Ubiquitination-Related Gene Signatures: Novel Prognostic Biomarkers and Therapeutic Guides in Cancer
Ubiquitination, a crucial post-translational modification, is increasingly recognized for its role in tumorigenesis, progression, and therapy response.
Ubiquitination-Related Gene Signatures: Novel Prognostic Biomarkers and Therapeutic Guides in Cancer
Abstract
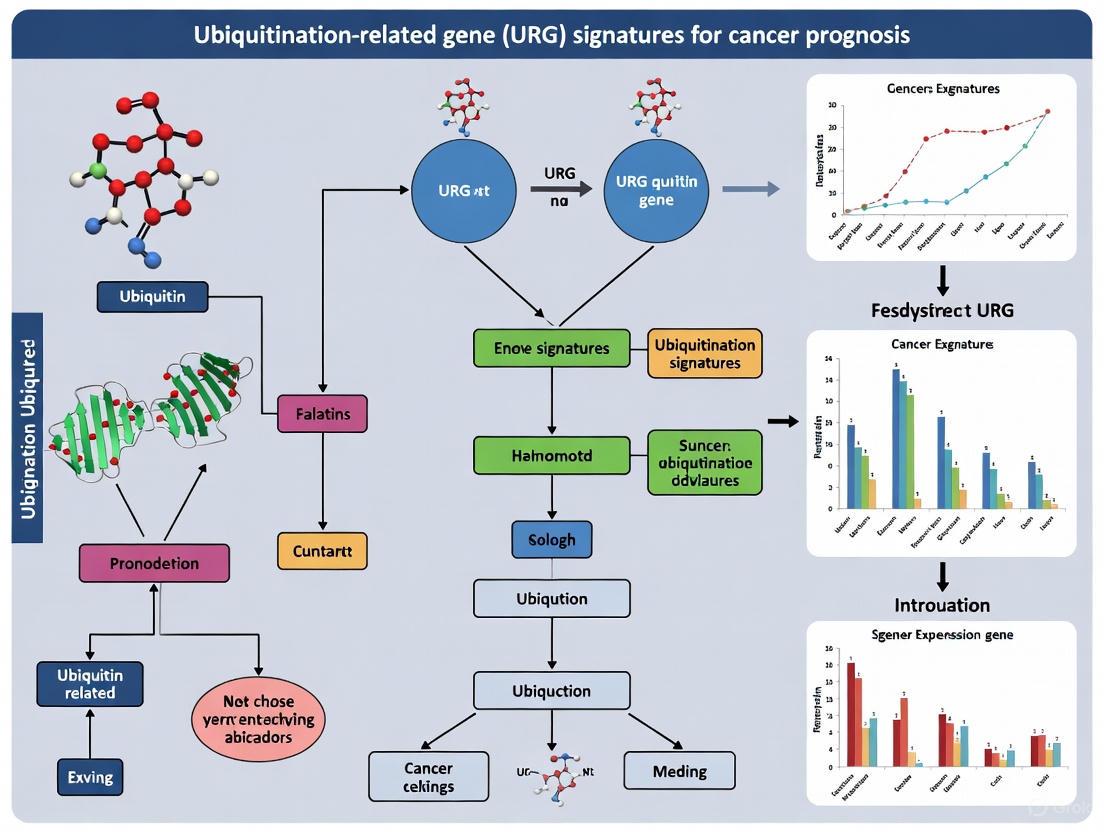
Ubiquitination, a crucial post-translational modification, is increasingly recognized for its role in tumorigenesis, progression, and therapy response. This article synthesizes current research on ubiquitination-related gene (URG) signatures as powerful prognostic tools across multiple cancers, including colon, breast, pancreatic, and cervical cancer. We explore the foundational biology of ubiquitination in cancer, detail the bioinformatic methodologies for developing multi-gene signatures, address key challenges in optimization and clinical translation, and evaluate validation frameworks and comparative performance against established biomarkers. Aimed at researchers, scientists, and drug development professionals, this review highlights the potential of URGs to refine risk stratification, illuminate tumor microenvironment interactions, and ultimately guide the development of personalized oncology therapeutics.
The Ubiquitin System: From Basic Biology to Cancer Prognosis
Ubiquitination is a crucial reversible post-translational modification (PTM) that regulates virtually all aspects of eukaryotic cell biology, from protein degradation to cell signaling, DNA repair, and immune responses [1]. This sophisticated enzymatic system operates through a sequential cascade involving E1 (ubiquitin-activating), E2 (ubiquitin-conjugating), and E3 (ubiquitin-ligase) enzymes, which collaboratively attach the 76-amino acid protein ubiquitin to substrate proteins. The specificity and outcomes of ubiquitination are remarkably diverse—a single ubiquitin (monoubiquitination) or multiple ubiquitins forming chains (polyubiquitination) can be attached to substrates, with at least eight distinct linkage types (Met1, Lys6, Lys11, Lys27, Lys29, Lys33, Lys48, Lys63) creating a complex "ubiquitin code" that determines functional consequences [2] [1]. The reverse reaction, deubiquitination, is carried out by deubiquitinases (DUBs), which hydrolyze ubiquitin-substrate and ubiquitin-ubiquitin bonds, providing dynamic regulation of ubiquitin signaling [3] [4]. This elaborate system maintains cellular homeostasis by controlling protein stability, localization, and activity, with particular relevance to cancer biology where ubiquitination-related gene (URG) signatures are emerging as powerful prognostic tools.
The Ubiquitination Cascade: Mechanism and Key Enzymes
The Enzymatic Pathway
The ubiquitination cascade is an ATP-dependent process that requires the sequential action of three enzyme families [2] [5]:
- E1 Ubiquitin-Activating Enzymes: A single E1 enzyme (Uba1 in humans) initiates the cascade by activating ubiquitin in an ATP-dependent reaction, forming a thioester bond between its catalytic cysteine and the C-terminus of ubiquitin [6] [5].
- E2 Ubiquitin-Conjugating Enzymes: The activated ubiquitin is transferred to the catalytic cysteine of an E2 enzyme via a transthiolation reaction. Humans express several dozen E2s that influence the type of ubiquitin chain formed [6] [7].
- E3 Ubiquitin Ligases: E3s recruit E2~Ub complexes and substrate proteins, facilitating ubiquitin transfer. With over 600 members in humans, E3s provide substrate specificity to the ubiquitin system [2] [8].
Table 1: Major Enzyme Classes in the Ubiquitin System
| Enzyme Class | Number in Humans | Core Function | Key Features |
|---|---|---|---|
| E1 (Activating) | 2 [7] | Ubiquitin activation | ATP-dependent; forms E1~Ub thioester; gatekeeper of ubiquitin conjugation |
| E2 (Conjugating) | Several dozen [7] | Ubiquitin carriage | Determines ubiquitin chain type; forms E2~Ub thioester; interacts with E3s |
| E3 (Ligase) | 500-1000 [2] [8] | Substrate recognition | Provides specificity; directly or indirectly catalyzes ubiquitin transfer |
| DUBs | ~100 [3] | Ubiquitin removal | Cleaves ubiquitin from substrates; recycles ubiquitin; edits ubiquitin chains |
The final step of ubiquitination involves an attack on the E2~Ub thioester bond by a lysine ε-amino group from the substrate protein, forming a stable isopeptide bond. In RING E3 ligases, ubiquitin is transferred directly from the E2 to the substrate, while in HECT and RBR E3s, ubiquitin is first transferred to the E3 before substrate modification [2] [8].
E3 Ubiquitin Ligase Structural Families
E3 ubiquitin ligases are classified into four major families based on their structural features and mechanism of action [2] [8]:
- RING (Really Interesting New Gene) E3 Ligases: The largest E3 family, characterized by a RING domain that binds E2s and facilitates direct ubiquitin transfer from E2 to substrate. RING E3s can function as monomers or multi-subunit complexes like cullin-RING ligases (CRLs) [2].
- HECT (Homologous to E6AP C-Terminus) E3 Ligases: Contain a HECT domain that forms a thioester intermediate with ubiquitin before transferring it to substrates. The HECT family includes Nedd4, HERC, and other HECT subfamilies with distinct protein-interaction domains [2].
- RBR (RING-Between-RING-RING) E3 Ligases: Hybrid mechanisms incorporating aspects of both RING and HECT E3s. RBRs contain a RING1 domain that binds E2~Ub, then transfer ubiquitin to a catalytic cysteine in the RING2 domain before substrate modification [7].
- U-box E3 Ligases: Structurally similar to RING E3s but stabilized by different interactions, functioning as E3/E4 enzymes in ubiquitination processes [2].
The Ubiquitin Code and Cellular Functions
Ubiquitin Linkage Types and Functional Consequences
The ubiquitin code derives from the ability of ubiquitin itself to be modified on its seven lysine residues or N-terminal methionine, creating structurally and functionally distinct polyubiquitin signals [2] [1]:
Table 2: Ubiquitin Linkage Types and Their Primary Functions
| Linkage Type | Primary Functions | Structural Features |
|---|---|---|
| K48-linked | Major proteasomal degradation signal [2] | Targets substrates to 26S proteasome |
| K63-linked | DNA repair, cytokine signaling, autophagy, endocytosis [2] | Non-proteolytic signaling roles |
| Met1-linked (Linear) | NF-κB activation, immune signaling [2] [1] | Assembled by LUBAC complex; regulates inflammation |
| K11-linked | Cell cycle regulation, proteasomal degradation [2] | Involved in ER-associated degradation |
| K27-linked | Protein secretion, DNA damage repair, mitochondrial quality control [2] | Associated with Parkin E3 ligase |
| K29-linked | Proteasomal degradation, innate immune response [2] | Regulates AMPK-related kinases |
| K6-linked | DNA damage response [2] | Less characterized; implicated in genomic stability |
| K33-linked | Intracellular trafficking, regulation of IFN signaling [2] | Controls kinase activity and trafficking |
Deubiquitinases (DUBs): Regulation of the Ubiquitin Code
Deubiquitinases counterbalance ubiquitin signaling by removing ubiquitin modifications from substrate proteins. The human genome encodes approximately 100 DUBs, categorized into seven families based on their catalytic mechanisms [3] [4]:
- Cysteine Protease DUB Families: Include ubiquitin-specific proteases (USPs), ubiquitin C-terminal hydrolases (UCHs), ovarian tumor proteases (OTUs), Josephins, MINDY, and ZUFSP. These utilize a catalytic triad of Cys, His, and Asp/Asn residues for nucleophilic attack on the isopeptide bond [3].
- Metalloprotease DUB Family: JAB1/MPN/MOV34 (JAMM) domain DUBs use a catalytic zinc ion for hydrolysis [3].
DUBs perform three major cellular functions: (1) generating free ubiquitin from linear gene-encoded fusions; (2) trimming polyubiquitin chains to edit signals; and (3) reversing ubiquitin signals by removing ubiquitin from modified proteins [3]. Their dysregulation is implicated in cancer, neurodegenerative diseases, and immune disorders, making them attractive therapeutic targets [3] [4].
Experimental Protocols for Ubiquitination Research
Protocol 1: In Vitro Ubiquitination Assay
Purpose: To reconstitute ubiquitination of a specific substrate and characterize E1-E2-E3 interactions.
Materials:
- Purified E1, E2, E3 enzymes, and substrate protein
- Ubiquitin, ATP, and energy regeneration system
- Reaction buffer: 50 mM Tris-HCl (pH 7.5), 50 mM NaCl, 10 mM MgCl₂, 1 mM DTT
Method:
- Prepare master mix containing 2.5 μM E1, 5-10 μM E2, and 2.5-5 μM E3 in reaction buffer
- Add 5-10 μM substrate, 50 μM ubiquitin, and 2 mM ATP with energy regeneration system
- Incubate at 30°C for 0-120 minutes, taking timepoints at 0, 15, 30, 60, and 120 minutes
- Stop reactions with SDS-PAGE loading buffer containing 50 mM DTT
- Analyze by SDS-PAGE and Western blotting with ubiquitin-specific and substrate-specific antibodies
- For chain linkage specificity, use linkage-specific ubiquitin antibodies (e.g., anti-K48, anti-K63)
Technical Notes: For structural studies, disulfide crosslinking strategies can stabilize E1-E2 complexes as demonstrated in Uba1-Cdc34 structural studies [6]. E2-E3 specificity can be mapped by testing different E2 combinations with a specific E3.
Protocol 2: Ubiquitin Chain Linkage Analysis
Purpose: To determine the specific polyubiquitin chain linkage types assembled by an E2-E3 pair.
Materials:
- Ubiquitin mutants (K48R, K63R, K48-only, K63-only, etc.)
- Linkage-specific ubiquitin antibodies
- Mass spectrometry reagents: trypsin, Glu-C, chromatographic materials
Method:
- Set up ubiquitination reactions with wild-type and lysine-mutant ubiquitins
- For antibody-based detection:
- Perform Western blotting with linkage-specific antibodies
- Compare migration patterns with mutant ubiquitins that restrict chain formation
- For mass spectrometry analysis:
- Enrich ubiquitinated substrates via immunoaffinity purification
- Digest with trypsin/Glu-C to generate signature ubiquitin peptides
- Analyze by LC-MS/MS for identification of linkage-specific diGly remnants
- Quantify relative abundance of different chain types
Technical Notes: K48-linked chains typically target substrates for proteasomal degradation, while K63-linked chains mediate signaling functions [2]. RING E3s generally allow E2s to determine linkage specificity, while HECT and RBR E3s often dictate chain topology [7].
Visualization of Ubiquitin Signaling
The Ubiquitination Enzymatic Cascade
The Ubiquitin Code and Cellular Outcomes
Research Reagent Solutions
Table 3: Essential Research Reagents for Ubiquitination Studies
| Reagent Category | Specific Examples | Research Application | Key Features |
|---|---|---|---|
| E1 Enzymes | Recombinant Uba1, Uba6 | In vitro ubiquitination assays | Essential for initial ubiquitin activation; ATP-dependent |
| E2 Enzymes | Cdc34, UbcH5, Ubc13 | Chain formation studies | Determines ubiquitin chain linkage specificity [6] |
| E3 Ligases | MDM2, Parkin, c-Cbl, APC/C | Substrate specificity studies | Over 600 human E3s provide substrate recognition [2] [8] |
| DUBs | USP14, UCH37, OTUB1 | Deubiquitination assays | Cleave ubiquitin from substrates; edit ubiquitin chains [3] |
| Ubiquitin Variants | K48-only, K63-only, K48R | Chain linkage analysis | Determine specificity of ubiquitin chain formation |
| Linkage-specific Antibodies | Anti-K48, Anti-K63, Anti-M1 | Western blot, immunofluorescence | Identify specific ubiquitin chain linkages |
| Proteasome Inhibitors | Bortezomib, MG132 | Functional validation | Block proteasomal degradation of ubiquitinated substrates |
| DUB Inhibitors | PR-619, b-AP15 | DUB functional studies | Investigate DUB roles in cellular pathways [4] |
Cancer Prognosis Applications of Ubiquitination-Related Genes
Ubiquitination-related gene (URG) signatures are emerging as powerful tools for cancer prognosis and treatment stratification. In breast cancer, the 70-gene MammaPrint signature has been validated in prospective clinical trials for predicting recurrence risk and guiding adjuvant chemotherapy decisions [9]. Similarly, in colorectal cancer, the 12-gene Oncotype DX assay stratifies Stage II/III patients by recurrence risk, though clinicopathological factors like T stage and mismatch repair status remain important [9]. For hepatocellular carcinoma (HCC), multiple mRNA, lncRNA, and miRNA signatures have been developed, including a 5-gene signature (HN1, RAN, RAMP3, KRT19, TAF9) that predicts survival across diverse patient cohorts [9]. The molecular subtyping of cancers based on URGs reveals distinct biological behaviors—proliferation-class HCCs characterized by chromosomal instability versus non-proliferation class with better differentiation [9]. These URG signatures refine traditional TNM staging by capturing the underlying biological heterogeneity of tumors, enabling more personalized treatment approaches. However, challenges remain in standardizing analytical approaches, validating signatures across diverse populations, and translating these molecular tools into routine clinical practice.
The ubiquitin system represents a sophisticated regulatory network that maintains cellular homeostasis through precise control of protein fate and function. The enzymatic cascade of E1, E2, and E3 enzymes creates a diverse ubiquitin code that is dynamically interpreted and edited by DUBs to regulate virtually all cellular processes. Understanding the mechanisms and specificity of these enzymes provides critical insights into disease pathogenesis, particularly in cancer, where ubiquitination-related gene signatures are emerging as valuable prognostic and predictive biomarkers. Continued research on ubiquitination mechanisms, combined with advanced proteomic and genomic technologies, will accelerate the development of targeted therapies and precision medicine approaches that exploit the ubiquitin system for therapeutic benefit.
Ubiquitination Dysregulation as a Hallmark of Cancer Pathogenesis
Ubiquitination is a critical, reversible, and enzymatically regulated post-translational modification that serves as a fundamental regulatory mechanism governing cellular homeostasis. This process orchestrates a vast array of cellular functions including targeted proteolysis, metabolism, signal transduction, and cell cycle regulation [10]. The ubiquitin-proteasome system (UPS) comprises ubiquitin and its degradation by the proteasome, responsible for 80–90% of cellular proteolysis [10]. The ubiquitination process is regulated through a cascade of reactions mediated by ubiquitin-activating enzymes (E1), ubiquitin-conjugating enzymes (E2), and ubiquitin ligases (E3), while ubiquitin chains can be removed by deubiquitinating enzymes (DUBs) [10].
Dysregulation of ubiquitination pathways represents a fundamental hallmark of cancer pathogenesis, contributing to various aspects of tumor development and progression. Ubiquitination plays a crucial regulatory role in tumor metabolic reprogramming and is involved in processes including cell survival, proliferation, and differentiation [10]. Furthermore, it influences protein levels of immune checkpoint regulators like PD-1/PD-L1 in the tumor microenvironment, thereby modulating immunotherapy efficacy [10]. This application note explores the multifaceted roles of ubiquitination dysregulation in cancer and provides detailed protocols for investigating ubiquitination-related prognostic signatures and mechanisms.
Ubiquitination-Related Gene Signatures as Prognostic Biomarkers
Pan-Cancer Ubiquitination Signatures
Recent multi-cancer analyses have revealed that ubiquitination-related gene signatures provide powerful prognostic biomarkers across diverse cancer types. A comprehensive study integrating data from 4,709 patients across 26 cohorts spanning five solid tumor types (lung cancer, esophageal cancer, cervical cancer, urothelial cancer, and melanoma) identified key nodes and prognostic pathways within the ubiquitination-modification network [10]. This research established a conserved ubiquitination-related prognostic signature (URPS) that effectively stratified patients into high-risk and low-risk groups with distinct survival outcomes across all analyzed cancers [10].
The URPS demonstrated significant value as a novel biomarker for predicting immunotherapy response, with the potential to identify patients most likely to benefit from immunotherapy in clinical settings [10]. At single-cell resolution, URPS enabled more precise classification of distinct cell types and was associated with macrophage infiltration within the tumor microenvironment [10]. Experimental validation confirmed that the OTUB1-TRIM28 ubiquitination regulatory axis plays a crucial role in modulating the MYC pathway and influencing patient prognosis [10].
Tissue-Specific Ubiquitination Signatures
Lung Adenocarcinoma (LUAD)
In lung adenocarcinoma, ubiquitination-related risk scores (URRS) calculated from the expression of four genes (DTL, UBE2S, CISH, and STC1) effectively stratified patient prognosis [11]. Patients with higher URRS had significantly worse outcomes (Hazard Ratio [HR] = 0.54, 95% Confidence Interval [CI]: 0.39–0.73, p < 0.001), a finding validated across six external cohorts (Hazard Ratio [HR] = 0.58, 95% Confidence Interval [CI]: 0.36–0.93, pmax = 0.023) [11]. The high URRS group exhibited higher PD1/L1 expression levels (p < 0.05), tumor mutation burden (TMB, p < 0.001), tumor neoantigen load (TNB, p < 0.001), and tumor microenvironment scores (p < 0.001) [11].
Table 1: Key Ubiquitination-Related Prognostic Genes in Lung Adenocarcinoma
| Gene | Function | Prognostic Association | Potential Therapeutic Implications |
|---|---|---|---|
| DTL | Ubiquitin ligase component | Worse prognosis with upregulation | Potential therapeutic target |
| UBE2S | Ubiquitin-conjugating enzyme E2 | Worse prognosis with upregulation | Linked to chemotherapy response |
| CISH | Cytokine inducible SH2-containing protein | Better prognosis with upregulation | Immunomodulatory role |
| STC1 | Secreted glycoprotein | Worse prognosis with upregulation | Associated with tumor progression |
Esophageal Squamous Cell Carcinoma (ESCC)
Comprehensive analysis of ESCC identified 85 ubiquitination-related differentially expressed genes (URDEGs), with five key genes (BUB1B, CHEK1, DNMT1, IRAK1, and PRKDC) demonstrating significant prognostic value [12]. These genes play essential roles in critical processes such as cell cycle regulation and immune response, and their varied expression in ESCC tissues supports their potential as therapeutic targets [12].
Gastric Cancer
In gastric cancer, USP2 expression was significantly reduced in cancer cells and patient samples (p < 0.05) [13]. Patients with low USP2 expression were primarily associated with genetic variations, neoantigen loads, microsatellite instability (MSI) scores, and immune cell infiltration (p < 0.05) [13]. Functional experiments demonstrated that USP2 overexpression suppressed proliferation, migration, and cell cycle progression while enhancing apoptosis in gastric cancer cells [13].
Experimental Protocols for Ubiquitination Research
Protocol 1: Detecting Protein Ubiquitination Modification
This protocol describes a standardized method for detecting K27-linked polyubiquitination of mitochondrial antiviral signaling protein (MAVS), which can be adapted for other proteins of interest [14].
Materials and Reagents
Table 2: Essential Research Reagents for Ubiquitination Detection
| Reagent/Cell Line | Specification | Function/Application | Source/Reference |
|---|---|---|---|
| 293T cells | Human embryonic kidney cell line | Protein expression platform | [14] |
| HA-Ub-K27 plasmid | Expresses HA-tagged ubiquitin with only K27 residue | Specific ubiquitination detection | [14] |
| Myc-MAVS plasmid | Myc-tagged mitochondrial antiviral signaling protein | Target protein for ubiquitination | [14] |
| Anti-Myc antibody | Monoclonal antibody (9E10) | Immunoprecipitation of target protein | Santa Cruz, sc-40 [14] |
| Anti-HA-tag antibody | Polyclonal antibody | Detection of ubiquitinated proteins | GenScript, A00168 [14] |
| Protein G PLUS-Agarose | Agarose conjugate | Antibody binding for immunoprecipitation | Santa Cruz, sc-2002 [14] |
| Protease inhibitor cocktail | Inhibits protein degradation | Maintains protein integrity during processing | Cell Signaling Technology, 5871S [14] |
Step-by-Step Procedure
Cell Preparation and Transfection (Timing: 24 hours)
- Passage 293T cells when 90% confluent in 10 cm dishes
- Transfect cells with plasmids encoding HA-Ub-K27, Myc-MAVS, and relevant experimental vectors using Lipofectamine 2000 reagent according to manufacturer's instructions
- Incubate cells for 24-48 hours at 37°C with 5% CO₂ to allow protein expression
Cell Lysis and Protein Extraction (Timing: 1 hour)
- Aspirate media and wash cells with 3 mL ice-cold phosphate-buffered saline (PBS)
- Lyse cells in 1 mL IP lysis buffer (supplemented with protease inhibitor cocktail and 1 mM PMSF) per 10 cm dish
- Incubate on ice for 30 minutes with occasional vortexing
- Centrifuge at 12,000 × g for 15 minutes at 4°C to pellet cell debris
- Transfer supernatant to fresh tubes for immunoprecipitation
Immunoprecipitation (Timing: 4 hours to overnight)
- Pre-clear lysates by incubating with 20 μL Protein G PLUS-Agarose for 30 minutes at 4°C
- Centrifuge at 2,500 × g for 5 minutes and transfer supernatant to new tubes
- Add 1-5 μg anti-Myc antibody (for exogenous protein) or anti-MAVS antibody (for endogenous protein) per 500 μg total protein
- Incubate with rotation for 2 hours at 4°C
- Add 20 μL Protein G PLUS-Agarose and continue incubation overnight at 4°C
Western Blot Detection (Timing: 6 hours)
- Wash beads three times with 1 mL ice-cold lysis buffer
- Elute proteins by boiling in 2× SDS loading buffer for 10 minutes
- Separate proteins by SDS-PAGE and transfer to PVDF membrane
- Block membrane with 5% non-fat milk in TBST for 1 hour
- Incubate with primary antibodies (anti-HA for exogenous ubiquitination or anti-ub-K27 for endogenous ubiquitination) diluted in blocking buffer overnight at 4°C
- Incubate with appropriate HRP-conjugated secondary antibodies for 1 hour at room temperature
- Develop using enhanced chemiluminescence substrate
Figure 1: Experimental Workflow for Detecting Protein Ubiquitination
Protocol 2: Developing Ubiquitination-Related Prognostic Signatures
This protocol outlines the bioinformatics approach for constructing ubiquitination-related risk models based on methodologies successfully applied in lung adenocarcinoma and other cancers [11].
Data Collection and Preprocessing
Data Acquisition
- Obtain gene expression profiles and corresponding clinical datasets from public repositories (TCGA, GEO)
- Collect ubiquitination-related genes (URGs) from specialized databases (iUUCD 2.0: http://iuucd.biocuckoo.org/)
- For TCGA-LUAD datasets, retain only cancerous tissues, excluding formalin-fixed samples and recurrent tissues
- Filter patients with survival time of fewer than 3 months
Data Normalization and Filtering
- Normalize RNA-seq data using appropriate methods (e.g., FPKM, TPM)
- Perform quality control to remove low-quality samples
- Annotate clinical endpoints (overall survival, progression-free survival)
Molecular Subtype Identification
Consensus Clustering
- Apply unsupervised clustering using the "ConsensusClusterPlus" R package
- Set parameters: maxK = 5, reps = 1000, pItem = 0.8, pFeature = 1, clusterAlg="km", distance="euclidean"
- Repeat clustering 1000 times to ensure classification stability
- Explore prognostic performance and clinical features across molecular subtypes
Differential Expression Analysis
- Identify differently expressed URGs between molecular subtypes using "limma" R package
- Apply filtering thresholds: adjusted p-value ≤ 0.05 and |log2FC| ≥ 0.8
Prognostic Model Construction
Feature Selection
- Perform univariate Cox regression analysis to identify prognostic URGs
- Apply Random Survival Forest algorithm (variable importance > 0.25) using "randomForestSRC" package
- Conduct LASSO Cox regression algorithm using "cv.glmnet" function (family='cox', type.measure = 'deviance')
- Select overlapping genes identified by all three methods
Risk Score Calculation
- Perform multivariate Cox regression analysis on selected genes
- Calculate ubiquitination-related risk scores (URRS) using the formula: [ Risk\,score = \sum \beta{RNA} * Exp{RNA} ] where βRNA represents the coefficient from multivariate Cox regression and ExpRNA represents gene expression levels
- Stratify patients into high-risk and low-risk groups based on median risk score
Model Validation
- Validate prognostic performance in independent external datasets
- Evaluate time-dependent receiver operating characteristic (ROC) curves
- Assess calibration and discrimination metrics
Key Ubiquitination Pathways in Cancer Pathogenesis
OTUB1-TRIM28-MYC Regulatory Axis
Experimental studies have revealed that the OTUB1-TRIM28 ubiquitination regulatory enzyme influences the histological fate of cancer cells by modulating MYC and its downstream targets, while altering oxidative stress pathways [10]. This regulation ultimately leads to immunotherapy resistance and poor prognosis in patients. Ubiquitination score positively correlates with squamous or neuroendocrine transdifferentiation in adenocarcinoma [10].
Figure 2: OTUB1-TRIM28-MYC Ubiquitination Regulatory Axis in Cancer
USP22 in Oncogenic Signaling
USP22 regulates oncogenic signaling pathways to drive lethal tumor phenotypes by modulating nuclear receptor and oncogenic signaling [15]. In multiple xenograft models of human cancer, USP22 deregulation demonstrated control over androgen receptor (AR) accumulation and signaling, enhancing expression of critical target genes co-regulated by AR and MYC [15]. USP22 not only reprogrammed AR function but was sufficient to induce the transition to therapeutic resistance [15].
Table 3: Key Ubiquitination-Related Enzymes in Cancer Pathogenesis
| Enzyme | Class | Cancer Types Involved | Mechanism of Action | Therapeutic Implications |
|---|---|---|---|---|
| USP22 | Deubiquitinase | Prostate, Breast | Modulates AR and MYC signaling; promotes therapeutic resistance | Potential target for advanced disease |
| OTUB1 | Deubiquitinase | Multiple solid tumors | Regulates MYC pathway; influences oxidative stress | Impacts immunotherapy response |
| USP2 | Deubiquitinase | Gastric, Various | Stabilizes oncoproteins (EGFR, MDM2, CyclinD1) | Downregulation indicates poor prognosis in gastric cancer |
| UBE2S | Ubiquitin-conjugating E2 | Lung adenocarcinoma | Promotes tumor progression | Component of prognostic signature |
Clinical Applications and Therapeutic Implications
Prognostic Stratification
Ubiquitination-related gene signatures provide robust tools for prognostic stratification across multiple cancer types. The URPS effectively identifies patient subgroups with distinct survival outcomes and molecular characteristics [10]. Similarly, the URRS model in lung adenocarcinoma enables identification of high-risk patients who may benefit from more aggressive therapeutic interventions [11].
Predicting Treatment Response
Ubiquitination signatures demonstrate significant value in predicting response to various cancer treatments:
Immunotherapy Prediction: URPS serves as a novel biomarker for predicting immunotherapy response, potentially identifying patients more likely to benefit from immune checkpoint inhibitors [10].
Chemotherapy Sensitivity: In lung adenocarcinoma, the IC50 values of various chemotherapy drugs were significantly lower in the high URRS group, indicating increased sensitivity [11].
Targeted Therapy Development: Ubiquitination regulatory modifiers for traditionally "undruggable" targets like MYC can be screened through constructed pan-cancer ubiquitination regulatory networks, providing new therapeutic alternatives [10].
Technical Considerations and Limitations
When implementing ubiquitination-related prognostic models, several technical considerations merit attention:
Platform Compatibility: Ensure consistent normalization across different gene expression platforms when validating signatures in independent datasets.
Sample Quality: Use high-quality RNA samples with minimal degradation to ensure accurate quantification of ubiquitination-related genes.
Multicenter Validation: Prospective validation across multiple institutions is necessary to establish generalizability.
Functional Characterization: Computational predictions should be complemented with experimental validation to establish causal relationships.
The protocols and applications described herein provide a framework for investigating ubiquitination dysregulation in cancer pathogenesis and developing clinically relevant prognostic tools. As research in this field advances, ubiquitination-related signatures are poised to become increasingly important in precision oncology approaches.
