Ubiquitin's Double-Edged Sword: Orchestrating DNA Repair and Driving Cancer
This article explores the critical and dualistic role of the ubiquitin-proteasome system (UPS) in the DNA damage response (DDR) and cancer pathogenesis.
Ubiquitin's Double-Edged Sword: Orchestrating DNA Repair and Driving Cancer
Abstract
This article explores the critical and dualistic role of the ubiquitin-proteasome system (UPS) in the DNA damage response (DDR) and cancer pathogenesis. We first establish the foundational mechanisms by which ubiquitination—through specific E3 ligases like RNF8, RNF168, and MDM2—controls key DDR pathways, including homologous recombination and non-homologous end joining. The discussion then progresses to methodological advances, detailing how this knowledge is being translated into innovative therapeutic strategies, such as proteasome inhibitors, PROTACs, and molecular glues. We further address the challenges in targeting the UPS, including drug resistance and specificity, and present optimization strategies. Finally, we validate these concepts by examining emerging links between DDR-associated ubiquitination and other cancer hallmarks, such as metabolic reprogramming, providing a comparative analysis of therapeutic targets for precision oncology.
The Ubiquitin Code: Decoding Its Fundamental Role in DNA Damage Signaling and Repair
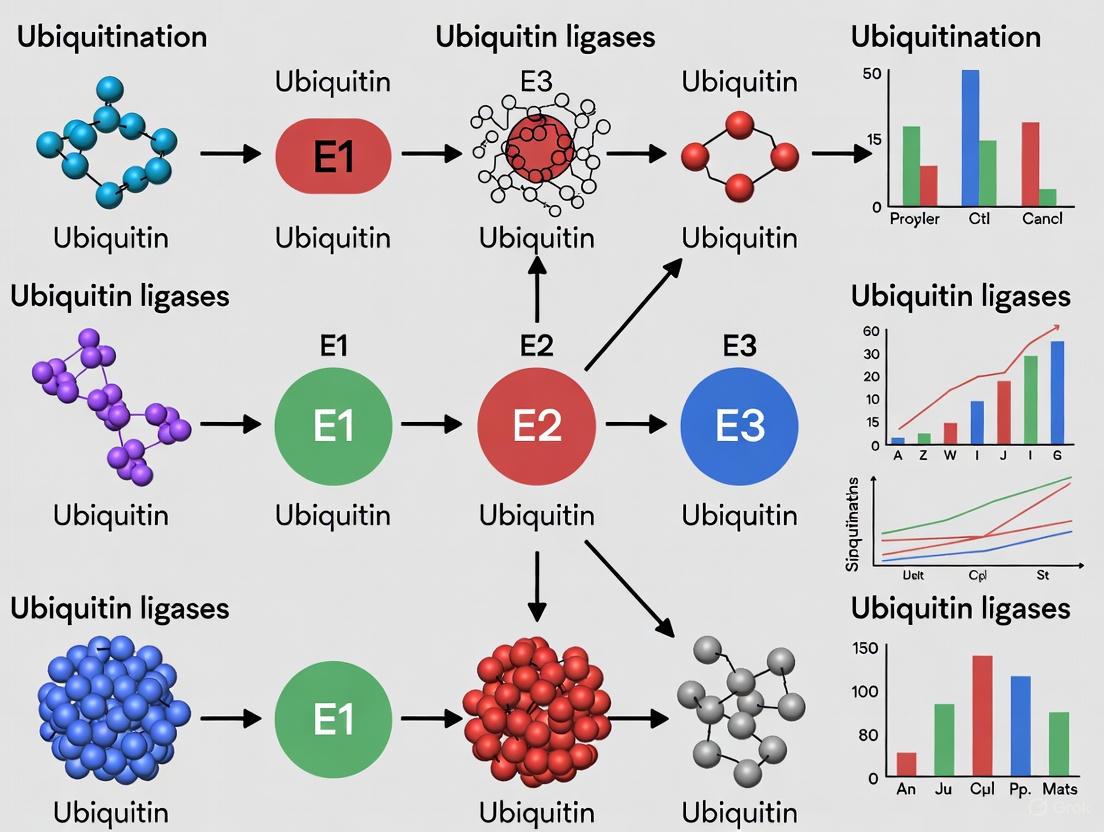
The DNA Damage Response (DDR) is a complex signaling network essential for maintaining genomic integrity. Its failure is a hallmark of cancer. Post-translational modifications, particularly ubiquitination, are central to the precise spatiotemporal regulation of the DDR. Ubiquitination, the covalent attachment of the small protein ubiquitin to substrate proteins, is orchestrated by a sequential enzymatic cascade involving E1 (activating), E2 (conjugating), and E3 (ligating) enzymes. This process can target proteins for proteasomal degradation, alter their activity, or mediate critical protein-protein interactions at DNA repair foci. Understanding this cascade is paramount for developing novel cancer therapeutics that target the DDR.
The Enzymatic Cascade: E1, E2, and E3 Mechanics
The ubiquitination cascade is a three-step process that results in the attachment of ubiquitin to a lysine residue on a substrate protein.
- Step 1: Activation by E1. The E1 ubiquitin-activating enzyme uses ATP to form a high-energy thioester bond between its active-site cysteine and the C-terminus of ubiquitin.
- Step 2: Conjugation by E2. The activated ubiquitin is transferred to the active-site cysteine of an E2 ubiquitin-conjugating enzyme.
- Step 3: Ligation by E3. An E3 ubiquitin ligase facilitates the transfer of ubiquitin from the E2 to a specific substrate protein, forming an isopeptide bond. E3s provide the critical substrate specificity to the system.
Ubiquitin itself contains seven lysine residues (K6, K11, K27, K29, K33, K48, K63), allowing for the formation of polyubiquitin chains. Chain topology determines the fate of the modified protein. K48-linked chains typically target proteins for proteasomal degradation, while K63-linked and linear/Met1-linked chains are key non-proteolytic signals in DDR signaling, serving as scaffolds to recruit repair proteins.
Diagram 1: Core Ubiquitination Cascade
Title: Core ubiquitination enzyme mechanism.
E1, E2, and E3 Enzymes in DDR Pathways
The DDR employs a specific repertoire of E1, E2, and E3 enzymes to coordinate the detection, signaling, and repair of DNA lesions. The following table summarizes key players.
Table 1: Key Ubiquitination Enzymes in the DNA Damage Response
| Enzyme | Example | Role in DDR | Ubiquitin Linkage | Primary Function in DDR |
|---|---|---|---|---|
| E1 | UBA1 | Master activator for most ubiquitination events in DDR. | N/A | Primes the entire ubiquitination response. |
| E2 | UBC13/UEV1A | Works with RNF168 and others. | K63 | Generates K63-linked chains for repair protein recruitment. |
| E2 | BRCA1/BARD1 | Heterodimer with E3 activity. | K6 | Involved in DNA repair; role in homologous recombination. |
| E3 (RING) | RNF8 | Early responder to DNA double-strand breaks (DSBs). | K63, K48 | Initiates the histone ubiquitination cascade to amplify the signal. |
| E3 (RING) | RNF168 | Amplifies the ubiquitin signal at DSBs. | K63, K13 | Ubiquitinates H2A/H2AX; essential for recruiting 53BP1, BRCA1. |
| E3 (RING) | BRCA1 | Tumor suppressor; functions in complex with BARD1. | Multiple | Promotes homologous recombination (HR) repair. |
| E3 (HECT) | HERC2 | Regulates RNF8 and RNF168. | Multiple | Facilitates RNF168 accumulation at damage sites; regulates XPA in NER. |
| E3 (RBR) | Parkin | Implicated in mitochondrial quality control and DDR. | Multiple | Accumulates at DSBs; promotes mitophagy in response to damage. |
The canonical pathway for DSB repair involves the sequential action of E3s. The E3 RNF8 is recruited to sites of DNA damage and ubiquitinates histones, creating a platform for the recruitment of RNF168. RNF168 then amplifies this signal by further ubiquitinating histone H2A, which recruits downstream effectors like 53BP1 (promoting non-homologous end joining, NHEJ) and BRCA1 (promoting homologous recombination, HR).
Diagram 2: RNF8/RNF168 Cascade at DSBs
Title: RNF8/RNF168 signaling at DNA breaks.
Quantitative Data in DDR Ubiquitination
Quantitative studies are crucial for understanding the kinetics and dynamics of the ubiquitin cascade in DDR.
Table 2: Quantitative Metrics of Ubiquitination in DDR
| Parameter | Experimental Finding | Method Used | Biological Significance |
|---|---|---|---|
| RNF168 Turnover | Half-life at DSBs: ~90 seconds (live-cell imaging). | FRAP (Fluorescence Recovery After Photobleaching) | Indicates a highly dynamic and regulated process at repair foci. |
| Ubiquitin Chain Type at DSBs | ~60-70% K63-linked; ~15-20% K48-linked (by mass spectrometry). | Ubiquitin Chain Restriction (UbiCRest) Assay | Dominance of K63 chains underscores their scaffolding role in DDR. |
| Inhibitor Potency (TAK-243) | IC₅₀ for global ubiquitination: ~5-10 nM; IC₅₀ for cancer cell growth: ~1-50 nM. | Cell Viability Assay (CTG), Immunoblotting | Demonstrates high potency of E1 inhibition as an anticancer strategy. |
| BRCA1/BARD1 Activity | Catalytic rate (k~cat~) for ubiquitin discharge: ~0.02 min⁻¹. | In vitro ubiquitination assay | Provides kinetic insight into the efficiency of this tumor suppressor complex. |
Experimental Protocols for Studying DDR Ubiquitination
Protocol 1: In Vitro Ubiquitination Assay This assay reconstitutes the ubiquitination cascade using purified components to study a specific E2-E3 pair.
- Reaction Setup: In a 30 µL volume, combine:
- 50-100 nM E1 enzyme
- 1-2 µM E2 enzyme
- 0.5-1 µM E3 enzyme (or E3 complex like BRCA1/BARD1)
- 2-5 µM Substrate protein
- 10-20 µg Ubiquitin
- 2 mM ATP
- Reaction Buffer: 50 mM Tris-HCl (pH 7.5), 50 mM NaCl, 5 mM MgCl₂, 1 mM DTT.
- Incubation: Incubate the reaction at 30°C for 60-90 minutes.
- Termination: Stop the reaction by adding 4x Laemmli SDS-PAGE sample buffer with 100 mM DTT.
- Analysis: Resolve proteins by SDS-PAGE and analyze by immunoblotting using antibodies against the substrate, ubiquitin, or specific ubiquitin linkages (e.g., anti-K63-Ub).
Protocol 2: Monitoring Ubiquitination in Cells after DNA Damage
- Cell Treatment: Treat cells (e.g., U2OS, HeLa) with a DNA-damaging agent (e.g., 2 Gy Ionizing Radiation (IR), 1 µM Camptothecin, or 10 µM Etoposide).
- Lysis: At desired time points post-treatment (e.g., 1, 4, 8 hours), lyse cells in RIPA buffer (150 mM NaCl, 1% NP-40, 0.5% sodium deoxycholate, 0.1% SDS, 50 mM Tris pH 8.0) supplemented with 10 mM N-Ethylmaleimide (NEM) to inhibit deubiquitinases (DUBs), and protease/phosphatase inhibitors.
- Immunoprecipitation (IP): Pre-clear the lysate. Incubate with an antibody against the protein of interest (e.g., anti-H2AX, anti-53BP1) and Protein A/G beads for 2-4 hours at 4°C.
- Wash and Elute: Wash beads extensively with lysis buffer. Elute bound proteins with SDS sample buffer.
- Analysis: Perform SDS-PAGE and immunoblotting. Probe for ubiquitin (anti-Ub) to detect ubiquitination of the immunoprecipitated protein.
Diagram 3: IP-Based Ubiquitination Workflow
Title: Immunoprecipitation assay for ubiquitination.
The Scientist's Toolkit: Key Research Reagents
Table 3: Essential Reagents for DDR Ubiquitination Research
| Reagent | Function/Application | Example |
|---|---|---|
| TAK-243 (MLN7243) | A potent, specific inhibitor of the E1 enzyme UBA1. Used to block global ubiquitination and study its functional consequences in DDR. | MedChemExpress, HY-107469 |
| Neratinib | An EGFR/HER2 inhibitor that also covalently inhibits the E2 enzyme UBC13, specifically blocking K63-linked ubiquitination in DDR. | Selleckchem, S2150 |
| Ubiquitin Mutants (K0, K48-only, K63-only) | Mutant ubiquitin plasmids or proteins where all lysines are mutated to arginine (K0) or only a single lysine remains. Essential for defining chain topology in assays. | Boston Biochem, UbiSelect Kits |
| Linkage-Specific Ub Antibodies | Antibodies that specifically recognize polyubiquitin chains linked through K48, K63, etc. Critical for immunoblotting and immunofluorescence. | Cell Signaling Tech (#8081 for K48, #5621 for K63) |
| TUBE (Tandem Ubiquitin-Binding Entity) | Recombinant proteins with high affinity for polyubiquitin chains. Used to enrich and purify ubiquitinated proteins from cell lysates, protecting them from DUBs. | LifeSensors, UM401, UM402 |
| DNA Damage Inducers | Pharmacological agents to induce specific DNA lesions (e.g., Etoposide for DSBs, Hydroxyurea for replication stress). | Sigma-Aldrich |
The ubiquitination cascade in the DDR represents a fertile ground for cancer drug discovery. The dependency of many cancers on robust DDR pathways for survival, especially those with underlying DNA repair deficiencies (e.g., BRCA-mutant cancers), creates a therapeutic window. Key strategies include:
- E1 Inhibition: TAK-243 is in clinical trials, inducing global ubiquitination shutdown and catastrophic proteotoxic stress.
- Targeting Specific E3s: PROTACs (Proteolysis Targeting Chimeras) hijack E3s like VHL or CRBN to degrade oncoproteins. Developing inhibitors for DDR-specific E3s is an active area.
- USP Inhibitors: Inhibiting Deubiquitinating Enzymes (DUBs) that reverse DDR signaling, such as USP1 or USP7, can hyper-stabilize ubiquitin signals and disrupt repair.
In conclusion, the E1-E2-E3 enzymatic cascade is a master regulator of the DDR, controlling the fidelity and choice of DNA repair pathways. Its precise mechanistic dissection, aided by the quantitative and experimental approaches outlined here, continues to reveal novel vulnerabilities that can be exploited for targeted cancer therapy.
Ubiquitination, a pivotal post-translational modification, was initially recognized for its role in targeting proteins for proteasomal degradation. However, it is now established as a versatile regulatory mechanism influencing nearly every aspect of cellular function, with particular significance in the DNA damage response (DDR) and cancer pathogenesis [1] [2]. The modification involves the covalent attachment of ubiquitin, a 76-amino acid polypeptide, to substrate proteins. This process is catalyzed by a sequential enzymatic cascade involving ubiquitin-activating (E1), conjugating (E2), and ligase (E3) enzymes [1] [3]. The functional outcome of ubiquitination is profoundly determined by the topology of the ubiquitin modification. Monoubiquitination, the attachment of a single ubiquitin moiety, and polyubiquitination, the formation of ubiquitin chains, can produce diverse signals interpreted by the cell through specific ubiquitin-binding domains (UBDs) [1]. The complexity of this "ubiquitin code" is immense, as ubiquitin itself contains seven lysine residues (K6, K11, K27, K29, K33, K48, K63) and an N-terminal methionine (M1), all of which can form structurally and functionally distinct polyubiquitin chains [2]. This review delineates the functional diversity of mono-ubiquitination and various polyubiquitin chains, framing their roles within the context of DDR and the subsequent implications for cancer research and therapeutic development.
The Ubiquitination Machinery and Signaling Output
The Enzymatic Cascade
The ubiquitination process is a ATP-dependent, three-step enzymatic cascade:
- Activation (E1): A ubiquitin-activating enzyme (E1) utilizes ATP to adenylate the C-terminus of ubiquitin, forming a high-energy thioester bond between a cysteine residue in its active site and ubiquitin (E1~Ub) [1] [3].
- Conjugation (E2): The activated ubiquitin is then transferred to a cysteine residue of a ubiquitin-conjugating enzyme (E2), forming a similar E2~Ub thioester intermediate [1] [3].
- Ligation (E3): Finally, a ubiquitin ligase (E3) facilitates the transfer of ubiquitin from the E2 to a lysine ε-amino group on the substrate protein. E3s, of which there are ~600 in humans, provide substrate specificity. They primarily fall into two classes: RING E3s that act as scaffolds to bring the E2 and substrate together, and HECT E3s that form a catalytic thioester intermediate with ubiquitin before transferring it to the substrate [1] [3].
This process is reversible through the action of deubiquitinating enzymes (DUBs), which cleave ubiquitin from substrates, providing dynamic control over ubiquitin signaling [1] [2].
Ubiquitin Chain Diversity and Functional Consequences
The modification is not a single event but can take several forms, each with distinct functional consequences:
- Monoubiquitination: Attachment of one ubiquitin molecule to a single lysine on a substrate. It often serves as a signaling event, regulating processes like endocytosis, histone function, and DNA repair [1] [2].
- Multi-Monoubiquitination: Attachment of single ubiquitin molecules to multiple different lysine residues on the same substrate protein [1].
- Polyubiquitination: Formation of a chain of ubiquitin molecules linked through one of the eight linkage sites on ubiquitin itself. The chain topology dictates the functional outcome [1] [2]:
- K48-linked chains: The canonical signal for proteasomal degradation of the modified substrate [1] [4].
- K63-linked chains: Primarily involved in non-proteolytic signaling, regulating processes like DNA repair, kinase activation, and inflammation [1] [4].
- Other linkages (K6, K11, K27, K29, K33, M1/linear): Implicated in various processes, including DNA repair, autophagy, and immune signaling [1] [2].
The following diagram illustrates the ubiquitination cascade and the diverse functional outcomes driven by different ubiquitin modifications.
The different ubiquitin linkages are utilized by the cell to generate a complex code, with distinct chain topologies directing specific biological outcomes. The table below summarizes the key characteristics and primary functions of the major ubiquitin linkage types.
Table 1: Functional Diversity of Ubiquitin Linkages in Cellular Signaling and Disease
| Linkage Type | Chain Topology | Primary Functional Role | Role in DNA Damage Response (DDR) | Implication in Cancer |
|---|---|---|---|---|
| Monoubiquitination | Single ubiquitin moiety | Signal for DNA repair, endocytosis, histone regulation, transcriptional activation [1] [2] | Recruitment of repair factors like BRCA1 and RAD51; H2A/H2B monoubiquitination in chromatin remodeling [1] [5] | Altered DNA repair fidelity; dysregulated growth factor signaling [2] |
| K48-linked | Closed conformation | Canonical signal for proteasomal degradation [1] [4] | Termination of DDR by degrading checkpoint and repair proteins [1] | Stabilization of oncoproteins (e.g., c-Myc) or destabilization of tumor suppressors (e.g., p53) [3] [2] |
| K63-linked | Extended conformation | Non-proteolytic signaling: kinase activation, DNA repair, protein trafficking, inflammation [1] [4] | Facilitates recruitment and activation of DDR kinases (e.g., ATM, ATR) and repair complexes at damage sites [1] [4] | Activates pro-tumorigenic pathways (PI3K/Akt, NF-κB); promotes invasion and metastasis [4] |
| K6-linked | Not well characterized | Implicated in DNA repair, mitochondrial homeostasis [1] | Involved in the Fanconi Anemia pathway for interstrand crosslink repair [1] | Potential role in genomic instability [1] |
| K11-linked | Unique mixed conformation | Cell cycle regulation, ER-associated degradation (ERAD) [1] | Regulation of mitotic checkpoints in response to damage [1] | Dysregulated in various cancers; target of APC/C E3 ligase [1] |
| K27-linked | Not well characterized | Innate immune signaling, mitophagy [2] | Emerging role in DDR pathway choice [2] | Linked to tumor immune evasion [2] |
| K29-linked | Not well characterized | Targeting to proteasomal/lysosomal degradation [1] | Potential role in degrading DDR proteins [1] | Altered degradation of oncogenic substrates [1] |
| M1-linear | Linear chain | NF-κB activation, inflammation, cell death [2] | Regulates NF-κB-mediated survival signaling in response to genotoxic stress [2] | Promotes pro-survival signaling in lymphoma and other cancers [2] |
Mono-ubiquitination and K63-Linked Ubiquitination in DNA Damage Response
The DDR is a paradigm for the non-degradative functions of ubiquitination. The coordinated actions of monoubiquitination and K63-linked polyubiquitination are critical for the efficient detection, signaling, and repair of DNA lesions, particularly double-strand breaks (DSBs).
Monoubiquitination in DDR
Monoubiquitination acts as a dynamic beacon in the DDR:
- Histone Monoubiquitination: The E3 ligases RNF2 and BMI1 catalyze the monoubiquitination of histone H2A at lysine 119. This modification contributes to chromatin condensation and transcriptional repression around DSB sites, facilitating the assembly of repair complexes [2]. Conversely, monoubiquitination of histone H2B is involved in transcription-coupled repair mechanisms.
- Recruitment of Repair Factors: Key DDR proteins are regulated by monoubiquitination. For instance, the monoubiquitination of FANCD2 and FANCI within the Fanconi Anemia (FA) pathway is an essential step for their recruitment to DNA interstrand crosslinks and their function in repair [1].
- Regulation of Immune Checkpoints: Beyond direct repair, monoubiquitination of the immune checkpoint protein PD-L1 at K263 by the E3 ligase AIP4 promotes its internalization and lysosomal degradation, thereby potentially inhibiting immune escape of cancer cells [2].
K63-Linked Ubiquitination in DDR
K63-linked ubiquitin chains serve as a central scaffolding platform for the DDR:
- RNF8/RNF168 Cascade: Following DNA damage, the E3 ligases RNF8 and RNF168 are sequentially recruited to DSB sites. They catalyze the extensive deposition of K63-linked ubiquitin chains on histones H2A and H2AX. This creates a binding platform that is recognized by UBD-containing proteins such as BRCA1, 53BP1, and RAP80, which are essential for mediating downstream repair processes like homologous recombination (HR) and non-homologous end joining (NHEJ) [1].
- Kinase Activation: K63-linked ubiquitination directly activates key kinases in the DDR. For example, the ubiquitination of the kinase Akt by the E3 ligase TRAF6 promotes its membrane translocation and activation, contributing to cell survival signals upon damage [4].
The diagram below integrates these mechanisms into a cohesive signaling pathway activated at DNA double-strand break sites.
Experimental Methods for Studying Ubiquitination
Deciphering the ubiquitin code requires sophisticated methodologies to identify substrates, specific linkage types, and functional consequences.
Ubiquitinomics and Proteomic Profiling
Label-free Quantitative Ubiquitinomics is a powerful mass spectrometry-based approach for system-wide profiling of ubiquitination sites [6].
- Workflow: Complex protein extracts from tissues or cells (e.g., cancer vs. normal) are digested with a protease like trypsin.
- Ubiquitin Remnant Enrichment: The resulting peptides are incubated with anti-K-ε-GG antibody beads (PTMScan Ubiquitin Remnant Motif Kit), which specifically enrich for peptides containing the diglycine (K-ε-GG) remnant left on lysine residues after tryptic digestion of ubiquitinated proteins.
- Identification and Quantification: The enriched peptides are analyzed by liquid chromatography-tandem mass spectrometry (LC-MS/MS). The identification of the K-ε-GG signature allows for the precise mapping of ubiquitination sites, while label-free quantification compares the abundance of these sites across different samples [6].
- Application: This technique was used to identify 1,249 ubiquitinated sites within 608 differentially ubiquitinated proteins (DUPs) in human sigmoid colon cancer tissues, revealing pathway alterations in glycolysis, ferroptosis, and Salmonella infection [6].
Functional Validation Experiments
Following proteomic discovery, functional validation is crucial:
- In Vitro Ubiquitination Assays: These reconstitute the ubiquitination cascade using purified components: E1 enzyme, E2 enzyme, E3 ligase (e.g., RNF168), ATP, ubiquitin, and the substrate protein (e.g., histone H2A). The reaction products are analyzed by western blot to detect slower-migrating ubiquitinated forms of the substrate, confirming a direct relationship [1].
- Mutagenesis: To confirm the functional importance of a specific ubiquitination site, the target lysine residue in the substrate is mutated to arginine (K→R), which prevents ubiquitination. The functional properties of the wild-type and mutant protein (e.g., ability to activate signaling, localize to DNA damage sites, or be degraded) are then compared in cellular models [2] [4].
- DUB Specificity Assays: To determine which DUB reverses a specific modification, purified DUBs (e.g., OTUD7B for K63 chains, OTULIN for M1-linear chains) are incubated with ubiquitinated substrates or defined ubiquitin chains. Chain cleavage is monitored by western blot or mass spectrometry to establish DUB linkage specificity [2].
The Scientist's Toolkit: Key Research Reagents
The following table details essential reagents and tools used in ubiquitination research, as featured in the cited studies.
Table 2: Key Research Reagents for Ubiquitination Studies
| Reagent / Tool | Function and Application in Research | Example Use Case |
|---|---|---|
| Anti-K-ε-GG Antibody (PTMScan) | Immuno-enrichment of tryptic peptides containing the di-glycine lysine remnant for LC-MS/MS-based ubiquitinome analysis [6]. | Identification of differentially ubiquitinated proteins (DUPs) and sites in cancer tissues versus normal controls [6]. |
| Specific E3 Ligase Inhibitors (e.g., Nutlin-3a) | Small molecule that disrupts the MDM2-p53 interaction, stabilizing p53 and activating its tumor suppressor function [3]. | Studying p53-dependent apoptosis and cell cycle arrest; model therapeutic for cancers with wild-type p53 [3]. |
| Linkage-Specific Ubiquitin Antibodies | Antibodies that specifically recognize polyubiquitin chains formed through a particular lysine linkage (e.g., K48-only or K63-only). | Determining the topology of ubiquitin chains on a substrate protein via western blot or immunofluorescence [4]. |
| Activity-Based DUB Probes | Ubiquitin derivatives with electrophilic traps that covalently bind to the active sites of catalytically active DUBs. | Profiling active DUB families in cell lysates and identifying specific DUBs involved in a pathway [2]. |
| Tandem Ubiquitin-Binding Entities (TUBEs) | Engineered protein reagents with high affinity for polyubiquitin chains, which can protect substrates from deubiquitination and be used for purification. | Isolation and characterization of ubiquitinated proteins and protein complexes from cellular extracts [1]. |
| PROTACs (Proteolysis Targeting Chimeras) | Bifunctional molecules that recruit an E3 ligase to a target protein of interest, inducing its ubiquitination and degradation [2]. | Targeted protein degradation for functional studies and as a novel therapeutic strategy (e.g., ARV-110 targeting the androgen receptor) [2]. |
The functional diversity of ubiquitination presents a rich landscape for therapeutic intervention in cancer. Strategies have evolved beyond proteasome inhibition (e.g., Bortezomib) to include highly specific agents [3].
- E3 Ligase-Targeted Therapies: Small molecules like Nutlin-3a (targeting MDM2) aim to reactivate p53 in tumors. Immunomodulatory drugs (Thalidomide, Lenalidomide) recruit novel substrates to the CRL4CRBN E3 complex, leading to their degradation [3].
- DUB Inhibitors: Inhibiting specific DUBs can modulate the stability of oncoproteins or key signaling molecules. For instance, targeting USP2, which stabilizes PD-1, could enhance anti-tumor immunity [2].
- Next-Generation Degraders: PROTACs and molecular glues (e.g., ARV-110, ARV-471, CC-90009) represent a paradigm shift, hijacking the ubiquitin system to deliberately degrade previously "undruggable" oncogenic targets [2].
In conclusion, the functional roles of monoubiquitination and the various polyubiquitin chains extend far beyond protein degradation. They form a sophisticated code that orchestrates the DNA damage response, and its dysregulation is a hallmark of cancer. The continued elucidation of this code, powered by advanced ubiquitinomics and functional studies, is uncovering a new generation of therapeutic targets and modalities, offering promising avenues for precise cancer interventions.
The RNF8/RNF168 signaling axis constitutes a critical ubiquitination cascade in the DNA damage response (DDR), orchestrating the repair of double-strand breaks (DSBs) through coordinated recruitment of repair factors. This ubiquitin-driven pathway amplifies DNA damage signals, facilitates the assembly of BRCA1 and 53BP1 repair complexes at chromatin lesions, and ultimately influences the critical choice between homologous recombination (HR) and non-homologous end joining (NHEJ) repair pathways. Dysregulation of this axis contributes to genomic instability, cancer predisposition, and human diseases such as RIDDLE syndrome. This technical review examines the molecular architecture, regulatory mechanisms, and experimental approaches for investigating the RNF8/RNF168 pathway, providing researchers with foundational knowledge and methodologies to advance targeted therapeutic strategies in cancer treatment.
DNA double-strand breaks (DSBs) represent one of the most deleterious forms of DNA damage, with unrepaired lesions leading to genomic instability, chromosomal translocations, and cell death. To counteract this threat, cells have evolved sophisticated DNA damage response (DDR) mechanisms that sense, signal, and repair DSBs [7]. The cellular response to DSBs occurs in the context of chromatin and involves a highly coordinated series of post-translational modifications (PTMs) including phosphorylation, ubiquitination, and SUMOylation, which collectively regulate the recruitment and activity of DNA repair proteins [8] [9].
Ubiquitination has emerged as a central regulatory mechanism in the DDR, with E3 ubiquitin ligases serving as critical determinants of substrate specificity. The ubiquitination process involves a sequential enzymatic cascade: a ubiquitin-activating enzyme (E1) activates ubiquitin, a ubiquitin-conjugating enzyme (E2) receives the activated ubiquitin, and a ubiquitin ligase (E3) facilitates the transfer of ubiquitin to specific substrate proteins [10] [11]. RING-type E3 ligases, the largest class of E3 enzymes, function as scaffolds that bring E2 enzymes into proximity with their substrate proteins, thereby promoting ubiquitin transfer [10]. The RNF8/RNF168 axis represents a pivotal ubiquitin signaling pathway that controls DSB repair by regulating the assembly of repair complexes at damaged chromatin, making it a focus of intense research in cancer biology and therapeutic development [9] [12].
The RNF8/RNF168 Signaling Cascade: Molecular Mechanisms
Pathway Initiation and RNF8 Recruitment
The RNF8/RNF168 signaling cascade initiates with the activation of the ataxia-telangiectasia mutated (ATM) kinase at DSB sites. ATM phosphorylates the histone variant H2AX on serine 139 (generating γ-H2AX), creating a binding platform for the mediator protein MDC1 [9]. RNF8 is then recruited to DSBs through the interaction of its N-terminal FHA domain with ATM-phosphorylated TQXF motifs on MDC1 [13] [9]. Once localized to chromatin lesions, RNF8, in concert with the E2 enzyme UBC13, catalyzes the formation of K63-linked ubiquitin chains on currently unidentified non-nucleosomal target proteins in the vicinity of damaged chromatin, referred to as "Target X" [9].
Table 1: Key Domains and Functions of RNF8
| Domain | Location | Function | Structural Features |
|---|---|---|---|
| FHA Domain | N-terminal | Recruits RNF8 to DSBs via interaction with phosphorylated MDC1 | Phosphopeptide recognition domain |
| RING Domain | C-terminal | Catalyzes ubiquitin transfer from E2 to substrates | C3HC4-type RING finger; E2 interaction |
RNF168 Recruitment and Amplification
RNF168 is recruited to DSBs through its ubiquitin-dependent recruitment modules (UDM1 and UDM2), which recognize the K63-linked ubiquitin chains deposited by RNF8 [7]. The UDM1 module, consisting of LRM1, UMI, and MIU1 motifs, preferentially binds K63-linked ubiquitin chains and functions downstream of RNF8 [7]. Once recruited, RNF168 catalyzes the monoubiquitination of histone H2A and H2AX at K13/K15, creating an amplification loop that facilitates robust accumulation of RNF168 at damage sites through its UDM2 module [7] [9]. This self-amplifying mechanism establishes a strong local ubiquitin signal that serves as a docking platform for downstream repair factors.
Table 2: Structural and Functional Domains of RNF168
| Domain | Location | Function | Clinical Significance |
|---|---|---|---|
| RING Domain | N-terminal (a.a. 15-58) | Catalytic E3 ligase activity; recognizes E2~Ub conjugate | Mutations associated with RIDDLE syndrome |
| UDM1 | Middle region | Initial recruitment via K63-ubiquitin chain binding | Contains LRM1, UMI, and MIU1 motifs |
| UDM2 | C-terminal region | Self-amplification via H2A/X K15ub binding | Contains UAD, MIU2, and LRM2 motifs |
Recruitment of Downstream Effectors: BRCA1 and 53BP1
The ubiquitin landscape established by RNF8 and RNF168 directly regulates the recruitment of two critical downstream effectors with opposing functions in DSB repair pathway choice: the BRCA1-BARD1 complex and 53BP1 [9] [12]. BRCA1 is recruited to DSBs through its interaction partner RAP80, which binds to K63-linked ubiquitin chains deposited by RNF8/RNF168 [9] [12]. In contrast, 53BP1 recruitment requires RNF168-mediated H2A/X ubiquitination and recognizes dimethylated histone H4K20, with the RNF8/RNF168 pathway facilitating the removal of competing factors like KDM4A/JMJD2A that antagonize 53BP1 binding [14]. The balanced recruitment of these factors determines whether cells prioritize homologous recombination (HR) or non-homologous end joining (NHEJ) repair pathways.
Table 3: Experimental Evidence for RNF8/RNF168 in DSB Repair
| Experimental Approach | Key Findings | Biological Significance | Reference |
|---|---|---|---|
| RNF168 knockout mice | 60% developed hyperplastic lesions at 13 months; 18% developed mammary adenocarcinomas | RNF8 deficiency promotes genomic instability and tumorigenesis | [13] |
| Clinical data analysis (5,143 cases) | Low full-length RNF8 expression correlates with poor prognosis in luminal B and basal-like breast cancer | RNF8 serves as a potential prognostic biomarker | [13] |
| RNF8/RNF168-dependent degradation | Degradation of KDM4A/JMJD2A triggers 53BP1 recruitment to DNA damage sites | Regulation of repair pathway choice through histone mark accessibility | [14] |
| ZNF451-RNF168 SUMOylation | ZNF451 catalyzes SUMO2 modification of RNF168, stabilizing it at damage sites | SUMO-ubiquitin crosstalk regulates RNF168 activity | [15] |
Table 4: RNF8/RNF168-Dependent Ubiquitination Events in DSB Repair
| Ubiquitination Target | Ubiquitin Linkage Type | Functional Consequence | Regulating E3 Ligase |
|---|---|---|---|
| Histone H2A/H2AX (K13/K15) | Monoubiquitination | Recruitment of 53BP1 and BRCA1 complexes | RNF168 |
| KDM4A/JMJD2A | K48-linked (proteasomal degradation) | Removal of 53BP1 antagonist, promotes NHEJ | RNF8/RNF168 |
| Unknown "Target X" | K63-linked polyubiquitination | Recruitment of RNF168 to damage sites | RNF8 |
Experimental Protocols for Studying the RNF8/RNF168 Axis
Assessing RNF8/RNF168 Recruitment to DSBs by Immunofluorescence
Purpose: To visualize and quantify the recruitment of RNF8 and RNF168 to sites of DNA damage. Methodology:
- Cell Culture and DNA Damage Induction: Seed appropriate cells (e.g., U2OS, HeLa, or MEFs) on glass coverslips. Induce DSBs using ionizing radiation (2-10 Gy) or laser microirradiation, or treat with DSB-inducing agents such as neocarzinostatin (NCS).
- Immunostaining: At specific time points post-damage, fix cells with 4% paraformaldehyde, permeabilize with 0.5% Triton X-100, and block with 5% BSA. Incubate with primary antibodies against RNF8 or RNF168, followed by species-appropriate fluorescent secondary antibodies.
- Counterstaining and Microscopy: Counterstain with DAPI to visualize nuclei and γ-H2AX to mark DSB sites. Analyze samples by confocal microscopy, quantifying foci number and intensity using image analysis software (e.g., ImageJ). Key Controls: Include cells treated with siRNA targeting RNF8 or RNF168 to verify antibody specificity [13] [7].
Analyzing RNF168-Dependent Ubiquitination by Immunoblotting
Purpose: To detect RNF168-mediated ubiquitination of histone H2A/H2AX. Methodology:
- Cell Lysis and Fractionation: Harvest cells after DNA damage induction and lyse using RIPA buffer. For chromatin-enriched fractions, pre-extract cells with CSK buffer before solubilizing chromatin.
- Immunoblotting: Separate proteins by SDS-PAGE and transfer to PVDF membranes. Probe with antibodies specific for ubiquitinated H2A (K13/K15) or H2AX (K13/K15). Validate equal loading with histone H3 or total H2A/H2AX antibodies.
- Quantification: Use densitometry to quantify ubiquitination levels normalized to loading controls. Key Reagents: Commercial antibodies specifically recognizing H2A ubiquitinated at K13/K15 are essential for accurate detection [7] [9].
Functional Assays for DSB Repair Pathway Choice
Purpose: To determine how RNF8/RNF168 activity influences HR versus NHEJ efficiency. HR and NHEJ Reporter Assays:
- Stable Cell Line Generation: Transfect cells with DR-GFP (for HR) or EJ5-GFP (for NHEJ) reporter constructs and select stable integrants.
- DSB Induction and Repair Measurement: Introduce DSBs in the reporter locus using I-SceI endonuclease. Quantify repair efficiency by flow cytometric analysis of GFP-positive cells 48-72 hours post-transfection.
- Pathway Manipulation: Knock down RNF8 or RNF168 using siRNA and compare repair efficiency to control cells. Alternative Approach: Monitor the formation of RAD51 foci (HR marker) versus 53BP1 foci (NHEJ promoter) in cells with modulated RNF8/RNF168 expression [9] [12].
