Ubiquitination-Related Genes as Prognostic Biomarkers in Cancer: From Molecular Mechanisms to Clinical Applications
This comprehensive review explores the rapidly advancing field of ubiquitination-related genes (UbRGs) as prognostic biomarkers in oncology.
Ubiquitination-Related Genes as Prognostic Biomarkers in Cancer: From Molecular Mechanisms to Clinical Applications
Abstract
This comprehensive review explores the rapidly advancing field of ubiquitination-related genes (UbRGs) as prognostic biomarkers in oncology. Ubiquitination, a crucial post-translational modification, regulates protein stability and function across diverse cellular processes. Recent multi-omics studies have established that dysregulation of UbRGs significantly impacts cancer initiation, progression, and therapeutic response. This article synthesizes current methodologies for developing UbRG-based prognostic signatures, validates their predictive accuracy across multiple cancer types including laryngeal, ovarian, pancreatic, and esophageal cancers, and examines their role in shaping tumor immune microenvironments. For researchers, scientists, and drug development professionals, we provide critical insights into both the transformative potential and current challenges in translating UbRG biomarkers into clinical practice for personalized cancer treatment.
The Ubiquitin-Proteasome System in Cancer: Molecular Foundations and Pathogenic Mechanisms
Ubiquitination is a crucial post-translational modification that regulates virtually all cellular processes in eukaryotes, from protein degradation to DNA repair and signal transduction [1]. This sophisticated enzymatic cascade involves three core components: ubiquitin-activating enzymes (E1), ubiquitin-conjugating enzymes (E2), and ubiquitin ligases (E3), which work in sequence to attach the small protein modifier ubiquitin to substrate proteins [1]. The reverse reaction, deubiquitination, is carried out by deubiquitinating enzymes (DUBs), which remove ubiquitin signals to maintain cellular homeostasis [2]. The balance between ubiquitination and deubiquitination determines the fate and function of thousands of cellular proteins, and its dysregulation is implicated in numerous human diseases, particularly cancer [3] [2]. This guide provides a comprehensive comparison of these core components, their experimental analysis, and their emerging roles as therapeutic targets in cancer research, fulfilling a critical need for a consolidated resource in this rapidly advancing field.
The Ubiquitination Cascade: Core Components and Mechanisms
The ubiquitination pathway represents a sophisticated regulatory system where E1, E2, and E3 enzymes function in concert to confer specificity and diversity to ubiquitin signaling [1].
The Enzymatic Cascade
- E1 (Ubiquitin-Activating Enzymes): Initiation begins with E1 enzymes, which activate ubiquitin in an ATP-dependent process. Humans possess two E1 enzymes (UBA1 and UBA6) that catalyze the formation of a thioester bond between their catalytic cysteine and the C-terminal glycine of ubiquitin [4] [3].
- E2 (Ubiquitin-Conjugating Enzymes): Approximately 40 E2 enzymes in humans receive activated ubiquitin from E1 through a transthiolation reaction, forming an E2~Ub thioester intermediate [4] [3]. E2s contain a conserved ~150-amino acid ubiquitin-conjugating (UBC) catalytic core domain [4].
- E3 (Ubiquitin Ligases): The ~600-1000 human E3 enzymes provide substrate specificity by recognizing target proteins and facilitating ubiquitin transfer from E2~Ub to substrate lysine residues [1] [3]. E3s are categorized into RING, HECT, and RBR families based on their mechanism of action [1].
Table 1: Core Enzymes in the Ubiquitination Machinery
| Enzyme Class | Human Genes | Core Function | Key Structural Features | Catalytic Mechanism |
|---|---|---|---|---|
| E1 (Activating) | 2 | Ubiquitin activation and E2 charging | Adenylation, catalytic cysteine, and UFD domains | ATP-dependent ubiquitin C-terminal adenylation, thioester formation with E1 active site cysteine |
| E2 (Conjugating) | ~40 | Ubiquitin carriage and transfer | Conserved UBC domain (~150 residues) with active site cysteine | Transthiolation: ubiquitin transfer from E1 to E2 active site cysteine |
| E3 (Ligating) | ~600-1000 | Substrate recognition and ubiquitin ligation | RING, HECT, or RBR domains | RING: Direct transfer from E2 to substrate; HECT: Forms E3~Ub intermediate before substrate transfer |
| DUBs | ~100 | Ubiquitin removal and recycling | USP, OTU, UCH, MJD, MINDY, or JAMM/MPN+ domains | Hydrolysis of isopeptide bond between ubiquitin and substrate lysine |
Deubiquitinating Enzymes (DUBs)
DUBs constitute approximately 100 proteases categorized into six families: USP, OTU, UCH, MJD, MINDY, and JAMM [2]. These enzymes perform critical regulatory functions by reversing ubiquitination events, processing ubiquitin precursors, and maintaining free ubiquitin pools [2]. DUBs ensure the dynamic nature of ubiquitin signaling and have emerged as important players in disease pathogenesis, particularly in cancer [2] [5].
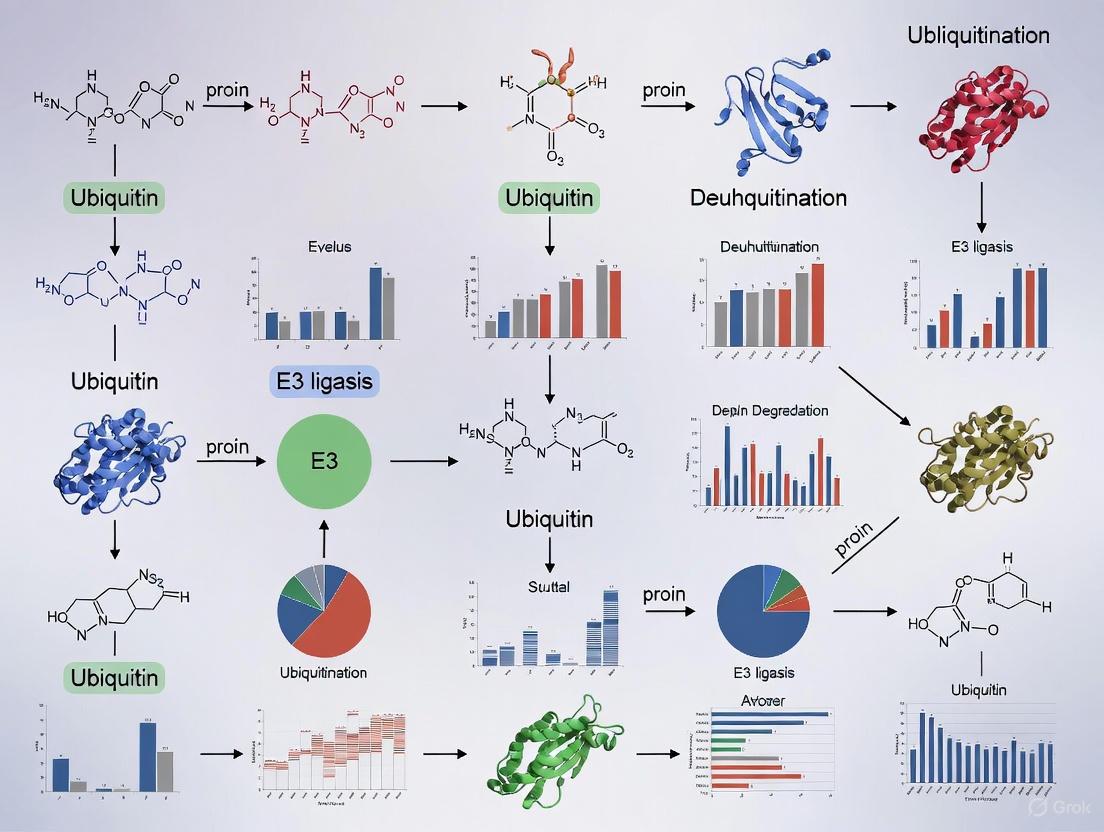
Diagram 1: The Ubiquitination Cascade and Its Reversal by DUBs. This diagram illustrates the sequential action of E1, E2, and E3 enzymes in conjugating ubiquitin to substrate proteins, and the counteracting role of DUBs in removing ubiquitin signals.
Comparative Structural and Functional Analysis
E2 Enzymes: Key Structural Determinants
E2 enzymes serve as central hubs in the ubiquitination cascade, functioning as more than simple ubiquitin carriers [4]. Their conserved UBC domain features four α-helices and a four-stranded β-sheet with an active-site cysteine preceding a short 3₁₀ helix [4]. E2 enzymes are classified into four classes:
- Class I: Contain only the UBC core domain
- Class II: Have additional N-terminal extensions
- Class III: Contain C-terminal extensions
- Class IV: Possess both N- and C-terminal extensions [3]
Critical E2 surfaces include the N-terminal helix (α1) for E1 and E3 interactions, the β2-β3 loop, and the 3₁₀-to-α2 loop [4]. The E2 backside binding site (distinct from the active site) facilitates non-covalent ubiquitin binding that can influence ubiquitin transfer and chain assembly [6].
E3 Ligases: Mechanisms of Substrate Recognition
E3 ligases employ diverse strategies for substrate recognition:
- RING E3s: Function as scaffolds that simultaneously bind E2~Ub and substrate, facilitating direct ubiquitin transfer from E2 to substrate [1].
- HECT E3s: Form a covalent thioester intermediate with ubiquitin before transferring it to substrates [1] [7].
- RBR E3s: Utilize a hybrid mechanism incorporating aspects of both RING and HECT E3s [4].
Table 2: E2 Enzymes in Human Cancers
| E2 Enzyme | Synonyms | Regulated Targets | Relevant Cancers | Primary Functions |
|---|---|---|---|---|
| UBE2C | UBCH10 | AKT degradation | Breast, esophageal, hepatocellular, lung, thyroid cancers [3] | Cell cycle regulation |
| UBE2T | FANCT, PIG50 | Facilitates β-catenin nuclear translocation | Breast, nasopharyngeal, bladder, hepatocellular, gastric cancers [3] | DNA damage repair, Wnt signaling |
| UBE2N | UBC13 | NF-κB and p38 signaling activation with UBE2V1/V2 | B-cell lymphoma, neuroblastoma, colon, breast cancers [3] | NF-κB signaling, DNA repair |
| UBE2S | E2-EPF | p53 degradation | Colorectal, breast, endometrial, lung, liver cancers [3] | Proteasomal degradation |
| UBE2A/B | RAD6A/B | p53 monoubiquitination, PCNA monoubiquitination | Ovarian, breast cancers, melanoma [3] | DNA damage tolerance, translation |
Experimental Approaches for Studying Ubiquitination
Key Methodologies
- In Vitro Ubiquitination Assays: Reconstituted systems with purified E1, E2, E3, ubiquitin, and ATP allow direct assessment of ubiquitination activity [7]. These assays can monitor autoubiquitination, substrate ubiquitination, and free chain formation [7].
- Global Protein Stability (GPS) Profiling: A genome-wide screening strategy that identifies E3 substrates using reporter proteins fused with potential substrates [1]. Inhibiting E3 ligase activity causes substrate accumulation, revealing regulatory relationships [1].
- shRNA/CRISPR-Cas9 Screening: Functional genomic approaches to identify E3 substrates and components of ubiquitination pathways through targeted gene disruption [1].
- Mass Spectrometry-Based Ubiquitinomics: Advanced proteomic techniques enable system-wide identification of ubiquitination sites and ubiquitin chain linkages [7].
Key Research Reagents
Table 3: Essential Research Reagents for Ubiquitination Studies
| Reagent/Category | Specific Examples | Function/Application | Experimental Use |
|---|---|---|---|
| E1 Inhibitors | TAK-243 (MLN7243), PYR-41 | Inhibit ubiquitin activation | Blocks global ubiquitination; studies of ubiquitin-dependent processes |
| E3 Ligase Modulators | Nutlin-3a, Idasanutlin (RG7388) | MDM2-p53 interaction inhibitors | Stabilizes p53; studies of p53 pathway and cancer models |
| DUB Inhibitors | HBX19818, P22077 | Target USP10 | Induces anti-proliferative effects in FLT3-mutant AML |
| Molecular Glue Degraders | Mezigdomide (CC-92480), XMU-MP-8 | Induce neo-protein interactions | Targeted protein degradation; studies of oncoprotein elimination |
| SUMOylation Inhibitors | Subasumstat (TAK-981), ML-792, 2-D08 | Inhibit SUMOylation cascade | Studies of SUMO-targeted ubiquitin ligases (StUbLs) and protein stability |
| Recombinant Proteins | E1, E2, E3 enzymes, Ubiquitin variants | Enzyme sources for in vitro assays | Reconstitute ubiquitination cascades; mechanistic studies |
Diagram 2: Experimental Workflow for Studying Ubiquitination. This workflow outlines the key steps from biochemical reconstitution to functional validation in cellular systems.
Ubiquitination Machinery in Cancer and Targeted Therapies
E2 Enzymes as Oncogenic Drivers
Dysregulation of specific E2 enzymes promotes tumorigenesis through diverse mechanisms:
- UBE2T is overexpressed in multiple cancers and facilitates β-catenin nuclear translocation while inhibiting SOX6 expression, promoting Wnt signaling activation [3].
- UBE2C promotes tumor progression through AKT degradation and is elevated in breast, esophageal, hepatocellular, and lung cancers [3].
- UBE2N partners with UBE2V1 or UBE2V2 to activate NF-κB and p38 signaling pathways, driving progression in B-cell lymphoma, neuroblastoma, and various solid tumors [3].
DUBs in Cancer Pathogenesis
DUBs demonstrate context-dependent roles in cancer, functioning as both tumor promoters and suppressors:
- USP9X exhibits dual functions in pancreatic cancer—promoting tumor cell survival in human models while acting as a suppressor in mouse models [2].
- USP22 is recognized as a cancer stem cell marker that promotes PDAC proliferation by regulating DYRK1A and PTEN-MDM2-p53 signaling [2].
- USP21 promotes PDAC growth by activating mTOR signaling and inducing micropinocytosis to support amino acid sustainability [2].
- BAP1 mutations lead to a hereditary cancer syndrome predisposing to mesothelioma, melanoma, breast cancer, and renal carcinoma [2].
Emerging Therapeutic Strategies
Novel approaches targeting the ubiquitination machinery show significant promise:
- Proteasome Inhibitors: Bortezomib and related compounds disrupt protein degradation, but their application is limited by non-specific effects [1].
- SUMO-Targeted Ubiquitin Ligases (StUbLs): Drugs like arsenic trioxide and fulvestrant leverage SUMO-primed ubiquitination to inactivate oncogenic fusion proteins like PML-RARα and estrogen receptor α [8].
- Molecular Glue Degraders: Compounds such as Mezigdomide (CC-92480) redirect E3 ligases to target oncoproteins for degradation [9].
- HUWE1-Targeting Compounds: BI8622 and BI8626 represent early-stage inhibitors that surprisingly function as HUWE1 substrates themselves, being ubiquitinated by their target ligase [7].
The ubiquitination machinery represents a sophisticated regulatory network with profound implications for cancer biology and therapeutics. While E3 ligases have traditionally received the most attention, recent research highlights the critical functions of E2 enzymes in determining ubiquitin chain topology and the context-dependent roles of DUBs in maintaining protein homeostasis. The experimental approaches outlined here—from in vitro ubiquitination assays to genome-wide screening strategies—provide powerful tools for deciphering the complexities of this system. As our understanding of ubiquitination deepens, new therapeutic opportunities continue to emerge, particularly through targeted protein degradation strategies and selective inhibition of specific pathway components. Future research will likely focus on developing more specific modulators of E2 and E3 activities and elucidating the complex regulatory networks that coordinate ubiquitin signaling in both normal physiology and disease states.
Ubiquitination, once recognized primarily as a mechanism for targeting proteins to the proteasome for degradation, is now understood to be a versatile post-translational modification with profound regulatory functions across cellular signaling and immune responses. This modification involves the sequential action of E1 activating, E2 conjugating, and E3 ligase enzymes that attach ubiquitin molecules to target proteins, creating a complex code that determines protein fate and function [10] [11]. Beyond the traditional K48-linked polyubiquitin chains that signal proteasomal degradation, atypical ubiquitin linkages—including K63, M1, K11, K27, and K29 chains—orchestrate diverse non-proteolytic processes such as signal transduction, protein trafficking, inflammation, and immune cell differentiation [12] [11]. The emerging paradigm recognizes ubiquitination as a central regulatory mechanism in immunity and cancer, with E3 ligases and deubiquitinases (DUBs) acting as precise molecular switches that control pathway activation, immune cell polarization, and cellular homeostasis. This review examines the expanding landscape of non-degradative ubiquitination, its implications for immune regulation and cancer progression, and the prognostic value of ubiquitination-related genes in clinical oncology.
Mechanistic Insights: Ubiquitination in Signaling and Immunity
Regulation of Immune Cell Function through Ubiquitination
Ubiquitination plays a critical role in fine-tuning immune responses by modulating key signaling pathways in various immune cell types. In regulatory T cells (Tregs), which are essential for maintaining immune tolerance, the E3 ligase GRAIL (RNF128) regulates IL-2 receptor signaling through a sophisticated mechanism involving competitive mono-ubiquitination [13] [10]. GRAIL mono-ubiquitinates Lys724 on cullin-5 (CUL5), thereby blocking neddylation—a ubiquitin-like modification required for activation of the CRL5 E3 ligase complex. When active, CRL5 promotes ubiquitination and degradation of phosphorylated JAK1 (pJAK1), leading to desensitization of IL-2R signaling and impaired STAT5 phosphorylation, which is crucial for Treg suppressive function [13] [10]. In autoimmune conditions, diminished GRAIL expression disrupts this balance, resulting in excessive CRL5-mediated desensitization of IL-2R signaling and compromised Treg function. Pharmacological inhibition of neddylation has demonstrated potential in restoring IL-2R signaling and Treg suppressive capacity, highlighting the therapeutic relevance of this regulatory axis [13].
In macrophages, ubiquitination governs functional plasticity and polarization states along the pro-inflammatory M1 to anti-inflammatory M2 spectrum. Multiple E3 ligases and DUBs regulate key inflammatory pathways including NF-κB, NLRP3 inflammasome assembly, and metabolic reprogramming [11]. The E3 ligases Cbl-b and Itch, along with GRAIL, dampen inflammatory signaling by targeting adaptor proteins like MyD88 and TRIF, thereby preventing excessive M1 polarization [11]. Conversely, the deubiquitinase BRCC3 removes inhibitory ubiquitin chains from NLRP3, facilitating inflammasome assembly and IL-1β maturation [11]. OTULIN, a linear linkage-specific deubiquitinase, hydrolyzes M1-linked ubiquitin chains generated by the LUBAC complex on components of TLR and TNF signaling pathways; its deficiency leads to uncontrolled NF-κB activation and severe autoinflammation [12] [11]. This intricate balance of ubiquitin ligases and DUBs allows macrophages to dynamically adjust their functional state in response to environmental cues.
Table 1: Key E3 Ubiquitin Ligases and Deubiquitinases in Immune Regulation
| Enzyme | Type | Immune Cell/Process | Mechanism of Action | Functional Outcome |
|---|---|---|---|---|
| GRAIL (RNF128) | E3 Ligase (RING-type) | Regulatory T Cells | Mono-ubiquitinates CUL5 at Lys724 to block CRL5 neddylation | Sustains IL-2R signaling and Treg suppressive function [13] [10] |
| CRL5 Complex | E3 Ligase (Cullin-RING) | Cytokine Signaling | Neddylation-dependent ubiquitination of pJAK1 | Desensitizes IL-2R signaling [13] |
| Cbl-b | E3 Ligase | Macrophages, T Cells | Ubiquitinates MyD88 and TRIF adaptor proteins | Terminates TLR signaling; prevents excessive M1 polarization [11] |
| OTULIN | Deubiquitinase (Linear linkage-specific) | Macrophage Inflammation | Hydrolyzes M1-linked ubiquitin chains on TLR/TNF pathway components | Restrains NF-κB activation; deficiency causes autoinflammation [12] [11] |
| BRCC3 | Deubiquitinase | Macrophage Inflammasome | Removes K48/K63 ubiquitin from NLRP3 | Promotes NLRP3 inflammasome assembly and IL-1β maturation [11] |
Ubiquitination in Inflammatory Signaling Pathways
The NF-κB pathway exemplifies how ubiquitination extends beyond protein degradation to directly activate signaling cascades. Upon stimulation of toll-like receptors (TLRs) or cytokine receptors, K63-linked and linear M1-linked polyubiquitin chains serve as essential scaffolds for signal propagation [12]. TLR activation recruits the adaptors MyD88 and IRAK1/4, leading to TRAF6 ubiquitination with K63 chains in cooperation with the E2 enzyme Ubc13. These non-degradative ubiquitin modifications create docking platforms that recruit downstream kinases like TAK1, initiating the NF-κB activation program [12]. Similarly, TNF receptor stimulation engages the LUBAC complex, which extends K63 ubiquitination on NEMO with linear M1 chains, recruiting the IKK complex and culminating in IκBα phosphorylation, K48-linked ubiquitination, and degradation—releasing NF-κB dimers to translocate to the nucleus and drive transcription of inflammatory genes [12] [14].
The NLRP3 inflammasome, responsible for caspase-1 activation and IL-1β maturation, is similarly regulated by ubiquitination. The E3 ligase HUWE1 modifies NLRP3 with atypical K27-linked chains to regulate inflammasome activity, while BRCC3-mediated deubiquitination removes degradative ubiquitin marks, permitting NLRP3 oligomerization and inflammasome assembly [12] [11]. These examples illustrate how the ubiquitin code—comprising different chain types and linkages—functions as a sophisticated language that coordinates inflammatory responses without necessarily targeting components for destruction.
Diagram 1: Ubiquitin-dependent NF-κB activation. Multiple ubiquitin linkage types (K63, M1, K48) coordinate signaling through TLR4 and TNF receptors, culminating in NF-κB nuclear translocation and inflammatory gene transcription.
Prognostic Value of Ubiquitination-Related Genes in Cancer
Ubiquitination-Based Prognostic Signatures Across Cancers
The dysregulation of ubiquitination pathways has emerged as a significant factor in cancer progression and patient outcomes. Comprehensive bioinformatics analyses have identified ubiquitination-related gene signatures with robust prognostic value across diverse malignancies. In diffuse large B-cell lymphoma (DLBCL), a three-gene ubiquitination signature comprising CDC34, FZR1, and OTULIN effectively stratifies patients into distinct risk categories [15]. Elevated expression of CDC34 and FZR1 coupled with low OTULIN expression correlates with poor prognosis, with significant differences in immune scores and drug sensitivity observed between high- and low-risk groups [15]. Similarly, in cervical cancer, a five-gene signature (MMP1, RNF2, TFRC, SPP1, and CXCL8) demonstrates strong predictive value for patient survival, with the risk score model showing area under the curve (AUC) values >0.6 for 1-, 3-, and 5-year survival [16]. Immune microenvironment analysis revealed significant differences in 12 immune cell types between risk groups, including memory B cells and M0 macrophages, along with differential expression of four immune checkpoints [16].
Ovarian cancer studies have identified a 17-gene ubiquitination-based prognostic signature that effectively stratifies patients by overall survival [17]. The high-risk group showed significantly lower survival probability (P < 0.05), with the model achieving AUC values of 0.703, 0.704, and 0.705 for 1-, 3-, and 5-year survival, respectively [17]. Immune infiltration analysis demonstrated higher levels of CD8+ T cells (P < 0.05), M1 macrophages (P < 0.01), and follicular helper cells (P < 0.05) in the low-risk group, while high-risk patients exhibited more frequent mutations in MUC17 and LRRK2 genes [17]. Functional validation identified FBXO45 as a key E3 ubiquitin ligase promoting ovarian cancer growth, spread, and migration via the Wnt/β-catenin pathway [17].
Table 2: Ubiquitination-Related Prognostic Signatures in Cancer
| Cancer Type | Key Ubiquitination-Related Genes | Prognostic Value | Immune Microenvironment Associations |
|---|---|---|---|
| Diffuse Large B-Cell Lymphoma (DLBCL) | CDC34, FZR1, OTULIN | Elevated CDC34/FZR1 + low OTULIN = poor prognosis [15] | Significant differences in immune scores between risk groups; correlation with T-cell infiltration and endocytosis [15] |
| Cervical Cancer | MMP1, RNF2, TFRC, SPP1, CXCL8 | AUC >0.6 for 1/3/5-year survival [16] | 12 immune cell types differentially abundant (including memory B cells, M0 macrophages); 4 immune checkpoints differentially expressed [16] |
| Ovarian Cancer | 17-gene signature including FBXO45 | 1-year AUC=0.703, 3-year AUC=0.704, 5-year AUC=0.705 [17] | Low-risk group: higher CD8+ T cells, M1 macrophages, follicular helper cells; different mutation profiles [17] |
| Pan-Cancer | UBE2T, UBD | Overexpression correlates with poor survival across multiple cancers [18] [19] | Correlation with immune infiltration, checkpoint expression, TMB, MSI, and neoantigens [18] [19] |
Pan-Cancer Analysis of Ubiquitination Enzymes
Comprehensive pan-cancer analyses reveal that specific ubiquitination enzymes demonstrate consistent prognostic value across diverse cancer types. Ubiquitin-conjugating enzyme E2T (UBE2T) shows elevated expression in multiple tumors, where its upregulation associates with poor clinical outcomes [18]. Genetic variation analysis identifies "amplification" as the predominant alteration in UBE2T, followed by mutations, with copy number variations occurring frequently across pan-cancer cohorts [18]. UBE2T expression correlates with sensitivity to targeted agents including trametinib and selumetinib, while showing negative correlation with CD-437 and mitomycin sensitivity. Functional enrichment analyses implicate UBE2T in cell cycle regulation, ubiquitin-mediated proteolysis, p53 signaling, and mismatch repair pathways [18].
Similarly, ubiquitin D (UBD) demonstrates overexpression in 29 cancer types, where it associates with poor prognosis and higher histological grades [19]. Gene amplification represents the most common genetic alteration, with patients harboring these alterations exhibiting significantly reduced overall survival rates. Epigenetically, 16 cancer types show reduced UBD promoter methylation, potentially contributing to its overexpression [19]. UBD expression significantly correlates with tumor microenvironment features including immune infiltration, checkpoint expression, microsatellite instability (MSI), tumor mutational burden (TMB), and neoantigen load. Pathway analyses indicate UBD involvement in neurodegeneration, proteolysis, and apoptosis, with additional roles in NF-κB, Wnt, and SMAD2 signaling through interactions with MAD2, p53, and β-catenin [19].
Experimental Approaches and Methodologies
Bioinformatics Pipelines for Ubiquitination Signature Development
The development of ubiquitination-related prognostic signatures follows standardized bioinformatics workflows that integrate multi-omics data. Typical pipelines begin with differential gene expression analysis between tumor and normal tissues using packages such as DESeq2 or limma, with filtering criteria generally set at fold change >2 and false discovery rate (FDR) <0.05 [15] [16]. Ubiquitination-related genes are identified from databases such as the Ubiquitin and Ubiquitin-like Conjugation Database (UUCD), which catalogs E1, E2, and E3 enzymes [17]. Survival-associated ubiquitination genes are selected through univariate Cox regression analysis, followed by least absolute shrinkage and selection operator (LASSO) Cox regression to identify the most prognostic genes using the glmnet package with 10-fold cross-validation [15] [16].
Risk scores are calculated using the formula: Risk score = Σ(Coefi × Expri), where Coefi represents the regression coefficient from multivariate Cox regression and Expri denotes the expression level of each gene [16] [17]. Patients are stratified into high- and low-risk groups based on the median risk score, with Kaplan-Meier survival analysis and log-rank tests employed to evaluate prognostic performance. Receiver operating characteristic (ROC) curves at 1, 3, and 5 years assess predictive accuracy, with AUC values >0.6 generally considered clinically informative [16] [17]. Additional validation typically includes independent prognostic analysis through univariate and multivariate Cox regression, immune microenvironment assessment using tools such as CIBERSORT or ESTIMATE, and drug sensitivity analysis with packages like oncoPredict to calculate half maximal inhibitory concentration (IC50) values [15] [16].
Diagram 2: Bioinformatics workflow for developing ubiquitination-related prognostic signatures. The pipeline integrates multi-omics data to identify, validate, and apply ubiquitination-based biomarkers across cancer types.
Table 3: Essential Research Reagents and Resources for Ubiquitination Studies
| Reagent/Resource | Type | Function/Application | Examples/Sources |
|---|---|---|---|
| DESeq2 / limma | Bioinformatics Package | Differential gene expression analysis | Bioconductor [15] [16] |
| UUCD Database | Ubiquitin Enzyme Database | Comprehensive catalog of E1, E2, E3 enzymes | http://uucd.biocuckoo.org/ [17] |
| glmnet | Bioinformatics Package | LASSO Cox regression analysis | CRAN [15] [16] |
| CIBERSORT | Computational Tool | Immune cell infiltration analysis | https://cibersort.stanford.edu/ [15] [16] |
| oncoPredict | R Package | Drug sensitivity analysis (IC50 calculation) | Bioconductor [15] |
| TCGA/GTEx | Databases | Transcriptomic and clinical data | https://www.cancer.gov/ccg/research/genome-sequencing/tcga [17] [18] [19] |
| GEPIA2 | Web Tool | Gene expression analysis and visualization | http://gepia2.cancer-pku.cn/ [18] [19] |
| cBioPortal | Web Resource | Cancer genomics and visualization | https://www.cbioportal.org/ [18] [19] |
| Neddylation Inhibitors (NAEi) | Small Molecules | Pharmacological inhibition of neddylation pathway | Research compounds [13] [10] |
| PROTACs | Therapeutic Modality | Targeted protein degradation via ubiquitin-proteasome system | Clinical development [17] |
The expanding landscape of ubiquitination research reveals an intricate regulatory system that extends far beyond its traditional role in protein degradation to encompass sophisticated control of immune signaling, cell fate decisions, and cancer progression. Non-degradative ubiquitin linkages, particularly K63 and M1 chains, serve as critical signaling scaffolds in inflammation and immunity, while the balanced expression of E3 ligases and deubiquitinases maintains immune homeostasis. In clinical oncology, ubiquitination-related genes demonstrate remarkable prognostic value across diverse malignancies, with multi-gene signatures effectively stratifying patients by survival outcomes, immune microenvironment composition, and therapeutic vulnerabilities. The integration of bioinformatics approaches with experimental validation has accelerated the discovery of ubiquitination-based biomarkers, while emerging therapeutic strategies—including neddylation pathway inhibitors and PROTAC technology—hold significant promise for targeting the ubiquitin system in cancer and immune disorders. As our understanding of the ubiquitin code continues to evolve, so too will opportunities for diagnostic innovation and therapeutic intervention across the spectrum of human disease.
Mechanisms of Ubiquitination Dysregulation in Carcinogenesis
Ubiquitination, a pivotal post-translational modification, is a highly specific process involving the covalent attachment of ubiquitin to substrate proteins, thereby regulating their stability, localization, and activity [20] [21]. This enzymatic cascade is mediated by ubiquitin-activating (E1), ubiquitin-conjugating (E2), and ubiquitin-ligating (E3) enzymes, with E3 ligases providing substrate specificity [22] [20]. The dysregulation of this system contributes significantly to tumorigenesis by affecting critical cellular processes including cell cycle progression, DNA repair, apoptosis, and immune surveillance [20] [23] [21]. This review objectively compares the prognostic value of ubiquitination-related genes across multiple cancer types, supported by experimental data and detailed methodologies, to establish their utility in cancer research and drug development.
Ubiquitination Machinery and Cancer-Associated Alterations
The ubiquitin-proteasome system (UPS) comprises approximately 2 E1 enzymes, 40 E2 enzymes, and over 600 E3 ligases in human cells, along with deubiquitinating enzymes (DUBs) that reverse the process [22] [20]. These components collectively maintain protein homeostasis, and their dysfunction can lead to carcinogenesis through multiple mechanisms. E3 ligases, in particular, demonstrate remarkable substrate specificity, making them attractive therapeutic targets [20]. Oncogenic alterations in the UPS include mutations in E3 ligase genes leading to accelerated degradation of tumor suppressors, overexpression of specific E2 enzymes driving cell cycle progression, and aberrant DUB activity stabilizing oncoproteins [22] [20] [21].
Different ubiquitination linkage types dictate distinct functional outcomes for substrate proteins. While K48-linked polyubiquitination typically targets proteins for proteasomal degradation, K63-linked chains often regulate protein activity and subcellular localization [22] [24]. Monoubiquitination plays roles in DNA damage repair and histone modification, with recent evidence implicating it in cancer immune evasion [21]. The complexity of the ubiquitin code—encompassing chain topology, length, and modification types—creates a sophisticated regulatory layer that is frequently disrupted in cancer [20] [21].
Table 1: Ubiquitination Linkage Types and Their Roles in Cancer
| Linkage Type | Primary Function | Role in Cancer | Examples |
|---|---|---|---|
| K48 | Targets proteins for proteasomal degradation | Accumulation of oncoproteins; loss of tumor suppressors | p53 degradation by MDM2 [22] [20] |
| K63 | Regulates activity, localization, and signaling | Activation of oncogenic signaling pathways | β-catenin stabilization [22] |
| K11 | Cell cycle regulation and trafficking | Dysregulated cell cycle progression in cancer | APC/C-mediated cyclin degradation [22] [20] |
| K27 | Mitochondrial autophagy | Impaired cellular homeostasis | Parkin-mediated mitophagy [20] |
| K6 | DNA damage repair | Genomic instability | RNF168-mediated DNA repair [25] [20] |
| M1 (Linear) | NF-κB activation | Inflammation and cancer progression | LUBAC complex in lymphoma [21] |
| Monoubiquitination | Histone modification, endocytosis | Altered gene expression, immune evasion | PD-L1 internalization [21] |
Comparative Analysis of Ubiquitination-Related Prognostic Models Across Cancers
Recent research has established ubiquitination-related gene signatures as powerful prognostic tools across diverse malignancies. These models typically employ bioinformatic analyses of public datasets (e.g., TCGA, GEO) to identify ubiquitination-related genes with significant associations with patient survival, which are then incorporated into risk stratification systems.
