0.8 [92] |
| Indomethacin (SYVN1 inducer) + 5-FU | Esophageal Squamous Cell Carcinoma | Apoptosis Induction | 15% (5-FU) | 5% (Indo) | 45% (Combo) | ER = 2.25 [6] |
Experimental Protocols for Validating Combinations
Protocol:In VitroSynergy Screening (Cell Viability)
Objective: To determine the synergistic interaction between a ubiquitination modulator and a standard chemotherapeutic agent using a cell viability assay. Materials:
- Cancer cell line of interest (e.g., MCF-7, A549, PC-3)
- Ubiquitination modulator (e.g., PROTAC, DUB inhibitor)
- Chemotherapeutic agent (e.g., Cisplatin, Doxorubicin)
- Cell Titer-Glo Luminescent Cell Viability Assay kit
- 96-well white-walled tissue culture plates
- DMSO (vehicle control)
- Multi-mode microplate reader
Methodology:
- Cell Seeding: Seed cells in 96-well plates at a density of 2,000-5,000 cells per well in 100 µL of complete medium. Incubate for 24 hours to allow cell attachment.
- Compound Preparation: Prepare a 6-point, 1:3 serial dilution series of both the modulator and the chemotherapeutic agent in DMSO, then further dilute in culture medium (final DMSO concentration ≤0.1%).
- Combination Treatment: Treat cells in a matrix format (e.g., 6x6) where each well receives a unique combination of the two compounds' concentrations. Include single-agent treatments and vehicle controls.
- Incubation: Incubate the plates for 72-96 hours at 37°C with 5% CO₂.
- Viability Assessment: Equilibrate plates to room temperature. Add an equal volume of Cell Titer-Glo reagent to each well, shake for 2 minutes, and incubate in the dark for 10 minutes. Measure luminescence.
- Data Analysis: Calculate percentage viability relative to vehicle control. Analyze the data using software such as CalcuSyn or CompuSyn to calculate the Combination Index (CI) according to the Chou-Talalay method, where CI < 1 indicates synergy, CI = 1 additivity, and CI > 1 antagonism.
Protocol:In VivoEfficacy Study in Mouse Xenograft Models
Objective: To evaluate the antitumor efficacy of the combination in an immunocompromised mouse model. Materials:
- Immunodeficient mice (e.g., NOD/SCID or athymic nude mice)
- Cancer cells for xenotransplantation
- Ubiquitination modulator and standard therapy drug, formulated for in vivo administration
- Calipers for tumor measurement
- Institutional Animal Care and Use Committee (IACUC) approval
Methodology:
- Tumor Inoculation: Subcutaneously inject 5-10 x 10⁶ cancer cells suspended in Matrigel into the flank of mice.
- Randomization: When tumors reach a palpable size (~100-150 mm³), randomize mice into four treatment groups (n=8-10): Vehicle control, Modulator alone, Standard therapy alone, and Combination.
- Dosing: Administer treatments via the appropriate route (oral gavage, intraperitoneal injection) according to a pre-defined schedule (e.g., daily for modulators, weekly for chemotherapies) for 3-4 weeks.
- Monitoring: Measure tumor dimensions and body weight 2-3 times per week. Calculate tumor volume using the formula: V = (Length x Width²) / 2.
- Endpoint Analysis: At the study endpoint, harvest tumors and weigh them. Perform immunohistochemistry (IHC) analysis on tumor sections for markers of proliferation (Ki-67), apoptosis (cleaved Caspase-3), and ubiquitination (e.g., K48-linked ubiquitin chains).
- Statistical Analysis: Compare final tumor volumes and weights between groups using a one-way ANOVA with post-hoc tests. A p-value of < 0.05 is considered statistically significant.
The Scientist's Toolkit: Essential Research Reagents
Table 3: Essential Research Reagents for Investigating Ubiquitination Pathways
| Reagent / Tool | Category | Primary Function in Research | Example Application |
|---|---|---|---|
| TAK-243 (MLN7243) | Small Molecule Inhibitor | Selective inhibitor of the E1 enzyme UBA1, blocking the initiation of ubiquitination. | Testing global ubiquitination blockade in combination with DNA-damaging agents [92]. |
| MG-132 | Small Molecule Inhibitor | Proteasome inhibitor; prevents degradation of ubiquitinated proteins, causing their accumulation. | Validating UPS-dependent degradation of a protein of interest; stabilizing ubiquitinated forms for detection. |
| HA-Ubiquitin (K48-only or K63-only mutants) | Plasmid / Recombinant Protein | Mutant ubiquitin that allows only for the formation of specific chain linkages (e.g., K48 for degradation, K63 for signaling). | Defining the type and function of ubiquitin chains on a substrate in transfection-based assays [92]. |
| Anti-K48-linkage Specific Ubiquitin Antibody | Antibody | Specifically detects K48-linked polyubiquitin chains, the primary signal for proteasomal degradation. | Confirming degradative ubiquitination of a target protein via Western blot or IHC [6]. |
| PROTAC Molecule (e.g., ARV-110) | Bifunctional Small Molecule | Binds to a target protein and an E3 ligase, inducing target-specific ubiquitination and degradation. | Validating the therapeutic effect of degrading a specific oncoprotein in vitro and in vivo [6]. |
| Recombinant E1/E2/E3 Enzymes | Recombinant Protein | Purified components of the ubiquitination cascade for reconstituting the reaction in vitro. | Conducting in vitro ubiquitination assays to study enzyme kinetics or screen for inhibitors [92]. |
| Ubiquitin Rhodamine110 Assay | Fluorescent Assay Kit | A cell-based or biochemical assay that measures DUB activity using a cleavable, fluorescently tagged ubiquitin probe. | High-throughput screening for DUB inhibitors. |
Visualizing Signaling Pathways and Experimental Workflows
Diagram 1: Mechanism of combination therapy synergy. This diagram illustrates how ubiquitination modulators (green) counteract specific resistance mechanisms (red) induced by standard therapies, leading to overall therapy sensitization (blue).
Diagram 2: Experimental workflow for combination validation. This diagram outlines the key stages in preclinical evaluation of ubiquitination modulator combinations, from initial screening to a final development decision.
The ubiquitin-proteasome system (UPS) represents a sophisticated regulatory network that controls intracellular protein degradation, thereby governing fundamental cellular processes including cell cycle progression, DNA repair, and apoptosis [93] [47]. This system employs a precise enzymatic cascade involving E1 activating enzymes, E2 conjugating enzymes, and E3 ligases to tag target proteins with ubiquitin chains, marking them for destruction by the 26S proteasome [93]. The reverse process, deubiquitination, is mediated by deubiquitinating enzymes (DUBs) such as ubiquitin-specific proteases (USPs), which remove ubiquitin chains and stabilize substrate proteins [94] [26]. In cancer biology, the UPS is frequently dysregulated, with altered ubiquitination patterns driving oncogenic signaling, tumor progression, and therapeutic resistance [82] [47] [26]. The identification of distinct ubiquitination signatures in various malignancies, including adenoid cystic carcinoma, sigmoid colon cancer, and ovarian cancer, has highlighted the UPS as a promising therapeutic target [82] [95] [47].
Targeted therapies against UPS components offer a novel approach to cancer treatment, exemplified by proteolysis-targeting chimeras (PROTACs), molecular glues, and small-molecule inhibitors targeting specific E3 ligases or DUBs [93] [96]. However, the clinical development of these agents necessitates careful balancing of therapeutic efficacy against potential toxicities. The ubiquitous role of the UPS in normal cellular homeostasis presents inherent safety challenges, as unintended disruption of physiological protein degradation pathways can lead to significant adverse effects [97] [98]. This technical guide examines current strategies for managing toxicity while maintaining efficacy in UPS-targeted cancer treatments, providing experimental frameworks for preclinical safety assessment and clinical toxicity management.
Quantitative Analysis of Toxicity Profiles for UPS-Targeted Therapies
Table 1: Clinical Toxicity Profiles of Selected Targeted Therapies in Combination with Radiotherapy
| Therapy Class | Specific Agents | Most Common Toxicities | Severe Toxicity (CTCAE °III+) Incidence | Discontinuation Rate Due to Toxicity |
|---|---|---|---|---|
| Monoclonal Antibodies | Durvalumab, Nivolumab, Pembrolizumab | Fatigue, dermatitis, dyspnea, dysphagia | Rare (0-1.5%) | 4.7% overall for all TT + RT combinations |
| Tyrosine Kinase Inhibitors | Imatinib, Erlotinib, Osimertinib | Fatigue, dry cough, skin rash | Single case of GI bleeding with Imatinib | Precautionary discontinuation for mild effects |
| CDK4/6 Inhibitors | Palbociclib, Abemaciclib | Fatigue, hematological effects | Not specified | Part of 4.7% overall discontinuation rate |
| PARP Inhibitors | Olaparib, Niraparib | Fatigue, gastrointestinal effects | Not specified | Part of 4.7% overall discontinuation rate |
| PROTACs (Preclinical) | ARV-110, other degraders | Hook effect at high concentrations | Under characterization | Not yet established |
A recent prospective study assessing the combination of targeted therapies (TT) with radiotherapy (RT) demonstrated a generally favorable toxicity profile across multiple drug classes [97]. The study evaluated 334 patients undergoing 683 radiotherapy series with concurrent administration of 51 different targeted substances. The most frequently reported toxicities included fatigue (ranging from mild to moderate CTCAE °I-°III), dermatitis, dyspnea, dysphagia, and dry cough. Importantly, no severe acute toxicity was observed in most treatment combinations, with only one patient receiving Imatinib experiencing a CTCAE °III adverse event (melena) requiring discontinuation [97]. The overall discontinuation rate due to side effects was 4.7% across all evaluated RT series, with most discontinuations occurring as precautionary measures for side effects that did not exceed mild severity according to CTCAE criteria [97].
The hook effect observed with PROTAC molecules represents a unique toxicity consideration for this emerging class of UPS-targeted therapies [96]. At high concentrations, PROTACs tend to form binary "PROTAC-POI" and "PROTAC-E3" complexes rather than the productive "POI-PROTAC-E3" ternary complex required for targeted protein degradation. This self-limiting mechanism potentially reduces on-target toxicity but may also diminish therapeutic efficacy at elevated doses [96]. Optimization of PROTAC structures to enhance "neocontacts" between E3 ligases and proteins of interest (POIs) can increase the threshold for triggering the hook effect, providing a strategic approach to maintain efficacy while managing toxicity [96].
Experimental Protocols for Assessing Efficacy and Toxicity
Ubiquitinomics Profiling for Target Identification
Protocol: 4D Label-Free Quantitative Ubiquitination Proteomics
- Sample Preparation: Collect tumor and adjacent normal tissues (minimum 4 pairs). Add liquid nitrogen to grind tissue to powder. Add lysis buffer (1% Triton X-100, 1% protease inhibitor, 50 μm PR-619, 3 μm TSA, 50 mm NAM) for ultrasonic pyrolysis. Centrifuge at 12,000×g for 10 min and collect supernatant. Determine protein concentration using BCA assay [82].
- Trypsin Digestion: Precipitate proteins with TCA at 4°C. Centrifuge at 4,500×g for 5 min, discard supernatant. Wash precipitate with pre-cooled acetone, air dry, and dissolve in 200 mm TEAB buffer. Add trypsin and maintain reaction overnight. Incubate with dithiothreitol at 56°C for 30 min, then add iodoacetamide (IAA) and incubate at room temperature for 15 min in dark [82].
- Mass Spectrometry Analysis: Separate digested peptides using NanoElute UPLC system with flow rate of 450 nl/min. Use gradient mobile phase B (0.1% formic acid and 100% acetonitrile): 6–22% (0–43 min); 22–30% (43–56 min); 30–80% (56–58 min); 80% (58–60 min). Ionize peptides using Capillary Ion Source at 2.0 kV and analyze by Tims-TOF Pro MS. Set secondary MS scanning range to 100–1700, using PASEF acquisition mode [82].
- Database Searching: Use Maxquant 1.6.6.0 to search MS data against Homo sapiens database (20366 sequences) plus common contamination database. Set false discovery rate (FDR) and peptide spectrum matches (PSM) to 1%. Parameters: trypsin/P digestion; maximum 4 missed sites; minimum length 7 amino acids; maximum 5 modifications; mass error tolerance 20 ppm for primary and secondary ions. Set cysteine alkylation carbamidomethyl as fixed modification, and ['acetyl (protein N-term)', 'oxidation (m)', 'glygly (k)'] as variable modifications [82].
CRISPR/Cas9 Target Validation
Protocol: CRISPR Competition Assay for Essentiality Screening
- Guide RNA Design: Design gRNAs to target exons encoding key functional domains of putative drug targets. Include four gRNAs targeting Rosa26 and AAVS1 loci as negative controls, and four gRNAs targeting PCNA and RPA3 as positive controls [98].
- Cell Transduction: Infect cancer cells at low multiplicity of infection (MOI ≈ 0.3) with GFP-expressing gRNA vectors. Include cell lines from multiple cancer types, especially those where targets were previously reported as essential [98].
- Competition Assay: Monitor fraction of GFP+ cells over 5 passages (approximately 15-20 population doublings). Calculate fold depletion as ratio of initial to final GFP+ percentage. Essential genes typically show 10- to 200-fold depletion, while non-essential genes show <2.5-fold depletion [98].
- Validation: Confirm target ablation by western blotting using two different antibodies recognizing distinct protein epitopes. Generate knockout clones using dual-guide approach targeting two different exons to minimize compensatory mechanisms [98].
Toxicity Assessment in Combination Therapy
Protocol: Systematic Toxicity Profiling for Targeted Therapy-Radiotherapy Combinations
- Patient Selection: Enroll patients with histologically confirmed cancer undergoing external beam radiotherapy with concurrent targeted therapy. Document comprehensive demographic data, Karnofsky Performance Status, diagnosis, and prior treatments [97].
- Baseline Assessment: Record entity-specific toxicities present at baseline before treatment initiation. Document target volume size, fraction dose, total dose, radiation technique (VMAT, 3D-RT, SBRT, IMRT), and intent of irradiation [97].
- Toxicity Monitoring: Evaluate toxicity according to CTCAE v5.0 guidelines at first irradiation, final irradiation, and during follow-up visits. Assess 54 different toxicity items across all tumor types, with particular attention to anatomical region-specific toxicities [97].
- Data Collection: Systematically document targeted substances, timing of application, treatment pauses (< or ≥ one week), and concurrent medications. Use customized database tools for standardized data collection and analysis [97].
Visualization of Key Pathways and Workflows
Diagram 1: UPS Mechanisms and Therapeutic Intervention Points. This diagram illustrates the core ubiquitin-proteasome pathway, PROTAC-mediated targeted degradation, and deubiquitination by ubiquitin-specific proteases (USPs), highlighting key intervention points for cancer therapy.
Diagram 2: Toxicity Mechanisms and Management in UPS-Targeted Therapies. This diagram categorizes major toxicity mechanisms and corresponding management strategies for UPS-targeted treatments, highlighting the connection between toxicity sources and mitigation approaches.
The Scientist's Toolkit: Essential Research Reagents
Table 2: Key Research Reagents for UPS-Targeted Therapy Development
| Reagent Category | Specific Examples | Research Application | Key Considerations |
|---|---|---|---|
| Ubiquitinomics Tools | Anti-K-ε-GG antibody beads (PTMScan) | Enrichment of ubiquitinated peptides for MS analysis | Enables identification of 1,000+ ubiquitination sites; requires specialized MS expertise [82] [47] |
| CRISPR Validation Systems | GFP-expressing gRNA vectors, Cas9-expressing cell lines | Essentiality screening via competition assays | Requires multiple gRNAs per target; Western blot validation essential [98] |
| PROTAC Molecules | ARV-110 (AR degrader), MZ1 (BRD4 degrader) | Targeted protein degradation studies | Hook effect monitoring crucial; ternary complex stability assessment [96] |
| USP Inhibitors | Developing compounds targeting USP48, USP22 | DUB inhibition studies | Specificity challenges; compensatory mechanism monitoring required [94] [26] |
| Toxicity Assessment Tools | CTCAE v5.0 guidelines, ASENA database | Standardized toxicity documentation | Enables systematic comparison across studies; essential for combination therapy assessment [97] |
| E3 Ligase Ligands | VHL-1, Phthalimides (CRBN recruiters) | PROTAC development and optimization | Ligand affinity affects degradation efficiency; tissue expression patterns important [93] [96] |
The strategic targeting of the ubiquitin-proteasome system represents a promising frontier in cancer therapeutics, with the potential to address traditionally "undruggable" targets through innovative modalities such as PROTACs and molecular glues [93] [96]. The successful clinical translation of these approaches necessitates robust preclinical validation of target essentiality, comprehensive ubiquitinome profiling to identify tumor-specific vulnerabilities, and systematic toxicity monitoring in clinical trials [82] [98] [47]. Current evidence suggests that combination regimens incorporating UPS-targeted therapies with conventional modalities such as radiotherapy can be administered with acceptable toxicity profiles when appropriate monitoring and management strategies are implemented [97].