Signaling Pathway Visualization
Diagram 1: RNF8/RNF168 Signaling Cascade in DSB Repair. This diagram illustrates the sequential recruitment and activation of RNF8 and RNF168 at DNA double-strand breaks, culminating in the recruitment of BRCA1 and 53BP1 to influence repair pathway choice between homologous recombination and non-homologous end joining.
The Scientist's Toolkit: Essential Research Reagents
Table 5: Key Research Reagents for Studying RNF8/RNF168 Function
| Reagent/Tool | Specific Example | Experimental Application | Key Function |
|---|---|---|---|
| RNF8/RNF168 Antibodies | Anti-RNF168 (e.g., Abcam ab154833) | Immunofluorescence, Immunoblotting | Detect protein localization and expression |
| Ubiquitin Linkage-Specific Antibodies | Anti-K63-ubiquitin chain antibodies | Immunoblotting | Identify specific ubiquitin linkages |
| H2A Ubiquitination-Specific Antibodies | Anti-H2A-K13ub/K15ub | Chromatin immunoprecipitation, Immunoblotting | Detect RNF168-dependent histone modification |
| siRNA/shRNA Libraries | ON-TARGETplus siRNA pools | Functional knockdown studies | Deplete RNF8/RNF168 to assess functional consequences |
| DDR Inhibitors | ATM inhibitors (KU-55933) | Pathway modulation | Dissect regulatory relationships in the cascade |
| Reporter Cell Lines | DR-GFP (HR), EJ5-GFP (NHEJ) | Repair pathway choice assays | Quantify HR and NHEJ efficiency |
| DNA Damaging Agents | Neocarzinostatin (NCS), Etoposide | Controlled induction of DSBs | Activate the DDR under experimental conditions |
Regulatory Mechanisms and Cross-Talk
The RNF8/RNF168 axis is subject to multiple layers of regulation to ensure appropriate signaling amplitude and duration. Negative feedback mechanisms involve RNF169, which competes with RNF168 for binding to ubiquitinated histones, thereby attenuating the signal [12]. Additionally, the E3 ligase RNF126 directly ubiquitinates RNF168, inhibiting its ability to ubiquitinate γH2AX [12]. Recent research has revealed important SUMO-ubiquitin cross-talk, with ZNF451 catalyzing SUMOylation of RNF168 to stabilize it and enhance its accumulation at damage sites [15]. The mTOR-S6K pathway has also been shown to regulate RNF168, linking growth signaling to DNA damage response [15].
The RNF8/RNF168 pathway interfaces with other post-translational modification systems, including crosstalk with the SUMOylation pathway through proteins like HERC2, which promotes RNF8 oligomerization and facilitates RNF168 recruitment [12]. The proteasome-associated deubiquitinase USP14 regulates DNA damage repair by targeting RNF168-dependent ubiquitination, adding another layer of control [15]. These intricate regulatory networks ensure that the RNF8/RNF168 signaling axis responds appropriately to DNA damage while preventing excessive signaling that could disrupt chromatin structure and function.
The RNF8/RNF168 signaling axis represents a master regulatory module that controls the cellular response to DNA double-strand breaks through coordinated ubiquitin signaling. By establishing a specific ubiquitin landscape at damaged chromatin, this pathway regulates the critical balance between homologous recombination and non-homologous end joining repair pathways. The detailed mechanistic understanding of RNF8/RNF168 function has significant implications for cancer therapy, particularly in exploiting synthetic lethal relationships for targeted treatment approaches.
Future research directions should focus on elucidating the structural basis of RNF8/RNF168 interactions, identifying novel substrates of these E3 ligases, and developing small molecule modulators that can selectively target components of this pathway. The integration of advanced techniques such as cryo-electron microscopy, proximity-dependent biotinylation, and chemical biology approaches will further illuminate the dynamic regulation of this crucial DNA repair pathway. As our understanding of the RNF8/RNF168 axis deepens, so too will opportunities for therapeutic intervention in cancer and other diseases characterized by genomic instability.
The post-translational modification of proteins by ubiquitin is a master regulatory mechanism that controls virtually all aspects of the cellular response to DNA damage, including replication stress. Ubiquitylation involves a sequential enzymatic cascade whereby the E1 activating enzyme, E2 conjugating enzyme, and E3 ligase work in concert to attach the 76-amino acid ubiquitin protein to specific substrate lysine residues [1] [16]. The versatility of this modification arises from the ability of ubiquitin to form different topological structures—including monoubiquitination and various polyubiquitin chains—that create distinct signaling platforms recognized by proteins containing ubiquitin-binding domains (UBDs) [1]. Within the context of DNA damage and cancer research, understanding how ubiquitination regulates specific repair and tolerance pathways has become paramount, as dysregulation of these processes contributes directly to genome instability, cancer predisposition, and response to genotoxic therapies [17].
When replication forks stall at DNA lesions, cells activate sophisticated mechanisms to bypass the damage and complete DNA synthesis. Two crucial ubiquitin-regulated pathways that respond to replication-blocking lesions are Translesion Synthesis (TLS) and the Fanconi Anemia (FA) pathway. While both pathways utilize specialized E3 ubiquitin ligases and ubiquitin-binding effectors to maintain genome stability, they operate through distinct yet interconnected mechanisms. This review provides an in-depth examination of how ubiquitination controls TLS and FA pathway activation in response to replication stress, with particular emphasis on experimental approaches, key regulatory nodes, and therapeutic implications for cancer treatment.
The Ubiquitin Code in DNA Damage Tolerance
Principles of Ubiquitin Signaling
Ubiquitin modification creates a complex "code" that cells decipher to coordinate DNA repair and damage tolerance. Monoubiquitination typically serves as a recruitment signal for DNA repair proteins containing ubiquitin-binding domains, while Lys63-linked polyubiquitin chains often create signaling platforms that facilitate protein complex assembly at damage sites [1]. In contrast, Lys48-linked polyubiquitin chains primarily target substrates for proteasomal degradation [16]. This ubiquitin code is dynamically written by E3 ubiquitin ligases and erased by deubiquitinating enzymes (DUBs), providing exquisite temporal and spatial control over DNA damage response pathways [16].
Ubiquitin-Dependent Recruitment in DNA Repair
The recruitment of repair proteins to sites of DNA damage frequently depends on their ability to recognize specific ubiquitin signals through specialized ubiquitin-binding domains (UBDs) such as ubiquitin-interacting motifs (UIMs) and ubiquitin-binding domains (UBDs) [1]. For example, in the FA pathway, multiple downstream effectors including FAN1 and SLX4 contain ubiquitin-binding motifs that are essential for their recruitment to monoubiquitinated FANCD2-FANCI complexes at stalled replication forks [18]. Similarly, TLS polymerases possess ubiquitin-binding domains that facilitate their interaction with monoubiquitinated PCNA [19]. This paradigm of ubiquitin-dependent recruitment ensures that specialized DNA repair and damage tolerance machinery are specifically localized to sites of replication stress while minimizing inappropriate activity at undamaged DNA.
Ubiquitination in the Fanconi Anemia Pathway
The FA Pathway: From Core Complex to ICL Repair
The Fanconi Anemia pathway represents a specialized DNA repair system dedicated primarily to the resolution of DNA interstrand crosslinks (ICLs), which covalently link both strands of the DNA double helix and present formidable blocks to replication and transcription [18] [20]. The FA pathway comprises at least 23 FANC proteins that function in a coordinated, multi-step process to recognize, incise, and repair ICLs [20]. Pathogenic mutations in any of these genes cause Fanconi anemia, a recessive disorder characterized by bone marrow failure, developmental abnormalities, and extreme cancer predisposition [18].
The central regulatory event in the FA pathway is the monoubiquitination of the FANCD2-FANCI (ID) complex, which serves as a molecular switch that activates the entire repair cascade [18] [20]. This critical modification is catalyzed by the FA core complex—a multi-subunit E3 ubiquitin ligase consisting of FANCA, FANCB, FANCC, FANCE, FANCF, FANCG, FANCL, and associated proteins FAAP20 and FAAP100 [20]. Within this complex, FANCL provides the catalytic RING domain that confers E3 ligase activity, while FANCT/UBE2T serves as the dedicated E2 conjugating enzyme [20]. The monoubiquitination occurs specifically at lysine 561 of FANCD2 and lysine 523 of FANCI, creating a binding platform for downstream repair factors including nucleases and homologous recombination proteins [18].
Table 1: Core Components of the Fanconi Anemia Ubiquitin Ligase Complex
| Component | Gene | Function | Domain Features |
|---|---|---|---|
| FANCL | FANCL | Catalytic E3 ubiquitin ligase | RING, ELF, DRWD domains |
| FANCT | UBE2T | E2 ubiquitin-conjugating enzyme | Ubiquitin-conjugating (E2) domain |
| FANCA | FANCA | Core complex scaffold | - |
| FANCB | FANCB | Core complex scaffold | - |
| FANCC | FANCC | Core complex scaffold | - |
| FANCE | FANCE | Substrate recognition | Facilitates FANCD2 binding |
| FANCF | FANCF | Core complex stabilization | - |
| FANCG | FANCG | Core complex stabilization | - |
Downstream Effectors of the Monoubiquitinated ID Complex
Once monoubiquitinated, the ID complex undergoes a conformational change that enables it to stably associate with chromatin and recruit structure-specific nucleases including FANCQ/XPF and the FANCP/SLX4 scaffold complex [20]. These nucleases perform the critical "unhooking" step whereby incisions are made on either side of the ICL, releasing the crosslink and allowing translation synthesis polymerases to synthesize DNA across the resulting lesion [20]. The repair process is completed through homologous recombination (HR), which involves multiple FA/HR proteins including FANCD1/BRCA2, FANCN/PALB2, FANCO/RAD51C, FANCR/RAD51, and FANCS/BRCA1 [20]. Finally, the pathway is inactivated through deubiquitination of the ID complex by the USP1 deubiquitinating enzyme, restoring the pathway to its basal state [20].
Figure 1: The Fanconi Anemia DNA Repair Pathway. The FA core complex, with FANCL as the catalytic E3 subunit and UBE2T as the E2, monoubiquitinates the FANCI-FANCD2 (ID) complex in response to interstrand crosslinks. The monoubiquitinated ID complex recruits nucleases and other downstream effectors to complete ICL repair.
Pathophysiological Implications of FA Pathway Deficiency
The clinical manifestations of Fanconi anemia underscore the critical importance of the FA pathway in maintaining genomic stability. Studies using mouse models have revealed that endogenous metabolites, particularly reactive aldehydes such as acetaldehyde and formaldehyde, constitute a major source of endogenous DNA damage that requires the FA pathway for repair [20]. This has led to a "two-tier" model of genome protection in which the first tier consists of detoxifying enzymes like ALDH2 and ADH5 that convert reactive aldehydes to harmless metabolites, while the second tier is the FA pathway that repairs any DNA lesions that escape detoxification [20]. Deficiency in both tiers leads to accelerated bone marrow failure and leukemogenesis, highlighting the synergistic relationship between metabolic protection and DNA repair in preventing tissue degeneration and cancer [20].
Ubiquitination in Translesion Synthesis
TLS Polymerases and Their Regulation
Translesion Synthesis is a DNA damage tolerance mechanism that enables replication to proceed past blocking DNA lesions through the deployment of specialized DNA polymerases. Unlike high-fidelity replicative polymerases, TLS polymerases possess more open active sites that can accommodate damaged DNA templates, though this comes at the cost of reduced fidelity when copying undamaged DNA [19]. The mammalian TLS machinery includes several specialized polymerases such as Polη, Polκ, Polι, Rev1, and Polζ (a complex containing Rev3L, Rev7, and other subunits), each with distinct lesion bypass specificities [21] [19].
The central regulatory mechanism governing TLS polymerase recruitment involves monoubiquitination of PCNA (proliferating cell nuclear antigen), the sliding clamp that tethers DNA polymerases to the replication machinery [19]. In response to replication-blocking lesions, PCNA becomes monoubiquitinated at lysine 164 through the coordinated action of the Rad6 E2 enzyme and Rad18 E3 ligase [22] [19]. Monoubiquitinated PCNA then serves as a binding platform for TLS polymerases, many of which contain ubiquitin-binding domains that facilitate their recruitment to stalled replication forks [19].
Temporal and Mechanistic Aspects of TLS
The precise timing and location of TLS activity has been a subject of ongoing investigation. Early models proposed that TLS polymerases are recruited directly to stalled replication forks to restart replication in an "on-the-fly" manner. However, recent evidence indicates that TLS frequently occurs after replication fork restart, primarily filling single-stranded DNA gaps left behind by re-priming events downstream of lesions [21]. This gap-filling model is supported by studies showing that TLS polymerase recruitment depends on PrimPol, a primase-polymerase that re-initiates DNA synthesis downstream of replication-blocking lesions [21].
Table 2: Translesion Synthesis Polymerases and Their Characteristics
| Polymerase | Lesion Specificity | Ubiquitin Binding Domain | Cellular Function |
|---|---|---|---|
| Polη | Cisplatin adducts, UV-induced cyclobutane pyrimidine dimers | UBZ | Error-free bypass of UV lesions |
| Polκ | Benzo[a]pyrene diol epoxide (BPDE) adducts | - | Error-free bypass of bulky adducts |
| Polι | Minor groove adducts | - | Insertion polymerase |
| Rev1 | Template for deoxycytidine monophosphate insertion | UBM | Scaffold function, dCMP transferase |
| Polζ (Rev3-Rev7) | Extension across from various lesions | - | Major extender polymerase |
The requirement for PCNA ubiquitination in TLS appears to vary across organisms and experimental systems. In avian DT40 cells, PCNA ubiquitination is not required for maintaining normal fork progression on damaged DNA but is essential for filling post-replicative gaps [23]. Similarly, in mammalian cells, PCNA ubiquitination significantly enhances TLS efficiency but is not absolutely essential, as TLS polymerases can be recruited through alternative mechanisms in its absence [19]. This partial redundancy ensures maintenance of essential DNA damage tolerance capacity even when the primary regulatory mechanism is compromised.
Lesion-Specific Polymerase Recruitment
Different types of DNA damage trigger the recruitment of specific TLS polymerases through mechanisms that are still being elucidated. Recent studies using proximity ligation assays (PLA) to monitor endogenous polymerase recruitment have demonstrated that Polκ is specifically recruited to benzo[a]pyrene diol epoxide (BPDE) lesions, while Polη is preferentially recruited to cisplatin adducts [21]. This lesion-specific polymerase recruitment depends on PrimPol-mediated replication restart and occurs predominantly during gap filling rather than directly at stalled forks [21]. When the appropriate TLS polymerase is deficient, unrepaired ssDNA gaps accumulate and are subsequently converted to cytotoxic double-strand breaks, explaining the lesion-specific sensitivity patterns observed in polymerase-deficient cells [21].
Experimental Approaches for Studying Ubiquitination in Replication Stress
Proximity Ligation Assay (PLA) for TLS Polymerase Recruitment
Purpose: To detect and quantify the recruitment of specific TLS polymerases to DNA lesions during replication stress.
Methodology:
- Cell Treatment and EdU Labeling: Treat cells with DNA damaging agents (e.g., 10 μM BPDE or cisplatin) for 1-2 hours, with EdU added during the final 30 minutes to label nascent DNA [21].
- Cell Fixation and Permeabilization: Fix cells with paraformaldehyde and permeabilize with Triton X-100.
- Click Chemistry Reaction: Use copper-catalyzed azide-alkyne cycloaddition to conjugate biotin to EdU-labeled DNA.
- Antibody Incubation: Incubate with primary antibodies against the TLS polymerase of interest (e.g., Polκ or Polη) and streptavidin to detect biotinylated EdU.
- Proximity Ligation: Apply PLUS and MINUS PLA probes against the primary antibody and streptavidin, followed by ligation and amplification using fluorescently labeled oligonucleotides.
- Microscopy and Quantification: Image PLA foci by fluorescence microscopy and quantify foci per nucleus [21].
Key Controls:
- Include untreated controls to establish baseline signals.
- Use polymerase-depleted cells (siRNA) to confirm signal specificity.
- Compare different DNA damaging agents to establish lesion specificity [21].
SIRF Assay for Protein Recruitment to Nascent DNA
Purpose: To quantitatively analyze protein interactions at DNA replication forks using the in situ analysis of protein interactions at DNA replication forks (SIRF) assay.
Methodology:
- EdU Labeling: Pulse-label cells with EdU (10 μM, 10-30 minutes) to incorporate thymidine analog into nascent DNA.
- Cell Fixation and Permeabilization: Fix cells with formaldehyde and permeabilize with 0.5% Triton X-100.
- Click Chemistry: Conjugate biotin-azide to EdU using copper-catalyzed cycloaddition.
- Immunostaining: Incubate with primary antibody against protein of interest and anti-biotin antibody.
- Proximity Ligation: Apply species-specific PLA probes, followed by ligation and rolling circle amplification.
- Fluorescence Detection and Analysis: Detect amplification products with fluorescent oligonucleotides and quantify SIRF foci per cell [21].
Applications:
- Measure recruitment of TLS polymerases (Polκ, Polη) to nascent DNA.
- Assess PCNA ubiquitination at replication forks.
- Analyze PrimPol recruitment to stalled replication forks [21].
Figure 2: Experimental Workflow for Proximity Ligation Assays. The diagram illustrates the key steps in PLA-based detection of protein recruitment to DNA damage sites, incorporating EdU labeling for nascent DNA detection and proximity ligation for signal amplification.
Analysis of PCNA Ubiquitination
Purpose: To detect and quantify PCNA monoubiquitination in response to replication stress.
Methodology:
- Cell Lysis: Prepare whole cell extracts or chromatin-enriched fractions in denaturing lysis buffer.
- Immunoprecipitation: Use anti-PCNA antibody conjugated to protein A/G beads for immunoprecipitation.
- Western Blotting: Separate proteins by SDS-PAGE and transfer to PVDF membrane.
- Detection: Probe with anti-ubiquitin and anti-PCNA antibodies to distinguish monoubiquitinated PCNA (shifted band) from unmodified PCNA [19].
Alternative Approach:
- Use cells expressing epitope-tagged ubiquitin (e.g., His-Ub or HA-Ub) for nickel pull-down under denaturing conditions followed by PCNA immunoblotting [19].
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Research Reagents for Studying Ubiquitination in Replication Stress
| Reagent/Cell Line | Specific Application | Function/Mechanism |
|---|---|---|
| PcnaK164R/K164R MEFs | Study PCNA ubiquitination-deficient TLS | Expresses PCNA mutant that cannot be ubiquitinated at K164 [19] |
| Rad18-/- cells | Analyze Rad18-dependent ubiquitination | Lacks the E3 ligase responsible for PCNA monoubiquitination [19] |
| Usp1-/- cells | Study enhanced PCNA ubiquitination | Lacks the deubiquitinating enzyme that removes Ub from PCNA [19] |
| siRNA libraries | Gene knockdown studies | Deplete specific TLS polymerases or FA proteins [21] |
| Anti-BPDE DNA adduct antibody | Detect specific DNA lesions | Recognizes and binds to BPDE-DNA adducts for PLA [21] |
| EdU (5-ethynyl-2'-deoxyuridine) | Nascent DNA labeling | Incorporates into replicating DNA for click chemistry detection [21] |
| PLA (Proximity Ligation Assay) kits | Protein-protein/DNA interactions | Amplifies signals from proximal binding events [21] |
Interplay Between TLS and FA Pathways
Emerging evidence indicates significant functional crosstalk between the TLS and FA pathways in responding to replication stress. The E3 ubiquitin ligase Rad18, which monoubiquitinates PCNA to activate TLS, also contributes to FANCD2 monoubiquitination and FA pathway activation [22]. This functional connection was demonstrated through experiments showing that Rad18 overexpression induces DNA damage-independent FANCD2 monoubiquitination, while Rad18 deficiency attenuates DNA damage-induced FANCD2 modification [22]. However, Rad18-mediated FANCD2 ubiquitination requires an intact FA core complex, indicating that Rad18 functions upstream of the core complex rather than directly ubiquitinating FANCD2 [22].
This interplay between TLS and FA pathways creates a coordinated response network wherein both pathways are activated by common upstream regulators but specialize in different aspects of replication stress management. The FA pathway primarily handles the complex task of ICL repair through nucleolytic incision and homologous recombination, while TLS provides a more rapid mechanism for bypassing simpler replication-blocking lesions. The shared regulation through ubiquitination ensures that both pathways can be coordinately activated in response to different types and levels of replication stress.
Therapeutic Implications and Cancer Relevance
Targeting Ubiquitination in Cancer Therapy
The critical role of ubiquitination in DNA damage response pathways presents attractive opportunities for cancer therapeutic intervention. Many E3 ubiquitin ligases and deubiquitinating enzymes are deregulated in human cancers, making them potential targets for small molecule inhibitors [17]. For example, inhibitors of USP1, the deubiquitinating enzyme that inactivates the FA pathway, have shown promise in sensitizing cancer cells to DNA crosslinking agents [20]. Similarly, targeting the Rad18-mediated PCNA ubiquitination could modulate TLS activity and alter the response to genotoxic therapies.
The synthetic lethal relationships between DNA repair pathways provide particularly promising therapeutic avenues. Cancers with deficiencies in specific DNA repair pathways (e.g., homologous recombination deficiencies in BRCA-mutant cancers) often develop heightened dependence on backup pathways such as TLS [21]. Inhibition of these backup pathways can therefore selectively target repair-deficient cancer cells while sparing normal cells. For instance, the finding that BRCA-deficient cells are hypersensitive to TLS inhibition suggests that TLS polymerases could be therapeutic targets in BRCA-mutant cancers [21].
Biomarker Development and Treatment Stratification
Understanding the regulation of TLS and FA pathways has important implications for cancer biomarker development and treatment stratification. The lesion-specific recruitment patterns of TLS polymerases [21] suggest that polymerase expression levels could predict responses to specific chemotherapeutic agents. Similarly, the expression levels of FA pathway components may serve as biomarkers for sensitivity to crosslinking agents such as cisplatin and mitomycin C [18] [20].
The role of endogenous metabolites in driving DNA damage accumulation in FA-deficient cells [20] also suggests potential preventive strategies aimed at reducing exposure to genotoxic metabolites, particularly in individuals with inherited FA pathway deficiencies. This might include dietary modifications or pharmacological approaches to enhance detoxification of reactive aldehydes in FA patients.
Ubiquitination serves as a central regulatory mechanism that coordinates the cellular response to replication stress through both the Fanconi Anemia and Translesion Synthesis pathways. The FA pathway utilizes a sophisticated multi-component E3 ubiquitin ligase complex to monoubiquitinate the FANCD2-FANCI heterodimer, triggering a complex repair process for DNA interstrand crosslinks. In parallel, the TLS pathway employs Rad18-dependent monoubiquitination of PCNA to recruit specialized polymerases that bypass replication-blocking lesions. While these pathways operate through distinct mechanisms, they exhibit significant functional crosstalk and are often co-regulated in response to replication stress.
Future research directions include elucidating the structural basis for ubiquitin-dependent protein recruitment in these pathways, developing more specific inhibitors targeting key ubiquitin-regulating enzymes, and exploring the therapeutic potential of manipulating these pathways for cancer treatment. The continued dissection of ubiquitin signaling in DNA damage response will undoubtedly yield new insights into genome maintenance mechanisms and provide novel approaches for targeting the vulnerabilities of cancer cells.
The integrity of the genome is continuously challenged by endogenous and exogenous DNA-damaging agents. Among the most deleterious lesions are DNA double-strand breaks (DSBs), which can lead to genomic instability, cellular senescence, and tumorigenesis if not properly repaired [24] [25] [26]. Eukaryotic cells have evolved sophisticated DNA damage response (DDR) systems that detect lesions, signal their presence, and facilitate repair. These processes occur in the context of chromatin, the complex of DNA and proteins that packages the genome within the nucleus. Central to the DDR are post-translational modifications (PTMs) of histones, which alter chromatin structure and create binding platforms for repair factors [27] [24]. Ubiquitination of histones—the covalent attachment of ubiquitin to lysine residues—has emerged as a pivotal regulatory mechanism that guides DNA repair pathway choice and efficiency [28] [24] [25]. Within cancer research, understanding these mechanisms is crucial, as dysregulation of chromatin ubiquitination contributes to tumorigenesis and influences responses to DNA-damaging chemotherapeutics [29] [27].
This review examines the mechanisms and functions of histone ubiquitination in the recruitment of DNA repair factors. We detail the specific ubiquitin marks deposited in response to damage, the enzymatic cascades that create them, the reader proteins that interpret them, and the functional consequences for repair pathway choice, with a particular focus on implications for cancer biology.
Core Mechanisms of Histone Ubiquitination
Histone Ubiquitination Writers and Erasers
Protein ubiquitylation is an enzymatic process involving a cascade of E1 (activating), E2 (conjugating), and E3 (ligating) enzymes. Histone ubiquitination primarily results in monoubiquitylation, which serves a signaling rather than degradative function [28] [30]. The reversal of these marks is catalyzed by deubiquitylating enzymes (DUBs), ensuring dynamic control over the DDR [28].
Table 1: Major Histone Ubiquitin Marks in the DNA Damage Response
| Histone Mark | E3 Ligase(s) | Deubiquitinase(s) | Primary Function | Associated Repair Pathway |
|---|---|---|---|---|
| H2AK13ub/H2AK15ub | RNF168 | n.d. | DSB signaling; 53BP1 recruitment | NHEJ [31] [25] |
| H2AK119ub | Ring2 (PRC1), 2A-HUB | BAP1 | Transcription repression; DDR role emerging | Multiple [28] [30] |
| H2Bub1 (H2BK120ub) | RNF20/RNF40 | USP22, USP3 | Transcription activation; H3K4/H3K79 methylation | HR, NER [29] [28] |
| H2AK127/129ub | BRCA1-BARD1 | n.d. | SMARCAD1 recruitment; HR promotion | HR [25] |
n.d.: not definitively established in the search results.
The RNF8-RNF168 ubiquitin ligase cascade plays a central role in DSB signaling. RNF8 is recruited to DSBs by phosphorylated MDC1 and initiates histone ubiquitination. RNF168 then amplifies this signal by depositing non-canonical K27-linked ubiquitin chains and catalyzing monoubiquitylation of H2A at K13 and K15, creating a binding site for the key repair factor 53BP1 [31] [25]. Another critical E3 ligase, BRCA1-BARD1, promotes homologous recombination by ubiquitinating H2A at K127/129, which is recognized by the ubiquitin reader SMARCAD1 to initiate chromatin remodeling [25].
Readers of Ubiquitinated Histones
The ubiquitin marks deposited on histones are interpreted by specialized "reader" proteins that contain ubiquitin-binding domains. These readers transduce the ubiquitin signal into specific downstream biological outcomes, such as the recruitment of repair machinery.
Table 2: Key Readers of Ubiquitinated Histones in DNA Repair
| Reader Protein | Histone Ubiquitin Mark Recognized | Functional Outcome | Impact on Repair Pathway |
|---|---|---|---|
| 53BP1 | H2AK15ub | Promotes NHEJ; Blocks HR | NHEJ promotion [24] [25] |
| SMARCAD1 | H2AK127/129ub | Initiates chromatin remodeling for resection | HR promotion [25] |
| BRPF1 | H2AK119ub | n.d. | n.d. [30] |
| ZMYM2 | H2AK119ub | n.d. | n.d. [30] |
The 53BP1 reader exemplifies the precision of this recognition system. It binds to H2AK15ub in a bivalent manner, simultaneously recognizing both H2AK15ub and H4K20me2 marks. This dual recognition ensures specific recruitment to DSB sites, where 53BP1 promotes non-homologous end joining by protecting DNA ends from resection [24] [25].
Figure 1: The RNF8-RNF168 Ubiquitin Signaling Cascade in DSB Repair. This pathway initiates with double-strand break detection and culminates in 53BP1 recruitment to promote non-homologous end joining (NHEJ).
Pathway-Specific Regulation by Ubiquitination
The Balance Between NHEJ and HR
The choice between the two major DSB repair pathways—non-homologous end joining (NHEJ) and homologous recombination (HR)—is critically regulated by histone ubiquitination and its crosstalk with other modifications. The RNF8-RNF168 axis establishes a chromatin platform marked by H2AK15ub that promotes the recruitment of 53BP1, a key NHEJ factor [24] [25]. Conversely, when HR is the preferred pathway, the TIP60/NuA4 acetyltransferase complex acetylates H2AK15, directly blocking its ubiquitination and thereby impairing 53BP1 binding [25]. TIP60 also acetylates H4K16, which physically inhibits 53BP1 binding to H4K20me2, further promoting HR [25]. Additionally, the removal or absence of methylation at H4K20 (H4K20me0) creates a binding site for the BRCA1-BARD1 complex, which ubiquitinates H2A at K127/129 to recruit SMARCAD1 and initiate the chromatin remodeling necessary for end resection [25].
Figure 2: Histone Modification Crosstalk Regulates Repair Pathway Choice. The competition between ubiquitination and acetylation at H2AK15 determines whether 53BP1 or BRCA1-BARD1 is recruited, guiding the choice between NHEJ and HR.
Ubiquitination in Replication Stress and Other Repair Pathways
Beyond DSB repair, chromatin ubiquitination plays crucial roles in managing replication stress. The MRN complex, traditionally associated with DSB sensing, is recruited to stalled replication forks in an ubiquitin-dependent manner. Recent research has shown that RNF168 and its histone targets H2AK13ub and H2AK15ub are required for proper replication fork progression and prevention of reversed fork accumulation, particularly at repetitive genomic sequences [31]. This suggests that DSB signaling factors are co-opted for replication fork stability, with ubiquitin marks serving as central regulators.
In nucleotide excision repair (NER), H2B ubiquitination (H2Bub1) has been implicated in the repair of platinum-based chemotherapeutic lesions. Following platinum-induced DNA damage, global H2Bub1 levels decrease, but H2Bub1 becomes specifically enriched downstream of transcription start sites of genes involved in NER, ERK/MAPK signaling, and immune response [29]. This gene-specific enrichment correlates with increased expression of these cancer-related genes, suggesting H2Bub1 helps regulate the transcriptional response to therapeutic DNA damage.
Chromatin Ubiquitination in Cancer and Therapy
Dysregulation of histone ubiquitination contributes significantly to tumorigenesis and cancer progression. Abnormal levels of histone ubiquitination modifiers disrupt gene expression patterns and DNA repair fidelity, leading to genomic instability [27] [32]. For instance, the H2AK119ub-specific E3 ligase Ring1B is a Polycomb group protein frequently mutated in human cancers, while the corresponding DUB BAP1 is a recognized tumor suppressor [30]. The proper balance of these opposing activities is essential for maintaining epigenetic programs that suppress malignant transformation.
The response to cancer therapeutics is also heavily influenced by chromatin ubiquitination. Platinum-based chemotherapeutics like cisplatin induce DNA damage that triggers ubiquitin-mediated chromatin remodeling [29]. This remodeling is associated with the expression of key cancer genes and pathways, including p53 target genes, DNA repair genes like XPC and POLH, and genes linked to platinum resistance. Understanding these mechanisms provides opportunities for therapeutic intervention, such as targeting the ubiquitin ligases or readers that control repair pathway choice in cancer cells.
Experimental Approaches and Research Tools
Key Methodologies for Studying Chromatin Ubiquitination
Investigating the role of ubiquitination in the DDR requires a combination of biochemical, cellular, and genomic approaches. Key methodologies include:
Chromatin Immunoprecipitation (ChIP) Sequencing: Used to map the localization of ubiquitinated histones and repair factors genome-wide. For example, this approach revealed H2Bub1 enrichment downstream of transcription start sites of specific cancer-related genes after platinum treatment [29].
Co-immunoprecipitation and Western Blotting: Essential for identifying protein-protein interactions and monitoring protein modifications. These techniques demonstrated the interaction between βTrCP and MRN complex proteins and the GSK3 kinase dependence of this association [26].
In vitro Ubiquitination Assays: Employ purified E1, E2, and E3 enzymes with histone substrates to reconstitute ubiquitination events biochemically. This approach confirmed SCF(βTrCP) as a novel ubiquitin ligase for MRN complex proteins [26].
Site-Directed Mutagenesis: Used to identify critical residues for ubiquitination and protein interactions. Mutagenesis of the putative degron motif in MRE11 (MRE11Δβ) abrogated its interaction with βTrCP, localizing the binding site to amino acids 596-603 [26].
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Research Reagents for Studying Chromatin Ubiquitination
| Reagent/Category | Specific Examples | Function/Application | Experimental Context |
|---|---|---|---|
| Ubiquitin Ligase Inhibitors | Small molecule inhibitors of RNF168, Ring2 | Probe function of specific E3 ligases; Potential therapeutic agents | Study of DSB signaling pathway choice [27] |
| Deubiquitinase Inhibitors | BAP1 inhibitors, USP22 inhibitors | Stabilize ubiquitin marks; Enhance DNA damage sensitivity | Cancer therapy combination approaches [27] [30] |
| Kinase Inhibitors | PF4708671 (p70S6K inhibitor), Lithium Chloride (GSK3 inhibitor) | Disrupt kinase-dependent ubiquitin ligase interactions | MRN complex regulation studies [26] |
| Site-Directed Mutants | MRE11Δβ (degron mutant), H2A K13/15R mutants | Disrupt specific protein interactions or ubiquitination sites | Mechanism of reader recruitment and repair pathway choice [31] [26] |
| Antibodies for Detection | Anti-H2AK15ub, Anti-H2Bub1, Anti-53BP1 | Detect specific ubiquitin marks and recruited factors in IF, ChIP, WB | Monitoring DDR activation and repair progression [29] [25] |
Concluding Perspectives
Chromatin ubiquitination represents a sophisticated signaling system that orchestrates the cellular response to DNA damage by creating platforms for the recruitment of specific repair factors. The precise placement and interpretation of ubiquitin marks on histones guides critical decisions in DNA repair, including pathway choice between NHEJ and HR. In cancer biology, the dysregulation of these processes contributes to tumorigenesis and influences therapeutic responses. Future research will likely focus on developing more specific modulators of ubiquitin writers, erasers, and readers as potential cancer therapeutics, particularly in combination with existing DNA-damaging agents. The integration of chromatin ubiquitination signaling with other epigenetic networks and with the broader context of nuclear organization represents an exciting frontier for understanding genome maintenance in health and disease.
From Mechanism to Medicine: Therapeutic Targeting of the Ubiquitin System in Cancer
The ubiquitin-proteasome pathway (UPP) represents the major pathway for intracellular protein degradation in eukaryotic cells, regulating critical processes including cell cycle progression, apoptosis, transcription, and DNA repair [33]. More than 80% of cellular proteins are degraded through this highly specific system, wherein proteins are tagged with polyubiquitin chains for recognition and breakdown by the 26S proteasome [33]. The 26S proteasome consists of a core 20S catalytic particle capped by two 19S regulatory particles that recognize ubiquitinated substrates [33]. Malignant cells exhibit heightened dependence on proteasome function to maintain protein homeostasis and eliminate misfolded proteins, creating a therapeutic vulnerability that can be exploited pharmacologically [33]. Proteasome inhibitors have emerged as powerful therapeutic agents that disrupt this critical cellular pathway, inducing apoptosis preferentially in cancer cells.
Bortezomib, a first-in-class dipeptidyl boronic acid proteasome inhibitor, has revolutionized the treatment landscape for hematologic malignancies, particularly multiple myeloma and mantle cell lymphoma [34]. This whitepaper examines the clinical success of bortezomib and next-generation proteasome inhibitors within the broader context of ubiquitination in DNA damage response and cancer research, providing researchers and drug development professionals with a comprehensive technical resource on the mechanisms, applications, and experimental methodologies underlying this critical drug class.
Mechanistic Foundations of Proteasome Inhibition
Molecular Pharmacology of Proteasome Inhibitors
Bortezomib exerts its antineoplastic activity through reversible, high-affinity inhibition of the chymotrypsin-like (CT-L) activity of the 26S proteasome's β5 subunit [34]. This inhibition disrupts the regulated degradation of intracellular proteins, leading to accumulation of polyubiquitinated proteins and induction of endoplasmic reticulum stress [34] [35]. The primary mechanisms through which bortezomib exerts cytotoxic effects include:
- Inhibition of NF-κB signaling: By preventing degradation of IκB, bortezomib inhibits nuclear translocation of the transcription factor NF-κB, downregulating expression of anti-apoptotic and proliferative genes [33]
- Cell cycle arrest: Stabilization of cyclin-dependent kinase inhibitors (e.g., p21, p27) and tumor suppressors (e.g., p53) induces G1/S and G2/M phase arrest [34] [33]
- Activation of apoptotic pathways: Accumulation of pro-apoptotic proteins (NOXA, BIM), caspase activation, and JNK pathway stimulation promote mitochondrial-mediated apoptosis [34] [35]
- Disruption of protein homeostasis: Accumulation of misfolded proteins triggers the unfolded protein response and endoplasmic reticulum stress [35]
Ubiquitination in DNA Damage Response and Cancer
The ubiquitin-proteasome system plays an integral role in the DNA damage response (DDR), particularly in double-strand break (DSB) repair pathway choice between non-homologous end joining (NHEJ) and homologous recombination (HR) [24]. Key E3 ubiquitin ligases, including RNF8 and RNF168, establish a ubiquitin-dependent signaling cascade at DNA damage sites that recruits repair proteins such as 53BP1 (promoting NHEJ) and BRCA1 (promoting HR) [24]. Proteasome inhibition disrupts this delicate regulatory network, potentially sensitizing cancer cells to DNA-damaging agents and contributing to genomic instability.
The intersection between ubiquitination, DDR, and cancer metabolism represents an emerging research frontier. E3 ubiquitin ligases such as NEDD4, APC/CCDH1, FBXW7, and Pellino1 regulate enzymes in key metabolic pathways including glycolysis, the TCA cycle, and fatty acid metabolism, while simultaneously modulating DDR components [36]. This dual regulatory capacity positions the ubiquitin-proteasome system as a critical link between metabolic reprogramming and genomic integrity maintenance in cancer cells.
