Ubiquitination-Specific Antibodies in Cancer Immunohistochemistry: From Basic Mechanisms to Clinical Prognosis
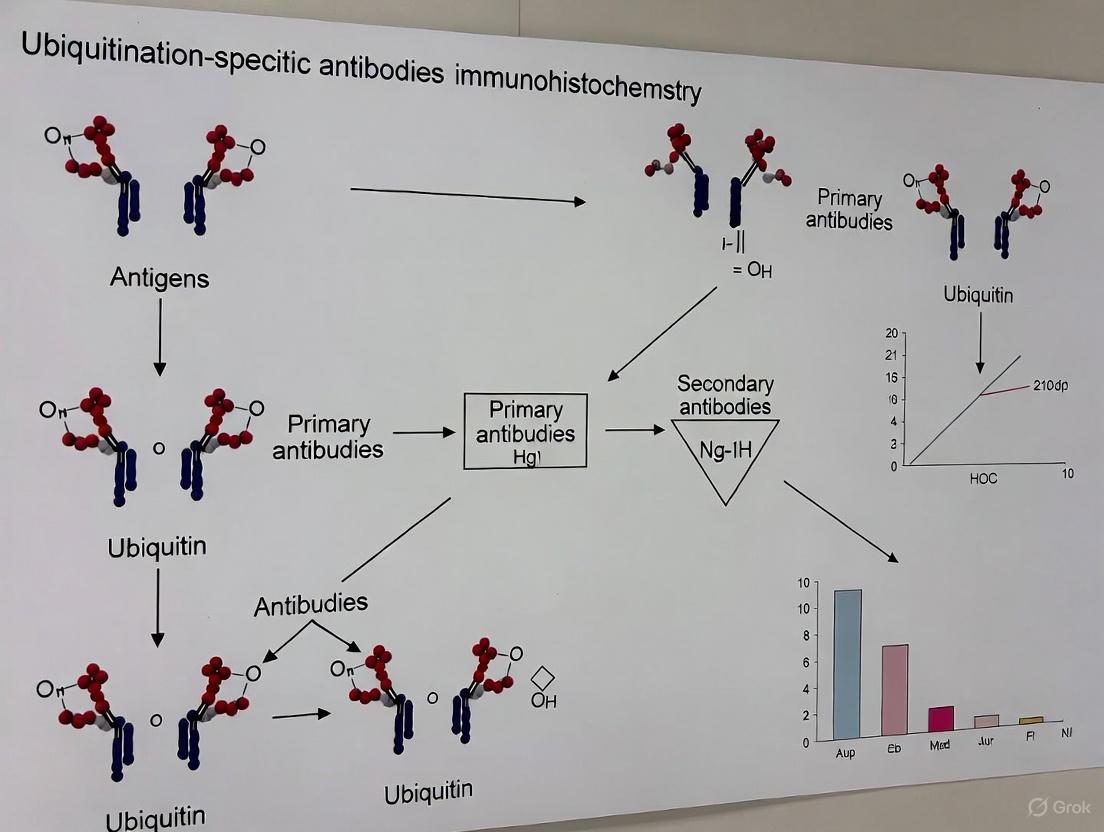
This article provides a comprehensive resource for researchers and drug development professionals on the application of ubiquitination-specific antibodies in cancer immunohistochemistry (IHC).
Ubiquitination-Specific Antibodies in Cancer Immunohistochemistry: From Basic Mechanisms to Clinical Prognosis
Abstract
This article provides a comprehensive resource for researchers and drug development professionals on the application of ubiquitination-specific antibodies in cancer immunohistochemistry (IHC). It explores the foundational role of the ubiquitin-proteasome system (UPS) and deubiquitinating enzymes (DUBs) like USP2 and UBE2C in tumorigenesis, detailing their validated prognostic value in gastric, breast, and prostate cancers. A thorough methodological guide covers antibody selection, protocol optimization, and IHC troubleshooting to ensure assay specificity and reproducibility. Finally, the article emphasizes critical validation strategies, including the use of genetic and pharmacological controls, to confirm antibody specificity for ubiquitination marks, thereby supporting robust biomarker development and precise diagnostic applications in oncology.
The Ubiquitin System in Cancer: Defining Key Targets for Immunohistochemistry
Core Components and Mechanism of the UPS
The Ubiquitin-Proteasome System (UPS) is the primary pathway for targeted intracellular protein degradation in eukaryotic cells, playing crucial roles in maintaining protein homeostasis, regulating cell cycle progression, and controlling signal transduction [1]. This highly conserved system ensures the precise elimination of damaged, misfolded, or short-lived regulatory proteins through an ATP-dependent process [1].
The UPS operates through a coordinated enzymatic cascade that tags target proteins for degradation, followed by their recognition and processing by a large proteolytic complex. The process begins with ubiquitin activation by the E1 enzyme, forming a thioester bond between E1's cysteine residue and ubiquitin's C-terminal glycine, powered by ATP hydrolysis. The activated ubiquitin is then transferred to the ubiquitin-conjugating enzyme (E2). Finally, a ubiquitin ligase (E3) facilitates the transfer of ubiquitin from E2 to a lysine residue on the target protein, forming an isopeptide bond [1]. E3 ligases provide substrate specificity, recognizing particular target proteins through specialized domains [1].
The ubiquitinated protein is then recognized and degraded by the proteasome, a large multi-subunit complex. The 26S proteasome consists of a barrel-shaped 20S core particle (CP) that contains the proteolytic active sites, flanked by one or two 19S regulatory particles (RP) that recognize ubiquitinated proteins, remove the ubiquitin tags, unfold the substrate, and translocate it into the catalytic core for degradation [1] [2]. The degradation products are short peptide fragments that are further broken down into amino acids for reuse in protein synthesis [1].
Table 1: Core Components of the Ubiquitin-Proteasome System
| Component | Function | Key Characteristics |
|---|---|---|
| Ubiquitin | A 76-amino acid protein tag | Highly conserved; covalently attached to target proteins [1] |
| E1 Enzyme | Ubiquitin-activating enzyme | Activates ubiquitin in an ATP-dependent process [1] |
| E2 Enzyme | Ubiquitin-conjugating enzyme | Transfers activated ubiquitin from E1 to E3 [1] |
| E3 Ligase | Ubiquitin ligase | Provides substrate specificity; catalyzes ubiquitin transfer to target protein [1] |
| 26S Proteasome | Proteolytic complex | Degrades ubiquitinated proteins; consists of 20S core and 19S regulatory particles [1] |
| DUBs | Deubiquitinating enzymes | Remove ubiquitin tags; regulate ubiquitin recycling and protein stability [3] |
Diagram 1: The UPS pathway for targeted protein degradation.
Deubiquitinating Enzymes (DUBs): Classification and Functions
Deubiquitinating enzymes (DUBs) constitute a diverse family of proteases that counterbalance ubiquitination by removing ubiquitin moieties from substrate proteins. With approximately 100 members identified in the human genome, DUBs regulate virtually all cellular processes influenced by ubiquitination, including protein stability, subcellular localization, and functional activation [3]. DUBs are categorized into six major families based on their sequence and domain conservation:
- USPs (Ubiquitin-Specific Proteases): The largest family, characterized by broad substrate specificity and diverse cellular functions [3].
- OTUs (Ovarian Tumor Proteases): Known for linkage specificity toward particular ubiquitin chain types [3].
- UCHs (Ubiquitin C-Terminal Hydrolases): Primarily involved in processing ubiquitin precursors and recycling ubiquitin [3].
- MJDs (Machado-Josephin Domain-containing Proteases): Characterized by a catalytic Josephin domain [3].
- MINDYs (Motif-Interacting with Ubiquitin-containing Novel DUB Family): Preferentially cleave lysine-48-linked polyubiquitin chains [3].
- JAMMs (JAB1, MPN, MOV34 Family): Metalloproteases that require zinc for catalytic activity [3].
DUBs perform three primary biological functions: (1) maintaining cellular free ubiquitin levels by processing ubiquitin precursors and recycling ubiquitin from degraded proteins; (2) rescuing substrate proteins from degradation by removing ubiquitin chains before proteasomal recognition; and (3) editing ubiquitin chains to alter signaling outcomes [2]. The balance between ubiquitinating enzymes and DUBs determines the fate, activity, and localization of key regulatory proteins in cancer and other diseases [3].
Table 2: Major DUB Families and Their Characteristics
| DUB Family | Catalytic Type | Key Features | Representative Members |
|---|---|---|---|
| USPs | Cysteine protease | Largest family; diverse functions and substrates | USP9X, USP22, USP34 [3] |
| OTUs | Cysteine protease | Often exhibit linkage specificity | OTUD1 [3] |
| UCHs | Cysteine protease | Process ubiquitin precursors; recycle ubiquitin | BAP1 [3] |
| MJDs | Cysteine protease | Characterized by Josephin domain | Ataxin-3 [3] |
| MINDYs | Cysteine protease | Preferentially cleave K48-linked chains | MINDY1, MINDY2 [3] |
| JAMMs | Zinc metalloprotease | Metal-dependent catalysis | POH1, BRCC36 [3] |
UPS and DUBs in Cancer: Mechanisms and Therapeutic Implications
Dysregulation of the UPS is increasingly recognized as a hallmark of cancer, contributing to tumor initiation, progression, and therapeutic resistance [1]. In multiple myeloma (MM), excessive proteasomal activity is a significant factor in pathogenesis, making proteasome inhibitors like bortezomib, carfilzomib, and ixazomib first-line therapeutic agents [1]. The UPS influences cancer through multiple mechanisms, including regulation of cell cycle controllers, transcription factors, and apoptosis regulators [1].
DUBs have emerged as critical players in oncogenesis, functioning as either tumor promoters or suppressors depending on cellular context [3]. For instance, USP9X demonstrates context-dependent roles in pancreatic ductal adenocarcinoma (PDAC)—promoting tumor cell survival in human pancreatic tumor cells while acting as a suppressor in mouse models [3]. USP28 promotes cell cycle progression and inhibits apoptosis in PDAC cells by stabilizing FOXM1 to activate the Wnt/β-catenin pathway [3]. USP22, identified as a cancer stem cell marker, promotes PDAC cell proliferation by increasing DYRK1A levels [3].
The UPS also plays a crucial role in tumor immune evasion by regulating immune checkpoint proteins such as PD-1/PD-L1 [2]. The E3 ubiquitin ligase SPOP can promote ubiquitination and degradation of PD-L1 in colorectal cancer cells, while competitive binding by ALDH2 or BCLAF1 can inhibit this process, thereby stabilizing PD-L1 and facilitating immune evasion [2]. Small-molecule SGLT2 inhibitors like canagliflozin can disrupt these interactions, promoting SPOP-mediated PD-L1 degradation and enhancing T-cell antitumor activity [2].
DUBs contribute significantly to chemoresistance across various cancers by stabilizing oncogenic proteins, regulating DNA damage repair, and inhibiting apoptosis [4]. In breast cancer, USP22 contributes to chemoresistance, stemness, and epithelial-mesenchymal transition by regulating the Warburg effect through c-Myc deubiquitination [4]. In non-small cell lung cancer, USP35 mediates cisplatin-induced apoptosis by stabilizing BIRC3 [4]. These findings highlight DUBs as promising therapeutic targets to overcome treatment resistance.
Diagram 2: DUB-mediated mechanisms in cancer progression.
Experimental Protocols
In Vitro Ubiquitin Conjugation Assay
The in vitro ubiquitination assay is a fundamental technique for investigating ubiquitination events, enabling researchers to determine if a protein of interest can be ubiquitinated, identify the type of ubiquitination (mono-, poly-, or multi-mono-ubiquitination), characterize chain linkage specificity, and identify the required E2 and E3 enzymes [5].
Table 3: Reaction Components for In Vitro Ubiquitination Assay
| Component | Stock Concentration | Volume for 25 µL Reaction | Final Concentration |
|---|---|---|---|
| 10X E3 Ligase Reaction Buffer | 10X (500 mM HEPES, pH 8.0, 500 mM NaCl, 10 mM TCEP) | 2.5 µL | 1X (50 mM HEPES, 50 mM NaCl, 1 mM TCEP) |
| Ubiquitin | 1.17 mM (10 mg/mL) | 1 µL | ~100 µM |
| MgATP Solution | 100 mM | 2.5 µL | 10 mM |
| Substrate Protein | Variable (user-specific) | X µL | 5-10 µM |
| E1 Enzyme | 5 µM | 0.5 µL | 100 nM |
| E2 Enzyme | 25 µM | 1 µL | 1 µM |
| E3 Ligase | 10 µM | X µL | 1 µM |
| dH₂O | N/A | Variable (to 25 µL total) | N/A |
Procedure:
- Combine all components in a microcentrifuge tube in the order listed in Table 3.
- For a negative control, replace the MgATP Solution with an equivalent volume of dH₂O.
- Incubate in a 37°C water bath for 30-60 minutes.
- Terminate the reaction by either:
- Adding 25 µL of 2X SDS-PAGE sample buffer (if not for downstream applications)
- Adding 0.5 µL of 500 mM EDTA or 1 µL of 1 M DTT (for downstream enzymatic applications)
- Analyze reaction products by SDS-PAGE and Western blot [5].
Analysis:
- Coomassie Staining: Visualizes all protein species; ubiquitination products typically appear as a smear or ladder of bands above the substrate.
- Western Blot with Anti-Ubiquitin Antibody: Confirms the presence of ubiquitin in modified proteins.
- Western Blot with Anti-Substrate Antibody: Verifies that the substrate of interest is ubiquitinated.
- Western Blot with Anti-E3 Ligase Antibody: Distinguishes substrate ubiquitination from E3 autoubiquitination [5].
Ubi-Tagging for Site-Specific Protein Conjugation
Ubi-tagging is a novel modular technique for site-specific protein conjugation that exploits the natural ubiquitination machinery. This method enables efficient generation of homogeneous multimeric conjugation products within 30 minutes, addressing limitations of traditional conjugation strategies such as heterogeneity and long reaction times [6].
The ubi-tagging system requires three key determinants: (1) ubiquitination enzymes specific for the desired lysine linkage type; (2) a donor ubi-tag having a free C-terminal glycine with the conjugating enzyme-specific lysine mutated to arginine to prevent homodimer formation; and (3) an acceptor ubi-tag carrying the corresponding conjugation lysine residue with an unreactive C terminus [6].
Procedure for Generating Fluorescently Labeled Fab' Fragments:
- Prepare the conjugation reaction containing:
- 10 µM Fab-Ub(K48R)don
- 50 µM Rhodamine-Ubacc-ΔGG
- 0.25 µM E1 enzyme
- 20 µM K48-specific E2-E3 fusion protein (gp78RING-Ube2g2)
- Reaction buffer
- Incubate at 37°C for 30 minutes.
- Purify the conjugated product (Rho-Ub2-Fab) using protein G affinity purification.
- Verify conjugation efficiency and product identity by SDS-PAGE and mass spectrometry [6].
This technology enables various applications including bispecific T-cell engagers and nanobody-antigen conjugates with superior efficiency compared to traditional methods like sortase-mediated tagging, particularly for hydrophobic, poorly soluble peptides [6].
Research Reagent Solutions
Table 4: Essential Research Reagents for UPS and DUB Studies
| Reagent Category | Specific Example | Application | Key Features |
|---|---|---|---|
| Linkage-Specific Ubiquitin Antibodies | Anti-Ubiquitin (linkage-specific K27) [EPR17034] [7] | WB, IHC-P, ICC/IF, Flow Cyt (Intra) | Rabbit recombinant monoclonal; specific for K27-linked ubiquitin chains |
| General Ubiquitin Antibodies | Ubiquitin Polyclonal Antibody (10201-2-AP) [8] | WB, IHC, IF/ICC, FC (Intra), CoIP, ELISA | Rabbit polyclonal; reacts with human, mouse, rat; detects ubiquitin monomers and conjugates |
| Recombinant Enzymes | E1, E2, E3 enzymes [5] | In vitro ubiquitination assays | Essential components for reconstituting ubiquitination cascade |
| Ubiquitin Variants | K48R mutant, ΔGG mutant [6] | Ubi-tagging conjugation | Engineered ubiquitin for controlled conjugation |
| Proteasome Inhibitors | Bortezomib, Carfilzomib [1] | Functional UPS studies | FDA-approved for multiple myeloma; research tools |
| DUB Inhibitors | Small-molecule DUB inhibitors [4] | Mechanistic and therapeutic studies | Emerging class targeting specific DUB families |
Concluding Remarks
The Ubiquitin-Proteasome System and Deubiquitinating Enzymes represent sophisticated regulatory networks essential for cellular homeostasis, with profound implications for cancer biology and therapy. The development of targeted inhibitors against specific UPS components and DUBs holds significant promise for advancing cancer treatment, particularly in combination with existing modalities like chemotherapy and immunotherapy. Continued research into the intricate mechanisms of ubiquitination and deubiquitination will undoubtedly yield novel insights and therapeutic strategies for cancer and other diseases characterized by proteostasis imbalance.
Ubiquitin-Specific Proteases (USPs) as Key Regulators in Cancer Signaling Pathways
Ubiquitin-specific proteases (USPs) represent the largest subfamily of deubiquitinating enzymes (DUBs), functioning as critical regulators of protein stability and function through their ability to remove ubiquitin moieties from target proteins. This post-translational modification directly influences protein degradation, localization, and activity, thereby controlling essential cellular processes. In cancer biology, USPs have emerged as pivotal players in tumor initiation, progression, and therapeutic resistance through their regulation of key oncogenic and tumor-suppressive pathways. The context-dependent expression and activity of various USPs across cancer types highlight their significance as potential diagnostic biomarkers and therapeutic targets in oncology.
Recent advances in cancer research have illuminated the complex regulatory networks governed by USP family members, revealing their profound impact on critical cancer hallmarks including sustained proliferation, evasion of growth suppressors, resistance to cell death, and activation of metastasis. The development of targeted therapies against specific USPs represents a promising frontier in precision oncology, with numerous investigational compounds currently under preclinical and clinical evaluation.
USP Family Members and Their Cancer-Related Functions
Key USP Family Members in Oncogenesis
USP7 (HAUSP) has emerged as a critical regulator in multiple cancer types, including breast, ovarian, prostate, cervical, and colorectal cancers [9]. USP7 demonstrates a dual role in oncogenesis through its regulation of the p53-MDM2 axis. By deubiquitinating and stabilizing MDM2, the primary negative regulator of p53, USP7 indirectly suppresses p53-mediated tumor suppression [9]. This mechanism enables cancer cells to bypass critical cell cycle checkpoints and apoptosis mechanisms. USP7 also stabilizes other oncogenic proteins like HIF-1α, further promoting tumor progression and therapy resistance. The enzyme's overexpression has been particularly implicated in cancers with aberrant RAS/RAF/MEK/ERK signaling, highlighting its importance in these aggressive tumor subtypes [9].
USP21 demonstrates significant oncogenic potential across multiple cancer types. Research has established that USP21 promotes pancreatic ductal adenocarcinoma (PDAC) growth by activating mTOR signaling through binding to MAPK3 and inducing micropinocytosis to support amino acid sustainability [3]. Additionally, USP21 maintains cancer stem cell properties in PDAC by stabilizing TCF7, a key transcription factor in the Wnt pathway [3]. In orthotopic pancreatic transplantation models, USP21 expression drives pathological progression from pancreatic intraepithelial neoplasia (PanIN) to fully developed PDAC, underscoring its role in tumor initiation [3]. Beyond pancreatic cancer, USP21 overexpression is observed in hepatocellular carcinoma and non-small cell lung cancer, where it stabilizes oncoproteins like NF-κB and β-catenin to drive tumor proliferation and metastasis [10].
USP38 exhibits context-dependent roles in cancer progression, functioning as either an oncogene or tumor suppressor depending on the tissue type [11]. In lung adenocarcinoma, gastric cancer, and esophageal squamous cell carcinoma, USP38 is significantly overexpressed, with high expression levels correlating with lymph node metastasis, advanced TNM staging, and poor prognosis [11]. Mechanistically, USP38 regulates the stability of key proteins including HDAC1/3, LSD1, KLF5, METTL14, c-Myc, and HIF-1α, thereby influencing critical signaling pathways such as JAK2/STAT3 [11]. Conversely, in colorectal cancer and clear cell renal carcinoma, USP38 expression is significantly reduced and appears to function as a tumor suppressor [11], highlighting the tissue-specific nature of USP regulation.
USP28 promotes cell cycle progression and inhibits apoptosis in pancreatic ductal adenocarcinoma by stabilizing FOXM1, a key proliferation-associated transcription factor, thereby activating the Wnt/β-catenin pathway [3]. Similarly, USP5 accelerates PDAC tumor growth by prolonging the half-life of FOXM1 and regulates DNA damage response, cell cycle arrest, and apoptosis to promote tumor formation [3].
USP9X demonstrates particularly complex, context-dependent functions in pancreatic cancer. In human pancreatic tumor cells, USP9X promotes tumor cell survival and malignant phenotypes, while in KPC (KrasLSL-G12D/+; Trp53LSL-R172H/+; Pdx1-Cre) mouse models, it acts as a tumor suppressor [3]. As a suppressor, USP9X regulates the Hippo pathway through cooperation with LATS kinase and YAP/TAZ to impede PDAC growth [3]. Sleeping Beauty transposon-mediated insertional mutagenesis screens revealed that USP9X has the highest mutation frequency in PDAC, observed in at least 50% of tumors [3].
Table 1: USP Family Members and Their Roles in Cancer
| USP Member | Cancer Types Involved | Key Substrates | Biological Functions |
|---|---|---|---|
| USP7 | Colorectal, Breast, Ovarian, Prostate, Cervical | MDM2, HIF-1α, p53 | Regulates p53-MDM2 axis, stabilizes oncoproteins, promotes therapy resistance |
| USP21 | Pancreatic, Hepatocellular, Non-small cell lung | β-catenin, TCF7, MAPK3 | Promotes cancer stemness, activates mTOR signaling, enhances micropinocytosis |
| USP38 | Lung adenocarcinoma, Gastric, Esophageal, Colorectal | HDAC1/3, LSD1, KLF5, c-Myc | Context-dependent oncogene/tumor suppressor, regulates JAK2/STAT3 pathway |
| USP28 | Pancreatic ductal adenocarcinoma | FOXM1 | Activates Wnt/β-catenin pathway, promotes cell cycle progression |
| USP5 | Pancreatic ductal adenocarcinoma | FOXM1 | Regulates DNA damage response, promotes tumor growth |
| USP9X | Pancreatic ductal adenocarcinoma | LATS kinase, YAP/TAZ | Context-dependent roles, regulates Hippo pathway |
| USP22 | Pancreatic, Breast | PTEN, DYRK1A | Cancer stem cell marker, regulates PTEN-MDM2-p53 signaling |
| USP33 | Pancreatic, Hepatocellular, Lung | Various metastasis regulators | Influences malignant phenotype and metastatic progression |
| USP34 | Pancreatic ductal adenocarcinoma | AKT, PKC pathways | Facilitates cancer cell survival through AKT and PKC signaling |
USP Regulation of Key Signaling Pathways in Cancer
USPs regulate multiple critical signaling pathways that drive cancer progression. The Wnt/β-catenin pathway is frequently modulated by USPs including USP28, USP21, and USP5, which stabilize key components such as TCF7 and FOXM1 to promote tumor proliferation and stemness [3]. The p53 pathway is primarily regulated through USP7-mediated stabilization of MDM2, leading to subsequent p53 degradation and impaired tumor suppression [9]. The mTOR signaling pathway is activated by USP21 through MAPK3 stabilization, enhancing nutrient acquisition and metabolic adaptation in pancreatic cancer [3] [10]. Additionally, the JAK2/STAT3 pathway is influenced by USP38 through stabilization of various transcription factors and epigenetic regulators [11].
Table 2: USP-Regulated Signaling Pathways in Cancer
| Signaling Pathway | Regulating USPs | Molecular Mechanisms | Cancer Outcomes |
|---|---|---|---|
| Wnt/β-catenin | USP28, USP21, USP5 | Stabilization of TCF7, FOXM1 | Enhanced proliferation, stemness, cell cycle progression |
| p53 Tumor Suppressor | USP7 | Stabilization of MDM2, leading to p53 degradation | Evasion of apoptosis, genomic instability, chemoresistance |
| mTOR Signaling | USP21 | Stabilization of MAPK3, induction of micropinocytosis | Metabolic reprogramming, nutrient acquisition, growth |
| JAK2/STAT3 | USP38 | Regulation of HDAC1/3, LSD1, KLF5, c-Myc | Proliferation, survival, inflammation, immune evasion |
| Hippo Pathway | USP9X | Regulation of LATS kinase and YAP/TAZ | Context-dependent tumor promotion or suppression |
| PI3K/Akt | USP34 | Activation of AKT and PKC pathways | Cell survival, growth, metabolism |
| PD-1/PD-L1 Immune Checkpoint | Various USPs | Regulation of PD-L1 stability through ubiquitin machinery | Immune evasion, immunotherapy resistance |
Experimental Protocols for USP Research
Immunohistochemistry Protocols for USP Detection
Immunohistochemistry (IHC) provides a powerful technique for detecting USP expression and localization in tissue samples, offering insights into their potential as diagnostic and prognostic biomarkers in cancer.
Sample Preparation: For frozen tissue sections, dissect tissue of interest (<10 mm) and place in a pre-labeled tissue mold. Cover the tissue sample in cryo-embedding media (OCT) and freeze the tissue block by slowly submerging in liquid nitrogen or placing on dry ice. Store frozen tissue blocks at -80°C until sectioning. Section the tissue block into 6-15 μm thick sections using a cryostat set at -20°C and transfer sections onto positively charged glass slides. Fix sections in ice-cold acetone for 10 minutes, then wash slides in PBS twice for 5 minutes each [12].
For formalin-fixed paraffin-embedded (FFPE) sections, following tissue fixation, rinse the tissue in PBS and dehydrate through a series of ethanol solutions (50%, 70%, 80%, 95%, 100%) for 30 minutes each. Clear tissue in three changes of xylene for 20 minutes each, then infiltrate with paraffin through three changes of 60°C paraffin for 1 hour each. Embed in paraffin blocks, section into 5-15 μm slices, and transfer to silanized or gel-coated slides. For immunostaining, deparaffinize slides in xylene and rehydrate through a descending ethanol series [12].
Antigen Retrieval: For heat-induced epitope retrieval (HIER), boil slides in 10 mM sodium citrate buffer (pH 6.0), 1 mM EDTA (pH 8.0), or 10 mM Tris/1 mM EDTA (pH 9.0) for 15-20 minutes at approximately 98°C using a pressure cooker, microwave, or steamer. Cool slides completely before proceeding with immunostaining. For protease-induced epitope retrieval (PIER), incubate sections with protease solution (e.g., 0.05% trypsin in 0.1% calcium chloride or 0.5% pepsin in 10mM HCl) at 37°C for 10 minutes in a humidity chamber [12].
Antibody Staining and Detection: For fluorescence-based detection, block non-specific binding by incubating with blocking buffer for 1 hour at room temperature. Incubate tissue sections with primary antibody diluted in blocking buffer overnight at 4°C. Wash sections three times with wash buffer (TBS or PBS plus 0.025% Triton X-100), then incubate with fluorescently conjugated secondary antibody (typically 1:500-1:1000 dilution) for 1-2 hours at room temperature. After washing, counterstain with DAPI (0.5 μg/mL) for 5 minutes, then mount with anti-fade mounting medium [12].
For chromogenic detection, after primary antibody incubation and washing, incubate samples with 0.3% hydrogen peroxide in TBS for 15 minutes to block endogenous peroxidase activity. Incubate with biotinylated secondary antibody for 1 hour at room temperature, then with ABC reagent for 30 minutes. Develop with DAB substrate for approximately 10 minutes, counterstain with hematoxylin, and mount with appropriate mounting medium [12].
Computational Approaches for USP Inhibitor Discovery
Virtual Screening and QSAR Modeling: Robust quantitative structure-activity relationship (QSAR) models can be developed using curated USP inhibitors, molecular fingerprint descriptors, and random forest algorithms. For USP7 inhibitor identification, models have been developed using 837 curated inhibitors, achieving high predictive accuracy (R² = 0.96 ± 0.01, Q² = 0.92 ± 0.02) [9]. Virtual screening identifies high-potential compounds from natural product and chemical databases including NPASS, TCM, and ZINC [9] [10].