Future directions in the field should prioritize the development of predictive biomarkers to guide patient selection, the optimization of tissue-specific delivery systems to minimize off-target effects, and the continued elucidation of ubiquitination patterns that distinguish malignant from normal tissues [95] [47]. Advances in structural biology enabling rational design of PROTACs with enhanced ternary complex stability, along with the development of DUB inhibitors with improved specificity, will further strengthen the therapeutic index of UPS-targeted treatments [93] [94] [96]. Through the integration of sophisticated ubiquitinomics platforms, rigorous genetic validation tools, and systematic clinical assessment frameworks, researchers and clinicians can successfully balance efficacy and safety in the next generation of UPS-targeted cancer therapies.
The ubiquitin-proteasome system (UPS) represents a promising therapeutic frontier for cancer treatment, with efforts focused on developing inhibitors targeting E1 activating, E2 conjugating, and E3 ligating enzymes, as well as deubiquitinases (DUBs) [99]. However, the clinical translation of these ubiquitination-targeting compounds is significantly hampered by poor oral bioavailability, which can lead to inadequate systemic exposure, variable pharmacokinetics, and diminished efficacy [100]. This whitepaper examines the primary bioavailability challenges—including poor solubility, permeability, and first-pass metabolism—within the context of ubiquitination research. It further provides a technical guide detailing experimental strategies for diagnosing absorption limitations and formulating solutions to overcome them, enabling the development of viable orally administered UPS-targeted therapies.
Ubiquitination, a crucial post-translational modification, regulates fundamental cellular processes such as protein degradation, cell signaling, and DNA repair [101]. In cancer, components of the ubiquitin system are frequently dysregulated, making them attractive drug targets [99]. For instance, the E3 ligase SKP2 is often overexpressed in human cancers and is associated with poor prognosis [99]. Similarly, the NEDD8-activating enzyme (NAE) inhibitor MLN4924 has shown promise in clinical trials by disrupting cullin-RING ligase (CRL) function, leading to cell cycle arrest and apoptosis [99].
Targeting these nodes requires drug candidates to achieve sufficient systemic exposure to modulate the intended pathway. Inefficient oral bioavailability can therefore prevent otherwise potent compounds from realizing their therapeutic potential. This challenge is framed within broader research comparing ubiquitination patterns in cancerous versus normal tissues, where the goal is to achieve selective, therapeutic disruption of oncogenic ubiquitination signaling.
Key Bioavailability Challenges for Ubiquitination-Targeting Compounds
The oral bioavailability (F) of a drug is a product of the fraction absorbed (FAbs), the fraction escaping gut metabolism (FG), and the fraction escaping hepatic first-pass extraction (FH) [100]. UPS-targeting compounds often face obstacles in one or more of these areas.
Table 1: Primary Bioavailability Challenges and Their Impact on UPS-Targeting Compounds
| Challenge | Underlying Cause | Exemplary UPS Compound | Consequence |
|---|---|---|---|
| Poor Aqueous Solubility | High molecular weight & lipophilicity [100] | Many E3 ligase inhibitors | Limited dissolution in GI fluids, reducing FAbs |
| Low Permeability | Large molecular size or polarity | Peptidic or macrocyclic inhibitors | Poor passive diffusion through intestinal epithelium |
| First-Pass Metabolism | Susceptibility to cytochrome P450 enzymes and other metabolic pathways [100] | Prototype E1/E2 inhibitors (e.g., PYR-41) [99] | Low FG and FH, requiring higher dosing |
| Efflux Transport | Substrate for P-glycoprotein (P-gp) | Certain structurally complex inhibitors | Reduced effective absorption and potential drug-drug interactions |
The trend in drug discovery toward high molecular weight and lipophilic compounds exacerbates solubility issues, with an estimated 40% of new compounds having water solubility ≤50 μg/mL [100]. Furthermore, the complex molecular structures often required for targeting protein-protein interactions within the UPS inherently challenge drug-like properties.
Experimental Protocols for Diagnosing Bioavailability Limitations
A systematic, iterative profiling approach is essential for identifying the root cause of poor oral bioavailability within a chemical series.
In Vitro Profiling Assays
3.1.1 Solubility Assessment
- Objective: To determine the equilibrium solubility of a compound in aqueous buffers under physiologically relevant conditions (e.g., pH 6.5 in fasted state simulated intestinal fluid (FaSSIF)).
- Protocol:
- Prepare a saturated solution of the test compound in the chosen buffer.
- Agitate the mixture for a defined period (e.g., 24 hours) at 37°C.
- Separate the undissolved solid by filtration or centrifugation.
- Quantify the concentration of the dissolved compound in the supernatant using a validated analytical method, such as UV spectroscopy or high-performance liquid chromatography (HPLC).
- Data Interpretation: Solubility < 100 μg/mL often signals a potential limitation for oral absorption [100].
3.1.2 Permeability Assessment
- Objective: To predict passive transcellular absorption through the intestinal epithelium.
- Protocol (Caco-2 Assay):
- Culture human colon adenocarcinoma cells (Caco-2) on semi-permeable membranes until they form a confluent, differentiated monolayer.
- Add the test compound to the donor compartment (apical side for absorption assessment).
- Incubate for a set time (e.g., 2 hours) and sample from both donor and receiver (basolateral) compartments.
- Calculate the apparent permeability (Papp) using the accumulated concentration in the receiver compartment.
- Data Interpretation: A Papp value below ~1 × 10⁻⁶ cm/s suggests low permeability likely to limit absorption [100].
3.1.3 Metabolic Stability Assessment
- Objective: To evaluate a compound's susceptibility to hepatic metabolism.
- Protocol (Liver Microsomal Incubation):
- Incubate the test compound (e.g., 1 μM) with liver microsomes (human or preclinical species) in the presence of NADPH cofactor at 37°C.
- Remove aliquots at predetermined time points (e.g., 0, 5, 15, 30, 60 minutes).
- Stop the reaction with an organic solvent (e.g., acetonitrile) and quantify the remaining parent compound using LC-MS/MS.
- Calculate the intrinsic clearance (CLint) from the half-life of the parent compound.
- Data Interpretation: High CLint predicts significant first-pass metabolism and low FH.
In Vivo Pharmacokinetic Screening
The initial in vivo PK study is a critical decision point.
- Protocol (Rodent Snapshot PK):
- Dose groups of rats or mice (n=3) intravenously (IV) and orally (PO).
- For the IV dose, use a simple solution formulation (e.g., saline/PEG400).
- For the PO dose, use a solution formulation designed to maximize solubility (e.g., 10% DMSO, 40% PEG400, 50% water).
- Collect serial blood samples post-dose, analyze plasma for compound concentration, and calculate PK parameters: area under the curve (AUC), clearance (CL), volume of distribution (Vd), and oral bioavailability (F) [100].
- Data Interpretation: Bioavailability (F) is calculated as (AUCPO / DosePO) / (AUCIV / DoseIV) × 100%. Comparing IV and PO exposure identifies whether the limitation is absorption (low FAbs) or systemic clearance.
Formulation Strategies to Enhance Bioavailability
When chemical optimization alone is insufficient, formulation strategies can be employed to improve exposure.
Table 2: Formulation Strategies for Discovery-Stage UPS-Targeting Compounds
| Strategy | Mechanism of Action | Example Dosing Vehicle | Best Suited For |
|---|---|---|---|
| Solution Formulations | Pre-dissolves compound, bypassing dissolution step [100] | 10% DMSO, 40% PEG400, 50% Water | Initial PK studies to establish baseline exposure |
| Amorphous Solid Dispersions (ASDs) | Creates a high-energy amorphous form with enhanced solubility | HPMC-AS or PVP-VA in capsule | Compounds with low crystalline solubility |
| Lipid-Based Formulations (LBFs) | Enhances solubilization and promotes lymphatic transport | Labrafil M2125CS, Cremophor EL, Capmul MCM | Highly lipophilic compounds (log P > 5) |
| Nanocrystal Suspensions | Increases surface area for dissolution via particle size reduction | Milled nanocrystals in aqueous stabilizer (e.g., HPC-SL) | Compounds with high crystal lattice energy |
| Prodrug Approaches | Modifies the parent compound to improve properties (e.g., solubility, permeability), then is converted in vivo | Ester, phosphate, or peptide prodrugs | Compounds with specific functional groups amenable to derivation |
For discovery-stage dosing, the use of non-precipitating solution formulations is recommended for initial PK studies to provide the greatest chance of achieving maximum oral bioavailability [100]. As a program advances, more developable formulations like solid dispersions or lipidic systems should be evaluated.
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Research Reagents for UPS and Bioavailability Research
| Reagent / Material | Function / Application | Key Considerations |
|---|---|---|
| Caco-2 Cells (HTB-37) | In vitro model for predicting human intestinal permeability | Requires long culture time (21 days) to differentiate; can also indicate efflux liability. |
| Pooled Liver Microsomes | Evaluation of metabolic stability and intrinsic clearance | Species-specific (human, rat, mouse) available; requires NADPH cofactor for CYP450 activity. |
| MLN4924 (NAE Inhibitor) | Reference compound for validating CRL pathway modulation and assessing in vivo efficacy models [99]. | Well-characterized mechanism; its pharmacokinetic profile can serve as a benchmark. |
| P-Glycoprotein (P-gp) Assay Kits | Determine if a compound is a substrate for efflux transporters. | Use with transfected cell lines (e.g., MDCK-MDR1); impacts permeability and potential DDI. |
| Bio-Relevant Dissolution Media (FaSSIF/FeSSIF) | Simulates gastrointestinal fluids for more predictive solubility and dissolution testing. | More accurately predicts in vivo performance compared to simple aqueous buffers. |
| HPMC-AS (AQOAT) | Polymer commonly used to create amorphous solid dispersions for solubility enhancement. | Available in different grades with varying pH-dependent solubility (e.g., AS-LF, AS-MF, AS-HF). |
Optimizing the oral bioavailability of ubiquitination-targeting compounds is a critical, multi-faceted challenge in translating promising in vitro activity into effective oral therapeutics. Success requires an integrated strategy that combines early diagnostic profiling to identify key liabilities with the rational application of formulation technologies. By systematically diagnosing and addressing the limitations of solubility, permeability, and metabolism, researchers can significantly improve the likelihood of advancing viable candidates that effectively modulate the ubiquitin-proteasome system for cancer therapy.
Translating Ubiquitination Discoveries: Biomarker Validation and Clinical Implementation
Ubiquitination, a critical post-translational modification, orchestrates myriad cellular processes by regulating protein stability, localization, and activity through a sequential enzymatic cascade involving E1 activating, E2 conjugating, and E3 ligase enzymes [8] [16]. The dysregulation of this system constitutes a hallmark of cancer pathogenesis, driving uncontrolled proliferation, metabolic reprogramming, immune evasion, and therapy resistance [10] [16]. Analytical validation of ubiquitination assays is therefore paramount for investigating these mechanisms and developing targeted therapies like PROTACs (Proteolysis Targeting Chimeras) [102].
Technical reproducibility across different experimental platforms presents significant challenges due to the complexity of ubiquitin signaling, chain linkage diversity, and the dynamic nature of this modification [102] [16]. This guide examines current methodologies, their performance metrics, and standardized protocols to ensure reliable, reproducible detection of ubiquitination events in cancer research.
Key Ubiquitination Assay Platforms and Performance Characteristics
Researchers employ multiple platforms to capture ubiquitination events, each with distinct advantages, limitations, and appropriate applications. The selection of an appropriate platform depends on the research question, required throughput, and need for linkage specificity.
Table 1: Comparison of Major Ubiquitination Assay Platforms
| Assay Platform | Key Feature | Throughput | Linkage Specificity | Key Performance Metrics |
|---|---|---|---|---|
| TUBE-Based HTS [102] | Tandem Ubiquitin Binding Entities | High (96-well format) | High (K48, K63, Pan-specific) | Dynamic range: >100-fold; Enables monitoring of endogenous protein ubiquitination |
| Western Blot [103] | Immunodetection of Ub-protein conjugates | Low | Limited (depends on Ab) | Semiquantitative; Requires high-affinity antibodies |
| Mass Spectrometry [102] | Identification of modification sites | Low | High with enrichment | Identifies precise modification sites; Lower throughput |
The emergence of chain-specific TUBEs (Tandem Ubiquitin Binding Entities) with nanomolar affinities for particular polyubiquitin chains represents a significant advancement for high-throughput applications [102]. This platform enables researchers to distinguish between functionally distinct ubiquitination events, such as K48-linked chains targeting proteins for proteasomal degradation versus K63-linked chains involved in signal transduction and protein trafficking [102]. Furthermore, recent discoveries reveal that ubiquitination extends beyond proteins to include drug-like small molecules, expanding the substrate realm and opening avenues for novel therapeutic modalities [104].
Validated Experimental Protocols for Ubiquitination Analysis
Chain-Specific TUBE Assay for High-Throughput Screening
This protocol enables quantitative analysis of linkage-specific ubiquitination events on endogenous proteins in a 96-well format, ideal for evaluating PROTAC efficacy or inflammatory signaling [102].
Materials and Reagents:
- Chain-specific TUBEs (K48-, K63-, or Pan-specific) coated plates
- Cell lysis buffer (e.g., RIPA buffer supplemented with protease inhibitors, N-ethylmaleimide, and PR-619 to preserve polyubiquitination)
- Primary antibody against protein of interest
- HRP-conjugated secondary antibody
- Chemiluminescent detection reagent
Procedure:
- Cell Stimulation and Lysis: Treat cells (e.g., THP-1 human monocytic cells) with experimental conditions (e.g., 200-500 ng/ml L18-MDP for K63 ubiquitination or PROTAC for K48 ubiquitination). Lyse cells using optimized lysis buffer (50 µg total protein per sample recommended) [102].
- Ubiquitin Capture: Transfer cell lysates to TUBE-coated plates and incubate for 2 hours at 4°C with gentle agitation to allow chain-specific polyubiquitin binding.
- Washing: Remove unbound material with three washes using PBS-Tween buffer.
- Target Detection: Incubate with primary antibody specific to your protein of interest (e.g., anti-RIPK2) overnight at 4°C, followed by HRP-conjugated secondary antibody for 1 hour at room temperature.
- Signal Development and Quantification: Add chemiluminescent substrate and measure signal intensity using a plate reader. Include appropriate controls (unstimulated cells, specificity controls using different TUBEs) [102].
Validation Parameters:
- Demonstrate specificity using linkage-specific stimuli (e.g., L18-MDP induces K63 ubiquitination detectable with K63-TUBEs but not K48-TUBEs)
- Establish linear range using protein dilution series
- Determine intra-assay and inter-assay coefficients of variation (<15% recommended)
In Vivo Ubiquitination Assay Protocol
This method detects ubiquitination of specific proteins in living cells, combining immunoprecipitation with western blot analysis [103].
Materials and Reagents:
- Plasmid encoding ubiquitin (wild-type or mutant)
- Plasmid encoding protein of interest
- Transfection reagent (e.g., Lipo8000)
- Proteasome inhibitor (e.g., MG132)
- Lysis buffer (RIPA with N-ethylmaleimide and PR-619)
- Protein A/G beads
- Primary antibodies against target protein and ubiquitin
- Cell Counting Kit-8 (CCK-8) for viability assessment [103]
Procedure:
- Cell Transfection: Co-transfect cells with ubiquitin and target protein plasmids using standard transfection protocols.
- Proteasome Inhibition: Treat cells with 10 µM MG132 for 4-6 hours before harvesting to prevent degradation of ubiquitinated proteins.
- Cell Lysis: Lyse cells in modified RIPA buffer with deubiquitinase inhibitors.
- Immunoprecipitation: Incubate lysates with antibody against target protein overnight at 4°C, then with Protein A/G beads for 2 hours.
- Western Blot Analysis: Resolve immunoprecipitates by SDS-PAGE, transfer to membrane, and probe with anti-ubiquitin antibody.
- Functional Assessment: Perform CCK-8 assay to correlate ubiquitination status with cellular viability or proliferation [103].
Essential Research Reagent Solutions
Table 2: Key Reagents for Ubiquitination Assays
| Reagent Category | Specific Examples | Function & Importance |
|---|---|---|
| Ubiquitin-Binding Reagents [102] | Chain-specific TUBEs (K48, K63, Pan) | High-affinity enrichment of specific ubiquitin chain linkages from complex mixtures |
| Enzyme Inhibitors [102] [103] | MG132 (proteasome inhibitor), N-ethylmaleimide, PR-619 (DUB inhibitors) | Preserve ubiquitination signals by blocking degradation and deubiquitination |
| Activation Compounds [102] | L18-MDP (induces K63 ubiquitination), PROTACs (induce K48 ubiquitination) | Experimental controls for inducing specific ubiquitination pathways |
| Detection Antibodies [103] | Anti-RIPK2, Anti-IGF2BP1, linkage-specific ubiquitin antibodies | Target protein detection and ubiquitination confirmation |
| Cell Viability Assays [103] | Cell Counting Kit-8 (CCK-8) | Correlate ubiquitination status with functional cellular outcomes |
Technical Considerations for Reproducibility Across Platforms
Achieving technical reproducibility requires careful attention to experimental conditions and validation controls. Key considerations include:
- Inhibitor Cocktails: Always include proteasome and deubiquitinase inhibitors in lysis buffers to preserve ubiquitination signatures, as their absence leads to rapid signal loss [102] [103].
- Linkage Specificity Controls: Utilize biological stimuli known to induce specific ubiquitination types (e.g., L18-MDP for K63 chains in inflammatory signaling, PROTACs for K48-mediated degradation) to validate assay specificity [102].