Clinical Applications and Efficacy Data
Regulatory Approvals and Indications
Bortezomib has received extensive regulatory approvals for hematologic malignancies, demonstrating its transformative clinical impact [34]. The table below summarizes key regulatory milestones:
Table 1: Bortezomib Regulatory Approval Timeline
| Year | Regulatory Agency | Indication |
|---|---|---|
| 2003 | FDA | Accelerated approval for relapsed/refractory multiple myeloma (MM) after ≥2 prior therapies |
| 2005 | FDA | Regular approval for MM progressing after ≥1 prior therapy |
| 2006 | FDA | Relapsed/refractory mantle cell lymphoma (MCL) |
| 2008 | FDA | Previously untreated MM |
| 2014 | FDA | Retreatment of MM patients with previous response to bortezomib who relapsed ≥6 months after completion |
| 2014 | FDA & EMA | Previously untreated MCL |
Beyond its approved indications, bortezomib demonstrates clinical efficacy in several off-label hematologic malignancies, including light chain (AL) amyloidosis, lymphoplasmacytic lymphoma/Waldenström macroglobulinemia, and peripheral T-cell lymphomas [34]. The drug's clinical utility has been further expanded by the availability of generic formulations since 2015, potentially improving accessibility in lower-income countries [34].
Efficacy Across Hematologic Malignancies
Clinical trial data has established bortezomib as a cornerstone therapy in multiple myeloma, both as monotherapy and in combination regimens:
- Newly diagnosed MM: Bortezomib combination regimens induce higher response rates compared to non-bortezomib-containing regimens, with complete response rates of 30-35% in frontline therapy [34]
- Relapsed/refractory MM: Bortezomib demonstrates significant activity with improved time to progression and overall survival versus dexamethasone alone [34]
- Mantle cell lymphoma: Bortezomib achieves objective response rates of 31-47% in relapsed/refractory disease, leading to its regulatory approval [34]
Recent advances have focused on optimizing bortezomib administration, with subcutaneous delivery demonstrating non-inferior efficacy to intravenous administration while reducing peripheral neuropathy incidence [34]. Similarly, once-weekly dosing maintains efficacy while improving safety profiles compared to twice-weekly regimens [34].
Next-Generation Proteasome Inhibitors
Second-generation proteasome inhibitors have been developed to address limitations of bortezomib, particularly resistance and toxicity profiles:
Table 2: Comparison of Proteasome Inhibitors in Clinical Use
| Agent | Mechanism | Key Indications | Administration | Distinguishing Features |
|---|---|---|---|---|
| Bortezomib | Reversible boronic acid inhibitor | MM, MCL | IV, SC | First-in-class; peripheral neuropathy risk |
| Carfilzomib | Irreversible epoxide ketone inhibitor | RRMM | IV | Reduced peripheral neuropathy; irreversible binding |
| Ixazomib | Reversible boronate inhibitor | RRMM | Oral | First oral PI; convenient administration |
Carfilzomib's irreversible binding mechanism and reduced neurotoxicity have established its role in bortezomib-resistant disease, while ixazomib offers the convenience of oral administration [37]. These agents represent the ongoing evolution of proteasome-targeted therapy in hematologic malignancies.
Resistance Mechanisms and Overcoming Treatment Limitations
Molecular Mechanisms of Resistance
Despite initial efficacy, both primary and acquired resistance to bortezomib represent significant clinical challenges. Multiple molecular mechanisms contribute to proteasome inhibitor resistance:
- Proteasomal subunit mutations: Point mutations in the PSMB5 gene encoding the β5 proteasome subunit reduce bortezomib binding affinity [34]
- Proteasome overexpression: Upregulation of proteasomal subunits and increased proteasome activity in resistant cell lines [34]
- Activation of alternative protein clearance pathways: Induction of autophagy and aggresome formation as compensatory degradation mechanisms [38]
- Altered expression of regulatory proteins: Loss of chromosomal region 8p21 and subsequent overexpression of C-MAF and MAF-B transcription factors associated with poor bortezomib response [34]
- Bone marrow microenvironment protection: Stromal cell interactions confer survival advantages to malignant cells [34]
In acute myeloid leukemia (AML), resistance mechanisms differ significantly from multiple myeloma, with AML cells activating backup stress-response systems including HSF1-regulated pathways and autophagy to maintain protein homeostasis despite proteasome inhibition [38].
Novel Combination Strategies
Rational combination approaches present promising strategies to overcome resistance and expand the therapeutic utility of proteasome inhibitors:
- Dual proteasome and autophagy inhibition: Combining bortezomib with Lys05 (autophagy inhibitor) demonstrates synergistic anti-leukemic activity in AML models [38]
- Immunotherapy combinations: Bortezomib combined with daratumumab (anti-CD38 monoclonal antibody) shows enhanced efficacy in multiple myeloma [39]
- Bispecific antibody combinations: Ongoing clinical trials investigate proteasome inhibitors with T-cell engaging bispecific antibodies to enhance antitumor immunity [40]
These combination approaches leverage mechanistic insights into resistance pathways to develop more effective treatment regimens, particularly in malignancies with intrinsic proteasome inhibitor resistance.
Ubiquitin-Proteasome System in DNA Damage Response: Research Applications
Experimental Models and Methodologies
Research into the intersection of proteasome inhibition and DNA damage response employs specialized experimental approaches:
Table 3: Research Reagent Solutions for UPS and DDR Studies
| Research Tool | Application | Experimental Utility |
|---|---|---|
| Bortezomib-resistant cell lines | Resistance mechanism studies | Models with PSMB5 mutations or proteasome overexpression for investigating resistance pathways |
| RNF8/RNF168 siRNA | Ubiquitin signaling dissection | Elucidates E3 ligase-specific roles in DSB repair pathway choice |
| HSF1 inhibitors | Stress response pathway analysis | Targets compensatory mechanisms in proteasome-inhibited cells |
| Autophagy inhibitors (Lys05) | Combination therapy modeling | Blocks alternative protein degradation during proteasome inhibition |
| SENP inhibitors | SUMOylation pathway studies | Investigates crosstalk between ubiquitin and SUMO modifications in DDR |
| γH2AX staining | DNA damage quantification | Measures DSB formation and repair kinetics following proteasome inhibition |
These research tools enable detailed mechanistic studies of how proteasome inhibition impacts DNA damage signaling and repair, providing insights for rational combination therapy development.
DNA Damage Signaling Pathway Visualization
The following diagram illustrates key ubiquitin-mediated signaling events in DNA double-strand break repair and their perturbation by proteasome inhibitors:
Diagram 1: Ubiquitin signaling in DNA damage response
This ubiquitin-directed signaling network highlights critical regulatory nodes where proteasome inhibition alters DNA repair pathway choice, potentially contributing to genomic instability and cancer cell death.
Future Directions and Therapeutic Prospects
The future clinical development of proteasome inhibitors focuses on several key areas:
- Novel combination regimens: Rational drug combinations based on mechanistic insights into resistance pathways and synthetic lethal interactions [38] [40]
- Expansion to solid tumors: Overcoming intrinsic resistance mechanisms in non-hematologic malignancies [33]
- Earlier treatment lines: Moving proteasome inhibitors into frontline therapy based on improved safety profiles and combination regimens [34] [40]
- Biomarker-driven patient selection: Developing predictive biomarkers for treatment response to optimize therapeutic outcomes [34]
- Next-generation inhibitor development: Designing agents with improved specificity, reduced toxicity, and activity against resistant disease [33] [37]
The ongoing elucidation of connections between ubiquitin-proteasome system function, DNA damage response, and cellular metabolism continues to reveal new therapeutic opportunities. As research uncovers additional complexity in ubiquitin signaling networks, particularly in the context of chromatin dynamics and epigenetic regulation, novel targets for combination therapy with proteasome inhibitors will likely emerge.
Proteasome inhibitors represent a paradigm for successful targeting of protein homeostasis in cancer therapy. Their clinical development illustrates the translation of basic science insights regarding ubiquitin-mediated protein degradation into transformative cancer therapeutics, providing a roadmap for future drug development targeting the diverse cellular functions of the ubiquitin-proteasome system.
Targeted protein degradation (TPD) represents a paradigm shift in cancer drug discovery, moving beyond traditional inhibition to the catalytic elimination of disease-causing proteins. This approach has unlocked therapeutic possibilities for previously "undruggable" targets, including transcription factors, mutant oncoproteins, and scaffolding proteins that lack conventional binding pockets and constitute an estimated 85-90% of the human proteome. [41] By harnessing the cell's innate protein destruction machinery, particularly the ubiquitin-proteasome system (UPS), TPD technologies offer unprecedented opportunities for precision oncology. Among TPD strategies, proteolysis-targeting chimeras (PROTACs) and molecular glues have emerged as leading platforms, demonstrating remarkable clinical potential in treating resistant cancers and overcoming limitations of conventional therapeutics. Their application within the context of ubiquitination in DNA damage response provides a sophisticated framework for developing novel cancer therapies that target fundamental cancer survival pathways.
The ubiquitin-proteasome system serves as the primary proteolytic pathway for regulated protein degradation in eukaryotic cells, tightly governing critical cellular processes including DNA repair, stress response, and cell proliferation. [42] Essential components include ubiquitin-activating enzymes (E1), ubiquitin-conjugating enzymes (E2), ubiquitin ligases (E3), deubiquitinating enzymes (DUBs), and the 26S proteasome. The process involves a multi-step enzymatic cascade wherein E3 ligases provide critical substrate specificity, determining which proteins are tagged for destruction. [43] [42] With over 600 E3 ligases encoded in the human genome, this system offers remarkable specificity that can be co-opted for therapeutic purposes, particularly in cancer therapy where precise target engagement is paramount for efficacy and safety.
Molecular Mechanisms and Comparative Advantages
PROTACs: Heterobifunctional Degraders
PROTACs are heterobifunctional molecules comprising three core components: a ligand that binds the protein of interest (POI), a ligand that recruits an E3 ubiquitin ligase, and a linker that bridges these two domains. [41] [42] The mechanism of action involves the formation of a POI-PROTAC-E3 ternary complex that spatially positions the POI within ubiquitinating range of the E3 ligase. This proximity enables transfer of ubiquitin chains to lysine residues on the target protein, marking it for recognition and degradation by the 26S proteasome. Following degradation, the PROTAC molecule dissociates and can participate in further catalytic cycles, enabling sustained target suppression with sub-stoichiometric dosing. [42]
Table 1: Key E3 Ligases Utilized in PROTAC Design for Cancer Therapy
| E3 Ligase | Key Ligands | Cancer Applications | Clinical Status |
|---|---|---|---|
| Cereblon (CRBN) | Thalidomide, Lenalidomide, Pomalidomide | Multiple myeloma, Hematologic malignancies | Multiple clinical trials (ARV-110, ARV-471) |
| Von Hippel-Lindau (VHL) | VHL ligands | Solid tumors, Renal cell carcinoma | Clinical trials |
| MDM2 | Nutlin-3, RG7112 | Cancers with wild-type p53 | Preclinical and clinical development |
| IAP (Inhibitor of Apoptosis Protein) | Bestatin derivatives | Various cancers | Preclinical development |
The degradation efficiency and selectivity of PROTACs are influenced by several interdependent factors. While high-affinity binding of both warheads is important, the stability and cooperativity of the ternary complex are often more critical determinants of success. [41] Linker properties—including length, flexibility, polarity, and spatial orientation—directly affect the protein-protein interface and determine whether the ternary complex adopts a ubiquitination-competent conformation. [41] This sophisticated mechanism allows PROTACs to target proteins traditionally considered undruggable, including transcription factors like MYC and STAT3, mutant oncoproteins such as KRAS G12C, and scaffolding proteins lacking conventional binding pockets. [41]
Molecular Glues: Monovalent Inducers of Protein-Protein Interactions
Molecular glues are typically small, monovalent molecules (<500 Da) that induce or enhance protein-protein interactions (PPIs) by reshaping the surface of an E3 ligase or target protein to create novel binding interfaces. [44] [45] Unlike PROTACs, they do not contain separate warheads connected by a linker but function by inserting themselves into protein interfaces to stabilize naturally weak or induced interactions. The term "molecular glue" was initially coined to describe the mechanism of immunosuppressants like cyclosporin A and FK506, but has since been expanded to include degraders such as thalidomide and its analogs (lenalidomide, pomalidomide) that redirect E3 ligase activity. [44]
Molecular glues demonstrate several pharmacological advantages over PROTACs, including lower molecular weight, improved cell permeability, and more favorable drug-like properties that often align better with established principles of oral bioavailability. [45] [46] They function through a catalytic, sub-stoichiometric mechanism similar to PROTACs, enabling efficient and sustained target degradation at low concentrations. [45] A key parameter describing molecular glue activity is cooperativity, which quantifies how effectively the compound enhances the affinity between the E3 ligase and the target protein. [44]
Table 2: Classification of Molecular Glues by Mechanism of Action
| Type | Mechanism | Examples | Functional Outcome |
|---|---|---|---|
| Type I (Non-native) | Induce novel PPIs that block native protein function | Rapamycin, Cyclosporin A, FK506 | Inhibition without degradation |
| Type II (Native) | Stabilize or redirect endogenous PPIs to induce degradation | Lenalidomide, Pomalidomide, Auxin | Target protein degradation |
| Allosteric Regulators | Bind one protein to induce conformational changes enabling new PPIs | CC-885, CR8 | Enhanced degradation specificity |
| Direct Bridgers | Physically link two proteins at their interface | Rapamycin (FKBP12-mTOR) | Inhibition of protein function |
Comparative Advantages Over Conventional Therapies
Targeted protein degraders offer several fundamental advantages compared to traditional occupancy-based inhibitors. First, as catalytic entities, they operate through transient binding rather than continuous target occupancy, enabling a single degrader molecule to eliminate multiple copies of the target protein. This sub-stoichiometric mechanism provides greater efficiency at lower doses and potentially reduces toxicity profiles. [44] [41] Second, while protein inhibitors typically block only specific functional domains (e.g., active sites), degraders ablate all functions of the target protein, including scaffolding and protein-interaction roles that are often critical in oncogenic signaling. [44] This comprehensive elimination provides higher sensitivity against drug-resistant targets and better addresses non-enzymatic protein functions that drive cancer progression. [44]
Third, PROTACs and molecular glues can effectively target proteins that have been considered undruggable due to lack of deep binding pockets or extensive flat surfaces. By requiring only a binding event rather than functional inhibition, degraders can utilize shallow binding sites that would be inadequate for conventional inhibitors. [41] [47] This significantly expands the druggable proteome, particularly for challenging target classes like transcription factors that drive numerous cancer pathways but have historically evaded therapeutic targeting.
Application in DNA Damage Response and Cancer Therapy
Integrating TPD with Ubiquitination in DNA Damage Response
The ubiquitin-proteasome system plays an integral role in the DNA damage response (DDR), controlling the stability, localization, and activity of numerous DNA repair proteins. E3 ubiquitin ligases function as critical regulatory nodes in the DDR network, orchestrating the appropriate cellular response to genotoxic stress—a vulnerability that cancer therapies can exploit. PROTACs and molecular glues provide sophisticated tools to intentionally manipulate this system for therapeutic benefit, particularly in cancers with deficient DNA repair pathways.
MDM2 exemplifies the connection between ubiquitination, DDR, and cancer therapy. As both an E3 ligase and a key negative regulator of p53—the "guardian of the genome"—MDM2 represents a compelling target for TPD approaches. PROTACs have been developed both to harness MDM2's E3 ligase activity for degrading other oncoproteins and to directly target MDM2 itself for degradation, thereby stabilizing and activating p53 in cancers with wild-type p53 status. [43] This dual functionality positions MDM2 at the forefront of PROTAC innovation and demonstrates how TPD can interface with established DDR pathways to achieve therapeutic outcomes.
The following diagram illustrates the core mechanism of PROTACs in targeting proteins involved in DNA damage response pathways:
Key Targets in Cancer Therapy
PROTACs and molecular glues have demonstrated significant efficacy against diverse cancer targets, with particular success in oncology where conventional approaches have repeatedly failed. Androgen receptor (AR) variants that drive resistance to standard antagonists in prostate cancer remain susceptible to degradation-based strategies, as demonstrated by the clinical advancement of ARV-110. [41] Similarly, estrogen receptor (ER) degradation via ARV-471 has shown promise in treating hormone-resistant breast cancer. [47] These successes highlight the ability of TPD to overcome resistance mechanisms that limit conventional targeted therapies.
Transcription factors such as STAT3—long considered among the most challenging cancer targets—are now tractable through systematic degradation. [41] Additional promising targets include BRD4, a bromodomain protein that regulates oncogene expression; BCL-xL, an anti-apoptotic protein; and various protein kinases that drive proliferative signaling in cancer cells. [41] [42] The expanding repertoire of targetable proteins demonstrates the versatility of TPD approaches across cancer types and molecular subtypes.
Table 3: Promising Cancer Targets for TPD Approaches
| Target Protein | Cancer Type | E3 Ligase Recruited | Development Stage |
|---|---|---|---|
| Androgen Receptor (AR) | Prostate Cancer | CRBN, VHL | Phase III (ARV-110) |
| Estrogen Receptor (ER) | Breast Cancer | CRBN | Phase III (ARV-471) |
| BTK | Hematologic Malignancies | CRBN | Clinical Trials |
| STAT3 | Various Cancers | CRBN | Preclinical/Clinical |
| BRD4 | Hematologic Malignancies | CRBN, VHL | Preclinical/Clinical |
| BCL-xL | Various Cancers | VHL | Preclinical |
| KRAS Mutants | Pancreatic, Lung Cancer | CRBN | Preclinical |
Clinical Progress and Validation
The clinical translation of PROTAC technology has accelerated remarkably, with the first molecules entering human trials in 2019 and already progressing to Phase III completion by 2024. [41] Bavdegalutamide (ARV-110), an AR degrader, has demonstrated tolerability and antitumor activity in patients with metastatic castration-resistant prostate cancer who had progressed on standard therapies. [47] Similarly, vepdegestrant (ARV-471), an oral ER degrader, has shown promising results in ER-positive/HER2-negative breast cancer and has advanced to phase 3 clinical trials. [47]
These clinical advancements validate TPD as a viable therapeutic modality and highlight its potential to address significant unmet needs in oncology. The successful translation of PROTACs from academic concept to clinical reality in under two decades represents one of the fastest paradigm shifts in modern drug development, underscoring the profound potential of this approach to transform cancer treatment.
Experimental Design and Methodologies
PROTAC Design and Optimization
The rational design of PROTACs begins with selection of appropriate warheads for the target protein and E3 ligase. For proteins with established inhibitors (e.g., kinases), these compounds can be adapted as PROTAC warheads. Similarly, known ligands for E3 ligases such as CRBN (e.g., lenalidomide derivatives) or VHL (e.g., VH298) serve as starting points for the E3-recruiting moiety. [41] [42] The linker connecting these domains is systematically optimized for length, composition, and flexibility to enable productive ternary complex formation. Common linker chemistries include polyethylene glycol (PEG) chains, alkyl chains, and heteroaromatic groups, typically ranging from 5-15 atoms in length. [42]
The following workflow outlines the key stages in PROTAC development and validation:
Critical to PROTAC optimization is the evaluation of ternary complex formation through techniques such as surface plasmon resonance (SPR), isothermal titration calorimetry (ITC), and X-ray crystallography. These biophysical approaches provide insights into the cooperativity factor—a key parameter defining how effectively the PROTAC enhances the interaction between the POI and E3 ligase. [44] High positive cooperativity indicates that the PROTAC induces a favorable interaction between the two proteins, often correlating with efficient degradation.
Molecular Glue Discovery Approaches
Unlike the rational design approach often employed for PROTACs, molecular glues have traditionally been discovered serendipitously through phenotypic screening or retrospective characterization of compounds with unusual biological activities. [44] [45] However, systematic approaches are emerging, including:
- Correlation screening: Identifying compounds that cause degradation patterns correlating with specific E3 ligase expression.
- Ternary complex screening: Directly assessing compounds that enhance PPIs between E3 ligases and potential substrates.
- Structural-based design: Leveraging atomic-level understanding of E3 ligase binding interfaces to design glues.
For example, the compound CR8 was identified as a molecular glue through correlation analysis that linked its degradation profile to CDK12-cyclin K complex formation and recruitment of the DDB1-CUL4-RBX1 E3 ligase. [46] This highlights the potential of systematic approaches to uncover molecular glue activity from compound libraries.
The Scientist's Toolkit: Essential Research Reagents
Table 4: Key Research Reagents for TPD Investigations
| Reagent/Category | Function/Application | Examples/Specifics |
|---|---|---|
| E3 Ligase Ligands | Recruit specific E3 ligases in PROTAC design | CRBN: Lenalidomide derivatives; VHL: VH298 derivatives; MDM2: Nutlin-3 |
| Target Protein Warheads | Bind protein of interest | Kinase inhibitors; BET inhibitors; AR/AR antagonists |
| Linker Libraries | Connect warheads and E3 ligands | PEG chains, alkyl chains, alkynes (5-15 atom lengths) |
| Ubiquitination Assays | Detect target ubiquitination | Ubiquitin remnant immunoassays, TUBE probes |
| Proteasome Inhibitors | Confirm proteasome-dependent degradation | Bortezomib, MG132, Carfilzomib |
| Ternary Complex Assays | Measure cooperativity and binding | SPR, ITC, FP, AlphaScreen |
| Degradation Readouts | Quantify protein loss | Western blot, immunofluorescence, CETSA, targeted proteomics |
Current Challenges and Future Perspectives
Addressing Technical and Clinical Hurdles
Despite remarkable progress, TPD faces several significant challenges. The "hook effect"—whereby high PROTAC concentrations paradoxically reduce degradation efficiency by forming non-productive binary complexes—complicates dose optimization and requires careful pharmacokinetic/pharmacodynamic (PK/PD) modeling. [41] [48] Molecular weight and polarity constraints can limit oral bioavailability and tissue distribution, though molecular glues generally exhibit more favorable drug-like properties. [45] [46]
E3 ligase dependency presents another challenge, as tumor-specific expression patterns may limit activity in certain contexts, and resistance can emerge through E3 ligase downregulation or mutation. [43] This has motivated expansion of the E3 ligase toolbox beyond the widely utilized CRBN and VHL to include alternatives such as MDM2, DCAF15, and IAPs. [43] Off-target effects remain a concern, particularly as PROTAC warheads may engage unintended proteins, though computational approaches like graph attention neural networks are being developed to predict and mitigate these risks. [49]
Future Directions in TPD Research
The future of TPD in cancer therapy will likely encompass several innovative directions. First, expansion of the E3 ligase repertoire will enable tissue-specific targeting and reduce susceptibility to resistance mechanisms. [43] Second, dual-targeting PROTACs capable of simultaneously degrading multiple oncoproteins offer promise for addressing complex cancer networks and preventing compensatory signaling. [50] Third, advanced delivery systems such as nanoparticles, cell-penetrating peptides, and antibody-PROTAC conjugates (AbTACs) may improve tissue targeting and cellular uptake. [47] [50]
Integration of TPD with other therapeutic modalities represents another promising avenue. Combining degraders with conventional inhibitors, immunotherapies, or DNA-damaging agents may yield synergistic effects, particularly in resistant cancers. Furthermore, extension of TPD beyond oncology to neurodegenerative diseases, viral infections, and inflammatory conditions demonstrates the broad potential of this platform. [41] [45]
As the field continues to mature, TPD technologies are poised to fundamentally reshape the cancer therapeutic landscape. With their ability to target previously undruggable proteins, overcome resistance mechanisms, and achieve potent and durable responses, PROTACs and molecular glues represent a transformative approach that aligns with the future of precision oncology. Their integration with the ubiquitin system in DNA damage response creates unique opportunities for synergistic combinations and personalized treatment strategies tailored to the molecular vulnerabilities of individual cancers.
The ubiquitin-proteasome system (UPS) represents a crucial regulatory mechanism for controlling protein stability, function, and localization within eukaryotic cells [51]. This enzymatic cascade involves the sequential action of ubiquitin-activating (E1), conjugating (E2), and ligase (E3) enzymes, which collectively tag target proteins with ubiquitin molecules [51] [52]. Among these components, E3 ubiquitin ligases are particularly significant as they confer substrate specificity, recognizing hundreds of individual protein targets for ubiquitination [51]. The human genome encodes over 600 E3 ligases, which can be classified into three major families based on their structural features and catalytic mechanisms: Really Interesting New Gene (RING) finger type, Homologous to E6AP C-Terminus (HECT) type, and RING-Between-RING (RBR) type ligases [51] [52] [53].
Dysregulation of E3 ligase activity has been intimately linked to oncogenesis through multiple mechanisms, including excessive degradation of tumor suppressor proteins, stabilization of oncoproteins, and altered DNA damage response pathways [51] [53]. This technical guide examines key oncogenic E3 ligases with emphasis on the MDM2-p53 axis, explores emerging inhibitory strategies, and places these developments within the broader context of ubiquitination in DNA damage response and cancer research.
E3 Ligase Classifications and Functional Mechanisms
Structural and Mechanistic Diversity of E3 Ubiquitin Ligases
E3 ubiquitin ligases employ distinct catalytic mechanisms to transfer ubiquitin to substrate proteins. RING-type E3 ligases, the largest family comprising over 600 members, function as scaffolds that simultaneously bind E2~Ub conjugates and substrate proteins, facilitating direct ubiquitin transfer without a covalent E3-Ub intermediate [51] [52]. In contrast, HECT-type E3s form a transient thioester bond with ubiquitin before transferring it to the substrate, while RBR-type E3s utilize a hybrid mechanism that combines aspects of both RING and HECT mechanisms [51] [52].
The cullin-RING ligase (CRL) family represents an important subgroup of multi-subunit RING E3s that utilize cullin proteins as scaffolds to bring together substrate-recognition modules and RING-bound E2 enzymes [52]. CRLs are responsible for approximately 20% of all ubiquitination events in cells and employ various adaptor proteins (e.g., Skp1, Elongin B/C) and substrate receptors (e.g., F-box proteins, SOCS-box proteins) to achieve target specificity [52].
Table 1: Major E3 Ubiquitin Ligase Families and Their Characteristics
| E3 Family | Catalytic Mechanism | Representative Members | Key Structural Features |
|---|---|---|---|
| RING Finger | Direct transfer from E2 to substrate | MDM2, CRL family, TRAF6 | RING domain for E2 binding, substrate recognition domains |
| HECT Type | Transient E3-Ub thioester intermediate | NEDD4 family, HERC family, HUWE1 | C-terminal HECT domain, various N-terminal substrate-binding domains |
| RBR Type | Hybrid RING-HECT mechanism | Parkin, HOIP, ARIH1 | RING1, IBR, and RING2 domains; catalytic cysteine in RING2 |
Ubiquitin Signaling Diversity
Ubiquitination generates diverse signals through different ubiquitin chain linkages. K48-linked polyubiquitination primarily targets substrates for proteasomal degradation, while K63-linked chains typically regulate signal transduction, endocytosis, and DNA repair processes [51] [53]. Other linkage types (K6, K11, K27, K29, K33, and linear M1-linked chains) mediate specialized functions in various cellular pathways, including innate immune signaling and protein trafficking [51].
The MDM2-p53 Axis: Regulation and Therapeutic Targeting
MDM2 as the Primary Negative Regulator of p53
The MDM2-p53 interaction represents one of the most extensively characterized E3-substrate relationships in cancer biology. MDM2 (HDM2 in humans) functions as the master negative regulator of the p53 tumor suppressor by multiple mechanisms: (1) direct binding to p53's transactivation domain to block its transcriptional activity; (2) RING domain-dependent ubiquitination of p53 leading to proteasomal degradation; and (3) nuclear export of p53 [54] [55]. This regulatory relationship is balanced by a negative feedback loop wherein p53 transcriptionally activates MDM2 expression, creating an oscillatory circuit that maintains p53 at low levels under normal conditions [54] [55].
Genetic evidence firmly establishes the physiological significance of MDM2-mediated p53 regulation, as demonstrated by the embryonic lethality of Mdm2-null mice, which is completely rescued by simultaneous p53 deletion [54] [55]. MDM2's E3 ligase activity depends on its C-terminal RING domain, which facilitates E2 binding and ubiquitin transfer [55]. MDM4 (MDMX), a structural homolog of MDM2, also negatively regulates p53 but lacks intrinsic ubiquitin ligase activity; instead, it heterodimerizes with MDM2 to enhance p53 degradation [54].
Regulatory Complexity of the MDM2-p53 Pathway
Multiple mechanisms modulate the MDM2-p53 interaction in response to cellular stress. Post-translational modifications of both proteins following DNA damage disrupt their binding, enabling p53 stabilization and activation [54]. Phosphorylation of p53 at N-terminal sites (e.g., Ser15, Ser20) interferes with MDM2 binding, while MDM2 phosphorylation at Ser395 after ionizing radiation inhibits its nuclear export function [54]. Additionally, competitive binding proteins such as ARF (p14ARF in humans) activate p53 by sequestering MDM2 and inhibiting its E3 ligase function [54]. Ribosomal proteins (L11, L23, L5) can also bind MDM2 and inhibit its activity in response to nucleolar stress, providing a link between ribosome biogenesis and p53 regulation [54].
The following diagram illustrates the core regulatory circuit between MDM2 and p53 and the primary mechanisms of therapeutic intervention:
Targeting MDM2-p53: Small Molecule Inhibitors and Beyond
Conventional MDM2-targeting approaches have focused on small molecules that disrupt the MDM2-p53 interaction. Nutlin-3a represents the prototypical compound in this class, which binds MDM2's p53-interaction pocket, preventing p53 binding and leading to p53 stabilization and activation [54]. Similarly, MI-219 and related compounds have demonstrated efficacy in activating the p53 pathway in cancer cells with wild-type p53 [54]. An alternative strategy involves directly inhibiting MDM2's E3 ligase activity, as exemplified by HL198 compounds that block ubiquitin transfer to p53 [54].
Recent advances have yielded novel MDM2 inhibitors with distinct mechanisms of action. The MMRi series represents a new class of compounds that specifically target the MDM2-MDM4 E3 ligase complex rather than simply disrupting p53 binding [56]. MMRi36 functions as an MDM2-MDM4 E3 ligase activator that stabilizes the heterodimer and promotes MDM2/MDM4 degradation, while its derivative MMRi36C dissociates the RING heterodimers and inhibits E3 ligase activity [56]. These compounds induce p53-independent apoptosis in drug-resistant leukemic cells, expanding the therapeutic potential beyond tumors with wild-type p53 [56].
Table 2: Selected MDM2-Targeting Therapeutic Agents and Their Mechanisms
| Compound | Class/Type | Mechanism of Action | Development Status |
|---|---|---|---|
| Nutlin-3a | Small molecule inhibitor | Disrupts MDM2-p53 binding by occupying p53-binding pocket | Preclinical research tool |
| MI-219 | Small molecule inhibitor | Binds MDM2 with high affinity, stabilizing p53 | Preclinical development |
| HL198 | Small molecule inhibitor | Inhibits MDM2 E3 ligase activity directly | Preclinical research |
| MMRi36/MMRi36C | E3 ligase modulator | Targets MDM2-MDM4 E3 ligase activity; MMRi36C dissociates heterodimers | Research phase |
| MDM2-recruiting PROTACs | Heterobifunctional degrader | Uses MDM2 as E3 ligase to degrade oncoproteins | Early development |
E3 Ligases in DNA Damage Response and Cancer Therapeutics
Expanding the Target Spectrum Beyond MDM2
While MDM2 represents a paradigmatic example, numerous other E3 ligases play critical roles in oncogenesis and represent promising therapeutic targets. The NEDD4 family of HECT-type E3 ligases, including members such as WWP1, WWP2, ITCH, NEDD4, NEDD4L, SMURF1, and SMURF2, regulate various cancer-relevant pathways including TGFβ signaling, Akt signaling, and p53-mediated apoptosis [57]. These ligases demonstrate altered expression across multiple cancer types, with NEDD4 members showing increased expression in pancreatic, esophageal, gastric, and colon cancers, while displaying decreased expression in thyroid, kidney, and testicular cancers [57].
The TGFβ pathway exemplifies the complex regulation by E3 ligases in cancer development. Multiple E3s including SMURF1, SMURF2, and others fine-tune TGFβ signaling duration and intensity by regulating receptor and SMAD protein stability [58]. In early tumorigenesis, SMURF2-mediated degradation of TGFβ receptors supports the tumor-suppressive functions of TGFβ signaling, while in advanced cancers, altered E3 activity may contribute to the oncogenic switch in TGFβ function [58].
E3 Ligases in Colorectal Cancer: A Case Study in Pathway Regulation
Comprehensive studies in colorectal cancer (CRC) reveal the multifaceted roles of E3 ligases in regulating oncogenic pathways. Multiple E3s influence CRC proliferation by controlling cell cycle regulators: TRIM6 promotes proliferation by degrading the anti-proliferative protein TIS21, while ITCH and HERC3 suppress proliferation by targeting CDK4 and RPL23A for degradation, respectively [53]. Metastatic processes are similarly regulated by E3 activity, with FBXO11 and TRIM16 inhibiting epithelial-mesenchymal transition (EMT) by degrading the transcription factor Snail, and HERC3 suppressing metastasis through degradation of EIF5A2 [53].
Cancer stem cell (CSC) maintenance and therapy resistance in CRC are also influenced by E3 networks. FBXW11-mediated degradation of the tumor suppressor HIC1 promotes stem-like properties, while TRAF6 suppresses CSC characteristics by ubiquitinating the stemness marker ALDH1B1 [53]. MDM2 contributes to oxaliplatin resistance by enhancing p53 ubiquitination in a WDR35-dependent manner, highlighting the role of E3 adaptor proteins in therapy response [53].
Advanced Therapeutic Platforms: PROTACs and E3 Ligase Engineering
PROTAC Technology and MDM2 Recruitment
Proteolysis-Targeting Chimeras (PROTACs) represent a revolutionary approach in targeted protein degradation that leverages E3 ligases to eliminate specific protein targets [59]. These heterobifunctional molecules consist of a target protein-binding warhead connected via a linker to an E3 ligase-recruiting ligand, forming a ternary complex that facilitates target ubiquitination and degradation [59]. While early PROTAC development focused heavily on the E3 ligases CRBN and VHL, recent expansion to other E3s including MDM2 has broadened the therapeutic scope [59].
MDM2 possesses dual utility in PROTAC applications: (1) as an E3 ligase recruiter for degrading various oncoproteins (MDM2-harnessing PROTACs), and (2) as a direct degradation target itself (MDM2-targeted PROTACs) [59]. MDM2-based PROTACs have been developed against diverse targets including the androgen receptor (AR), epidermal growth factor receptor (EGFR) mutants, and cyclin-dependent kinases (CDKs) [59]. Optimization of PROTAC efficacy involves careful tuning of warhead affinity, linker length and composition, and E3 ligase selection to promote productive ternary complex formation [59].
The following diagram illustrates the PROTAC mechanism of action for targeted protein degradation:
Research Reagent Solutions for E3 Ligase Studies
Table 3: Essential Research Reagents for E3 Ligase and Ubiquitination Studies
| Reagent Category | Specific Examples | Research Applications | Key Functions |
|---|---|---|---|
| Small Molecule Inhibitors | Nutlin-3a (MDM2), Compound A (SMURF2) | Pathway inhibition studies, functional validation | Disrupt E3-substrate interactions or inhibit catalytic activity |
| PROTAC Molecules | MD-224 (MDM2-degrading), MAT-5 (MDM2-harnessing) | Targeted protein degradation studies | Induce selective degradation of target proteins via UPS |
| Expression Plasmids | Wild-type/mutant MDM2, NEDD4 family members | Overexpression, structure-function studies | Introduce E3 ligases or mutants into cellular models |
| siRNA/shRNA Libraries | MDM2 siRNA, NEDD4 family siRNA pools | Loss-of-function studies | Knock down endogenous E3 ligase expression |
| Antibodies | Phospho-specific p53, MDM2, ubiquitin remnants | Immunoblotting, immunohistochemistry | Detect protein expression, modification, and localization |
| Ubiquitination Assay Kits | In vitro ubiquitination kits, linkage-specific antibodies | Biochemical activity assays | Measure E3 ligase activity and ubiquitin chain topology |
Experimental Approaches: Methodologies for E3 Ligase Research
Protocol: Assessing MDM2 E3 Ligase Inhibition and p53-Independent Apoptosis
Based on studies of novel MDM2-MDM4 E3 ligase inhibitors [56], the following experimental protocol can be employed to evaluate candidate compounds:
Cell Culture and Treatment:
- Culture p53-null leukemic cells (e.g., THP-1, SKW-3) in appropriate medium supplemented with 10% FBS at 37°C in 5% CO₂.
- Seed cells in 6-well plates at 2.5 × 10⁵ cells/mL and allow to adhere overnight.
- Treat cells with candidate inhibitors (e.g., MMRi36, MMRi36C) at concentrations ranging from 0.1-10 µM for 6-48 hours. Include DMSO vehicle control.
Apoptosis Assessment:
- Harvest cells by gentle centrifugation (300 × g, 5 minutes).
- Wash once with cold PBS and resuspend in 1× binding buffer.
- Stain with Annexin V-FITC and propidium iodide (BD Pharmingen Kit #556547) according to manufacturer's protocol.
- Analyze by flow cytometry within 1 hour to quantify early (Annexin V+/PI-) and late (Annexin V+/PI+) apoptotic populations.
MDM2-MDM4 Complex Analysis:
- Lyse treated cells in IP lysis buffer supplemented with protease inhibitors.
- Perform immunoprecipitation using anti-MDM2 or anti-MDM4 antibodies conjugated to magnetic beads.
- Analyze complexes by Western blotting using antibodies against MDM2, MDM4, and ubiquitin.
- For heterodimer dissociation assessment, use non-reducing conditions to preserve complex integrity.
Western Blot Analysis:
- Separate proteins (20-30 µg per lane) by SDS-PAGE (10% gel) and transfer to PVDF membranes.
- Block membranes with 5% non-fat milk in TBST for 1 hour at room temperature.