Pan-Cancer Landscape of Ubiquitination-Related Genes (URGs)
The ubiquitin–proteasome system (UPS) represents a crucial post-translational modification mechanism that governs protein degradation and numerous non-proteolytic signaling pathways in eukaryotic cells [16]. Ubiquitination involves a sequential enzymatic cascade mediated by ubiquitin-activating enzymes (E1), ubiquitin-conjugating enzymes (E2), and ubiquitin ligases (E3), which collectively confer substrate specificity and facilitate the transfer of ubiquitin molecules to target proteins [17] [16]. The human genome encodes more than 600 E3 ubiquitin ligases that regulate diverse cellular processes, including cell cycle progression, DNA damage response, immune signaling, and metabolic reprogramming [17] [18]. Mounting evidence indicates that dysregulated ubiquitination pathways contribute significantly to tumor initiation, progression, metastasis, and therapeutic resistance across cancer types [17] [16] [10]. This application note provides a comprehensive pan-cancer analysis of ubiquitination-related genes (URGs), detailing prognostic signatures, molecular mechanisms, and experimental protocols for investigating URGs in cancer research.
Pan-Cancer Molecular Signatures and Prognostic Models
Ubiquitination-Related Prognostic Signatures Across Cancers
Recent multi-cancer analyses have revealed conserved ubiquitination-related molecular patterns that demonstrate significant prognostic value. A comprehensive study integrating data from 4,709 patients across 26 cohorts of five solid tumor types (lung cancer, esophageal cancer, cervical cancer, urothelial cancer, and melanoma) identified key nodes within the ubiquitination-modification network and established a conserved ubiquitination-related prognostic signature (URPS) [10]. This signature effectively stratified patients into high-risk and low-risk groups with distinct survival outcomes across all analyzed cancers and demonstrated potential for predicting immunotherapy response [10].
Table 1: Ubiquitination-Related Gene Signatures in Pan-Cancer Analysis
| Cancer Type | Key URGs Identified | Prognostic Value | Biological Implications |
|---|---|---|---|
| Pan-Cancer (5 solid tumors) | URPS signature | Stratified high/low risk groups; predicted immunotherapy response | Associated with MYC pathway, oxidative phosphorylation; influenced immune cell infiltration [10] |
| Triple-Negative Breast Cancer | 11-URG signature | Favorable predictive ability for overall survival | Correlated with immune infiltration; all immune cells and immune-related pathways higher in low-risk group [19] |
| Lung Adenocarcinoma | DTL, UBE2S, CISH, STC1 | Hazard Ratio = 0.54, 95% CI: 0.39–0.73 | Higher PD1/L1 expression, TMB, TNB, and TME scores in high-risk group; lower IC50 for chemotherapy drugs [11] |
| Breast Cancer | ATG5, FBXL20, DTX4, BIRC3, TRIM45, WDR78 | Significant survival differences (p < 0.05) in multiple datasets | Associated with Vd2 gd T cells and myeloid dendritic cells; linked to microbial diversity [20] |
The ubiquitination score derived from these analyses positively correlates with squamous or neuroendocrine transdifferentiation in adenocarcinoma and is associated with immunotherapy resistance and poor prognosis [10]. At single-cell resolution, URPS enabled precise classification of distinct cell types and correlated with macrophage infiltration within the tumor microenvironment [10]. Functional validation revealed that the OTUB1-TRIM28 ubiquitination axis plays a crucial role in modulating the MYC pathway and influencing patient prognosis [10].
Cancer-Type Specific URG Signatures
In addition to pan-cancer signatures, cancer-type specific URG models have demonstrated robust prognostic capabilities. In triple-negative breast cancer (TNBC), an 11-URG signature classified patients into clusters with significantly different immune signatures and overall survival outcomes [19]. Similarly, in lung adenocarcinoma, a 4-gene ubiquitination-related risk score (URRS) based on DTL, UBE2S, CISH, and STC1 expression effectively stratified patients, with high URRS associated with worse prognosis (Hazard Ratio = 0.54, 95% CI: 0.39–0.73, p < 0.001) [11]. This signature was validated across six external cohorts and correlated with higher PD-1/PD-L1 expression, tumor mutation burden (TMB), tumor neoantigen load (TNB), and tumor microenvironment scores [11].
Molecular Mechanisms and Pathogenic Pathways
Ubiquitination in Hallmarks of Cancer
Ubiquitination regulates fundamental cancer hallmarks through diverse molecular mechanisms. E3 ubiquitin ligases function as critical regulatory nodes controlling protein abundance and activity in a timely and specific manner, with frequent deregulation observed in human cancers through genetic, epigenetic, or post-translational alterations [17]. The schematic below illustrates the ubiquitination enzyme cascade and its role in cancer-relevant pathways:
Diagram 1: Ubiquitination enzyme cascade and cancer-relevant pathways. The E1-E2-E3 enzymatic cascade leads to substrate ubiquitination and proteasomal degradation. E3 ligases specifically target cancer-relevant proteins including RTKs, p53, MYC pathway components, and immune checkpoints.
Key URG Mechanisms in Oncogenesis
Specific URGs demonstrate distinct mechanistic roles in cancer pathogenesis. UBR5, an E3 ubiquitin ligase frequently amplified in cancers, promotes tumor growth through multiple mechanisms, including AKT signaling activation, immune evasion through PD-L1 transactivation, and recruitment of immunosuppressive tumor-associated macrophages [21] [22]. In lung adenocarcinoma, UBR5 is overexpressed and its loss decreases cell viability, clonogenic potential, and in vivo tumor growth, accompanied by reduced AKT phosphorylation [22]. The interaction between ubiquitination and key cancer pathways extends to metabolic reprogramming, with ubiquitination scores showing enrichment in oxidative phosphorylation and MYC signaling pathways across multiple cancer types [10].
Experimental Protocols and Methodologies
Protocol for Constructing URG Prognostic Signatures
The establishment of ubiquitination-related prognostic models follows a standardized bioinformatics workflow that can be applied across cancer types, as illustrated below:
Diagram 2: Workflow for constructing URG prognostic signatures. The process encompasses data acquisition, pattern discovery, signature development, and clinical validation phases.
Data Collection and Preprocessing
- Data Sources: Obtain RNA sequencing data and corresponding clinical information from public repositories such as The Cancer Genome Atlas (TCGA), Gene Expression Omnibus (GEO), and dbGaP [19] [11]. The METABRIC database is particularly valuable for breast cancer studies [19].
- URG Compilation: Curate ubiquitination-related genes from specialized databases including the Ubiquitin and Ubiquitin-like Conjugation Database (UUCD) and iUUCD 2.0, which comprehensively catalog E1, E2, E3 enzymes, and deubiquitinases [19] [11].
- Data Preprocessing: Normalize gene expression data using FPKM or TPM normalization. Remove batch effects using the ComBat function in the "sva" R package. Exclude patients with survival time less than 30 days to avoid perioperative mortality bias [19] [11].
Molecular Classification and Signature Development
- Unsupervised Clustering: Perform non-negative matrix factorization (NMF) or consensus clustering using the "ConsensusClusterPlus" R package to identify molecular subtypes based on URG expression patterns [19] [11]. Determine optimal cluster number (k) using cophenetic, dispersion, and silhouette metrics.
- Differential Expression Analysis: Identify differentially expressed URGs between molecular subtypes using the "limma" R package, with adjusted p-value ≤ 0.05 and |log2FC| ≥ 0.8 as significance thresholds [11].
- Prognostic Gene Selection: Apply univariate Cox regression (p < 0.01), Random Survival Forests (variable importance > 0.25), and LASSO-Cox regression to identify robust prognostic URGs [19] [11]. Use 10-fold cross-validation to determine the optimal lambda value in LASSO analysis.
- Risk Score Calculation: Construct the prognostic signature using the formula: Risk score = Σ(βi × Expi), where βi represents the coefficient from multivariate Cox regression and Expi represents gene expression value [11].
Model Validation and Clinical Correlation
- Validation Cohorts: Validate the prognostic model in independent external datasets. For TNBC, the METABRIC cohort can serve as training set with GSE58812 as validation [19]. For lung adenocarcinoma, validate using multiple GEO datasets (GSE30219, GSE37745, GSE41271, GSE42127, GSE68465, GSE72094) [11].
- Survival Analysis: Assess prognostic performance using Kaplan-Meier curves and log-rank tests. Evaluate predictive accuracy via time-dependent receiver operating characteristic (ROC) analysis and calculate area under the curve (AUC) values [19] [11].
- Clinical Utility Assessment: Correlate risk scores with clinicopathological features, immune cell infiltration (using CIBERSORT, MCP-counter, or ESTIMATE algorithms), tumor mutation burden, and therapy response [19] [11].
Protocol for Functional Validation of URGs
In Vitro Functional Assays
- Gene Manipulation: Perform UBR5 knockdown using shRNA or siRNA in lung adenocarcinoma cell lines (A549, H460) [22]. Use lentiviral transduction for stable knockdown and confirm efficiency via Western blotting.
- Cell Viability Assessment: Conduct cell viability assays using Alamar Blue reagent. Plate 2,000 cells per well in 96-well plates post-knockdown and measure fluorescence daily for four consecutive days [22].
- Clonogenic Assays: Seed 1,000 transfected cells in 6-well plates and culture for 10-14 days with medium changes every two days. Fix colonies with ethanol, stain with crystal violet, and count colonies exceeding 50 cells [22].
- Signaling Pathway Analysis: Analyze downstream signaling pathways (e.g., AKT, MAPK) via Western blotting following URG perturbation. Use antibodies targeting total and phosphorylated proteins (e.g., pAKT S473, total AKT) [22].
In Vivo Tumorigenesis assays
- Xenograft Models: Subcutaneously inject 1.25 × 10^5 UBR5-knockdown or control A549 cells suspended in 200μL PBS into each flank of NRGS mice (NOD/RAG1/2−/−IL2Rγ−/−) [22].
- Tumor Monitoring: Measure tumor dimensions twice weekly using calipers. Calculate tumor volume using the formula: Volume = (Length × Width^2)/2. Continue monitoring for 4-6 weeks or until tumors reach ethical endpoint size [22].
- Statistical Analysis: Compare tumor volumes between experimental groups using Wilcoxon paired t-test. Perform one-way ANOVA for multiple group comparisons in in vitro studies [22].
The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential Research Reagents for URG Investigation
| Reagent Category | Specific Examples | Research Application | Technical Notes |
|---|---|---|---|
| Bioinformatics Tools | "sva" R package (batch effect removal), "ConsensusClusterPlus" (molecular subtyping), "glmnet" (LASSO regression), "ESTIMATE" (TME scoring) | Computational analysis of URG signatures and prognostic model development | Apply ComBat algorithm for batch correction; use 10-fold cross-validation in LASSO [19] [11] |
| Cell Line Models | A549, H460 (lung adenocarcinoma); MDA-MB-231 (TNBC); HEK293T (protein interaction studies) | Functional validation of URG mechanisms in relevant cancer contexts | Regularly authenticate cell lines by STR profiling; routinely test for mycoplasma contamination [22] |
| Antibodies | UBR5 (Bethyl, A300-573A), pAKT S473 (CST, 4060), FLAG (CST, 14793), GAPDH (Santa Cruz, sc47724) | Protein expression analysis, immunoprecipitation, and Western blotting | Validate antibodies for specific applications; use appropriate loading controls [22] |
| Animal Models | NRGS mice (NOD/RAG1/2−/−IL2Rγ−/−), nude mice | In vivo tumorigenesis and therapeutic efficacy studies | Monitor tumor volumes twice weekly; adhere to ethical endpoint guidelines [22] |
| Ubiquitination Assays | Anti-K-ε-GG antibody-based enrichment, LC-MS/MS, co-immunoprecipitation | Identification of ubiquitination sites and ubiquitinated protein substrates | Use ubiquitin remnant motif analysis (A-X(1/2/3)-K*); validate findings with DUB treatments [23] |
Clinical Applications and Therapeutic Implications
URG Signatures in Precision Oncology
Ubiquitination-related gene signatures demonstrate significant clinical utility in prognostication and treatment stratification. The 11-URG signature in TNBC enables patient stratification into high-risk and low-risk groups with distinct overall survival, with the low-risk group exhibiting enhanced immune cell infiltration and immune-related pathway activation [19]. Similarly, the 4-gene URRS in lung adenocarcinoma identifies patients with higher tumor mutation burden, neoantigen load, and PD-1/PD-L1 expression who may benefit from immunotherapy [11]. These signatures can be incorporated into nomograms combining risk scores with clinicopathological characteristics to enhance predictive accuracy for clinical decision-making [19].
Therapeutic Targeting of Ubiquitination Pathways
The ubiquitin-proteasome system presents promising therapeutic targets, with several clinical strategies emerging:
- Proteasome Inhibitors: Bortezomib, carfilzomib, and ixazomib are FDA-approved for multiple myeloma and mantle cell lymphoma, demonstrating the clinical viability of UPS targeting [16].
- Targeted Protein Degradation: Proteolysis-targeting chimeras (PROTACs) and molecular glues represent innovative approaches that hijack the ubiquitin system to degrade disease-causing proteins [18]. These technologies enable targeting of previously "undruggable" oncoproteins and can overcome drug resistance mechanisms.
- E3 Ligase Modulation: Specific E3 ligases such as MDM2, IAPs, VHL, and CRBN are being exploited for targeted protein degradation approaches [18]. UBR5 represents a promising therapeutic target, with knockdown studies demonstrating reduced tumor growth in lung adenocarcinoma models [22].
The integration of URG signatures with therapeutic response prediction holds particular promise for immunotherapy applications. URPS demonstrates potential for identifying patients likely to benefit from immune checkpoint blockade across multiple cancer types [10]. Furthermore, ubiquitination regulates PD-L1 expression through mechanisms such as UBR5-mediated transactivation, suggesting combination therapeutic strategies that simultaneously target URGs and immune checkpoints [21].
The pan-cancer landscape of ubiquitination-related genes reveals conserved molecular patterns with significant prognostic and therapeutic implications. URG signatures consistently stratify patients across cancer types and demonstrate associations with tumor microenvironment composition, therapy response, and clinical outcomes. Standardized protocols for URG signature development and validation enable robust biomarker discovery, while functional characterization of specific URGs such as UBR5 provides mechanistic insights and reveals novel therapeutic targets. The integration of URG signatures into clinical decision-making frameworks and the development of URG-targeted therapies represent promising avenues for advancing precision oncology in the coming years.
URG Expression Patterns and Their Association with Clinical Outcomes
Ubiquitination-Related Genes (URGs) represent a critical class of molecules involved in the post-translational regulation of protein stability and function. Among these, Upregulated Gene 4 (URG4/URGCP) has emerged as a significant oncogene across multiple cancer types. This application note details the expression patterns of URG4 and its association with clinical outcomes, providing researchers with standardized protocols for evaluating URG4 as a prognostic biomarker. The content is framed within the broader context of developing ubiquitination-related gene signatures for cancer prognosis research, with particular relevance to researchers, scientists, and drug development professionals working in oncology biomarker discovery.
Quantitative Analysis of URG4 Expression and Clinical Correlations
URG4 Expression Patterns Across Cancers
URG4 demonstrates differential overexpression in multiple malignancies compared to normal tissues. Studies have consistently shown that elevated URG4 expression correlates with advanced disease progression and poor clinical outcomes.
Table 1: URG4 Expression and Clinical Correlations in Various Cancers
| Cancer Type | Sample Size | High URG4 Expression | Key Clinical Correlations | Prognostic Impact |
|---|---|---|---|---|
| Gastric Cancer [24] | 61 patients | 37 (61%) | Significantly correlated with T stage (p<0.005) and lymphovascular invasion (p<0.005) | Significant association with 2-year survival (p<0.05) |
| Cervical Cancer [25] | 167 patients | 59 (35.13%) | Correlated with clinical stage (p<0.0001), tumor size (p=0.012), T classification (p=0.023), lymph node metastasis (p=0.001) | Shorter OS and DFS; independent prognostic factor |
| Multiple Cancers [24] [25] | Various | Varies by cancer | Associated with tumor progression, metastasis, recurrence in gastric, bladder, lung, colon, thyroid, prostate cancers, glioblastoma, neuroblastoma, leukemia | Poor survival outcomes across cancer types |
Statistical Analysis of URG4 Clinical Impact
The quantitative assessment of URG4's clinical significance involves several statistical measures that researchers should incorporate in their analyses:
Table 2: Statistical Measures for Quantitative Data Analysis in URG Studies
| Statistical Measure | Calculation Method | Application in URG Research | Advantages/Limitations |
|---|---|---|---|
| Mean | Sum of observations divided by number of observations [26] | Comparing average URG4 expression levels between tumor and normal tissues | Uses all data values but vulnerable to outliers |
| Median | Middle value of ordered data [26] | Describing central tendency of URG4 expression scores | Not affected by outliers; better for skewed data |
| Standard Deviation | Square root of the average squared deviations from the mean [26] | Measuring variability in URG4 expression within patient cohorts | Useful for establishing reference intervals; vulnerable to outliers |
| Hazard Ratio (HR) | Coefficient from Cox proportional hazards model | Quantifying URG4's impact on survival outcomes | Provides effect size for prognostic impact |
| p-value | Probability of obtaining test results at least as extreme as observed | Determining statistical significance of URG4 correlations | Standard threshold of p<0.05 typically used |
Experimental Protocols for URG4 Analysis
Immunohistochemistry (IHC) Protocol for URG4 Detection
Principle: This protocol enables the detection and semi-quantification of URG4 protein expression in formalin-fixed, paraffin-embedded (FFPE) tissue sections [24] [25].
Reagents Required:
- Primary antibody: Rabbit polyclonal URG4 antibody (e.g., Abcam Cat No: 103,323)
- Secondary detection system: Avidin-biotin-peroxidase complex
- Substrate: Diaminobenzidine (DAB)
- Counterstain: Mayer's hematoxylin
- Antigen retrieval solution (e.g., citrate buffer, pH 6.0)
Procedure:
- Sectioning: Cut paraffin-embedded tumor tissue blocks at 4-micron thickness.
- Deparaffinization and Rehydration:
- Incubate slides at 60°C for 30 minutes
- Deparaffinize in xylene (3 changes, 5 minutes each)
- Rehydrate through graded ethanol series (100%, 95%, 70%) to distilled water
- Antigen Retrieval:
- Perform heat-induced epitope retrieval in citrate buffer (pH 6.0)
- Heat in microwave or pressure cooker for 10-20 minutes
- Cool slides to room temperature for 30 minutes
- Immunostaining:
- Block endogenous peroxidase activity with 3% H₂O₂ for 10 minutes
- Apply primary URG4 antibody at 1:100 dilution for 60 minutes at room temperature
- Apply biotinylated secondary antibody for 30 minutes
- Apply avidin-biotin-peroxidase complex for 30 minutes
- Develop with DAB substrate for 5-10 minutes
- Counterstaining and Mounting:
- Counterstain with Mayer's hematoxylin for 1-2 minutes
- Dehydrate through graded alcohols and xylene
- Mount with permanent mounting medium
Scoring System: [24]
- Frequency of positive cells: None: 0; 1-25%: 1; 26-50%: 2; >50%: 3
- Staining intensity: None: 0; Mild: 1; Moderate: 2; Strong: 3
- Total Score: Multiply frequency and intensity scores
- Interpretation: Scores 0-4: Low URG4 expression; Scores 6-9: High URG4 expression
RNA Extraction and Quantitative PCR Protocol
Principle: This protocol enables quantification of URG4 mRNA expression levels in cell lines and tissue samples [25].
Reagents Required:
- TRIzol reagent for RNA extraction
- DNase I, RNase-free
- Reverse transcription kit with random hexamers
- Quantitative PCR master mix
- URG4-specific primers:
- Sense: 5'-CGCAATCATCTCCTTCCATT-3'
- Antisense: 5'-TCCACGAAGTCCTCGTTCTC-3'
- Housekeeping gene primers (e.g., GAPDH, β-actin)
Procedure:
- RNA Extraction:
- Homogenize tissue or cells in TRIzol reagent
- Add chloroform (0.2 ml per 1 ml TRIzol) and centrifuge at 12,000 × g for 15 minutes at 4°C
- Transfer aqueous phase to fresh tube
- Precipitate RNA with isopropyl alcohol, wash with 75% ethanol
- Dissolve RNA in RNase-free water
- DNA Digestion:
- Treat RNA samples with DNase I to remove genomic DNA contamination
- Inactivate DNase by heat treatment or EDTA
- cDNA Synthesis:
- Use 2 μg of total RNA for reverse transcription
- Incubate with random hexamers and reverse transcriptase at appropriate conditions
- Quantitative PCR:
- Prepare reaction mix with cDNA, primers, and PCR master mix
- Run amplification with following conditions:
- Initial denaturation: 95°C for 10 minutes
- 40 cycles of: 95°C for 15 seconds, 60°C for 1 minute
- Calculate relative expression using 2^(-ΔΔCt) method
Statistical Analysis Protocol for Clinical Correlations
Principle: This protocol provides a standardized approach for analyzing associations between URG4 expression and clinical parameters [24] [26].
Software Requirements:
- Statistical software (e.g., R 4.2.2, SPSS, GraphPad Prism)
- Appropriate packages for survival analysis (e.g., "survival" package in R)
Procedure:
- Data Preparation:
- Code clinical parameters appropriately (e.g., T stage as ordinal variable)
- Classify URG4 expression as high/low based on predetermined cut-off
- Descriptive Statistics:
- Calculate mean, median, standard deviation for continuous variables
- Generate frequency tables for categorical variables
- Association Analysis:
- Use Chi-square or Fisher's exact tests for categorical variables (e.g., URG4 expression vs. lymph node status)
- Apply Wilcoxon rank-sum test for continuous variables between groups
- Survival Analysis:
- Perform Kaplan-Meier analysis for overall survival and disease-free survival
- Use log-rank test to compare survival curves between high and low URG4 groups
- Conduct univariate and multivariate Cox regression analyses to identify independent prognostic factors
- Interpretation:
- Consider p-value < 0.05 as statistically significant
- Report hazard ratios with 95% confidence intervals for Cox models
Visualization of Experimental Workflow
Figure 1: Experimental workflow for URG4 expression analysis and clinical correlation studies. The diagram illustrates the integrated approach combining laboratory techniques with clinical data analysis to validate URG4 as a prognostic biomarker.
URG4 in Cancer Signaling Pathways
Figure 2: URG4 signaling pathways in cancer progression. The diagram illustrates the molecular mechanisms through which URG4 overexpression drives tumor aggressiveness and poor clinical outcomes.
Research Reagent Solutions
Table 3: Essential Research Reagents for URG4 Investigation
| Reagent Category | Specific Product/Example | Function/Application | Technical Notes |
|---|---|---|---|
| Primary Antibodies | Rabbit polyclonal URG4 antibody (Abcam Cat No: 103,323) [24] | Detection of URG4 protein in IHC and Western blot | Optimal dilution 1:100 for IHC; validate specificity with controls |
| PCR Primers | URG4-specific primers: Sense 5'-CGCAATCATCTCCTTCCATT-3', Antisense 5'-TCCACGAAGTCCTCGTTCTC-3' [25] | mRNA quantification via RT-qPCR | Verify amplification efficiency; use appropriate housekeeping genes |
| RNA Extraction Kits | TRIzol reagent [25] | RNA isolation from cells and tissues | Maintain RNase-free conditions; measure RNA quality/purity |
| Statistical Software | R software (version 4.2.2 or higher) [24] | Statistical analysis and survival curves | Use "survival" package for Kaplan-Meier and Cox regression analyses |
| Cell Lines | Cancer cell lines relevant to studied cancer type (e.g., gastric, cervical) [25] | In vitro validation studies | Authenticate cell lines regularly; monitor for contamination |
URG4 represents a promising ubiquitination-related oncogene with significant prognostic value across multiple cancer types. The standardized protocols and analytical frameworks presented in this application note provide researchers with comprehensive methodologies for investigating URG4 expression patterns and their clinical associations. The consistent correlation between high URG4 expression and poor survival outcomes highlights its potential utility as a prognostic biomarker and therapeutic target. Future research should focus on validating these findings in larger prospective cohorts and elucidating the precise molecular mechanisms through which URG4 promotes tumor progression.
The Rationale for Multi-Gene URG Signatures Over Single-Gene Biomarkers
In the field of cancer prognosis research, the transition from single-gene biomarkers to multi-gene signatures represents a paradigm shift toward embracing molecular complexity. Traditional single-gene biomarkers, while valuable for specific contexts, often fail to capture the heterogeneous nature of carcinogenesis and tumor progression [27]. Ubiquitination-related genes (URGs) constitute a particularly compelling class of biomarkers, as they regulate nearly all biological processes—including DNA damage repair, cell-cycle regulation, signal transduction, and protein degradation—through the ubiquitin-proteasome system (UPS) [27]. However, relying on individual URGs for prognostic predictions presents significant limitations, as the complex, interconnected nature of ubiquitination pathways means that no single gene can adequately represent the system's overall behavior.
Multi-gene URG signatures address this limitation by providing a more comprehensive view of the biological state. By simultaneously evaluating multiple genes, these signatures can capture pathway activity, identify robust prognostic patterns, and ultimately offer more accurate predictions of patient outcomes [27] [28]. This approach aligns with the understanding that cancer is driven by complex molecular networks rather than isolated genetic alterations.
Theoretical Foundation: Comparative Advantages of Multi-Gene Signatures
Enhanced Prognostic Accuracy and Robustness
Multi-gene signatures demonstrate superior performance in prognostic stratification compared to single-gene approaches by capturing cooperative biological effects. Where single-gene biomarkers may show variable performance across different patient populations due to tumor heterogeneity, multi-gene signatures maintain more consistent prognostic value by aggregating signals from multiple pathways [28]. This robustness is particularly evident in large-scale validation studies, where multi-gene signatures have demonstrated stable performance across diverse clinical cohorts and microarray platforms [29].
Biological Comprehensiveness
The molecular complexity of carcinogenesis involves coordinated dysregulation across multiple biological pathways. Multi-gene URG signatures can simultaneously reflect various aspects of tumor biology, including immune response, cellular stress adaptation, and metabolic reprogramming [27]. This comprehensive perspective enables more accurate patient stratification and provides insights into the underlying biological mechanisms driving disease progression.
Table 1: Comparative Analysis of Single-Gene vs. Multi-Gene Biomarker Approaches
| Characteristic | Single-Gene Biomarkers | Multi-Gene Signatures |
|---|---|---|
| Biological Coverage | Limited to single pathway components | Comprehensive coverage across multiple pathways |
| Prognostic Stability | Vulnerable to tumor heterogeneity | Robust across diverse populations |
| Technical Validation | Straightforward but limited | Complex but more informative |
| Clinical Utility | Often insufficient for standalone decisions | Better suited for clinical stratification |
| Mechanistic Insight | Narrow focus on specific functions | Systems-level understanding |
Experimental Protocols for Multi-Gene URG Signature Development
Protocol 1: Identification and Prioritization of Ubiquitination-Related Genes
Purpose: To systematically identify differentially expressed URGs with potential prognostic significance from transcriptomic datasets.
Materials and Reagents:
- RNA sequencing data from tumor and matched normal tissues
- Ubiquitin-related gene sets from validated databases (e.g., GeneCards)
- Differential expression analysis tools (DESeq2 package)
- Functional annotation databases (GO, KEGG)
Procedure:
- Data Acquisition: Obtain RNA-seq data from both tumor and normal adjacent tissues. For cervical cancer research, the TCGA-GTEx-CESC dataset provides 304 tumor and 13 normal samples [27].
- Differential Expression Analysis: Identify differentially expressed genes (DEGs) using DESeq2 with threshold p-value <0.05 and \|log2Fold Change\| > 0.5 [27].
- Ubiqutination Gene Filtering: Extract a comprehensive list of ubiquitination-related genes (UbLGs) from GeneCards database using search term "Ubiquitin-like modifiers" with relevance score ≥3 [27].
- Intersection Analysis: Identify crossover genes by intersecting DEGs with UbLGs to obtain ubiquitination-related differentially expressed genes.
- Functional Enrichment: Perform GO and KEGG pathway enrichment analysis using clusterProfiler package (p.adjust <0.05 & count >2) to identify biological processes and pathways significantly enriched in the crossover genes [27].
Technical Notes: The threshold of \|log2Fold Change\| > 0.5 represents a balance between detecting biologically relevant changes and maintaining statistical stringency. For studies requiring higher specificity, this threshold can be increased to 1.0.
Protocol 2: Prognostic Model Construction and Validation
Purpose: To develop a multi-gene risk score model and validate its prognostic performance in independent datasets.
Materials and Reagents:
- Clinical survival data matched with expression profiles
- Statistical computing environment (R Studio)
- Survival analysis packages (survival, glmnet)
- Validation datasets from GEO database
Procedure:
- Feature Selection: Subject crossover genes to univariate Cox regression analysis (p < 0.05) to identify genes with significant prognostic value [27].
- LASSO Regularization: Apply Least Absolute Shrinkage and Selection Operator (LASSO) Cox regression to the significant genes from univariate analysis to prevent overfitting and select the most robust biomarkers [27].
- Risk Score Calculation: Construct a prognostic model using the formula: Risk score = Σ(coefi * expressioni), where coefi represents the coefficient derived from multivariate Cox regression for each gene, and expressioni represents the normalized expression value of each gene [27].
- Patient Stratification: Divide patients into high-risk and low-risk groups based on the median risk score or optimal cutoff determined by survival analysis.
- Model Validation: Validate the prognostic model in independent testing sets and external validation cohorts (e.g., GSE52903 for cervical cancer) using time-dependent ROC analysis for 1, 3, and 5-year survival [27].
Technical Notes: The ratio of 7:3 for training-to-testing set split provides sufficient data for model development while maintaining adequate validation power. For smaller datasets, leave-one-out cross-validation or repeated k-fold cross-validation is recommended.
Protocol 3: Immune Microenvironment and Therapeutic Response Analysis
Purpose: To characterize the tumor immune microenvironment and predict therapeutic responses based on the URG signature.
Materials and Reagents:
- Immune cell infiltration estimation algorithms (CIBERSORT, ESTIMATE, xCell)
- Immunotherapy response predictors
- Drug sensitivity databases (GDSC, CMap)
Procedure:
- Immune Infiltration Profiling: Estimate the abundance of various immune cell types in the tumor microenvironment using multiple algorithms (CIBERSORT, ESTIMATE, MCPcounter, xCell, ssGSEA) [30] [27].
- Immune Checkpoint Analysis: Compare expression of critical immune checkpoint molecules (e.g., PD-1, PD-L1, CTLA-4) between high-risk and low-risk groups [27].
- Drug Sensitivity Prediction: Correlate risk scores with drug sensitivity data from GDSC database to identify potential therapeutic vulnerabilities [30].
- Connectivity Mapping: Utilize Connectivity Map (CMap) approach to identify small molecules that might reverse the high-risk gene expression signature [30].