Ovarian Cancer
In ovarian cancer, a 17-gene ubiquitination-related signature effectively stratified patients into high-risk and low-risk groups with significantly different overall survival (p < 0.05) [25]. The model demonstrated high prognostic accuracy with area under the curve (AUC) values of 0.703, 0.704, and 0.705 for 1-, 3-, and 5-year survival, respectively [25]. The high-risk group exhibited distinct immune profiles with lower levels of CD8+ T cells (p < 0.05), M1 macrophages (p < 0.01), and follicular helper T cells (p < 0.05), along with higher mutation frequencies in MUC17 and LRRK2 genes [25]. Experimental validation identified FBXO45 as a key E3 ubiquitin ligase promoting ovarian cancer growth, spread, and migration via the Wnt/β-catenin pathway [25].
Lung Adenocarcinoma
A four-gene ubiquitination-related risk score (URRS) comprising DTL, UBE2S, CISH, and STC1 effectively predicted prognosis in lung adenocarcinoma (LUAD) [26]. Patients with higher URRS had significantly worse outcomes (Hazard Ratio [HR] = 0.54, 95% Confidence Interval [CI]: 0.39–0.73, p < 0.001), a finding validated across six external cohorts (HR = 0.58, 95% CI: 0.36–0.93, pmax = 0.023) [26]. The high URRS group showed higher PD-1/PD-L1 expression (p < 0.05), increased tumor mutation burden (TMB, p < 0.001), elevated tumor neoantigen load (TNB, p < 0.001), and distinct tumor microenvironment scores (p < 0.001) [26]. Upregulation of STC1, UBE2S, and DTL was associated with poorer prognosis, while CISH upregulation correlated with better outcomes [26].
Breast Cancer
A six-gene ubiquitination signature (ATG5, FBXL20, DTX4, BIRC3, TRIM45, and WDR78) demonstrated robust prognostic power in breast cancer [27]. This signature was validated across multiple external datasets (TCGA-BRAC, GSE1456, GSE16446, GSE20711, GSE58812, and GSE96058), with Kaplan-Meier curves showing significant survival differences (p < 0.05) [27]. Single-cell analysis revealed distinct immune compositions between risk groups, with Vd2 γδ T cells less abundant in the low-risk group and myeloid dendritic cells absent in the high-risk group [27]. Tumor microbiological analysis further identified notable variations in microorganism diversity between risk groups [27].
Esophageal Squamous Cell Carcinoma
In ESCC, researchers identified five key ubiquitination-related genes (BUB1B, CHEK1, DNMT1, IRAK1, and PRKDC) with significant prognostic value through analysis of TCGA-ESCC, GSE20347, and in-house datasets [28]. These genes play crucial roles in cell cycle regulation and immune responses, with functional enrichment analyses linking them to ESCC pathogenesis [28]. The study highlighted these genes as promising biomarkers and therapeutic targets for a cancer type with a 5-year survival rate below 20% [28].
Table 2: Comparison of Ubiquitination-Related Prognostic Models Across Cancers
| Cancer Type | Key Genes in Signature | HR (High vs. Low Risk) | Validation Approach | Clinical/Biological Associations |
|---|---|---|---|---|
| Ovarian Cancer | 17-gene signature | Significant (p < 0.05) [25] | External datasets (GSE165808, GSE26712) [25] | Altered immune infiltration (CD8+ T cells, M1 macrophages); FBXO45/Wnt/β-catenin pathway activation [25] |
| Lung Adenocarcinoma | DTL, UBE2S, CISH, STC1 | 0.54 (95% CI: 0.39-0.73) [26] | 6 external GEO datasets [26] | Higher PD-1/PD-L1, TMB, TNB; distinct TME [26] |
| Breast Cancer | ATG5, FBXL20, DTX4, BIRC3, TRIM45, WDR78 | Significant (p < 0.05) [27] | 6 external datasets [27] | Altered immune cell composition (Vd2 γδ T cells, dendritic cells); microbial diversity [27] |
| Esophageal Squamous Cell Carcinoma | BUB1B, CHEK1, DNMT1, IRAK1, PRKDC | Significant (p < 0.05) [28] | TCGA, GSE20347, in-house data [28] | Cell cycle and immune response pathways [28] |
Experimental Protocols for Ubiquitination Research
Prognostic Model Development Workflow
The development of ubiquitination-related prognostic models follows a systematic bioinformatics pipeline [25] [26] [28]:
Data Collection and Preprocessing: Transcriptomic data and clinical information are obtained from public databases (TCGA, GEO). Normalization and batch effect correction are applied using tools like the "limma" R package [25] [26] [28].
Ubiquitination-Related Gene Selection: URGs are compiled from databases such as iUUCD 2.0 and UUCD, typically including E1, E2, and E3 enzymes [25] [26].
Differential Expression Analysis: Differentially expressed URGs between tumor and normal tissues are identified using |logFC| ≥ 0.5-1 and adjusted p-value < 0.05 as thresholds [25] [28].
Prognostic Gene Selection: Univariate Cox regression, LASSO regression, and Random Survival Forests are applied to identify URGs with significant survival associations [25] [26].
Risk Model Construction: A risk score formula is developed: Risk score = Σ(Coefi × Expri), where Coefi is the regression coefficient and Expri is the gene expression level [25] [26].
Validation: Models are validated using internal cross-validation and external independent datasets, assessing performance via Kaplan-Meier survival analysis, ROC curves, and AUC values [25] [26] [27].
Diagram 1: FBXO45 promotes ovarian cancer progression via Wnt/β-catenin pathway. Based on experimental validation in ovarian cancer [25].
Functional Validation Experiments
Beyond bioinformatic analyses, functional experiments are crucial for validating the mechanistic roles of ubiquitination factors:
Gene Manipulation in Cell Lines:
Phenotypic Assays:
Molecular Mechanism Studies:
Immunological Analyses:
Key Signaling Pathways in Ubiquitination-Mediated Carcinogenesis
Regulation of Immune Checkpoints
The ubiquitin-proteasome system plays a crucial role in regulating PD-1/PD-L1 stability, thereby influencing tumor immune evasion [24]. Multiple E3 ligases target PD-L1 for degradation, including SPOP which promotes PD-L1 ubiquitination and proteasomal degradation in colorectal cancer [24]. Conversely, competitive binding partners such as ALDH2 and SGLT2 can inhibit SPOP-mediated PD-L1 degradation, stabilizing PD-L1 and promoting immune escape [24]. The small-molecule SGLT2 inhibitor canagliflozin can disrupt SGLT2-PD-L1 interaction, restoring SPOP-mediated PD-L1 degradation and enhancing T cell antitumor activity [24]. Additional regulatory mechanisms include CDK4-mediated phosphorylation of SPOP, which promotes 14-3-3γ binding and impairs SPOP's tumor suppressor function [24].
Diagram 2: UPS regulation of PD-L1 stability impacts tumor immune evasion. Based on mechanism described in review [24].
Oncoprotein and Tumor Suppressor Regulation
Ubiquitination critically regulates key oncoproteins and tumor suppressors:
- p53: The E3 ligase MDM2 binds to p53, promoting its ubiquitination and degradation; MDM2 overexpression is observed in various cancers [22] [20].
- RAS proteins: Ubiquitination dynamically regulates RAS stability, membrane localization, and signaling, with heterogeneity across different RAS isoforms (KRAS4A, KRAS4B, NRAS, HRAS) [29].
- β-catenin: K11-linked polyubiquitination can stabilize β-catenin in colorectal cancer cells, contrary to the typical degradation signal [22].
- c-Myc: Multiple E3 ligases including FBXW7 regulate c-Myc stability, with dysregulation contributing to sustained oncogenic signaling [20].
Table 3: Research Reagent Solutions for Ubiquitination Studies
| Reagent/Category | Specific Examples | Function/Application | Experimental Context |
|---|---|---|---|
| Cell Culture Reagents | DMEM, RPMI 1640, Fetal Bovine Serum | Cell line maintenance and experiments | Ovarian cancer cell culture (A2780, HEY) [25] |
| Molecular Biology Kits | RNAiso Reagent, RNA Reverse Transcription Kit, Real-time PCR Kit | Gene expression analysis | Validation of ubiquitination-related gene expression [25] [26] |
| Transfection Reagents | Lipo2000 | Nucleic acid delivery for gene modulation | FBXO45 functional studies in ovarian cancer [25] |
| Protein Analysis Reagents | High-performance RIPA lysate, Phosphatase/Protease Inhibitor Mix, ECL Chemiluminescent Liquid | Protein extraction and detection | Western blot analysis of ubiquitination pathways [25] |
| Antibodies | FBXO45, WNT1, β-cadherin, c-Myc, GAPDH | Target protein detection | Pathway validation in ovarian cancer [25] |
| Proteasome Inhibitors | Bortezomib, Carfilzomib, Ixazomib | Clinical targeting of UPS | Multiple cancer types [20] |
| E1-Targeting Compounds | MLN7243, MLN4924 | Experimental inhibition of ubiquitination cascade | Preclinical cancer models [20] |
| E2-Targeting Compounds | Leucettamol A, CC0651 | Selective E2 enzyme inhibition | Preclinical studies [20] |
| E3-Targeting Compounds | Nutlin, MI-219 (MDM2 inhibitors) | Specific E3 ligase modulation | p53 stabilization approaches [20] |
| DUB Inhibitors | Compounds G5, F6 | Deubiquitinase inhibition | Experimental therapeutic strategy [20] |
Therapeutic Implications and Future Directions
Targeting the ubiquitin-proteasome system has yielded significant clinical successes, particularly with proteasome inhibitors such as bortezomib in multiple myeloma [20]. Emerging strategies include:
- PROTACs (Proteolysis-Targeting Chimeras): Bifunctional molecules that recruit E3 ligases to target specific proteins for degradation; several are in clinical trials including ARV-110 and ARV-471 [25] [21].
- Molecular Glues: Small molecules that enhance interaction between E3 ligases and target proteins; examples include CC-90009 in clinical trials for leukemia [21].
- Specific E3 Ligase Modulators: Compounds like indomethacin enhance SYVN1-mediated ITGAV ubiquitination in esophageal squamous cell carcinoma, while honokiol induces KRT18 ubiquitination in melanoma [21].
The prognostic models based on ubiquitination-related genes not only stratify patient risk but also inform treatment selection. High-risk lung adenocarcinoma patients with elevated URRS showed lower IC50 values for various chemotherapy drugs, suggesting increased susceptibility [26]. Similarly, the integration of ubiquitination signatures with immune profiling may guide immunotherapy approaches, particularly given the role of UPS in regulating PD-1/PD-L1 [24].
Future research directions should focus on validating these prognostic models in prospective clinical trials, developing isoform-specific ubiquitination modulators, and exploring combination therapies targeting both ubiquitination pathways and conventional oncogenic drivers. The heterogeneity of ubiquitination patterns across cancer types and even within specific molecular subtypes necessitates personalized approaches based on comprehensive ubiquitination profiling.
Comprehensive Databases for Ubiquitination-Related Gene Discovery
Ubiquitination is a crucial post-translational modification that regulates protein stability, function, and localization, thereby influencing nearly all cellular processes in eukaryotic cells. This sophisticated process involves a cascade of enzymes: ubiquitin-activating enzymes (E1), ubiquitin-conjugating enzymes (E2), ubiquitin ligases (E3), and deubiquitinating enzymes (DUBs) [16] [30]. The ubiquitin-proteasome system (UPS) degrades approximately 80% of intracellular proteins, maintaining genomic stability and modulating signaling pathways to regulate critical processes including cell proliferation, apoptosis, DNA damage repair, and immune responses [16]. Given its fundamental role in cellular homeostasis, dysregulation of ubiquitination pathways is intimately associated with various diseases, particularly cancer. Recent studies have demonstrated that abnormalities in ubiquitination-related genes are closely linked to numerous cancers including cervical cancer [16], esophageal squamous cell carcinoma [28], lung adenocarcinoma [26], ovarian cancer [17], and acute myeloid leukemia [31]. The growing recognition of ubiquitination's pathological significance has accelerated the need for comprehensive databases that facilitate the systematic discovery and analysis of ubiquitination-related genes, particularly for developing prognostic models and targeted therapies in oncology.
Comprehensive Database Comparison
Researchers have access to several specialized databases that catalog ubiquitination-related genes and enzymes. These resources vary in scope, content, and functionality, making each suitable for different research applications. The table below provides a detailed comparison of major databases used in contemporary ubiquitination research.
Table 1: Comparison of Major Ubiquitination-Related Gene Databases
| Database Name | Primary Focus | Number of Genes | Gene Categories | Key Features | Use Cases in Cancer Research |
|---|---|---|---|---|---|
| iUUCD 2.0 [26] | Ubiquitin and ubiquitin-like conjugation | 966 genes | E1, E2, E3 enzymes | Comprehensive coverage of ubiquitination enzymes; regularly updated | Identification of prognostic signatures in lung adenocarcinoma [26] |
| UUCD [17] | Ubiquitinating enzymes | 929 genes | E1 (8), E2 (39), E3 (882) | Categorized by enzyme type; established resource | Development of ovarian cancer risk models [17] |
| GeneCards [16] [28] | Integrated human genes | 465 ubiquitination-related genes (score ≥3) [16]; 1,274 URGs (score >5) [28] | Various ubiquitination-related categories | Relevance scoring system; integrates multiple data sources | Screening ubiquitination-related differentially expressed genes [16] [28] |
| Molecular Signatures Database (MSigDB) [28] | Annotated gene sets | 542 ubiquitination-related genes | Gene sets related to ubiquitination | Collection of biologically defined gene sets | Functional enrichment analysis [28] |
The selection of an appropriate database depends heavily on research objectives. For studies focused specifically on ubiquitination enzymes, iUUCD 2.0 and UUCD offer specialized curation. For broader investigations that include ubiquitination-related cellular components and processes, GeneCards provides a more comprehensive resource with relevance scoring to prioritize genes [16] [28]. The Molecular Signatures Database is particularly valuable for pathway analysis and gene set enrichment studies [28]. Each database has been instrumental in various cancer research contexts, enabling the identification of prognostic biomarkers and potential therapeutic targets across multiple cancer types.
Experimental Protocols for Ubiquitination-Related Gene Analysis
Standardized Workflow for Prognostic Model Development
Research into ubiquitination-related genes typically follows a systematic workflow that integrates bioinformatics analysis with experimental validation. The standard methodology encompasses data acquisition, differential expression analysis, prognostic model construction, and experimental validation, as exemplified by studies in cervical cancer [16], lung adenocarcinoma [26], and ovarian cancer [17]. The following diagram illustrates this comprehensive research workflow:
Diagram 1: Research workflow for ubiquitination-related gene discovery
Detailed Methodologies for Key Analytical Steps
Data Acquisition and Preprocessing
Research typically begins with acquiring transcriptomic data from public repositories such as The Cancer Genome Atlas (TCGA), Gene Expression Omnibus (GEO), and Genotype-Tissue Expression (GTEx) [16] [26]. For example, in lung adenocarcinoma research, the TCGA-LUAD cohort serves as the primary training set, while multiple GEO datasets (GSE30219, GSE37745, GSE41271, GSE42127, GSE68465, and GSE72094) provide validation cohorts [26]. Similar approaches are employed in cervical cancer studies using TCGA-GTEx-CESC datasets [16] and in ovarian cancer research combining TCGA-OV and GTEx data [17]. Quality control measures include removing samples with survival times fewer than 3 months, excluding formalin-fixed samples, and filtering recurrent tissues to ensure data integrity [26]. Normalization procedures vary by platform, with microarray data typically processed using the "limma" R package [28] [26] and RNA-seq data analyzed with DESeq2 [16] or edgeR [17].
Identification of Ubiquitination-Related Differentially Expressed Genes
Differentially expressed genes (DEGs) between tumor and normal tissues are identified using established thresholds (typically |log2Fold Change| > 0.5-1.0 and adjusted p-value < 0.05) [16] [17]. These DEGs are then intersected with ubiquitination-related genes (URGs) obtained from specialized databases to identify ubiquitination-related differentially expressed genes (UbDEGs). For instance, in Crohn's disease research, investigators identified 32 UbDEGs by intersecting DEGs from the GSE95095 dataset with ubiquitination-related genes from GeneCards with a relevance score >10 [32]. In tuberculosis research, 96 UbDEGs were identified using similar methodology [33]. Functional enrichment analysis of these UbDEGs using Gene Ontology (GO) and Kyoto Encyclopedia of Genes and Genomes (KEGG) pathways typically reveals their involvement in critical processes including cell cycle regulation, immune response, and protein catabolism [16] [28] [33].
Prognostic Model Construction Using Machine Learning
Ubiquitination-related prognostic models are constructed using various machine learning algorithms. Least Absolute Shrinkage and Selection Operator (LASSO) Cox regression is widely employed to prevent overfitting and select the most informative genes [16] [26]. For example, in cervical cancer research, univariate Cox analysis followed by LASSO algorithms identified five key biomarkers (MMP1, RNF2, TFRC, SPP1, and CXCL8) [16]. Similarly, in lung adenocarcinoma, researchers applied univariate Cox regression, Random Survival Forests, and LASSO Cox regression to identify a four-gene signature (DTL, UBE2S, CISH, and STC1) [26]. Risk scores are calculated using the formula: Risk score = Σ(Coefi × Expi), where Coefi represents the regression coefficient from multivariate Cox analysis, and Expi represents gene expression level [26] [17]. Patients are stratified into high-risk and low-risk groups based on the median risk score, with Kaplan-Meier survival analysis and receiver operating characteristic (ROC) curves used to evaluate prognostic performance.
Immune Infiltration and Tumor Microenvironment Analysis
The tumor immune microenvironment is analyzed using algorithms such as CIBERSORT [32] [33], ESTIMATE [17], and quanTIseq [32]. These tools calculate the abundance of specific immune cell types in tumor tissues based on gene expression data. Studies consistently reveal significant differences in immune cell infiltration between high-risk and low-risk groups defined by ubiquitination-related signatures. For example, in ovarian cancer, the low-risk group showed higher levels of CD8+ T cells, M1 macrophages, and follicular helper T cells [17]. In cervical cancer, 12 types of immune cells, including memory B cells and M0 macrophages, exhibited significant differences between risk groups [16]. Additionally, immune checkpoint expression (e.g., PD-1, PD-L1) often correlates with risk scores, suggesting implications for immunotherapy response [16] [26].
Experimental Validation
Bioinformatics findings require experimental validation using various laboratory techniques. Reverse Transcription Quantitative Polymerase Chain Reaction (RT-qPCR) is routinely employed to verify gene expression trends identified through computational analysis [16] [32] [26]. For example, in cervical cancer research, RT-qPCR confirmed that MMP1, TFRC, and CXCL8 were upregulated in tumor tissues compared to normal controls [16]. Cell culture studies using cancer cell lines (e.g., Caco-2 cells for Crohn's disease research [32], A2780 and HEY cells for ovarian cancer [17]) further validate the functional relevance of identified genes. Gene knockdown or overexpression experiments, followed by assessments of proliferation, migration, and invasion, elucidate the biological roles of specific ubiquitination-related genes. For instance, in ovarian cancer, FBXO45 was experimentally validated to promote cancer growth, spread, and migration via the Wnt/β-catenin pathway [17].
Table 2: Essential Research Reagents and Resources for Ubiquitination Studies
| Category | Specific Reagents/Resources | Application | Key Features |
|---|---|---|---|
| Cell Lines | Caco-2 [32], A2780 [17], HEY [17] | In vitro validation experiments | Well-characterized models for specific cancer types |
| Molecular Biology Kits | RNeasy Mini Kit [31], RevertAid First Strand cDNA Synthesis Kit [32], SYBR Green Real-time PCR Master Mix [32] [31] | RNA extraction, cDNA synthesis, qPCR detection | High purity and sensitivity for gene expression analysis |
| Cell Culture Reagents | DMEM/RPMI 1640 media [17], Fetal Bovine Serum [17], Lipopolysaccharide (LPS) [32] | Cell maintenance and inflammatory stimulation | Standardized conditions for cell-based assays |
| Bioinformatics Tools | DESeq2 [16], limma [28] [26], clusterProfiler [16], CIBERSORT [32] [33], ESTIMATE [17] | Differential expression, functional enrichment, immune infiltration analysis | Statistical rigor and specialized algorithms for omics data |
| Experimental Assays * | Hematoxylin and Eosin (H&E) Staining [32], Immunohistochemistry [32] | Histological analysis and protein localization | Morphological assessment and tissue-based validation |
Clinical Applications and Therapeutic Implications
The systematic discovery of ubiquitination-related genes has significant clinical implications, particularly in prognostic stratification and therapeutic development. Ubiquitination-related prognostic models demonstrate robust predictive power across multiple cancer types. For instance, in lung adenocarcinoma, the ubiquitination-related risk score (URRS) effectively stratified patients with significantly different survival outcomes (HR = 0.54, 95% CI: 0.39-0.73, p < 0.001), with consistent validation in six external cohorts (HR = 0.58, 95% CI: 0.36-0.93, p_max = 0.023) [26]. Similarly, in cervical cancer, the risk model based on five ubiquitination-related biomarkers showed predictive value for 1-, 3-, and 5-year survival (AUC > 0.6 for all time points) [16]. Beyond prognosis, these models provide insights into therapeutic response. High-risk patients typically exhibit higher tumor mutation burden (TMB), increased tumor neoantigen load (TNB), and elevated PD-1/PD-L1 expression, suggesting enhanced susceptibility to immunotherapy [26]. Additionally, ubiquitination-related genes represent promising therapeutic targets themselves, with several emerging as targets for Proteolysis Targeting Chimeras (PROTACs) in ovarian cancer and other malignancies [17].
Comprehensive databases for ubiquitination-related gene discovery have become indispensable resources in cancer research, enabling the development of robust prognostic models and identification of novel therapeutic targets. Specialized databases like iUUCD 2.0 and UUCD provide curated catalogs of ubiquitination enzymes, while broader resources like GeneCards offer comprehensive ubiquitination-related gene sets with relevance scoring. The integration of these databases with standardized analytical workflows—encompassing differential expression analysis, machine learning-based prognostic model construction, immune microenvironment characterization, and experimental validation—has generated significant insights into the role of ubiquitination in cancer biology and clinical outcomes. As mass spectrometry technologies advance [34] and multi-omics datasets expand [35], these databases will continue to evolve, offering increasingly sophisticated resources for unraveling the complexities of ubiquitination in human health and disease. The ongoing refinement of ubiquitination-related biomarkers and therapeutic targets holds particular promise for advancing precision oncology approaches across diverse cancer types.
Pan-Cancer Patterns of Ubiquitination Gene Alterations
Ubiquitination, a critical post-translational modification, has emerged as a central regulatory mechanism in oncogenesis and cancer progression. The ubiquitin-proteasome system (UPS) orchestrates the precise degradation of cellular proteins, thereby controlling fundamental processes including cell cycle progression, DNA repair, and immune responses [20]. This enzymatic cascade involves the sequential action of ubiquitin-activating (E1), ubiquitin-conjugating (E2), and ubiquitin-ligating (E3) enzymes, which collectively target specific substrates for proteasomal degradation [22]. Mounting evidence demonstrates that dysregulation of ubiquitination pathways constitutes a hallmark across diverse cancer types, making systematic analysis of these alterations imperative for both prognostic assessment and therapeutic development [36] [20]. This review synthesizes current understanding of pan-cancer ubiquitination gene alterations, their prognostic significance, and emerging clinical implications.
Key Ubiquitination-Related Genes with Pan-Cancer Significance
Comprehensive bioinformatics analyses across multiple cancer types have identified several ubiquitination-related genes with consistent alterations and prognostic significance.
Table 1: Key Ubiquitination-Related Genes with Pan-Cancer Alterations
| Gene | Encoded Protein | Primary Alteration Types | Cancer Types with Documented Alterations | Prognostic Association |
|---|---|---|---|---|
| UBE2T | E2 ubiquitin-conjugating enzyme | Amplification, mRNA overexpression | Multiple myeloma, breast cancer, renal cell carcinoma, ovarian cancer, cervical cancer, retinoblastoma, pancreatic cancer [18] [37] | Poor overall survival [18] [37] |
| UBD | Ubiquitin D (FAT10) | Gene amplification, mRNA overexpression, promoter hypomethylation | Gliomas, colorectal carcinoma, hepatocellular carcinoma, breast cancer [19] | Poor prognosis, higher histological grades [19] |
| UBE2C | E2 ubiquitin-conjugating enzyme | mRNA overexpression | Hepatocellular carcinoma, esophageal cancer, breast cancer, gastric cancer [22] | Enhanced tumor proliferation, apoptosis inhibition [22] |
| BUB1B, CHEK1, DNMT1, IRAK1, PRKDC | Various ubiquitination-related proteins | Differential expression | Esophageal squamous cell carcinoma [28] | Significant prognostic value [28] |
| OTUB1 | Deubiquitinating enzyme | Regulatory network alterations | Multiple solid tumors (lung, esophageal, cervical, urothelial, melanoma) [36] | Immunotherapy resistance, poor prognosis [36] |
Table 2: Ubiquitination-Related Risk Models Across Cancer Types
| Cancer Type | Key Genes in Signature | Clinical Applications | Validation Approach |
|---|---|---|---|
| Lung Adenocarcinoma | DTL, UBE2S, CISH, STC1 [26] | Prognosis prediction, immune infiltration assessment, therapy response [26] | TCGA training + 6 external GEO datasets validation [26] |
| Ovarian Cancer | 17-gene signature including FBXO45 [17] | Prognostic stratification, immune microenvironment characterization [17] | TCGA/GTEx training + GSE165808/GSE26712 validation [17] |
| Multiple Solid Tumors | URPS (Ubiquitination-Related Prognostic Signature) [36] | Immunotherapy response prediction, histological subtype classification [36] | 23 datasets across 6 cancer types + single-cell RNA-seq [36] |
| Esophageal Squamous Cell Carcinoma | BUB1B, CHEK1, DNMT1, IRAK1, PRKDC [28] | Prognostic biomarker identification, therapeutic target discovery [28] | TCGA-ESCC, GSE20347, and in-house dataset integration [28] |
Experimental Methodologies for Ubiquitination Gene Analysis
Bioinformatics and Multi-Omics Data Integration
Contemporary ubiquitination research employs sophisticated bioinformatics pipelines integrating data from The Cancer Genome Atlas (TCGA), Genotype-Tissue Expression (GTEx), and Gene Expression Omnibus (GEO) databases [18] [36] [26]. Standard analytical workflows include:
- Differential Expression Analysis: Identification of ubiquitination-related differentially expressed genes (URDEGs) using R packages such as "limma" with thresholds typically set at |log fold change| >0.5 and adjusted p-value <0.05 [28].
- Genetic Alteration Analysis: Assessment of mutation frequencies, copy number variations (CNV), and single nucleotide variants (SNV) using cBioPortal and GSCALite databases [18] [19].
- Survival Analysis: Evaluation of prognostic significance through Kaplan-Meier curves and Cox regression models, with patients stratified by median gene expression or risk scores [18] [26].
- Immune Infiltration Correlation: Investigation of relationships between ubiquitination gene expression and tumor immune microenvironment using algorithms such as TIMER and QUANTISEQ [19].
Functional Validation Experiments
Bioinformatics findings require experimental validation through both in vitro and in vivo approaches:
- Gene Expression Validation: Reverse transcription-quantitative PCR (RT-qPCR) and western blotting to confirm mRNA and protein expression differences between normal and cancer cells [18] [37]. Standard protocols include RNA extraction with TRIzol, cDNA synthesis with PrimeScript RT Master Mix, and qPCR with SYBR Green chemistry [18].
- Cellular Functional Assays: Investigation of ubiquitination gene effects on proliferation (CCK-8 assays), invasion (Transwell assays), and epithelial-mesenchymal transition [18].
- Pathway Analysis: Gene Ontology (GO), Kyoto Encyclopedia of Genes and Genomes (KEGG), and Gene Set Enrichment Analysis (GSEA) to identify biological processes and signaling pathways affected by ubiquitination genes [18] [28].
Ubiquitination-Associated Signaling Pathways in Cancer
Ubiquitination genes converge on several crucial cancer-related pathways:
- Cell Cycle Regulation: UBE2T and UBE2C participate in ubiquitin-mediated proteolysis of cell cycle regulators, with UBE2C specifically cooperating with the anaphase promoting complex/cyclosome (APC/C) E3 complex to polyubiquitinate proteins for degradation [22].
- p53 Signaling Pathway: Multiple E3 ubiquitin ligases, including MDM2, target p53 for degradation, effectively reducing tumor suppressor activity and promoting oncogenesis [22] [20].
- DNA Repair Mechanisms: UBE2T functions in the Fanconi anemia DNA repair pathway, with dysregulation contributing to genomic instability [18] [37].
- Immune Response Regulation: Ubiquitination genes including UBD modulate PD-L1 expression and antigen presentation, thereby influencing antitumor immunity [19].
Table 3: Essential Research Reagents and Databases for Ubiquitination Studies
| Resource Category | Specific Tools/Reagents | Primary Application | Key Features |
|---|---|---|---|
| Bioinformatics Databases | TCGA, GTEx, cBioPortal, GEPIA2.0 [18] [26] [19] | Gene expression analysis, mutation profiling, survival correlation | Multi-omics data integration, user-friendly visualization |
| Experimental Reagents | UBE2T antibody (cat. no. A6853; Abclonal) [18] [37] | Protein detection via western blotting | Specificity for ubiquitination enzymes |
| PrimeScript RT Master Mix, TB Green Premix Ex Taq II [18] [37] | RT-qPCR for gene expression validation | High sensitivity and reproducibility | |
| Cell Line Resources | Cancer Cell Line Encyclopedia (CCLE) [18] [37] | In vitro modeling of ubiquitination gene functions | Comprehensive collection of characterized cancer cell lines |
| Methodological Approaches | LASSO Cox regression [36] [26] | Prognostic model development | Handles high-dimensional data, prevents overfitting |
| Consensus clustering [26] | Molecular subtype identification | Unsupervised pattern recognition in ubiquitination signatures |
Systematic pan-cancer analyses have revealed consistent patterns of ubiquitination gene alterations across diverse malignancies, with UBE2T, UBD, and UBE2C emerging as particularly significant players. These alterations associate consistently with poor prognosis, advanced disease stages, and therapy resistance, highlighting their potential value as both biomarkers and therapeutic targets. The development of multi-gene ubiquitination signatures shows particular promise for prognostic stratification and treatment response prediction. Future research directions should focus on validating these findings in prospective clinical cohorts and developing targeted therapies that exploit specific vulnerabilities created by ubiquitination pathway alterations. As our understanding of the ubiquitin code in cancer deepens, we anticipate increasing translation of these findings into clinical practice, potentially offering new avenues for cancer diagnosis and treatment.
Building Prognostic Signatures: Computational Methods and Clinical Implementation
The advent of large-scale genomic databases has revolutionized cancer research, enabling the identification of molecular patterns across diverse patient populations and tissue types. Among these resources, The Cancer Genome Atlas (TCGA), Gene Expression Omnibus (GEO), and Genotype-Tissue Expression (GTEx) project represent three foundational pillars that provide complementary data for comprehensive oncogenomic investigations. TCGA offers a systematically characterized collection of molecular profiles from thousands of tumor samples across numerous cancer types, generating comprehensive genomic data including RNA sequencing, mutations, DNA methylation, and copy number variations [38]. GEO serves as a public functional genomics data repository supporting MIAME-compliant data submissions, containing array- and sequence-based data from diverse experimental conditions [39]. GTEx complements these resources by providing a comprehensive atlas of gene expression and regulation across diverse normal human tissues from nearly 1,000 individuals, establishing the largest resource for studying human gene expression variation across tissues and individuals [38] [40].
In the specific context of evaluating ubiquitination-related genes in cancer, these databases enable researchers to identify dysregulated ubiquitination pathways, develop prognostic models, and discover potential therapeutic targets. Ubiquitination, a critical post-translational modification process that regulates protein degradation and signaling pathways, has been implicated in various cancers [26]. The integration of data from TCGA, GEO, and GTEx allows for systematic investigation of how ubiquitination-related genes contribute to tumorigenesis, disease progression, and treatment response across different cancer types.
Database Comparative Analysis
Table 1: Core Characteristics of Major Genomic Databases
| Feature | TCGA | GEO | GTEx |
|---|---|---|---|
| Primary Focus | Molecular characterization of human cancer | Curated gene expression data from diverse studies | Normal human tissue gene expression |
| Data Types | RNA-seq, DNA methylation, copy number variation, mutations, clinical data | Array- and sequence-based data from submitted studies | RNA-seq, whole genome sequencing, histology images, eQTL data |
| Sample Types | Primary tumor, solid tissue normal, blood derived normal, metastatic samples | Varies by submitted study (cell lines, tissues, experimental models) | Normal tissues from 54 tissue sites across nearly 1,000 individuals |
| Cancer Applications | Tumor vs. normal comparison, prognostic modeling, multi-omics integration | Method validation, independent cohort verification, meta-analysis | Normal tissue reference, control for tissue-specific expression |
| Ubiquitination Research Utility | Identify cancer-associated URGs, build prognostic models | Validate findings in independent cohorts | Establish normal URG expression baselines |
Table 2: Data Accessibility and Analytical Considerations
| Consideration | TCGA | GEO | GTEx |
|---|---|---|---|
| Access Method | TCGAbiolinks R package, GDC portal | GEOquery R package, GEO2R web tool | UCSC Xena browser, recount3 R package |
| Normalization | Fragments per kilobase million (FPKM) | Varies by platform and submission | Transcripts per million (TPM) |
| Sample Size | ~11,000 patients across 33 cancer types | Millions of samples across thousands of studies | ~1,000 donors across 54 tissue sites |
| Key Limitations | Limited normal tissue samples, batch effects | Heterogeneous data quality, varied platforms | Post-mortem collection, limited clinical data |
| Integration Potential | High with clinical outcomes | High for validation studies | Essential for normal tissue reference |
Experimental Strategies for Ubiquitination Research
Ubiquitination-Related Gene Selection and Processing
Research into ubiquitination-related genes typically begins with compiling a comprehensive gene set from specialized databases such as the iUUCD 2.0 database, which contains ubiquitin-activating enzymes (E1s), ubiquitin-conjugating enzymes (E2s), and ubiquitin-protein ligases (E3s) [26]. In colorectal cancer research, one study derived 2,830 ubiquitination-related genes from this resource [41], while ovarian cancer investigations have utilized 929 ubiquitination-related genes categorized into E1 (8 genes), E2 (39 genes), and E3 (882 genes) [25]. For esophageal squamous cell carcinoma (ESCC), researchers combined ubiquitination-related genes from GeneCards (with relevance scores >5.00), published literature, and the Molecular Signatures Database, resulting in 1,274 unique ubiquitination-related genes [28].