- Probe with primary antibodies (MDM2, MDM4, p53, cleaved caspase-3, β-actin) overnight at 4°C.
- Incubate with HRP-conjugated secondary antibodies for 2 hours at room temperature.
- Detect using enhanced chemiluminescence and quantify band intensities.
Protocol: Evaluating E3 Ligase Expression and Network Analysis in Cancer Models
Comprehensive analysis of E3 ligase families in cancer follows established methodologies [57]:
Multi-Omics Data Integration:
- Extract RNA-seq expression data for E3 ligase families (e.g., NEDD4 members) from TCGA datasets across multiple cancer types.
- Process count data using DESeq2 in R to identify differentially expressed E3 ligases (adjusted p-value < 0.05, |log2FC| > 1).
- Analyze mutation frequency and copy number variations from genomic datasets.
- Correlate genetic alterations with clinical parameters including stage, grade, and survival outcomes.
Protein Interaction Network Mapping:
- Retrieve E3 ligase interaction partners from BioGRID database.
- Perform enrichment analysis using ClusterProfiler (R) for Gene Ontology terms and KEGG pathways.
- Construct protein-protein interaction networks using Cytoscape with emphasis on cancer-relevant pathways (p53, Akt, apoptosis, autophagy).
- Calculate Pearson Correlation Coefficients between E3 ligase expression and pathway activity scores.
Functional Validation in Cell Models:
- Culture relevant cancer cell lines (e.g., A549, H1299 for lung cancer).
- Transfect with E3 expression plasmids or siRNA oligonucleotides using appropriate transfection reagents.
- Assess pathway modulation by Western blotting for key proteins (p53, Akt, p-Akt, p62, LC3).
- Evaluate functional outcomes including apoptosis (Annexin V/PI staining), proliferation (MTT assay), and migration (transwell assay).
The strategic inhibition of oncogenic E3 ligases represents a promising frontier in cancer therapeutics that extends well beyond the established MDM2-p53 axis. Advances in understanding E3 ligase mechanisms, combined with emerging technologies like PROTACs, are expanding the druggable proteome to include previously intractable targets. The integration of E3 ligase research with DNA damage response pathways provides particular opportunity for synthetic lethal approaches in cancer therapy.
Future directions will likely focus on developing isoform-selective E3 inhibitors, optimizing tissue-specific delivery of PROTAC molecules, and identifying predictive biomarkers for E3-targeted therapies. Additionally, combining E3 ligase inhibitors with conventional DNA-damaging agents or immunotherapies may yield synergistic antitumor effects. As our understanding of ubiquitin signaling in cancer continues to evolve, so too will opportunities for therapeutic intervention through targeted modulation of E3 ligase activity.
Harnessing Deubiquitinating Enzymes (DUBs) as Novel Anti-Cancer Targets
The ubiquitin-proteasome system (UPS) represents a crucial regulatory mechanism for protein degradation and function in eukaryotic cells, with deubiquitinating enzymes (DUBs) serving as essential regulators that reverse ubiquitination by cleaving ubiquitin from substrate proteins. As a dynamic and reversible post-translational modification, ubiquitination regulates virtually all cellular processes, including cell cycle progression, DNA damage response, and programmed cell death. DUBs constitute a family of approximately 100 proteases that counteract the activity of E3 ubiquitin ligases, thereby controlling the stability, activity, and localization of numerous substrate proteins. The human DUB family encompasses several structurally distinct classes, including ubiquitin-specific proteases (USPs), ovarian tumor proteases (OTUs), ubiquitin C-terminal hydrolases (UCHs), Machado-Josephin domain-containing proteases (MJDs), JAMM/MPN domain-associated metallopeptidases (JAMMs), and motif-interacting with Ub-containing novel DUB family proteins (MINDYs) [60] [61] [62].
Dysregulation of DUB activity is increasingly recognized as a hallmark of cancer, with numerous DUBs demonstrating oncogenic or tumor-suppressive functions across various cancer types. The aberrant expression of specific DUBs contributes to tumorigenesis by stabilizing oncoproteins, destabilizing tumor suppressors, and activating key cancer-promoting signaling pathways. Consequently, DUBs have emerged as promising therapeutic targets in oncology, offering novel opportunities for intervention in cancers that remain difficult to treat with conventional therapies [61] [62] [63]. This whitepaper examines the role of DUBs in cancer biology, with particular emphasis on their functions in the DNA damage response, and explores the therapeutic potential of DUB inhibition in cancer treatment.
Molecular Mechanisms of DUBs in Cancer Pathways
Regulation of Key Oncogenic Signaling Pathways
DUBs exert profound effects on cancer development and progression through their regulation of critical signaling pathways. The Wnt/β-catenin cascade, frequently dysregulated in cancers, is modulated by several DUBs including USP28, which promotes cell cycle progression and inhibits apoptosis in pancreatic ductal adenocarcinoma (PDAC) by stabilizing the transcription factor FOXM1 [61]. Similarly, USP21 enhances PDAC growth by activating mTOR signaling and supporting amino acid sustainability through micropinocytosis [61]. The stability of oncogenic transcription factors is also controlled by DUBs; for instance, USP5 prolongs the half-life of FOXM1 to accelerate PDAC tumor growth, while USP9X regulates the Hippo pathway components LATS kinase and YAP/TAZ to impact PDAC growth [61].
Table 1: Key DUBs and Their Oncogenic Substrates in Cancer
| DUB | Cancer Type | Key Substrate(s) | Biological Effect |
|---|---|---|---|
| USP28 | Pancreatic, Colorectal | FOXM1 | Promotes cell cycle progression, inhibits apoptosis |
| USP21 | Pancreatic | TCF7, MAPK3 | Maintains cancer cell stemness, activates mTOR signaling |
| USP5 | Pancreatic | FOXM1 | Regulates DNA damage response, promotes tumor formation |
| USP9X | Pancreatic | LATS kinase, YAP/TAZ | Context-dependent tumor suppressor or oncogene |
| USP7 | Multiple | p53, MDM2, PTEN | Regulates genome stability, immune response |
| USP22 | Multiple | PTEN, DYRK1A | Cancer stem cell marker, promotes proliferation |
| USP1 | Multiple | ID proteins, FANCD2 | DNA interstrand crosslink repair, translesion synthesis |
| OTUD1 | Colorectal | IREB2 | Enhances ferroptosis susceptibility, antitumor immunity |
DUBs in the DNA Damage Response
The role of DUBs in the DNA damage response represents a critical aspect of their function in cancer biology, with particular relevance to therapeutic interventions. Ubiquitin-specific protease 1 (USP1) serves as a key regulator of DNA repair pathways, often being overexpressed in various cancers where its expression correlates with poor prognosis [64]. USP1, in complex with its binding partner UAF1 (USP1-associated factor 1), deubiquitinates monoubiquitin signals in DNA interstrand crosslink repair and translesion synthesis pathways. These activities enable cancer cells to overcome replication stress and repair DNA damage induced by chemotherapeutic agents, positioning USP1 as a attractive target for therapeutic intervention [64].
USP7 represents another crucial DUB in the DNA damage response, regulating the stability of both MDM2 and p53. Although USP7 can directly stabilize p53, it exhibits higher binding affinity for MDM2, an E3 ligase that targets p53 for proteasomal degradation. Thus, USP7 inhibition results in MDM2 degradation and subsequent p53 stabilization, activating apoptosis in cancer cells [65]. Beyond its direct effects on cancer cells, USP7 inhibition also demonstrates significant immunomodulatory properties, activating antitumor immune responses and enhancing T-cell cytotoxicity, which underscores its potential as a target for cancer immunotherapy [65].
Therapeutic Targeting of DUBs: Experimental Approaches and Protocols
DUB Inhibitor Development
The development of small molecule inhibitors targeting specific DUBs has gained considerable momentum in recent years, with several compounds showing promise in preclinical and clinical studies. Selective inhibitors have been developed for various DUBs including USP1, USP7, USP14, and USP30, demonstrating antitumor activity in diverse cancer models [62]. These inhibitors function by disrupting the deubiquitination of key oncogenic substrates, leading to their degradation and subsequent inhibition of cancer-promoting pathways.
A notable example is OAT-4828, a novel and highly potent USP7-selective inhibitor with a pharmacokinetic profile suitable for oral administration. In vivo studies using melanoma and colon cancer models have demonstrated that OAT-4828 significantly alters the tumor microenvironment, enhancing T-cell activity and decreasing levels of immunosuppressive proteins such as programmed death-ligand 1 [65]. The compound exerts its effects through MDM2 depletion and p53 restoration, while also displaying unexpected anti-angiogenic properties not observed with MDM2 inhibitors alone [65].
Table 2: Selected DUB Inhibitors in Cancer Therapeutics
| Inhibitor | Target DUB | Development Stage | Proposed Mechanism | Cancer Type |
|---|---|---|---|---|
| OAT-4828 | USP7 | Preclinical | MDM2 degradation, p53 stabilization, T-cell activation | Melanoma, Colon cancer |
| AZ-1 | USP25/USP28 | Preclinical | Suppresses NF-κB signaling | Intracellular bacterial infection models |
| USP1 inhibitors | USP1 | Preclinical | Disruption of DNA damage repair | Non-small cell lung cancer |
| WP1130 | USP9X | Preclinical | Degradation of anti-apoptotic proteins | Multiple cancers |
| 6-gingerol | USP14 | Preclinical | Suppresses autophagic flux, induces ferroptosis | Lung cancer |
Experimental Assessment of DUB Inhibition
USP7 Ub-rhodamine 110 Assay Protocol: This biochemical assay provides a robust method for evaluating USP7 inhibitory activity in a high-throughput format. The assay is conducted in half-area black 96-well plates using an assay buffer containing 50 mM HEPES (pH 7.5), 150 mM sodium chloride, 2 mM dithiothreitol (DTT), 0.05% Tween 20, 1 mg/mL bovine serum albumin (BSA), and 1% DMSO, with a final reaction volume of 45 µL. The assay components include USP7 enzyme (0.4 nM final concentration), the test compound, and Ub-Rho110Gly substrate (500 nM final concentration). Following plate centrifugation at 250 rpm for 2 minutes, the reaction is incubated at 25°C in the dark for 30 minutes, with fluorescence measured at excitation 485 nm and emission 535 nm using a plate reader [65].
Ub-CHOP2 Reporter Assay Protocol: This alternative assay for USP7 activity utilizes a reporter system where USP7 removes ubiquitin from the Ub-CHOP2 enzyme, activating it to catalyze its substrate. The assay is performed in black 96-well plates using a buffer containing 20 mM Tris (pH 8), 2 mM CaCl₂, 0.05% Tween, 2 mM DTT, and 1% DMSO, with a final reaction volume of 50 µL. The reaction mixture includes USP7 enzyme (0.75 nM final concentration), the test compound, and substrates (100 nM Ub-CHOP2-Reporter and 100 nM CHOP2-Substrate final concentrations). After centrifugation at 250 rpm for 2 minutes, plates are incubated at 25°C in the dark for 60 minutes, with fluorescence measured at excitation 485 nm and emission 531 nm [65].
In Vivo Evaluation of DUB Inhibitors: For in vivo assessment of DUB inhibitors, studies are typically conducted in immunocompetent mouse models such as BALB/c or C57BL/6 mice implanted with syngeneic tumor cells (e.g., CT26 colon carcinoma or B16F10 melanoma). Compounds are administered orally, with tumor volume measured regularly and immune cell populations analyzed by flow cytometry to evaluate effects on the tumor microenvironment [65].
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Research Reagents for DUB Studies
| Reagent/Category | Specific Examples | Function/Application |
|---|---|---|
| Biochemical Assay Kits | Ub-rhodamine 110 assay, Ub-CHOP2 assay | High-throughput screening of DUB inhibitors |
| Cell Line Models | B16F10, CT26, PANC-1, SW480 | In vitro assessment of DUB inhibitor efficacy |
| Animal Models | BALB/c, C57BL/6 mice | In vivo evaluation of antitumor activity and immune modulation |
| Recombinant DUBs | USP7, USP1, USP14 | Structural studies and biochemical characterization |
| Selective Inhibitors | OAT-4828 (USP7), AZ-1 (USP25/28) | Mechanistic studies and therapeutic validation |
Visualization of DUB Mechanisms and Experimental Approaches
USP7 Mechanism and Inhibition Pathway
DNA Damage Response and DUB Regulation
The targeting of deubiquitinating enzymes represents a promising frontier in cancer therapeutics, offering the potential to modulate key cancer-associated pathways with precision. The integral roles of DUBs in regulating DNA damage response, immune recognition, and cell death pathways position them as attractive targets for combination therapies with conventional chemotherapeutics and immunotherapies. As research in this field advances, the development of increasingly selective DUB inhibitors and their validation in clinical settings will be essential for realizing the full potential of this therapeutic approach. Furthermore, understanding the complex interplay between different DUBs and their context-dependent functions in various cancer types will be critical for designing effective treatment strategies that maximize therapeutic efficacy while minimizing potential adverse effects.
The DNA Damage Response (DDR) network represents a critical safeguard mechanism that maintains genomic integrity, with its dysfunction being a hallmark of cancer. Within this complex signaling network, ubiquitination has emerged as a crucial post-translational modification that dynamically regulates nearly every aspect of the DDR, from damage recognition to repair pathway choice [1] [16]. This intricate ubiquitin signaling system involves a cascade of E1 (activating), E2 (conjugating), and E3 (ligating) enzymes that conjugate ubiquitin to target proteins, with deubiquitinating enzymes (DUBs) providing reversibility [16]. The diversity of ubiquitin chain linkages—including K48-linked chains that target proteins for proteasomal degradation and K63-linked chains that function in DNA repair signaling—creates a sophisticated "ubiquitin code" that determines cellular outcomes following genotoxic stress [1].
The therapeutic exploitation of DDR deficiencies in cancer has gained significant momentum, exemplified by the clinical success of PARP inhibitors in BRCA-mutant cancers through synthetic lethality [66]. However, the clinical utility of PARP inhibitors is confined mainly to specific genetic contexts, highlighting the need for broader treatment strategies [66]. This limitation has driven the development of next-generation DDR inhibitors targeting diverse components of the DDR network, including ATM, ATR, WEE1, and DNA-PK inhibitors [66]. These agents offer potential therapeutic benefits across a broader range of tumor types, independent of specific genetic alterations like homologous recombination deficiencies, representing a more inclusive approach to overcoming resistance to DNA-damaging therapies [66].
This review analyzes the current landscape of emerging clinical candidates targeting the DDR, with particular emphasis on those modulating ubiquitination pathways, and examines the integrated preclinical strategies employed to advance these promising therapeutics.
Ubiquitination in DNA Damage Response: Mechanistic Foundations
The Ubiquitin Cascade in DNA Damage Signaling
Upon DNA damage induction, particularly double-strand breaks (DSBs), a rapid and extensive accumulation of ubiquitin conjugates occurs at damage sites within seconds [16]. This ubiquitin accumulation is orchestrated through sequential actions of E3 ubiquitin ligases that modify histones and DDR proteins, creating platforms for the recruitment of downstream repair factors. The RNF8-RNF168 ubiquitin ligase axis plays a particularly crucial role in establishing a ubiquitin signaling platform that recruits key regulators of repair pathway choice, including 53BP1 for non-homologous end joining (NHEJ) and BRCA1 for homologous recombination (HR) [24]. RNF8 and RNF168 promote the formation of two chromatin modifications that 53BP1 recognizes: H2AK15ub and H4K20me2 [24].
The histone ubiquitylation of H2A, H2B, and H2AX subunits represents one of the initial events promoting nucleosome destabilization at damage sites [16]. CHFR (checkpoint with Forkhead-associated and RING finger domain protein), which is recruited to DSBs by poly(ADP-ribose), regulates the first wave of histone ubiquitylation [16]. CHFR ubiquitylates PARP1 via both K48-linked and K63-linked ubiquitin chains, promoting the dissociation of PARP1 from damage sites [16]. The epigenetic inactivation of CHFR has been described in several cancer types, including breast, colorectal, gastric, and lung cancers, highlighting the clinical relevance of this ubiquitin-mediated regulation [16].
Repair Pathway Choice Through Ubiquitin Signaling
The balance between the two major DSB repair pathways—NHEJ and HR—is critically regulated by ubiquitin-mediated signaling events that integrate cell cycle context with chromatin environment [24]. When HR is preferred during S/G2 phases, the TIP60/NuA4 acetyltransferase complex acetylates H2AK15, directly blocking ubiquitination and impairing 53BP1 binding [24]. TIP60 is also responsible for acetylating the H4K16 site, which physically inhibits 53BP1 binding to H4K20me2, thereby promoting HR [24]. Conversely, the removal of H4K16ac from chromatin by deacetylases HDAC1 and HDAC2 promotes NHEJ [24]. The removal or absence of methylation at H4K20 (H4K20me0) guides pathway choice toward HR by opening the binding site for the BRCA1-BARD1 complex, the main HR player [24].
The following diagram illustrates the key regulatory steps in ubiquitin-mediated DSB repair pathway choice:
This intricate ubiquitin signaling network provides multiple nodes for therapeutic intervention, particularly through the development of small molecule inhibitors targeting specific E3 ligases or ubiquitin-binding domains. The context-dependent nature of these signaling events also offers opportunities for biomarker-driven patient selection strategies.
Clinical Trial Landscape: DNA-Damaging Agents and DDR Inhibitors
Current Clinical Combinations and Outcomes
The strategic combination of DNA-damaging agents (DDAs) with DNA damage response inhibitors (DDRis) represents a promising approach to overcome therapeutic resistance in cancer. A comprehensive analysis of 221 clinical trials investigating DDA-DDRi combinations revealed 22 distinct DDAs and 46 DDRis across various cancer types [66]. These DDAs were classified into eight subclasses based on their mechanisms of action, while DDRis were categorized into 14 distinct subclasses according to their specific targets [66]. From this extensive dataset, 89 trials with interpretable outcomes were selected for detailed analysis and assigned outcome scores based on predefined criteria reflecting clinical effectiveness, safety, and benefit across different tumor types and patient populations [66].
The clinical development of PARP inhibitors has been particularly fruitful, with multiple approvals for ovarian, breast, and prostate cancers [66]. However, the clinical utility of PARP inhibitors is confined mainly to specific genetic contexts, highlighting the need for broader treatment strategies [66]. This limitation has driven the development of next-generation DDRis targeting diverse components of the DDR network, including ATM, ATR, WEE1, and DNA-PK inhibitors [66]. These agents offer potential therapeutic benefits across a broader range of tumor types, independent of specific genetic alterations like homologous recombination deficiencies, representing a more inclusive approach to overcoming resistance to DNA-damaging therapies [66].
Table 1: Selected Promising Clinical Candidates in DNA Damage Response Pathways
| Drug Name | Target | Development Phase | Key Indications | Notable Characteristics |
|---|---|---|---|---|
| ART0380 | ATR Kinase | Phase I | Advanced solid tumors | Initially discovered and developed by MD Anderson's Therapeutics Discovery division [67] |
| Ivonescimab | PD-1/VEGF | Phase III | ROS1-positive NSCLC | Dual-acting drug; showed superior PFS vs. Keytruda in Phase III [68] |
| Amlitelimab | OX40L | Phase III | Eczema, Asthma, HS | Different mechanism than Dupixent; projected >$8B peak sales [68] |
| Fenebrutinib | BTK | Phase III | Relapsing MS | Reversible binding; potentially better safety profile [68] |
| Sonelokimab | IL-17/Albumin | Phase III | Hidradenitis Suppurativa | Binds two inflammatory cytokines + albumin; potentially better dosing [68] |
Emerging Clinical Data and Recent Approvals
The first half of 2025 witnessed significant progress in oncology drug approvals, with the FDA's Center for Drug Evaluation and Research (CDER) approving eight novel cancer drugs [69]. These recent approvals reflect ongoing innovations in targeted therapies, including antibody-drug conjugates (ADCs) for solid tumors, small molecule targeted therapies, and biomarker-guided approaches representing significant advances in precision medicine [69]. Several therapeutics addressing rare cancers also gained approval, including the first treatment for KRAS-mutated ovarian cancer and a non-surgical treatment option for patients with neurofibromatosis type 1 [69].
Promising clinical results presented at the AACR Annual Meeting 2025 highlighted emerging trends in cancer therapy. Researchers from MD Anderson Cancer Center presented data on a personalized vaccine platform called NeoAg-VAX for patients with microsatellite-stable metastatic colorectal cancer (MSS mCRC) [67]. This approach uses bioinformatics and sequencing tools to deliver up to 10 tumor-derived proteins targeted to each patient's specific combination of mutations [67]. When combined with or without pembrolizumab immunotherapy, the personalized vaccine was safe and feasible to administer, leading to strong immune responses in most vaccinated patients [67].
Another significant presentation featured a Phase II trial investigating metastasis-directed radiation therapy without systemic therapy in patients with oligometastatic clear cell renal cell carcinoma (ccRCC) [67]. The study demonstrated a median progression-free survival of 18 months, with a median of 34 months systemic therapy-free survival, without compromising overall survival [67]. The researchers also validated a novel tumor-informed circulating tumor DNA (ctDNA) assay to detect molecular residual disease (MRD), with patients who were MRD-negative at baseline showing significantly longer systemic therapy-free survival compared to MRD-positive patients (54 months vs. 27 months) [67].
Table 2: Selected FDA Novel Cancer Drug Approvals in H1 2025
| Drug Name | Active Ingredient | Approval Date | Approved Indication |
|---|---|---|---|
| Avmapki Fakzynja Co-Pack | Avutometinib and Defactinib | 5/8/2025 | KRAS-mutated recurrent low-grade serous ovarian cancer (LGSOC) after prior systemic therapy [69] |
| Emrelis | Telisotuzumab Vedotin-tllv | 5/14/2025 | Locally advanced or metastatic, non-squamous NSCLC with high c-Met protein overexpression after prior systemic therapy [69] |
| Ibtrozi | Taletrectinib | 6/11/2025 | Locally advanced or metastatic ROS1-positive non-small cell lung cancer [69] |
| Gomekli | Mirdametinib | 2/11/2025 | Neurofibromatosis type 1 patients with symptomatic plexiform neurofibromas not amenable to complete resection [69] |
| Romvimza | Vimseltinib | 2/14/2025 | Symptomatic tenosynovial giant cell tumors where surgical resection would cause worsening functional limitation or severe morbidity [69] |
Preclinical Models in DDR Drug Development
Integrated Preclinical Screening Approaches
The development of effective DDR-targeted therapies relies on robust preclinical models that can accurately predict clinical responses. Given the high attrition rates in oncology drug development (approximately 95%), maintaining an effective drug discovery pipeline requires patient-relevant, clinically predictive models within the preclinical screening process [69]. An integrated approach leveraging multiple model systems provides complementary insights that enhance decision-making and improve success rates in clinical translation.
Cell lines represent the foundational step in DDR drug discovery, serving as initial high-throughput systems to evaluate drug candidates against multiple cancer types and diverse genetic backgrounds [69]. These models enable researchers to discover predictive biomarkers for drug responses and conduct various assays, including drug efficacy testing, high-throughput cytotoxicity screening, in vitro drug combination studies, and colony-forming assays [69]. The major advantage of cell lines lies in their reproducibility, standardization, and scalability for large-scale screening efforts. However, their limitations include inadequate representation of tumor heterogeneity and failure to recapitulate the tumor microenvironment (TME) [69].
Organoid models have emerged as invaluable tools in oncology research, revolutionizing drug discovery workflows [69]. These three-dimensional models are grown from patient tumor samples and faithfully recapitulate the phenotypic and genetic features of the original tumors [69]. The regulatory landscape for organoids is evolving rapidly, with the FDA announcing in April 2025 that animal testing requirements for monoclonal antibodies and other drugs will be reduced, refined, or potentially replaced entirely with advanced approaches including organoids [69]. Organoids support high-throughput screening of therapeutic candidates, more effectively predict tumor responses to treatments than cell lines, and are more cost-effective than animal models [69]. They have been successfully used to identify new therapeutic targets, including MTAP in pancreatic cancer and SIRT1 in bladder cancer [69].
Patient-derived xenograft (PDX) models, created by implanting patient tumor tissue into immunodeficient mice, preserve key genetic and phenotypic characteristics of patient tumors and are considered the gold standard of preclinical cancer research [69]. These models maintain the architecture of the original tumor and include components of the TME, enabling more accurate prediction of clinical outcomes and improving clinical trial success rates [69]. PDX models are particularly valuable for biomarker discovery and validation, clinical stratification, exploring new indications, and developing drug combination strategies [69].
Biomarker Development in Preclinical Models
The early identification and validation of biomarkers is crucial to DDR drug development, enabling researchers to identify patients with targetable biological features, track drug activity, and identify early indicators of treatment effectiveness [69]. An integrated biomarker strategy that leverages multiple preclinical models provides a structured approach to biomarker development:
- PDX-derived cell lines enable large-scale screening to identify potential correlations between genetic mutations and drug responses, generating initial sensitivity or resistance biomarker hypotheses [69].
- Organoid testing allows refinement and validation of biomarker hypotheses using more complex 3D tumor models, with multiomics approaches (genomics, transcriptomics, proteomics) helping to identify robust biomarker signatures [69].
- PDX models provide final validation of biomarker hypotheses before clinical trials, offering insights into biomarker distribution within heterogeneous tumor environments [69].
This sequential approach to biomarker development is particularly relevant for DDR-targeted therapies, where patient selection based on DDR deficiency markers (such as BRCA mutations for PARP inhibitors) has been crucial for clinical success [66]. The integration of ubiquitination-specific biomarkers represents an emerging frontier in this field, with potential to identify patients most likely to benefit from therapies targeting the ubiquitin-proteasome system or specific E3 ligases.
Experimental Protocols for Assessing Ubiquitination in DDR
Protocol for Monitoring Ubiquitination at DNA Damage Sites
Objective: To quantify the spatial and temporal dynamics of ubiquitin conjugation at DNA double-strand break sites induced by targeted irradiation.
Methodology:
- Cell Preparation and Damage Induction:
- Seed U2OS cells expressing GFP-tagged ubiquitin on 35mm glass-bottom dishes.
- Allow cells to adhere for 24 hours under standard culture conditions.
- Induce localized DNA damage using a micro-irradiator with a 365nm laser at 30% power with 10 iterations.
Image Acquisition and Quantification:
- Capture time-lapse images every 15 seconds for 15 minutes post-irradiation using a confocal microscope with environmental control (37°C, 5% CO₂).
- Quantify ubiquitin accumulation by measuring fluorescence intensity within the irradiated region normalized to background cytoplasmic signal.
- Generate kinetic curves of ubiquitin recruitment and dispersal.
Inhibition Studies:
- Pre-treat cells with proteasome inhibitors (e.g., MG132, 10μM for 4 hours) or specific E1 inhibitors (e.g., PYR-41, 50μM for 2 hours) before irradiation.
- Compare ubiquitin dynamics in inhibitor-treated versus vehicle-control cells.
This protocol enables the functional assessment of ubiquitin signaling dynamics at DNA damage sites and can be adapted for testing the effects of novel DDR inhibitors on ubiquitination events.
Protocol for Evaluating DDR Inhibitor Combinations
Objective: To assess synergistic interactions between DNA-damaging agents and DDR inhibitors using 3D tumor organoid models.
Methodology:
- Organoid Culture and Treatment:
- Establish patient-derived organoids from colorectal cancer biopsies in Basement Membrane Extract matrix.
- Culture in appropriate stem cell medium with growth factors for 7 days until organoids reach 100-200μm diameter.
Drug Treatment and Viability Assessment:
- Treat organoids with serial dilutions of DDR inhibitors (e.g., ATR inhibitor ART0380) as single agents and in combination with DNA-damaging agents (e.g., cisplatin).
- Incubate for 96 hours, then assess viability using CellTiter-Glo 3D assay according to manufacturer's protocol.
- Calculate combination indices using the Chou-Talalay method to determine synergistic (CI<1), additive (CI=1), or antagonistic (CI>1) effects.
Immunofluorescence Analysis:
- Fix organoids after 24 hours of treatment and stain for γH2AX (DNA damage marker), cleaved caspase-3 (apoptosis), and RAD51 foci (HR repair).
- Image using high-content confocal microscopy and quantify foci per nucleus across multiple organoids.
This integrated approach provides comprehensive data on drug efficacy, mechanism of action, and effects on DNA repair pathways in a clinically relevant model system.
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Research Reagent Solutions for Ubiquitination and DDR Studies
| Reagent/Category | Specific Examples | Function/Application | Considerations |
|---|---|---|---|
| Cell Line Panels | CrownBio's collection: >500 cancer cell lines [69] | Initial high-throughput drug screening across diverse genetic backgrounds | Enables correlation of mutation status with drug response; limited TME representation |
| Organoid Biobanks | Patient-derived organoid collections [69] | 3D disease modeling, therapy response prediction, biomarker identification | Preserves tumor architecture and heterogeneity; more complex culture requirements |
| PDX Model Collections | CrownBio's PDX database (world's largest collection) [69] | Gold standard for in vivo efficacy studies, biomarker validation | Maintains tumor-stroma interactions; resource-intensive and lower throughput |
| DDR Antibodies | γH2AX, p-ATM, p-CHK1, p-CHK2, RAD51 | Immunofluorescence detection of DNA damage and repair markers | Critical for mechanistic studies; require careful validation for specific applications |
| Ubiquitination Probes | TUBE (Tandem Ubiquitin Binding Entity), K48- and K63-linkage specific antibodies | Detection and purification of specific ubiquitin chain linkages | Essential for deciphering the ubiquitin code in DDR; specificity validation required |
| Inhibitor Libraries | Proteasome inhibitors, E1 inhibitors, DUB inhibitors, specific E3 ligase inhibitors | Functional dissection of ubiquitin pathways in DDR | Tool compounds enable target validation; attention to selectivity important |
The field of DNA damage response therapeutics continues to evolve rapidly, with an expanding repertoire of clinical candidates targeting various nodes of the DDR network. The integration of ubiquitination mechanisms into this therapeutic landscape offers exciting opportunities for developing more precise and effective cancer treatments. The clinical progress in combining DNA-damaging agents with DDR inhibitors, alongside the emergence of novel agents like ATR kinase inhibitor ART0380, demonstrates the continued translation of basic DDR research into clinical applications [66] [67].
The future of DDR-targeted therapy will likely be shaped by several key trends, including the development of more selective inhibitors targeting specific E3 ubiquitin ligases or ubiquitin-binding domains, the identification of novel synthetic lethal interactions involving ubiquitination pathway components, and the refinement of biomarker strategies for patient selection. Additionally, the growing integration of advanced preclinical models—including cell lines, organoids, and PDX models—provides a powerful framework for accelerating the development of these promising therapeutic candidates [69]. As our understanding of the intricate relationships between ubiquitination signaling, DNA repair, and cancer progression deepens, so too will our ability to strategically target these pathways for therapeutic benefit across a broad spectrum of malignancies.
Navigating the Challenges: Resistance and Optimization in UPS-Targeted Therapies
Mechanisms of Resistance to Proteasome Inhibitors and E3-Targeting Drugs
The ubiquitin-proteasome system (UPS) represents a critical therapeutic target in oncology, particularly for hematological malignancies such as multiple myeloma and mantle cell lymphoma. While proteasome inhibitors (PIs) and drugs targeting E3 ubiquitin ligases have transformed treatment paradigms, the development of resistance remains a significant clinical challenge that limits long-term efficacy. This whitepaper examines the complex molecular mechanisms underlying acquired resistance to these therapeutic classes, focusing on mutations in proteasome subunits, adaptive overexpression of proteasome components, alterations in E3 ligase function, and activation of compensatory survival pathways. Within the broader context of ubiquitination in DNA damage response cancer research, we synthesize current understanding of resistance mechanisms, present structured experimental data, and provide methodological frameworks for investigating these pathways in preclinical models. The insights gathered aim to inform the development of novel strategies to overcome resistance and improve patient outcomes.
The ubiquitin-proteasome system (UPS) serves as the primary pathway for regulated intracellular protein degradation in eukaryotic cells, playing essential roles in maintaining protein homeostasis, cell cycle progression, DNA damage response, and apoptosis [70]. Protein degradation via this pathway involves two key sequential steps: (1) covalent attachment of ubiquitin chains to target proteins through a cascade involving E1 (activating), E2 (conjugating), and E3 (ligating) enzymes, and (2) degradation of the polyubiquitinated proteins by the 26S proteasome complex with recycling of ubiquitin by deubiquitinating enzymes (DUBs) [70]. The 26S proteasome consists of a 20S core particle (CP) capped by 19S regulatory particles (RP). The 20S CP is a barrel-shaped structure comprising four stacked heptameric rings (α7β7β7α7) with three catalytic β-subunits (β1, β2, and β5) responsible for caspase-like, trypsin-like, and chymotrypsin-like activities, respectively [71] [70].
Table 1: Clinically Approved Proteasome Inhibitors
| Inhibitor | Electrophile | Reversibility | Primary Subunit Target | Key Clinical Indications |
|---|---|---|---|---|
| Bortezomib | Boronate | Reversible | β5 (CT-L) | Multiple Myeloma, Mantle Cell Lymphoma |
| Carfilzomib | Epoxyketone | Irreversible | β5 (CT-L) | Multiple Myeloma |
| Ixazomib | Boronate | Reversible | β5 (CT-L) | Multiple Myeloma |
Cancer cells exhibit heightened dependence on proteasome function due to increased protein turnover and heightened proteotoxic stress, making them particularly vulnerable to proteasome inhibition [71]. This vulnerability has been successfully exploited therapeutically with the development of PIs such as bortezomib, carfilzomib, and ixazomib, which have revolutionized treatment for multiple myeloma and mantle cell lymphoma [70]. Simultaneously, E3 ubiquitin ligases have emerged as attractive therapeutic targets due to their substrate specificity. There are over 600 E3 ligases in humans, categorized into three main families based on their structural domains and mechanisms of action: Really Interesting New Gene (RING), Homologous to E6AP C-Terminus (HECT), and RING-Between-RING (RBR) families [52]. Notable therapeutic advances targeting E3 ligases include immunomodulatory imide drugs (IMiDs) such as lenalidomide and pomalidomide, which recruit the CRL4CRBN E3 ligase to degrade specific transcription factors like IKZF1/3 in multiple myeloma [72].
Despite the clinical success of these agents, treatment efficacy is ultimately limited by the development of drug resistance through diverse molecular mechanisms. Understanding these resistance pathways is crucial for developing strategies to overcome them and improve long-term patient outcomes.
Mechanisms of Resistance to Proteasome Inhibitors
Resistance to PIs can be either intrinsic, present before treatment initiation, or acquired, developing during therapy. Multiple overlapping mechanisms contribute to clinical resistance, encompassing alterations in the drug target, activation of compensatory pathways, and adaptive changes in cellular homeostasis.
Mutations in Proteasome Catalytic Subunits
A primary mechanism of acquired resistance to PIs involves mutations in the genes encoding proteasome catalytic subunits, particularly PSMB5, which encodes the β5 subunit responsible for chymotrypsin-like activity that is preferentially inhibited by most PIs [71]. These mutations often occur in the inhibitor-binding pocket and reduce drug binding affinity through steric hindrance or altered interaction geometries.
Table 2: Documented PSMB5 Mutations in Proteasome Inhibitor Resistance
| Mutation | Proteasome Inhibitor Affected | Experimental System | Functional Consequence |
|---|---|---|---|
| Ala49Thr | Bortezomib, Carfilzomib | Human multiple myeloma cell lines | Reduced binding affinity |
| Ala50Val | Bortezomib | Human multiple myeloma cell lines | Steric hindrance in substrate pocket |
| Cys52Phe | Bortezomib | Human leukemia cell lines | Altered active site conformation |
| Gly110Ala/Arg | Bortezomib | Salinispora tropica (marizomib resistance) | Natural resistance mutation |
The functional consequence of these mutations is a reduction in inhibitory potency while generally preserving proteolytic activity, providing resistant cells with a selective advantage under therapeutic pressure. In addition to point mutations, overexpression of mutant PSMB5 alleles has been observed in resistant cell lines, further amplifying the resistance phenotype [71].
Overexpression and Upregulation of Proteasome Subunits
Another significant resistance mechanism involves the increased expression and assembly of proteasome subunits, effectively increasing the target capacity that must be inhibited to achieve therapeutic effect. Resistant cancer cells can exhibit elevated transcript and protein levels of standard proteasome subunits as well as immunoproteasome subunits (β1i, β2i, β5i) [71]. This adaptive response is mediated in part by the transcription factor Nrf1, which activates the proteasome bounce-back response upon proteasome inhibition by translocating to the nucleus and binding antioxidant response elements (AREs) in proteasome subunit gene promoters [70]. The resulting increase in proteasome content and capacity enables continued protein turnover despite therapeutic concentrations of PIs, allowing cell survival.
Activation of Compensatory Protein Clearance Pathways
When proteasome function is compromised, cancer cells can activate alternative protein degradation systems to alleviate proteotoxic stress. Key among these is the autophagy-lysosomal pathway, which becomes upregulated in many PI-resistant models [70]. Additionally, aggressive formation represents a coordinated cellular response to sequester misfolded proteins and mitigate proteostatic stress. Pharmacological inhibition of these compensatory pathways can resensitize resistant cells to PIs, supporting their functional role in the resistance phenotype [70].
Alterations in Apoptotic Signaling and Survival Pathways
The efficacy of PIs ultimately depends on engaging apoptotic cell death programs, and resistance frequently involves disruptions in these pathways. Upregulation of anti-apoptotic Bcl-2 family proteins, including Bcl-2 itself and Mcl-1, has been documented in PI-resistant cells, raising the threshold for apoptosis induction [73]. Additionally, perturbations in the unfolded protein response (UPR) and ER stress signaling can alter cell fate decisions toward survival rather than death under conditions of proteasome inhibition [71]. The intricate interplay between the UPS and Bcl-2 family proteins creates a regulatory axis where proteasome inhibition can lead to stabilization of both pro- and anti-apoptotic factors, with the balance determining cellular outcome [73].