Technical Notes: Using multiple complementary algorithms for immune infiltration analysis provides a more comprehensive and reliable assessment than any single method.
Case Study: A 5-Gene URG Signature in Cervical Cancer
A recent study demonstrated the practical application of multi-gene URG signatures in cervical cancer, identifying five key biomarkers (MMP1, RNF2, TFRC, SPP1, and CXCL8) through the protocols described above [27]. The risk score model constructed from these biomarkers effectively predicted patient survival rates with AUC values exceeding 0.6 for 1, 3, and 5-year survival [27]. Experimental validation using RT-qPCR confirmed that MMP1, TFRC, and CXCL8 were significantly upregulated in tumor tissues compared to normal controls [27].
Immune microenvironment analysis revealed that 12 types of immune cells—including memory B cells and M0 macrophages—as well as four immune checkpoints exhibited significant differences between the high-risk and low-risk groups defined by the URG signature [27]. This comprehensive analysis demonstrates how multi-gene URG signatures can simultaneously inform about prognosis, tumor biology, and potential therapeutic strategies.
Table 2: Essential Research Reagent Solutions for URG Signature Development
| Reagent/Resource | Function | Application Context |
|---|---|---|
| DESeq2 Package | Differential expression analysis | Identifying ubiquitination-related DEGs |
| LASSO-Cox Model | Regularized regression | Selecting robust prognostic genes |
| CIBERSORT Algorithm | Immune cell quantification | Tumor microenvironment characterization |
| GDSC Database | Drug sensitivity resource | Predicting therapeutic response |
| clusterProfiler | Functional enrichment | Pathway analysis of signature genes |
Visualization of Workflows and Signaling Pathways
Workflow for URG Signature Development: This diagram illustrates the comprehensive pipeline for developing and validating multi-gene URG signatures, from initial data collection through final mechanistic insights.
Ubiquitin-Proteasome Signaling Pathway: This visualization represents the core ubiquitination machinery and its connection to critical cellular processes, highlighting how multi-gene signatures capture system-wide dynamics rather than isolated components.
The rationale for employing multi-gene URG signatures over single-gene biomarkers is firmly grounded in their ability to capture the complexity of cancer biology and provide more robust, clinically actionable prognostic information. The protocols outlined herein provide a standardized framework for developing and validating these signatures, with particular emphasis on ubiquitination-related genes that play fundamental roles in cellular regulation.
Future developments in this field will likely focus on integrating multi-omics data—including genomic, epigenomic, and proteomic information—to further enhance the predictive power of these signatures [30] [28]. Additionally, the application of advanced machine learning methods, such as the ABF-CatBoost integration described in colon cancer research [31], promises to unlock even more sophisticated pattern recognition capabilities for prognostic stratification.
As these methodologies continue to evolve, multi-gene URG signatures are poised to become increasingly integral to personalized cancer management, enabling more precise prognosis prediction and tailored therapeutic interventions across diverse cancer types.
Constructing and Applying URG Signatures: A Step-by-Step Guide
The discovery of ubiquitination-related gene (URG) signatures for cancer prognosis is fundamentally dependent on the integrated use of large-scale, publicly available databases. The Cancer Genome Atlas (TCGA), Gene Expression Omnibus (GEO), and the Integrated Annotations for Ubiquitin and Ubiquitin-like Conjugation Database (IUUCD) collectively provide the essential data infrastructure for this research. These resources enable researchers to identify and validate molecular patterns linked to patient survival across various cancer types, forming the foundation for prognostic model development.
TCGA provides comprehensive multi-omics data and clinical information across numerous cancer types, serving as the primary source for initial model training and discovery. GEO complements TCGA by providing additional validation datasets from independent studies, enhancing the robustness of findings. The IUUCD serves as a specialized curated repository that defines the universe of genes involved in ubiquitination pathways, with one study utilizing 807 URGs from this database for cervical cancer analysis [32]. The synergy between these databases enables a systematic research pipeline from gene selection through model validation, firmly grounding URG signature development in large-scale genomic data.
Database Specifications and Access Protocols
Database Characteristics and Applications
Table 1: Core Database Specifications for URG Prognostic Research
| Database | Primary Content | Key Features for URG Research | Access Methods |
|---|---|---|---|
| The Cancer Genome Atlas (TCGA) | RNA-seq, clinical data, mutations, survival data | Pan-cancer genomic profiles; clinical outcome data; standardized processing | GDC Data Portal (portal.gdc.cancer.gov); GDC API; TCGA-specific R packages |
| Gene Expression Omnibus (GEO) | Microarray and RNA-seq datasets from independent studies | Validation cohorts; platform diversity; independent patient populations | Web interface (ncbi.nlm.nih.gov/geo); GEOquery R package; manually curated datasets |
| IUUCD (Integrated Annotations for Ubiquitin and Ubiquitin-like Conjugation Database) | Curated ubiquitination-related genes (E1, E2, E3 enzymes, deubiquitinases) | Comprehensive URG lists; functional classifications; conjugation pathway annotations | Web interface (iuucd.biocuckoo.org); downloadable gene lists |
Data Retrieval and Processing Workflows
TCGA Data Access Protocol:
- Data Identification: Access the GDC Data Portal and identify relevant cancer cohort (e.g., TCGA-CESC for cervical cancer, TCGA-HNSCC for head and neck cancer)
- Data Download: Retrieve RNA-seq data (FPKM or TPM normalized), clinical metadata, and somatic mutation data using the GDC Data Transfer Tool or API
- Data Processing: Convert gene identifiers, filter out low-expression genes, and normalize data if necessary using R/Bioconductor packages
- Clinical Data Integration: Merge expression matrices with survival data and other clinical parameters (age, stage, grade) for analysis
GEO Data Access Protocol:
- Dataset Identification: Search GEO using keywords (e.g., "cervical cancer," "expression profiling") and platform identifiers
- Data Retrieval: Download Series Matrix Files using the GEOquery R package or manually from the website
- Data Normalization: Apply appropriate normalization methods based on platform (e.g., RMA for microarray, TPM for RNA-seq)
- Batch Effect Assessment: Evaluate and correct for technical variations between different datasets when integrating multiple studies
IUUCD Gene List Curation:
- URG Compilation: Download comprehensive URG lists from IUUCD, typically containing 800-2,800 genes depending on inclusion criteria [32] [33]
- Functional Categorization: Classify genes into E1 activating enzymes, E2 conjugating enzymes, E3 ligases, and deubiquitinating enzymes
- Custom Filtering: Apply relevance scoring when needed (e.g., GeneCards relevance score ≥5) to focus on high-confidence URGs [34]
Integrated Analytical Workflow for URG Signature Development
The development of URG prognostic signatures follows a multi-stage analytical process that integrates data from all three databases. The workflow below illustrates this comprehensive analytical pipeline:
Key Experimental Protocols in URG Signature Research
Bioinformatics and Statistical Methodology
Differential Expression Analysis Protocol:
- Data Preparation: Normalize raw count data using DESeq2 or edgeR for RNA-seq data
- Expression Filtering: Filter genes with low expression across samples (e.g., counts <10 in >90% of samples)
- Statistical Testing: Identify differentially expressed URGs using moderated t-tests (limma package) or negative binomial tests (DESeq2) with thresholds of |log2FC| > 0.5 and adjusted p-value < 0.05 [27]
- Result Integration: Intersect differentially expressed genes with IUUCD-derived URG lists to identify candidate prognostic genes
Consensus Clustering Protocol:
- Gene Selection: Extract expression profiles of prognosis-associated URGs identified through univariate Cox regression
- Cluster Algorithm: Apply k-means clustering with 1000 iterations using ConsensusClusterPlus R package
- Optimal Cluster Determination: Determine optimal cluster number (k) based on cumulative distribution function (CDF) curve analysis [32]
- Survival Validation: Validate clusters using Kaplan-Meier survival analysis to ensure clinical relevance of molecular subtypes
WGCNA Co-expression Network Analysis:
- Network Construction: Build signed co-expression networks using blockwiseModules function in WGCNA R package
- Soft Threshold Selection: Choose appropriate soft-thresholding power (typically 9-12) based on scale-free topology fit > 0.9 [32]
- Module Identification: Identify co-expression modules using hierarchical clustering and dynamic tree cutting
- Module-Trait Association: Correlate module eigengenes with clinical traits and molecular subtypes to select hub modules for further analysis
LASSO Cox Regression Modeling:
- Variable Input: Input prognosis-associated URGs from univariate analysis (p < 0.05) into glmnet R package
- Parameter Tuning: Perform 10-fold cross-validation to identify optimal lambda (λ) value that minimizes partial likelihood deviance
- Gene Selection: Retain non-zero coefficient genes to construct parsimonious prognostic signature
- Risk Score Calculation: Compute risk score using formula: Risk Score = Σ(Coefi × Expri), where Coefi is LASSO-derived coefficient and Expri is gene expression value [32] [35]
Experimental Validation Techniques
RT-qPCR Validation Protocol:
- RNA Extraction: Isolate total RNA from tumor and adjacent normal tissues using TRIzol reagent
- cDNA Synthesis: Reverse transcribe 1μg RNA using M-MuLV reverse transcriptase with oligo(dT) primers
- qPCR Amplification: Perform reactions in triplicate using SYBR Green master mix on real-time PCR system
- Data Analysis: Calculate relative expression using 2^(-ΔΔCt) method with 18S rRNA or GAPDH as reference genes [27] [36]
Transwell Migration Assay Protocol:
- Cell Preparation: Seed serum-starved cancer cells (e.g., HeLa) in upper chamber of 8μm transwell inserts
- Chemoattractant Application: Add complete culture medium to lower chamber as chemoattractant
- Incubation: Incubate for 24 hours at 37°C with 5% CO₂
- Staining and Quantification: Fix migrated cells with methanol, stain with crystal violet, and count under microscope [32]
Western Blot Analysis Protocol:
- Protein Extraction: Lyse cells in RIPA buffer with protease and phosphatase inhibitors
- Protein Separation: Resolve 20-30μg protein by SDS-PAGE and transfer to PVDF membranes
- Antibody Incubation: Block with 5% BSA, incubate with primary antibodies (e.g., anti-USP21, anti-FBXO45) overnight at 4°C, then with HRP-conjugated secondary antibodies
- Detection: Visualize using enhanced chemiluminescence substrate and imaging system [35] [37]
Signaling Pathways and Biological Mechanisms
URG signatures frequently implicate specific biological pathways in cancer progression. The diagram below illustrates key pathways identified through URG prognostic signature research:
Research Reagent Solutions
Table 2: Essential Research Reagents for URG Prognostic Signature Validation
| Reagent Category | Specific Examples | Research Application | Technical Notes |
|---|---|---|---|
| Cell Lines | HeLa (cervical cancer), A2780 (ovarian cancer), HNSC lines | Functional validation of URG roles in proliferation, migration | Authenticate with STR profiling; regular mycoplasma testing |
| Antibodies | Anti-USP21, Anti-FBXO45, Anti-CDC20, Anti-UbcH10 | Protein expression validation; mechanistic studies | Validate specificity using knockdown controls |
| qPCR Reagents | SYBR Green master mix, M-MuLV reverse transcriptase | Expression validation of signature genes in tissues/cells | Normalize to reference genes (18S rRNA, GAPDH) |
| Invasion Assay Tools | Transwell chambers (8μm pore), Matrigel, crystal violet | Functional assessment of URG effects on cell migration | Use serum-free medium in upper chamber as chemoattractant control |
| Bioinformatics Tools | R packages: DESeq2, limma, WGCNA, glmnet, survival | Statistical analysis and model construction | Maintain reproducible code with version control |
The strategic integration of TCGA, GEO, and IUUCD databases provides a robust framework for developing ubiquitination-related gene signatures in cancer prognosis research. The standardized protocols outlined in this document enable researchers to move systematically from data acquisition through experimental validation, ensuring reproducible and clinically relevant findings. As ubiquitination continues to emerge as a promising therapeutic target in oncology, these data sourcing and analytical methodologies will remain fundamental to advancing our understanding of cancer biology and developing personalized treatment approaches.
Ubiquitination-related genes (URGs) play a crucial regulatory role in tumor development and progression, making them valuable targets for cancer prognosis research [38] [39]. The analysis of URGs through bulk RNA-sequencing (RNA-seq) enables the identification of molecular signatures that can predict patient survival and therapeutic response [40]. This application note details a comprehensive bioinformatic workflow for identifying and validating URG-based prognostic signatures, focusing on differential expression analysis and unsupervised clustering techniques. Such methodologies have demonstrated significant value in various cancers, including diffuse large B-cell lymphoma (DLBCL), laryngeal cancer, and cervical cancer, offering insights into potential therapeutic targets and personalized treatment approaches [38] [39] [40].
Bioinformatic Protocol for URG Signature Discovery
Data Acquisition and Preprocessing
The initial phase focuses on obtaining and preparing high-quality transcriptomic data from publicly available repositories or newly generated sequencing data.
- Data Sources: Utilize databases such as The Cancer Genome Atlas (TCGA) and the Gene Expression Omnibus (GEO) to acquire RNA-seq data and corresponding clinical information for the cancer type of interest [39] [40]. It is critical to collect a sufficient number of samples; for example, studies have utilized datasets ranging from 46 laryngeal cancer patients to over 1,800 DLBCL samples [38] [39].
- Quality Control (QC) and Trimming: Assess raw sequencing data (FASTQ files) for potential technical errors, including adapter contamination, unusual base composition, and duplicated reads using tools like FastQC or multiQC [41]. Clean the data by removing low-quality sequences and adapters with trimming tools such as fastp or Trim_Galore [41] [42]. Fastp has been shown to significantly enhance processed data quality and is advantageous due to its rapid analysis and operational simplicity [42].
- Alignment and Quantification: Map the cleaned reads to an appropriate reference genome or transcriptome using a splice-aware aligner like STAR [43] [41]. An alternative, faster approach is pseudo-alignment with tools such as Salmon or Kallisto, which estimate transcript abundances without full base-by-base alignment and are well-suited for large datasets [43] [41]. The final step is read quantification, where tools like featureCounts or HTSeq-count are used to generate a raw count matrix, summarizing the number of reads mapped to each gene in each sample [41].
Table 1: Key Tools for RNA-seq Data Preprocessing
| Processing Step | Recommended Tools | Primary Function |
|---|---|---|
| Quality Control | FastQC, multiQC | Identifies technical errors in raw sequencing data |
| Read Trimming | fastp, Trimmomatic, Cutadapt | Removes adapter sequences and low-quality bases |
| Read Alignment | STAR, HISAT2 | Maps reads to a reference genome |
| Pseudo-alignment | Salmon, Kallisto | Estimates transcript abundance without full alignment |
| Read Quantification | featureCounts, HTSeq-count | Generates a raw count matrix of gene expression |
Data Normalization and Differential Expression Analysis
The raw count matrix cannot be directly used for comparisons between samples due to technical biases such as sequencing depth and gene length. Normalization is therefore a critical step.
- Normalization Techniques: Various methods are available to correct for these technical biases. TPM (Transcripts per Million) and FPKM (Fragments per Kilobase of Million) are within-sample normalization methods that correct for sequencing depth and gene length [41] [44]. For differential expression analysis, between-sample normalization methods like the Trimmed Mean of M-values (TMM) from the
edgeRpackage and the Relative Log Expression (RLE) used byDESeq2are generally recommended, as they also correct for library composition [41] [44]. A benchmark study showed that RLE, TMM, and GeTMM (a gene-length-corrected TMM) produce metabolic models with lower variability and can more accurately capture disease-associated genes compared to TPM and FPKM [44]. - Differential Expression Analysis: Identify genes that are differentially expressed between conditions (e.g., tumor vs. normal) using statistical packages in R. The
limmapackage, built on a linear-modeling framework, can be used for this purpose [43] [38]. The criteria for defining differentially expressed genes (DEGs) typically include a Fold Change > 2 and a False Discovery Rate (FDR) < 0.05 [38].
Identification of Ubiquitination-Related Prognostic Genes
This stage involves filtering the DEGs to isolate those with prognostic value that are also related to ubiquitination.
- URG Curation: Compile a comprehensive list of URGs from specialized databases such as the Integrated Annotations for Ubiquitin and Ubiquitin-like Conjugation Database (IUUCD) or UbiBrowser [39] [40]. One study curated 807 such genes for analysis in cervical cancer [40].
- Survival-Associated URG Screening: Intersect the list of DEGs with the curated URGs to identify differentially expressed URGs. Then, perform univariate Cox regression analysis to screen for URGs significantly associated with overall survival (OS) [38] [39]. The optimal cut-off value for each gene's expression, used to stratify patients into high and low expression groups, can be determined using the
surv_cutpointfunction from the "survminer" R package [38]. Signature Construction via LASSO Regression: To refine the list of candidate genes and avoid overfitting, apply the Least Absolute Shrinkage and Selection Operator (LASSO) Cox regression analysis using the
glmnetR package [38] [39] [40]. This technique penalizes the coefficients of less important genes, shrinking some to zero, and retains the most valuable genes for predicting patient survival. A prognostic risk score is subsequently calculated for each patient using the formula:Risk Score = Σ (Coeff~i~ * Exp~i~)
where Coeff represents the regression coefficient from multivariate Cox regression and Exp denotes the gene expression level [39]. Patients are then stratified into high-risk and low-risk subgroups based on the median risk score.
Table 2: Example Ubiquitination-Related Gene Signatures from Cancer Studies
| Cancer Type | Identified Ubiquitination-Related Signature Genes | References |
|---|---|---|
| Diffuse Large B-Cell Lymphoma (DLBCL) | CDC34, FZR1, OTULIN | [38] |
| Laryngeal Cancer | PPARG, LCK, LHX1 | [39] |
| Cervical Cancer | KLHL22, UBXN11, FBXO25, ANKRD13A, WSB1, WDTC1, ASB1, INPPL1, USP21, MIB2, USP30, TRIM32, SOCS1 | [40] |
Unsupervised Clustering for Molecular Subtyping
Unsupervised clustering is used to discover intrinsic molecular subtypes within the cancer data based on the expression of prognostic URGs, without using pre-defined labels.
- Consensus Clustering: Use the
ConsensusClusterPlusR package to perform unsupervised consensus clustering [38] [40]. This algorithm repeatedly samples the data and clusters the samples to provide a consensus on the stable subgroups. Parameters are typically set to 1,000 repetitions to ensure robust results [38]. The optimal number of clusters (k) is determined based on the cumulative distribution function (CDF) curve's clustering score [40]. - Cluster Validation: The prognostic value of the identified molecular subtypes is confirmed using Kaplan-Meier survival analysis. A significant log-rank test p-value (e.g., p < 0.05) indicates that the subtypes have distinct survival outcomes [40]. For example, in a cervical cancer study, three distinct subtypes were identified, with one subtype (C3) showing significantly improved prognosis and another (C2) associated with adverse clinical outcomes [40].
Functional Enrichment and Immune Microcharacterization
Downstream analyses help interpret the biological relevance of the risk signature and molecular subtypes.
- Enrichment Analysis: Conduct Gene Ontology (GO) and Kyoto Encyclopedia of Genes and Genomes (KEGG) pathway enrichment analyses using the
clusterProfilerR package [38] [40]. This identifies biological processes, cellular components, molecular functions, and pathways that are overrepresented in the gene sets associated with the high-risk group or specific molecular subtypes. Thresholds are typically set at FDR < 0.2 and P < 0.05 [38]. - Immune Microenvironment Assessment: The CIBERSORT algorithm or similar tools can be used to analyze the composition of immune cell infiltration in the tumor microenvironment [38] [39]. Differences in immune cell abundance between high-risk and low-risk groups are examined using statistical tests like the Wilcoxon rank-sum test. Furthermore, the correlation between signature URGs and infiltrating immune cells can be analyzed using Spearman correlation [38].
- Drug Sensitivity Prediction: The
oncoPredictR package can be employed to calculate the half-maximal inhibitory concentration (IC~50~) of various drugs, identifying therapeutics that may be more effective in specific risk groups [38]. For instance, one study found significant differences in the concentration of Osimertinib between high- and low-risk DLBCL groups [38].
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Reagents and Computational Tools for URG Prognostic Analysis
| Item Name | Function / Application | Specifications / Notes |
|---|---|---|
| R Statistical Software | Primary platform for statistical analysis, normalization, and modeling. | Version 4.2.0 or newer. Essential packages: limma, DESeq2, edgeR, glmnet, survival, survminer, ConsensusClusterPlus. |
| TCGA & GEO Datasets | Sources of RNA-seq data and clinical information for model training and validation. | Ensure datasets include clinical follow-up information (overall survival). |
| IUUCD / UbiBrowser | Databases for curating a comprehensive list of ubiquitination-related genes (URGs). | Provides the foundational gene set for screening prognostic candidates. |
| FastQC / multiQC | Quality control tools for assessing raw and processed sequencing data. | Generates reports on base quality, adapter content, and sequence duplication. |
| Salmon | Rapid transcript-level quantification of RNA-seq data. | Preferred for its speed and accuracy in estimating transcript abundance. |
| DESeq2 / edgeR | R/Bioconductor packages for normalizing count data and identifying differentially expressed genes. | Use their built-in normalization methods (RLE or TMM) designed for DE analysis. |
| CIBERSORT | Computational deconvolution algorithm to characterize immune cell infiltration from RNA-seq data. | Infers relative abundances of 22 human immune cell types. |
| oncoPredict | R package for predicting drug sensitivity and inferring therapeutic response from genomic data. | Useful for associating risk groups with potential efficacy of chemotherapeutic or targeted agents. |
This protocol outlines a robust and reproducible bioinformatic workflow for deriving ubiquitination-related gene signatures from RNA-seq data. By integrating differential expression analysis, supervised regression techniques, and unsupervised clustering, researchers can identify molecular subtypes and build prognostic models that have demonstrated significant value in predicting patient survival and informing therapeutic strategies across multiple cancer types [38] [39] [40]. This workflow provides a powerful framework for advancing personalized cancer medicine.
In the field of cancer prognosis research, the discovery of molecular signatures has been revolutionized by the application of machine learning (ML) algorithms. These computational approaches enable researchers to identify robust biomarker patterns from high-dimensional genomic data, providing insights into disease progression and potential therapeutic targets. Within the specific context of ubiquitination-related gene (URG) signatures for cancer prognosis, LASSO Cox regression and Support Vector Machine-Recursive Feature Elimination (SVM-RFE) have emerged as powerful methods for prognostic model development and feature selection, respectively.
Ubiquitination plays a critical regulatory role in tumor development and progression through post-translational modification processes that affect protein degradation and signaling pathways. The integration of ML techniques with ubiquitination research has facilitated the construction of risk models across various cancers, demonstrating significant potential for improving prognostic accuracy and personalized treatment strategies.
Theoretical Foundation and Key Algorithms
LASSO Cox Regression for Prognostic Modeling
Least Absolute Shrinkage and Selection Operator (LASSO) Cox regression represents a fusion of survival analysis and regularization techniques, making it particularly valuable for cancer prognosis studies where the goal is to identify a parsimonious set of genes most predictive of patient survival outcomes.
The algorithm operates by applying an L1 penalty constraint during model fitting, which effectively shrinks less important coefficients to zero, thereby performing feature selection simultaneously with model construction. This characteristic is particularly advantageous in high-dimensional genomic data where the number of features (genes) vastly exceeds the number of observations (patients). The mathematical formulation incorporates both the Cox partial likelihood and a penalty parameter (λ) that controls the strength of regularization. Optimization of this parameter is typically achieved through k-fold cross-validation (often 10-fold), which identifies the λ value that minimizes prediction error while maintaining model simplicity.
In practical applications for URG signature development, LASSO Cox has demonstrated remarkable utility. For instance, in diffuse large B-cell lymphoma (DLBCL), researchers applied LASSO Cox to identify a three-gene ubiquitination-related signature (CDC34, FZR1, and OTULIN) that effectively stratified patients into distinct risk groups [38]. Similarly, in lung adenocarcinoma, the method identified a four-gene signature (DTL, UBE2S, CISH, and STC1) that showed significant prognostic value across multiple validation cohorts [11].
SVM-RFE for Diagnostic Feature Selection
Support Vector Machine-Recursive Feature Elimination (SVM-RFE) represents a powerful feature selection algorithm that combines the classification prowess of SVMs with a recursive backward elimination procedure. The fundamental strength of this approach lies in its ability to identify features that optimally separate classes (e.g., tumor vs. normal tissue) based on margin maximization principles.
The algorithm operates through an iterative elimination process that ranks features according to their importance scores, typically derived from the weights of the SVM hyperplane. In each iteration, the least important features are removed, and the model is retrained until the optimal feature subset is identified. To enhance robustness, this process is often implemented with repeated cross-validation (e.g., 10-fold cross-validation with 5 repeats), which ensures stability in feature selection and mitigates overfitting.
In cancer research, SVM-RFE has demonstrated exceptional performance in identifying diagnostic biomarkers. A study on breast cancer utilizing DNA replication-related genes reported that SVM-RFE achieved remarkable accuracy (AUC = 0.995) in classifying tumor and normal samples, outperforming other feature selection methods [45]. Similarly, in hepatocellular carcinoma (HCC), SVM-RFE identified nine mitotic cell cycle genes that showed robust diagnostic performance across multiple datasets with AUC values exceeding 0.81 [46].
Table 1: Comparative Analysis of LASSO Cox and SVM-RFE Applications in Cancer Studies
| Cancer Type | Algorithm | Genes Identified | Performance Metrics | Reference |
|---|---|---|---|---|
| Diffuse Large B-Cell Lymphoma | LASSO Cox | CDC34, FZR1, OTULIN | Stratified risk groups with significant survival differences | [38] |
| Lung Adenocarcinoma | LASSO Cox | DTL, UBE2S, CISH, STC1 | Validated across 6 external cohorts (HR = 0.58) | [11] |
| Breast Cancer | SVM-RFE | CDK1, TK1, DTL, RRM2, EGFR, RMI2, RECQL4, RAD51, GINS1, CCNA2 | AUC = 0.995 in training and validation sets | [45] |
| Hepatocellular Carcinoma | SVM-RFE | CDKN3, TRIP13, RACGAP1, FBXO43, EZH2, SPDL1, E2F1, TUBE1, CDC6 | AUC > 0.81 across multiple datasets | [46] |
| Ovarian Cancer | LASSO Cox | 17-gene ubiquitination signature | 1-year AUC = 0.703, 3-year AUC = 0.704, 5-year AUC = 0.705 | [37] |
| Laryngeal Cancer | LASSO Cox | PPARG, LCK, LHX1 | Significant prognostic stratification in validation cohorts | [39] |
Application Notes: Protocol for URG Signature Development
Integrated Workflow for Prognostic Signature Development
The development of a ubiquitination-related gene signature for cancer prognosis requires a systematic approach that integrates both SVM-RFE and LASSO Cox regression methods in a complementary workflow. This integrated strategy leverages the strengths of both algorithms—SVM-RFE for robust feature selection and LASSO Cox for survival model construction.
A typical workflow begins with data acquisition from public repositories such as The Cancer Genome Atlas (TCGA) and Gene Expression Omnibus (GEO), followed by preprocessing and normalization to ensure data quality. The next critical step involves identifying differentially expressed genes (DEGs) between tumor and normal tissues, with subsequent intersection against a curated list of ubiquitination-related genes. The resulting ubiquitination-related DEGs then undergo dual-path analysis: (1) SVM-RFE for diagnostic biomarker identification, and (2) univariate Cox regression followed by LASSO Cox for prognostic signature development.
This integrated approach has been successfully implemented across multiple cancer types. In breast cancer research, scientists applied this workflow to identify DNA replication-related genes with both diagnostic and prognostic value [45]. Similarly, in glioma studies, researchers have employed complex machine learning workflows incorporating multiple algorithms to develop extracellular matrix-related prognostic signatures [47].
Detailed Protocol for LASSO Cox Regression Analysis
Objective: To develop a ubiquitination-related gene prognostic signature for cancer survival prediction.
Materials and Reagents:
- R software environment (version 4.0 or higher)
- 'glmnet' package for LASSO implementation
- 'survival' package for Cox regression analysis
- 'survminer' package for survival visualization
- Gene expression matrix (FPKM or TPM normalized)
- Corresponding clinical data with survival information
Procedure:
Data Preparation and Preprocessing
- Obtain RNA-seq data and clinical information from TCGA or GEO databases
- Filter patients to include only those with complete survival information
- Normalize expression data using log2(TPM + 1) transformation
- Merge ubiquitination-related DEGs with survival data
Univariate Cox Regression Screening
- Perform initial screening of ubiquitination-related DEGs using univariate Cox regression
- Apply Benjamini-Hochberg FDR correction for multiple testing (significance threshold: FDR < 0.05)
- Test proportional hazards assumption using Schoenfeld residuals (p > 0.05)
- Exclude genes violating proportional hazards assumption
LASSO Cox Regression Implementation
- Input significant genes from univariate analysis into LASSO Cox model
- Set family = 'cox' and type.measure = 'deviance' in cv.glmnet function
- Perform 10-fold cross-validation to determine optimal lambda (λ) value
- Select the lambda.min value that minimizes partial likelihood deviance
- Extract genes with non-zero coefficients at optimal lambda
Risk Score Calculation and Model Validation
- Calculate risk score using formula: Risk score = Σ(βi × Expi)
- Stratify patients into high-risk and low-risk groups based on median risk score
- Validate prognostic performance using Kaplan-Meier survival analysis
- Assess predictive accuracy with time-dependent ROC curves
Technical Notes:
- For enhanced model stability, consider repeated cross-validation (e.g., 100 repetitions)
- Address potential multicollinearity among genes before LASSO implementation
- Validate the model in independent external cohorts when available
This protocol has been successfully applied in multiple cancer studies. For example, in laryngeal cancer research, scientists followed a similar approach to identify a three-gene ubiquitination signature (PPARG, LCK, and LHX1) that effectively stratified patient prognosis [39]. The resulting model demonstrated significant associations with immune landscape alterations and therapeutic options.
Detailed Protocol for SVM-RFE Implementation
Objective: To identify optimal diagnostic ubiquitination-related gene features for cancer classification.