The standard workflow involves identifying differentially expressed genes between tumor and normal tissues using thresholds such as |log fold change| >0.5-1.0 and adjusted p-value <0.05 [28] [25]. The limma R package is commonly employed for differential expression analysis of microarray data, while edgeR or DESeq2 are used for RNA-seq data [28] [25]. The intersection between differentially expressed genes and the ubiquitination-related gene set yields ubiquitination-related differentially expressed genes for further investigation.
Prognostic Model Development
Ubiquitination-related risk models are typically developed using TCGA data as the discovery cohort. For lung adenocarcinoma, one study applied unsupervised clustering, univariate Cox regression, Random Survival Forests, and LASSO Cox regression to identify prognostic ubiquitination-related genes [26]. Similarly, for ovarian cancer, researchers performed univariate Cox analysis followed by LASSO regression and a DEVIANCE test to select 17 genes for their prognostic model [25].
The risk score is calculated using the formula: Risk score = Σ(Coefi × Expri), where Coefi represents the regression coefficient from the multivariate Cox analysis, and Expri represents the gene expression value [26] [25]. Patients are then stratified into high-risk and low-risk groups based on the median risk score. Model performance is validated using external GEO datasets and evaluated through Kaplan-Meier survival analysis, time-dependent receiver operating characteristic curves, and Cox regression analyses adjusting for clinical covariates [26] [41] [25].
Functional Validation and Experimental Follow-up
Experimental validation of bioinformatics predictions strengthens the biological relevance of findings. Standard laboratory reagents and protocols for validating ubiquitination-related gene expression include RNA extraction using reagents such as RNAiso, cDNA synthesis with reverse transcription kits, and quantitative PCR with real-time fluorescence quantitative PCR kits [25]. For functional assays, researchers employ cell culture systems (e.g., DMEM or RPMI 1640 media with fetal bovine serum), transfection reagents (e.g., Lipofectamine 2000), and Western blotting reagents including RIPA lysis buffer, protease inhibitors, and ECL chemiluminescent detection [25].
Table 3: Essential Research Reagents for Ubiquitination Studies
| Reagent Category | Specific Examples | Research Application |
|---|---|---|
| Cell Culture | DMEM, RPMI 1640, Fetal Bovine Serum, Trypsin | Maintenance and propagation of cancer cell lines |
| Molecular Biology | RNAiso Reagent, Reverse Transcription Kits, Quantitative PCR Kits | Gene expression analysis and validation |
| Protein Analysis | RIPA Lysis Buffer, Protease Inhibitors, ECL Chemiluminescent Liquid | Protein detection and ubiquitination assessment |
| Functional Assays | Crystal Violet Staining, Paraformaldehyde, Transfection Reagents | Cellular proliferation, migration, and invasion assays |
| Key Antibodies | FBXO45, WNT1, β-catenin, c-myc, GAPDH | Pathway analysis and target validation |
Integrated Data Mining Workflow
Database Integration Workflow for Ubiquitination Research
Analytical Methodologies and Technical Approaches
Differential Expression Analysis
The identification of differentially expressed ubiquitination-related genes employs distinct statistical approaches depending on data types. For microarray data from GEO datasets, the limma R package is commonly used with precision weights (vooma) for linear modeling and empirical Bayes moderation for variance estimation [28] [42]. For RNA-seq data from TCGA and GTEx, researchers typically utilize edgeR or DESeq2 packages that implement negative binomial distributions to model count data [25]. The integration of normal tissue expression data from GTEx with TCGA tumor data enhances the statistical power for identifying cancer-associated ubiquitination-related genes, particularly for cancers with limited normal tissue samples in TCGA [43].
Multiple testing correction is crucial in these analyses, with the Benjamini-Hochberg procedure commonly applied to control the false discovery rate. Thresholds for significance typically include adjusted p-values <0.05-0.01 and absolute log2 fold changes >0.5-1.0, depending on the specific study design and sample size [28] [25]. For chromatin accessibility data integration, tools like the "ChIPseeker" package annotate ATAC-seq peaks to genes, which are then intersected with ubiquitination-related differentially expressed genes [43].
Advanced Machine Learning Applications
Machine learning algorithms have become integral to ubiquitination-related cancer research. Random Survival Forests provide robust handling of high-dimensional data and complex interactions, with parameters typically set to ntree=100-500 and variable importance calculated through permutation [26] [43]. LASSO Cox regression performs feature selection and regularization to enhance model interpretability and prevent overfitting, with the optimal penalty parameter (λ) determined through 10-fold cross-validation [26] [41].
For tissue classification and biomarker discovery, Random Forest classifiers with balanced class weights address dataset imbalance, while t-distributed Stochastic Neighbor Embedding (t-SNE) visualizes high-dimensional integrin expression patterns with perplexity parameters between 30-50 [44]. These approaches have demonstrated high accuracy in distinguishing tissue origins and disease status based on ubiquitination-related gene expression patterns.
Multi-Omics Data Integration
Advanced studies increasingly integrate multiple data types to comprehensively understand ubiquitination in cancer. One lung adenocarcinoma study combined ATAC-seq data measuring chromatin accessibility with RNA-seq data to identify consensus genes affected by both epigenetic and transcriptional regulation [43]. The random forest and LASSO algorithms selected predictive genes, followed by artificial neural network construction with five hidden layers for model development.
Single-cell RNA sequencing data further enhances resolution by identifying cell-type-specific expression of ubiquitination-related genes. Processing pipelines typically include quality control (excluding cells with <200 genes or >15% mitochondrial genes), normalization using the LogNormalize method, identification of highly variable genes, and clustering based on principal components [25]. This approach reveals how ubiquitination-related genes vary across cell populations within tumors.
The strategic integration of TCGA, GEO, and GTEx databases provides a powerful framework for investigating ubiquitination-related genes in cancer research. Each database offers unique strengths—TCGA provides comprehensive molecular profiling of tumors, GEO enables validation across diverse cohorts, and GTEx establishes normal tissue expression baselines. The experimental strategies and analytical workflows outlined herein facilitate the development of robust prognostic models, identification of novel therapeutic targets, and advancement of personalized cancer treatment approaches based on ubiquitination pathways. As these databases continue to expand and novel analytical methods emerge, researchers will uncover increasingly sophisticated insights into the complex roles of ubiquitination in cancer biology.
Bioinformatic Pipelines for Identifying Prognostic UbRG Signatures
Ubiquitination, a vital post-translational modification, has emerged as a crucial regulatory mechanism in cancer biology, governing cellular processes including cell cycle progression, DNA repair, apoptosis, and immune responses [28]. The ubiquitin-proteasome system (UPS), comprising ubiquitin-activating enzymes (E1), ubiquitin-conjugating enzymes (E2), ubiquitin ligases (E3), and deubiquitinating enzymes, represents a sophisticated regulatory network whose disruption contributes significantly to tumorigenesis and cancer progression [26] [45]. In recent years, bioinformatic approaches have enabled researchers to systematically analyze ubiquitination-related genes (UbRGs) across multiple cancer types, leading to the development of prognostic signatures that stratify patient risk and inform therapeutic decisions [25] [26].
The clinical imperative for these signatures is substantial. Across multiple cancer types—including esophageal squamous cell carcinoma (ESCC), ovarian cancer, lung adenocarcinoma (LUAD), head and neck squamous cell carcinoma (HNSCC), and prostate cancer—studies have consistently demonstrated that UbRG-based models provide independent prognostic value beyond conventional clinical parameters [28] [46] [47]. These signatures not only predict survival outcomes but also offer insights into tumor microenvironment composition, mutation burden, and potential responses to chemotherapy, targeted therapy, and immunotherapy [26] [45] [48]. This comparative guide examines the leading bioinformatic pipelines for identifying prognostic UbRG signatures, their methodological frameworks, performance characteristics, and clinical applications.
Computational Methodologies for UbRG Signature Development
Data Acquisition and Preprocessing
The foundation of any robust UbRG signature begins with comprehensive data acquisition and rigorous preprocessing. Researchers typically obtain transcriptomic data and clinical information from public repositories such as The Cancer Genome Atlas (TCGA) and Gene Expression Omnibus (GEO) [28] [26]. Ubiquitination-related gene sets are compiled from specialized databases including the Ubiquitin and Ubiquitin-like Conjugation Database (UUCD), iUUCD 2.0, GeneCards, and the Molecular Signatures Database (MSigDB) [25] [26] [48].
A critical preprocessing step involves differential expression analysis between tumor and normal tissues using R packages like limma or edgeR, applying thresholds such as |log fold change (FC)| > 0.5-1.0 and adjusted p-value (adj. P) < 0.05 [28] [25]. For studies focusing on survival outcomes, patients with survival times less than 30-90 days are typically excluded to avoid perioperative mortality bias [26] [45]. Dataset stratification into training and validation cohorts ensures model robustness, with common splits ranging from 50-50 to 70-30 ratios [46] [48].
Table 1: Primary Data Sources for Ubiquitination-Related Gene Signature Development
| Data Category | Specific Sources | Common Applications |
|---|---|---|
| Transcriptomic Data | TCGA, GEO (GSE20347, GSE13213, GSE30219, etc.) | Differential expression analysis, model training and validation |
| Ubiquitin-Related Gene Databases | UUCD, iUUCD 2.0, GeneCards, MSigDB, Published Literature | Reference ubiquitination-related gene sets |
| Clinical Data | TCGA Clinical Data Resource, GEO Supplementary Data | Survival analysis, clinical correlation studies |
| Mutation Data | cBioPortal, TCGA Mutation Annotation Files | Tumor mutation burden analysis, mutation landscape characterization |
Signature Construction Approaches
Conventional Risk Score Models
The most prevalent approach for UbRG signature development involves constructing risk score models based on multivariable Cox regression coefficients. This method follows the formula:
Risk score = Σ(Expression of Genei × Coefficienti) [26] [45]
The construction typically employs a multi-step statistical process: (1) univariate Cox regression to identify survival-associated UbRGs; (2) least absolute shrinkage and selection operator (LASSO) Cox regression to prevent overfitting and select the most informative genes; (3) multivariable Cox regression to calculate coefficients for the final model [26] [45]. Patients are then stratified into high-risk and low-risk groups based on median risk scores or optimized cut-off values.
This approach has demonstrated prognostic utility across multiple malignancies. In lung adenocarcinoma, a 4-gene signature (DTL, UBE2S, CISH, and STC1) effectively stratified patients with significantly different overall survival (hazard ratio [HR] = 0.54, 95% confidence interval [CI]: 0.39-0.73, p < 0.001) [26]. Similarly, in esophageal squamous cell carcinoma, a 5-gene signature (BUB1B, CHEK1, DNMT1, IRAK1, and PRKDC) showed significant prognostic value [28].
Gene-Pair Signatures
An innovative alternative to conventional risk scoring employs ubiquitin-related gene pairs (UbRGPs) that compare relative expression levels within individual samples [46] [48]. This method generates a binary matrix where each gene pair receives a score of 1 if the first gene's expression exceeds the second, and 0 otherwise. The significant advantage of this approach is its elimination of batch effects and normalization requirements, as it relies on relative rather than absolute expression values [46].
For lung adenocarcinoma, a 6-UbRGP signature demonstrated robust prognostic performance, with the high-risk group showing significantly worse overall survival and distinct tumor microenvironment characteristics [48]. The risk score calculation follows the same principles as conventional models but uses gene-pair scores rather than direct expression values.
Diagram 1: Ubiquitin-Related Gene Pair (UbRGP) Signature Development Workflow. This approach transforms absolute gene expression values into relative comparisons within each sample, eliminating batch effects and normalization requirements.
Unsupervised Clustering Approaches
Beyond supervised risk modeling, unsupervised clustering methods like ConsensusClusterPlus identify molecular subtypes based on UbRG expression patterns [26] [48]. This approach reveals intrinsic biological subgroups without prior survival information, potentially uncovering novel disease classifications. In lung adenocarcinoma, this method has identified distinct ubiquitination subtypes with differential mutation frequencies and tumor mutation burdens [26].
Performance Comparison of UbRG Signatures Across Cancers
The prognostic accuracy of UbRG signatures has been extensively validated across cancer types. Performance metrics typically include time-dependent receiver operating characteristic (ROC) curves, Kaplan-Meier survival analysis, and concordance indices (C-index) [25] [46].
Table 2: Performance Metrics of UbRG Signatures Across Cancer Types
| Cancer Type | Signature Genes | AUC (1-year) | AUC (3-year) | AUC (5-year) | Hazard Ratio (High vs. Low Risk) |
|---|---|---|---|---|---|
| Ovarian Cancer [25] | 17-gene signature | 0.703 | 0.704 | 0.705 | Significant (P < 0.05) |
| Lung Adenocarcinoma [26] | DTL, UBE2S, CISH, STC1 | NR | NR | NR | 0.54 (95% CI: 0.39-0.73) |
| Head and Neck Squamous Cell Carcinoma [46] | 11-gene pair signature | 0.744 | 0.852 | 0.861 | Significant (P < 0.001) |
| Esophageal Squamous Cell Carcinoma [28] | BUB1B, CHEK1, DNMT1, IRAK1, PRKDC | NR | NR | NR | Significant prognostic value |
NR = Not Reported
Multivariate Cox regression analyses consistently demonstrate that UbRG signatures serve as independent prognostic factors beyond conventional clinical parameters like age, stage, and grade [46] [45]. For instance, in head and neck squamous cell carcinoma, an 11-gene pair signature remained significantly associated with overall survival after adjusting for clinical covariates [46].
Functional Characterization of UbRG Signatures
Biological Pathway Associations
UbRG signatures consistently associate with critical cancer-related pathways through functional enrichment analyses. Gene Ontology (GO) and Kyoto Encyclopedia of Genes and Genomes (KEGG) analyses frequently identify cell cycle regulation, immune response, protein modification, and catabolic processes as significantly enriched [28] [45].
In esophageal squamous cell carcinoma, the prognostic UbRGs (BUB1B, CHEK1, DNMT1, IRAK1, and PRKDC) play key roles in essential processes including cell cycle and immune response [28]. Similarly, in lung adenocarcinoma, ubiquitination-related signatures associate with cell cycle progression, DNA replication, and p53 signaling pathways [26] [45].
Tumor Microenvironment and Immune Landscape
UbRG signatures provide remarkable insights into tumor microenvironment composition and immune landscape. In ovarian cancer, the low-risk group defined by a 17-gene UbRG signature showed significantly higher levels of CD8+ T cells, M1 macrophages, and follicular helper T cells, suggesting a more robust anti-tumor immune response [25]. High-risk patients exhibited more mutations in MUC17 and LRRK2, while low-risk patients had more RYR2 mutations [25].
In lung adenocarcinoma, UbRG signatures correlate with tumor mutation burden (TMB), tumor neoantigen load (TNB), and PD-1/PD-L1 expression levels [26]. High-risk patients typically demonstrate increased TMB, TNB, and immune checkpoint expression, suggesting potential responsiveness to immunotherapy [26] [45].
Diagram 2: Tumor Microenvironment (TME) and Therapeutic Analysis Framework. UbRG signatures enable comprehensive characterization of the immune landscape and mutation profile, informing potential therapeutic strategies.
Experimental Validation and Clinical Translation
Laboratory Validation Approaches
While bioinformatic discoveries provide compelling associations, experimental validation remains crucial for establishing biological causality. Common validation approaches include:
- Reverse Transcription Quantitative PCR (RT-qPCR): Used to verify differential expression of signature genes in independent patient samples [28] [26].
- Cell Culture and Transfection: Manipulation of signature gene expression in cancer cell lines to assess functional impacts on proliferation, invasion, and migration [25].
- Western Blot Analysis: Examination of protein expression and pathway alterations following genetic manipulation [25].
- Drug Sensitivity Assays: Assessment of how signature genes influence response to chemotherapeutic agents and targeted therapies [45].
For example, in ovarian cancer, FBXO45 was experimentally validated as a key E3 ubiquitin ligase promoting cancer growth, spread, and migration via the Wnt/β-catenin pathway [25]. Similarly, in lung adenocarcinoma, RT-qPCR validation confirmed the differential expression of signature genes (DTL, UBE2S, CISH, and STC1) in independent patient samples [26].
Therapeutic Implications and Drug Prediction
UbRG signatures show significant promise for guiding therapeutic decisions. Several studies have correlated risk scores with drug sensitivity, enabling potential treatment stratification [26] [45]. In lung adenocarcinoma, the high-risk group showed lower IC50 values for various chemotherapeutic drugs, suggesting increased sensitivity [26]. Similarly, UbRG signatures can predict responses to immune checkpoint inhibitors through assessment of TMB, TNB, and immune cell infiltration [45] [48].
The emergence of proteolysis-targeting chimeras (PROTACs) that specifically target ubiquitin enzymes further highlights the clinical relevance of these signatures [25]. PROTACs offer advantages including reduced dosage frequency, enhanced therapeutic duration, minimized toxicity, and ability to overcome drug resistance [25]. UbRG signatures could potentially identify patients most likely to benefit from these novel therapeutic approaches.
Table 3: Key Research Reagents and Computational Tools for UbRG Signature Development
| Resource Type | Specific Tools/Reagents | Application in UbRG Research |
|---|---|---|
| Bioinformatic Tools | limma R package, edgeR, ConsensusClusterPlus, ESTIMATE, CIBERSORT | Differential expression analysis, clustering, tumor microenvironment estimation |
| Statistical Packages | survival R package, glmnet (LASSO), timeROC, randomForestSRC | Survival analysis, feature selection, model validation |
| Ubiquitin Databases | UUCD, iUUCD 2.0, GeneCards | Reference ubiquitination-related gene sets |
| Laboratory Reagents | RT-qPCR kits (Takara RR064A), RNAiso Reagent (Takara), Lipo2000 transfection reagent | Experimental validation of signature genes |
| Therapeutic Databases | CellMiner, GDSC, PROTACdb | Drug sensitivity prediction, targeted therapy development |
Bioinformatic pipelines for identifying prognostic UbRG signatures have evolved into sophisticated frameworks that integrate multi-omics data, advanced statistical modeling, and experimental validation. These signatures provide valuable insights into cancer biology, prognosis, and therapeutic opportunities across diverse malignancies. The consistent demonstration of independent prognostic value, coupled with associations to therapy response, positions UbRG signatures as promising tools for advancing personalized cancer care. Future directions will likely focus on standardized analytical pipelines, multi-cancer meta-analyses, and integration with proteomic data to further enhance clinical utility.
Multivariate Cox Regression and LASSO Analysis for Signature Development
In the evolving landscape of cancer research, the development of robust prognostic signatures has become indispensable for advancing personalized medicine. The integration of multivariate Cox regression with LASSO (Least Absolute Shrinkage and Selection Operator) analysis represents a powerful statistical framework for identifying optimal gene signatures from high-dimensional transcriptomic data. This analytical approach enables researchers to distill complex biological information into clinically applicable models that can predict patient survival, therapeutic response, and disease progression with remarkable accuracy. The methodology is particularly valuable for investigating ubiquitination-related genes, which play crucial regulatory roles in cancer pathogenesis through post-translational modification of proteins involved in cell cycle control, DNA repair, and immune recognition.
This comparison guide objectively evaluates how this analytical framework has been implemented across different cancer types, focusing on methodological approaches, performance metrics, and clinical applicability. By examining diverse applications—from ovarian cancer to diffuse large B-cell lymphoma—we aim to provide researchers with a comprehensive understanding of best practices and considerations for developing prognostic signatures that can ultimately inform clinical decision-making and drug development strategies.
Comparative Analysis of Prognostic Signatures
Table 1: Comparison of Prognostic Signatures Across Cancer Types
| Cancer Type | Signature Genes | Sample Size | Validation Cohorts | Performance (AUC) | Biological Focus |
|---|---|---|---|---|---|
| Ovarian Cancer | 17-gene signature | 376 tumors + 88 normal [17] | GSE165808, GSE26712 [17] | 1-year: 0.703, 3-year: 0.704, 5-year: 0.705 [17] | Ubiquitination-related genes |
| DLBCL | CDC34, FZR1, OTULIN | 1,800 samples [49] | GSE181063 [49] | Significant survival stratification (P<0.05) [49] | Ubiquitination-survival associated DEGs |
| Colon Cancer | 9-gene G2M signature | TCGA-COAD (n=451) [50] | GSE39582, GSE17536, GSE17537 [50] | Significant survival difference (P<0.05) [50] | G2M cell cycle genes |
| Colorectal Cancer | 3-gene ORGSig | 64 oxaliplatin-treated [51] | GSE87211 [51] | Training: 1-year: 0.791, 3-year: 0.767 [51] | Oxaliplatin resistance |
| Colorectal Cancer | 9-gene DAMP signature | 591 cancer and para-carcinoma [52] | AC-ICAM cohort [52] | Relatively high AUC value [52] | Damage-associated molecular patterns |
Table 2: Methodological Approaches Across Studies
| Study Focus | Variable Selection Method | Validation Approach | Clinical Integration | Additional Analyses |
|---|---|---|---|---|
| Ovarian Cancer Ubiquitination | COX univariate + LASSO + DEVIANCE test [17] | External datasets + experimental validation [17] | Nomogram for survival probability [17] | Immune infiltration, gene mutations, FBXO45 pathway [17] |
| DLBCL Ubiquitination | Univariate Cox + LASSO Cox [49] | External dataset GSE181063 [49] | Risk stratification based on median score [49] | Immune microenvironment, drug sensitivity, single-cell analysis [49] |
| Colon Cancer G2M | Univariate Cox + LASSO [50] | Multiple GEO datasets [50] | Nomogram with stage, age, gender [50] | Multi-omics analysis, immune infiltration, drug sensitivity [50] |
| CRC Oxaliplatin Resistance | Univariate Cox + LASSO + stepwise multivariate Cox [51] | GEO cohort + other cancer types [51] | Nomogram for 1-, 2-, 3-year PFS [51] | WGCNA, TME analysis, TNFAIP2 functional validation [51] |
| CRC DAMP Signature | Univariate Cox + Lasso Cox + multivariate Cox [52] | cBioportal database [52] | Nomogram incorporating RiskScore [52] | Immune infiltration, TIDE score, drug sensitivity [52] |
Methodological Framework
Core Analytical Pipeline
The development of prognostic signatures follows a systematic workflow that integrates statistical learning with biological validation. The standard approach begins with differential expression analysis to identify genes with significant expression changes between normal and tumor tissues. For ubiquitination-related signatures in ovarian cancer, researchers identified 162 co-expressed genes by intersecting differentially expressed genes with a curated set of 929 ubiquitination-related genes from the UUCD database [17].
The variable selection process typically employs univariate Cox regression as an initial filter to identify genes with potential prognostic value, followed by LASSO regression to address multicollinearity and prevent overfitting. The LASSO method applies an L1 penalty that shrinks coefficients of less relevant variables to zero, effectively selecting the most predictive features. In the DLBCL study, this approach narrowed 7 ubiquitination-survival-related differentially expressed genes down to 3 key genes (CDC34, FZR1, and OTULIN) with non-zero coefficients [49].
The final signature development incorporates multivariate Cox regression to assign appropriate weights to each selected gene, creating a risk score formula. For example, the ovarian cancer ubiquitination signature calculates risk score as the sum of each gene's expression multiplied by its regression coefficient [17]. Patients are then stratified into high- and low-risk groups based on the median risk score for survival analysis.
Advanced Methodological Innovations
Recent studies have implemented sophisticated enhancements to improve signature robustness. Some approaches have integrated multiple machine learning algorithms beyond the standard Cox-LASSO framework. One colorectal cancer study evaluated 93 different algorithmic combinations, incorporating methods like elastic network, CoxBoost, and survival-SVM to identify the optimal strategy based on the highest average C-index across validation cohorts [53].
The multi-omics integration represents another advancement, with studies incorporating not only transcriptomic data but also genomic variations, miRNA regulation, and protein interactions. The G2M signature study in colon cancer employed multi-omics analysis exploring protein expression, miRNA regulation, protein interactions, genomic variations, and drug sensitivity [50].
Validation frameworks have also become increasingly rigorous, typically employing both internal cross-validation and external validation in independent cohorts. The most robust studies supplement computational validation with experimental functional validation, as demonstrated by the ovarian cancer study that conducted in vitro experiments to confirm the role of FBXO45 in promoting cancer progression via the Wnt/β-catenin pathway [17].
Experimental Protocols
Ubiquitination Signature Development Protocol
Data Collection and Preprocessing
- Obtain RNA-seq data and clinical information from TCGA and GTEx databases [17]
- Identify differentially expressed genes using edgeR package with threshold |logFC| ≥ 1 and adjusted p-value < 0.01 [17]
- Curate ubiquitination-related gene set from UUCD database (8 E1, 39 E2, 882 E3 genes) [17]
Signature Construction
- Perform univariate Cox regression to identify prognostic ubiquitination-related genes (p < 0.05) [17]
- Apply LASSO regression with 10-fold cross-validation using glmnet package to select optimal genes [25]
- Conduct multivariate Cox regression to assign coefficients and calculate risk score: Risk score = Σ(Coefi × Expressioni) [17]
- Stratify patients into high/low-risk groups based on median risk score
Validation and Functional Analysis
- Validate signature in external datasets (e.g., GSE165808, GSE26712 for ovarian cancer) [17]
- Analyze immune infiltration using CIBERSORT or ESTIMATE algorithms [17] [49]
- Perform gene mutation analysis using "maftools" package [17]
- Conduct experimental validation through cell culture, transfection, and functional assays [17]
Advanced Machine Learning Protocol
Multi-Algorithm Framework
- Acquire and preprocess data from TCGA and GEO datasets, removing batch effects [53]
- Calculate immune enrichment scores using ssGSEA with 29 immune gene sets [53]
- Identify immune subgroups using ConsensusClusterPlus with 1,000 repetitions [53]
- Screen differentially expressed genes between immune subgroups (|log2FC| > 0.585, FDR < 0.05) [53]
Machine Learning Optimization
- Evaluate 93 algorithmic combinations including Enet, LASSO, Ridge, stepwise Cox, CoxBoost, plsRcox, SuperPC, GBM, and survival-SVM [53]
- Perform 10-fold cross-validation in training cohort [53]
- Select optimal model based on highest average C-index across multiple validation cohorts [53]
- Validate signature in independent datasets and compare performance with existing signatures [53]
Visualization of Analytical Workflows
Ubiquitination Signature Development Pathway
Figure 1: Ubiquitination Signature Development Workflow - This diagram illustrates the comprehensive analytical pipeline for developing ubiquitination-related prognostic signatures, from initial data collection through validation and experimental confirmation.
LASSO Cox Regression Mechanism
Figure 2: LASSO Cox Regression Mechanism - This diagram visualizes the mathematical and computational framework of LASSO Cox regression, highlighting how it balances model complexity with predictive accuracy through regularization and cross-validation.
Research Reagent Solutions
Table 3: Essential Research Reagents and Resources
| Reagent/Resource | Application | Specifications | Source/Reference |
|---|---|---|---|
| TCGA-OV Data | Transcriptomic analysis | 376 tumor + 88 normal ovarian tissues [17] | TCGA Database |
| GTEx Data | Normal tissue reference | 88 normal ovarian tissues [17] | GTEx Database |
| UUCD Database | Ubiquitination gene curation | 929 ubiquitination-related genes [17] | http://uucd.biocuckoo.org/ |
| edgeR Package | Differential expression analysis | [17] | |
| glmnet Package | LASSO regression implementation | [17] [51] | |
| GEO Datasets | External validation | GSE165808, GSE26712, GSE181063, etc. | GEO Database |
| ESTIMATE Algorithm | Tumor microenvironment scoring | [17] [52] | |
| CIBERSORT | Immune cell infiltration analysis | [53] [49] | |
| DMEM | Cell culture | 12800017 | Gibco [17] |
| RNAiso Reagent | RNA extraction | 9108 | Takara [17] |
| Real-time PCR Kit | Gene expression validation | RR064A | Takara [17] |
| Lipo2000 | Transfection reagent | 31985-062 | Thermo fisher [17] |
The integration of multivariate Cox regression with LASSO analysis has established itself as a robust methodological framework for developing prognostic signatures across diverse cancer types. This comparative analysis demonstrates that while the core analytical approach remains consistent, implementation specifics must be tailored to the biological context and clinical application. The most successful signatures incorporate multi-level validation, including external cohorts and functional experiments, to ensure clinical relevance and biological plausibility.
For ubiquitination-related signatures specifically, the emerging evidence highlights their value not only in prognosis but also in revealing novel therapeutic opportunities, particularly in the context of PROTAC-based therapies that target the ubiquitin-proteasome system. As the field advances, the integration of multi-omics data and machine learning algorithms promises to further enhance the precision and clinical utility of these prognostic tools, ultimately supporting more personalized and effective cancer management strategies.
Construction and Validation of UbRG-Based Risk Models
Within the field of oncology, the pursuit of robust prognostic biomarkers is a cornerstone of personalized medicine. Recent research has increasingly focused on the ubiquitination process, a vital post-translational modification that regulates protein degradation and numerous cellular signaling pathways. The construction and validation of risk models based on ubiquitination-related genes (UbRGs) have emerged as a powerful strategy for predicting patient outcomes, understanding tumor biology, and identifying potential therapeutic targets. This review provides a systematic comparison of UbRG-based risk models across various cancer types, evaluating their prognostic performance, methodological frameworks, and clinical applicability to establish their collective value in cancer research.
UbRG Risk Models Across Different Cancers
Ubiquitination-related risk models have been developed for a diverse array of malignancies. The table below summarizes the key characteristics and performance metrics of recently published models.
Table 1: Comparison of UbRG-Based Prognostic Risk Models in Various Cancers
| Cancer Type | Key UbRG Biomarkers | Model Performance (AUC) | Validation Cohorts | Clinical Utility |
|---|---|---|---|---|
| Head and Neck Squamous Cell Carcinoma (HNSCC) [46] | 11-Gene Pair Signature | 1-year: 0.744, 3-year: 0.852, 5-year: 0.861 | TCGA (Internal training/testing) | Independent prognostic factor; guides chemotherapy drug selection. |
| Lung Adenocarcinoma (LUAD) [26] | DTL, UBE2S, CISH, STC1 | Hazard Ratio (HR) = 0.58 (in validation) | 6 external GEO datasets | Predicts response to immunotherapy and chemotherapy; correlates with TMB and TME. |
| Ovarian Cancer (OV) [25] | 17-Gene Signature (incl. FBXO45) | 1-year: 0.703, 3-year: 0.704, 5-year: 0.705 | GSE165808, GSE26712 | Reflects immune microenvironment (CD8+ T cells, M1 macrophages); linked to Wnt/β-catenin pathway. |
| Cervical Cancer (CC) [16] | MMP1, RNF2, TFRC, SPP1, CXCL8 | AUC > 0.6 for 1/3/5 years | Self-seq, TCGA-GTEx, GSE52903 | Associated with infiltration of memory B cells and M0 macrophages; differential immune checkpoint expression. |
Core Methodological Framework for Model Construction
The construction of a UbRG-based risk model follows a structured bioinformatics pipeline, which ensures robustness and reliability. The workflow below illustrates the key stages from data collection to model application.
Detailed Experimental Protocols
Data Acquisition and UbRG Selection
- Data Sources: Transcriptomic data and corresponding clinical information (e.g., survival time, status, stage) are primarily sourced from public repositories such as The Cancer Genome Atlas (TCGA) and the Gene Expression Omnibus (GEO) [46] [26] [16]. For proteomic models, data may be obtained from The Cancer Proteome Atlas (TCPA) [54] [55].
- UbRG Curation: Ubiquitination-related genes are systematically compiled from specialized databases like GeneCards (using a relevance score threshold) or the iUUCD 2.0 database, which catalogs E1 ubiquitin-activating enzymes, E2 ubiquitin-conjugating enzymes, and E3 ubiquitin ligases [46] [26].
Signature Construction via LASSO Cox Regression
This is a critical step for feature selection and model building to prevent overfitting.
- Purpose: To identify the most predictive UbRGs from a large pool of candidates and build a parsimonious model [46] [26] [16].
- Protocol:
- Input: A matrix of expression values for candidate UbRGs derived from univariate Cox analysis (p < 0.05).
- Algorithm: A LASSO (Least Absolute Shrinkage and Selection Operator) Cox regression model is fitted using the
glmnetpackage in R. This method applies a penalty term (lambda) that shrinks the coefficients of less important genes to zero, effectively performing variable selection [26] [16]. - Cross-Validation: A 10-fold cross-validation is typically performed (e.g., 1000 cycles) to determine the optimal value of lambda (λ) that minimizes the model's deviance [54].
- Output: A final set of prognostic UbRGs and their regression coefficients (β).
Risk Score Calculation and Patient Stratification
Formula: The risk score for each patient is calculated using the following equation [26] [16]:
( \text{Risk score} = \sum{i=1}^{N} (Coefi \times Exp_i) )
Where ( Coefi ) is the regression coefficient from the multivariate Cox or LASSO analysis for gene *i*, and ( Expi ) is the expression level of gene i in the sample.
- Stratification: Patients are divided into high-risk and low-risk groups based on the median risk score or an optimal cut-off value determined from the training data [46] [55].
Model Validation and Evaluation
- Validation Cohorts: The model's performance is rigorously tested. This includes internal validation (e.g., splitting the TCGA cohort into training and test sets) and, more importantly, external validation using independent datasets from GEO or other sources [26] [16].
- Performance Metrics:
- Survival Analysis: Kaplan-Meier (K-M) curves and log-rank tests are used to compare overall survival (OS) between the high-risk and low-risk groups. A p-value < 0.05 is considered statistically significant [46] [25].
- Predictive Accuracy: Time-dependent Receiver Operating Characteristic (ROC) curves are generated, and the Area Under the Curve (AUC) is calculated for 1, 3, and 5 years to evaluate the model's discrimination ability [46] [16].
- Prognostic Independence: Univariate and multivariate Cox regression analyses are conducted to determine if the risk score is an independent prognostic factor when adjusted for other clinical variables like age, gender, and tumor stage [46] [55].
Biological and Clinical Correlations
Association with Tumor Immunity
A consistent finding across multiple UbRG models is their strong correlation with the tumor immune microenvironment, which has critical implications for immunotherapy. The diagram below outlines the common immune patterns associated with high-risk and low-risk patient groups.
- HNSCC: The high-risk group showed significantly higher infiltration of M2 macrophages (which are pro-tumoral) and a higher tumor mutation burden (TMB) [46].