Diagram 1: Proteasome inhibitor resistance mechanisms.
Mechanisms of Resistance to E3-Targeting Drugs
E3 ubiquitin ligases represent promising therapeutic targets due to their substrate specificity, but resistance to E3-targeting agents emerges through diverse mechanisms that vary by drug class and cellular context.
Alterations in E3 Ligase Expression and Function
The most straightforward resistance mechanism to E3-targeting drugs involves changes in the expression or activity of the targeted E3 ligase itself. In the case of IMiDs, resistance can occur through downregulation or mutation of CRBN, the substrate receptor component of the CRL4CRBN E3 ligase complex [72]. CRBN mutations have been identified that disrupt drug binding while maintaining basal ligase activity, thereby conferring resistance without compromising essential cellular functions. Similarly, overexpression of the E3 ligase MDM2, which negatively regulates p53, can confer resistance to DNA-damaging agents by enhancing p53 degradation even in the presence of therapies designed to stabilize p53 [74] [72].
Substrate Stabilization and Mutation
Alterations in E3 ligase substrates represent another key resistance mechanism. This can occur through mutations in degron motifs (recognition elements for ubiquitination) that prevent productive E3-substrate interaction, as observed with IκBα mutations that impede its recognition by SCFβ-TrCP, leading to constitutive NF-κB activation [74]. Additionally, changes in substrate phosphorylation or other post-translational modifications that are prerequisites for E3 recognition can prevent substrate ubiquitination and degradation, even with intact E3 ligase function.
Upregulation of Compensatory E3 Ligases
When specific E3 ligases are inhibited, cells may upregulate functionally related E3 ligases that can ubiquitinate overlapping substrate sets, maintaining degradation of key regulatory proteins. This compensatory mechanism has been observed in the context of E3 ligases that regulate cell cycle progression, where inhibition of one cell cycle-regulating E3 leads to increased expression of others with similar functions [74]. This functional redundancy represents a fundamental challenge in targeting specific E3 ligases for cancer therapy.
Modulation of Deubiquitinating Enzymes (DUBs)
Counterbalancing the activity of E3 ubiquitin ligases are deubiquitinating enzymes (DUBs) that remove ubiquitin chains from substrates. Upregulation of specific DUBs can confer resistance to E3-targeting therapies by preventing substrate degradation. For example, increased expression of USP7 (HAUSP) can stabilize MDM2 and promote p53 degradation even when p53-stabilizing therapies are employed [75]. Similarly, USP9x-mediated deubiquitination of Mcl-1 can promote cell survival in the presence of therapies designed to degrade this anti-apoptotic protein [75].
Diagram 2: E3-targeting drug resistance mechanisms.
Experimental Approaches for Investigating Resistance Mechanisms
Systematic investigation of resistance mechanisms requires integrated experimental approaches spanning molecular biology, genomics, and chemical biology. Below are key methodologies for elucidating these pathways.
Generation of Resistant Cell Models
Protocol: Development of Proteasome Inhibitor-Resistant Cell Lines
- Initiate selection with low concentrations of PI (e.g., 5-10 nM bortezomib) in human cancer cell lines (e.g., MM.1S, RPMI-8226 for multiple myeloma).
- Culture cells in stepwise increasing drug concentrations over 6-9 months, not exceeding 2-3-fold increases when cells demonstrate stable proliferation.
- Clone resistant populations by limiting dilution to establish homogeneous resistant sublines.
- Validate resistance phenotype through dose-response assays (MTT/Alamar Blue) and proteasome activity measurements.
- Maintain resistant lines under continuous selective pressure but culture in drug-free medium for 2 weeks before experiments to assess stability of resistance.
Protocol: CRISPR Screening for E3-Targeting Drug Resistance Genes
- Transduce target cells with a genome-wide CRISPR/Cas9 knockout library (e.g., Brunello or GeCKO v2).
- Select transduced cells with puromycin for 7 days.
- Split cells into treatment (IC50-IC70 of E3-targeting drug) and control (DMSO) groups for 14-21 days.
- Harvest genomic DNA and amplify integrated sgRNA sequences by PCR.
- Sequence amplified products by next-generation sequencing and identify enriched sgRNAs in treatment versus control using specialized algorithms (MAGeCK, BAGEL).
Molecular Profiling of Resistant Cells
Comprehensive characterization of resistant models should include:
- Whole exome sequencing to identify acquired mutations in proteasome subunits, E3 ligases, and related pathways
- RNA sequencing to quantify transcriptomic adaptations, including proteasome subunit overexpression and alternative pathway activation
- Proteomic analysis (LC-MS/MS) to measure changes in protein abundance and post-translational modifications
- Ubiquitinome profiling using di-Gly remnant enrichment to map global changes in protein ubiquitination
Table 3: Key Analytical Methods for Resistance Mechanism Investigation
| Method | Application | Key Readouts |
|---|---|---|
| Whole Exome Sequencing | Mutation identification | PSMB5 mutations, CRBN mutations |
| RNA Sequencing | Transcriptome profiling | Proteasome subunit overexpression, Alternative pathway activation |
| Tandem Mass Tag Proteomics | Protein quantification | Changes in proteasome composition, Apoptotic regulators |
| - Activity-Based Protein Profiling | Proteasome activity measurement | Residual CT-L, T-L, C-L activities in resistant cells |
| - Co-immunoprecipitation + MS | Protein complex analysis | Altered E3 ligase-substrate interactions |
| - Cellular Thermal Shift Assay | Drug-target engagement | Reduced drug binding to mutated targets |
Functional Validation Approaches
Candidate resistance genes identified through genomic approaches require functional validation:
- CRISPR/Cas9-mediated gene knockout: Confirm resistance causality by knocking out identified mutant genes in parental cells.
- cDNA overexpression: Test if candidate genes confer resistance when overexpressed in sensitive cells.
- siRNA/shRNA knockdown: Reverse resistance phenotype by knocking down overexpressed genes in resistant cells.
- Gene editing to introduce specific mutations: Use base editing or prime editing to introduce specific resistance-associated mutations in isogenic backgrounds.
The Scientist's Toolkit: Essential Research Reagents
Table 4: Key Research Reagents for Investigating UPS Resistance Mechanisms
| Reagent Category | Specific Examples | Research Application | Functional Role |
|---|---|---|---|
| Proteasome Inhibitors | Bortezomib, Carfilzomib, MG132, Epoxomicin | Inducing and studying resistance | Selective pressure application, proteasome activity modulation |
| - E3-Targeting Compounds | Lenalidomide, Pomalidomide, MLN4924, PROTACs | E3 ligase function studies | CRL4CRBN recruitment, cullin neddylation inhibition, targeted degradation |
| - Activity Reporters | Proteasome activity probes (MV151), Ubiquitin mutants (K48R, K63R) | Monitoring pathway function | Visualization of active proteasomes, chain linkage specificity determination |
| - Antibodies | Anti-PSMB5, Anti-CRBN, Anti-Ubiquitin, Anti-K48-Ub, Anti-K63-Ub | Detection and quantification | Western blot, immunofluorescence, monitoring expression changes |
| - Cell Lines | MM.1S, RPMI-8226, HCT116, HEK293T, Resistant derivatives | Model systems | Parental and resistant isogenic pairs for comparative studies |
| - CRISPR Libraries | GeCKO v2, Brunello, SAM | Genetic screens | Genome-wide loss-of-function screening for resistance genes |
| - Apoptosis Assays | Annexin V staining, Caspase-3/7 activity assays, JC-1 mitochondrial potential | Cell death quantification | Measuring apoptotic response in resistant vs. sensitive cells |
Resistance to proteasome inhibitors and E3-targeting drugs represents a multifaceted challenge in cancer therapeutics, driven by diverse molecular adaptations including target mutations, pathway compensations, and apoptotic evasion. Understanding these mechanisms within the broader context of ubiquitination in DNA damage response and cancer biology provides critical insights for developing next-generation therapeutic strategies. Promising approaches include combination therapies targeting complementary pathways, developing non-cross-resistant inhibitors, and exploiting emerging technologies such as PROTACs that simultaneously engage multiple components of the UPS. As our understanding of resistance mechanisms deepens, so too will our ability to design more durable and effective treatment regimens for cancer patients. Future research directions should focus on comprehensive characterization of resistance in clinical samples, development of predictive biomarkers for early detection of emerging resistance, and innovative therapeutic modalities that preemptively target resistance mechanisms before they become clinically established.
The ubiquitin-proteasome system (UPS) represents a pivotal regulatory network in eukaryotic cells, governing protein stability, function, and localization. Ubiquitination, a post-translational modification involving the covalent attachment of ubiquitin to target proteins, plays particularly crucial roles in the DNA damage response (DDR) and cellular metabolism—both fundamental processes frequently dysregulated in cancer [36]. The specificity of ubiquitination is primarily determined by E3 ubiquitin ligases, which recognize substrate proteins and facilitate ubiquitin transfer [36]. With over 600 E3 ligases encoded in the human genome, this system offers remarkable potential for therapeutic targeting [76].
The development of ubiquitin-based drugs, particularly within the context of DNA damage response cancer research, represents a frontier in oncology therapeutics. Targeted protein degradation (TPD) has emerged as a revolutionary strategy that capitalizes on the cell's intrinsic ubiquitin-proteasome system to eliminate disease-causing proteins [76]. Unlike traditional small molecule inhibitors that merely block protein function, degraders such as PROTACs (proteolysis-targeting chimeras) and molecular glues catalytically destroy target proteins, offering potential advantages in efficacy, dosing, and overcoming resistance [76]. However, achieving sufficient specificity to minimize off-target effects remains a significant challenge in the field. This technical guide examines the sources of off-target effects in ubiquitin-based drugs and outlines systematic strategies to enhance specificity, with particular emphasis on applications in DNA damage response and cancer metabolism.
The Specificity Challenge in Ubiquitin-Based Therapeutics
Fundamental Mechanisms of Off-Target Effects
Off-target effects in ubiquitin-based therapies arise from multiple intrinsic properties of the ubiquitin system and compound characteristics:
E3 Ligase Promiscuity: Many E3 ligases, including HUWE1, display broad substrate specificity, potentially leading to unintended degradation of non-target proteins [77]. During DNA damage response, certain E3 ligases like RNF8 and RNF168 participate in extensive signaling networks, creating vulnerability for off-target signaling [36] [24].
Ternary Complex Instability: The transient nature of E3 ligase-PROTAC-target protein interactions can result in imperfect specificity, particularly concerning the "hook effect" where high PROTAC concentrations saturate individual binding sites without forming productive ternary complexes [76] [78].
Ligand Cross-Reactivity: Warheads designed to bind specific E3 ligases or target proteins may exhibit affinity for structurally similar off-target proteins. For instance, CRBN-binding molecules like thalidomide derivatives can neosubstrate degradation of unintended targets [76].
Ubiquitin Spillover: Even when ternary complexes form specifically, the proximity-induced ubiquitination may affect neighboring proteins in the same complex through "bystander ubiquitination" [78].
Quantitative Assessment of Off-Target Effects
Comprehensive profiling of the "ubiquitinome"—the complete set of ubiquitinated proteins in a cell—provides a systematic approach to identify off-target effects. Global analysis using diGly remnant capture following trypsin digestion has identified approximately 19,000 ubiquitination sites within ~5,000 proteins [79]. This methodology enables quantitative tracking of temporal changes in ubiquitination site abundance in response to therapeutic interventions, allowing researchers to distinguish intended therapeutic effects from off-target ubiquitination events.
Table 1: Experimental Approaches for Identifying Off-Target Effects in Ubiquitin-Based Therapeutics
| Method | Application | Key Readout | Considerations |
|---|---|---|---|
| diGly Proteomics | System-wide ubiquitination mapping | ~19,000 ubiquitination sites across ~5,000 proteins | Requires specific antibodies; may miss low-abundance sites [79] |
| Ternary Complex Stability Assays | Assessment of complex formation kinetics | Kd, half-life of ternary complex | May not fully recapitulate cellular environment [78] |
| Cellular Thermal Shift Assay (CETSA) | Target engagement verification | Thermal stability shifts of target proteins | Can detect direct and indirect stabilization effects [76] |
| Pulse-Chase Proteomics | Protein turnover measurement | Degradation rates of multiple proteins | Distinguishes direct vs. indirect degradation effects [76] |
Strategic Approaches to Enhance Specificity
Ligase Selection and Engineering
The choice of E3 ligase fundamentally influences degrader specificity. Tissue-specific or context-dependent E3 ligase expression provides natural opportunities for enhanced selectivity:
Ligase Expression Profiling: Comprehensive analysis of E3 ligase expression patterns across tissues and disease states enables selection of ligases with restricted expression profiles. For instance, leveraging E3 ligases uniquely expressed in cancerous tissues can enhance tumor-selective degradation while sparing healthy tissues [78].
Specialized E3 Ligase Families: Focus on E3 ligases with naturally constrained substrate recognition, such as VHL, which primarily targets HIF-1α under normoxic conditions [76]. Engineering derivatives of these ligases with further refined specificity represents a promising approach.
Ligase-Specific Warhead Optimization: Structure-guided design of E3 ligase ligands to minimize cross-reactivity with structurally similar ligases. Crystallographic studies of ligase-warhead interactions enable rational optimization of binding specificity [76].
Table 2: Selected E3 Ligases in Targeted Protein Degradation and Their Characteristics
| E3 Ligase | Native Substrate | Tissue Expression | Specificity Considerations |
|---|---|---|---|
| VHL | HIF-1α | Ubiquitous | Well-defined binding pocket; oxygen-dependent substrate recognition [76] |
| CRBN | – | Ubiquitous | Binds diverse small molecules; susceptibility to neosubstrate formation [76] |
| MDM2 | p53 | Ubiquitous (overexpressed in some cancers) | Native role in specific pathway; potential for p53 stabilization [76] |
| IAP Family | Caspases | Varies by family member | Can simultaneously degrade target and IAPs (dual pharmacology) [76] |
| HUWE1 | Multiple substrates | Ubiquitous | Broad substrate specificity; potential for off-target degradation [77] |
Molecular Design Strategies
PROTAC Optimization
The modular architecture of PROTACs enables multiple engineering strategies to enhance specificity:
Linker Optimization: Systematic variation of linker length, composition, and rigidity to optimize spatial orientation in the ternary complex. Studies demonstrate that even single-atom changes in linker composition can significantly impact degradation specificity [78].
Affinity-Balance Engineering: Deliberate modulation of individual binding affinities rather than maximal affinity for both warheads. Moderate affinity (nanomolar to micromolar range) often supports sufficient ternary complex formation while reducing off-target binding [78].
Macrocyclization: Conformational constraint through macrocyclization enhances selectivity by reducing structural flexibility and pre-organizing the PROTAC in its bioactive conformation. Macrocyclic PROTACs demonstrate improved selectivity profiles compared to their linear counterparts [78].
Context-Activatable Degraders
Novel PROTAC modalities that remain inactive until encountering specific disease microenvironment conditions offer powerful specificity enhancements:
Photoactivatable PROTACs: Incorporation of photolabile groups that enable spatiotemporal control of PROTAC activity through light exposure, confining activity to precisely defined regions [78].
Hypoxia-Activated PROTACs: Utilization of hypoxia-labile groups that trigger PROTAC activation specifically in the hypoxic tumor microenvironment, leveraging a hallmark feature of solid tumors [78].
Protease-Activatable PROTACs: Design of PROTACs containing peptide sequences cleavable by tumor-specific proteases, restricting activity to proteolytically active tumor regions [78].
Experimental Approaches for Specificity Validation
Ternary Complex Characterization
Robust assessment of ternary complex formation and stability provides critical insights into degradation specificity:
Diagram 1: Ternary complex formation pathway
Surface Plasmon Resonance (SPR) with Ternary Complex Capability: Protocol: Immobilize either POI or E3 ligase on sensor chip. Introduce PROTAC alone to confirm binary binding. Subsequently, introduce the third component in the presence of saturating PROTAC concentrations to detect enhanced binding response indicative of ternary complex formation. Key Parameters: Measure binding response units (RU) increase beyond additive effects of individual interactions. Data Interpretation: Stable ternary complexes typically demonstrate slow dissociation kinetics and enhanced binding response compared to binary interactions [76].
Crystallography of Ternary Complexes: Protocol: Co-crystallize POI-PROTAC-E3 ligase complexes using vapor diffusion methods. Collect diffraction data at synchrotron sources (resolution ≤3.0 Å recommended). Key Parameters: Analyze protein-protein interface areas, conformational changes in ligase and POI, and solvent-accessible surface burial. Data Interpretation: Productive complexes typically show extensive protein-protein interfaces (≥800 Ų) and complementary surface topology [76].
Specificity Profiling
Global Ubiquitinome Monitoring: Protocol: Adapt the diGly capture methodology [79]. Treat cells with degraders vs. DMSO control. Harvest cells, denature proteins, and digest with trypsin. Immunoprecipitate diGly-modified peptides using specific antibodies. Analyze by LC-MS/MS. Key Parameters: Quantify fold-change in ubiquitination sites (≥2-fold increase considered significant). Monitor known off-target substrates specific to E3 ligase employed. Data Interpretation: Successful degraders show selective increase in target protein ubiquitination without widespread changes in ubiquitinome [79].
Competitive Activity-Based Protein Profiling: Protocol: Use broad-spectrum cysteine-reactive probes (e.g., iodoacetamide-alkyne) to assess ligase engagement in complex proteomes. Pre-treat cells with degraders at various concentrations, then add probes. Click in biotin for enrichment and identify bound proteins by MS. Key Parameters: Calculate % reduction in probe labeling for target E3 ligase relative to DMSO control. Data Interpretation: Selective degraders show preferential reduction in target E3 ligase labeling without affecting unrelated cysteine-containing proteins [77].
The Scientist's Toolkit: Key Research Reagents
Table 3: Essential Reagents for Assessing Off-Target Effects in Ubiquitin-Based Drug Development
| Reagent/Category | Specific Examples | Primary Function | Specificity Assessment Application |
|---|---|---|---|
| E3 Ligase Ligands | VHL ligand VH032, CRBN ligand lenalidomide, MDM2 ligand Nutlin-3 | Recruit endogenous E3 ligase machinery | Warhead specificity profiling; ternary complex formation assays [76] |
| diGly Remnant Antibodies | Commercial monoclonal anti-diGly antibodies (e.g., Cell Signaling Technology #8805) | Enrich ubiquitinated peptides from proteomic digests | System-wide identification of ubiquitination changes; off-target ubiquitination monitoring [79] |
| Ubiquitin Activating Enzymes | Recombinant UBA1 (E1), UBE2L3/UBE2D3 (E2s) | Reconstitute ubiquitination cascade in vitro | Biochemical specificity assessment; compound ubiquitination potential [77] |
| Proteasome Inhibitors | Bortezomib, MG132, Epoxomicin | Block proteasomal degradation | Stabilize ubiquitinated proteins for detection; validate degradation mechanism [79] [76] |
| Deubiquitinase Enzymes | Recombinant USP2 catalytic domain | Strip ubiquitin from substrates | Confirm ubiquitin-dependent effects; distinguish direct vs. indirect ubiquitination [79] |
| Activity-Based Probes | HA-Ub-VS, ubiquitin-based suicide inhibitors | Monitor ubiquitin enzyme activities | Assess target engagement and selectivity in complex proteomes [77] |
Achieving specificity in ubiquitin-based drugs requires a multi-faceted approach combining strategic E3 ligase selection, rational molecular design, and rigorous experimental validation. The expanding toolkit for profiling the ubiquitinome and characterizing ternary complexes provides unprecedented capability to identify and mitigate off-target effects during drug development. As the field advances, several promising areas are emerging:
Tissue-Specific E3 Ligase Exploitation: Increased mapping of E3 ligase expression patterns across tissues and disease states will enable more selective targeting approaches [78].
Nanotechnology Integration: Nano-PROTACs and antibody-PROTAC conjugates show promise in enhancing tissue-specific delivery while minimizing systemic exposure [78].
Multi-Specific Degraders: Trivalent PROTACs simultaneously engaging multiple E3 ligases may enhance specificity through combinatorial recognition logic [78].
Computational Prediction Advances: Machine learning models trained on structural and ubiquitinome data are becoming increasingly capable of predicting degradation specificity during compound design [76].
The integration of these strategies will ultimately enable the development of ubiquitin-based therapies with precision matching their revolutionary mechanism of action, particularly in the context of DNA damage response and cancer metabolism where selective intervention is paramount for therapeutic success.
Proteolysis Targeting Chimeras (PROTACs) represent a paradigm shift in therapeutic strategy, moving beyond simple inhibition to direct protein degradation. These heterobifunctional molecules harness the cell's endogenous ubiquitin-proteasome system (UPS) to selectively degrade disease-relevant proteins, offering a powerful approach for targeting previously "undruggable" oncogenes and resistance mechanisms in cancer [80] [42]. The UPS, a fundamental pathway for maintaining cellular protein homeostasis, becomes a powerful weapon against cancer when co-opted by PROTAC technology [1] [80].
The relevance of PROTACs is particularly pronounced in the context of DNA damage response (DDR) in cancer research. Many cancers rely on efficient DDR pathways for survival and therapy resistance, making these pathways attractive therapeutic targets [24] [81]. The ubiquitin system itself plays critical roles in DDR, where specialized ubiquitin chains (e.g., K63-linked) help coordinate repair protein recruitment and pathway choice at DNA double-strand breaks [1] [24]. By designing PROTACs that degrade key DDR components, researchers can selectively sensitize cancer cells to genotoxic therapies or exploit inherent DNA repair deficiencies.
PROTAC Mechanism of Action and Molecular Components
The Ubiquitin-Proteasome System and Ternary Complex Formation
PROTACs function by catalyzing a three-step process that culminates in target protein degradation. A typical PROTAC molecule consists of three key elements: a ligand that binds to the protein of interest (POI), a ligand that recruits an E3 ubiquitin ligase, and a chemical linker connecting these two moieties [82] [42]. Mechanistically, the PROTAC simultaneously engages both the POI and an E3 ubiquitin ligase, forming a productive POI-PROTAC-E3 ligase ternary complex [83]. This complex brings the POI into close proximity with the E3 ligase, which then facilitates the transfer of ubiquitin chains from an E2 conjugating enzyme to lysine residues on the POI [82] [80]. Once polyubiquitinated (typically with K48-linked chains comprising at least four ubiquitin molecules), the POI is recognized and degraded by the 26S proteasome [80] [42]. The PROTAC molecule is subsequently released unchanged and can catalyze additional rounds of degradation, operating in a sub-stoichiometric, catalytic manner [82].
Visualization of the PROTAC Mechanism and Ubiquitin Signaling
The following diagram illustrates the core mechanism of action of PROTACs and their relationship with key ubiquitin signaling in the DNA damage response:
Strategic Optimization of PROTAC Components
Linker Chemistry and Design Principles
The linker in PROTAC design is far more than a simple tether—it critically influences the molecule's spatial conformation, degradation efficiency, and physicochemical properties. Optimal linker design ensures proper distance and orientation between the POI and E3 ligase to facilitate stable ternary complex formation [83] [84].
Linker Composition and Properties: Linkers are typically composed of 5-15 carbon atoms or other atomic chains and can be categorized as flexible (e.g., PEG-based, alkyl chains) or rigid (e.g., incorporating piperazine, piperidine, or spirocycles) [82] [42]. Flexible linkers offer conformational freedom but may entropically penalize ternary complex formation, while rigid linkers reduce the energetic cost of complex formation by pre-organizing the PROTAC into a bioactive conformation [82]. Recent advances have introduced functionalized "smart" linkers with capabilities such as photo-switching for spatiotemporal control or cleavable elements for targeted release [84].
Optimization Strategies: Linker optimization involves systematic variation of length and composition to maximize degradation potency. For instance, incorporating rigid structures like spirocycles or piperidines has been shown to significantly improve degradation potency and oral bioavailability [82]. The optimal linker length is typically determined empirically, as it depends on the specific spatial arrangement required for productive ternary complex formation between the particular POI and E3 ligase pair [83].
E3 Ligase Selection and Expanding the Toolkit
E3 ubiquitin ligase selection fundamentally influences PROTAC efficacy, selectivity, and therapeutic potential. While over 600 E3 ligases exist in humans, current PROTAC designs predominantly utilize a small subset, with CRBN and VHL being the most extensively validated [82] [80].
Dominant E3 Ligases in Current Use: Cereblon (CRBN) recruitment, typically via thalidomide or its derivatives (e.g., pomalidomide, lenalidomide), dominates clinical-stage PROTACs due to favorable drug-like properties and broad tissue expression [82] [80]. Von Hippel-Lindau (VHL) recruitment, using small-molecule ligands like VHL-1, offers an alternative with distinct recognition properties. The choice between CRBN and VHL recruiters can significantly impact degradation efficiency due to differences in their spatial orientation requirements and natural substrate preferences [82].
Emerging E3 Ligases and Tissue Specificity: A major frontier in PROTAC development involves expanding the E3 ligase repertoire to address limitations of current systems. New E3 ligands are being developed with novel scaffolds such as phenyl glutarimide (PG) derivatives and TX-16, which offer improved stability and affinity compared to traditional thalidomide derivatives [82]. Additionally, leveraging E3 ligases with restricted tissue expression patterns (e.g., KLHL20 in prostate, DCAF15 in gastrointestinal tract) represents a promising strategy to achieve tissue-selective degradation and reduce off-target effects [83].
Table 1: Key E3 Ubiquitin Ligases in PROTAC Design
| E3 Ligase | Common Ligands | Advantages | Limitations | Clinical Stage Examples |
|---|---|---|---|---|
| Cereblon (CRBN) | Thalidomide, Lenalidomide, Pomalidomide | Excellent drug-like properties, extensive validation | Teratogenicity risk, limited structural diversity | ARV-110, ARV-471, NX-2127 [82] |
| Von Hippel-Lindau (VHL) | VHL-1 and derivatives | Alternative to CRBN, different structural constraints | Lower cell permeability in some designs | DT-2216 [82] |
| MDM2 | Nutlin-3a | Early validation in PROTAC design | Potential p53 activation | Preclinical candidates [42] |
| IAP (cIAP1) | Methyl bestatin analogues | Alternative recruitment strategy | Potential non-specific apoptosis induction | Preclinical candidates [42] |
Experimental Approaches for PROTAC Characterization
Ternary Complex Analysis and Cooperativity Assessment
A critical determinant of PROTAC efficacy is the formation of a stable ternary complex, quantified by the cooperativity factor (α). This factor is defined as the ratio of binary (POI/PROTAC or E3 ligase/PROTAC) and ternary (POI/PROTAC/E3 ligase) dissociation constants [83]. When α > 1, the ternary complex is more stable than the binary complexes, indicating positive cooperativity that enhances degradation efficiency [83].
Methodology for Cooperativity Measurement:
- AlphaScreen/AlphaLISA Assay: This bead-based proximity assay is widely used to study ternary complex formation. Donor beads conjugated to the POI and acceptor beads conjugated to the E3 ligase emit a signal when brought together by the PROTAC. The signal intensity correlates with ternary complex stability, allowing calculation of binding affinities and cooperativity [83].
- Biolayer Interferometry (BLI): BLI measures binding kinetics by immobilizing one component (e.g., POI) on a biosensor tip and monitoring interference pattern changes as other components (PROTAC, E3 ligase) bind. This enables real-time assessment of ternary complex formation and dissociation constants [83].
- Surface Plasmon Resonance (SPR): Similar to BLI, SPR measures biomolecular interactions through changes in refractive index at a sensor surface. It provides high-quality kinetic data for ternary complex formation but requires careful experimental design [83].
- Time-Resolved Fluorescence Resonance Energy Transfer (TR-FRET): This technique uses fluorescently labeled POI and E3 ligase to measure energy transfer when brought together by PROTAC, allowing quantification of ternary complex formation in solution [83].
Functional Degradation Assessment
Beyond ternary complex formation, comprehensive PROTAC characterization requires multiple orthogonal assays to confirm degradation efficiency and specificity.
Protocol for Degradation Efficacy Evaluation:
- Cell Culture and Treatment: Seed appropriate cancer cell lines (e.g., prostate cancer lines for AR-targeting PROTACs) in multi-well plates and allow to adhere for 24 hours.
- PROTAC Dosing: Treat cells with serially diluted PROTAC concentrations (typically from 1 nM to 10 μM) for predetermined timepoints (e.g., 6, 16, 24 hours).
- Protein Extraction and Quantification: Lyse cells in RIPA buffer with protease inhibitors, quantify protein concentration using BCA assay.
- Western Blot Analysis: Separate proteins by SDS-PAGE, transfer to PVDF membrane, and probe with target-specific antibodies. Include loading controls (e.g., GAPDH, β-actin).
- Quantitative Analysis: Measure band intensity to determine DC50 (concentration causing 50% degradation) and Dmax (maximum degradation achieved) [83].
- Cellular Proliferation/Viability Assays: Complement degradation data with cell viability assays (e.g., CellTiter-Glo) to establish correlation between degradation and functional effects.
- Proteasome Dependence Verification: Include control experiments with proteasome inhibitors (e.g., MG-132) to confirm UPS-dependent degradation.
- Selectivity Assessment: Use global proteomics approaches (e.g., TMT or SILAC mass spectrometry) to evaluate off-target degradation and confirm selectivity [83].
Table 2: Key Quantitative Parameters in PROTAC Optimization
| Parameter | Definition | Optimal Range | Experimental Method |
|---|---|---|---|
| DC₅₀ | Concentration causing 50% target degradation | Low nM range preferred | Western blot with quantification [83] |
| Dmax | Maximum degradation achieved | >80% for robust efficacy | Western blot with quantification [83] |
| Cooperativity (α) | Ratio of ternary vs. binary complex stability | α > 1 (positive cooperativity) | BLI, SPR, AlphaScreen [83] |
| Catalytic Efficiency | Number of degradation cycles per PROTAC | >1 for catalytic advantage | Cellular degradation kinetics [82] |
| Selectivity Index | Ratio of on-target vs. off-target degradation | >10-fold preferred | Global proteomics [83] |
Research Reagent Solutions for PROTAC Development
Table 3: Essential Research Tools for PROTAC Development
| Reagent Category | Specific Examples | Function/Application | Commercial Sources |
|---|---|---|---|
| Recombinant E3 Ligases | CRBN, VHL, BIRC3, BIRC7, HERC4, MGRN1, RanBP2, RNF34, RNF34L, TRIM37, WWP2, CBL [82] | In vitro ubiquitination assays, binding studies, ternary complex analysis | SignalChem Biotech, Sino Biological [82] |
| Target Proteins | Recombinant AR, ER, BTK, BRD4, STAT3, CDKs | PROTAC screening and characterization | Multiple suppliers (e.g., Sino Biological) [82] |
| Functional Assay Reagents | Ubiquitin, E1/E2 enzymes, ATP, proteasome complexes | Biochemical assessment of ubiquitination and degradation | Enzo Life Sciences, Boston Biochem [82] |
| Cellular Degradation Reporters | Engineered cell lines with tagged targets (e.g., HaloTag, NanoLuc) | High-throughput degradation screening | Custom engineering or commercial sources [83] |
| Characterization Antibodies | Phospho-specific, ubiquitin remnant, target-specific antibodies | Detection of degradation and ubiquitination | Cell Signaling Technology, Abcam [83] |
Clinical Translation and Applications in DNA Damage Response
The therapeutic potential of PROTACs is demonstrated by the rapid clinical advancement of multiple candidates, particularly in oncology. As of 2025, over 40 PROTAC drug candidates are undergoing clinical evaluation, with three agents reaching Phase III trials [85].
Promising Clinical Candidates:
- Vepdegestrant (ARV-471): An ER-targeting PROTAC for ER+/HER2- breast cancer that has demonstrated statistically significant improvement in progression-free survival in patients with ESR1 mutations in Phase III trials (VERITAC-2) [85].
- BMS-986365 (CC-94676): An AR-targeting PROTAC for metastatic castration-resistant prostate cancer (mCRPC) that has shown approximately 100 times greater potency than enzalutamide in suppressing AR-driven gene transcription [85].
- BGB-16673: A BTK-targeting PROTAC for B-cell malignancies that has advanced to Phase III trials, offering potential solutions to BTK inhibitor resistance mutations [85].
Connection to DNA Damage Response: The intersection of PROTAC technology with DDR pathways creates compelling therapeutic opportunities. For instance, PROTACs targeting CDKs (particularly transcriptional CDKs like CDK7, CDK9, and CDK12) can simultaneously disrupt cell cycle progression and DNA damage response transcription, potentially sensitizing tumors to DNA-damaging agents [81]. CDK12 inhibition via degradation, for example, causes homologous recombination deficiency, making cancers more vulnerable to PARP inhibitors [81]. Additionally, PROTACs targeting key DDR components themselves (e.g., BRCA1, PARP, or DNA repair kinases) could provide novel mechanisms to exploit synthetic lethal relationships in cancer cells.
PROTAC technology has evolved from a conceptual framework to a clinically validated approach with transformative potential for cancer therapy, particularly in targeting DNA damage response pathways. The strategic optimization of linker chemistry and E3 ligase selection remains central to developing PROTACs with enhanced efficacy, selectivity, and drug-like properties. Future directions will likely focus on expanding the E3 ligase toolbox beyond the current CRBN/VHL dominance, developing tissue-selective degraders, and exploiting novel mechanistic insights into ternary complex formation. The integration of artificial intelligence and computational approaches is already accelerating PROTAC design, from predicting ternary complex structures to optimizing linker properties [83]. As this field advances, the rational design of PROTACs targeting components of the ubiquitin-mediated DNA damage response represents a promising frontier for precision oncology, potentially offering new therapeutic options for cancers with specific vulnerabilities.
The ubiquitin-proteasome system (UPS) represents a master regulatory network that controls virtually all DNA damage response (DDR) pathways through spatiotemporal control of protein stability, localization, and function. Mounting clinical evidence firmly establishes the UPS as a critical orchestrator of radioresistance and chemoresistance through its manipulation of DNA repair fidelity, metabolic reprogramming, and immune evasion [86]. The ubiquitin system's unique clinical advantages—including dynamic reversibility, chain topology diversity, and recent breakthroughs in targeted degradation (e.g., PROTACs)—enable precise disruption of therapy resistance networks in cancer [86]. As UPS-targeted therapies emerge as fundamental components of next-generation oncology treatment protocols, the development of robust biomarkers to identify responsive patients becomes increasingly critical for advancing precision medicine. This technical guide examines current methodologies and frameworks for biomarker development in the context of UPS-targeted therapies, with particular emphasis on their application within DDR pathways.
Biomarker Types and Clinical Applications in UPS-Targeted Therapy
Biomarkers for UPS-targeted therapies span multiple molecular classes and clinical applications, each with distinct validation requirements and implementation challenges. The table below summarizes key biomarker categories and their roles in patient stratification for UPS-targeted therapies.
Table 1: Biomarker Types and Clinical Applications in UPS-Targeted Therapy
| Biomarker Category | Molecular Examples | Clinical Application | Validation Considerations |
|---|---|---|---|
| Genetic Alterations | E3 ligase mutations, DUB amplifications, substrate mutations | Predictive of sensitivity to specific UPS-targeted agents | Functional validation of impact on ubiquitination; cohort size for rare mutations |
| Expression Signatures | Multi-gene ubiquitination signatures (e.g., MMP1, RNF2, TFRC, SPP1, CXCL8) [87] | Prognostic stratification; treatment selection | Analytical validity across platforms; clinical utility in prospective trials |
| Protein Ubiquitination | K48-linked vs K63-linked chain accumulation, monoubiquitination patterns | Pharmacodynamic monitoring; mechanism of action confirmation | Sample preservation requirements; antibody specificity validation |
| Functional Capacity | DNA repair deficiency signatures, synthetic lethal interactions [88] | Predictive of vulnerability to UPS inhibition | Assay standardization; quantitative cutpoints for clinical decision-making |
The contextual duality of UPS components presents both challenges and opportunities for biomarker development. For example, FBXW7 exhibits opposing roles in radiation response depending on tumor genetics: it promotes radioresistance in p53-wild type colorectal tumors by degrading p53, but enhances radiosensitivity in non-small cell lung cancer with SOX9 overexpression by destabilizing SOX9 and alleviating p21 repression [86]. This highlights the critical importance of understanding tumor-specific genetic backgrounds when developing predictive biomarkers for UPS-targeted therapies.
Biomarker Discovery Methodologies and Experimental Protocols
Systematic Genetic Interaction Mapping
Comprehensive mapping of synthetic lethal relationships within the DDR network provides a powerful approach for identifying biomarker candidates. The recently developed SPIDR (Systematic Profiling of Interactions in DNA Repair) platform represents a cutting-edge methodology for large-scale genetic interaction screening [88].
Table 2: Key Experimental Parameters for CRISPRi Synthetic Lethality Screening
| Parameter | Specification | Rationale |
|---|---|---|
| Library Design | 548 core DDR genes; 697,233 guide-level interactions | Comprehensive coverage of DNA repair pathways |
| Screening System | CRISPR interference (CRISPRi) with dual-sgRNA expression | Avoids DSB generation; models hypomorphic mutations |
| Cell Model | RPE-1 TP53 knockout cells | Karyotypically normal background with intact DDR |
| Experimental Endpoint | 14-day proliferation assay | Identifies synthetic lethal interactions affecting fitness |
| Analysis Pipeline | GEMINI (variational Bayesian) | Specialized for genetic interaction discovery from CRISPR data |
Protocol Overview:
- Library Construction: Design sgRNAs targeting all genes with "DNA repair" GO term (GO:0006281), including at least two sgRNAs per gene paired with every other sgRNA
- Cell Line Engineering: Generate clonal cell line stably expressing catalytically inactive Cas9-KRAB fusion protein
- Lentiviral Transduction: Transduce cells with dual-sgRNA library at low MOI to ensure single integration events
- Phenotypic Screening: Collect T0 cells 96 hours post-transduction and T14 cells after 14 days of proliferation
- Next-Generation Sequencing: Quantify sgRNA abundance by NGS at both time points
- Genetic Interaction Scoring: Apply GEMINI pipeline to identify synthetic lethal interactions (score ≤ -1) exceeding single-gene effects
This approach successfully identified previously unknown synthetic lethal interactions, such as WDR48 with USP1 in FEN1/LIG1-deficient cells and FANCM with SMARCAL1, providing novel biomarker hypotheses for UPS-targeted therapy [88].