Materials and Reagents:
- R software with e1071, caret, and ROCR packages
- Python with scikit-learn (alternative implementation)
- Normalized gene expression data (tumor vs. normal samples)
- Pre-defined ubiquitination-related gene set
Procedure:
Data Preparation and Feature Filtering
- Prepare expression matrix with samples as rows and genes as columns
- Filter out highly correlated genes (Pearson r > 0.9) to reduce redundancy
- Partition data into training (70%) and testing (30%) sets
- Apply z-score normalization to gene expression values
SVM-RFE Parameter Optimization
- Initialize SVM with linear kernel (kernel = 'linear')
- Set up recursive feature elimination with 10-fold cross-validation
- Configure repeated CV with 5 repeats for enhanced robustness
- Run feature selection with minimum feature set set to 1
Iterative Feature Elimination
- Train initial SVM model with all candidate features
- Rank features based on weight magnitude (|w|) in the decision hyperplane
- Eliminate bottom 10-20% of features in each iteration
- Retrain model with reduced feature set
- Repeat process until feature set is empty
Model Evaluation and Feature Selection
- Plot performance (AUC) against number of features
- Identify the feature subset that maximizes classification accuracy
- Validate selected features on independent test set
- Assess generalizability with external datasets when available
Performance Assessment
- Calculate AUC, sensitivity, specificity, precision, and F1-score
- Perform permutation testing (n = 100) to establish significance
- Compare with alternative feature selection methods (e.g., RF-RFE)
Technical Notes:
- For large feature sets, consider implementing the algorithm in chunks to reduce computational burden
- Balance class distribution in training data if sample sizes are unequal
- For non-linear relationships, explore radial basis function (RBF) kernel, though interpretation becomes more challenging
In breast cancer research, this approach has yielded exceptional results, with SVM-RFE achieving near-perfect classification (AUC = 0.995) of tumor and normal samples using DNA replication-related genes [45]. The method consistently outperforms alternative feature selection approaches in multiple cancer types.
Table 2: Essential Research Reagents and Computational Tools for URG Signature Development
| Category | Item | Specification/Version | Application Purpose | Key Features |
|---|---|---|---|---|
| Software Packages | R Statistical Software | 4.0 or higher | Primary analysis environment | Comprehensive statistical computing |
| glmnet | 4.1 or higher | LASSO Cox regression | Efficient regularization path computation | |
| e1071 | 1.7 or higher | SVM-RFE implementation | SVM modeling with various kernels | |
| caret | 6.0 or higher | Classification and regression training | Streamlined machine learning workflow | |
| survival | 3.2 or higher | Survival analysis | Cox proportional hazards modeling | |
| Data Resources | The Cancer Genome Atlas (TCGA) | Multiple cancer types | Primary data source | Multi-omics data with clinical annotation |
| Gene Expression Omnibus (GEO) | Multiple platforms | Validation datasets | Diverse experimental designs | |
| UUCD 2.0 Database | Downloaded March 2017 | Ubiquitination-related gene sets | Comprehensive ubiquitin enzyme catalog | |
| Computational Methods | 10-fold Cross-Validation | Standard protocol | Parameter optimization | Robust performance estimation |
| Kaplan-Meier Analysis | Log-rank test | Survival difference assessment | Non-parametric survival curve comparison | |
| Time-dependent ROC | timeROC package | Predictive accuracy assessment | Evaluation of prognostic performance over time |
Case Studies in Ubiquitination-Related Cancer Research
DLBCL: A Three-Gene Ubiquitination Signature
In diffuse large B-cell lymphoma, researchers employed LASSO Cox regression to develop a concise prognostic signature based on three ubiquitination-related genes: CDC34, FZR1, and OTULIN [38]. The study analyzed three datasets (GSE181063, GSE56315, and GSE10846) comprising 1,800 DLBCL samples, identifying ubiquitination-related survival-associated differentially expressed genes.
The investigation revealed that elevated expression of CDC34 and FZR1, coupled with low expression of OTULIN, correlated with poor prognosis in DLBCL patients. The resulting risk stratification showed significant differences in immune scores and drug sensitivity patterns between high-risk and low-risk groups. Specifically, the high-risk group demonstrated increased sensitivity to Boehringer Ingelheim compound 2536 and Osimertinib, suggesting potential therapeutic implications.
This study exemplifies the power of LASSO Cox regression in distilling complex ubiquitination-related processes into a clinically actionable prognostic tool. The three-gene signature not only stratified patient survival but also provided insights into associated immune microenvironment alterations and potential treatment vulnerabilities.
Pan-Cancer Applications and Validation
The utility of ubiquitination-related gene signatures extends across multiple cancer types, demonstrating the broad applicability of these ML approaches. In lung adenocarcinoma, a four-gene ubiquitination signature (DTL, UBE2S, CISH, and STC1) developed through LASSO Cox regression effectively stratified patient prognosis across six external validation cohorts [11]. The high-risk group showed significantly worse outcomes (HR = 0.58, 95% CI: 0.36-0.93) and distinctive immune profiles with higher PD-1/PD-L1 expression, tumor mutation burden, and tumor neoantigen load.
Similarly, in ovarian cancer, a comprehensive study identified a 17-gene ubiquitination signature that effectively predicted patient survival (1-year AUC = 0.703, 3-year AUC = 0.704, 5-year AUC = 0.705) [37]. The investigation further revealed distinct immune infiltration patterns, with low-risk patients exhibiting higher levels of CD8+ T cells, M1 macrophages, and follicular cells. Experimental validation confirmed the functional role of FBXO45, a key E3 ubiquitin ligase in the signature, in promoting ovarian cancer growth through the Wnt/β-catenin pathway.
Laryngeal cancer research yielded a three-gene ubiquitination signature (PPARG, LCK, LHX1) that effectively stratified patient prognosis and informed treatment strategies [39]. The study demonstrated that the low-risk group had more activated immune function and higher infiltration of anti-cancer immune cells, suggesting greater potential benefit from immunotherapy. Experimental validation confirmed that PPARG knockdown reduced expression of immunosuppressive cytokines (IL6, TGFB1, TGFB2, and VEGFC), providing mechanistic insights into the signature's biological relevance.
Technical Considerations and Best Practices
Methodological Optimization Strategies
Successful implementation of LASSO Cox and SVM-RFE in ubiquitination-related signature development requires attention to several technical considerations that significantly impact model performance and biological validity.
For LASSO Cox regression, data preprocessing plays a crucial role in model stability. Proper normalization of gene expression data (e.g., log2(TPM+1) transformation) helps address heteroscedasticity and ensures more reliable coefficient estimation. When working with multiple datasets, cross-platform batch effects must be addressed using methods such as Combat or surrogate variable analysis. Additionally, the proportional hazards assumption should be rigorously tested using Schoenfeld residuals, as violations can lead to biased estimates and invalid inferences.
For SVM-RFE implementation, feature pre-screening can enhance computational efficiency, particularly with large ubiquitination-related gene sets. Removing highly correlated features (Pearson r > 0.9) reduces redundancy without sacrificing discriminatory power. The choice of SVM kernel also warrants consideration—while linear kernels offer interpretability through feature weights, nonlinear kernels may capture complex interactions at the cost of transparency. Class imbalance between tumor and normal samples should be addressed through techniques such as synthetic minority oversampling (SMOTE) or adjusted class weights.
Validation Frameworks and Clinical Translation
Robust validation represents a critical component of URG signature development, encompassing multiple dimensions from statistical verification to biological confirmation.
Statistical validation should include both internal validation (through bootstrapping or repeated cross-validation) and external validation in independent cohorts. Temporal validation using time-split cohorts can provide insights into model performance over time. For prognostic signatures, clinical utility assessment should extend beyond standard performance metrics (C-index, AUC) to include decision curve analysis that evaluates net benefit over existing clinical standards.
Biological validation strengthens the credibility of computational findings. Experimental approaches such as Western blot, qRT-PCR, and ELISA can confirm differential expression of signature genes at protein and mRNA levels [39]. Functional validation through gene knockdown or overexpression experiments establishes causal relationships between signature genes and cancer phenotypes. For ubiquitination-related signatures, investigating connections to known ubiquitination pathways and processes provides mechanistic context.
Clinical translation requires consideration of practical implementation factors, including the development of standardized assay protocols, establishment of clinically relevant risk thresholds, and demonstration of cost-effectiveness compared to existing standards. The ultimate goal is the development of clinically actionable tools that improve patient stratification and treatment decision-making.
The integration of machine learning approaches, particularly LASSO Cox regression and SVM-RFE, has significantly advanced the development of ubiquitination-related gene signatures in cancer prognosis research. These methods provide powerful computational frameworks for distilling complex molecular profiles into clinically actionable biomarkers that improve risk stratification and therapeutic decision-making.
The consistent success of these approaches across diverse cancer types—from DLBCL and lung adenocarcinoma to ovarian and laryngeal cancers—underscores their robustness and generalizability. Furthermore, the biological insights gleaned from these signatures, particularly regarding immune microenvironment interactions and ubiquitination pathway dysregulation, highlight the dual utility of these models as both prognostic tools and discovery engines.
As the field advances, future work should focus on standardizing analytical pipelines, enhancing model interpretability, and strengthening the connection between computational predictions and biological mechanisms. The integration of multi-omics data and the development of dynamic models that incorporate temporal changes in ubiquitination processes represent promising directions for next-generation signature development. Through continued refinement and validation, these machine learning-driven approaches will increasingly contribute to personalized cancer management strategies centered on the ubiquitination machinery.
Ubiquitination-related genes (URGs) have emerged as crucial regulators of oncogenesis and tumor progression, representing promising biomarkers for cancer prognosis and therapeutic targeting. The ubiquitin-proteasome system (UPS), a critical post-translational modification pathway, governs numerous cellular processes including protein degradation, cell cycle progression, DNA repair, and immune responses [40] [19]. Dysregulation of ubiquitination pathways contributes significantly to cancer development by altering the stability and function of oncoproteins and tumor suppressors [48] [11]. Recent advances in bioinformatics and multi-omics technologies have enabled the development of molecular signatures based on URGs that show remarkable predictive accuracy for patient survival across multiple cancer types. This application note presents validated URG signatures in specific cancers, detailing their prognostic value, associated biological pathways, and implications for clinical practice and drug development.
Validated URG Signatures Across Cancers
Comprehensive analyses of cancer genomics datasets have yielded several robust URG signatures with prognostic significance. The table below summarizes key validated URG signatures across different cancer types.
Table 1: Validated Ubiquitination-Related Gene Signatures in Specific Cancers
| Cancer Type | Signature Size | Key Genes | Validation | Prognostic Value |
|---|---|---|---|---|
| Cervical Cancer | 13-gene | KLHL22, UBXN11, FBXO25, ANKRD13A, WSB1, WDTC1, ASB1, INPPL1, USP21, MIB2, USP30, TRIM32, SOCS1 | TCGA-CESC, GEO datasets | Risk classification significantly correlated with survival in univariate and multivariate analyses [40] |
| Triple-Negative Breast Cancer | 11-gene | Not specified in excerpt | METABRIC, GSE58812 | Favorable prediction of overall survival, validated in test set [19] |
| Breast Cancer | 4-gene | CDC20, PCGF2, UBE2S, SOCS2 | GSE42568, TCGA, GSE20685 | High-risk group showed significantly worse overall survival (p < 0.001) [49] |
| Lung Adenocarcinoma | 4-gene | DTL, UBE2S, CISH, STC1 | 6 external GEO datasets | Higher URRS associated with worse prognosis (HR = 0.58, 95% CI: 0.36-0.93) [11] |
These signatures demonstrate the consistent prognostic value of URGs across diverse cancer types. The cervical cancer 13-gene signature represents one of the most comprehensive models, incorporating genes from multiple ubiquitination pathway components including E3 ligases (KLHL22, FBXO25, MIB2, TRIM32), ubiquitin-binding proteins (UBXN11, ANKRD13A), and deubiquitinating enzymes (USP21, USP30) [40]. Similarly, the breast cancer 4-gene signature includes both risk factors (CDC20, PCGF2, UBE2S) and protective factors (SOCS2), highlighting the complex dual roles of ubiquitination pathways in cancer progression [49].
URG Signature Development Workflow
The development of validated URG signatures follows a systematic bioinformatics pipeline combining multiple computational approaches. The standardized workflow ensures robust signature identification and validation.
Figure 1: Workflow for developing and validating URG prognostic signatures, showing key steps from data acquisition to clinical application.
Detailed Methodological Framework
Data Acquisition and Preprocessing
Research begins with collecting gene expression data and corresponding clinical information from large-scale cancer genomics databases such as The Cancer Genome Atlas (TCGA) and Gene Expression Omnibus (GEO) [40] [49]. The ubiquitin-related genes are typically obtained from the Integrated Annotations for Ubiquitin and Ubiquitin-Like Conjugation Database (IUUCD), which comprehensively catalogues E1 ubiquitin-activating enzymes, E2 ubiquitin-conjugating enzymes, E3 ubiquitin ligases, and deubiquitinating enzymes [40] [11]. Quality control measures include excluding patients with survival times of fewer than 30 days and removing batch effects using algorithms like the ComBat function in the "sva" R package [19].
Molecular Subtyping Using URGs
Unsupervised consensus clustering analysis based on URG expression profiles identifies molecular subtypes with distinct clinical outcomes. The "ConsensusClusterPlus" R package implements this analysis using the k-means method with 1000 iterations to ensure clustering stability [40]. The cumulative distribution function (CDF) curve determines the optimal cluster number (k). For example, in cervical cancer, three distinct molecular subtypes (C1-C3) showed significantly different prognostic outcomes, with the C3 subtype demonstrating improved prognosis compared to the poor-outcome C2 subtype (log-rank p = 0.011) [40].
Feature Selection and Signature Construction
Weighted correlation network analysis (WGCNA) identifies co-expressed gene modules associated with clinical traits of interest [40]. Following this, the least absolute shrinkage and selection operator (LASSO) Cox regression model, implemented via the "glmnet" package, selects the most informative prognostic genes while preventing overfitting [40] [49]. The final risk score calculation follows the formula:
Risk Score = Σ(Coefi * Expri)
Where Coefi represents the regression coefficient from multivariate Cox analysis, and Expri represents the gene expression value [40] [11]. Patients are stratified into high-risk and low-risk groups based on the median risk score for subsequent survival analysis.
URG Signaling Pathways in Cancer
Ubiquitination-related genes encompass multiple enzyme families that coordinate a sophisticated regulatory network controlling protein stability and function. The complexity of this system enables fine-tuned regulation of cancer-relevant pathways.
Figure 2: Ubiquitination machinery and cancer-relevant pathways showing URG signature genes involved in the ubiquitin-proteasome system.
Functional Roles of URG Signature Components
URG signatures encompass genes representing multiple facets of ubiquitination machinery. E3 ubiquitin ligases such as TRIM32 and SOCS1 (in the cervical cancer signature) recognize specific substrate proteins for ubiquitination, determining pathway specificity [40]. E2 conjugating enzymes like UBE2S (in breast cancer and lung adenocarcinoma signatures) transfer activated ubiquitin to E3 ligases or directly to substrates [49] [11]. Deubiquitinating enzymes including USP21 and USP30 (in the cervical cancer signature) reverse ubiquitination, providing regulatory counterbalance [40]. The functional enrichment analyses of URG signatures consistently reveal associations with critical cancer pathways including cell cycle regulation, DNA replication and repair, immune response, and chromatin modification [40] [49].
The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential Research Reagents and Resources for URG Signature Validation
| Resource | Function | Application Examples | Key Features |
|---|---|---|---|
| IUUCD Database | Comprehensive ubiquitin and ubiquitin-like conjugation database | Source of 807 URGs for cervical cancer study [40] | Curated collection of E1, E2, E3, and DUB genes |
| TCGA Datasets | Multi-dimensional cancer genomics data | Training set for 13-gene cervical cancer signature [40] | Standardized RNA-seq, clinical, and survival data |
| GEO Datasets | Public repository of functional genomics data | Validation sets for 4-gene breast cancer signature (GSE20685) [49] | Independent cohorts for signature validation |
| ConsensusClusterPlus | R package for unsupervised clustering | Molecular subtyping of cervical cancer samples [40] | Implements multiple clustering algorithms with stability assessment |
| WGCNA | R package for weighted correlation network analysis | Identification of co-expressed gene modules in cervical cancer [40] | Construction of scale-free co-expression networks |
| LASSO Cox Regression | Feature selection and regularization method | Development of 4-gene breast cancer signature [49] | Prevents overfitting in high-dimensional data |
| CIBERSORT/ESTIMATE | Algorithms for immune cell infiltration analysis | Tumor microenvironment characterization in breast cancer [48] | Quantification of immune cell fractions from bulk RNA-seq data |
Experimental Protocol: URG Signature Development and Validation
Computational Protocol for URG Signature Construction
Objective: Develop and validate a ubiquitination-related gene signature for cancer prognosis prediction.
Materials:
- Hardware: Computer with minimum 8GB RAM and multi-core processor
- Software: R statistical environment (version 4.2.0 or higher)
- R packages: ConsensusClusterPlus, WGCNA, glmnet, survival, survminer, clusterProfiler
- Data: TCGA and GEO datasets for specific cancer type, IUUCD URG list
Procedure:
Data Acquisition and Curation (Duration: 1-2 days)
- Download RNA-seq data and clinical information from TCGA and GEO databases
- Obtain ubiquitination-related gene list from IUUCD database (807 genes)
- Merge datasets and remove batch effects using ComBat algorithm
- Exclude patients with survival time <30 days and missing clinical information
Molecular Subtyping (Duration: 4-6 hours)
- Perform univariate Cox regression to identify prognostic URGs (p < 0.05)
- Conduct unsupervised consensus clustering using ConsensusClusterPlus
- Set parameters: maxK = 5, reps = 1000, pItem = 0.8, pFeature = 1, clusterAlg = "km", distance = "euclidean"
- Determine optimal cluster number (k) based on CDF curve
- Validate subtype differences using Kaplan-Meier survival analysis
Co-expression Network Analysis (Duration: 1 day)
- Perform WGCNA to identify gene modules associated with clinical traits
- Select soft-thresholding power based on scale-free topology criterion
- Identify module-trait relationships and extract hub genes
- Conduct functional enrichment analysis of key modules using GO and KEGG
Prognostic Signature Construction (Duration: 6-8 hours)
- Apply LASSO Cox regression to identify optimal gene combination
- Perform 10-fold cross-validation to determine lambda parameter
- Calculate risk score: Risk Score = Σ(Coefi * Expri)
- Stratify patients into high-risk and low-risk groups using median risk score
Signature Validation (Duration: 1 day)
- Assess prognostic performance using Kaplan-Meier survival analysis
- Evaluate prediction accuracy using time-dependent ROC curves
- Validate signature in independent external datasets
- Perform univariate and multivariate Cox regression to confirm independence from other clinical variables
Functional Validation Protocol for Signature Genes
Objective: Experimentally validate the biological role of key URG signature components.
Materials:
- Cell lines: Relevant cancer cell lines (e.g., HeLa for cervical cancer, MCF-7 for breast cancer)
- Reagents: Antibodies against target proteins, transfection reagents, transwell chambers
- Equipment: PCR system, Western blot apparatus, cell culture incubator
Procedure:
Gene Expression Manipulation (Duration: 3-4 days)
- Design and synthesize siRNA or CRISPR/Cas9 constructs for gene knockdown
- Develop overexpression plasmids for signature genes
- Transfect cells using appropriate transfection reagents
- Validate manipulation efficiency using RT-qPCR and Western blotting
Functional Assays (Duration: 5-7 days)
- Perform transwell migration assays to assess cell invasion capability
- Use 24-well transwell chambers with 8μm pore sizes
- Plate cells in serum-free medium in upper chamber
- Incubate for 24 hours, then stain migrated cells with crystal violet
- Conduct MTT or CCK-8 assays to evaluate cell proliferation
- Analyze cell cycle distribution using flow cytometry
Mechanistic Studies (Duration: 1-2 weeks)
- Examine downstream pathways using Western blotting
- Assess protein stability and degradation pathways
- Identify interaction partners using co-immunoprecipitation
- Validate substrate ubiquitination status
Discussion and Clinical Implications
The validated URG signatures presented herein demonstrate consistent prognostic value across multiple cancer types, highlighting the fundamental role of ubiquitination pathways in cancer progression. These signatures not only predict patient outcomes but also provide insights into tumor biology and potential therapeutic vulnerabilities.
URG signatures show strong associations with tumor microenvironment characteristics and immunotherapy response. In cervical cancer, the high-risk group defined by the 13-gene signature showed significantly higher levels of TIDE scores, T-cell exclusion, cancer-associated fibroblast (CAF) scores, and myeloid-derived suppressor cell (MDSC) scores compared to the low-risk group [40]. Similarly, in breast cancer, ubiquitination-related signatures correlate with immune cell infiltration patterns and response to immune checkpoint inhibitors [48]. These findings suggest that URG signatures may inform immunotherapy selection and combination strategies.
The utility of URG signatures extends beyond prognosis prediction to therapeutic targeting. For instance, the experimental validation of USP21 in the cervical cancer signature demonstrated its role in promoting migration ability of cervical cancer cells [40], nominating it as a potential therapeutic target. Additionally, drug sensitivity analysis reveals associations between URG risk scores and response to chemotherapy agents, potentially guiding treatment selection [48] [11].
Future research directions should focus on translating these molecular signatures into clinical practice through the development of standardized diagnostic assays, validation in prospective clinical trials, and integration with existing prognostic systems. Furthermore, mechanistic studies of individual signature genes may uncover novel therapeutic targets within the ubiquitin-proteasome system, expanding treatment options for cancer patients with poor prognostic signatures.
The integration of molecular risk signatures with comprehensive analysis of the tumor microenvironment (TME) represents a transformative approach in cancer prognostics and therapeutic stratification. Among various molecular processes, ubiquitination—a critical post-translational modification regulating protein degradation and signaling—has emerged as a rich source of prognostic biomarkers across multiple cancer types. The development of ubiquitination-related gene (URG) signatures enables not only accurate risk stratification but also provides insights into immune modulation and treatment sensitivity.
Ubiquitination-related signatures have demonstrated remarkable prognostic value in diverse malignancies including diffuse large B-cell lymphoma (DLBCL), laryngeal cancer, lung adenocarcinoma (LUAD), and breast cancer [38] [39] [11]. These signatures leverage the fundamental role of the ubiquitin-proteasome system in regulating oncogenic pathways, DNA repair mechanisms, and immune responses within the TME. The clinical utility of these signatures extends beyond mere prognosis, offering a framework for understanding therapy resistance and guiding personalized treatment approaches.
This protocol outlines comprehensive methodologies for developing, validating, and applying URG signatures within the context of TME analysis and therapy response prediction. We provide detailed experimental workflows and analytical frameworks to bridge the gap between risk quantification and clinical stratification.
Ubiquitination-Related Gene Signatures in Cancer Prognosis
Established URG Signatures Across Cancers
Multiple cancer types have demonstrated prognostic significance through URG signatures. In DLBCL, a 3-gene signature comprising CDC34, FZR1, and OTULIN effectively stratified patients into distinct risk categories [38]. Elevated expression of CDC34 and FZR1 coupled with low OTULIN expression correlated with poor prognosis, with significant differences in immune scores and drug sensitivity observed between risk groups.
In laryngeal cancer, a URG signature based on PPARG, LCK, and LHX1 showed strong discriminatory power for overall survival prediction [39]. The signature demonstrated excellent applicability across most clinical conditions and correlated significantly with immune landscape alterations, where the low-risk group exhibited more activated immune function and higher infiltration of anti-cancer immune cells.
For lung adenocarcinoma, researchers developed a 4-gene ubiquitination-related risk score (URRS) based on DTL, UBE2S, CISH, and STC1 [11]. This signature consistently predicted poorer prognosis in high-risk patients across six external validation cohorts and correlated with higher PD-1/PD-L1 expression, tumor mutation burden, and tumor neoantigen load.
A 6-gene ubiquitination signature (ATG5, FBXL20, DTX4, BIRC3, TRIM45, and WDR78) demonstrated robust prognostic performance in breast cancer, validated across multiple external datasets including TCGA-BRAC, GSE1456, GSE16446, GSE20711, GSE58812, and GSE96058 [20]. The signature showed superior predictive ability compared to traditional clinical indicators.
Table 1: Established Ubiquitination-Related Gene Signatures in Cancer Prognosis
| Cancer Type | Signature Genes | Risk Association | Validation |
|---|---|---|---|
| Diffuse Large B-Cell Lymphoma | CDC34, FZR1, OTULIN | High CDC34/FZR1 + Low OTULIN = Poor Prognosis [38] | Internal & External Datasets |
| Laryngeal Cancer | PPARG, LCK, LHX1 | Risk Score Stratification [39] | TCGA + GEO (GSE65858) |
| Lung Adenocarcinoma | DTL, UBE2S, CISH, STC1 | High URRS = Worse Prognosis [11] | 6 External GEO Cohorts |
| Breast Cancer | ATG5, FBXL20, DTX4, BIRC3, TRIM45, WDR78 | Risk Score Stratification [20] | Multiple External Datasets |
Computational Methodologies for Signature Development
The development of robust URG signatures follows a structured analytical workflow incorporating multiple computational biology approaches:
Data Acquisition and Preprocessing: RNA-seq data and clinical information are obtained from public repositories such as The Cancer Genome Atlas (TCGA) and Gene Expression Omnibus (GEO). Data normalization is performed using standardized approaches (e.g., TPM, FPKM), with careful exclusion of samples lacking essential clinical information or with poor quality metrics [39] [11].
Identification of Prognostic URGs: Differential expression analysis between tumor and normal tissues identifies ubiquitination-related genes with significant expression alterations. Univariate Cox regression analysis then screens these differentially expressed URGs for significant association with overall survival. Feature selection techniques, including Least Absolute Shrinkage and Selection Operator (LASSO) Cox regression and Random Survival Forests, identify the most prognostic gene subsets while preventing overfitting [38] [11] [50].
Risk Model Construction: Multivariate Cox regression coefficients are used to calculate risk scores using the formula: Risk score = Σ(βi × Expi), where β represents the coefficient from multivariate Cox regression and Exp denotes gene expression level [38] [39]. Patients are stratified into high-risk and low-risk subgroups based on median risk score or optimized cut-off values.
Validation Strategies: Robust validation involves both internal validation (cross-validation) and external validation using independent cohorts. Performance metrics include Kaplan-Meier survival analysis, time-dependent receiver operating characteristic (ROC) curves, concordance index (C-index) calculation, and calibration plots [30] [51].
Tumor Microenvironment Analysis in Risk Stratification
Immune Landscape Characterization
Comprehensive TME analysis provides biological context for URG-based risk stratification. Multiple computational approaches enable detailed characterization of immune infiltration patterns:
Immune Cell Deconvolution: Algorithms such as CIBERSORT, ESTIMATE, MCP-counter, xCell, and ssGSEA calculate the relative abundance of infiltrating immune cells from bulk RNA-seq data [30] [51]. These tools leverage cell-type-specific gene signatures to infer cellular composition, allowing comparison of immune infiltration between URG risk groups.
Single-Cell RNA Sequencing (scRNA-seq): scRNA-seq provides unprecedented resolution for analyzing cellular heterogeneity within the TME. The standard analytical workflow includes: quality control (filtering cells with <200 or >6,000 genes), log-normalization, principal component analysis, graph-based clustering, and t-distributed stochastic neighbor embedding (t-SNE) or uniform manifold approximation and projection (UMAP) for visualization [38] [52]. Cell types are annotated using reference-based (SingleR) and manual annotation approaches based on established marker genes.
Spatial Transcriptomics: This emerging technology preserves spatial context while capturing transcriptome-wide data, enabling investigation of spatial relationships between tumor cells and immune populations [53]. Analysis reveals how URG expression patterns correlate with specific tissue architectures and cellular neighborhoods.
Table 2: TME Analysis Methods for URG Signature Integration
| Method Category | Specific Techniques | Key Applications in URG Context |
|---|---|---|
| Bulk Deconvolution | CIBERSORT, ESTIMATE, xCell, MCP-counter, ssGSEA | Quantifying immune cell abundance differences between URG risk groups [30] [51] |
| Single-Cell Analysis | Seurat, Scanpy, SingleR, AUCell | Identifying cell-type-specific URG expression [38] [52] |
| Spatial Analysis | 10X Visium, Slide-seq, MERFISH | Mapping URG expression in tissue context [53] |
| Cell-Cell Communication | NicheNet, CellChat, ICELLNET | Inferring signaling networks altered by URG risk [52] |
TME Alterations Across URG Risk Groups
Studies consistently demonstrate significant TME differences between URG-defined risk groups. In laryngeal cancer, the low-risk URG signature group showed more activated immune function, higher infiltration of anti-cancer immune cells, and stronger expression of immune-promoting cytokines compared to the high-risk group [39]. Individual signature genes correlated distinctly with immune profiles—PPARG and LHX1 showed negative correlation, while LCK positively correlated with immuno-promoting microenvironments.
In lung adenocarcinoma, the high URRS group exhibited significantly higher PD-1/PD-L1 expression levels, tumor mutation burden, tumor neoantigen load, and overall TME scores [11]. These findings suggest that high-risk patients may be more amenable to immunotherapy approaches despite their poorer prognosis.
Early-onset colorectal cancer studies using single-cell integration analysis revealed reduced tumor-immune cell interactions in younger patients, with significant downregulation of ligands such as CEACAM1, CEACAM5, and CD99 in epithelial cells [52]. This highlights how age-related differences in TME composition may interact with molecular risk signatures.
Therapy Response Prediction
Drug Sensitivity Analysis
URG signatures demonstrate significant utility in predicting response to various therapeutic modalities. Computational approaches for drug sensitivity prediction include:
oncoPredict Algorithm: This R package calculates the half maximal inhibitory concentration (IC50) values for 198 drugs in cancer samples based on gene expression patterns [38] [39]. The method leverages pre-existing drug sensitivity databases to infer how URG risk groups may respond to specific chemotherapeutic and targeted agents.
GDSC Database Analysis: The Genomics of Drug Sensitivity in Cancer database provides a comprehensive resource linking molecular features to drug response [30] [51]. Integration of URG signatures with GDSC data enables identification of therapeutic vulnerabilities specific to risk groups.
Connectivity Map (CMap) Approach: This methodology identifies connections between URG expression patterns and drug-induced transcriptional profiles, suggesting potential repositioning opportunities [30].
URG-Based Therapeutic Stratification
Substantial evidence supports the application of URG signatures in treatment selection across cancer types:
In DLBCL, significant differences in concentration for Boehringer Ingelheim compound 2536 and Osimertinib were observed between high- and low-risk URG groups [38], suggesting tailored therapeutic approaches based on ubiquitination profiles.
For laryngeal cancer, chemotherapy was predicted to be more effective in high-risk patients, while immune checkpoint inhibitors would show superior efficacy in low-risk patients [39]. This stratification aligns with the observed immune profiles of each risk group.
Lung adenocarcinoma patients with high URRS showed lower IC50 values for various chemotherapy drugs [11], indicating increased susceptibility to conventional chemotherapeutic agents despite their poorer overall prognosis.
Machine learning frameworks integrating URG signatures with clinical variables have demonstrated superior performance in predicting treatment response compared to traditional clinical indicators alone [51] [50]. These approaches enable truly personalized therapeutic decision-making.
Experimental Protocols
Protocol 1: URG Signature Development and Validation
Objective: To develop and validate a ubiquitination-related gene signature for cancer prognosis using transcriptomic data.