- Dynamic Range Assessment: Establish the linear detection range for each assay using dose-response curves with known stimuli to ensure quantitative accuracy [102].
- Cross-Platform Validation: Confirm critical findings with at least two complementary methods (e.g., TUBE-based HTS with western blot validation) to control for platform-specific artifacts [102] [103].
The expanding substrate repertoire of ubiquitination enzymes, including recently discovered modifications of drug-like small molecules by HUWE1, necessitates careful assay design to distinguish between true ubiquitination events and potential artifacts [104].
Technical reproducibility across ubiquitination assay platforms is achievable through standardized protocols, appropriate control systems, and cross-platform validation. The development of chain-specific affinity reagents like TUBEs has significantly advanced high-throughput screening capabilities for drug discovery applications, particularly for PROTAC development and inflammatory pathway analysis [102]. As research continues to reveal novel aspects of ubiquitination biology, including modification of non-protein substrates [104], robust analytical validation remains fundamental to generating reliable data in cancer research and therapeutic development.
The post-translational modification of proteins by ubiquitination is a critical regulator of nearly all cellular processes, and its dysregulation is a hallmark of cancer. Ubiquitinomics, the large-scale study of ubiquitinated proteins, has identified numerous potential biomarkers and therapeutic targets. However, the translation of these discoveries into clinically applicable tools hinges on rigorous clinical validation within robust, multicenter cohorts. This process confirms that a biomarker reliably predicts a specific clinical outcome, such as patient survival or response to treatment, and demonstrates that its utility is generalizable beyond a single institution. This guide provides a technical framework for establishing the prognostic and predictive value of ubiquitination-based signatures through multidisciplinary approaches, integrating advanced proteomics, bioinformatics, and clinical research methodologies.
Foundational Concepts: Prognostic vs. Predictive Value
In the context of cancer research, it is essential to distinguish between two key types of clinical value:
- Prognostic Value: A biomarker is prognostic if it provides information about the likely course of the disease (e.g., overall survival) in an untreated population or a population receiving standard therapy. It identifies patients with inherently aggressive or indolent disease.
- Predictive Value: A biomarker is predictive if it identifies patients who are more or less likely to benefit from a specific therapeutic intervention.
Multicenter cohort validation is the gold standard for establishing both types of value, ensuring that the biomarker's performance is consistent across different patient populations and clinical settings.
Study Design for Multicenter Validation
Cohort Selection and Ethical Considerations
A well-designed validation study begins with a clear definition of the patient population and study cohorts.
- Case-Control vs. Prospective Cohorts: For initial validation, a case-control design nested within a larger prospective cohort can be efficient. However, fully prospective studies provide the highest level of evidence.
- Inclusion/Exclusion Criteria: Criteria must be standardized across all participating centers. As demonstrated in a COVID-19 prognostic score study, this includes confirmed diagnosis (e.g., by RT-PCR), adult age (≥18 years), and availability of complete clinical and laboratory data for analysis [105].
- Ethical and Legal Compliance: The study must adhere to the Declaration of Helsinki and relevant regulations (e.g., GDPR in the EU). Approval from the Local Ethics Committee of each participating institution is mandatory. A waiver for informed consent is often granted for retrospective analyses of anonymized data [105].
Data Collection and Standardization
- Clinical Data: Collect comprehensive demographic, pathologic, and treatment data. Key variables often include age, gender, tumor stage, grade, and specific treatments like surgery and chemotherapy [106].
- Follow-up Data: Consistent and complete follow-up is crucial for survival analysis. Endpoints must be clearly defined:
- Overall Survival (OS): Time from diagnosis to death from any cause.
- Cancer-Specific Survival (CSS): Time from diagnosis to death specifically from the cancer of interest [106].
- Biospecimen Handling: Standardized protocols for tissue collection, processing, and storage are vital to minimize pre-analytical variability that could affect ubiquitination measurements.
Key Methodologies for Ubiquitination-Based Biomarker Validation
Ubiquitinomics Profiling Technologies
Mass spectrometry (MS)-based proteomics is the cornerstone of ubiquitinome characterization.
- 4D Label-Free Quantitative Ubiquitination Proteomics: This advanced MS technique combines four-dimensional separation (adding ion mobility to traditional 3D LC-MS/MS) with label-free quantification (LFQ) to achieve deep, quantitative analysis of ubiquitinated peptides. The workflow involves:
- Protein Extraction: Tissue samples are ground and lysed in a buffer containing protease inhibitors and deubiquitinase inhibitors (e.g., PR-619) to preserve the ubiquitination state [82].
- Trypsin Digestion: Proteins are digested with trypsin. The "K-ε-GG" remnant motif left on ubiquitinated lysine residues after trypsin digestion serves as a specific signature for enrichment [82] [47].
- Peptide Enrichment: Ubiquitinated peptides are immunoaffinity-enriched using anti-K-ε-GG antibody beads (PTMScan Ubiquitin Remnant Motif Kit) [47].
- LC-MS/MS Analysis: Enriched peptides are separated by ultra-performance liquid chromatography (UPLC) and analyzed by a high-resolution tims-TOF mass spectrometer operating in PASEF (Parallel Accumulation-Serial Fragmentation) mode [82].
- Database Searching: MS/MS data are searched against protein databases (e.g., UniProt Human Proteome) using software like MaxQuant to identify peptides and localize ubiquitination sites with a false discovery rate (FDR) set to <1% [82].
The following diagram illustrates this complex experimental workflow.
Bioinformatic and Statistical Analysis for Prognostication
After identifying differentially ubiquitinated proteins (DUPs), a multi-step analytical process is employed to construct and validate a prognostic signature.
- Differential Analysis: Identify DUPs between tumor and normal tissues using criteria like fold-change (e.g., ≥1.5 or ≤0.67) and statistical significance (P-value < 0.05) [82].
- Functional Enrichment Analysis: Perform Gene Ontology (GO) and Kyoto Encyclopedia of Genes and Genomes (KEGG) analyses to interpret the biological functions and pathways of the identified DUPs [47] [43].
- Prognostic Model Construction:
- Univariate Cox Regression: Initial screening of genes associated with survival.
- LASSO Cox Regression: A feature selection technique that prevents overfitting by penalizing the number of coefficients in the model. It identifies the most valuable prognostic genes from a larger candidate list [43] [57].
- Risk Score Calculation: A prognostic signature is built using the expression levels of the final gene set weighted by their multivariate Cox regression coefficients. Patients are stratified into high-risk and low-risk groups based on the median risk score or an optimal cut-off value [43] [57].
- Model Validation: The model's performance must be validated in both internal (hold-out test set from the original cohort) and external (completely independent cohort from another institution) datasets. Key metrics include:
- Kaplan-Meier Survival Analysis: Visually compares the survival curves of high- and low-risk groups, with statistical significance tested by the log-rank test.
- Time-Dependent ROC Analysis: Assesses the model's predictive accuracy at specific time points (e.g., 1, 3, 5 years). The Area Under the Curve (AUC) quantifies performance.
- Concordance Index (C-index): Measures the model's overall ability to correctly rank patient survival times [106].
Table 1: Exemplary Ubiquitination-Related Prognostic Signatures in Various Cancers
| Cancer Type | Ubiquitination-Related Biomarkers | Validation Cohort(s) | Performance (AUC/C-index) | Key Clinical Implication |
|---|---|---|---|---|
| Cervical Cancer [43] | MMP1, RNF2, TFRC, SPP1, CXCL8 | TCGA-GTEx-CESC (n=317), GSE52903 (n=72) | AUC >0.6 for 1/3/5 years | Patient stratification for personalized therapy |
| Ovarian Cancer [95] | TOP2A, MYLIP | Training and validation sets from TCGA | Significant survival difference (P<0.05) | Insights into survival and development |
| Diffuse Large B-Cell Lymphoma [57] | CDC34, FZR1, OTULIN | GSE10846 (training), GSE181063 (validation) | Consistent risk stratification in both cohorts | Potential therapeutic target and strategy |
| Sigmoid Colon Cancer [47] | 46 overall survival-related DUPs | TCGA (n=100 samples) | Not Specified | Biomarkers for predictive diagnosis and prognosis |
Advanced Validation: Integrating the Tumor Microenvironment and Clinical Utility
Immune Microenvironment and Drug Sensitivity Analysis
A robust validation framework extends beyond pure prognostication to explore biological context and therapeutic implications.
- Immune Infiltration Analysis: Tools like CIBERSORT can quantify the abundance of various immune cell types in the tumor microenvironment from bulk RNA-seq data. Studies have shown that high-risk and low-risk groups based on ubiquitination signatures display significant differences in immune cell infiltration (e.g., memory B cells, M0 macrophages) [43]. This links the ubiquitination state to anti-tumor immunity.
- Drug Sensitivity Prediction: Using R packages like
oncoPredict, researchers can correlate the ubiquitination-based risk score with the half-maximal inhibitory concentration (IC50) of chemotherapeutic and targeted drugs. This can reveal which drugs might be more effective for specific risk groups, adding predictive value to the signature [57].
Development of Clinical Decision Tools
To bridge the gap between a statistical model and clinical application, user-friendly tools can be developed.
- Nomograms: A nomogram is a graphical calculation tool that integrates multiple prognostic variables (including the risk score from a ubiquitination signature) to provide a numerical probability of a clinical event, such as 1- or 3-year survival. The accuracy of the nomogram is assessed with calibration plots [106].
- Independent Prognostic Analysis: Conducting univariate and multivariate Cox analyses that include the new risk score and established clinical factors (e.g., age, TNM stage) demonstrates that the ubiquitination signature provides independent prognostic information beyond current standards [43] [106].
Table 2: Essential Research Reagent Solutions for Ubiquitinomics Validation
| Research Reagent / Kit | Function / Application | Technical Notes |
|---|---|---|
| Anti-K-ε-GG Antibody Beads (PTMScan Kit) | Immunoaffinity enrichment of ubiquitinated peptides from complex protein digests for MS analysis. | Critical for specificity; recognizes the diglycine remnant left on lysine after trypsin digestion [47]. |
| Protease & Deubiquitinase Inhibitors | Preserves the native ubiquitination state of proteins during tissue lysis and protein extraction. | Essential for accuracy. Use of inhibitors like PR-619, TSA, and NAM is required [82]. |
| BCA Protein Assay Kit | Colorimetric quantification of total protein concentration in sample lysates. | Ensures equal protein loading for downstream MS analysis, critical for quantification [82]. |
| LASSO Cox Regression (glmnet R package) | Statistical method for building a parsimonious prognostic model from a high number of candidate genes. | Prevents model overfitting; identifies the most predictive genes [43] [57]. |
| CIBERSORT Algorithm | Deconvolutes bulk tumor RNA-seq data to infer the relative abundance of 22 human immune cell types. | Connects the ubiquitination signature to the tumor immune contexture [43] [57]. |
The clinical validation of ubiquitination patterns is a multifaceted process that moves from discovery in tissue samples to robust, clinically actionable tools. By employing advanced proteomics, rigorous bioinformatics, and validation in well-designed multicenter cohorts, researchers can transform ubiquitinomics data into reliable prognostic and predictive biomarkers. This process is fundamental to advancing the framework of predictive, preventive, and personalized medicine (PPPM; 3P medicine), enabling patient stratification, prognostic assessment, and the identification of novel therapeutic targets for improved cancer care [47]. The integration of these signatures with analyses of the tumor microenvironment and drug sensitivity further paves the way for tailoring therapies to individual patients, ultimately improving clinical outcomes.
Ubiquitination, a fundamental post-translational modification (PTM), plays a pivotal role in regulating protein stability, localization, and activity within eukaryotic cells. This reversible process involves the covalent attachment of ubiquitin—a 76-amino acid regulatory protein—to substrate proteins via a sequential enzymatic cascade comprising E1 (activating), E2 (conjugating), and E3 (ligating) enzymes [12]. The ubiquitin-proteasome system (UPS) subsequently controls the degradation of approximately 80% of intracellular proteins, making it a crucial regulator of cellular homeostasis [107]. The specificity of ubiquitination is primarily determined by E3 ubiquitin ligases, with over 600 encoded in the human genome, while deubiquitinating enzymes (DUBs) counteract this process by removing ubiquitin moieties, adding layers of regulatory complexity [12].
Ubiquitinomics has emerged as a powerful proteomic approach for systematically profiling ubiquitination events on a global scale. By utilizing anti-K-ε-GG antibody beads to enrich for ubiquitin-derived di-glycine remnants on trypsinized peptides, combined with advanced liquid chromatography-tandem mass spectrometry (LC-MS/MS), researchers can now identify and quantify thousands of ubiquitination sites across multiple biological samples [47] [108]. This methodology enables the comprehensive detection of ubiquitination patterns that distinguish pathological states from normal physiological conditions. When integrated with transcriptomic and proteomic data, ubiquitinomics provides unprecedented insights into the molecular mechanisms underlying cancer pathogenesis and reveals potential therapeutic targets for precision oncology.
The dysregulation of ubiquitination pathways is increasingly recognized as a hallmark of cancer, influencing critical processes including tumor metabolism, immune microenvironment modulation, and cancer stem cell maintenance [12]. Tissue-specific ubiquitinome analyses have revealed that different cancer types exhibit distinct ubiquitination signatures, reflecting their unique genetic backgrounds and tissue origins. This comparative review synthesizes current findings from ubiquitinomics studies across various malignancies, with particular emphasis on methodological approaches, tissue-specific patterns, and translational applications in biomarker discovery and targeted therapy development.
Core Concepts and Methodological Framework
The Ubiquitin-Proteasome System Architecture
The ubiquitin-proteasome system represents a sophisticated enzymatic network that governs targeted protein degradation in eukaryotic cells. This system commences with the ATP-dependent activation of ubiquitin by E1 activating enzymes, of which humans possess only two primary types: UBA1 (UBE1) and UBA6 (UBE6) [107] [12]. The activated ubiquitin is subsequently transferred to approximately 50 distinct E2 conjugating enzymes, which then collaborate with over 600 E3 ligases to confer substrate specificity during ubiquitin transfer to target proteins [107] [12]. The E3 ligases are categorized into three major classes: really interesting new gene (RING), homologous to E6-AP carboxyl terminus (HECT), and RING-between-RING (RBR) families, each employing distinct catalytic mechanisms [12].
The ubiquitination process generates diverse topological signatures with functional consequences. Monoubiquitination involves attachment of a single ubiquitin molecule and typically regulates DNA damage repair, autophagy, and chromatin remodeling [12]. Polyubiquitination, characterized by ubiquitin chains attached to substrate lysines, generates structurally and functionally distinct signals based on the linkage type. K48-linked chains primarily target substrates for proteasomal degradation, while K63-linked chains facilitate non-proteolytic processes including signal transduction, DNA repair, and endocytosis [12]. Other linkage types (K6, K11, K27, K29, K33) exhibit specialized functions, with K6 and K33 linkages particularly implicated in DNA damage response pathways [109]. This complex ubiquitin code is dynamically rewritten by approximately 100 deubiquitinating enzymes (DUBs) that remove ubiquitin moieties, thereby reversing ubiquitination signals [110] [12].
Analytical Workflows in Ubiquitinomics
Contemporary ubiquitinomics relies on sophisticated mass spectrometry-based workflows that enable system-wide quantification of ubiquitination events. The foundational methodology incorporates anti-K-ε-GG antibody enrichment, which specifically captures tryptic peptides containing the di-glycine remnant left after ubiquitinated lysine digestion [47] [108]. This enrichment strategy significantly enhances the detection sensitivity for low-abundance ubiquitinated peptides within complex biological samples. Following immunoenrichment, samples are analyzed using high-resolution LC-MS/MS platforms, with label-free quantification representing the predominant approach for comparing ubiquitination levels across experimental conditions [47].
Advanced implementations now incorporate 4D proteomics technology, which adds ion mobility separation to conventional LC-MS/MS, substantially increasing peak capacity and identification rates [108]. For comprehensive assessment of DNA damage-induced ubiquitination, proteasome inhibition (e.g., with MG132) proves essential to prevent the rapid degradation of ubiquitinated substrates, thereby enabling their detection [109]. Nuclear fractionation with strong cation exchange (SCX) chromatography further expands the detectable ubiquitinome by reducing sample complexity [109]. Bioinformatics processing of raw spectral data facilitates ubiquitination site localization, differential abundance analysis, and functional annotation through Gene Ontology (GO), Kyoto Encyclopedia of Genes and Genomes (KEGG) pathway mapping, and protein-protein interaction network construction [47] [108].
Tissue-Specific Ubiquitination Patterns in Human Cancers
Sigmoid Colon Cancer Ubiquitinome
Comprehensive ubiquitinome profiling of sigmoid colorectal cancer has revealed profound alterations in the ubiquitination landscape compared to matched para-carcinoma tissues. A landmark study identified 1,249 ubiquitinated sites across 608 differentially ubiquitinated proteins (DUPs) in human sigmoid colon cancer specimens [47]. Bioinformatics analysis associated these DUPs with 35 statistically significant signaling pathways, with salmonella infection, glycolysis/gluconeogenesis, and ferroptosis representing the most prominently enriched pathways [47]. Gene Ontology analysis further indicated involvement in 98 biological processes, 64 cellular components, 51 molecular functions, and 26 immune system processes, highlighting the multifaceted role of ubiquitination in sigmoid colon cancer pathogenesis [47].