- Lung Adenocarcinoma: The high-risk group was characterized by higher TMB, higher tumor neoantigen burden (TNB), and elevated expression of PD-1 and PD-L1 immune checkpoints, suggesting a potential vulnerability to immunotherapy [26].
- Ovarian Cancer: The low-risk group exhibited higher levels of anti-tumor immune cells, including CD8+ T cells, M1 macrophages, and follicular helper T cells [25].
Therapeutic Implications
UbRG signatures demonstrate significant potential in guiding treatment strategies:
- Chemotherapy: Studies in HNSCC and LUAD have analyzed the IC50 values of common chemotherapy drugs, revealing distinct sensitivities between risk groups. This allows for the recommendation of specific chemotherapeutic agents tailored to a patient's UbRG risk profile [46] [26].
- Immunotherapy: The association between high-risk scores and an immunosuppressive microenvironment with elevated immune checkpoint expression (as seen in LUAD) provides a strong rationale for selecting patients who are more likely to benefit from PD-1/PD-L1 blockade therapy [26].
- Targeted Therapy: The functional validation of specific UbRGs, such as FBXO45 in ovarian cancer promoting malignancy via the Wnt/β-catenin pathway, directly points to novel targets for drug development, including the potential for PROTACs (Proteolysis-Targeting Chimeras) [25].
Table 2: Key Reagents and Resources for UbRG Model Development and Validation
| Category | Specific Item / Database | Function in Research | Example Use |
|---|---|---|---|
| Data Resources | TCGA Database | Provides primary transcriptome and clinical data for model training. | Used as primary cohort in HNSCC, LUAD, OV studies [46] [25] [26]. |
| GEO Database | Source of independent datasets for external model validation. | Validation in GSE30219, GSE37745 for LUAD; GSE52903 for CC [26] [16]. | |
| GeneCards / iUUCD 2.0 | Definitive sources for curating lists of ubiquitination-related genes (UbRGs). | Used to obtain 1058 UbRGs for HNSCC study; 966 URGs for LUAD study [46] [26]. | |
| Laboratory Reagents | RNAiso Reagent (Takara) | For total RNA extraction from tissue samples. | Used in RNA extraction for RT-qPCR validation in ovarian cancer study [25]. |
| Real-time PCR Kits (Takara) | For quantitative validation of gene expression (RT-qPCR). | Used to confirm expression of key genes like FBXO45 in OV [25]. | |
| Primary Antibodies (e.g., Abcam, CST) | For protein-level validation via Western Blot or IHC. | IHC validation of CDH3 and EIF4G1 in breast cancer tissues [55]. | |
| Software & Algorithms | R packages: glmnet, survival, timeROC |
Core statistical analysis, including LASSO Cox regression and survival analysis. | Used for model construction and ROC analysis across all cited studies [46] [26] [16]. |
| CIBERSORT | Algorithm for deconvoluting immune cell infiltration from transcriptome data. | Analyzed immune cell infiltration in cervical cancer risk groups [16]. |
The construction and validation of UbRG-based risk models represent a significant advancement in cancer prognostics. The consistent methodological framework—centered on feature selection via LASSO Cox regression—has produced models with strong and validated predictive power across multiple cancer types. These models transcend simple outcome prediction by providing deep insights into the tumor immune microenvironment and practical guidance for chemotherapy, immunotherapy, and targeted therapy. The integration of UbRG signatures with clinical nomograms further enhances their potential for individualized patient management. Future research should focus on the functional characterization of individual UbRGs within these signatures and the transition of these models into prospective clinical trials to fully realize their promise in precision oncology.
In the evolving landscape of cancer prognosis, nomograms have emerged as indispensable statistical tools that integrate multiple clinical and molecular variables to generate individualized survival predictions. These visual predictive models represent a significant advancement beyond traditional staging systems by quantifying the contribution of specific risk factors to produce numerical probabilities of clinical outcomes. The integration of molecular signatures, particularly ubiquitination-related genes (URGs), has further refined prognostic accuracy across multiple cancer types. Ubiquitination, a crucial post-translational modification regulating protein degradation and cellular homeostasis, has recently been identified as a significant factor in tumorigenesis and treatment response. This review comprehensively evaluates the development, validation, and clinical application of URG-based nomograms, providing researchers with methodological frameworks and comparative analyses to guide future prognostic model development in oncology.
Methodological Frameworks for Nomogram Development
Core Statistical Principles and Construction Workflows
Nomogram development follows rigorous statistical protocols to ensure predictive accuracy and clinical applicability. The foundational process begins with patient cohort identification from cancer databases such as The Cancer Genome Atlas (TCGA) and Surveillance, Epidemiology, and End Results (SEER), followed by random splitting into training and validation sets, typically in a 7:3 ratio [56] [57]. Variable selection employs least absolute shrinkage and selection operator (LASSO) regression analysis to identify the most relevant prognostic predictors while reducing overfitting [58] [59]. Significant variables then undergo multivariate Cox regression analysis to determine independent prognostic factors, with hazard ratios and confidence intervals calculated for each covariate.
The visual nomogram construction assigns weighted points to each prognostic variable based on its contribution to survival outcomes. These points are summed to generate total scores that correlate with predicted survival probabilities at specific timepoints (typically 1, 3, and 5 years) [59] [57]. The model performance is subsequently validated through multiple statistical measures including concordance indices (C-index), calibration curves, time-dependent receiver operating characteristic (ROC) curves, and decision curve analysis (DCA) to evaluate predictive accuracy, discriminative ability, and clinical utility [60] [56].
Ubiquitination-Related Gene Signature Development
The integration of URGs into prognostic models follows specialized bioinformatics workflows. Researchers typically extract URG sets from databases such as GeneCards (relevance score ≥5) or the integrated Ubiquitin and Ubiquitin-like Conjugation Database (iUUCD) [58] [61]. Differential expression analysis identifies URGs with significant expression variations between tumor and normal tissues. Survival-associated URGs are then identified through univariate Cox regression analysis, with LASSO Cox regression further refining the gene signature to prevent overfitting [62] [59].
A risk score formula is subsequently developed using the expression values of signature genes weighted by their regression coefficients: Risk score = Σ (Coefficienti × Expressioni) [59] [61]. Patients are stratified into high-risk and low-risk groups based on median risk score cutoffs, with survival differences validated through Kaplan-Meier analysis. This URG signature is then integrated with clinical parameters to construct comprehensive prognostic nomograms [58] [61].
Figure 1: Workflow for developing ubiquitination-related gene (UGRG) prognostic nomograms
Comparative Analysis of URG-Based Prognostic Models Across Cancers
Model Architectures and Performance Metrics
The application of URG-based nomograms has demonstrated substantial prognostic value across diverse malignancies. The following table summarizes key performance metrics for recently developed models:
Table 1: Comparative Performance of URG-Based Prognostic Nomograms Across Cancer Types
| Cancer Type | URG Signature Genes | C-Index | AUC Values | Clinical Endpoint | Reference |
|---|---|---|---|---|---|
| Head and Neck Squamous Cell Carcinoma | 11-gene pair signature | 0.744-0.861* | 0.744 (1-year), 0.852 (3-year), 0.861 (5-year) | Overall Survival | [58] |
| Prostate Cancer | ARIH2, FBXO6, GNB4, HECW2, LZTR1, RNF185 | 0.750-0.850* | 0.850 (1-year), 0.843 (3-year), 0.778 (5-year) | Biochemical Recurrence | [59] |
| Sarcoma | CALR, CASP3, BCL10, PSMD7, PSMD10 | Not specified | Significantly stratified survival (p<0.001) | Overall Survival | [62] |
| Endometrial Cancer | 22-gene signature | Not specified | Accurate risk stratification (p<0.05) | Overall Survival | [61] |
Range represents training and validation cohort performance
The HNSCC model exemplifies a robust prognostic tool, demonstrating excellent discriminatory power with area under curve (AUC) values increasing from 0.744 at 1-year to 0.861 at 5-year survival, suggesting improving predictive accuracy for longer-term outcomes [58]. Similarly, the prostate cancer nomogram maintained high AUC values exceeding 0.77 across all timepoints, indicating consistent performance [59]. A critical observation across studies is that URG-based models frequently outperform traditional staging systems, with the uveal melanoma nomogram demonstrating superior predictive capability compared to the AJCC staging system (C-index 0.714 vs conventional staging) [60].
Methodological Variations in URG Signature Development
Different research groups have employed varying strategies for URG signature development, influencing model characteristics and clinical applicability:
Table 2: Methodological Approaches in URG Signature Development
| Methodological Aspect | HNSCC Study [58] | Prostate Cancer Study [59] | Sarcoma Study [62] |
|---|---|---|---|
| URG Source | GeneCards (relevance score ≥5) | iUUCD Database | GeneCards (relevance score ≥5) |
| Feature Selection | LASSO Cox regression | Univariate Cox → LASSO → Multivariate Cox | LASSO Cox regression |
| Signature Size | 11 gene pairs | 6 genes | 5 genes |
| Validation Approach | Internal validation (training/test split) | External validation (GEO dataset) | Multiple GEO datasets + RT-qPCR |
| Clinical Integration | Age, stage, gender, TNM classification | Gleason grade, PSA, pathological T stage | Immune features, drug sensitivity |
The HNSCC study employed an innovative gene-pair approach that compares relative expression levels between genes, reducing technical variability and enhancing robustness across datasets [58]. In contrast, the prostate cancer research implemented a rigorous multi-step selection process, progressively refining 236 significant URGs identified through univariate analysis to a final 6-gene signature via LASSO and multivariate Cox regression [59]. The sarcoma study uniquely complemented bioinformatics analysis with experimental validation through RT-qPCR, confirming upregulated expression of prognostic URGs in clinical samples [62].
The Scientist's Toolkit: Essential Reagents and Databases
Table 3: Essential Research Resources for URG Nomogram Development
| Resource Category | Specific Tools | Application in Nomogram Development | Key Features |
|---|---|---|---|
| Cancer Databases | TCGA, SEER, GEO | Patient cohorts, clinical data, expression profiles | Large sample sizes, multi-omics data, clinical outcomes |
| URG Repositories | GeneCards, iUUCD | Comprehensive URG identification | Relevance scoring, functional annotations |
| Bioinformatics Tools | "limma" (R), "glmnet" (R) | Differential expression, LASSO regression | Statistical rigor, reproducibility |
| Validation Packages | "timeROC", "rms", "survival" (R) | Model performance assessment | C-index calculation, calibration plots, survival analysis |
| Experimental Validation | RT-qPCR, immunohistochemistry | Confirmatory analysis of URG expression | Translational bridge between bioinformatics and clinical application |
The selection of appropriate databases fundamentally influences nomogram quality. TCGA provides comprehensive molecular characterization across cancer types, while SEER offers extensive clinical data with long-term follow-up [58] [56]. GeneCards and iUUCD serve as authoritative sources for URG identification, with GeneCards offering relevance scores that facilitate prioritization of high-confidence candidates [58] [61]. The R package ecosystem provides specialized tools for each analytical step, with "glmnet" implementing LASSO regularization to prevent overfitting—a critical consideration when developing multi-gene signatures [59] [61].
Critical Assessment of Methodological Limitations and Bias
Despite their promising performance, URG-based nomograms face several methodological challenges that warrant careful consideration. A systematic review of glioma nomograms revealed that 82.1% of studies (32 of 39) lacked external validation, substantially limiting generalizability [63]. Additionally, many studies utilize relatively small sample sizes that may not adequately represent population heterogeneity, potentially overestimating model performance through overfitting.
The proportional hazards (PH) assumption fundamental to Cox regression models remains frequently unverified in nomogram development studies. Violations of this assumption can lead to biased hazard ratios and compromised predictions [63]. Furthermore, variable selection approaches may overlook clinically relevant factors not captured in cancer databases, creating incomplete prognostic representations.
Ethnographic bias represents another significant limitation, with the glioma nomogram review noting that all included studies originated from China, potentially limiting global applicability [63]. Similarly, most publicly available datasets disproportionately represent Western populations, creating geographic imbalances in training data. Prospective multi-center studies incorporating diverse populations are essential to validate existing nomograms across demographic groups.
Technical limitations in URG detection methodologies also affect model reproducibility. RNA sequencing platform variations, normalization approaches, and batch effects can substantially influence expression measurements, potentially altering risk classifications [58] [59]. The transition from transcriptomic data to functional protein-level validation remains challenging, as mRNA expression may not fully correlate with enzymatic activity in the ubiquitination cascade.
Figure 2: Key limitations and recommended solutions in URG nomogram development
URG-based nomograms represent a significant advancement in personalized cancer prognosis, effectively integrating molecular signatures with clinical parameters to generate individualized survival predictions. The consistent demonstration of superior performance compared to traditional staging systems across multiple cancer types underscores their clinical potential. However, methodological standardization, external validation in diverse populations, and functional characterization of signature genes remain essential for widespread clinical adoption.
Future development should prioritize multi-center prospective validation studies to establish generalizability across healthcare systems and demographic groups. Incorporation of additional molecular features such as epigenetic markers, microRNA regulators, and immune profiling parameters may further enhance predictive accuracy. Additionally, functional studies elucidating the mechanistic roles of signature URGs in tumor progression will strengthen biological plausibility and potentially identify novel therapeutic targets.
The integration of URG-based nomograms into clinical decision support systems presents an promising avenue for precision oncology, potentially guiding treatment intensification for high-risk patients and sparing low-risk patients from excessive therapy. As validation evidence accumulates and methodological rigor improves, these sophisticated predictive tools are poised to become fundamental components of individualized cancer care, ultimately improving patient outcomes through personalized risk assessment and treatment selection.
Integrating UbRG Signatures with Standard Clinicopathological Parameters
The ubiquitin-proteasome system (UPS) represents a crucial regulatory mechanism in cellular homeostasis, governing protein degradation and influencing virtually all cancer hallmarks, from uncontrolled proliferation to metastasis [64]. Ubiquitination-related genes (UbRGs) encode enzymes—including E1 ubiquitin-activating enzymes, E2 ubiquitin-conjugating enzymes, and E3 ubiquitin ligases—that orchestrate the precise tagging of cellular proteins for degradation, thereby regulating key signaling pathways [65]. Recent advances in high-throughput genomic technologies have enabled the systematic investigation of UbRG expression patterns across human malignancies, revealing their profound prognostic potential.
Current oncology practice relies heavily on standard clinicopathological parameters, including tumor stage, grade, and nodal status, for prognostic stratification and treatment decisions. However, significant heterogeneity in clinical outcomes exists among patients with similar clinicopathological profiles, underscoring the limitations of these conventional parameters [66]. The integration of molecular signatures with traditional clinicopathological factors represents a promising approach to enhance prognostic precision and enable truly personalized cancer management. UbRG signatures have emerged as particularly valuable biomarkers due to their central role in oncogenesis and cancer progression, offering insights into tumor biology that complement conventional parameters [64] [65] [58].
This comparative analysis examines the emerging evidence supporting the integration of UbRG signatures with standard clinicopathological parameters across multiple cancer types, evaluating their collective prognostic value, methodological considerations, and potential clinical applications.
Methodological Framework for UbRG Signature Development
Data Acquisition and UbRG Compilation
The construction of UbRG signatures follows a systematic bioinformatics pipeline, beginning with comprehensive data acquisition. Researchers typically obtain RNA sequencing data and corresponding clinical information from large-scale public repositories such as The Cancer Genome Atlas (TCGA) and Gene Expression Omnibus (GEO) [64] [65]. Ubiquitination-related genes are compiled from specialized databases including the iUUCD 2.0 database, which contains extensive information on ubiquitin-related enzymes and regulators, or the GeneCards database with relevance scoring [64] [58]. This initial phase yields a master list of UbRGs—ranging from approximately 763 to 1,393 genes depending on the database and filtering criteria—which serves as the foundation for subsequent analyses [64] [67].
Signature Construction Using Machine Learning Approaches
The core of UbRG signature development involves sophisticated statistical learning methods to identify optimal gene combinations with prognostic significance. Researchers typically employ a multi-step regression approach:
- Univariate Cox Regression: Initial screening identifies individual UbRGs significantly associated with overall survival (OS) or other clinical endpoints [64] [65].
- LASSO-Penalized Cox Regression: This technique reduces overfitting by applying a penalty term that shrinks coefficients of less informative genes to zero, retaining only the most prognostically relevant UbRGs in the final signature [64] [58].
- Multivariate Cox Regression: Final coefficient estimation for each included gene, used to calculate a comprehensive risk score for each patient [64].
The resulting risk score formula takes the general form:
[ Risk\ Score = \sum{i=1}^{n} (Expression\ of\ Genei \times Corresponding\ Coefficient_i) ]
where n represents the number of genes in the final signature [67]. Patients are subsequently stratified into high-risk and low-risk groups based on the median risk score or optimized cut-off values.
Table 1: UbRG Signatures Across Cancer Types
| Cancer Type | Number of UbRGs in Signature | Risk Stratification Power | Clinical Parameters Integrated | Reference |
|---|---|---|---|---|
| Breast Cancer | 8 genes | Significant OS difference (p<0.001) | Histology, subtype, T/N status, AJCC stage | [64] |
| Head and Neck SCC | 11 gene pairs | Significant OS difference (p<0.001) | Age, clinical stage, gender, TNM, grade | [58] |
| Liver HCC | 12 genes | Significant OS and PFS differences | Age, clinical stage, gender, TNM | [67] |
| Ovarian Cancer | 22 genes | Validated in external cohort | Age, stage, residual disease | [65] |
Validation and Nomogram Construction
Robust validation represents a critical step in UbRG signature development. Researchers typically employ both internal validation (using bootstrap resampling or split-sample approaches within the original dataset) and external validation (using independent cohorts from GEO or other sources) [64] [67]. To facilitate clinical translation, prognostic nomograms are often constructed by integrating the UbRG signature with standard clinicopathological variables. These graphical tools incorporate factors such as age, TNM classification, histology, and AJCC stage alongside the UbRG risk score, generating individualized survival probability estimates at 1, 3, and 5 years [64] [58]. The predictive accuracy of these nomograms is assessed using time-dependent receiver operating characteristic (ROC) curves and calibration plots, with reported area under the curve (AUC) values frequently exceeding 0.75, indicating good discriminatory power [58] [67].
Comparative Performance Analysis: UbRG Signatures Versus Conventional Parameters
Prognostic Value Across Cancer Types
Multiple studies have demonstrated that UbRG signatures provide prognostic information beyond standard clinicopathological parameters across diverse malignancies. In breast cancer, an 8-gene UbRG signature effectively stratified patients into distinct risk groups with significant differences in overall survival (p<0.001), even after adjusting for conventional factors like ER status, AJCC stage, and T/N status [64]. Similarly, in head and neck squamous cell carcinoma (HNSCC), an 11-gene pair signature maintained independent prognostic value in multivariate analysis, with the high-risk group exhibiting significantly reduced overall survival compared to the low-risk group (p<0.001) [58]. The consistent performance of UbRG signatures across these diverse cancer types suggests fundamental associations with core oncogenic processes.
In liver hepatocellular carcinoma (LIHC), a 12-gene UbRG signature demonstrated significant stratification power for both overall survival and progression-free survival, with the risk score emerging as an independent predictor in multivariate Cox regression analyses [67]. The signature showed particular promise in identifying high-risk patients within early-stage disease, potentially addressing a critical limitation of conventional staging systems. Similar findings were reported in ovarian cancer, where a 22-gene UbRG signature maintained prognostic significance in external validation and demonstrated associations with immune infiltration patterns and therapeutic response [65].
Predictive Performance Metrics
Quantitative assessment of predictive performance reveals the added value of UbRG signatures compared to conventional parameters alone. In HNSCC, the integration of UbRG signatures with clinicopathological variables in a nomogram achieved AUC values of 0.744, 0.852, and 0.861 for 1-, 3-, and 5-year overall survival, respectively, outperforming models based solely on traditional parameters [58]. These findings indicate excellent discriminatory power that improves with longer follow-up durations. Similarly, in liver cancer, the UbRG signature demonstrated robust predictive accuracy with time-dependent ROC analysis, maintaining AUC values above 0.70 across multiple timepoints [67].
Table 2: Performance Comparison of Prognostic Models
| Cancer Type | Model Type | 1-Year AUC | 3-Year AUC | 5-Year AUC | Independent Prognostic Value | Reference |
|---|---|---|---|---|---|---|
| Head and Neck SCC | UbRG nomogram | 0.744 | 0.852 | 0.861 | Yes (p<0.05) | [58] |
| Liver HCC | UbRG signature | >0.70 | >0.70 | >0.70 | Yes (p<0.05) | [67] |
| Breast Cancer | UbRG signature | N/R | N/R | N/R | Yes (p<0.001) | [64] |
| Ovarian Cancer | UbRG signature | N/R | N/R | N/R | Yes (external validation) | [65] |
Abbreviations: AUC, area under the curve; N/R, not reported
Biological Insights and Functional Mechanisms
Immune Microenvironment Modulation
Beyond pure prognostic stratification, UbRG signatures provide insights into fundamental biological processes shaping cancer progression. A prominent mechanism involves modulation of the tumor immune microenvironment. In breast cancer, UbRG signatures were significantly associated with distinct immune infiltration patterns, particularly involving M2 macrophages and other immunosuppressive cell populations [64]. Similarly, in HNSCC, high-risk patients defined by UbRG signatures demonstrated increased infiltration of M2 macrophages and elevated tumor mutation burden (TMB), suggesting an immunologically active but suppressed microenvironment [58]. These findings position UbRG signatures as potential biomarkers for immunotherapy response prediction, extending their utility beyond prognostic stratification alone.
In ovarian cancer, UbRG signatures were closely linked with immune cell infiltration (ICI) patterns within the tumor microenvironment, influencing B cells, plasma cells, CD4+ memory T cells, and M1 macrophages [65]. Specifically, Ube2j1—a key gene within the ovarian cancer UbRG signature—was found to modulate the immune microenvironment through the JAK2/STAT3/PD-L1 pathway, providing a mechanistic explanation for the association between ubiquitination processes and anti-tumor immunity [65]. This intersection between UbRG expression and immune regulation offers promising avenues for combination therapeutic strategies targeting both ubiquitination pathways and immune checkpoints.
Signaling Pathway Alterations
Functional enrichment analyses consistently reveal that UbRG signatures capture alterations in key oncogenic signaling pathways. In liver cancer, UbRG high-risk groups showed enrichment of pathways related to cell cycle regulation, DNA replication, and cancer-related signaling [67]. Similarly, in breast cancer, Gene Set Enrichment Analysis (GSEA) indicated activation of proliferation and survival pathways in high-risk patients identified by UbRG signatures [64]. These pathway alterations likely explain the more aggressive clinical behavior observed in high-risk patients and suggest potential therapeutic vulnerabilities.
The experimental validation of specific UbRGs further supports their functional importance. In breast cancer models, FBXL6 and PDZRN3 were experimentally validated to significantly influence cancer development through in vitro and in vivo experiments [64]. Similarly, in ovarian cancer, Ube2j1 was demonstrated to regulate malignant progression through the JAK2/STAT3 pathway, providing direct mechanistic evidence for the bioinformatics-derived signatures [65]. These functional studies strengthen the biological plausibility of UbRG signatures and confirm their role in cancer pathogenesis rather than mere association.
Technical Considerations and Research Reagents
Essential Research Reagent Solutions
The development and validation of UbRG signatures rely on specialized research reagents and methodologies. Key resources include:
Table 3: Essential Research Reagents and Resources for UbRG Studies
| Reagent/Resource | Function and Application | Examples/Specifications | Reference |
|---|---|---|---|
| iUUCD 2.0 Database | Comprehensive UbRG compilation | Contains 763-1,393 UbRGs with functional annotations | [64] [67] |
| TCGA/GE0 Datasets | Transcriptome and clinical data | Breast cancer (TCGA-BRCA), LIHC, HNSCC, ovarian cancer | [64] [65] [58] |
| LASSO-Cox Regression | Variable selection and model building | Implemented via "glmnet" R package with tenfold cross-validation | [64] [67] |
| ConsensusClusterPlus | Molecular subtyping based on UbRG expression | PAM algorithm with 1,000 repetitions for stability | [64] |
| CIBERSORT | Immune cell infiltration quantification | Deconvolutes expression data to estimate 22 immune cell types | [64] |
| Western Blot Reagents | Protein expression validation | Antibodies against specific UbRGs (e.g., FBXL6, PDZRN3) | [64] |
| qRT-PCR Systems | Gene expression confirmation | Validation of signature genes in cell lines | [64] [65] |
Methodological Standardization Challenges
Several methodological challenges require consideration when interpreting UbRG signature studies. The variable number of genes included in different signatures (ranging from 8 in breast cancer to 22 in ovarian cancer) reflects both cancer-specific biology and analytical approaches [64] [65]. The use of different UbRG databases (iUUCD 2.0 versus GeneCards) with varying inclusion criteria further complicates direct comparison across studies. Additionally, the statistical methods for risk stratification, while generally based on median risk scores, may incorporate more complex optimization algorithms in some implementations [58] [67].
Technical validation remains essential for confirming bioinformatics findings. Western blot analysis serves as the gold standard for protein-level validation of UbRG expression, typically using antibodies against specific ubiquitination-related proteins such as FBXL6 and PDZRN3 [64]. Quantitative real-time PCR (qRT-PCR) provides mRNA-level confirmation in cell lines and clinical specimens, while functional studies using siRNA knockdown or overexpression validate the biological roles of individual UbRGs in cancer phenotypes [64] [65]. These orthogonal validation approaches strengthen the credibility of computational predictions and support clinical translation.
Clinical Translation and Therapeutic Implications
Predictive Biomarkers for Treatment Response
UbRG signatures show promise as predictive biomarkers for treatment response across multiple therapeutic modalities. In breast cancer, UbRG signatures were associated with differential sensitivity to endocrine therapy (tamoxifen, fulvestrant), chemotherapy (cyclophosphamide, cisplatin, paclitaxel, epirubicin), and targeted agents (gefitinib, lapatinib) [64]. Similarly, in liver cancer, risk groups defined by UbRG signatures demonstrated varied sensitivity to targeted and chemotherapeutic agents, with potential implications for treatment selection [67]. These findings suggest that UbRG signatures could inform personalized therapy approaches beyond pure prognostic stratification.
The connection between UbRG signatures and tumor mutation burden (TMB) further enhances their therapeutic relevance. In HNSCC, high-risk patients defined by UbRG signatures exhibited significantly elevated TMB compared to low-risk patients, suggesting potential increased responsiveness to immunotherapy [58]. As tumor mutation burden has emerged as a biomarker for immune checkpoint inhibitor response across multiple cancer types, this association positions UbRG signatures as potential indirect predictors of immunotherapy benefit.
Integration into Clinical Decision-Making
The integration of UbRG signatures with standard clinicopathological parameters addresses critical gaps in current prognostic systems. While traditional parameters like AJCC stage and TNM classification provide essential anatomical and morphological information, UbRG signatures add functional biological dimension that captures tumor aggressiveness and therapeutic vulnerabilities [64] [58] [67]. This integration is particularly valuable for patients with intermediate-risk disease by conventional staging, where UbRG signatures may enable more refined risk stratification and treatment intensification or de-escalation.
Despite these promising applications, challenges remain in clinical implementation. Current biomarker testing rates in advanced cancer remain suboptimal (approximately 35% across major cancer types), highlighting logistical and educational barriers to widespread molecular testing integration [68]. Additionally, the transition from genomics-guided "stratified medicine" to truly "personalized medicine" requires incorporation of multiple biomarker layers beyond genomics alone, including proteomic, pharmacogenetic, and microenvironmental factors [69]. UbRG signatures represent an important step in this evolution, but further refinement and standardization will be necessary for routine clinical application.
Visualizing the UbRG Signature Workflow
The following diagram illustrates the comprehensive workflow for developing and validating UbRG prognostic signatures:
UbRG Signature Development Workflow
The accumulating evidence across multiple cancer types demonstrates that UbRG signatures provide significant prognostic information beyond standard clinicopathological parameters. These molecular signatures capture fundamental biological processes—particularly immune microenvironment modulation and oncogenic pathway activation—that drive cancer progression and treatment resistance. The integration of UbRG signatures with conventional parameters in prognostic nomograms represents a powerful approach to personalized cancer care, enabling more accurate risk stratification and potentially informing therapeutic selection.
Despite these advances, further research is needed to standardize analytical approaches, validate signatures in prospective cohorts, and establish clinically applicable cut-off values. The integration of UbRG signatures with other molecular biomarkers, including those derived from liquid biopsies and multi-omics platforms, may further enhance their predictive power [66] [70]. As precision medicine evolves from "stratified" approaches based primarily on genomics toward truly "personalized" models incorporating multiple data layers, UbRG signatures are poised to play an increasingly important role in cancer prognostication and treatment personalization.
Addressing Technical Challenges and Enhancing Predictive Performance
Distinguishing Prognostic vs. Predictive Biomarker Values in Clinical Context
In the pursuit of precision oncology, biomarkers have emerged as indispensable tools for refining diagnosis, prognosis, and treatment selection. Within this landscape, a fundamental distinction exists between prognostic and predictive biomarkers, each serving a distinct clinical purpose [71]. Understanding this dichotomy is paramount for researchers and drug development professionals aiming to develop targeted therapies and personalized treatment strategies.
A prognostic biomarker provides information about the natural history of a patient's disease, independent of therapy. It identifies the likelihood of a clinical event, such as disease recurrence or progression, in patients who have the disease or medical condition of interest [71]. For example, a prognostic biomarker might identify patients with early-stage cancer who are at high risk of metastasis, thus potentially benefiting from more aggressive therapy, even though the biomarker itself does not predict response to that specific therapy.
In contrast, a predictive biomarker identifies individuals who are more likely than similar individuals without the biomarker to experience a favorable or unfavorable effect from exposure to a specific medical product or environmental agent [71]. The canonical example is the BRAF V600E mutation in late-stage melanoma, which predicts response to BRAF inhibitors like vemurafenib [71]. Critically, establishing a biomarker as predictive generally requires evidence from a controlled study comparing a treatment to a control in patients with and without the biomarker [71].
This guide objectively compares these biomarker values within the context of ubiquitination-related genes in cancer research, providing experimental frameworks for their evaluation and distinction.
Conceptual and Statistical Differentiation
Fundamental Definitions and Clinical Implications
The following table delineates the core characteristics of prognostic and predictive biomarkers.
Table 1: Core Characteristics of Prognostic and Predictive Biomarkers
| Feature | Prognostic Biomarker | Predictive Biomarker |
|---|---|---|
| Primary Question | What is the likely natural course of my patient's disease? | Which treatment is most likely to benefit my patient? |
| Clinical Utility | Stratifies patients by risk of future outcomes (e.g., recurrence, death) | Guides selection of specific treatments; is a cornerstone of precision medicine |
| Study Design Required | Often identified from observational data of patients with the disease [71]. | Requires a comparison of treatment to a control in patients with and without the biomarker [71]. |
| Interpretation | The biomarker's effect is consistent across different treatments. | A statistical treatment-by-biomarker interaction must be present [71]. |
| Effect on Outcome | Shows a main effect on the clinical outcome. | The effect on outcome depends on the treatment received. |
Statistical Considerations and Interpretation
Distinguishing between these biomarkers hinges on statistical analysis. A common misinterpretation occurs when a difference in outcome associated with biomarker status in a single treatment group is taken as evidence of a predictive effect [71]. In reality, this same difference might exist across all treatments, making the biomarker prognostic, not predictive.
The ideal predictive biomarker demonstrates a qualitative treatment-by-biomarker interaction, where there is clear benefit from the experimental treatment in one biomarker subgroup (e.g., positive) but a lack of benefit, or even harm, in the other subgroup (e.g., negative) [71]. This contrasts with a quantitative interaction, where the experimental therapy is better for both subgroups but to different degrees, which may not justify withholding treatment based on biomarker status [71].
When evaluating biomarker studies, it is critical to note that significant mean group differences between cases and controls do not imply the characteristic applies to all individuals. For a biomarker to have diagnostic utility (e.g., 80% sensitivity and 80% specificity), a very large effect size (Cohen's d of ~1.66) is required [72].
Diagram 1: Biomarker Clinical Utility Pathways
Ubiquitination-Related Genes as Biomarkers in Cancer
The Ubiquitin-Proteasome System (UPS) in Cellular Homeostasis
The ubiquitin-proteasome system (UPS) is a critical post-translational regulatory mechanism involving a sequential enzymatic cascade: E1 (ubiquitin-activating), E2 (ubiquitin-conjugating), and E3 (ubiquitin-ligase) enzymes [73]. This system regulates essential cellular processes, including cell cycle control, DNA damage repair, and apoptosis, by targeting proteins for proteasomal degradation or altering their function [73]. Dysregulation of UPS members is strongly linked to cancer pathogenesis, as they can control the stability of key oncoproteins and tumor suppressors [73].
A Ubiquitin-Related Gene Signature in Epithelial Ovarian Carcinoma
A 2024 study constructed a ubiquitin-related risk model for Epithelial Ovarian Carcinoma (EOC), a highly fatal gynecological malignancy [74]. The model comprised 12 genes: HSP90AB1, FBXO9, SIGMAR1, STAT1, SH3KBP1, EPB41L2, DNAJB6, VPS18, PPM1G, AKAP12, FRK, and PYGB [74]. Patients were categorized into high-risk and low-risk groups based on this signature.
Table 2: Ubiquitin-Related Gene Signature in EOC: Prognostic Value and Functional Associations [74]
| Gene in Signature | Hazard Ratio (HR) | Putative Role (Protective/Risk) | Associated Biological Processes |
|---|---|---|---|
| HSP90AB1, FBXO9, SIGMAR1, STAT1, SH3KBP1, DNAJB6, PPM1G | HR < 1 | Protective | Cell cycle regulation, signal transduction, DNA damage response [73]. |
| EPB41L2, VPS18, AKAP12, FRK, PYGB | HR > 1 | Risk | Focal adhesion, actin cytoskeleton regulation, metabolic reprogramming. |
| Overall High-Risk Signature | N/A | Prognostic Indicator | Associated with poorer overall survival, specific TME (B cells, M2 macrophages, fibroblasts), and lower sensitivity to chemotherapy [74]. |
The study demonstrated this signature's prognostic power, as the high-risk group had significantly worse overall survival [74]. Furthermore, the risk groups exhibited distinct tumor microenvironment (TME) features and differential sensitivity to chemotherapeutics, suggesting potential for future predictive applications that require validation in treated versus control cohorts [74].
Experimental Protocols for Biomarker Evaluation
Protocol 1: Developing a Ubiquitin-Related Gene Signature
This protocol is adapted from the methodology used to establish the EOC ubiquitin-signature [74].