Materials:
- RNA-seq data from TCGA and GEO databases
- R software environment with packages: limma, survminer, glmnet, ConsensusClusterPlus, survival, survminer, timeROC
- Clinical annotation data including survival outcomes
Procedure:
Data Preprocessing
- Download RNA-seq data (TPM or FPKM format) and corresponding clinical information
- Normalize expression data using log2(TPM+1) transformation
- Filter samples to exclude recurrent tumors, metastases, and those with missing survival data
- Merge multiple datasets where appropriate, applying batch correction using ComBat or similar methods
Identification of Prognostic URGs
- Obtain ubiquitination-related gene list from iUUCD 2.0 or UbiBrowser 2.0 databases
- Perform differential expression analysis using limma package (criteria: |logFC| > 1, FDR < 0.05)
- Conduct univariate Cox regression analysis to identify survival-associated URGs
- Apply LASSO Cox regression with 10-fold cross-validation for feature selection
- Perform multivariate Cox regression to identify independently prognostic URGs
Risk Model Construction
- Calculate risk scores using formula: Risk score = Σ(βi × Expi)
- Determine optimal cut-off value using surv_cutpoint function from survminer package
- Stratify patients into high-risk and low-risk groups based on median risk score or optimized cut-off
Model Validation
- Perform Kaplan-Meier survival analysis with log-rank test to compare survival between risk groups
- Generate time-dependent ROC curves at 1, 3, and 5 years using timeROC package
- Calculate concordance index (C-index) to assess model performance
- Validate signature in independent external cohorts using same risk score formula and cut-off
Statistical Analysis
- Compare clinical characteristics between risk groups using Chi-square or Fisher's exact tests
- Perform univariate and multivariate Cox regression to assess independence from clinical variables
- Construct nomogram integrating URG signature and clinical factors using rms package
- Evaluate nomogram performance using calibration curves and decision curve analysis
Protocol 2: TME Characterization in URG Risk Groups
Objective: To analyze tumor microenvironment differences between URG-defined risk groups.
Materials:
- Transcriptomic data stratified by URG risk groups
- R packages: CIBERSORT, ESTIMATE, MCP-counter, xCell, IOBR
- Single-cell RNA-seq data if available
- Immunohistochemistry/immunofluorescence validation materials
Procedure:
Immune Cell Infiltration Analysis
- Apply CIBERSORT algorithm to estimate relative proportions of 22 immune cell types
- Calculate ESTIMATE scores (stromal, immune, ESTIMATE) for each sample
- Use MCP-counter to quantify absolute abundances of 8 immune and 2 stromal cell populations
- Apply xCell and ssGSEA for additional immune characterization
- Compare immune infiltration scores between URG risk groups using Wilcoxon rank-sum test
Single-Cell RNA-seq Analysis (if available)
- Quality control: Filter cells with <200 or >6,000 detected genes and >5% mitochondrial reads
- Normalize data using log-normalization or SCTransform
- Perform dimensionality reduction using PCA
- Cluster cells using FindNeighbors and FindClusters functions in Seurat
- Visualize clusters using UMAP or t-SNE
- Annotate cell types using SingleR package and manual marker identification
- Compare cell type proportions between conditions using Chi-square tests
Cell-Cell Communication Analysis
- Prepare ligand-receptor interaction databases (CellChatDB, CellPhoneDB)
- Infer cell-cell communication networks using CellChat or NicheNet
- Identify differentially expressed ligands and receptors between URG risk groups
- Visualize communication patterns using circle, hierarchy, or chord plots
Spatial Validation (optional)
- Perform multiplex immunohistochemistry/immunofluorescence for key immune markers
- Quantify immune cell densities in specific tumor regions (core, invasive margin)
- Correlate spatial distribution patterns with URG risk scores
Protocol 3: Therapy Response Prediction
Objective: To predict therapy response based on URG risk stratification.
Materials:
- URG risk-stratified transcriptomic data
- R packages: oncoPredict, pRRophetic, IMvigor210CoreBiologies
- Drug sensitivity databases: GDSC, CTRP
Procedure:
Chemotherapy Response Prediction
- Apply oncoPredict algorithm to estimate IC50 values for 198 drugs
- Compare IC50 values between URG risk groups using Wilcoxon rank-sum test
- Identify drugs with significantly different sensitivity between groups (FDR < 0.05)
- Validate predictions using independent drug response datasets when available
Immunotherapy Response Prediction
- Calculate T-cell inflamed score or IFN-γ signature
- Estimate tumor immunophenotype using immunophenoscore algorithm
- Predict response to immune checkpoint inhibitors using previously validated signatures
- Compare immunotherapy response rates between URG risk groups in validation cohorts (e.g., IMvigor210)
Targeted Therapy Prediction
- Identify actionable mutations and alterations using mutational signatures
- Predict response to targeted agents based on pathway activation status
- Integrate URG risk with molecular subtypes for refined treatment recommendations
Experimental Validation (in vitro)
- Select cell lines representing different URG risk profiles
- Treat with identified therapeutic agents across concentration ranges
- Assess viability using MTT, CellTiter-Glo, or similar assays
- Calculate experimental IC50 values and compare with computational predictions
The Scientist's Toolkit
Table 3: Essential Research Reagents and Computational Tools
| Category | Item | Specification/Usage | Key Applications |
|---|---|---|---|
| Data Resources | TCGA Database | RNA-seq and clinical data for 33 cancer types | Model training and validation [38] [39] [11] |
| GEO Database | Curated microarray and RNA-seq datasets | Independent validation [38] [39] [20] | |
| iUUCD 2.0 / UbiBrowser 2.0 | Ubiquitination-related gene annotations | URG candidate identification [39] [11] | |
| Computational Tools | R Software Environment | v4.0+ with specialized packages | Statistical analysis and visualization [38] [39] |
| Limma Package | Differential expression analysis | Identifying dysregulated URGs [38] [30] | |
| CIBERSORT | Immune cell deconvolution algorithm | TME characterization [38] [30] [51] | |
| Seurat Package | Single-cell RNA-seq analysis | TME heterogeneity [38] [52] | |
| oncoPredict | Drug sensitivity prediction | Therapy response profiling [38] [39] | |
| Experimental Reagents | Single-Cell RNA-seq Kits | 10X Genomics Chromium System | TME characterization at single-cell resolution [52] |
| Multiplex IHC/IF Panels | Validated antibody panels | Spatial validation of TME findings [53] | |
| Cell Viability Assays | MTT, CellTiter-Glo | Experimental validation of drug sensitivity [39] |
The integration of ubiquitination-related gene signatures with comprehensive TME analysis represents a powerful framework for advancing cancer prognosis and therapeutic stratification. The protocols outlined herein provide a systematic approach for developing validated URG signatures, characterizing their associated TME contexts, and applying these insights to predict treatment response. As single-cell technologies and spatial transcriptomics continue to evolve, they will further refine our understanding of how ubiquitination processes shape the tumor ecosystem. The implementation of these methodologies promises to enhance personalized cancer medicine by bridging molecular risk assessment with clinically actionable treatment strategies.
Overcoming Challenges in URG Signature Development and Implementation
Addressing Tumor Heterogeneity and Batch Effects in Genomic Data
The development of robust ubiquitination-related gene (URG) signatures for cancer prognosis is fundamentally challenged by two inherent complexities of modern genomic data: tumor heterogeneity and batch effects. Tumor heterogeneity, comprising both spatial (across different tumor regions) and temporal (over time) variations, drives cancer progression and therapeutic resistance by creating diverse cellular ecosystems within a single tumor [54]. Simultaneously, technical batch effects arising from the integration of multiple datasets—a common practice in biomarker discovery—can introduce non-biological variations that obscure true biological signals and compromise the validity of prognostic models [55] [19]. This protocol details a comprehensive analytical framework to address these challenges specifically within the context of URG signature development, enabling more accurate and clinically translatable prognostic biomarkers.
Background
The Ubiquitin-Proteasome System in Cancer
Ubiquitination is a highly conserved post-translational modification that regulates protein degradation, localization, and activity through the coordinated action of E1 (activating), E2 (conjugating), and E3 (ligase) enzymes [49] [19]. The ubiquitin-proteasome system (UPS) influences crucial cancer-associated processes including cell cycle progression, DNA repair, immune response, and epithelial-mesenchymal transition [11] [55]. Dysregulation of URGs has been implicated across multiple cancer types, making them promising candidates for prognostic signatures [49] [11] [55].
Analytical Challenges in URG Signature Development
The development of multi-gene URG signatures faces specific technical challenges:
- Data Source Heterogeneity: URG studies typically integrate data from public repositories like TCGA and GEO, which exhibit substantial technical variability [49] [55] [19].
- Spatial Complexity: Ubiquitination processes vary across tumor microenvironments, including distinct spatial hubs such as tertiary lymphoid structures and immune-reactive regions [56].
- Multi-Omic Integration: Advanced spatial multi-omics technologies now capture URGs alongside genomic, epigenomic, transcriptomic, proteomic, and metabolomic data, each with distinct resolution and noise characteristics [54].
Table 1: Common Data Sources for URG Prognostic Model Development
| Data Source | Sample Type | Typical Use Case | Key References |
|---|---|---|---|
| The Cancer Genome Atlas (TCGA) | Primary tumor samples | Model training and validation | [49] [11] [55] |
| Gene Expression Omnibus (GEO) | Various (cell lines, tissues) | Independent validation | [49] [55] [19] |
| METABRIC | Breast cancer samples | Breast cancer-specific models | [19] |
| IUUCD Database | Ubiquitination enzymes | URG gene list compilation | [49] [11] [55] |
Computational Methods and Protocols
Initial Data Acquisition and URG Compilation
Protocol 1: URG List Curation
- Download the comprehensive URG list from the Integrated Ubiquitin and Ubiquitin-like Conjugation Database (iUUCD) [49] [11] [55].
- Extract gene expression matrices from primary data sources (e.g., TCGA, GEO) using appropriate platforms (e.g., UCSC Xena, GEO2R) [49] [55].
- Perform log₂(x+1) transformation on expression values to stabilize variance [55].
- Merge URG lists with expression matrices to create the foundational dataset for analysis.
Protocol 2: Data Preprocessing and Quality Control
- Sample Filtering: Exclude samples with survival duration <30 days to avoid perioperative mortality bias [55] [19].
- Normalization: Convert raw counts to Transcripts Per Million (TPM) or apply variance-stabilizing transformation [55].
- Batch Effect Assessment: Perform Principal Component Analysis (PCA) to visualize batch effects before correction [19].
Batch Effect Correction Strategies
Protocol 3: Batch Effect Removal Using Combat
Protocol 4: Multi-Dataset Integration for Meta-Analysis
- Apply the ComBat algorithm from the 'sva' R package to remove batch effects when integrating multiple cohorts (e.g., METABRIC and GEO datasets) [19].
- Validate integration success using PCA visualization showing merged clusters post-correction.
- For complex multi-omic integration, employ specialized algorithms:
- Horizontal Integration: For same omics type across slices, use shared features as anchors [54].
- Vertical Integration: For different omics from same tissue, use individual cells as reference [54].
- Diagonal Integration: For different omics from different slices, employ graph-based alignment methods [54].
Addressing Tumor Heterogeneity in URG Signature Development
Protocol 5: Molecular Subtyping to Account for Inter-Tumor Heterogeneity
- Perform non-negative matrix factorization (NMF) clustering based on URG expression patterns [55] [19].
- Determine optimal cluster number (k=2-10) using cophenetic coefficient and dispersion metrics [55] [19].
- Validate clusters by assessing survival differences, immune infiltration patterns, and pathway enrichment.
- Develop subtype-specific URG signatures when global models show poor performance.
Protocol 6: Spatial Heterogeneity Analysis
- Utilize spatial transcriptomics data (e.g., 10X Visium, Stereo-seq) to map URG expression across tumor regions [54].
- Apply spatial domain identification tools (e.g., GraphST, STitch3D) to identify spatially coherent URG expression patterns [54].
- Correlate spatial URG patterns with tumor microenvironment features using CARD or inferCNV [57] [54].
Prognostic Model Construction with Heterogeneity-Aware Validation
Protocol 7: URG Signature Development Using Regularized Regression
- Perform univariate Cox regression to identify prognostic URGs (p<0.05) [49] [55].
- Apply Least Absolute Shrinkage and Selection Operator (LASSO) Cox regression with 10-fold cross-validation to select optimal gene panel [49] [11] [55].
- Calculate risk score using the formula:
Risk score = (β1 × Gene1 Expression) + (β2 × Gene2 Expression) + ... + (βn × Genen Expression)[49] [19]. - Stratify patients into high-risk and low-risk groups using median risk score cutoff.
Protocol 8: Multi-Level Validation Strategy
- Internal Validation: Assess signature performance in training data using time-dependent ROC analysis [49] [19].
- External Validation: Apply signature to independent datasets (e.g., validate TCGA model in GEO datasets) [49] [11] [55].
- Clinical Validation: Evaluate signature independence from standard clinicopathological factors using multivariate Cox regression [49] [55].
Table 2: Computational Tools for Addressing Heterogeneity and Batch Effects
| Tool Category | Specific Tools | Primary Function | Applicable Step |
|---|---|---|---|
| Batch Correction | ComBat (sva package), PRECAST, FAST | Remove technical variations | Data Preprocessing |
| Spatial Analysis | GraphST, STitch3D, SPACEL, PASTE | Analyze spatial heterogeneity | Tumor Heterogeneity Assessment |
| Clustering | NMF, Consensus Clustering | Identify molecular subtypes | Tumor Heterogeneity Assessment |
| Feature Selection | LASSO, Random Survival Forest | Select optimal URG panels | Model Construction |
| Validation | Time-dependent ROC, Decision Curve Analysis | Assess model performance | Model Validation |
Visualizing Analytical Workflows
URG Signature Development Workflow
Spatial Multi-Omics Integration Framework
Research Reagent Solutions
Table 3: Essential Research Reagents and Computational Tools for URG Prognostic Studies
| Category | Specific Resource | Function | Application in URG Studies |
|---|---|---|---|
| Databases | iUUCD 2.0 Database | Comprehensive URG compilation | Source of ubiquitination-related genes for analysis |
| Data Sources | TCGA, GEO, METABRIC | Clinical and genomic data | Training and validation datasets for model development |
| Spatial Technologies | 10X Visium, CosMx SMI, MERFISH | Spatially resolved molecular profiling | Mapping URG expression in tumor microenvironment hubs |
| Batch Correction Tools | ComBat (sva R package), PRECAST | Technical variation removal | Integrating multiple datasets while preserving biological signals |
| Clustering Algorithms | NMF, Consensus Clustering | Molecular subtyping | Identifying URG-based cancer subtypes with prognostic significance |
| Feature Selection Methods | LASSO Cox Regression, Random Survival Forest | Dimensionality reduction | Selecting optimal URG combinations for prognostic signatures |
| Validation Frameworks | Time-dependent ROC, Decision Curve Analysis | Model performance assessment | Evaluating clinical utility of URG signatures |
Discussion
The integration of these computational protocols enables the development of URG prognostic signatures that are robust to both technical artifacts and biological complexity. Key considerations for implementation include:
Technology Selection: The choice of spatial omics platforms should balance resolution with coverage area, as technologies like Visium HD (2-55μm resolution) and Xenium (subcellular resolution) offer different advantages for URG localization studies [54].
Algorithm Selection: For large-scale integrations, methods like FAST and SPIRAL provide scalable solutions, while STELLAR enables annotation transfer across datasets using graph geometric learning [54].
Clinical Translation: Successful URG signatures like the 4-gene panel (CDC20, PCGF2, UBE2S, SOCS2) in breast cancer and the 6-gene panel in colon cancer demonstrate the clinical potential of this approach when heterogeneity is properly addressed [49] [55].
Future directions should focus on single-cell ubiquitination profiling, dynamic modeling of ubiquitination networks, and integration of URG signatures with therapeutic response prediction. The analytical framework presented here provides a foundation for developing URG-based biomarkers that can guide personalized cancer treatment strategies.
The 'Fit-for-Purpose' Principle in Analytical Method Validation
The clinical development of new anticancer drugs can be compromised by a lack of qualified biomarkers. An indispensable component to successful biomarker qualification is assay validation, which is also a regulatory requirement. To foster flexible yet rigorous biomarker method validation, the fit-for-purpose approach has been developed, creating a vital bridge between fundamental analytical science and applied clinical cancer research [58]. This framework is particularly crucial for validating assays that measure ubiquitination-related gene (URG) signatures, which have emerged as powerful prognostic tools across diverse cancer types including breast cancer, lung adenocarcinoma, ovarian cancer, and laryngeal cancer [49] [37] [11].
The core principle of fit-for-purpose validation is "the confirmation by examination and the provision of objective evidence that the particular requirements for a specific intended use are fulfilled" [58]. This approach recognizes that the stringency of validation should be dictated by the biomarker's position in the spectrum between research tool and clinical endpoint. For URG signatures, which function as prognostic clinical tools, robust validation is essential for clinical adoption and regulatory approval [58].
Fit-for-Purpose Validation Framework
Core Principle and Application to URG Signatures
The fit-for-purpose approach progresses through two parallel tracks that eventually converge. The first is experimental, focusing on establishing the method's purpose and agreeing upon outcomes, target values, or acceptance limits. The second is operational, characterizing assay performance through experimentation. The critical evaluation step involves comparing technical performance against predefined purpose-specific expectations [58].
For URG signatures, this means validation requirements differ based on the signature's specific clinical application. A signature intended for early cancer detection requires exceptional sensitivity and specificity, while one designed for monitoring treatment response must demonstrate robust quantitative characteristics over the dynamic range relevant to therapeutic intervention [58] [59].
The Validation Lifecycle
Biomarker method validation proceeds through five discrete stages, each with distinct objectives and deliverables for URG signature development [58]:
- Stage 1 (Definition): Define purpose and select candidate assay
- Stage 2 (Planning): Assemble reagents, write validation plan, finalize assay classification
- Stage 3 (Experimental Verification): Performance verification and fitness-for-purpose evaluation
- Stage 4 (In-Study Validation): Assess robustness in clinical context
- Stage 5 (Routine Use): Quality control monitoring and proficiency testing
This process incorporates continuous improvement through iterative refinement, potentially returning to earlier stages as new information emerges during validation [58].
Biomarker Assay Classification and Validation Parameters
Categorical Framework for Assay Validation
The American Association of Pharmaceutical Scientists (AAPS) and US Clinical Ligand Society have identified five general classes of biomarker assays, each requiring distinct validation approaches [58]:
Table 1: Biomarker Assay Categories and Definitions
| Assay Category | Definition | Examples in URG Research |
|---|---|---|
| Definitive Quantitative | Uses calibrators and regression model to calculate absolute quantitative values; reference standard fully characterized and representative of biomarker | Mass spectrometric analysis of ubiquitin conjugates |
| Relative Quantitative | Uses response-concentration calibration with reference standards not fully representative of biomarker | qPCR-based URG expression profiling |
| Quasi-Quantitative | No calibration standard, but continuous response expressed in terms of sample characteristic | Immunohistochemistry scoring of ubiquitination |
| Qualitative (Categorical) | Ordinal (discrete scoring scales) or nominal (yes/no situations) | Presence/absence of specific URG mutation |
Recommended Performance Parameters by Assay Category
The validation parameters investigated should align with the assay classification and intended use. The following table summarizes the consensus position on parameters for each biomarker assay class [58]:
Table 2: Recommended Performance Parameters for Biomarker Method Validation by Assay Category
| Performance Characteristic | Definitive Quantitative | Relative Quantitative | Quasi-Quantitative | Qualitative |
|---|---|---|---|---|
| Accuracy | + | |||
| Trueness (Bias) | + | + | ||
| Precision | + | + | + | |
| Reproducibility | + | |||
| Sensitivity | + | + | + | + |
| LLOQ | LLOQ | LLOQ | ||
| Specificity | + | + | + | + |
| Dilution Linearity | + | + | ||
| Parallelism | + | + | ||
| Assay Range | + | + | + | |
| Quantitation Range | LLOQ–ULOQ | LLOQ–ULOQ |
Abbreviations: LLOQ = lower limit of quantitation; ULOQ = upper limit of quantitation
Experimental Protocols for URG Signature Validation
Protocol: Definitive Quantitative Assay Validation for URG Expression
Purpose: To validate a reverse transcription quantitative PCR (RT-qPCR) assay for absolute quantification of URG expression in tumor samples [49] [35].
Materials and Reagents:
- RNA extraction kit (e.g., TRIzol)
- Reverse transcription system
- Quantitative PCR master mix
- Sequence-specific primers and probes for target URGs
- Calibrators (synthetic RNA standards)
- Nuclease-free water
- Quality control reference materials
Procedure:
- Sample Preparation: Extract RNA from 20-40 patient specimens representing the entire working range of the method and spectrum of expected diseases [60].
- Reverse Transcription: Convert RNA to cDNA using standardized conditions.
- Calibration Curve: Prepare 5-8 concentrations of synthetic RNA calibrators covering the expected quantitative range (e.g., 10²-10⁸ copies/μL).
- Analysis: Run calibrators and patient samples in triplicate across 3 separate days to assess inter-day variability [58].
- Data Analysis: Calculate accuracy profiles using β-expectation tolerance intervals to determine the confidence interval for future measurements [58].
Acceptance Criteria: During pre-study validation, precision and accuracy should typically vary by <25% (30% at LLOQ). For in-study patient sample analysis, adapt acceptance limits based on purpose, potentially using a 4:6:25 rule or confidence intervals [58].
Protocol: Comparison of Methods Experiment
Purpose: To estimate systematic error (inaccuracy) when implementing a new URG measurement method against an established comparative method [60].
Materials:
- Minimum 40 patient specimens covering entire working range
- Test and comparative method reagents and equipment
- Data analysis software with regression capabilities
Procedure:
- Sample Selection: Select 40+ different patient specimens covering the entire working range of the method, representing the spectrum of diseases expected in routine application [60].
- Analysis: Analyze specimens by both test and comparative methods within 2 hours of each other to minimize stability issues [60].
- Experimental Design: Include several analytical runs on different days (minimum 5 days recommended) to minimize systematic errors from a single run [60].
- Data Collection: If possible, perform duplicate measurements to identify sample mix-ups, transposition errors, and other mistakes.
Data Analysis:
- Graphical Assessment: Create difference plots (test minus comparative results vs. comparative result) or comparison plots (test result vs. comparative result).
- Statistical Calculations: For wide analytical ranges, use linear regression statistics (slope, y-intercept, standard deviation of points about the line). For narrow ranges, calculate average difference (bias) between methods [60].
- Systematic Error Estimation: For regression analysis, calculate Yc = a + bXc, then SE = Yc - Xc, where Xc is the medical decision concentration [60].
Protocol: Construction and Validation of URG Prognostic Signatures
Purpose: To develop and validate a ubiquitination-related gene signature for cancer prognosis prediction [38] [49] [37].
Materials:
- Gene expression datasets (TCGA, GEO)
- Statistical software (R with packages: glmnet, survminer, randomForestSRC)
- Ubiquitination-related gene database (IUUCD 2.0, UbiBrowser)
- Clinical outcome data
Procedure:
- Data Collection: Obtain RNA-seq data and clinical information from appropriate databases (TCGA, GEO) [38] [35].
- Differential Expression Analysis: Identify differentially expressed URGs using limma package with criteria such as fold change >2 and FDR <0.05 [38] [49].
- Prognostic Gene Screening: Perform univariate Cox regression to identify URGs associated with overall survival [49] [35].
- Feature Selection: Apply LASSO Cox regression with 10-fold cross-validation to select the most valuable prognostic genes [38] [49].
- Signature Construction: Calculate risk scores using the formula: Risk score = Σ(βi × Expi), where β represents coefficients from multivariate Cox regression and Exp denotes gene expression level [38] [49].
- Validation: Stratify patients into high-risk and low-risk groups based on median risk score and validate prognostic performance using Kaplan-Meier curves and log-rank tests [38] [35].
Visualization of Experimental Workflows
Fit-for-Purpose Validation Workflow
URG Prognostic Signature Development
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Research Reagents and Resources for URG Signature Validation
| Category | Specific Resource | Function/Application | Examples/Sources |
|---|---|---|---|
| Ubiquitin Gene Databases | iUUCD 2.0 Database | Comprehensive repository of ubiquitination-related genes | E1, E2, E3 enzymes; 966 URGs [11] |
| Gene Expression Data | TCGA, GEO Databases | Source of transcriptomic and clinical data for model development | TCGA-LUAD, GSE65858 [11] [35] |
| Statistical Analysis Tools | R Packages (glmnet, survminer) | Statistical analysis and prognostic model development | LASSO regression, survival analysis [38] [49] |
| Laboratory Reagents | RNA Extraction Kits, qPCR Reagents | Experimental validation of URG expression | TRIzol, reverse transcription systems [35] |
| Cell Line Resources | Validated Cancer Cell Lines | Functional validation of URG signatures | A2780, HEY ovarian cancer cells [37] |
Analytical Considerations for URG Signatures
Total Error and Acceptance Criteria
For definitive quantitative methods, analytical accuracy depends on the total error in the method, consisting of the sum of systematic error (bias) and random error (intermediate precision). Total error must account for all relevant sources of variation: day, analyst, analytical platform, or batch [58].
While bioanalysis of small molecules typically requires precision and accuracy within <15% (20% at LLOQ), more flexibility is allowed in biomarker method validation where 25% is often the default value (30% at LLOQ) during pre-study validation [58].
Method Comparison Approaches
When comparing URG measurement methods, several analytical approaches ensure proper validation:
- Bland-Altman Difference: Appropriate when evaluating bias of a candidate method and the comparative method is not a reference method [61]
- Direct Comparison: Suitable when the comparative method can be considered to give true results [61]
- Regression Analysis: Essential when the relationship between methods is concentration-dependent [60]
The accuracy profile approach recommended by the Societe Francaise des Sciences et Techniques Pharmaceutiques (SFSTP) provides a robust visual method to assess what percentage of future values will likely fall within pre-defined acceptance limits [58].
The fit-for-purpose principle provides a flexible yet rigorous framework for validating analytical methods, particularly those measuring ubiquitination-related gene signatures for cancer prognosis. By aligning validation stringency with intended use and applying appropriate performance criteria across the five biomarker assay categories, researchers can ensure their URG signatures meet regulatory requirements while providing clinically meaningful prognostic information. The experimental protocols and validation approaches outlined here provide a roadmap for developing robust, clinically applicable URG signatures that can ultimately guide personalized cancer treatment strategies.
The development of ubiquitination-related gene (URG) signatures for cancer prognosis represents a transformative approach in oncology research, offering potential for personalized treatment strategies. However, the clinical utility of these multi-gene signatures is entirely dependent on the implementation of rigorous technical and biological validation strategies. Ubiquitination, a crucial post-translational modification process involving E1 (activating), E2 (conjugating), and E3 (ligase) enzymes, regulates diverse cellular processes including protein degradation, cell cycle control, and DNA repair, with significant implications for tumor development and progression [38] [37]. The complex nature of ubiquitination pathways and the high-dimensional omics data used to derive URG signatures necessitate comprehensive validation frameworks to ensure prognostic models are robust, reproducible, and clinically applicable.
This application note provides detailed methodologies for establishing validation strategies that confirm both the technical reliability of URG signature assays and their biological relevance across diverse patient populations and cancer types. We focus specifically on practical protocols that researchers can implement throughout the development pipeline, from initial discovery to clinical translation.
Biological Validation Strategies
Functional Characterization of URGs
Biological validation begins with confirming the functional roles of identified URGs in relevant cancer pathways. The core methodology involves a series of interconnected experiments designed to establish mechanistic links.
Table 1: Key Experiments for Biological Validation of URGs
| Experiment Type | Key Readouts | Technical Replicates | Biological Replicates |
|---|---|---|---|
| Gene Knockdown/Knockout | Cell proliferation, apoptosis, colony formation | n ≥ 3 | n ≥ 2 independent experiments |
| Ubiquitination Assays | Ubiquitin conjugation, substrate stability | n ≥ 3 | n ≥ 2 independent experiments |
| Pathway Analysis | Downstream signaling activation | n ≥ 3 | n ≥ 2 independent experiments |
| Immunohistochemistry | Protein localization, expression levels | n ≥ 3 tissue sections | n ≥ 10 patient samples |
Protocol: Gene Silencing and Phenotypic Assays
Principle: Determine the functional consequences of modulating URG expression in cancer-relevant phenotypes.
Materials:
- Validated siRNA or CRISPR/Cas9 constructs targeting URGs
- Appropriate cancer cell lines (minimum of two: one representing good prognosis signature, one representing poor prognosis signature)
- Transfection reagents (e.g., Lipofectamine-based systems)
- Cell culture media and supplements
- Assay kits for proliferation, apoptosis, and invasion
Procedure:
- Cell Seeding: Plate cells in 96-well or 6-well plates at 30-50% confluence 24 hours prior to transfection.
- Gene Modulation: Transfect cells with URG-targeting siRNA (10-50 nM) or CRISPR/Cas9 constructs using appropriate transfection reagents per manufacturer's protocol.
- Efficiency Validation: 48-72 hours post-transfection, harvest cells and validate knockdown efficiency via qRT-PCR (for siRNA) or western blotting (for protein).
- Phenotypic Assays:
- Proliferation: Use MTT or CCK-8 assays at 0, 24, 48, and 72 hours post-transfection.
- Apoptosis: Analyze using Annexin V/propidium iodide staining with flow cytometry.
- Invasion/Migration: Perform Transwell assays with Matrigel coating (invasion) or without (migration).
- Data Analysis: Normalize all measurements to negative control transfection groups. Statistical analysis should include Student's t-test for comparisons between two groups or ANOVA for multiple groups, with p < 0.05 considered significant.
Protocol: Co-immunoprecipitation for Ubiquitination Detection
Principle: Directly confirm ubiquitination of putative substrates by URGs.
Materials:
- Antibodies against URGs and putative substrates
- Protein A/G agarose beads
- Lysis buffer (50 mM Tris-HCl pH 7.4, 150 mM NaCl, 1 mM EDTA, 1% NP-40) supplemented with protease inhibitors and 10 mM N-ethylmaleimide (to inhibit deubiquitinases)
- Ubiquitin detection antibody
- HEK293T or other suitable mammalian cells for overexpression studies
Procedure:
- Cell Transfection: Co-transfect cells with plasmids expressing URG, putative substrate, and HA- or MYC-tagged ubiquitin.
- Protein Extraction: 48 hours post-transfection, lyse cells in lysis buffer. Clear lysates by centrifugation at 14,000 × g for 15 minutes at 4°C.
- Immunoprecipitation: Incubate 500 μg of total protein with 2 μg of substrate antibody overnight at 4°C. Add protein A/G beads and incubate for 2-4 hours.
- Washing and Elution: Wash beads 3-5 times with lysis buffer. Elute proteins with 2× Laemmli buffer at 95°C for 5 minutes.
- Detection: Analyze eluates by western blotting using ubiquitin antibody to detect ubiquitinated substrates and URG antibody to confirm interaction.
Immune Microenvironment Validation
URG signatures have demonstrated significant associations with tumor immune microenvironments, necessitating validation of these interactions [38] [37].