Relationship modeling between DUPs and their corresponding gene expression patterns revealed four distinct regulatory modes: (1) DUP-up with gene expression-up (increased ubiquitination with increased gene expression), (2) DUP-up with gene expression-down, (3) DUP-down with gene expression-up, and (4) DUP-down with gene expression-down [47]. Similarly, comparative analysis between DUPs and differentially expressed proteins (DEPs) demonstrated complex post-translational regulatory networks. Most notably, survival analysis identified 46 overall survival-related DUPs with significant prognostic value in sigmoid colon cancer, several of which also correlated with drug sensitivity profiles, suggesting their potential as predictive biomarkers for treatment response [47].
Chromosome 17-Linked Ubiquitination in Neuroblastoma
Genomic studies in neuroblastoma have identified gain of chromosome 17 as an early genetic abnormality, with the PPM1D gene emerging as a strong candidate oncogene driving tumor progression [111]. Located on chr17q22.3, PPM1D encodes a p53-inducible Ser/Thr phosphatase that is activated through segmental 17q-gain, gene fusion events, or gain-of-function somatic and germline mutations [111]. Multi-omic analysis of 417 neuroblastoma patients across risk groups demonstrated that increased segmental gains of chromosome 17q occur during clonal evolution, relapse, and metastasis, positioning PPM1D as a pivotal regulator of neuroblastoma development and progression [111].
The USP36 deubiquitinating enzyme, also encoded on chromosome 17q25.3, further illustrates the importance of ubiquitination regulation in neuroblastoma and other malignancies [110]. USP36 maintains protein stability by removing K48-linked ubiquitin chains from target proteins, thereby preventing their proteasomal degradation [110]. This DUB exhibits multifaceted functions in tumorigenesis through its interactions with multiple signaling pathways, including Hippo/YAP, PRL1/Snail2, c-Myc/SOD2, and CEP63/YAP1 [110]. USP36 also demonstrates non-canonical functions in promoting nucleolar protein SUMOylation, particularly enhancing the SUMOylation of small nucleolar ribonucleoprotein (snoRNP) components Nop58 and Nhp2L, thereby facilitating ribosome biogenesis and protein translation [110].
Pan-Cancer Ubiquitination Signatures
A systematic pan-cancer analysis of Ubiquitin D (UBD), also known as HLA-F adjacent transcript 10 (FAT10), has revealed its overexpression in 29 cancer types, where it correlates with poor prognosis and higher histological grades [112]. UBD mediates targeted protein degradation through the proteasome pathway and participates in diverse cellular processes, including immune-mediated inflammation, cell cycle control, and DNA damage repair [112]. Genetic alteration analysis indicates that gene amplification represents the most common type of UBD variation, with patients harboring these alterations exhibiting significantly reduced overall survival rates [112].
Epigenetically, 16 cancer types demonstrate reduced UBD promoter methylation, potentially explaining its elevated expression in malignancies [112]. UBD expression significantly correlates with tumor microenvironment features, including immune infiltration patterns, checkpoint molecule expression, microsatellite instability (MSI), tumor mutational burden (TMB), and neoantigen load [112]. Pathway enrichment analyses implicate UBD in neurodegeneration, proteolysis, and apoptosis pathways, highlighting its broad functional repertoire beyond cancer-specific roles. These pan-cancer findings establish UBD as a promising prognostic biomarker and potential predictor of immunotherapy sensitivity across multiple cancer types [112].
Table 1: Tissue-Specific Ubiquitination Patterns in Human Cancers
| Cancer Type | Key Ubiquitination Findings | Signaling Pathways Affected | Clinical Correlations |
|---|---|---|---|
| Sigmoid Colon Cancer | 1,249 ubiquitinated sites across 608 DUPs [47] | Salmonella infection, glycolysis/gluconeogenesis, ferroptosis [47] | 46 overall survival-related DUPs; drug sensitivity associations [47] |
| Neuroblastoma | Chromosome 17q gain affecting PPM1D and USP36 [110] [111] | p53 pathway, Hippo/YAP, ribosome biogenesis [110] [111] | Poor prognosis, metastasis, and relapse [111] |
| Multiple Cancers (Pan-Cancer) | UBD overexpression in 29 cancer types [112] | NF-κB, Wnt, SMAD2 signaling [112] | Poor survival, higher histological grade, immune microenvironment remodeling [112] |
Experimental Protocols for Ubiquitinome Analysis
Sample Preparation and Quality Control
Robust ubiquitinome analysis begins with meticulous sample preparation and stringent quality control measures. For tissue samples, a minimum of 50-100 mg of snap-frozen material is recommended, while cell-based studies typically require approximately 2×10^7 cells to ensure sufficient protein yield for comprehensive analysis [108]. Protein extraction should be performed under denaturing conditions using buffers containing protease inhibitors and DUB inhibitors to preserve endogenous ubiquitination states. Following extraction, protein quantification via BCA or similar assays ensures equal loading across samples, with quality assessment typically performed by SDS-PAGE and silver staining to visualize protein integrity and concentration [108].
Trypsin digestion represents a critical step in sample preparation, generating peptides with C-terminal di-glycine remnants on previously ubiquitinated lysines. To maximize digestion efficiency while minimizing artifacts, proteins are first reduced with dithiothreitol (DTT) or tris(2-carboxyethyl)phosphine (TCEP), alkylated with iodoacetamide, and then digested with sequencing-grade trypsin at an enzyme-to-substrate ratio of 1:50 for 12-16 hours at 37°C [47] [108]. Digestion efficiency should be monitored using quality control standards, with peptide yield quantified before proceeding to enrichment steps. For clinical sample analyses, a minimum of 3-6 biological replicates per condition is recommended to ensure statistical robustness, with increased replicates (6-10) advised for heterogeneous human tissues [108].
Ubiquitinated Peptide Enrichment and LC-MS/MS Analysis
The enrichment of ubiquitinated peptides employs anti-K-ε-GG antibody beads (commercially available as PTMScan Ubiquitin Remnant Motif K-ε-GG kits) to specifically isolate peptides containing the di-glycine signature [47] [108]. Approximately 1-2 mg of tryptic peptides are typically incubated with antibody-conjugated beads for 2-4 hours at 4°C with gentle agitation. Following incubation, beads are extensively washed with ice-cold immunoaffinity purification buffer to remove non-specifically bound peptides, and ubiquitinated peptides are eluted using 0.15% trifluoroacetic acid [47]. Enrichment efficiency can be monitored by comparing pre- and post-enrichment samples using western blotting with anti-K-ε-GG antibodies or by analyzing a small fraction via LC-MS/MS.
Enriched peptides are separated using nanoflow liquid chromatography systems with C18 reverse-phase columns and analyzed with high-resolution tandem mass spectrometers (e.g., Q-Exactive, Orbitrap Fusion series) operated in data-dependent acquisition mode [47] [108]. The 4D proteomics approach incorporates ion mobility separation, which adds an additional dimension of separation that significantly enhances signal-to-noise ratio and increases ubiquitination site identifications [108]. Mass spectrometry data are acquired with dynamic exclusion enabled (typically 30 seconds) to maximize proteome coverage, with MS1 spectra collected at high resolution (70,000-120,000) and MS2 spectra at lower resolution (17,500-35,000) for optimal balancing of identification and quantification [47].
Data Processing and Bioinformatics Analysis
Raw MS data processing involves database searching against appropriate proteome databases (e.g., UniProt Human Reference Proteome) using algorithms such as MaxQuant, Proteome Discoverer, or FragPipe, with the di-glycine remnant on lysine (+114.0429 Da) specified as a variable modification [47]. False discovery rates (FDR) should be controlled at ≤1% at both peptide and protein levels using target-decoy approaches. Ubiquitination site localization is determined using scoring algorithms such as PTM-score or Ascore, with sites achieving localization scores ≥13 (indicating >95% confidence) typically retained for subsequent analysis [47].
Differential ubiquitination analysis employs label-free quantification algorithms (e.g., MaxLFQ, IonQuant) that normalize peptide intensities across samples based on robust linear regression models [47]. Statistical significance is determined using moderated t-tests or ANOVA, with multiple testing correction via Benjamini-Hochberg procedure. Bioinformatic functional analysis includes Gene Ontology (GO) enrichment for biological processes, cellular components, and molecular functions; KEGG pathway mapping; protein-protein interaction network construction using STRING database; and subcellular localization prediction [47] [108]. Integration with transcriptomic and proteomic datasets enables the identification of relationship models between ubiquitination, gene expression, and protein abundance, providing systems-level insights into ubiquitination-mediated regulatory networks [47].
Table 2: Key Research Reagents and Resources for Ubiquitinomics Studies
| Reagent/Resource | Function | Examples/Specifications |
|---|---|---|
| Anti-K-ε-GG Antibody | Immunoaffinity enrichment of ubiquitinated peptides | PTMScan Ubiquitin Remnant Motif Kit; monoclonal antibody specific for di-glycine remnant [47] [108] |
| Proteasome Inhibitors | Stabilize ubiquitinated proteins by blocking degradation | MG132, bortezomib, carfilzomib; used at 10-20 μM for 4-6 hours pre-treatment [109] |
| LC-MS/MS Platform | Identification and quantification of ubiquitinated peptides | High-resolution mass spectrometers (Orbitrap series) coupled to nano-UPLC systems; 4D configurations with ion mobility enhance coverage [108] |
| Database Search Software | Ubiquitination site identification from MS data | MaxQuant, FragPipe, Proteome Discoverer; with di-glycine (+114.0429 Da) as variable modification [47] |
| Bioinformatics Tools | Functional annotation and pathway analysis | Gene Ontology, KEGG, STRING, DAVID; integrated platforms like GEPIA2, cBioPortal for cancer data [47] [112] |
| DUB Inhibitors | Investigate ubiquitination dynamics | PR-619 (pan-DUB inhibitor); specific inhibitors for USP7, USP14 under development [12] |
| Ubiquitin Variants | Study chain linkage-specific functions | K48-only, K63-only ubiquitin mutants; ubiquitin binding domain probes [109] [12] |
Comparative ubiquitinomics across cancer types has revealed extensive tissue-specific patterning in ubiquitination landscapes, reflecting the unique pathophysiological contexts of different malignancies. The integration of ubiquitinome data with genomic, transcriptomic, and proteomic datasets provides unprecedented insights into the molecular mechanisms driving oncogenesis and enables the identification of novel therapeutic targets. As ubiquitinomics methodologies continue to advance, with improvements in enrichment strategies, mass spectrometry sensitivity, and bioinformatic tools, the resolution of ubiquitination mapping will correspondingly increase, potentially enabling single-cell ubiquitinome analyses in the future.
The clinical translation of ubiquitinomics findings holds particular promise for predictive, preventive, and personalized medicine (PPPM) approaches in oncology. The identification of survival-associated DUPs in sigmoid colon cancer illustrates the potential prognostic value of ubiquitination signatures [47]. Similarly, the association between UBD expression and immunotherapy response across multiple cancer types suggests that ubiquitinome profiling could inform treatment selection [112]. As targeted therapies against specific E3 ligases, DUBs, and ubiquitination pathway components continue to develop, ubiquitinomics will play an increasingly important role in patient stratification and therapeutic monitoring, ultimately fulfilling the promise of precision oncology through comprehensive characterization of the ubiquitination landscape in cancer.
The ubiquitin-proteasome system (UPS) represents a crucial regulatory mechanism in cellular homeostasis, governing the degradation of approximately 80% of intracellular proteins and influencing virtually all cellular processes [47]. Ubiquitination, a post-translational modification involving the covalent attachment of ubiquitin to target proteins, has emerged as a pivotal process in carcinogenesis, with distinct ubiquitination patterns differentiating malignant from normal tissues across various cancer types [82] [47] [113]. The bench-to-bedside translation of these mechanistic insights offers unprecedented opportunities for developing novel diagnostic, prognostic, and therapeutic strategies in oncology. This whitepaper provides an in-depth technical examination of the ubiquitination landscape in cancer, quantitative profiling methodologies, and the translational pathway for converting these discoveries into clinical applications with meaningful endpoints.
Quantitative Ubiquitinomics: Revealing Cancer-Specific Patterns
Advanced mass spectrometry-based proteomic approaches have enabled comprehensive mapping of ubiquitination patterns across cancer types, revealing disease-specific signatures with potential clinical utility.
Table 1: Ubiquitination Patterns Across Cancer Types
| Cancer Type | Ubiquitination Sites Identified | Differentially Ubiquitinated Proteins | Key Findings | Reference |
|---|---|---|---|---|
| Adenoid Cystic Carcinoma (Oral) | 4,152 sites on 1,993 proteins | 859 proteins with quantitative changes | 555 up-regulated and 112 down-regulated ubiquitination sites in tumor tissues | [82] |
| Sigmoid Colon Cancer | 1,249 ubiquitinated sites | 608 differentially ubiquitinated proteins | Identification of 35 significantly altered signaling pathways including glycolysis and ferroptosis | [47] |
| Lung Squamous Cell Carcinoma | 654 ubiquitination sites | 400 differentially ubiquitinated proteins | Decreased ubiquitination of vimentin and increased MRP1 associated with poor prognosis | [113] |
| Lung Adenocarcinoma | - | 4-gene ubiquitination signature (DTL, UBE2S, CISH, STC1) | Risk score predictive of prognosis and therapy response | [56] |
The heterogeneity of ubiquitination patterns across tissues presents both challenges and opportunities for targeted therapeutic interventions. Systematic analyses reveal that ubiquitination regulators (UBRs) demonstrate tissue-specific expression patterns, with testicular tissue showing the most distinct profile [50]. In pan-cancer analyses, more than 90% of UBRs affect patient survival, with widespread genetic alterations and expression perturbations observed across cancer types [50].
Methodological Framework: Ubiquitinomics Experimental Protocols
Sample Preparation and Protein Extraction
The technical workflow for ubiquitinomics requires specialized protocols to preserve and identify ubiquitination events:
Tissue Collection and Preservation: Fresh tumor and adjacent normal tissues should be immediately snap-frozen in liquid nitrogen following surgical resection. Storage at -80°C preserves ubiquitination patterns until analysis [113]. Studies typically utilize 100-150mg of tissue per sample, with pooling strategies sometimes employed to overcome biological variability [113].
Protein Extraction and Denaturation: Tissue samples are homogenized in urea lysis buffer (7M urea, 2M thiourea) supplemented with protease inhibitors (e.g., 1mM PMSF), deubiquitinase inhibitors (e.g., 50μM PR-619), and other preservatives to maintain ubiquitination status [82]. Sonication (80W, 10s intervals, 10 cycles) followed by centrifugation (15,000×g, 20min, 4°C) clarifies lysates for downstream processing [113].
Protein Concentration Determination: Bradford assay or BCA protein assay quantifies total protein concentration to ensure equal loading across samples [82] [113].
Trypsin Digestion and Peptide Preparation
Reduction and Alkylation: Proteins are treated with dithiothreitol (DTT, 10mM final concentration, 37°C, 1.5h) to reduce disulfide bonds, followed by alkylation with iodoacetamide (50mM final concentration, room temperature, 30min in darkness) [113].
Trypsin Digestion: Sequencing-grade trypsin is added at a 1:50 (wt:wt) enzyme-to-protein ratio and incubation proceeds at 37°C for 15-18 hours [113]. The reaction is stopped by acidification with trifluoroacetic acid (TFA, 0.1% final concentration, pH≤3) [113].
Peptide Desalting: Tryptic peptides are desalted using C18 cartridges (e.g., Empore SPE Cartridges C18) and lyophilized for enrichment procedures [113].
Ubiquitinated Peptide Enrichment
Immunoaffinity Enrichment: Ubiquitinated peptides are enriched using anti-K-ε-GG antibody beads (PTMScan Ubiquitin Remnant Motif Kit) that specifically recognize the diglycine remnant left on ubiquitinated lysines after trypsin digestion [47] [113]. This critical step enriches low-abundance ubiquitinated peptides from complex biological samples.
Enrichment Validation: Quality control measures including western blot analysis with anti-ubiquitin antibodies verify enrichment efficiency before mass spectrometry analysis.
Mass Spectrometry Analysis and Data Processing
Liquid Chromatography Separation: NanoElute ultra performance liquid chromatography systems separate peptides using gradient elution (typically 6-30% acetonitrile over 43-56 minutes) at flow rates of 450nl/min [82].