Ubiquitination-Related Gene Signature Development
The development of multi-gene signatures from ubiquitination-related genes (UbLGs) enables prognostic stratification and treatment response prediction. The following protocol outlines key steps for UbLG signature development:
Protocol: Ubiquitination-Related Biomarker Signature Development [87]
Data Acquisition and Processing:
- Collect transcriptomic data from tumor and normal samples (self-seq and public databases)
- Identify differentially expressed genes (DEGs) using DESeq2 (p-value <0.05 & |log2Fold Change| > 0.5)
- Overlap DEGs with curated ubiquitination-related genes (UbLGs) from GeneCards (score ≥3)
Biomarker Identification:
- Perform univariate Cox regression analysis on crossover genes (p < 0.05)
- Apply LASSO Cox regression for feature selection and biomarker identification
- Validate biomarkers in independent cohorts using Kaplan-Meier survival analysis and ROC curves
Model Construction and Validation:
- Calculate risk score: risk score = Σ(coef(genei) * expression(genei))
- Stratify patients into high-risk and low-risk groups based on optimal threshold
- Evaluate model performance using C-index and time-dependent ROC analysis
- Conduct immune infiltration analysis to correlate risk scores with tumor microenvironment features
This approach successfully identified a 5-gene ubiquitination signature (MMP1, RNF2, TFRC, SPP1, and CXCL8) predictive of cervical cancer outcomes, demonstrating the clinical potential of UbLG-based biomarkers [87].
Diagram 1: UPS in DDR and targeted therapy. The ubiquitin signaling cascade is activated by DNA damage, leading to substrate modification and specific cellular outcomes. UPS-targeted therapies can exploit synthetic lethal relationships in this pathway.
Analytical Validation and Verification Frameworks
Antibody and Reagent Validation
Robust biomarker assays require rigorous validation of core reagents, particularly antibodies for ubiquitination detection. Key considerations include:
- Genetic Validation: Use knockout or knockdown cells to confirm target specificity
- Affinity Measurements: Quantitative determination of binding kinetics for critical reagents
- Cross-reactivity Profiling: Assessment against related targets (e.g., different ubiquitin chain types)
- Lot-to-Lot Consistency: Monitoring performance across multiple production batches
Recombinant antibodies offer significant advantages for biomarker assays due to their precise epitope targeting, minimal variability, and sustainable production [89]. For ubiquitination-specific detection, antibodies must distinguish between ubiquitin chain topologies (K48, K63, monoubiquitination) with high specificity, as different chain architectures dictate distinct functional outcomes in DDR [86].
PCR Chip Technologies for Biomarker Analysis
Microfluidic PCR chips enable highly sensitive biomarker detection with applications in UPS-targeted therapy monitoring:
Technology Overview [90]:
- Platform: Microfluidic devices with nanoliter-volume reaction chambers
- Detection Methods: Real-time quantitative PCR, digital PCR, multiplex PCR
- Applications: Rare mutation detection, absolute quantification, multiplex biomarker analysis
- Advantages: High sensitivity, reduced reagent consumption, rapid thermal cycling
Protocol: PCR Chip-Based Biomarker Validation:
- Sample Preparation: Extract nucleic acids from patient samples (tissue, blood, liquid biopsy)
- Chip Priming: Load samples into microfluidic chambers via capillary action or pressure
- Amplification: Perform thermal cycling with integrated microheaters (30-40 cycles)
- Detection: Monitor fluorescence in real-time or endpoint readout
- Analysis: Quantify target abundance using standard curves (qPCR) or Poisson statistics (dPCR)
PCR chips are particularly valuable for detecting low-abundance biomarkers such as rare mutations in UPS components or circulating tumor DNA with ubiquitination-related gene alterations [90].
The Scientist's Toolkit: Essential Research Reagent Solutions
Table 3: Key Research Reagents for UPS Biomarker Development
| Reagent Category | Specific Examples | Research Application | Technical Considerations |
|---|---|---|---|
| CRISPR Screening Libraries | SPIDR dual-sgRNA library [88] | Systematic genetic interaction mapping | Coverage of DDR genes; paired sgRNA design |
| Ubiquitination-Specific Antibodies | K48-linkage specific, K63-linkage specific, monoubiquitin antibodies | Detection of specific ubiquitin chain types | Chain topology specificity; application validation |
| PCR Chip Platforms | Digital PCR chips, multiplex PCR chips [90] | Sensitive nucleic acid biomarker detection | Chamber density; optical compatibility; throughput |
| Recombinant Antibodies | Recombinant validated antibodies [89] | Consistent biomarker detection in IHC/ELISA | Epitope mapping; lot-to-lot consistency |
| Targeted Metabolomics Kits | Biocrates Quant 500 MxP kit [91] | Quantitative metabolite profiling | Coverage of ubiquitination-related metabolites |
| Proteasome Activity Assays | Fluorogenic substrate panels | UPS functional assessment | Substrate specificity; inhibition controls |
Machine Learning Approaches for Biomarker Integration
Machine learning (ML) algorithms provide powerful tools for integrating multi-omics data to identify biomarkers for UPS-targeted therapy response. Key applications include:
- Feature Selection: Algorithms like Boruta, SVM-RFE, and LASSO identify relevant biomarkers from high-dimensional data [92] [93]
- Classification Models: Random Forest, XGBoost, and SVM classify patients into response categories [93]
- Survival Analysis: Cox proportional hazards models with regularization identify prognostic biomarkers [87]
Implementation Workflow:
- Data Preprocessing: Normalize multi-omics data (genomics, transcriptomics, proteomics)
- Feature Selection: Apply LASSO or SVM-RFE to identify most predictive features
- Model Training: Optimize hyperparameters via Bayesian optimization or Grid Search
- Validation: Evaluate performance using nested cross-validation and independent cohorts
ML approaches are particularly valuable for addressing the contextual duality of UPS components by modeling complex interactions between tumor genetics, UPS alterations, and therapeutic vulnerabilities [86].
Diagram 2: Biomarker development and validation. The workflow integrates multi-omics data through machine learning to develop biomarker signatures, followed by rigorous analytical and clinical validation before application.
Clinical Translation and Therapeutic Integration
The successful translation of UPS-focused biomarkers requires careful consideration of clinical implementation pathways:
- Companion Diagnostic Development: Co-development with UPS-targeted therapeutic agents
- Clinical Trial Design: Enrichment strategies using predictive biomarkers
- Regulatory Considerations: Analytical validity, clinical validity, and clinical utility demonstration
Biomarker-guided therapeutic strategies are particularly promising for ubiquitin-targeting agents. For example, EGFR-directed PROTACs selectively degrade β-TrCP substrates in EGFR-dependent tumors (e.g., lung and head/neck squamous cell carcinomas), suppressing DNA repair while minimizing impact on normal tissues [86]. Biomarkers that identify tumors dependent on specific UPS components can significantly enhance the therapeutic index of these targeted approaches.
The integration of UPS biomarkers with other DDR deficiencies creates opportunities for synthetic lethal therapeutic strategies. The comprehensive genetic interaction map generated by SPIDR screening identified numerous therapeutically exploitable synthetic lethal relationships, such as between ERCC2 mutations and DNA-PKcs inhibition in bladder cancer [88]. Such relationships provide a robust foundation for biomarker-driven clinical trial designs in precision oncology.
Biomarker development for UPS-targeted therapy represents a rapidly advancing frontier in precision oncology. The complex regulatory networks governed by ubiquitination in DNA damage response provide both challenges and opportunities for biomarker discovery. Success in this field requires integrating multiple approaches—from systematic genetic interaction mapping and multi-omics profiling to machine learning and rigorous clinical validation. As UPS-targeted therapies continue to evolve, particularly with the emergence of PROTACs and other degradation-based modalities, robust biomarkers will be essential for identifying patients most likely to benefit from these innovative treatments. The frameworks and methodologies outlined in this technical guide provide a foundation for advancing biomarker development in this critical area of cancer therapeutics.
The ubiquitin-proteasome system (UPS) is a master regulator of cellular protein homeostasis, controlling the stability, activity, and localization of a vast array of proteins critical to cancer cell survival and therapy resistance [94]. This system employs a cascade of enzymes—E1 (activating), E2 (conjugating), and E3 (ligating)—to tag proteins with ubiquitin chains, with different chain topologies dictating distinct functional outcomes [94] [95]. The UPS has emerged as a pivotal mediator of tumor responses to conventional and novel anticancer therapies. Within the context of DNA damage response (DDR) in cancer research, ubiquitination plays an indispensable role in orchestrating the complex network of signaling and repair pathways that determine cell fate following genotoxic insult from radiation or chemotherapy [96] [97]. More recently, the strategic manipulation of ubiquitin signaling has revealed promising opportunities to overcome resistance mechanisms and enhance therapeutic efficacy across multiple treatment modalities.
Radiotherapy and many chemotherapeutic agents exert their cytotoxic effects primarily through direct and indirect DNA damage [86] [96]. The subsequent DDR, while essential for genomic integrity in normal cells, represents a major mechanism of therapy resistance in malignancies [97]. The ubiquitin system regulates every facet of this response, from initial damage sensing and cell cycle checkpoint activation to repair pathway choice and execution, apoptosis, and immune activation [86] [98]. Furthermore, cancer cells exploit the plasticity of ubiquitin signaling to rewire metabolic pathways, evade immune surveillance, and acquire stem-like properties that foster treatment resistance [86] [99]. This mechanistic understanding has positioned the UPS as an attractive therapeutic target for combination strategies aimed at synthetically sensitizing tumors to established cancer treatments.
Biological Rationale for Combination Approaches
Ubiquitin-Mediated Regulation of DNA Damage Response
The ubiquitin system regulates all major DNA repair pathways through precise spatiotemporal control of key DDR components. Following radiation-induced double-strand breaks, the sequential action of E3 ligases RNF8 and RNF168 orchestrates the accumulation of repair proteins at damage sites through histone ubiquitination [96] [98]. The chain topology of ubiquitin modifications critically determines repair pathway choice and efficiency. For instance, K63-linked ubiquitin chains, such as those deposited by FBXW7 on XRCC4, enhance the accuracy of non-homologous end joining (NHEJ) [86] [98], while K48-linked chains typically target proteins for proteasomal degradation, as exemplified by FBXW7-mediated degradation of p53 in colorectal cancer models, promoting radioresistance [86]. Monoubiquitination events, including UBE2T/RNF8-mediated H2AX monoubiquitylation, accelerate damage detection in hepatocellular carcinoma [98]. These ubiquitin-dependent processes create therapeutic vulnerabilities exploitable through combination regimens.
Ubiquitin-Dependent Immune Evasion Mechanisms
Tumor cells manipulate ubiquitin signaling to suppress antitumor immunity through multiple mechanisms. A key pathway involves the regulation of PD-L1 stability, where the E3 ligase SPOP normally promotes PD-L1 ubiquitination and degradation [100]. However, cancer cells often upregulate competitive binders like ALDH2 or SGLT2 that shield PD-L1 from SPOP-mediated degradation, resulting in increased PD-L1 surface expression and T-cell suppression [100]. Additionally, TRIM21 utilizes K48-linked ubiquitination to degrade VDAC2 in nasopharyngeal carcinoma, suppressing mitochondrial DNA release and cGAS/STING-mediated immune activation [86] [98]. Conversely, deubiquitinases (DUBs) such as USP7 can stabilize inhibitory immune checkpoints, while USP14 inhibition leads to accumulation of K63-ubiquitinated IRF3, triggering STING-dependent antitumor immunity [98]. These mechanisms provide a strong rationale for combining ubiquitin-targeting agents with immunotherapy.
Strategic Combination Modalities
Ubiquitin-Targeting Agents with Radiotherapy
Table 1: Selected Ubiquitin-Targeting Agents in Combination with Radiotherapy
| Target | Agent Type | Combination Rationale | Cancer Models | Key Effects |
|---|---|---|---|---|
| E3 Ligases (General) | PROTACs | Degrade radioresistance mediators | Breast, Lung, HNSCC | Suppress DNA repair, enhance tumor-specific targeting [86] |
| β-TrCP | EGFR-directed PROTAC | Selective degradation in EGFR-dependent tumors | Lung cancer, HNSCC | Suppress DNA repair, minimize normal tissue effects [86] |
| BRD4/2 | RT-PROTAC (X-ray activated) | Tumor-localized activation | Breast cancer | Synergistic tumor growth inhibition [86] [98] |
| USP14 | Small molecule inhibitors | Disrupt NHEJ, promote HR, stabilize K63-IRF3 | Glioma, NSCLC | Impair DNA repair, activate STING immunity [86] [98] |
| FBXW7 | Context-dependent modulation | p53 status determines therapeutic outcome | Colorectal cancer (p53-wt), NSCLC (p53-null) | p53-wt: radiosensitization; p53-null: radioresistance [86] |
Radiotherapy remains a cornerstone for solid tumor treatment, but its efficacy is often limited by radioresistance mechanisms orchestrated through the ubiquitin system [86] [98]. Innovative combination approaches leverage the dynamic reversibility and chain topology diversity of ubiquitin signaling to disrupt these resistance networks. PROTACs (Proteolysis-Targeting Chimeras) represent a particularly promising class of ubiquitin-targeting agents that exploit endogenous E3 ligases to degrade specific target proteins [86] [94]. These heterobifunctional molecules simultaneously bind to a target protein and an E3 ubiquitin ligase, leading to polyubiquitination and subsequent proteasomal degradation of the target [86]. The specificity of PROTACs enables precise disruption of radioresistance drivers while potentially sparing normal tissues.
Emerging platforms are further enhancing the therapeutic index of ubiquitin-targeting radiosensitizers. Radiation-responsive PROTAC (RT-PROTAC) prodrugs are activated specifically by tumor-localized X-rays, enabling spatial control of protein degradation [86]. Similarly, X-ray-responsive nanomicelles (e.g., diselenide-bridged RCNprotac) selectively release PROTACs within irradiated tumors, as demonstrated with MZ1 targeting BRD4 in breast cancer models [86] [98]. Beyond PROTACs, inhibitors targeting context-specific E3 ligases and DUBs show significant potential. For instance, USP14 inhibition disrupts error-prone NHEJ repair while promoting error-free homologous recombination in NSCLC models, and concurrently activates STING-dependent antitumor immunity through K63-ubiquitinated IRF3 accumulation [86] [98].
Ubiquitin-Targeting Agents with Chemotherapy
Table 2: Ubiquitin-Targeting Agents in Combination with Chemotherapy
| Target | Agent Type | Chemotherapy Partner | Cancer Models | Key Effects |
|---|---|---|---|---|
| Proteasome | Bortezomib, Carfizomib, Ixazomib | Diverse chemotherapeutics | Multiple Myeloma, Mantle Cell Lymphoma | FDA-approved combinations, disrupt protein homeostasis [94] [101] |
| USP1 | Small molecule inhibitors | Platinum-based drugs | BRCA-mutant models | Enhance synthetic lethality, overcome resistance [97] |
| USP7 | Small molecule inhibitors | DNA-damaging agents | Prostate cancer, NSCLC | Stabilize p53, enhance apoptosis [101] |
| E3 Ligase Complexes | Monofunctional degraders | Standard chemotherapy | Various solid tumors | Degrade specific oncoproteins and resistance factors [17] |
The combination of ubiquitin-targeting agents with chemotherapy builds upon the established success of proteasome inhibitors in hematological malignancies and expands into novel mechanisms targeting specific E3 ligases and DUBs [94] [101]. Proteasome inhibitors like bortezomib, carfizomib, and ixazomib are now first-line therapies for multiple myeloma, where they disrupt the degradation of pro-apoptotic proteins and cell cycle regulators, sensitizing cancer cells to conventional chemotherapeutics [94]. The efficacy of these combinations stems from the critical role of the UPS in maintaining protein homeostasis and eliminating damaged proteins generated by chemotherapeutic insult.
Beyond broad proteasome inhibition, targeted approaches against specific DUBs and E3 ligases offer enhanced specificity. USP1 inhibition shows promise in combination with platinum-based chemotherapy, particularly in BRCA-deficient models, by interfering with DNA damage tolerance and repair pathways [97]. Similarly, USP7 inhibitors stabilize the tumor suppressor p53 and its transcriptional targets, enhancing apoptosis in response to DNA-damaging chemotherapeutics [101]. The functional diversity of E3 ligases, which numbers over 600 in humans, enables highly specific targeting of individual oncoproteins and resistance mechanisms through monofunctional degraders that exploit endogenous E3 activity without the heterobifunctional structure of PROTACs [17] [95].
Ubiquitin-Targeting Agents with Immunotherapy
The intersection of ubiquitin signaling and immune regulation represents a fertile ground for combination strategies with immune checkpoint inhibitors [99] [100]. The PD-1/PD-L1 axis is extensively regulated by ubiquitin-mediated degradation, with multiple E3 ligases and DUBs controlling the stability and surface expression of these immune checkpoints. The E3 ligase SPOP normally promotes PD-L1 ubiquitination and degradation, but this tumor-suppressive function is often circumvented in cancer through multiple mechanisms [100]. Competitive binding by proteins like ALDH2 in colorectal cancer or BCLAF1 in hepatocellular carcinoma prevents SPOP from accessing PD-L1, leading to its stabilization and immune suppression [100]. Similarly, the small molecule canagliflozin, originally developed as an SGLT2 inhibitor, was found to disrupt the SGLT2-PD-L1 interaction, freeing PD-L1 for SPOP-mediated degradation and enhancing T-cell cytotoxicity [100].
Additional ubiquitin-related targets offer complementary approaches to enhance immunotherapy. The WNT/β-catenin pathway, frequently hyperactivated in immunotherapy-resistant tumors, is regulated by multiple E3 ligases including FBXW7, which targets CHD4 for degradation, suppressing WNT signaling in triple-negative breast cancer [99]. Similarly, USP10 stabilizes MOF in esophageal squamous cell carcinoma, activating WNT/β-catenin signaling, while USP4 promotes β-catenin stability and nuclear localization [99]. Targeting these regulators can potentially reverse the immune-excluded phenotypes associated with WNT pathway activation. Furthermore, the interferon signaling pathway, crucial for antitumor immunity, is regulated by ubiquitin-dependent mechanisms, with ISG12a promoting β-catenin degradation through stabilization of the Axin destruction complex [99].
Experimental Methodologies and Research Tools
Key Research Reagent Solutions
Table 3: Essential Research Reagents for Investigating Ubiquitin-Based Combinations
| Reagent Category | Specific Examples | Research Application | Key Functions |
|---|---|---|---|
| E3 Ligase Modulators | PROTACs (e.g., MZ1, EGFR-directed PROTACs), Small molecule inhibitors (e.g., TRIM21 inhibitors) | Target validation, mechanism studies | Induce targeted protein degradation or functional inhibition [86] [98] |
| DUB Inhibitors | HBX 41,108 (USP7 inhibitor), PR957 (immunoproteasome inhibitor), USP14 inhibitors | Functional screening, therapeutic testing | Block deubiquitination, enhance degradation of target proteins [101] |
| Ubiquitin Chain-Specific Tools | K48- and K63-linkage specific antibodies, Ubiquitin mutants (K48R, K63R) | Mechanistic studies, signaling analysis | Detect specific chain topologies, dissect chain-specific functions [86] [95] |
| Proteasome Inhibitors | Bortezomib, Carfizomib, MG132 | Control experiments, combination studies | Block protein degradation, induce ER stress, activate apoptosis [94] [101] |
| Radiation-Responsive Platforms | RT-PROTAC prodrugs, X-ray-responsive nanomicelles (e.g., RCNprotac) | Spatiotemporally controlled activation | Enable tumor-localized protein degradation [86] |
Essential Experimental Workflows
The investigation of ubiquitin-targeting combination therapies requires specialized methodologies that capture the complexity of ubiquitin signaling and its therapeutic manipulation. For DNA damage-focused studies, standardized assays for quantifying DNA repair capacity are essential, including γH2AX foci formation as a marker of double-strand breaks, comet assays to measure DNA damage, and RAD51 foci formation to assess homologous recombination proficiency [96] [97]. These should be complemented with colony formation assays to measure clonogenic survival following combination treatment, providing a comprehensive view of DNA repair inhibition and radiosensitization/chemosensitization [86].
For immune-focused combinations, flow cytometric analysis of immune cell populations and surface PD-L1 expression is fundamental, supplemented with co-culture assays measuring T-cell-mediated tumor cell killing [99] [100]. To dissect the underlying molecular mechanisms, techniques such as ubiquitin pulldown followed by mass spectrometry identifies changes in the ubiquitinome, while immunoprecipitation and immunoblotting with linkage-specific ubiquitin antibodies reveal chain topology alterations [86] [98]. CRISPR-based functional screens can identify novel synthetic lethal interactions between ubiquitin system components and therapeutic agents [86] [97].
Diagram 1: Mechanism of Action for Ubiquitin-Targeting Combination Therapies. This diagram illustrates the convergent pathways through which ubiquitin-targeting agents synergize with conventional cancer therapies. DNA damage from radiation or chemotherapy combines with ubiquitin system manipulation to produce enhanced therapeutic effects through multiple synergistic mechanisms.
Clinical Translation and Future Directions
The clinical translation of ubiquitin-targeting combination therapies faces several challenges, including functional redundancy within the ubiquitin system, on-target toxicity to normal tissues, and adaptive resistance mechanisms [86] [101]. However, strategic approaches are emerging to address these limitations. Biomarker-guided patient selection is critical for maximizing therapeutic efficacy, as exemplified by the context-dependent functions of E3 ligases like FBXW7, which can exert either pro-tumorigenic or tumor-suppressive effects depending on p53 status and cellular background [86] [17]. The development of predictive biomarkers, such as TRIM26-mediated GPX4 K63 ubiquitination as a biomarker for ferroptosis inducers, will enable more precise patient stratification [86].
Future innovation will likely focus on several key areas. First, the expansion of targeted protein degradation technologies beyond PROTACs, including molecular glues and lysosome-targeting chimeras (LYTACs), offers new modalities for targeting previously "undruggable" proteins [94]. Second, the development of tissue-specific and temporally controlled ubiquitin-targeting agents, such as radiation-activated prodrugs, may enhance therapeutic indices by limiting activity to tumor microenvironments [86] [98]. Finally, the integration of ubiquitin-targeting strategies with emerging therapeutic modalities, including cellular therapies and epigenetic modulators, represents a promising frontier for overcoming resistance mechanisms and expanding the reach of cancer therapy.
The dynamic reversibility of ubiquitin modifications, the vast diversity of E3 ligases with their precise substrate specificities, and the growing arsenal of ubiquitin-targeting technologies collectively position the ubiquitin system as a central therapeutic node in the next generation of cancer combination therapies. As our understanding of the intricate ubiquitin networks governing therapy response continues to deepen, so too will our ability to strategically manipulate this system to overcome treatment resistance and improve outcomes across the spectrum of human malignancies.
Connecting the Dots: Validating Ubiquitination's Role in Cancer Hallmarks and Comparative Therapeutics
The ubiquitin system, a crucial post-translational regulatory mechanism, has emerged as a pivotal integrator of two fundamental cancer hallmarks: defective DNA damage response (DDR) and metabolic reprogramming. This whitepaper examines the RNF20-HIF1α axis as a paradigmatic model of this integration, detailing the molecular mechanisms through which ubiquitination links genomic instability to metabolic adaptations in cancer cells. We present quantitative data from key studies, experimental protocols for investigating this axis, and visualizations of the underlying signaling networks. Furthermore, we provide a comprehensive toolkit of research reagents to facilitate continued investigation into this critical pathway, which offers promising therapeutic vulnerabilities for cancer treatment, particularly in tumors with DDR deficiencies.
The ubiquitin-proteasome system (UPS) orchestrates a vast array of cellular processes through spatiotemporal control of protein stability, localization, and interaction networks. In the context of cancer, ubiquitination has been extensively studied in individual pathways, but its role as an integrator between different hallmarks of cancer remains an emerging frontier [98]. Particularly, the molecular crosstalk between genomic instability driven by DDR defects and the metabolic rewiring that supports rapid tumor growth represents a critical interface that is largely mediated by ubiquitin-related signaling.
The RNF20-HIF1α axis exemplifies this integration, demonstrating how defects in a chromatin-associated E3 ubiquitin ligase can simultaneously impair DNA repair mechanisms and drive pro-tumorigenic metabolic adaptations [102] [103]. This whitepaper synthesizes current mechanistic understanding of this pathway, presents key experimental data, and provides methodological resources to advance research in this area, framed within the broader context of ubiquitination in DNA damage response cancer research.
Molecular Mechanisms of the RNF20-HIF1α Axis
RNF20 in DNA Damage Response and Tumor Suppression
RNF20, in complex with RNF40, functions as the major E3 ubiquitin ligase responsible for monoubiquitination of histone H2B (H2Bub1) in mammalian cells [103]. This histone modification plays dual roles in maintaining genomic stability: facilitating transcriptional elongation through nucleosome destabilization, and promoting timely repair of DNA double-strand breaks (DSBs) at damage sites [103] [25].
Key tumor-suppressive functions of RNF20 include:
- Haploinsufficiency-driven tumorigenesis: Ablation of a single Rnf20 allele significantly increases spontaneous lung tumor incidence in mice (24 of 32 heterozygous mice versus 1 of 20 wild-type littermates) [103].
- DNA repair defects: Rnf20 haploinsufficiency results in increased γH2AX foci (marker of DSBs) and pronounced defects in DNA repair following oxidative stress [103].
- p53 pathway activation: RNF20-H2Bub1 enables adequate tumor suppression via the p53 axis, with haploinsufficiency leading to inadequate p53-mediated control [103].
The clinical relevance is underscored by findings that decreased RNF20 levels correlate with poor survival in lung adenocarcinoma patients and are frequently observed in high-grade adenocarcinomas and small cell lung carcinomas [103].
Metabolic Reprogramming Through HIF1α Stabilization
The connection between RNF20 deficiency and metabolic reprogramming centers on HIF1α stabilization. Mechanistically, RNF20 controls Rbx1 expression, thereby regulating the activity of the VHL ubiquitin ligase complex that normally targets HIF1α for proteasomal degradation [102] [103]. Under RNF20-deficient conditions, this regulation is disrupted, leading to:
- HIF1α accumulation even under normoxic conditions
- Transcriptional activation of glycolytic genes
- Promoter-proximal pause release of RNA polymerase II at HIF1α target genes
- Metabolic rewiring toward aerobic glycolysis (Warburg effect) [103]
This RNF20-HIF1α metabolic axis operates independently of H2Bub1, indicating a non-canonical function of RNF20 in metabolic regulation [103].
Integrated Signaling Network
The diagram below illustrates the core signaling pathway of the RNF20-HIF1α axis:
Figure 1: RNF20-HIF1α Axis Core Signaling Pathway. This diagram illustrates the dual mechanisms by which RNF20 regulates both genomic stability (left, green) and metabolic programming (right, red). Under RNF20-deficient conditions, the protective functions on the left are diminished while the pathogenic outcomes on the right are enhanced.
Quantitative Experimental Evidence
Key Findings from Preclinical Models
Table 1: Quantitative Findings on RNF20-HIF1α Axis in Cancer Models
| Experimental System | Key Finding | Quantitative Measurement | Biological Impact | Reference |
|---|---|---|---|---|
| Rnf20+/- mouse model | Spontaneous lung tumor formation | 24/32 heterozygous vs 1/20 wild-type mice developed tumors | 56% showed SCLC features; 44% adenocarcinoma | [103] |
| Rnf20+/- MLE12 cells | DNA repair defects | Increased γH2AX foci without DNA-damaging agents | Pronounced repair defects after H2O2 treatment | [103] |
| Human lung adenocarcinoma | RNF20 correlation with survival | Lower RNF20 strongly correlated with poor survival | KMplotter analysis showing significant survival difference | [103] |
| HIF-1 recruitment complex | RNF20/40 requirement for transcription | FACT/RNF20/40 crucial for HIF-1 target gene expression | Mediates histone ubiquitination and transcriptional activation | [104] |
Therapeutic Intervention Data
Table 2: Experimental Therapeutic Approaches Targeting Related Ubiquitin Pathways
| Therapeutic Approach | Molecular Target | Experimental Outcome | Cancer Context | Reference |
|---|---|---|---|---|
| HIF1α inhibition | HIF1α transcriptional activity | Rescued increased growth and invasion from RNF20 deficiency | Proposed strategy for RNF20-low lung cancers | [103] |
| SMURF2 targeting | HIF1α stability | SMURF2 promotes HIF1α ubiquitination and degradation | Potential strategy across multiple cancer types | [105] |
| Glucose uptake inhibition | Metabolic reprogramming | Suppressed RNF20 deficiency-driven tumor growth | Targets downstream effect of HIF1α activation | [103] |
| USP14 inhibition | K63-ubiquitinated IRF3 | Accumulated K63-modified IRF3, triggering STING immunity | Glioblastoma and head/neck cancers | [98] |
Experimental Protocols and Methodologies
Establishing RNF20 Haploinsufficiency Models
CRISPR-Cas9 Gene Editing in Lung Epithelial Cells [103]:
- Design guide RNAs targeting early exons of RNF20 gene
- Transfect MLE12 mouse lung epithelial cells with CRISPR-Cas9 constructs
- Single-cell cloning and expansion of edited cells
- Genotype validation through sequencing and Western blotting
- Functional validation via H2Bub1 measurement by immunoblotting
Critical Note: Multiple studies have been unable to establish homozygous RNF20 deletion, suggesting essential cellular function and necessitating haploinsufficient models [103].
Assessing DNA Damage Response Defects
γH2AX Foci Formation and Repair Kinetics Assay [103]:
- Culture conditions: Plate isogenic control and RNF20-deficient cells on coverslips
- Damage induction: Treat with H2O2 (200 μM, 30 minutes) or ionizing radiation (2-5 Gy)
- Time-course fixation: At baseline, immediately post-treatment, and at 2, 6, and 24 hours recovery
- Immunofluorescence: Stain with anti-γH2AX antibody and appropriate fluorescent secondary
- Image acquisition: Capture minimum of 50 cells per condition using high-resolution microscopy
- Quantification: Automated counting of γH2AX foci per nucleus using ImageJ or similar software
Metabolic Reprogramming Assessment
Seahorse Metabolic Analysis Protocol:
- Cell preparation: Seed 20,000-40,000 cells per well in XF96 cell culture microplates
- Assay medium preparation: Use XF Base medium supplemented with 1mM pyruvate, 2mM glutamine, and 10mM glucose
- Drug preparation:
- Oligomycin (ATP synthase inhibitor): 1.5 μM final concentration
- FCCP (mitochondrial uncoupler): 1.0 μM final concentration
- Rotenone/Antimycin A (ETC inhibitors): 0.5 μM final concentration each
- Run program: Measure oxygen consumption rate (OCR) and extracellular acidification rate (ECAR) under basal conditions and after drug injections
- Data analysis: Normalize to protein content and calculate glycolytic and mitochondrial function parameters
Chromatin Immunoprecipitation for HIF1α Target Genes
ChIP-qPCR Protocol for HIF1α Binding [104]:
- Cross-linking: Treat cells with 1% formaldehyde for 10 minutes at room temperature
- Cell lysis: Prepare nuclei and sonicate chromatin to 200-500 bp fragments
- Immunoprecipitation: Incubate with HIF1α antibody or species-matched control IgG overnight at 4°C
- Bead capture: Use protein A/G magnetic beads for 2 hours at 4°C
- Washing and elution: Series of washes with low salt, high salt, LiCl buffers, followed by elution buffer
- Reverse cross-linking: Incubate at 65°C overnight with proteinase K
- DNA purification: Use spin columns or phenol-chloroform extraction
- qPCR analysis: Amplify known HIF1α target gene promoters (e.g., VEGF, GLUT1, LDHA)
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Research Reagents for Investigating the RNF20-HIF1α Axis
| Reagent Category | Specific Examples | Research Application | Key Function | Validation Source |
|---|---|---|---|---|
| Cell Line Models | Rnf20+/- MLE12 cells, A549 lung adenocarcinoma, BEAS-2B normal bronchial epithelium | Comparative studies of RNF20 function | Modeling haploinsufficiency in relevant tissue context | [103] |
| Antibodies | Anti-RNF20, Anti-H2Bub1 (Lys120), Anti-γH2AX (Ser139), Anti-HIF1α | Western blot, immunofluorescence, ChIP | Detecting protein expression, DNA damage, histone modifications | [103] [104] |
| Chemical Inhibitors | HIF1α inhibitors (e.g., PX-478), 2-DG (glucose uptake inhibitor), MG132 (proteasome inhibitor) | Functional intervention studies | Probing pathway dependencies and therapeutic vulnerabilities | [103] [98] |
| CRISPR Tools | RNF20-targeting gRNAs, non-targeting controls, Cas9 expression vectors | Genetic manipulation | Establishing isogenic cell lines with RNF20 modulation | [103] |
| qPCR Assays | HIF1α target genes (VEGF, GLUT1, LDHA, PDK1), DNA repair genes | Gene expression analysis | Quantifying transcriptional outputs of pathway activation | [103] [104] |
Extended Ubiquitin Network in DDR-Metabolism Crosstalk
Beyond the RNF20-HIF1α axis, multiple ubiquitin-related pathways interface with DDR and metabolic reprogramming:
SMURF2-HIF1α Regulatory Axis
SMURF2 represents a parallel ubiquitination pathway that regulates HIF1α stability. As an E3 ubiquitin ligase, SMURF2 targets HIF1α for ubiquitination and proteasomal degradation under both normoxic and hypoxic conditions [105]. This pathway introduces an additional layer of complexity to HIF1α regulation, with SMURF2 acting predominantly as a tumor suppressor in breast and renal cancers, while exhibiting context-dependent oncogenic functions in other malignancies [105].
Diverse Ubiquitin Chain Typologies in Radiation Resistance
Cancer cells exploit different ubiquitin chain topologies to drive radioresistance through both DDR and metabolic adaptation:
- K48-linked ubiquitination: Mediates proteasomal degradation of tumor suppressors (e.g., FBXW7-mediated p53 degradation in colorectal cancer) [98]
- K63-linked ubiquitination: Facilitates assembly of DNA repair complexes (e.g., FBXW7 modification of XRCC4 for NHEJ) and pro-survival signaling [98]
- Monoubiquitination: Regulates chromatin dynamics (H2Bub1 by RNF20/40) and non-histone protein function (FANCD2 in DNA crosslink repair) [98]
The diagram below illustrates the broader ubiquitin network connecting DDR to metabolic reprogramming:
Figure 2: Extended Ubiquitin Network in DDR and Metabolic Reprogramming. This diagram illustrates how different ubiquitin chain typologies (K48, K63, monoubiquitination) mediate crosstalk between DNA damage response pathways (green) and metabolic reprogramming (red), collectively contributing to therapeutic resistance (yellow).
The RNF20-HIF1α axis represents a prototypical example of ubiquitin-mediated integration between DNA damage response and metabolic reprogramming in cancer. This pathway demonstrates how deficiency in a chromatin-modifying E3 ligase can simultaneously drive genomic instability through impaired DNA repair and promote metabolic adaptations through HIF1α stabilization. The experimental evidence from preclinical models underscores the therapeutic potential of targeting this axis, particularly through HIF1α inhibition or metabolic interventions in RNF20-deficient tumors.
Future research directions should focus on:
- Developing more specific modulators of RNF20 activity
- Exploring combinatorial approaches targeting both DDR and metabolic vulnerabilities
- Investigating the context-dependent functions of related ubiquitin pathways (e.g., SMURF2-HIF1α)
- Validating these mechanisms in patient-derived organoids and clinical trial contexts
The intricate crosstalk between ubiquitin-regulated DDR and metabolic pathways presents both challenges and opportunities for cancer therapy, particularly in leveraging synthetic lethal approaches for tumors with specific ubiquitin pathway alterations.
E3 ubiquitin ligases represent a critical class of enzymes within the ubiquitin-proteasome system (UPS) that confer substrate specificity for protein ubiquitination, a fundamental post-translational modification regulating protein stability, localization, and activity [11]. These enzymes facilitate the transfer of ubiquitin from E2 conjugating enzymes to specific target proteins, determining their fate through proteasomal degradation or functional modulation [106] [1]. The human genome encodes over 600 E3 ligases, yet only a small fraction have been thoroughly characterized regarding their substrates, functions, and roles in disease pathogenesis [107] [108].
In the context of cancer biology, E3 ligases have emerged as pivotal regulators of DNA damage response (DDR) pathways, cell cycle progression, and apoptosis [8] [11]. Maintenance of genomic integrity is paramount for cell survival, and cells have evolved sophisticated DDR mechanisms to counteract constant genotoxic insults from both endogenous and exogenous sources [8]. When DNA damage occurs, E3 ligases coordinate the recruitment, activity, and turnover of DNA repair proteins through precise ubiquitination events, thereby orchestrating the appropriate cellular response to maintain genome stability [8] [1]. Dysregulation of these processes, through mutations or aberrant expression of E3 ligases or their substrates, can lead to uncontrolled proliferation, accumulation of DNA mutations, and ultimately cancer development [8] [109].
This review provides a comprehensive comparative analysis of major E3 ligases, with particular emphasis on their substrate profiles, associations with cancer, and druggability potential within the framework of DNA damage response and cancer therapeutics. By systematically evaluating these key aspects, we aim to highlight both current understanding and future directions for targeting E3 ligases in precision cancer medicine.
E3 Ligase Classification and Mechanisms
E3 ubiquitin ligases are classified into three primary structural families based on their domain architecture and mechanism of ubiquitin transfer: RING (Really Interesting New Gene), HECT (Homologous to E6-AP C-Terminus), and RBR (RING-Between-RING) types [106] [11].