Molecular Docking and Dynamics: Molecular docking studies assess binding interactions between potential inhibitors and USPs. For USP7, the catalytic domain (PDB ID: 5UQV) serves as the target structure, with docking validation achieved by redocking the co-crystallized ligand GNE6640 (RMSD = 0.330 Å) [9]. Top hits are evaluated via molecular docking, revealing strong interactions with key residues including Asp163, His217, Arg115, and Gln111 in USP7 [9]. Molecular dynamics simulations (200-500 ns) demonstrate compound stability and binding interactions over time [9] [10]. For USP21 inhibitors, molecular dynamics simulations for 500 ns analyze conformational flexibility and stability of USP21-phytoconstituent complexes [10].
ADMET Profiling: Compounds with promising binding affinities undergo ADMET (absorption, distribution, metabolism, excretion, and toxicity) prediction using computational tools to assess drug-likeness. PAINS (pan-assay interference compounds) analysis removes compounds prone to non-specific binding, ensuring selectivity for the target USP [10].
Visualization of USP Signaling Networks
USP Regulation of Cancer Signaling Pathways
Therapeutic Applications and Research Tools
USP-Targeted Therapeutic Strategies
The development of USP inhibitors represents a promising therapeutic strategy in oncology, with several approaches showing significant preclinical potential. For USP7, integrative computational approaches have identified promising inhibitor candidates including NPC472846, TCM11676, TCM36723, ZINC18193314, and ZINC65536649, which demonstrate strong binding interactions and high stability in molecular dynamics simulations [9]. Molecular dynamics simulations (200 ns) revealed that TCM36723 and ZINC65536649 exhibit the highest dynamic stability, while NPC472846 induces well-maintained conformational states [9]. MM-GBSA free energy calculations identified NPC472846 as the top binder (-45.7 kcal/mol), followed by ZINC65536649 (-40.4 kcal/mol) and TCM11676 (-39.9 kcal/mol), all outperforming the reference ligand GNE6640 (-31.6 kcal/mol) [9].
For USP21, bioactive phytoconstituents have emerged as promising inhibitor candidates. Virtual screening of the IMPPAT 2.0 database of Indian medicinal plants identified Ranmogenin A and Tokorogenin as potential USP21 inhibitors [10]. These compounds form stable protein-ligand complexes with USP21 throughout 500 ns molecular dynamics simulations and exhibit favorable pharmacokinetic properties with moderate predicted anticancer activity based on PASS analysis [10].
Combination therapies represent another promising approach, particularly for overcoming resistance to existing treatments. For instance, targeting the ubiquitin machinery in combination with PD-1/PD-L1 immune checkpoint inhibitors may enhance therapeutic efficacy by modulating PD-L1 expression levels [13]. Similarly, USP inhibition may sensitize cancer cells to conventional chemotherapy and targeted therapies by disrupting protective mechanisms.
The Scientist's Toolkit: Essential Research Reagents
Table 3: Essential Research Reagents for USP Studies
| Reagent/Category | Specific Examples | Research Applications | Technical Considerations |
|---|---|---|---|
| Antibodies | Anti-USP7, Anti-USP21, Anti-USP38 | Immunohistochemistry, Western blotting, Immunoprecipitation | Validation of specificity using knockout controls is essential |
| Cell Lines | Cancer cell lines with USP overexpression/knockdown | Functional assays, Drug screening | Include multiple cell lines representing different cancer types |
| Chemical Inhibitors | USP7 inhibitors (e.g., GNE6640), Natural product derivatives | Mechanism studies, Combination therapy screening | Monitor selectivity and potential off-target effects |
| Expression Vectors | USP overexpression constructs, CRISPR-Cas9 systems | Gain/loss-of-function studies, Structural studies | Use inducible systems for studying essential USPs |
| Computational Tools | Molecular docking software, QSAR models, MD simulation platforms | Virtual screening, Binding mode analysis, Dynamics studies | Validate computational predictions with experimental data |
| Animal Models | Xenograft models, Genetically engineered mouse models | Preclinical efficacy evaluation, Toxicity assessment | Consider species differences in USP expression and function |
Ubiquitin-specific proteases represent master regulators of cancer signaling pathways, with individual USPs demonstrating specialized functions in specific cancer types and contexts. The complex regulatory networks governed by USPs highlight their significance as potential diagnostic biomarkers and therapeutic targets in oncology. Future research directions should focus on elucidating the context-dependent functions of USPs, developing highly selective inhibitors with favorable pharmacological properties, and exploring combination therapies that leverage USP inhibition to enhance existing treatment modalities. As our understanding of USP biology continues to expand, these enzymes will undoubtedly remain at the forefront of cancer research and therapeutic development.
The ubiquitin-proteasome system (UPS) is a critical regulator of cellular protein homeostasis, and its dysregulation is a hallmark of cancer. Ubiquitin-specific proteases (USPs), the largest subfamily of deubiquitinating enzymes, play multifaceted roles in tumorigenesis and cancer progression by stabilizing oncoproteins or tumor suppressors. This application note synthesizes recent evidence on the roles of specific USPs in gastric, breast, and biliary tract cancers, highlighting their clinical relevance, molecular mechanisms, and potential as therapeutic targets. We provide detailed experimental protocols for investigating USP functions and a curated list of essential research reagents to facilitate cancer research and drug development in this emerging field.
Protein ubiquitination is a reversible post-translational modification that regulates virtually all cellular processes, including cell cycle progression, DNA damage repair, and apoptosis [14]. The ubiquitin-proteasome system (UPS) maintains protein homeostasis through a coordinated enzymatic cascade involving E1 activating, E2 conjugating, and E3 ligase enzymes, which can be reversed by deubiquitinating enzymes (DUBs) [15] [14]. Ubiquitin-specific proteases (USPs) constitute the largest DUB subfamily and are increasingly recognized as critical regulators in cancer pathogenesis, functioning as either oncogenes or tumor suppressors depending on cellular context [15].
This application note examines the roles of specific USPs in three cancer types—gastric, breast, and biliary tract cancers—framed within the context of ubiquitination-specific antibodies and immunohistochemistry cancer research. We summarize quantitative clinical data, describe molecular mechanisms with visual pathway diagrams, and provide detailed experimental protocols to support research and therapeutic development in this rapidly advancing field.
USP Roles in Gastric Cancer
Gastric cancer (GC) remains a leading cause of cancer-related mortality worldwide, underscoring the need for novel therapeutic targets [16] [17]. Multiple USPs have been identified as key players in GC progression, metastasis, and treatment response.
Oncogenic USPs in Gastric Cancer
Table 1: Oncogenic USPs in Gastric Cancer and Their Clinical Significance
| USP | Expression in GC | Clinical Correlation | Target/Pathway | Functional Outcome |
|---|---|---|---|---|
| USP15 | Upregulated [16] | Positive correlation with tumor size, depth of invasion, lymph node involvement, TNM stage, perineural and vascular invasion; poor prognosis [16] | Wnt/β-catenin pathway [16] | Promotes cell proliferation, invasion, EMT, and tumor growth [16] |
| USP14 | Upregulated [17] | Associated with unfavorable prognosis; enriched at invasive tumor edge [17] | KPNA2/c-MYC nuclear translocation [17] | Promotes proliferation, migration, and invasion [17] |
| USP35 | Upregulated [18] | Associated with nodal metastasis, higher tumor grade, and poor prognosis; induced by H. pylori infection [18] | Snail1 deubiquitination and stabilization [18] | Promotes EMT, invasion, metastasis, and lung colonization [18] |
Tumor-Suppressive USP in Gastric Cancer
Table 2: Tumor-Suppressive USP in Gastric Cancer
| USP | Expression in GC | Clinical Correlation | Target/Pathway | Functional Outcome |
|---|---|---|---|---|
| USP2 | Significantly reduced [19] | Low expression associated with genetic variations, neoantigen loads, MSI scores, and immune cell infiltration [19] | Focal adhesion and ECM receptor interaction pathways [19] | Suppresses proliferation, migration; enhances apoptosis; correlates with drug sensitivity [19] |
Diagram 1: USP Signaling Network in Gastric Cancer. This diagram illustrates the molecular mechanisms of oncogenic (yellow) and tumor-suppressive (green) USPs in gastric cancer, highlighting their subcellular localization and functional outcomes.
USP Roles in Breast Cancer
Breast cancer is the most prevalent malignancy in women worldwide, with USPs emerging as key regulators of its immune microenvironment and therapeutic response [20] [21].
USP-Mediated Regulation of Breast Cancer Progression
Table 3: Key USPs in Breast Cancer and Their Functions
| USP | Role in Breast Cancer | Molecular Mechanism | Therapeutic Implication |
|---|---|---|---|
| USP36 | Oncogenic [21] | Deubiquitinates and stabilizes ERα; enhances estrogen signaling [21] | Promotes tamoxifen resistance; combined USP36 inhibition + tamoxifen potential therapy [21] |
| USP7 | Oncogenic [20] | Stabilizes Foxp3 in Tregs; enhances immunosuppressive function [20] | Contributes to immune evasion; potential target for immunotherapy [20] |
| USP1 | Regulatory [20] | Promotes proteasomal degradation of Foxp3 [20] | Modulates Treg differentiation and function [20] |
| USP12 | Regulatory [20] | Activates CD4+ T-cell responses [20] | Potential role in antitumor immunity [20] |
USP Roles in Biliary Tract Cancer
Biliary tract carcinoma (BTC) encompasses a group of highly heterogeneous malignancies with dismal five-year survival rates of less than 20% [15] [22]. USP dysregulation represents a key molecular event in BTC pathogenesis.
USP-Driven Mechanisms in Biliary Tract Cancer
Table 4: USP Functions in Biliary Tract Cancer
| USP | Expression in BTC | Molecular Target | Functional Role in BTC |
|---|---|---|---|
| USP1 | Upregulated [22] | PARP1 deubiquitination and stabilization [22] | Promotes growth and metastasis; regulated by GCN5-mediated acetylation [22] |
| Multiple USPs (USP1, USP3, USP7, USP8, USP9X, USP21, USP22) | Differential expression profiles [15] | Regulation of key oncoproteins (PTEN, c-Myc) and signaling pathways (Wnt/β-catenin, PI3K/AKT, MAPK) [15] | Promote proliferation, apoptosis evasion, invasion, and metastasis [15] |
Diagram 2: USP Mechanisms in Breast and Biliary Tract Cancers. This diagram illustrates cell-type-specific USP functions, highlighting their roles in therapeutic resistance and cancer progression.
Experimental Protocols for USP Research
Protocol: Immunohistochemical Analysis of USP Expression in Cancer Tissues
Purpose: To evaluate USP protein expression and localization in formalin-fixed paraffin-embedded (FFPE) cancer tissues and correlate with clinicopathological characteristics.
Materials:
- FFPE tissue sections (4-5 μm thickness)
- Specific primary antibodies against USPs (e.g., anti-USP15, anti-USP14)
- Antigen retrieval solution (citrate buffer, pH 6.0)
- Hydrogen peroxide block
- Blocking serum
- Biotinylated secondary antibody
- Streptavidin-HRP conjugate
- DAB chromogen substrate
- Hematoxylin counterstain
Procedure:
- Deparaffinize sections in xylene and rehydrate through graded ethanol series.
- Perform antigen retrieval by heating slides in citrate buffer (pH 6.0) for 20 minutes.
- Block endogenous peroxidase activity with 3% hydrogen peroxide for 10 minutes.
- Incubate with blocking serum for 1 hour at room temperature.
- Apply primary antibody diluted in blocking buffer overnight at 4°C.
- Incubate with biotinylated secondary antibody for 1 hour at room temperature.
- Apply streptavidin-HRP conjugate for 30 minutes.
- Develop with DAB chromogen for 5-10 minutes.
- Counterstain with hematoxylin, dehydrate, and mount.
Scoring Method: Evaluate staining based on intensity (0-3) and percentage of positive cells (0-100%). Multiply intensity × percentage to generate a final score [16] [19].
Protocol: Co-immunoprecipitation (Co-IP) for USP-Substrate Interaction
Purpose: To validate physical interactions between USPs and their substrate proteins.
Materials:
- Cell lysates (RIPA buffer with protease inhibitors)
- Primary antibodies against target USP and substrate
- Protein A/G agarose beads
- Normal IgG control
- Western blotting equipment and reagents
Procedure:
- Pre-clear 500 μg protein lysate with 20 μL Protein A/G agarose and normal IgG for 2 hours at 4°C.
- Incubate pre-cleared lysate with specific antibody for 4 hours at 4°C.
- Add Protein A/G beads and incubate overnight at 4°C with gentle rotation.
- Wash beads 3-4 times with lysis buffer.
- Elute bound proteins by boiling in 2× SDS sample buffer.
- Analyze by Western blotting with appropriate antibodies [21] [22].
Protocol: Deubiquitination Assay
Purpose: To demonstrate USP-mediated removal of ubiquitin chains from substrate proteins.
Materials:
- Plasmid constructs for USP, substrate, and ubiquitin
- Proteasome inhibitor (MG132)
- Ubiquitin mutants (K48-only, K63-only, K0)
- Co-IP reagents
- Western blotting equipment
Procedure:
- Co-transfect cells with USP, substrate, and ubiquitin expression vectors.
- Treat cells with 10 μM MG132 for 6 hours before harvesting to prevent substrate degradation.
- Lyse cells and perform immunoprecipitation of the substrate.
- Analyze ubiquitination levels by Western blotting with anti-ubiquitin antibody.
- Compare ubiquitination levels in presence of wild-type USP versus catalytically inactive mutant [22] [18].
Protocol: Functional Assays for USP Role in Cancer
Cell Proliferation Assay:
- Seed GC cells (2,000 cells/well) in 96-well plates.
- Assess viability at 24, 48, 72, and 96 hours using CCK-8 reagent.
- Measure absorbance at 450 nm [16] [19].
Migration and Invasion Assays:
- For migration: Seed 5 × 10^4 cells in serum-free medium into transwell upper chamber.
- For invasion: Coat membrane with Matrigel before seeding cells.
- Fill lower chamber with medium containing 10% FBS as chemoattractant.
- Incubate for 24-48 hours, then fix, stain, and count migrated/invaded cells [16] [17] [19].
In Vivo Tumorigenesis Assay:
- Subcutaneously inject 5 × 10^6 GC cells into nude mice.
- Measure tumor volume weekly using calipers.
- Harvest tumors after 4-6 weeks for weight measurement and IHC analysis [17].
The Scientist's Toolkit: Essential Research Reagents
Table 5: Key Research Reagents for USP Investigation in Cancer
| Reagent Category | Specific Examples | Research Application | Key Features |
|---|---|---|---|
| USP Inhibitors | IU1 (USP14 inhibitor) [17] | Functional validation of USP roles | Specific binding to activated USP14; inhibits catalytic activity |
| Small-molecule USP inhibitors and PROTACs [15] | Therapeutic development | Targeted degradation of specific USPs | |
| Antibodies | Anti-USP15 (#66310; Cell Signaling Technology) [16] | IHC, Western blot, IP | Validated for immunohistochemistry (1:100 dilution) |
| Antibodies for USPs, KPNA2, PARP1, Snail1, ERα [17] [21] [22] | Various applications | Target-specific detection in multiple techniques | |
| Expression Vectors | HA-tagged, Flag-tagged, Myc-tagged USP constructs [21] [22] [18] | Gain-of-function studies | Enable overexpression and tracking of USPs |
| Catalytically inactive mutants (e.g., USP15 C269S, USP36 C131A, USP35 C450A) [16] [21] [18] | Mechanism studies | Control for enzyme activity-dependent effects | |
| Ubiquitin Tools | HA-Ub, HA-K48, HA-K63, HA-K48R mutants [21] [18] | Ubiquitination assays | Determine linkage-specific deubiquitination |
| ΔGG ubiquitin mutant [14] | Negative controls | Cannot be conjugated to substrates | |
| Cell Lines | GC: HGC-27, SGC-7901, MKN-45 [16] [17] | In vitro models | Represent different GC subtypes |
| Breast cancer: MCF-7, T47D [21] | Hormone-responsive models | ER-positive breast cancer models | |
| BTC: HuCC-T1, HCCC-9810, RBE [22] | Cholangiocarcinoma models | For BTC-specific mechanisms |
USPs represent promising therapeutic targets and prognostic biomarkers in gastric, breast, and biliary tract cancers. The experimental protocols and research tools outlined in this application note provide a foundation for investigating USP functions in cancer pathogenesis and developing targeted therapies. Future research should focus on developing more specific USP inhibitors, understanding USP interactions within complex signaling networks, and exploring combination therapies that leverage USP modulation to overcome treatment resistance.
Ubiquitination is a critical post-translational modification that regulates protein degradation and function, playing a fundamental role in cellular homeostasis. The ubiquitin-proteasome system (UPS) has emerged as a significant player in cancer pathogenesis, with specific components serving as potential diagnostic and prognostic biomarkers. Among these, ubiquitin-conjugating enzyme E2 C (UBE2C) has been extensively validated as a prognostic marker in multiple malignancies, particularly breast and gastric cancers. This application note synthesizes current research on UBE2C, providing structured experimental data, validated protocols, and molecular pathways to facilitate its application in cancer research and drug development.
UBE2C as a Prognostic Marker: Quantitative Evidence
Prognostic Significance in Breast Cancer
Table 1: UBE2C as a Prognostic Marker in Breast Cancer
| Cohort/Study | Sample Size | Detection Method | Key Prognostic Findings | Statistical Significance |
|---|---|---|---|---|
| Node-positive BC [23] | 92 | IHC | Significant impact on MFS and OS | HR=6.79, P=0.002 (MFS); HR=7.14, P=0.009 (OS) |
| Validation Cohort [24] | 121 | IHC, RT-qPCR | High UBE2C = poor prognosis; Predictive model with TN staging & Ki-67 | AUC=0.870 (95% CI: 0.786-0.953) |
| METABRIC [25] | 1,980 | mRNA expression | Correlated with poor prognosis features | Association with LVI: P=0.002 |
| TCGA [25] | 854 | mRNA expression | Correlated with poor prognosis features | Association with LVI: P<0.001 |
| IHC Cohort [25] | 619 | IHC | Independent prognostic predictor | P=0.011, HR=1.45 (95% CI: 1.10-1.93) |
| Multicenter Study [26] | 209 | IHC | Positive expression in 70.8% of tumors; Correlated with aggressive features | Correlated with tumor size, grade, stage (all P<0.05) |
Prognostic Significance in Gastric Cancer
Table 2: UBE2C as a Prognostic Marker in Gastric Cancer
| Study | Sample Size | Cancer Type | Detection Method | Key Findings | Statistical Significance |
|---|---|---|---|---|---|
| Multi-center [27] | 1,759 | Intestinal-type GC | IHC | Overexpression predicts poor outcome | P<0.05 |
| Multi-center [27] | 6 cell lines | Intestinal-type GC | Copy Number Analysis | CNV gain in 4/5 intestinal-type lines | No CNV in diffuse-type lines |
| Functional Study [27] | In vitro/in vivo | Intestinal-type GC | Functional assays | Knockdown inhibits proliferation, migration, invasion | P<0.05 |
UBE2C in Cancer Biology: Molecular Mechanisms
UBE2C, also known as UBCH10, is a member of the ubiquitin-conjugating enzyme (E2) family and plays a crucial role in the ubiquitin-proteasome system. It is encoded by the UBE2C gene located at chromosome 20q13.12 and consists of 179 amino acids with a molecular weight of approximately 20 kDa [28]. UBE2C interacts with the anaphase-promoting complex/cyclosome (APC/C) E3 ubiquitin ligase to regulate the degradation of key mitotic proteins, including securin and cyclin B, facilitating the metaphase-to-anaphase transition and mitotic exit [28].
In cancer, UBE2C overexpression leads to chromosomal instability, missegregation, and aneuploidy, promoting tumorigenesis and progression [28]. The enzyme's expression is tightly regulated throughout the cell cycle, accumulating during S and G2 phases and degrading after mitosis via auto-ubiquitination [28].
Diagram 1: UBE2C in Cell Cycle Regulation and Cancer Pathogenesis. This diagram illustrates the central role of UBE2C in regulating key cell cycle transitions through the targeted degradation of cyclins and securin, ultimately contributing to genomic instability and cancer progression when dysregulated.
Signaling Pathways Regulated by UBE2C
Breast Cancer Pathways
In breast cancer, UBE2C expression correlates with aggressive tumor behavior through multiple signaling pathways. High UBE2C expression is associated with activation of the AKT/mTOR signaling pathway, promoting cell proliferation [28]. Additionally, UBE2C downregulates the tumor suppressor Numb, enhancing breast cancer malignancy [29]. The correlation between UBE2C and adhesion molecules (E-cadherin and N-cadherin) suggests its involvement in epithelial-mesenchymal transition, a key process in cancer metastasis [25].
Gastric Cancer Pathways
In intestinal-type gastric cancer, UBE2C overexpression activates the ERK signaling pathway, promoting cancer cell proliferation [27]. Inhibition of UBE2C results in G2/M cell cycle arrest and reduces levels of phosphorylated AURKA through the Wnt/β-catenin and PI3K/Akt signaling pathways, subsequently inhibiting gastric cancer development and progression [28].
Diagram 2: UBE2C-Activated Signaling Pathways in Breast and Gastric Cancers. This diagram summarizes the major signaling pathways regulated by UBE2C across different cancer types, highlighting the diverse mechanisms through which it promotes oncogenesis.
Experimental Protocols & Methodologies
Immunohistochemistry Protocol for UBE2C Detection
Sample Preparation:
- Collect 3-4μm thick sections from formalin-fixed, paraffin-embedded tumor tissues
- Mount on Superfrost Plus slides for better adhesion
- Deparaffinize in xylene and rehydrate through graded alcohol series
Antigen Retrieval:
- Use citrate buffer (pH 6.0) for UBE2C antigen retrieval
- Steam samples for 20-30 minutes before incubation
- Block endogenous peroxidase activity with 3% hydrogen peroxide in methanol
Antibody Incubation and Detection:
- Incubate with primary UBE2C antibody overnight at 4°C
- Recommended antibodies: Boston Biochem (dilution 1:500) [23] or Anti-UBE2C Mouse Monoclonal Antibody (1:100 dilution) [24]
- Use biotin-streptavidin-peroxidase detection system (Kit ChemMate, Dako)
- Visualize with 3,3'-diaminobenzidine tetrahydrochloride (DAB)
- Counterstain with haematoxylin
Scoring and Evaluation:
- Evaluate staining intensity (0-3) and percentage of positive cells (0-100%)
- Calculate H-score: (staining intensity × percentage of positive cells)
- For categorical assessment, use cut-off of 11% positive cells [23]
- Have two pathologists independently evaluate samples in a double-blind manner
RNA Expression Analysis Protocol
RNA Extraction and Reverse Transcription:
- Extract total RNA using Trizol reagent
- Reverse transcribe to cDNA using First-strand cDNA Synthesis Kit
- Use human GAPDH gene as internal control
qPCR Analysis:
- Prepare reaction mixture with SYBR Green QPCR Master Mix
- Use primers: UBE2C-forward: AGTGGCTACCCTTACAATGCG; UBE2C-reverse: TTACCCTGGGTGTCCACGTT [29]
- Amplification conditions: denaturation at 94°C for 5 min, 40 cycles of 94°C for 30s, 58°C for 30s, and 72°C for 30s
- Analyze relative expression using the 2−ΔΔCt method
Functional Validation Assays
Cell Culture and Transfection:
- Culture cancer cells in RPMI-1640 medium with 10% fetal bovine serum
- Transfect with siRNAs or eukaryotic expression vectors using Lipofectamine 2000
- Harvest cells 3-5 days post-transfection for analysis
Proliferation and Invasion Assays:
- Perform growth assays using cell counting or MTT assay
- Conduct colony formation assays to assess clonogenic potential
- Use Transwell assays with Matrigel to evaluate invasive capability
- Analyze cell cycle distribution by flow cytometry
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Research Reagents for UBE2C Studies
| Reagent Type | Specific Product | Application | Key Features | Reference |
|---|---|---|---|---|
| Primary Antibodies | Rabbit anti-human UBE2C monoclonal antibody (Abnova) | IHC | Validated for FFPE tissues; 1:100 dilution | [26] |
| Primary Antibodies | Mouse anti-human UBE2C monoclonal antibody (Santa Cruz, SC-100611) | IHC | Suitable for intestinal-type gastric cancer; 1:50 dilution | [27] |
| Primary Antibodies | UBE2C Polyclonal antibody (PTGlab, 12134-2-AP) | WB, IHC, IP, ELISA | Reacts with human, mouse, rat; 1:50-1:500 for IHC | [30] |
| Primary Antibodies | UBE2C (WHO0011065M1, Sigma-Aldrich) | IHC, WB | Validated in SKBR3 cells; single band at ~20 KDa | [25] |
| Detection Systems | Novolink Max Polymer Detection kit | IHC | Enhanced sensitivity for low-abundance targets | [25] |
| Detection Systems | Kit ChemMate (Dako) | IHC | Biotin-streptavidin-peroxidase system | [23] |
| RNA Analysis Kits | First-strand cDNA Synthesis Kit | RT-qPCR | High-efficiency reverse transcription | [24] |
| Transfection Reagents | Lipofectamine 2000 | Functional studies | High efficiency for siRNA delivery | [27] |
UBE2C has been extensively validated as a robust prognostic marker in both breast and gastric cancers, with strong associations with aggressive tumor behavior, metastasis, and poor survival outcomes. The structured protocols and reagents outlined in this application note provide researchers with standardized methodologies for investigating UBE2C in cancer pathology. Furthermore, UBE2C's central role in critical cancer signaling pathways positions it as a promising therapeutic target, warranting further investigation into targeted therapies that modulate its activity in ubiquitination-dependent oncogenesis.
Within the broader context of ubiquitination-specific antibodies and immunohistochemistry in cancer research, the Ubiquitin-Specific Protease (USP) family of deubiquitinating enzymes has emerged as a critical regulator of oncogenic processes. USPs catalyze the removal of ubiquitin moieties from target proteins, thereby modulating their stability, localization, and function [15]. The delicate balance between ubiquitination and deubiquitination is essential for cellular homeostasis, and its disruption can lead to tumorigenesis [31]. This application note provides a detailed framework for analyzing the correlation between USP expression, tumor grade, and patient survival outcomes using data from The Cancer Genome Atlas (TCGA). By integrating bioinformatic analyses with experimental validation protocols, this resource enables researchers to identify and characterize USP family members as potential prognostic biomarkers and therapeutic targets across human malignancies.
Results and Data Analysis
USP Expression Patterns Across Human Cancers
Table 1: USP Family Member Expression and Prognostic Significance in Human Cancers
| USP Member | Cancer Type(s) | Expression Pattern | Correlation with Survival | Key Substrates/Pathways |
|---|---|---|---|---|
| USP35 [32] | Kidney clear cell carcinoma (KIRC) | Significant overexpression in tumor tissues | Poor overall survival | Glycerophospholipid metabolism, immune modulation |
| USP5 [33] | Pan-cancer (multiple types) | Overexpressed in most cancers | Poor prognosis in multiple cancers | Spliceosome, RNA splicing |
| USP13 [34] | High-grade serous ovarian cancer | Highly amplified and overexpressed | Decreased overall and progression-free survival | PI3K/AKT pathway, metastasis |
| USP45 [35] | Pan-cancer (multiple types) | Upregulated in most tumors | Poor overall and recurrence-free survival | Immune checkpoint regulation |
| USP7 [36] | HER2+ breast cancer | Highly expressed | Poor prognosis | HER2 stabilization |
| USP6, USP41 [37] | Osteosarcoma | Overexpressed in tumor cells | Correlated with patient survival | Cell viability, apoptosis regulation |
Analysis of TCGA data reveals that numerous USP family members demonstrate significant overexpression in various cancer types compared to normal tissues. For instance, USP35 shows marked overexpression in kidney clear cell carcinoma (KIRC) tumor tissues, with its high expression correlating with advanced disease stages and poor survival outcomes [32]. Similarly, USP5 exhibits pan-cancer overexpression across multiple cancer types including breast invasive carcinoma, colon adenocarcinoma, and lung adenocarcinoma, with generally poor prognosis associated with its high expression [33]. The genomic amplification of USP13 occurs in approximately 19.5% of ovarian serous cystadenocarcinoma cases, with its high mRNA expression significantly associated with decreases in overall survival, progression-free survival, and post-progression survival [34].