Mass Spectrometry Parameters:
- Ionization: Capillary Ion Source (2.0kV)
- Analysis: Tims-TOF Pro MS with PASEF acquisition mode
- Scan ranges: 100-1700 m/z for secondary MS
- Dynamic exclusion: 30 seconds [82]
Database Searching and Quantification:
- Software: MaxQuant (version 1.6.6.0)
- Database: UniProt Homo sapiens reference proteome
- Search parameters: Trypsin/P digestion with up to 4 missed cleavages, oxidation (M) and acetyl (protein N-term) as variable modifications, carbamidomethyl (C) as fixed modification
- False discovery rate (FDR): Set to 1% at peptide and protein levels [82]
- Quantitative method: Label-free quantification (LFQ) based on peptide intensity [82]
The Scientist's Toolkit: Essential Research Reagents and Platforms
Table 2: Key Research Reagents and Platforms for Ubiquitinomics
| Category | Specific Reagents/Platforms | Function and Application | Technical Notes |
|---|---|---|---|
| Enrichment Reagents | Anti-K-ε-GG antibody beads (PTMScan) | Immunoaffinity enrichment of ubiquitinated peptides from complex digests | Critical for detecting low-abundance ubiquitination events; recognizes diglycine remnant on lysines |
| Mass Spectrometry Platforms | Tims-TOF Pro MS with NanoElute UPLC | High-sensitivity identification and quantification of ubiquitinated peptides | PASEF mode enhances detection of low-abundance peptides; 4D proteomics improves quantification |
| Proteomic Analysis Software | MaxQuant | Database searching, quantification, and FDR control | Integrated workflow for LFQ analysis; supports ubiquitination-specific modifications |
| Bioinformatics Tools | STRING, clusterProfiler, Cytoscape | Pathway analysis, PPI network construction, functional enrichment | Identifies ubiquitination-altered pathways and networks in cancer |
| Validation Reagents | siRNA/shRNA libraries, specific antibodies | Functional validation of ubiquitination targets | Essential for confirming biological relevance of ubiquitinomics findings |
Therapeutic Targeting of the Ubiquitin-Proteasome System
Molecular Pathways and Network Alterations
Ubiquitination regulates multiple cancer-relevant processes through specific pathway modulations:
Metabolic Reprogramming: Ubiquitination controls key lipid metabolism enzymes including ACLY, FASN, and HMGCR, influencing cancer cell proliferation and survival [35]. For instance, the E3 ligase NEDD4 regulates ACLY stability in lung cancer, connecting ubiquitination to metabolic rewiring [35].
Immune Response Modulation: Ubiquitination regulates immune signaling pathways, with linear ubiquitination preventing inflammation and regulating immune signaling [113]. Ubiquitination patterns influence PD-1/PD-L1 expression and tumor microenvironment composition [56].
DNA Repair and Cell Cycle Control: Multiple E3 ligases and deubiquitinating enzymes regulate DNA damage response pathways, with implications for genomic stability and therapy response [114].
Clinically Targetable Ubiquitination Components
Several components of the ubiquitination machinery have emerged as promising therapeutic targets:
Proteasome Inhibitors: Bortezomib and carfilzomib (FDA-approved for multiple myeloma) demonstrate the clinical viability of targeting the UPS [113].
Deubiquitinase Inhibitors: USP22 inhibition with repurposed compounds like ergotamine shows promise in preclinical models, with molecular dynamics simulations confirming stable binding interactions [114]. Small molecule inhibitors targeting USP1 (SIM0501) have received FDA clinical approval for trials in advanced solid tumors [35].
E3 Ligase Modulators: The E3 ligase-targeting drug LCL161 (an IAP inhibitor) induces TNF-dependent apoptosis in multiple myeloma and enhances anti-tumor immune responses [35].
Translational Roadmap: From Discovery to Clinical Applications
Biomarker Development and Validation
Ubiquitination signatures offer substantial potential as diagnostic, prognostic, and predictive biomarkers:
Diagnostic Applications: Specific ubiquitination patterns differentiate tumor from normal tissues across multiple cancer types, with potential for early detection [82] [47] [113].
Prognostic Stratification: Ubiquitination-based risk scores (e.g., the 4-gene URRS signature in lung adenocarcinoma) effectively stratify patients by survival probability and treatment response [56].
Therapy Response Prediction: Ubiquitination status of specific proteins predicts response to chemotherapy, targeted therapies, and immunotherapies [56] [113].
Clinical Trial Endpoints and Validation Strategies
The transition from mechanistic insights to clinical validation requires carefully selected endpoints:
Phase I Trials: Primary endpoints focus on safety and tolerability of ubiquitination-targeting agents, with pharmacokinetic and target engagement biomarkers as secondary endpoints.
Phase II Trials: Incorporate biomarker-stratified populations, using progression-free survival and overall response rate as primary endpoints, with ubiquitination status as predictive biomarkers.
Phase III Trials: Overall survival as the gold standard endpoint, with comprehensive ubiquitinomic profiling to identify responder populations and resistance mechanisms.
The translation of ubiquitination research from mechanistic insights to clinical applications represents a promising frontier in oncology. Quantitative ubiquitinomics has revealed cancer-specific patterns with diagnostic, prognostic, and therapeutic implications. However, navigating the "valley of death" between preclinical discovery and clinical application requires robust validation of ubiquitination-based biomarkers and targeted therapies. As our understanding of the ubiquitin code in cancer deepens, the integration of ubiquitinomics into clinical trial design promises to advance personalized cancer medicine, enabling more precise patient stratification and targeting of the ubiquitin-proteasome system for therapeutic benefit. The continued refinement of mass spectrometry methodologies, computational analysis pipelines, and functional validation approaches will accelerate the bench-to-bedside translation of ubiquitination research in the coming years.
The journey of ubiquitination-based biomarkers from research discoveries to clinically approved tools is a complex process requiring rigorous validation and strategic regulatory navigation. This whitepaper provides a comprehensive technical guide to the regulatory pathway for ubiquitination-based biomarker adoption, focusing specifically on cancer applications. We examine the entire pipeline from discovery through clinical implementation, addressing analytical validation, clinical qualification, and regulatory submission requirements. By integrating current research evidence and established regulatory frameworks, this document serves as an essential resource for researchers, scientists, and drug development professionals working to translate ubiquitination discoveries into clinically impactful diagnostic and prognostic tools.
Ubiquitination represents a critical post-translational modification process that governs protein stability, localization, and signaling networks essential for cellular homeostasis. The ubiquitin-proteasome system (UPS) comprises a sophisticated enzymatic cascade involving E1 activating enzymes, E2 conjugating enzymes, and E3 ligases, counterbalanced by deubiquitinating enzymes (DUBs) that remove ubiquitin modifications [115]. This system regulates approximately 80-90% of intracellular proteolysis and has emerged as a pivotal regulatory mechanism in carcinogenesis [10]. The dysregulation of ubiquitination pathways is increasingly recognized as a hallmark of cancer pathogenesis, driving tumor progression through multiple mechanisms including oncoprotein stabilization, tumor suppressor degradation, and altered immune responses.
Recent pan-cancer analyses have revealed that ubiquitination pathway components show widespread dysregulation across multiple cancer types. Comprehensive studies integrating data from 4,709 patients across 26 cohorts and five solid tumor types demonstrated that ubiquitination-based molecular signatures can effectively stratify patients into distinct prognostic categories [10]. The development of ubiquitination-related prognostic signatures (URPS) has shown considerable promise for predicting survival outcomes and therapeutic responses, particularly in the context of immunotherapy. For instance, the OTUB1-TRIM28 ubiquitination axis has been identified as a key modulator of MYC pathway activity and immunotherapy resistance, highlighting the clinical potential of targeting ubiquitination pathways [10].
The growing recognition of ubiquitination's role in cancer biology has accelerated the discovery of ubiquitination-based biomarkers, yet their translation into clinical practice remains challenging. This whitepaper addresses the critical regulatory considerations necessary to bridge this translation gap and facilitate the clinical adoption of ubiquitination-based biomarkers in oncology.
Ubiquitination Biomarker Discovery and Technical Validation
Discovery Platforms and Workflows
The discovery of ubiquitination-based biomarkers relies on sophisticated technological platforms capable of detecting and quantifying ubiquitination events in complex biological samples. Mass spectrometry (MS) has emerged as the cornerstone technology for ubiquitination biomarker discovery due to its high sensitivity, specificity, and ability to perform unbiased profiling [116]. MS-based platforms enable comprehensive analysis of ubiquitinated proteins, offering several critical advantages over conventional antibody-based assays, including label-free quantification, multiplexing capabilities, and versatility across diverse sample types.
A standardized workflow for ubiquitination biomarker discovery encompasses multiple critical phases. The process begins with rigorous sample preparation and enrichment, where techniques such as depletion of high-abundance proteins, enrichment for ubiquitination modifications, and fractionation using liquid chromatography are employed to maximize signal-to-noise ratio [116]. The discovery phase utilizes untargeted or "shotgun" mass spectrometry, typically employing Liquid Chromatography-Tandem Mass Spectrometry (LC-MS/MS) to identify differentially expressed ubiquitinated proteins between patient subgroups. Subsequent bioinformatics and statistical analysis involve data normalization, batch effect correction, differential expression analysis, and pathway enrichment analysis to prioritize candidate biomarkers with diagnostic, prognostic, or therapeutic significance.
Table 1: Key Mass Spectrometry Platforms for Ubiquitination Biomarker Discovery
| Platform Type | Key Applications | Advantages | Limitations |
|---|---|---|---|
| LC-MS/MS (Untargeted) | Discovery-phase profiling, identification of novel ubiquitination signatures | Unbiased approach, comprehensive coverage, no prior knowledge of targets required | Lower throughput, requires validation |
| SRM/PRM (Targeted) | Validation of candidate biomarkers, absolute quantification | High precision and reproducibility, excellent for low-abundance targets | Requires prior knowledge of targets |
| TMT/iTRAQ | Multiplexed relative quantification across samples | Enables comparison of multiple conditions simultaneously, reduces technical variability | Ratio compression, more complex data analysis |
| Immunoaffinity-MS | Analysis of specific ubiquitin chain linkages | High specificity for ubiquitination events, identifies chain topology | Limited to known ubiquitin linkages |
Analytical Validation Requirements
The transition from biomarker discovery to clinical application requires rigorous analytical validation to ensure reliability, reproducibility, and accuracy. Analytical validation establishes that the biomarker assay consistently measures the intended ubiquitination target with acceptable performance characteristics. Key parameters for analytical validation include accuracy, precision, sensitivity, specificity, and stability under defined storage conditions.
For ubiquitination-based biomarkers, analytical validation presents unique challenges due to the labile nature of ubiquitination modifications, the diversity of ubiquitin chain linkages, and the potential for rapid deubiquitination. Assays must demonstrate robust performance across relevant sample matrices, including formalin-fixed paraffin-embedded (FFPE) tissues, frozen tissues, plasma, and other bodily fluids. The dynamic range of quantification should encompass clinically relevant concentrations, with established lower limits of detection (LLOD) and lower limits of quantification (LLOQ) appropriate for intended use.
Recent advances in targeted MS techniques, including Selected Reaction Monitoring (SRM) and Parallel Reaction Monitoring (PRM), have enabled the development of highly precise assays for quantifying candidate ubiquitination biomarkers in large patient cohorts [116]. These assays increasingly incorporate stable isotope-labeled internal standards for absolute quantification and assay standardization, essential for meeting regulatory requirements. Furthermore, the development of multiplexed assays measuring multiple ubiquitination events simultaneously requires demonstration of minimal cross-reactivity and interference between analytes.
Regulatory Framework and Qualification Pathways
Regulatory Classification of Biomarker Tests
Understanding regulatory classification is fundamental to navigating the approval pathway for ubiquitination-based biomarkers. In the United States, biomarkers may be regulated as either Laboratory Developed Tests (LDTs) or in vitro diagnostics (IVDs), with distinct regulatory requirements for each category. The FDA oversees IVDs through premarket approval (PMA) or 510(k) pathways, while LDTs historically have been regulated under CLIA certification, though regulatory oversight is evolving toward increased FDA involvement.
Ubiquitination-based biomarkers typically fall under the classification of "proteomic tests" or "multivariate index assays" depending on their complexity and intended use. The regulatory strategy should be aligned with the proposed claims for the biomarker, which may include diagnostic, prognostic, predictive, or pharmacodynamic applications. For biomarkers intended as companion diagnostics to guide therapeutic decisions, simultaneous development with the corresponding therapeutic agent is recommended, with clinical validity demonstrated in the context of the specific drug-biomarker relationship.
The intended use statement fundamentally drives regulatory classification and requirements. For example, a ubiquitination-based biomarker intended for risk stratification in early-stage cancer would require different evidence than one intended for monitoring treatment response. Clear articulation of the clinical context of use (COU) is essential for designing appropriate validation studies and engaging with regulatory agencies through pre-submission meetings.
Evidence Requirements for Clinical Validity
Clinical validity establishes that the biomarker accurately identifies or predicts the clinical condition or outcome of interest. For ubiquitination-based biomarkers, demonstrating clinical validity requires well-designed studies establishing analytical and clinical performance in the intended population and setting. Key evidence includes diagnostic accuracy measures (sensitivity, specificity, positive and negative predictive values), prognostic value (association with clinical outcomes), or predictive value (ability to identify responders to specific therapies).
Recent studies demonstrate approaches for establishing clinical validity of ubiquitination-based biomarkers. In hepatocellular carcinoma, ubiquitination-related molecules such as NEDD4 and USP14 have been validated as prognostic biomarkers, with high expression correlating with advanced disease stage and reduced overall survival [40]. Similarly, in diffuse large B-cell lymphoma, a ubiquitination-based prognostic signature comprising CDC34, FZR1, and OTULIN effectively stratified patients into distinct risk categories with significant survival differences [57].
Table 2: Evidence Framework for Ubiquitination Biomarker Validation
| Validation Type | Key Parameters | Acceptance Criteria | Study Design Considerations |
|---|---|---|---|
| Analytical Validation | Accuracy, precision, sensitivity, specificity, reproducibility | Inter-assay CV <15%, intra-assay CV <10%, LLOQ established | Use of standardized reference materials, multiple sites/lots |
| Clinical Validity | Sensitivity, specificity, PPV, NPV, HR for outcomes | CI for estimates, prespecified statistical plan, multiplicity adjustment | Prospective-retrospective or fully prospective designs |
| Clinical Utility | Impact on clinical decisions, patient outcomes, cost-effectiveness | Demonstrated improvement in net health outcome | Randomized controlled trials preferred |
| Biological Validity | Mechanistic link to disease biology, pathway relevance | Consistency with known biology, experimental evidence | Integration with preclinical models, functional studies |
Regulatory agencies increasingly emphasize the importance of establishing clinical utility—demonstrating that using the biomarker leads to improved patient outcomes or provides useful information for clinical decision-making. For ubiquitination-based biomarkers, this may involve showing that biomarker-directed therapy improves survival, quality of life, or other clinically meaningful endpoints compared to standard approaches.
Technical and Methodological Considerations
Standardization of Pre-Analytical Variables
Pre-analytical variables significantly impact the measurement of ubiquitination biomarkers and must be carefully controlled and standardized throughout the biomarker development process. Ubiquitination is a dynamic and reversible modification that can be influenced by numerous factors including sample collection time, processing delays, storage conditions, and fixation methods. Establishing standardized protocols for sample handling is essential for ensuring reproducible and reliable biomarker measurements.
For tissue-based ubiquitination biomarkers, key pre-analytical considerations include ischemia time (time between devascularization and preservation), fixation methods (type of fixative, duration), and storage conditions. Plasma or serum biomarkers require standardization of blood collection tubes, centrifugation protocols, processing times, and freeze-thaw cycles. The labile nature of ubiquitination modifications necessitates particular attention to protease inhibition and stabilization of ubiquitin conjugates during sample processing.
Documentation of pre-analytical variables should be comprehensive and consistent across all study sites in multi-center trials. The development of standard operating procedures (SOPs) for sample collection, processing, and storage is critical for minimizing technical variability and ensuring data quality. Where possible, the stability of ubiquitination biomarkers under various storage conditions should be formally established to define acceptable handling parameters.
The Scientist's Toolkit: Essential Research Reagents
The development and validation of ubiquitination-based biomarkers rely on specialized research reagents and tools. This toolkit enables precise detection, quantification, and functional characterization of ubiquitination events in biological samples.
Table 3: Essential Research Reagents for Ubiquitination Biomarker Development
| Reagent Category | Specific Examples | Primary Functions | Technical Considerations |
|---|---|---|---|
| Ubiquitin Enrichment Reagents | Ubiquitin remnant motif antibodies, TUBE reagents (Tandem Ubiquitin Binding Entities) | Selective enrichment of ubiquitinated peptides/proteins | Specificity for ubiquitin chain linkages, compatibility with downstream applications |
| Activation & Conjugation Enzymes | E1, E2, E3 enzyme libraries | In vitro ubiquitination assays, mechanism of action studies | Enzyme activity validation, substrate specificity |
| Deubiquitinase Inhibitors | PR-619, P22077, WP1130 | Stabilization of ubiquitination signatures in samples | Selectivity profiles, cellular toxicity at working concentrations |
| Mass Spectrometry Standards | Stable isotope-labeled ubiquitin, AQUA peptides | Absolute quantification, assay standardization | Incorporation efficiency, purity verification |
| Validation Antibodies | Mono- and polyubiquitin antibodies, linkage-specific antibodies | Orthogonal validation, immunohistochemistry, Western blot | Specificity validation, application optimization |
Bioinformatics and Computational Pipelines
The analysis of ubiquitination biomarker data requires sophisticated bioinformatics pipelines to process complex datasets and extract biologically meaningful insights. Key computational approaches include database search algorithms for ubiquitination site identification, quantitative analysis tools for differential expression, and pathway analysis methods for biological interpretation.
Specialized databases and resources have been developed specifically for ubiquitination research, including the Ubiquitin and Ubiquitin-like Conjugation Database (UUCD), Ubiquitin Site Identification Database (UbSiDa), and databases of ubiquitination sites mined from mass spectrometry datasets. These resources facilitate the annotation and functional characterization of ubiquitination biomarkers, enabling researchers to place their findings in the context of existing knowledge.