- Data Acquisition: Obtain RNA sequencing data and corresponding clinical information (especially overall survival data) for a cancer cohort from a public repository like The Cancer Genome Atlas (TCGA). Obtain normal tissue data from a repository like the Genotype-Tissue Expression (GTEx) project.
- Identification of Differentially Expressed Genes (DEGs): Using a statistical package (e.g.,
limmain R), identify genes differentially expressed between tumor and normal tissues. Set appropriate thresholds (e.g., |log2 fold-change| > 1, adjusted p-value < 0.05). - Intersection with Ubiquitin-Related Genes: Cross-reference the identified DEGs with a curated list of ubiquitin-related genes (e.g., from the GeneCards database) to derive a set of Differentially Expressed Ubiquitin-Related Genes (DEURGs).
- Model Construction via LASSO-Cox Regression: Subject the DEURGs to Least Absolute Shrinkage and Selection Operator (LASSO)-Cox regression analysis. This penalized regression technique selects the most robust prognostic genes from the panel while preventing overfitting.
- Risk Score Calculation: For each patient, calculate a risk score based on the expression levels of the final gene set, weighted by their regression coefficients from the multivariate Cox analysis.
- Validation: Divide the cohort into training and test sets (e.g., 60:40 split). Validate the model's prognostic performance in the test set using Kaplan-Meier survival analysis and time-dependent receiver operating characteristic (ROC) curves.
Protocol 2: Distinguishing Prognostic from Predictive Value
This protocol outlines the gold-standard approach for establishing a predictive biomarker [71].
- Study Design: A randomized controlled trial (RCT) is the ideal setting. Patients are randomized to receive either the experimental therapy or a control therapy (standard of care/placebo).
- Biomarker Measurement: Collect patient samples (e.g., tumor tissue) at baseline and analyze the biomarker status (e.g., presence/absence of a specific ubiquitin-ligase mutation) for all participants in the trial. It is critical that this is done blinded to treatment assignment and outcome.
- Data Analysis:
- Step 1 - Prognostic Assessment: Within the control group only, assess the association between the biomarker and clinical outcome. A significant association indicates a prognostic effect.
- Step 2 - Predictive Assessment: Test for a statistically significant treatment-by-biomarker interaction in a statistical model that includes terms for treatment, biomarker, and their interaction. A significant interaction term suggests the effect of treatment differs by biomarker status, indicating a predictive effect.
- Step 3 - Visualization: Plot the outcomes (e.g., survival curves) for all four groups: Biomarker+/Experimental, Biomarker+/Control, Biomarker-/Experimental, Biomarker-/Control. A predictive biomarker is visually suggested when the curves for the biomarker-positive group show a large separation between treatments, while the curves for the biomarker-negative group are close together.
Diagram 2: Predictive Biomarker Validation Workflow
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Reagent Solutions for Ubiquitination and Biomarker Research
| Reagent / Solution | Core Function | Specific Application in Biomarker Research |
|---|---|---|
| Ubiquitin-Activating Enzyme (E1) Inhibitors | Inhibits the initial step of ubiquitin activation, globally disrupting the UPS [73]. | Tool for functional validation; knocking down UBA1 can help establish its role in cancer cell survival [73]. |
| Proteasome Inhibitors (e.g., Bortezomib) | Block the 26S proteasome, preventing degradation of polyubiquitinated proteins [73]. | Used therapeutically and experimentally to study the effect of stabilizing proteins normally degraded via the UPS. |
| E3 Ubiquitin Ligase Assay Kits | Measure the activity of specific E3 ligases (e.g., BRCA1/BARD1 complex) in vitro [73]. | Functional characterization of specific E3 ligases identified in genomic screens as potential biomarkers. |
| Anti-Ubiquitin & Anti-Linkage Antibodies | Detect ubiquitin and specific polyubiquitin chain linkages (K48, K63, K11, etc.) [73]. | Immunohistochemistry (IHC) to visualize ubiquitination patterns in tumor tissues; used in the EOC study for validation [74]. |
| PROTACs (Proteolysis-Targeting Chimeras) | Bifunctional molecules that recruit E3 ligases to target specific proteins for degradation [73]. | Emerging therapeutic modality that directly leverages the UPS; can be used to probe the function of biomarker genes. |
| qRT-PCR Assays | Quantify gene expression levels from tissue or cell samples. | Used to measure the expression of the 12-gene ubiquitin signature in patient tissues, as performed in the EOC study [74]. |
The distinction between prognostic and predictive biomarkers is foundational to precision oncology. Prognostic biomarkers, like the 12-gene ubiquitin signature in EOC, inform about disease aggressiveness and natural history, enabling risk-adapted management strategies. Predictive biomarkers, best identified through randomized studies analyzing treatment-by-biomarker interactions, directly guide therapeutic selection. The ubiquitin-proteasome system represents a rich source of potential biomarkers due to its central role in controlling cellular protein homeostasis. As research progresses, the integration of robust prognostic signatures with validated predictive biomarkers will be crucial for advancing personalized cancer therapy and improving patient outcomes.
Overcoming Tumor Heterogeneity in Ubiquitination Pathway Analysis
The ubiquitin pathway is a crucial post-translational modifier that regulates nearly all cellular processes in cancer biology, functioning through a coordinated enzymatic cascade involving E1 activating, E2 conjugating, and E3 ligase enzymes, along with deubiquitinases (DUBs) that reverse the process [75]. This pathway serves as a master regulator of protein stability, localization, and interaction, governing key cancer-related processes including cell-cycle progression, p53 activation, DNA damage repair, apoptosis, and immune response [75] [76]. As such, comprehensive analysis of ubiquitination-related genes (URGs) offers significant potential for prognostic stratification and therapeutic development in oncology.
However, a fundamental challenge in translating ubiquitination pathway analysis to clinical applications lies in overcoming tumor heterogeneity. Intratumoral heterogeneity presents a substantial obstacle for biomarker assessment, as demonstrated in head and neck squamous cell carcinoma where immunohistochemical biomarkers including those related to proliferation and apoptosis show considerable variation within individual tumors [77]. This heterogeneity is biomarker-specific rather than a general tumor characteristic, complicating the development of reliable prognostic models based on single biopsy samples [77]. Similar challenges extend to ubiquitination pathway analysis, requiring sophisticated methodological approaches to account for variability in gene expression, mutation profiles, and cellular composition across tumor regions and patient populations.
Methodological Approaches for Heterogeneity-Resilient Analysis
Pan-Cancer Genomic Characterization
Large-scale genomic studies across multiple cancer types provide a powerful strategy for distinguishing consistent ubiquitination pathway alterations from stochastic heterogeneity. The integrated genomic analysis of 9,125 tumor samples across 33 cancer types from The Cancer Genome Atlas represents a comprehensive approach to identifying robust ubiquitination-related driver events despite underlying heterogeneity [75]. This study characterized 929 ubiquitin-related genes and 95 deubiquitinase genes, identifying somatic driver candidates through complementary computational approaches including hotspot mutation analysis and MutSigCV [75].
Table 1: Key Ubiquitination-Related Driver Genes Identified Through Pan-Cancer Analysis
| Gene | Alteration Type | Cancer Context | Functional Role |
|---|---|---|---|
| FBXW7 | Hotspot & LoF mutations | UCEC, UCS, SKCM, STAD, LUSC | Substrate recognition component of SCF ubiquitin ligase complex |
| MDM2 | Amplification | Multiple cancers | E3 ubiquitin ligase for p53 degradation |
| SPOP | Hotspot mutations | Prostate cancer | Substrate recognition component of CUL3-based E3 ligase |
| BAP1 | LoF mutations | Mesothelioma, RCC | Deubiquitinase with role in chromatin regulation |
| VHL | LoF mutations | Renal cell carcinoma | Component of E3 ubiquitin ligase complex |
The experimental protocol for this approach involves: (1) collection of multi-platform molecular data from large patient cohorts; (2) curation of comprehensive ubiquitination pathway gene sets; (3) application of complementary driver identification algorithms to account for different alteration types; and (4) cancer-type-specific pattern recognition to distinguish context-dependent effects from noise [75]. This methodology successfully identified cancer-type-specific mutation patterns, such as FBXW7 mutations with distinct hotspot versus loss-of-function distributions across uterine, melanoma, and gastrointestinal cancers [75].
Multi-Omics Integration and Molecular Subtyping
Integrative analysis of multiple molecular datasets enables the identification of ubiquitination-related subtypes that transcend tissue-of-origin classifications. In gastric cancer, researchers have applied ten clustering algorithms to transcriptomic and DNA methylation data from 359 samples, identifying three distinct molecular subtypes (CS1, CS2, CS3) with significant differences in survival outcomes, tumor immune microenvironment composition, and therapeutic responses [78]. This approach leverages the MOVICS pipeline, which integrates CIMLR, iClusterBayes, MoCluster, COCA, ConsensusClustering, IntNMF, LRAcluster, NEMO, PINSPlus, and SNF algorithms to ensure robust subtype identification [78].
The workflow for multi-omics subtyping includes: (1) data extraction and preprocessing of gene expression and DNA methylation data; (2) dimensionality reduction and clustering using multiple algorithms; (3) determination of optimal cluster number using gap statistics and cluster prediction index; (4) characterization of subtype-specific biological features; and (5) validation in independent cohorts [78]. This methodology revealed subtype-specific ubiquitination patterns and their association with immune activation status, providing a heterogeneity-aware classification framework.
Ubiquitination-Based Prognostic Model Construction
Disease-specific ubiquitination-related risk models offer another approach to overcoming heterogeneity by consolidating multiple ubiquitination signals into unified prognostic signatures. In lung adenocarcinoma, researchers developed a ubiquitination-related risk score (URRS) based on four genes (DTL, UBE2S, CISH, and STC1) that effectively stratified patients into distinct prognostic groups despite underlying heterogeneity [26]. The model construction involved univariate Cox regression, Random Survival Forests, and LASSO Cox regression to identify the most informative ubiquitination-related features [26].
Table 2: Ubiquitination-Based Prognostic Models Across Cancer Types
| Cancer Type | Key Genes in Signature | Validation Cohorts | Clinical Utility |
|---|---|---|---|
| Lung Adenocarcinoma | DTL, UBE2S, CISH, STC1 | 6 external GEO datasets | Prognosis, TME assessment, drug response prediction |
| Ovarian Cancer | 17-gene signature including FBXO45 | GSE165808, GSE26712 | Prognosis, immune microenvironment characterization |
| Esophageal Squamous Cell Carcinoma | BUB1B, CHEK1, DNMT1, IRAK1, PRKDC | GSE20347, in-house dataset | Prognostic biomarkers, therapeutic targets |
| Diffuse Large B-Cell Lymphoma | CDC34, FZR1, OTULIN | GSE181063 | Prognosis, drug sensitivity assessment |
The standard protocol for ubiquitination-related risk model development includes: (1) acquisition of gene expression and clinical data from public repositories; (2) identification of differentially expressed URGs between tumor and normal tissues; (3) selection of prognostic URGs through univariate Cox regression; (4) feature refinement using LASSO or Random Survival Forest methods; (5) risk score calculation based on multivariate Cox coefficients; (6) stratification of patients into high-risk and low-risk groups; and (7) validation in independent cohorts [26] [17] [15]. This approach effectively distills heterogeneous ubiquitination patterns into clinically actionable signatures.
Digital Pathology and Intratumoral Heterogeneity Quantification
Advanced digital image analysis enables direct measurement and incorporation of intratumoral heterogeneity into ubiquitination pathway assessment. In hormone receptor-positive breast cancer, researchers have employed hexagonal tiling to compute heterogeneity indicators for protein expression, revealing that intratumoral heterogeneity of PR and Ki67 provided superior prognostic information compared to simple expression levels [79]. The methodology included digital image analysis of full-face surgical excision slides using the HALO platform, followed by computational heterogeneity assessment [79].
The experimental workflow comprises: (1) immunohistochemical staining of target proteins on tissue sections; (2) whole-slide scanning at high resolution; (3) digital image analysis with tissue segmentation and biomarker quantification; (4) application of spatial sampling methods (hexagonal tiling) to assess regional variation; (5) calculation of heterogeneity metrics including Haralick's texture entropy and Ashman's D bimodality; and (6) correlation of heterogeneity indices with clinical outcomes [79]. This approach directly addresses spatial heterogeneity rather than attempting to overcome it through averaging.
Single-Cell Resolution and Microenvironment Contextualization
Single-cell RNA sequencing provides unprecedented resolution for dissecting cellular heterogeneity within the ubiquitination landscape. In ovarian cancer, researchers have integrated single-cell data from the E-MTAB-8381 dataset to contextualize ubiquitination-related gene expression across different cell types within the tumor microenvironment [17]. This approach enables the delineation of cell-type-specific ubiquitination patterns that bulk sequencing methods inevitably obscure.
The standard analytical pipeline includes: (1) processing of single-cell RNA sequencing data with quality control filtering; (2) normalization and identification of highly variable genes; (3) dimensionality reduction using PCA and UMAP; (4) graph-based clustering to identify cell populations; (5) cell type annotation using reference datasets; and (6) assessment of ubiquitination-related gene expression across distinct cellular compartments [17]. This methodology revealed how ubiquitination patterns differ between malignant, immune, and stromal cells, providing crucial context for interpreting bulk sequencing data.
Table 3: Key Research Reagent Solutions for Ubiquitination Pathway Analysis
| Reagent/Resource | Function | Application Examples |
|---|---|---|
| HALO Digital Pathology Platform | Whole-slide image analysis with tissue segmentation | Quantification of protein expression heterogeneity in breast cancer [79] |
| ConsensusClusterPlus R Package | Unsupervised clustering for molecular subtyping | Identification of ubiquitination-related subtypes in lung adenocarcinoma [26] |
| MOVICS Pipeline | Multi-omics integration and clustering | Gastric cancer subtyping using 10 clustering algorithms [78] |
| CIBERSORT Algorithm | Immune cell infiltration estimation from bulk RNA data | Characterization of tumor immune microenvironment in ubiquitination subtypes [78] [15] |
| ESTIMATE Algorithm | Stromal and immune scoring in tumor samples | Tumor microenvironment assessment in ovarian cancer risk models [17] |
| Maftools R Package | Somatic mutation analysis and visualization | Mutation landscape characterization in ubiquitination-related subtypes [26] [17] |
| IMvigor210CoreBiologies R Package | Access to immunotherapy cohort data | Validation of ubiquitination signatures in immunotherapy context [26] |
Comparative Analysis of Methodological Performance
Each methodological approach offers distinct advantages and limitations for addressing tumor heterogeneity in ubiquitination pathway analysis. Pan-cancer genomic characterization provides extensive sample sizes for robust driver identification but may obscure cancer-type-specific patterns. Multi-omics integration captures complex molecular relationships but requires sophisticated computational infrastructure. Prognostic model development yields clinically applicable tools but depends heavily on cohort selection and validation. Digital pathology directly quantifies spatial heterogeneity but is limited to protein markers with reliable antibodies. Single-cell resolution offers unparalleled cellular specificity but faces challenges in scalability and cost.
The evidence suggests that hybrid approaches combining multiple methodologies yield the most heterogeneity-resilient insights. For instance, the ovarian cancer study integrated bulk tissue prognostic modeling with single-cell validation and functional experiments, demonstrating how FBXO45 promotes ovarian cancer progression through the Wnt/β-catenin pathway [17]. Similarly, the lung adenocarcinoma analysis combined unsupervised clustering with prognostic model development and drug sensitivity prediction [26]. These integrated methodologies provide complementary strategies for addressing heterogeneity at different biological levels.
The comprehensive analysis of ubiquitination pathways in cancer requires sophisticated methodological approaches that explicitly account for tumor heterogeneity rather than attempting to eliminate it. The emerging paradigm recognizes heterogeneity as an inherent biological feature that can be measured, modeled, and incorporated into analytical frameworks. The methodologies reviewed herein—from pan-cancer genomics to single-cell resolution—provide powerful strategies for distinguishing consistent ubiquitination pathway alterations from stochastic heterogeneity, enabling more reliable prognostic assessment and therapeutic target identification.
Future directions in the field will likely involve increased integration of spatial transcriptomics to bridge the gap between single-cell resolution and tissue context, application of deep learning to identify heterogeneity patterns that escape conventional statistical methods, and development of dynamic models that capture temporal heterogeneity in response to therapeutic interventions. As these methodologies mature, they will enhance our ability to extract meaningful biological signals from heterogeneous ubiquitination pathway data, ultimately advancing precision oncology approaches that account for the complex reality of tumor ecosystems.
Optimizing Signature Stability Across Diverse Patient Populations and Datasets
The pursuit of robust prognostic biomarkers represents a critical frontier in modern oncology, with ubiquitination-related genes (UbRGs) emerging as a particularly promising class of molecular signatures. The ubiquitin-proteasome system (UPS) regulates virtually all cellular processes through targeted protein degradation, playing pivotal roles in tumor proliferation, invasion, immune evasion, and treatment resistance [80] [17]. However, the clinical translation of prognostic signatures faces a fundamental challenge: maintaining predictive accuracy across heterogeneous patient populations and disparate datasets. Tumor heterogeneity—both inter-patient and intra-tumoral—introduces substantial variability in molecular profiling data, compromising model generalizability and clinical utility [81]. This review systematically evaluates computational and experimental strategies for enhancing UbRG signature stability, providing researchers with evidence-based frameworks for developing clinically applicable prognostic tools.
Methodological Comparison of UbRG Signature Development
Computational Approaches for Stable Feature Selection
Table 1: Comparative Analysis of UbRG Signature Development Methods
| Method Category | Specific Techniques | Application in UbRG Studies | Reported Stability Metrics |
|---|---|---|---|
| Machine Learning Frameworks | Random Survival Forest (RSF), Ridge Regression [82] | PTM-related signature in breast cancer; 117 algorithm combinations tested | C-index >0.67 across datasets; AUC: 0.692-0.802 (1-5 year survival) |
| Heterogeneity-Aware Selection | Integrated Heterogeneity Score (IHS) [81] | TNBC prognostic model using low-heterogeneity genes CYP4B1 and GBP1 | IHS threshold <0.5; consistent 3-9 year prediction (AUC>0.6) |
| Regularization Methods | LASSO-Cox regression [16] [17] | Cervical cancer (5-gene signature); Ovarian cancer (17-gene signature) | Cervical cancer AUC>0.6; Ovarian cancer 1-year AUC=0.703 |
| Multi-Omics Integration | GSVA, ESTIMATE, CIBERSORT [83] [81] [84] | Immune microenvironment analysis in breast cancer and TNBC | Correlation with immune infiltration patterns; validated in single-cell datasets |
The integration of machine learning (ML) frameworks has significantly advanced the stability of UbRG signatures. In breast cancer, a systematic comparison of 117 ML combinations identified RSF + Ridge regression as optimal for constructing a post-translational modification (PTM) signature containing ubiquitination-related components [82]. This approach demonstrated superior performance (C-index ranking first across multiple datasets) compared to 14 previously published signatures, highlighting how algorithm selection directly influences cross-dataset stability.
For addressing tumor heterogeneity specifically, the Integrated Heterogeneity Score (IHS) methodology represents a notable innovation [81]. By decomposing gene expression variance into within-tumor and between-tumor components, IHS quantifies transcriptomic heterogeneity at the gene level. Application of this method in triple-negative breast cancer (TNBC) identified CYP4B1 and GBP1 as low-heterogeneity biomarkers, enabling construction of a prognostic signature with consistent predictive performance across 3- to 9-year survival endpoints in both TCGA and METABRIC cohorts [81].
Experimental Validation Workflows
Table 2: Experimental Protocols for UbRG Signature Validation
| Validation Stage | Experimental Method | Key Parameters | Application Example |
|---|---|---|---|
| Wet-Lab Verification | RT-qPCR | TRIzol RNA extraction; SYBR Green methodology; 95°C 30s denaturing [16] [81] | Confirmation of MMP1, TFRC, CXCL8 upregulation in cervical cancer tissues [16] |
| Functional Assays | Cell culture, transfection, Western blot | DMEM/RPMI-1640 + 10% FBS; Lipo8000 transfection [17] | Validation of FBXO45 role in ovarian cancer progression via Wnt/β-catenin pathway [17] |
| Pathway Analysis | Immunohistochemistry, spatial transcriptomics | 4% paraformaldehyde fixation; hematoxylin-eosin staining [32] | SLC27A2 elevated in malignant spots; COL17A1/TNFRSF17 decreased [82] |
| Drug Response Testing | pRRophetic algorithm [81] | Integration of cell line screening with expression profiles | Identification of 6 targeted agents with enhanced efficacy in high-risk TNBC patients [81] |
Experimental validation constitutes an essential component for verifying signature biological relevance and clinical applicability. The standard workflow typically begins with Reverse Transcription Quantitative PCR (RT-qPCR) to confirm differential expression of identified UbRGs in patient tissues versus controls [16] [81]. This is frequently followed by functional assays in relevant cell lines; for instance, in ovarian cancer, FBXO45 (a key E3 ubiquitin ligase) was experimentally demonstrated to promote malignant progression via the Wnt/β-catenin pathway [17].
Advanced spatial validation techniques provide critical insights into signature stability across tumor microenvironments. Spatial transcriptomics in breast cancer revealed that SLC27A2 (a component of a PTM signature) exhibited higher expression in malignant spots, while COL17A1 and TNFRSF17 showed lower expression in these regions [82]. This spatial resolution helps contextualize signature performance across histologically diverse areas within tumors.
Signaling Pathways and Biological Mechanisms
UbRG signatures frequently converge on specific oncogenic pathways that contribute to their prognostic value. Experimental evidence has elucidated several key mechanisms:
Figure 1: Key Signaling Pathways Regulated by Ubiquitination-Related Genes in Cancer
The JAK2/STAT3/PD-L1 axis represents a clinically relevant mechanism through which UbRGs influence cancer progression. In ovarian cancer, Ube2j1 was found to regulate malignant progression and reshape the immune microenvironment via this pathway [80]. Simultaneously, the Wnt/β-catenin pathway emerges as another critical ubiquitination-regulated cascade, with FBXO45 identified as a stabilizer of β-catenin driving ovarian cancer growth and spread [17].
Beyond cancer-cell-autonomous effects, UbRG signatures significantly influence tumor-immune interactions. Comprehensive immune infiltration analyses across multiple cancer types consistently demonstrate that low-risk patients (by UbRG signatures) exhibit enhanced anti-tumor immunity, characterized by increased CD8+ T cells, M1 macrophages, and follicular helper T cells [17]. This immunologically active microenvironment likely contributes to the improved survival outcomes observed in these patients and may predict enhanced response to immune checkpoint inhibitors.
Research Reagent Solutions
Table 3: Essential Research Tools for UbRG Signature Development
| Reagent/Category | Specific Product/Platform | Research Application | Technical Specifications |
|---|---|---|---|
| Ubiquitin Detection | Human Ubiquitin ELISA Kit (Invitrogen #EHRPS27A) [85] | Quantification of ubiquitin in serum, plasma, cell media | Sensitivity: 30 pg/mL; Range: 27.43-20,000 pg/mL; Sample: 50μL plasma/serum |
| Gene Expression Analysis | RT-qPCR with SYBR Green [16] [81] | Validation of UbRG expression in tissues/cells | TRIzol RNA extraction; PrimeScript RT kit; 95°C 30s protocol |
| Cell Culture Models | A2780, HEY (ovarian); MDA-MB-231, MDA-MB-453 (breast) [81] [17] | Functional validation of UbRG biomarkers | Culture: DMEM/RPMI-1640 + 10% FBS; Transfection: Lipo8000 |
| Bioinformatics Tools | CIBERSORT, ESTIMATE, GSVA [81] [84] | Immune microenvironment deconvolution | Algorithmic quantification of 22 immune cell types |
| Spatial Validation | Single-cell RNA sequencing; Spatial transcriptomics [82] | Tissue context resolution of UbRG expression | E-MTAB-8381 dataset; UMAP visualization; cell type annotation |
The investigative workflow for UbRG signature development requires specialized reagents and platforms. For ubiquitin detection, the Human Ubiquitin ELISA Kit provides sensitivity down to 30 pg/mL, enabling quantification in diverse biological samples [85]. Cell line models spanning multiple cancer types (e.g., A2780 and HEY for ovarian cancer; MDA-MB-231 and MDA-MB-453 for breast cancer) serve as essential platforms for functional validation [81] [17].
Bioinformatics tools constitute a particularly crucial reagent category for signature development. Algorithms such as CIBERSORT and ESTIMATE enable deconvolution of immune infiltration patterns from bulk transcriptomic data, revealing how UbRG signatures reflect tumor microenvironment composition [81] [84]. These computational approaches are complemented by experimental platforms like single-cell RNA sequencing and spatial transcriptomics, which resolve expression patterns at cellular resolution across tissue architecture [82].
Integrated Workflow for Stable Signature Development
Figure 2: Integrated Workflow for Developing Stable UbRG Signatures Across Datasets
Based on synthesized evidence from multiple studies, an optimized workflow for developing stable UbRG signatures incorporates both computational robustness checks and experimental verification. The process begins with multi-dataset collection from sources like TCGA, GEO, and METABRIC, followed by systematic heterogeneity assessment using metrics like IHS to identify spatially stable biomarkers [81]. Machine learning selection then identifies optimal gene combinations, with RSF + Ridge regression emerging as particularly effective among 117 tested algorithms [82].
The critical innovation in this workflow is the stability optimization loop, where model performance feedback directly informs heterogeneity-aware feature selection. This iterative process continues through multi-cohort validation and experimental verification via RT-qPCR, functional assays, and spatial transcriptomics [16] [17] [82]. The final output includes clinically applicable tools like nomograms that integrate UbRG signatures with conventional staging systems, significantly enhancing prognostic accuracy (C-index >0.67) [81].
The optimization of UbRG signature stability across diverse populations represents a crucial advancement in cancer prognostication. Methodologies that explicitly address tumor heterogeneity—through integrated heterogeneity scoring, machine learning optimization, and multi-omics validation—demonstrate markedly improved performance across datasets and patient populations. The resulting signatures not only predict survival but also illuminate the biological mechanisms linking ubiquitination to cancer progression, particularly through immune modulation and pathway activation. As these approaches mature, they promise to deliver increasingly robust biomarkers that will ultimately enhance personalized cancer therapy and improve patient outcomes.
Addressing Technical Limitations in Ubiquitination-Specific Assays
Protein ubiquitination is a fundamental post-translational modification that regulates nearly all cellular processes in eukaryotes, including protein degradation, cell cycle progression, DNA repair, and immune responses [86] [87]. The ubiquitin-proteasome system (UPS) maintains proteostasis and cellular homeostasis through a coordinated enzymatic cascade involving E1 activating, E2 conjugating, and E3 ligase enzymes, with counterbalancing deubiquitinating enzymes (DUBs) completing the cycle [87] [88]. Dysregulation of ubiquitination pathways is intimately linked to the pathogenesis of various human diseases, particularly cancers and neurodegenerative disorders [86] [87]. In recent years, the prognostic value of ubiquitination-related genes (URGs) has become increasingly evident across multiple cancer types, including ovarian cancer, lung adenocarcinoma, breast cancer, and esophageal squamous cell carcinoma [25] [27] [26]. This has created an urgent need for precise, sensitive, and high-throughput ubiquitination detection methods to advance both basic research and clinical applications, particularly in the development of targeted therapies such as PROTACs (proteolysis-targeting chimeras) [86] [25].
Despite significant methodological advancements, current ubiquitination detection assays face substantial technical limitations that compromise their utility in both basic research and clinical prognostication. These challenges include poor sensitivity for low-abundance ubiquitinated proteins, linkage-type bias in ubiquitin chain recognition, limited throughput capacity, and an inability to monitor ubiquitination dynamics in real time [86] [87] [89]. This comprehensive guide objectively compares the performance of available ubiquitination detection platforms, provides detailed experimental protocols, and presents quantitative data to inform assay selection for specific research applications, with particular emphasis on prognostic model development in oncology.
Current Methodologies and Their Technical Constraints
Established Detection Platforms and Their Limitations
Contemporary ubiquitination detection methodologies span multiple technological approaches, each with distinctive advantages and limitations. The table below summarizes the principal techniques and their characteristic constraints:
Table 1: Comparison of Major Ubiquitination Detection Methodologies
| Method | Key Principle | Throughput | Sensitivity | Linkage Bias | Real-time Capability |
|---|---|---|---|---|---|
| Immunoblotting | Antibody-based detection using anti-ubiquitin antibodies [87] [89] | Low | Moderate | High (dependent on antibody specificity) | No |
| Mass Spectrometry | LC-MS/MS identification of ubiquitinated peptides with GG remnant signature [89] | Moderate | High for abundant proteins | Variable | No |
| Ubiquitin Tagging | Affinity purification of tagged ubiquitin (e.g., His, Strep) [89] | Moderate | Moderate | Low (general capture) | No |
| UBD-based Approaches | Tandem ubiquitin-binding domains for enrichment [86] [89] | Moderate | High | Variable (domain-dependent) | No |
| Fluorescence Polarization | FP monitoring of ubiquitin conjugation states [88] | High | High | Low | Yes |
| TR-FRET/AlphaScreen | Energy transfer-based proximity assays [86] | High | High | Moderate | No |
Mass spectrometry (MS)-based approaches enable high-throughput identification and quantification of ubiquitinated proteins and their modification sites but require expensive instrumentation, specialized expertise, and substantial starting material [86] [89]. Additionally, MS struggles with detecting ubiquitination on trace or ultra-trace target proteins in low-input proteome samples, limiting its application in clinical specimens with limited availability [86]. Antibody-based immunological methods, particularly western blotting, provide a simple and cost-effective means to monitor ubiquitination status but are constrained by the limited availability of high-affinity antibodies against the highly conserved ubiquitin protein itself [86] [87]. Furthermore, commercial antibodies frequently exhibit significant bias toward specific ubiquitin chain types, potentially skewing experimental results [87] [89]. For instance, many commonly used antibodies preferentially recognize K48-linked chains over atypical linkages such as K6, K11, K27, K29, and K33, leading to an incomplete picture of the cellular ubiquitin landscape [87] [89].
Throughput and Sensitivity Limitations in Current Platforms
Throughput limitations represent a significant bottleneck in ubiquitination research, particularly for drug discovery applications and large-scale prognostic model development. Traditional methods like immunoblotting are inherently low-throughput and labor-intensive, while even advanced MS approaches require substantial analysis time per sample [87]. Sensitivity constraints further compound these issues, as the stoichiometry of protein ubiquitination is typically very low under physiological conditions, and ubiquitinated forms often represent a minute fraction of the total protein pool [89]. This sensitivity challenge is particularly problematic in clinical cancer research, where prognostic model development requires accurate quantification of ubiquitination events in limited patient specimens [25] [26] [28].
The recent development of high-density 96-well plate formats coated with tandem hybrid ubiquitin-binding domains (ThUBDs) has addressed some throughput limitations by enabling parallel processing of multiple samples [86]. However, these platforms still cannot monitor ubiquitination dynamics in real time, restricting their utility for kinetic studies of enzyme inhibition or activation. The UbiReal assay represents a significant advancement in this regard, using fluorescence polarization to monitor all stages of ubiquitin conjugation and deconjugation in real time, including E1 activation, E2~Ub discharge, E3-dependent ubiquitin chain formation, and DUB-mediated hydrolysis [88].
Emerging Solutions and Comparative Performance Data
Advanced UBD-Based Platforms
Recent innovations in ubiquitin-binding domain (UBD) technology have yielded substantial improvements in assay performance. The ThUBD (tandem hybrid ubiquitin-binding domain) platform developed by Liu et al. combines advantages of different UBDs to achieve both high affinity for polyubiquitinated proteins and minimal bias toward different ubiquitin chain types [86]. This system employs ThUBD-coated high-density 96-well plates that demonstrate specific binding to approximately 5 pmol of polyubiquitin chains when coated with 1.03 μg ± 0.002 of ThUBD on Corning 3603-type plates [86]. The ThUBD platform can capture ubiquitinated proteins from complex cellular proteomes with dissociation constants (Kd) in the nanomolar range, significantly enhancing sensitivity compared to traditional TUBE (tandem ubiquitin-binding entity)-based assays [86].
Table 2: Quantitative Performance Comparison of Ubiquitination Detection Platforms
| Platform | Detection Limit | Dynamic Range | Assay Time | Linkage Recognition | Applications in Prognostic Models |
|---|---|---|---|---|---|
| ThUBD-coated Plates | 5 pmol polyUb chains [86] | 3 orders of magnitude [86] | 4-6 hours [86] | Unbiased recognition of all chain types [86] | Ovarian cancer [25], Lung adenocarcinoma [26] |
| UbiReal FP Assay | Sub-nanomolar [88] | Not specified | Real-time monitoring (minutes) [88] | Capable of distinguishing linkage types [88] | Drug screening [88] |
| Mass Spectrometry | ~1-5 fmol for standard samples [89] | 4-5 orders of magnitude [89] | 1-2 days per sample [89] | Variable with enrichment strategy [89] | Breast cancer [27], ESCC [28] |
| Traditional TUBE Assays | ~50-100 pmol [86] | 2 orders of magnitude [86] | 4-6 hours [86] | Significant bias (K48/K63 preference) [86] | Limited by accuracy concerns |
The unbiased recognition capability of ThUBD is particularly valuable for cancer prognostic applications, as different ubiquitin linkage types are associated with distinct cellular outcomes and disease states [87]. For example, K48-linked chains primarily target substrates for proteasomal degradation, while K63-linked chains regulate protein-protein interactions and signaling pathways [87]. In ovarian cancer, prognostic models based on ubiquitination-related genes have demonstrated significant predictive power, with risk stratification effectively separating patients with differential survival outcomes [25]. Similarly, in lung adenocarcinoma, a ubiquitination-related risk score (URRS) based on four genes (DTL, UBE2S, CISH, and STC1) showed strong prognostic performance across multiple validation cohorts [26].
Real-Time Monitoring Platforms
The UbiReal fluorescence polarization assay addresses a critical gap in ubiquitination research by enabling real-time monitoring of the complete ubiquitination cascade [88]. This approach utilizes fluorescently-labeled ubiquitin to track enzymatic activities through changes in molecular rotation and resulting fluorescence polarization. The assay comprehensively measures E1 activation, E2~Ub discharge and specificity, E3-dependent ubiquitin chain formation, and DUB-dependent hydrolysis in a low-volume, high-throughput format suitable for 384-well plates [88].