Correlation with Tumor Grade and Stage
Table 2: Association Between USP Expression and Clinicopathological Parameters
| USP Member | Cancer Type | Correlation with Tumor Grade/Stage | Other Clinical Correlations |
|---|---|---|---|
| USP35 [32] | KIRC | Correlated with advanced disease stages | Modulated immune cell recruitment |
| USP13 [34] | Ovarian cancer | Increased expression in advanced tumors | Correlation with peritoneal metastasis |
| USP5 [33] | Pan-cancer | Correlated with pathological stage in multiple cancers | Associated with molecular subtypes |
| USP45 [35] | Pan-cancer | Not specified | Correlated with tumor stemness features |
The relationship between USP expression and tumor progression extends to specific correlations with advanced disease stages and aggressive clinicopathological features. In kidney clear cell carcinoma, high USP35 expression correlates with advanced disease stages, suggesting its potential role in disease progression [32]. Similarly, USP13 mRNA expression increases in advanced ovarian tumors and correlates with tumor grade, indicating its involvement in disease aggressiveness [34]. Pan-cancer analysis of USP5 demonstrates correlations with pathological stages across various cancer types, reinforcing the connection between USP expression and tumor progression [33].
Experimental Protocols
TCGA Data Access and Processing Protocol
Protocol 3.1: Accessing and Processing TCGA Data for USP Expression Analysis
- Objective: To systematically access, download, and process TCGA data for analysis of USP family gene expression.
Materials and Equipment:
- GDC Data Portal (https://portal.gdc.cancer.gov/)
- R software environment (version 4.1.0 or later)
- UCSC Xena browser (https://xena.ucsc.edu/)
- cBioPortal (https://www.cbioportal.org/)
Procedure:
- Data Access:
- Navigate to the GDC Data Portal and select "Cohort Builder" or "Projects" to identify relevant cancer types.
- Apply filters for "Programs" → "TCGA" and select specific projects (e.g., TCGA-BRCA for breast cancer).
- Save the selection as a new cohort for subsequent analysis [38].
- File Selection and Download:
- Navigate to the "Repository" and apply filters to select RNA-Seq data and gene quantification files.
- For USP expression analysis, select "Transcriptome Profiling" → "Gene Expression Quantification" → "RNA-Seq" data.
- Add selected files to the cart and download using the GDC Data Transfer Tool for large datasets [38].
- Data Processing:
- For RNA sequencing data, use transcripts per million (TPM) values for gene expression normalization.
- Process clinical data to extract relevant parameters including tumor stage, grade, and survival outcomes.
- Perform differential expression analysis between tumor and normal tissues using the DESeq2 package in R [32].
- Quality Control:
- Verify data integrity using MD5 checksums provided in the manifest file.
- Assess sample quality and remove outliers based on clinical metadata.
- Data Access:
Troubleshooting Tips:
Survival and Correlation Analysis Protocol
Protocol 3.2: Survival Analysis and Clinical Correlation for USP Genes
- Objective: To evaluate the prognostic significance of USP expression and its correlation with clinicopathological parameters.
Materials and Equipment:
- R software with packages: survival, survminer, ggplot2
- TCGA clinical data files
- Processed USP expression matrix
Procedure:
- Data Integration:
- Survival Analysis:
- Perform Kaplan-Meier survival analysis for overall survival (OS), disease-specific survival (DSS), and progression-free interval (PFI).
- Use log-rank test to assess statistical significance between survival curves.
- Generate hazard ratios and confidence intervals using univariate Cox proportional hazards models [33].
- Clinical Correlation:
- Analyze association between USP expression levels and tumor stage/grade using appropriate statistical tests (Kruskal-Wallis test for multi-group comparisons, Wilcoxon test for two-group comparisons).
- Conduct multivariate analysis to adjust for potential confounding factors such as age, gender, and other clinical variables.
- Visualization:
- Create publication-quality Kaplan-Meier plots using the survminer package in R.
- Generate boxplots or violin plots to visualize USP expression across different tumor stages.
Expected Outcomes:
- Identification of USP family members with significant correlation to patient survival.
- Determination of association between USP expression and tumor progression metrics.
Experimental Validation Protocol
Protocol 3.3: Experimental Validation of USP Role in Cancer Progression
- Objective: To functionally validate the oncogenic role of USPs identified through bioinformatic analysis.
Materials and Equipment:
- Human cancer cell lines (e.g., 786-O and ACHN for renal cancer [32])
- Lentiviral vectors carrying shRNAs targeting USP of interest
- Lipofectamine 3000 transfection reagent
- Cell culture equipment and reagents
- Quantitative RT-PCR system
- Materials for functional assays: CCK-8 kit, Transwell chambers, crystal violet staining solution
Procedure:
- USP Knockdown:
- Transfect cancer cell lines with lentiviral vectors carrying specific shRNAs targeting the USP of interest (e.g., shUSP35-1, shUSP35-2, shUSP35-3) [32].
- Include a non-targeting control (shNC) for comparison.
- Select stable cell lines using 2 µg/mL puromycin.
- Confirm knockdown efficiency via quantitative real-time PCR (qRT-PCR) [32].
- Functional Assays:
- Cell Proliferation: Perform CCK-8 assay by seeding transfected cells in 96-well plates and measuring absorbance at 450nm at 24, 48, 72, and 96 hours [32].
- Colony Formation: Seed transfected cells in 6-well plates (500 cells/well), culture for 14 days, fix with 4% paraformaldehyde, stain with crystal violet, and count colonies [32].
- Cell Migration:
- Wound Healing Assay: Create a linear scratch in confluent cell monolayers and monitor wound closure at 0, 24, and 48 hours.
- Transwell Migration Assay: Seed cells in serum-free medium in upper chambers and assess migration toward complete medium in lower chambers after 24-48 hours [32].
- Pathway Analysis:
- Perform gene set enrichment analysis (GSEA) using RNA-seq data from USP knockdown vs control cells to identify affected pathways [32].
- Validate key pathway alterations through Western blot analysis of relevant protein markers.
- USP Knockdown:
Data Interpretation:
- Significant reduction in cell proliferation, colony formation, and migration in USP-knockdown cells supports oncogenic function.
- Identification of specific pathways enriched in GSAE provides mechanistic insights.
Visualizations
USP Analysis Workflow and Clinical Correlations
USP-Mediated Oncogenic Signaling Mechanisms
The Scientist's Toolkit
Table 3: Essential Research Reagents and Resources for USP-Cancer Studies
| Resource Category | Specific Examples | Application/Function |
|---|---|---|
| Bioinformatic Tools | GDC Data Portal, cBioPortal, UCSC Xena | TCGA data access and visualization |
| Statistical Software | R with DESeq2, survival, survminer packages | Differential expression and survival analysis |
| Cell Lines | 786-O (renal cancer), ACHN (renal cancer), HOS (osteosarcoma) | Functional validation of USP roles |
| Knockdown Reagents | Lentiviral shRNAs (shUSP35-1, shUSP35-2, shUSP35-3) | Targeted USP depletion |
| Functional Assays | CCK-8, Colony formation, Transwell migration | Assessment of proliferation and metastatic potential |
| USP Inhibitors | PR619 (broad-spectrum), DUBs-IN-2 (USP8-specific) | Pharmacological targeting of USP activity |
This toolkit encompasses essential resources for conducting comprehensive studies on USP family members in cancer. Bioinformatic tools provide the foundation for initial discovery and hypothesis generation, enabling researchers to access and analyze large-scale genomic data from TCGA [38]. Validation reagents including specific cell lines and knockdown constructs allow for functional assessment of USP roles in cancer progression, as demonstrated in renal carcinoma models with USP35 [32]. The inclusion of USP inhibitors such as PR619, a broad-spectrum DUB inhibitor that has shown efficacy in reducing primary tumor growth and metastasis in osteosarcoma models, provides opportunities for therapeutic exploration [37].
The integrated application of bioinformatic analysis of TCGA data and experimental validation provides a powerful approach for elucidating the roles of USP family members in cancer progression and their potential as prognostic biomarkers. The protocols outlined in this application note establish a standardized framework for identifying USPs with significant correlations to tumor grade and patient survival, enabling researchers to prioritize candidates for further functional characterization. The consistent pattern of USP overexpression across diverse cancer types, coupled with their association with advanced disease stages and poor clinical outcomes, highlights the broader significance of deubiquitination processes in tumorigenesis. These findings reinforce the importance of the ubiquitin-proteasome system as a rich source of therapeutic targets and support continued investigation into USP-directed therapies for cancer treatment.
A Practical Guide to IHC Protocol Development for Ubiquitination Markers
In the field of biomedical research, particularly in the study of complex processes like ubiquitination in cancer, the selection of appropriate antibodies is not merely a preliminary step but a critical determinant of experimental success. Antibodies, the specialized proteins produced by the immune system to recognize and bind to specific molecules, serve as the primary detection tools in techniques such as immunohistochemistry (IHC), which is essential for visualizing protein localization within tissue contexts [39]. For researchers investigating cancer mechanisms, the choice between monoclonal and polyclonal antibodies, coupled with careful consideration of host species compatibility, directly influences the specificity, reproducibility, and biological relevance of their findings. This application note provides a structured framework for selecting antibodies specifically tailored for cancer research, with a focus on ubiquitination studies, and includes detailed protocols to ensure optimal results in IHC experiments.
Core Differences: Monoclonal vs. Polyclonal Antibodies
Fundamental Characteristics and Production
Antibodies are categorized based on their origin and epitope specificity. Monoclonal antibodies (mAbs) are derived from a single clone of B cells and are characterized by their uniform structure and specificity for a single epitope on the target antigen. Their production involves immunizing a host animal, fusing its B cells with immortal myeloma cells to create hybridomas, and then screening and selecting clones that produce the desired antibody [40] [41]. This process ensures a consistent supply of genetically homogeneous antibodies [40].
In contrast, polyclonal antibodies (pAbs) originate from multiple B cell clones within an immunized animal. They represent a heterogeneous mixture of antibodies that recognize multiple different epitopes on the same target antigen. They are obtained by purifying immunoglobulins directly from the serum of the immunized animal, making their production generally quicker and less expensive [40] [42].
Comparative Analysis: Advantages and Disadvantages
The decision to use monoclonal or polyclonal antibodies involves weighing their distinct advantages and limitations, as summarized in the table below.
Table 1: Comprehensive Comparison of Monoclonal and Polyclonal Antibodies
| Feature | Monoclonal Antibodies | Polyclonal Antibodies |
|---|---|---|
| Origin & Specificity | Single B cell clone; binds to a single epitope [40] [41] | Multiple B cell clones; binds to multiple epitopes [40] [42] |
| Production Time | Time-consuming (+/- 6 months) [42] | Relatively quick (+/- 3 months) [42] |
| Cost | Higher due to complex manufacturing [40] | More cost-effective [40] |
| Batch-to-Batch Variability | Low reproducibility and high homogeneity [40] [42] | High variability between different productions [42] |
| Sensitivity | More sensitive for protein level quantification [42] | High sensitivity for detecting low-quantity proteins; superior for capturing native proteins [42] |
| Cross-Reactivity | Low, due to single-epitope recognition [42] | Higher potential, due to recognition of multiple epitopes [42] |
| Typical Applications | Precision-focused applications: diagnostic assays, therapeutic drugs (e.g., cancer therapies) [40] | Applications where broad specificity is needed: IHC, immunofluorescence, western blot [40] |
For general research applications, especially those requiring high sensitivity to detect low-abundance proteins or to capture native protein structures, the advantages of polyclonal antibodies often outweigh those of monoclonals. This is further enhanced when the serum is affinity-purified against the target antigen [42]. However, for applications requiring high specificity and consistency over the long term, such as therapeutic development or diagnostic manufacturing, monoclonal antibodies are the superior choice [42] [41].
The Critical Role of Host Species Compatibility
Strategic Selection of Host Species
The species in which an antibody is raised (the host species) is a critical, yet frequently overlooked, factor in experimental design. The primary consideration is to avoid interference from endogenous immunoglobulins when using secondary antibodies for detection. For example, if studying a mouse protein in mouse tissue, using a primary antibody raised in a mouse would lead to the secondary antibody binding to all endogenous mouse IgG in the tissue, creating overwhelming background signal. Therefore, a primary antibody from a different species (e.g., rabbit) must be selected [39].
Common Host Species and Their Properties
Different host species offer unique advantages based on their immune response characteristics and the volume of serum required.
Table 2: Key Host Species for Antibody Production and Their Properties
| Host Species | Key Characteristics | Common Applications/Considerations |
|---|---|---|
| Rabbit | High affinity and robust immune response; broad epitope recognition [40]. | Often preferred for monoclonal antibodies due to strong immune response; suitable for polyclonal production when high sensitivity is needed [40]. |
| Mouse | Well-established hybridoma technology; multiple stable fusion partners [40]. | A classic host for monoclonal antibody production. Not suitable for detecting mouse antigens in murine models without specialized workarounds [40]. |
| Goat | Strong reactivity across species, especially humans; adaptable with adjuvants [40]. | Frequently used for polyclonal antibody production, yielding high-volume serum for applications like blocking or detection [40]. |
| Chicken | Sustainable production (antibodies harvested from egg yolk); unique antibody structure [40]. | Useful as an alternative when mammalian cross-reactivity is a concern; reduced cross-reactivity with mammalian proteins [40]. |
| Llama | Enables production of single-domain VHH antibodies (small, stable) [40]. | Gaining traction for their unique properties, such as ease of use in immunoassays and potential for deep tissue penetration [40]. |
Application in Ubiquitination Cancer Research
The Ubiquitin-Proteasome System in Cancer
The Ubiquitin-Proteasome System (UPS) is a critical non-lysosomal pathway responsible for the controlled degradation of intracellular proteins, thereby regulating fundamental cellular processes including cell cycle progression, DNA repair, and immune response [43] [44]. Ubiquitination involves a cascade of E1 (activating), E2 (conjugating), and E3 (ligating) enzymes that attach ubiquitin molecules to target proteins, marking them for degradation by the proteasome [44]. This process is reversible through the action of deubiquitinating enzymes (DUBs), such as Ubiquitin-Specific Proteases (USPs), which remove ubiquitin moieties [43]. Dysregulation of ubiquitination and deubiquitination is a hallmark of various cancers, influencing tumor growth, metastasis, and immune evasion [43] [44]. For instance, USP7 can enhance tumor growth by modifying the immunosuppressive properties of regulatory T cells (Tregs) within the tumor microenvironment [43]. Another example is USP48, which has been shown to promote colorectal cancer progression by stabilizing the autophagy substrate protein SQSTM1/p62 and inhibiting autophagy [45].
Antibody Selection for Investigating USPs in Cancer
Research into USPs and other components of the UPS requires highly specific antibodies capable of distinguishing between different family members and their post-translationally modified states.
- Target Specificity: For differentiating between highly homologous USPs (e.g., USP7 vs. USP48), monoclonal antibodies are preferable due to their high specificity for a single epitope, minimizing cross-reactivity [40] [42]. This is crucial for accurately determining the expression and localization of a specific USP in cancer tissues.
- Detecting Modified Forms: When studying ubiquitination states or protein degradation, polyclonal antibodies can be advantageous because they are more likely to recognize a native protein and may be more sensitive in detecting low-quantity proteins or various conformational states of a target, such as ubiquitinated SQSTM1/p62 [42] [45].
- Multiplexing Experiments: For IHC experiments aiming to co-localize a USP with another protein (e.g., a cell lineage marker like GFAP), antibodies from different host species must be selected. For example, using a rabbit monoclonal anti-USP7 with a mouse monoclonal anti-GFAP allows for simultaneous detection with species-specific secondary antibodies conjugated to different fluorophores [46] [47].
The following diagram illustrates the logical decision-making process for selecting antibodies in ubiquitination cancer research.
Detailed IHC Protocol for Ubiquitination Markers
This protocol is optimized for the detection of ubiquitination-related proteins, such as USPs, in formalin-fixed, paraffin-embedded (FFPE) tissue sections, incorporating steps to overcome fixation-induced epitope masking [46] [39] [47].
Materials and Reagents
Table 3: Research Reagent Solutions for IHC
| Reagent/Material | Function/Purpose | Example/Note |
|---|---|---|
| FFPE Tissue Sections | Preserves tissue morphology and antigenicity for analysis. | Standard for clinical and research samples; requires deparaffinization. [39] |
| Primary Antibody | Binds specifically to the target protein (e.g., USP7). | Must be validated for IHC; selection of mono- vs. polyclonal is critical. [39] |
| Species-Specific Secondary Antibody | Binds to the primary antibody and is conjugated for detection. | Conjugated to enzyme (HRP) for chromogenic or fluorophore for fluorescent detection. [39] [47] |
| Antigen Retrieval Buffer | Reverses formaldehyde-induced cross-links, unmasking epitopes. | Citrate buffer (pH 6.0) or EDTA/TRIS buffer (pH 9.0); condition must be optimized. [46] [39] |
| Blocking Serum | Reduces non-specific binding of antibodies to the tissue. | Serum from the species in which the secondary antibody was raised. [39] |
| Detection Kit | Generates a visible signal at the site of antibody binding. | DAB chromogen for brown precipitate; or fluorophores for fluorescence. [47] |
| Hematoxylin | Counterstain that labels cell nuclei. | Provides histological context; blue stain. [47] |
Step-by-Step Methodology
Deparaffinization and Rehydration:
- Dewax FFPE sections by immersing them in xylene (or a safe substitute) for 5-10 minutes. Repeat twice.
- Rehydrate the tissue by passing through a series of ethanol solutions: 100% (twice), 95%, 70% (2-5 minutes each).
- Rinse thoroughly with distilled water and place in Tris-buffered saline (TBS) or phosphate-buffered saline (PBS). [39] [47]
Antigen Retrieval (Critical Step):
- Heat the retrieval buffer (e.g., 10 mM Sodium Citrate, pH 6.0) in a water bath or pressure cooker to 95-100°C.
- Immerse the slides in the pre-heated buffer and incubate for 20-30 minutes.
- Remove the container from heat and allow the slides to cool slowly in the buffer for at least 20 minutes at room temperature.
- Rinse the slides with distilled water and then with TBS or PBS containing a mild detergent like 0.025% Triton X-100 (TBS-T). [46] [39]
Quenching and Blocking:
- Quench endogenous peroxidase activity by incubating sections with 1.5-3% H₂O₂ in TBS for 10-30 minutes at room temperature (skip for fluorescence detection).
- Rinse slides 3 times in TBS for 5 minutes each.
- Carefully tap off excess liquid and outline the tissue with a hydrophobic pen.
- Apply enough appropriate blocking serum (e.g., 5-10% normal goat serum) to cover the tissue and incubate for 1 hour at room temperature in a humidity chamber. [46] [39]
Primary Antibody Incubation:
- Prepare the primary antibody (e.g., anti-USP48) at the optimal dilution in blocking serum or a commercial antibody diluent.
- Tap off the blocking serum and apply the primary antibody solution to the tissue section.
- Incubate overnight at 4°C in a humidity chamber for optimal results. Alternatively, a 1-2 hour incubation at room temperature can be tested during optimization. [39]
Secondary Antibody Incubation and Detection:
- Rinse the slides 3 times in TBS-T for 5 minutes each to remove unbound primary antibody.
- Apply the enzyme- or fluorophore-conjugated secondary antibody (e.g., HRP-Goat anti-Rabbit IgG) diluted in TBS or blocking serum. Incubate for 1 hour at room temperature in the dark (for fluorescence).
- Rinse again 3 times with TBS-T for 5 minutes each. [39] [47]
Signal Development and Counterstaining:
- For Chromogenic Detection (DAB): Prepare the DAB substrate according to the manufacturer's instructions. Apply to the tissue and monitor development under a microscope (typically 30 seconds to 5 minutes). Stop the reaction by immersing the slide in distilled water.
- For Fluorescence Detection: Proceed to counterstaining.
- Counterstain nuclei by applying hematoxylin (for chromogenic) or DAPI (for fluorescence) for the recommended time. Rinse thoroughly.
- For chromogenic staining, dehydrate the sections through a graded series of alcohols (70%, 95%, 100%) and clear in xylene. Coverslip using a permanent mounting medium. For fluorescence, use an anti-fade mounting medium. [46] [47]
The workflow for this protocol is visualized below.
The strategic selection of antibodies, informed by a clear understanding of the differences between monoclonal and polyclonal types and the imperative of host species compatibility, is foundational to robust and interpretable research in ubiquitination and cancer biology. By applying the principles and protocols outlined in this document, researchers can enhance the reliability of their experimental data, particularly in technically demanding applications like immunohistochemistry. As the field advances with new technologies such as recombinant antibodies, which offer superior batch-to-batch consistency, these foundational selection criteria will remain essential for driving discoveries in cancer mechanisms and the development of novel therapeutic strategies.
In the field of cancer research, the precise detection of ubiquitination markers via immunohistochemistry (IHC) is paramount for understanding tumor pathogenesis and developing targeted therapies. The ubiquitin-proteasome system (UPS) plays a critical role in regulating nearly all biological processes, including DNA damage repair, cell-cycle regulation, signal transduction, and protein degradation [48]. Dysregulation of this system is intimately linked with carcinogenesis [15]. However, the accurate visualization of ubiquitination-related proteins in formalin-fixed paraffin-embedded (FFPE) tissues presents significant technical challenges, primarily due to formalin-induced epitope masking. This application note establishes heated basic retrieval as the optimal starting point for unmasking ubiquitination targets, providing researchers with a standardized framework to enhance staining reproducibility and reliability in cancer studies.
The Scientific Rationale: Ubiquitination in Cancer Research
The Ubiquitin-Proteasome System and Cancer Pathogenesis
The ubiquitin-proteasome system represents the primary pathway for selective protein degradation in eukaryotes, preserving proteostasis and orchestrating critical cellular functions [15]. Ubiquitination involves a coordinated enzymatic cascade:
- E1 activating enzymes: Initiate ubiquitin activation
- E2 conjugating enzymes: Transfer activated ubiquitin
- E3 ligases: Confer substrate specificity for ubiquitin transfer [48] [15]
Approximately 80% of intracellular proteins are degraded via the UPS, maintaining genomic stability and modulating signaling pathways that regulate cell proliferation and apoptosis [48]. The balance of ubiquitination is further regulated by deubiquitinating enzymes (DUBs), with ubiquitin-specific proteases (USPs) representing the largest DUB subfamily [15].
Ubiquitination Targets as Biomarkers and Therapeutic Targets
Ubiquitination-related proteins have emerged as significant biomarkers and therapeutic targets across multiple cancer types:
- USP2 demonstrates significantly reduced expression in gastric cancer cells and patient samples, where it acts as a negative regulator of gastric cancer progression [19].
- USP9X maintains protein stability of the m6A reader IGF2BP2 in triple-negative breast cancer (TNBC), with high expression correlating with poor prognosis [49].
- A prognostic model incorporating ubiquitination-related genes (MMP1, RNF2, TFRC, SPP1, and CXCL8) effectively predicts survival rates in cervical cancer patients [48].
The therapeutic potential of targeting ubiquitination pathways is exemplified by proteolysis-targeting chimeras (PROTACs), which harness E3 ubiquitin ligases to selectively degrade disease-causing proteins [50]. These advancements underscore the critical need for reliable detection methods for ubiquitination targets in tissue samples.
Antigen Retrieval Fundamentals
The Challenge of Formalin Fixation
Formalin fixation creates methylene bridges between proteins, leading to epitope masking that prevents antibody binding [51]. This process alters the three-dimensional conformation of epitopes, rendering them inaccessible to primary antibodies even when present in the tissue [51]. Antigen retrieval reverses this masking by disrupting the crosslinks, thereby exposing binding sites and enabling accurate antibody recognition [51].
Heat-Induced Epitope Retrieval (HIER) as the Preferred Method
Heat-Induced Epitope Retrieval (HIER) has demonstrated superior effectiveness over Protease-Induced Epitope Retrieval (PIER) for most applications [52]. While PIER employs proteolytic enzymes to cleave protein crosslinks, it carries significant limitations including potential morphological tissue damage, epitope degradation leading to false-negative results, and difficulty balancing under-digestion and over-digestion [51].
HIER utilizes high temperatures (95-100°C) to disrupt protein crosslinks through thermal unfolding, with typical protocols involving 10-30 minute heating periods followed by cooling phases in buffer [51]. The mechanism involves both thermal disruption of crosslinks and chelation of calcium ions from protein cross-linking [51].
Table 1: Comparison of Antigen Retrieval Methods
| Parameter | Heat-Induced Epitope Retrieval (HIER) | Protease-Induced Epitope Retrieval (PIER) |
|---|---|---|
| Mechanism | Thermal unfolding of crosslinks | Enzymatic cleavage of proteins |
| Temperature | 95-100°C | 37°C |
| Incubation Time | 10-30 minutes | 10-20 minutes |
| Primary Risk | Tissue detachment from slides | Morphological damage to tissue |
| Buffer pH Range | Wide range (pH 6.0-9.0) | Specific to enzyme optimal activity |
| Reproducibility | High with temperature control | Variable due to enzyme activity |
Optimized Protocol for Ubiquitination Targets
Recommended Buffers for Ubiquitination Targets
For ubiquitination targets, basic retrieval buffers consistently outperform acidic options due to their enhanced ability to disrupt the formalin-induced crosslinks that mask ubiquitination epitopes. The following buffers are recommended:
- Tris-EDTA Buffer (10 mM Tris base, 1 mM EDTA solution, 0.05% Tween 20, pH 9.0) [53]
- EDTA Buffer (1 mM EDTA, pH 8.0) [53]
- Sodium Citrate Buffer (10 mM Sodium citrate, 0.05% Tween 20, pH 6.0) [53]
Basic conditions (pH 8.0-9.0) are particularly effective for ubiquitination targets due to their enhanced ability to disrupt the formalin-induced crosslinks that mask these epitopes.
Standardized HIER Protocol Using a Pressure Cooker
The pressure cooker method provides uniform heat distribution and consistent results, making it ideal for standardizing ubiquitination target detection [53].
Materials Required:
- Domestic stainless steel pressure cooker
- Hot plate
- Vessel with slide rack (400-500 mL capacity)
- Antigen retrieval buffer (Tris-EDTA pH 9.0 recommended) [53]
Step-by-Step Procedure:
- Add the appropriate antigen retrieval buffer to the pressure cooker [53].
- Place the pressure cooker on the hotplate and turn to full power [53].
- While waiting for the buffer to boil, deparaffinize and rehydrate the tissue sections [53].
- Once boiling, transfer slides from tap water to the pressure cooker (rest lid on top, do not secure at this point) [53].
- Secure the pressure cooker lid according to manufacturer's instructions [53].
- Once full pressure is reached, time exactly 3 minutes [53].
- After 3 minutes, turn off hotplate and place pressure cooker in sink [53].
- Activate pressure release valve and run cold water over the cooker [53].
- Once depressurized, open lid and run cold water into cooker for 10 minutes [53].
- Continue with standard IHC staining protocol [53].
Alternative HIER Methods
Microwave Method:
- Use microwaveable vessel with slide rack
- Heat at full power until boiling, then boil for 20 minutes [53]
- Monitor constantly for evaporation; do not allow slides to dry out [53]
- Cool with running tap water for 10 minutes after retrieval [53]
Vegetable Steamer Method:
- Pre-heat steamer according to manufacturer's instructions
- Pre-heat retrieval buffer to boiling in separate flask
- Place container with slide rack in steamer, add hot buffer
- Maintain at 95-100°C for 20 minutes [53]
- Cool with running tap water for 10 minutes [53]
Optimization Strategies and Troubleshooting
Systematic Optimization Approach
When establishing a new protocol for ubiquitination targets, a systematic optimization approach is recommended:
- Start with HIER at both low pH (citrate buffer, pH 6.0) and high pH (Tris-EDTA, pH 8.0-9.9) [51]
- Evaluate retrieval time by testing slides for 1, 2, 3, 4, and 5 minutes before IHC staining [53]
- Create a matrix to test different combinations of buffer pH and incubation times [52]
Table 2: Optimization Matrix for Antigen Retrieval Conditions
| Incubation Time | Acidic Buffer (pH 6.0) | Neutral Buffer (pH 7.2-7.6) | Basic Buffer (pH 9.0) |
|---|---|---|---|
| 1 minute | Slide #1 | Slide #2 | Slide #3 |
| 5 minutes | Slide #4 | Slide #5 | Slide #6 |
| 15 minutes | Slide #7 | Slide #8 | Slide #9 |
Troubleshooting Common Issues
- Weak or No Staining: Often caused by insufficient epitope unmasking. Try increasing heating time or switching to higher pH retrieval solution [51].