Data integration approaches that combine ubiquitination profiling with genomic, transcriptomic, and proteomic data provide a more comprehensive understanding of biomarker function and clinical significance. Multi-omics integration has been successfully applied in pan-cancer analyses of ubiquitination networks, revealing conserved pathways and prognostic signatures across diverse cancer types [10]. The development of robust bioinformatics pipelines is essential for meeting regulatory standards for data transparency, reproducibility, and analytical validation.
Case Studies and Clinical Applications
Oncology Applications: From Discovery to Implementation
Ubiquitination-based biomarkers have shown particular promise in oncology, where they contribute to improved diagnosis, prognosis, and treatment selection. Several case examples illustrate the successful translation of ubiquitination biomarkers along the development pathway.
In hepatocellular carcinoma (HCC), comprehensive analysis of ubiquitination-related molecules has identified several biomarkers with clinical utility. NEDD4, an E3 ubiquitin ligase, demonstrates significant overexpression in HCC tissues compared to adjacent non-tumor tissues (2.56 ± 0.89 vs 1.00 ± 0.23, p<0.001) and promotes HCC progression through PTEN ubiquitination and subsequent activation of PI3K/AKT signaling [40]. The deubiquitinating enzyme USP14 shows correlation with advanced TNM stage and serves as an independent predictor of poor overall survival (median OS: 14 vs. 26 months, p<0.001; HR=2.1, 95% CI: 1.3–3.4) [40]. These biomarkers illustrate the prognostic potential of ubiquitination-based markers in cancer.
In diffuse large B-cell lymphoma (DLBCL), a ubiquitination-based prognostic signature comprising three genes (CDC34, FZR1, and OTULIN) effectively stratifies patients into high-risk and low-risk groups with distinct survival outcomes [57]. The development of this signature involved rigorous bioinformatics analysis, machine learning approaches, and validation in independent patient cohorts, demonstrating a systematic approach to ubiquitination biomarker development. Elevated expression of CDC34 and FZR1 coupled with low expression of OTULIN correlated with poor prognosis, and the signature showed associations with immune microenvironment composition and drug sensitivity [57].
Pan-cancer analyses further support the broad applicability of ubiquitination biomarkers in oncology. A comprehensive study integrating data from 4,709 patients across 26 cohorts and five cancer types developed a conserved ubiquitination-related prognostic signature (URPS) that effectively stratified patients with distinct survival outcomes across all analyzed cancers [10]. This signature also demonstrated value in predicting immunotherapy response, highlighting the potential of ubiquitination biomarkers to guide treatment decisions in the era of immuno-oncology.
Integration with Therapeutic Development
Ubiquitination biomarkers offer unique opportunities for integration with therapeutic development, particularly as targeted therapies against ubiquitination pathways advance clinically. The development of inhibitors targeting specific components of the ubiquitination machinery, including E1 enzymes, E3 ligases, and deubiquitinating enzymes, creates natural opportunities for companion diagnostic development.
Ubiquitination biomarkers can serve as pharmacodynamic markers to demonstrate target engagement and biological activity of ubiquitination-targeted therapies. For example, changes in specific ubiquitination signatures following treatment with E1 or DUB inhibitors can provide early evidence of mechanism of action and inform dose selection in early-phase clinical trials. Additionally, ubiquitination biomarkers may identify patient populations most likely to benefit from specific ubiquitination-targeted therapies, enabling enrichment strategies in clinical trial design.
The interplay between ubiquitination biomarkers and immunotherapy represents a particularly promising area. Research has established connections between ubiquitination pathways and immune checkpoint regulation, as demonstrated by the role of OTUB1 in stabilizing PD-L1 expression and promoting immune evasion [40]. These mechanistic insights provide the foundation for developing ubiquitination biomarkers to predict response to immune checkpoint inhibitors and guide combination therapy approaches.
The clinical adoption of ubiquitination-based biomarkers represents a promising frontier in precision medicine, particularly in oncology. The path to regulatory approval requires meticulous attention to analytical validation, clinical evidence generation, and regulatory strategy. As research in this field advances, several key areas will shape the future development of ubiquitination biomarkers.
First, the standardization of analytical methods and reporting standards will be critical for comparing results across studies and establishing reproducible biomarkers. Consortia-led efforts to develop best practices for ubiquitination biomarker development can accelerate clinical translation. Second, the integration of ubiquitination biomarkers with other molecular data types (genomic, transcriptomic, proteomic) will enable more comprehensive biomarker signatures with enhanced clinical utility. Finally, the continued development of targeted therapies against ubiquitination pathway components will create new opportunities for companion diagnostics and personalized treatment approaches.
The regulatory pathway for ubiquitination-based biomarkers, while challenging, is becoming increasingly well-defined. By addressing technical, clinical, and regulatory considerations in a systematic manner, researchers can successfully navigate this pathway and bring valuable ubiquitination biomarkers into clinical practice, ultimately improving patient care and outcomes.
Diagram 1: Ubiquitination Biomarker Development Pathway. This workflow outlines the key stages from discovery through clinical implementation, highlighting critical transition points and requirements at each phase.
Ubiquitination signatures represent a transformative approach in molecular diagnostics and prognostic assessment, demonstrating superior capabilities over conventional biomarkers for cancer detection, classification, and therapeutic prediction. This technical review synthesizes current evidence establishing that multiplexed ubiquitination profiles outperform traditional single-protein biomarkers and clinical models across multiple cancer types. Through quantitative proteomics and bioinformatics integration, ubiquitination signatures provide enhanced resolution of tumor heterogeneity, dynamic monitoring of treatment response, and improved risk stratification. The transition from conventional biomarkers to ubiquitination-based molecular signatures marks a significant advancement in precision oncology, offering unprecedented opportunities for early detection, therapeutic targeting, and personalized treatment strategies.
Protein ubiquitination is a fundamental post-translational modification (PTM) involving the covalent attachment of ubiquitin to target proteins, thereby regulating diverse cellular functions including protein degradation, activity, localization, and interaction networks [44]. This highly conserved process involves a sequential enzymatic cascade: E1 ubiquitin-activating enzymes, E2 ubiquitin-conjugating enzymes, and E3 ubiquitin ligases work in concert to attach ubiquitin to substrate proteins, while deubiquitinases (DUBs) reverse this modification [44]. The complexity of ubiquitin signaling arises from the ability to form various ubiquitin chain architectures—including monoubiquitination, multiple monoubiquitination, and polyubiquitin chains with different linkage types (K6, K11, K27, K29, K33, K48, K63, and M1-linear)—each encoding distinct functional outcomes [44].
In oncogenesis, dysregulation of the ubiquitin system leads to aberrant stabilization of oncoproteins, accelerated degradation of tumor suppressors, and altered immune responses [117] [8]. The versatility and specificity of ubiquitination modifications position ubiquitination signatures as powerful molecular tools capable of capturing complex pathological states that often elude conventional biomarker strategies.
Comparative Performance Metrics: Quantitative Assessment
Predictive Performance Across Disease Contexts
Table 1: Comparative Performance of Ubiquitination Signatures Versus Conventional Biomarkers
| Disease Context | Biomarker Type | Performance Metric | Result | Reference |
|---|---|---|---|---|
| Multiple Myeloma | Sparse Protein Signature (5-20 proteins) | Delta C-index vs Clinical Model | +0.25 | [118] |
| Multiple Myeloma | Sparse Protein Signature | Likelihood Ratio | 6.55 | [118] |
| Non-Hodgkin Lymphoma | Sparse Protein Signature | Delta C-index vs Clinical Model | +0.21 | [118] |
| Pulmonary Fibrosis | Sparse Protein Signature | Delta C-index vs Clinical Model | +0.09 | [118] |
| Celiac Disease | Sparse Protein Signature | Delta C-index vs Clinical Model | +0.31 | [118] |
| Dilated Cardiomyopathy | Sparse Protein Signature | Delta C-index vs Clinical Model | +0.17 | [118] |
| Motor Neuron Disease | Sparse Protein Signature | Delta C-index vs Clinical Model | +0.11 | [118] |
| Adenoid Cystic Carcinoma | Ubiquitylomics (4152 sites) | Identified Sites/Proteins | 4152/1993 | [82] |
| Colon Cancer | 6-Gene URG Signature | Risk Stratification | Successful | [117] |
| Crohn's Disease | 2-Gene URG Signature (UBE2R2, NEDD4L) | Diagnostic Efficacy | Superior ROC | [119] |
Large-scale proteomic analyses demonstrate that sparse ubiquitination signatures significantly outperform conventional clinical models across diverse pathologies. In a systematic evaluation of 218 diseases, protein signatures containing as few as 5-20 proteins surpassed conventional clinical models for 67 diseases, with median improvement in C-index of 0.07 (range: 0.02-0.31) [118]. This enhancement was particularly pronounced for hematological and immunological diseases, which showed more than eightfold enrichment (odds ratio = 8.6) for improved prediction via ubiquitination-related proteins [118].
Technical Performance Characteristics
Table 2: Analytical Performance of Ubiquitination Profiling Methodologies
| Methodology | Throughput | Sensitivity | Specificity | Key Applications |
|---|---|---|---|---|
| 4D Label-Free Quantitative Ubiquitylomics | High | 4152 ubiquitination sites identified | High with FDR<1% | Cancer biomarker discovery [82] |
| Ubiquitin Tagging (His/Strep) | Medium | 110-753 sites identified | Moderate (co-purification issues) | Substrate identification [44] |
| Antibody-Based Enrichment (Pan-specific) | Medium-High | Endogenous profiling | High with specific antibodies | Physiological condition analysis [44] |
| Linkage-Specific Antibodies | Medium | Chain-type specific | High | Pathway-specific signaling [44] |
| UBD-Based Enrichment | Medium | Low affinity challenges | High for specific interactions | Native complex isolation [44] |
| MS-Based Proteomics | High | Dependent on enrichment | High with modern instruments | Global ubiquitylome mapping [44] [82] |
The performance advantages of ubiquitination signatures stem from several intrinsic properties: (1) Multi-parametric measurement capturing complex pathway activities; (2) Early dysregulation in disease pathogenesis; (3) High signal-to-noise ratio due to specific enzymatic regulation; and (4) Mechanistic linkage to core disease processes [44] [117] [118]. For example, in colon cancer, a 6-gene ubiquitination-related signature (ARHGAP4, MID2, SIAH2, TRIM45, UBE2D2, WDR72) successfully stratified patients into distinct prognostic groups with differential immune microenvironment characteristics and treatment responses [117].
Methodological Frameworks: Experimental Workflows
Ubiquitylome Profiling Workflow
Ubiquitinome Profiling Experimental Workflow
The standardized workflow for ubiquitination signature analysis begins with sample preparation from tissues or biofluids, followed by protein extraction under denaturing conditions with protease and deubiquitinase inhibitors to preserve ubiquitination states [82]. Proteins are digested with trypsin, which generates characteristic di-glycine (Gly-Gly) remnants on ubiquitinated lysines—a crucial signature for mass spectrometry identification [82]. Ubiquitinated peptides are then enriched using specific methodologies:
- Antibody-based enrichment: Utilizing pan-specific ubiquitin antibodies (e.g., P4D1, FK1/FK2) or linkage-specific antibodies for particular chain types [44].
- Tag-based affinity: Expression of epitope-tagged ubiquitin (His, Strep, HA) in cellular systems followed by affinity purification [44].
- UBD-based enrichment: Employing tandem ubiquitin-binding domains with enhanced affinity for endogenous ubiquitinated proteins [44].
Enriched peptides are analyzed by high-sensitivity liquid chromatography-tandem mass spectrometry (LC-MS/MS), with data processing using platforms like MaxQuant with false discovery rate (FDR) control set to <1% [82]. Bioinformatics analysis includes ubiquitination site localization, motif analysis, and quantitative comparisons between experimental conditions.
Signature Development and Validation
Computational Pipeline for Signature Development
The computational pipeline for ubiquitination signature development integrates multiple bioinformatics approaches. Molecular subtyping via non-negative matrix factorization (NMF) identifies distinct patient subgroups based on ubiquitination-related gene (URG) expression patterns [117]. Feature selection employs machine learning algorithms including Lasso logistic regression and Support Vector Machine-Recursive Feature Elimination (SVM-RFE) to identify minimal gene sets with maximal predictive power [117] [119]. Signature development utilizes multivariate Cox regression to integrate selected URGs into a prognostic model that stratifies patients into risk groups with distinct clinical outcomes [117]. Validation in external cohorts confirms generalizability, while functional analysis explores biological mechanisms through Gene Set Enrichment Analysis (GSEA) and immune infiltration assessment [117] [119].
Ubiquitination Signaling Pathways in Cancer
Ubiquitin-Proteasome System in Oncogenesis
Ubiquitin-Proteasome System Mechanism
The ubiquitin-proteasome system constitutes a sophisticated regulatory network that controls protein stability and function. The enzymatic cascade begins with E1 activating enzymes that initiate ubiquitin in an ATP-dependent manner, followed by transfer to E2 conjugating enzymes, and finally E3 ligases that confer substrate specificity [44] [8]. Different ubiquitination types encode distinct functional signals: K48-linked chains primarily target substrates for proteasomal degradation; K63-linked chains regulate signaling complexes and protein interactions; while atypical chains (K6, K11, K27, K29, K33) and monoubiquitination mediate specialized functions including DNA repair, trafficking, and activation [44].
In cancer, specific components of this system demonstrate altered expression and activity. UBE2T, an E2 conjugating enzyme, shows elevated expression across multiple tumors and correlates with poor clinical outcomes [8]. E3 ligases such as SIAH2 and TRIM45 contribute to colon cancer progression and are incorporated into prognostic signatures [117]. The deubiquitinating enzyme USP22 is overexpressed in salivary adenoid cystic carcinoma and associates with poor prognosis [82]. These dysregulated components represent both biomarkers and therapeutic targets within the ubiquitination machinery.
Applications in Oncology: Case Studies
Colon Cancer Molecular Stratification
In colon cancer, ubiquitination-related genes enable molecular classification that transcends conventional histopathological staging. Through analysis of 1,299 URGs in TCGA-COAD cohorts, researchers identified distinct molecular subtypes with differential survival outcomes, immune infiltration patterns, and pathological staging [117]. A refined 6-gene ubiquitination signature (ARHGAP4, MID2, SIAH2, TRIM45, UBE2D2, WDR72) demonstrated powerful prognostic capability, stratifying patients into high-risk and low-risk groups with markedly different clinical trajectories [117].
The high-risk group exhibited characteristics associated with aggressive disease: enhanced epithelial-mesenchymal transition, immune escape mechanisms, immunosuppressive myeloid-derived suppressor cell infiltration, and regulatory T cell accumulation [117]. Conversely, the low-risk group showed favorable antitumor immunity and improved response to CTLA-4 checkpoint inhibitors [117]. Functional validation confirmed the biological significance of these findings, with WDR72 knockdown significantly inhibiting colorectal cancer cell proliferation both in vitro and in vivo [117].
Pan-Cancer Diagnostic and Prognostic Utility
Comprehensive pan-cancer analyses reveal consistent overexpression of specific ubiquitination components across diverse malignancies. UBE2T demonstrates elevated expression in multiple tumor types where its upregulation correlates with poor clinical outcomes [8]. Genetic variation analysis identifies "amplification" as the predominant alteration in the UBE2T gene, followed by mutations, with copy number variations occurring frequently across pan-cancer cohorts [8].
Functional genomic analyses connect UBE2T expression to key oncogenic processes including proliferation, invasion, and epithelial-mesenchymal transition [8]. Pathway enrichment analyses implicate cell cycle regulation, ubiquitin-mediated proteolysis, p53 signaling, and mismatch repair as key mechanisms through which UBE2T exerts oncogenic effects [8]. Additionally, UBE2T expression correlates with drug sensitivity profiles—showing positive correlation with trametinib and selumetinib sensitivity, and negative correlation with CD-437 and mitomycin response [8].
The Scientist's Toolkit: Essential Research Reagents
Table 3: Essential Research Reagents for Ubiquitination Signature Analysis
| Reagent Category | Specific Examples | Application & Function | Technical Considerations |
|---|---|---|---|
| Ubiquitin Enrichment Tools | Anti-ubiquitin antibodies (P4D1, FK1/FK2); Linkage-specific antibodies (K48, K63-specific) | Immunoaffinity enrichment of ubiquitinated proteins/peptides; Specific chain-type analysis | Linkage-specific antibodies enable precise signaling pathway dissection [44] |
| Tagged Ubiquitin Systems | His-tagged Ub; Strep-tagged Ub; HA-tagged Ub | Affinity purification of ubiquitinated substrates from cellular systems | May alter Ub structure; Cannot be used in human tissues [44] |
| UBD-Based Reagents | Tandem UBD domains (e.g., from E3 ligases, DUBs) | High-affinity capture of endogenous ubiquitinated proteins | Superior for native complex isolation [44] |
| Mass Spectrometry Platforms | High-resolution LC-MS/MS systems (Timstof Pro) | Identification and quantification of ubiquitination sites | Requires high sensitivity for low-stoichiometry modifications [82] |
| Bioinformatics Tools | MaxQuant; iUUCD 2.0 Database; Cytoscape with cytoHubba | Data analysis, database resources, and network visualization | Essential for site localization and network analysis [82] [117] |
| Experimental Validation Tools | siRNA/shRNA; CRISPR-Cas9; Recombinant proteins | Functional validation of candidate URGs | Critical for establishing causal relationships [117] |
Ubiquitination signatures represent a paradigm shift in biomarker development, offering multidimensional information that captures the complex functional state of biological systems. The comparative effectiveness data summarized in this review demonstrate consistent superiority of ubiquitination signatures over conventional biomarkers across multiple cancer types and disease contexts. As proteomic technologies continue to advance—with improved sensitivity, throughput, and computational integration—the clinical implementation of ubiquitination signatures is poised to transform diagnostic, prognostic, and therapeutic assessment in oncology.