A key advantage of the UbiReal platform is its utility for studying small molecule modulators of ubiquitination. The system successfully recapitulated the IC₅₀ value of the E1 inhibitor PYR-41 and can be adapted to study E2-E3 pairing specificity and ubiquitin chain linkage preferences [88]. This capability is particularly relevant for drug development efforts targeting the ubiquitin-proteasome system, including PROTACs that redirect E3 ligase activity toward specific target proteins [86] [25]. From a prognostic perspective, the ability to monitor ubiquitination dynamics in real time provides insights into the functional consequences of URG expression patterns identified in cancer prognostic models [25] [26] [28].
Diagram 1: Ubiquitination Enzymatic Cascade. The sequential process of ubiquitin activation by E1, transfer to E2, substrate recognition by E3, and chain elongation.
Experimental Protocols for Key Applications
ThUBD-Coated Plate Assay for High-Throughput Ubiquitination Detection
Materials and Reagents:
- ThUBD protein (recombinantly expressed and purified)
- Corning 3603 high-binding 96-well plates
- Blocking buffer: 3% BSA in PBS
- Wash buffer: PBS with 0.05% Tween-20
- Detection antibody: ThUBD-HRP conjugate
- Substrate: TMB or other HRP-compatible substrate
- Stop solution: 1M H₂SO₄
Procedure:
- Plate Coating: Coat wells with 1.03 μg of ThUBD in 100 μL coating buffer (50 mM carbonate-bicarbonate buffer, pH 9.6). Incubate overnight at 4°C.
- Blocking: Remove coating solution and block with 200 μL blocking buffer for 2 hours at room temperature.
- Sample Incubation: Add 100 μL of cell lysate or purified ubiquitinated proteins to each well. Incubate for 2 hours at room temperature with gentle shaking.
- Washing: Wash plates 5 times with wash buffer using an automated plate washer.
- Detection: Add 100 μL of ThUBD-HRP conjugate (1:5000 dilution in blocking buffer) to each well. Incubate for 1 hour at room temperature.
- Signal Development: Add 100 μL TMB substrate and incubate for 15-30 minutes. Stop reaction with 50 μL stop solution.
- Quantification: Measure absorbance at 450 nm using a plate reader [86].
Applications in Prognostic Research: This protocol enables rapid screening of ubiquitination patterns across multiple patient samples, facilitating the development and validation of ubiquitination-based prognostic models. For example, in ovarian cancer, similar approaches have identified 17 ubiquitination-related genes with significant prognostic value, enabling stratification of patients into distinct risk categories [25].
UbiReal Fluorescence Polarization Assay for Real-Time Monitoring
Materials and Reagents:
- Fluorescein-labeled ubiquitin (F-Ub, Boston Biochem U-590)
- E1, E2, E3 enzymes of interest
- Reaction buffer: 50 mM Tris-HCl (pH 7.5), 50 mM NaCl, 5 mM MgCl₂, 0.1 mg/mL BSA, 1 mM DTT
- ATP regeneration system: 2 mM ATP, 10 mM creatine phosphate, 3.5 U/mL creatine kinase
- Black 384-well low-volume microplates
Procedure:
- Reaction Setup: In a 10 μL reaction volume, combine reaction buffer, ATP regeneration system, 100 nM F-Ub, 50 nM E1, and varying concentrations of E2/E3 enzymes.
- Plate Preparation: Dispense reactions into black 384-well plates. Centrifuge briefly to eliminate bubbles.
- Real-Time Monitoring: Place plate in a fluorescence polarization-compatible plate reader preheated to 30°C. Monitor mP (milliPolarization) values every 30 seconds for 1-2 hours.
- Enzyme Addition: For sequential monitoring, use multichannel dispensers to add E2 or E3 enzymes after establishing baseline readings.
- Data Analysis: Plot mP values versus time. Calculate initial rates from the linear portion of the curve [88].
Applications in Drug Discovery: This protocol is particularly valuable for screening small molecule inhibitors of ubiquitination enzymes, which has significant implications for targeted cancer therapies. The real-time capability enables detailed kinetic analysis of compound effects on specific steps of the ubiquitination cascade, supporting the development of therapeutics that modulate ubiquitination pathways identified as prognostic markers in cancer [88].
Diagram 2: Ubiquitination Assay Workflow for Prognostic Model Development. Integrated process from clinical sample collection to prognostic model building.
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Research Reagents for Ubiquitination Assays
| Reagent Category | Specific Examples | Function | Applications in Prognostic Research |
|---|---|---|---|
| Ubiquitin-Binding Domains | ThUBD, TUBE, UIM, UBA | Capture and enrichment of ubiquitinated proteins | Enables quantification of ubiquitination patterns for risk model development [86] [89] |
| Linkage-Specific Antibodies | K48-specific, K63-specific, M1-linear specific | Detection of specific ubiquitin chain types | Identifies chain-type specific signatures associated with patient outcomes [87] [89] |
| Activity-Based Probes | Ub-AMC, Ub-rhodamine, HA-Ub-VS | Monitoring DUB activity and ubiquitination dynamics | Functional assessment of ubiquitination enzymes identified in prognostic signatures [88] |
| Tagged Ubiquitin Variants | His-Ub, HA-Ub, GFP-Ub, Strep-Ub | Affinity purification of ubiquitinated proteins | Isolation of ubiquitinated substrates from patient-derived samples [89] |
| Enzyme Inhibitors | PYR-41 (E1 inhibitor), MLN4924 (NAE inhibitor), Nutlin (MDM2 inhibitor) | Specific inhibition of ubiquitination cascade components | Functional validation of therapeutic targets identified through prognostic models [87] [90] |
The evolving methodology for ubiquitination detection represents a critical enabling technology for cancer prognostic research. Advanced platforms such as ThUBD-coated plates and UbiReal address fundamental technical limitations in sensitivity, throughput, and linkage bias, providing more accurate tools for quantifying ubiquitination events relevant to disease progression [86] [88]. The integration of these improved detection methods with prognostic model development has already demonstrated significant clinical potential across multiple cancer types, from ovarian cancer to lung adenocarcinoma [25] [26].
As ubiquitination continues to emerge as a rich source of prognostic biomarkers and therapeutic targets, further methodological refinements will enhance our ability to precisely quantify and characterize this complex post-translational modification. The ongoing development of highly specific intracellular ubiquitination tools, such as the recently described small molecule BRD1732 that undergoes direct ubiquitination, opens new avenues for probing ubiquitination dynamics in live cells and may lead to novel therapeutic strategies [90]. Through continued methodological innovation and rigorous validation in clinical samples, ubiquitination-specific assays will play an increasingly important role in precision oncology, enabling more accurate prognosis and personalized treatment selection based on the ubiquitination status of key regulatory pathways.
Strategies for Validating Protein-Level Expression of Identified UbRGs
The prognostic value of ubiquitination-related genes (UbRGs) in cancer is increasingly recognized, with recent studies identifying multi-gene signatures capable of predicting patient survival in cervical, ovarian, esophageal, and lung cancers [16] [28] [17]. However, transitioning from computationally identified UbRG signatures to clinically relevant biomarkers requires rigorous protein-level validation. This guide compares the performance, applications, and limitations of major experimental strategies for confirming protein expression of UbRGs, providing researchers with data-driven insights for selecting appropriate validation methodologies.
Comparative Analysis of Protein Validation Techniques
The table below summarizes the key characteristics of major technologies used for validating UbRG protein expression.
Table 1: Performance Comparison of Major Protein Validation Techniques
| Technique | Throughput | Sensitivity | Quantitative Capability | Spatial Context | Key Applications in UbRG Validation |
|---|---|---|---|---|---|
| IHC | Medium | Moderate | Semi-quantitative | Preserved | Tissue localization, differential expression between tumor/normal samples [91] |
| ICC/IF | Medium | Moderate | Semi-quantitative | Preserved (cellular) | Subcellular localization, co-localization studies [92] |
| Western Blot | Low | Moderate | Semi-quantitative | Lost | Specificity confirmation, molecular weight verification [92] |
| Flow Cytometry | High | High | Quantitative | Limited | Surface UbRG expression, immune cell profiling [93] |
| ELISA | High | High | Quantitative | Lost | Biomarker quantification in patient sera/lysates [91] [94] |
| LC-MS/MS | Medium | Very High | Quantitative | Lost | Unbiased quantification, PTM characterization [94] |
Experimental Protocols for Key Validation Methods
Immunohistochemistry (IHC) Protocol for Tissue Validation
IHC provides spatial context for UbRG expression within tumor microenvironments, crucial for understanding cancer biology [91]. The following protocol has been employed in UbRG validation studies:
- Tissue Preparation: Use formalin-fixed, paraffin-embedded (FFPE) tissue sections (4-5 μm thickness) from both tumor and adjacent normal tissues.
- Antigen Retrieval: Perform heat-induced epitope retrieval using citrate buffer (pH 6.0) or EDTA buffer (pH 8.0) at 95-100°C for 20-30 minutes.
- Blocking and Primary Antibody Incubation: Block endogenous peroxidase with 3% H₂O₂, then block nonspecific sites with 5% normal serum. Incubate with validated anti-UbRG primary antibodies overnight at 4°C.
- Detection and Visualization: Apply appropriate secondary antibodies conjugated with enzyme (e.g., HRP) followed by DAB chromogen substrate. Counterstain with hematoxylin.
- Scoring and Analysis: Use semi-quantitative scoring systems (e.g., H-score) incorporating staining intensity (0-3+) and percentage of positive cells [91].
Orthogonal Antibody Validation for UbRGs
Confirming antibody specificity is paramount for UbRG validation, particularly given the challenges of ubiquitination pathways [93] [92]. The following table outlines essential validation approaches:
Table 2: Antibody Validation Strategies for Ubiquitination Research
| Validation Method | Experimental Approach | Interpretation of Positive Results | Key Considerations for UbRGs |
|---|---|---|---|
| Genetic Knockout/Knockdown | CRISPR-Cas9 KO or siRNA knockdown in cell lines followed by Western blot/ICC | Significant reduction or elimination of signal in KO/KD samples | Partial knockdown may be insufficient for low-abundance UbRGs [92] |
| Orthogonal Antibodies | Compare two antibodies recognizing different epitopes of the same UbRG | Concordant staining patterns across multiple cell types | Limited by availability of multiple validated antibodies [92] |
| Tagged Protein Expression | Express tagged (e.g., GFP, FLAG) UbRG in cell lines without endogenous expression | Colocalization of antibody signal and tag detection | Overexpression may mask off-target binding; ensure endogenous expression levels [93] |
| Correlation with Omics Data | Compare antibody staining intensity with RNA-seq or proteomics data from multiple cell lines | Correlation between protein detection and transcript/protein abundance | Does not prove direct binding but supports specificity [93] |
Mass Spectrometry-Based Validation (LC-MS/MS)
Liquid chromatography-tandem mass spectrometry (LC-MS/MS) provides highly specific, antibody-independent UbRG quantification, overcoming limitations of immunoassays [94]:
- Sample Preparation: Extract proteins from tissue homogenates or cell lysates. Digest with trypsin to create peptides. For ubiquitination-specific studies, include enrichment steps using ubiquitin remnant motifs.
- Chromatographic Separation: Separate peptides using reverse-phase LC with acetonitrile gradients.
- Mass Spectrometry Analysis: Analyze eluted peptides using high-resolution tandem MS with data-dependent acquisition.
- Data Analysis: Identify and quantify UbRGs by searching fragmentation spectra against protein databases. Normalize using internal standards or label-free quantification.
Recent studies demonstrate LC-MS/MS's superiority over ELISA for specific hormone measurements, with machine learning classification models revealing significantly better results with MS-based approaches [94].
Research Reagent Solutions for UbRG Validation
The table below outlines essential reagents and their applications in UbRG validation workflows.
Table 3: Key Research Reagents for Ubiquitination-Related Protein Validation
| Reagent Category | Specific Examples | Research Applications | Function in Validation |
|---|---|---|---|
| Validated Antibodies | Anti-MMP1, Anti-RNF2, Anti-FBXO45 [16] [17] | IHC, Western Blot, Flow Cytometry | Primary detection of UbRG targets |
| Cell Lines | A2780 (ovarian cancer), HEY (ovarian cancer) [17] | Genetic manipulation, overexpression studies | Provide cellular context for antibody validation |
| CRISPR-Cas9 Tools | KO plasmids, sgRNAs targeting specific UbRGs [92] | Genetic knockout validation | Confirm antibody specificity by signal elimination |
| Expression Plasmids | FLAG-tagged UbRGs, GFP-tagged constructs [93] | Overexpression studies | Confirm antibody detection in controlled systems |
| Mass Spectrometry Standards | Stable isotope-labeled peptides [94] | LC-MS/MS quantification | Enable precise quantification of UbRG expression |
Strategic Workflows for UbRG Validation
The following diagrams illustrate recommended experimental workflows for validating protein-level expression of UbRGs.
Diagram 1: Comprehensive UbRG Validation Workflow
Diagram 2: Antibody Validation Protocol for UbRGs
Validating protein-level expression of computationally identified UbRGs requires a multifaceted approach combining complementary techniques. IHC provides essential spatial context within tumor tissues, while orthogonal antibody validation ensures specificity through genetic and independent antibody approaches. For UbRGs with limited antibody availability, LC-MS/MS offers a powerful antibody-independent alternative with superior specificity and quantitative capabilities. The strategic integration of these methods, following the workflows outlined in this guide, enables robust translation of bioinformatically-derived UbRG signatures into clinically relevant protein biomarkers with validated prognostic value in cancer research.
Integrating Multi-omics Data to Improve Signature Robustness
Cancer prognosis has been revolutionized by molecular signatures, yet their clinical translation is often hindered by limited robustness. Single-omics approaches provide incomplete biological insights, failing to capture the complex interplay between different molecular layers that drive cancer progression. Multi-omics integration addresses this limitation by combining data from genomics, transcriptomics, epigenomics, and other molecular levels to identify more reliable prognostic biomarkers. This approach is particularly valuable for studying complex biological processes like ubiquitination, which plays crucial regulatory roles in tumor development and therapy response. The integration of multi-omics data enhances signature robustness by capturing complementary information, reducing false discoveries, and providing a more comprehensive view of cancer biology. This review examines current methodologies for multi-omics integration, with a specific focus on their application in evaluating ubiquitination-related genes across various cancers, and provides comparative analysis of their performance in prognostic model development.
Multi-omics Integration Frameworks and Methodologies
Integration Strategies and Technical Approaches
Multi-omics data integration employs three primary strategies, each with distinct advantages for prognostic signature development. Early integration combines raw data from different omics layers at the beginning of analysis, potentially capturing complex relationships but facing challenges with dimensionality and data heterogeneity. Intermediate integration processes each omics dataset separately before combining them during feature selection or model building, offering flexibility in handling different data types. Late integration analyzes each omics dataset independently and combines only the final results, preserving dataset-specific characteristics but potentially missing cross-omics interactions [95].
The PRISM framework exemplifies a comprehensive approach to multi-omics survival analysis, systematically evaluating feature selection methods and survival models through a pipeline that selects features within single-omics datasets before integration via feature-level fusion [96]. This framework employs statistical and machine learning techniques including univariate/multivariate Cox filtering and Random Forest importance, alongside survival models such as CoxPH, ElasticNet, GLMBoost, and Random Survival Forest [96]. Adaptive integration approaches using genetic programming have demonstrated particular effectiveness for breast cancer survival analysis, evolving optimal combinations of molecular features associated with cancer outcomes [95].
Comparative Performance of Integration Algorithms
Recent studies have systematically compared multi-omics integration methods for cancer classification. In breast cancer subtype classification, statistical-based approaches like MOFA+ have demonstrated superior performance compared to deep learning-based methods like MoGCN [97]. MOFA+ employs unsupervised factor analysis to capture sources of variation across different omics modalities through latent factors, providing a low-dimensional interpretation of multi-omics data [97]. When evaluated using linear and nonlinear machine learning models, MOFA+ achieved an F1 score of 0.75 in nonlinear classification, outperforming deep learning alternatives and identifying more biologically relevant pathways [97].
For prognostic modeling, machine learning integration has shown significant value. One study analyzing lung adenocarcinoma employed ten machine learning algorithms—including Lasso, Ridge, Elastic Net, Random Forest, and SVM—to identify prognostic genes and stratify patients [98]. The random survival forest method demonstrated particular utility for calculating risk scores that effectively categorized patients into prognostic groups with distinct clinical outcomes [98].
Table 1: Comparison of Multi-omics Integration Approaches
| Integration Method | Key Characteristics | Best Use Cases | Performance Examples |
|---|---|---|---|
| Statistical (MOFA+) | Unsupervised factor analysis using latent factors | Breast cancer subtyping, Feature selection | F1 score: 0.75 in BC subtyping; Identified 121 relevant pathways [97] |
| Deep Learning (MoGCN) | Graph convolutional networks with autoencoders | Pattern recognition in complex datasets | Identified 100 relevant pathways in BC analysis [97] |
| PRISM Framework | Multi-stage feature selection with survival modeling | Survival prediction across cancer types | C-index: BRCA 0.698, CESC 0.754, UCEC 0.754, OV 0.618 [96] |
| Adaptive Genetic Programming | Evolutionary optimization of feature combinations | Biomarker discovery in heterogeneous cancers | C-index of 78.31 (training) and 67.94 (test) in breast cancer [95] |
| Early Integration | Combines raw data from different omics initially | Capturing complex cross-omics relationships | Requires careful handling of dimensionality and heterogeneity [95] |
Ubiquitination-Related Gene Signatures in Cancer Prognosis
Ubiquitination Processes and Cancer Relevance
Ubiquitination is a crucial post-translational modification process involving the covalent attachment of ubiquitin to target proteins, thereby modifying substrates for degradation or stabilization. This process is mediated by the coordinated action of E1 ubiquitin-activating enzymes, E2 ubiquitin-conjugating enzymes, and E3 ubiquitin ligases [17]. These enzymes play critical roles in regulating diverse cellular processes including tumor proliferation, invasion, apoptosis, DNA damage response, metabolism, immune responses, and drug resistance [17]. The ubiquitin-proteasome system has emerged as a promising therapeutic target, with PROTACs (proteolysis-targeting chimeras) offering novel approaches for precision cancer therapy [17].
Dysregulation of ubiquitination pathways contributes significantly to cancer development and progression. Pathogenic mutations in ubiquitination-related genes such as BRCA1 substantially increase cancer risk, with BRCA1 mutations elevating ovarian cancer risk by 75-fold [17]. Approximately 50 ubiquitination-related genes have been targeted by PROTACs, with several emerging as promising clinical targets for cancer treatment [17]. The systematic analysis of ubiquitination-related genes across cancer types provides valuable insights for prognostic model development and therapeutic targeting.
Performance of Ubiquitination-Based Prognostic Signatures
Ubiquitination-related gene signatures have demonstrated robust prognostic value across multiple cancer types. In ovarian cancer, a 17-gene ubiquitination-based prognostic model showed consistent performance with AUC values of 0.703, 0.704, and 0.705 for 1-year, 3-year, and 5-year overall survival prediction, respectively [99] [17]. The high-risk group identified by this signature had significantly lower overall survival and distinct immune microenvironment characteristics, including lower levels of CD8+ T cells, M1 macrophages, and follicular cells [99] [17].
Similar approaches in colorectal cancer developed a 14-gene ubiquitination-related pathway gene signature (URPGS) that effectively stratified patients into high-risk and low-risk groups for overall survival [100]. The URPGS correlated with advanced clinical stages, lymph node metastasis, and recurrence, with higher scores associated with poorer post-chemotherapy survival outcomes [100]. Through machine learning integration, HSPA1A was identified as a key regulator in colorectal cancer progression, with experimental validation confirming its role in promoting cell proliferation, migration, and invasion [100].
In diffuse large B-cell lymphoma (DLBCL), a 3-gene ubiquitination signature comprising CDC34, FZR1, and OTULIN effectively predicted patient outcomes [15]. Elevated expression of CDC34 and FZR1 coupled with low OTULIN expression correlated with poor prognosis, and the signature demonstrated significant associations with immune microenvironment composition and drug sensitivity [15].
Table 2: Ubiquitination-Related Prognostic Signatures Across Cancers
| Cancer Type | Signature Size | Performance Metrics | Key Genes | Experimental Validation |
|---|---|---|---|---|
| Ovarian Cancer | 17 genes | 1-year AUC: 0.703, 3-year AUC: 0.704, 5-year AUC: 0.705 [99] [17] | FBXO45 | FBXO45 promotes growth, spread, migration via Wnt/β-catenin pathway [17] |
| Colorectal Cancer | 14 genes | Significant stratification of high/low risk groups (p<0.05) [100] | HSPA1A | Knockdown inhibited proliferation, migration, invasion in vitro and in vivo [100] |
| DLBCL | 3 genes | Significant survival difference between risk groups (p<0.05) [15] | CDC34, FZR1, OTULIN | Correlation with endocytosis mechanisms, T-cell infiltration, and drug sensitivity [15] |
Experimental Protocols and Methodologies
Multi-omics Data Processing and Integration Workflow
Standardized protocols for multi-omics data processing are essential for robust prognostic signature development. The PRISM framework exemplifies a comprehensive approach, retrieving data from TCGA using the UCSCXenaTools R package and processing multiple omics modalities including gene expression (GE), DNA methylation (DM), miRNA expression (ME), and copy number variations (CNV) [96]. For gene expression data, features with more than 20% missing values are typically removed, with retention of the top 10% most variable genes using a 90th percentile variance threshold [96]. miRNA processing often excludes features with over 20% missing values, retaining only miRNAs present in more than 50% of samples with non-zero expression [96]. DNA methylation data is commonly restricted to specific CpG probes (e.g., 27k) to enable cross-cancer comparisons, while CNV data processed via the GISTIC2 algorithm requires minimal additional processing [96].
Batch effect correction represents a critical step in multi-omics integration. Effective approaches include unsupervised ComBat through the Surrogate Variable Analysis (SVA) package for transcriptomic and microbiomics data, with the Harman method implemented for methylation data [97]. Following quality control and normalization, feature selection methods such as LASSO Cox regression analysis identify the most valuable prognostic genes, often with ten-fold cross-validation to determine optimal penalty parameters [15] [100].
Diagram 1: Multi-omics Integration Workflow. This diagram illustrates the standard workflow for developing prognostic signatures from multi-omics data, from initial collection through experimental validation.
Ubiquitination-Related Gene Signature Development
The development of ubiquitination-specific prognostic signatures follows a systematic bioinformatics pipeline. Researchers typically begin by compiling a comprehensive list of ubiquitination-related genes from databases such as the UUCD (Ubiquitin and Ubiquitin-like Conjugation Database), which includes approximately 929 genes categorized into E1 (8 genes), E2 (39 genes), and E3 (882 genes) enzymes [17]. Differential expression analysis between tumor and normal tissues identifies ubiquitination-related genes with significant expression changes, often using thresholds of |logFC| ≥ 1 and adjusted p-value < 0.01 [17].
Prognostic model construction typically employs multivariate Cox regression with LASSO regularization to select the most informative genes and prevent overfitting. The risk score is calculated using the formula: Risk score = Σ(Coefi × Expri), where Coefi represents the regression coefficient and Expri denotes the gene expression level [17] [15] [100]. Patients are stratified into high-risk and low-risk groups based on the median risk score, with model performance evaluated through Kaplan-Meier survival analysis, time-dependent ROC curves, and validation in independent cohorts [17] [15].
Functional validation of key genes often includes in vitro experiments such as cell proliferation assays (CCK-8), wound healing assays, Transwell invasion assays, and in vivo models including zebrafish xenografts [100]. For example, FBXO45 validation in ovarian cancer demonstrated its role in promoting cancer growth, spread, and migration via the Wnt/β-catenin pathway [17], while HSPA1A knockdown in colorectal cancer significantly inhibited cell proliferation, migration, and invasion [100].
Successful multi-omics integration relies on specialized computational tools and comprehensively annotated datasets. The Cancer Genome Atlas (TCGA) represents the primary data source, providing multi-omics profiles across numerous cancer types, accessible through platforms such as UCSC Xena and cBioPortal [96] [97]. The Gene Expression Omnibus (GEO) database supplies additional validation datasets with clinical information, while ubiquitination-specific gene sets are available from the Molecular Signatures Database (MSigDB) and Ubiquitin and Ubiquitin-like Conjugation Database (UUCD) [17] [100].
For computational analysis, R packages including "limma" for differential expression, "glmnet" for LASSO regression, "survival" for survival analysis, and "clusterProfiler" for functional enrichment form the core analytical toolkit [17] [15] [100]. Multi-omics integration frequently employs MOFA+ for statistical integration or deep learning frameworks like MoGCN for complex pattern recognition [97]. Single-cell RNA sequencing analysis typically utilizes the Seurat package for quality control, normalization, and cell type annotation [17] [98].
Table 3: Essential Research Resources for Multi-omics Integration
| Resource Category | Specific Tools/Databases | Primary Function | Application in Research |
|---|---|---|---|
| Data Resources | TCGA, GEO, GTEx | Provide multi-omics data with clinical annotations | Primary data source for model development and validation [96] [17] |
| Ubiquitination Databases | UUCD, MSigDB | Curated lists of ubiquitination-related genes | Reference for identifying ubiquitination-related features [17] [100] |
| Statistical Analysis | limma, survival, survminer | Differential expression and survival analysis | Identify prognostic genes and assess clinical utility [17] [15] |
| Machine Learning | glmnet, randomForest, XGBoost | Feature selection and model building | Develop prognostic signatures and stratify patients [98] [100] |
| Multi-omics Integration | MOFA+, MoGCN, PRISM | Integrate multiple omics datasets | Identify cross-omics patterns and biomarkers [96] [97] |
| Experimental Validation | CCK-8, Transwell, zebrafish models | Functional assessment of candidate genes | Verify biological role of key signature genes [17] [100] |
Experimental Validation Reagents
Functional validation of ubiquitination-related prognostic genes requires specific reagents and model systems. Key laboratory reagents include cell culture media (DMEM, RPMI 1640) supplemented with fetal bovine serum, penicillin-streptomycin solutions, transfection reagents such as Lipo8000, and antibodies for Western blot analysis [17]. Commercially available cell counting kits (CCK-8) enable proliferation assays, while Transwell chambers coated with Matrigel facilitate invasion assays [100].
For in vivo validation, zebrafish xenograft models provide a versatile platform for assessing tumor growth and metastatic potential [100]. These systems are particularly valuable for evaluating genes identified through bioinformatics analyses, such as FBXO45 in ovarian cancer and HSPA1A in colorectal cancer [17] [100]. Additional functional assays may include quantitative real-time PCR for gene expression quantification, flow cytometry for apoptosis analysis, and dual-luciferase reporter assays for investigating transcriptional regulation [98].
Multi-omics integration significantly enhances the robustness of prognostic signatures in cancer research by capturing complementary biological information across molecular layers. Statistical approaches like MOFA+ demonstrate particular strength in feature selection for cancer subtyping, while machine learning integration enables effective patient stratification based on ubiquitination-related gene signatures. These signatures have shown consistent prognostic value across diverse cancers including ovarian, colorectal, and lymphoid malignancies, with performance metrics validating their clinical potential.
The integration of ubiquitination-related genes into prognostic models provides not only predictive power but also insights into therapeutic targets, especially with the emergence of PROTAC-based therapies. Standardized workflows encompassing rigorous bioinformatics analysis followed by experimental validation remain essential for developing clinically relevant signatures. As multi-omics technologies evolve and datasets expand, integrated approaches will increasingly drive precision oncology forward, enabling more accurate prognosis and personalized treatment strategies based on comprehensive molecular profiling.
Clinical Validation and Comparative Analysis Across Cancer Types
Pan-Cancer Validation of Ubiquitination-Related Prognostic Signatures
In the evolving landscape of oncology, the pursuit of robust prognostic biomarkers has increasingly focused on molecular signatures that transcend individual cancer types. Among these, ubiquitination-related gene signatures have emerged as powerful predictors of clinical outcomes across diverse malignancies. The ubiquitin-proteasome system (UPS), a critical post-translational modification pathway regulating approximately 80-90% of intracellular protein degradation, represents a cornerstone of cellular homeostasis whose dysregulation is intimately linked with tumorigenesis and cancer progression [36] [18]. This review synthesizes current evidence validating ubiquitination-related prognostic signatures across multiple cancer types, examining their performance characteristics, methodological frameworks for development, and implications for clinical translation in the era of personalized oncology.
Comparative Performance of Ubiquitination-Related Prognostic Signatures
Table 1: Ubiquitination-Related Prognostic Signatures Across Cancer Types
| Cancer Type | Key Ubiquitination-Related Genes | Performance (AUC) | Clinical Validation | Immune Correlates |
|---|---|---|---|---|
| Cervical Cancer | MMP1, RNF2, TFRC, SPP1, CXCL8 | 1-year: >0.6, 3-year: >0.6, 5-year: >0.6 [16] | TCGA-GTEx-CESC, self-seq data [16] | Correlated with memory B cells, M0 macrophages, immune checkpoints [16] |
| Lung Adenocarcinoma | DTL, UBE2S, CISH, STC1 | HR = 0.54, 95% CI: 0.39-0.73, p < 0.001 [26] | 6 external validation cohorts [26] | Higher PD1/L1, TMB, TNB, TME scores in high-risk group [26] |
| Ovarian Cancer | 17-gene signature including FBXO45 | 1-year: 0.703, 3-year: 0.704, 5-year: 0.705 [17] | GSE165808, GSE26712 [17] | Enhanced CD8+ T cells, M1 macrophages in low-risk group [17] |
| Diffuse Large B-Cell Lymphoma | CDC34, FZR1, OTULIN | Significant survival stratification (p<0.05) [15] | GSE181063, GSE56315, GSE10846 [15] | Associated with endocytosis, T-cell infiltration, drug sensitivity [15] |
| Pan-Cancer (5 solid tumors) | URPS signature | Consistent stratification across cancer types [36] | 4,709 patients from 26 cohorts [36] | Correlation with macrophage infiltration, immunotherapy response [36] |
The consistent performance of ubiquitination-related signatures across distinct cancer types underscores their fundamental role in tumor biology. The pan-cancer ubiquitination regulatory network analysis demonstrated that a conserved ubiquitination-related prognostic signature (URPS) effectively stratified patients into high-risk and low-risk groups with distinct survival outcomes across all analyzed cancers, including lung cancer, esophageal cancer, cervical cancer, urothelial cancer, and melanoma [36]. This cross-cancer validation highlights the fundamental role of ubiquitination pathways in determining tumor behavior irrespective of tissue origin.
Methodological Framework for Signature Development
Standardized Bioinformatics Pipeline
The development of ubiquitination-related prognostic signatures follows a methodological framework that integrates multi-omics data with clinical outcome measures:
Diagram 1: Methodological workflow for developing ubiquitination-related prognostic signatures, illustrating the sequential steps from data acquisition to functional validation.
Key Analytical Techniques
Differential Expression Analysis: Identification of differentially expressed genes (DEGs) between tumor and normal tissues using packages such as DESeq2 (v1.36.0) with thresholds of p-value <0.05 and |log2Fold Change| >0.5 [16]. The limma package is alternatively employed with criteria of Fold Change >2 and FDR <0.05 [15].
Ubiquitination Gene Filtering: Intersection of DEGs with curated ubiquitination-related gene sets from specialized databases including UUCD (Ubiquitin and Ubiquitin-like Conjugation Database) containing 929 ubiquitination-related genes [17], or GeneCards database using "Ubiquitin-like modifiers" as keywords with relevance score ≥3, yielding 465 ubiquitination-related genes [16].
Prognostic Model Construction: Univariate Cox regression initially identifies ubiquitination-related genes with significant survival association (p<0.05) [16] [17]. Least absolute shrinkage and selection operator (LASSO) Cox regression with 10-fold cross-validation then selects the most informative genes while preventing overfitting [15] [26]. Risk scores are calculated using the formula: Risk score = Σ(Coefi × Expressioni), where Coef_i represents the regression coefficient from multivariate Cox analysis [17] [26].
Validation Approaches: Models are typically validated through internal training-test set splits (e.g., 7:3 ratio) [16] and external validation using independent GEO datasets [26] or cross-cancer validation in pan-cancer studies [36]. Performance is assessed via Kaplan-Meier survival analysis, time-dependent receiver operating characteristic (ROC) curves, and concordance index (C-index) calculations [16].
Molecular Mechanisms and Signaling Pathways
Ubiquitination-related prognostic signatures exert their influence through several interconnected biological pathways that determine tumor behavior and therapeutic response:
Diagram 2: Molecular mechanisms linking ubiquitination signatures to cancer progression and treatment response, showing the pathway from core ubiquitination machinery to clinical implications.
The OTUB1-TRIM28 ubiquitination axis has been identified as a key regulator modulating the MYC pathway and influencing patient prognosis across multiple cancers [36]. In ovarian cancer, FBXO45, an E3 ubiquitin ligase component of prognostic signatures, promotes tumor growth, spread, and migration via the Wnt/β-catenin pathway [17]. Additionally, ubiquitination signatures consistently correlate with immune checkpoint expression and immune cell infiltration patterns, particularly CD8+ T cells and macrophages, providing a molecular bridge between the ubiquitin-proteasome system and antitumor immunity [16] [17] [26].
Table 2: Key Research Reagents and Databases for Ubiquitination-Related Cancer Research
| Resource | Type | Primary Application | Key Features |
|---|---|---|---|
| TCGA Database | Data Repository | Gene expression analysis | Multi-omics data for 33 cancer types [36] [18] |
| GTEx Database | Data Repository | Normal tissue comparison | Normal tissue transcriptomes for reference [16] [17] |
| GEO Datasets | Data Repository | Validation cohorts | Independently generated gene expression data [15] [26] |
| UUCD 2.0 | Specialized Database | Ubiquitination gene curation | 966 ubiquitination-related genes with classification [26] |
| CIBERSORT | Computational Tool | Immune infiltration analysis | Deconvolutes immune cell fractions from expression data [16] [15] |
| DESeq2 | Bioinformatics Package | Differential expression | Identifies significantly dysregulated genes [16] |
| cBioPortal | Analysis Platform | Genomic alteration analysis | Mutation, CNA, and expression integration [101] [18] |
| ESTIMATE | Computational Tool | TME scoring | Calculates stromal and immune scores in TME [17] |
Discussion and Clinical Implications
The accumulating evidence for ubiquitination-related prognostic signatures underscores their dual utility as both predictive biomarkers and potential therapeutic targets. The consistent performance of these signatures across multiple cancer types suggests they capture fundamental biological processes driving cancer progression rather than tissue-specific phenomena. Several important implications emerge from these findings:
First, ubiquitination signatures offer enhanced prognostic stratification beyond conventional clinicopathological parameters. In lung adenocarcinoma, the ubiquitination-related risk score (URRS) demonstrated significant predictive power for overall survival (HR=0.54, p<0.001) and was validated across six independent cohorts [26]. Similarly, in ovarian cancer, the 17-gene ubiquitination signature maintained stable predictive performance across 1, 3, and 5-year survival endpoints (AUC: 0.703-0.705) [17].