- High Background: May indicate over-retrieval or tissue damage. Systematically test buffer pH and timing to resolve IHC artifacts [51].
- Tissue Detachment: Use appropriate slide adhesives and avoid vigorous boiling. Consider using a water bath set to 60°C overnight for delicate tissues [53].
Essential Controls and Validation
Required Experimental Controls
- Negative Controls: Sections processed without primary antibody to check for non-specific secondary antibody binding [51].
- Positive Controls: Tissues with known antigen expression to confirm protocol and reagent functionality [51].
- Specificity Controls: Use methods like knockout/knockdown validation or blocking peptides to confirm antibody target specificity [51].
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Reagents for Ubiquitination Target IHC
| Reagent | Function | Specific Recommendations |
|---|---|---|
| Retrieval Buffers | Break formalin-induced crosslinks | Tris-EDTA (pH 9.0) for most ubiquitination targets [53] |
| Primary Antibodies | Target-specific detection | Use validated antibodies against ubiquitination markers (e.g., USP2, USP9X) [19] [49] |
| Detection System | Visualize antibody binding | Standard HRP-based detection kits |
| Blocking Reagents | Reduce non-specific background | Serum or protein-based blocking solutions |
| Slide Adhesives | Prevent tissue detachment | Poly-L-lysine or other adhesives for high-temperature protocols |
Optimized antigen retrieval is fundamental for accurate detection of ubiquitination targets in cancer research. Heated basic retrieval using Tris-EDTA buffer (pH 9.0) provides an effective starting point for most ubiquitination markers, enabling researchers to reliably study the crucial role of the ubiquitin-proteasome system in tumor pathogenesis. By implementing this standardized protocol with appropriate controls and optimization strategies, researchers can enhance reproducibility and generate more reliable data for both diagnostic applications and therapeutic development targeting ubiquitination pathways.
Determining Optimal Primary Antibody Concentration and Incubation Conditions
In the field of cancer research, immunohistochemistry (IHC) serves as a cornerstone technique for visualizing the spatial distribution and abundance of proteins within the complex architecture of tumor tissues [47]. When investigating dynamic post-translational modifications such as protein ubiquitination—a key regulator of cancer-relevant processes including protein degradation, cell signaling, and DNA repair—the reliability of IHC data is paramount [54]. The specificity and sensitivity of this technique are fundamentally governed by the precise optimization of primary antibody application. This protocol details a systematic approach to determining the optimal primary antibody concentration and incubation conditions, with a specific emphasis on challenges and considerations pertinent to ubiquitination-specific antibodies in cancer research models.
Antibody Selection and Key Considerations
The first critical step in any IHC experiment is the selection of an appropriate primary antibody. The choice between monoclonal and polyclonal antibodies involves a careful trade-off between specificity and robustness, a consideration especially acute for detecting ubiquitination.
Monoclonal vs. Polyclonal Antibodies
- Monoclonal Antibodies: These are derived from a single B-cell clone and are specific for a single epitope [55] [56] [57]. This high specificity is advantageous for distinguishing ubiquitin chains with specific linkage types (e.g., K48 vs. K63) [54]. However, they can be vulnerable to epitope masking induced by tissue fixation, a significant risk when the epitope is the labile ubiquitin-protein isopeptide bond [55] [57].
- Polyclonal Antibodies: These are heterogeneous populations derived from multiple B-cell clones and recognize multiple epitopes on the target antigen [55] [56] [57]. This makes them generally more resistant to changes in antigen conformation caused by fixation and are often a practical starting point [57] [58]. The primary drawback is their higher potential for cross-reactivity and lot-to-lot variability [56] [57].
For ubiquitination-specific antibodies, a major challenge is the size and instability of the ubiquitin modification. The native isopeptide linkage can be cleaved by deubiquitinases, and the large size of ubiquitin (76 amino acids) complicates antigen design [54]. Therefore, verifying that an antibody has been validated for IHC on fixed tissue, ideally with examples in the literature, is essential.
Research Reagent Solutions
The table below outlines essential materials and reagents required for the optimization of IHC protocols for ubiquitination research.
Table 1: Key Research Reagents for IHC Optimization in Ubiquitination Studies
| Item | Function & Importance |
|---|---|
| Formalin-Fixed Paraffin-Embedded (FFPE) Tissue Sections | Standard sample preparation method for cancer research; fixation cross-links proteins and can mask epitopes, necessitating antigen retrieval [47] [59]. |
| Ubiquitination-Specific Primary Antibodies | Key reagent for detecting specific ubiquitin-protein conjugates or linkage-specific polyubiquitin chains; require rigorous validation [54]. |
| Antigen Retrieval Buffers (e.g., EDTA, Citrate) | Critical for reversing formaldehyde-induced cross-links and unmasking epitopes, making them accessible to the primary antibody [60]. |
| Validated Positive Control Tissues/Cells | Tissue or cell lines known to express the target ubiquitinated protein; essential for confirming protocol functionality [56]. |
| Isotype Control IgG | Non-immune immunoglobulin of the same species and isotype as the primary antibody; critical for distinguishing specific signal from background [56]. |
| Protein-Blocking Serum | Reduces non-specific binding of antibodies to charged sites on the tissue, thereby lowering background staining [47]. |
| Signal Amplification Kits (e.g., TSA) | Systems like tyramide signal amplification (TSA) can enhance detection sensitivity for low-abundance targets like specific ubiquitin modifications [60]. |
Experimental Protocol for Optimization
The following section provides a detailed, step-by-step methodology for establishing the optimal working conditions for a primary antibody in IHC.
Preliminary Setup and Sample Preparation
- Tissue Sectioning: Cut 4-5 µm sections from FFPE tissue blocks of your positive control tissue (e.g., cancer cell line xenograft or human tumor tissue with known ubiquitination status) [59].
- Slide Mounting and Baking: Mount sections on charged glass slides and bake at 60°C for 30-60 minutes to ensure adhesion.
- Deparaffinization and Rehydration: Immerse slides in xylene (or substitute) followed by a graded series of ethanol (100%, 95%, 70%) and finally distilled water.
- Antigen Retrieval: Perform heat-induced epitope retrieval (HIER) using an appropriate buffer (e.g., Tris-EDTA, pH 9.0, or citrate, pH 6.0). The optimal buffer and heating time must be determined empirically for each antibody-target pair [60].
- Blocking: Incubate sections with a protein block (e.g., 5-10% normal serum from the species of the secondary antibody or a commercial protein block) for 30 minutes at room temperature to minimize non-specific binding.
Primary Antibody Titration
The core of optimization is a titration assay where antibody concentration is varied while other parameters are held constant.
- Prepare Antibody Dilutions: Reconstitute the antibody according to the manufacturer's instructions. Prepare a series of dilutions in an appropriate antibody diluent. A typical starting range for monoclonal antibodies is 5-25 µg/mL, and for antigen-affinity purified polyclonal antibodies, it is 1.7-15 µg/mL [55] [57].
- Apply to Sections: Apply the different antibody dilutions to serial tissue sections. Ensure each section is fully covered.
- Incubate: A common and effective starting point is an overnight incubation at 4°C in a humidity chamber to prevent evaporation [47] [55] [57].
- Controls: Include critical controls on separate sections:
- No-Primary Control: Incubate with antibody diluent only. This identifies background from the detection system.
- Isotype Control: Incubate with a non-specific IgG at the same concentration as your highest primary antibody concentration. This identifies non-specific antibody binding.
Detection and Visualization
- Washing: After incubation, wash slides thoroughly with a buffered solution like PBS or TBS to remove unbound antibody.
- Apply Secondary Antibody: Incubate with a species-specific secondary antibody conjugated to an enzyme (e.g., HRP) or a fluorophore. For chromogenic detection, polymer-based HRP systems are recommended due to their high sensitivity and low background [56].
- Visualize: For enzyme conjugates, apply a chromogen substrate such as 3,3'-Diaminobenzidine (DAB). For fluorescent conjugates, apply a counterstain like DAPI to visualize nuclei.
- Mounting and Imaging: Coverslip the sections using an aqueous mounting medium (for fluorescence) or a permanent mounting medium (for chromogenic stains). Image the slides using a brightfield or fluorescence microscope.
Analysis and Interpretation
Evaluate the stained slides systematically. The optimal dilution is the one that provides the strongest specific signal (e.g., crisp nuclear, cytoplasmic, or membranous staining in expected patterns) with the lowest non-specific background [55] [58].
Table 2: Optimization of Primary Antibody Incubation Conditions
| Parameter | Standard Starting Condition | Optimization Adjustment | Rationale |
|---|---|---|---|
| Concentration | Monoclonal: 5-25 µg/mLPolyclonal: 1.7-15 µg/mL [55] [57] | Titrate in a serial dilution series | To find the balance between specific signal intensity and non-specific background. |
| Incubation Time | Overnight (~16 hours) [55] [57] | Shorten to 1-2 hours at room temperature if background is high; extend if signal is weak. | Longer incubations can increase binding but also risk higher background; lower temperatures allow for longer, more specific incubations [58]. |
| Incubation Temperature | 4°C [55] [57] | Increase to room temperature or 37°C | Higher temperatures accelerate binding kinetics but can increase non-specific binding and lead to antibody or tissue degradation. |
Workflow Visualization
The following diagram summarizes the logical workflow for the primary antibody optimization process, from initial setup to final analysis.
Troubleshooting Common Issues
- High Background Staining: This is frequently caused by a primary antibody concentration that is too high [58]. Re-titrate using a wider range of higher dilutions. Alternatively, reduce the incubation time or increase the stringency of washing. Using F(ab')2 fragment secondary antibodies can also help by preventing Fc receptor binding [56].
- Weak or Absent Specific Signal: The antibody concentration may be too low, or the epitope may be inadequately retrieved [58]. Re-optimize antigen retrieval conditions (buffer pH, heating time). Consider using a signal amplification method such as tyramide signal amplification (TSA), which is particularly useful for detecting low-abundance targets like specific ubiquitin modifications [60].
- Inconsistent Staining Between Experiments: This can arise from lot-to-lot variability in polyclonal antibodies or variations in incubation times and temperatures. For long-term projects, switching to a monoclonal antibody can improve consistency. Ensure all steps of the protocol are timed and performed uniformly [56].
Concluding Remarks
The rigorous optimization of primary antibody concentration and incubation conditions is a non-negotiable prerequisite for generating reliable, reproducible, and interpretable IHC data. This is especially true in the challenging context of cancer research utilizing ubiquitination-specific antibodies, where targets may be labile and of low abundance. By following the systematic, iterative protocol outlined in this document—centered on careful antibody selection, methodical titration, and the consistent use of controls—researchers can establish robust IHC assays. These optimized protocols are fundamental for advancing our understanding of the critical role ubiquitination plays in cancer biology and therapy.
Protocol for Formalin-Fixed Paraffin-Embedded (FFPE) Tissue Processing and Staining
In the field of cancer research, particularly in the study of post-translational modifications such as ubiquitination, immunohistochemistry (IHC) on Formalin-Fixed Paraffin-Embedded (FFPE) tissues is a cornerstone technique. This protocol details the specialized processing and staining of FFPE tissues, with emphasis on applications for ubiquitination-specific antibodies. The preservation of tissue morphology combined with the specific detection of ubiquitination-related proteins, such as ubiquitin-specific proteases (USPs) and other components of the ubiquitin-proteasome system, enables critical insights into cancer biology, patient prognosis, and therapeutic target validation [15] [61]. Proper execution of this protocol is essential for generating reliable, reproducible data that can inform drug development strategies.
Core Principles of FFPE Tissue Processing
The fundamental objective of FFPE processing is to preserve tissue architecture and antigenicity for long-term storage and analysis. Optimal fixation is the most critical step, as it stabilizes proteins and prevents degradation.
Fixation
- Fixative of Choice: 10% Neutral Buffered Formalin (10% NBF) is the most widely used fixative in diagnostic pathology and research. The concentration of formaldehyde in 10% NBF is nearly identical to that in 4% Paraformaldehyde (PFA) [62].
- Tissue Preparation: Trim tissue specimens to a thickness of 2-3 mm before immersion in fixative to ensure adequate penetration [63].
- Fixation Time: Immerse tissue in a minimum volume of 20 parts fixative to 1 part tissue for 6 to 72 hours at room temperature [63] [62]. Under-fixation can lead to poor tissue preservation, while over-fixation can cause excessive protein cross-linking, masking epitopes and reducing antibody binding [62] [64].
- Post-Fixation Handling: Following fixation, wash tissue thoroughly with PBS to remove residual fixative. Tissues can be stored in 70% ethanol until processing, though this is not recommended for brain or neurological samples [63].
Processing, Embedding, and Sectioning
After fixation, tissues undergo dehydration, clearing, and infiltration with paraffin wax to create a stable block suitable for thin-sectioning.
The following table summarizes the key steps for processing, embedding, and sectioning FFPE tissues.
Table 1: FFPE Tissue Processing, Embedding, and Sectioning Protocol
| Step | Solutions | Incubation Time | Notes |
|---|---|---|---|
| Dehydration | 50%, 70%, 85%, 95%, 100% Ethanol [62] | 20-30 minutes to 1-2 hours per solution [62] | Gradual dehydration prevents tissue distortion; larger tissues require longer incubation. |
| Clearing | Xylene or alternative clearing agent [12] [62] | 10-20 minutes, two changes [62] | Removes alcohol and prepares tissue for paraffin infiltration. |
| Infiltration | Molten Paraffin Wax (50-60°C) [12] [62] | 40 minutes to 1 hour, three changes [12] [62] | Performed in a vacuum oven or automated processor to ensure complete infiltration. |
| Embedding | Fresh Paraffin Wax | ~10 minutes to harden [62] | Tissue is oriented in a mold filled with wax and anchored with a cassette. |
| Sectioning | Using a microtome | 3-10 μm thickness [12] [62] | Blocks are chilled on ice for easier, thinner sectioning. Sections are floated on a 40-45°C water bath, placed on slides, and dried overnight at 37°C [62]. |
Immunohistochemical Staining Protocol for FFPE Tissues
The following comprehensive protocol is designed for the detection of ubiquitination-related proteins, which often require careful antigen retrieval for optimal results.
Deparaffinization and Rehydration
Before staining, the paraffin wax must be completely removed and the tissue hydrated to allow antibody penetration.
- Deparaffinize: Immerse slides in two changes of xylene (or a xylene-substitute) for 10-15 minutes each [62].
- Rehydrate: Pass slides through a graded series of ethanols: 100% ethanol (two changes, 5 minutes each), 95% ethanol (two changes, 5 minutes each), 85% ethanol (5 minutes), 75% ethanol (5 minutes), and finally, water (three washes) [65] [62].
- Critical Note: From this point onward, the tissue sections must not be allowed to dry out, as this causes non-specific antibody binding and high background staining [62].
Antigen Retrieval
Formalin fixation creates methylene bridges that cross-link proteins and mask epitopes. Antigen retrieval is essential to break these cross-links and expose antigenic sites, a step particularly crucial for detecting ubiquitination targets [62] [64].
Table 2: Antigen Retrieval Methods
| Method | Buffer / Solution | Typical Conditions | Application Notes |
|---|---|---|---|
| Heat-Induced Epitope Retrieval (HIER) | 10 mM Sodium Citrate, pH 6.0 [12] [65] | Boil for 15-20 minutes, then cool to RT [12] | The most common method. Can be performed in a pressure cooker, microwave, or steamer [12]. |
| 1 mM EDTA, pH 8.0 [12] | Boil for 15 minutes, then cool to RT [12] | Often used for more challenging targets. | |
| 10 mM Tris/1 mM EDTA, pH 9.0 [12] | Boil for 20 minutes, then cool to RT [12] | Suitable for a range of phospho-specific and other antibodies. | |
| Protease-Induced Epitope Retrieval (PIER) | 0.05% Trypsin [12] or Proteinase K (20 μg/mL) [65] | 10-20 minutes at 37°C [12] [65] | Used for specific antigens susceptible to heat degradation. Digestion time must be carefully optimized to avoid tissue damage. |
Staining for Ubiquitination Targets
The following workflow details the steps for antibody incubation and detection. The specific conditions for ubiquitination-related primary antibodies (e.g., anti-USP7, anti-OTUB1) must be determined empirically.
Diagram 1: IHC Staining Workflow for FFPE Tissues
Blocking:
- Block Endogenous Peroxidase: If using an HRP-based detection system, incubate slides with 0.3% hydrogen peroxide in distilled water for 15-40 minutes at room temperature to quench endogenous peroxidase activity [65].
- Block Non-Specific Binding: Incubate sections with a blocking buffer, such as 10% normal serum from the species in which the secondary antibody was raised, for 1 hour at room temperature to prevent non-specific antibody binding [65].
Antibody Incubation:
- Primary Antibody: Dilute the primary antibody (e.g., anti-USP7) in blocking buffer. Apply to the tissue section and incubate overnight at 4°C in a humidified chamber [12] [65]. The optimal dilution must be determined by a dilution series.
- Wash: Wash slides three times in PBS or TBS buffer for 5-10 minutes each [12] [65].
- Secondary Antibody & Amplification: For unconjugated primary antibodies, incubate with a biotinylated secondary antibody for 1 hour at room temperature. Wash, then incubate with an avidin-biotin complex (ABC) reagent for 30 minutes [12] [65]. This step is not needed for directly conjugated primary antibodies.
Detection and Visualization:
- Chromogenic Development: Incubate sections with the chromogen 3,3’-Diaminobenzidine (DAB) for approximately 10 minutes, or until the desired brown color develops. Monitor closely under a microscope to prevent over-development [12] [65].
- Stop Reaction: Rinse slides in three changes of distilled water [12].
Counterstaining, Dehydration, and Mounting
- Counterstain: Immerse slides in Hematoxylin to stain cell nuclei blue [12] [65].
- Dehydrate and Clear: Pass slides through a reverse ethanol series to dehydrate: 70% ethanol, 90% ethanol, 100% ethanol (two changes), and finally xylene (two changes), for 3-5 minutes each [12] [65].
- Mount: Apply a resinous mounting medium and affix a coverslip. Allow slides to dry before microscopic analysis [12] [65].
The Scientist's Toolkit: Essential Reagents for Ubiquitination IHC
Table 3: Key Research Reagent Solutions for IHC
| Reagent / Solution | Function / Purpose | Example |
|---|---|---|
| 10% NBF | Cross-links and preserves tissue architecture and antigen integrity. | 10% Neutral Buffered Formalin [63] [62] |
| Antigen Retrieval Buffer | Breaks protein cross-links formed during fixation to expose hidden epitopes. | Sodium Citrate Buffer (pH 6.0) [12] [65] |
| Blocking Serum | Reduces non-specific background staining by blocking reactive sites. | 10% Normal Goat Serum [65] |
| Primary Antibody | Specifically binds to the protein target of interest. | Anti-USP7, Anti-OTUB1, Anti-TRIM28 [66] [15] [61] |
| Detection System | Amplifies the primary antibody signal for visualization. | Biotinylated Secondary Antibody + ABC Kit [12] [65] |
| Chromogen | Produces an insoluble colored precipitate at the antigen site. | 3,3’-Diaminobenzidine (DAB) [12] [65] |
| Counterstain | Provides contrast by staining non-target cellular components. | Hematoxylin [12] [65] |
Application in Ubiquitination Cancer Research: Linking Protocol to Biology
The robust detection of ubiquitination system components in FFPE tissues is pivotal for translating molecular findings into clinical insights. The following diagram illustrates how key ubiquitination regulators, detectable via IHC, influence oncogenic pathways.
Diagram 2: Ubiquitination Regulators in Cancer Signaling
Prognostic Biomarker Discovery: IHC analysis of ubiquitination-related proteins in FFPE patient cohorts can identify valuable prognostic markers. For example, overexpression of USP7 in gastric cancer tissues is correlated with poor disease-free survival, marking it as a potential biomarker [61]. Similarly, a ubiquitination-related prognostic signature (URPS) can stratify patients with lung, esophageal, and cervical cancers into distinct risk groups with different overall survival outcomes [66].
Mechanistic Insights into Tumor Progression: IHC enables the spatial localization of key players in oncogenic pathways. Research shows that the OTUB1-TRIM28 ubiquitination axis modulates the MYC pathway, influencing cancer cell fate, oxidative stress, and ultimately, patient prognosis [66]. Validating such findings requires precise detection of these proteins in FFPE tissue contexts.
Predicting and Understanding Therapy Response: The ubiquitination status of immune checkpoint proteins like PD-L1 directly impacts immunotherapy efficacy [66] [15]. IHC on FFPE tissues from patients receiving immunotherapy can help identify those more likely to benefit, guiding personalized treatment strategies.
Concluding Remarks
This detailed protocol for FFPE tissue processing and staining provides a foundational framework for high-quality immunohistochemical analysis in cancer research. When applied within the context of ubiquitination studies, it becomes a powerful tool for uncovering the roles of deubiquitinating enzymes, E3 ligases, and their substrates in tumorigenesis. The ability to reliably detect these targets in archived clinical samples bridges the gap between basic molecular research and clinical application, facilitating the discovery of novel prognostic biomarkers and therapeutic targets for drug development.
Application Note: USP11 IHC as a Prognostic Tool in Prostate Cancer
Background and Clinical Significance
Ubiquitin-specific protease 11 (USP11) plays a critical role as a deubiquitinating enzyme that maintains phosphatase and tensin homolog (PTEN) protein integrity by reversing its polyubiquitination, thereby inhibiting PI3K/AKT pathway activation and supporting its tumor-suppressive function [67]. In prostate cancer, the loss of USP11 expression is strongly associated with disease progression and poor clinical outcomes, making it a valuable prognostic biomarker [67].
Clinical validation studies have demonstrated that reduced USP11 staining intensity correlates significantly with established indicators of aggressive disease, including higher Gleason scores, elevated PSA titers, and advanced pathological stage [67]. Patients exhibiting positive USP11 staining experience significantly longer biochemical recurrence-free and clinical recurrence-free survival compared to those with negative staining, highlighting its prognostic utility in routine pathological assessment [67].
Quantitative Clinical Correlations of USP11 Expression
Table 1: Correlation Between USP11 IHC Staining Intensity and Clinicopathological Parameters in Prostate Cancer
| Clinical Parameter | USP11 Staining Pattern | Statistical Significance | Clinical Implications |
|---|---|---|---|
| Tissue Type | Lower in cancerous vs. benign peri-tumoral tissues | p < 0.001 | aids differentiation of malignant from normal tissue |
| PSA Titer | Lower staining with higher PSA levels | p < 0.001 | indicator of disease burden |
| Gleason Score | Lower staining with higher scores | p < 0.001 | marker of tumor aggressiveness |
| Pathologic Stage | Lower staining with advanced stage | p < 0.001 | predictor of disease progression |
| Lymph Node Involvement | Lower staining with node positivity | p < 0.001 | indicator of metastatic spread |
| Survival Outcomes | Positive staining associated with longer recurrence-free survival | p < 0.001 | independent prognostic factor |
Detailed IHC Protocol for USP11
Tissue Preparation and Staining Procedure
- Tissue Microarray Construction: 286 tissue microarrays were constructed, including 20 for adjacent non-neoplastic tissues and 266 for prostate cancer tissues [67].
- Sectioning: Cut formalin-fixed, paraffin-embedded (FFPE) tissue sections at 4μm thickness.
- Deparaffinization and Rehydration: Use xylene and graded ethanol series (100%, 95%, 70%) [67].
- Antigen Retrieval: Perform heat-induced epitope retrieval using citrate buffer (pH 6.0) [67].
- Primary Antibody Incubation: Incubate with anti-USP11 antibody overnight at 4°C [67].
- Detection System: Use Novolink Max Polymer Detection kit with appropriate secondary antibodies [67].
- Visualization: Develop with DAB chromogen and counterstain with hematoxylin [67].
Scoring and Interpretation
A pathologist blinded to clinical outcome data should score the staining using a binary system (positive or negative) [67]. The staining intensity should be evaluated consistently across tissue cores, with careful attention to nuclear and cytoplasmic localization patterns.
Application Note: UBE2C IHC in Breast Cancer Diagnosis and Prognosis
Biological Rationale and Clinical Relevance
Ubiquitin-conjugating enzyme E2C (UBE2C) is a key component of the ubiquitin-proteasome system that regulates cell cycle progression through mitotic cyclin degradation [68]. In breast cancer, UBE2C overexpression drives tumor aggressiveness by promoting proliferation, migration, invasion, and metastasis through regulation of the JNK signaling pathway [69] [70].
Comprehensive studies across multiple large cohorts including METABRIC (n=1,980), TCGA (n=854), and Kaplan-Meier Plotter (n=3,951) have consistently demonstrated that high UBE2C expression correlates with poor prognosis across all molecular subtypes, with the strongest associations in HER2-enriched and triple-negative breast cancers [68]. UBE2C overexpression is significantly associated with features of aggressive disease, including high tumor grade, large tumor size, lymphovascular invasion, hormone receptor negativity, and HER2 positivity [68].
Quantitative Biomarker Correlations of UBE2C
Table 2: UBE2C Expression Associations with Breast Cancer Biomarkers and Outcomes
| Parameter | UBE2C Association | Statistical Significance | Clinical Utility |
|---|---|---|---|
| Molecular Subtypes | Highest in HER2-enriched and TNBC | p < 0.001 | identifies aggressive subtypes |
| E-cadherin | Negative correlation | p < 0.001 | indicates EMT activation |
| N-cadherin | Positive correlation | p < 0.001 | confirms mesenchymal phenotype |
| Matrix Metalloproteinases | Positive correlation | p < 0.001 | reflects invasion potential |
| Cell Cycle Markers | Positive with p53, Ki67, EGFR, PI3K | p < 0.001 | indicates proliferation drive |
| Patient Survival | Independent predictor of poor outcome | HR = 1.45, 95% CI 1.10-1.93 | prognostic stratification |
Comprehensive IHC Protocol for UBE2C
Tissue Processing and Staining
- Antibody Validation: Validate UBE2C antibody (WHO0011065M1, Sigma-Aldrich, 1:300) using immunoblotting with SKBR3 human BC cells, showing a single specific band at ~20 kDa [68].
- Tissue Section Preparation: Cut FFPE sections at 4-5μm thickness.
- Deparaffinization: Use xylene and ethanol series following standard protocols.
- Antigen Retrieval: Perform citrate antigen retrieval (pH 6.0) [68].
- Primary Antibody Incubation: Incubate with UBE2C antibody (1:100 dilution) overnight at 4°C [68].
- Detection System: Apply Novolink Max Polymer Detection kit with appropriate incubation times [68].
- Visualization: Develop with DAB and counterstain with hematoxylin.
Scoring System and Quality Control
- Digital Scanning: Scan stained slides using high-resolution digital scanner (NanoZoomer) at 20× magnification [68].
- Semi-quantitative Assessment: Use the H-score method: (staining intensity 0-3) × (percentage of positive tumor cells) [68].
- Intensity Categories: 0 (no staining), 1 (weak), 2 (moderate), 3 (strong) [68].
- Final H-score Range: 0-300, with median cutoff of 20 for low vs. high expression [68].
- Quality Control: Exclude cores with <15% tumor area or folded tissue; perform blind double-scoring by two researchers to ensure interobserver concordance [68].
UBE2C in Breast Cancer Signaling Pathways
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Reagent Solutions for Ubiquitination Pathway IHC
| Reagent | Specifications | Application | Function |
|---|---|---|---|
| Anti-USP11 Antibody | Validated for IHC on FFPE tissues | Prostate cancer staining | Detects USP11 deubiquitinase expression |
| Anti-UBE2C Antibody | Sigma-Aldrich WHO0011065M1, 1:300 dilution | Breast cancer staining | Identifies UBE2C conjugating enzyme |
| Novolink Max Polymer | Polymer-based detection system | Both protocols | Enhances sensitivity and specificity |
| Citrate Buffer (pH 6.0) | Standard antigen retrieval solution | Both protocols | Exposes target epitopes in FFPE tissues |
| DAB Chromogen | Liquid DAB substrate system | Both protocols | Visualizes antibody binding |
| β-actin Antibody | Clone AC-15, 1:5000 dilution | Western blot control | Housekeeping protein for normalization |
Discussion and Clinical Implications
The implementation of standardized IHC protocols for USP11 in prostate cancer and UBE2C in breast cancer provides valuable tools for diagnostic pathology and therapeutic decision-making. The complementary nature of these biomarkers - where loss of USP11 function and gain of UBE2C function both indicate aggressive disease - highlights the critical balance of ubiquitination processes in cancer pathogenesis.