Protocol: Immune Cell Infiltration Analysis
Principle: Quantify immune cell populations in tumors stratified by URG signature risk groups.
Materials:
- Tumor tissue sections (formalin-fixed, paraffin-embedded)
- Antibodies for immune cell markers (CD8, CD4, CD68, CD20, etc.)
- Immunofluorescence staining equipment
- Flow cytometry-capable tumor dissociation kits (for fresh tissues)
- CIBERSORT or similar computational deconvolution software
Procedure:
- Tissue Staining: Perform multiplex immunofluorescence staining for T-cell (CD3+, CD8+), B-cell (CD20+), and macrophage (CD68+) markers on sequential tissue sections.
- Digital Image Analysis: Scan slides and quantify immune cell densities in intratumoral and stromal regions using automated image analysis software.
- Flow Cytometry: For fresh tissues, dissociate tumors to single-cell suspensions, stain with immune cell marker antibodies, and analyze by flow cytometry.
- Computational Validation: Use transcriptomic data and CIBERSORT analysis to infer immune cell proportions in URG high-risk versus low-risk groups.
- Statistical Correlation: Correlate URG expression patterns with immune cell infiltration using Spearman correlation analysis.
Technical Validation Strategies
Analytical Validation of URG Signatures
Technical validation ensures that URG signature assays consistently and accurately measure what they claim to measure across different experimental conditions and platforms.
Table 2: Technical Performance Standards for URG Signature Assays
| Performance Characteristic | Acceptance Criteria | Validation Approach |
|---|---|---|
| Accuracy | ≥ 90% agreement with reference method | Comparison to gold standard (e.g., RNA-seq) |
| Precision | CV ≤ 15% for intra-assay; CV ≤ 20% for inter-assay | Repeated measurements of same samples |
| Sensitivity | Limit of detection: 0.1-1 ng RNA | Dilution series of known RNA quantities |
| Specificity | No cross-reactivity with homologous genes | Blast analysis of primers/probes |
| Reproducibility | ≥ 95% concordance between operators/labs | Inter-laboratory study with standardized protocols |
Protocol: Platform Transfer and Cross-Platform Validation
Principle: Ensure URG signatures maintain prognostic performance when transferred across different measurement platforms.
Materials:
- RNA samples with known URG risk scores (minimum n=30, representing range of risk scores)
- Multiple platform reagents: RNA-seq, microarray, Nanostring, qRT-PCR
- Bioinformatics tools for data normalization and transformation
Procedure:
- Sample Preparation: Distribute aliquots of the same RNA samples to different platforms following manufacturer's specifications for RNA quality and quantity.
- Parallel Processing: Process samples on all platforms within the same timeframe to minimize degradation effects.
- Data Normalization: Apply platform-specific normalization methods (e.g., RMA for microarray, TPM for RNA-seq, housekeeping genes for qRT-PCR).
- Signature Application: Apply the pre-specified URG signature algorithm to each platform's data to calculate risk scores.
- Concordance Assessment: Calculate intraclass correlation coefficients (ICC) between risk scores derived from different platforms. ICC > 0.9 indicates excellent reproducibility.
- Prognostic Consistency: Compare Kaplan-Meier survival curves between risk groups for each platform. Consistent separation indicates robust signature performance.
Statistical Validation of Prognostic Performance
Robust statistical validation is essential to demonstrate that URG signatures provide prognostic value beyond standard clinical parameters and are not overfitted to the development dataset.
Protocol: Internal Validation Using Resampling Methods
Principle: Estimate the optimism (overfitting) in prognostic model performance using resampling techniques [62].
Materials:
- Dataset with clinical outcomes and URG expression data (minimum n=100 for reliable validation)
- Statistical software with penalized regression capabilities (R recommended)
- Computing resources capable of handling iterative resampling
Procedure:
- Model Development: Develop the URG signature using the entire dataset with appropriate penalized regression methods (LASSO or elastic net) to minimize overfitting.
- k-Fold Cross-Validation:
- Randomly split data into k equal subsets (typically k=5 or 10)
- Iteratively use k-1 folds for model training and the remaining fold for validation
- Repeat process k times until each subset has served as validation
- Calculate performance metrics (C-index, time-dependent AUC) for each iteration
- Bootstrap Validation:
- Generate 100-200 bootstrap samples by resampling with replacement
- Develop model on each bootstrap sample and test on full original sample
- Calculate optimism as performance on bootstrap sample minus performance on original sample
- Apply optimism correction to original model performance
- Nested Cross-Validation: For small sample sizes (n < 200), implement nested cross-validation with inner loop for hyperparameter tuning and outer loop for performance estimation.
Protocol: External Validation in Independent Cohorts
Principle: Demonstrate generalizability of URG signatures in completely independent patient populations [38] [63].
Materials:
- Independent validation cohort with similar inclusion criteria to development cohort
- Pre-specified statistical analysis plan
- Clinical and outcome data for the validation cohort
Procedure:
- Cohort Selection: Identify appropriate validation cohort(s) with comparable patient characteristics but potential differences in geography, treatment era, or sample processing.
- Blinded Analysis: Apply the pre-specified URG signature algorithm without any model retraining or parameter adjustments.
- Performance Assessment:
- Discrimination: Calculate C-index and time-dependent AUC for survival prediction
- Calibration: Assess agreement between predicted and observed outcomes using calibration plots
- Clinical Net Benefit: Compare signature stratification against standard staging using decision curve analysis
- Subgroup Analysis: Evaluate signature performance across predefined subgroups (e.g., by cancer stage, treatment type, molecular subtypes).
Integrated Validation Workflow
A comprehensive URG validation strategy incorporates both technical and biological elements throughout the development pipeline, from discovery to clinical application.
Research Reagent Solutions
Table 3: Essential Research Reagents for URG Validation Studies
| Reagent Category | Specific Examples | Primary Function in Validation |
|---|---|---|
| Ubiquitination Assay Kits | Ubiquitin Ligase Assay Kit (Cayman Chemical), Ubiquitination Assay Kit (Abcam) | In vitro confirmation of E3 ligase activity and substrate ubiquitination |
| URG Antibodies | Anti-CDC34, Anti-FZR1, Anti-OTULIN, Anti-FBXO45 [38] [37] | Protein expression validation, immunohistochemistry, western blotting |
| Proteasome Inhibitors | MG-132, Bortezomib, Carfilzomib | Stabilization of ubiquitinated proteins for detection |
| Ubiquitin Mutants | K48-only, K63-only ubiquitin mutants, Ubiquitin-aldehyde | Determining ubiquitin chain linkage specificity |
| PCR/RNA-seq Reagents | TaqMan Gene Expression Assays, SMARTer RNA-seq kits | Transcriptomic validation of URG expression patterns |
| Cell Line Models | A2780 (ovarian), DLBCL cell lines, HEK293T (overexpression) [38] [37] | Functional validation in relevant biological contexts |
| Bioinformatics Tools | CIBERSORT, ESTIMATE, maftools, survminer [38] [37] | Computational validation in tumor microenvironments and clinical datasets |
Robust technical and biological validation represents the critical path for translating promising URG signatures from discovery to clinical utility. The integrated framework presented here addresses both analytical performance and biological relevance, providing researchers with a comprehensive roadmap for establishing URG signatures as reliable prognostic tools. As ubiquitination-targeted therapies like PROTACs continue to advance [37], rigorously validated URG signatures will play an increasingly important role in guiding targeted treatment strategies and advancing personalized cancer care.
The ubiquitin-proteasome system represents a critical regulatory network in oncogenesis and tumor progression, governing protein degradation and influencing virtually all cellular processes. Recent advances in bioinformatics have enabled the identification of ubiquitination-related gene (URG) signatures with significant prognostic value across diverse cancer types, including diffuse large B-cell lymphoma (DLBCL), ovarian cancer, and lung adenocarcinoma [38] [37] [11]. These signatures demonstrate remarkable potential for stratifying patient risk, predicting therapeutic response, and guiding personalized treatment strategies. However, the translation of these computational discoveries into robust, clinically applicable assays presents substantial methodological challenges. This protocol details a comprehensive framework for validating URG signatures through analytical and clinical verification stages, providing researchers with standardized procedures to bridge the gap between bioinformatics discovery and clinical implementation.
Key URG Signatures and Their Clinical Implications
Table 1: Prognostic Ubiquitination-Related Gene Signatures in Oncology
| Cancer Type | Key URG Signature Genes | Prognostic Value | Biological Pathways | Citation |
|---|---|---|---|---|
| Diffuse Large B-Cell Lymphoma (DLBCL) | CDC34, FZR1, OTULIN | Elevated CDC34/FZR1 with low OTULIN correlated with poor prognosis | Endocytosis, T-cell regulation | [38] |
| Ovarian Cancer | 17-gene signature (including FBXO45) | High-risk group had significantly lower overall survival (P < 0.05) | Wnt/β-catenin signaling | [37] |
| Lung Adenocarcinoma (LUAD) | DTL, UBE2S, CISH, STC1 | Higher URRS associated with worse prognosis (HR = 0.54, p < 0.001) | PD1/PD-L1, TMB, TME | [11] |
The consistent emergence of URG signatures across multiple cancer types underscores the fundamental role of ubiquitination in tumor biology. In DLBCL, a 3-gene signature comprising CDC34, FZR1, and OTULIN effectively stratifies patients into distinct prognostic subgroups, with elevated expression of CDC34 and FZR1 coupled with low OTULIN expression correlating with poor outcomes [38]. Similarly, in ovarian cancer, a 17-gene URG signature identifies patients with significantly different overall survival, while in lung adenocarcinoma, a 4-gene signature (DTL, UBE2S, CISH, and STC1) demonstrates robust prognostic performance across multiple validation cohorts [37] [11]. These signatures not only predict survival but also correlate with therapeutic response, tumor microenvironment composition, and immune infiltration patterns, offering multidimensional clinical insights beyond conventional staging systems.
Experimental Protocol: From Bioinformatics Discovery to Clinical Validation
Stage 1: Computational Identification and Analytical Validation
Data Acquisition and Pre-processing
- Data Sources: Utilize publicly available repositories including TCGA (The Cancer Genome Atlas), GEO (Gene Expression Omnibus), and GTEx databases for gene expression profiles and corresponding clinical data [38] [37] [11].
- Inclusion Criteria: Apply consistent filtering criteria across datasets, excluding patients with survival time <3 months, formalin-fixed samples, and recurrent tissues to minimize confounding variables [11].
- Ubiquitination Gene Compendium: Compile comprehensive URG lists from specialized databases such as iUUCD 2.0 (approximately 966 genes) or UUCD (929 genes), categorized into E1 (activators), E2 (conjugators), and E3 (ligases) enzymes [37] [11].
Signature Development and Computational Validation
- Differential Expression Analysis: Identify differentially expressed URGs using the "limma" R package with thresholds of |logFC| ≥ 1-2 and adjusted p-value < 0.05 [38] [37].
- Prognostic Modeling: Apply multivariate Cox regression analysis, LASSO Cox regression, and Random Survival Forests to identify optimal gene combinations [38] [11].
- Risk Score Calculation: Compute risk scores using the formula: Risk score = Σ(βi × Expi), where β represents the coefficient from multivariate Cox regression and Exp denotes gene expression level [38].
- Validation Framework: Employ both internal (cross-validation) and external (independent cohorts) validation strategies to assess signature robustness [11].
Stage 2: Wet-Lab Experimental Validation
Cell Culture and Transfection
- Cell Lines: Utilize authenticated cancer cell lines relevant to the cancer type of interest (e.g., A2780 and HEY for ovarian cancer) [37].
- Validation: Perform short tandem repeat (STR) analysis and mycoplasma testing to ensure cell line authenticity and absence of contamination [37].
- Culture Conditions: Maintain cells in appropriate media (DMEM or RPMI 1640) supplemented with 10% fetal bovine serum and 1% penicillin-streptomycin at 37°C with 5% CO₂ [37].
- Gene Manipulation: Employ transfection reagents (e.g., Lipo8000) for overexpression or knockdown of signature URGs using plasmid constructs or siRNAs [37].
Functional Validation Assays
Proliferation Assessment:
- Perform MTT or CCK-8 assays at 0, 24, 48, and 72 hours post-transfection
- Plate 2-3 × 10³ cells per well in 96-well plates
- Measure absorbance at 450-490 nm using a microplate reader
Migration and Invasion Capacity:
- Utilize Transwell chambers (8-μm pore size) pre-coated with (invasion) or without (migration) Matrigel
- Seed 5-10 × 10⁴ cells in serum-free medium in the upper chamber
- Add complete medium to the lower chamber as chemoattractant
- After 24-48 hours, fix with methanol and stain with 0.1% crystal violet
- Count cells in five random fields under a microscope
Apoptosis Analysis:
- Detect apoptotic cells using Annexin V-FITC/PI staining followed by flow cytometry
- Analyze data with FlowJo software
Molecular Pathway Investigation
Western Blot Analysis:
- Extract total proteins using RIPA lysis buffer with protease inhibitors
- Separate 20-40 μg protein by SDS-PAGE and transfer to PVDF membranes
- Block with 5% non-fat milk for 1 hour at room temperature
- Incubate with primary antibodies (1:1000) overnight at 4°C
- Incubate with HRP-conjugated secondary antibodies (1:5000) for 1 hour at room temperature
- Visualize using enhanced chemiluminescence substrate
Pathway-Focused PCR Arrays:
- Utilize commercially available pathway-specific PCR arrays (e.g., Wnt/β-catenin, NF-κB, or apoptosis pathways)
- Isolve total RNA using TRIzol reagent
- Synthesize cDNA using reverse transcription kits
- Perform qPCR according to manufacturer's instructions
The Scientist's Toolkit: Essential Research Reagents and Solutions
Table 2: Key Research Reagent Solutions for URG Signature Validation
| Reagent Category | Specific Examples | Application Purpose | Technical Notes |
|---|---|---|---|
| Cell Culture Media | DMEM, RPMI 1640 (Gibco) | Cell line maintenance | Supplement with 10% FBS and 1% penicillin-streptomycin |
| Transfection Reagents | Lipo8000 | Introduction of genetic constructs | Optimize reagent:DNA ratio for specific cell lines |
| Antibody Sources | Wuhan Boster Biological Technology | Western blot, IHC detection | Validate specificity for target proteins |
| RNA Isolation Kits | TRIzol-based systems | Total RNA extraction | Ensure RNA integrity number (RIN) >8.0 for sequencing |
| Ubiquitination Assays | PROTAC molecules, E1/E2/E3 inhibitors | Functional validation of ubiquitination | Include MG132 proteasome inhibitor controls |
Clinical Translation: Analytical and Clinical Validation Framework
Analytical Validation for Clinical Implementation
- Reference Genome Standards: Adopt hg38 as the reference genome for alignment to ensure consistency with current clinical standards [64].
- Comprehensive Variant Calling: Implement a standardized set of analyses including single nucleotide variants (SNV), copy number variants (CNV), structural variants (SV), short tandem repeats (STR), and loss of heterozygosity (LOH) [64].
- Quality Assurance Protocols:
- Verify data integrity using file hashing (e.g., MD5 or sha1)
- Confirm sample identity through genetic fingerprinting and relatedness checks
- Implement containerized software environments for reproducibility [64]
- Performance Validation: Utilize standard truth sets (GIAB for germline, SEQC2 for somatic) supplemented by recall testing of previous clinical cases [64].
Clinical Verification and Utility Assessment
- Prognostic Performance: Evaluate the signature's ability to stratify patients into distinct risk groups with significant differences in overall survival, recurrence-free survival, or other clinically relevant endpoints [38] [37] [11].
- Predictive Value Assessment:
- Clinical Utility Determination:
- Assess whether signature implementation changes clinical decision-making
- Evaluate impact on patient outcomes in prospective studies
- Analyze cost-effectiveness of signature-guided therapy selection
The translation of ubiquitination-related gene signatures from bioinformatics discoveries to clinical assays represents a promising frontier in precision oncology. The standardized framework presented herein provides a comprehensive roadmap for researchers seeking to validate and implement these molecular signatures in clinical practice. Through rigorous computational analysis, systematic experimental validation, and adherence to established clinical standards, URG signatures can evolve into powerful tools for patient stratification, therapeutic selection, and ultimately, improved cancer care. As the field advances, continued refinement of these protocols will be essential to fully realize the clinical potential of ubiquitination-based biomarkers across the oncological spectrum.
Cost and Accessibility Considerations for Widespread Clinical Adoption
The development of ubiquitination-related gene (URG) signatures represents a significant advancement in the field of cancer prognostics, offering the potential for refined risk stratification and treatment personalization for diseases such as Diffuse Large B-Cell Lymphoma (DLBCL), breast cancer, and laryngeal cancer [38] [49] [39]. However, for these molecular tools to transition from research discoveries to clinically impactful tests, specific cost and accessibility considerations must be addressed. Widespread clinical adoption is contingent not only on prognostic accuracy but also on the economic viability and practical implementability of the technology across diverse healthcare settings. This document outlines the major cost components, evaluates accessibility challenges, and provides detailed application protocols to facilitate the broader clinical integration of URG-based prognostic signatures.
Quantitative Cost Analysis of URG Signature Implementation
The deployment of a URG prognostic test in a clinical setting involves initial development, validation, and recurring operational costs. The primary expenditures are associated with genomic data generation, computational analysis, and clinical reporting. The following table summarizes the key cost components and factors influencing their variability.
Table 1: Cost Components for Clinical Implementation of a URG Prognostic Signature
| Cost Category | Description | Key Cost Drivers & Variability |
|---|---|---|
| Data Generation | Expenses related to generating gene expression data from patient tumor samples. | - Technology Platform: RNA sequencing (RNA-seq) provides comprehensive data but is more costly than targeted assays like RT-qPCR or nanostring.- Sample Throughput: Batch processing can reduce per-sample costs.- Sample Quality & Preparation: RNA preservation and extraction methods impact success rates and costs. |
| Bioinformatic Analysis | Costs for the computational infrastructure and personnel required to process raw data and calculate risk scores. | - Software Licensing: Use of commercial software vs. open-source tools (e.g., R packages).- Computational Resources: Cloud computing fees vs. maintaining on-premise servers.- Bioinformatician Salaries: Expertise required for pipeline maintenance and result interpretation. |
| Signature Scoring | The process of applying the specific URG model (e.g., Risk score = Σ(Coefficient * Gene Expression)) to patient data. |
- Model Complexity: Number of genes in the signature (e.g., 3-gene for DLBCL [38], 4-gene for breast cancer [49]).- Algorithm: Standardized scoring algorithms reduce computational costs. |
| Validation & Compliance | Costs associated with analytical and clinical validation to meet regulatory standards (e.g., FDA, CLIA). | - Scope of Validation: Number of samples and clinical cohorts required.- Regulatory Pathway: Complexity of clearance/approval from bodies like the FDA [65]. |
The most significant factor influencing cost is the choice of technology for data generation. While research studies often utilize bulk RNA-Seq from databases like TCGA and GEO for signature discovery [49] [39], clinical applications may favor more targeted, cost-effective methods like RT-qPCR for routine use. Furthermore, the development of standardized, automated bioinformatic pipelines, potentially leveraging open-source tools such as the GSVA or AUCell R packages used in research settings [66], can significantly reduce the ongoing operational costs associated with data analysis.
Accessibility Challenges and Strategic Solutions
Achieving equitable access to URG-based testing requires overcoming several barriers related to infrastructure, expertise, and economic models.
Table 2: Key Accessibility Challenges and Proposed Mitigation Strategies
| Accessibility Challenge | Impact on Adoption | Proposed Mitigation Strategy |
|---|---|---|
| Computational Infrastructure | Hospitals without robust bioinformatics departments cannot perform in-house analysis. | - Centralized Reference Labs: Establish specialized labs to process samples from multiple centers.- Cloud-Based Solutions: Develop user-friendly web portals where clinicians can upload data and receive reports.- Simplified Outputs: Integrate signature scoring into existing clinical laboratory software. |
| Technical Expertise Gap | Oncologists and pathologists may lack training to interpret complex genomic risk scores. | - Clear Reporting: Generate patient reports that clearly state risk category (High/Low) and clinical implications.- Educational Initiatives: Develop guidelines and training on the clinical utility of URG signatures.- Decision Support Tools: Integrate prognostic results with clinical data in electronic health records. |
| Reimbursement & Economic Model | Uncertainty regarding insurance coverage can deter healthcare providers from offering the test. | - Health Economic Studies: Conduct cost-effectiveness analyses demonstrating long-term savings from improved treatment allocation.- Phased Implementation: Initially offer testing within the context of clinical trials or research protocols to generate real-world evidence.- Engage Payers Early: Collaborate with insurance companies to establish coverage policies based on clinical utility. |
Detailed Experimental and Computational Protocols
To ensure reproducibility and facilitate adoption, standardized protocols for both wet-lab and computational procedures are essential.
Protocol: Gene Expression Quantification from FFPE Tissue
This protocol is critical for generating the input data for the URG signature from the most common type of clinical specimen, Formalin-Fixed Paraffin-Embedded (FFPE) tissue.
Key Research Reagent Solutions:
- RNA Extraction Kit (FFPE-grade): Specifically designed to recover fragmented RNA from archived tissues. Function: Isolates high-quality RNA for downstream applications.
- Reverse Transcription Kit with Random Hexamers: Converts RNA into complementary DNA (cDNA). Function: Essential for preparing RNA for either RT-qPCR or RNA-seq library preparation.
- RT-qPCR Assay: Includes primers and probes specific for the signature genes (e.g., CDC34, FZR1, OTULIN for DLBCL [38]) and reference genes (e.g., GAPDH, ACTB). Function: Enables precise, targeted quantification of gene expression.
- RNA-Seq Library Prep Kit: For comprehensive transcriptome profiling. Function: Prepares cDNA libraries for sequencing on platforms like Illumina.
Methodology:
- RNA Extraction: Following deparaffinization, extract total RNA from 3-5 sections (5-10 µm thick) of FFPE tissue using an FFPE-grade RNA extraction kit. Quantify RNA yield and assess quality using an instrument like a Fragment Analyzer; an RNA Quality Number (RQN) >5 is generally acceptable for targeted assays.
- cDNA Synthesis: Reverse transcribe 100-500 ng of total RNA into cDNA using a reverse transcription kit with random hexamers.
- Gene Expression Quantification (Two Options):
- Option A - RT-qPCR: Perform RT-qPCR in triplicate for each signature gene and reference genes. Use a standard thermal cycling protocol. Calculate the relative expression (e.g., ΔCq method) for each gene.
- Option B - RNA Sequencing: Prepare sequencing libraries from the cDNA using a stranded mRNA-seq library prep kit. Sequence the libraries on an appropriate platform to a minimum depth of 20 million reads per sample.
- Data Normalization: For RT-qPCR, normalize target gene Cq values to the average of reference genes. For RNA-seq data, normalize raw read counts using a method like TPM (Transcripts Per Million) or perform variance-stabilizing transformation as part of the bioinformatic pipeline [38].
Protocol: Computational Risk Score Calculation and Stratification
This protocol details the steps to process gene expression data and generate a clinical risk categorization.
Methodology:
- Data Input and Preprocessing:
- Input the normalized gene expression matrix.
- Log2-transform the expression values if necessary (typical for RNA-seq data).
- Z-score normalize the expression of each URG across the patient cohort to ensure all genes are on a comparable scale.
- Risk Score Calculation:
- Apply the predefined signature formula. For example, a generic risk score is calculated as:
Risk Score = (β₁ * Exp₁) + (β₂ * Exp₂) + ... + (βₙ * Expₙ)where β is the coefficient for each gene derived from the original multivariate Cox model, and Exp is the normalized expression value of that gene for the patient [38] [49]. - Example: A DLBCL risk score might be calculated as:
Risk Score = (0.25 * Z-score(CDC34)) + (0.31 * Z-score(FZR1)) + (-0.19 * Z-score(OTULIN))[38].
- Apply the predefined signature formula. For example, a generic risk score is calculated as:
- Patient Stratification:
- Report Generation:
- Generate a clinical report stating the patient's risk group, the associated prognostic implications, and a note on the assay's validation status.
Visualization of Clinical Implementation Workflow
The following diagram illustrates the end-to-end process from sample collection to clinical reporting, highlighting key decision points and cost centers.
Diagram 1: Clinical URG Testing Workflow and Cost Centers.
The transition of ubiquitination-related gene signatures from robust research tools to routine clinical tests is a multi-faceted challenge centered on economics and accessibility. By focusing on strategic cost management through technology choice and process standardization, and by proactively addressing barriers related to infrastructure and expertise, the translational pathway can be significantly accelerated. The detailed cost analyses and standardized protocols provided here serve as a foundational guide for laboratories and institutions aiming to implement these powerful prognostic assays, ultimately contributing to more personalized and effective cancer care.
Validation Frameworks and Competitive Analysis of URG Signatures
The FDA Biomarker Qualification Program (BQP) represents a critical regulatory pathway for the development and acceptance of biomarkers for use in drug development. Established to address the challenge that "there is really no one in charge of developing them," the program provides a structured framework for collaborative biomarker validation outside of any single drug application [67]. The mission of the BQP is to work with external stakeholders to develop biomarkers as drug development tools (DDTs), with qualified biomarkers having the potential to advance public health by encouraging efficiencies and innovation in drug development [68].
Qualification is defined as a conclusion that within the stated context of use (COU), the DDT can be relied upon to have a specific interpretation and application in drug development and regulatory review [69]. Once qualified, biomarkers become publicly available for any drug development program for the qualified COU, and can generally be included in IND, NDA, or BLA submissions without needing FDA to reconsider and reconfirm their suitability [69]. This program is particularly valuable for biomarkers intended for widespread use across multiple drug development programs, such as ubiquitination-related gene (URG) signatures for cancer prognosis, where individual sponsors may lack the resources or incentive to undertake complete validation independently.
The Biomarker Qualification Pathway
Structured Submission Process
The BQP operates through a well-defined, multi-stage submission process formalized by the 21st Century Cures Act in 2016 [69] [67]. This process involves three distinct stages that provide increasing levels of detail for biomarker development:
- Stage 1: Letter of Intent (LOI) - Initial submission containing background information on the biomarker and its proposed context of use
- Stage 2: Qualification Plan (QP) - Detailed development plan outlining the intended studies and data to support qualification
- Stage 3: Full Qualification Package (FQP) - Complete submission of all data and analyses supporting the biomarker's qualification [70]
The FDA aims to complete reviews of LOIs, QPs, and FQPs within 3, 6, and 10 months respectively, though actual review times have frequently exceeded these targets [71]. For instance, LOI reviews have taken a median of 6 months (twice as long as the target), while QP reviews have taken a median of 14 months [71].
Program Performance and Challenges
An analysis of the BQP's performance reveals several important trends and challenges:
- As of July 2025, only eight biomarkers have been fully qualified through the program, with seven of these qualified before the 21st Century Cures Act was enacted in 2016 [71]
- Approximately half of accepted projects (30/61) remain at the initial LOI stage [71]
- Safety biomarkers represent the most successfully qualified category (4/8), while biomarkers intended as surrogate endpoints have seen limited success [67] [71]
- Development of Qualification Plans is time-consuming, taking a median of 32 months, with surrogate endpoints requiring even longer (47 months) [71]
These statistics indicate that while the BQP provides a valuable pathway for certain biomarker types, researchers developing novel prognostic signatures, such as URG-based cancer biomarkers, should be prepared for substantial time investments and consider alternative pathways where appropriate.
Figure 1: The FDA Biomarker Qualification Process follows a structured, multi-stage pathway with defined review targets at each stage [69] [70].
Application to Ubiquitination-Related Gene Signatures
Ubiquitination Signatures as Prognostic Biomarkers
Recent research has demonstrated the significant potential of ubiquitination-related gene (URG) signatures as prognostic biomarkers across multiple cancer types. The ubiquitin-proteasome system, comprising ubiquitin-activating enzymes (E1s), ubiquitin-conjugating enzymes (E2s), ubiquitin ligases (E3s), and deubiquitinating enzymes, plays a crucial regulatory role in tumor development and progression [38] [11]. Several studies have successfully developed URG-based prognostic models:
In Diffuse Large B-Cell Lymphoma (DLBCL), a ubiquitination-based prognostic signature identified three key ubiquitination-related genes (CDC34, FZR1, and OTULIN) that effectively stratified patients into high-risk and low-risk groups with significant survival differences [38]. Elevated expression of CDC34 and FZR1, coupled with low expression of OTULIN, correlated with poor prognosis, and the signature demonstrated relationships with immune microenvironment composition and drug sensitivity [38].
Similarly, in lung adenocarcinoma (LUAD), researchers constructed a ubiquitination-related risk score (URRS) based on four genes (DTL, UBE2S, CISH, and STC1) that significantly predicted patient prognosis [11]. Patients with higher URRS had worse outcomes (Hazard Ratio [HR] = 0.54, 95% Confidence Interval [CI]: 0.39-0.73, p < 0.001), with validation across six external cohorts confirming the prognostic value [11].
For liver hepatocellular carcinoma (LIHC), a twelve-URG signature effectively categorized patients into distinct risk groups, with high-risk patients showing significantly reduced overall survival and progression-free survival [72]. This signature also correlated with immune status and drug sensitivity patterns, highlighting its potential clinical utility [72].
Experimental Protocols for URG Signature Development
The development of robust URG signatures for regulatory qualification requires methodologically sound approaches. Below is a detailed protocol for constructing and validating ubiquitination-related prognostic signatures:
Protocol 1: URG Signature Development and Validation
Step 1: Data Acquisition and Preprocessing
- Obtain gene expression profiles and clinical data from public databases (e.g., TCGA, GEO) [38] [11]
- Acquire ubiquitination-related genes from specialized databases (e.g., iUUCD 2.0) [11] [73]
- Preprocess data: normalize expression values, filter low-expression genes, and remove outliers
Step 2: Identification of Prognostic URGs
- Perform differential expression analysis between tumor and normal tissues using R package "limma" [73]
- Conduct survival analysis (univariate Cox regression) to identify URGs associated with patient outcomes
- Apply LASSO Cox regression to select the most informative genes and prevent overfitting [38] [11]
Step 3: Signature Construction
- Calculate risk scores using the formula: Risk score = Σ(βi × Expi) where β represents coefficients from multivariate Cox regression and Exp denotes gene expression levels [11]
- Stratify patients into high-risk and low-risk groups based on median risk score
- Validate signature performance in independent datasets
Step 4: Comprehensive Functional Characterization
- Analyze immune microenvironment composition using CIBERSORT or similar tools [38]
- Assess tumor mutation burden (TMB) and neoantigen load between risk groups [11]
- Evaluate drug sensitivity patterns using appropriate packages (e.g., oncoPredict) [38]
- Perform pathway enrichment analysis (GO, KEGG) to understand biological mechanisms [73]
Table 1: Key Research Reagent Solutions for URG Signature Development
| Reagent/Resource | Function | Source |
|---|---|---|
| iUUCD 2.0 Database | Comprehensive repository of ubiquitination-related genes | [11] [73] |
| TCGA Datasets | Clinical and genomic data for model training and validation | [11] [73] |
| GEO Datasets | Independent datasets for external validation | [38] [11] |
| CIBERSORT Algorithm | Deconvolution of immune cell infiltration from expression data | [38] |
| oncoPredict Package | Prediction of drug sensitivity based on genomic features | [38] |
Protocol 2: Analytical Validation for Regulatory Submission
Step 1: Assay Performance Verification
- Establish precision, accuracy, and reproducibility of the URG measurement platform
- Determine linearity, limits of detection, and quantification for each signature component
- Verify sample stability under various storage conditions
Step 2: Clinical Cutpoint Validation
- Apply predetermined cutpoints to independent validation cohorts
- Assess robustness of risk stratification across patient subgroups
- Evaluate performance consistency across different clinical sites
Step 3: Computational Validation
- Verify signature algorithm implementation and computational reproducibility
- Conduct sensitivity analyses to assess impact of individual component genes
- Perform cross-platform compatibility assessments if applicable
Figure 2: Experimental workflow for developing ubiquitination-related gene signatures, from initial data acquisition through regulatory preparation [38] [11] [73].