Second, the strong association between ubiquitination signatures and immune microenvironment composition positions them as potential biomarkers for immunotherapy response. The observed correlations with immune checkpoint expression, T-cell infiltration, and tumor mutational burden suggest these signatures may help identify patients most likely to benefit from immune checkpoint inhibition [36] [26]. This is particularly relevant given the emerging role of ubiquitination in regulating PD-1/PD-L1 dynamics [36].
Third, the experimental validation of signature components like FBXO45 in ovarian cancer [17] and UBE2T in pancreatic cancer models [18] provides mechanistic insights and nominates potential therapeutic targets. The development of proteolysis-targeting chimeras (PROTACs) that specifically target ubiquitin enzymes further highlights the therapeutic relevance of these findings [17].
The pan-cancer validation of ubiquitination-related prognostic signatures represents a significant advancement in molecular oncology with dual implications for prognostication and therapeutic development. The consistent performance of these signatures across cervical cancer, lung adenocarcinoma, ovarian cancer, DLBCL, and other malignancies underscores the fundamental role of ubiquitination pathways in determining cancer behavior. Future research directions should focus on prospective validation in clinical trials, functional characterization of signature components, and development of targeted therapies exploiting these pathways. As the ubiquitin-proteasome system continues to reveal its complexity, ubiquitination-related signatures are poised to become integral components of precision oncology approaches across cancer types.
Comparative Performance Against Traditional Staging Systems
The TNM (Tumor, Node, Metastasis) staging system has served as the cornerstone of cancer prognosis and treatment decisions for decades. This traditional framework classifies cancer based on anatomical characteristics: the size and extent of the primary tumor (T), the involvement of regional lymph nodes (N), and the presence of distant metastasis (M). While invaluable for initial stratification, its predictive power is fundamentally limited, with studies indicating it achieves only approximately 57-60% accuracy for predicting overall survival in cancers like laryngeal cancer [102]. This limitation stems from its inability to capture the underlying molecular heterogeneity of tumors, which significantly influences clinical outcomes and therapeutic responses.
Ubiquitination, a crucial post-translational modification that regulates protein degradation and signaling pathways, is deeply implicated in cancer initiation and progression [26]. The ubiquitin-proteasome system (UPS) involves a cascade of enzymes—E1 (activating), E2 (conjugating), and E3 (ligating)—that control the stability and function of numerous oncoproteins and tumor suppressors [16]. The integration of ubiquitination-related gene (UbRG) signatures represents a paradigm shift in prognostic assessment. These multi-gene biomarkers move beyond anatomical description to quantify the molecular drivers of tumor behavior, offering a more nuanced and biologically grounded approach to risk stratification. This review provides a comparative analysis of the prognostic performance of these emerging UbRG signatures against traditional staging systems across various cancer types.
Performance Comparison of Ubiquitination-Related Gene Signatures
Table 1: Comparative Performance of Ubiquitination-Related Gene Signatures vs. Traditional Staging
| Cancer Type | UbRG Signature Genes | Performance of UbRG Signature (AUC) | Performance of TNM Stage (AUC) | Reference & Dataset |
|---|---|---|---|---|
| Laryngeal Cancer | PPARG, LCK, LHX1 | 1-year OS: 0.7373-year OS: 0.7625-year OS: 0.793 [102] | ~0.57-0.60 [102] | TCGA-LC, GSE65858 |
| Lung Adenocarcinoma (LUAD) | DTL, UBE2S, CISH, STC1 | HR = 0.58, 95% CI: 0.36–0.93, p<0.023 (Validation cohorts) [26] | Not specified | TCGA-LUAD, 6 GEO cohorts |
| Epithelial Ovarian Carcinoma (EOC) | HSP90AB1, FBXO9, SIGMAR1, STAT1, SH3KBP1, EPB41L2, DNAJB6, VPS18, PPM1G, AKAP12, FRK, PYGB | 1-year OS: 0.7373-year OS: 0.7625-year OS: 0.793 [74] | Not specified | TCGA-EOC |
| Diffuse Large B-Cell Lymphoma (DLBCL) | CDC34, FZR1, OTULIN | Significant separation of survival curves in high/low-risk groups (p<0.05) [49] | Not applicable (Lymphoma uses Ann Arbor staging) | GSE10846, GSE181063 |
| Cervical Cancer (CC) | MMP1, RNF2, TFRC, SPP1, CXCL8 | AUC >0.6 for 1/3/5 years [16] | Not specified | Self-seq, TCGA-GTEx-CESC |
Table 2: Association of UbRG Signatures with Clinical and Tumor Microenvironment Features
| Cancer Type | Prognostic Value | Immune Microenvironment Correlation | Therapeutic Prediction |
|---|---|---|---|
| Laryngeal Cancer | Powerful independent prognostic factor [102] | Low-risk group: More activated immune function, higher infiltration of anti-cancer immune cells [102] | Low-risk: More responsive to immune checkpoint inhibitors [102] |
| Lung Adenocarcinoma | URRS group had worse prognosis (HR=0.54, p<0.001) [26] | High URRS: Higher PD1/L1, TMB, TNB, and TME scores (p<0.001) [26] | High URRS: Lower IC50 for various chemotherapy drugs [26] |
| Epithelial Ovarian Carcinoma | High-risk group had significantly worse prognosis [74] | High-risk: Higher abundance of M2 macrophages, cancer-associated fibroblasts; lower TMB [74] | High-risk: Reduced sensitivity to chemotherapy (except dasatinib) [74] |
The data compiled from multiple cancer types consistently demonstrates that ubiquitination-related gene (UbRG) signatures outperform traditional TNM staging in prognostic accuracy. In laryngeal cancer, the UbRG signature showed superior predictive power for overall survival (OS) across 1, 3, and 5 years compared to the TNM stage [102]. Furthermore, these signatures provide critical insights that TNM staging cannot, such as the status of the tumor immune microenvironment and likely response to immunotherapy or chemotherapy [102] [26] [74]. This makes UbRG models not just prognostic tools, but potential guides for personalized treatment selection.
Key Experimental Protocols for UbRG Signature Development
The development and validation of ubiquitination-related gene signatures follow a robust bioinformatics and experimental pipeline. The workflow below illustrates the key stages of this process.
Diagram 1: Workflow for Developing Ubiquitination-Related Gene Signatures.
Data Acquisition and Preprocessing
The process begins with the collection of large-scale genomic and clinical data. Researchers typically obtain RNA-sequencing (RNA-seq) data and corresponding clinical information (e.g., survival time, status, and TNM stage) from public repositories such as The Cancer Genome Atlas (TCGA) and the Gene Expression Omnibus (GEO) [102] [26]. A training cohort (e.g., TCGA) is defined for model development, and one or more independent validation cohorts (e.g., from GEO) are held out for subsequent testing. Ubiquitin-related genes (UbRGs) are systematically collected from specialized databases like iUUCD 2.0 and UbiBrowser [102] [26]. Data preprocessing involves normalizing gene expression values (e.g., to TPM or FPKM) and filtering samples with incomplete clinical information.
Identification of Prognostic Ubiquitination-Related Genes
This phase involves narrowing down the vast number of UbRGs to a concise set with the strongest prognostic value.
- Differential Expression Analysis: The "limma" R package is used to identify UbRGs that are differentially expressed (DUbRGs) between tumor and normal tissues. Criteria such as a false discovery rate (FDR) < 0.05 and an absolute log2 fold change > 1 are typically applied [102].
- Prognostic Gene Screening: A univariate Cox regression analysis is performed on the DUbRGs to identify those significantly associated with overall survival (OS) in the training cohort. Genes with a p-value < 0.05 are considered to have prognostic potential [16] [26].
- Feature Selection via LASSO Regression: To prevent overfitting and select the most robust genes, Least Absolute Shrinkage and Selection Operator (LASSO) Cox regression is employed. This technique penalizes the complexity of the model, shrinking the coefficients of less important genes to zero. The optimal penalty parameter (lambda) is determined via 10-fold cross-validation, resulting in a minimal set of non-zero coefficient genes for the final signature [102] [49].
Model Construction, Validation, and Correlation Analysis
- Risk Model Construction: A ubiquitination-related risk score (URRS) is calculated for each patient using a formula derived from multivariate Cox regression. The formula is:
Risk score = Σ (Coefficient_i * Expression_i)for each of thensignature genes [26] [49]. Patients are then stratified into high-risk and low-risk groups based on the median risk score. - Performance Validation: The prognostic performance of the signature is rigorously assessed. Kaplan-Meier (K-M) survival analysis with log-rank tests is used to evaluate the significance of survival difference between the risk groups. The predictive accuracy is quantified using time-dependent Receiver Operating Characteristic (ROC) curves and the Area Under the Curve (AUC) for 1-, 3-, and 5-year overall survival [102] [16]. The model's stability is confirmed by applying the same risk score formula to the independent validation cohorts.
- Comprehensive Correlation Analysis: The biological and clinical relevance of the signature is explored by analyzing its association with the tumor immune microenvironment (using tools like CIBERSORT and MCP-counter), tumor mutation burden (TMB), expression of immune checkpoints (e.g., PD-1, PD-L1), and sensitivity to chemotherapy/targeted therapies (via R packages like "oncoPredict") [26] [74] [49].
Table 3: Key Research Reagent Solutions for UbRG Signature Development
| Category / Reagent | Specific Examples | Function and Application |
|---|---|---|
| Bioinformatics Databases | TCGA, GEO, cBioPortal, UALCAN, GTEx | Source for high-throughput gene expression data and clinical information [102] [103] [26]. |
| Ubiquitin Gene Compendiums | iUUCD 2.0, UbiBrowser, GeneCards | Curated lists of ubiquitination-related genes (E1, E2, E3, DUBs) for study focus [102] [16] [26]. |
| R Software Packages | "limma" (Differential Expression), "glmnet" (LASSO), "survival" (Cox regression), "survminer" (K-M plots), "CIBERSORT" (Immune deconvolution) | Core tools for statistical analysis, model building, and visualization [102] [26] [49]. |
| Experimental Validation Reagents | qRT-PCR Assays, Western Blot Antibodies, ELISA Kits | Wet-lab validation of signature gene expression and protein levels in cell lines or patient tissues [102] [16] [26]. |
The evidence from multiple cancer types indicates that prognostic models based on ubiquitination-related genes consistently surpass the predictive capability of the traditional TNM staging system. These molecular signatures provide a more accurate and biologically relevant method for risk stratification by directly quantifying processes fundamental to cancer progression. Furthermore, their ability to reveal the state of the tumor immune microenvironment and predict responses to immunotherapy and chemotherapy offers a tangible path toward more personalized and effective cancer treatment. While further clinical validation is needed, UbRG signatures represent a significant advancement in prognostic oncology, moving the field from anatomical description to molecular function.
The ubiquitin-proteasome system, once primarily recognized for its role in protein degradation, has emerged as a critical regulator of tumor immunology. Ubiquitination-related genes (UbRGs) orchestrate complex cellular processes including immune cell activation, cytokine signaling, and antigen presentation, thereby shaping the tumor immune microenvironment (TIME) and influencing response to immunotherapy [80] [74]. The growing appreciation of UbRGs in cancer immunology coincides with the clinical advent of proteolysis-targeting chimeras (PROTACs) that strategically target ubiquitin enzymes, opening new avenues for precision cancer therapy [17]. This review synthesizes current evidence linking UbRG expression patterns with immune landscape alterations and therapeutic responses across multiple cancer types, providing a comparative analysis of prognostic models and their potential clinical applications.
UbRG-Based Prognostic Signatures Across Cancers
Comprehensive bioinformatics analyses have identified distinct UbRG signatures with significant prognostic value across various malignancies. These signatures not only predict patient survival but also correlate with specific immune microenvironment characteristics.
Table 1: Comparative Analysis of UbRG-Based Prognostic Models Across Cancers
| Cancer Type | Key UbRG Biomarkers | Prognostic Performance (AUC) | Immune Correlations | Therapeutic Implications |
|---|---|---|---|---|
| Ovarian Cancer [17] | 17-gene signature (including FBXO45) | 1-year: 0.7033-year: 0.7045-year: 0.705 | ↑ CD8+ T cells, M1 macrophages, follicular cells in low-risk group | JAK2/STAT3/PD-L1 pathway targeting; Wnt/β-catenin inhibition |
| Epithelial Ovarian Carcinoma [74] | 12-gene signature (HSP90AB1, FBXO9, STAT1, etc.) | 1-year: 0.7373-year: 0.7625-year: 0.793 | ↑ B cells, M2 macrophages, neutrophils in high-risk group | Dasatinib sensitivity; Other chemoresistance |
| Cervical Cancer [16] [104] | MMP1, RNF2, TFRC, SPP1, CXCL8 | AUC >0.6 for 1/3/5 years | 12 immune cell types differentially infiltrated; 4 checkpoints altered | Immunotherapy stratification based on risk profile |
| Lung Adenocarcinoma [105] | 9-gene signature (B4GALT4, DNAJB4, HEATR1, etc.) | Significant OS separation (p<0.05) | Negative correlation with most immune cells | TAE684, Cisplatin, Midostaurin sensitivity |
| Laryngeal Cancer [106] | PPARG, LCK, LHX1 | Strong discrimination in validation cohorts | Activated immune function in low-risk group | Chemotherapy for high-risk; ICIs for low-risk |
The consistent pattern emerging across these studies indicates that UbRG-based stratification effectively identifies patients with distinct immune profiles and therapeutic vulnerabilities. Low-risk patients typically demonstrate immunologically "hot" tumors with enhanced cytotoxic immune infiltration, while high-risk patients often exhibit immunosuppressive microenvironments characterized by alternative macrophage polarization and exclusion of effector immune cells [17] [74] [106].
Methodological Framework for UbRG-Immune Microenvironment Analysis
Bioinformatics Pipelines for UbRG Signature Development
The construction of UbRG-based prognostic models follows a systematic bioinformatics workflow that integrates multi-omics data with clinical outcomes:
Data Acquisition and Processing: RNA-seq data and clinical information are sourced from public repositories (TCGA, GTEx, GEO). Normalization procedures include transcripts per kilobase million (TPM) or fragments per kilobase million (FPKM) normalization to account for sequencing depth and gene length [16] [17] [106]. Quality control measures exclude samples with excessive mitochondrial gene content (>15%) or low gene counts (<200) in single-cell analyses [17].
Identification of Differentially Expressed UbRGs: Differential expression analysis between tumor and normal tissues employs packages such as DESeq2 or limma with thresholds typically set at |log2 fold change| > 1 and false discovery rate (FDR) < 0.05 [16] [17]. Ubiquitin-related genes are compiled from specialized databases including UUCD, UbiBrowser, and GeneCards [17] [106].
Prognostic Model Construction: Univariate Cox regression initially identifies survival-associated UbRGs (p < 0.05), followed by least absolute shrinkage and selection operator (LASSO)-Cox regression to prevent overfitting and select the most predictive genes [16] [74]. Risk scores are calculated using the formula:
Risk score = Σ(Coef_i × Expression_i), where Coef_i represents the regression coefficient derived from multivariate Cox analysis [17] [106].Immune Microenvironment Characterization: Immune cell infiltration is quantified using algorithms such as CIBERSORT, TIMER, MCP-counter, and ESTIMATE [17] [74]. These computational approaches deconvolute bulk tumor transcriptomes to infer relative abundances of specific immune cell populations.
Experimental Validation Approaches
Table 2: Experimental Methods for Validating UbRG Functions
| Method Category | Specific Techniques | Application in UbRG Studies | Key Outcomes |
|---|---|---|---|
| Gene Expression Validation | RT-qPCR, Western blot, IHC [16] [17] [106] | Confirm differential expression of identified UbRGs | Verification of MMP1, TFRC, CXCL8 upregulation in cervical cancer [16] |
| Functional Assays | CCK-8, Wound healing, Transwell invasion [105] [17] | Assess proliferation, migration, and invasion | HEATR1 knockdown reduces LUAD cell survival and invasion [105] |
| Mechanistic Studies | Pathway inhibition, Co-immunoprecipitation, ELISA [17] [106] | Elucidate signaling pathways and protein interactions | FBXO45 promotes OC progression via Wnt/β-catenin [17]; PPARG regulates immunosuppressive cytokines [106] |
| Therapeutic Testing | Drug sensitivity assays, ICB response models [74] [106] | Evaluate correlation with treatment response | High-risk EOC patients show dasatinib sensitivity [74] |
UbRG Modulation of Signaling Pathways in Immune Regulation
Ubiquitination-related genes influence immunotherapy response through regulation of critical signaling pathways that bridge tumor cell intrinsic behavior with immune microenvironment modulation:
JAK2/STAT3/PD-L1 Axis in Ovarian Cancer
In ovarian cancer, Ube2j1 was identified as a key regulator of malignant progression through activation of the JAK2/STAT3/PD-L1 pathway [80]. This signaling cascade creates an immunosuppressive feedback loop wherein STAT3 activation increases PD-L1 expression on tumor cells, facilitating T-cell exhaustion and immune evasion. The UbRG-mediated control of this axis provides a mechanistic basis for the correlation between high-risk signatures and suppressed anti-tumor immunity, suggesting potential for combination therapies targeting both ubiquitination pathways and immune checkpoints.
Wnt/β-Catenin Pathway Regulation
The E3 ubiquitin ligase FBXO45 was experimentally demonstrated to promote ovarian cancer growth, spread, and migration via the Wnt/β-catenin pathway [17]. As Wnt signaling has established roles in modulating T-cell differentiation and dendritic cell function, this connection reveals how UbRGs can simultaneously drive tumor progression and shape the immune landscape. The identification of such dual-function pathways highlights the potential for targeted interventions that disrupt tumor-intrinsic mechanisms while concurrently enhancing anti-tumor immunity.
Table 3: Key Research Reagents and Platforms for UbRG-Immune Microenvironment Studies
| Resource Category | Specific Tools | Function/Application | Reference |
|---|---|---|---|
| Bioinformatics Platforms | UCSC Xena, GEO, TCGA | Data retrieval and integration | [16] [17] [106] |
| UbRG Databases | UUCD, UbiBrowser, GeneCards | Comprehensive UbRG compendiums | [17] [106] |
| Analysis Packages | DESeq2, limma, edgeR | Differential expression analysis | [16] [17] |
| Immune Deconvolution Algorithms | CIBERSORT, TIMER, MCP-counter, ESTIMATE | Immune cell infiltration quantification | [17] [74] |
| Experimental Reagents | Lipo8000 transfection reagent, specific antibodies | Functional validation experiments | [17] |
| Cell Lines | A2780, HEY (ovarian cancer) | In vitro mechanistic studies | [17] |
Clinical Translation and Therapeutic Implications
The integration of UbRG signatures into clinical decision-making frameworks offers promising avenues for treatment personalization:
Predictive Biomarkers for Immunotherapy
UbRG-based classification demonstrates significant utility in predicting response to immune checkpoint inhibitors (ICIs). In laryngeal cancer, the three-gene UbRG signature (PPARG, LCK, LHX1) identified patients with more activated immune function, higher infiltration of anti-cancer immune cells, and stronger expression of immune-promoting cytokines in the low-risk group, suggesting enhanced likelihood of ICI response [106]. Similarly, in ovarian cancer, distinct immune checkpoint expression patterns were observed between UbRG-based risk groups, providing biomarkers for patient selection [74].
Companion Diagnostics for Targeted Therapies
Beyond immunotherapy prediction, UbRG signatures inform sensitivity to various targeted agents. For instance, in lung adenocarcinoma, drug sensitivity analysis revealed that TAE684, Cisplatin, and Midostaurin exhibited the strongest negative correlation with risk scores [105]. This suggests that UbRG profiling could guide selection of conventional and targeted therapies based on individual tumor molecular features, potentially overcoming resistance mechanisms governed by the ubiquitin-proteasome system.
Nomogram Integration for Personalized Prognostication
Several studies have combined UbRG signatures with clinical parameters to generate nomograms that provide individualized survival probability estimates [17] [106]. These integrative models demonstrate superior predictive accuracy compared to traditional staging systems alone, offering clinicians a practical tool for risk stratification and treatment intensification or de-escalation decisions.
The comprehensive analysis of ubiquitination-related genes across multiple cancer types reveals their profound influence on tumor immune microenvironments and therapy responses. The consistent pattern emerging from these studies positions UbRG signatures as robust prognostic biomarkers with potential to guide both immunotherapy selection and targeted therapy approaches. Future research directions should include prospective validation of these signatures in clinical trial cohorts, functional dissection of novel UbRG-mediated immune regulatory mechanisms, and development of UbRG-targeted therapeutics such as PROTACs that simultaneously modulate oncogenic signaling and immune recognition. As our understanding of the ubiquitin-immune interface deepens, UbRG-based classification promises to become an increasingly essential component of precision oncology frameworks.
Within the field of cancer research, the ubiquitination process has emerged as a critical regulatory mechanism influencing tumor progression, metastasis, and therapeutic response. Ubiquitination-related genes (UbRGs) encode enzymes and binding proteins that orchestrate the precise control of protein stability, localization, and activity. The development of multi-gene signatures based on UbRGs represents a cutting-edge approach for prognostic prediction and treatment stratification in oncology. This guide provides an objective comparison of validated UbRG signatures across multiple cancer types, supported by experimental data and detailed methodologies for research application.
Comparative Analysis of Validated UbRG Signatures
The table below summarizes key validated ubiquitination-related gene signatures across various cancers, highlighting their prognostic value and validation approaches.
Table 1: Validated Ubiquitination-Related Gene Signatures in Specific Cancers
| Cancer Type | Key UbRG Signature Genes | Prognostic Value | Validation Approach | Clinical Implications |
|---|---|---|---|---|
| Ovarian Cancer [25] | 17-gene signature including FBXO45 | 1-year AUC: 0.703; 3-year AUC: 0.704; 5-year AUC: 0.705 | TCGA/GTEx datasets; experimental validation of FBXO45 | High-risk group had lower overall survival (P<0.05); FBXO45 promotes growth via Wnt/β-catenin pathway |
| Lung Adenocarcinoma [26] | DTL, UBE2S, CISH, STC1 | HR = 0.54, 95% CI: 0.39-0.73, p<0.001 | 6 external validation cohorts; RT-qPCR confirmation | High-risk associated with higher PD1/L1 expression, TMB, TNB, and TME scores |
| Cervical Cancer [16] | MMP1, RNF2, TFRC, SPP1, CXCL8 | AUC >0.6 for 1/3/5 years | Self-seq and TCGA-GTEx-CESC datasets; RT-qPCR validation | Model predicts survival; 12 immune cell types differed between risk groups |
| Colorectal Cancer [107] | 14-gene URPGS including HSPA1A | Significant survival stratification (p<0.001) | LASSO regression; in vitro/in vivo HSPA1A validation | Correlated with advanced stage, lymph node metastasis, and recurrence |
| Colon Cancer [108] | ARHGAP4, MID2, SIAH2, TRIM45, UBE2D2, WDR72 | Significant survival differences (p<0.05) | NMF clustering; in vitro/in vivo WDR72 validation | Low-risk group showed better response to CTLA4 inhibitors |
| Diffuse Large B-Cell Lymphoma [15] | CDC34, FZR1, OTULIN | Significant survival correlation (p<0.05) | Three GEO datasets; single-cell analysis | High CDC34/FZR1 and low OTULIN with poor prognosis |
| Breast Cancer [27] | ATG5, FBXL20, DTX4, BIRC3, TRIM45, WDR78 | Significant survival differences (p<0.05) | Multiple external datasets (TCGA-BRAC, GSE1456, etc.) | Superior predictive ability compared to traditional clinical indicators |
Detailed Methodologies for UbRG Signature Development
Bioinformatics Workflow for Signature Identification
The development of UbRG signatures follows a systematic bioinformatics pipeline, as demonstrated across multiple cancer studies [25] [16] [107]. The standard workflow encompasses several critical stages that ensure robust signature development.
Diagram 1: UbRG Signature Development Workflow. This standardized pipeline illustrates the multi-step process for identifying and validating ubiquitination-related gene signatures across cancer types.
Key Statistical and Machine Learning Approaches
The construction of UbRG signatures employs sophisticated analytical methods to ensure prognostic robustness:
Feature Selection: Univariate Cox regression initially identifies UbRGs with prognostic potential (p<0.05), followed by Least Absolute Shrinkage and Selection Operator (LASSO) regression to prevent overfitting and select the most relevant genes [25] [16] [107]. For example, in the ovarian cancer study, this approach distilled 162 co-expressed UbRGs down to a final 17-gene signature [25].
Risk Score Calculation: The ubiquitination-related risk score (URRS) is computed using the formula:
Risk score = Σ(Coefi × Expri)
where Coefi represents the regression coefficient from multivariate Cox analysis, and Expri denotes the gene expression level [26]. Patients are stratified into high- and low-risk groups based on median risk score cutoff.
Validation Frameworks: Successful signatures undergo rigorous internal validation (training/test splits) and external validation across multiple independent cohorts (e.g., GEO datasets) [25] [26]. Model performance is assessed through Kaplan-Meier survival analysis, time-dependent receiver operating characteristic (ROC) curves, and calculation of the concordance index (C-index).
Advanced Machine Learning Integration: Some studies implement comprehensive machine learning frameworks comparing 117 algorithm combinations to identify optimal prognostic models [82]. Random Survival Forests, Ridge regression, and other algorithms complement traditional statistical methods.
Experimental Validation Protocols
Functional Characterization of Key UbRG Targets
Following bioinformatics identification, experimental validation is crucial for establishing biological relevance. The table below outlines common experimental approaches and their applications in UbRG studies.
Table 2: Experimental Methods for UbRG Signature Validation
| Method Category | Specific Techniques | Application Examples | Key Outcomes |
|---|---|---|---|
| In Vitro Functional Assays | CCK-8 proliferation, wound healing, Transwell invasion, RT-qPCR, Western blot | CRC (HSPA1A) [107], LUAD (HEATR1) [105], PCa (USP21) [109] | Confirmed roles in proliferation, migration, invasion |
| In Vivo Models | Mouse xenografts, zebrafish xenograft models | CRC (HSPA1A) [107], PCa (USP21) [109] | Demonstrated effects on tumor growth and metastasis |
| Pathway Analysis | Co-IP, mass spectrometry, luciferase reporter, ChIP | Ovarian Cancer (FBXO45) [25], PCa (USP21/YBX1/HIF1-α) [109] | Identified Wnt/β-catenin, HIF1-α signaling involvement |
| Clinical Correlation | Tissue microarrays, IHC, patient-derived organoids | PCa (USP21) [109], Colon Cancer (ARHGAP4, SIAH2) [108] | Confirmed expression patterns and clinical relevance |
Pathway Visualization: FBXO45 in Ovarian Cancer
The FBXO45 gene, identified as a key component in the ovarian cancer UbRG signature, exemplifies the mechanistic insights gained from experimental validation [25]. The diagram below illustrates its functional role in cancer progression.
Diagram 2: FBXO45 Mechanism in Ovarian Cancer. Experimental validation confirmed FBXO45 promotes ovarian cancer growth, spread, and migration via the Wnt/β-catenin pathway [25].
The Scientist's Toolkit: Essential Research Reagents
Table 3: Essential Research Reagents for UbRG Investigation
| Reagent/Category | Specific Examples | Application | Study References |
|---|---|---|---|
| Cell Culture | DMEM/RPMI 1640 media, FBS, penicillin-streptomycin | Maintenance of cancer cell lines | [25] [107] |
| Molecular Biology Kits | RNAiso Reagent, RNA Reverse Transcription Kit, Real-time PCR kits | Gene expression analysis | [25] [107] |
| Transfection Reagents | Lipofectamine 2000/3000 | Genetic manipulation (overexpression/knockdown) | [25] [109] |
| Protein Analysis | RIPA lysis buffer, protease inhibitors, ECL chemiluminescent | Western blotting, protein detection | [25] [109] |
| Functional Assays | CCK-8, Matrigel, crystal violet, Transwell chambers | Proliferation, invasion, migration assays | [107] [109] |
| Antibodies | GAPDH, FBXO45, WNT1, β-cadherin, c-myc | Target protein detection | [25] |
| Specialized Reagents | Bay-805 (USP21 inhibitor) | Therapeutic targeting of deubiquitinases | [109] |
Clinical and Therapeutic Implications
Immune Microenvironment Associations
UbRG signatures demonstrate consistent associations with tumor immune landscapes, informing immunotherapy response prediction:
In ovarian cancer, the low-risk UbRG group showed significantly higher levels of CD8+ T cells (P<0.05), M1 macrophages (P<0.01), and follicular helper T cells (P<0.05) [25], suggesting a more immunologically active microenvironment.
Colon cancer patients in the low-risk UbRG group demonstrated better response to CTLA4 checkpoint inhibitors [108], providing potential guidance for immunotherapy selection.
Differential immune checkpoint expression between UbRG risk groups has been observed in cervical cancer [16], indicating variable susceptibility to immune checkpoint blockade.
Therapeutic Targeting Potential
UbRG signatures not only prognosticate outcomes but also reveal therapeutic opportunities:
Risk stratification informs chemotherapy response, with high-risk UbRG groups showing lower IC50 values for various chemotherapeutic agents in lung adenocarcinoma [26].
Specific UbRG components represent direct drug targets, as demonstrated by the efficacy of Bay-805, a USP21 inhibitor, in suppressing prostate cancer progression [109].
UbRG signatures may guide patient selection for emerging proteolysis-targeting chimera (PROTAC) therapies, which exploit ubiquitination machinery for targeted protein degradation [25].
Validated ubiquitination-related gene signatures represent robust tools for prognostic stratification across diverse cancer types. The consistent methodology for signature development—spanning bioinformatics discovery, statistical modeling, and experimental validation—ensures reproducible and biologically relevant results. These signatures provide insights into cancer biology through their association with key signaling pathways and immune microenvironment composition, while simultaneously offering clinical utility for outcome prediction and treatment selection. As the ubiquitin field continues to evolve, these multi-gene signatures will likely play an increasingly important role in precision oncology approaches.
Independent Cohort Validation and Cross-Platform Consistency
The evaluation of ubiquitination-related gene (URG) signatures for cancer prognosis has emerged as a significant area of translational research. These molecular signatures, often derived from large-scale genomic databases like The Cancer Genome Atlas (TCGA), promise to enhance clinical decision-making through precise risk stratification. However, their transition from computational discovery to clinical application depends critically on two fundamental principles: independent cohort validation, which assesses generalizability across distinct patient populations, and cross-platform consistency, which ensures performance stability across different measurement technologies. This review systematically examines current evidence regarding the validation of URG signatures across multiple cancer types, providing researchers with a comprehensive analysis of methodological approaches and performance metrics.
Comparative Analysis of Validation Studies
Validation Frameworks Across Cancer Types
Table 1: Independent Validation of Ubiquitination-Related Gene Signatures Across Cancers
| Cancer Type | Signature Size (Genes) | Discovery Cohort | Validation Cohort(s) | Key Performance Metrics | Reference |
|---|---|---|---|---|---|
| Ovarian Cancer | 17 | TCGA-OV (376 tumors) | GSE165808 (49 samples), GSE26712 (153 samples) | 1-year AUC: 0.703, 3-year AUC: 0.704, 5-year AUC: 0.705 | [25] [17] |
| Cervical Cancer | 5 | Self-seq + TCGA-GTEx-CESC | TCGA-CESC training/test sets | 1/3/5-year AUC > 0.6 | [16] [104] |
| Cervical Cancer | 13 | TCGA-CESC | GEO datasets (GSE52903, GSE44001) | Significant risk stratification (log-rank p < 0.05) | [110] |
| Colorectal Cancer | 14 | TCGA-CRC | GSE17536 (177 samples), GSE87211 (203 samples) | Significant survival difference between risk groups (p < 0.05) | [100] |
| Lung Adenocarcinoma | 4 | TCGA-LUAD | 6 GEO datasets (GSE30219, GSE37745, etc.) | HR = 0.58, 95% CI: 0.36-0.93, pmax = 0.023 | [26] |
The validation approaches for ubiquitination-related gene signatures demonstrate remarkable consistency in methodology across different cancer types. Researchers typically employ a split-sample approach, dividing discovery cohorts into training and test sets, followed by external validation using completely independent datasets from repositories like the Gene Expression Omnibus (GEO). This multi-cohort verification strategy provides evidence that URG signatures capture fundamental biological mechanisms rather than cohort-specific artifacts.
For ovarian cancer, a 17-gene signature demonstrated consistent predictive accuracy across multiple time points, with area under the curve (AUC) values remaining stable between 0.703-0.705 at 1, 3, and 5 years [25]. This temporal consistency suggests robust prognostic capability throughout the clinical course. Similarly, in lung adenocarcinoma, a 4-gene signature (DTL, UBE2S, CISH, and STC1) validated across six independent GEO datasets consistently identified high-risk patients with significantly worse outcomes (HR = 0.58, 95% CI: 0.36-0.93) [26].
Cross-Platform Consistency in Transcriptomic Measurement
Table 2: Cross-Platform Performance of Ubiquitination-Related Gene Signatures
| Study Context | Primary Platform | Validation Platform | Consistency Metrics | Technical Challenges Noted | |
|---|---|---|---|---|---|
| Cervical Cancer (5-gene signature) | RNA sequencing (Self-seq) | Microarray (TCGA-GTEx) | Maintained prognostic significance (AUC > 0.6) | Normalization between platforms required | [16] |
| Cervical Cancer (13-gene signature) | RNA sequencing (TCGA) | Microarray (GEO datasets) | Stable risk stratification in external cohorts | Batch effect correction applied | [110] |
| Colorectal Cancer | Microarray (TCGA) | Multiple microarray platforms (GEO) | Consistent prognostic performance | Cross-platform normalization essential | [100] |
| Multi-omics Pan-cancer Analysis | RNA sequencing (TCGA) | Microarray, RNA-seq, clinical assays | Pathway-level consistency identified | Platform-specific bias in expression levels | [111] |
Cross-platform consistency represents a more rigorous test of signature robustness than validation within the same measurement technology. The evaluated studies demonstrate that well-constructed URG signatures maintain prognostic value across different transcriptomic platforms, including RNA sequencing and various microarray technologies.