For USP11, the straightforward binary scoring system (positive/negative) facilitates integration into routine pathological assessment, while the H-score method for UBE2C allows for more granular quantification of expression levels. Both assays demonstrate robust performance on FFPE tissue sections, making them widely applicable in clinical diagnostic laboratories.
The strong association of these biomarkers with therapeutic resistance and disease recurrence suggests potential utility in guiding treatment intensity and surveillance strategies. Additionally, the involvement of both biomarkers in key signaling pathways (PTEN/PI3K for USP11 and JNK for UBE2C) reveals opportunities for targeted therapeutic interventions that may reverse their oncogenic effects.
Solving Common IHC Challenges: From High Background to Lack of Staining
In the field of cancer research, particularly in studies focusing on ubiquitination, immunohistochemistry (IHC) serves as a critical technique for visualizing the distribution and abundance of specific molecules within the context of tissue morphology [71]. The unique value of IHC lies in its ability to confirm target molecule expressions, such as ubiquitinated proteins, without destroying the histological architecture, allowing for assessment within the tissue microenvironment [71]. However, researchers often encounter a significant challenge: a lack of specific staining. This issue can stem from problems related to antigen integrity or antibody viability, potentially leading to false-negative results and misinterpretation of data. This is especially critical when working with ubiquitination-specific antibodies, where proper staining is essential for exploring biomarkers and therapeutic targets in cancer. This article provides detailed protocols and application notes to diagnose and resolve these common IHC problems, framed within the context of ubiquitination research.
Core Principles: Antigen Integrity and Antibody Viability
Successful IHC staining depends on the preservation of the target antigen in the tissue section and the effective binding of a viable, specific antibody to that antigen.
- Antigen Integrity refers to the preservation of the target epitope's structure and accessibility throughout tissue processing and staining. Factors like improper fixation, over-fixation, or prolonged ischemia can degrade or mask the antigen [71].
- Antibody Viability concerns the ability of the primary antibody to bind its target epitope with high affinity and specificity. Loss of potency can occur due to protein degradation, denaturation from improper storage, microbial contamination, or repeated freeze-thaw cycles [72].
A failure in either of these components can lead to a lack of specific staining. The following sections provide a systematic approach to diagnosing and resolving these issues.
Diagnostic Workflow and Experimental Protocols
A structured diagnostic approach is crucial for identifying the root cause of poor staining. The diagram below outlines a logical troubleshooting pathway.
Protocol: Validation Using Positive and Negative Controls
Always include control slides to assess the performance of your staining reagents and methods [73].
- Positive Control: Use a tissue or cell pellet known to express the target antigen at high levels (e.g., a known ubiquitin-positive cancer sample). Its proper staining confirms that the antibody and procedure are working.
- Negative Control: Omit the primary antibody or use an isotype control. This helps identify non-specific background staining from the detection system or secondary antibody cross-reactivity [72].
- Procedure:
- Process control and test samples simultaneously using the same reagents.
- If the positive control fails to stain, the issue lies with the antibody or IHC protocol.
- If the positive control stains correctly but the test sample does not, the issue is likely with the antigen integrity in the test sample or its expression level.
Protocol: Assessing and Optimizing Antigen Retrieval
Epitopes can be masked during formaldehyde-based fixation due to protein cross-linking. Heat-Induced Epitope Retrieval (HIER) is the most widely used method to reverse this [71].
- Test Different Retrieval Methods: Compare staining results using:
- Test Different Retrieval Buffers:
- Enzymatic Retrieval: For a limited set of antigens (e.g., some cytokeratins), try enzymatic retrieval with trypsin or proteinase K for 10-20 minutes at 37°C [71].
Protocol: Titrating the Primary Antibody
Both overly high and overly low antibody concentrations can cause a lack of specific staining [72].
- Prepare a Dilution Series: Using the manufacturer's recommended dilution as a starting point, prepare a series of dilutions (e.g., 1:10, 1:50, 1:100, 1:200, 1:500).
- Stain Consecutive Sections: Apply each dilution to consecutive tissue sections from the same block, ensuring all other protocol steps are identical.
- Analyze Results: Identify the dilution that provides the strongest specific signal with the lowest background. Extremely high concentrations can cause a "prozone effect," paradoxically reducing signal [72].
Protocol: Verifying the Detection System
A weak or inactive detection system will result in no signal, even if the antibody binding occurs.
- Test Enzyme-Substrate Reactivity: Place a drop of the enzyme (e.g., HRP) on nitrocellulose and dip it into the prepared substrate. A colored spot should form immediately if both are active [72].
- Use Polymer-Based Detection: Polymer-based detection reagents are more sensitive than traditional avidin/biotin-based systems and can enhance signal [73].
- Check Substrate Buffer pH: Ensure the pH of the substrate buffer is appropriate for the specific chromogen being used (e.g., DAB) [72].
Quantitative Data and Troubleshooting Guide
The following table consolidates key quantitative findings from relevant literature and critical thresholds for IHC troubleshooting.
Table 1: Quantitative Data from Ubiquitination Research and IHC Thresholds
| Parameter / Finding | Quantitative Value / Description | Context & Significance |
|---|---|---|
| uH2B in LUAD vs Normal [74] | 92.6% (150/162) of LUAD tissues showed negative/weak uH2B staining vs. 96.5% (55/57) of normal tissues with robust staining (p < 0.0001). | Demonstrates profound loss of a specific ubiquitination mark (uH2B) in lung adenocarcinoma, establishing it as a relevant biomarker. |
| Survival Correlation [74] | Low uH2B expression correlated with significantly poorer overall and progression-free survival in LUAD patients. | Highlights the prognostic value of accurately detecting ubiquitination marks via IHC. |
| RNF20 & DNA Damage [74] | RNF20 knockdown impaired DNA damage repair, increasing sensitivity to cisplatin and PARP inhibitor Olaparib. | Suggests IHC for RNF20/uH2B could help identify patients who may benefit from specific targeted therapies. |
| Minimum Text Contrast [75] | WCAG enhanced contrast requirement: ≥ 4.5:1 for large text, ≥ 7.0:1 for other text. | A guideline for ensuring sufficient color contrast in generated diagrams and figures for publication and presentation. |
| Fixation Time [71] | Recommendation: 10% Neutral Buffered Formalin for ~24 hours at room temperature. | Standard protocol to preserve antigen integrity; under- or over-fixation can mask epitopes. |
| Section Thickness [71] | Recommendation: ~4 μm for paraffin sections. | Thicker sections can cause higher background and reduce reagent penetration. |
Table 2: Troubleshooting Guide for Lack of Specific Staining
| Problem Category | Potential Cause | Recommended Solution |
|---|---|---|
| Antigen Integrity | Prolonged ischemia before fixation [71] | Minimize ischemic time, especially for sensitive antigens (e.g., Ki-67, phosphoproteins). Rapid fixation is critical. |
| Over-fixation [71] | Adhere to recommended 24-hour fixation in 10% NBF. Overfixation can cause irreversible epitope damage. | |
| Inadequate antigen retrieval [73] | Optimize HIER method and buffer. Use microwave or pressure cooker, not a water bath. Test different pH conditions. | |
| Epitope degradation during slide storage [71] | Use freshly cut sections. If storage is necessary, store at 4°C protected from oxidants. | |
| Antibody Viability | Antibody degradation/denaturation [72] | Aliquot antibodies to avoid freeze-thaw cycles. Store according to manufacturer's instructions. Check expiration dates. |
| Incorrect antibody concentration [72] | Perform a titration experiment to determine the optimal dilution for your specific tissue and conditions. | |
| Incompatible antibody diluent [73] | Use the diluent recommended by the antibody manufacturer. Titration may be required if a different diluent is used. | |
| Detection System | Inactive enzyme (HRP/AP) or substrate [72] | Test enzyme-substrate reactivity on nitrocellulose. Ensure buffers (e.g., for DAB) are prepared correctly and are not contaminated. |
| Inhibition of secondary antibody [72] | If the secondary concentration is too high, it can inhibit binding. Test decreasing concentrations. | |
| Endogenous enzyme activity not blocked [72] | Quench endogenous peroxidases with 3% H₂O₂ for 10 minutes. Block endogenous alkaline phosphatase with levamisole. |
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Research Reagent Solutions for Ubiquitination IHC
| Reagent / Material | Function & Application Notes |
|---|---|
| 10% Neutral Buffered Formalin (NBF) | Standard fixative for tissue preservation. Maintains morphology but can mask epitopes, necessitating antigen retrieval. |
| Sodium Citrate Buffer (pH 6.0) | A common antigen retrieval buffer used in HIER to break cross-links and unmask epitopes [72]. |
| Protein Blocking Serum | Reduces nonspecific background staining by blocking reactive sites on the tissue. Use 5-10% normal serum from the species of the secondary antibody [71]. |
| Ubiquitination-Specific Primary Antibodies (e.g., anti-uH2B) | Key reagents for detecting specific ubiquitin marks. Must be validated for IHC application. Proper storage and titration are critical for viability [74]. |
| Polymer-Based Detection System | A highly sensitive detection method that avoids endogenous biotin issues and provides superior signal amplification compared to biotin-based systems [73]. |
| DAB (3,3'-Diaminobenzidine) Chromogen | A stable, chromogenic substrate for HRP that produces a brown, insoluble precipitate at the site of antibody binding, visible under a microscope [71]. |
| Hematoxylin Counterstain | A blue stain that labels cell nuclei, providing morphological context to the specific brown DAB signal [71]. |
Case Study: RNF20 and uH2B in Lung Adenocarcinoma
The following experimental workflow, derived from a study on RNF20 and uH2B in lung adenocarcinoma (LUAD), illustrates a successful application of IHC in ubiquitination cancer research [74].
Key Experimental Protocols from the Case Study [74]:
- IHC Staining & Scoring: Performed IHC on 162 LUAD and matched normal tissues. Nuclear uH2B immunostaining was scored, with a score < 6 defined as low expression. This quantitative scoring allowed for correlation with patient prognosis.
- RNF20 Knockdown: A549 cells were transfected with lentivirus carrying RNF20-specific shRNA. Knockdown efficiency and its effect on uH2B levels were confirmed by Western blot.
- Functional Assays:
- Proliferation: Cell proliferation was measured using CCK-8 assay at 24, 48, and 72 hours.
- Migration: A scratch (wound healing) assay was performed, with migration into the scratch area measured at 0, 24, and 36 hours.
- DNA Damage Repair: γH2AX and RAD51 expression were analyzed by IHC and/or Western blot in control and RNF20-knockdown cells at various time points (1h, 4h, 24h) after irradiation.
Diagnosing and resolving a lack of specific staining in IHC requires a systematic approach that meticulously evaluates both antigen integrity and antibody viability. By implementing robust protocols for validation controls, antigen retrieval optimization, antibody titration, and detection system verification, researchers can ensure the reliability of their data. This is paramount in advancing cancer research, particularly in the nuanced field of ubiquitination, where accurate detection of marks like uH2B can reveal critical insights into tumor behavior, patient prognosis, and potential therapeutic strategies.
In the specialized field of cancer research utilizing ubiquitination-specific antibodies for immunohistochemistry (IHC), achieving high signal-to-noise ratio is paramount for accurate data interpretation. High background staining can obscure specific signals, leading to erroneous conclusions about protein localization and expression levels of ubiquitination pathway components in tumor tissues. This application note provides detailed protocols for two fundamental approaches to minimize background: optimizing blocking strategies and performing antibody titration, with specific consideration for ubiquitination targets in cancer pathology.
The ubiquitin-proteasome system (UPS) regulates critical cellular processes including cell cycle control, DNA damage repair, and apoptosis, with dysregulation strongly linked to carcinogenesis [14]. Investigating ubiquitination-related biomarkers such as MMP1, RNF2, TFRC, SPP1, and CXCL8—identified as significantly associated with cervical cancer outcomes—requires precise IHC visualization [48]. Similarly, studying deubiquitinating enzymes like USP2, which shows significantly reduced expression in gastric cancer cells and patient samples, demands techniques that preserve specific signal while minimizing non-specific background [19].
The Science of Background Staining
Causes of High Background in IHC
Non-specific background staining in IHC arises from multiple factors, primarily through non-specific antibody binding, inadequate blocking of endogenous activities, or suboptimal washing procedures. In the context of ubiquitination research, where targets may have both nuclear and cytoplasmic localization, these challenges are particularly pronounced.
The primary mechanisms include:
- Non-specific antibody binding: Antibodies may bind non-specifically to tissue components through ionic, hydrophobic, or van der Waals interactions, or through binding to Fc receptors present in certain tissues [71].
- Inadequate blocking: Insufficient blocking of non-specific binding sites allows antibodies to attach to areas without the target antigen [76].
- Endogenous enzyme activity: Unblocked endogenous peroxidase or alkaline phosphatase activities generate signal independent of antibody binding [71].
- Overfixation: Excessive cross-linking from prolonged formaldehyde fixation can mask epitopes while simultaneously increasing non-specific background [47].
- Antibody concentration: Excessive primary or secondary antibody concentrations saturate specific binding sites and promote non-specific binding [76] [77].
Table 1: Troubleshooting Common Causes of High Background in Ubiquitination IHC
| Cause | Effect on Signal | Solution |
|---|---|---|
| Insufficient blocking | Uniform background across tissue section | Increase blocking agent concentration or duration; use normal serum from secondary antibody species [76] [71] |
| Endogenous enzyme activity | Background particularly pronounced in erythrocytes and granulocytes | Block with 3% H₂O₂ for peroxidase; levamisol for alkaline phosphatase [71] |
| Primary antibody concentration too high | High signal with poor localization to expected cellular compartments | Perform antibody titration to determine optimal dilution [76] [77] |
| Inadequate washing | Irregular staining patterns with higher background around tissue edges | Increase wash volume, frequency, and duration; incorporate detergent (e.g., 0.01-0.1% Tween-20) [76] [78] |
| Overfixation | Weak specific signal with generalized background | Optimize fixation time; employ antigen retrieval techniques [71] [47] |
Blocking Strategies for Ubiquitination IHC
Blocking Agent Selection
Effective blocking requires using agents that occupy non-specific binding sites without interfering with antigen-antibody interactions. Selection should be based on tissue type, antibody characteristics, and detection system.
Blocking Strategy Selection
Protocol: Optimized Blocking for Ubiquitination IHC
Materials:
- Normal serum from species of secondary antibody
- Protein blocking buffer (1-5% BSA in PBS)
- Tris-buffered saline with Tween-20 (TBS-T)
- Hydrogen peroxide (3% in methanol)
- Levamisol (for alkaline phosphatase systems)
Procedure:
- Deparaffinize and rehydrate tissue sections following standard protocols [79].
- Perform antigen retrieval using appropriate method (heat-induced or enzymatic) optimized for your ubiquitination target [71].
- Block endogenous peroxidases by incubating with 3% H₂O₂ for 10-15 minutes at room temperature [71].
- Wash slides 2×3 minutes with TBS-T.
- Apply protein block using 5-10% normal serum from the same species as the secondary antibody OR commercial blocking solution for 1 hour at room temperature in a humidity chamber [71].
- TIP: For tissues with high Fc receptor expression (lymphoid tissues, bone marrow), use F(ab')₂ fragments instead of whole IgG molecules or include specific Fc receptor blocking [71].
- Remove blocking solution by tapping slides; do not wash before antibody application.
- Proceed immediately with primary antibody application.
Troubleshooting Notes:
- If background persists, try increasing blocking time to overnight at 4°C [71].
- For tissues with high endogenous biotin (frozen sections), use an endogenous biotin blocking kit [71].
- When switching sample types (e.g., from cell culture to serum), re-optimize blocking as matrix effects can significantly impact background [78].
Antibody Titration for Optimal Signal
Principles of Antibody Titration
Antibody titration is essential for identifying the concentration that provides maximal specific signal with minimal background. For ubiquitination targets, which may have variable expression levels in cancer tissues, optimal dilution is critical for accurate assessment.
The fundamental principle is that insufficient antibody results in weak specific signal, while excess antibody increases non-specific binding and background [77]. The optimal concentration achieves the highest signal-to-noise ratio, typically slightly below saturation point.
Table 2: Antibody Titration Series Example
| Tube | Starting Concentration | Dilution Factor | Final Concentration | Expected Result |
|---|---|---|---|---|
| 1 | 5 µg/mL | - | 5 µg/mL | High background, potentially saturated signal |
| 2 | 5 µg/mL | 1:2 | 2.5 µg/mL | Strong signal, moderate background |
| 3 | 5 µg/mL | 1:4 | 1.25 µg/mL | Optimal signal-to-noise |
| 4 | 5 µg/mL | 1:8 | 0.625 µg/mL | Good resolution, slightly weak signal |
| 5 | 5 µg/mL | 1:16 | 0.3125 µg/mL | Weak specific signal |
| 6 | 5 µg/mL | 1:32 | 0.156 µg/mL | Minimal detectable signal |
| 7 | - | No antibody | - | Background control |
Protocol: Antibody Titration for Ubiquitination Targets
Materials:
- Primary antibody (ubiquitination-specific)
- Secondary antibody compatible with detection system
- Positive control tissue (known to express target)
- Negative control tissue (known absent target)
- Staining equipment and reagents
Procedure:
- Prepare a titration series of the primary antibody using at least 6 points with 1:2 dilutions plus an unstained control [77].
- Use the same conditions as your final experiment (temperature, incubation time, cell type, and number) [77].
- Include a positive control antibody with known performance to validate the staining process.
- Process all slides simultaneously to minimize technical variation.
- Stain tissues following standardized IHC protocol with identical incubation times and conditions for all slides.
- Develop and counterstain all slides simultaneously.
Antibody Titration Workflow
Data Analysis and Interpretation
Quantitative Analysis:
- Acquire images of stained tissues using consistent microscope settings across all samples.
- Measure staining intensity using image analysis software (e.g., Fiji ImageJ) [79].
- For each dilution, measure the median fluorescence intensity (MFI) for both positive and negative cell populations.
- Calculate the Separation Index for each concentration using the formula:
Separation Index = (MFIpositive - MFInegative) / (84thpercentilenegative - 16thpercentilenegative) [77]
- Identify the optimal concentration that yields the highest Separation Index.
Validation:
- Repeat titration for each new antibody lot [77].
- Verify optimal concentration in multiple tissue samples with varying expression levels.
- Confirm specificity using appropriate negative controls.
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Reagents for Ubiquitination IHC Optimization
| Reagent Category | Specific Examples | Function & Application Notes |
|---|---|---|
| Blocking Agents | Normal serum, BSA, non-fat dry milk, commercial blockers | Reduce non-specific binding; select based on secondary antibody species and detection system [71] |
| Wash Buffers | TBS-T, PBS-T (0.01-0.1% Tween-20) | Remove unbound antibodies; higher detergent concentrations reduce background but may affect epitope integrity [76] [78] |
| Antigen Retrieval Reagents | Citrate buffer (pH 6.0), Tris-EDTA (pH 9.0), proteinase K | Reverse formaldehyde cross-linking; optimal method must be determined empirically for each ubiquitination target [71] [79] |
| Detection Systems | HRP-based, AP-based, polymer systems | Signal generation; polymer systems often provide higher sensitivity with lower background [47] |
| Primary Antibodies | Ubiquitination-specific (anti-ubiquitin, anti-K48, anti-K63, etc.) | Target recognition; validate specificity for ubiquitination research using appropriate controls [48] [19] |
Implementing systematic blocking strategies and antibody titration protocols is essential for generating reliable, reproducible IHC data in ubiquitination cancer research. The optimal conditions must be determined empirically for each antibody-tissue combination, particularly when studying ubiquitination pathway components that may have complex subcellular localization patterns in cancer tissues. By following these detailed protocols, researchers can significantly improve signal-to-noise ratio, enabling more accurate assessment of ubiquitination-related biomarkers in cancer development, progression, and therapeutic response.
In the field of cancer research, particularly in studies investigating ubiquitination-specific antibodies for immunohistochemistry (IHC), the quality of tissue morphology directly determines the reliability and interpretability of experimental results. Suboptimal tissue fixation and sectioning introduce significant artifacts that compromise protein localization, epitope preservation, and quantitative analysis of ubiquitination patterns—processes now recognized as fundamental to cancer hallmarks including immune evasion, metabolic reprogramming, and therapeutic resistance [43] [44]. The ubiquitin-proteasome system (UPS) regulates approximately 80-90% of cellular proteolysis, with ubiquitin-specific proteases (USPs) representing the largest family of deubiquitinating enzymes [43] [44]. Accurate visualization of these components via IHC requires impeccable tissue preservation to prevent misinterpretation of protein stability, localization, and expression levels that are crucial for understanding cancer mechanisms and developing targeted therapies.
Table 1: Impact of Pre-Analytical Variables on Ubiquitination IHC
| Pre-Analytical Variable | Effect on Tissue Morphology | Impact on Ubiquitination Detection |
|---|---|---|
| Delayed Fixation | Autolysis, cytoplasmic vacuolization, nuclear pyknosis | Altered ubiquitin conjugate distribution, false-negative USP staining |
| Inadequate Fixation Time | Incomplete preservation, shrinkage artifacts | Epitope masking, unreliable quantification of HER2 and PD-L1 ubiquitination status |
| Incorrect Fixative pH | Poor nuclear detail, cytoplasmic basophilia | Impaired detection of nuclear ubiquitination events (e.g., histone modifications) |
| Section Thickness Variation | Uneven staining, cellular overlapping | Inaccurate stereological counts, compromised quantification of protein expression levels |
| Knife Chatter & Compression | Tissue folds, linear basophilic streaks | Mechanical disruption of cellular architecture where UPS components localize |
Optimizing Fixation Protocols for Ubiquitination Studies
Fixative Composition and Temperature Optimization
Recent experimental research has systematically evaluated fixation conditions for optimal preservation of delicate cellular structures. A 2025 study investigating paraffin sectioning techniques for complex tissues compared three fixative solutions under different temperature conditions, demonstrating that a mixture of 1% paraformaldehyde and 1.25% glutaraldehyde at 4°C provided superior preservation of ocular structures compared to Davidson's solution or 4% paraformaldehyde alone [80]. The mixed solution maintained a smooth tissue surface, preserved lens transparency, and yielded significantly higher scores for critical structures including Zinn's zonule and retinal morphology, with anterior segment total scores of 27.67±4.74 compared to 22.83±2.98 for Davidson's solution and 23.17±3.04 for formaldehyde alone [80]. For ubiquitination research, this enhanced structural preservation is crucial for accurate subcellular localization of ubiquitin conjugates and deubiquitinating enzymes such as USP7, which shuttles between nuclear and cytoplasmic compartments and requires impeccable morphology for valid interpretation of its functions in cancer immunity [43].
Pre-Fixation Treatments and Tissue Processing
The same study demonstrated that appropriate pre-fixation treatments significantly enhance morphological preservation. A clinical approach involving a 0.5-cm corneal limbal incision prior to fixation yielded superior preservation of delicate structures including the ciliary body (scoring 7.04±1.30), Zinn's zonule (2.96±0.95), and retina (5.17±1.58) compared to more invasive hemisection approaches [80]. For ubiquitination research, such optimized pre-fixation treatments help preserve labile protein modifications and prevent the rapid deubiquitination that can occur post-excision, particularly for phospho-ubiquitin signatures and Met1-linear ubiquitin chains that play critical roles in NF-κB signaling and cancer progression [44].
Diagram 1: Optimal Tissue Processing Workflow for Ubiquitination IHC (Short title: Ubiquitination IHC Workflow)
Advanced Sectioning Techniques and Quality Control
Precise Section Thickness Measurement
Accurate section thickness is paramount for quantitative stereological analyses in ubiquitination research, particularly when applying physical disector methods to estimate numerical densities of ubiquitin-positive structures. Conventional orthogonal re-embedding (ORE) techniques for thickness measurement have been improved by incorporating a calibration foil of known thickness, allowing for mathematical correction of obliquely sectioned samples [81]. However, spectral reflectance (SR) measurement has emerged as a more practicable and precise alternative, demonstrating less than 1% deviation from ORE measurements while requiring only seconds to perform [81]. This method enables researchers to verify that section thickness matches the nominal microtome setting, which is crucial for disector analyses where the counting volume is defined by section thickness and the area of the counting frame [81]. For ubiquitination studies, this precision ensures accurate quantification of ubiquitin-positive foci, particularly when investigating small structures such as nuclear dots or cytoplasmic inclusions that may represent aggressive assemblies or signaling complexes in cancer cells.
Table 2: Section Thickness Measurement Techniques Comparison
| Method | Principle | Accuracy | Time Requirement | Applications |
|---|---|---|---|---|
| Spectral Reflectance (SR) | Optical interference pattern analysis | <1% deviation from reference | Seconds | Plastic sections (0.5-3μm), ideal for routine QC |
| Orthogonal Re-embedding (ORE) with Calibration Foil | Geometric calculation from oblique sections | High (with angle correction) | Days (processing, embedding, sectioning) | Validation studies, method calibration |
| Nominal Microtome Setting | Mechanical advancement precision | Highly variable (up to 50% error) | None | Preliminary sectioning only (requires verification) |
Minimizing Sectioning Artifacts
Sectioning-induced distortions such as compression, chatter, and knife marks significantly compromise the assessment of tissue architecture and ubiquitin staining patterns. These artifacts are particularly problematic when evaluating the tumor microenvironment where USP7-mediated regulation of Treg cells and tumor-associated macrophages occurs in specific spatial contexts [43]. Methods to minimize these artifacts include proper knife alignment, optimized cutting speed and angle, and appropriate tissue support through optimal embedding. Furthermore, the application of statistical models for deformation analysis, such as Rayleigh-Bessel distributions for anisotropic deformations, can help researchers identify and account for preparation-induced tissue distortions in their quantitative analyses [82].
Integration with Ubiquitination-Specific Cancer Research
Implications for USP and Immune Marker Analysis
The UPS plays a critical role in regulating immune checkpoint proteins, with USP7 and USP2 directly modulating PD-1/PD-L1 stability through deubiquitination [43] [44]. Suboptimal tissue morphology artificially alters the apparent subcellular localization and expression levels of these proteins, potentially leading to incorrect conclusions about their regulation in the tumor microenvironment. For instance, USP7 stabilizes Foxp3 in regulatory T cells and modulates T-cell activation through deubiquitination of Tip60 [43]. Proper fixation is essential to preserve these delicate immune cell populations and their spatial relationships within tumor tissues. Furthermore, the College of American Pathologists has recently updated cancer biomarker reporting protocols, including specific guidance for HER2 testing in non-small cell lung cancer and other solid tumors [83] [84]. Since ubiquitination directly affects the stability and trafficking of HER2 and other therapeutic targets, high-quality tissue sections are prerequisite for accurate biomarker assessment and treatment selection.
Quality Control for Advanced Imaging Techniques
As super-resolution microscopy approaches enable visualization of single proteins in dense cellular clusters, the requirements for tissue preservation have become increasingly stringent. Recent advancements in quantification of absolute labeling efficiency at the single-protein level highlight the critical importance of optimizing binder labeling efficiency, which is significantly affected by fixation quality [85]. Studies evaluating nanobody labeling efficiencies for various tags revealed substantial variations, from nearly 50% for anti-GFP (clone 1H1) to below 10% for anti-mEOS2 (clone 1E8) [85]. These efficiencies can be improved to 62±5% by combining two nanobody clones targeting distinct epitopes, and further enhanced to 76±8% by concatenating tags [85]. For ubiquitination research, these findings underscore the necessity of optimal tissue morphology to achieve sufficient labeling efficiency for accurate quantification of ubiquitin chain types and their spatial organization within cancer cells.