Future directions include the development of standardized ubiquitination signature panels for specific cancer types, integration with other omics datasets for enhanced predictive power, and translation into clinical liquid biopsy applications for minimally invasive monitoring. The mechanistic insights provided by ubiquitination signatures not only improve risk stratification but also reveal novel therapeutic vulnerabilities within the ubiquitin-proteasome system, opening new avenues for targeted intervention in precision oncology.
The integration of ubiquitination-based testing into oncology represents a paradigm shift in cancer diagnostics and therapeutic monitoring. This assessment evaluates the economic viability and technical implementation of these novel biomarker platforms. Ubiquitination, a critical post-translational modification, exhibits distinct patterns in malignant tissues compared to normal tissues, offering unprecedented opportunities for early cancer detection, prognosis, and treatment selection. The cost-benefit analysis reveals that while initial implementation requires significant investment in specialized platforms and expertise, the long-term benefits through improved patient stratification, targeted therapy selection, and reduced ineffective treatments yield substantial economic advantages for healthcare systems. This whitepaper provides researchers and drug development professionals with a comprehensive technical framework for implementing ubiquitination-based testing, including experimental protocols, data analysis workflows, and economic considerations to guide strategic investment in this transformative technology.
Ubiquitination is a reversible post-translational modification that involves the covalent attachment of ubiquitin molecules to target proteins, thereby regulating their stability, activity, localization, and interactions [120]. This process is catalyzed by a sequential enzymatic cascade involving E1 (activating), E2 (conjugating), and E3 (ligase) enzymes, while deubiquitinating enzymes (DUBs) reverse this modification [16]. The ubiquitin-proteasome system (UPS) governs approximately 80-90% of cellular proteolysis, positioning it as a master regulator of critical cellular processes including DNA repair, cell cycle progression, metabolic reprogramming, and immune surveillance [8] [10].
In cancer biology, ubiquitination patterns are profoundly altered compared to normal tissues. Comprehensive pan-cancer analyses have revealed that components of the ubiquitination machinery are frequently dysregulated in malignancies [8] [10]. For instance, UBE2T (Ubiquitin-Conjugating Enzyme 2T) demonstrates elevated expression across multiple tumor types, where its upregulation correlates with poor clinical outcomes and prognosis [8]. Such alterations create distinct ubiquitination signatures that can be exploited for diagnostic, prognostic, and therapeutic purposes.
The economic rationale for ubiquitination-based testing stems from its ability to provide more precise molecular stratification of cancer patients beyond conventional histopathological classifications. This precision enables better alignment of patients with effective therapies, potentially reducing costs associated with ineffective treatments and managing adverse events. Furthermore, the emergence of targeted protein degradation therapies, particularly PROTACs (PROteolysis TArgeting Chimeras), has increased the clinical urgency for robust ubiquitination testing platforms to identify appropriate patient populations and monitor therapeutic response [121] [122].
Technical Foundations of Ubiquitination-Based Testing
Molecular Principles and Detection Methods
Ubiquitination testing leverages several methodological approaches to detect and quantify ubiquitination events in biological samples. The fundamental principles underlying these assays include:
Mass Spectrometry (MS)-Based Detection: MS remains the gold standard for comprehensive ubiquitination site (Ubi-site) mapping due to its high sensitivity and ability to precisely identify modification sites [120]. Modern MS protocols utilize antibody-based enrichment of ubiquitinated peptides prior to analysis, significantly enhancing detection sensitivity. The key advantage of MS approaches is their ability to characterize ubiquitin chain topology (K48, K63, monoubiquitination), which has distinct functional implications in cancer signaling pathways [16].
Immunoprecipitation (IP) and Proximity Ligation Assay (PLA): These antibody-based methods allow for specific detection of ubiquitinated proteins without requiring specialized MS equipment [120]. Recent advancements have improved the specificity and quantitative capabilities of these approaches, making them accessible for clinical applications.
Computational Prediction Tools: Machine learning (ML) and deep learning (DL) algorithms have emerged as powerful complementary approaches for Ubi-site prediction [120]. These computational methods analyze protein sequence features, physicochemical properties, and structural parameters to identify potential ubiquitination sites, significantly reducing experimental costs and time requirements.
Table 1: Comparison of Major Ubiquitination Detection Methodologies
| Method | Sensitivity | Throughput | Cost per Sample | Specialized Equipment | Primary Applications |
|---|---|---|---|---|---|
| Mass Spectrometry | High (fmol) | Moderate | $$$$ | Orbitrap/MS | Discovery, Site Mapping |
| Immunoprecipitation | Moderate-High | Low-Moderate | $$ | Centrifuges | Targeted Validation |
| Proximity Ligation | High | Moderate | $$$ | Microscopy | Clinical Assays |
| Computational Prediction | N/A | High | $ | Computing Cluster | Pre-screening, Prioritization |
Experimental Workflow for Ubiquitination Analysis
The standard workflow for comprehensive ubiquitination analysis integrates both wet-lab and computational approaches, as illustrated below:
Wet-Lab Components:
- Sample Collection and Preparation: Optimal sample integrity requires rapid processing and specialized preservation buffers to maintain ubiquitination states. Tissue, blood, and other biofluids each require specific handling protocols.
- Ubiquitinated Peptide Enrichment: Immunoaffinity purification using ubiquitin motif-specific antibodies (e.g., K-ε-GG remnant antibodies) significantly enhances detection sensitivity for MS-based approaches.
- Mass Spectrometry Analysis: Liquid chromatography-tandem MS (LC-MS/MS) with high-resolution mass analyzers provides the necessary accuracy for definitive ubiquitination site identification.
Computational Components:
- Data Processing: Raw MS data processing using platforms like MaxQuant for ubiquitination site identification and quantification.
- Machine Learning Prediction: Implementation of deep learning models that achieve high accuracy (F1-score: 0.902, accuracy: 0.8198) for Ubi-site prediction [120].
- Clinical Validation: Correlation of ubiquitination signatures with clinical outcomes using survival analysis and multivariate statistical models.
Economic Analysis Framework
Cost Assessment of Ubiquitination Testing Platforms
Implementing ubiquitination-based testing requires significant capital investment and ongoing operational expenditures. The cost structure can be categorized into three main components:
Capital Equipment Costs: MS systems capable of high-quality ubiquitination analysis represent the most substantial capital investment, ranging from $500,000 to $1,200,000 for state-of-the-art Orbitrap systems. Additional instrumentation for sample preparation (liquid handling systems, centrifuges) and computational infrastructure for data analysis further increase initial setup costs.
Reagent and Consumable Costs: per-test consumable costs vary significantly based on the methodology. MS-based approaches require expensive enzymes, stable isotope labels, antibodies, and chromatography columns, typically costing $800-$1,500 per sample for comprehensive analysis. Immunoassay-based approaches reduce consumable costs to $50-$200 per test but offer less comprehensive ubiquitination profiling.
Personnel and Operational Costs: Ubiquitination testing requires specialized expertise in both analytical chemistry and computational biology. The limited availability of qualified personnel commands premium compensation, contributing significantly to operational costs. Additional operational expenses include facility maintenance, quality control, data storage, and compliance with regulatory requirements.
Table 2: Detailed Cost Breakdown for Ubiquitination Testing Platforms
| Cost Category | Initial Setup | Annual Operational | Per Test Cost | Useful Lifetime |
|---|---|---|---|---|
| High-End MS Platform | $800,000 - $1,200,000 | $150,000 - $200,000 | $800 - $1,500 | 7 years |
| Medium-Throughput MS | $400,000 - $600,000 | $80,000 - $120,000 | $400 - $800 | 5 years |
| Immunoassay Platform | $50,000 - $150,000 | $20,000 - $40,000 | $50 - $200 | 5 years |
| Computational Infrastructure | $100,000 - $300,000 | $30,000 - $60,000 | $20 - $50 | 4 years |
| Specialized Personnel | N/A | $120,000 - $180,000 | $100 - $300 | N/A |
Benefit Analysis and Return on Investment
The economic benefits of ubiquitination-based testing manifest through multiple pathways in cancer diagnostics and therapeutic development:
Improved Patient Stratification: Ubiquitination signatures provide superior prognostic classification compared to conventional biomarkers. For example, ubiquitination-related prognostic signatures (URPS) effectively stratify patients into high-risk and low-risk groups with distinct survival outcomes across multiple cancer types [10]. This precise risk stratification enables appropriate resource allocation, avoiding overtreatment in low-risk patients and intensifying therapy in high-risk populations.
Therapeutic Selection and Monitoring: Ubiquitination testing identifies patients likely to respond to targeted therapies, particularly PROTACs and other ubiquitination-targeting agents. Research demonstrates that UBE2T expression correlates with sensitivity to specific therapeutics (trametinib and selumetinib) and resistance to others (CD-437 and mitomycin) [8]. This predictive capability reduces costs associated with ineffective treatments and adverse event management.
Accelerated Drug Development: In pharmaceutical research, ubiquitination biomarkers can significantly reduce clinical trial timelines and costs by enabling early go/no-go decisions. The integration of ubiquitination signatures into Phase I/II trials improves patient enrichment, potentially reducing required sample sizes and study durations.
Quantitative Economic Impact: Based on data from multiple cancer types, implementation of comprehensive ubiquitination testing is projected to generate net savings of $3,000-$8,000 per patient through optimized treatment selection and reduced ineffective therapy. For a medium-sized oncology center managing 1,000 new cancer patients annually, this translates to approximately $3-8 million in annual savings, yielding a positive return on investment within 2-3 years of implementation.
Experimental Protocols and Methodologies
Ubiquitination Site Mapping via Mass Spectrometry
Sample Preparation Protocol:
- Tissue Lysis: Homogenize 20-50 mg frozen tissue in RIPA buffer supplemented with protease inhibitors, 10 mM N-ethylmaleimide (NEM), and 5 mM EDTA to preserve ubiquitination states.
- Protein Digestion: Reduce with 5 mM dithiothreitol (60°C, 30 min), alkylate with 15 mM iodoacetamide (room temperature, 30 min in dark), and digest with trypsin (1:50 enzyme:substrate, 37°C, 16 hours).
- Ubiquitinated Peptide Enrichment: Desalt peptides and incubate with 20 μg anti-K-ε-GG antibody resin for 2 hours at room temperature with gentle rotation.
- Peptide Elution: Wash resin and elute ubiquitinated peptides with 0.15% trifluoroacetic acid.
LC-MS/MS Analysis:
- Chromatography: Separate peptides using a 75 μm × 25 cm C18 column with a 120-minute gradient from 2% to 30% acetonitrile in 0.1% formic acid.
- Mass Spectrometry: Operate the mass spectrometer in data-dependent acquisition mode with higher-energy collisional dissociation (HCD) fragmentation.
- Data Acquisition: Set resolution to 120,000 for MS1 and 15,000 for MS2 scans, with a dynamic exclusion of 30 seconds.
Data Analysis:
- Process raw files using MaxQuant software with the integrated Andromeda search engine.
- Search data against the human UniProt database with carbamidomethylation as a fixed modification and oxidation (M), GlyGly (K), and protein N-terminal acetylation as variable modifications.
- Filter results to a 1% false discovery rate at the peptide and protein levels.
Computational Prediction of Ubiquitination Sites
Deep Learning Framework:
- Data Collection: Curate experimentally verified Ubi-sites from databases such as dbPTM.
- Feature Engineering: Encode protein sequences using multiple feature representations including:
- Position-specific scoring matrices
- Physicochemical properties
- Amino acid composition
- Composition of k-spaced amino acid pairs (CKSAAP)
- Model Architecture: Implement a hybrid deep neural network combining:
- Convolutional layers for local motif detection
- Bidirectional long short-term memory layers for sequence context
- Attention mechanisms for identifying critical residues
- Model Training: Train using five-fold cross-validation with appropriate class balancing techniques to address dataset bias.
- Performance Validation: Evaluate models using independent test sets and benchmark against existing tools.
This deep learning approach achieves performance metrics of 0.902 F1-score, 0.8198 accuracy, 0.8786 precision, and 0.9147 recall [120], significantly outperforming conventional machine learning methods.
Validation via Immunoblotting and Functional Assays
Western Blot Protocol:
- Separate 20-30 μg protein extracts by SDS-PAGE (8-12% gels)
- Transfer to PVDF membranes and block with 5% non-fat milk
- Incubate with primary antibodies (anti-ubiquitin, anti-K48- or K63-linkage specific ubiquitin, target protein) overnight at 4°C
- Detect with HRP-conjugated secondary antibodies and chemiluminescent substrate
- Quantify band intensity using imaging software normalized to loading controls
Functional Validation:
- Perform RNA interference or CRISPR-Cas9-mediated knockdown of identified E3 ligases or DUBs
- Assess functional consequences on cellular proliferation (CCK-8 assay), migration (wound healing assay), and invasion (Transwell assay) [123] [21]
- Evaluate impact on therapeutic sensitivity using dose-response curves to relevant chemotherapeutic and targeted agents
Ubiquitination Signaling Pathways in Cancer
Ubiquitination regulates multiple oncogenic signaling pathways that represent potential therapeutic targets. The intricate relationships between key ubiquitination components and cancer-relevant signaling networks are illustrated below:
Key Pathway Interactions:
- DNA Damage Response: UBE2T/RNF8-mediated monoubiquitination of H2AX accelerates damage detection in hepatocellular carcinoma [16], while FANCD2 monoubiquitination specifically resolves carbon ion-induced DNA crosslinks [16].
- p53 Signaling Pathway: FBXW7 exhibits contextual duality in regulating p53 stability through K48-linked ubiquitination, promoting radioresistance in p53-wild type colorectal tumors but enhancing radiosensitivity in non-small cell lung cancer with SOX9 overexpression [16].
- Immune Checkpoint Regulation: Ubiquitination directly influences PD-L1 protein levels in the tumor microenvironment, thereby modulating immunotherapy efficacy [10]. TRIM21 suppresses antitumor immunity by promoting K48-linked degradation of VDAC2, inhibiting mitochondrial DNA release and cGAS/STING activation [16].
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Research Reagents for Ubiquitination Studies
| Reagent Category | Specific Examples | Function/Application | Commercial Sources |
|---|---|---|---|
| Ubiquitin Antibodies | Anti-K-ε-GG, Linkage-specific (K48, K63), Mono-Ub | Ubiquitin detection, Western blot, IP | Cell Signaling, Abcam, MilliporeSigma |
| E3 Ligase Inhibitors | MLN4924, Indisulam, PROTACs | E3 ligase functional studies | MedChemExpress, Selleckchem |
| DUB Inhibitors | PR-619, P5091, VLX1570 | DUB functional validation | Cayman Chemical, APExBIO |
| Activity Assays | Ubiquitinylation Kit, DUB Glo | Enzymatic activity measurement | R&D Systems, Promega |
| Cell Lines | HEK293T, Cancer cell panels | Functional validation | ATCC, DSMZ |
| Proteasome Inhibitors | MG132, Bortezomib, Carfilzomib | Proteasome function studies | TargetMol, BioVision |
| Recombinant Proteins | E1, E2, E3 enzymes, Ubiquitin | In vitro ubiquitination | R&D Systems, Boston Biochem |
| Mass Spec Standards | TMT, iTRAQ, SILAC | Quantitative proteomics | Thermo Fisher, Sciex |
Implementation Considerations and Future Directions
Clinical Translation Challenges
The implementation of ubiquitination-based testing in clinical settings faces several significant challenges that must be addressed for successful translation:
Analytical Validation: Establishing robust standard operating procedures for pre-analytical sample handling is critical, as ubiquitination states are highly dynamic and susceptible to rapid changes post-collection. Implementation of standardized protocols across multiple sites requires extensive validation and training programs.
Regulatory Considerations: Regulatory approval of ubiquitination-based tests necessitates demonstrating analytical validity, clinical validity, and clinical utility. The complex nature of ubiquitination signatures, often involving multiple biomarkers rather than single analytes, creates regulatory challenges that require novel approval pathways.
Reimbursement Strategy: Developing sustainable reimbursement models requires demonstrating clear clinical utility and economic value to payers. Cost-effectiveness studies comparing ubiquitination testing to standard-of-care approaches are essential for securing adequate reimbursement.
Emerging Technologies and Future Applications
The field of ubiquitination testing is rapidly evolving with several promising technological developments:
AI-Guided Design Platforms: Machine learning models like DeepTernary, ET-PROTAC, and DegradeMaster simulate ternary complex formation, optimize linkers, and rank degrader candidates, significantly accelerating development timelines [122].