Strategic Implementation for URG Signature Qualification
Context of Use Definition
A critical component of successful biomarker qualification is the precise definition of the context of use (COU). For URG signatures in cancer prognosis, the COU should clearly specify:
- Intended Purpose: Prognostic stratification, therapy selection, or disease monitoring
- Patient Population: Specific cancer type, stage, and relevant molecular subtypes
- Technical Specifications: Measurement platform, sample requirements, and analysis protocol
- Interpretation Guidelines: Risk score calculation and clinical decision thresholds
The qualified COU defines the boundaries within which the available data adequately justify use of the biomarker, and as additional data are obtained, researchers can submit new projects to expand upon a qualified COU [69].
Evidence Generation Strategy
Given the program's historical challenges with novel biomarker types, researchers pursuing qualification of URG signatures should consider the following strategic approaches:
- Generate Multi-Omics Evidence: Combine genomic, transcriptomic, and proteomic data to strengthen biological plausibility [74]
- Demonstrate Clinical Utility: Establish clear relationships between URG signatures and clinically relevant endpoints (overall survival, treatment response) [38] [11]
- Validate Across Diverse Cohorts: Ensure performance consistency across multiple independent patient populations [11] [73]
- Characterize Mechanistic Foundations: Elucidate the biological pathways connecting ubiquitination processes to cancer prognosis [74]
Table 2: BQP Submission Characteristics and Considerations for URG Signatures
| Submission Aspect | Current Program State | URG-Specific Considerations |
|---|---|---|
| Review Timelines | Frequently exceed targets (LOI: 6 months median) [71] | Plan for potential delays; initiate early |
| Success Rates | 8 biomarkers qualified total; none since 2018 [71] | Consider parallel pathways (e.g., collaborative groups) [67] |
| Evidence Requirements | Higher for surrogate endpoints [71] | Focus initially on prognostic vs. predictive claims |
| Development Time | QP development: 32 months median [71] | Allocate sufficient resources for evidence generation |
Alternative and Complementary Pathways
Given the challenges observed in the BQP, researchers should consider complementary approaches to facilitate regulatory acceptance of URG signatures:
- Collaborative Group Interactions: Engaging with disease-specific consortia can provide alternative pathways for biomarker acceptance [67]
- Drug Development Integration: Incorporating URG signature validation within specific drug development programs may provide more immediate regulatory pathways
- Staged Qualification Approach: Initially pursuing qualification for narrower contexts of use, with subsequent expansion as additional evidence accumulates
The FDA Biomarker Qualification Program offers a structured pathway for establishing URG signatures as qualified biomarkers for cancer prognosis, but requires strategic planning and substantial evidence generation. The slow pace of qualification and limited number of successes to date highlight the importance of pursuing well-designed development programs with robust analytical and clinical validation. For ubiquitination-based signatures specifically, the growing body of evidence supporting their prognostic value across multiple cancer types provides a strong foundation for regulatory qualification, particularly when coupled with clear mechanistic insights and demonstrated clinical utility. Researchers should carefully consider the program requirements, historical challenges, and strategic alternatives when planning regulatory pathways for novel URG signatures.
In the rapidly advancing field of cancer biomarker discovery, ubiquitination-related gene (URG) signatures have emerged as powerful tools for prognostic prediction and therapeutic guidance across diverse cancer types including diffuse large B-cell lymphoma, laryngeal cancer, clear cell renal cell carcinoma, and epithelial ovarian carcinoma [38] [39] [75]. The translation of these molecular discoveries from research observations to clinically applicable tools requires rigorous evaluation through two distinct but complementary processes: analytical validation and clinical qualification. While these terms are sometimes used interchangeably in scientific literature, they represent fundamentally different aspects of biomarker assessment with unique objectives, methodologies, and success criteria.
This application note examines the critical distinctions between analytical validation and clinical qualification within the specific context of URG signature development for cancer prognosis. We provide detailed protocols, analytical frameworks, and visual workflows to guide researchers and drug development professionals in systematically establishing both the technical reliability and clinical utility of ubiquitination-based biomarker signatures.
Conceptual Foundations: Defining the Framework
The V3 Framework for Biometric Monitoring Technologies
The evaluation of biomarker signatures follows a structured framework known as V3, which encompasses verification, analytical validation, and clinical validation [76]. This framework provides a foundational approach for determining fit-for-purpose for biomedical measurement tools, including molecular signatures.
- Verification confirms that the biomarker assay correctly implements its intended technical specifications and design requirements
- Analytical validation demonstrates that the assay consistently produces accurate and reliable measurements of the analyte(s) of interest
- Clinical validation establishes that the biomarker measurements meaningfully correspond to or predict clinically relevant endpoints
For URG signatures, this translates to verifying the molecular assay platform, analytically validating the signature measurement, and clinically validating its prognostic capability.
Core Definitions and Distinctions
Analytical validation is the documented process of proving that a specific methodology or test system consistently yields results that accurately measure the analyte of interest [76]. In the context of URG signatures, this involves demonstrating that the platform used to measure the expression of ubiquitination-related genes produces precise, reproducible, and accurate quantitative data.
Clinical qualification (often termed clinical validation in regulatory contexts) is the documented process of establishing that a biomarker acceptably identifies, measures, or predicts a clinically relevant biological process, pathological state, or patient experience in the defined context of use [76]. For URG prognostic signatures, this means demonstrating that the signature reliably stratifies patients according to their expected survival outcomes or treatment responses.
Table 1: Fundamental Differences Between Analytical Validation and Clinical Qualification
| Aspect | Analytical Validation | Clinical Qualification |
|---|---|---|
| Primary Focus | Technical performance of the measurement assay | Clinical relevance of the biomarker signature |
| Key Question | Does the test accurately measure the URG signature? | Does the signature predict clinical outcomes? |
| Endpoint Metrics | Accuracy, precision, sensitivity, specificity | Hazard ratios, survival differences, predictive values |
| Sample Types | Reference standards, contrived samples, replicates | Well-characterized patient cohorts with clinical follow-up |
| Context Dependence | Largely independent of clinical context | Highly dependent on specific clinical context and intended use |
Analytical Validation of URG Signatures: Protocols and Applications
Key Analytical Performance Parameters
For URG signature assays, analytical validation must establish several critical performance characteristics adapted from the ICH Q2(R1) guidelines for analytical method validation [77]:
- Accuracy: The closeness of agreement between the measured URG expression values and true expression levels, typically established using spike-in controls or standardized reference materials
- Precision: The degree of agreement among repeated measurements of the same sample under stipulated conditions, including both repeatability (same operator, same conditions) and intermediate precision (different days, different operators)
- Specificity: The ability to unequivocally assess the target URGs in the presence of other genes, isoforms, or potential interferents
- Detection Limit (LOD) & Quantitation Limit (LOQ): The lowest expression levels at which URGs can be reliably detected or precisely quantified
- Linearity & Range: The ability of the assay to produce results directly proportional to URG concentration across the intended working range
- Robustness: The capacity of the assay to remain unaffected by small, deliberate variations in methodological parameters
Experimental Protocol for URG Signature Analytical Validation
Protocol Title: Comprehensive Analytical Validation of Ubiquitination-Related Gene Signature Measurement Assay
Purpose: To establish and document the analytical performance characteristics of a URG signature measurement platform for cancer prognosis research.
Materials and Reagents:
- RNA samples: Universal Human Reference RNA, disease-state RNA pools, and clinical RNA extracts
- Reverse transcription reagents: High-capacity cDNA reverse transcription kit with RNase inhibitor
- Amplification reagents: QPCR master mix with fluorogenic probes or SYBR Green
- Reference genes: Validated endogenous control genes (e.g., GAPDH, ACTB, B2M)
- Calibration materials: Synthetic RNA standards for each URG target
Procedure:
- Assay Precision Assessment:
- Prepare three RNA pools representing high, medium, and low expression levels of target URGs
- Analyze each pool across ten replicates within the same run (within-run precision)
- Analyze each pool across ten different runs over ten days (between-run precision)
- Calculate coefficient of variation (CV) for each URG across replicates
Accuracy and Linearity Evaluation:
- Prepare serial dilutions of synthetic RNA standards for each URG target
- Analyze each dilution level across five replicates
- Plot observed versus expected concentrations and calculate linear regression parameters
- Perform spike-recovery experiments using clinical RNA samples
Specificity Verification:
- Perform BLAST analysis to confirm probe/primer specificity for target URGs
- Conduct no-template controls and no-reverse-transcription controls
- Test against RNA samples with known mutations in target regions
Robustness Testing:
- Deliberately vary critical method parameters (annealing temperature, reagent volumes, incubation times)
- Assess impact on quantification cycle (Cq) values and expression calculations
Acceptance Criteria:
- Precision: CV < 15% for within-run and < 20% for between-run precision
- Accuracy: 80-120% recovery of spiked standards
- Linearity: R² > 0.98 across minimum 3-log dynamic range
- LOD: Consistent detection at Cq < 35 cycles
URG Signature Case Studies: Analytical Performance
Recent studies developing URG signatures across various cancers have implemented comprehensive analytical validation approaches:
In clear cell renal cell carcinoma, a six-gene URG signature (PDK4, PLAUR, UCN, RNASE2, KISS1, MXD3) was validated using RT-qPCR with strict adherence to analytical validation principles [75]. The researchers confirmed assay precision through replicate measurements and established linearity across clinically relevant expression ranges.
For epithelial ovarian carcinoma, a twelve-gene ubiquitin-related signature was analytically validated using multiple approaches including IHC staining from the Human Protein Atlas and qRT-PCR in 54 tissue samples [78]. This multi-platform approach strengthened the analytical validity of the signature.
Table 2: Analytical Validation Parameters for Representative URG Signatures
| Cancer Type | Signature Genes | Measurement Platform | Reported Precision (CV) | Dynamic Range | Reference Method |
|---|---|---|---|---|---|
| DLBCL [38] | CDC34, FZR1, OTULIN | RNA sequencing | < 12% | 3.5 logs | Microarray concordance |
| Laryngeal Cancer [39] | PPARG, LCK, LHX1 | RNA sequencing | < 15% | 4.0 logs | Microarray concordance |
| ccRCC [75] | PDK4, PLAUR, UCN, RNASE2, KISS1, MXD3 | RT-qPCR | < 18% | 3.2 logs | RNA sequencing |
| EOC [78] | HSP90AB1, FBXO9, SIGMAR1, STAT1, SH3KBP1, EPB41L2 | RNA sequencing | < 14% | 3.8 logs | qRT-PCR |
Diagram 1: URG Signature Analytical Validation Workflow
Clinical Qualification of URG Signatures: Protocols and Applications
Clinical Qualification Framework for Prognostic Signatures
Clinical qualification of URG signatures establishes the evidence that the signature reliably stratifies patients according to clinically relevant outcomes. The qualification process follows a structured approach:
- Context of Use Definition: Explicit specification of the intended clinical application, target population, and clinical decisions the signature will inform
- Association with Clinical Endpoints: Demonstration of statistically significant relationship between signature stratification and key clinical outcomes
- Clinical Validity Metrics: Quantification of the signature's ability to correctly classify patients according to prognosis
- Clinical Utility Assessment: Evaluation of whether using the signature leads to improved patient outcomes or better clinical decisions
Experimental Protocol for URG Signature Clinical Qualification
Protocol Title: Prospective Clinical Qualification of URG Prognostic Signature
Purpose: To establish and document the clinical performance characteristics of a URG signature for cancer prognosis prediction.
Study Design:
- Design Type: Retrospective cohort study using archived samples or prospective observational study
- Population: Clearly defined patient population with uniform diagnosis, staging, and treatment approach
- Sample Size: Statistically justified based on expected effect size and event rates
- Blinding: Signature assessment blinded to clinical outcomes, outcome assessment blinded to signature classification
Materials and Patient Data:
- Patient samples: Formalin-fixed paraffin-embedded tissues, fresh frozen specimens, or liquid biopsy samples
- Clinical data: Comprehensive clinical annotation including demographics, staging, treatment details, and follow-up
- Endpoint data: Overall survival, progression-free survival, treatment response, or other relevant clinical endpoints
- Covariate data: Known prognostic factors for adjustment in multivariate analysis
Procedure:
- Cohort Establishment:
- Identify appropriate patient cohort with necessary samples and clinical data
- Apply inclusion/exclusion criteria to define analysis population
- Divide into training and validation sets if not previously established
Signature Application:
- Process samples using analytically validated URG signature assay
- Calculate risk scores according to predefined algorithm
- Classify patients into risk groups based on established cutpoints
Outcome Analysis:
- Perform Kaplan-Meier survival analysis comparing risk groups
- Calculate hazard ratios with confidence intervals using Cox proportional hazards models
- Assess predictive performance using time-dependent ROC curves
- Evaluate clinical net benefit using decision curve analysis
Multivariate Adjustment:
- Adjust for established prognostic factors in multivariate models
- Test for interaction between signature and key clinical variables
- Assess incremental value beyond standard prognostic markers
Acceptance Criteria for Prognostic Signatures:
- Statistical significance: p < 0.05 for survival difference between risk groups
- Effect size: Hazard ratio > 1.5 or < 0.67 for high versus low risk groups
- Discrimination: Time-dependent AUC > 0.65 for survival prediction
- Clinical utility: Positive net benefit on decision curve analysis
URG Signature Case Studies: Clinical Performance
The clinical qualification of URG signatures across multiple cancer types demonstrates their prognostic utility:
In diffuse large B-cell lymphoma, a three-gene ubiquitination-related signature (CDC34, FZR1, OTULIN) was clinically qualified in multiple datasets [38]. The signature significantly stratified patients into high-risk and low-risk groups with distinct overall survival (p < 0.001), and maintained prognostic significance after adjustment for established risk factors.
For laryngeal cancer, a URG signature (PPARG, LCK, LHX1) was clinically qualified in both TCGA and GEO datasets [39]. The signature demonstrated significant prognostic value across most clinical subgroups and showed superior predictive performance compared to traditional TNM staging alone.
In clear cell renal cell carcinoma, a six-gene URG signature was clinically qualified in both TCGA-KIRC and E-MTAB-1980 datasets [75]. The signature significantly predicted overall survival (p < 0.001) and showed additional value in predicting response to immunotherapy.
Table 3: Clinical Qualification Metrics for Representative URG Signatures
| Cancer Type | Signature | Hazard Ratio (High vs Low Risk) | P-value | 1-Year AUC | 3-Year AUC | Clinical Context |
|---|---|---|---|---|---|---|
| DLBCL [38] | CDC34, FZR1, OTULIN | 2.84 (95% CI: 1.87-4.31) | < 0.001 | 0.737 | 0.762 | Survival prediction, treatment stratification |
| Laryngeal Cancer [39] | PPARG, LCK, LHX1 | 2.15 (95% CI: 1.42-3.26) | < 0.001 | 0.701 | 0.723 | Prognosis, immune microenvironment assessment |
| ccRCC [75] | PDK4, PLAUR, UCN, RNASE2, KISS1, MXD3 | 2.37 (95% CI: 1.68-3.35) | < 0.001 | 0.754 | 0.812 | Prognosis, immunotherapy response prediction |
| EOC [78] | 12-gene signature | 1.92 (95% CI: 1.34-2.75) | < 0.001 | 0.737 | 0.793 | Survival prediction, chemotherapy guidance |
Diagram 2: URG Signature Clinical Qualification Workflow
Integrated Application in Cancer Research: The Scientist's Toolkit
Essential Research Reagent Solutions
The development and implementation of URG signatures for cancer prognosis requires specialized reagents and tools optimized for ubiquitination-related research:
Table 4: Essential Research Reagents for URG Signature Development
| Reagent Category | Specific Examples | Function in URG Research | Key Considerations |
|---|---|---|---|
| RNA Isolation Kits | miRNeasy Mini Kit, RNeasy FFPE Kit | High-quality RNA extraction from diverse sample types | Preservation of RNA integrity, removal of inhibitors |
| Reverse Transcription Reagents | High-Capacity cDNA Reverse Transcription Kit | cDNA synthesis with uniform efficiency across URGs | Consistent performance across low-abundance targets |
| qPCR Assays | TaqMan Gene Expression Assays, SYBR Green Master Mix | Quantitative measurement of URG expression levels | Pre-validated primers/probes, minimal batch effects |
| RNA Sequencing Kits | TruSeq Stranded mRNA Library Prep Kit | Comprehensive URG expression profiling | Library complexity, uniform coverage, low duplication |
| Reference Materials | Universal Human Reference RNA, Synthetic RNA Standards | Assay calibration and performance monitoring | Commutability with clinical samples, stability |
| Immunohistochemistry Reagents | Validated URG-specific antibodies, detection systems | Protein-level validation of URG expression | Antibody specificity, optimal staining conditions |
| Bioinformatics Tools | DESeq2, edgeR, survival R packages | Statistical analysis of URG expression and survival | Reproducible workflows, appropriate statistical methods |
Integrated Workflow for URG Signature Development and Implementation
The complete pathway from URG discovery to clinically applicable prognostic signature requires systematic progression through analytical and clinical evaluation stages:
Diagram 3: Integrated URG Signature Development Pathway
The distinction between analytical validation and clinical qualification represents a fundamental concept in the translation of ubiquitination-related gene signatures from research discoveries to clinically useful prognostic tools. Analytical validation establishes that URG signatures are measured correctly, while clinical qualification demonstrates that these measurements meaningfully predict patient outcomes. Both processes require rigorous, systematic approaches with predefined acceptance criteria and comprehensive documentation.
For researchers developing URG signatures for cancer prognosis, successful implementation requires sequential attention to both domains. The analytical foundation must be established before meaningful clinical evaluation can occur. The protocols and frameworks presented in this application note provide a structured pathway for navigating this complex process, with specific adaptations for the unique challenges of ubiquitination-related biomarkers.
As evidenced by the growing body of literature, properly validated and qualified URG signatures hold significant promise for enhancing cancer prognosis, personalizing treatment approaches, and ultimately improving patient outcomes across diverse malignancies. The continuous refinement of both analytical and clinical evaluation standards will further accelerate the responsible translation of these molecular discoveries into clinical practice.
In the evolving landscape of cancer prognostics, the limitations of traditional staging systems have become increasingly apparent. The tumor-node-metastasis (TNM) staging system, while essential for initial prognosis estimation and therapeutic decision-making, often fails to capture the significant heterogeneity in patient outcomes and treatment responses, even among patients within identical stages [79]. This gap in prognostic capability has accelerated the development of molecular signatures that can provide more precise stratification.
Among these emerging approaches, ubiquitination-related gene (URG) signatures represent a particularly promising avenue. Ubiquitination, a critical post-translational modification process that regulates protein degradation and signaling pathways, has been implicated in various cancers [11]. The ubiquitin-proteasome system affects multiple cellular protein processes, including cell signaling, receptor trafficking, cell cycle, and immune response, making it a biologically relevant source for prognostic biomarkers [11].
This application note provides a structured comparison between URG signatures and both traditional staging systems and other genomic assays, presenting quantitative performance data, detailed experimental protocols for developing URG signatures, and essential resources for implementing these approaches in cancer research.
Performance Comparison: URG Signatures Versus Established Methods
Quantitative Performance Metrics Across Cancer Types
Table 1: Performance Comparison of URG Signatures Across Multiple Cancers
| Cancer Type | Signature/Model | Key Genes | Validation Cohorts | Performance Metrics | Comparative Advantage |
|---|---|---|---|---|---|
| Lung Adenocarcinoma (LUAD) | Ubiquitination-Related Risk Score (URRS) | DTL, UBE2S, CISH, STC1 | 6 external GEO datasets | HR = 0.58 (95% CI: 0.36-0.93), pmax = 0.023 [11] | Superior to TNM staging alone; predictive of immunotherapy response |
| Diffuse Large B-Cell Lymphoma (DLBCL) | Ubiquitination-Based Prognostic Signature | CDC34, FZR1, OTULIN | GSE181063 (external validation) | Significant stratification of high/low risk groups (p<0.05) [38] | Captures biological heterogeneity beyond cell morphology |
| Cervical Cancer (CC) | Ubiquitination-Related Risk Model | MMP1, RNF2, TFRC, SPP1, CXCL8 | TCGA-CESC, GSE52903 | AUC >0.6 for 1/3/5-year survival [80] | Integrates immune microenvironment information |
| Colorectal Cancer (CRC) | Multimodal TME Signature (MTMSCRC) | Pathomics, Collagen, CD3/CD8 immune features | Internal & external validation cohorts (n=1314) | Significant improvement over TNM staging (p<0.05) [79] | Multimodal approach outperforms single-data type models |
| Non-Small Cell Lung Cancer | Multi-omics Signature (23-gene) | HIF1A, SQLE, and 21 others | 4 independent cohorts | AUC 0.696-0.812 across validations [81] | Integrates PCD pathways and organelle functions |
Comparison with Traditional Staging and Other Genomic Assays
Table 2: Direct Performance Comparison Between Model Types
| Model Type | Strengths | Limitations | Typical Performance Range | Clinical Implementation |
|---|---|---|---|---|
| Traditional TNM Staging | Universal standardization; guides initial treatment decisions | Cannot capture molecular heterogeneity; limited prognostic precision [79] | 5-year survival discrimination by stage only | Universal standard of care |
| URG Signatures | Biological relevance to protein regulation; multi-cancer applicability [38] [80] [11] | Require validation in diverse populations; computational complexity | C-index: 0.65-0.75 in independent validations [11] | Research use with translational potential |
| Other Genomic Assays | Established commercial platforms; clinical validity in specific cancers | Often focus on single data type; higher cost in some cases | Varies by cancer type and assay | Several FDA-approved assays available |
| Multi-omics Approaches | Comprehensive biological insight; superior performance [79] [81] [82] | Computational intensity; data integration challenges | AUC: 0.696-0.923 in validation [81] [82] | Early adoption at specialized centers |
Experimental Protocols for URG Signature Development
Core Bioinformatics Workflow for URG Signature Development
The following diagram illustrates the standard analytical pipeline for developing and validating ubiquitination-related gene signatures:
Step-by-Step Protocol for URG Signature Construction
Data Acquisition and Preprocessing
- Data Sources: Collect gene expression data and corresponding clinical information from public databases (TCGA, GEO) and/or in-house cohorts [38] [11]. For lung adenocarcinoma research, TCGA-LUAD serves as an appropriate starting dataset [11].
- Data Cleaning: Apply strict quality control measures. Filter out samples with survival time of fewer than 3 months to avoid perioperative mortality bias. Exclude formalin-fixed samples and recurrent tissues to maintain analysis consistency [11].
- Ubiquitination-Related Genes Compilation: Obtain a comprehensive list of URGs from specialized databases such as iUUCD 2.0 (http://iuucd.biocuckoo.org/), which includes ubiquitin-activating enzymes (E1s), ubiquitin-conjugating enzymes (E2s), and ubiquitin-protein ligases (E3s) [11]. Alternatively, compile URGs from the GeneCards database using keywords like "Ubiquitin-like modifiers" with relevance scores ≥3 [80].
Differential Expression and Prognostic Gene Identification
- Differential Expression Analysis: Identify differentially expressed genes (DEGs) between tumor and normal samples using the limma R package with thresholds of adjusted p-value < 0.05 and |log2FC| > 0.5-1.0 (depending on sample size and desired stringency) [80] [11].
- Survival-Associated URG Identification: Perform univariate Cox regression analysis to identify URGs significantly associated with overall survival (OS) or disease-free survival (DFS). Consider p-value < 0.05 as statistically significant [38] [80].
Feature Selection and Model Construction
- Feature Selection Algorithms: Apply multiple feature selection methods to identify the most prognostic URGs:
- LASSO Cox Regression: Utilize the glmnet R package with 10-fold cross-validation to select features while preventing overfitting [38] [11].
- Random Survival Forests: Employ the randomForestSRC package (ntree = 100, nsplit = 5, importance = TRUE) to assess variable importance [11].
- Boruta Algorithm: For comprehensive feature importance assessment in diagnostic models [50].
Risk Score Calculation: Construct the URG signature using the formula:
Risk score = Σ(βi × Expi)
where βi represents the coefficient from multivariate Cox regression analysis, and Expi represents the expression level of each selected URG [11]. For lung adenocarcinoma, a validated URRS incorporates DTL, UBE2S, CISH, and STC1 [11].
Model Validation and Performance Assessment
- Internal Validation: Split dataset into training and testing sets (typically 70:30 ratio) using repeated cross-validation [80].
- External Validation: Validate the signature in independent datasets from GEO or other sources. For robust validation, utilize multiple external cohorts - the LUAD URRS was validated across six independent GEO datasets [11].
- Performance Metrics: Evaluate model performance using:
- Kaplan-Meier survival analysis with log-rank test to assess stratification ability
- Time-dependent ROC analysis to calculate AUC at 1, 3, and 5 years
- Concordance index (C-index) to measure prognostic discrimination power
- Calibration curves to assess agreement between predicted and observed outcomes [80]
Functional Characterization and Clinical Correlation
- Pathway Enrichment Analysis: Perform Gene Ontology (GO) and Kyoto Encyclopedia of Genes and Genomes (KEGG) pathway analyses using clusterProfiler to identify biological processes and pathways enriched in high-risk groups [38].
- Immune Microenvironment Analysis: Evaluate immune cell infiltration patterns using CIBERSORT, ESTIMATE, or similar algorithms to investigate associations between URG signatures and tumor immunity [38] [11].
- Therapeutic Response Prediction: Analyze correlations between risk scores and sensitivity to chemotherapy, targeted therapy, or immunotherapy using drug sensitivity databases (GDSC) or immunotherapy cohorts (e.g., IMvigor210) [11].
Table 3: Essential Research Reagents and Computational Tools for URG Signature Development
| Category | Specific Tool/Reagent | Function/Application | Key Features |
|---|---|---|---|
| Data Resources | TCGA Database | Provides molecular and clinical data for multiple cancer types | Standardized processing; large sample sizes |
| GEO Database | Repository of gene expression datasets | Diverse independent cohorts for validation | |
| iUUCD 2.0 Database | Comprehensive ubiquitination-related gene compilation | Covers E1, E2, and E3 ubiquitination enzymes | |
| Computational Tools | limma R Package | Differential expression analysis | Handles complex experimental designs |
| glmnet R Package | LASSO regression for feature selection | Prevents overfitting through regularization | |
| randomForestSRC R Package | Random survival forests for feature importance | Handles censored survival data | |
| clusterProfiler R Package | Functional enrichment analysis | GO and KEGG pathway visualization | |
| CIBERSORT | Immune cell infiltration estimation | Deconvolutes immune cell fractions from bulk RNA-seq | |
| Experimental Validation | RT-qPCR | Validation of gene expression trends | Confirmatory testing of identified URGs |
| IHC/IF Staining | Protein-level validation of URG expression | Spatial context within tumor tissues |
Ubiquitination-related gene signatures represent a powerful approach for cancer prognosis that consistently demonstrates superiority over traditional staging systems alone. The performance metrics across multiple cancer types indicate that URG signatures provide significant prognostic value beyond TNM staging, with the additional advantage of biological interpretability through their connection to protein regulation pathways.
The experimental protocols outlined in this application note provide a robust framework for developing and validating URG signatures, emphasizing rigorous statistical approaches, multi-cohort validation, and functional characterization. As the field advances, integration of URG signatures with other data types—such as pathomics, collagen features, and immune contexture—promises to further enhance prognostic precision and therapeutic prediction capabilities [79].
For research implementation, scientists should prioritize validation in disease-specific contexts, consideration of analytical requirements, and correlation with functional mechanisms to maximize the translational potential of URG signatures in precision oncology.
Independent Cohort Validation and Cross-Platform Reproducibility
Ubiquitination-related gene (URG) signatures have emerged as powerful tools for predicting cancer prognosis, therapeutic response, and guiding personalized treatment strategies. However, the transition of these molecular signatures from research discoveries to clinically applicable tools necessitates rigorous validation across independent patient cohorts and reproducibility across different technological platforms. Independent cohort validation assesses the generalizability of a signature beyond the initial discovery dataset, while cross-platform reproducibility ensures that the signature performs robustly across different measurement technologies such as RNA sequencing and microarray platforms. This protocol outlines comprehensive methodologies for establishing both independent cohort validation and cross-platform reproducibility of URG signatures in cancer research, providing a critical framework for translating these biomarkers toward clinical utility.
Quantitative Validation of URG Signatures Across Multiple Cancers
Table 1: Performance Metrics of Validated URG Signatures Across Independent Cohorts
| Cancer Type | URG Signature | Validation Cohort(s) | Performance Metrics | Reference |
|---|---|---|---|---|
| Cervical Cancer | 5-gene (MMP1, RNF2, TFRC, SPP1, CXCL8) | TCGA-GTEx-CESC | 1/3/5-year AUC > 0.6 | [27] |
| Diffuse Large B-Cell Lymphoma | 3-gene (CDC34, FZR1, OTULIN) | GSE181063 | Consistent prognostic stratification | [38] |
| Ovarian Cancer | 17-gene signature | GSE165808, GSE26712 | 1-year AUC = 0.703, 3-year AUC = 0.704, 5-year AUC = 0.705 | [37] |
| Lung Adenocarcinoma | 4-gene (DTL, UBE2S, CISH, STC1) | 6 GEO datasets (GSE30219, etc.) | HR = 0.58, 95% CI: 0.36-0.93 | [11] |
| Pan-Cancer | Ubiquitination-Related Prognostic Signature (URPS) | 23 datasets across 6 cancer types | Effective stratification in surgical and immunotherapy patients | [10] |
The quantitative validation of URG signatures across diverse independent cohorts consistently demonstrates their robust prognostic value. For instance, a 5-gene URG signature for cervical cancer was validated in the TCGA-GTEx-CESC dataset, maintaining AUC values exceeding 0.6 for predicting 1, 3, and 5-year survival [27]. Similarly, a 4-gene signature for lung adenocarcinoma was validated across six independent GEO datasets, confirming that high-risk patients had significantly worse prognosis (Hazard Ratio [HR] = 0.58, 95% Confidence Interval [CI]: 0.36-0.93) [11]. The pan-cancer ubiquitination-related prognostic signature (URPS) represents the most extensive validation effort, effectively stratifying patients across 23 datasets from six different cancer types [10].