Diagram 2: Variables Affecting Ubiquitination IHC Quality (Short title: Ubiquitination IHC Quality Variables)
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Research Reagent Solutions for Ubiquitination IHC
| Reagent/Material | Function | Application Notes |
|---|---|---|
| Paraformaldehyde-Glutaraldehyde Mixed Fixative | Protein cross-linking with structural stabilization | Optimal: 1% PFA + 1.25% glutaraldehyde at 4°C; preserves delicate structures for USP localization [80] |
| CALFA-Tag Nanobody System | Reference tag for labeling efficiency quantification | Enables precise determination of binder labeling efficiency (≥76% with concatenated tags) [85] |
| DNA-Conjugated Primary Antibodies | Multiplexed detection via Exchange-PAINT | Site-specific conjugation (transglutaminase vs GlyCLICK) affects efficiency; critical for quantifying ubiquitin chain types [85] |
| Spectral Reflectometer | Non-contact section thickness measurement | Enables rapid QC (seconds per measurement) with <1% deviation; essential for disector-based quantification [81] |
| Calibration Foils for ORE | Reference standard for section thickness validation | Allows mathematical correction for oblique sectioning angles in traditional thickness measurement [81] |
| CAP Biomarker Reporting Templates | Standardized documentation of IHC results | Ensures consistent reporting of HER2, PD-L1, and other biomarkers affected by ubiquitination [83] [84] |
Addressing suboptimal tissue morphology through optimized fixation and sectioning protocols is not merely a technical concern but a fundamental requirement for advancing our understanding of ubiquitination processes in cancer biology. As research continues to elucidate the complex roles of USPs in regulating immune checkpoints, metabolic reprogramming, and therapeutic resistance, the demand for precise protein localization and quantification will only increase. The protocols and quality control measures outlined here provide a foundation for generating reliable, reproducible data in ubiquitination-focused cancer research, ultimately supporting the development of novel therapeutic strategies targeting the ubiquitin-proteasome system.
Within the framework of investigating ubiquitination pathways in cancer, achieving an optimal signal-to-noise ratio (S/N) in immunohistochemistry (IHC) is paramount for generating reliable and interpretable data. Immunohistochemistry allows for the visualization of target molecule distribution within the context of the tissue microenvironment, a feature that is particularly valuable for studying the subcellular localization of ubiquitinated proteins in cancer biopsies [71]. However, the technique is fraught with potential variables that can compromise results through high background staining (noise) or weak specific signal [86]. This application note provides detailed protocols and data-driven strategies for optimizing key parameters—incubation time, temperature, and detection systems—to enhance the S/N ratio, with a specific focus on applications using ubiquitination-specific antibodies in cancer research.
The Scientist's Toolkit: Essential Research Reagent Solutions
The following table details key reagents and their critical functions in optimizing IHC experiments for ubiquitination markers in cancer samples.
Table 1: Key Research Reagent Solutions for IHC Optimization
| Reagent Solution | Function & Importance in Optimization |
|---|---|
| Cell Line-Based FFPE Controls | Provides highly consistent reference materials for assessing staining sensitivity and specificity across experimental runs; essential for normalizing results in quantitative studies of ubiquitination [87]. |
| Polymer-Based Detection Systems | Offers superior sensitivity and lower background compared to traditional avidin-biotin complex (ABC) systems, thereby improving S/N. This is crucial for detecting low-abundance ubiquitinated proteins [87]. |
| Basic Epitope Retrieval Solution | Effectively unmask cross-linked epitopes in formalin-fixed, paraffin-embedded (FFPE) tissues. For over 80% of antibodies, basic retrieval solutions provide a stronger specific signal, forming the foundation for a high S/N ratio [87]. |
| Highly Cross-Adsorbed Secondary Antibodies | Minimizes non-specific cross-reactivity with endogenous immunoglobulins or non-target serum proteins in tissue sections, a key factor in reducing background noise [88]. |
| Fluorophore-Conjugated Antibodies with Optimized DOL | Antibodies conjugated with a defined Degree of Labeling (DOL) ensure a bright, specific signal without the increased background that can result from over-labeling. Titration is required for each primary antibody [88]. |
| Protein Blocking Reagents | Blocks charged sites on the tissue section to prevent non-specific binding of the primary and secondary antibodies, a critical step for noise reduction. Normal serum from the secondary antibody species is often ideal [71]. |
Optimization Parameters and Quantitative Data
Systematic optimization of incubation conditions and detection system selection is fundamental to maximizing the S/N ratio. The following table summarizes the impact of key variables and provides quantitative guidance.
Table 2: Optimization Parameters for Signal-to-Noise Ratio in IHC
| Parameter | Impact on Signal-to-Noise Ratio | Recommended Protocol & Quantitative Data |
|---|---|---|
| Primary Antibody Incubation Time & Temperature | Time: Longer incubation can increase signal intensity by allowing more time for the antibody to reach binding equilibrium.Temperature: Lower temperatures (e.g., 4°C) slow reaction kinetics but can significantly reduce non-specific binding and background, leading to a higher S/N ratio [87]. | - Room Temperature (RT): 30-60 minutes [71].- 4°C Overnight: This is the recommended method for research purposes to achieve the highest S/N, as it maximizes specific binding while minimizing non-specific background [87]. |
| Secondary Antibody Concentration | Excessive concentration is a major cause of high background noise. Titration is essential to find the concentration that yields maximal signal with minimal background [88]. | - Starting Concentration: Do not exceed 5 µg/mL for mouse or 2 µg/mL for rabbit primary antibodies when using polymer systems [87].- Optimal Range: For fluorescent secondaries, the optimal S/N is typically achieved between 1-10 µg/mL. Concentrations >10 µg/mL can cause a drastic increase in background [88]. |
| Degree of Labeling (DOL) | The average number of fluorophores per antibody molecule. A higher DOL increases signal intensity but can also increase background due to hydrophobic interactions. An optimal range must be determined [88]. | - Example DOL Ranges for Alexa Fluor Plus secondaries: 2-4 (e.g., Plus 594) to 8-11 (e.g., Plus 555). A DOL of 2-4 for a 594-nm conjugate can provide a 2 to 3-fold higher S/N ratio compared to benchmark antibodies [88]. |
| Epitope Retrieval Method | The choice of retrieval method and pH directly influences the exposure of the target epitope, fundamentally determining the maximum achievable signal [87]. | - Primary Method: Heat-Induced Epitope Retrieval (HIER) using a basic pH solution is recommended as a starting point, as it provides stronger staining for most antibodies [87].- Methods: Autoclave (120°C for 10 min), heating plate (100°C for 30 min), or microwave (750-800W for 10 min) [71]. |
| Detection System | The choice of detection system directly impacts sensitivity. Polymer-based systems are generally more sensitive and produce less background than ABC systems [87]. | - Polymer Systems: Allow for the use of lower primary antibody concentrations, reducing cost and potential background [87].- Tyramide Signal Amplification (TSA): Can be used for higher sensitivity detection of low-abundance targets but requires careful optimization to control background [86]. |
Experimental Protocols for Key Optimization Experiments
Protocol: Titration of Primary and Secondary Antibodies
This protocol is designed to establish the optimal working concentration for both primary and secondary antibodies, which is the most critical step in minimizing background and maximizing signal.
Materials:
- FFPE tissue sections (e.g., a known ubiquitin-positive cancer cell line pellet or tissue) [87]
- Ubiquitination-specific primary antibody
- Compatible secondary antibody (chromogenic or fluorescent)
- Epitope retrieval solution (basic pH, e.g., citrate buffer pH 6 or EDTA/TRIS buffer pH 9)
- Blocking solution (e.g., 5-10% normal serum, BSA, or commercial protein block)
- Washing buffer (e.g., TBST or PBS)
- Humidified chamber
Method:
- Section and Retrieve: Cut serial sections of the control FFPE block. Deparaffinize and rehydrate the sections through a series of xylenes and graded alcohols. Perform epitope retrieval using a standardized HIER method (e.g., 100°C for 30 min in basic buffer) [71] [87].
- Block: Apply protein block for 30 minutes at room temperature to reduce non-specific binding.
- Primary Antibody Titration:
- Wash: Wash the slides 3 times for 5 minutes each with washing buffer.
- Secondary Antibody Titration (If needed):
- For a given primary antibody concentration (e.g., 1 µg/mL), apply a dilution series of the secondary antibody (e.g., 1, 2, 5, and 10 µg/mL) to different sections [88].
- Incubate for 30-60 minutes at room temperature.
- Wash: Wash the slides 3 times for 5 minutes each with washing buffer.
- Detect and Visualize: Apply the appropriate chromogenic substrate or mount the slides for fluorescence imaging.
- Analysis: The optimal concentration is the one that yields the strongest specific signal with the lowest non-specific background. A further increase in concentration that does not enhance the specific signal but increases background should be avoided.
Protocol: Comparing Incubation Time and Temperature
This protocol evaluates the effect of incubation conditions on the S/N ratio.
Materials: (As in Protocol 4.1)
Method:
- Prepare Sections: Process control FFPE sections as in Steps 1-2 of Protocol 4.1.
- Apply Primary Antibody: Use a single, mid-range concentration of the primary antibody (as determined from Protocol 4.1) on all sections.
- Incubate under Varied Conditions:
- Condition A: Incubate for 30 minutes at room temperature.
- Condition B: Incubate for 60 minutes at room temperature.
- Condition C: Incubate overnight (~16 hours) at 4°C [87].
- Wash and Detect: Continue with the standardized protocol for washing, secondary antibody application (using the optimal concentration), and detection.
- Analysis: Compare the staining intensity and background levels across the three conditions. The 4°C overnight incubation is expected to provide the highest S/N ratio by allowing the binding reaction to reach equilibrium with minimal non-specific binding [87].
Workflow and Relationship Diagrams
The following diagram illustrates the logical decision-making process for optimizing the signal-to-noise ratio in IHC, integrating the key parameters discussed in this note.
Diagram 1: IHC S/N Optimization Workflow. This flowchart outlines the key steps for optimizing an IHC assay, highlighting critical parameters (green nodes) that have the most significant impact on the final signal-to-noise ratio.
The relationship between antibody concentration, degree of labeling (DOL), and the resulting signal and noise is complex. The following diagram visualizes how these parameters interact to produce the final S/N ratio, which is the critical performance indicator.
Diagram 2: Parameter Impact on S/N Ratio. This diagram shows the competing effects of increasing antibody concentration or Degree of Labeling (DOL). While both specific signal and background noise tend to increase, the optimal S/N is found at the point where the signal is maximized relative to the noise, requiring empirical titration.
Concluding Remarks
Optimizing the signal-to-noise ratio in IHC is a systematic process that requires careful attention to antibody concentrations, incubation conditions, and detection technologies. For researchers studying ubiquitination in cancer, where targets may be of low abundance or have specific subcellular localizations, employing a 4°C overnight primary antibody incubation, using titrated and highly validated reagents, and selecting modern polymer-based detection systems are among the most effective strategies to generate high-quality, publication-ready data. As emphasized throughout, the inclusion of appropriate controls is non-negotiable for validating the performance of any optimized assay [87].
When to Persist with Optimization vs. Selecting a New Antibody Lot
In the field of cancer research, particularly when studying ubiquitination pathways using immunohistochemistry (IHC), the question of whether to persist with optimizing a problematic antibody lot or to simply select a new one represents a critical decision point. Ubiquitination-specific antibodies, such as those targeting linkage-specific chains (e.g., K48-linked ubiquitin), present unique challenges due to the subtle nature of their targets and the critical role of proper validation in ensuring research reproducibility [89] [90].
Studies indicate that a significant percentage of commercially available antibodies fail to perform as expected in their intended applications, with data from the Human Protein Atlas suggesting that at least 50% of over 2,500 commercially available antibodies did not perform as expected in their intended assay [90]. This reproducibility crisis underscores the importance of systematic approaches to antibody validation and optimization, particularly for complex targets like ubiquitination markers in cancer research.
Decision Framework: Persist or Replace?
The following decision matrix provides a structured approach to determining whether to persist with optimization of an existing antibody lot or select a new one.
Table 1: Antibody Troubleshooting Decision Matrix
| Evaluation Criteria | Persist with Optimization | Select New Lot/New Antibody |
|---|---|---|
| Specificity Issues | A single unexpected band in Western blot or slight off-target staining that can be blocked | Multiple non-specific bands in Western blot or high background staining resistant to blocking |
| Signal Intensity | Weak but detectable specific signal that responds to concentration changes | No signal observed even at high concentrations (5-25 µg/mL for monoclonal antibodies) [91] |
| Validation Evidence | Some validation pillars (e.g., expected localization) are positive | Multiple validation pillars fail (e.g., genetic, orthogonal methods) [90] |
| Literature Support | Well-cited antibody with published protocols for your application | Limited or conflicting reports of performance in your specific application |
| Target Consideration | Common target with established protocols | Difficult target like ubiquitination where specific epitopes may be masked |
Diagram 1: Antibody persistence decision pathway
Optimization Strategies: When to Persist
Systematic Optimization Protocol
When the decision is made to persist with an antibody lot, follow this structured optimization protocol:
Antibody Titration
Antigen Retrieval Optimization
- Compare EDTA (pH 8.5-9.0) and citrate (pH 6.0) buffers
- Optimize retrieval time and temperature (e.g., 100°C for 20-40 minutes)
- For formalin-fixed tissues, heat-mediated antigen retrieval at 100°C in EDTA buffer (pH 8.5) for 32 minutes has shown success for ubiquitin staining [89]
Incubation Condition Adjustments
- Test incubation times: 1 hour at room temperature vs. overnight at 4°C
- Consider lower temperature incubation (4°C) for longer incubation periods to reduce non-specific background [91]
- Optimize diluent composition (e.g., addition of carrier proteins)
Addressing Specific Ubiquitination Antibody Challenges
Ubiquitination-specific antibodies present unique challenges that may respond to optimization:
- Epitope Accessibility: Linkage-specific ubiquitin antibodies (e.g., K48-specific) may require enhanced antigen retrieval due to the compact structure of polyubiquitin chains
- Fixation Effects: Overfixation with formaldehyde can mask target epitopes through cross-linking; extended antigen retrieval may be necessary [47]
- Cellular Compartmentalization: Verify expected subcellular localization—nuclear, cytoplasmic, or membranous—as an initial validation step [90]
Validation Requirements: Knowing When to Move On
The Four Pillars of Antibody Validation
Rigorous validation is essential before employing any antibody in cancer research. The following pillars should be assessed to determine whether an antibody lot is salvageable:
Table 2: Pillars of Antibody Validation for Ubiquitination Research
| Validation Step | Methodology | Interpretation for Ubiquitination Antibodies |
|---|---|---|
| Architectural Localization | IHC staining assessed for expected tissue, cellular, and subcellular patterns | K48-ubiquitin expected in cytoplasmic inclusions in certain cancers; compare to literature [89] |
| Orthogonal Validation | Western blot, mass spectrometry, or other independent protein assessment | Western blot should show characteristic ubiquitin smearing pattern around 8-10 kDa and higher molecular weight complexes [89] |
| Genetic Validation | Genetic manipulation (knockdown/overexpression) of target in cell lines | siRNA-mediated reduction of ubiquitin should correspondingly reduce signal intensity |
| Independent Epitope | Correlation with multiple antibodies targeting non-overlapping epitopes | Compare multiple ubiquitin linkage-specific antibodies (K48, K63, etc.) for distinct patterns |
When Validation Fails: Selecting a New Lot
Consider selecting a new antibody lot or entirely new antibody when the following conditions occur despite optimization efforts:
- Multiple validation pillars fail: Particularly when genetic validation (Uhlen Pillar 1) and orthogonal methods (Uhlen Pillar 2) both indicate non-specificity [90]
- Irreproducible results across experiments: High lot-to-lot variability, especially problematic with polyclonal antibodies [91]
- Inability to achieve signal-to-noise ratio: Even after extensive optimization of concentration, retrieval, and detection
- Inconsistent with established biology: Staining pattern contradicts known ubiquitination biology in cancer pathways
For ubiquitination-specific antibodies, specifically confirm linkage specificity through Western blot against a panel of linkage-specific ubiquitin standards when available [89].
Essential Reagents and Research Tools
Table 3: Essential Research Reagent Solutions for Ubiquitination IHC
| Reagent/Category | Specific Examples | Function in Ubiquitination IHC |
|---|---|---|
| Linkage-Specific Antibodies | Anti-Ubiquitin (linkage-specific K48) [EP8589] (ab140601) [89] | Detects specific polyubiquitin chain linkages involved in proteasomal degradation |
| Validation Tools | siRNA for ubiquitin genes, ubiquitin mutant cell lines | Genetic validation of antibody specificity through target modulation |
| Antigen Retrieval Buffers | EDTA buffer (pH 8.5-9.0), citrate buffer (pH 6.0) | Exposes masked ubiquitin epitopes compromised by formalin fixation |
| Detection Systems | OptiView DAB IHC Detection Kit, fluorescent secondary antibodies | Amplifies signal while maintaining specificity for low-abundance targets |
| Control Materials | Tissue microarrays with known ubiquitination status, recombinant ubiquitin proteins | Provides positive and negative controls for assay validation |
| Fixation Alternatives | Precipitative fixatives (methanol, acetone) for specific applications | Alternative to cross-linking fixatives that may better preserve certain epitopes |
The decision to persist with optimization or select a new antibody lot represents a balance between efficient resource allocation and the pursuit of robust, reproducible data. For ubiquitination-specific cancer research, where targets are often subtle and biologically significant, a systematic approach to this decision is particularly critical. By applying the structured framework and validation protocols outlined in this document, researchers can make informed decisions that maximize the likelihood of generating reliable, publication-quality data while minimizing wasted time and resources.
Ensuring Specificity: Validation Strategies for Ubiquitination-Specific Antibodies
The Critical Role of Positive and Negative Controls in IHC Assay Validation
Immunohistochemistry (IHC) serves as a cornerstone technique in pathology and cancer research, providing critical insights into protein localization and expression within tissue architecture. The reliability of IHC data, particularly for high-stakes applications such as predictive biomarker analysis in oncology, is fundamentally dependent on rigorous validation and continuous quality control. This application note details the essential role of positive and negative controls in ensuring IHC assay specificity, sensitivity, and reproducibility. Within the context of ubiquitination-specific antibodies in cancer research, we provide evidence-based protocols, structured data presentation, and visual workflows to guide researchers and drug development professionals in implementing a robust validation framework that meets current regulatory and scientific standards.
Immunohistochemistry has evolved from a supplementary technique to an indispensable tool in diagnostic pathology and therapeutic development, particularly in the era of precision medicine. The principle of IHC involves specific binding of antibodies tagged with labels to target antigens within tissues, visualizing the localization and distribution of specific antigens [92]. For ubiquitination-specific antibodies in cancer research—where detecting ubiquitin-modified proteins can reveal critical insights into protein degradation, signaling pathways, and therapeutic targets—the accuracy of IHC results is paramount.
Validation ensures that an IHC assay is reliable and reproducible for biomarker detection in clinical and research settings [93]. The purpose of an assay directly correlates with the level of validation required, with assays informing patient care decisions demanding the most robust validation [93]. Controls serve as the fundamental mechanism for verifying that observed staining patterns are accurate and biologically relevant rather than artifacts of the staining process. As emphasized in international guidelines, proper utilization of controls provides objective evidence that the IHC assay fulfills its intended use, confirming the level of certainty and test performance characteristics [94] [95]. Without appropriate controls, interpretation of ubiquitination patterns in cancer tissues becomes speculative, potentially compromising research conclusions and therapeutic development.
Classification and Functions of IHC Controls
Positive Controls: Demonstrating Assay Sensitivity
Positive controls are tissues or cells known to express the target antigen of interest [96]. They serve multiple critical functions in IHC validation:
- Protocol Verification: Positive controls validate that the entire IHC protocol, including antigen retrieval, antibody dilution, incubation conditions, and detection systems, is functioning correctly [92].
- Analytical Sensitivity Assessment: They demonstrate that the assay can detect the target antigen at the expected expression levels, providing confidence in negative results obtained from test samples [96].
- Lot-to-Lot Variation Monitoring: Regular inclusion of positive controls helps monitor consistency of reagent performance across different lots and over time.
The optimal selection of positive controls requires in-depth experience and knowledge of biological processes in the context of the intended use of each IHC test [95]. For ubiquitination-specific antibodies, positive controls should include tissues with known, well-characterized ubiquitination patterns relevant to the cancer type under investigation.
Negative Controls: Establishing Assay Specificity
Negative controls verify that observed staining results from specific antibody-antigen interaction rather than non-specific binding or technical artifacts. The international ad hoc expert panel on standardization of negative controls in diagnostic IHC has classified negative controls into several categories [95]:
Table 1: Classification of Negative Controls in IHC
| Control Type | Preparation Method | Purpose | Interpretation |
|---|---|---|---|
| Negative Reagent Control (NRC) | Primary antibody replaced with non-immune immunoglobulin of same isotype and concentration | Identifies false-positive staining due to non-specific antibody binding | No specific staining should be observed |
| No Primary Antibody Control | Primary antibody omitted entirely; antibody diluent alone applied | Detects background staining from detection system or endogenous enzymes | Verifies staining is specific to primary antibody |
| Negative Tissue Control (NTC) | Tissue known not to express the target antigen | Confirms specificity of staining in a biological context | Absence of staining in known negative tissue |
| Isotype Control | Incubation with non-immune antibody of same isotype | Checks for non-specific interactions of the antibody with tissue components | Background should be negligible and distinct from specific staining |
| Absorption Control | Primary antibody pre-absorbed with excess target antigen | Demonstrates antibody binding specificity through competitive inhibition | Significant reduction or elimination of specific staining |
The specific negative control strategy should be tailored based on "fit-for-use" principles, considering factors such as the detection system utilized, with polymer-based systems potentially requiring different approaches than avidin-biotin based systems [95].
Experimental Protocols for Control Implementation
Protocol: Comprehensive IHC Validation with Integrated Controls
This protocol provides a step-by-step methodology for validating IHC assays, with specific emphasis on implementation for ubiquitination-specific antibodies in cancer research.
Materials and Reagents
- Test tissue sections (formalin-fixed, paraffin-embedded recommended)
- Positive control tissues with known ubiquitination expression
- Negative control tissues lacking target ubiquitinated proteins
- Ubiquitination-specific primary antibodies
- Isotype-matched control antibodies
- Detection system (polymer-based recommended)
- Antigen retrieval solutions (citrate buffer, pH 6.0, or Tris-EDTA, pH 9.0)
- Blocking solution (serum or protein block)
- Phosphate-buffered saline (PBS)
- Hematoxylin counterstain
- Mounting medium
Methodology
Slide Preparation
- Cut tissue sections at 4-5μm thickness.
- Place on charged slides to ensure adhesion.
- Dry slides at 60°C for 20-60 minutes.
Deparaffinization and Rehydration
- Incubate slides at 60°C for 10 minutes.
- Deparaffinize in xylene (3 changes, 5 minutes each).
- Rehydrate through graded alcohols (100%, 95%, 70%) to distilled water.
Antigen Retrieval
- Perform heat-induced epitope retrieval using appropriate buffer and pH.
- For ubiquitinated proteins, test multiple retrieval conditions during validation.
- Cool slides to room temperature for 30 minutes.
Blocking
- Block endogenous peroxidase activity with 3% H₂O₂ for 10 minutes.
- Rinse with PBS.
- Apply protein block for 10 minutes to reduce non-specific binding.
Antibody Application
- Apply ubiquitination-specific primary antibody at optimized dilution to test and positive control sections.
- Apply isotype control antibody to negative control section.
- For no-primary control, apply antibody diluent only.
- Incubate according to optimized conditions (typically 30-90 minutes at room temperature or overnight at 4°C).
Detection
- Apply labeled polymer secondary antibody for 30 minutes.
- Develop with DAB chromogen for 5-10 minutes.
- Monitor development under microscope.
Counterstaining and Mounting
- Counterstain with hematoxylin for 30-60 seconds.
- Dehydrate through graded alcohols and xylene.
- Mount with permanent mounting medium.
Validation Assessment
- Positive control must show appropriate expected staining.
- All negative controls must show absence of specific staining.
- Test tissues should show appropriate subcellular localization.
- Compare results with expected patterns based on literature.
Protocol: Quantitative Image Analysis for Control Assessment
Incorporating digital image analysis provides objective assessment of control performance, reducing subjective interpretation.
Materials and Reagents
- Whole slide scanner
- Image analysis software (e.g., Aperio ImageScope)
- Positive pixel count algorithm
- Annotated regions of interest
Methodology
Slide Scanning
- Scan all control and test slides at 20X magnification.
- Ensure consistent lighting and focus across all scans.
Region Annotation
- Annotate identical tissue regions across all control slides.
- Use consistent annotation size and location.
Algorithm Application
- Apply positive pixel count algorithm with standardized thresholds.
- For ubiquitination staining, establish thresholds during validation.
- Record quantitative data for each control.
Data Analysis
- Calculate average staining intensity for positive controls.
- Determine background staining levels from negative controls.
- Establish acceptable ranges for future assay runs.
A study demonstrated that digital image analysis correlated well with pathologist scores but had increased sensitivity for discriminating subtle variations, providing reproducible digital quantification across sites as well as within and among staining runs [97].
Quantitative Validation Criteria and Performance Metrics
Analytical Validation Requirements
The College of American Pathologists (CAP) guidelines provide evidence-based recommendations for IHC assay validation, emphasizing the need for objective performance criteria [98].
Table 2: IHC Validation Performance Requirements
| Validation Parameter | Requirement | Evidence | Application to Ubiquitination Antibodies |
|---|---|---|---|
| Sample Size | Minimum of 10 positive and 10 negative cases for alternative fixatives [98] | CAP 2024 Guideline Update | Ensure sufficient cases representing different cancer types with varying ubiquitination patterns |
| Concordance Threshold | 90% for all IHC assays [98] | CAP 2024 Guideline Update | Compare with orthogonal methods (e.g., western blot) for ubiquitination detection |
| Comparator Options | Multiple options from most to least stringent [98] | CAP Systematic Review | For novel ubiquitination antibodies, use multiple comparators including known positive tissues |
| Scoring System Validation | Separate validation for each assay-scoring system combination [98] | CAP 2024 Guideline Update | Validate both nuclear and cytoplasmic ubiquitination scoring separately |
| Precision Monitoring | Quantitative tracking of interrun, intrarun, and intersite variability [97] | Image Analysis Study | Implement digital image analysis for objective quantification |
Control-Based Validation Outcomes
Implementation of proper controls enables quantitative assessment of IHC assay performance characteristics:
Table 3: Control Performance Metrics
| Performance Characteristic | Assessment Method | Acceptance Criterion | Impact on Ubiquitination Research |
|---|---|---|---|
| Sensitivity | Staining of low-expressing positive control | Consistent detection of expected low-level staining | Ensures detection of biologically relevant low-level ubiquitination |
| Specificity | Evaluation of negative controls | Absence of specific staining in all negative controls | Confirms ubiquitination signal is not background or non-specific binding |
| Reproducibility | Inter-run control staining consistency | >90% concordance between runs | Enables longitudinal studies of ubiquitination changes in cancer models |
| Precision | Intra-run control staining consistency | >95% concordance within run | Supports quantitative assessment of ubiquitination levels |
| Accuracy | Comparison with known positive and negative tissues | 100% agreement with expected results | Validates biological conclusions about ubiquitination in cancer pathways |
Visual Workflows for IHC Control Implementation
IHC Control Implementation Workflow
IHC Validation Strategy Based on Biomarker Type
The Scientist's Toolkit: Essential Research Reagent Solutions
Table 4: Essential Reagents for Ubiquitination IHC Validation
| Reagent Category | Specific Examples | Function in Validation | Quality Considerations |
|---|---|---|---|
| Primary Antibodies | Recombinant antibodies [99], IHC-Validated antibodies [99], Ubiquitination-specific monoclonal antibodies | Target detection with high specificity | Batch-to-batch reproducibility, validation for FFPE tissues [99] |
| Control Tissues | Tissue microarrays with known ubiquitination status, Cell line pellets with induced ubiquitination | Positive and negative control material | Consistent fixation and processing, known biomarker status |
| Detection Systems | Polymer-based detection systems, Chromogenic substrates (DAB) | Signal amplification and visualization | Sensitivity, low background, compatibility with automation |
| Antigen Retrieval Reagents | Citrate buffer (pH 6.0), Tris-EDTA (pH 9.0), Enzyme retrieval solutions | Epitope unmasking after fixation | pH stability, lot consistency, optimization for ubiquitination |
| Blocking Reagents | Normal serum, Protein blocks, Endogenous enzyme blockers | Reduction of non-specific background staining | Compatibility with primary antibody host species |
| Isotype Controls | Same isotype as primary antibody, Non-immune immunoglobulin | Specificity verification for monoclonal antibodies | Matching concentration, formulation, and host species |
The implementation of robust positive and negative controls represents a fundamental requirement for rigorous IHC assay validation, particularly in the context of ubiquitination-specific cancer research where accurate protein localization and quantification drives critical research conclusions and therapeutic development decisions. As IHC continues to evolve, several emerging trends will shape future control strategies:
Digital Pathology Integration: The adoption of digital pathology and artificial intelligence (AI) platforms enables automated interpretation of complex staining patterns, providing more accurate and reproducible quantification of both test and control samples [92]. Algorithm-based automated image analysis presents an efficient, effective method for tracking variability of IHC staining over time [97].