Research in cervical cancer provides compelling evidence for cross-platform stability. A 5-gene signature (MMP1, RNF2, TFRC, SPP1, and CXCL8) derived from RNA sequencing data maintained prognostic performance when validated on microarray-based datasets [16]. Similarly, a separate 13-gene signature for cervical cancer developed from TCGA RNA-seq data successfully stratified risk in independent GEO datasets generated on different microarray platforms [110]. These findings suggest that the biological signal captured by URG signatures transcends technical variations in measurement approaches.
A critical methodological consideration emerging from these studies is the essential requirement for appropriate batch effect correction and normalization when integrating data across platforms. The consistency observed in these validation efforts suggests that ubiquitination-related processes represent fundamental biological pathways whose measurement remains informative despite technical variations in assessment platforms.
Experimental Protocols for Signature Validation
Standardized Computational Validation Pipelines
The studies examined employed remarkably consistent computational methodologies for signature validation, creating a de facto standard approach in the field:
Data Preprocessing: Rigorous quality control, normalization, and batch effect correction using established bioinformatic packages like "ComBat" or surrogate variable analysis (SVA) to minimize technical variations between discovery and validation cohorts [16] [110].
Risk Score Calculation: Application of standardized formulas where risk score = Σ(Coefficienti × Expressioni) for all signature genes, using coefficients derived from the discovery cohort and applied unchanged to validation datasets [25] [26].
Stratification Approach: Division of patients into high-risk and low-risk groups based on the median risk score from the discovery cohort, maintaining consistent cutoff values across validation sets [100] [110].
Performance Assessment: Evaluation using time-dependent receiver operating characteristic (ROC) curves, Kaplan-Meier survival analysis with log-rank tests, and calculation of hazard ratios (HR) through Cox proportional hazards regression [25] [26].
This methodological standardization enables meaningful comparison across studies and cancer types while providing a framework for evaluating new prognostic signatures.
Experimental Validation of Key Ubiquitination Genes
Beyond computational validation, several studies implemented experimental approaches to verify the functional roles of critical genes within their signatures:
In Vitro Functional Assays: For the ovarian cancer 17-gene signature, FBXO45 was experimentally validated as a key E3 ubiquitin ligase promoting cancer progression through proliferation, migration, and invasion assays in A2780 and HEY cell lines [25] [17].
Pathway Mechanistic Studies: Investigation of underlying mechanisms confirmed that FBXO45 exerts its oncogenic effects through activation of the Wnt/β-catenin signaling pathway, providing biological plausibility for its inclusion in the signature [17].
Additional Experimental Corroboration: In colorectal cancer, HSPA1A was identified as a critical regulator through machine learning approaches, with functional validation demonstrating its role in promoting proliferation, migration, and invasion through epithelial-mesenchymal transition [100].
These experimental validations provide crucial biological context for computational findings, strengthening the case for the clinical relevance of URG signatures by demonstrating their connection to fundamental cancer mechanisms.
Diagram Title: URG Signature Validation Workflow
Key Signaling Pathways in Ubiquitination-Related Prognosis
The biological plausibility of URG signatures is strengthened by their association with established cancer-related pathways:
Wnt/β-catenin Pathway: Identified as a key mechanism through which FBXO45 promotes ovarian cancer progression in the 17-gene signature, connecting ubiquitination to fundamental processes of cell proliferation and metastasis [25] [17].
KRAS/MAPK Pathway: In pancreatic cancer, A2ML1 was found to promote progression through downregulation of LZTR1 expression and subsequent activation of the KRAS/MAPK pathway, driving epithelial-mesenchymal transition [111].
Cell Cycle and p53 Signaling: Pan-cancer analysis of UBE2T revealed enrichment in critical pathways including "cell cycle," "ubiquitin-mediated proteolysis," "p53 signaling," and "mismatch repair" as key mechanisms through which ubiquitination enzymes exert oncogenic effects [18].
Immune-Related Pathways: Multiple studies demonstrated associations between URG signatures and tumor immune microenvironment characteristics, including immune cell infiltration and checkpoint expression, suggesting connections between ubiquitination and cancer immunology [25] [26].
These pathway associations provide mechanistic explanations for the prognostic capability of URG signatures, positioning ubiquitination as a central regulator of multiple cancer hallmarks rather than an isolated cellular process.
Table 3: Essential Research Reagents and Resources for URG Signature Development
| Resource Category | Specific Tools/Solutions | Application Context | Functional Purpose | Representative Examples | ||
|---|---|---|---|---|---|---|
| Bioinformatic Databases | TCGA, GTEx, GEO databases | Signature discovery and validation | Provide transcriptomic and clinical data | TCGA-OV, TCGA-CESC, GSE165808 [25] [16] | ||
| Ubiquitin Gene Curations | UUCD, iUUCD 2.0, MSigDB | Candidate gene identification | Define ubiquitination-related gene sets | 929 UBQ genes from UUCD [25], 1,006 genes from MSigDB [100] | ||
| Computational Packages | "edgeR", "DESeq2", "limma" | Differential expression analysis | Identify differentially expressed genes | OV DEGs with | logFC | ≥ 1, p < 0.01 [25] |
| Statistical Modeling Tools | "glmnet", "survival", "randomForestSRC" | Prognostic model construction | LASSO Cox regression, survival analysis | 17-gene model via LASSO [25], 4-gene via RSF [26] | ||
| Experimental Assays | RT-qPCR, Western blot, Transwell | Experimental validation | Verify gene expression and functional roles | FBXO45 validation in A2780/HEY cells [25] [17] |
This toolkit represents the essential methodological infrastructure supporting URG signature development and validation. The consistency of resources across independent studies highlights the establishment of standardized approaches in the field.
Diagram Title: URG-Associated Signaling Pathways
The independent validation of ubiquitination-related gene signatures across multiple cancer types and technological platforms provides compelling evidence for their robustness and potential clinical utility. The consistent methodological approaches emerging across studies represent a maturation of the field, while experimental verification of key signature genes establishes biological plausibility. Future research directions should include validation in prospective clinical cohorts, standardization of analytical pipelines, and exploration of ubiquitination-specific therapeutic interventions like PROTACs that could translate these prognostic findings into targeted treatment strategies.
Comparative Analysis of Different Ubiquitination Enzyme Families as Biomarkers
Within the realm of cancer research, the ubiquitin-proteasome system (UPS) has emerged as a critical regulator of cellular homeostasis, influencing nearly all biological processes, from cell cycle progression and DNA damage repair to immune responses [21]. The ubiquitination process is mediated by a sequential enzymatic cascade involving ubiquitin-activating enzymes (E1), ubiquitin-conjugating enzymes (E2), and ubiquitin ligases (E3), which collectively confer substrate specificity [16] [21]. Dysregulation of these enzymes is a hallmark of various cancers, making them attractive targets for prognostic biomarkers and therapeutic interventions. This guide provides a comparative analysis of the prognostic value of E1, E2, and E3 enzyme families across multiple cancer types, supported by experimental data and detailed methodologies, to inform researchers and drug development professionals.
Methodological Approaches for Ubiquitination Biomarker Discovery
The identification and validation of ubiquitination-related biomarkers rely on a consolidated workflow that integrates bioinformatics, machine learning, and experimental validation. The typical research pipeline involves the following key stages:
Data Acquisition and Preprocessing: Publicly available transcriptomic datasets from sources such as The Cancer Genome Atlas (TCGA) and the Gene Expression Omnibus (GEO) are primary resources. These datasets provide gene expression profiles from both tumor and normal adjacent tissues for differential expression analysis [28] [16] [26]. Ubiquitination-related genes (URGs) are compiled from databases like the iUUCD 2.0 and UUCD, or by searching repositories like GeneCards with relevant keywords [26] [17].
Differential Expression and Prognostic Analysis: Differentially expressed genes (DEGs) between cancerous and normal tissues are identified using R packages such as limma or DESeq2, with thresholds commonly set at |log2 fold change| > 0.5 and an adjusted p-value < 0.05 [28] [16]. The intersection of DEGs and URGs yields ubiquitination-related differentially expressed genes (URDEGs). The prognostic value of these URDEGs is then assessed using univariate Cox regression analysis, with Kaplan-Meier survival curves visualizing the survival differences between patient groups with high and low gene expression [28] [16] [17].
Feature Selection and Model Construction: To avoid overfitting and identify the most robust biomarkers, machine learning algorithms are employed. The Least Absolute Shrinkage and Selection Operator (LASSO) Cox regression is frequently used for feature selection [16] [26] [27]. Random Forest and Support Vector Machine-Recursive Feature Elimination (SVM-RFE) are also common choices [32] [33]. A prognostic risk model is then constructed based on the expression of the selected genes and their regression coefficients from multivariate Cox analysis. Patients are stratified into high-risk and low-risk groups based on the median risk score [16] [26] [17].
Validation and Functional Characterization: The prognostic model's performance is validated using independent external datasets and evaluated by time-dependent Receiver Operating Characteristic (ROC) curves and calibration plots [16] [17]. The biological functions and signaling pathways associated with the biomarker genes are investigated through Gene Ontology (GO) and Kyoto Encyclopedia of Genes and Genomes (KEGG) enrichment analyses [28] [16]. Furthermore, the tumor immune microenvironment is analyzed using algorithms like CIBERSORT and ESTIMATE to explore correlations between biomarker expression and immune cell infiltration [16] [17] [33].
Experimental Validation: Finally, the expression trends of key biomarker genes are confirmed experimentally in cell lines or patient tissues using techniques such as quantitative reverse transcription polymerase chain reaction (RT-qPCR) and western blot analysis [28] [32] [16].
The following diagram illustrates this complex research workflow.
Comparative Analysis of Ubiquitination Enzyme Families
The prognostic utility of specific enzymes from the E1, E2, and E3 families has been systematically investigated across numerous cancers. The following table summarizes key biomarkers, their enzyme family, associated cancers, and primary prognostic value.
Table 1: Prognostic Ubiquitination Enzyme Biomarkers in Cancer
| Enzyme Family | Key Biomarker | Cancer Type | Prognostic Value | Proposed Function/Pathway |
|---|---|---|---|---|
| E2 | UBE2S | Lung Adenocarcinoma (LUAD) [26] | Poor Prognosis [26] | Cell cycle regulation [26] |
| E2 | UBE2R2 | Crohn's Disease [32] | Diagnostic Biomarker [32] | Correlated with M2 macrophage infiltration [32] |
| E3 Ligase | BIRC3 | Breast Cancer (BC) [27] | Component of prognostic signature [27] | Part of a 6-gene risk model [27] |
| E3 Ligase | FBXO45 | Ovarian Cancer (OV) [17] | Promotes growth & migration [17] | Activates Wnt/β-catenin pathway [17] |
| E3 Ligase | RNF2 | Cervical Cancer (CC) [16] | Component of prognostic signature [16] | Part of a 5-gene risk model [16] |
| E3 Ligase | NEDD4L | Crohn's Disease [32] | Diagnostic Biomarker [32] | Positively correlated with M2 macrophage infiltration [32] |
| E3 Ligase | TRIM68 | Tuberculosis (as a model) [33] | Immune Process Regulation [33] | Correlates with immune cell infiltration [33] |
E1 Enzymes
The E1 family, comprising only a few enzymes, initiates the ubiquitination cascade. While they are less frequently reported as standalone prognostic biomarkers in the analyzed literature compared to E2 and E3 enzymes, their activity is fundamental to the entire process. One study calculated scores for ubiquitin families in tuberculosis and found that the E1 score was significantly lower in patients compared to healthy controls, suggesting a potential role in disease pathogenesis [33]. Their broad, non-specific action may limit their utility as precise biomarkers, but they remain critical upstream regulators.
E2 Enzymes
E2 enzymes, which work in concert with E3 ligases, have demonstrated significant prognostic value. In lung adenocarcinoma (LUAD), high expression of UBE2S is an independent factor for poor prognosis and is associated with higher tumor mutation burden (TMB) and immune infiltration levels [26]. In Crohn's disease, UBE2R2 was identified as a key diagnostic biomarker, with its expression negatively correlated with infiltration of anti-inflammatory M2 macrophages, highlighting its role in immune dysregulation [32]. This positions E2 enzymes as promising biomarkers for predicting patient survival and immune context.
E3 Ligases
E3 ligases, the largest and most diverse enzyme family, confer substrate specificity and are the most extensively studied for their prognostic utility. Their roles are highly context-dependent.
- In Cancer Prognostic Models: Multi-gene signatures incorporating E3 ligases are powerful prognostic tools. In breast cancer, a signature including BIRC3, TRIM45, and FBXL20 accurately stratified patients into high and low-risk groups [27]. Similarly, in cervical cancer, RNF2 was part of a 5-gene signature that effectively predicted patient survival [16].
- In Tumor Progression and Signaling: Specific E3s drive oncogenic pathways. In ovarian cancer, FBXO45 was experimentally validated to promote tumor growth, spread, and migration by activating the Wnt/β-catenin signaling pathway [17].
- In Immune Regulation: The role of E3s extends to the tumor immune microenvironment. For instance, in infectious disease models like tuberculosis, TRIM68 was a hub gene strongly correlated with various immune cells, indicating a crucial role in immune processes [33]. Furthermore, E3s like AIP4 regulate immune checkpoints by mediating the monoubiquitination and subsequent degradation of PD-L1, thereby influencing cancer immune escape [21].
Detailed Experimental Protocols for Key Studies
Protocol 1: Development of a Ubiquitination-Related Prognostic Signature
This protocol outlines the general methodology for constructing and validating a multi-gene prognostic signature, as applied in studies on cervical, lung, and breast cancers [16] [26] [27].
- Cohort Selection and Data Preprocessing: Obtain RNA sequencing (RNA-seq) or microarray data from public repositories (e.g., TCGA, GEO). For TCGA-LUAD, one study included 304 tumor samples and 13 normal samples from the UCSC Xena database [26]. Split the data into training and testing sets, typically in a 7:3 ratio [16].
- Identification of Ubiquitination-Related DEGs: Compile a list of ubiquitination-related genes (URGs) from databases (e.g., iUUCD, GeneCards). Identify differentially expressed genes (DEGs) between tumor and normal tissues using the
limmaorDESeq2R package (|log2FC| > 0.5, adjusted p-value < 0.05). The intersection of DEGs and URGs yields ubiquitination-related DEGs for analysis [28] [16]. - Prognostic Gene Selection: Perform univariate Cox regression analysis on the URDEGs to identify genes significantly associated with overall survival (p < 0.05). Apply a machine learning algorithm, such as LASSO Cox regression, to further shrink the candidate gene set and prevent overfitting [16] [27].
- Risk Model Construction: Calculate a risk score for each patient using the formula: Risk score = Σ (Coeffi * Expri), where Coeffi is the regression coefficient from the multivariate Cox model, and Expri is the expression level of each selected gene [17]. Stratify patients into high-risk and low-risk groups based on the median risk score.
- Model Validation: Validate the model's predictive power in the internal testing set and external independent validation sets (e.g., GEO datasets). Use Kaplan-Meier survival analysis with a log-rank test to compare survival between risk groups. Evaluate the model's accuracy using time-dependent Receiver Operating Characteristic (ROC) curve analysis for 1, 3, and 5-year overall survival [16] [17] [27].
- Correlation with Tumor Microenvironment: Investigate differences in the tumor immune microenvironment between risk groups using the CIBERSORT or ESTIMATE algorithm to quantify immune cell infiltration [16] [17].
Protocol 2: Functional Validation of a Key Ubiquitination BiomarkerIn Vitro
This protocol details the experimental steps for validating the functional role of a key ubiquitination-related gene, as demonstrated for FBXO45 in ovarian cancer [17].
- Cell Culture and Transfection: Culture relevant human cancer cell lines (e.g., A2780 and HEY for ovarian cancer) in appropriate media (e.g., DMEM/RPMI-1640 with 10% fetal bovine serum). Transfect cells with either small interfering RNA (siRNA) to knock down the gene of interest (e.g., FBXO45) or an overexpression plasmid, using a transfection reagent like Lipo8000.
- Functional Assays:
- Cell Proliferation Assay: Assess cell viability and proliferation at 0, 24, 48, and 72 hours after transfection using the Cell Counting Kit-8 (CCK-8) according to the manufacturer's instructions.
- Transwell Assay: Evaluate cell migration and invasion. For the invasion assay, coat the upper chamber of a Transwell insert with Matrigel. Seed transfected cells in the upper chamber with serum-free medium, and place complete medium in the lower chamber. After 24-48 hours of incubation, fix the cells that have invaded through the membrane, stain with crystal violet, and count under a microscope.
- Western Blot Analysis: Lyse transfected cells using RIPA buffer. Separate proteins by SDS-PAGE and transfer to a PVDF membrane. Block the membrane, then incubate with primary antibodies (e.g., anti-FBXO45, anti-β-catenin, anti-c-Myc) overnight at 4°C. After washing, incubate with an HRP-conjugated secondary antibody. Detect the signal using an ECL kit to analyze the expression of the target protein and key components of its putative signaling pathway (e.g., Wnt/β-catenin) [17].
The logical flow from bioinformatics discovery to experimental validation is summarized below.
Successful research in this field relies on a suite of specific reagents, databases, and computational tools. The following table details essential components of the research toolkit.
Table 2: Essential Research Reagents and Resources for Ubiquitination Biomarker Studies
| Category | Item/Source | Function/Application |
|---|---|---|
| Public Databases | TCGA (The Cancer Genome Atlas) | Source of multi-omics data and clinical information for various cancers [28] [16]. |
| GEO (Gene Expression Omnibus) | Repository of publicly available gene expression datasets for discovery and validation [32] [16]. | |
| iUUCD 2.0 / UUCD | Curated databases for identifying ubiquitination-related genes (E1, E2, E3 enzymes) [26] [17]. | |
| Bioinformatics Tools | R package limma / DESeq2 |
Statistical analysis of differential gene expression from microarray or RNA-seq data [28] [16]. |
R package survival / survminer |
Performing Cox regression and generating Kaplan-Meier survival curves [28] [16]. | |
R package glmnet |
Implementing LASSO regression analysis for feature selection [32] [16]. | |
| CIBERSORT / ESTIMATE | Algorithmic deconvolution of transcriptomic data to quantify immune cell infiltration [32] [17]. | |
| Experimental Reagents | siRNA / Plasmid Vectors | For knocking down or overexpressing target genes in cell lines for functional studies [17]. |
| CCK-8 / MTT Reagent | Colorimetric assays for measuring cell proliferation and viability [17]. | |
| Transwell Chambers | Assay systems for evaluating cell migration and invasion capabilities [17]. | |
| Specific Primary Antibodies | Essential for Western Blot and Immunohistochemistry to detect protein expression and pathway activation (e.g., β-catenin, c-Myc) [17]. |
This comparative analysis underscores the significant and distinct prognostic value of different ubiquitination enzyme families in human diseases, particularly cancer. While E1 enzymes act as essential upstream regulators, E2 and E3 enzymes frequently emerge as powerful standalone biomarkers or components of multi-gene prognostic signatures due to their closer proximity to specific cellular processes. The E3 ligase family, with its vast diversity and substrate specificity, represents a particularly rich source of biomarkers and therapeutic targets. The consistency of bioinformatics methodologies, combining differential expression analysis with robust machine learning and survival statistics, provides a reliable framework for future biomarker discovery. The translation of these computational findings through in vitro functional validation, as detailed in the experimental protocols, is crucial for establishing biological relevance and uncovering underlying mechanisms, such as the involvement of the Wnt/β-catenin pathway. For researchers, focusing on the E2 and E3 families within specific cancer types and integrating their analysis with features of the tumor immune microenvironment holds great promise for developing more accurate prognostic tools and informing the development of novel targeted therapies, including PROTACs.
Conclusion
The systematic investigation of ubiquitination-related genes has established their significant value as prognostic biomarkers across multiple cancer types. Research demonstrates that UbRG-based signatures consistently outperform traditional staging systems in predicting patient survival while providing crucial insights into tumor immune microenvironment composition and therapy response. The convergence of evidence from laryngeal, ovarian, pancreatic, and esophageal cancers highlights the universal importance of ubiquitination pathways in cancer biology. Future directions should focus on standardizing detection methodologies, validating signatures in prospective clinical trials, and developing ubiquitination-targeted therapies. As our understanding of context-specific ubiquitination networks deepens, these biomarkers promise to enhance personalized treatment strategies and ultimately improve cancer patient outcomes through more precise prognostic stratification and therapeutic targeting.
References
- 1. Biochemistry, Ubiquitination - StatPearls - NCBI Bookshelf - NIH [https://www.ncbi.nlm.nih.gov/books/NBK556052/]
- 2. The multifaceted roles of deubiquitinating enzymes (DUBs) ... [https://www.nature.com/articles/s41419-025-08052-7]
- 3. Ubiquitin-Conjugating Enzymes in Cancer - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC8227520/]
- 4. Mechanism and disease association of E2-conjugating enzymes [https://pmc.ncbi.nlm.nih.gov/articles/PMC5095918/]
- 5. Advances in deubiquitinating enzymes in lung ... [https://www.jcancer.org/v12p5573.htm]
- 6. A MUB E2 structure reveals E1 selectivity between cognate ... [https://www.nature.com/articles/ncomms12580]
- 7. Selective ubiquitination of drug-like small molecules by the ... [https://www.nature.com/articles/s41467-025-63442-x]
- 8. Opinion Reprogramming SUMO-primed ubiquitylation [https://www.sciencedirect.com/science/article/pii/S0165614725002056]
- 9. E1/E2/E3 Enzyme | Inhibitors [https://www.medchemexpress.com/Targets/E1_E2_E3%20Enzyme.html?srsltid=AfmBOop6jmIo3heI9Wm-Hv2pwBuRCG70of8SeElcFDN1atC57lbgjhTy]
- 10. The role of ubiquitin ligases in regulating immune cell ... [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2025.1625419/full]
- 11. Ubiquitination in macrophage plasticity: from inflammatory ... [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2025.1621328/full]
- 12. The Role of Protein Ubiquitination in the Onset and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12248740/]
- 13. The role of ubiquitin ligases in regulating immune cell ... [https://pubmed.ncbi.nlm.nih.gov/41169371/?utm_source=FeedFetcher&utm_medium=rss&utm_campaign=None&utm_content=02i9GA6P2bIZqSc9xSZsmTslld7_UH_F38AhGIo1Bn9&fc=None&ff=20251031095819&v=2.18.0.post22+67771e2]
- 14. NF-κB and apoptosis: colorectal cancer progression and novel ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12261797/]
- 15. A novel ubiquitination-based molecular signature predicts ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12619766/]
- 16. Identification and validation of ubiquitination-related genes for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12343280/]
- 17. Prognostic model of ubiquitination-related genes in ovarian ... [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2025.1654180/full]
- 18. Comprehensive pan‑cancer analysis reveals ubiquitin ... [https://www.spandidos-publications.com/10.3892/ol.2025.15237]
- 19. Pan-cancer multi-omics profiling reveals ubiquitin D as a ... [https://link.springer.com/article/10.1007/s12672-025-03545-5]
- 20. The role of ubiquitination in tumorigenesis and targeted ... [https://www.nature.com/articles/s41392-020-0107-0]
- 21. Ubiquitination and deubiquitination in cancer [https://molecular-cancer.biomedcentral.com/articles/10.1186/s12943-024-02046-3]
- 22. Progress in Anticancer Drug Development Targeting ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9737479/]
- 23. Ubiquitination in cancer: mechanisms and therapeutic ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12479132/]
- 24. Molecular mechanisms and potential targeting strategies of ... [https://www.spandidos-publications.com/10.3892/or.2025.9000?text=fulltext]
- 25. Prognostic model of ubiquitination-related genes in ovarian ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12450667/]
- 26. Construction of ubiquitination-related risk model for ... [https://www.nature.com/articles/s41598-025-92177-4]
- 27. Construction and validation of a ubiquitination-related ... [https://www.sciencedirect.com/science/article/pii/S2405844024115848]
- 28. Prognostic value of ubiquitination-related differentially ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11635202/]
- 29. The ubiquitin code of RAS proteins: Decoding its role in ... [https://www.sciencedirect.com/science/article/pii/S2589004225012908]
- 30. The ubiquitin-proteasome system: A potential target for ... [https://pubmed.ncbi.nlm.nih.gov/40370547/]
- 31. Microarray-based analysis and clinical validation identify ... [https://jhoonline.biomedcentral.com/articles/10.1186/s13045-016-0356-0]
- 32. Identification of ubiquitination-related key biomarkers and ... [https://www.nature.com/articles/s41598-025-88148-4]
- 33. Identification and validation of ubiquitination-related ... [https://www.aging-us.com/article/205198/text]
- 34. Harnessing Mass Spectrometry for Biomarker Discovery in ... [https://blog.crownbio.com/biomarker-and-mass-spectrometry-aml]
- 35. The Global Neurodegeneration Proteomics Consortium [https://www.nature.com/articles/s41591-025-03834-0]
- 36. Constructing a pancancer ubiquitination regulatory network to ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12382526/]
- 37. Comprehensive pan-cancer analysis reveals ubiquitin ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12402753/]
- 38. How To Download Gene Expression Data From TCGA and ... [https://ngs101.com/how-to-download-gene-expression-data-from-tcga-and-gtex-using-r-a-complete-guide-for-cancer-genomics-research/]
- 39. Gene Expression Omnibus - NCBI - NIH [https://www.ncbi.nlm.nih.gov/geo/]
- 40. Genotype-Tissue Expression Project (GTEx) [https://www.genome.gov/Funded-Programs-Projects/Genotype-Tissue-Expression-Project]
- 41. Identification of crucial ubiquitin-associated genes for ... [https://www.sciencedirect.com/science/article/abs/pii/S0378111924000969]
- 42. GEO2R - GEO - NCBI - NIH [https://www.ncbi.nlm.nih.gov/geo/geo2r/]
- 43. Multi-omics data-based modeling reveals tumorigenesis [https://pmc.ncbi.nlm.nih.gov/articles/PMC12604227/]
- 44. A machine learning-based investigation of integrin ... [https://www.nature.com/articles/s41598-025-89497-w]
- 45. Prognostic Signature, Immune Features, and Therapeutic ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9398812/]
- 46. Ubiquitination-Related Gene Signature, Nomogram and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11276148/]
- 47. Ubiquitin-proteasome Pathway-linked Gene Signatures as ... [https://ar.iiarjournals.org/content/45/5/1825]
- 48. Identification of Ubiquitin-Related Gene-Pair Signatures for ... [https://www.mdpi.com/2072-6694/14/14/3478]
- 49. A novel ubiquitination-based molecular signature predicts ... [https://link.springer.com/article/10.1007/s00277-025-06668-5]
- 50. Development and validation of G2M signature-based ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12336104/]
- 51. Development of a prognostic model for chemotherapy ... [https://www.nature.com/articles/s41598-025-05556-2]
- 52. Development of a prognostic prediction model based on ... [https://www.nature.com/articles/s41598-025-10592-z]
- 53. A novel machine learning-based immune prognostic signature ... [https://bmccancer.biomedcentral.com/articles/10.1186/s12885-025-13437-0]
- 54. Construction and validation of a novel and superior protein ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9705836/]
- 55. Construction and validation of a prognostic risk model for ... [https://bmcmedgenomics.biomedcentral.com/articles/10.1186/s12920-022-01299-5]
- 56. Nomogram for development and validation of a prognosis ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12554507/]
- 57. Nomogram for the prediction of the prognosis of patients ... [https://www.nature.com/articles/s41598-025-05738-y]
- 58. Genes | Free Full-Text | Ubiquitination-Related Gene Signature, Nomogram and Immune Features for Prognostic Prediction in Patients with Head and Neck Squamous Cell Carcinoma [https://www.mdpi.com/2073-4425/15/7/880]
- 59. Identification of a Ubiquitin Related Genes Signature for Predicting Prognosis of Prostate Cancer - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC8801742/]
- 60. nomogram prediction and comparison with AJCC system [https://pubmed.ncbi.nlm.nih.gov/40679529/]
- 61. Gene signature and prognostic value of ubiquitination-related genes in endometrial cancer - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC9824913/]
- 62. Frontiers | Integration of ubiquitination-related genes in predictive signatures for prognosis and immunotherapy response in sarcoma [https://www.frontiersin.org/journals/oncology/articles/10.3389/fonc.2024.1446522/full]
- 63. Limitations of nomogram models in predicting survival ... [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2025.1547506/full]
- 64. The Clinical Prediction Value of the Ubiquitination Model ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11705054/]
- 65. Prognostic Value of Ubiquitination-Related Genes in Ovarian ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12283211/]
- 66. Cancer Biomarkers: Reflection on Recent Progress, Emerging ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12468363/]
- 67. A novel ubiquitination-related gene signature for overall ... [https://link.springer.com/article/10.1007/s12672-025-01768-0]
- 68. Biomarker Testing in Advanced Cancer: Suboptimal Rates ... [https://ascopost.com/news/july-2025/biomarker-testing-in-advanced-cancer-suboptimal-rates-despite-guideline-recommendations-and-growing-insurance-coverage/]
- 69. Precision cancer medicine 2025: some concerns - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC12439214/]
- 70. Biomarkers Conference 2025 | Clinical Biomarkers 2025 ... [https://biomarkers.cancersummit.org/]
- 71. Understanding Prognostic versus Predictive Biomarkers [https://www.ncbi.nlm.nih.gov/books/NBK402284/]
- 72. The meaning of significant mean group differences for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8601419/]
- 73. Ubiquitination Enzymes in Cancer, Cancer Immune Evasion ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11763706/]
- 74. Ubiquitin-related gene markers predict immunotherapy ... [https://www.nature.com/articles/s41598-024-76945-2]
- 75. Integrated Genomic Analysis of the Ubiquitin Pathway across ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5916807/]
- 76. Ubiquitination in cancer: mechanisms and therapeutic ... [https://pubmed.ncbi.nlm.nih.gov/40537889/]
- 77. Intratumor heterogeneity is biomarker specific and ... [https://www.sciencedirect.com/science/article/abs/pii/S0720048X21001480]
- 78. Prognostic molecular subtype reveals the heterogeneity of ... [https://www.nature.com/articles/s41598-025-96686-0]
- 79. Independent Prognostic Value of Intratumoral ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7308549/]
- 80. Prognostic Value of Ubiquitination-Related Genes in ... [https://pubmed.ncbi.nlm.nih.gov/40697329/]
- 81. Breaking the heterogeneity barrier: a robust prognostic ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12518079/]
- 82. Integrating machine learning and experimental validation ... [https://www.nature.com/articles/s41598-025-23772-8]
- 83. Integrating machine learning and experimental validation ... [https://pubmed.ncbi.nlm.nih.gov/41238648/]
- 84. Pan-cancer landscape of cellular senescence ... [https://www.nature.com/articles/s41598-025-23412-1]
- 85. Human Ubiquitin ELISA Kit (EHRPS27A) - Invitrogen [https://www.thermofisher.com/elisa/product/Human-Ubiquitin-ELISA-Kit/EHRPS27A]
- 86. A High-Throughput Method for Specific, Rapid, Precise and ... [https://www.sciencedirect.com/science/article/abs/pii/S0039914025015681]
- 87. Ubiquitination detection techniques - PMC - PubMed Central [https://pmc.ncbi.nlm.nih.gov/articles/PMC10625345/]
- 88. A High-Throughput Assay for Monitoring Ubiquitination in ... [https://www.frontiersin.org/journals/chemistry/articles/10.3389/fchem.2019.00816/full]
- 89. Current methodologies in protein ubiquitination ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9373315/]
- 90. Highly specific intracellular ubiquitination of a small molecule [https://www.nature.com/articles/s41589-025-02011-1]
- 91. Comparison of immunohistochemistry with immunoassay ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC2362713/]
- 92. Antibody Validation Protocols - How To Choose The Most ... [https://bitesizebio.com/35190/antibody-validation-protocol-and-research/]
- 93. Antibody Validation for Flow Cytometry [https://blog.addgene.org/antibody-validation-for-flow-cytometry]
- 94. Comparing immunoassay and mass spectrometry ... [https://www.sciencedirect.com/science/article/pii/S0306453025001027]
- 95. Adaptive multi-omics integration framework for breast ... [https://www.nature.com/articles/s41598-025-22202-z]
- 96. Multi-omics prognostic marker discovery and survival ... [https://www.nature.com/articles/s41598-025-20572-y]
- 97. Comparative analysis of statistical and deep learning-based ... [https://translational-medicine.biomedcentral.com/articles/10.1186/s12967-025-06662-5]
- 98. Machine learning integration with multi-omics data ... [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2025.1651270/full]
- 99. Prognostic model of ubiquitination-related genes in ovarian ... [https://pubmed.ncbi.nlm.nih.gov/40990020/]
- 100. Integrative analysis of ubiquitination-related genes ... [https://link.springer.com/article/10.1007/s12032-025-02662-z]
- 101. Pan-cancer landscape of UBD/FAT10 and experimental ... [https://www.frontiersin.org/articles/10.3389/fonc.2025.1615898/full]
- 102. A novel ubiquitin-related genes-based signature ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11965687/]
- 103. Pan-cancer multi-omics profiling reveals ubiquitin D as a ... [https://pubmed.ncbi.nlm.nih.gov/41023261/]
- 104. Identification and validation of ubiquitination-related genes ... [https://pubmed.ncbi.nlm.nih.gov/40809844/]
- 105. Identification of biomarkers based on ubiquitin-correlated ... [https://pubmed.ncbi.nlm.nih.gov/40894221/]
- 106. A novel ubiquitin-related genes-based signature ... [https://www.frontiersin.org/journals/pharmacology/articles/10.3389/fphar.2025.1513948/full]
- 107. Integrative analysis of ubiquitination-related genes identifies ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11922989/]
- 108. Exploration of the ubiquitination-related molecular ... [https://www.frontiersin.org/journals/genetics/articles/10.3389/fgene.2024.1292249/full]
- 109. USP21/YBX1/HIF1-α promotes the progression of prostate ... [https://translational-medicine.biomedcentral.com/articles/10.1186/s12967-025-07199-3]
- 110. Identification and validation of a thirteen-gene signature ... [https://link.springer.com/article/10.1007/s12672-025-02459-6]
- 111. Multi-omics integration and machine learning uncover ... [https://translational-medicine.biomedcentral.com/articles/10.1186/s12967-025-06711-z]