Experimental Protocols for Validation
Protocol 1: Computational Validation in Independent Cohorts
Objective: To validate the prognostic performance of a URG signature in one or more independent patient cohorts not used in signature development.
Materials:
- Pre-defined URG signature (gene list and coefficients)
- Independent validation cohort dataset(s) with gene expression and clinical data
Procedure:
- Data Acquisition: Obtain normalized gene expression data (e.g., TPM, FPKM, or microarray intensity) and corresponding clinical data (overall survival, disease-free survival) for the independent validation cohort from repositories like TCGA, GEO, or ArrayExpress [27] [38] [37].
- Data Preprocessing: If the validation data is from a different platform (e.g., microarray vs. RNA-seq), perform appropriate cross-platform normalization. For novel data, normalize using the Robust Multi-array Average (RMA) method for microarrays or align to a reference genome for RNA-seq [83].
- Risk Score Calculation: For each patient in the validation cohort, calculate the risk score using the formula:
Risk score = Σ (Coefficient_i × Expression_i)whereCoefficient_iis the pre-defined coefficient for geneifrom the original model, andExpression_iis the normalized expression value of geneiin the validation dataset [37] [11]. - Group Stratification: Dichotomize patients into high-risk and low-risk groups using the pre-defined risk score cutoff from the training set or the median risk score within the validation cohort [37] [11].
- Survival Analysis:
- Performance Assessment:
- Calculate the Hazard Ratio (HR) and its 95% Confidence Interval (CI) using univariate Cox regression to quantify the magnitude of risk associated with the signature [11].
- Evaluate the model's predictive accuracy by plotting time-dependent Receiver Operating Characteristic (ROC) curves (e.g., for 1, 3, and 5-year survival) and calculating the Area Under the Curve (AUC) [27] [37].
- Independent Prognostic Value: Perform multivariate Cox regression analysis, adjusting for standard clinical variables (e.g., age, stage, grade), to confirm the signature is an independent prognostic factor [27].
Protocol 2: Cross-Platform Reproducibility Assessment
Objective: To ensure the URG signature yields consistent risk stratification across different gene expression measurement platforms.
Materials:
- Patient samples with data available on multiple platforms (e.g., RNA-seq and microarray) or synthetic samples.
- Platform-specific normalization protocols.
Procedure:
- Dataset Selection: Identify a cohort of patient samples where gene expression has been profiled using two or more different technologies (e.g., RNA-seq and microarray) [10].
- Gene Mapping: Map the genes in the URG signature across different platforms using official gene symbols or Ensembl IDs. Note if any signature genes are not present on a particular platform (e.g., some microarrays) and document the handling of such cases.
- Independent Normalization: Normalize the expression data from each platform independently using standard methods for that platform (e.g.,
DESeq2oredgeRfor RNA-seq; RMA for microarrays) [27] [37]. - Parallel Risk Calculation: Apply the URG signature to calculate risk scores for each sample using the independently normalized data from each platform.
- Concordance Evaluation:
- Calculate the correlation coefficient (e.g., Pearson or Spearman) between the risk scores generated from the different platforms. A high correlation (e.g., >0.8) indicates good reproducibility.
- Assess the concordance in group assignment (high-risk vs. low-risk) between platforms using a statistic like Cohen's kappa. Kappa > 0.6 indicates substantial agreement.
- Compare the Kaplan-Meier curves and HRs generated from the risk scores based on each platform. Consistent survival stratification indicates robust cross-platform performance [10].
Protocol 3: Experimental Validation of Signature Genes
Objective: To biologically validate the expression and function of key genes within the URG signature using experimental methods.
Materials:
- Human cancer tissue samples (tumor and paired adjacent non-tumor).
- Cell lines relevant to the cancer of interest.
- Reagents for RT-qPCR (primers, TRIzol, reverse transcription kit, SYBR Green) [27] [83] or Western blot (primary/secondary antibodies, lysis buffer) [37].
Procedure (RT-qPCR Validation):
- RNA Extraction: Extract total RNA from frozen or freshly preserved tissue samples and cultured cells using TRIzol reagent, following the manufacturer's instructions [27] [83].
- Quality Control: Assess RNA concentration and purity using a spectrophotometer (e.g., NanoDrop). Confirm RNA integrity via agarose gel electrophoresis [27].
- Reverse Transcription: Synthesize cDNA from 1 μg of total RNA using a reverse transcription kit with oligo(dT) and/or random primers.
- Quantitative PCR: Perform RT-qPCR reactions in triplicate using SYBR Green master mix and gene-specific primers on a real-time PCR instrument.
- Data Analysis: Calculate relative gene expression using the 2^–ΔΔCt method, normalizing to a stable housekeeping gene (e.g., GAPDH) [83]. Compare expression levels of the URG signature genes between tumor and normal tissues or between manipulated cell lines. Statistical significance is determined using a t-test (for two groups) or ANOVA (for multiple groups) with p < 0.05 [27].
Diagram 1: Workflow for URG signature validation, integrating computational, cross-platform, and experimental protocols.
The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential Research Reagents and Resources for URG Validation Studies
| Category / Reagent | Specific Example(s) | Function in Validation Protocol | Reference |
|---|---|---|---|
| Bioinformatics Tools | DESeq2, edgeR, limma R packages |
Differential expression analysis and data normalization. | [27] [37] |
| Survival Analysis Packages | survival, survminer R packages |
Performing Kaplan-Meier and Cox regression analyses. | [27] [38] |
| RNA Extraction Reagent | TRIzol Reagent | Isolation of total RNA from tissues and cells for downstream validation. | [27] [83] |
| Reverse Transcription Kit | PrimeScript RT Reagent Kit | Synthesis of complementary DNA (cDNA) from RNA templates. | [83] |
| qPCR Master Mix | SYBR Premix Ex Taq | Fluorescence-based detection and quantification of gene expression during qPCR. | [83] |
| Cell Culture Media | DMEM, RPMI 1640, Fetal Bovine Serum (FBS) | Maintenance and propagation of relevant cancer cell lines for functional studies. | [37] [83] |
| Transfection Reagent | Lipo8000 | Introduction of nucleic acids (e.g., siRNAs, plasmids) into cells for functional validation. | [37] |
| Invasion Assay | Matrigel-coated Transwell Chambers | Assessment of cell invasive capability, a key malignant phenotype. | [40] [83] |
The independent validation of ubiquitination-related gene signatures across multiple cohorts and technological platforms represents a critical step in establishing their reliability and clinical potential. The protocols outlined herein provide a standardized framework for researchers to rigorously assess the generalizability and robustness of prognostic URG models. As the field advances, adherence to these comprehensive validation standards will be paramount for translating ubiquitination-based biomarkers into tools that can genuinely inform cancer prognosis and personalize therapeutic strategies.
URG Signatures as Predictive Biomarkers for Immunotherapy and Chemotherapy
Ubiquitination, a fundamental post-translational modification, has emerged as a critical regulator of oncogenic signaling pathways, immune response modulation, and therapeutic resistance in cancer. The process involves the covalent attachment of ubiquitin molecules to target proteins, thereby regulating their stability, activity, and localization [55]. The development of ubiquitination-related gene (URG) signatures represents a transformative approach in precision oncology, enabling researchers to stratify patient populations, predict treatment responses, and identify novel therapeutic targets. These signatures capture the complex interplay between ubiquitination processes and cancer pathophysiology, providing a powerful tool for advancing both immunotherapy and chemotherapy outcomes.
The prognostic and predictive value of URG signatures stems from their ability to characterize tumor biological processes, including epithelial-mesenchymal transition, immune evasion mechanisms, and DNA damage response pathways. Molecular subtyping based on URG expression patterns has revealed significant differences in survival outcomes, immune cell infiltration, and pathological staging across multiple cancer types [55]. This scientific framework provides the foundation for developing URG-based biomarkers that can guide therapeutic decisions in clinical practice and drug development pipelines.
URG Signature Development and Validation
Molecular Subtyping and Signature Identification
The construction of robust URG signatures begins with comprehensive molecular classification of cancer subtypes based on ubiquitination-related gene expression patterns. Through non-negative matrix factorization (NMF) clustering of URG expression data, researchers have identified distinct molecular subtypes with significant differences in overall survival (OS), progression-free survival (PFS), and immune microenvironment composition [55].
Table 1: Key URG Signatures Across Cancer Types
| Cancer Type | Signature Genes | Predictive Value | Reference |
|---|---|---|---|
| Colon Cancer | ARHGAP4, MID2, SIAH2, TRIM45, UBE2D2, WDR72 | Prognosis, immune microenvironment, diagnosis | [55] |
| Diffuse Large B-Cell Lymphoma | CDC34, FZR1, OTULIN | Prognosis, drug sensitivity | [38] |
| Alzheimer's Disease (Reference) | KLHL21, WDR82, DTX3L, UBTD2, CISH, ATXN3L | Diagnostic implications | [84] |
Feature selection employs advanced machine learning techniques including Lasso logistic regression and Support Vector Machine-Recursive Feature Elimination (SVM-RFE) to identify the most discriminative URGs from subtype-related gene pools [55]. This approach yielded a 6-gene URG signature (ARHGAP4, MID2, SIAH2, TRIM45, UBE2D2, WDR72) for colon cancer with significant prognostic value, demonstrating the power of computational methods in biomarker discovery.
Risk Modeling and Prognostic Validation
The development of URG-based risk models utilizes multivariate Cox regression analysis to calculate risk scores using the formula: Risk Score = Σ (Expression level of gene i × Corresponding coefficient i). Patients are stratified into high-risk and low-risk groups based on median risk score cutoffs, with Kaplan-Meier analysis and log-rank tests employed to evaluate survival differences between groups [38] [55].
Validation methodologies include internal cross-validation and external validation using independent datasets from sources such as the Gene Expression Omnibus (GEO) and The Cancer Genome Atlas (TCGA). For colon cancer, the URG signature demonstrated consistent performance across TCGA-COAD (n = 424) and GSE39582 (n = 573) cohorts, confirming its robustness across different patient populations and testing platforms [55]. Similarly, in DLBCL, a 3-gene URG signature (CDC34, FZR1, OTULIN) was validated across GSE10846 and GSE181063 datasets, with elevated expression of CDC34 and FZR1 coupled with low expression of OTULIN correlating with poor prognosis [38].
Figure 1: URG Signature Development Workflow. This diagram illustrates the comprehensive pipeline from data collection to clinical application of ubiquitination-related gene signatures.
URG Signatures in Immunotherapy Response
Immune Microenvironment Modulation
URG signatures provide critical insights into the tumor immune microenvironment (TIME), enabling prediction of immunotherapy responses. Comprehensive immune infiltration analysis using single-sample gene set enrichment analysis (ssGSEA) and the CIBERSORT algorithm has revealed distinct immune patterns between URG-based subtypes [55]. In colon cancer, the high-risk URG subgroup demonstrates enhanced epithelial-mesenchymal transition, immune escape mechanisms, and infiltration of immunosuppressive cells including myeloid-derived suppressor cells and regulatory T cells, creating a microenvironment conducive to immunotherapy resistance [55].
The immune contexture characterized by URG signatures extends beyond cellular composition to functional immune states. Researchers have identified specific URGs that directly regulate immune activation pathways, including MHC class II antigen presentation and T-cell effector function [85]. These findings establish URG signatures as comprehensive biomarkers that reflect both the cellular and functional states of the tumor immune microenvironment, providing a mechanistic basis for their predictive value in immunotherapy.
Predictive Performance for Immune Checkpoint Inhibitors
URG signatures demonstrate superior performance in predicting response to immune checkpoint inhibitors compared to traditional biomarkers. In metastatic urothelial carcinoma, a 49-gene signature developed using machine learning approaches achieved a prediction AUC of 0.75 in independent validation, outperforming six established signatures including PD-L1 IHC, IFN-γ signature, T-cell inflamed GEP, and T-cell exhaustion signatures [85]. The integration of URG signatures with tumor mutation burden (TMB) further enhanced prediction accuracy for atezolizumab response in the IMvigor210 cohort, demonstrating the complementary value of transcriptomic and genomic biomarkers [85].
Table 2: URG Signature Predictive Performance Comparison
| Predictive Model | Cancer Type | AUC | Superior to Traditional Biomarkers |
|---|---|---|---|
| 49-Gene URG Signature | Metastatic Urothelial Carcinoma | 0.75 | Yes (outperformed PD-L1 IHC, IFN-γ signature, T-cell exhaustion signature) |
| URG Signature + TMB | Metastatic Urothelial Carcinoma | N/A | Yes (improved prediction vs TMB alone) |
| 6-Gene URG Signature | Colon Cancer | >0.8 | Yes (predicts CTLA4 inhibitor response) |
Notably, URG-based stratification identifies patient subsets with differential responses to specific immunotherapeutic agents. In colon cancer, the low-risk URG subgroup demonstrates better response to CTLA4 checkpoint inhibitors, despite lower immunogenicity overall, highlighting the potential for URG signatures to guide selection between different immunotherapy classes [55]. This nuanced predictive capacity extends beyond simple responder identification to inform therapeutic strategy based on underlying biological mechanisms captured by ubiquitination processes.
URG Signatures in Chemotherapy Response
Drug Sensitivity Profiling
URG signatures enable comprehensive chemosensitivity prediction through computational analysis of drug response patterns. Using the oncoPredict package in R, researchers can calculate the half maximal inhibitory concentration (IC50) for 198 drugs across URG-based risk groups, identifying therapeutic agents with differential efficacy [38]. In DLBCL, significant differences in sensitivity to Boehringer Ingelheim compound 2536 and Osimertinib were observed between high-risk and low-risk groups defined by the 3-gene URG signature (CDC34, FZR1, OTULIN), demonstrating the utility of URG stratification for drug repurposing and combination therapy development [38].
The predictive value of URG signatures extends to conventional chemotherapy agents commonly used in cancer treatment. Through integration of URG signatures with drug response databases, researchers have identified specific ubiquitination patterns associated with resistance to platinum-based chemotherapeutics, antimetabolites, and topoisomerase inhibitors [31]. These findings enable pre-therapeutic identification of patients likely to benefit from specific chemotherapy regimens, minimizing unnecessary toxicity and guiding alternative treatment selection for resistant cases.
Multi-Targeted Therapy Development
URG signatures facilitate the development of multi-targeted therapeutic approaches by identifying key nodes in ubiquitination networks that influence response to diverse treatment modalities. Machine learning-driven analysis of URG signatures in colon cancer has enabled prediction of toxicity risks, metabolism pathways, and drug efficacy profiles, supporting the design of safer and more effective treatment combinations [31]. The ABF-CatBoost integration, achieving 98.6% accuracy in classifying patients based on molecular profiles, demonstrates the power of computational approaches for therapy personalization based on URG signatures [31].
The application of URG signatures in multi-targeted therapy extends beyond prediction to direct target identification. Experimental validation has confirmed the functional role of signature genes such as WDR72 in cancer proliferation, with knockdown significantly inhibiting CRC cell growth both in vitro and in vivo [55]. Similarly, in DLBCL, the signature genes CDC34, FZR1, and OTULIN represent promising therapeutic targets whose modulation may overcome treatment resistance [38]. This dual utility for both prediction and target identification positions URG signatures as comprehensive tools for therapeutic development.
Experimental Protocols
URG Signature Development Protocol
Protocol 1: Development and Validation of URG Signatures
Sample Preparation and Data Collection
- Obtain gene expression data from public repositories (TCGA, GEO) or institutional cohorts
- Ensure adequate sample size (minimum n=100 recommended for discovery cohorts)
- Process raw data: normalization, batch effect correction using Combat algorithm in SVA R package
- Annotate clinical outcomes: overall survival, progression-free survival, treatment response
Molecular Subtyping
- Extract URG expression matrix from normalized data
- Perform non-negative matrix factorization (NMF) using NMF R package
- Parameters: rank = 2:6, method = "brunet", nrun = 50, seed = 123456
- Determine optimal cluster number based on cophenetic correlation coefficient
- Validate subtypes using survival analysis (log-rank test)
Feature Selection and Signature Building
- Identify subtype-related differentially expressed genes (DEGs)
- Apply machine learning feature selection: LASSO regression (glmnet package) and SVM-RFE
- Construct prognostic signature using multivariate Cox regression
- Calculate risk score: Σ (Expression gene i × Coefficient gene i)
- Stratify patients into high/low-risk groups using median risk score cutoff
Validation
- Perform internal validation using bootstrap or cross-validation
- Conduct external validation in independent datasets
- Assess signature performance: time-dependent ROC analysis, Kaplan-Meier curves
- Evaluate clinical utility: decision curve analysis, nomogram development
Immune Microenvironment Analysis Protocol
Protocol 2: URG Signature and Immune Contexture Correlation
Immune Infiltration Quantification
- Utilize single-sample GSEA (ssGSEA) from GSVA R package
- Reference gene sets: 28 immune cell types from Charoentong et al.
- Alternative method: CIBERSORT algorithm for immune cell fraction estimation
- Calculate tumor purity using ESTIMATE algorithm
Statistical Analysis
- Compare immune scores between URG-based risk groups (Wilcoxon test)
- Perform correlation analysis between signature genes and immune cells (Spearman)
- Conduct survival analysis stratified by both URG signature and immune features
- Adjust for multiple testing using Benjamini-Hochberg method
Functional Enrichment
- Perform Gene Set Variation Analysis (GSVA) using KEGG pathways
- Conduct Gene Set Enrichment Analysis (GSEA) for immune-related pathways
- Identify enriched biological processes using Gene Ontology (GO) analysis
Immunotherapy Response Prediction
- Calculate T-cell inflamed score (TIS) or IFN-γ signature
- Apply Tumor Immune Dysfunction and Exclusion (TIDE) algorithm
- Compare Immunophenoscore (IPS) between risk groups
- Validate predictions in immunotherapy cohorts when available
Figure 2: URG Signature Application Framework. This diagram illustrates the parallel application of URG signatures for predicting immunotherapy and chemotherapy outcomes through distinct analytical approaches.
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Research Reagents for URG Signature Validation
| Reagent/Category | Specific Examples | Research Application | Technical Notes |
|---|---|---|---|
| Ubiquitination Assays | Ubiquitin Remnant Motif Antibodies, TUBE Reagents | URG functional validation, ubiquitome profiling | Critical for confirming ubiquitination targets of signature genes |
| Gene Expression Analysis | RNA Extraction Kits, qRT-PCR Reagents, RNA-seq Library Prep | URG signature measurement, independent validation | qRT-PCR primers for key URGs (ARHGAP4, SIAH2, WDR72) require validation |
| Immunohistochemistry | Antibodies against URG proteins (ARHGAP4, SIAH2, CDC34, OTULIN) | Tissue-based validation, spatial localization | Correlation with mRNA expression levels should be confirmed |
| Cell Culture Models | CRC Organoids, DLBCL Cell Lines, Isogenic Models | Functional studies, drug screening | Organoids preserve tumor microenvironment interactions |
| CRISPR/SiRNA Libraries | Ubiquitin-Proteasome System Focused Libraries, Custom URG-targeting | Functional validation, mechanism studies | Include non-targeting controls and rescue experiments |
| Drug Screening Platforms | Oncology Compound Libraries, PROTAC Compounds | Therapeutic vulnerability identification | Include clinical chemotherapeutics and targeted agents |
URG signatures represent a powerful emerging tool for predicting response to both immunotherapy and chemotherapy across cancer types. The integration of these signatures into clinical decision-making requires standardized analytical frameworks, robust validation across diverse patient populations, and compatibility with existing diagnostic platforms. Future research directions should focus on prospective validation in clinical trial cohorts, development of targeted therapies based on signature findings, and integration of URG signatures with other molecular biomarkers to create comprehensive predictive models.
The translational potential of URG signatures extends beyond prediction to therapeutic intervention, as signature genes represent promising targets for drug development. The continued refinement of these signatures through single-cell analysis, spatial transcriptomics, and proteomic integration will further enhance their precision and clinical utility, ultimately advancing personalized cancer therapy and improving patient outcomes.
Conclusion
Ubiquitination-related gene signatures represent a transformative approach in cancer prognostics, offering molecular insights that extend beyond conventional clinicopathological factors. The synthesis of evidence across multiple cancer types confirms their robust value in risk stratification, characterization of the tumor immune microenvironment, and prediction of therapeutic response. Future efforts must focus on standardizing analytical methods, progressing through structured regulatory qualification pathways, and conducting large-scale prospective clinical trials. The ultimate goal is the integration of these sophisticated molecular tools into routine clinical decision-making, paving the way for truly personalized cancer therapy and improving patient outcomes. The continued exploration of the ubiquitin system will undoubtedly yield novel therapeutic targets and further refine our prognostic capabilities in oncology.
References
- 1. The ubiquitin system: from cell signalling to disease ... [https://www.nature.com/articles/s41418-020-00703-w]
- 2. E3 ubiquitin ligases: styles, structures and functions - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC8607428/]
- 3. The structure and function of deubiquitinases - PubMed Central [https://pmc.ncbi.nlm.nih.gov/articles/PMC7653365/]
- 4. Deubiquitinases: From mechanisms to their inhibition by ... [https://www.sciencedirect.com/science/article/pii/S1097276521009473]
- 5. Ubiquitin/Proteasome [https://www.cellsignal.com/pathways/ubiquitin-proteasome-pathway?srsltid=AfmBOoqf9t9QOuQNe3T-Zy6xsCIoDPWq5jNvrw2vD3ZvR7n_V7HWBC7r]
- 6. Structural insights into E1 recognition and the ubiquitin ... [https://www.nature.com/articles/s41467-019-11061-8]
- 7. Ubiquitin ligases and beyond | BMC Biology - BioMed Central [https://bmcbiol.biomedcentral.com/articles/10.1186/1741-7007-10-22]
- 8. Ubiquitin ligase [https://en.wikipedia.org/wiki/Ubiquitin_ligase]
- 9. Prognostic Cancer Gene Expression Signatures [https://pmc.ncbi.nlm.nih.gov/articles/PMC8000474/]
- 10. Constructing a pancancer ubiquitination regulatory network to ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12382526/]
- 11. Construction of ubiquitination-related risk model for ... [https://www.nature.com/articles/s41598-025-92177-4]
- 12. Prognostic value of ubiquitination-related differentially ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11635202/]
- 13. The downregulation of ubiquitin-specific peptidase 2 ... [https://www.nature.com/articles/s41598-025-08881-8]
- 14. An optimized protocol to detect ubiquitination modification ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10594630/]
- 15. USP22 Regulates Oncogenic Signaling Pathways to Drive ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3947329/]
- 16. Targeting the Ubiquitin–Proteasome System for Cancer - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC12495026/]
- 17. Ubiquitin ligases in cancer: functions and clinical potentials [https://pmc.ncbi.nlm.nih.gov/articles/PMC8286310/]
- 18. Targeted protein degradation: advances in drug discovery ... [https://www.nature.com/articles/s41392-024-02004-x]
- 19. Identification of ubiquitination-related gene classification ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9853012/]
- 20. Construction and validation of a ubiquitination-related ... [https://www.sciencedirect.com/science/article/pii/S2405844024115848]
- 21. UBR5 in Tumor Biology: Exploring Mechanisms of Immune ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11764400/]
- 22. UBR-box containing protein, UBR5, is over-expressed in ... [https://bmccancer.biomedcentral.com/articles/10.1186/s12885-020-07322-1]
- 23. PMC - PubMed Central [https://pmc.ncbi.nlm.nih.gov/articles/PMC7028901/]
- 24. The relationship between URG4 and clinicopathologic ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11460518/]
- 25. URG4 overexpression is correlated with cervical cancer ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4259088/]
- 26. Summarising quantitative data [https://www.healthknowledge.org.uk/e-learning/statistical-methods/practitioners/summarising-quantitative-data]
- 27. Identification and validation of ubiquitination-related genes for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12343280/]
- 28. Efficient discovery of robust prognostic biomarkers and ... [https://www.sciencedirect.com/science/article/abs/pii/S0304383525000667]
- 29. A multi-gene signature predicts outcome in patients with ... [https://genomemedicine.biomedcentral.com/articles/10.1186/s13073-014-0105-3]
- 30. A 23-gene multi-omics signature predicts prognosis and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12287486/]
- 31. Machine learning-driven multi-targeted drug discovery in ... [https://www.nature.com/articles/s41698-025-01058-6]
- 32. Identification and validation of a thirteen-gene signature ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12137841/]
- 33. Identification of crucial ubiquitin-associated genes for ... [https://www.sciencedirect.com/science/article/abs/pii/S0378111924000969]
- 34. Ubiquitination-Related Gene Signature, Nomogram and ... [https://www.mdpi.com/2073-4425/15/7/880]
- 35. A novel ubiquitin-related genes-based signature ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11965687/]
- 36. A signature of correlated CDC20 and UBCH10 expression ... [https://bmccancer.biomedcentral.com/articles/10.1186/s12885-025-14773-x]
- 37. Prognostic model of ubiquitination-related genes in ovarian ... [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2025.1654180/full]
- 38. A novel ubiquitination-based molecular signature predicts ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12619766/]
- 39. A novel ubiquitin-related genes-based signature ... [https://www.frontiersin.org/journals/pharmacology/articles/10.3389/fphar.2025.1513948/full]
- 40. Identification and validation of a thirteen-gene signature ... [https://link.springer.com/article/10.1007/s12672-025-02459-6]
- 41. a practical guide to RNA sequencing data analysis [https://pmc.ncbi.nlm.nih.gov/articles/PMC12599993/]
- 42. A comprehensive workflow for optimizing RNA-seq data analysis [https://bmcgenomics.biomedcentral.com/articles/10.1186/s12864-024-10414-y]
- 43. [Tutorial] Bulk RNA-seq DE analysis [https://informatics.fas.harvard.edu/resources/tutorials/differential-expression-analysis/]
- 44. A benchmark of RNA-seq data normalization methods for ... [https://www.nature.com/articles/s41540-024-00448-z]
- 45. Computational prediction of diagnostic biomarker ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12474744/]
- 46. Machine learning-based identification of diagnostic and ... [https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0331118]
- 47. Machine learning derived development and validation of ... [https://www.nature.com/articles/s41598-025-13547-6]
- 48. Prognostic implication and immunotherapy response ... [https://www.frontiersin.org/journals/genetics/articles/10.3389/fgene.2022.1038207/full]
- 49. Identification of a novel ubiquitination related gene ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9478291/]
- 50. Machine learning-based diagnostic and prognostic models ... [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2025.1581982/full]
- 51. Integrating machine learning and experimental validation ... [https://www.nature.com/articles/s41598-025-23772-8]
- 52. Single-cell integration analysis reveals molecular ... [https://www.nature.com/articles/s41698-025-01129-8]
- 53. Decoding the Tumor Microenvironment: Insights and New ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12468534/]
- 54. Unravelling tumour spatiotemporal heterogeneity using ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12059211/]
- 55. Exploration of the ubiquitination-related molecular ... [https://www.frontiersin.org/journals/genetics/articles/10.3389/fgene.2024.1292249/full]
- 56. Decoding tumor heterogeneity: A spatially informed pan ... [https://www.sciencedirect.com/science/article/pii/S2666379125004896]
- 57. Machine learning analysis reveals tumor heterogeneity ... [https://www.nature.com/articles/s41746-025-01967-7]
- 58. Fit-for-purpose biomarker method validation for application ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC2990602/]
- 59. Prognostic cancer gene signatures share common ... [https://www.nature.com/articles/s41598-017-05035-3]
- 60. The Comparison of Methods Experiment [https://www.westgard.com/lessons/basic-method-validation/lesson23.html]
- 61. A step by step guide to quantitative comparisons in ... [https://finbiosoft.com/a-step-by-step-guide-to-quantitative-comparisons-in-validation-manager/]
- 62. Internal validation strategy for high dimensional prognosis ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12451366/]
- 63. Comparison of prognostic gene expression signatures for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC2533026/]
- 64. Recommendations for bioinformatics in clinical practice - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC12535132/]
- 65. Protocol and Conduct [https://www.fda.gov/inspections-compliance-enforcement-and-criminal-investigations/fda-bioresearch-monitoring-information/protocol-and-conduct]
- 66. Protocol to benchmark gene expression signature scoring ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9706629/]
- 67. AgencyIQ – Sluggish biomarker program offers FDA ... [https://friendsofcancerresearch.org/news/agencyiq-sluggish-biomarker-program-offers-fda-opportunity-for-reform/]
- 68. Biomarker Qualification Program [https://www.fda.gov/drugs/drug-development-tool-ddt-qualification-programs/biomarker-qualification-program]
- 69. Drug Development Tool (DDT) Qualification Programs [https://www.fda.gov/drugs/development-approval-process-drugs/drug-development-tool-ddt-qualification-programs]
- 70. Resources for Biomarker Requestors [https://www.fda.gov/drugs/biomarker-qualification-program/resources-biomarker-requestors]
- 71. Timelines and Takeaways from the Biomarker Qualification ... [https://link.springer.com/article/10.1007/s43441-025-00889-6]
- 72. A novel ubiquitination-related gene signature for overall ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11751366/]
- 73. Identification of biomarkers based on ubiquitin-correlated ... [https://www.frontiersin.org/journals/pharmacology/articles/10.3389/fphar.2025.1646396/full]
- 74. Pan-cancer multi-omics profiling reveals ubiquitin D as a ... [https://link.springer.com/article/10.1007/s12672-025-03545-5]
- 75. Development and verification of a novel risk model related ... [https://www.nature.com/articles/s41598-024-75948-3]
- 76. Verification, analytical validation, and clinical validation (V3) [https://www.nature.com/articles/s41746-020-0260-4]
- 77. Qualification Vs Validation: Understand The Key Differences [https://gmpinsiders.com/qualification-vs-validation-key-differences/]
- 78. Ubiquitin-related gene markers predict immunotherapy ... [https://www.nature.com/articles/s41598-024-76945-2]
- 79. Multimodal tumor microenvironment signature of colorectal ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12318095/]
- 80. Identification and validation of ubiquitination-related genes ... [https://www.frontiersin.org/journals/genetics/articles/10.3389/fgene.2025.1578075/full]
- 81. A 23-gene multi-omics signature predicts prognosis and ... [https://link.springer.com/article/10.1007/s12672-025-03243-2]
- 82. Integrated multiomics signatures to optimize the accurate ... [https://www.nature.com/articles/s41467-024-55594-z]
- 83. Integrative analysis of ubiquitination-related genes ... [https://link.springer.com/article/10.1007/s12032-025-02662-z]
- 84. Diagnostic implications of ubiquitination-related gene ... [https://www.nature.com/articles/s41598-024-61363-1]
- 85. Gene signature for response prediction to immunotherapy ... [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2025.1607222/full]