Standardization Across Platforms: With the growing significance of multiplex IHC and complex biomarker panels, standardized control materials that work across multiple platforms and detection methodologies will become increasingly important. International collaborative efforts continue to address these standardization challenges.
Regulatory Harmonization: As reflected in updated CAP guidelines, regulatory requirements for IHC validation continue to evolve toward greater harmonization and evidence-based standards [98]. Researchers developing ubiquitination-specific antibodies for both research and potential clinical applications should implement validation strategies that address both current and anticipated future requirements.
Through diligent implementation of the controls, protocols, and validation strategies outlined in this application note, researchers can ensure the generation of reliable, reproducible, and biologically meaningful data from IHC studies of ubiquitination in cancer research, ultimately accelerating our understanding of protein regulation in oncogenesis and supporting the development of novel therapeutic approaches.
Peptide Competition Assays for Confirming Antibody Specificity to Ubiquitin Marks
In the field of cancer research, the precise detection of post-translational modifications (PTMs) such as ubiquitination via immunohistochemistry (IHC) is paramount for understanding tumorigenesis, patient prognosis, and therapeutic targeting. Ubiquitination, the covalent attachment of ubiquitin to target proteins, regulates critical processes including protein degradation, DNA repair, and cell cycle progression, with its dysregulation being a hallmark of cancer [100] [101]. However, a significant challenge in utilizing IHC for ubiquitin detection is confirming that the observed staining pattern is specific for the ubiquitin modification and not an artifact of non-specific antibody binding. Peptide Competition Assays (PCA) serve as a critical validation method to confirm antibody specificity, ensuring that the data generated in ubiquitin-focused cancer research is both reliable and interpretable [102].
The complexity of the ubiquitin pathway, involving multiple ubiquitin-like proteins and chain linkages, further underscores the need for rigorous antibody validation. Non-specific staining can lead to incorrect conclusions about the subcellular localization and abundance of ubiquitinated proteins in tumor tissues, potentially misdirecting research efforts and therapeutic development. This application note provides a detailed protocol for performing PCA to validate the specificity of ubiquitin-specific antibodies within the context of IHC cancer research, ensuring that researchers can confidently link staining patterns to biological and clinical outcomes.
The Principle of Peptide Competition Assay
The fundamental principle of a Peptide Competition Assay is the specific competition for the antibody's binding site between the target antigen present on a tissue section (in IHC) or a membrane (in immunoblotting) and the free, solubilized peptide used as the immunogen. An antibody pre-incubated with its corresponding immunizing peptide will be blocked from binding to the target antigen in the biological sample. A successful assay is therefore indicated by a significant reduction or complete absence of staining in the competed sample compared to the uncontested control [102].
This method is particularly crucial for anti-peptide polyclonal antibodies and domain-specific antibodies, such as those targeting specific ubiquitin marks. In the context of ubiquitination, antibodies may be developed against specific ubiquitin chain linkages (e.g., K48, K63) or mono-ubiquitination sites. The PCA can distinguish specific band reactivity or staining patterns from non-specific signals, a common issue when probing complex lysates or tissue samples [102]. For ubiquitin-specific antibodies, the assay typically involves parallel experiments: one set with the antibody pre-adsorbed with the ubiquitin peptide used for immunization, and a control set with a non-specific peptide or no peptide. The specific disappearance of a staining pattern in the competed sample confirms that the antibody is specifically recognizing the intended ubiquitin epitope.
Materials and Reagents
Research Reagent Solutions
The following table details the essential materials and reagents required to perform a robust PCA for antibody validation.
Table 1: Key Research Reagents for Peptide Competition Assays
| Reagent | Function/Description | Example/Note |
|---|---|---|
| Primary Antibody | The ubiquitin-specific antibody being validated. | e.g., Recombinant monoclonal anti-ubiquitin antibody [103]. |
| Immunizing Peptide | The specific ubiquitin peptide against which the antibody was raised. | Reconstituted in molecular biology-grade water [102]. |
| Control Peptide | A non-specific peptide to rule out non-selective competition. | A scrambled version or an unrelated ubiquitin peptide. |
| Blocking Buffer | Reduces non-specific antibody binding to the sample. | Commercially available or lab-made (e.g., with BSA or serum) [102]. |
| Secondary Antibody | Conjugated antibody for detection. | e.g., HRP- or AP-conjugated goat anti-rabbit IgG [102]. |
| Detection Substrate | For chromogenic or chemiluminescent signal development. | HRP or ALP substrates for Western Blot or IHC [102]. |
| Dilution Buffer | Buffer for diluting antibodies and peptides. | Optimized buffer (e.g., PBS or TBS with carrier protein) [102]. |
| Cell or Tissue Lysates | Sample containing the target ubiquitinated proteins. | Whole cell lysates; optimized for antigen presence [102]. |
Quantitative Parameters for PCA
Optimal PCA results are achieved by using a molar excess of peptide to antibody. The following table summarizes the key quantitative parameters for setting up the assay.
Table 2: Quantitative Parameters for Peptide Competition Assay
| Parameter | Recommended Condition | Notes |
|---|---|---|
| Peptide Excess | 200- to 500-fold molar excess over antibody | No significant difference observed between 200-fold and 500-fold excess [102]. |
| Antibody Concentration | Use pre-optimized concentration for IHC/WB | e.g., 1 µg/mL, as used in example protocols [102]. |
| Incubation Time | 30 minutes at room temperature | Can be extended to 1-2 hours at 37°C or 2-24 hours at 4°C for difficult blocks [102]. |
| Incubation Temperature | Room temperature (with gentle rocking) | Alternative temperatures can be tested if initial results are suboptimal [102]. |
| Centrifugation | 15 minutes at 4°C (10k–15k rpm) | Pellets immune complexes to reduce background staining [102]. |
Experimental Protocol
Pre-Assay Optimization
Prior to performing the PCA, it is critical to optimize the conditions for your IHC experiment. This includes determining the ideal amount of antigen (e.g., tissue section thickness, antigen retrieval method), the optimal dilution of the primary and secondary antibodies, the composition of the dilution and blocking buffers, and other experimental conditions. These optimized parameters must be kept constant throughout the PCA to ensure valid results [102].
Step-by-Step PCA Procedure
The following workflow diagram illustrates the key stages of the Peptide Competition Assay procedure:
Figure 1: PCA Experimental Workflow. The procedure involves setting up parallel competition reactions before applying the treated antibodies to samples for immunohistochemistry.
Step 1: Reagent Preparation
- Gently thaw the primary ubiquitin antibody on ice.
- Reconstitute the lyophilized immunizing ubiquitin peptide and a control non-specific peptide to a concentration of 100 µM using Water for Molecular Biology. For a peptide with a molecular mass of 1500 Da, reconstituting 100 µg with 0.67 mL of water yields a 100 µM solution. Allow the peptide to dissolve at room temperature and triturate gently with a pipette [102].
Step 2: Prepare Peptide-Antibody Mixtures Label three microcentrifuge tubes for the competition reactions:
- Tube (a): No-peptide control. Add 973 µL of dilution buffer and 27 µL of water.
- Tube (b): Specific competition. Add 973 µL of dilution buffer and 27 µL of the reconstituted ubiquitin peptide (100 µM).
- Tube (c): Control competition. Add 973 µL of dilution buffer and 27 µL of the reconstituted non-specific control peptide (100 µM).
- Pipette 1 mL of the 2X stock primary antibody solution into each of the three tubes. The final mixture will contain the antibody at its optimal working concentration and a 200-fold molar excess of peptide [102].
Step 3: Incubation and Clearing
- Incubate the tubes for 30 minutes at room temperature with gentle rocking. If competition is inefficient, consider longer incubation times (1–2 hours at 37°C or 2–24 hours at 4°C) [102].
- Centrifuge the samples for 15 minutes at 4°C in a microfuge (10,000–15,000 rpm) to pellet any large immune complexes. Carefully collect the supernatant, leaving behind approximately 5–10 µL at the bottom to avoid disturbing the pellet. This step is crucial to reduce background staining [102].
Step 4: Immunohistochemistry
- Apply the supernatant from each tube to identical test samples, such as serial sections of paraffin-embedded cancer tissue arrays mounted on slides.
- Proceed with the pre-optimized IHC protocol, including incubation with the primary antibody mixtures, washing steps, incubation with a labeled secondary antibody, and final development with a chromogenic substrate [102].
Data Interpretation and Analysis
Expected Outcomes
The results from a properly executed PCA provide a clear, visual confirmation of antibody specificity. The expected outcomes for each experimental condition are summarized in the table below.
Table 3: Interpretation of Peptide Competition Assay Results
| Experimental Condition | Expected Staining Result | Interpretation |
|---|---|---|
| Antibody + No Peptide | Strong, specific staining pattern. | Represents the maximum signal for the antibody under optimized conditions. |
| Antibody + Ubiquitin Peptide | Significant reduction or absence of specific staining. | Positive PCA Result. Confirms staining is specific to the target ubiquitin epitope. |
| Antibody + Control Peptide | Strong, specific staining pattern (similar to no-peptide control). | Confirms that the loss of signal is due to specific competition, not non-specific effects. |
Troubleshooting and Optimization
- Partial Inhibition: If the specific competition only partially reduces the signal, it indicates that the peptide concentration is insufficient to completely block all antibody binding sites. In this case, increase the molar excess of the peptide (e.g., from 200-fold to 500-fold) [102].
- High Background: If high background staining is observed, ensure the centrifugation step was performed correctly to pellet immune complexes. Re-optimize blocking conditions and wash stringency in the base IHC protocol [102].
- No Staining in Control: A lack of staining in the no-peptide control suggests the primary antibody itself was compromised or the IHC conditions were not optimal. Re-visit the pre-assay optimization steps.
Application in Cancer Research: A Case Study
The validation of ubiquitin-specific antibodies is particularly relevant in cancer research, where ubiquitination plays a direct role in oncogenesis and tumor suppression. For instance, the SCF (Skp1-Cullin1-F-box-protein) E3 ubiquitin ligase complexes, which include RING-component proteins like RBX2/SAG, are crucial for the targeted degradation of tumor suppressors and oncoproteins. Overexpression of SAG (Sensitive to Apoptosis Gene) has been documented in human lung cancers and is correlated with poor patient survival [100].
Validated antibodies are essential for accurately assessing the localization and expression levels of key ubiquitination players like SAG in clinical samples. Using IHC on human tumor tissue arrays, researchers can investigate the correlation between SAG protein levels and clinical outcomes. A properly validated antibody ensures that the staining pattern observed truly represents SAG distribution and not non-specific background, thereby providing reliable data for prognostic assessments [100]. Furthermore, the emergence of novel technologies that target ubiquitin pathways, such as PROTABs (Proteolysis-Targeting Antibodies) that redirect cell-surface E3 ligases like ZNRF3/RNF43 to degrade oncogenic receptors, underscores the need for highly specific reagents to validate target engagement and degradation in both preclinical models and clinical specimens [104].
The Peptide Competition Assay is an indispensable tool in the molecular pathologist's arsenal, providing a straightforward and definitive method for confirming the specificity of ubiquitin-specific antibodies used in IHC. In the context of cancer research, where the accurate interpretation of protein expression and modification in tumor tissues can directly influence diagnostic, prognostic, and therapeutic decisions, rigorous antibody validation is not just good practice—it is a necessity. By adhering to the detailed protocol and guidelines outlined in this application note, researchers can generate robust, reliable, and interpretable data on ubiquitin marks, thereby advancing our understanding of cancer biology and paving the way for novel therapeutic strategies.
Using Cell Line-Based FFPE Controls as Consistent Reference Standards
In the field of cancer research, particularly in the study of protein ubiquitination, the validation of immunohistochemistry (IHC) assays for novel, poorly characterized targets presents a significant challenge. While tissue controls are beneficial for well-characterized proteins, they are less suitable for initial assay development where expression patterns are not yet defined. Formalin-fixed, paraffin-embedded (FFPE) cell line controls provide a standardized alternative, offering known expression levels of target proteins in a controlled system. This application note details the implementation of these controls, framed within the critical context of ubiquitination-specific antibody research in cancer, providing researchers and drug development professionals with standardized protocols to enhance reproducibility and reliability in their IHC workflows.
The Role of Standardized Controls in Ubiquitination Research
The ubiquitin-proteasome system (UPS) is a crucial intracellular pathway for specific protein degradation, playing a vital role in cellular processes such as apoptosis, and its dysregulation is implicated in multiple cancers [105]. Deubiquitinating enzymes (DUBs), including ubiquitin-specific proteases (USPs), function as intrinsic oncogenes or tumor suppressors and are involved in chemoresistance [105]. Recent studies have highlighted specific DUBs such as USP44 in neuroblastoma chemoresistance [105], USP5 in stabilizing GPX4 to inhibit ferroptosis in breast cancer [106], and USP10 in driving cancer stemness in colorectal cancer [107].
Research in this field increasingly relies on IHC to visualize and quantify the expression and localization of these components in tissue samples. The development and validation of antibodies against UPS targets requires controls with defined expression levels to ensure specificity and reproducibility. Cell line-based FFPE controls address this need by providing a consistent reference standard that recapitulates the processing conditions of patient tissues, enabling more accurate antibody characterization and assay optimization.
Advantages of Cell Line-Based FFPE Controls
Table 1: Advantages of Cell Line-Based FFPE Controls over Traditional Tissue Controls
| Aspect | Cell Line-Based FFPE Controls | Traditional Tissue Controls |
|---|---|---|
| Standardization | High; controlled genetic background and culture conditions [108] | Variable; depends on donor and sampling site [106] |
| Expression Knowledge | Defined expression levels (e.g., high, medium, low, knockout) can be engineered [109] | Expression patterns may be unknown for novel targets |
| Homogeneity | High; cross-block variation of <5% in cell number [108] | Low; inherent tissue heterogeneity |
| Availability | Unlimited; can be produced in large batches [108] [109] | Limited by tissue availability and donor variability |
| Suitability for Novel Targets | Ideal for initial antibody characterization and selection [109] | Less suitable for poorly characterized proteins |
Protocol: Generation of FFPE Cell Pellet Controls for IHC
The following protocol for creating standardized FFPE cell pellet controls is adapted from established methodologies [109] and can be applied to cell lines relevant to ubiquitination research.
Materials and Equipment
- Cell Lines: Select lines with known expression (high, medium, low) of the target ubiquitination protein (e.g., DUBs, E3 ligases). Engineered lines (e.g., CRISPR knockout, transfected overexpressors) are highly valuable [109].
- Fixative: 4% neutral buffered formalin or paraformaldehyde solution [109] [110].
- Dehydration Reagents: Ethanol series (e.g., 70%, 95%, 100%) [110].
- Clearing Agent: Xylene or xylene substitute.
- Embedding Medium: Paraffin wax.
- Equipment: Centrifuge, tissue processing cassettes, embedding center.
Step-by-Step Procedure
- Cell Culture and Harvesting: Culture the selected cell lines under standard conditions. Harvest cells at approximately 80% confluence using trypsinization. For optimal preservation of cell surface antigens, a proprietary trypsin-free method can be employed [108].
- Pellet Formation: Centrifuge the cell suspension to form a firm pellet. Carefully aspirate the supernatant without disturbing the pellet.
- Fixation: Resuspend the cell pellet in a sufficient volume of 4% neutral buffered formalin. Fix for a standardized period at room temperature (e.g., 24-48 hours). Prolonged fixation (e.g., beyond 72 hours) can contribute to RNA fragmentation and may affect antigenicity [110].
- Dehydration: Process the fixed pellet through a series of graded ethanol baths (e.g., 70%, 95%, 100%) to remove all water.
- Clearing: Treat the dehydrated pellet with a clearing agent like xylene to remove the alcohol and make the pellet miscible with paraffin.
- Infiltration and Embedding: Infiltrate the pellet with molten paraffin wax at 63°C. Then, embed the pellet in a paraffin block, orienting it to ensure an optimal cross-section is available for slicing [110].
- Sectioning: Section the block using a microtome to produce thin slices (typically 4-5 µm thick). Sections can be placed on slides to create pellet arrays or stored as whole blocks [108].
Table 2: Key Reagent Solutions for FFPE Control Preparation
| Research Reagent | Function in Protocol |
|---|---|
| 4% Neutral Buffered Formalin | Cross-links proteins and preserves cellular morphology by fixation. |
| Ethanol Series (70%, 95%, 100%) | Dehydrates the fixed cell pellet by removing water. |
| Xylene | Clearing agent that removes alcohol and allows paraffin infiltration. |
| Paraffin Wax | Embedding medium that provides support for microtome sectioning. |
| Cell Lines (CRISPR/Transfected) | Provides the biological material with defined target protein expression. |
Application in Ubiquitination-Specific IHC: A Case Study
To illustrate the utility of these controls, consider developing an IHC assay for USP44, a deubiquitinase that enhances cisplatin sensitivity in neuroblastoma by stabilizing the E3 ligase STUB1 [105].
Control Selection:
- Positive Control: A cell line (e.g., a neuroblastoma line like KELLY or SK-N-AS) engineered to overexpress USP44.
- Negative Control: The same cell line with USP44 knocked out using CRISPR-Cas9.
- Background Control: A cell line expressing endogenous levels of USP44.
Assay Validation:
- The FFPE cell pellets from these lines are processed and sectioned alongside patient tissues.
- Staining intensity and localization in the controls provide a benchmark for interpreting results in patient samples.
- The known expression levels in the controls allow for the determination of antibody sensitivity and specificity, ensuring that observed staining in patient tissues is biologically relevant and not an artifact.
This approach ensures that the downstream observation of the USP44-STUB1-LRPPRC axis [105] is based on a rigorously validated IHC assay.
Visualizing Workflow and Signaling Pathways
The following diagrams illustrate the experimental workflow for creating FFPE controls and a key ubiquitination signaling pathway relevant to cancer research, constructed using the specified color palette.
FFPE Cell Pellet Control Workflow
USP44-STUB1-LRPPRC Signaling Axis
The adoption of standardized, cell line-based FFPE controls is a critical advancement for research into the ubiquitin-proteasome system in cancer. These controls provide the reproducibility and defined reference standards necessary to develop robust IHC assays for novel DUBs, E3 ligases, and other ubiquitination-related proteins. By implementing the protocols outlined in this document, researchers in both academic and drug development settings can enhance the reliability of their data, ultimately accelerating the discovery of new therapeutic targets and biomarkers in cancer biology.
Correlating IHC Results with Genomic and Transcriptomic Data from TCGA
Integrating immunohistochemistry (IHC) with genomic and transcriptomic data is crucial for advancing cancer research, particularly in the study of ubiquitination pathways. This protocol provides a detailed methodology for correlating protein expression data from IHC with molecular data from The Cancer Genome Atlas (TCGA) to validate ubiquitination-specific antibodies and identify novel regulatory networks. The correlation between IHC and RNA sequencing (RNA-seq) has been demonstrated for key biomarkers including HER2/ERBB2, ER/ESR1, and PGR in breast cancer and PDL1 in lung cancer, showing high (Spearman’s rho 0.65–0.798) and statistically significant (p < 0.00004) correlations [111]. This integration is especially valuable for ubiquitination research, where post-translational modifications play critical roles in cancer development, progression, and therapy response [66].
Data Acquisition from TCGA
Accessing TCGA Data
The Cancer Genome Atlas (TCGA) contains molecular characterization of over 20,000 primary cancer and matched normal samples spanning 33 cancer types, including genomic, epigenomic, transcriptomic, and proteomic data [112]. Researchers can access this data through the Genomic Data Commons Data Portal, which provides web-based analysis and visualization tools.
Relevant Data Types for Ubiquitination Research
- RNA-seq data: Transcriptomic profiles for correlation with IHC results
- Clinical data: Patient demographics, survival outcomes, and treatment history
- Proteomic data: Limited protein expression data for validation
- Genomic data: Mutation and copy number variation data for ubiquitination pathway genes
Experimental Protocol for IHC-Transcriptomic Correlation
Sample Preparation and IHC Staining
- Tissue Selection: Use formalin-fixed paraffin-embedded (FFPE) tissue samples with tumor cell content >50% as validated in previous studies [111]
- Sectioning: Cut 4-5μm sections from FFPE blocks and mount on charged slides
- Deparaffinization and Rehydration:
- Xylene: 3 changes, 5 minutes each
- Ethanol series: 100%, 95%, 70% (2 minutes each)
- Rinse in distilled water
- Antigen Retrieval:
- Use citrate buffer (pH 6.0) or EDTA buffer (pH 8.0)
- Heat in pressure cooker or microwave (95-100°C for 20 minutes)
- Cool to room temperature for 30 minutes
- Ubiquitination-Specific Antibody Staining:
- Primary antibody incubation: Dilute ubiquitination-specific antibodies in PBS with 1% BSA
- Incubate overnight at 4°C in humidified chamber
- Secondary antibody incubation: Use HRP-conjugated antibodies for 30 minutes at room temperature
- Detection and Counterstaining:
- Develop with DAB chromogen for 2-10 minutes
- Counterstain with hematoxylin for 30-60 seconds
- Dehydrate through ethanol series and xylene
- Mount with permanent mounting medium
IHC Scoring and Quantification
- Digital Pathology Analysis:
- Scan slides at 20x magnification using whole slide scanner
- Use image analysis software to quantify staining intensity
- Generate H-scores (range 0-300) based on staining intensity and percentage of positive cells
- Pathologist Evaluation:
- Independent evaluation by two board-certified pathologists
- Resolve discrepancies through consensus review
- Use standardized scoring systems (0-3+) for clinical biomarkers
RNA Sequencing Data Processing
- Data Extraction from TCGA:
- Download RNA-seq data through Genomic Data Commons portal
- Select samples matching IHC cohort characteristics
- Quality Control and Normalization:
- Assess RNA integrity number (RIN) when available
- Normalize read counts using TPM or FPKM methods
- Apply batch effect correction when necessary
Statistical Correlation Methodology
Data Integration Approach
- Sample Matching:
- Ensure TCGA samples match IHC cohort in cancer type, stage, and histology
- Account for potential differences in sample processing protocols
- Correlation Analysis:
- Use non-parametric Spearman correlation for IHC scores and RNA expression
- Calculate correlation coefficients and statistical significance
- Generate receiver operating characteristic (ROC) curves for biomarker validation
Validation Metrics
The correlation between RNA sequencing and IHC-measured expression has been demonstrated with AUC values of 0.963 for HER2, 0.921 for ESR1, 0.912 for PGR, and 0.922 for PDL1, indicating excellent diagnostic accuracy [111].
Ubiquitination-Specific Research Applications
Ubiquitination Regulatory Network Analysis
Integrate IHC data with ubiquitination-specific regulatory networks to identify key nodes and prognostic pathways. The ubiquitination-related prognostic signature (URPS) can stratify patients into high-risk and low-risk groups with distinct survival outcomes across multiple cancer types [66].
OTUB1-TRIM28-MYC Pathway Validation
Utilize the correlation framework to validate the OTUB1-TRIM28 ubiquitination pathway, which modulates MYC signaling and influences patient prognosis. This pathway represents a potential therapeutic target for improving immunotherapy efficacy [66].
Data Analysis Workflow
Table 1: Validated Correlations Between IHC and RNA-seq Data for Cancer Biomarkers
| Biomarker | Cancer Type | Spearman's rho | P-value | AUC | Sample Size |
|---|---|---|---|---|---|
| HER2/ERBB2 | Breast Cancer | 0.798 | <0.00004 | 0.963 | 39 |
| ER/ESR1 | Breast Cancer | 0.65 | <0.00004 | 0.921 | 39 |
| PGR | Breast Cancer | 0.65 | <0.00004 | 0.912 | 39 |
| PDL1 | Lung Cancer | 0.70 | <0.00004 | 0.922 | 19 |
Table 2: Essential Research Reagent Solutions for Ubiquitination IHC-TCGA Correlation Studies
| Reagent Type | Specific Examples | Function/Application |
|---|---|---|
| Ubiquitination-specific Antibodies | Anti-OTUB1, Anti-TRIM28, Anti-Ubiquitin | Detection of ubiquitination pathway components in IHC |
| RNA Extraction Kits | FFPE RNA extraction kits | Isolate high-quality RNA from archived samples |
| IHC Detection Systems | HRP-DAB systems, fluorescent secondary antibodies | Visualize antibody binding in tissue sections |
| Library Preparation Kits | Illumina TruSeq, Ion Torrent kits | Prepare RNA-seq libraries from extracted RNA |
| Data Analysis Software | ImageJ, R/Bioconductor, GDC tools | Quantify IHC, process RNA-seq, perform statistical analysis |
Ubiquitination Pathway Diagram
Technical Considerations and Limitations
Sample Quality and Compatibility
- FFPE vs. Fresh Frozen: FFPE samples may yield degraded RNA but still provide high-quality expression profiles that cluster with fresh-frozen samples [111]
- RNA Integrity: Consider RNA Integrity Number (RIN) when selecting samples, with optimal RIN >7.0 for best results
- Batch Effects: Account for platform-specific variations in RNA-seq data from different sources
Analytical Considerations
- Normalization Methods: Use consistent normalization approaches across datasets
- Multiple Testing Correction: Apply appropriate corrections (e.g., Bonferroni, FDR) for multiple comparisons
- Cohort Matching: Ensure clinical and pathological characteristics are comparable between IHC and TCGA cohorts
This protocol establishes a robust framework for correlating IHC results with genomic and transcriptomic data from TCGA, with specific application to ubiquitination research. The demonstrated correlations between protein and RNA expression support the utility of this integrated approach for validating ubiquitination-specific antibodies and identifying novel therapeutic targets. By implementing these standardized methodologies, researchers can enhance the reliability and translational impact of cancer biomarker studies.
Comparative Analysis of IHC with Other Ubiquitination Detection Methods (Western Blot, ELISA)
Ubiquitination is a crucial post-translational modification involving the covalent attachment of ubiquitin, a highly conserved 76-amino acid protein, to substrate proteins [113]. This modification regulates diverse cellular functions including protein degradation via the proteasome, cell cycle control, DNA damage repair, and signal transduction pathways [113]. The complexity of ubiquitination lies in the variety of ubiquitin chain linkages (K48, K63, K11, K6, K27, K29, K33, and M1-linear), each generating distinct cellular signals and functional outcomes [113]. In cancer research, detecting and understanding ubiquitination patterns is essential as dysregulation in the ubiquitination cascade contributes to tumor development and progression, making it an attractive target for therapeutic interventions [113].
This application note provides a comparative analysis of three principal ubiquitination detection techniques—Immunohistochemistry (IHC), Western Blot, and Enzyme-Linked Immunosorbent Assay (ELISA)—within the context of ubiquitination-specific antibodies in cancer research. We present detailed protocols, performance comparisons, and practical guidance to assist researchers and drug development professionals in selecting appropriate methodologies for their specific experimental requirements.
Technical Comparison of Detection Methods
Method Principles and Applications
Immunohistochemistry (IHC) enables the visualization of ubiquitin localization within the context of intact tissue architecture. This preservation of spatial information allows researchers to correlate ubiquitination patterns with specific cellular compartments, tumor regions, or tumor microenvironment components, providing invaluable insights for cancer pathology [114].
Western Blot separates proteins by molecular weight before detection, providing information about protein size and the ability to distinguish between different ubiquitinated forms of a protein [115] [116]. This technique is particularly valuable for detecting protein modifications, including ubiquitination, and confirming protein identity [117].
Enzyme-Linked Immunosorbent Assay (ELISA) is a plate-based technique designed for sensitive quantification of proteins, including ubiquitin and ubiquitinated proteins, in complex biological samples [115] [116]. Its high throughput and quantitative capabilities make it suitable for screening applications in drug development [118] [117].