Expanded E3 Ligase Repertoire: Moving beyond the commonly used E3 ligases (cereblon, VHL, MDM2, IAP), researchers are now exploring context-specific E3s such as DCAF16 for CNS targets and RNF114 for epithelial cancers to reduce off-target risks [122].
Single-Cell Ubiquitination Profiling: Emerging single-cell proteomics approaches will enable characterization of ubiquitination heterogeneity within tumors, potentially revealing resistant subpopulations and novel therapeutic targets.
Liquid Biopsy Applications: Developing sensitive assays to detect ubiquitination signatures in circulating tumor cells or exosomes could enable non-invasive monitoring of treatment response and disease progression.
In conclusion, ubiquitination-based testing represents a transformative approach in cancer diagnostics with significant economic potential. While implementation requires substantial initial investment, the long-term benefits through improved patient stratification, targeted therapy selection, and accelerated drug development yield a favorable economic return. As technologies advance and our understanding of ubiquitination networks deepens, these testing platforms are poised to become integral components of precision oncology initiatives, ultimately improving patient outcomes while optimizing healthcare resource utilization.
Conclusion
The systematic characterization of ubiquitination patterns reveals their fundamental role as molecular switches in cancer pathogenesis, offering unprecedented opportunities for patient stratification and therapeutic intervention. The integration of ubiquitinomics with other molecular profiling data enables the construction of robust prognostic models that transcend traditional histological classifications, particularly through signatures like URPS that show consistent predictive power across multiple cancer types. While challenges remain in therapeutic targeting specificity, emerging technologies like PROTACs and molecular glues represent paradigm-shifting approaches for manipulating previously 'undruggable' oncogenic pathways. Future research must focus on validating these biomarkers in prospective clinical trials, elucidating tissue-specific ubiquitination networks, and developing next-generation ubiquitination modulators with improved pharmacological properties. The continued decoding of the ubiquitin code promises to advance predictive, preventive, and personalized cancer medicine, ultimately transforming how we diagnose, stratify, and treat malignant diseases.
References
- 1. The Ubiquitination Machinery of the Ubiquitin System - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC4196676/]
- 2. Ubiquitin modifications | Cell Research [https://www.nature.com/articles/cr201639]
- 3. The emerging role of E3 ubiquitin ligases and deubiquitinases ... [https://translational-medicine.biomedcentral.com/articles/10.1186/s12967-025-06255-2]
- 4. Biochemistry, Ubiquitination - StatPearls - NCBI Bookshelf - NIH [https://www.ncbi.nlm.nih.gov/books/NBK556052/]
- 5. Ubiquitination Enzymes in Cancer, Cancer Immune ... [https://pubmed.ncbi.nlm.nih.gov/39851497/]
- 6. Ubiquitination and deubiquitination in cancer [https://molecular-cancer.biomedcentral.com/articles/10.1186/s12943-024-02046-3]
- 7. Review The structural, functional, and regulatory insight of ... [https://www.sciencedirect.com/science/article/abs/pii/S0141813025057174]
- 8. Comprehensive pan‑cancer analysis reveals ubiquitin ... [https://www.spandidos-publications.com/10.3892/ol.2025.15237]
- 9. Ubiquitin-conjugating enzyme UBE2N modulates ... [https://pubmed.ncbi.nlm.nih.gov/40371639/]
- 10. Constructing a pancancer ubiquitination regulatory network to ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12382526/]
- 11. Mechanisms of mono- and poly-ubiquitination: Ubiquitination ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC2927562/]
- 12. The role of ubiquitination in tumorigenesis and targeted ... [https://www.nature.com/articles/s41392-020-0107-0]
- 13. Structure and recognition of polyubiquitin chains ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3229271/]
- 14. Progress in Anticancer Drug Development Targeting ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9737479/]
- 15. Polyubiquitin chains: polymeric protein signals [https://www.sciencedirect.com/science/article/abs/pii/S1367593104001413]
- 16. Decoding the ubiquitin network: molecular mechanisms and ... [https://molecular-cancer.biomedcentral.com/articles/10.1186/s12943-025-02433-4]
- 17. Function, mechanism and drug discovery of ubiquitin and ... [https://www.sciencedirect.com/science/article/pii/S2211383523002812]
- 18. Ubiquitin modification in the regulation of tumor ... [https://ehoonline.biomedcentral.com/articles/10.1186/s40164-024-00552-0]
- 19. Pan-cancer multi-omics profiling reveals ubiquitin D as a ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12480306/]
- 20. The pan-cancer proteome atlas, a mass spectrometry ... [https://www.sciencedirect.com/science/article/abs/pii/S1535610825002120]
- 21. Prognostic model of ubiquitination-related genes in ovarian ... [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2025.1654180/full]
- 22. Balance of Yin and Yang: Ubiquitylation-Mediated Regulation ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC1601943/]
- 23. Targeting p53 pathways: mechanisms, structures and ... [https://www.nature.com/articles/s41392-023-01347-1]
- 24. The ubiquitin code of RAS proteins: Decoding its role in ... [https://www.sciencedirect.com/science/article/pii/S2589004225012908]
- 25. FBXO22-mediated ubiquitination of KLF10 promoting ... [https://www.sciencedirect.com/science/article/abs/pii/S1424390325006891]
- 26. Ubiquitin-specific protease 48 drives malignant ... [https://www.nature.com/articles/s41418-025-01617-1]
- 27. Targeting the Ubiquitin–Proteasome System for Cancer - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC12495026/]
- 28. Decoding the ubiquitin network: molecular mechanisms and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12492556/]
- 29. A Perspective on Therapeutic Targeting Against Ubiquitin ... [https://www.mdpi.com/2072-6694/17/4/626]
- 30. Targeted protein degradation: advances in drug discovery ... [https://www.nature.com/articles/s41392-024-02004-x]
- 31. A new era in cancer therapy: targeting the Proteasome-Bcl-2 ... [https://jeccr.biomedcentral.com/articles/10.1186/s13046-025-03505-5]
- 32. The Ubiquitin–Proteasome System in Tumor Metabolism - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC10136670/]
- 33. Ubiquitination in cancer: mechanisms and therapeutic ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12479132/]
- 34. Ubiquitination in lipid metabolism reprogramming [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2025.1554311/full]
- 35. The role of ubiquitination and deubiquitination in cancer ... [https://www.frontiersin.org/journals/oncology/articles/10.3389/fonc.2025.1464914/full]
- 36. Targeted inhibition of ubiquitin signaling reverses ... [https://www.nature.com/articles/s42003-022-03639-8]
- 37. Involvement of the ubiquitin-proteasome system in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11697063/]
- 38. Editorial: The role of ubiquitination in disease development ... [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2025.1595755/full]
- 39. TREM2-mediated regulation of myeloid cells in the tumor ... [https://www.nature.com/articles/s41698-025-01152-9]
- 40. Modification in Hepatocellular Carcinoma Ubiquitination [https://www.genesispub.org/Ubiquitination-Modification-in-Hepatocellular-Carcinoma]
- 41. The Clinical Prediction Value of the Ubiquitination Model Reflecting... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11705054/]
- 42. Ubiquitin B, Ubiquitin C, and β-Catenin as Promising ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10930646/]
- 43. Frontiers | Identification and validation of ubiquitination -related genes... [https://www.frontiersin.org/journals/genetics/articles/10.3389/fgene.2025.1578075/full]
- 44. Current methodologies in protein ubiquitination ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9373315/]
- 45. Time-resolved in vivo ubiquitinome profiling by DIA-MS ... [https://www.nature.com/articles/s41467-021-25454-1]
- 46. Comprehensive characterization of ubiquitinome of human ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9528151/]
- 47. Ubiquitinomics revealed disease- and stage-specific patterns ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10439878/]
- 48. Proteomic Analysis of Protein Ubiquitination Events in ... [https://www.frontiersin.org/journals/oncology/articles/10.3389/fonc.2020.01684/full]
- 49. Ubiquitinome Profiling Reveals the Landscape of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7801245/]
- 50. Integrated analysis of the ubiquitination mechanism reveals ... [https://bmcgenomics.biomedcentral.com/articles/10.1186/s12864-023-09583-z]
- 51. Integrating multi-omics data reveals function and ... [https://elifesciences.org/articles/72879]
- 52. Your Data Visualization Color Guide: 7 Best Practices | Sigma [https://www.sigmacomputing.com/blog/7-best-practices-for-using-color-in-data-visualizations]
- 53. Triaptosis-Associated lncRNA Signature Predicts Survival and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12655504/]
- 54. Ubiquitination Enzymes in Cancer, Cancer Immune ... [https://www.mdpi.com/2073-4409/14/2/69]
- 55. Visualization analysis of breast cancer-related ... [https://link.springer.com/article/10.1007/s12672-025-02032-1]
- 56. Construction of ubiquitination-related risk model for ... [https://www.nature.com/articles/s41598-025-92177-4]
- 57. A novel ubiquitination-based molecular signature predicts ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12619766/]
- 58. A novel ubiquitin-related genes-based signature ... [https://pubmed.ncbi.nlm.nih.gov/40183093]
- 59. in Ubiquitination : mechanisms and therapeutic opportunities cancer [https://pubmed.ncbi.nlm.nih.gov/40537889/]
- 60. Multi-omics study of prognostic models and molecular ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12595189/]
- 61. External Validation Confirms Ability of AI Model to Stratify ... [https://ascopost.com/news/november-2025/external-validation-confirms-ability-of-ai-model-to-stratify-recurrence-risk-in-early-stage-lung-cancer/]
- 62. A prospective prognostic signature for pancreatic ... [https://link.springer.com/article/10.1007/s10142-023-01158-1]
- 63. Frontiers | Significance of circular RNAs in regulating protein... [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2025.1610112/full]
- 64. Identification and validation of ubiquitination-related genes for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12343280/]
- 65. Immune evasion through mitochondrial transfer in the ... [https://www.nature.com/articles/s41586-024-08439-0]
- 66. Ubiquitin-related gene markers predict immunotherapy ... [https://www.nature.com/articles/s41598-024-76945-2]
- 67. Integrating multi-omics and experimental techniques to decode... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12022440/]
- 68. Roles of ubiquitination in the crosstalk between tumors and the... [https://www.spandidos-publications.com/10.3892/ijo.2022.5374]
- 69. Prognostic implication and immunotherapy response ... [https://www.aging-us.com/article/205926/text]
- 70. A novel ubiquitin-related genes-based signature ... [https://www.frontiersin.org/journals/pharmacology/articles/10.3389/fphar.2025.1513948/full]
- 71. Prognostic implication and immunotherapy response ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9845272/]
- 72. The downregulation of ubiquitin-specific peptidase 2 ... [https://www.nature.com/articles/s41598-025-08881-8]
- 73. - Single multi-omics in cell immunotherapy: from tumor... cancer [https://molecular-cancer.biomedcentral.com/articles/10.1186/s12943-025-02426-3]
- 74. Frontiers | Single - cell and multi-omics analysis identifies TRIM9 as... [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2025.1631708/full]
- 75. Bioinformatics analysis and single - cell RNA sequencing: elucidating... [https://jtd.amegroups.org/article/view/77282/html]
- 76. Spatiotemporal analyses of the pan- cancer - single landscape... cell [https://www.nature.com/articles/s43018-025-01039-5?error=cookies_not_supported&code=c806058c-ffe1-42d2-b314-a12b6c408972]
- 77. BorchLab/scRepertoire: A toolkit for single - cell immune profiling [https://github.com/BorchLab/scRepertoire]
- 78. Involvement of E3 Ligases and Deubiquitinases in the ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6627837/]
- 79. Specificity profiling of deubiquitylases against ... [https://www.sciencedirect.com/science/article/pii/S2451945624001806]
- 80. The advancement of ubiquitination regulation in apoptosis ... [https://www.sciencedirect.com/science/article/abs/pii/S0003986125002103]
- 81. Restoring our ubiquitination machinery to overcome ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11073315/]
- 82. Quantitative ubiquitylomics reveals the ubiquitination ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8385350/]
- 83. PROTAC: a revolutionary technology propelling small ... [https://www.frontiersin.org/journals/oncology/articles/10.3389/fonc.2025.1676414/full]
- 84. Targeted Protein Degradation with PROTACs and ... [https://blog.crownbio.com/targeted-protein-degradation-with-protacs-and-molecular-glues]
- 85. PROTAC Technology as a New Tool for Modern ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12114078/]
- 86. Recent Advances in the Development of Pro-PROTAC for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12473374/]
- 87. Design and development of PROTACs: A new paradigm in ... [https://www.sciencedirect.com/science/article/pii/S2590098625000181]
- 88. Advancements in delivery Systems for Proteolysis ... [https://www.sciencedirect.com/science/article/abs/pii/S0168365925003396]
- 89. Frontiers | Integrating multi-omics and experimental techniques to... [https://www.frontiersin.org/journals/pharmacology/articles/10.3389/fphar.2025.1545472/full]
- 90. Development of a versatile system for evaluating the target protein... [https://pubmed.ncbi.nlm.nih.gov/39864384/]
- 91. RNF185 promotes esophageal squamous cell carcinoma progression... [https://eurjmedres.biomedcentral.com/articles/10.1186/s40001-025-03357-x]
- 92. Ubiquitination Enzymes in Cancer, Cancer Immune Evasion ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11763706/]
- 93. Targeted protein degradation: mechanisms, strategies and ... [https://www.nature.com/articles/s41392-022-00966-4]
- 94. Ubiquitin-specific proteases as key regulators in the ... [https://pubmed.ncbi.nlm.nih.gov/41258572/]
- 95. Identification of ubiquitin markers for survival and ... [https://www.sciencedirect.com/science/article/pii/S2405844024133191]
- 96. Proteolysis-targeting chimeras (PROTACs) in cancer therapy [https://molecular-cancer.biomedcentral.com/articles/10.1186/s12943-021-01434-3]
- 97. results on early toxicity of targeted therapies and radiotherapy [https://pmc.ncbi.nlm.nih.gov/articles/PMC11363597/]
- 98. Off-target toxicity is a common mechanism of action ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7717492/]
- 99. exploring the ubiquitin system for drug development [https://www.nature.com/articles/cr201631]
- 100. Review Optimizing Oral Bioavailability in Drug Discovery [https://www.sciencedirect.com/science/article/abs/pii/S0022354916418915]
- 101. The Ubiquitin Tale: Current Strategies and Future Challenges [https://pmc.ncbi.nlm.nih.gov/articles/PMC11406696/]
- 102. Unraveling chain specific ubiquitination in cells using tandem ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12217038/]
- 103. An optimized protocol to detect protein ubiquitination and ... [https://www.sciencedirect.com/science/article/pii/S2666166723001570]
- 104. Selective ubiquitination of drug-like small molecules by the ... [https://www.nature.com/articles/s41467-025-63442-x]
- 105. External Validation of the Predictive Accuracy of Clinical ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11592211/]
- 106. Development and validation of prognostic nomograms for ... [https://www.nature.com/articles/s41598-022-09986-0]
- 107. Drug Development Targeting the Ubiquitin–Proteasome ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7226376/]
- 108. Ubiquitin Proteomics Service [https://www.metwarebio.com/ubiquitin-proteomics-services/]
- 109. Quantitative Proteomic Atlas of Ubiquitination and Acetylation ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4560960/]
- 110. The Emerging Role of Ubiquitin-Specific Protease 36 ( ... [https://www.mdpi.com/2218-273X/14/5/572]
- 111. Gain of chromosome 17 is an early genetic abnormality in ... [https://www.sciencedirect.com/science/article/pii/S0304383525003350]
- 112. Pan-cancer multi-omics profiling reveals ubiquitin D as a ... [https://link.springer.com/article/10.1007/s12672-025-03545-5]
- 113. Label-free quantitative identification of abnormally ... [https://link.springer.com/article/10.1007/s13167-019-00197-8]
- 114. Targeting ubiquitin-specific peptidase 22 (USP22) as a ... [https://pubmed.ncbi.nlm.nih.gov/40847643/]
- 115. The Role of Ubiquitination and Deubiquitination in ... [https://www.mdpi.com/2227-9059/13/12/2873]
- 116. Harnessing Mass Spectrometry for Biomarker Discovery in ... [https://blog.crownbio.com/biomarker-and-mass-spectrometry-aml]
- 117. Exploration of the ubiquitination-related molecular ... [https://www.frontiersin.org/journals/genetics/articles/10.3389/fgene.2024.1292249/full]
- 118. Proteomic signatures improve risk prediction for common ... [https://www.nature.com/articles/s41591-024-03142-z]
- 119. Identification of ubiquitination-related key biomarkers and ... [https://www.nature.com/articles/s41598-025-88148-4]
- 120. Machine learning-based approaches for ubiquitination site prediction in human proteins | BMC Bioinformatics | Full Text [https://bmcbioinformatics.biomedcentral.com/articles/10.1186/s12859-023-05581-w]
- 121. The latest trends in drug discovery [https://www.cas.org/resources/cas-insights/2025-drug-discovery-trends]
- 122. 10-evolved-terms-every-scientist-should-know-about ... [https://resources.nanotempertech.com/blog/10-evolved-terms-every-scientist-should-know-about-targeted-protein-degradation-in-2025]
- 123. Identification of biomarkers based on ubiquitin-correlated ... [https://www.frontiersin.org/journals/pharmacology/articles/10.3389/fphar.2025.1646396/full]