RING-type E3 ligases represent the largest family and function primarily as scaffolds that directly facilitate the transfer of ubiquitin from E2 enzymes to substrate proteins without forming an intermediate thioester bond [11]. Notable examples include MDM2, BRCA1, and RNF168, which play critical roles in cell cycle regulation and DNA damage response [8] [109].
HECT-type E3 ligases, comprising 28 members in humans, form an obligate thioester intermediate with ubiquitin before transferring it to the substrate protein [106]. The NEDD4 family represents the largest subgroup within HECT-type E3s and includes NEDD4, NEDD4L, ITCH, WWP1, WWP2, SMURF1, SMURF2, NEDL1, and NEDL2 [106]. These enzymes typically contain C2 domains for membrane binding, WW domains for protein-protein interactions, and a catalytic HECT domain [106].
RBR-type E3 ligases employ a hybrid mechanism, combining aspects of both RING and HECT-type enzymes [11]. They feature two RING domains with a conserved cysteine residue in the second RING domain that forms a thioester intermediate with ubiquitin similar to HECT-type E3s [11]. Parkin represents a well-characterized example of this family.
The complexity of ubiquitin signaling is further enhanced by the ability of E3 ligases to generate diverse ubiquitin chain linkages (K6, K11, K27, K29, K33, K48, K63, and linear chains), each conferring distinct functional consequences for the modified substrate [1]. For instance, K48-linked chains typically target proteins for proteasomal degradation, while K63-linked chains often serve non-proteolytic functions in DNA repair and signaling pathways [1].
Table 1: Major E3 Ligase Families and Their Characteristics
| E3 Family | Mechanism of Action | Representative Members | Key Structural Domains |
|---|---|---|---|
| RING | Direct transfer from E2 to substrate; functions as scaffold | MDM2, BRCA1, RNF168, RNF4, TRAIP | RING domain (Zn²⁺-binding) |
| HECT | Forms thioester intermediate with ubiquitin before substrate transfer | NEDD4, NEDD4L, ITCH, SMURF2 | C2 domain, WW domains, HECT domain |
| RBR | Hybrid mechanism with RING and HECT-like features | Parkin, HOIP | RING1, IBR, RING2 domains |
Major E3 Ligases in DNA Damage Response and Cancer
RNF168
RNF168 is a RING-type E3 ligase critically involved in the DNA damage response, particularly in the repair of DNA double-strand breaks (DSBs) [8]. It functions downstream of RNF8 to amplify ubiquitin signaling at DNA damage sites, creating a platform for the recruitment of DNA repair proteins such as 53BP1 and BRCA1 [8]. RNF168 catalyzes the ubiquitylation of histones H2A and H2AX, forming K63-linked ubiquitin chains that serve as docking sites for various DNA repair factors [8] [1].
Inherited mutations in RNF168 are associated with human genetic disorders characterized by chromosomal instability, immunodeficiency, and increased cancer predisposition [8]. The precise regulation of RNF168 activity is essential for maintaining genome stability, as both loss-of-function and overexpression can lead to defective DNA repair and accumulation of genomic alterations that drive carcinogenesis [8].
BRCA1-BARD1
The BRCA1-BARD1 complex represents a heterodimeric RING-type E3 ligase that plays multifaceted roles in DNA damage response, particularly in homologous recombination (HR) repair of DNA double-strand breaks [8]. BRCA1 facilitates the recruitment of repair proteins to damage sites and promotes DNA end resection through its E3 ligase activity [8]. It also participates in the regulation of cell cycle checkpoints and centrosome duplication [8].
Germline mutations in BRCA1 are well-established drivers of hereditary breast and ovarian cancer syndromes, highlighting its critical function as a tumor suppressor [8]. The BRCA1-BARD1 complex primarily generates K6-linked ubiquitin chains, which have been implicated in DNA repair processes, though the complete repertoire of its substrates and their specific functions remain areas of active investigation [8].
NEDD4 Family E3 Ligases
The NEDD4 family of HECT-type E3 ligases comprises nine members that have emerged as important regulators of DNA damage response [106]. These enzymes share a common modular structure consisting of an N-terminal C2 domain, multiple WW domains for substrate recognition, and a C-terminal HECT catalytic domain [106].
NEDD4 (NEDD4-1), the prototypical family member, regulates the stability of various DDR proteins, including PTEN and components of the PP2A complex, thereby influencing cell survival and apoptosis following DNA damage [106]. NEDD4L (NEDD4-2) participates in the regulation of cell cycle checkpoints and has been shown to ubiquitylate Ku70 and Ku80, central components of the non-homologous end joining (NHEJ) pathway [106].
ITCH, another NEDD4 family member, controls the stability of key DDR regulators such as p73 and TXNIP, while WWP1 modulates the activities of ATM and p53 in response to genotoxic stress [106]. SMURF2 has been implicated in the regulation of RNF20 stability and topological organization of chromatin, influencing DNA accessibility for repair machinery [106].
Dysregulation of NEDD4 family members has been documented in various cancers, with context-dependent roles as either oncogenes or tumor suppressors [106]. For instance, NEDD4 is frequently overexpressed in lung and prostate cancers, promoting the degradation of tumor suppressors like PTEN, while NEDD4L exhibits both oncogenic and tumor suppressive functions depending on cellular context [109] [106].
Table 2: Cancer-Associated E3 Ligases and Their Roles in DNA Damage Response
| E3 Ligase | Family | Key Substrates in DDR | Cancer Associations | Therapeutic Targeting |
|---|---|---|---|---|
| RNF168 | RING | Histones H2A/H2AX, 53BP1 | Genetic disorders with cancer predisposition; regulates DSB repair | Under investigation |
| BRCA1 | RING | Unknown (generates K6-linked chains) | Hereditary breast and ovarian cancer; tumor suppressor | PARP inhibitor sensitivity |
| NEDD4 | HECT | PTEN, PP2A components | Overexpressed in lung, prostate cancer; regulates cell survival | Preclinical development |
| MDM2 | RING | p53, itself | Amplified in various cancers; negative regulator of p53 | Nutlin-3a, RG7112 (clinical) |
| TRAIP | RING | Components of replication fork | Mutated in various cancers; regulates replication stress | Under investigation |
| HUWE1 | HECT | MCL1, p53 | Dysregulated in cancer; regulates apoptosis and DNA repair | Preclinical development |
Experimental Approaches for E3 Ligase Research
Substrate Identification Methods
Identifying physiological substrates of E3 ligases remains a significant challenge in the field. Traditional biochemical methods, including yeast two-hybrid screening, co-immunoprecipitation coupled with mass spectrometry, and ubiquitination assays, have identified numerous E3-substrate interactions but are often resource-intensive and may miss transient interactions [110].
Recently, novel approaches have emerged to address these limitations. E3-Substrate Tagging by Ubiquitin Biotinylation (E-STUB) represents a proximity-dependent labeling method that specifically biotinylates ubiquitylated substrates in close proximity to an E3 ligase of interest, enabling their subsequent identification and characterization [111]. This technique has proven valuable for mapping both direct and collateral targets of E3 ligases, including those modified by PROTACs and molecular glues [111].
Computational approaches have also advanced significantly. DeepUSI is a deep learning-based framework that predicts E3-substrate interactions (ESIs) using protein sequence information [110]. This method employs convolutional neural networks (CNNs) trained on comprehensive datasets of experimentally validated ESIs to identify potential substrates across the human proteome [110]. When applied to cancer-associated E3 and deubiquitinating enzyme (DUB) genes, DeepUSI successfully identified druggable substrates with functional implications, providing valuable insights for therapeutic development [110].
Binding Affinity Assessment
Evaluating the interaction between E3 ligases and their ligands is crucial for drug discovery efforts. Cellular target engagement assays combined with in-cell ELISA provide a robust protocol for determining the binding affinity of ligands toward E3 ubiquitin ligases like CRBN [112]. This approach offers several advantages, including ease of establishment, relatively low cost, rapid time frame, and applicability to various E3 ligase systems with appropriate modifications [112].
The protocol involves treating cells with E3 ligands, followed by cell fixation, permeabilization, and incubation with antibodies against the E3 ligase of interest [112]. The signal quantification provides a measure of cellular target engagement, enabling ranking of compound affinity and facilitating the development of potent E3 ligands for PROTAC design [112].
Diagram 1: Experimental Workflow for E3 Ligase Research. This diagram outlines the integrated approaches for studying E3 ligases, from substrate identification to therapeutic development.
Druggability of E3 Ligases and Therapeutic Applications
Expanding the PROTACtable E3 Ligase Landscape
PROteolysis-TArgeting Chimeras (PROTACs) represent a groundbreaking therapeutic modality that hijacks the ubiquitin-proteasome system to selectively degrade disease-causing proteins [107] [108]. These bifunctional molecules consist of two ligands connected by a linker: one binding to an E3 ubiquitin ligase and the other to a protein of interest (POI), facilitating the formation of a ternary complex that leads to POI ubiquitination and degradation [107].
Despite the existence of over 600 E3 ligases in the human genome, current PROTAC development heavily relies on only a handful, predominantly Cereblon (CRBN) and Von Hippel-Lindau (VHL), which together account for the majority of PROTACs in clinical and preclinical development [107] [108]. This limited repertoire poses several challenges, including potential resistance mechanisms through E3 ligase mutations and restricted tissue specificity [107].
Systematic characterization of E3 ligases across multiple dimensions—including chemical ligandability, expression patterns, protein-protein interactions, structural features, functional essentiality, and cellular localization—has identified numerous underutilized E3 ligases with high potential for PROTAC development [107]. Analysis of 1,075 unique E3 ligases revealed that 686 (63.8%) interact with known ligands, suggesting substantial opportunities for expanding the PROTACtable E3 ligase landscape [107]. Notably, 275 E3 ligases (25.6%) received high confidence scores (5 or 6) based on available functional and substrate information, comparable to currently utilized E3s like VHL and CRBN [107].
Promising candidates for future PROTAC development include RNF4, HUWE1, and FBXO7, which have well-documented roles in the ubiquitin-proteasome system and numerous known substrate interactions [107]. Additionally, members of the CUL2 complex, such as KLHDC2, and N-degron pathway ligases represent novel avenues for therapeutic exploration [108].
Diagram 2: Mechanism of PROTAC-induced Protein Degradation. This diagram illustrates how PROTAC molecules facilitate the ubiquitination and degradation of target proteins by recruiting E3 ubiquitin ligases.
Clinically Targeted E3 Ligases
MDM2, a key negative regulator of the tumor suppressor p53, represents one of the most extensively targeted E3 ligases for cancer therapy [109]. Nutlin-3a was the first small-molecule inhibitor developed to disrupt the MDM2-p53 interaction, stabilizing p53 and activating its tumor-suppressive functions in cancers with wild-type p53 [109]. Subsequent derivatives, including RG7112 and RG7388, have demonstrated enhanced potency and are under clinical evaluation [109]. Alternative MDM2 inhibitors like RITA and PRIMA1 employ distinct mechanisms of action, further expanding the therapeutic arsenal against this important E3 ligase [109].
Cereblon (CRBN) modulators, particularly immunomodulatory imide drugs (IMiDs) such as thalidomide, lenalidomide, and pomalidomide, represent another class of successful E3-targeting therapeutics [108]. These compounds function as molecular glues that redirect CRBN E3 ligase activity toward novel substrates, including transcription factors IKFZ1 and IKFZ3, leading to their degradation and exerting therapeutic effects in hematological malignancies [108].
Emerging strategies focus on developing tissue-specific or tumor-selective degraders by exploiting the differential expression patterns of E3 ligases [107]. For instance, DT2216, a PROTAC targeting BCL-XL, leverages the poor expression of VHL in platelets to minimize thrombocytopenia, a dose-limiting side effect of conventional BCL-XL inhibitors [107].
Table 3: Clinically Advanced E3-Targeting Therapeutics
| E3 Ligase | Therapeutic Agent | Mechanism | Development Stage | Key Applications |
|---|---|---|---|---|
| MDM2 | Nutlin-3a | Disrupts MDM2-p53 interaction; stabilizes p53 | Preclinical/Research | Cancers with wild-type p53 |
| MDM2 | RG7112, RG7388 | Second-generation MDM2 inhibitors with improved potency | Clinical trials | Solid tumors, hematologic malignancies |
| CRBN | Thalidomide, Lenalidomide | Molecular glue degraders of IKFZ1/IKFZ3 | FDA-approved | Multiple myeloma, MDS |
| CRBN | CC-90009 (CELMoD) | Targeted degradation of GSPT1 | Clinical trials | Acute myeloid leukemia |
| VHL | Various PROTACs | Recruitment for targeted protein degradation | Clinical/preclinical | Multiple cancer types |
The Scientist's Toolkit: Essential Research Reagents and Methodologies
Advancing E3 ligase research requires specialized reagents and methodologies tailored to the unique challenges of studying ubiquitination and protein degradation. The following toolkit summarizes key resources for experimental investigations:
Table 4: Essential Research Reagents for E3 Ligase Studies
| Research Tool | Function/Application | Key Features | Examples/References |
|---|---|---|---|
| E-STUB | Proximity-dependent labeling of E3 substrates | Identifies direct and collateral ubiquitylation targets; applicable to PROTAC characterization | [111] |
| DeepUSI | Computational prediction of E3-substrate interactions | Deep learning framework using protein sequences; identifies druggable substrates | [110] |
| Cellular Target Engagement Assay | Measures binding affinity of E3 ligands | In-cell ELISA format; modifiable for different E3 systems | [112] |
| Ubiquitination Assays | Direct detection of substrate ubiquitylation | In vitro and in vivo systems; uses specific linkage antibodies | [8] [1] |
| PROTAC Design Platforms | Development of targeted protein degraders | Incorporates E3 ligase binders with target protein ligands | [107] [108] |
| E3 Ligase Profiling Resources | Comprehensive characterization of E3 ligases | Assesses ligandability, expression, PPIs, and cellular localization | E3 Atlas [107] |
The comparative analysis of major E3 ligases presented herein underscores their critical roles in maintaining genome stability through DNA damage response pathways and their profound implications in cancer pathogenesis. The substrate specificity, diverse mechanisms of action, and tissue-selective expression patterns of different E3 ligase families offer unique opportunities for therapeutic intervention.
Future research directions should prioritize the expansion of the PROTACtable E3 ligase landscape beyond the currently limited repertoire of CRBN and VHL. Systematic characterization of underutilized E3 ligases, as facilitated by resources like E3 Atlas, will enable the development of degraders with improved tissue specificity, reduced susceptibility to resistance mechanisms, and enhanced capacity to target previously undruggable proteins [107]. Additionally, advancing our understanding of context-dependent E3-substrate interactions, particularly in different tissue types and disease states, will be crucial for maximizing therapeutic efficacy while minimizing off-target effects [11].
The integration of innovative technologies—including deep learning approaches for substrate prediction, novel proximity labeling methods for mapping E3-substrate networks, and advanced structural biology techniques for elucidating ternary complex formation—will accelerate both fundamental understanding and therapeutic translation of E3 ligase biology [110] [111] [11]. Furthermore, combining E3-targeting therapies with conventional DNA-damaging agents or other targeted therapies may yield synergistic effects and overcome resistance mechanisms in cancer treatment.
As research continues to unravel the complexities of the ubiquitin code and its implementation by E3 ligases in DNA damage response, the potential for developing precision medicines that selectively modulate pathogenic proteins represents a promising frontier in cancer therapeutics. The comparative framework established in this analysis provides a foundation for guiding future investigations toward the most promising E3 ligase targets and therapeutic strategies.
The DNA damage response (DDR) is a sophisticated signaling network that detects, signals, and repairs DNA lesions to maintain genomic integrity. At the heart of this process lies ubiquitination, a post-translational modification (PTM) that orchestrates nearly every aspect of DDR through complex crosstalk with other modifications, particularly phosphorylation and acetylation. This intricate interplay generates a sophisticated regulatory code that governs protein stability, interaction networks, and functional outcomes in response to genotoxic stress. The ubiquitin system employs a cascade of E1 (activating), E2 (conjugating), and E3 (ligase) enzymes to attach ubiquitin to substrate proteins, with ~35 E2 and ~1000 E3 enzymes in humans providing immense combinatorial possibilities [113]. Deubiquitinating enzymes (DUBs) reverse this process, adding another layer of regulation. The complexity deepens through the formation of different ubiquitin chain topologies linked via specific lysine residues (K6, K11, K27, K29, K33, K48, K63), with K48-linked chains typically targeting proteins for proteasomal degradation and K63-linked chains facilitating non-proteolytic signaling complexes [86] [1]. Beyond these well-characterized linkages, emerging evidence reveals that all seven ubiquitin linkage types create a diverse "ubiquitin code" that is extensively interpreted, edited, and rewritten through crosstalk with phosphorylation and acetylation events [1] [24].
Fundamental Mechanisms of PTM Crosstalk
Crosstalk between ubiquitination, phosphorylation, and acetylation occurs through two primary mechanisms: (1) through the catalytic machineries where enzymes from one PTM pathway modify components of another, and (2) through substrate-level crosstalk where different PTMs compete for or coordinately regulate the same target protein [114].
Enzymatic Cascade Interdependence
The enzymes that catalyze ubiquitination, phosphorylation, and acetylation frequently modify each other, creating interconnected regulatory networks. For instance, many E3 ubiquitin ligases and DUBs are themselves regulated by phosphorylation, which can modulate their enzymatic activity, subcellular localization, or substrate specificity [113] [115]. Similarly, ubiquitin itself can be acetylated at multiple lysine residues (K6, K11, K27, K33, K48, K63), which directly impacts its ability to form specific polyubiquitin chain types [113]. The acetylation of ubiquitin at K6 or K48 has been shown to impair the formation of polyubiquitin chains at K11, K48, or K63 in vitro, demonstrating how one PTM can directly shape the topology of another [113]. This hierarchical regulation creates temporal sequences of PTM events that dynamically control DDR signaling.
Substrate-Level Coordination
At the substrate level, phosphorylation and acetylation can directly influence the ubiquitination of target proteins by creating or masking degrons (recognition motifs for E3 ligases), modulating substrate stability, or altering interaction interfaces. This crosstalk can produce either synergistic or antagonistic functional outcomes [114]. A prime example is the tumor suppressor p53, which is regulated by a complex PTM network where phosphorylation at specific serine residues (e.g., S15, S392) modulates subsequent ubiquitination events that control its stability and transcriptional activity [116]. Similarly, acetylation of histones and DDR factors can either promote or antagonize ubiquitin signaling depending on the specific modification site and cellular context [24].
Quantitative Landscape of PTM Crosstalk in DDR
Table 1: Key Crosstalk Nodes Between Ubiquitination, Phosphorylation, and Acetylation in DDR
| Target Protein | Ubiquitination Event | Interacting PTM | Functional Outcome | Biological Role in DDR |
|---|---|---|---|---|
| p53 | K48-linked ubiquitination by UBE4B | Phosphorylation at S15 and S392 | Regulates p53 stability and accumulation | Cell fate decisions after DNA damage [116] |
| H2A/H2AX | K63-linked ubiquitination by RNF8/RNF168 | Phosphorylation at S139 (γH2AX) | Facilitates repair protein recruitment | DSB signaling and repair pathway choice [24] |
| H2AK15 | Ubiquitination by RNF168 | Acetylation by TIP60 | Antagonistic regulation | Promotes HR over NHEJ when acetylated [24] |
| H4K16 | - | Acetylation by TIP60 | Inhibits 53BP1 binding to H4K20me2 | Promotes HR repair in S/G2 phases [24] |
| UBE4B | - | Phosphorylation by ATR | Reduces binding to p53 | Enhances p53 stabilization after damage [116] |
| Ubiquitin | Chain formation at K6, K11, K27, K33, K48, K63 | Acetylation at multiple lysines | Impairs specific chain formation | Modulates entire ubiquitin signaling [113] |
Table 2: Enzymes Regulating PTM Crosstalk in DDR
| Enzyme | Enzyme Type | PTM Catalyzed | Crosstalk Targets | Impact on Ubiquitination |
|---|---|---|---|---|
| ATM/ATR | Kinase | Phosphorylation | UBE4B, H2AX, MDC1 | Creates phospho-degrons for ubiquitin ligases [116] [117] |
| TIP60 | Acetyltransferase | Acetylation | H2AK15, H4K16 | Antagonizes ubiquitin-dependent 53BP1 recruitment [24] |
| HDAC1/2 | Deacetylase | Deacetylation | H4K16 | Promotes NHEJ by facilitating 53BP1 binding [24] |
| Wip1 (PPM1D) | Phosphatase | Dephosphorylation | UBE4B, p53 | Stabilizes UBE4B activity; promotes p53 degradation [116] |
| RNF8 | E3 Ubiquitin Ligase | K63 ubiquitination | H2A, H2AX | Requires prior phosphorylation for recruitment [24] |
Molecular Mechanisms of Pathway Coordination
DSB Repair Pathway Choice Through Histone Code Integration
The choice between two major DSB repair pathways—non-homologous end joining (NHEJ) and homologous recombination (HR)—is critically regulated by the interplay between ubiquitination, phosphorylation, and acetylation on histones surrounding the break site [24]. The initial DDR signaling event involves phosphorylation of histone H2AX at serine 139 (γH2AX) by the PI3K-like kinases ATM, ATR, and DNA-PKcs [24]. This phosphorylation event serves as a platform for the recruitment of the E3 ubiquitin ligases RNF8 and RNF168, which catalyze K63-linked ubiquitination of histones H2A and H2AX, creating a recruitment platform for downstream repair factors [24].
The critical pathway decision point revolves around the balance between 53BP1, which promotes NHEJ, and BRCA1, which promotes HR. This balance is regulated by acetylation that antagonizes ubiquitin-dependent 53BP1 recruitment. Specifically, the TIP60 acetyltransferase acetylates H2AK15, directly blocking its ubiquitination by RNF168 and thus impairing 53BP1 binding [24]. Additionally, TIP60-mediated acetylation of H4K16 physically inhibits 53BP1 binding to its recognition mark H4K20me2 [24]. These acetylation events are counteracted by HDAC1 and HDAC2, which promote NHEJ by removing inhibitory acetyl groups [24]. This intricate PTM crosstalk ensures that repair pathway choice is tightly coordinated with cell cycle phase and cellular context.
p53 Regulation Through Multilayered PTM Integration
The tumor suppressor p53 exemplifies how multiple PTMs are integrated to fine-tune DDR outcomes. p53 stability and activity are regulated by a complex network of modifications, with phosphorylation and acetylation directly influencing its ubiquitination status [116]. In response to DNA damage, kinases including ATM and ATR phosphorylate p53 at multiple serine residues (S15 and S392), which reduces its binding to the negative regulator UBE4B, an E3/E4 ubiquitin ligase that targets p53 for degradation [116].
The phosphorylation of UBE4B itself through ATR-mediated signaling further reduces its binding affinity for p53, leading to p53 accumulation and activation [116]. This phosphorylation is reversed by the phosphatase Wip1, which dephosphorylates UBE4B and stabilizes its activity, creating a negative feedback loop that fine-tunes p53 dynamics after DNA damage [116]. Additionally, p53 acetylation can influence its ubiquitination by modulating interactions with E3 ligases such as MDM2. This multilayered regulation allows precise control over p53 activity, enabling appropriate cell fate decisions in response to DNA damage.
Experimental Approaches for Studying PTM Crosstalk
Research Reagent Solutions for PTM Crosstalk Investigation
Table 3: Essential Research Reagents for Studying PTM Crosstalk in DDR
| Reagent Category | Specific Examples | Research Application | Key Function in PTM Studies |
|---|---|---|---|
| Kinase Inhibitors | ATR inhibitors (VE-822); ATM inhibitors (KU-60019) | Dissecting phosphorylation-ubiquitination crosstalk | Block specific phosphorylation events to study downstream effects on ubiquitination [116] [117] |
| Deubiquitinase Inhibitors | USP14 inhibitors; G5 | Investigating ubiquitin chain dynamics | Prevent deubiquitination to study ubiquitin chain stability and function [86] |
| HDAC Inhibitors | Vorinostat; Romidepsin | Probing acetylation-ubiquitination interplay | Increase cellular acetylation levels to study impact on ubiquitin signaling [24] |
| PROTACs | EGFR-directed PROTACs; RT-PROTAC | Targeted protein degradation | Exploit ubiquitination to degrade specific targets; research and therapeutic applications [86] |
| Phospho-specific Antibodies | Anti-γH2AX (S139); anti-p53 (S15) | Monitoring phosphorylation events | Detect specific phosphorylation marks crucial for PTM crosstalk [24] [116] |
| Ubiquitin Linkage-specific Antibodies | Anti-K48 ubiquitin; Anti-K63 ubiquitin | Characterizing ubiquitin chain topology | Discriminate between different ubiquitin linkage types in cellular signaling [86] [1] |
Methodological Workflows for Comprehensive PTM Analysis
The investigation of PTM crosstalk requires integrated experimental approaches that capture the dynamics of multiple modification types. Advanced mass spectrometry (MS) methods form the cornerstone of these investigations, enabling system-wide identification and quantification of phosphorylation, acetylation, and ubiquitination sites [113]. For comprehensive analysis of ubiquitination-acetylation crosstalk, immunoaffinity enrichment of acetylated peptides followed by MS analysis can identify acetylation sites on ubiquitin itself and on E1, E2, and E3 enzymes [113].
For functional studies, CRISPR-based screening approaches can identify novel regulators of PTM crosstalk, as demonstrated by the identification of TRIM21 as a radiosensitization target [86]. Combined with chemical inhibition of specific kinases or acetyltransferases, these approaches can establish causal relationships between different PTM pathways. Live-cell imaging using fluorescently tagged ubiquitin biosensors in combination with phosphorylation or acetylation reporters can provide temporal resolution of the sequence of PTM events at DNA damage sites marked by proteins such as 53BP1 or BRCA1 [24].
To study the functional consequences of specific PTM crosstalk events, mutational approaches are essential. For example, creating acetylation-mimetic (glutamine) or acetylation-deficient (arginine) mutants of ubiquitin lysine residues allows researchers to investigate how acetylation at specific sites impacts ubiquitin chain formation and function [113]. Similarly, phosphorylation site mutants of E3 ligases like UBE4B can reveal how phosphorylation regulates their activity and substrate interactions [116].
Visualization of PTM Crosstalk Pathways
Diagram 1: PTM Crosstalk Governing DSB Repair Pathway Choice. This diagram illustrates how phosphorylation, ubiquitination, and acetylation events are integrated to determine the choice between NHEJ and HR repair pathways after DNA double-strand breaks.
Diagram 2: Phosphorylation-Ubiquitination Crosstalk in p53 Regulation. This diagram shows how UBE4B phosphorylation by ATR reduces its ability to ubiquitinate p53, leading to p53 stabilization, while Wip1-mediated dephosphorylation has the opposite effect.
Therapeutic Implications and Future Perspectives
The intricate crosstalk between ubiquitination, phosphorylation, and acetylation in DDR presents both challenges and opportunities for cancer therapy. Targeting key nodes in these interconnected networks offers promising strategies for overcoming therapy resistance [86] [117]. The development of inhibitors against specific kinases (ATR, ATM, DNA-PKcs), DUBs, and HDACs has demonstrated the potential of exploiting PTM crosstalk for therapeutic benefit [86] [24] [117].
Emerging technologies are opening new avenues for manipulating PTM crosstalk therapeutically. Proteolysis-targeting chimeras (PROTACs) represent a particularly promising approach that exploits the ubiquitin system to target specific proteins for degradation [86]. These bifunctional molecules link a binder for the target protein to a ligand for an E3 ubiquitin ligase, effectively hijacking the ubiquitination machinery to degrade proteins of interest. The development of radiotherapy-triggered PROTAC (RT-PROTAC) prodrugs that are activated by tumor-localized X-rays to degrade specific targets such as BRD4/2 demonstrates how the principles of PTM crosstalk can be leveraged for spatially controlled therapeutic interventions [86].
Future research directions should focus on developing more comprehensive maps of PTM crosstalk networks using systematic proteomic approaches, with particular emphasis on temporal dynamics and spatial organization within subcellular compartments. The integration of computational modeling with experimental validation will be essential for predicting cellular responses to combinatorial perturbations of multiple PTM pathways. Additionally, further exploration of less-characterized ubiquitin linkage types (K6, K11, K27, K29, K33) and their crosstalk with other PTMs may reveal novel regulatory mechanisms and therapeutic opportunities.
As our understanding of PTM crosstalk in DDR continues to deepen, we can anticipate more sophisticated therapeutic strategies that simultaneously target multiple nodes in these interconnected networks. Such approaches will likely play an increasingly important role in overcoming therapy resistance and improving outcomes for cancer patients.
The ubiquitin-proteasome system (UPS) represents a crucial regulatory mechanism in maintaining genomic integrity through its control of the DNA damage response (DDR). Ubiquitination, the second most common post-translational modification after phosphorylation, involves a coordinated enzymatic cascade that tags target proteins with ubiquitin molecules, determining their stability, activity, and localization [118] [119]. This process begins with ubiquitin activation by E1 enzymes, proceeds through ubiquitin conjugation via E2 enzymes, and culminates in substrate-specific ubiquitination by E3 ligases [36] [119]. The specificity of E3 ligases—with over 600 identified in the human genome—makes them particularly attractive therapeutic targets in cancer research [118].
Dysregulation of ubiquitination pathways creates vulnerabilities in cancer cells, especially those with pre-existing DDR deficiencies. The successful application of synthetic lethality in treating homologous recombination-deficient cancers with PARP inhibitors demonstrates the therapeutic potential of targeting these pathways [97]. As we explore the validation of novel ubiquitination targets, sophisticated preclinical models that faithfully recapitulate human tumor biology become indispensable tools for translating basic research into clinical applications [120] [121].
The Scientific Foundation: Ubiquitination in DNA Damage Response and Repair
Ubiquitination Mechanisms in DNA Damage Signaling
The DDR network relies heavily on ubiquitin signaling to coordinate repair processes with cell cycle checkpoints and other cellular functions. Ubiquitination plays a particularly critical role in determining the pathway choice for repairing double-strand breaks (DSBs)—one of the most lethal forms of DNA damage [36]. The initial steps of DSB repair involve RNF8 and RNF168-mediated ubiquitination of histone H2A and H2AX, which creates a platform for the recruitment of additional repair factors [36]. The Ku70-Ku80 heterodimer's ubiquitination status serves as a key determinant in directing repair toward non-homologous end joining (NHEJ) or homologous recombination (HR) pathways [36].
Beyond pathway selection, ubiquitination regulates repair protein activity and stability, allowing precise spatiotemporal control over the DNA repair process [36]. The functional consequences of ubiquitination depend on the linkage type and chain topology. K48-linked polyubiquitination typically targets substrates for proteasomal degradation, while K63-linked chains often facilitate protein-protein interactions and activation of signaling complexes [118] [119]. Other linkage types, including K6, K11, K27, K29, and K33, serve specialized functions in specific contexts such as cell cycle regulation and mitochondrial autophagy [118].
Connecting Ubiquitination, DNA Repair, and Cancer Metabolism
Recent research has revealed unexpected connections between ubiquitination in DDR and cancer metabolism. E3 ligases such as NEDD4, APC/CCDH1, FBXW7, and Pellino1 appear to function as molecular bridges between these processes [36]. For instance, hexokinase 2 (HK2), a key glycolytic enzyme, undergoes K63-linked ubiquitination by HUWE1 and TRAF6, leading to its re-localization and activation [36]. This enhanced glycolytic activity supports tumor growth while potentially creating dependencies on specific DDR pathways. Similarly, pyruvate kinase M2 (PKM2), critical for the final step of glycolysis, is regulated by ubiquitination through Parkin, CHIP, and TRIM58 [36].
Table 1: Key E3 Ligases Connecting DNA Damage Response and Cancer Metabolism
| E3 Ligase | Role in DNA Damage Response | Role in Cancer Metabolism | Therapeutic Potential |
|---|---|---|---|
| NEDD4 | Regulates DNA repair factor stability | Controls metabolic enzyme turnover | Under investigation |
| APC/CCDH1 | Cell cycle control after damage | Degrades metabolic enzymes | Preclinical validation |
| FBXW7 | Mutated in cancers with genomic instability | Targets oncogenic metabolic regulators | High-interest target |
| Pellino1 | Inflammatory signaling in DDR | Links metabolism to inflammation | Emerging target |
These connections suggest that ubiquitination-targeted therapies may simultaneously disrupt cancer cell metabolism and DDR, creating powerful synthetic lethal interactions. This paradigm underscores the importance of developing robust preclinical models to validate these complex interactions before clinical translation.
Model Systems: From Basic Tools to Advanced Platforms
Patient-Derived Xenograft (PDX) Models
PDX models are established by implanting fresh patient tumor tissue into immunocompromised mice, creating a system that maintains key characteristics of the original malignancy [120] [121]. The transplantation can be performed subcutaneously, orthotopically (into the corresponding tissue of origin), or in specialized sites such as the renal capsule or intracapsular fat pad [120]. The process typically requires 40-50 days for initial engraftment, with subsequent passages stabilizing at similar timeframes [120].
These models demonstrate significant advantages over traditional cell line-derived xenografts, including preservation of tumor heterogeneity, maintenance of architectural features, and retention of molecular signatures found in patient tumors [120] [122]. This fidelity makes PDX models particularly valuable for studying ubiquitination in DDR, as the complex interactions between DNA repair pathways and tumor microenvironment can be maintained.
Table 2: Comparison of Immunodeficient Mouse Strains for PDX Modeling
| Mouse Strain | Genetic Defect | Immune Deficiencies | Success Rate | Best Applications |
|---|---|---|---|---|
| Nude | Foxn1 mutation | T cells | Low | Easy monitoring, accessible models |
| NOD-SCID | Prkdc mutation | T and B cells | Moderate | General purpose studies |
| NSG/NOG | Prkdc + IL2Rγ null | T, B, NK cells, reduced macrophages/dendritic cells | High | Human immune system reconstitution |
| BRG/BRJ | Rag2 + Jak3 null | T, B, NK cells | High | Radiation-resistant studies |
Quality Control and Authentication Methods
Robust quality control is essential for maintaining PDX model integrity, particularly when studying precise molecular processes like ubiquitination in DDR. Short tandem repeat (STR) profiling serves as the primary authentication method but shows variability in match rates (92.6% in one large study) compared to single nucleotide polymorphism (SNP) analysis (99.2% match rate) [122]. This discrepancy is particularly pronounced in models with microsatellite instability (MSI), where STR analysis becomes less reliable [122].
In a comprehensive analysis of 325 PDX models, 91.1% were fully matched, 7.4% were undeterminable (primarily due to MSI), and 1.5% were unmatched due to contamination or mishandling [122]. These findings highlight the necessity of implementing complementary authentication methods, particularly for MSI-high models where ubiquitination processes may be altered due to mismatch repair deficiencies.
Complementary Model Systems
While PDX models represent the gold standard for in vivo studies, other model systems offer complementary advantages. Patient-derived organoids (PDOs) maintain cellular diversity and heterogeneity while enabling higher-throughput screening [123]. In glioblastoma organoid models, for example, researchers have observed upregulation of ATM, ATR, MDM2, and CDKN1A following radiation and temozolomide treatment, recapitulating the therapy resistance observed in patients [123].
Genetically engineered mouse models (GEMMs) provide controlled systems for studying specific genetic alterations but may not fully capture human tumor biology and therapeutic responses [120]. The emerging "mouse hospital" concept, where PDX models undergo drug testing regimens that mirror clinical trials, represents a powerful approach for predictive biomarker discovery and treatment validation [120].