Comparative Performance Characteristics
Table 1: Comparative Analysis of Ubiquitination Detection Methods
| Feature | IHC | Western Blot | ELISA |
|---|---|---|---|
| Spatial Information | Preserved (tissue context) | Lost (lysate) | Lost (lysate) |
| Throughput | Low | Moderate | High [116] [117] |
| Sensitivity | Variable | Moderate (ng/mL range) [117] | High (pg/mL range) [117] |
| Quantification | Semi-quantitative | Semi-quantitative [117] | Fully quantitative [117] |
| Molecular Weight Information | No | Yes [115] [116] | No |
| Detection of PTMs | Possible with specific antibodies | Yes (size shifts) [117] | Limited |
| Sample Type | Tissue sections | Cell/tissue lysates | Cell/tissue lysates, serum, other fluids [116] |
| Key Applications in Cancer Research | Tumor heterogeneity, subcellular localization, biomarker validation | Protein characterization, modification detection, assay validation [115] | Biomarker quantification, drug response monitoring, high-throughput screening [118] |
Table 2: Performance Metrics from Experimental Comparisons
| Parameter | Western Blot | ELISA |
|---|---|---|
| Dynamic Range | 1.41 (ratio of highest to lowest density) [119] | 5.31 (ratio of highest to lowest O.D.) [119] |
| Average Standard Error (C2C12 cells, various treatments) | 0.180-0.240 [119] | 0.018-0.161 [119] |
| Test-Retest Reliability (Interclass Correlation) | ≤0.4 (poor) [119] | ≥0.7 (good) [119] |
| Typical Detection Limit | ~0.1-10 ng [117] | ~0.01-0.1 ng [117] |
Experimental Protocols
Immunohistochemistry (IHC) for Ubiquitin Detection
Principle: IHC utilizes antibodies to detect ubiquitin or ubiquitinated proteins in tissue sections, preserving spatial and morphological context [114]. This is particularly valuable in cancer research for assessing tumor heterogeneity and subcellular localization of ubiquitination events.
Sample Preparation:
- Fixation: Use 10% neutral buffered formalin for 24-48 hours followed by standard paraffin embedding [114].
- Sectioning: Cut 4-5 μm thick sections and mount on charged slides.
- Deparaffinization and Antigen Retrieval: Perform heat-induced epitope retrieval using citrate buffer (pH 6.0) or EDTA buffer (pH 8.0) [114].
Staining Procedure:
- Block endogenous peroxidase activity with 3% H₂O₂ in methanol for 10 minutes.
- Apply protein block (1-5% normal serum from secondary antibody species) for 30 minutes to reduce non-specific binding [114].
- Incubate with primary anti-ubiquitin antibody (e.g., VU-1 monoclonal antibody) [120] diluted in antibody diluent overnight at 4°C.
- Apply species-specific secondary antibody conjugated to HRP or AP for 30-60 minutes at room temperature [114] [121].
- Develop signal using chromogenic substrates:
- Counterstain with hematoxylin, dehydrate, clear, and mount [114].
Controls:
- Positive Control: Tissue known to express ubiquitin (e.g., human brain tissue) [114] [120].
- Negative Control: Omission of primary antibody or use of non-immune IgG [114].
- Specificity Control: Peptide competition with immunizing peptide [122].
Western Blot for Ubiquitin Detection
Principle: Western blot separates proteins by molecular weight using gel electrophoresis, followed by transfer to a membrane and immunodetection with ubiquitin-specific antibodies [116] [117]. This method provides information about protein size and modification states.
Sample Preparation and Electrophoresis:
- Prepare cell or tissue lysates using RIPA buffer supplemented with proteasome inhibitors (e.g., MG132) and deubiquitinase inhibitors (e.g., N-ethylmaleimide) to preserve ubiquitination signals.
- Determine protein concentration and dilute with Laemmli buffer.
- Denature at 95°C for 5 minutes.
- Load 20-50 μg protein per lane on 4-20% gradient SDS-PAGE gels.
- Run electrophoresis at 100-150V until proper separation is achieved.
Transfer and Detection:
- Transfer proteins to PVDF or nitrocellulose membrane using wet or semi-dry transfer systems [117].
- Block membrane with 5% non-fat milk or BSA in TBST for 1 hour.
- Incubate with primary anti-ubiquitin antibody (e.g., VU-1 monoclonal antibody) [120] diluted in blocking buffer overnight at 4°C.
- Wash membrane 3× with TBST, 5 minutes each.
- Incubate with HRP-conjugated secondary antibody for 1 hour at room temperature.
- Wash membrane 3× with TBST, 5 minutes each.
- Develop using chemiluminescent substrates and image with CCD-based system [121].
Controls:
- Positive Control: Cell lysate known to contain ubiquitinated proteins [114].
- Negative Control: Lysate from ubiquitin knockdown cells or no primary antibody control [114].
- Loading Control: Antibodies to housekeeping proteins (e.g., GAPDH, β-actin, tubulin) [114].
ELISA for Ubiquitin Detection
Principle: ELISA quantitatively detects ubiquitin or ubiquitinated proteins in solution using capture and detection antibodies in a microplate format [116]. The sandwich ELISA format is particularly sensitive and specific for ubiquitin detection.
Procedure:
- Coat 96-well plate with capture antibody (2-10 μg/mL in carbonate buffer) overnight at 4°C [116].
- Wash 3× with PBS containing 0.05% Tween-20 (PBST).
- Block with 1-5% BSA or non-fat milk in PBS for 1-2 hours at room temperature.
- Add samples and standards diluted in blocking buffer, incubate 2 hours at room temperature or overnight at 4°C.
- Wash 3× with PBST.
- Add detection antibody (biotinylated or enzyme-conjugated), incubate 1-2 hours.
- Wash 3× with PBST.
- If using biotinylated antibody, add streptavidin-HRP and incubate 30-45 minutes.
- Wash 3× with PBST.
- Add substrate solution (TMB for HRP) and incubate until color development [121].
- Stop reaction with acid and read absorbance at appropriate wavelength.
Controls:
- Positive Control: Purified ubiquitin or lysate known to contain ubiquitinated proteins [114].
- Negative Control: Zero blank (buffer only) and sample known not to contain ubiquitin [114].
- Standard Curve: Serial dilutions of purified ubiquitin for quantification [114].
Research Reagent Solutions
Table 3: Essential Reagents for Ubiquitination Detection
| Reagent Type | Specific Examples | Function & Application Notes |
|---|---|---|
| Primary Antibodies | VU-1 monoclonal antibody [120] | Recognizes free ubiquitin, K48-, K63-, K11- and linear chains; works for WB, ELISA, IHC [120] |
| Detection Systems | HRP-conjugated secondary antibodies [121] | Signal generation for colorimetric, chemiluminescent detection |
| Chromogenic Substrates | DAB (HRP), BCIP/NBT (AP) [121] | Produce insoluble colored precipitates for WB and IHC |
| Chromogenic Substrates (Soluble) | TMB, PNPP [121] | Produce soluble colored products for ELISA quantification |
| Blocking Reagents | BSA, non-fat milk, normal serum [114] | Reduce non-specific antibody binding |
| Positive Control | Ubiquitin-rich tissue (brain) [120], cell lysates | Validate assay performance |
| Inhibitors | MG132 (proteasome), N-ethylmaleimide (deubiquitinase) | Preserve ubiquitination signals in samples |
Method Selection Guide
Integrated Workflow for Comprehensive Ubiquitination Analysis
For a comprehensive analysis of ubiquitination in cancer research, we recommend an integrated approach that leverages the complementary strengths of each technique:
Initial Screening and Quantification: Begin with ELISA for high-throughput quantification of ubiquitin levels across multiple samples or treatment conditions [119] [117]. This approach is ideal for biomarker studies, drug screening, and time-course experiments where quantitative data is prioritized.
Validation and Characterization: Use Western blot to confirm ELISA results and characterize ubiquitinated proteins [115]. Western blot provides information about protein size, specificity of detection, and can distinguish between different ubiquitinated forms.
Spatial and Pathological Context: Apply IHC to validate findings in tissue context [114]. This is particularly important for understanding tumor heterogeneity, subcellular localization, and correlating ubiquitination patterns with histological features.
Strategic Application in Cancer Research
- Biomarker Discovery: ELISA for initial screening → Western blot for verification → IHC for tissue localization [118].
- Drug Mechanism Studies: Western blot for target engagement → ELISA for quantification → IHC for in situ validation.
- Diagnostic Applications: IHC for clinical pathology → Western blot as confirmatory test [115].
The VU-1 monoclonal antibody has demonstrated superior performance across all three platforms, recognizing free ubiquitin and multiple polyubiquitin linkage types (K48, K63, K11, and linear chains) with high specificity [120]. This cross-platform compatibility makes it an excellent choice for researchers employing multiple detection methods in their ubiquitination studies.
Each ubiquitination detection method offers unique advantages that serve different research needs in cancer biology. IHC provides essential spatial context within tissue architecture, Western blot delivers molecular weight information and modification characterization, while ELISA offers superior quantification and throughput capabilities. The strategic integration of these methodologies, supported by well-validated reagents like the VU-1 antibody, enables comprehensive analysis of the ubiquitination system in cancer research. This multi-faceted approach accelerates biomarker validation, drug discovery, and therapeutic development by providing complementary data that strengthens experimental conclusions and facilitates translation of findings from bench to bedside.
Conclusion
The integration of ubiquitination-specific antibodies in IHC represents a powerful tool for cancer research and diagnostic pathology, providing critical insights into tumor biology and patient prognosis. The consistent demonstration that USP expression patterns correlate with clinical outcomes across multiple cancer types underscores their potential as robust biomarkers. Future directions should focus on standardizing validation protocols using cell-line based controls and peptide competition assays to ensure reproducibility. Furthermore, the development of small-molecule inhibitors targeting specific USPs, informed by IHC findings, opens promising avenues for targeted cancer therapies. As the field advances, combining IHC with digital pathology and multi-omics data will enhance the precision of ubiquitination-based biomarker discovery, ultimately improving personalized cancer treatment strategies.
References
- 1. Targeting the Ubiquitin–Proteasome System for Cancer - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC12495026/]
- 2. Molecular mechanisms and potential targeting strategies of ... [https://www.spandidos-publications.com/10.3892/or.2025.9000]
- 3. The multifaceted roles of deubiquitinating enzymes (DUBs ... [https://www.nature.com/articles/s41419-025-08052-7]
- 4. Emerging role of deubiquitinases in modulating cancer ... [https://www.sciencedirect.com/science/article/abs/pii/S1359644625000522]
- 5. Protocol for In Vitro Ubiquitin Conjugation Reaction [https://www.rndsystems.com/resources/protocols/vitro-ubiquitin-conjugation-reaction]
- 6. Site-directed multivalent conjugation of antibodies to ... [https://www.nature.com/articles/s41551-024-01342-z]
- 7. Anti-Ubiquitin (linkage-specific K27) antibody [EPR17034] [https://www.abcam.com/en-us/products/primary-antibodies/ubiquitin-linkage-specific-k27-antibody-epr17034-ab181537]
- 8. ubiquitin antibody (10201-2-AP) [https://www.ptglab.com/products/ubiquitin-Antibody-10201-2-AP.htm?srsltid=AfmBOooWKLAgoxBTRYqYTZj9RsMS-nNv9v4mKwF-js9fpzLisR2HuVjb]
- 9. Structure-guided discovery of ubiquitin-specific protease 7 ... [https://www.sciencedirect.com/science/article/abs/pii/S0010482525015999]
- 10. Exploring bioactive phytoconstituents as USP21 inhibitors ... [https://www.nature.com/articles/s41598-025-94825-1]
- 11. USP38: an important regulatory factor in tumor malignant ... [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2025.1612723/full]
- 12. Immunohistochemistry Protocols [https://www.antibodies.com/applications/immunohistochemistry/ihc-protocol]
- 13. PD-1/PD-L1 Cancer Immunotherapeutics Reshape Tumor ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12532714/]
- 14. Ubiquitination Enzymes in Cancer, Cancer Immune ... [https://www.mdpi.com/2073-4409/14/2/69]
- 15. Molecular Mechanisms of the Ubiquitin-Specific Proteases ... [https://www.mdpi.com/2227-9059/13/11/2586]
- 16. Ubiquitin-specific protease 15 contributes to gastric cancer ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8311539/]
- 17. The deubiquitination enzyme USP14 promotes ... [https://www.nature.com/articles/s41419-025-08065-2]
- 18. Ubiquitin-specific Protease 35 Promotes Gastric Cancer ... [https://www.ijbs.com/v20p0953.htm]
- 19. The downregulation of ubiquitin-specific peptidase 2 ... [https://www.nature.com/articles/s41598-025-08881-8]
- 20. Unravelling the role of ubiquitin-specific proteases in breast ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11841324/]
- 21. USP36 promotes tumorigenesis and tamoxifen resistance in ... [https://jeccr.biomedcentral.com/articles/10.1186/s13046-024-03160-2]
- 22. USP1 promotes cholangiocarcinoma progression by ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10567853/]
- 23. Validation of UBE2C protein as a prognostic marker in node ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC2713693/]
- 24. Validation of a Disease-Free Survival Prediction Model ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10149777/]
- 25. Ubiquitin-conjugating enzyme 2C (UBE2C) is a poor ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8960565/]
- 26. The clinicopathological significance of UBE2C in breast cancer [https://cancerci.biomedcentral.com/articles/10.1186/s12935-017-0455-1]
- 27. UBE2C Is a Potential Biomarker of Intestinal-Type Gastric ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6082955/]
- 28. Ubiquitination-Binding Enzyme 2C is Associated with ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11637980/]
- 29. UBE2S and UBE2C confer a poor prognosis to breast ... [https://www.frontiersin.org/journals/oncology/articles/10.3389/fonc.2023.992233/full]
- 30. UBE2C antibody (12134-2-AP) [https://www.ptglab.com/products/UBE2C-Antibody-12134-2-AP.htm?srsltid=AfmBOopGg1HLT8HrIYAcxc9AJgiikxzL1WI4ddCSa0X2tpNSXHr4_0nj]
- 31. Ubiquitin Specific Protease 26 (USP26) Expression Analysis ... [https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0098638]
- 32. Oncogenic and immunological functions of USP35 in pan ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11972461/]
- 33. A pan-cancer analysis of the role of USP5 in human cancers [https://www.nature.com/articles/s41598-023-35793-2]
- 34. USP13 promotes development and metastasis of high ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8956511/]
- 35. Comprehensive Analysis Reveals USP45 as a Novel ... [https://www.frontiersin.org/journals/molecular-biosciences/articles/10.3389/fmolb.2022.886904/full]
- 36. The deubiquitinase USP7 stabilizes HER2 expression and ... [https://www.sciencedirect.com/science/article/pii/S1476558625000727]
- 37. Overexpression of the Ubiquitin Specific Proteases USP43, ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8464711/]
- 38. Accessing and Downloading TCGA Data - BTEP Coding Club [https://bioinformatics.ccr.cancer.gov/docs/btep-coding-club/CC2024/TCGA/TCGA_download/]
- 39. Antibody Selection and Protocol Optimization [https://www.neobiotechnologies.com/resources/antibodies-for-ihc/?srsltid=AfmBOoqSIDSH7_eHkTNh3RDSyymEg1XTEWh3qQQinLqr-OXGaftfgf1l]
- 40. Monoclonal vs. Polyclonal Antibodies [https://www.thermofisher.com/us/en/home/life-science/antibodies/primary-antibodies/monoclonal-vs-polyclonal-antibodies.html]
- 41. An Essential Guide to Monoclonal vs Polyclonal Antibodies [https://www.neobiotechnologies.com/resources/monoclonal-antibodies-vs-polyclonal-antibodies/?srsltid=AfmBOorT42ymh_1_74WwBenHnU0G0jQ6A6vddTCHCEKbK13oEHj2rDN-]
- 42. Polyclonal vs. monoclonal antibodies [https://www.ptglab.com/news/blog/polyclonal-vs-monoclonal-antibodies/?srsltid=AfmBOopwW5ZflciZU3BmaCKBnx8h7ArSN2kP52AaZDDwBz7F5ow5CM7D]
- 43. Targeting ubiquitin specific proteases (USPs) in cancer ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10472646/]
- 44. Ubiquitination and deubiquitination in cancer [https://molecular-cancer.biomedcentral.com/articles/10.1186/s12943-024-02046-3]
- 45. Ubiquitin-specific protease 48 drives malignant ... [https://www.nature.com/articles/s41418-025-01617-1]
- 46. Immunohistochemistry and Multiple Labeling with Antibodies ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4541582/]
- 47. Immunohistochemistry (IHC): The Complete Guide [https://www.antibodies.com/applications/immunohistochemistry]
- 48. Identification and validation of ubiquitination-related genes for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12343280/]
- 49. The deubiquitinase USP9X and E3 ligase WWP1 ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12500958/]
- 50. Targeted protein degradation: advances in drug discovery ... [https://www.nature.com/articles/s41392-024-02004-x]
- 51. Antigen Retrieval in IHC: Why It Matters and How to Get ... [https://www.atlasantibodies.com/knowledge-hub/blog/antigen-retrieval-in-ihc-why-it-matters-and-how-to-get-it-right/]
- 52. Optimizing HIER Antigen Retrieval for IHC [https://www.bosterbio.com/blog/post/protocol-for-optimizing-hier-antigen-retrieval-conditions?srsltid=AfmBOoo6jH310SX7STFCW-h7T0XhRyJ60HrA9tYK9ixouvdeJVk024ph]
- 53. IHC antigen retrieval protocol [https://www.abcam.com/en-us/technical-resources/protocols/ihc-antigen-retrieval]
- 54. Strategy for Development of Site-Specific Ubiquitin ... [https://www.frontiersin.org/journals/chemistry/articles/10.3389/fchem.2020.00111/full]
- 55. Primary Antibody Selection & Optimization [https://www.rndsystems.com/resources/protocols/primary-antibody-selection-optimization]
- 56. Selecting Antibodies For IHC [https://www.ptglab.com/support/immunohistochemistry-protocol/selecting-antibodies-for-ihc/?srsltid=AfmBOorx40wzSIGNXhonaFryMKncL1IJ7b0OA-8I46QIkJGrd1O1uyKv]
- 57. IHC Primary Antibody Selection & Optimization [https://www.novusbio.com/primary-antibody-selection-optimization?srsltid=AfmBOoqq2ouXGMWB5Gkn0OetVt8ssC7hCGyPCmJjFfdVh1dgntHjJhbi]
- 58. Antibody Selection and Protocol Optimization [https://www.neobiotechnologies.com/resources/antibodies-for-ihc/?srsltid=AfmBOoqoWxtT7yPeMgbNkItREw4QSwQP0-DQaKAoNsdBmZ8ALP06w4Qp]
- 59. Optimisation and validation of immunohistochemistry ... [https://pubmed.ncbi.nlm.nih.gov/33616195/]
- 60. Optimising multiplex immunofluorescence staining for ... [https://www.sciencedirect.com/science/article/pii/S1046202323001585]
- 61. Ubiquitin specific protease 7 is a potential therapeutic ... [https://www.frontiersin.org/journals/oncology/articles/10.3389/fonc.2025.1530924/full]
- 62. IHC-P protocols [https://www.abcam.com/en-us/technical-resources/protocols/ihc-with-samples-in-paraffin]
- 63. Optimal FFPE Tissue Fixation, Processing, and Embedding [https://cellcarta.com/science-hub/optimal-ffpe-tissue-fixation-processing-and-embedding-a-comprehensive-guide/]
- 64. An Overview of IHC Staining Procedures for Formalin ... [https://www.stagebio.com/blog/an-overview-of-staining-procedures-for-formalin-fixed-paraffin-embedded-ffpe-tissues]
- 65. Immunohistochemical Staining of Formalin-Fixed Paraffin- ... [https://www.thermofisher.com/us/en/home/references/protocols/cell-and-tissue-analysis/protocols/ihc-staining-formalin-fixed-paraffin-embedded-tissues.html]
- 66. Constructing a pancancer ubiquitination regulatory network to ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12382526/]
- 67. The Correlations between the Intensity of Histopathological ... [https://www.mdpi.com/1424-8247/16/12/1703]
- 68. Ubiquitin-conjugating enzyme 2C (UBE2C) is a poor ... [https://link.springer.com/article/10.1007/s10549-022-06531-5]
- 69. The Potential Role of Ubiquitin-Conjugating Enzyme E2C ... [https://pubmed.ncbi.nlm.nih.gov/40713465/]
- 70. The potential role of Ubiquitin-conjugating enzyme E2C ... [https://www.sciencedirect.com/science/article/abs/pii/S1526820925001867]
- 71. Immunohistochemistry for Pathologists: Protocols, Pitfalls, ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5122731/]
- 72. IHC Troubleshooting Guide [https://www.thermofisher.com/us/en/home/life-science/protein-biology/protein-biology-learning-center/protein-biology-resource-library/pierce-protein-methods/ihc-troubleshooting-guide.html]
- 73. Immunohistochemistry (IHC) Troubleshooting Guide & the ... [https://www.cellsignal.com/learn-and-support/troubleshooting/ihc-troubleshooting-guide?srsltid=AfmBOor7Kcy87xy9A7D1eoOCPl0fEhbEcOu-V-WdR-66yk2xADIVdX1o]
- 74. Effect of defective H2B ubiquitination on the malignancy ... [https://www.nature.com/articles/s41598-025-06219-y]
- 75. Text has enhanced contrast | ACT Rule | WAI [https://www.w3.org/WAI/standards-guidelines/act/rules/09o5cg/]
- 76. How to deal with high background in ELISA [https://www.abcam.com/en-us/technical-resources/troubleshooting/high-background-elisa]
- 77. Antibody Titration | McGovern Medical School [https://med.uth.edu/imm/flow-cytometry-services/protocols-and-guidelines/antibody-titration/]
- 78. Elisa troubleshooting tips – High background - Blog [https://www.arp1.com/blog/post/elisa-troubleshooting-tips-high-background.html]
- 79. Semi-quantitative Determination of Protein Expression ... [https://en.bio-protocol.org/en/bpdetail?id=3465&type=0]
- 80. [Experimental optimization of paraffin sectioning ... [https://pubmed.ncbi.nlm.nih.gov/40921659/]
- 81. Practicable methods for histological section thickness ... [https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0192879]
- 82. Statistics of deformations in histology and application to ... [https://pubmed.ncbi.nlm.nih.gov/18215807/]
- 83. Cancer Protocol Templates [https://www.cap.org/protocols-and-guidelines/cancer-reporting-tools/cancer-protocol-templates]
- 84. HER2 IHC Testing Updates for mNSCLC [https://www.her2know.com/newsletter/her2-ihc-testing-mnsclc-jan-2025-update.html]
- 85. Quantification of absolute labeling efficiency at the single- ... [https://www.nature.com/articles/s41592-024-02242-5]
- 86. Ten Approaches That Improve Immunostaining: A Review of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8836139/]
- 87. Expert Tips On IHC Antibody Selection, Optimization & ... [https://www.bosterbio.com/boster-interviews/expert-tips-on-ihc-antibody-selection-optimization-and-ihc-negative-controls?srsltid=AfmBOopRrfvAKtdyR3CwI7OIiG_0LhMuxuZ1Pbhlq6nIsAqsNKgqo8nc]
- 88. Alexa Fluor Plus Secondary Antibody Development & ... [https://www.thermofisher.com/us/en/home/references/newsletters-and-journals/bioprobes-journal-of-cell-biology-applications/bioprobes-80/alexa-fluor-plus-secondary-antibodies-development-optimization.html]
- 89. Anti-Ubiquitin (linkage-specific K48) antibody [EP8589] [https://www.abcam.com/en-us/products/primary-antibodies/ubiquitin-linkage-specific-k48-antibody-ep8589-ab140601]
- 90. Antibody validation for protein expression on tissue slides [https://pmc.ncbi.nlm.nih.gov/articles/PMC7807291/]
- 91. IHC Primary Antibody Selection & Optimization [https://www.novusbio.com/primary-antibody-selection-optimization?srsltid=AfmBOormw265pN08S6zs4YIAbdpAkE5G70aBWEIyOpcryHyxCctSETAj]
- 92. Review of immunohistochemistry techniques: Applications, ... [https://www.sciencedirect.com/science/article/abs/pii/S0740257024000467]
- 93. Optimizing Immunohistochemistry Validation and ... [https://www.precisionformedicine.com/blog/optimizing-ihc-validation-regulatory-strategies]
- 94. Indirect clinical validation for predictive biomarkers in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12488805/]
- 95. Standardization of Negative Controls in Diagnostic ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4206554/]
- 96. Controls in IHC [https://www.abcam.com/en-us/technical-resources/guides/ihc-guide/controls-in-ihc]
- 97. An Image Analysis Solution For Quantification and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7368846/]
- 98. Principles of Analytic Validation of Immunohistochemical ... [https://www.cap.org/protocols-and-guidelines/cap-guidelines/current-cap-guidelines/principles-of-analytic-validation-of-immunohistochemical-assays]
- 99. Antibodies And Reagents For Cancer Research [https://vectorlabs.com/antibodies-reagents-for-cancer-research/?srsltid=AfmBOooaWu25QFUz8q-UBx9KCyZ2cO5Ehm7QV7SwdoD4-ufpULMlQ8o6]
- 100. Validation of SAG/RBX2/ROC2 E3 ubiquitin ligase as an ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC2819752/]
- 101. Current Methods of Post-Translational Modification Analysis and Their... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8072572/]
- 102. Peptide Competition Assay (PCA) Protocol [https://www.rockland.com/resources/peptide-competition-assay-protocol/?srsltid=AfmBOoo08XcfcPPezf-Fz1s7DNx0lYgTR5oPCu-wE1Pq5Dctw2_a4jMU]
- 103. (80992-1-RR) | Proteintech ubiquitin antibody [https://www.ptglab.com/products/ubiquitin-Antibody-80992-1-RR.htm]
- 104. Antibody targeting of E3 ubiquitin ligases for receptor ... [https://www.nature.com/articles/s41586-022-05235-6]
- 105. The deubiquitinase USP44 enhances cisplatin ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11812030/]
- 106. FASN inhibits ferroptosis in breast cancer via USP5 ... [https://jeccr.biomedcentral.com/articles/10.1186/s13046-025-03548-8]
- 107. USP10 drives cancer stemness and enables super ... [https://www.nature.com/articles/s41388-024-03141-x]
- 108. FFPE Cancer Cell Line Controls [https://www.amsbio.com/ffpe-cancer-cell-line-controls/]
- 109. Standardized Processing for Formalin-Fixed, Paraffin- ... [https://pubmed.ncbi.nlm.nih.gov/35969105/]
- 110. Optimization of FFPE preparation and identification of gene ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10830353/]
- 111. RNA Sequencing in Comparison to Immunohistochemistry for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7277916/]
- 112. The Cancer Genome Atlas Program (TCGA) - NCI [https://www.cancer.gov/ccg/research/genome-sequencing/tcga]
- 113. Ubiquitination detection techniques - PMC - PubMed Central [https://pmc.ncbi.nlm.nih.gov/articles/PMC10625345/]
- 114. How to Design Positive and Negative Controls for IHC , WB & ELISA [https://www.bosterbio.com/how-to-design-positive-negative-controls-ihc-western-blot-elisa]
- 115. ELISA vs Western Blot: When to Use Each Immunoassay ... [https://www.thermofisher.com/blog/life-in-the-lab/western-blot-or-elisa/]
- 116. vs. Western | Abcam blotting ELISA [https://www.abcam.com/en-us/knowledge-center/western-blot/elisa-vs-western-blot]
- 117. ELISA vs. Western Blot: Choosing the Best Immunoassay ... [https://www.metwarebio.com/elisa-vs-western-blot-comparison/]
- 118. and Other Immunological Techniques: When to... Comparing ELISA [https://www.linkedin.com/pulse/comparing-elisa-other-immunological-techniques-when-choose-zierf]
- 119. Comparisons of ELISA and Western blot assays for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5506881/]
- 120. The most efficient monoclonal Antibody for ubiquitin detection [https://www.tebubio.com/en_fr_eur/content/post/vu-1-the-most-efficient-monoclonal-antibody-for-ubiquitin-detection]
- 121. Chromogenic Detection for Western , Blot , and IHC ELISA [https://www.jacksonimmuno.com/secondary-antibody-resource/immuno-techniques/chromogenic-detection-for-western-blot-ihc-and-elisa/]
- 122. Hallmarks of Antibody Validation: Complementary Strategies [https://www.cellsignal.com/about-us/approach-validation-principles/complementary-assay?srsltid=AfmBOorck6s-B_dyzl4PXm4QC2dCxjEJVyGRhZoH9QLuhAe4DBBaco_Z]