Experimental Protocols: Methodologies for Target Validation
PDX Model Establishment and Maintenance
Tissue Implantation Protocol:
- Sample Acquisition: Obtain fresh tumor tissue from surgical resection or biopsy (larger specimens from radical resections yield higher success rates) [121]
- Tissue Processing: Within 1 hour of resection, place tissue in cold preservation medium (e.g., DMEM with 10% FBS and antibiotics) [120] [121]
- Preparation: Cut tissue into 2-3 mm³ fragments using sterile technique, either maintaining tissue structure or generating single-cell suspensions based on research needs [121]
- Implantation: Mix fragments with basement membrane matrix (e.g., Matrigel) and implant into selected site of immunocompromised mice [121]
- Monitoring: Measure tumor dimensions 2-3 times weekly using calipers, calculating volume as (length × width²)/2 [120]
- Passaging: Once tumors reach 1-2 cm³ (typically 40-50 days), harvest and repeat process for subsequent generations [120]
Key Considerations:
- For ubiquitination studies, snap-freeze portions of each passage for molecular analyses to monitor target engagement
- Orthotopic implantation may better preserve tumor microenvironment but requires advanced imaging for monitoring
- Banking early passage stocks (F1-F3) prevents genetic drift and ensures reproducible experiments [120]
Assessing Ubiquitination in DDR Using PDX Models
Ubiquitination Assay Protocol:
- Sample Preparation: Lyse PDX tumor tissue in RIPA buffer containing protease inhibitors, N-ethylmaleimide (to inhibit deubiquitinases), and iodoacetamide (to block free thiols) [118]
- Immunoprecipitation: Incubate lysates with antibodies against target proteins (e.g., histone H2AX, Ku70/80) coupled to protein A/G beads [36]
- Ubiquitin Detection: Resolve immunoprecipitates by SDS-PAGE, transfer to membranes, and probe with anti-ubiquitin antibodies specific for linkage types (K48, K63, etc.) [119]
- Functional Validation: Combine with proximity ligation assays or immunofluorescence to localize ubiquitination events within tumor sections
DNA Damage Readouts:
- Immunofluorescence for γH2AX and 53BP1 foci to quantify DSBs
- Alkaline comet assays to measure single-strand and double-strand breaks
- Western blotting for DDR players (ATM, ATR, CHK1, CHK2 phosphorylation) [97]
Therapeutic Testing in PDX Models
The "patient-derived clinical trial (PCT)" approach involves:
- Cohort Design: Group PDX models by molecular subtypes (e.g., BRCA1/2 mutant, HR-deficient, specific E3 ligase expressions) [97]
- Treatment Regimens: Mirror clinical dosing schedules for single agents and combinations
- Endpoint Analysis: Monitor tumor growth inhibition, perform histopathological assessment, and analyze molecular changes in ubiquitination and DDR pathways [120]
For ubiquitination-targeted therapies, particular attention should be paid to:
- On-target effects: Monitoring substrate stabilization (e.g., p53 for MDM2 inhibitors)
- Synthetic lethal interactions: Testing combinations with DNA-damaging agents in DDR-deficient backgrounds [97]
- Biomarker development: Identifying predictive signatures of response using molecular profiling
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Research Reagent Solutions for Ubiquitination and DDR Studies
| Reagent Category | Specific Examples | Research Application | Considerations |
|---|---|---|---|
| E1 Inhibitors | MLN7243, MLN4924 | Block global ubiquitination; study upstream UPS components | High toxicity limits therapeutic use |
| Proteasome Inhibitors | Bortezomib, Carfilzomib, Ixazomib | Validate proteasome-dependent ubiquitination roles | FDA-approved; can induce integrated stress response |
| E3 Ligase-Targeting | Nutlin, MI-219 (MDM2); Various PROTACs | Specific substrate stabilization; targeted protein degradation | Varying specificity; potential off-target effects |
| DUB Inhibitors | Compounds G5, F6 | Study deubiquitination effects on substrate stability | Emerging specificity challenges |
| DNA Damage Inducers | PARP inhibitors; ATR/CHK1/WEE1 inhibitors | Create synthetic lethal scenarios with ubiquitination defects | Dose carefully to avoid overwhelming systems |
| Authentication Tools | STR panels; SNP arrays; MSI detection assays | Quality control for PDX models | Essential for model fidelity; regular monitoring |
Data Generation and Analysis: From Validation to Application
Molecular Profiling in PDX Models
Comprehensive molecular characterization of PDX models enables correlation of treatment responses with specific genetic features relevant to ubiquitination and DDR. This includes:
Genomic Analyses:
- Whole exome sequencing to identify mutations in DDR genes (BRCA1/2, ATM, ATR) and ubiquitination pathway components [122]
- Copy number variation assessment to detect amplifications or deletions affecting E3 ligases or DDR genes
- MSI status determination given its impact on STR profiling and potential connection to ubiquitination pathways [122]
Transcriptomic and Proteomic Approaches:
- RNA sequencing to evaluate expression of ubiquitination-related genes and DDR pathways
- Reverse-phase protein arrays to quantify phosphorylation of DDR players and ubiquitination cascade components
- Mass spectrometry-based ubiquitinomics to identify specific ubiquitination sites and linkage types in response to treatments
Biomarker Validation for Targeted Therapies
PDX models provide ideal platforms for validating predictive biomarkers for ubiquitination-targeted therapies. The workflow includes:
- Hypothesis Generation: Identify potential biomarkers from -omics data (e.g., E3 ligase expression, DDR gene mutations, ubiquitination signatures)
- Analytical Validation: Develop robust assays (IHC, RT-qPCR, targeted mass spectrometry) for candidate biomarkers
- Clinical Correlation: Compare PDX responses with biomarker status across molecularly characterized models
- Threshold Determination: Establish cutoff values for continuous biomarkers (e.g., expression levels) that predict response
For example, in acute lymphoblastic leukemia models, FBXO8 has been identified as a prognostic biomarker through integrated analysis of ubiquitination-related genes, with knockdown experiments validating its functional role in disease progression [124].
Therapeutic Applications: From Bench to Bedside
Successful Clinical Translations
The validation of ubiquitination targets in PDX models has enabled several successful therapeutic developments:
PARP Inhibitors: The paradigm for targeting DDR deficiencies, with olaparib first approved in 2014 for BRCA-mutant ovarian cancer [97]. PDX models were instrumental in validating the synthetic lethal interaction between PARP inhibition and homologous recombination deficiency.
Next-Generation PARP1-Selective Inhibitors: Developed to maintain efficacy while reducing side effects, demonstrating how PDX models can guide compound optimization [97].
E3 Ligase-Targeting Therapies: Multiple compounds targeting E3 ligases such as MDM2 are in clinical development, with PDX models providing critical proof-of-concept data [118].
Emerging Therapeutic Opportunities
Current research using PDX models has identified several promising avenues for targeting ubiquitination in DDR:
Combination Therapies: PDX studies have revealed synergistic interactions between:
- E1/E2/E3 inhibitors and DNA-damaging chemotherapy
- Ubiquitination pathway inhibitors and immunotherapy (via modulation of immune checkpoint protein stability)
- DUB inhibitors and targeted therapies in specific molecular contexts
Context-Specific Vulnerabilities: PDX screens have identified tumor types with particular susceptibility to ubiquitination pathway disruption, including:
- Cancers with FBXW7 mutations exhibiting specific metabolic dependencies [36]
- BRCA1/2-deficient tumors sensitive to combined PARP and ubiquitination pathway inhibition [97]
- MSI-high cancers with altered protein degradation requirements [122]
The integration of PDX models and patient-derived data has fundamentally advanced our ability to validate ubiquitination targets in the DNA damage response. These models provide unprecedented fidelity to human tumor biology while enabling controlled intervention studies impossible in clinical settings. The continued refinement of PDX platforms—including the incorporation of humanized immune systems, advanced imaging modalities, and multi-omics profiling—will further enhance their predictive power.
Future directions in the field include:
- Spatial Omics Applications: Mapping ubiquitination and DDR events within tumor architectural contexts
- Dynamic Biomarker Development: Identifying real-time indicators of target engagement and treatment response
- Microenvironment Integration: Studying how ubiquitination in stromal components influences DDR and therapeutic outcomes
- Computational Model Integration: Combining PDX data with artificial intelligence approaches to predict novel synthetic lethal interactions
As we continue to unravel the complex interplay between ubiquitination and DNA damage response, PDX models will remain indispensable tools for translating these insights into transformative cancer therapies.
PDX Model Workflow for Target Validation: This diagram illustrates the comprehensive process from patient sample acquisition to clinical translation, highlighting critical quality control checkpoints and parallel experimental pathways.
Ubiquitination in DNA Damage Response: This diagram outlines how different ubiquitination types regulate DNA repair pathway choice and cellular outcomes following DNA damage detection.
Targeted protein degradation (TPD) represents a paradigm shift in drug discovery, moving beyond the transient inhibition offered by conventional small molecules to the irreversible elimination of pathogenic proteins [125]. This approach is particularly relevant in DNA damage response (DDR) cancer research, where the ubiquitin-proteasome system (UPS) plays a fundamental regulatory role [1] [80]. The UPS controls almost every aspect of the DDR, from signaling DNA lesions to enforcing cell cycle checkpoints and facilitating DNA repair pathways [1]. Dysregulation of ubiquitin-mediated processes is a hallmark of many cancers, making components of this system attractive therapeutic targets [1] [126]. Within this context, three distinct therapeutic modalities—conventional inhibitors, PROteolysis TArgeting Chimeras (PROTACs), and molecular glues—offer complementary strategies for intervening in disease pathways. This review provides a comparative analysis of these modalities, focusing on their mechanisms, relative advantages, and applications in targeting the ubiquitin system in DDR and cancer biology.
Mechanistic Foundations and Comparative Profiles
Conventional Small-Molecule Inhibitors
Traditional inhibitors function through occupancy-driven pharmacology, where therapeutic effects correlate with target occupancy [125] [127]. These molecules typically bind to enzymatic active sites or functional domains, temporarily suppressing protein activity [80] [125]. For example, kinase inhibitors like palbociclib bind to the ATP-binding pocket of CDK4/6, competing with ATP and preventing phosphorylation of downstream substrates [127]. However, this approach requires sustained target engagement through high drug concentrations and faces limitations against proteins lacking defined binding pockets, such as transcription factors and scaffolding proteins [125].
PROTACs (PROteolysis TArgeting Chimeras)
PROTACs are heterobifunctional molecules consisting of three elements: a warhead that binds the protein of interest (POI), a ligand that recruits an E3 ubiquitin ligase, and a linker connecting these two moieties [128] [80] [129]. Rather than merely inhibiting the target, PROTACs catalyze its ubiquitination and subsequent degradation by the proteasome [80] [129]. The mechanism involves the formation of a productive ternary complex (POI-PROTAC-E3 ligase), where the E3 ligase transfers ubiquitin chains to the target protein, marking it for destruction [128] [80]. This event-driven mechanism enables catalytic activity, as a single PROTAC molecule can facilitate the degradation of multiple target proteins [80] [129]. PROTACs have been developed to target various proteins, including nuclear receptors and kinases, by recruiting E3 ligases such as VHL, CRBN, and MDM2 [80] [129].
Molecular Glues
Molecular glues are monovalent small molecules that induce or stabilize protein-protein interactions between an E3 ubiquitin ligase and a target protein, leading to the target's degradation [128] [130] [131]. Unlike PROTACs, molecular glues typically possess a simpler structure and function by binding to an E3 ligase (or occasionally the target protein) and creating a new molecular interface—a "neo-pocket"—that facilitates interaction with a protein that would not normally bind [128] [131] [125]. The classic examples are immunomodulatory imide drugs (IMiDs) like thalidomide, lenalidomide, and pomalidomide, which bind to the CRL4CRBN E3 ligase and redirect it to degrade transcription factors IKZF1 and IKZF3 in multiple myeloma [128] [130] [80]. Other examples include the CDK inhibitor CR8, which acts as a molecular glue to degrade cyclin K [128], and indisulam, which recruits RBM39 to the DCAF15 E3 ligase [128] [130].
Table 1: Comparative Analysis of Therapeutic Modalities
| Feature | Conventional Inhibitors | PROTACs | Molecular Glues |
|---|---|---|---|
| Mechanism of Action | Occupancy-driven inhibition [125] | Event-driven degradation [125] | Event-driven degradation [125] |
| Molecular Architecture | Single pharmacophore | Heterobifunctional (POI ligand + E3 ligand + linker) [80] | Monovalent, single small molecule [125] |
| Molecular Weight | Low (typically <500 Da) | High (typically 700-1000 Da) [128] | Low (similar to conventional drugs) [128] [131] |
| Target Requirement | Requires a functional or ligandable pocket | Requires a binder for the POI [131] | Can degrade proteins without a ligandable pocket [131] |
| Effect on Protein | Transiently suppresses function | Eliminates the entire protein [80] | Eliminates the entire protein [80] |
| Potency | Stoichiometric | Catalytic/sub-stoichiometric [80] | Catalytic/sub-stoichiometric [80] |
| Druggability | Limited to proteins with druggable pockets | Expands the druggable proteome [80] | Significantly expands the druggable proteome [131] |
| Key Challenge | Target inhibition, drug resistance | Cell permeability, oral bioavailability due to size [128] | Serendipitous discovery, rational design [128] [125] |
Table 2: E3 Ligases and Targets in Protein Degradation Therapies
| E3 Ligase | Therapeutic Modality | Target Protein(s) | Indication(s) | Example Compound(s) |
|---|---|---|---|---|
| CRBN | Molecular Glue [130] | IKZF1, IKZF3, GSPT1, CK1α [130] | Multiple Myeloma, AML [130] | Thalidomide, Lenalidomide, Pomalidomide [130] |
| DCAF15 | Molecular Glue [130] | RBM39, RBM23 [130] | Leukemia, MDS [130] | Indisulam, E7820 [130] |
| VHL | PROTAC [80] | BRD4, ERRα, BCR-ABL [80] | Cancer [80] | Various Preclinical PROTACs [80] |
| CRBN | PROTAC [80] | BRD4, BTK, AR, ER [80] | Cancer (e.g., Prostate, Breast) [80] | ARV-110, ARV-471 [129] |
| MDM2 | PROTAC [80] | AR, SMARCA2/4 [80] | Cancer [80] | Various Preclinical PROTACs [80] |
The Ubiquitin-Proteasome System and DNA Damage Response
The ubiquitin-proteasome system is a finely tuned mechanism for maintaining cellular protein homeostasis. The process begins with ubiquitin activation by an E1 enzyme in an ATP-dependent manner. The activated ubiquitin is then transferred to an E2 conjugating enzyme. Finally, an E3 ubiquitin ligase facilitates the transfer of ubiquitin from the E2 to a specific lysine residue on the target protein [1] [80]. The specificity of this system is largely determined by the E3 ligases, which number over 600 in humans [80]. Proteins tagged with K48-linked polyubiquitin chains are typically directed to the proteasome for degradation [1] [80].
In the context of DNA damage response, ubiquitin signaling plays multiple critical roles beyond just protein degradation. For instance, K63-linked ubiquitin chains serve as non-proteolytic signaling platforms that facilitate the recruitment of DNA repair proteins to sites of damage [1]. The RNF8/RNF168 E3 ligase cascade is a prime example, which builds ubiquitin scaffolds at DNA double-strand breaks (DSBs) to recruit factors like BRCA1 and 53BP1, thereby influencing the choice between homologous recombination and non-homologous end joining repair pathways [1]. The Fanconi anemia (FA) pathway, another crucial DDR mechanism, is regulated by a multi-step ubiquitination process where the FA core complex (containing the FANCL E3 ligase) monoubiquitinates FANCD2/FANCI, leading to their recruitment to damaged DNA and activation of DNA repair [1]. Deubiquitinating enzymes (DUBs) provide an additional layer of regulation by removing ubiquitin signals, thereby terminating DDR signals or reversing ubiquitination events [1] [126]. The interplay between DNA damage, ubiquitination, and autophagy further illustrates the complexity of this system, as demonstrated by findings that H. pylori infection promotes DNA damage by suppressing Rad51 expression through inhibition of autophagy and accumulation of p62, which promotes Rad51 ubiquitination [132].
Diagram 1: Ubiquitin-proteasome pathway in DNA damage response.
Direct Comparative Analysis: Advantages and Limitations
Molecular Glues vs. PROTACs
While both molecular glues and PROTACs achieve targeted protein degradation, they differ significantly in their design principles, discovery approaches, and drug-like properties.
Structural and Design Considerations: PROTACs are modular by design, comprising two distinct ligands connected by a linker. This structure allows researchers, in theory, to mix and match different POI binders and E3 ligands to create new degraders [80] [129]. However, this modularity comes at the cost of high molecular weight (often 700-1000 Da), which can challenge cellular permeability and oral bioavailability [128] [131]. Molecular glues, in contrast, are typically smaller, monofunctional molecules with properties that adhere more closely to Lipinski's "Rule of Five," resulting in better cell permeability and pharmacokinetic profiles [128] [125].
Mechanism of Target Engagement: A fundamental distinction lies in how these molecules engage the target. PROTACs require a pre-existing binding pocket on the target protein for their warhead to engage [131]. Molecular glues, however, can degrade proteins that lack such pockets because they induce interactions by binding to the E3 ligase and creating a new composite surface that recognizes the target protein [131] [125]. This allows molecular glues to target a broader range of proteins, including those considered "undruggable" by conventional means.
Discovery and Development: PROTAC discovery can follow a more rational path. Once suitable binders for a POI and an E3 ligase are identified, they can be linked and optimized [80] [129]. The discovery of molecular glues, however, has been largely serendipitous [128] [125]. Their mechanism often involves subtle remodeling of protein surfaces, making rational design and prediction extremely difficult. This unpredictability represents the primary bottleneck in molecular glue development [125].
Diagram 2: Comparative mechanisms of PROTACs and molecular glues.
Event-Driven vs. Occupancy-Driven Pharmacology
Both PROTACs and molecular glues operate on an event-driven pharmacological model, which fundamentally differs from the occupancy-driven model of conventional inhibitors [125]. In event-driven pharmacology, the pharmacological effect (protein degradation) is distinct from the molecular binding event. The degrader catalyzes a ubiquitination reaction and is then recycled to degrade additional target molecules [80]. This catalytic cycle allows for sub-stoichiometric activity, meaning lower drug concentrations can achieve a profound and sustained biological effect compared to inhibitors, which require continuous high target occupancy [80] [129]. This property may also reduce the risk of drug resistance, a common problem with traditional kinase inhibitors [80].
Experimental Approaches and Research Toolkit
Key Methodologies for Degrader Development and Validation
Ternary Complex Formation Assays: A critical step in degrader development is confirming the formation of a productive ternary complex (POI-degrader-E3). Techniques such as surface plasmon resonance (SPR) and biolayer interferometry (BLI) can be used to measure binding affinity and kinetics in real-time without labels [129]. Analytical ultracentrifugation (AUC) and X-ray crystallography/Cryo-EM provide structural insights into the ternary complex, revealing the orientation and protein-protein interactions that are crucial for efficient degradation [129].
Cellular Degradation and Selectivity Profiling: To confirm degradation activity in cells, researchers typically treat relevant cell lines with the degrader and measure target protein levels over time via western blotting [129]. To establish mechanism of action and specificity, global proteomics (e.g., tandem mass tag mass spectrometry, TMT-MS) is employed to quantify changes across thousands of proteins, identifying on-target degradation and potential off-target effects [130] [129]. Genetic validation using CRISPR-Cas9 to knock out the recruited E3 ligase is essential to confirm that degradation is dependent on the intended ubiquitin pathway [128] [129].
Functional Phenotypic Assays: Ultimately, degradation must translate into a desired biological effect. In DDR research, this is measured by assays such as cell viability/proliferation assays, flow cytometry-based cell cycle analysis, and direct DDR readouts like γH2AX immunofluorescence (a marker for DNA double-strand breaks) and clonogenic survival assays following DNA damage [132].
Table 3: Essential Research Reagents and Tools
| Reagent/Tool Category | Specific Examples | Primary Function in Research |
|---|---|---|
| E3 Ligase Ligands | Thalidomide analogs (for CRBN) [130]; VHL-1 (for VHL) [80]; Nutlin (for MDM2) [80] | Recruit specific E3 ligases in PROTAC design or study molecular glue mechanisms. |
| Target Protein Binders | Kinase inhibitors; BET bromodomain inhibitors (e.g., JQ1) [80]; AR/ER antagonists [129] | Serve as warheads in PROTACs to bind the protein targeted for degradation. |
| Proteomics Platforms | Tandem Mass Tag (TMT) Mass Spectrometry [129] | Unbiased global profiling of protein levels to confirm on-target degradation and identify off-targets. |
| Genetic Tools | CRISPR-Cas9 kits for E3 ligase knockout (e.g., CRBN, VHL) [128] [129] | Validate the specificity and mechanism of degradation by demonstrating E3-dependence. |
| DNA Damage Assays | Anti-γH2AX antibody [132]; Rad51 antibodies [132]; Comet Assay kits | Measure the functional consequences of degrading DDR proteins on genome integrity and repair. |
The strategic elimination of disease-causing proteins via targeted degradation offers a powerful complement to traditional inhibition. Within the framework of DDR and cancer research, the unique advantages of PROTACs and molecular glues—degrading previously "undruggable" targets, overcoming resistance, and acting catalytically—hold immense therapeutic potential. The future of the field lies in addressing its current limitations. For PROTACs, this involves optimizing pharmacokinetics and discovering new E3 ligases for tissue-specific targeting [129]. For molecular glues, the paramount challenge is moving from serendipitous discovery to rational design, which will require advances in structural biology, computational prediction of protein-protein interfaces, and sophisticated high-throughput screening platforms [131] [125]. As our understanding of the ubiquitin code in DNA damage response deepens, these degradation technologies are poised to deliver a new generation of precision oncology therapeutics.
Conclusion
The intricate involvement of ubiquitination in the DNA damage response solidifies its position as a master regulator of genome integrity and a pivotal vulnerability in cancer. The foundational understanding of E3 ligase functions has successfully paved the way for methodological breakthroughs, most notably in targeted protein degradation, offering unprecedented precision in oncoprotein targeting. While troubleshooting challenges like drug resistance remains critical, the validation of ubiquitination's role in connecting DDR to other cancer hallmarks, such as metabolic rewiring, opens vast new therapeutic landscapes. Future research must focus on elucidating the complete 'ubiquitin code' in different cancer types, developing next-generation degraders with enhanced specificity, and advancing biomarker-driven clinical trials to realize the full potential of targeting the ubiquitin system for precision oncology.
References
- 1. The ubiquitous role of ubiquitin in the DNA damage response [https://pmc.ncbi.nlm.nih.gov/articles/PMC7105183/]
- 2. Ubiquitination and deubiquitination in cancer [https://molecular-cancer.biomedcentral.com/articles/10.1186/s12943-024-02046-3]
- 3. Targeting ubiquitination for cancer therapies [https://pmc.ncbi.nlm.nih.gov/articles/PMC4976843/]
- 4. Role of K63-linked ubiquitination in cancer [https://www.nature.com/articles/s41420-022-01204-0]
- 5. modes of regulating methyltransferase Diverse by histone... activity [https://pubmed.ncbi.nlm.nih.gov/37429149/]
- 6. Ubiquitinomics revealed disease- and stage-specific patterns ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10439878/]
- 7. RNF168 and the DNA damage response pathway - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC8486888/]
- 8. E3 ligases: a ubiquitous link between DNA repair, DNA ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11346458/]
- 9. Frontiers | Put a RING on it: regulation and inhibition of RNF and... 8 [https://www.frontiersin.org/journals/genetics/articles/10.3389/fgene.2013.00128/full]
- 10. The enigma of the RING-UIM E3 ligases - PubMed Central - NIH [https://pmc.ncbi.nlm.nih.gov/articles/PMC12522283/]
- 11. E3 ubiquitin ligases and their therapeutic potential in ... [https://www.sciencedirect.com/science/article/abs/pii/S0006295225001376]
- 12. Ubiquitin E3 ligases in cancer: somatic mutation and ... [https://www.bmbreports.org/view.html?uid=1819&vmd=Full]
- 13. Ubiquitin ligase suppresses Notch signaling to regulate... RNF 8 [https://pmc.ncbi.nlm.nih.gov/articles/PMC6160000/]
- 14. - and RNF -dependent degradation of... 8 RNF 168 [https://pubmed.ncbi.nlm.nih.gov/22373579/]
- 15. ZNF451 collaborates with RNF to regulate 8 localization and... RNF 168 [https://www.nature.com/articles/s41418-025-01472-0?error=cookies_not_supported&code=828bfc28-daaf-4fda-9744-4aaa202020b8]
- 16. Regulation of the DNA damage response by ubiquitin ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4354423/]
- 17. Ubiquitin ligases in cancer: functions and clinical potentials [https://pmc.ncbi.nlm.nih.gov/articles/PMC8286310/]
- 18. Ubiquitylation and the Fanconi Anemia Pathway - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC3858975/]
- 19. PCNA Ubiquitination Is Important, But Not Essential for ... [https://journals.plos.org/plosgenetics/article?id=10.1371/journal.pgen.1002262]
- 20. The Fanconi Anemia DNA Repair Pathway [https://fanconi.org/clinical-care-guidelines/the-fanconi-anemia-dna-repair-pathway/]
- 21. Translesion-synthesis-mediated bypass of DNA lesions ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12051500/]
- 22. Rad18-mediated Translesion Synthesis of Bulky DNA ... [https://www.sciencedirect.com/science/article/pii/S0021925819888865]
- 23. PCNA Ubiquitination and REV1 Define Temporally Distinct ... [https://www.sciencedirect.com/science/article/pii/S1097276508003249]
- 24. Chromatin Ubiquitination Guides DNA Double Strand ... [https://www.frontiersin.org/journals/cell-and-developmental-biology/articles/10.3389/fcell.2022.928113/full]
- 25. Chromatin Ubiquitination Guides DNA Double Strand Break ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9294282/]
- 26. βTrCP facilitates MRN complex localization on chromatin to ... [https://www.nature.com/articles/s42003-025-08462-5]
- 27. Epigenetic modifications of histones in cancer [https://genomebiology.biomedcentral.com/articles/10.1186/s13059-019-1870-5]
- 28. Histone ubiquitylation and its roles in transcription and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4688114/]
- 29. remodelling after Ubiquitin is associated... chromatin DNA damage [https://pubmed.ncbi.nlm.nih.gov/32458023/]
- 30. Decoding histone ubiquitylation [https://www.frontiersin.org/journals/cell-and-developmental-biology/articles/10.3389/fcell.2022.968398/full]
- 31. Non-Canonical Ubiquitination in the Regulation of DNA ... Damage [https://www.imcr.uzh.ch/en/research/penengo/research/non-canonical.html]
- 32. Histone Modifications and their Role in Epigenetics of Cancer [https://pubmed.ncbi.nlm.nih.gov/34749606/]
- 33. Proteasome inhibitors in cancer therapy - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC3088792/]
- 34. Bortezomib for the Treatment of Hematologic Malignancies [https://pmc.ncbi.nlm.nih.gov/articles/PMC6544598/]
- 35. Bortezomib in cancer therapy: Mechanisms, side effects ... [https://www.sciencedirect.com/science/article/pii/S002432052400715X]
- 36. Ubiquitination Links DNA Damage and Repair Signaling to ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10179089/]
- 37. Safety assessment of proteasome inhibitors real world ... [https://www.nature.com/articles/s41598-025-96427-3]
- 38. Combination Therapy Could Expand Treatment Options for ... [https://today.ucsd.edu/story/combination-therapy-could-expand-treatment-options-for-aml-patients-extend-survival]
- 39. Johnson & Johnson reinforces its leadership in hematology ... [https://www.jnj.com/media-center/press-releases/johnson-johnson-reinforces-its-leadership-in-hematology-at-ash-2025-unveiling-new-paradigm-shifting-research]
- 40. October - November 2025: What's New in Myeloma? [https://www.myeloma.org/blog/october-november-2025-whats-new-myeloma]
- 41. Proteolysis‐Targeting Chimera (PROTAC) - PubMed Central [https://pmc.ncbi.nlm.nih.gov/articles/PMC12495453/]
- 42. PROTAC: a revolutionary technology propelling small ... [https://www.frontiersin.org/journals/oncology/articles/10.3389/fonc.2025.1676414/full]
- 43. Dual functionality of MDM2 in PROTACs expands the horizons ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12392632/]
- 44. Molecular Glues: The Adhesive Connecting Targeted Protein ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9910052/]
- 45. Molecular glues: A new path to the world of the unattainable [https://www.sciencedirect.com/science/article/abs/pii/S0141813025094188]
- 46. Molecular glue [https://en.wikipedia.org/wiki/Molecular_glue]
- 47. Proteolysis‐targeting chimeras in cancer therapy [https://pmc.ncbi.nlm.nih.gov/articles/PMC12535346/]
- 48. PK/PD modeling of targeted protein degraders [https://www.sciencedirect.com/science/article/pii/S1359644625000248]
- 49. Predicting PROTAC off-target effects via warhead ... [https://www.sciencedirect.com/science/article/pii/S2001037025004301]
- 50. Multitargeted protein degradation: Integrating small- ... [https://www.sciencedirect.com/science/article/pii/S259004982500089X]
- 51. E3 ubiquitin ligases: styles, structures and functions - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC8607428/]
- 52. Targeting E3 ubiquitin ligases and their adaptors as a ... [https://www.nature.com/articles/s12276-023-01087-w]
- 53. The involvement of E in the development and... 3 ubiquitin ligases [https://www.nature.com/articles/s41420-023-01760-z?error=cookies_not_supported&code=12718edf-7e3f-40ab-8185-64c4af2c1444]
- 54. p53 Ubiquitination: Mdm2 and Beyond - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC3737769/]
- 55. Mdm2-mediated ubiquitylation: p53 and beyond [https://www.nature.com/articles/cdd200968]
- 56. Novel Inhibitors for MDM2-MDM4 E3 Ligase Potently Induce ... [https://pubmed.ncbi.nlm.nih.gov/39795242/]
- 57. Expression and regulatory network of E ... 3 ubiquitin ligase [https://bmccancer.biomedcentral.com/articles/10.1186/s12885-023-11007-w]
- 58. : Key Regulators of TGFβ E in 3 ... Ubiquitin Ligases Signaling Cancer [https://pmc.ncbi.nlm.nih.gov/articles/PMC7825147/]
- 59. Dual functionality of MDM2 in PROTACs expands the horizons ... [https://biomarkerres.biomedcentral.com/articles/10.1186/s40364-025-00826-7]
- 60. Evolving role of deubiquitinating in oral enzymes (Review) cancer [https://www.spandidos-publications.com/10.3892/ol.2025.15100?text=fulltext]
- 61. The multifaceted roles of deubiquitinating enzymes (DUBs) ... [https://www.nature.com/articles/s41419-025-08052-7]
- 62. Recent advances in small molecule inhibitors of ... [https://www.sciencedirect.com/science/article/abs/pii/S0223523425000893]
- 63. The emerging role of deubiquitylating enzymes as therapeutic targets ... [https://cancerci.biomedcentral.com/articles/10.1186/s12935-022-02524-y]
- 64. USP1 in regulation of DNA repair pathways [https://www.sciencedirect.com/science/article/pii/S1568786425000035]
- 65. Therapeutic inhibition of USP7 promotes antitumor immune ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12481409/]
- 66. Frontiers | Clinical outcomes of DNA - damaging agents and DNA ... [https://www.frontiersin.org/journals/oncology/articles/10.3389/fonc.2025.1577468/full]
- 67. MD Anderson researchers present promising clinical results at... trial [https://www.news-medical.net/news/20250426/MD-Anderson-researchers-present-promising-clinical-trial-results-at-AACR-2025.aspx]
- 68. 10 clinical to watch the rest of trials | BioPharma Dive 2025 [https://www.biopharmadive.com/news/biotech-pharma-clinical-trials-watch-2025/736120/]
- 69. Transforming Cancer Therapy: Insights from 2025 H1 FDA Approvals... [https://blog.crownbio.com/transforming-cancer-therapy-insights-from-2025-h1-fda-approvals-and-preclinical-drug-discovery]
- 70. Revisiting Proteasome Inhibitors: Molecular Underpinnings ... [https://www.mdpi.com/1420-3049/27/7/2201]
- 71. The molecular mechanisms of acquired proteasome inhibitor ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3521846/]
- 72. Regulatory role of E3 ubiquitin ligases in multiple myeloma [https://pmc.ncbi.nlm.nih.gov/articles/PMC12343653/]
- 73. A new era in cancer therapy: targeting the Proteasome-Bcl-2 ... [https://jeccr.biomedcentral.com/articles/10.1186/s13046-025-03505-5]
- 74. E3 Ubiquitin Ligase in Anticancer Drugdsla Resistance [https://pmc.ncbi.nlm.nih.gov/articles/PMC8082683/]
- 75. Drug resistance mechanisms and treatment strategies ... [https://molecular-cancer.biomedcentral.com/articles/10.1186/s12943-024-02005-y]
- 76. Targeted protein degradation: advances in drug discovery ... [https://www.nature.com/articles/s41392-024-02004-x]
- 77. Selective ubiquitination of drug-like small molecules by the ... [https://www.nature.com/articles/s41467-025-63442-x]
- 78. PROTAC 2.0: Expanding the frontiers of targeted protein ... [https://www.sciencedirect.com/science/article/abs/pii/S1359644625000893]
- 79. Systematic and quantitative assessment of the ubiquitin ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3200427/]
- 80. Targeted protein degradation: mechanisms, strategies and ... [https://www.nature.com/articles/s41392-022-00966-4]
- 81. Targeting CDKs in cancer therapy: advances in PROTACs ... [https://www.nature.com/articles/s41698-025-00931-8]
- 82. and MGDs role in drug discovery PROTACs [https://www.news-medical.net/whitepaper/20250915/What-makes-PROTACs-and-MGDs-game-changers-in-drug-discovery.aspx]
- 83. Advancing Design Strategy of PROTACs for Cancer Therapy [https://pmc.ncbi.nlm.nih.gov/articles/PMC12188103/]
- 84. Rational design of the linkers in targeting chimeras - Chemical ... [https://pubs.rsc.org/en/content/articlelanding/2025/sc/d5sc04859a]
- 85. Degraders in Clinical Trails: PROTAC Update | Biopharma PEG 2025 [https://www.biochempeg.com/article/434.html]
- 86. Decoding the ubiquitin network: molecular mechanisms and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12492556/]
- 87. Identification and validation of ubiquitination-related genes ... [https://www.frontiersin.org/journals/genetics/articles/10.3389/fgene.2025.1578075/full]
- 88. Comprehensive interrogation of synthetic lethality in the ... [https://www.nature.com/articles/s41586-025-08815-4]
- 89. Traversing the Path from Bench to Cancer Biomarker Validation [https://www.the-scientist.com/traversing-the-path-from-bench-to-cancer-biomarker-validation-73484]
- 90. Polymerase Chain Reaction Chips for Biomarker Discovery and... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11944077/]
- 91. Machine learning-assisted quantitative metabolomics of ... [https://www.nature.com/articles/s41598-025-13475-5]
- 92. Machine learning in cancer prognostic and diagnostic ... [https://www.sciencedirect.com/science/article/pii/S2666053925001031]
- 93. Intervention of machine learning in bladder cancer ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12141719/]
- 94. Targeting the Ubiquitin–Proteasome System for Cancer - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC12495026/]
- 95. The roles of E in 3 progression and targeted... ubiquitin ligases cancer [https://pmc.ncbi.nlm.nih.gov/articles/PMC9991012/]
- 96. DNA damage response revisited: the p53 family and its ... [https://www.nature.com/articles/s12276-022-00863-4]
- 97. A new wave of innovations within the DNA damage response [https://www.nature.com/articles/s41392-023-01548-8]
- 98. Decoding the ubiquitin network: molecular mechanisms and... [https://molecular-cancer.biomedcentral.com/articles/10.1186/s12943-025-02433-4]
- 99. Ubiquitin modification in the regulation of tumor ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11367865/]
- 100. Molecular mechanisms and potential targeting strategies of ... [https://www.spandidos-publications.com/10.3892/or.2025.9000]
- 101. Pharmacological targets in the ubiquitin system offer new ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3219211/]
- 102. links the DNA damage response and metabolic rewiring in lung... RNF 20 [https://pubmed.ncbi.nlm.nih.gov/40436847/]
- 103. RNF20 links the DNA damage response and metabolic ... [https://www.nature.com/articles/s41467-025-60223-4]
- 104. Hypoxia-inducible factor 1 recruits FACT and RNF20/40 to ... [https://www.sciencedirect.com/science/article/pii/S2211124724003000]
- 105. Frontiers | Targeting the SMURF2- HIF axis: a new frontier in 1 ... α cancer [https://www.frontiersin.org/journals/oncology/articles/10.3389/fonc.2024.1484515/full]
- 106. The regulatory roles of the E3 ubiquitin ligase NEDD4 ... [https://www.frontiersin.org/journals/physiology/articles/10.3389/fphys.2022.968927/full]
- 107. Expanding PROTACtable genome universe of E3 ligases [https://www.nature.com/articles/s41467-023-42233-2]
- 108. Unlocking new degradation mechanisms [https://www.news-medical.net/health/Unlocking-new-degradation-mechanisms-with-alternative-E3-ligases.aspx]
- 109. E3 Ubiquitin Ligases and Their Therapeutic Applications in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11426868/]
- 110. Deep-learning based approach to identify substrates of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9883182/]
- 111. Identifying the targets of E3 ubiquitin ligases [https://www.ludwigcancerresearch.org/ludwig-link/september-2024/identifying-the-targets-of-e3-ubiquitin-ligases/]
- 112. Evaluation of the binding affinity of E3 ubiquitin ligase ... [https://www.sciencedirect.com/science/article/pii/S2666166720302756]
- 113. Acetylation, Phosphorylation, Ubiquitination (Oh My!) [https://pmc.ncbi.nlm.nih.gov/articles/PMC8946176/]
- 114. between Crosstalk and Other Post-translational... Ubiquitination [https://pmc.ncbi.nlm.nih.gov/articles/PMC7748009/]
- 115. An inventory of crosstalk between ubiquitination and other ... [https://www.sciencedirect.com/science/article/pii/S258900422300353X]
- 116. a key mechanism in p53 accumulation and cancer cell ... [https://www.nature.com/articles/s41420-025-02441-9]
- 117. DNA damage response signaling pathways and targets for ... [https://www.nature.com/articles/s41392-020-0150-x]
- 118. The role of ubiquitination in tumorigenesis and targeted ... [https://www.nature.com/articles/s41392-020-0107-0]
- 119. Ubiquitination Enzymes in Cancer, Cancer Immune Evasion ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11763706/]
- 120. Patient-derived xenograft models in cancer therapy [https://www.nature.com/articles/s41392-023-01419-2]
- 121. Patient-derived xenograft models: Current status, challenges ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12179623/]
- 122. Comprehensive DNA profiling strategy for patient-derived ... [https://www.nature.com/articles/s41598-025-21299-6]
- 123. Patient-derived tumor organoids mimic treatment-induced ... [https://www.sciencedirect.com/science/article/pii/S2589004224018297]
- 124. Ubiquitination and ALL: Identifying FBXO8 as a prognostic ... [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2025.1554231/full]
- 125. Review Molecular glues and PROTACs in targeted protein ... [https://www.sciencedirect.com/science/article/abs/pii/S0006295225005623]
- 126. A selective USP1-UAF1 inhibitor links deubiquitination to DNA ... [https://pubmed.ncbi.nlm.nih.gov/24531842/]
- 127. Inhibitors, PROTACs and Molecular Glues as Diverse Therapeutic Modalities to Target Cyclin-Dependent Kinase - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC8583118/]
- 128. Molecular Glues: A New Dawn After PROTAC | Biopharma PEG [https://www.biochempeg.com/article/271.html]
- 129. PROTAC targeted protein degraders: the past is prologue [https://www.nature.com/articles/s41573-021-00371-6]
- 130. Molecular glue degrader for tumor treatment - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC11697593/]
- 131. Molecular glues are beginning to stick [https://cen.acs.org/pharmaceuticals/drug-discovery/Molecular-glues-startups-search-beyond-PROTACS/100/i29]
- 132. of autophagy aggravates Inhibition and... DNA damage response [https://www.sigmaaldrich.com/TR/en/tech-docs/paper/1432739]